04 April 2023: Clinical Research
Accuracy of Coronal Magnetic Resonance Imaging Diagnosis of Multi-Segmental Lumbar Disc Herniation: A Single-Center Retrospective Analysis
Jiantian Li1ABCDEF, Jingyu Jia1A, Tianlong Wu1BC, Jinghong Yuan2ACF, Tao Tang1CF, Zhangyuan Jiang1B, Dingwen He1AC, Xigao Cheng1A*DOI: 10.12659/MSM.938577
Med Sci Monit 2023; 29:e938577
Abstract
BACKGROUND: Multi-segment herniation of lumbar intervertebral discs is a complex lumbar spine disease, and it is difficult to identify the responsible segment using only magnetic resonance imaging (MRI). The present study screened 47 patients with multi-segment lumbar disc herniation (MSLDH) to evaluate coronal magnetic resonance imaging (CMRI) of three-dimensional fast-field echo with water-selective excitation to identify the responsible segment of multi-segment lumbar disc herniation (MSLDH) and to assess the accuracy and utility of CMRI.
MATERIAL AND METHODS: This retrospective study included 44 patients with low back pain or lower-extremity symptoms from January 2019 to December 2021. The imaging (including CMRI) and clinical data of the patients were analyzed by 3 independent, blinded experts. The Kappa statistical method was used to characterize the reader-to-reader reliability to qualitatively evaluate the data.
RESULTS: CMRI showed high diagnostic performance, with 90.2% sensitivity, 94.9% positive predictive value (PPV), 80% negative predictive value (NPV), and 83.4% accuracy, and there were significant differences in hospital length of stay (P=0.013) and surgical bleeding (P=0.006) (P<0.01) between single-segment and multi-segment patients.
CONCLUSIONS: CMRI is highly accurate in revealing the shape, signal, and position of the intraspinal and extraspinal lumbosacral plexus, and reducing surgical segments can help improve postoperative outcomes for patients.
Keywords: Data Accuracy, Lumbosacral Plexus, Multiparametric Magnetic Resonance Imaging, Numbers Needed To Treat, radiculopathy, Spinal Nerve Roots, Humans, Intervertebral Disc Displacement, Reproducibility of Results, Magnetic Resonance Imaging, intervertebral disc, intervertebral disc degeneration, Lumbar Vertebrae
Background
Lumbar disc herniation (LDH) is one of the most common causes of low back pain, and often leads to sciatic nerve radiation pain such as hip pain and lower-extremity pain. With the aging of the population, the number of patients with multi-segment lumbar disc herniation (MSLDH) is gradually increasing [1]. The selection of surgical methods is still controversial. Comparison of surgical resection of a disc that is routinely damaged but does not necessarily produce symptoms with the symptomatic sites selected for surgery has the advantages of shorter surgery time, less traumatic bleeding, less economic burden, fewer complications, and better postoperative function. This is crucial to clearing the symptomatic sites of MSLDH when determining the treatment modality.
In recent clinical research on LDH (lumbar disc herniation), Arslan and Ebraheim [2,3] and others, in lumbar anatomy studies on cadavers, found that the origin of the S1 nerve root is mainly located above the intervertebral disc and the plane of the intervertebral disc; the origin of the L5 nerve root is mainly located at the plane of the intervertebral disc; the origin of the L4 nerve root is mainly below the intervertebral disc; and the origin of the L2 and L3 nerve roots are nearly all below the intervertebral disc. In anatomical studies, the anatomical data obtained from different cadavers are different [4], which may be caused by water loss in the cones and peri-pyramidal tissue that changed in height, thickness, or length. Therefore, according to a series of anatomical studies of MSLDH patients, not all intervertebral disc herniations compress the nerve root and cause ischialgia symptoms. In our past clinical observations, we have reached similar conclusions as in previous studies [2–4].
Since Mixter et al first reported intervertebral disc herniation [5], the diagnosis of intervertebral disc herniation has been continuously improved by use of techniques such as magnetic resonance imaging (MRI), myelography, SNRB (selective nerve root block), and DWI. Clinically, the surgeon determines the operation mode through a comprehensive analysis of the patient’s medical history, physical examination, and imaging examination to diagnose the symptomatic sites. In the 2014 guideline for the diagnosis and treatment of LDH in the journal Spine, it was proposed that MRI is the preferred imaging test for confirming lumbar disc herniation [6]. MRI has good tissue resolution and can clearly show the signal of the nucleus pulposus herniation and the degree of compression of the dura mater, but the continuous direction of the nerve root cannot be displayed, so we cannot determine the status of the herniated disc and nerve root. For patients with MSLDH, ordinary MRI imaging can diagnose most of the compressed herniated intervertebral discs, but it cannot clear the symptomatic sites of MSLDH. Before the introduction of MRI, three-dimensional imaging and traditional myelography were used to confirm and exclude the responsible lesions [7]. The use of selective nerve root block (SNRB) can also be used to identify the LDH segment responsible [8]. CT myelography and SNRB can effectively identify the responsible segment, but both are invasive tests and are not the first choice for diagnosis. At present, there is no non-invasive diagnostic method to identify the symptomatic sites for MSLDH.
In recent years, CMRI research has been continuously reported. CMRI can utilize the long T2 feature of water, retain high sensitivity to water signal in the case of complete attenuation of the magnetization vector of other tissues, and can clearly show the imaging of nerve root orientation. As early as 2012, Woo Mok Byun discussed the role of 3D MR lumbosacral radiculography in the diagnosis of symptomatic extraforaminal disc herniation [9]. In our previous studies, CMRI was used to improve the diagnosis of extremely lateral lumbar intervertebral disc herniation and distinguish between lumbar discs mimicking tumor and schwannomas [10,11]. So Hee Park, Sang Woo Kim, and Sartoretti E studied the value of ProSet MR Or CMRI in multiple lumbar foraminal stenosis and foraminal or extraforaminal lesions at L5-S1 [19–22]. The reliability, sensitivity, and specificity of CMRI in identifying stages of responsibility for MSLDH are unreported; therefore, we screened the data of 47 MSLDH patients coming to the hospital for surgery to evaluate the diagnosis of CMRI.
Material and Methods
Study Design
ETHICS APPROVAL:
This retrospective study was performed at the Second Affiliated Hospital of Nanchang University. This research was approved by the Medical Ethics Committee and Internal Review Board of our hospital, and informed consent was obtained from the patients.
SUMMARY OF PATIENTS:
This study retrospectively included 47 patients with low back pain or lower-extremity symptoms who visited the Second Affiliated Hospital of Nanchang University School of Medicine from January 2019 to December 2021, including 35 males and 12 females, with average age 57 years and age range of 26–87 years.
