10 February 2023: Review Articles
Effect of Acupoint Therapies on Postoperative Sleep Quality: A Narrative Review
Wenxin Wei1E, Xin Huang2E, Junchao Zhu1A*DOI: 10.12659/MSM.938920
Med Sci Monit 2023; 29:e938920
Abstract
ABSTRACT: Several studies have reported that sleep quality often decreases in patients after surgery, especially in elderly patients, which seriously affects postoperative prognosis and outcomes, inducing diseases such as postoperative delirium, long-term chronic pain, and potentially fatal cardiovascular events. With the popularization of comfortable medicine, medical workers pay more attention to the postoperative sleep quality of patients. The causes underlying the decrease in postoperative sleep quality may include postoperative pain, the severity of surgical trauma and stress, perioperative anxiety and depression, and postoperative complications. Patients with insomnia often use acupoint therapies as a safe and effective alternative to drugs. Acupoint therapies are among the oldest medical therapies of Traditional Chinese Medicine and are gradually gaining recognition among medical workers worldwide. Various types of acupoint stimulation methods such as transcutaneous electrical acupoint simulation (TEAS), acupressure, acupuncture, and electroacupuncture can change the brain’s local electrical activity, inhibit the central nervous system, and achieve deep sedation through stimulating the related acupoints, which provides a novel idea and basis for improvement in factors affecting postoperative sleep quality. This review explores the mechanism of acupoint therapies from several aspects of affecting the sleep quality of patients after surgery and its clinical results. We found that acupoint therapies effectively improve sleep quality and alleviate the postoperative complications of patients, and we emphasize the importance of acupoint therapies to guide future research and clinical practice. Large-scale, multicenter studies are needed to determine the optimal duration, frequency, and timing of acupoint stimulation for improving postoperative sleep quality.
Keywords: Acupuncture Points, Acupuncture Therapy, Postoperative Period, sleep quality, Humans, Aged, Transcutaneous Electric Nerve Stimulation, Electroacupuncture, Postoperative Complications
Background
Adequate sleep is essential to physical and mental health. Sleep and circadian rhythm disorders often occur in elderly patients after surgery, characterized by sleep fragmentation, decreased deep non-rapid eye movement (NREM) sleep, the initial decrease and subsequent rebound increase in rapid eye movement (REM) sleep, and daytime sleepiness [1,2]. More than 40% of patients reported sleep problems during the first night after surgery and these problems continued for several days [3]. Studies have found that decreased postoperative sleep quality is harmful to recovery and can lead to negative outcomes such as altered pain perception, cognitive impairment (such as delirium and Alzheimer disease), metabolic derangements, mood disturbances, and proinflammatory changes [4–7]. Vlisides Pet et al [8] indicated that 20–50% of elderly patients have postoperative delirium after major surgery, which is a predictor of mortality and prolonged intensive care unit or hospital stay. Long-term postoperative cognitive dysfunction is also a significant economic burden [9]. Recent evidence has shown that acupoint stimulation is related to increased postoperative sleep quality, and sleep improvement can improve postoperative outcome. Here, we review the evidence regarding the causes of decreased postoperative sleep quality, and the effect of acupoint stimulation on postoperative sleep quality in surgical patients.
Normal Sleep Patterns
Sleep is a vital physiological state that exists in all organisms with neurons and glial networks. It is characterized by decreased consciousness, relative inhibition of sensory activity, inhibition of almost all voluntary muscle activity, and reduced interaction with the surrounding environment [10]. The normal range of sleep duration for adults is 6–10 h, with the majority of the individuals sleeping the recommended 7- to 9-h range, with an average sleep duration of 8 h [11]. In humans, sleep is classified as 2 exclusive states – non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep – whose occurrence is driven by a cyclic organization. NREM sleep is further subdivided into the following stages: N1, N2, and N3, with N3 being designated as slow-wave sleep (SWS). REM sleep accounts for 20–25% of total sleep duration in adults. Typically, a person enters NREM sleep and experiences a sequence of “descending” stages and then an “ascent” (indicating greater brain activity) and enters REM sleep. These cycles repeat every 90–120 min. Owing to these cyclic shifts in sleep stages, SWS or N3 is skewed towards the beginning of the night, while REM sleep is typically skewed towards the end of the night [12]. The characteristics of sleep are relatively stable for a particular individual; however, the sleep duration and architecture vary according to age, individual habits, sleep schedules, and environmental constraints. Sleep structure changes with age. Compared with young people, older people have shorter sleep time, more frequent wake-up, and reduced N3 sleep duration, and tend to get up early [13].
