28 April 2023: Clinical Research
Individualized Scan Protocol Based on Body Mass Index in Dual-Energy Computed Tomography Pulmonary Angiography to Reduce Radiation and Contrast Doses with Improved Image Quality
Xin Fang1E, Xiaoyu TongDOI: 10.12659/MSM.939234
Med Sci Monit 2023; 29:e939234
Abstract
BACKGROUND: We evaluated an individualized dual-energy computed tomography (DECT) scan protocol by combining optimal monochromatic images with an appropriate ASIR-V reconstruction strength in computed tomography pulmonary angiography (CTPA) to reduce radiation and iodine doses and superior vena cava (SVC) artifacts.
MATERIAL AND METHODS: A total of 127 patients who underwent CTPA were prospectively enrolled and randomly divided into a standard (n=63) and individualized group (n=64). The standard group used 120 kVp, 150 mAs, and 60 mL contrast media at an injection rate of 5 mL/s; the individualized group used DECT imaging mode with tube current selected according to patients’ BMI (BMI ≤20 kg/m², 200 mA; 20< BMI ≤23 kg/m², 240 mA; 23< BMI ≤25 kg/m², 280 mA; BMI >25 kg/m², 320 mA). Contrast media intake was 130 mgI/kg with an injection time of 7 s. The data in the individualized group was reconstructed to 55-70 keV (5 keV interval) monochromatic images combined with 40-80% ASIR-V (10% interval). Radiation dose, contrast dose, and image quality were compared between the groups.
RESULTS: There were no significant differences in patient habitus. Compared with the standard group, the individualized group significantly decreased radiation dose by 33.93% (3.31±0.57 mSv vs 5.01±0.34 mSv) and contrast dose by 56.95% (9.04±1.40 gI vs 21.00±0.00 gI). The 60 keV image with 80%ASIR-V in the individualized group provided the best image quality and further reduced SVC beam-hardening artifacts.
CONCLUSIONS: The use of BMI-dependent DECT protocol in CTPA further reduces radiation dose, contrast agent dose, and SVC artifacts, with the 60 keV images reconstructed using 80%ASiR-V having the best image quality.
Keywords: Artifacts, Body Mass Index, Contrast Media, Pulmonary Artery, Humans, Angiography, computed tomography angiography, Radiation Dosage, Radiographic Image Interpretation, Computer-Assisted, signal-to-noise ratio, Vena Cava, Superior
Background
Pulmonary embolism (PE) is considered the third major cardiovascular emergency after coronary heart disease and stroke, with a high mortality and morbidity rate [1–3]. Therefore, an accurate and rapid diagnosis of pulmonary embolism is imperative for the clinical treatment of patients. Computed tomography pulmonary angiography (CTPA) is widely used in clinical work because of its high sensitivity and specificity [4–6]. It is considered the criterion standard for the detection of PE [7] and provides excellent details for visualizing pulmonary arteries and is a simple and noninvasive method for diagnosing thrombosis [8,9]. The image quality of CTPA depends mainly on the contrast between blood vessels and surrounding tissues. The degree of vascular enhancement is closely related to the patient’s body mass index (BMI) and the volume and flow rate of iodine contrast media [10]. At present, due to the limitation of the pulmonary circulation and CT imaging parameters, the radiation dose and iodine intake in CTPA is relatively high. Although it maximizes the image contrast and diagnostic ability, the beam-hardening artifact in the superior vena cava is high, which interferes with the display of adjacent structures and easily leads to misdiagnosis and missed diagnosis of small emboli around it, resulting in false-negative results [10]. At the same time, higher contrast dosage can potentially cause a series of clinical problems, such as the incidence of contrast-induced nephropathy (CIN) and contrast extravasation [11]. The incidence of CIN is increasing yearly, and it is the third cause of iatrogenic acute renal failure, next to abnormal renal blood perfusion and nephrotoxic drugs [11,12]. Although recent reports suggest that the adverse effects of contrast agents may be exaggerated, the European Society of Urogenital Radiology currently recommends the use of the lowest possible contrast dose to reduce the incidence of CIN and other adverse reactions [13].
The radiation dose is closely related to the scanning parameters, such as tube voltage, tube current, scanning time and pitch, and is greatly affected by the patient’s body size [14,15]. How to achieve acceptable image quality at a reduced contrast media and radiation dose on an individual patient level is a hot research topic.
The Revolution CT scanner (GE Healthcare) in our routine clinical application is capable of dual-energy CT (DECT) imaging, with rapid tube voltage switching between 80 kVp and 140 kVp (<0.5 ms) to acquire 101 monochromatic images in the range of 40–140 keV [16]. It is also equipped with the adaptive statistical iterative reconstruction-V algorithm (ASIR-V, GE Healthcare) to reduce image noise. The combination of DECT with ASIR-V has been extensively used for CTA imaging of various human body parts. However, to the best of our knowledge, there are few studies investigating the selection of optimal keV and ASIR-V levels in DECT for CTPA with reduced contrast and radiation dose based on patient BMI. This study aimed to demonstrate the value of using an individualized DECT scanning protocol in CTPA to reduce radiation dose and iodine dose while maintaining or improving image quality and reducing artifacts in the superior vena cava by combining the optimal monochromatic images with an appropriate ASIR-V reconstruction strength.
Material and Methods
PATIENT POPULATION:
This was a prospective study and was approved by the Ethics Committee of our institution, the First Affiliated Hospital of Dalian Medical University, and all patients provided signed informed consent. A total of 142 consecutive patients with clinically suspected PE who underwent CTPA examination in our hospital from August 2020 to December 2021 were considered, of whom we excluded patients with acute agitation (n=2), after lung resection (n=5), massive pleural effusion (n=3), contrast media allergy and liver and kidney dysfunction (n=3), and pacemaker or metal implant (n=2). Finally, 127 patients were enrolled in the study and randomly divided into the standard group (63 cases) and the individualized group (64 cases). The patient enrollment flowchart is shown in Figure 1.
CTPA SCANNING PROTOCOL:
All CT scans were performed on a 256-row single-source DECT scanner (Revolution CT, GE Healthcare, Milwaukee, WI, USA). The main scanning parameters of the standard group were tube voltage of 120 kVp and tube current of 150 mA. The individualized group was scanned using a DECT imaging mode with rapid kVp switching between 80 and 140 kVp in less than 0.5 ms. The tube current in the individualized group was selected according to patient’s BMI (BMI ≤20 kg/m2, 200 mA; 20< BMI ≤23 kg/m2, 240 mA; 23< BMI ≤25 kg/m2, 280 mA; BMI >25 kg/m2, 320 mA). The other scanning parameters were consistent with those of the standard group. The gantry rotation time was 0.5 s, and 80 mm of z-axis coverage was chosen. The pitch was 1.531: 1, and slice thickness and interval were both 5 mm.
The nonionic contrast media loversol (350 mgI/mL) was used, with an injection rate of 5 mL/s in the amount of 60 mL in the standard group, which is a standard injection protocol in our institution. The individualized group was injected with a low-iodine contrast media intake at 130 mgI/kg. The contrast media that first passed through the pulmonary artery was strongly associated with BMI. Larger patients have a greater volume of blood distribution than smaller patients, so patients with a high BMI require a higher flow rate and/or increased contrast dose [17]. We controlled the injection time to 7 s. After contrast injection, 30 mL of saline flush was injected at a flow rate of 5 mL/s. To obtain an optimal intraluminal contrast enhancement, the Smart Prep technique was used, with a region of interest placed on the pulmonary trunk, and the trigger threshold was 70 HU. The arterial-phase scan started 2 s after triggering. The scan range was from the upper edge of the lung apex to the lower edge of the bilateral costophrenic angle.
IMAGE RECONSTRUCTION:
The images of the standard group were reconstructed with a 1.25-mm slice thickness using ASIR-V at the standard 40% strength (40%ASIR-V). The virtual monochromatic images of the individualized group were reconstructed with a 1.25-mm slice thickness at the energy levels of 55–70 keV (interval 5 keV) with 40% to 80% ASIR-V (interval 10%). All images were transferred to the GE ADW 4.7 workstation for analysis with the GSI software. The images in the 2 groups were also reconstructed with maximum intensity projection and curved planar reconstruction for review.