INCLUSION CRITERIA:
Inclusion criteria: (1) history of low back pain and lower-extremity radiating pain; (2) underwent lumbar spine MRI examination and lumbar spine CMRI examination, and signed informed consent; (3) lumbar spine MRI examination showed multi-segment lumbar disc herniation (MSLDH: there are 2 or more lumbar nucleus pulposus herniations in different degrees, breaking through the annulus fibrosus or deforming the dura mater); and (4) received surgical treatment during hospitalization.
Exclusion criteria: (1) surgical patients with severe disease, such as obvious multi-segment severe compression or complicated infection, scoliosis, or schwannoma; (2) low back pain or lower-extremity symptoms other than LDH; and (3) history of lumbosacral trauma or lumbar surgery and contraindications for MRI.
INSPECTION TECHNIQUES:
The MRI scan sequence was performed using a 3.0T whole-body scanner (GE Medical Systems, UK) with spinal coils. Conventional axial and sagittal MRI fast spin echo was used to obtain MSLDH imaging, including axial T2 (TR, 4180 ms; TE, 102 ms) (TR, repetition time; TE, echo time), sagittal T2 (TR, 2200 ms; TE,120 ms), sagittal T1 (TR, 460ms; TE, 20 ms). Then, the 3D coronal plane sequence was modified: CUBE-MRN sequence (TR, 2000 ms; TE, 32 ms; slice thickness, 1 mm; pixel matrix, 512×256; reverse angle 20°) and fast coronal spin echo images of 2 signal intensities were collected. Finally, the imaging plane was centered on the level of L3 vertebra and was parallel to the longitudinal axis of lumbar spinal cord. ADW 4.6 software was used to reconstruct the coronal plane.
RESEARCH METHODS:
All imaging of patients were analyzed by 2 senior orthopedic surgeons (Jingyu Jia and Xigao Cheng), 2 junior orthopedic surgeons (Tianlong Wu and Dingwen He), and 1 radiologist (Wugen Li). A single-blind design was used during these evaluations, and the statistical analysis was performed by 2 authors (Jinghong Yuan and Tao Tang). According to the intraoperative observation and postoperative efficacy as the criterion standard for identifying responsible segments, comparison of pre-treatment pain with post-treatment pain was made by the visual analog scale (VAS) scores and the Oswestry Disability Index (ODI). We calculated the sensitivity, specificity, reliability, positive predictive rate, negative predictive rate, and accuracy in diagnosis of multi-segmental lumbar disc herniation, and evaluated the impact of the choice of surgical method on the patient after surgery. Three patients were lost to follow-up and were excluded from the study; finally, 44 patients with CMRI and surgery were included in our study.
All collected data were analyzed using IBM SPSS Statistics (SPSS, Inc., Chicago, IL, USA), version 22.0. We calculated the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of CMRI in diagnosing MSLDH. Statistical analysis was performed with the χ2 test and
The agreement between the 2 observers was analyzed using Kappa statistics. Kappa values between 0.00 and 0.20 indicate slight consistency, Kappa values between 0.21 and 0.40 indicate fair consistency, Kappa values between 0.41 and 0.60 indicate moderate consistency, Kappa values between 0.61 and 0.80 indicate basic consistency, and 1.0 indicates complete agreement.
Results
PATIENT POPULATION:
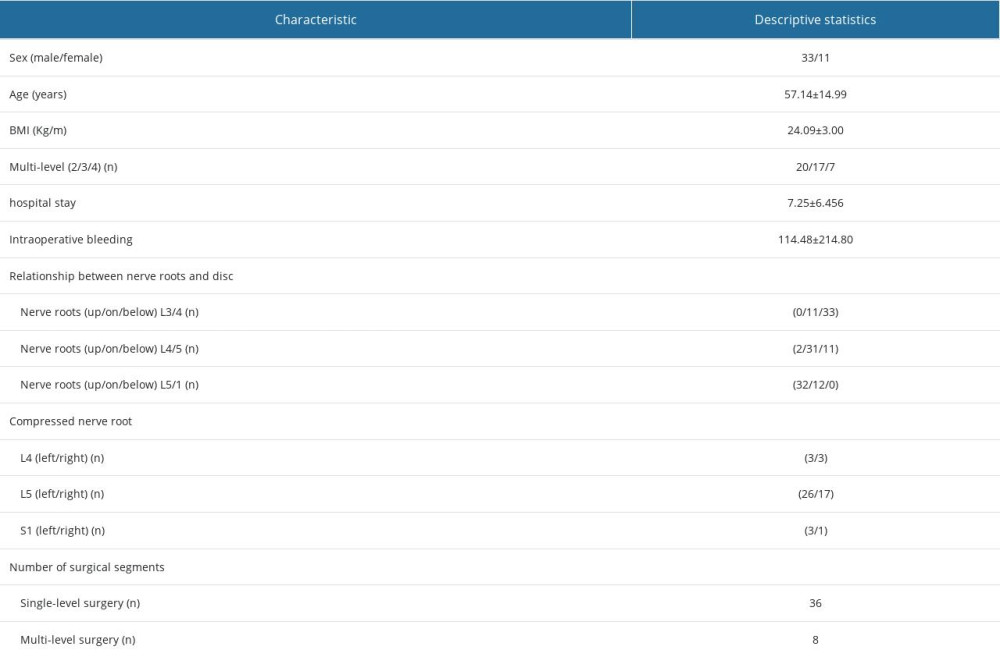
Lumbar MRI and CMRI showed among MLDH patients with several segments injured lumbar discs, 20 had 2 injured segments, 17 had 3 injured segments, and 7 had 4 injured segments. There were 119 herniated intervertebral and 238 nerve roots. Thirty-six patients underwent single-segment surgery, 8 patients underwent multi-segment surgery, 5 patients underwent SNRB, and 13 patients underwent electromyography. We divided the patients into a single-level surgery group and multi-level surgery group according to the number of surgical levels.
THE RELATIONSHIP BETWEEN NERVE ROOTS AND INTERVERTEBRAL DISCS:
We found that in 44 patients the relationship between the nerve root and the intervertebral disc was associated with the nerve root origin (the location of the nerve root from the dural sac) (Table 1). Among them, the origin of the L4/L5 nerve root was located above the intervertebral disc for 70.45%, and the origin of L5/S1 nerve root was located at the plane of the intervertebral disc for 72.73%. On CMRI, there were a series of morphological changes in nerve root compression caused by disc herniation, such as nerve root depression, ganglion enhancement, nerve root swelling, or nerve root disruption (Figure 1). According to intraoperative observation and postoperative efficacy analysis, there were 5 patients with false-negative results of CMRI examination, 1 patient did not improve after the operation due to unclear imaging, 2 patients had no significant improvement in pain symptoms after the operation, and 2 patients had no morphological changes of nerve roots. For patients with uncertain diagnosis, SNRB or routine electromyography should be performed before the operation.