Causes of Declined Postoperative Sleep Quality
PAIN:
Although great progress has been made in perioperative care, surgical patients still commonly experience persistent postoperative pain. Some biopsychosocial risk factors have been identified as important predictors of postoperative pain persistence and long-term poor recovery [17]. The prevalence of chronic pain after surgery ranges from 10–40% [18] and patients with chronic pain exhibit decreased sleep quality (10–36%) [19], such as frequent sleep-stage shifts, increased nocturnal awakenings, and decreased N3 or REM sleep [20]. The relationship of pain with short sleep duration or insomnia has been characterized extensively. It is widely accepted that the relationship between sleep and pain is bidirectional, with pain disrupting sleep and sleep disturbances also being a strong and reliable predictor of pain [2]. For example, it was reported that less than 6 h of sleep per night is associated with more severe pain the following day [21], and lower sleep efficiency is a significant predictor of pain severity after breast surgery [22]. Lack of sleep, both in quantity and in quality, predicts pain in the next 3 years [23]. The following possible underlying mechanisms have been identified in animal experiments: (1) The analgesic effects of endogenous and exogenous opioids depend on the undisturbed sleep structure or sleep continuity. Sleep deprivation may lead to the inhibition of opioid protein synthesis [24] and/or reduced affinity of m- and d-opioid receptors [25]. (2) After 96 h of REM sleep deprivation, the levels of 5-hydroxytryptamine (5-HT) and 5-hydroxyindoleaceticacid in different brain regions were decreased. REM sleep deprivation or continuous sleep interruption in general render the serotonin system functionally could not to support the pain inhibition induced by opioid activation [26]. (3) Other neurotransmitter systems (especially norepinephrine) [27] and neuroimmune factors (especially interleukins) are also affected by sleep deprivation and involved in the regulation of pain. Thus, improving sleep quality appears to reduce pain symptoms [28]. Correspondingly, the treatment of pain can also improve sleep quality.
SURGICAL TRAUMA AND STRESS:
Surgical trauma, stress response, and postoperative pain are the main factors that affect postoperative sleep quality [29]. Lutsey et al [14] demonstrated similar results, showing that major surgery (compared to minor surgery) is related to lower sleep efficiency after surgery. However, minor surgery, such as mastectomy for breast cancer, also produces a small decrease in sleep quality during the night after the operation, and then returns to normal after 2 weeks [30]. Rosenberg-Adamsen et al [31] reported that decreased sleep quality in patients after laparoscopic surgery was less severe, manifesting as decreased N3 sleep but not REM sleep, during the night after surgery; whereas after open surgery, patients had significantly decreased sleep quality manifested as increased N2 sleep, and decreased or lost N3 and REM sleep. In addition, the stress response induced by surgical trauma involves the endocrine metabolic system and inflammatory response, which can last for several days or weeks. Surgical injury followed by a complex stress response is an important cause of postoperative sleep quality decline [32]. The relevant findings are: (1) The inflammatory cytokines tumor necrosis factor (TNF) and interleukin-1 (IL-1) participate in the regulation of sleep. Injection of exogenous TNF or IL-1 can induce all symptoms related to sleep deprivation [33,34]. After administration of IL-1 into the lateral ventricle of rabbits, REM sleep was inhibited, non-REM sleep increased and hyperthermia, which was like that of postoperative patients [35]. (2) Interleukin-6 (IL-6) is also involved in sleep regulation. Preliminary evidence from animal models suggests the intricate contribution of IL-6R signaling to sleep structure [36]. Nocturnal circulating IL-6 levels are associated with the sleep quality; elevated IL-6 levels are associated with sleep interruption, and low levels were associated with good deep sleep [37]. On investigating sleep architecture, Hong et al found that the IL-6 levels were correlated with waking up more frequently during sleep (WASO), less slow-wave sleep, and reduced sleep efficiency [38]. These findings confirm that the magnitude of the surgical trauma and/or stress response may be key pathogenic factors in decreased postoperative sleep quality.
ANXIETY AND DEPRESSION:
Sleep is particularly difficult during hospitalization, considering that the challenges of sleep are multifactorial, hospitalization can cause anxiety and depression in patients due to their health concerns, disturbances from other patients, and an unfamiliar environment. Previous studies have found that patients with persistent anxiety and depression experience disrupted sleep quality such as altered rapid eye movement sleep (REMS) and felt less refreshed after awakening than the non-anxious ones in the first and sixth months after discharge from hospital [39,40]. Recent evidence suggested a bidirectional relationship between psychiatric disorders and sleep disturbances, in which they reinforce each other and share common and overlapping mechanisms. Postoperative sleep is characterized by an initial suppression of rapid eye movement (REM) and slow-wave sleep (SWS). REMS is the main regulator of emotional processes. This fact proves that individuals exposed to traumatic situations usually show fragmentation and reduced time in REMS, and are more likely to develop post-traumatic stress disorder 6 months after trauma [41]. Several studies showed that disturbed sleep can aggravate the consequences that could confer risk of anxiety-related symptoms [42], such as epigenome changes [43], alterations in neuroendocrine function [44], impaired cognitive function [45], and affective dysregulation [46]. Animal studies have suggested that this link is related to the structure of the limbic system due to the following: (1) in sleep-deprived rats, the proliferation of neurons in the dentate gyrus of the hippocampus [47] and the total volume of the hippocampus decreased [48]; (2) sleep-deprived rats also showed increased 5-HT hippocampal turnover [49] with 8 days of sleep restriction decreasing 5-HT1A receptor sensitivity [50], which are 2 well-known depression-related changes; and (3) REM sleep deprivation resulted in increased synthesis and secretion of norepinephrine (NA) in the locus coeruleus [51] and decreased binding capacity of β 1 and β 2 adrenergic receptors in the amygdala and hippocampus (2 brain regions receiving locus coeruleus projection) [52,53].
