17 January 2023: Clinical Research
Comparison of Outcomes Following Total Hip Arthroplasty Between Patients Diagnosed with Association Research Circulation Osseous (ARCO) Stage III and Stage IV Osteonecrosis of the Femoral Head: A Retrospective Study of 302 Patients
Meng Yang1ABC, Xiangke Li2D, Kung Chu1F, Zihang Li1E, Congcong Wei3B, Mengxuan Yao1E, Huijie Li4AB*DOI: 10.12659/MSM.938991
Med Sci Monit 2023; 29:e938991
Abstract
BACKGROUND: This retrospective study from a single center aimed to compare outcomes following total hip arthroplasty (THA) in 302 patients diagnosed with Association Research Circulation Osseous (ARCO) stage III and stage IV osteonecrosis of the femoral head (ONFH).
MATERIAL AND METHODS: The study included 302 patients who underwent THA for ONFH between January 2018 and September 2021. Patient groups included ARCO stage III (n=145) and ARCO stage IV (n=157). Outcomes measured included duration of disease, operative time, intraoperative blood volume, postoperative length of hospital stay, pain measured by the visual analog scale (VAS) score, Harris hip score (HHS), and forgotten joint score (FJS).
RESULTS: Patients with ARCO stage III ONFH had a significantly shorter operative time (P=0.009), shorter length of hospital stay (P=0.021), and reduced volume of intraoperative bleeding (P=0.021) compared with patients with ARCO stage IV ONFH. There were no significant differences in disease duration (P=0.310), postoperative complications (P=0.07), preoperative (P=0.086, P=0.156) and postoperative (P=0.062, P=0.173) HHS and VAS scores, respectively. Patients with stage III ONFH reported significantly higher FJS scores at 3 months, 6 months, and 1 year after THA.
CONCLUSIONS: Patients who underwent hip arthroplasty for ARCO stage III femoral head necrosis experienced shorter operative time and hospital stay, less intraoperative bleeding, and better restoration of hip function than those with ARCO stage IV. Moreover, stage III patients were more prone to “forget” their hip arthroplasty experience within 1 year of surgery.
Keywords: total hip arthroplasty, Osteonecrosis of the femoral head, stage, Pain, Humans, Arthroplasty, Replacement, Hip, Femur Head, Femur Head Necrosis, Treatment Outcome
Background
Osteonecrosis of femoral head (ONFH) refers to the structural changes and collapse of the femoral head caused by the death and subsequent repair of bone cells and bone marrow components after disruption of the blood supply to the femoral head. It manifests as joint pain, functional disorders, and a rapid disease progression. Untimely interventions are associated with a high risk of femoral head collapse and a poor prognosis. ONFH is prevalent between the ages of 30 and 50 years, irrespective of patient sex [1].
Association Research Circulation Osseous (ARCO) is a common staging method used to assess the extent of osteonecrosis of the femur and was first introduced in 1994. The latest revisions in 2019 include (1) the deletion of stage 0; (2) the division of stage III into early (IIIA) and advanced (IIIB) stages based on whether the degree of collapse exceeds 2 mm; and (3) removal of the location and size of necrosis from the staging subtypes. Bone trabecular changes and subchondral fractures were seen on ARCO stage III imaging, with unchanged joint space and femoral head collapse ≤2 mm (IIIA) and >2 mm (IIIB). Osteoarthritic manifestations of the hip, such as narrowing of the joint space, acetabular changes, and destruction, are visible on imaging in ARCO stage IV [2]. Koo et al [3] suggested the predictability of femoral head collapse in patients with osteonecrosis, which adds to the spectrum of possibilities for treating patients with intermediate to advanced stage diseases. ONFH is clinically managed by total hip arthroplasty (THA), as conservative treatment and hip preservation therapy are insufficient to satisfy the patients’ needs for daily living. However, given the comparatively young age of onset, prostheses can fail to fulfill their life-long use in patients owing to years of wear, and the optimal age for THA is about 60 to 75 years. Currently, new materials, techniques, and designs of artificial joint prostheses have been widely used in clinical practice, and the following factors should be thoroughly considered prior to the implementation of THA: (1) the necessity for THA; (2) expected surgical outcomes; (3) medical costs and risks; (4) contraindications; (5) effects on the elderly; (6) complications and management measures; and (7) patient condition. The only surgical indications for the implementation of THA are in those patients who present with collapsed femoral head, ONFH with moderate or severe persistent pain, functional impairment and with ARCO stage III or above, and pain that cannot be relieved by other non-surgical treatments [4]. Despite the increasing sophistication of the techniques associated with THA, the number of revision hip replacement cases has shown a rising trend. Previous literature has reported multiple causes for revision, including loosening, infection, dislocation, polyethylene liner wear, periprosthetic fracture, wear of the femoral replacement acetabulum, and mechanical fracture of the prosthesis [5].Therefore, this retrospective study from a single center aimed to compare outcomes following total hip arthroplasty in 302 patients diagnosed with ARCO stage III and stage IV ONFH.
Material and Methods
INCLUSION AND EXCLUSION CRITERIA:
The study was approved by the Ethics Committee of the Third Affiliated Hospital of Hebei Medical University (approval no.: 2020-004-1). Because this was a retrospective study with anonymous data, the Ethics Committee of this hospital waived the requirement of informed consent. The inclusion criteria were as follows: (1) patients who were diagnosed with ONFH (ARCO stage III or IV); (2) patients who underwent initial unilateral THA; (3) more than 1 year of follow-up; (4) in this study, all procedures were performed by surgically experienced senior surgeons; (5) the prostheses used were biologic total hip prostheses manufactured by Johnson & Johnson, USA, and Schluterich, UK, both with a ceramic-to-ceramic contact surface.
The exclusion criteria were as follows: (1) patients with previous hip revision; (2) previous femoral head osteotomy, femoral head nucleus pulposus decompression, femoral head decompression implant; (3) bilateral hip arthroplasty; (4) symptoms or signs of contralateral and other large joint lesions; (5) psychiatric disorders; (6) poorly controlled pre-existing underlying diseases; (7) contraindications to surgery an inability to tolerate surgery; and (8) refusal to sign the informed consent form and were unable to complete the treatment and follow-up.
PARTICIPANTS:
A total of 302 patients with ONFH undergoing THA at the Department of Orthopedics, Third Hospital of Hebei Medical University from January 2018 to September 2021 were recruited and assigned to either a stage III group (n=145) or a stage IV group (n=157) according to their ARCO stages.
