23 February 2023: Review Articles
Presentation, Diagnosis, and Management of Lower Back Pain Associated with Spinal Stenosis: A Narrative Review
Dawid Sobański12ADEF*, Rafał Staszkiewicz13ADEF, Magdalena Stachura24EF, Marcin Gadzieliński3EF, Beniamin Oskar Grabarek13AEFDOI: 10.12659/MSM.939237
Med Sci Monit 2023; 29:e939237
Abstract
ABSTRACT: Lower back pain (LBP) is an extremely common symptom experienced by people of all ages and is also one of the most frequent causes of disability worldwide. This article aims to review the presentation, diagnosis, and management of lower back pain associated with spinal stenosis. The paper we prepared was classified as a “literature narrative review.” Nonetheless, when searching for manuscripts included in our work and reviewing them critically, we concentrated on the keywords: “lower back pain”, “lumbar spine stenosis”, “diagnostic”, “rehabilitation”, “neurosurgery”, “spine”, and “elderly”. The incidence of chronic lower back pain (CLBP) increases linearly starting with the third decade of life until 60 years old, and it more often affects women. The course of non-specific LBP above all depends on factors not connected with the spine, which include psychological, behavioral, and social factors, determined by the way the condition is perceived by the patient the environment. Lumbar spine stenosis (LSS) is an age-related process of degeneration of the intervertebral discs, ligamentum flavum, and facet joints, which results in narrowing of the space around the neurovascular structures of the spine. Diagnosis of spinal pain syndromes includes radiography (RTG), computed tomography (CT), and magnetic resonance imaging (MRI). Based on the results of imaging studies, neurological examination, and the severity of the disease, treatment can consist of analgesics and rehabilitation, or, when conservative methods are insufficient, surgical treatment is indicated.
Keywords: Constriction, Pathologic, Low Back Pain, musculoskeletal pain, Radiography, Humans, Female, Middle Aged, Spinal Stenosis, Lumbar Vertebrae, intervertebral disc
Background
Lower back pain (LBP) is an extremely common symptom, which is experienced by people of all ages and is also one of the most frequent reasons for disability in the world [1,2]. The most noticeable increase in disabilities connected with LBP has been in countries where per capita income is low or average, such as Asia, Africa, and the Middle East, where the health and social care systems are significantly burdened and underfinanced, and their main priority is combating infectious diseases [1–3]. The growing incidence of LBP creates an economic burden because it is connected with employee absence and decreased company productivity [4]. For most patients, it is impossible to precisely define the source of LBP [4]. Non-specific LBP constitutes about 90–95% of all cases [4]. In approximately three-fourths of LBP patients, an improvement in their condition is measured in an increase in pain and the degree of disability seen within 1 month, but LBP is a chronic condition in about 25% of cases [4].
The incidence of chronic lower back pain (CLBP) increases linearly starting with the third decade of life until 60 years old, and it more often affects women [5,6]. The course of non-specific LBP above all depends on factors not connected with the spine, including psychological, behavioral, and social factors, determined by the way the condition is perceived by the patient and the surroundings [5,6].
Lumbar spine stenosis (LSS) is an age-related process of degeneration of the intervertebral discs, ligamentum flavum, and facet joints, which results in narrowing of the space around the neurovascular structures of the spine [7]. It is estimated that in the United States of America (USA) LSS occurs in more than 200 000 people and is the most common reason for neurosurgical spine surgeries of the lumbar region for people 65 years old and older [7].
The paper we prepared was classified as a “literature narrative review”, and we concentrated on the keywords: “lower back pain”, “lumbar spine stenosis”, “diagnostic”, “rehabilitation”, “neurosurgery”, “spine”, and “elderly”. Therefore, this article aims to review the presentation, diagnosis, and management of lower back pain associated with spinal stenosis.
Causes of Pain Syndromes of the Lumbar Spine
Imaging and clinical condition tests often cannot determine the exact reason for the pain syndromes of the lumbar spine region [8]. For example, Boden et al found that even though imaging diagnosis showed degenerative changes of the spine, the study subjects did not have any painful conditions of the lumbar spine [9]. On the other hand, Żytkowski found that only 15% of the diagnoses regarding spinal pain were then confirmed by intraoperative tests and autopsy [10].