Acupoint Stimulation Improves Factors Affecting Postoperative Sleep Quality
IMPROVEMENT IN ANXIETY AND DEPRESSION ON ACUPOINT STIMULATION:
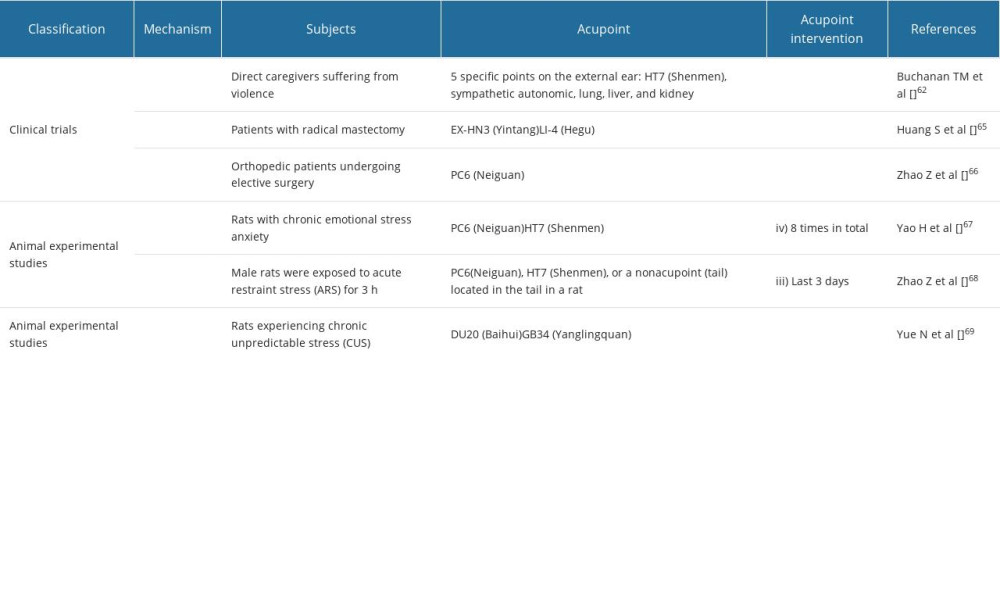
Preoperative and postoperative anxiety and depression are the main factors associated with deceased postoperative sleep quality. Patients with anxiety or depression may experience prolonged sleep onset latency and waking up frequently in the night, resulting in sleep fragmentation and poor sleep efficiency [60]. Patients with depression usually present with reduced REM sleep latency and prolonged REM sleep early in the night, resulting in an increase in the proportion of REM sleep in general [61]. Improving sleep quality in patients with depression can improve their prognosis. Buchanan et al [62] assessed auricular acupuncture therapy conducted 5 times for 30 min each session over 16 weeks, resulting in anxiety relief in different groups, such as healthy volunteers [63] and post-surgical patients [64]. Shujun and Junli found that with low-frequency stimulation, 10 min of TEAS treatment at EX-HN3 (Yintang) and LI-4 (Hegu) acupoints can effectively improve preoperative anxiety of breast cancer patients [65], and Zhifang et al [66] found that acupuncture at PC-6 (Neiguan) for 30 min at 40–50 Hz can reduce preoperative anxiety and improve sleep in patients undergoing elective orthopedic surgery.
Animal studies have found 3 possible underlying mechanisms. (1) The anti-anxiety effect of acupuncture may be related to the up-regulation of atrial natriuretic peptide (ANP) expression and the down-regulation of C-type natriuretic peptide (CNP) expression in peripheral adrenal medulla, thus inhibiting the release of corticosterone (CORT) and activity of the hypothalamus pituitary adrenal axis (HPA) [67]. (2) Acute restraint stress (ARS) is an emotional stressor that can activate a variety of neurochemical, physiological, endocrine, cognitive, and behavioral responses. Acupuncture can inhibit the increase of amygdaloid norepinephrine (NE) and 3-methoxy-4-hydroxy-phenylglycol (MHPG) brought about by ARS. Acupuncture can also prevent ARS-induced enhancements in the protein and mRNA expressions of tyrosine hydroxylase in the central nucleus of the amygdala (CeA) [68]. (3) Chronic unpredictable stress (CUS) can result in depression-related behavioral deficits in rats and neuroinflammation in the hippocampus, such as increased expression of NLRP3, up-regulation of the level of IL-1 βmRNA and IL-1 β mature protein, and activation of microglia. EA treatment can significantly reduce the depression-like behavior caused by CUS. The antidepressant effect of EA is accompanied by a significant decrease in the expression of certain NLRP3 and mature IL-1β. Meanwhile, EA treatment can drastically reverse the increased expression of P2X7 receptor, Iba-1, IL-18, TNF α, and IL-6 expression and decrease the glial fibrillary acidic protein (GFAP) expression induced by CUS [69] (Table 1).