SURGICAL METHODS:
The patient was placed in a lateral position, keeping the trunk and pelvis perpendicular to the ground to avoid the body leaning forward or backward and affecting the angle of implantation during surgery. After general anesthesia, a curved incision of approximately 10 cm was made through the posterior and lateral approaches to the hip joint, and the skin, subcutaneous tissue, and fascia were incised in sequence. The lower extremity was straightened and rotated inward to expose the stop of the external rotator muscle group behind the greater trochanter, and the joint capsule was exposed by truncating the stop of the external rotator muscle group. The joint capsule was incised in a “T” shape and then flexed, the hip was dislocated by inward tucking and internal rotation, and the femoral head was amputated at about 1.5 cm above the lesser trochanter. The joint capsule and its surrounding synovial tissue were removed along the acetabular rim, and the acetabulum was maintained at 45° of abduction and 15° of anterior tilt with an acetabular file, gradually expanding and deepening the acetabulum until the cancellous bone on the acetabular surface oozed blood evenly. After a successful acetabular fitting, a biological acetabular prosthesis was placed. The affected limb was bent at the knee, flexed at the hip, and maintained in internal rotation, and the proximal femoral medullary cavity was expanded sequentially using a marrow expander. After the satisfactory effect of the femoral stem trial mold was achieved, the femoral stem prosthesis and femoral head prosthesis were installed, and the joint was repositioned. The trauma cavity was irrigated and cleaned, and the incision was sutured layer by layer.
POSTOPERATIVE TREATMENT:
All patients maintained the affected limb in an abducted neutral position after THA, and their limbs were fixed with an anti-rotation shoe. Postoperative antibiotics were administered prophylactically. The drainage tube was removed 1 day after surgery, and anticoagulation therapy with low-molecular-weight heparin was performed. After discharge, oral anticoagulation was administered until 35 days after surgery to prevent deep vein embolism in the affected limb. On the first postoperative day, patients were instructed by the medical staff to perform isometric contraction of the quadriceps muscle and functional exercises of ankle pumping to promote the recovery of the strength and blood circulation of the affected limb. If the patient had good physical condition after surgery and the muscle strength of the affected limb had recovered normally, appropriate standing or walking with crutches could be carried out with the help of healthcare personnel in the early postoperative period. All patients were instructed to avoid excessive flexion, internal retraction, and internal rotation of the affected hip during activities and rehabilitation training within 4 weeks after surgery to avoid posterior dislocation of the hip joint, which could compromise the surgical effect.
OUTCOME MEASURES:
1) Perioperative indices: The duration of illness, mean operative time, intraoperative bleeding, postoperative hospital stay, and postoperative complications were recorded.
2) Functional recovery, postoperative pain, and awareness of the replaced joint: The Harris hip score (HHS) and visual analogue scale (VAS) scores were measured before surgery and 12 months after surgery. The forgotten joint score (FJS) was recorded at 3 months, 6 months, and 1 year after surgery in the 2 groups. The FJS is a scoring system that assesses the outcome of patients after arthroplasty and evaluates whether they are aware that they have had artificial joint surgery while performing their daily activities. The higher the score, the better the condition of the joint and the earlier unawareness of the replaced joint, indicating that the artificial joint is rarely affecting daily life. The FJS has shown a high degree of internal consistency of question items in other literature, as a scoring system displaying validity and sensitivity to changes in joint function [6].
STATISTICAL ANALYSIS:
IBM SPSS 19.0 (IBM Corp., Armonk, NY, USA) statistical software was used for data analysis. A chi-square test was used to compare categorical variables such as sex and surgical side. A paired-sample
Results
PATIENT CHARACTERISTICS:
A total of 302 patients were included in this study, including 145 patients with ARCO stage III (Figure 1) and 157 patients with ARCO stage IV (Figure 2), 190 men and 112 women (P=0.167). The patient characteristics between the 2 groups were comparable (P>0.05; Table 1).
PERIOPERATIVE INDICES:
All patients were followed up for 1 year, and the follow-up results showed no statistically significant difference in the mean duration of disease between the 2 groups (
No surgical death was reported in either group. The stage III group reported 10 cases of lower limb deep vein thrombosis, 1 case of joint prosthesis dislocation, 19 cases of thigh root pain, and 3 cases of joint abnormalities after THA. The stage IV group reported 102 cases of lower limb deep vein thrombosis, 9 cases of joint prosthesis dislocation, 67 cases of thigh root pain, and 12 cases of joint abnormalities. However, significant differences were absent in the comparison of postoperative complications (P=0.07; Table 2).
HHS AND VAS SCORES:
The HHS increased from 71.43+32.42 to 93.67+25.82, and the VAS score decreased from 6.99±1.51 to 0.93±0.87 in the stage III group. The HHS increased from 68.43+36.42 to 90.77+45.82, and the VAS score decreased from 6.48±1.01 to 0.63±0.23 in the stage IV group. No significant differences were observed between the 2 groups in terms of preoperative (P=0.086, P=0.156) and postoperative (P=0.062, P=0.173) HHS and VAS scores, respectively. THA provided significant hip function restoration and pain mitigation for patients with stage III and IV ONFH, as shown by the elevated HHS and reduced VAS scores (P<0.05; Tables 3, 4).
FORGOTTEN JOINT SCORES:
Moreover, patients with stage III ONFH reported earlier unawareness of the replaced joint and higher postoperative comfort at 3 months, 6 months, and 1 year after THA than those at stage IV, indicated by the higher FJS scores (P<0.05; Table 5).
Discussion
THA, a classical surgical procedure for the management of hip disease, is currently the most common and effective method for the treatment of advanced ONFH [7]. In the present study, THA for ARCO stage III patients resulted in shorter operative time, less intraoperative bleeding, and fewer postoperative complications. Prolonged operative time and excessive intraoperative hemorrhage are associated with an increased risk of postoperative complications due to a long exposure of the surgical field, and the current finding was consistent with the research results of Orland et al [8]. Benefits from the abridged operative time include shortened anesthesia time and the corresponding reduced anesthetic risks and toxic adverse effects of anesthetic drugs [9]. In the present study, ARCO stage III patients had a shorter hospital stay than those with ARCO stage IV disease. Long hospital stay and long-term bed rest result in limited limb movement and reduced body activities, which can easily cause poor blood circulation and the occurrence of lower limb deep vein thrombosis. The results of the present study were in line with the findings of Bawa [10] and Gruenwald [11]. Prolonged operation time and excessive intraoperative bleeding can foster the formation of postoperative complications and delay the postoperative care process, resulting in prolonged postoperative recovery and difficulty in “forgetting” the hip prosthesis.