OBJECTIVE IMAGE EVALUATION:
The regions of interest were placed in the pulmonary trunk, left pulmonary artery (the left upper and lower lobe arteries, and left lower segmental arteries), right pulmonary artery (the right upper and lower lobe arteries), and superior vena cava, with two-thirds of the target vessel diameter to measure the CT value and standard deviation (SD). The background was selected on the trapezius, with an average area of 50 mm2. The copy-and-paste function for regions of interest was used among the multiple monochromatic images in the individualized group for consistency. Each target was measured 3 times to get the mean value. The signal-to-noise ratio (SNR) was evaluated as the mean CT value of the target vessel divided by the standard deviation. The contrast-to-noise ratio (CNR) was calculated as CNR=(CT target – CT background)/SD background. The beam hardening artifacts of superior vena cava were measured, and an artifacts index (AI) was calculated as
SUBJECTIVE IMAGE EVALUATION:
In a randomized blinded design, 2 radiologists with more than 5 years of CTPA diagnostic experience independently evaluated the subjective image quality using a 5-point scale: 5, excellent contrast and sharp edge of vessels; 4, good contrast and sharp edge of vessels; 3, moderate vessel contrast; 2, fair image quality and unclear vessel edge; and 1, bad image quality and blurred vessel edge. The beam-hardening artifacts of the superior vena cava were recorded (1, no obvious artifacts; 2, obvious artifacts that affect the diagnosis). Because the degree of enhancement was not consistent in each patient, 2 senior radiologists could automatically adjust the window set to the best viewing condition based on their own diagnostic experience.
RADIATION DOSE AND CONTRAST MEDIA INTAKE:
Radiation dose was recorded on the device as CT dose-index volume (CTDIvol) in the unit of mGy and dose-length product (DLP) in the unit of mGy·cm, and effective dose (ED) was calculated using the formula ED=DLP×k, in which k represents the radiation dose conversion factor with a value of 0.014 mSv/(mGy·cm) for the chest. The patient’s BMI and the amount of contrast media dosage were recorded.
STATISTICAL ANALYSIS:
All statistical analyses were performed using SPSS version 24.0 (IBM Corp, Armonk, NY, USA) and GraphPad Prism version 8.0.1 (GraphPad Software, San Diego, CA, USA), with normally distributed data presented as mean±standard deviation. The chi-square test was used to analyze sex differences. The differences in age, height, weight, BMI, radiation dose, and iodine intake were analyzed by unpaired
Results
PATIENT POPULATION:
There were 65 men and 62 women in the study, with an age range of 30 to 87 (mean, 63.22±11.51) years and a BMI range of 17.3 to 33.22 (mean, 24.07±3.16) kg/m2. There were no significant differences in sex, age, height, weight, and BMI between the standard and individualized groups (P>0.05). The difference in personal factors is shown in Table 1.
OBJECTIVE IMAGE EVALUATION:
The objective measurements of images in the individualized group were significantly different than those of the standard group (P<0.05). In general, for images with a fixed energy level, CNR and SNR values increased, and beam-hardening artifacts (AI values) decreased as the ASIR-V strength increased. For the same ASIR-V strength, CNR and SNR values decreased, and AI values decreased as energy levels increased. Compared with images in the standard group (AI=63.38±34.39), all images in the individualized group had significantly lower beam-hardening artifacts in the superior vena cava (Table 2).
SUBJECTIVE IMAGE EVALUATION:
The subjective scores of image quality indicated an excellent consistency between the 2 observers (Kappa=0.948, P<0.05). The subjective scores were significantly different (P<0.05). The 60 keV with 80%ASIR-V image group had the highest image quality score. In the standard group, 69.84% of patients had beam-hardening artifacts that significantly affected the diagnosis, but only 7.81% were in the individualized group (Tables 3, 4 and Figure 2).
RADIATION DOSE AND CONTRAST MEDIA INTAKE:
Compared with the values in the standard group, CTDIvol, DLP, and ED in the individualized group were significantly decreased by 31.87%, 34.01%, and 33.93%, respectively (all P<0.05). The contrast media intake of the individualized group was 9.04±1.40 gI, 56.95% lower than that (21 gI) in the standard group (Figure 3).
Discussion
We showed that an individualized scan protocol based on BMI can reduce the radiation and contrast dose while maintaining adequate image quality and decreasing the superior vena cava artifacts in dual-energy computed tomography pulmonary angiography using 9.04±1.40 g iodine. Wu et al [18] also demonstrated that satisfactory image quality can be obtained with a lower contrast agent dose for CTPA. A prerequisite for accurate diagnosis of pulmonary embolism is the adequate enhancement of the pulmonary artery. Factors such as contrast dosage, concentration, injection flow rate, and patient BMI need to be considered [19]. Patients with a high BMI have a larger blood flow distribution [20], and the dosage and injection flow rate of contrast media need to be increased, so it is necessary to realize an individualized contrast agent injection protocol. Reducing the amount of contrast media can minimize the incidence of adverse reactions, but it may impair the image quality. To counter the decrease of attenuation caused by the contrast dose reduction in the low-dose research in CTPA, low tube voltages are often used. Alobeidi et al [21] used an 80 kVp in conjunction with an 80-mgI/kg body weight iodine dose to achieve a low iodine dose scan because the low kVp enhanced iodine attenuation while having a greater superior vena cava CT value. Boos et al [22] demonstrated the feasibility of applying a 70-kVp, high pitch, and 40-mL iodine contrast in patients with a BMI less than 35 kg/m2. Faggioni et al [23] showed the feasibility of 80-kV CTPA in lean patients using 40 mL of contrast medium with either a moderate (320 mg I/mL) or high (400 mg I/mL) iodine concentration. However, the use of low-kVp is often ruled out for large patients due to the severe loss of detection efficiency using low-kVp for imaging large patients [24,25]. However, DECT uses signals from both the low (80 kVp) and high (140 kVp) X-ray spectrums to generate a total of 101 sets of virtual monochromatic images in the range of 40 to 140 keV to better balance contrast and image noise. Using the lower energy images generated in DECT, the system can significantly improve the contrast between blood vessels and surrounding tissues [26,27] and optimize microvascular imaging while controlling the image noise to acceptable levels, and it has great potential in reducing the amount of contrast media. Image noise can further be reduced by using advanced reconstruction algorithms, such as the iterative reconstruction algorithm. The ASIR-V algorithm is a multi-model iterative reconstruction algorithm that integrates the system noise model, object model, and physical model. It is possible to accomplish varying degrees of noise reduction, considerably increase image contrast, and improve image quality by adjusting the algorithm’s strengths, all of which have been employed extensively in clinical situations. In the present study, we explored the best combination of monochromatic images and ASIR-V algorithm in CTPA and adopted an individualized contrast agent injection according to patients’ BMI to achieve individualized double-low dose (low radiation dose and contrast dose) CTPA. At the same time, we adopted 1.532 high-pitch technology to improve the scanning speed. A low contrast media injection protocol of 130 mgI/kg was used based on the patient’s weight, and the iodine contrast dose was 9.04±1.40 g of iodine, which was 56.95% less than that in the conventional CTPA scanning protocol.
The study by Borges et al [28] showed that the average transmission time from the elbow vein injection of contrast media to the pulmonary artery trunk was 7 s; therefore, in the individualized group, we fixed the contrast media injection time to 7 s. At the same time, to enhance the vascular enhancement effect and reduce the artifacts of the superior vena cava, 30 mL of saline flush was injected at 5 mL/s. We found that in the standard group, 69.84% (44 patients) had obvious beam-hardening artifacts in the superior vena cava that affected the diagnosis, while only 7.81% (5 patients) of the individualized group had the same. By measuring the SD value of the area with superior vena cava artifacts and calculating the artifact index, it was found that with the increase of ASIR-V weight, the artifact index showed a downward trend. It showed that ASIR-V with a high weight could also reduce the beam-hardening artifacts and improve image quality. The injection rate in the individualized group ranged from 2.5 mL/s to 5.3 mL/s (mean, 3.67±0.59 mL/s), which was about 26% lower than that in the standard group (5 mL/s). Patients’ physical comfort was better, and adverse reactions, such as fever and mild vomiting, were less for the patients in the individualized group.
We used the dual-energy CT scanning mode and selected the mA value according to the patient’s BMI to achieve individualized low radiation dose scanning. Compared with the conventional 120 kVp scanning group, the effective radiation dose of the individualized group was reduced by about 34%. Lenga et al [29] compared the radiation dose and image quality of single-energy CT and dual-source dual-energy CT in contrast-enhanced CT of the chest by analyzing 200 patients. The study demonstrated that dual-source dual-energy CT can be routinely performed for chest contrast-enhanced CT without increased radiation dose or decreased image quality, which is consistent with our study conclusions. In the present study, images with photon energies from 55 keV to 70 keV (5 keV interval) were generated for the individualized group. With the decrease in photon energy, vascular contrast increased significantly [15], while image noise also increased. To reduce the image noise, we reconstructed the virtual monochromatic images with 40% to 80% ASIR-V (10% interval) at each energy level. ASIR-V is a multi-model iterative reconstruction algorithm that integrates the system noise model, object model, and physical model and achieves different degrees of noise reduction by changing the weight of the algorithm [30,31]. Combined with subjective and objective image analysis, we showed that 60 keV plus 80%ASIR-V generated the best image quality in the individualized double-low CTPA group. Meanwhile, compared with the standard scanning mode, the SNR and CNR of each vessel were significantly improved. Our research showed that the individualized group could realize the purpose of low radiation dose and contrast media dose scanning, which is more beneficial for patients with obesity or overweight, and can obtain satisfactory diagnostic image quality.