IMPROVEMENT IN PAIN BY ACUPOINT STIMULATION:
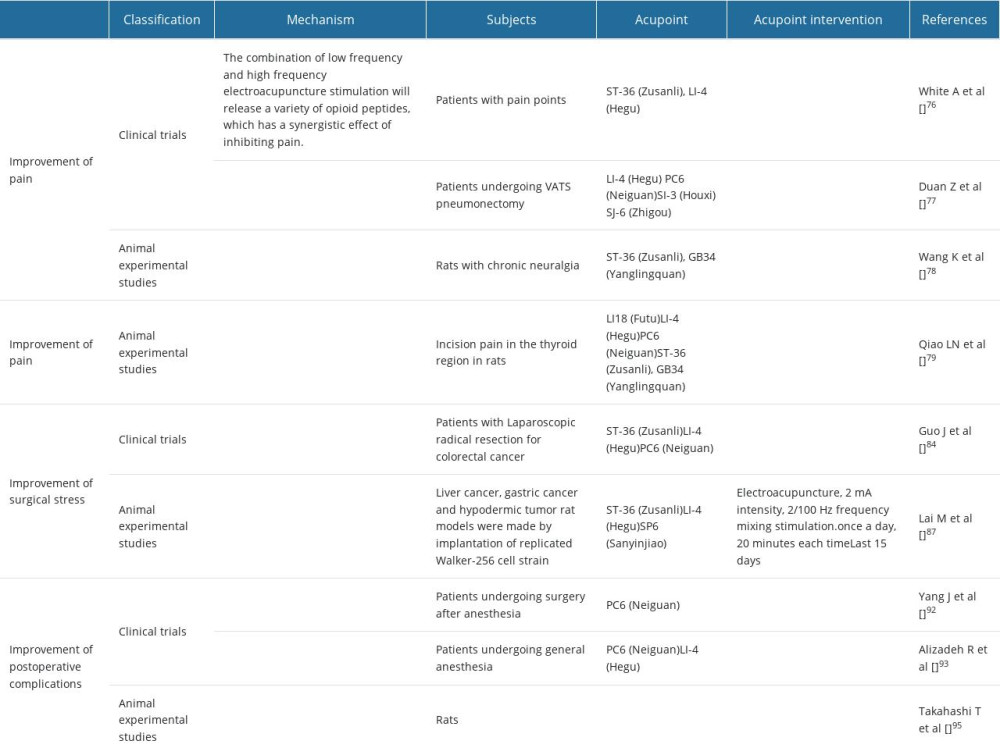
Postoperative pain is a common concern during the perioperative period, which can lead to decreased sleep quality, thus prolonging postoperative recovery time. Acupuncture can be an effective adjunctive intervention for postoperative pain by reducing the required doses of analgesics (mainly opioids) and subsequent complications. For high-risk patients, such as patients with chronic obstructive pulmonary disease or obstructive sleep apnea, the use of acupuncture is particularly valuable because these patients may have complications (mainly respiratory depression) due to use analgesics [70]. Asher et al [71] found that auricular acupuncture can be an effective treatment for several types of pain, especially postoperative pain. Postoperative pain can be reduced after acupoint stimulation at PC6 (Neiguan), GB-21 (Jinajing), LU1 (Zhongfu), LI-11 (Quchi), LI-4 (Hegu), TE-3 (Zhongzhu), TE-5 (Waiguan), and the auricular acupuncture points Shenmen, Heart, Lung, Tooth, Mouth, Uterus, Cushion, Thalamus, Hip, Knee, and Forehead [72–74]. EA also has been reported to alleviate pain and raise the pain threshold by about 20–30% in clinical practice [75]. White et al [76] used EA at ST-36 (Zusanli) and LI-4 (Hegu) with low-frequency (2 Hz) and high-frequency (100 Hz) to provoke the release of various types of endorphins (beta-endorphin, met-enkephalin and dynorphin) to combat pain, and a mixed combination of both low and high frequencies releases various opioid peptides and creates a synergetic effect that inhibits pain [76], which can effectively alleviate postoperative pain and improve postoperative sleep quality. TEAS in bilateral acupoints of LI-4 (Hegu), PC-6 (Nei guan), SI-3 (Houxi), and SJ-6 (Zhigou) at a frequency of 2/100 Hz for 30 min can effectively alleviate pain in elderly patients undergoing thoracoscopic surgery and promote rapid recovery after the operation [77]. There are 2 possible mechanisms in animal experiments: (1) Acupoint stimulation can reduce the pain of rats with chronic neuropathic pain, which may be related to its actions in down-regulating the levels of HMGB1 and its downstream proinflammatory cytokines TNF-α and IL-1 β in the hippocampus [78]. (2) Acupoint stimulation of PC6 (Neiguan) and LI4 (Hegu) can change the phosphorylation level of NR2B subunit of N-methyl-D-aspartate (NMDA) receptor in C1–C3 segment of spinal cord, up-regulate the expression of 5-HT2AR mRNA and protein, and effectively improve pain threshold and relieve pain [79] (Table 2).
IMPROVEMENT IN SURGICAL STRESS BY ACUPOINT STIMULATION:
Surgical pressure and inflammation contribute to the development of postoperative complications, resulting in delayed recovery and decreased sleep quality postoperatively. Clinical trials have shown that perioperative stress activates the sympathetic adrenal medullary system and hypothalamus pituitary adrenal axis, leading to the increase of stress hormones and inflammatory cytokines circulation, which are related to organ dysfunction, postoperative infection, and delayed postoperative recovery [80–83]. These surgical stress reactions and trauma are the main factors affecting postoperative sleep, mainly manifested by the initial inhibition of rapid eye movement (REM) and slow-wave sleep (SWS), and then rebound within 1 week after major surgery. There are 2 mechanisms of action: (1) Acupoint stimulation can reduce inflammation and stress response through regulating the expression of Bcl-2/Bax ratio, Caspase-3, IL-1, IL-6, IL-10, TNF-α and other inflammatory factors [84,85]. (2) Acupoint stimulation treatment can restore suppressed lymphocyte proliferation, increase NK cell activity in the spleen by approximately 44%, and significantly enhance the levels of serum IgM and IgA in postoperative rats with gastric carcinoma, which show that acupoint stimulation can regulate immunity and attenuate anesthesia- and surgery-induced immunosuppression [86,87] (Table 2).