In the present study, patients in the stage III group exhibited higher postoperative HSS scores than those in the stage IV group, which may be attributable to the significantly impaired mobility caused by the severe deformation of the femoral head and acetabulum and changes in the surrounding soft tissues. Moreover, the heavier intraoperative blood loss in stage IV patients than in stage III patients may be ascribed to the fact that more time was needed during surgery to remove the diseased femoral head, clean up the malformed acetabular medial wall and periacetabular osteophytes, and release the surrounding contracted muscles to achieve a better acetabular cup placement and joint mobility [12]. Shimizu et al [13] concluded that femoral head collapse has been reported in 32% to 79% of patients within 3 years of diagnosis. Disease progression leads to collapse of the femoral head and contracture of the joint capsule and muscles, resulting in reduced range of motion of the hip. In the present study, patients in the stage III group had more enhancement in the range of motion of the hips than those in the stage IV group, which was consistent with the results of Shimizu et al. The lower VAS scores in stage III patients than stage IV patients indicated milder postoperative pain. In a prospective study including 222 patients with osteoarthritis treated with THA, Fortin et al [14] concluded that patients with the worst function and pain at the time of surgery had worse function 2 years after surgery, which was attributed to the timing of total joint arthroplasty. This is consistent with the present study, in which patients in the stage III group exhibited better hip function restoration and milder pain than those in the stage IV group. Larsson et al [15] demonstrated the availability of the FJS score to assess how well a patient can “forget” the hip prosthesis in postoperative daily life. The present study confirmed that as femoral head necrosis progressed and the earlier the patients underwent hip replacement surgery, the earlier they could “forget” the presence of a hip prosthesis. Evidence in the present study also suggested patients with earlier stages of disease were more prone to “forget” the implanted prosthesis. Thus, the FJS score is recommended for the long-term evaluation of patients after hip replacement.
The present study has the following limitations. First, this study did not evaluate other factors that could affect the outcome of hip arthroplasty, such as the possibility that rehabilitation may increase the range of motion of the hip and promote further recovery of the hip joint [16]. Second, all artificial biological total hip prostheses applied in this study were made by Johnson & Johnson and Schluter, all of which had ceramic-to-ceramic contact surfaces. Failure to apply other types of hip prostheses failed to clarify whether other types of hip prostheses have an effect on the outcome after hip replacement [17]. Third, the short follow-up of this study failed to identify distant complications after hip arthroplasty, such as aseptic loosening after hip arthroplasty, as it has been shown that aseptic loosening currently accounts for the leading cause of revision after THA [18].
Conclusions
Patients who underwent hip arthroplasty for ARCO stage III femoral head necrosis experienced shorter operative time and hospital stay, less intraoperative bleeding, and better restoration of hip function than those with ARCO stage IV. Moreover, stage III patients were more prone to “forget” their hip arthroplasty experience within 1 year of surgery. When performing THA in patients with ONFH, in addition to considering delaying surgery to avoid premature revision of the hip, negative effects of ONFH progression on the patient’s physiology, psychology, and daily life should be considered.
Figures
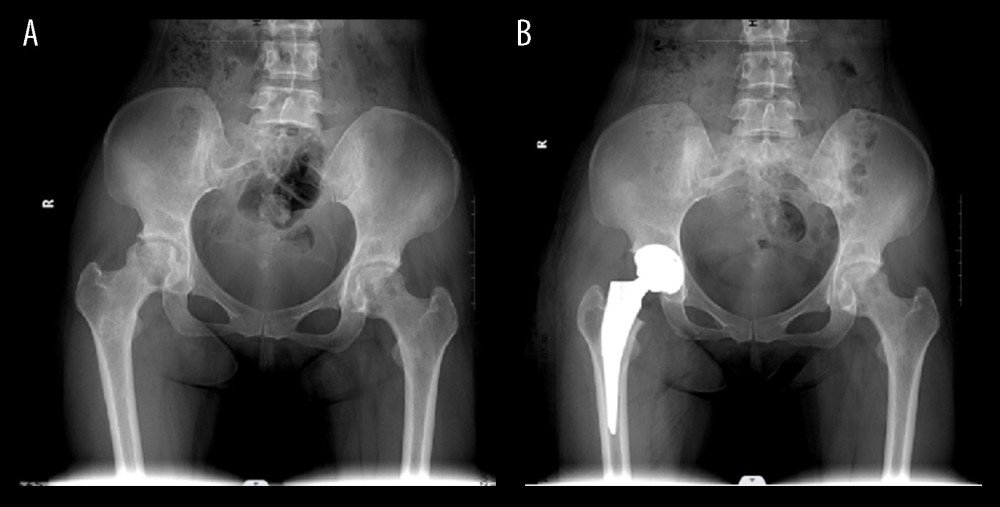 Figure 1. (A) Anteroposterior projection of preoperative X-ray of Association Research Circulation Osseous (ARCO) stage III patient shows collapsed femoral head with normal joint space. (B) Anteroposterior projection of postoperative X-ray of ARCO stage III patient shows well-positioned hip joint prosthesis.