This study also had some limitations. We used only a single parameter, BMI, for the study and grouping, which may not be the most relevant index. We did not calculate the difference in the detection rate of emboli in each group because it was not the same patient.
Conclusions
Compared with the conventional CTPA scanning protocol, the use of a BMI-dependent DECT protocol with the combination of appropriate ASIR-V weight in CTPA further reduced the contrast agent dose and radiation dose, and improved image quality and reduced superior vena cava artifacts, with the 60 keV images reconstructed using 80%ASiR-V having the best image quality.
Figures
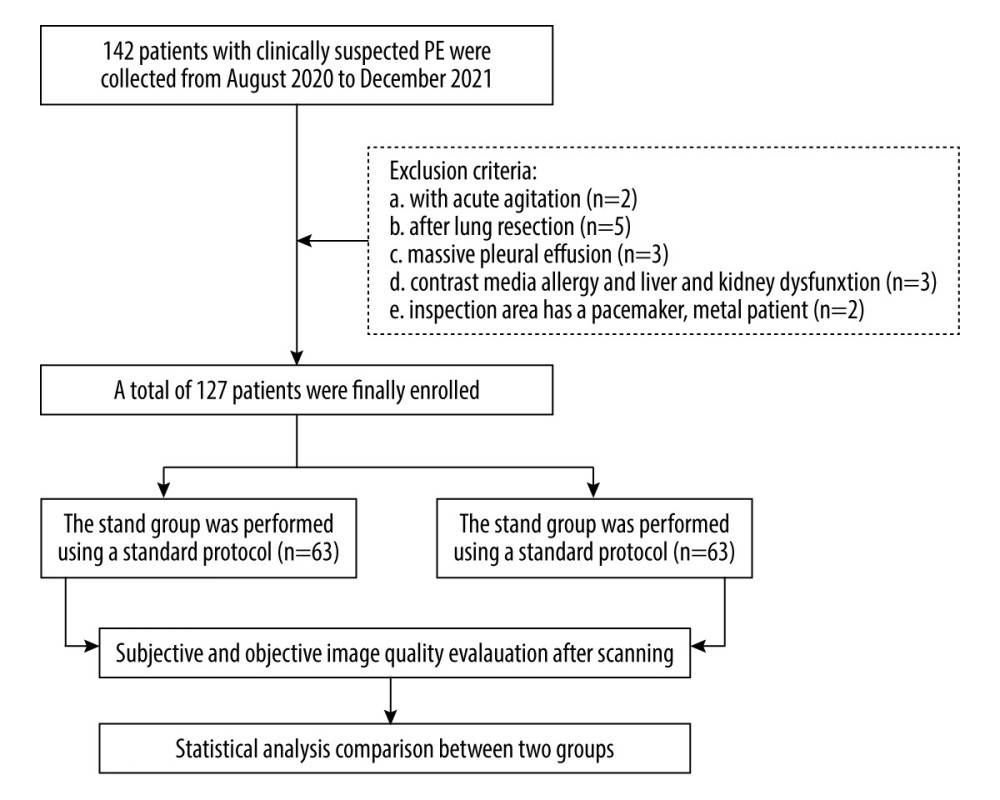 Figure 1. Flow chart of patients in the study.
Figure 1. Flow chart of patients in the study. 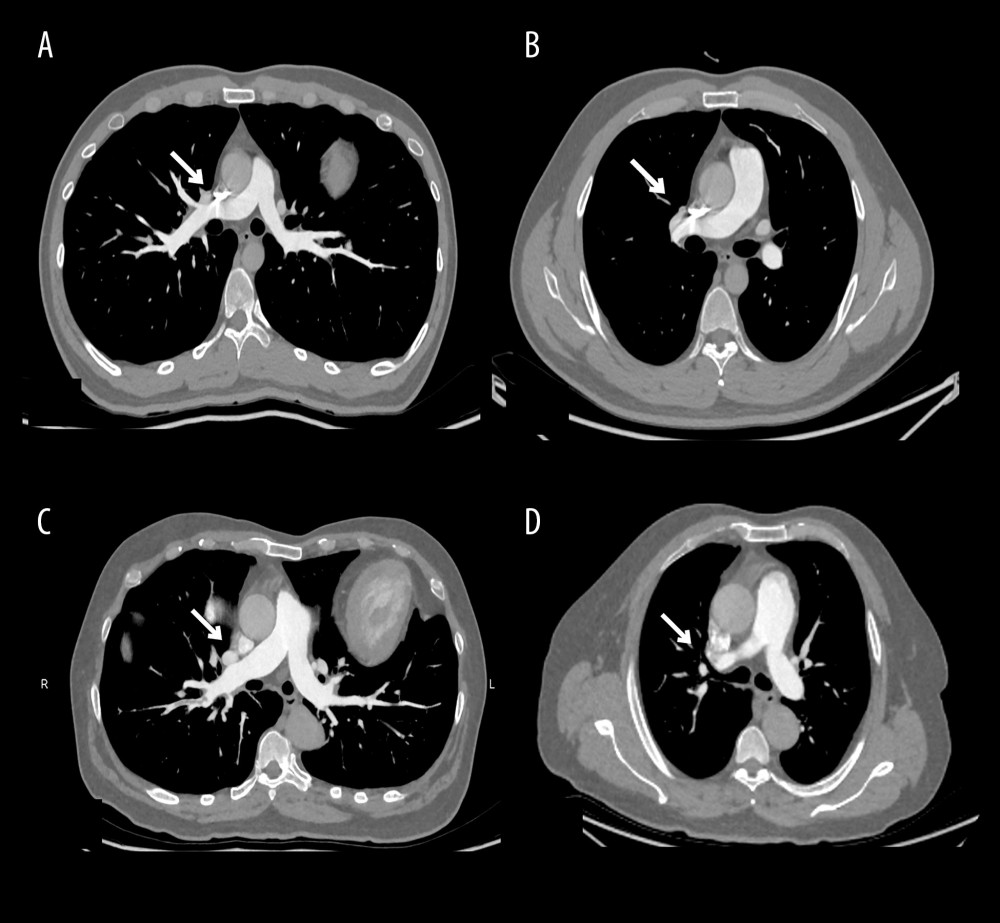 Figure 2. Computed tomography pulmonary angiography scans were obtained with standard protocol (A, B) and individualized protocol (C, D). In both images a and b, the superior vena cava showed obvious beam-hardening artifacts.
Figure 2. Computed tomography pulmonary angiography scans were obtained with standard protocol (A, B) and individualized protocol (C, D). In both images a and b, the superior vena cava showed obvious beam-hardening artifacts. 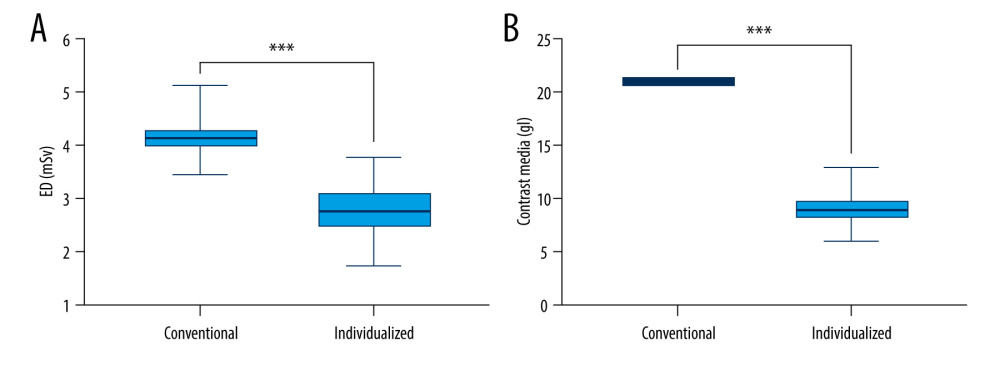 Figure 3. Comparison of (A) effective dose (ED) and (B) contrast media dose between standard and individualized groups. An independent sample t test was used to calculate P values.