IMPROVEMENT IN POSTOPERATIVE COMPLICATIONS BY ACUPOINT STIMULATION:
Surgery, both major and minor, always carries a risk of postoperative complications. Nausea and vomiting are the most common complications of pain within 24 h after surgery in adults [88]. The incidence of postoperative nausea and vomiting is 30%, while that of laparoscopic surgery is 70% [89]. Although self-limiting, postoperative nausea and vomiting (PONV) can lead to severe morbidity, including bleeding, aspiration pneumonia, electrolyte imbalance and torn sutures [90]. Moreover, PONV leads to postoperative sleep disturbance by disruption of gut microbiome diversity [91]. A review showed that PC6 (Neiguan) flows freely with the adverse flow of qi and regulates the digestive system. Therefore, stimulating the PC6 (Neiguan) acupoint is an effective method to prevent PONV, and acupoint pressing is a non-invasive and supplementary method that can be used to stimulate the PC6 (Neiguan) acupoint to prevent PONV after surgery [92]. The acupoint ST36 (Zu Sanli) helps to relax the gastrointestinal tract and improve the body’s recovery ability after surgery. Simultaneous stimulation of PC6 (Neiguan) and ST36 (Zusanli) can have a synergistic effect, regulating gastrointestinal function under the action of surgery and anesthetics, which can prevent PONV and accelerate gastrointestinal motility [93]. The acupoint ST36 (Zu Sanli) helps to relax the gastrointestinal tract and improve the body’s recovery ability after surgery. Simultaneous stimulation of PC6 (Neiguan) and ST36 (Zusanli) can have a synergistic effect, regulating gastrointestinal function under the action of surgery and anesthetics, which can prevent PONV and accelerate gastrointestinal motility. Animal studies have suggested 3 possible mechanisms: (1) acupoint stimulation can induce release of peripheral opioids to relieve pain and reduce the use of opioids, which can improve postoperative nausea and vomiting [94]. (2) Acupoint stimulation can alleviate delayed gastric emptying through CRF type-2 receptors, which mediates the outflow of parasympathetic efferent pathway [94]. (3) Sympathetic suppression prevents presynaptic catecholamines from blocking the release of parasympathetic acetylcholine [95]. (Table 2)
Conclusions
It is often noticed that sleep quality usually decreases after surgery, especially in elderly patients. Factors related to poor postoperative sleep quality include postoperative pain, the severity of surgical trauma and stress, perioperative anxiety and depression, and several other factors leading to patient discomfort. Various types of acupoint stimulation methods applied at corresponding acupoints can effectively alleviate postoperative pain, relieve perioperative anxiety and depression, improve the level of neurotransmitters in the body, and regulate the biological clock gene through different mechanisms of action, which can be used to improve postoperative sleep quality and may be helpful for postoperative recovery.
References
1. Chung F, Liao P, Yegneswaran B, Postoperative changes in sleep-disordered breathing and sleep architecture in patients with obstructive sleep apnea: Anesthesiology, 2014; 120(2); 287-98
2. Chung F, Liao P, Elsaid H, Factors associated with postoperative exacerbation of sleep-disordered breathing: Anesthesiology, 2014; 120(2); 299-311
3. Chouchou F, Khoury S, Chauny JM, Postoperative sleep disruptions: A potential catalyst of acute pain?: Sleep Med Rev, 2014; 18; 273-82
4. Weinhouse GL, Schwab RJ, Watson PL, Bench-to-bedside review: Delirium in ICU patients – importance of sleep deprivation: Crit Care, 2009; 13; 234
5. Thomas M, Sing H, Belenky G, Neural basis of alertness and cognitive performance impairments during sleepiness. I. Effects of 24 h of sleep deprivation on waking human regional brain activity: J Sleep Res, 2000; 9; 335-52
6. Rosen IM, Gimotty PA, Shea JA, Bellini LM, Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns: Acad Med, 2006; 81; 82-85
7. Copinschi G, Leproult R, Spiegel K, The important role of sleep in metabolism: Front Horm Res, 2014; 42; 59-72
8. Vlisides P, Avidan M, Recent advances in preventing and managing postoperative delirium: F1000Res, 2019; 8; F1000 F aculty Rev-607
9. Leslie DL, Marcantonio ER, Zhang Y, One-year health care costs associated with delirium in the elderly population: Arch Intern Med, 2008; 168; 27-32
10. Lopez R, Barateau L, Dauvilliers Y, Normal organization of sleep and its changes during life: Rev Prat, 2019; 69; 537-45
11. Hirshkowitz M, Whiton K, Albert SM, National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary: Sleep Health, 2015; 1; 40-43
12. McNamara P, Johnson P, McLaren D, REM and NREM sleep mentation: Int Rev Neurobiol, 2010; 92; 69-86