Figure 1. (A) Anteroposterior projection of preoperative X-ray of Association Research Circulation Osseous (ARCO) stage III patient shows collapsed femoral head with normal joint space. (B) Anteroposterior projection of postoperative X-ray of ARCO stage III patient shows well-positioned hip joint prosthesis. 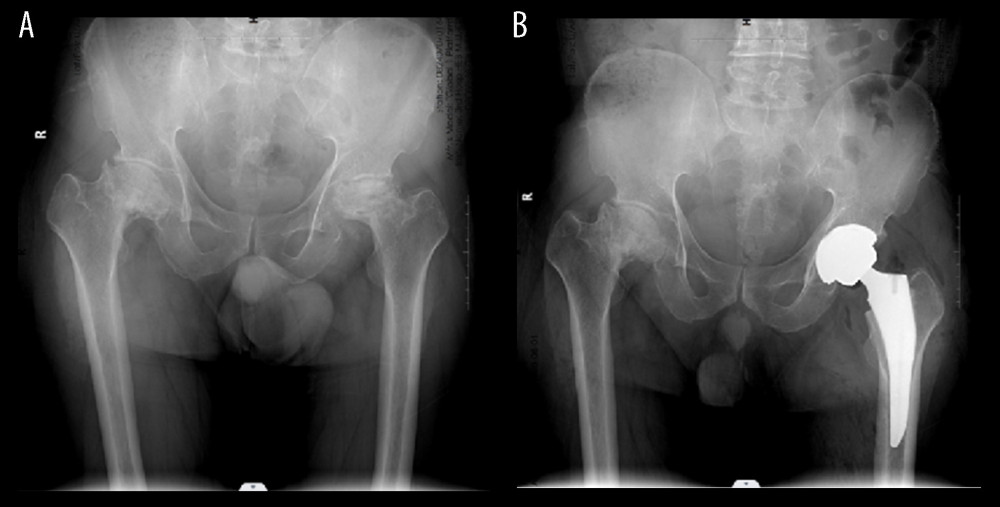 Figure 2. (A) Anteroposterior projection of preoperative X-ray of Association Research Circulation Osseous (ARCO) stage IV patient shows the absence of joint space and severe periacetabular hyperplasia. (B) Anteroposterior projection of postoperative X-ray of ARCO stage IV patient shows well-positioned hip joint prosthesis.
Figure 2. (A) Anteroposterior projection of preoperative X-ray of Association Research Circulation Osseous (ARCO) stage IV patient shows the absence of joint space and severe periacetabular hyperplasia. (B) Anteroposterior projection of postoperative X-ray of ARCO stage IV patient shows well-positioned hip joint prosthesis. Tables
Table 1. Patient characteristics.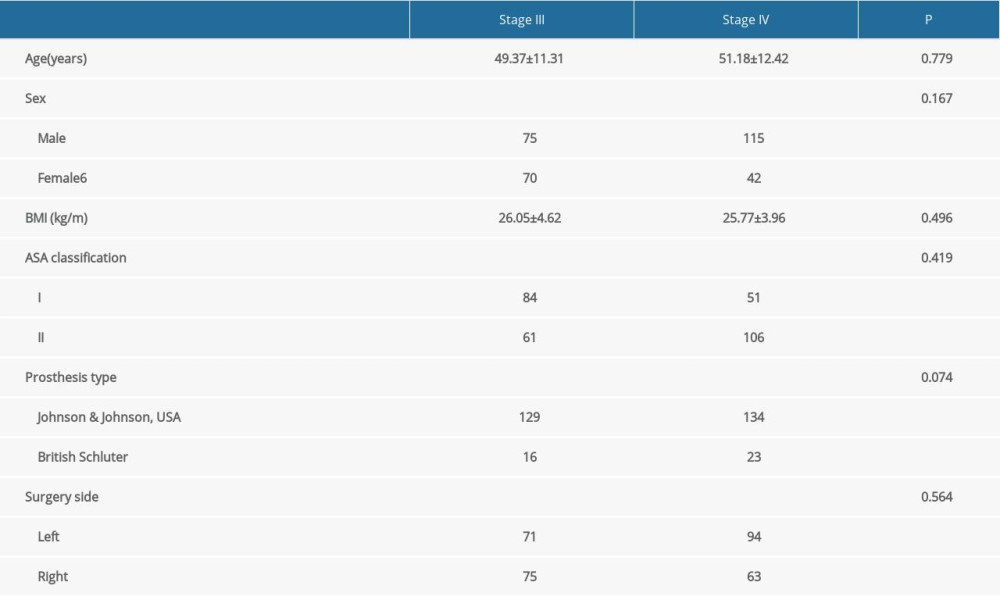 Table 2. Perioperative indices.
Table 2. Perioperative indices.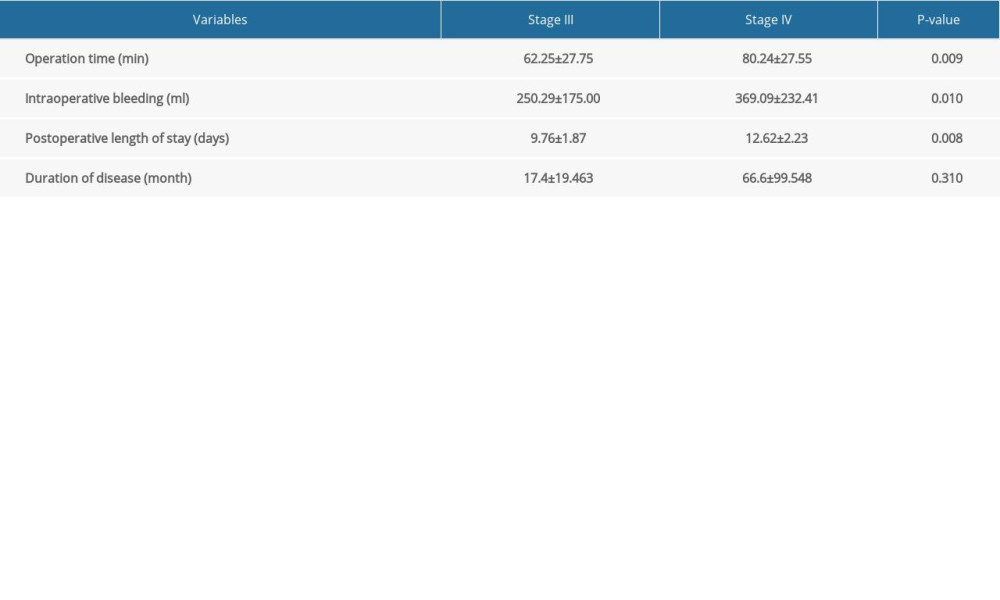 Table 3. Association Research Circulation Osseous (ARCO) stage III vs IV Harris hip score (HHS) and visual analogue scale (VAS) score in patients with femoral head necrosis after total hip arthroplasty.