Figure 3. Comparison of (A) effective dose (ED) and (B) contrast media dose between standard and individualized groups. An independent sample t test was used to calculate P values. Tables
Table 1. Demographic characteristics of patients.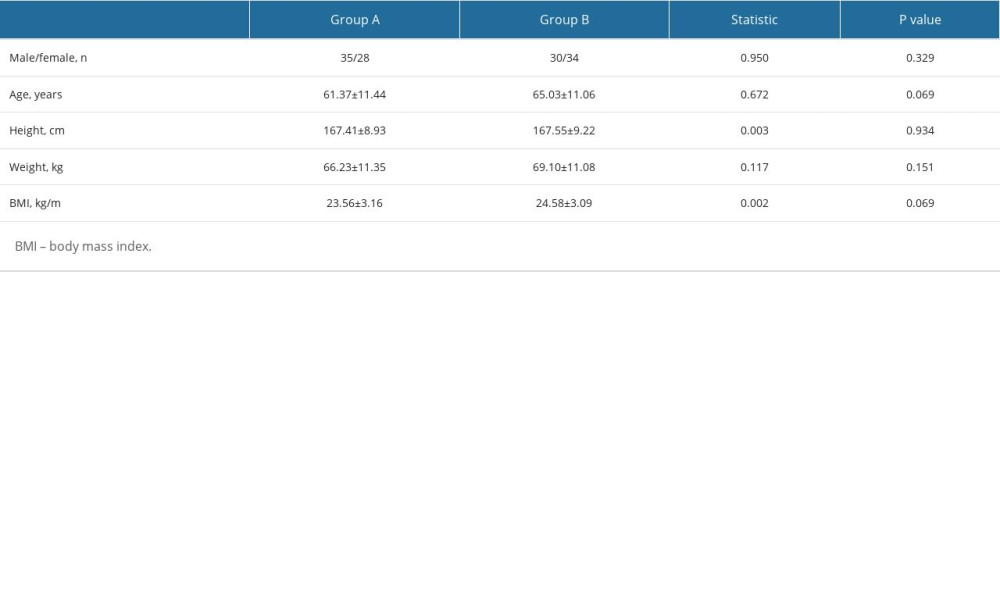 Table 2. Comparison of objective image quality of different monochromatic images combined with ASIR-V reconstruction in the individualized group.
Table 2. Comparison of objective image quality of different monochromatic images combined with ASIR-V reconstruction in the individualized group.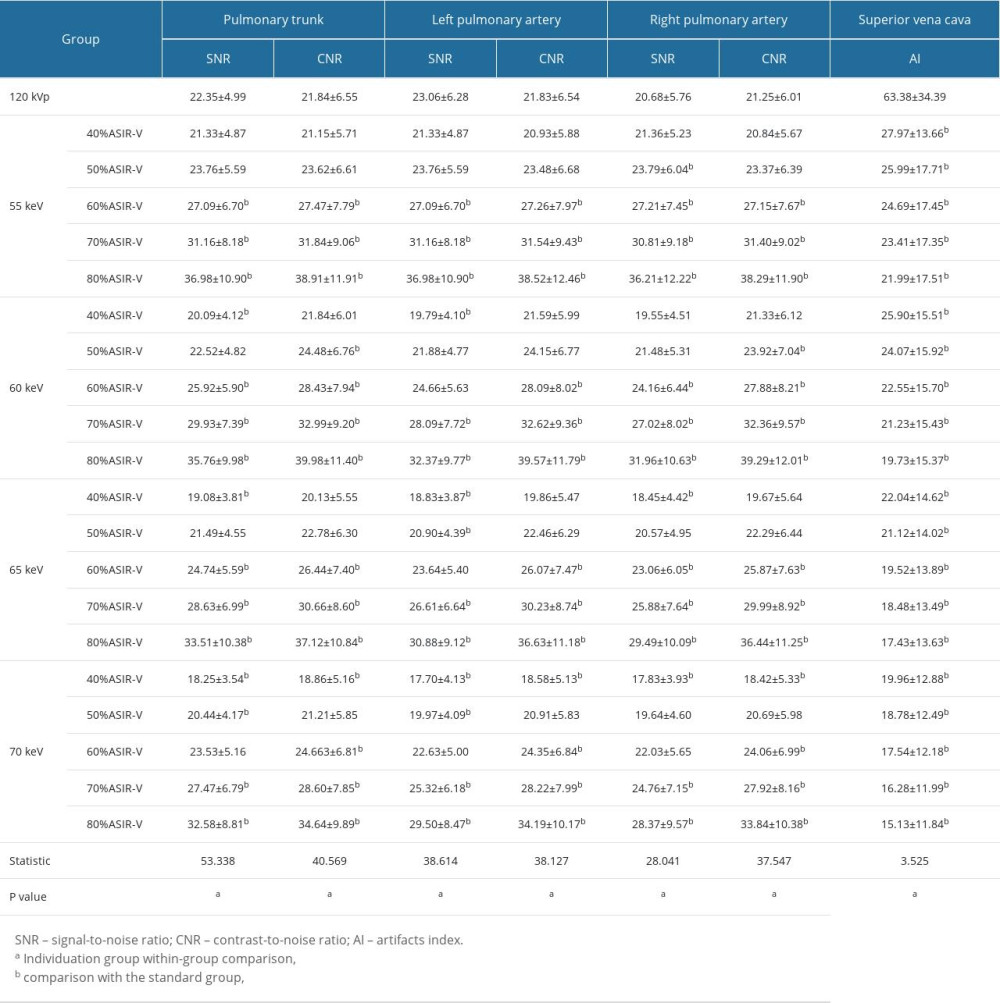 Table 3. Comparison of subjective image quality between standard and individualized groups.
Table 3. Comparison of subjective image quality between standard and individualized groups.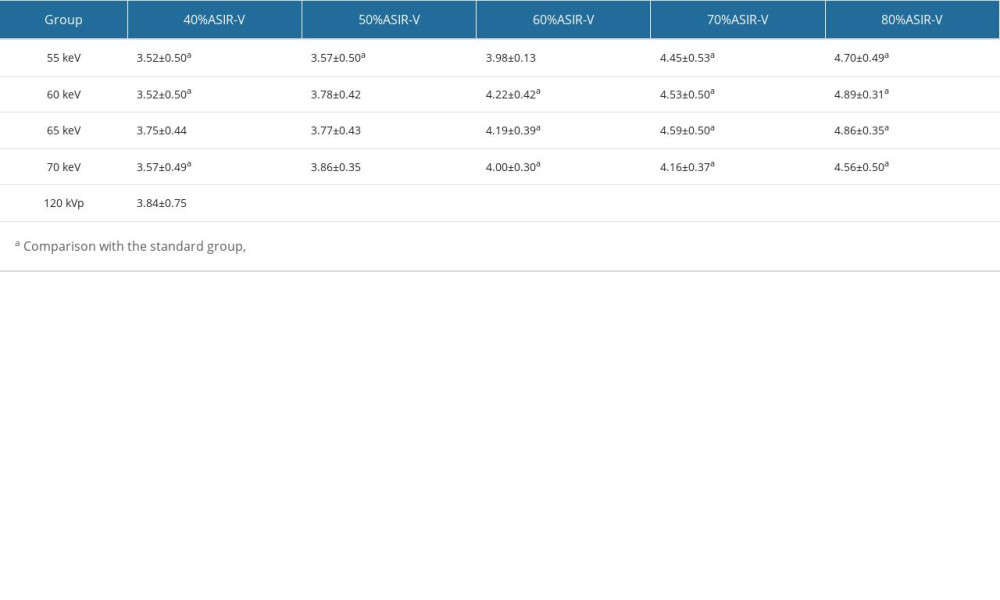 Table 4. Comparison of superior vena cava artifacts scores between standard and individualized groups.