ANALYSIS OF STATISTICS:
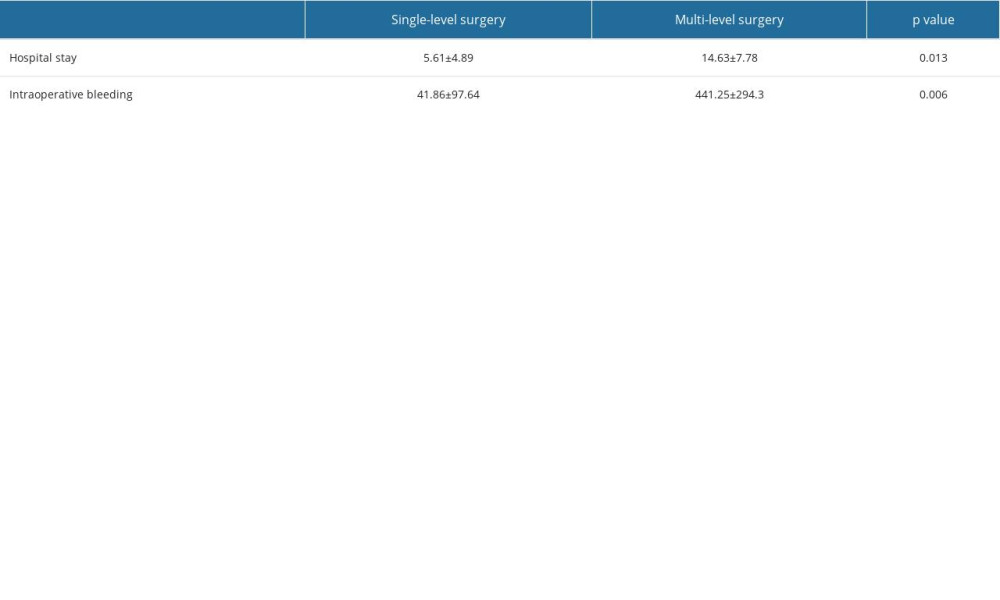
The diagnostic values for CMRI in MSLDH were 90.2% sensitivity, 33.3% specificity, 94.9% positive predictive value (PPV), 80% negative predictive value (NPV), and 83.4% accuracy. Analysis of interobserver agreement for identification the responsible focuses of MSLDH showed substantial agreement, with Kappa 0.808. The mean ODI scores were 3.33 before surgery, 1.93 at 1 month after surgery, 0.83 at 6 months after surgery, and 0.71 at 1 year after surgery. The mean VAS scores were 6.21 before surgery, 1.75 at 1 month after surgery, 0.96 at 6 months after surgery, and 0.8 at 1 year after surgery. Hospital stay (P=0.013) and surgical bleeding (P=0.006) were significantly different (P<0.01) between single-segment and multi-segment patients (Table 2, Figure 2).
Discussion
Lumbar disc herniation (LDH) is one of the most common diseases that cause low back and leg pain. With the aging of the population, the number of patients with multi-segment lumbar disc herniation is increasing. MRI is currently the criterion standard for clinical diagnosis [6]. Conventional MRI scans have a layer thickness of 3–5 mm, so the morphology of nerve roots cannot be clearly displayed. For various complex lumbar disc herniations in multi-segment lumbar disc herniation, unclear diagnosis often occurs [12,13]. In our preliminary studies, we found many patients had symptoms that were not consistent with the imaging. For example, the intervertebral disc bulges up and down along the posterior border of the vertebral body or the intervertebral disc is free, and the MRI scan directly jumps from the intervertebral disc plane to the next intervertebral disc plane, resulting in no lesion site being scanned when the disc is extremely laterally herniated or there is lumbar spondylolisthesis. Therefore, for patients with multi-segment lumbar disc herniation, identifying the site responsible for pain is difficult and controversial. CMRI has high accuracy in displaying the morphology, signal, and location of nerve roots. We sought to further explore the diagnostic value of CMRI in these complex MSLDH cases (Figures 3, 4).
MSLDH (multi-segment intervertebral disc herniation) refers to the presence of 2 or more lumbar nuclei of different degrees that break through the annulus fibrosus or cause compression and deformation of the dura mater. Early studies often used conventional MRI with auxiliary use of SNRB and conventional electromyography to diagnose and formulate surgical plans, and parallel MRI and 3D-MRI examinations for comparative diagnosis and comparative analysis. However, diagnosis is unclear due to different nerve roots in different patients, inconsistent exit locations, asymmetry of the same pair of nerve roots, and different changes in nerve root compression. In the past, some researchers have studied how to identify the responsible segment of lumbar intervertebral disc herniation, but the morphology of nerve roots cannot be shown non-invasively by these methods. Selective nerve root block (SNRB) can be used to diagnose the responsible segment of LDH. However, SNRB is invasive in humans and success is closely related to the clinician’s experience [14]. Lee et al found that myelography can determine the exact cause of radicular pain [15], and the diagnosis of lumbar radiculopathy is better than MRI, but myelography is not a preferred method because it was an invasive examination and has complications such as intracranial hypotension. Jung-Ha Kim summarized 14 diagnostic accuracy studies including 940 patients, showing sensitivity and specificity for different imaging techniques ranged from 76% to 81%, CT, while myelography and MRI showed comparable accuracy [16]. Studies by Liang and Eguchi [17,18] confirmed that decreased FA value and increased ADC value in DTI and DWI are important indicators of lumbosacral nerve root compression, which can be used clinically to quantify LDH-related lumbosacral radiculopathy. Mathematical modeling of diffusion tensor data showed differences in the delineation of ROI at different sites, but the evidence is insufficient to support DTI and DWI as diagnostic tools or predictors of clinical outcomes.
So Hee Park et al used ProSet magnetic resonance coronal imaging to evaluate sensitivity and specificity in patients with multiple lumbar foraminal stenosis, with diagnostic accuracy rates of 84.7% and 82.6% [19]. Sang Woo Kim and Ko Hashimoto studied the significance of CMRI in the diagnosis of L5-S1 foraminal and extraforaminal stenosis [20,21]. Sartoretti used compressed sensing technology to improve 3DMRI resolution to track nerve root paths and diagnose nerve root injuries more accurately [22]. 3DMRI and CMRI can clearly and non-invasively display the complete direction and degree of change of nerve roots, and the effectiveness and reliability of diagnosing lumbar intervertebral disc herniation compared with conventional MRI have been confirmed [23]. In previous studies, we used CMRI nerve root water imaging to improve the sensitivity and reliability of the identification of extraforaminal disc herniation and to differentiate between tumor-like disc herniation and schwannomas [10]; CMRI demonstrated significantly higher sensitivity (91.2%) and specificity (90.3%) than conventional MRI (70.6% and 76.3%), and the results were similar to our finding of 90.2%.