Table 3. Association Research Circulation Osseous (ARCO) stage III vs IV Harris hip score (HHS) and visual analogue scale (VAS) score in patients with femoral head necrosis after total hip arthroplasty.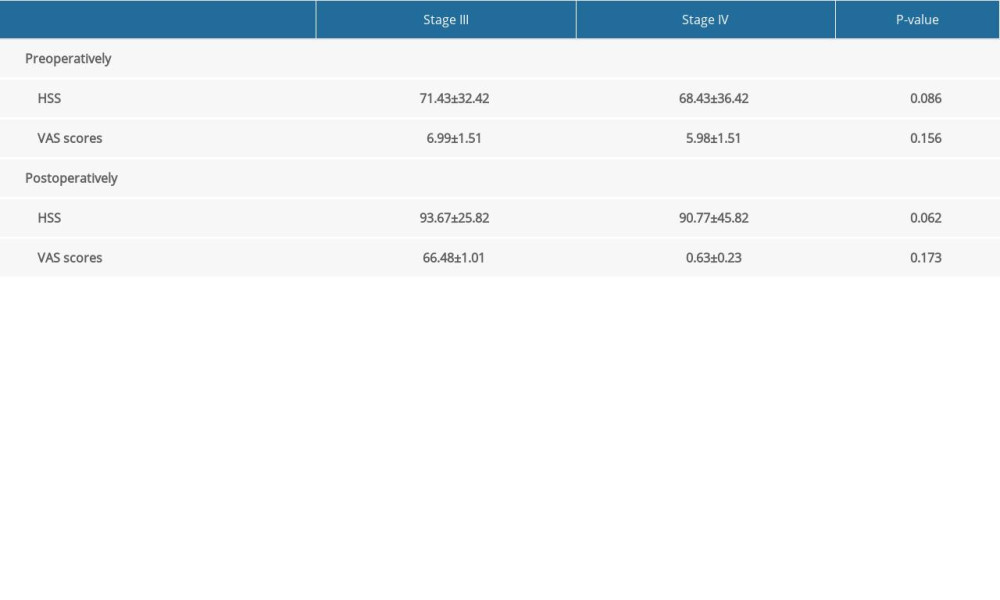 Table 4. Visual analogue scale (VAS) score and Harris hip score (HHS) before and after total hip arthroplasty in patients with femoral head necrosis at Association Research Circulation Osseous (ARCO) stage III and stage IV.
Table 4. Visual analogue scale (VAS) score and Harris hip score (HHS) before and after total hip arthroplasty in patients with femoral head necrosis at Association Research Circulation Osseous (ARCO) stage III and stage IV. Table 5. Results of independent sample t test for Association Research Circulation Osseous (ARCO) stage III vs stage IV forgotten joint scores (FJS) in patients with femoral head necrosis after total hip arthroplasty.
Table 5. Results of independent sample t test for Association Research Circulation Osseous (ARCO) stage III vs stage IV forgotten joint scores (FJS) in patients with femoral head necrosis after total hip arthroplasty.
References
1. Tan B, Li W, Zeng P, Epidemiological study based on China osteonecrosis of the femoral head database: Orthop Surg, 2021; 13(1); 153-60
2. Yoon BH, Mont MA, Koo KH, The 2019 revised version of association research circulation osseous staging system of osteonecrosis of the femoral head: J Arthroplasty, 2020; 35(4); 933-40
3. Koo KH, Mont MA, Cui Q, The 2021 association research circulation osseous classification for early-stage osteonecrosis of the femoral head to computed tomography-based study: J Arthroplasty, 2022; 37(6); 1074-82
4. Günther KP, Deckert S, Lützner C, Total hip replacement for osteoarthritis-evidence-based and patient-oriented indications: Dtsch Arztebl Int, 2021; 118(43); 730-36
5. Perticarini L, Rossi SMP, Benazzo F, Unstable total hip replacement: Why? Clinical and radiological aspects: Hip Int, 2020; 30(2 Suppl); 37-41
6. Kesterke N, Egeter J, Erhardt JB, Patient-reported outcome assessment after total joint replacement: Comparison of questionnaire completion times on paper and tablet computer: Arch Orthop Trauma Surg, 2015; 135(7); 935-41
7. Huten D, Bourgoin A, Lambotte JC, Treatment of aseptic osteonecrosis of the femoral head: Historical aspects: Morphologie, 2021; 105(349); 102-19
8. Orland MD, Lee RY, Naami EE, Surgical duration implicated in major postoperative complications in total hip and total knee arthroplasty: A retrospective cohort study: J Am Acad Orthop Surg Glob Res Rev, 2020; 4(11); e20.00043
9. Mahoney CR, Glesby MJ, DiCarlo EF, Total hip arthroplasty in patients with human immunodeficiency virus infection: Pathologic findings and surgical outcomes: Acta Orthop, 2005; 76(2); 198-203
10. Bawa H, Weick JW, Dirschl DR, Luu HH, Trends in deep vein thrombosis prophylaxis and deep vein thrombosis rates after total hip and knee arthroplasty: J Am Acad Orthop Surg, 2018; 26(19); 698-705