13. Foley DJ, Monjan AA, Brown SL, Sleep complaints among elderly persons: An epidemiologic study of three communities: Sleep, 1995; 18; 425-32
14. Lutsey PL, Bengtson LG, Punjabi NM, Obstructive sleep apnea and 15-year cognitive decline: The Atherosclerosis Risk in Communities (ARIC) study: Sleep, 2016; 39(2); 309-16
15. Chung F, Liao P, Yegneswaran B, Postoperative changes in sleep-disordered breathing and sleep architecture in patients with obstructive sleep apnea: Anesthesiology, 2014; 120; 287-298
16. Rosenberg J, Wildschiødtz G, Pedersen MH, Late postoperative nocturnal episodic hypoxaemia and associated sleep pattern: Br J Anaesth, 1994; 72; 145-50
17. Coppes OJM, Yong RJ, Kaye AD, Urman RD, Patient and surgery-related predictors of acute postoperative pain: Curr Pain Headache Rep, 2020; 24; 12
18. Nickel R, Raspe HH, Chronic pain: Epidemiology and health care utilization: Nervenarzt, 2001; 72; 897-906
19. Smith MT, Edwards RR, McCann UD, Haythornthwaite JA, The effects of sleep deprivation on pain inhibition and spontaneous pain in women: Sleep, 2007; 30; 494-505
20. Lee JS, Jeong DU, Sleep and pain: Sleep Med Psychophysiol, 2012; 19; 63-67
21. Edwards RR, Almeida DM, Klick B, Duration of sleep contributes to next-day pain report in the general population: Pain, 2008; 137; 202-7
22. Wright CE, Bovbjerg DH, Montgomery GH, Disrupted sleep the night before breast surgery is associated with increased postoperative pain: J Pain Symptom Manage, 2009; 37; 352-62
23. Auvinen JP, Tammelin TH, Taimela SP, Is insufficient quantity and quality of sleep a risk factor for neck, shoulder and low back pain? A longitudinal study among adolescents: Eur Spine J, 2010; 19; 641-49
24. Shapiro C, Girdwood P, Protein synthesis in rat brain during sleep: Neuropharmacology, 1981; 20; 457-60
25. Fadda P, Tortorella A, Fratta W, Sleep deprivation decreases mu and delta opioid receptor binding in the rat limbic system: Neurosci Lett, 1991; 129; 315-17
26. Farooqui SM, Brock JW, Zhou J, Changes in monoamines and their metabolite concentrations in REM sleep-deprived rat forebrain nuclei: Pharmacol Biochem Behav, 1996; 54; 385-91
27. Bjorvatn B, Grønli J, Hamre F, Effects of sleep deprivation on extracellular serotonin in hippocampus and frontal cortex of the rat: Neuroscience, 2002; 113; 323-30
28. Dimsdale JE, Ball ED, Carrier E, Effect of eszopiclone on sleep, fatigue, and pain in patients with mucositis associated with hematologic malignancies: Support Care Cancer, 2011; 19; 2015-20
29. Rosenberg-Adamsen S, Kehlet H, Dodds C, Rosenberg J, Postoperative sleep disturbances: mechanisms and clinical implications: Br J Anaesth, 1996; 76; 552-59
30. Hansen MV, Madsen MT, Wildschiødtz G, Sleep disturbances and changes in urinary 6-sulphatoxymelatonin levels in patients with breast cancer undergoing lumpectomy: Acta Anaesthesiol Scand, 2013; 57; 1146-53
31. Rosenberg-Adamsen S, Skarbye M, Wildschiodtz G, Sleep after laparoscopic cholecystectomy: Br J Anaesth, 1996; 77; 572-75
32. Lei M, Zhang P, Liu Y, Propofol and sufentanil may affect the patients’ sleep quality independently of the surgical stress response: A prospective nonrandomized controlled trial in 1033 patients’ undergone diagnostic upper gastrointestinal endoscopy: BMC Anesthesiol, 2017; 17; 53
33. Kapsimalis F, Richardson G, Opp MR, Kryger M, Cytokines and normal sleep: Curr Opin Pulm Med, 2005; 11; 481-84
34. Krueger JM, The role of cytokines in sleep regulation: Curr Pharm Des, 2008; 14; 3408-16
35. Kapás L, Hong L, Cady AB, Somnogenic, pyrogenic, and anorectic activities of tumor necrosis factor-alpha and TNF-alpha fragments: Am J Physiol, 1992; 263; R708-15
36. Oyanedel CN, Kelemen E, Scheller J, Peripheral and central blockade of interleukin-6 trans-signaling differentially affects sleep architecture: Brain Behav Immun, 2015; 50; 178-85
37. Vgontzas AN, Papanicolaou DA, Bixler EO, Circadian interleukin-6 secretion and quantity and depth of sleep: J Clin Endocrinol Metab, 1999; 84; 2603-7
38. Hong S, Mills PJ, Loredo JS, The association between interleukin-6, sleep, and demographic characteristics: Brain Behav Immun, 2005; 19; 165-72
39. Edéll-Gustafsson UM, Hetta JE, Anxiety, depression and sleep in male patients undergoing coronary artery bypass surgery: Scand J Caring Sci, 1999; 13(2); 137-43
40. Seifritz E, Contribution of sleep physiology to depressive pathophysiology: Neuropsychopharmacology, 2001; 25; S85-88
41. Mellman TA, Pigeon WR, Nowell PD, Nolan B, Relationships between REM sleep findings and PTSD symptoms during the early aftermath of trauma: J Trauma Stress, 2007; 20; 893-901