Zheng et al conducted a comprehensive analysis of the prognosis of 112 patients who underwent lumbar spine surgery [19–24], finding surgical fusion of non-responsible segments increase the operation time, intraoperative blood loss, and length of hospital stay, and reduce the range of motion of the lumbar spine, making recovery slower. “Failed Back Surgery Syndrome (FBSS)” may cause prolonged pain in patients due to precise preoperative intervention, further postoperative degeneration, or new lumbar spine lesions [20–25]. Due to age factors, older patients have more and more postoperative complications, have less tolerance of surgery, and more need for lumbar spine mobility than younger people. To demonstrate the effect of the number of surgical levels on patients, we divided our study population of 44 patients into a single-level surgery group and a multi-level surgery group according to the number of surgical levels, and performed univariate analysis. We found that the hospital stay and surgical bleeding were significantly different (
Through our research, we found that CMRI has high accuracy in identifying patients with multi-segment lumbar disc herniation. Since all included patients underwent surgical treatment after diagnosis, the criterion standard for diagnosing the responsible segment is intraoperative findings and postoperative efficacy. The total amount of FP and FN is small, so that the specificity of CMRI is not ideal.
Finally, this study has some limitations. First, due to factors such as use of different imaging equipment, techniques, and external interference, the MRI resolution is different, resulting in clearer imaging of nerve roots in CMRI. Second, due to the retrospective design of the study, the different duration of surgery among patients, and small sample size, selection bias cannot be completely ruled out. We selected the experimental group and control group from a single center, only single-factor chi-square analysis was performed, and the number of study groups was not representative, so it should be compared with other experimental groups with larger sample sizes.
Conclusions
CMRI is highly accurate in revealing the shape, signal, and position of intraspinal and extraspinal lumbosacral plexus, and reducing the number of surgical segments can help improve postoperative outcomes for patients.
Figures
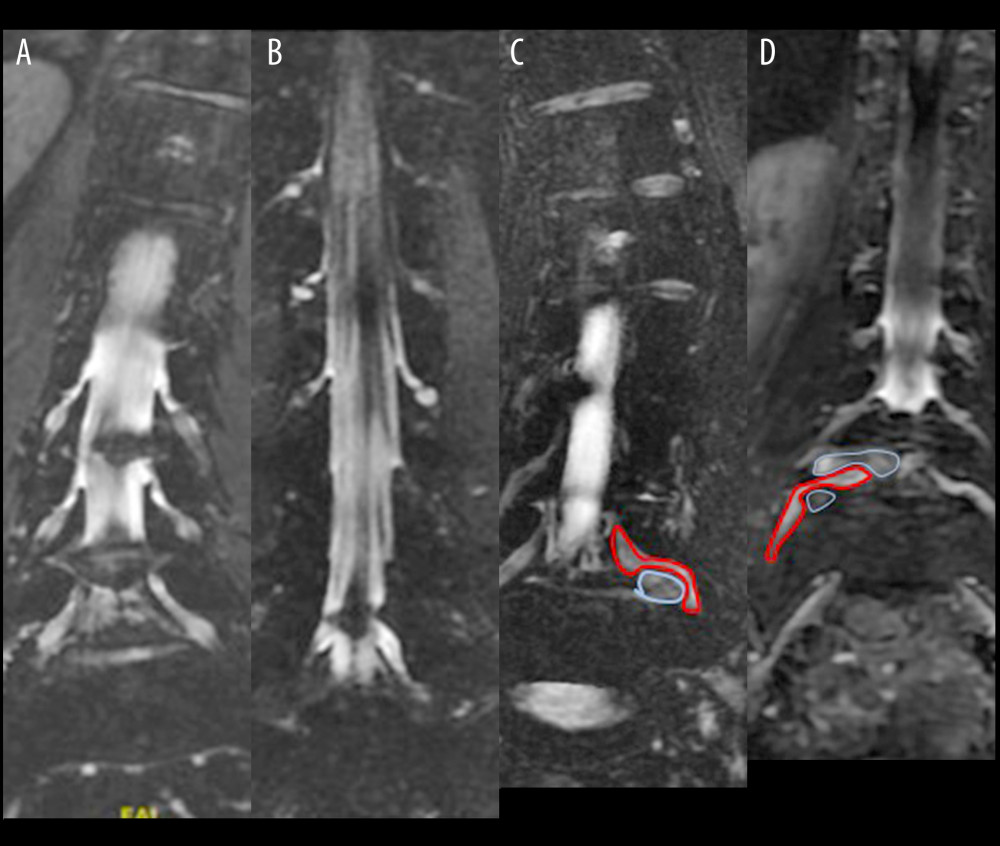 Figure 1. (A) The exit of the L4 nerve root is clear and obvious, and the herniated disc above does not compress the nerve root. In c2, (B) the exit of the L5 nerve root is just at the plane of the herniated disc, showing ganglion enhancement and nerve root interruption. (C) The herniated disc pushes against the ganglion. (D) The L5 nerve root is simultaneously compressed by the upper disc and pushed by the lower disc. MRI – magnetic resonance imaging; CMRI – coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation.