11. Gruenwald KJ, Arata MA, Fisher SE, Complication rates for the anterior approach to total hip arthroplasty: Orthopedics, 2020; 43(3); e147-50
12. Barrack RL, Krempec JA, Clohisy JC, Accuracy of acetabular component position in hip arthroplasty: J Bone Joint Surg Am, 2013; 95(19); 1760-68
13. Shimizu K, Moriya H, Akita T, Prediction of collapse with magnetic resonance imaging of avascular necrosis of the femoral head: J Bone Joint Surg Am, 1994; 76(2); 215-23
14. Fortin PR, Penrod JR, Clarke AE, Timing of total joint replacement affects clinical outcomes among patients with osteoarthritis of the hip or knee: Arthritis Rheum, 2002; 46(12); 3327-30
15. Larsson A, Rolfson O, Kärrholm J, Evaluation of Forgotten Joint Score in total hip arthroplasty with Oxford Hip Score as reference standard: Acta Orthop, 2019; 90(3); 253-57
16. Moyer R, Ikert K, Long K, Marsh J, The value of preoperative exercise and education for patients undergoing total hip and knee arthroplasty: A systematic review and meta-analysis: JBJS Rev, 2017; 5(12); e2
17. Boyer P, Huten D, Loriaut P, Is alumina-on-alumina ceramic bearings total hip replacement the right choice in patients younger than 50 years of age? A 7- to 15-year follow-up study: Orthop Traumatol Surg Res, 2010; 96(6); 616-22
18. Amstutz HC, Le Duff MJ, Aseptic loosening of cobalt chromium monoblock sockets after hip resurfacing: Hip Int, 2015; 25(5); 466-70
Figures
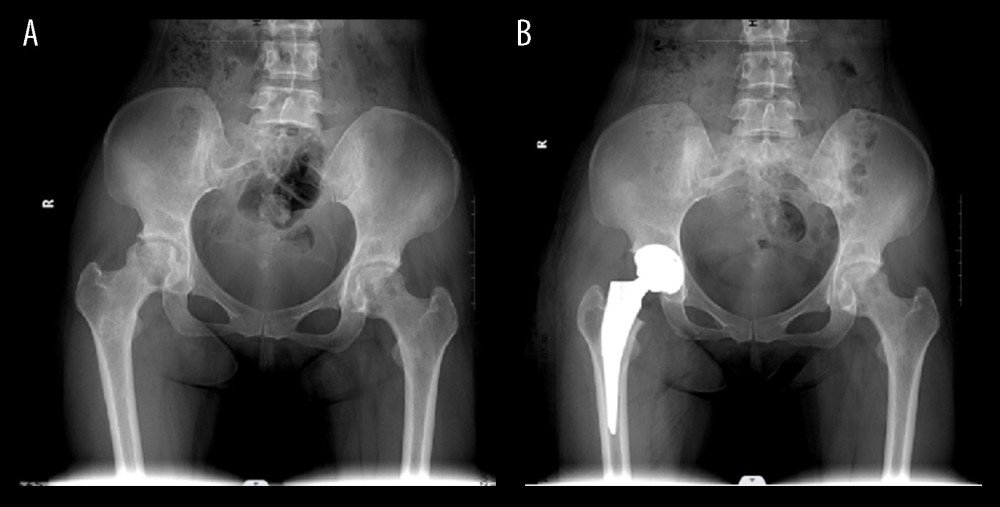 Figure 1. (A) Anteroposterior projection of preoperative X-ray of Association Research Circulation Osseous (ARCO) stage III patient shows collapsed femoral head with normal joint space. (B) Anteroposterior projection of postoperative X-ray of ARCO stage III patient shows well-positioned hip joint prosthesis.
Figure 1. (A) Anteroposterior projection of preoperative X-ray of Association Research Circulation Osseous (ARCO) stage III patient shows collapsed femoral head with normal joint space. (B) Anteroposterior projection of postoperative X-ray of ARCO stage III patient shows well-positioned hip joint prosthesis.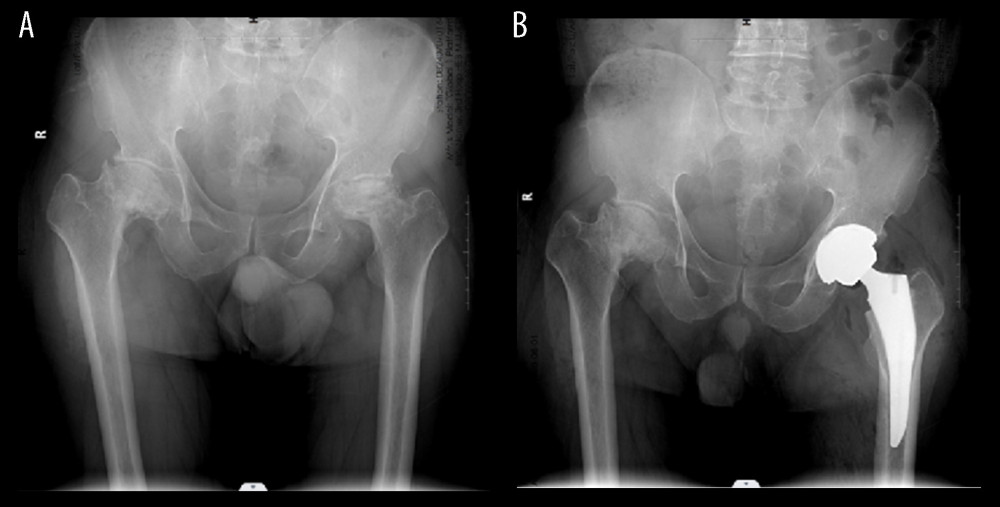 Figure 2. (A) Anteroposterior projection of preoperative X-ray of Association Research Circulation Osseous (ARCO) stage IV patient shows the absence of joint space and severe periacetabular hyperplasia. (B) Anteroposterior projection of postoperative X-ray of ARCO stage IV patient shows well-positioned hip joint prosthesis.
Figure 2. (A) Anteroposterior projection of preoperative X-ray of Association Research Circulation Osseous (ARCO) stage IV patient shows the absence of joint space and severe periacetabular hyperplasia. (B) Anteroposterior projection of postoperative X-ray of ARCO stage IV patient shows well-positioned hip joint prosthesis. Tables
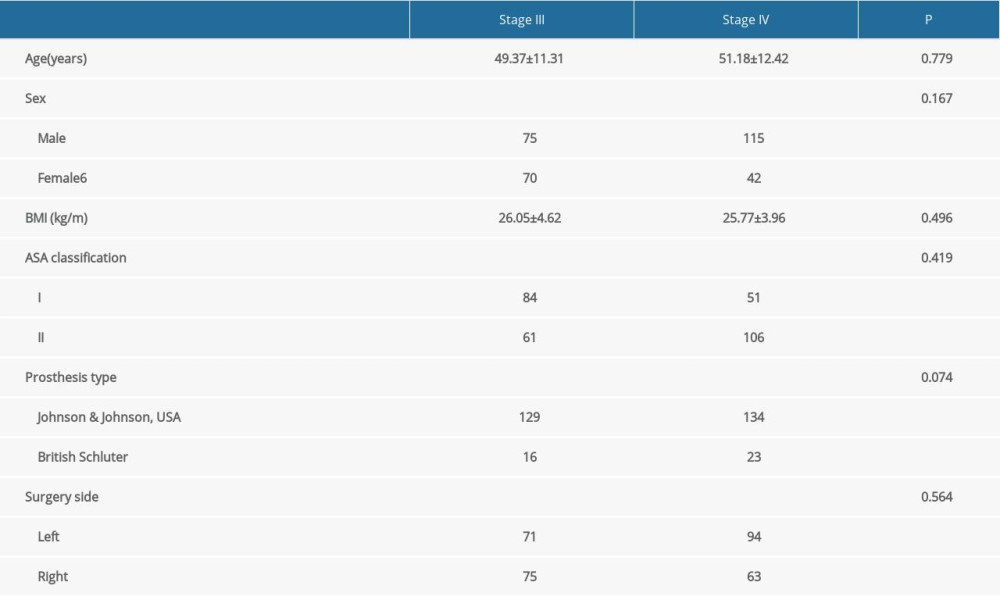 Table 1. Patient characteristics.