Table 4. Comparison of superior vena cava artifacts scores between standard and individualized groups.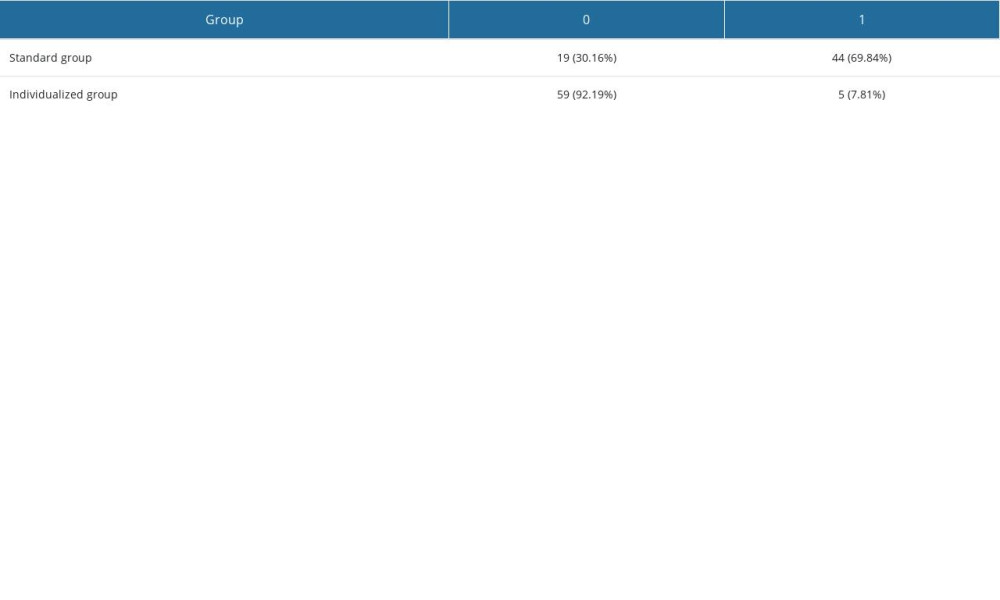
References
1. Sista AK, Kuo WT, Schiebler M, Madoff DC, Stratification, imaging, and management of acute massive and submassive pulmonary embolism: Radiology, 2017; 284(1); 5-24
2. Arrigo M, Jessup M, Mullens W, Acute heart failure: Natu Rev Dis Primers, 2020; 6(1); 16
3. Yoo HH, Nunes-Nogueira VS, Fortes Villas Boas PJ, Anticoagulant treatment for subsegmental pulmonary embolism: Cochrane Database Syst Rev, 2020; 2(2); CD010222
4. Esposito A, Palmisano A, Toselli M, Chest CT-derived pulmonary artery enlargement at the admission predicts overall survival in COVID-19 patients: Insight from 1461 consecutive patients in Italy: Eur Radiol, 2021; 31(6); 4031-41
5. Monti CB, Zanardo M, Cozzi A, Dual-energy CT performance in acute pulmonary embolism: A meta-analysis: Eur Radiol, 2021; 31(8); 6248-58
6. Vittoria de Martini I, Kobe AR, Roeren C, Diagnosis of acute heart failure in CT pulmonary angiography: Feasibility and accuracy: Eur Radiol, 2022; 32(8); 5287-96
7. Raja AS, Greenberg JO, Qaseem A, Evaluation of patients with suspected acute pulmonary embolism: Best practice advice from the clinical guidelines Committee of the American College of Physicians: Ann Intern Med, 2015; 163(9); 701-11
8. Hepburn-Brown M, Darvall J, Hammerschlag G, Acute pulmonary embolism: A concise review of diagnosis and management: Intern Med J, 2019; 49(1); 15-27
9. Weikert T, Winkel DJ, Bremerich J, Automated detection of pulmonary embolism in CT pulmonary angiograms using an AI-powered algorithm: Eur Radiol, 2020; 30(12); 6545-53
10. Jamali L, Alikhani B, Getzin T, Arterial attenuation in individualized computed tomography pulmonary angiography injection protocol adjusted based on the patient’s body mass index: J Res Med Sci, 2020; 25; 94
11. Ki YJ, Kwon SA, Kim HL, The prevention of contrast induced nephropathy by sarpogrelate: A prospective randomized controlled clinical trial: J Korean Med Sci, 2019; 34(40); e261
12. van der Molen AJ, Reimer P, Dekkers IA, Post-contrast acute kidney injury – Part 1: Definition, clinical features, incidence, role of contrast medium and risk factors: Recommendations for updated ESUR Contrast Medium Safety Committee guidelines: Eur Radiol, 2018; 28(7); 2845-55
13. Nyman U, Ahlkvist J, Aspelin P, Preventing contrast medium-induced acute kidney injury: Side-by-side comparison of Swedish-ESUR guidelines: Eur Radiol, 2018; 28(12); 5384-95
14. Li X, Ni QQ, Schoepf UJ, 70-kVp High-pitch computed tomography pulmonary angiography with 40 mL contrast agent: Initial experience: Acad Radiol, 2015; 22(12); 1562-70
15. Meyer M, Haubenreisser H, Schabel C, CT pulmonary angiography in patients with acute or chronic renal insufficiency: Evaluation of a low dose contrast material protocol: Sci Rep, 2018; 8(1); 1995
16. Yin XP, Zuo ZW, Xu YJ, The optimal monochromatic spectral computed tomographic imaging plus adaptive statistical iterative reconstruction algorithm can improve the superior mesenteric vessel image quality: Eur J Radiol, 2017; 89; 47-53
17. Ramadan SU, Kosar P, Sonmez I, Optimisation of contrast medium volume and injection-related factors in CT pulmonary angiography: 64-slice CT study: Eur Radiol, 2010; 20(9); 2100-7
18. Wu CC, Lee EW, Suh RD, Pulmonary 64-MDCT angiography with 30 mL of IV contrast material: Vascular enhancement and image quality: Am J Roentgenol, 2012; 199(6); 1247-51
19. Zantonelli G, Cozzi D, Bindi A, Acute pulmonary embolism: prognostic role of computed tomography pulmonary angiography (CTPA): Tomography (Ann Arbor, Mich), 2022; 8(1); 529-39
20. Yanaga Y, Awai K, Nakaura T, Contrast material injection protocol with the dose adjusted to the body surface area for MDCT aortography: Am J Roentgenol, 2010; 194(4); 903-8
21. Alobeidi H, Alshamari M, Widell J, Minimizing contrast media dose in CT pulmonary angiography with high-pitch technique: Br J Radiol, 2020; 93(1111); 20190995
22. Boos J, Kröpil P, Lanzman RS, CT pulmonary angiography: Simultaneous low-pitch dual-source acquisition mode with 70 kVp and 40 mL of contrast medium and comparison with high-pitch spiral dual-source acquisition with automated tube potential selection: Br J Radiol, 2016; 89(1062); 20151059
23. Faggioni L, Neri E, Sbragia P, 80-kV pulmonary CT angiography with 40 mL of iodinated contrast material in lean patients: Comparison of vascular enhancement with iodixanol (320 mg I/mL) and iomeprol (400 mg I/mL): Am J Roentgenol, 2012; 199(6); 1220-25
24. Rajiah P, Ciancibello L, Novak R, Ultra-low dose contrast CT pulmonary angiography in oncology patients using a high-pitch helical dual-source technology: Diagn Interv Radio (Ankara, Turkey), 2019; 25(3); 195-203
25. Holmquist F, Hansson K, Pasquariello F, Minimizing contrast medium doses to diagnose pulmonary embolism with 80-kVp multidetector computed tomography in azotemic patients: Acta Radiol (Stockholm, Sweden: 1987), 2009; 50(2); 181-93
26. Schneider D, Apfaltrer P, Sudarski S, Optimization of kiloelectron volt settings in cerebral and cervical dual-energy CT angiography determined with virtual monoenergetic imaging: Acad Radiol, 2014; 21(4); 431-36
27. Euler A, Parakh A, Falkowski AL, Initial results of a single-source dual-energy computed tomography technique using a split-filter: Assessment of image quality, radiation dose, and accuracy of dual-energy applications in an in vitro and in vivo study: Invest Radiol, 2016; 51(8); 491-98
28. Borges RR, Morato TN, Bezerra ASA, Evaluation of intravascular contrast media transit times in coronary computed tomography angiography: Radiol Bras, 2022; 55(3); 161-66
29. Lenga L, Leithner D, Peterke JL, Comparison of radiation dose and image quality of contrast-enhanced dual-source CT of the chest: Single-versus dual-energy and second-versus third-generation technology: Am J Roentgenol, 2019; 212(4); 741-47
30. Zhao Y, Li D, Liu Z, Comparison of image quality and radiation dose using different pre-ASiR-V and post-ASiR-V levels in coronary computed tomography angiography: J X-Ray Sci Technol, 2021; 29(1); 125-34
31. Ye K, Chen M, Zhu Q, Effect of adaptive statistical iterative reconstruction-V (ASiR-V) levels on ultra-low-dose CT radiomics quantification in pulmonary nodules: Quant Imaging Med Surg, 2021; 11(6); 2344-53
Figures
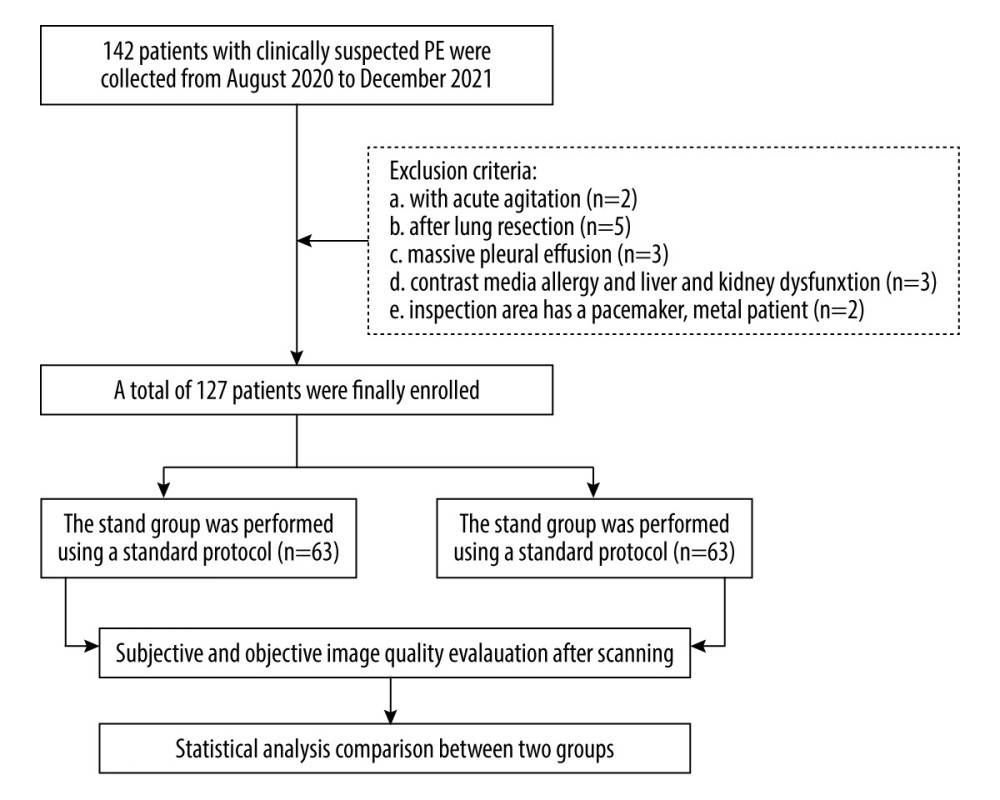 Figure 1. Flow chart of patients in the study.