Figure 1. (A) The exit of the L4 nerve root is clear and obvious, and the herniated disc above does not compress the nerve root. In c2, (B) the exit of the L5 nerve root is just at the plane of the herniated disc, showing ganglion enhancement and nerve root interruption. (C) The herniated disc pushes against the ganglion. (D) The L5 nerve root is simultaneously compressed by the upper disc and pushed by the lower disc. MRI – magnetic resonance imaging; CMRI – coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation. 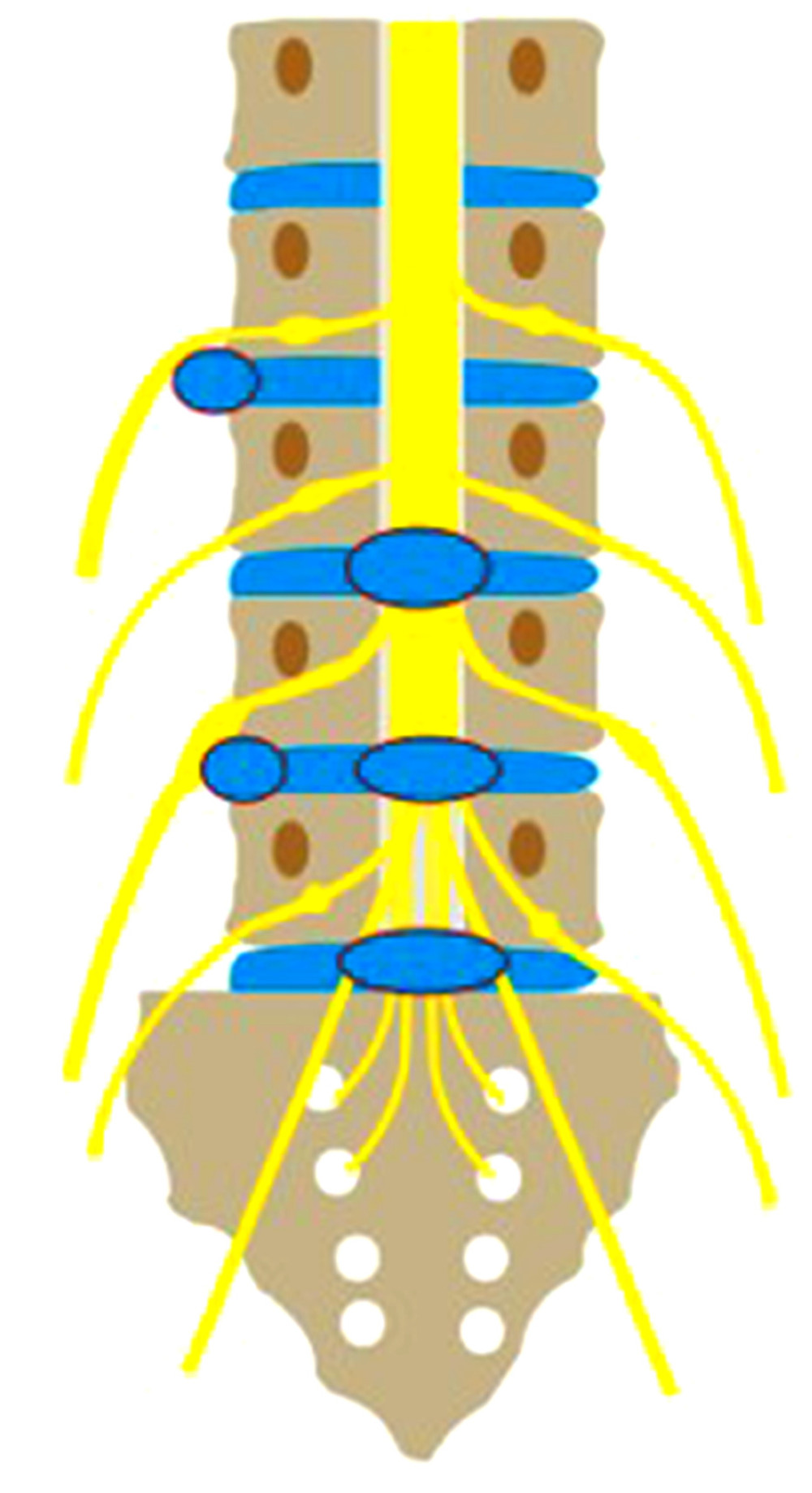 Figure 2. The relationship between the lumbosacral nerve and intervertebral disc herniation.
Figure 2. The relationship between the lumbosacral nerve and intervertebral disc herniation. 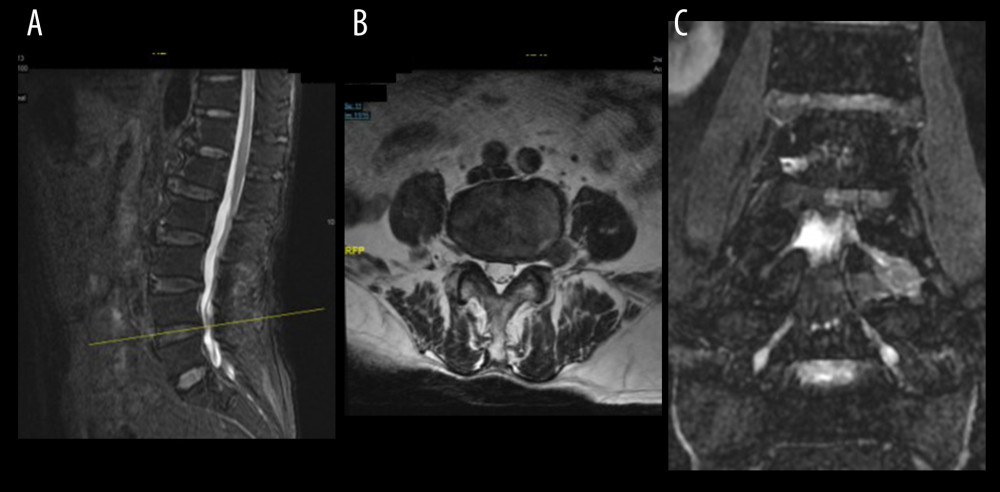 Figure 3. (A) Sagittal MRI localization, (B) Axial t2-weighted image shows good foraminal space, large herniated disc lateral to the foramina (red arrow), (C) CMRI clearly shows herniated disc (red arrow) pushing the squeezed nerve root (yellow arrow) is deformed, and the hyperintensity changes. MRI – magnetic resonance imaging; CMRI – coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation.