Table 1. Patient characteristics.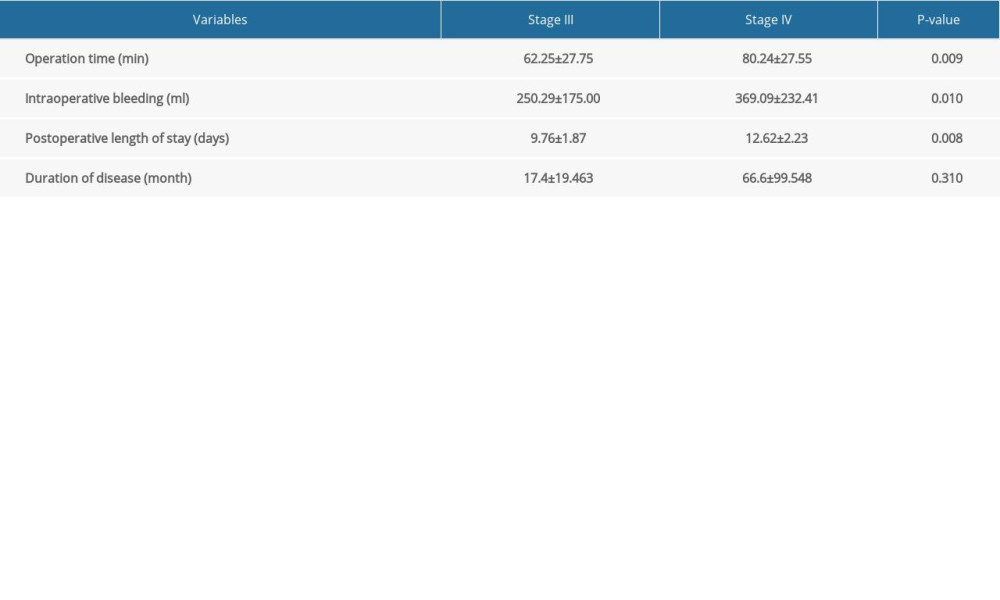 Table 2. Perioperative indices.
Table 2. Perioperative indices.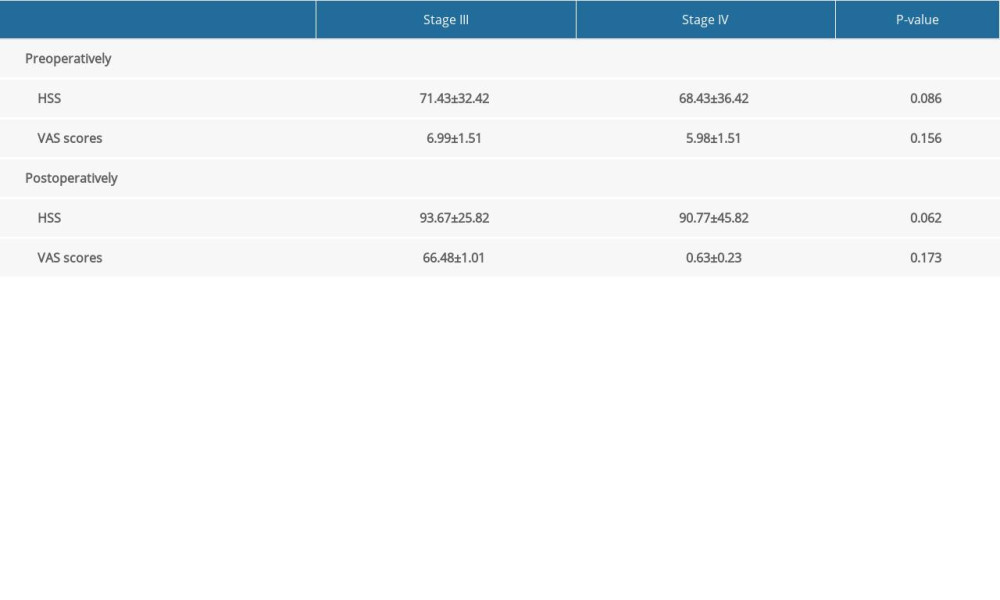 Table 3. Association Research Circulation Osseous (ARCO) stage III vs IV Harris hip score (HHS) and visual analogue scale (VAS) score in patients with femoral head necrosis after total hip arthroplasty.
Table 3. Association Research Circulation Osseous (ARCO) stage III vs IV Harris hip score (HHS) and visual analogue scale (VAS) score in patients with femoral head necrosis after total hip arthroplasty. Table 4. Visual analogue scale (VAS) score and Harris hip score (HHS) before and after total hip arthroplasty in patients with femoral head necrosis at Association Research Circulation Osseous (ARCO) stage III and stage IV.
Table 4. Visual analogue scale (VAS) score and Harris hip score (HHS) before and after total hip arthroplasty in patients with femoral head necrosis at Association Research Circulation Osseous (ARCO) stage III and stage IV. Table 5. Results of independent sample t test for Association Research Circulation Osseous (ARCO) stage III vs stage IV forgotten joint scores (FJS) in patients with femoral head necrosis after total hip arthroplasty.
Table 5. Results of independent sample t test for Association Research Circulation Osseous (ARCO) stage III vs stage IV forgotten joint scores (FJS) in patients with femoral head necrosis after total hip arthroplasty.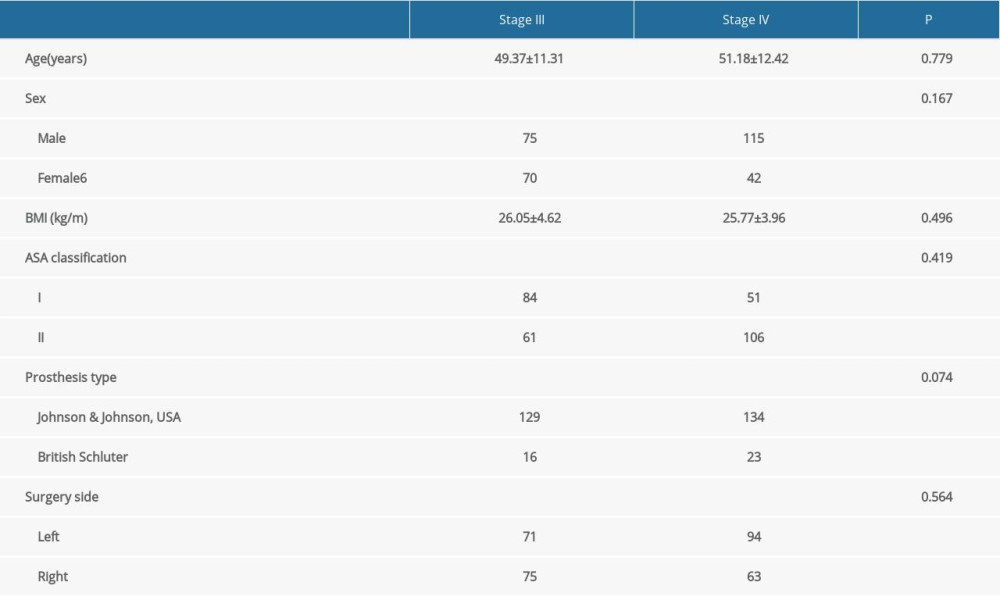 Table 1. Patient characteristics.