Figure 1. Flow chart of patients in the study.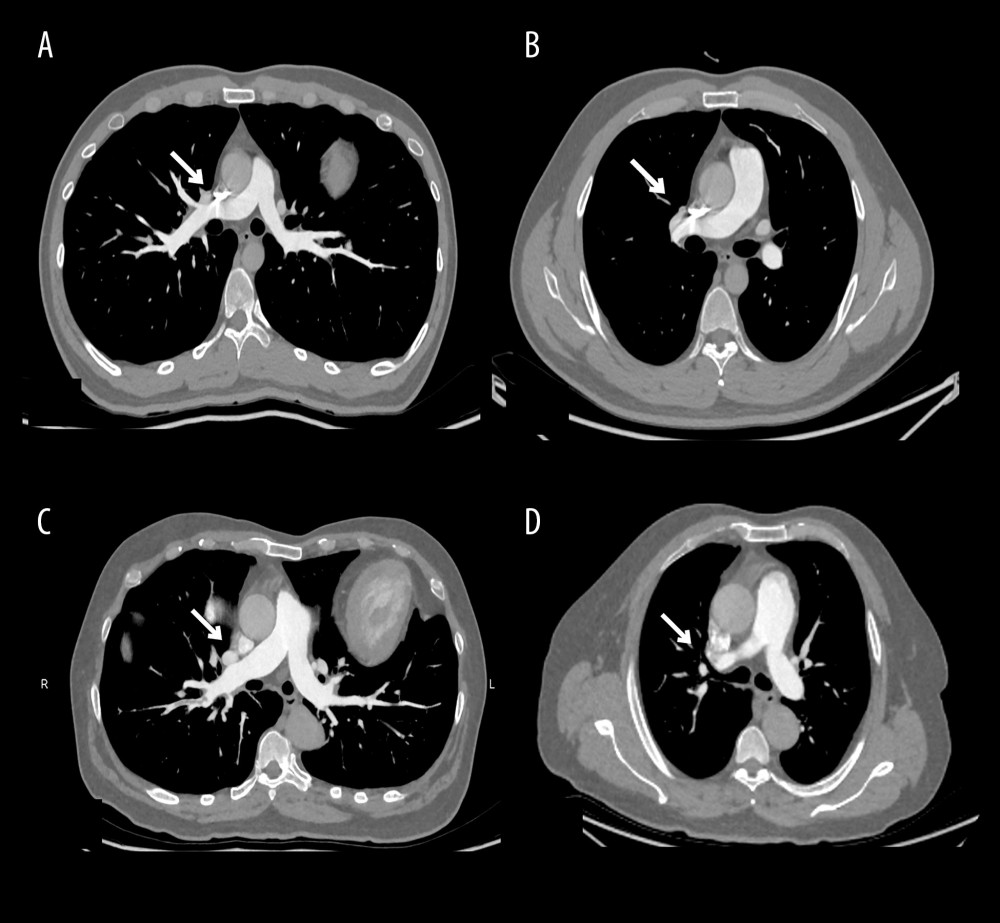 Figure 2. Computed tomography pulmonary angiography scans were obtained with standard protocol (A, B) and individualized protocol (C, D). In both images a and b, the superior vena cava showed obvious beam-hardening artifacts.
Figure 2. Computed tomography pulmonary angiography scans were obtained with standard protocol (A, B) and individualized protocol (C, D). In both images a and b, the superior vena cava showed obvious beam-hardening artifacts.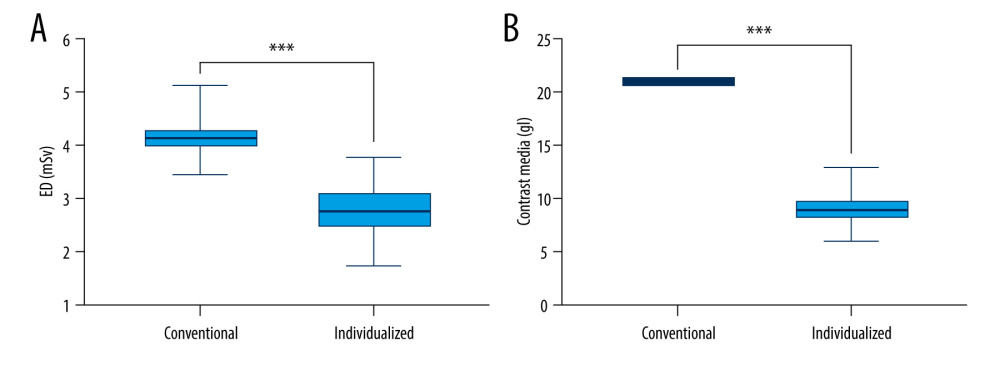 Figure 3. Comparison of (A) effective dose (ED) and (B) contrast media dose between standard and individualized groups. An independent sample t test was used to calculate P values.
Figure 3. Comparison of (A) effective dose (ED) and (B) contrast media dose between standard and individualized groups. An independent sample t test was used to calculate P values. Tables
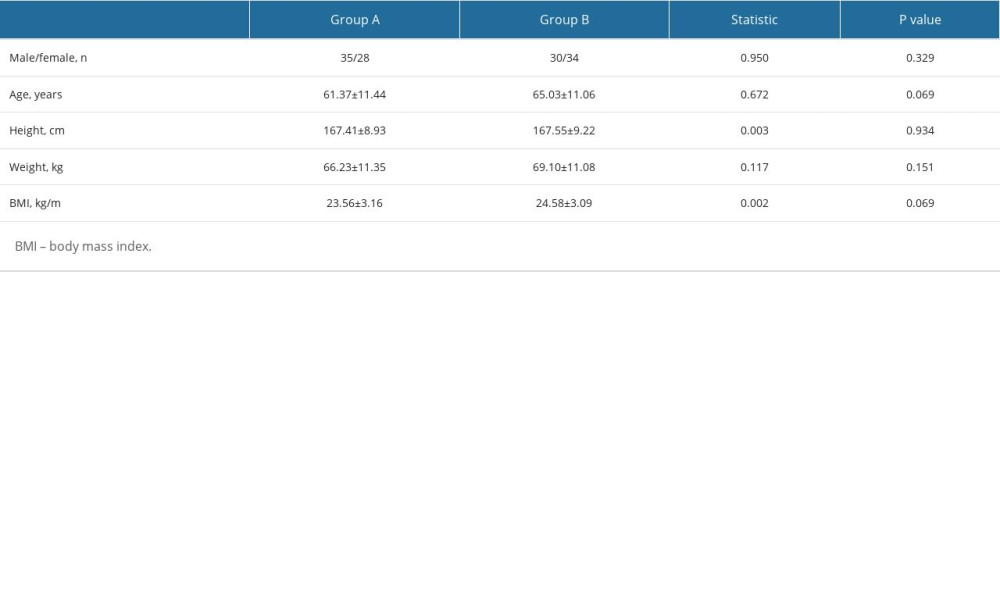 Table 1. Demographic characteristics of patients.