Figure 3. (A) Sagittal MRI localization, (B) Axial t2-weighted image shows good foraminal space, large herniated disc lateral to the foramina (red arrow), (C) CMRI clearly shows herniated disc (red arrow) pushing the squeezed nerve root (yellow arrow) is deformed, and the hyperintensity changes. MRI – magnetic resonance imaging; CMRI – coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation. 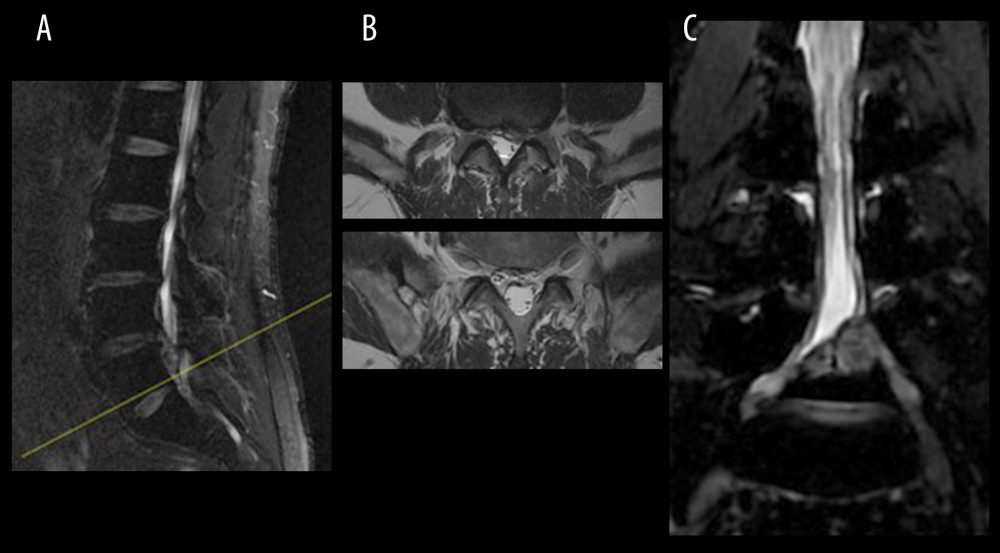 Figure 4. (A) Sagittal MRI localization, a circular low-density shadow can be seen at the posterior edge of the L5 vertebral body, (B) T2-weighted scan shows the b1 axial plane (yellow arrow) of the next scan image b2 axial plane (yellow arrow), just avoiding the circular low signal (red arrow), (C) CMRI clearly shows that the huge herniated intervertebral disc (red arrow) squeezes the nerve root. MRI, magnetic resonance imaging; CMRI, coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation.
Figure 4. (A) Sagittal MRI localization, a circular low-density shadow can be seen at the posterior edge of the L5 vertebral body, (B) T2-weighted scan shows the b1 axial plane (yellow arrow) of the next scan image b2 axial plane (yellow arrow), just avoiding the circular low signal (red arrow), (C) CMRI clearly shows that the huge herniated intervertebral disc (red arrow) squeezes the nerve root. MRI, magnetic resonance imaging; CMRI, coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation. References
1. Strömqvist F, Strömqvist B, Jönsson B, The outcome of lumbar disc herniation surgery is worse in old adults than in young adults: Acta Orthop, 2016; 87(5); 516-21
2. Arslan M, Cömert A, Açar Hİ, Nerve root to lumbar disc relationships at the intervertebral foramen from a surgical viewpoint: An anatomical study: Clin Anat, 2012; 25(2); 218-23
3. Ebraheim NA, Lu J, Morphometric evaluation of the sacral dorsal root ganglia: A cadaveric study. Surg Radiol Anat, 1998; 20(2); 105-8
4. Suh SW, Shingade VU, Lee SH, Origin of lumbar spinal roots and their relationship to intervertebral discs: A cadaver and radiological study: J Bone Joint Surg Br, 2005; 87(4); 518-22
5. Truumees E, A history of lumbar disc herniation from Hippocrates to the 1990s: Clin Orthop Relat Res, 2015; 473(6); 1885-95
6. Kreiner DS, Hwang SW, Easa JE, An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy: Spine J, 2014; 14(1); 180-91
7. McKay G, Torrie PA, Bertram W, Myelography in the assessment of degenerative lumbar scoliosis and its influence on surgical management: Korean J Spine, 2017; 14(4); 133-38
8. Kanna RM, Shetty AP, Rajasekaran S, Predictors of successful outcomes of selective nerve root blocks for acute lumbar disc herniation: Global Spine J, 2019; 9(5); 473-79
9. Byun WM, Jang HW, Kim SW, Three-dimensional magnetic resonance rendering imaging of lumbosacral radiculography in the diagnosis of symptomatic extraforaminal disc herniation with or without foraminal extension: Spine (Phila Pa 1976), 2012; 37(10); 840-44
10. Jia J, Wei Q, Wu T, Two cases in which 3D MRI was used to differentiate between a disc mass that mimics a tumor and neurinoma: BMC Musculoskelet Disord, 2018; 19(1); 154
11. Jia J, Ding R, Liu X, Coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation improves the sensitivity and reliability of identification of extraforaminal lumbar disc herniation: J Int Med Res, 2019; 47(12); 6053-60
12. Zarrabian MM, Diehn FE, Kotsenas AL, Dorsal lumbar disc migrations with lateral and ventral epidural extension on axial MRI: A case series and review of the literature: Am J Neuroradiol, 2016; 37(11); 2171-77