Table 1. Patient characteristics.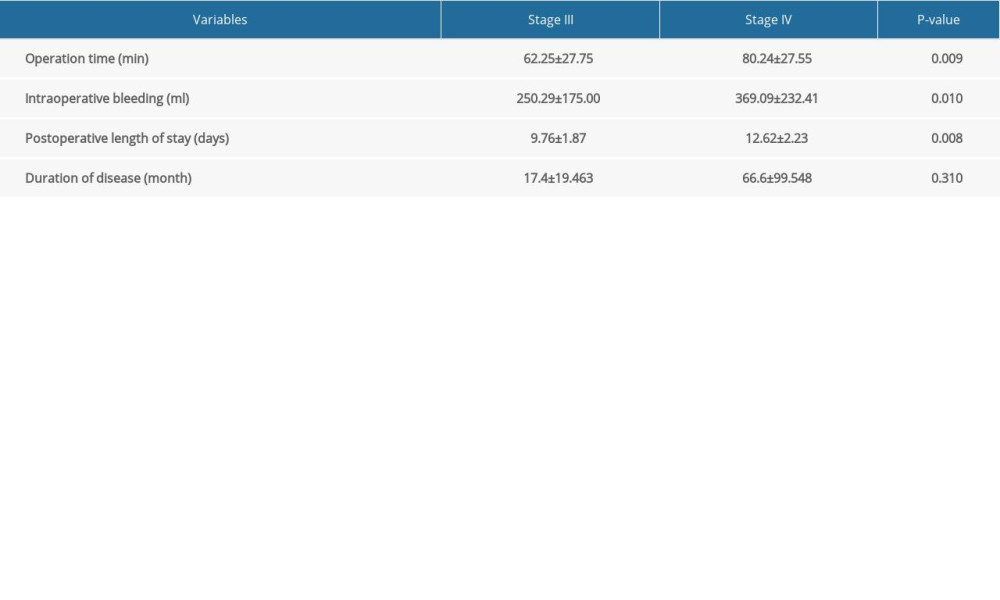 Table 2. Perioperative indices.
Table 2. Perioperative indices.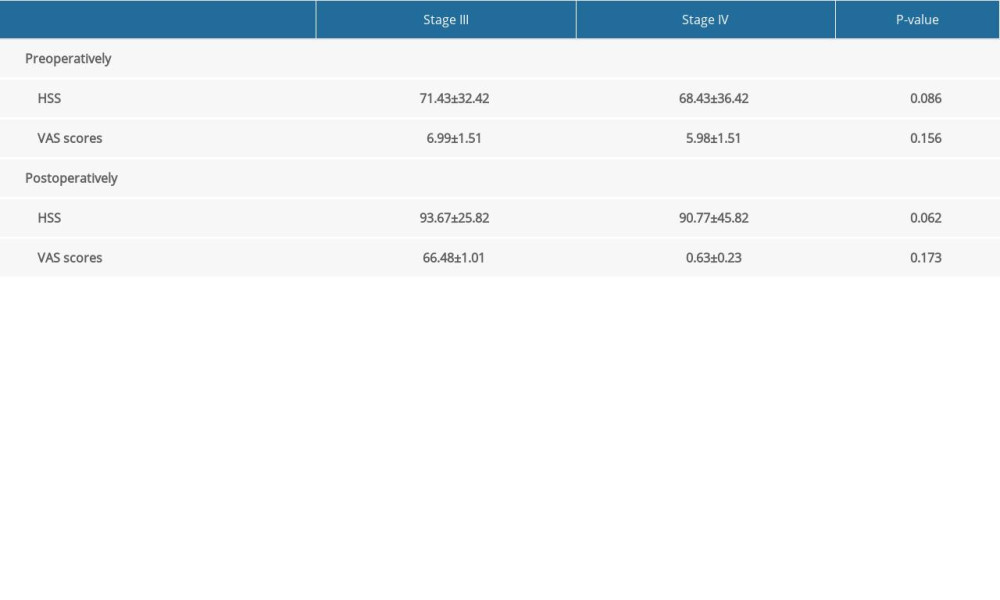 Table 3. Association Research Circulation Osseous (ARCO) stage III vs IV Harris hip score (HHS) and visual analogue scale (VAS) score in patients with femoral head necrosis after total hip arthroplasty.
Table 3. Association Research Circulation Osseous (ARCO) stage III vs IV Harris hip score (HHS) and visual analogue scale (VAS) score in patients with femoral head necrosis after total hip arthroplasty. Table 4. Visual analogue scale (VAS) score and Harris hip score (HHS) before and after total hip arthroplasty in patients with femoral head necrosis at Association Research Circulation Osseous (ARCO) stage III and stage IV.
Table 4. Visual analogue scale (VAS) score and Harris hip score (HHS) before and after total hip arthroplasty in patients with femoral head necrosis at Association Research Circulation Osseous (ARCO) stage III and stage IV. Table 5. Results of independent sample t test for Association Research Circulation Osseous (ARCO) stage III vs stage IV forgotten joint scores (FJS) in patients with femoral head necrosis after total hip arthroplasty.
Table 5. Results of independent sample t test for Association Research Circulation Osseous (ARCO) stage III vs stage IV forgotten joint scores (FJS) in patients with femoral head necrosis after total hip arthroplasty. In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