Table 1. Demographic characteristics of patients.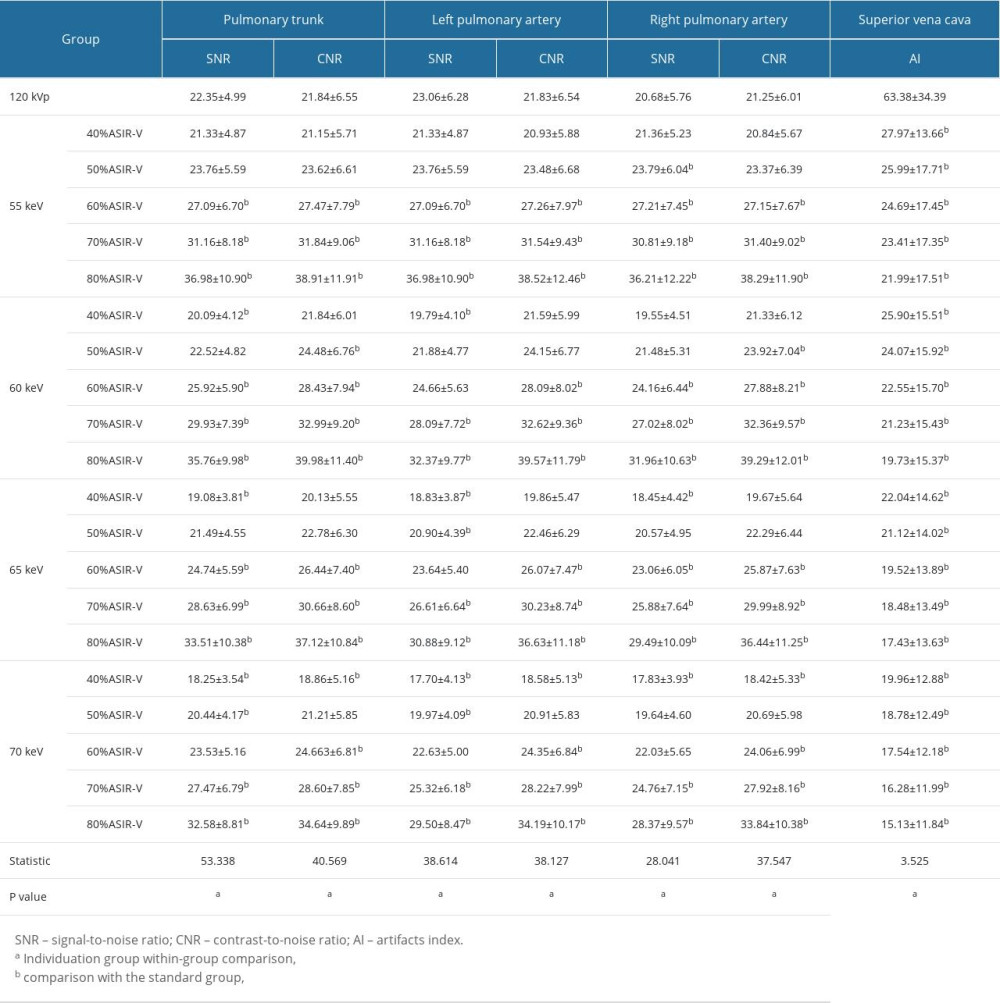 Table 2. Comparison of objective image quality of different monochromatic images combined with ASIR-V reconstruction in the individualized group.
Table 2. Comparison of objective image quality of different monochromatic images combined with ASIR-V reconstruction in the individualized group.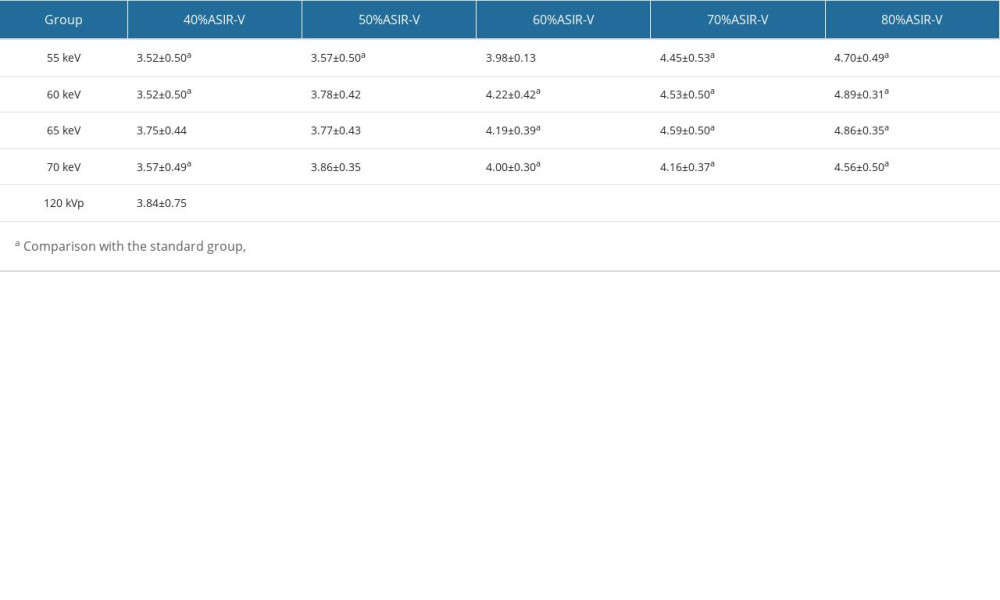 Table 3. Comparison of subjective image quality between standard and individualized groups.
Table 3. Comparison of subjective image quality between standard and individualized groups.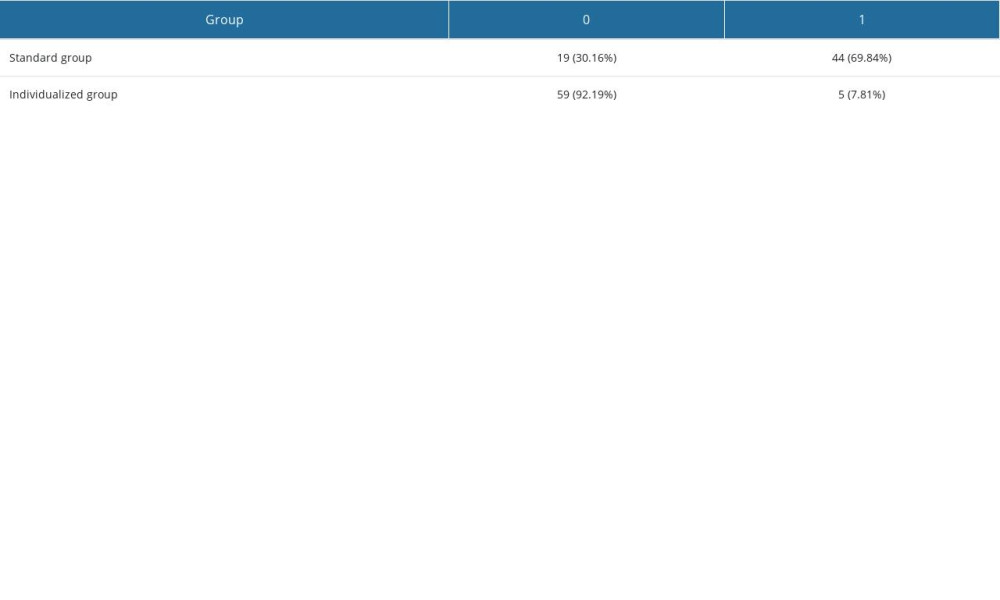 Table 4. Comparison of superior vena cava artifacts scores between standard and individualized groups.
Table 4. Comparison of superior vena cava artifacts scores between standard and individualized groups.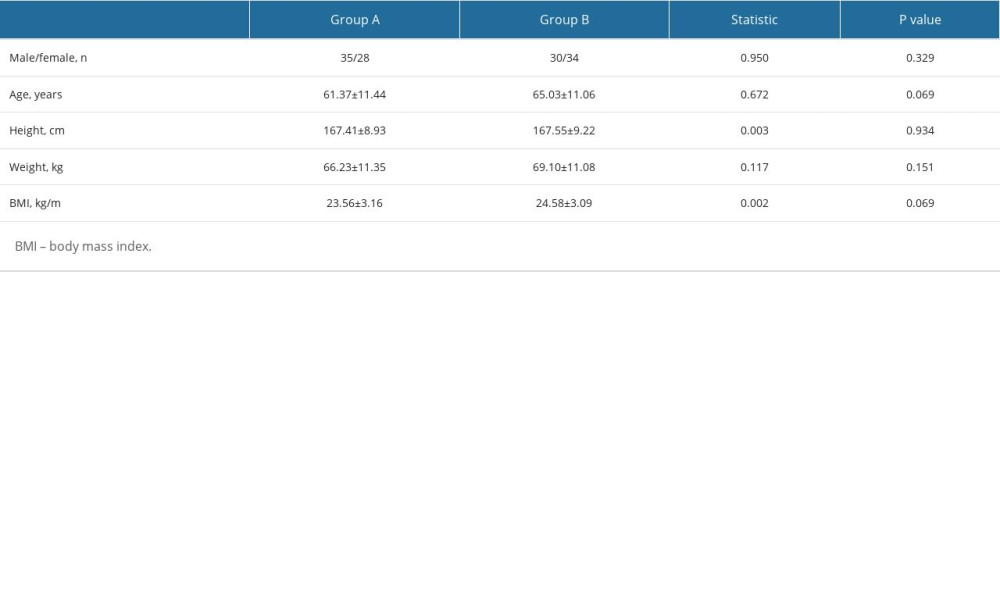 Table 1. Demographic characteristics of patients.