13. Kadler B, Shetye A, Patten DK, A primary inferior lumbar hernia misdiagnosed as a lipoma: Ann R Coll Surg Engl, 2019; 101(4); e96-e98
14. Wolff AP, Groen GJ, Wilder-Smith OH, Influence of needle position on lumbar segmental nerve root block selectivity: Reg Anesth Pain Med, 2006; 31(6); 523-30
15. Park CK, Lee HJ, Ryu KS, Comparison of root images between post-myelographic computed tomography and magnetic resonance imaging in patients with lumbar radiculopathy: J Korean Neurosurg Soc, 2017; 60(5); 540-49
16. Kim JH, van Rijn RM, van Tulder MW, Diagnostic accuracy of diagnostic imaging for lumbar disc herniation in adults with low back pain or sciatica is unknown; A systematic review: Chiropr Man Therap, 2018; 26; 37
17. Dammers R, Koehler PJ, Lumbar disc herniation: Level increases with age: Surg Neurol, 2002; 58(3–4); 209-12
18. Eguchi Y, Oikawa Y, Suzuki M, Diffusion tensor imaging of radiculopathy in patients with lumbar disc herniation: Preliminary results: Bone Joint J, 2016; 98-B(3); 387-94
19. Park SH, Jeon I, Kim SW, Diagnostic values of ProSet magnetic resonance coronal source imaging for detecting symptomatic lesion in multiple lumbar foraminal stenosis: Clin Neurol Neurosurg, 2016; 150; 185-89
20. Hashimoto K, Tanaka Y, Tsubakino T, Imaging diagnosis of lumbar foraminal stenosis in the fifth lumbar nerve root: Reliability and reproducibility of T1-weighted three-dimensional lumbar MRI: J Spine Surg, 2021; 7(4); 502-9
21. Kim SW, Kim CH, Kim MS, Usefulness of three dimensional proset MR images for diagnosis of symptomatic L5-S1 foraminal and extraforaminal stenosis: J Korean Neurosurg Soc, 2013; 54(1); 30-33
22. Sartoretti E, Sartoretti T, Schwenk Á, High-resolution 3D versus standardrsolution 2D T2-weighted turbo spin echo MRI for the assessment of lumbar nerve root compromise: Tomography, 2022; 8(1); 257-66
23. Kong C, Li XY, Sun SY, The value of contrast-enhanced three-dimensional isotropic T2-weighted turbo spin-echo SPACE sequence in the diagnosis of patients with lumbosacral nerve root compression: Eur Spine J, 2021; 30(4); 855-64
24. Zheng F, Cammisa FP, Sandhu HS, Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation: Spine (Phila Pa 1976), 2002; 27(8); 818-24
25. Baber Z, Erdek MA, Failed back surgery syndrome: Current perspectives: J Pain Res, 2016; 9; 979-87
Figures
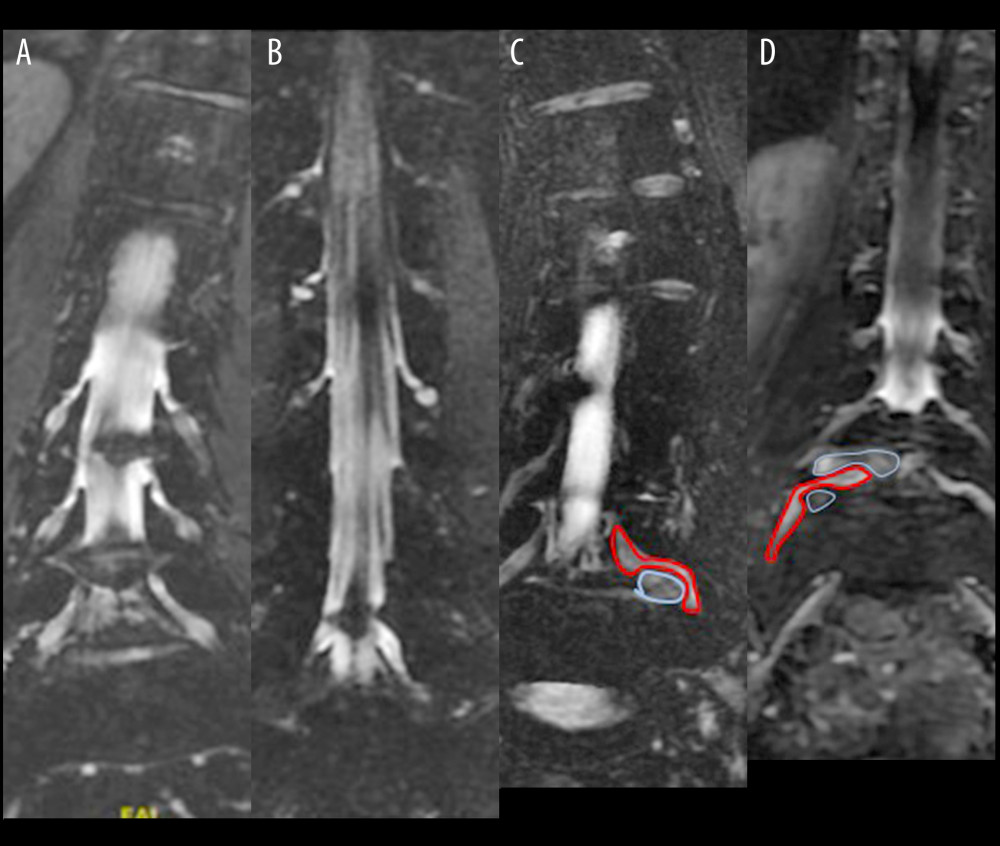 Figure 1. (A) The exit of the L4 nerve root is clear and obvious, and the herniated disc above does not compress the nerve root. In c2, (B) the exit of the L5 nerve root is just at the plane of the herniated disc, showing ganglion enhancement and nerve root interruption. (C) The herniated disc pushes against the ganglion. (D) The L5 nerve root is simultaneously compressed by the upper disc and pushed by the lower disc. MRI – magnetic resonance imaging; CMRI – coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation.
Figure 1. (A) The exit of the L4 nerve root is clear and obvious, and the herniated disc above does not compress the nerve root. In c2, (B) the exit of the L5 nerve root is just at the plane of the herniated disc, showing ganglion enhancement and nerve root interruption. (C) The herniated disc pushes against the ganglion. (D) The L5 nerve root is simultaneously compressed by the upper disc and pushed by the lower disc. MRI – magnetic resonance imaging; CMRI – coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation.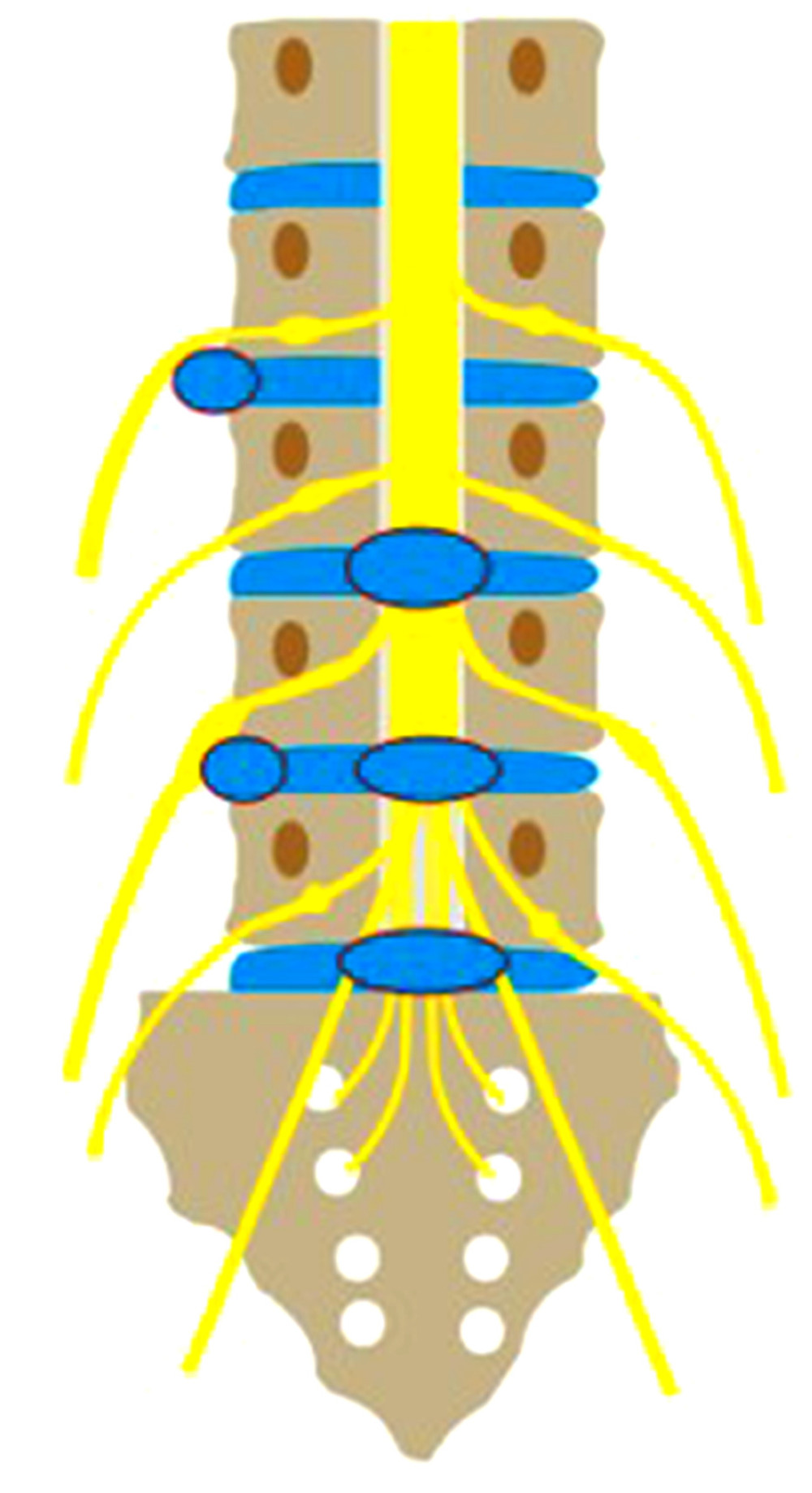 Figure 2. The relationship between the lumbosacral nerve and intervertebral disc herniation.