42. Lund HG, Reider BD, Whiting AB, Prichard JR, Sleep patterns and predictors of disturbed sleep in a large population of college students: J Adolesc Health, 2010; 46; 124-32
43. Gaine ME, Chatterjee S, Abel T, Sleep deprivation and the epigenome: Front Neural Circuits, 2018; 12; 14
44. Meerlo P, Sgoifo A, Suchecki D, Restricted and disrupted sleep: Effects on autonomic function, neuroendocrine stress systems and stress responsivity: Sleep Med Rev, 2008; 12; 197-210
45. Cousins JN, Sasmita K, Chee MWL, Memory encoding is impaired after multiple nights of partial sleep restriction: J Sleep Res, 2018; 27; 138-45
46. Reddy R, Palmer CA, Jackson C, Impact of sleep restriction versus idealized sleep on emotional experience, reactivity and regulation in healthy adolescents: J Sleep Res, 2017; 26; 516-25
47. Guzmán-Marín R, Suntsova N, Stewart DR, Sleep deprivation reduces proliferation of cells in the dentate gyrus of the hippocampus in rats: J Physiol, 2003; 549; 563-71
48. Novati A, Hulshof HJ, Koolhaas JM, Chronic sleep restriction causes a decrease in hippocampal volume in adolescent rats, which is not explained by changes in glucocorticoid levels or neurogenesis: Neuroscience, 2011; 190; 145-55
49. Asikainen M, Toppila J, Alanko L, Sleep deprivation increases brain serotonin turnover in the rat: Neuroreport, 1997; 8; 1577-82
50. Novati A, Roman V, Cetin T, Chronically restricted sleep leads to depression-like changes in neurotransmitter receptor sensitivity and neuroendocrine stress reactivity in rats: Sleep, 2008; 31; 1579-85
51. Khanday MA, Somarajan BI, Mehta R, Mallick BN, Noradrenaline from locus coeruleus neurons acts on pedunculo-pontine neurons to prevent REM sleep and induces its loss-associated effects in rats: eNeuro, 2016; 3 ENEURO.0108-16.2016
52. Hipólide DC, Tufik S, Raymond R, Nobrega JN, Heterogeneous effects of rapid eye movement sleep deprivation on binding to alpha- and beta-adrenergic receptor subtypes in rat brain: Neuroscience, 1998; 86; 977-87
53. Charifi C, Debilly G, Paut-Pagano L, Effect of noradrenergic denervation of medial prefrontal cortex and dentate gyrus on recovery after sleep deprivation in the rat: Neurosci Lett, 2001; 311; 113-16
54. World Health Organization, Acupuncture: Review and analysis of reports on controlled clinical trials: Parkinsonism & Related Disorders, 2002
55. Ernst E, Lee MS, Choi TY, Acupuncture for insomnia? An overview of systematic reviews: Eur J Gen Pract, 2011; 17; 116-23
56. Amorim D, Amado J, Brito I, Acupuncture and electroacupuncture for anxiety disorders: A systematic review of the clinical research: Complement Ther Clin Pract, 2018; 31; 31-37
57. Yuan W, Wang Q, Perioperative acupuncture medicine: A novel concept instead of acupuncture anesthesia: Chin Med J (Engl), 2019; 132; 707-15
58. Sahmeddini MA, Farbood A, Ghafaripuor S, Electro-acupuncture for pain relief after nasal septoplasty: A randomized controlled study: J Altern Complement Med, 2010; 16; 53-57
59. Chiou YF, Yeh ML, Wang YJ, Transcutaneous electrical nerve stimulation on acupuncture points improves myofascial pain, moods, and sleep quality: Rehabil Nurs, 2020; 45; 225-33
60. Peterson MJ, Benca RM, Sleep in mood disorders: Sleep Med Clin, 2008; 3; 231-49
61. Benca RM, Obermeyer WH, Thisted RA, Gillin JC, Sleep and psychiatric disorders. A meta-analysis: Arch Gen Psychiatry, 1992; 49; 651-70
62. Buchanan TM, Reilly PM, Vafides C, Dykes P, Reducing anxiety and improving engagement in health care providers through an auricular acupuncture intervention: Dimens Crit Care Nurs, 2018; 37; 87-96
63. Wang SM, Kain ZN, Auricular acupuncture: A potential treatment for anxiety: Anesth Analg, 2001; 92(2); 548-53
64. Wang SM, Peloquin C, Kain ZN, The use of auricular acupuncture to reduce preoperative anxiety: Anesth Analg, 2001; 93; 1178-80
65. Huang S, Si JNursing intervention of preoperative anxiety in breast cancer patients with transcutaneous electrical acupoint simulation: Guangdong Medical Journal, 2009; 30; 1206-7 [in Chinese]
66. Zhao Z, Chen F, Guo XEffect of acupoint stimulation regulation on relieving anxiety of orthopaedic patients undergoing elective surgery: Chin J Nurs, 2019; 54; 696-99 [in Chinese]
67. Yao H, Wei D, Cai D, Effects of acupuncture on ANP and CNP in adrenal gland and CORT in plasma in rats with chronic emotional stress anxiety: Zhongguo Zhen Jiu, 2016; 36; 169-74
68. Zhao Z, Kim SC, Liu H, Manual acupuncture at PC6 ameliorates acute restraint stress-induced anxiety in rats by normalizing amygdaloid noradrenergic response: Evid Based Complement Alternat Med, 2017; 2017; 4351723
69. Yue N, Li B, Yang L, Electro-acupuncture alleviates chronic unpredictable stress-induced depressive- and anxiety-like behavior and hippocampal neuroinflammation in rat model of depression: Front Mol Neurosci, 2018; 11; 149