Table 1. Demographic characteristics of patients.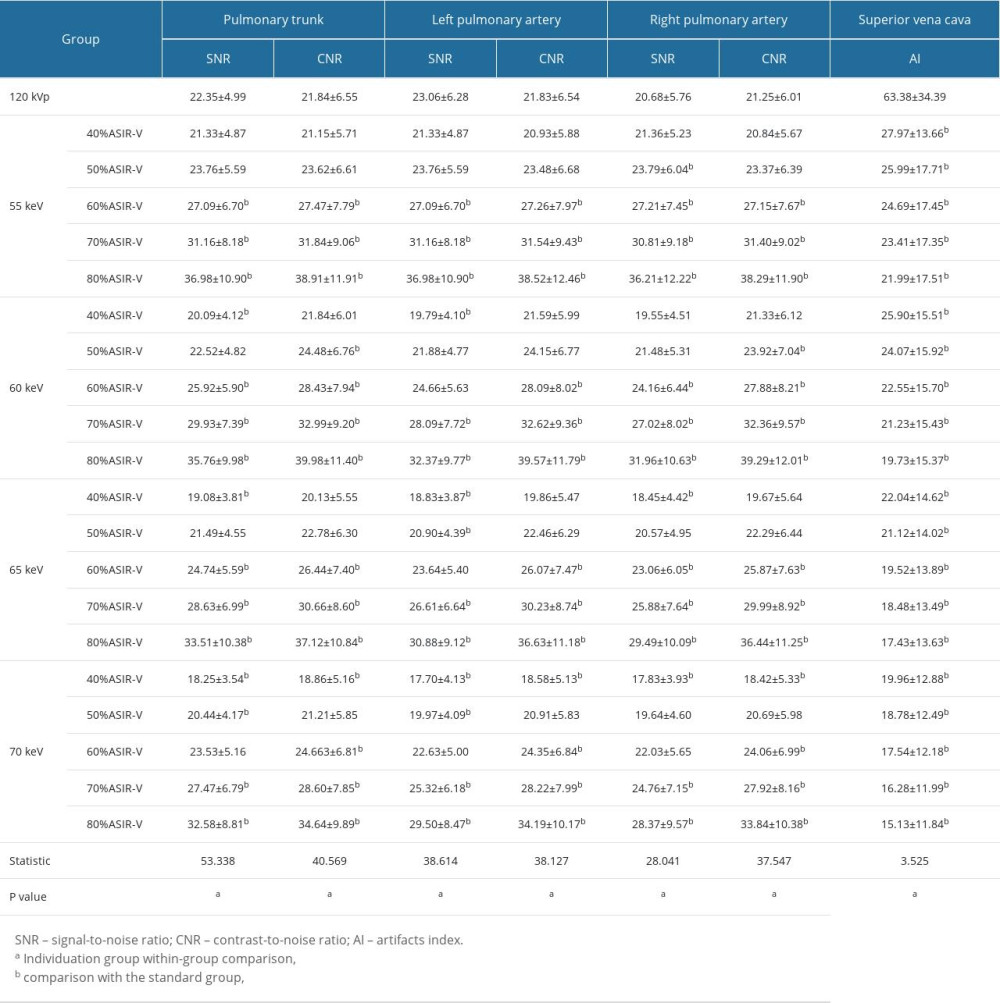 Table 2. Comparison of objective image quality of different monochromatic images combined with ASIR-V reconstruction in the individualized group.
Table 2. Comparison of objective image quality of different monochromatic images combined with ASIR-V reconstruction in the individualized group.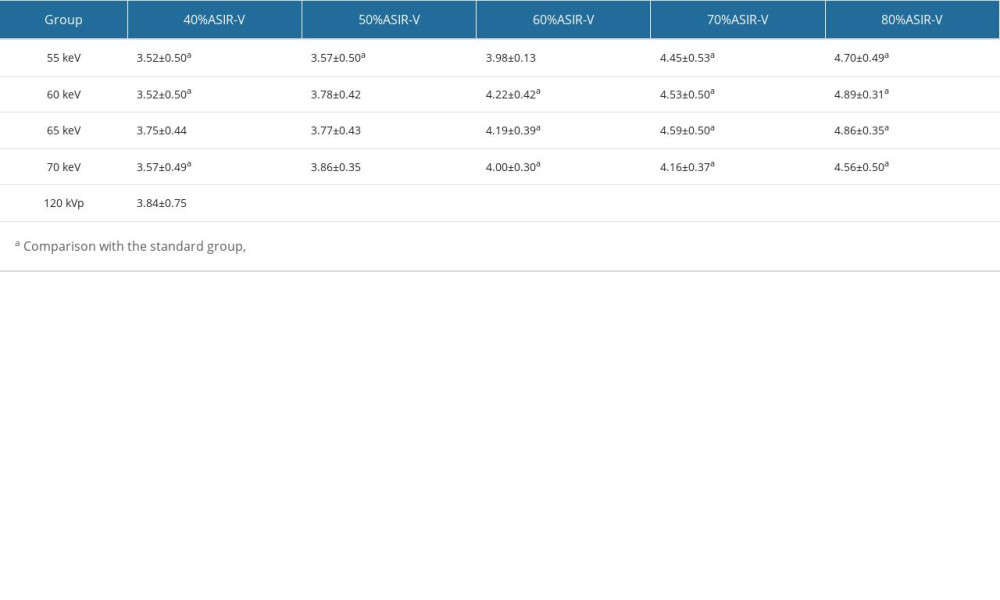 Table 3. Comparison of subjective image quality between standard and individualized groups.
Table 3. Comparison of subjective image quality between standard and individualized groups.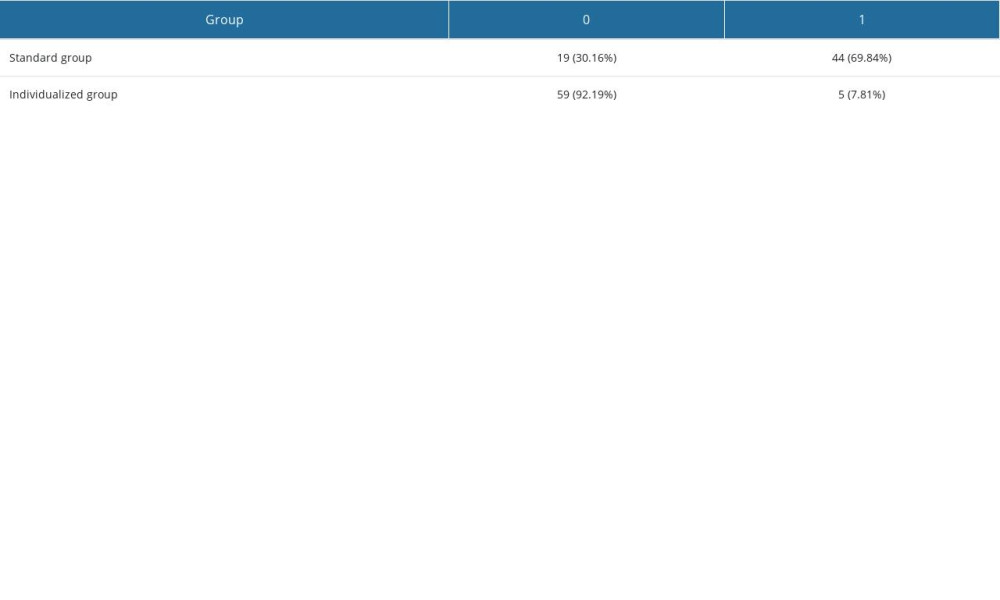 Table 4. Comparison of superior vena cava artifacts scores between standard and individualized groups.
Table 4. Comparison of superior vena cava artifacts scores between standard and individualized groups. In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