Figure 2. The relationship between the lumbosacral nerve and intervertebral disc herniation.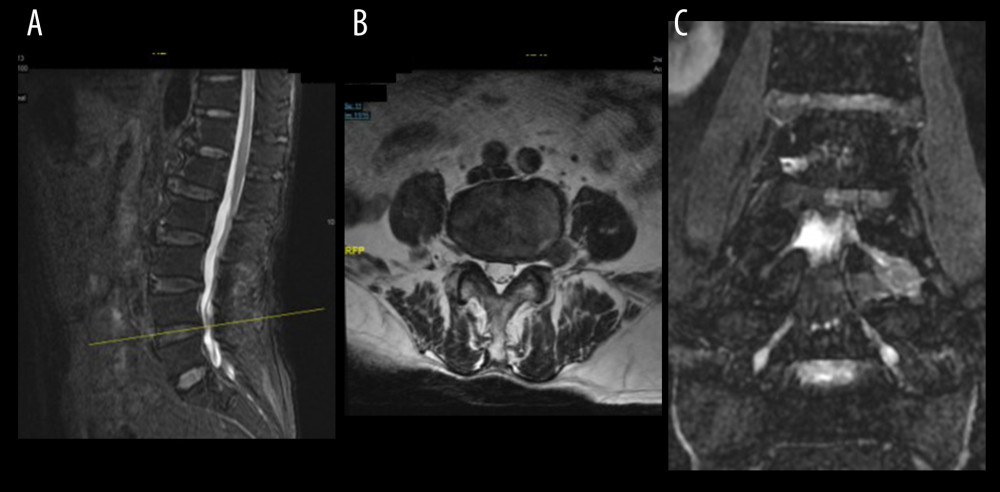 Figure 3. (A) Sagittal MRI localization, (B) Axial t2-weighted image shows good foraminal space, large herniated disc lateral to the foramina (red arrow), (C) CMRI clearly shows herniated disc (red arrow) pushing the squeezed nerve root (yellow arrow) is deformed, and the hyperintensity changes. MRI – magnetic resonance imaging; CMRI – coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation.
Figure 3. (A) Sagittal MRI localization, (B) Axial t2-weighted image shows good foraminal space, large herniated disc lateral to the foramina (red arrow), (C) CMRI clearly shows herniated disc (red arrow) pushing the squeezed nerve root (yellow arrow) is deformed, and the hyperintensity changes. MRI – magnetic resonance imaging; CMRI – coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation.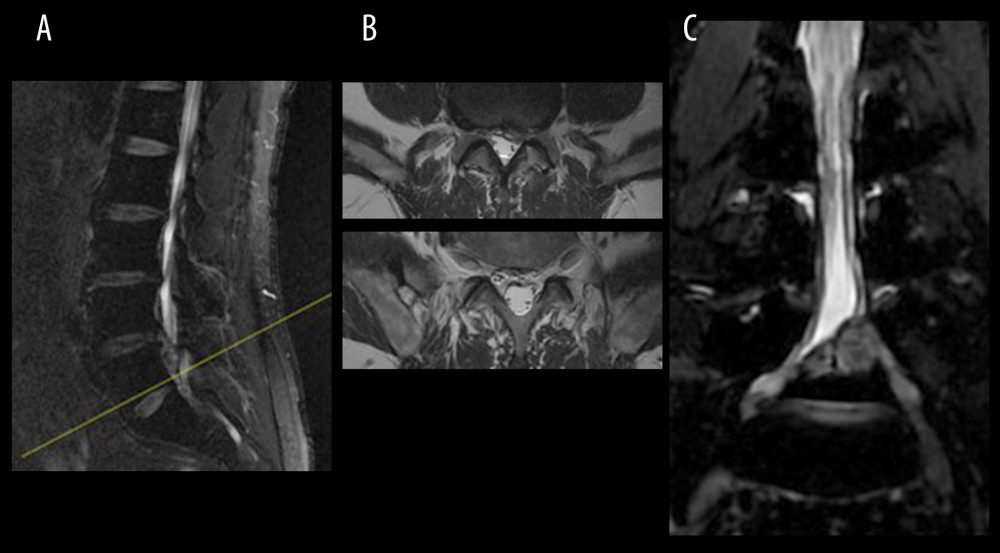 Figure 4. (A) Sagittal MRI localization, a circular low-density shadow can be seen at the posterior edge of the L5 vertebral body, (B) T2-weighted scan shows the b1 axial plane (yellow arrow) of the next scan image b2 axial plane (yellow arrow), just avoiding the circular low signal (red arrow), (C) CMRI clearly shows that the huge herniated intervertebral disc (red arrow) squeezes the nerve root. MRI, magnetic resonance imaging; CMRI, coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation.
Figure 4. (A) Sagittal MRI localization, a circular low-density shadow can be seen at the posterior edge of the L5 vertebral body, (B) T2-weighted scan shows the b1 axial plane (yellow arrow) of the next scan image b2 axial plane (yellow arrow), just avoiding the circular low signal (red arrow), (C) CMRI clearly shows that the huge herniated intervertebral disc (red arrow) squeezes the nerve root. MRI, magnetic resonance imaging; CMRI, coronal magnetic resonance imaging of three-dimensional fast-field echo with water-selective excitation. In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952