70. Taghavi R, Tabasi KT, Mogharabian N, The effect of acupuncture on relieving pain after inguinal surgeries: Korean J Pain, 2013; 26; 46-50
71. Asher GN, Jonas DE, Coeytaux RR, Auriculotherapy for pain management: A systematic review and meta-analysis of randomized controlled trials: J Altern Complement Med, 2010; 16; 1097-8
72. Xu M, Zhou SJ, Jiang CC, The effects of P6 electrical acustimulation on postoperative nausea and vomiting in patients after infratentorial craniotomy: J Neurosurg Anesthesiol, 2012; 24; 312-16
73. Liodden I, Howley M, Grimsgaard AS, Perioperative acupuncture and postoperative acupressure can prevent postoperative vomiting following paediatric tonsillectomy or adenoidectomy: A pragmatic randomised controlled trial: Acupunct Med, 2011; 29; 9-15
74. Ward U, Nilsson UG, Acupuncture for postoperative pain in day surgery patients undergoing arthroscopic shoulder surgery: Clin Nurs Res, 2013; 22; 130-36
75. Liu S, Wang B, Li S, Immune cell populations decrease during craniotomy under general anesthesia: Anesth Analg, 2011; 113; 572-77
76. White A, Cummings TM, Filshie J: An introduction to Western Medical Acupuncture, 2008, Churchill Livingstone/Elsevier
77. Duan Z, Wu X, Wang J, Liu FEffects of transcutaneous electrical acupoint stimulation-assisted anesthesia on pain and rapid recovery in elderly patients undergoing thoracoscopic surgery: Chin J Geriatr, 2020; 39; 323-27 [in Chinese]
78. Wang K, Zeng L, Zhou Y, Electroacupuncture relieves pain by down-regulating expression of hippocampal high mobility group protein 1 and contents of TNF-α and IL-1 β in rats with chronic neuropathic pain: Zhen Ci Yan Jiu, 2018; 43; 480-84
79. Qiao L, Yang Y, Liu JEffects of electroacupuncture at Futu on mRNA expression of 5-HT 1A and 5-HT 2A receptors in cervical spinal cord in rats with cervical incision pain: Acupuncture, 2011; 36; 391-94 [in Chinese]
80. Iwasaki M, Edmondson M, Sakamoto A, Ma D, Anesthesia, surgical stress, and “long-term” outcomes: Acta Anaesthesiol, 2015; 53; 99-104
81. Grech D, Li Z, Morcillo P, Intraoperative low-frequency electroacupuncture under general anesthesia improves postoperative recovery in a randomized trial: J Acupunct Meridian Stud, 2016; 9; 234-41
82. Tsigos C, Chrousos GP, Hypothalamic-pituitary-adrenal axis, neuroendocrine factors and stress: J Psychosom Res, 2002; 53; 865-71
83. Lohsiriwat V, Impact of an enhanced recovery program on colorectal cancer surgery: Asian Pac J Cancer Prev, 2014; 15; 3825-28
84. Guo J, Tang W, Guo FTranscutaneous electrical acupoint stimulation on inflammatory response and intestinal permeability in perioperative period of laparoscopic intestinal surgery: Zhongguo Zhen Jiu, 2018; 38; 1043-46 [in Chinese]
85. Feng B, Zhang Y, Luo L, Transcutaneous electrical acupoint stimulation for post-traumatic stress disorder: Assessor-blinded, randomized controlled study: Psychiatry Clin Neurosci, 2019; 73; 179-86
86. Rho SW, Choi GS, Ko EJ, Molecular changes in remote tissues induced by electro-acupuncture stimulation at acupoint ST36: Mol Cells, 2008; 25; 178-83
87. Lai M, Wang S, Zhang WEffects of electroacupuncture on tumor growth and immune function in the Walker-256 model rat: Zhongguo Zhen Jiu, 2008; 28; 607-9 [in Cinese]
88. Brettner F, Janitza S, Prüll K, Gender-specific differences in low-dose haloperidol response for prevention of postoperative nausea and vomiting: A register-based cohort study: PLoS One, 2016; 11; e0146746
89. Ko-Iam W, Sandhu T, Paiboonworachat S, Predictive factors for a long hospital stay in patients undergoing laparoscopic cholecystectomy: Int J Hepatol, 2017; 2017; 5497936
90. Rüsch D, Eberhart LH, Wallenborn J, Kranke P, Nausea and vomiting after surgery under general anesthesia: An evidence-based review concerning risk assessment, prevention, and treatment: Dtsch Arztebl Int, 2010; 107; 733-41
91. Smith RP, Easson C, Lyle SM, Gut microbiome diversity is associated with sleep physiology in humans: PLoS One, 2019; 14(10); e0222394
92. Yang J, Jiang Y, Chen Y, Acupressure the PC6 point for alleviating postoperative nausea and vomiting: A systematic review protocol: Medicine (Baltimore), 2019; 98; e16857
93. Alizadeh R, Esmaeili S, Shoar S, Acupuncture in preventing postoperative nausea and vomiting: Efficacy of two acupuncture points versus a single one: J Acupunct Meridian Stud, 2014; 7; 71-75
94. Zhang GG, Yu C, Lee W, Involvement of peripheral opioid mechanisms in electroacupuncture analgesia: Explore (NY), 2005; 1; 365-71
95. Takahashi T, Mechanism of acupuncture on neuromodulation in the gut – a review: Neuromodulation, 2011; 14; 8-12
In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952