The available literature shows that pain syndromes are caused by mechanical factors in about 90% of cases, while specific and non-specific inflammation, rheumatic processes, oncologic diseases, and pathologies of the nerve roots are the causes in the remaining 10% [11–13]. Table 1 shows the causes of pain in the lumbar region of the spine. On the other hand, using the location of pain and the type of pathology as the criteria for division, we can distinguish 4 categories of spinal pain, as shown in Table 2 [14]. However, when taking into account structures, which may be the potential source of back pain, we can distinguish 5 origins of pain in the lumbar region of the spine, as shown in Table 3 [15].
General Characteristics of Degenerative Stenosis of the Lumbar Region of the Spine
The spinal canal (according to Spivak) is divided sagittally into 3 regions: 1) the central zone; 2) the intermediate zone (more appropriately paracentral) of the lateral recess, and 3) the zone of the pedicle of the vertebral arch [16]. Another division is the transversal one, also into 3 anatomic regions: 1) pedicle level; 2) intermediate level (vertebral body), and 3) disc level [17,18].
Degenerative stenosis of the lumbar spine is almost always connected with hypertrophy and the creation of osteophytes in the area of the intervertebral joints [19,20]. Degeneration of the intervertebral joints is causes instability and impaired mobility [19–21].
Overloading and micro-injuries lead to hypertrophy of the spinal joints, significantly contributing to narrowing of the spinal canal [22]. This process involves both the anterior and posterior edges of the joint, as well as the non-joint part and the posterior joint surface [22]. In addition, it also involves the joint capsule, the yellow ligament, and the supraspinous ligament [22]. Over time, the intervertebral disc undergoes degeneration and there is a disappearance of segmental mobility and a narrowing of the intervertebral space, which causes shortening of the spinal canal [22]. There is a protrusion of the intervertebral disc, which eventually undergoes calcification and osteophytes, which cover the intervertebral disc [22]. As a result of the narrowing of intervertebral space, during the shortening of the spinal canal, the yellow ligaments are bent in the direction of the spinal canal, and they undergo hypertrophy and calcification [22].
Pathomechanism of Pain Syndromes of the Spine
An important work in understanding the etiopathogenesis of pain syndromes of the lumbar region of the spine was published by Kuslich et al, who described 193 cases of procedures performed on the lumbar region of the spine due to intervertebral disc (IVD) herniation or stenosis or the co-occurrence of both causes. Prior to administering anesthesia, each of the uncovered structures was stimulated and measured, and the pain response was noted [23], as shown in Table 4. In the summary section, the authors concluded that muscle tension is not a cause of pain in the lumbar region of the spine, but rather is an impulse reaction to pain [23]. This study undermined the observations made by Wyke, who believed that IVD is not a source of pain, since it does not contain nerve endings [24]. The findings of Ksulish et al [23] were later confirmed by subsequent research, which showed penetration of the free nerve endings into the damaged IVD after its mechanical damage, as well as the invasion of free nerve endings into the separated free part of the IVD (sequestrum) [25].
Sensory dysfunctions, paresthesias, lack of tendon reflexes, weakening of muscle strength, and sphincter dysfunctions are syndromes of irritation of the root nerves or the cauda equina [26,27].
They may occur together with the pain or each may be isolated. They are present at an advanced stage of the disease and they generally accompany a massive narrowing of the spinal canal or the intervertebral openings [28,29]. These symptoms are radicular in nature, but in the case of multi-layer changes or a high degree of central narrowing, they may not be obvious. Dysfunctions of the sphincters are a very rare symptom of extreme narrowing of the lumbar region, always connected with other symptoms [29,30]. The incidence of radicular pain or “neurological” symptoms allows for the determination of a potential level of damage to the cauda equina or part of the root nerve. The incidence of local pain in the lumbar spine, which is potentially somatically radiating, makes any attempts to determine the level of damage impossible [28–30].
Clinical Symptoms for Patients with Stenosis of the Lumbar Region of the Spine
Symptoms for patients with congenital stenosis of the lumbar region of the spine manifest quite early, often at the age of 30 or 40 years old, while acquired stenoses manifest themselves as radiculopathy and claudication, usually after the age of 50 [31–33]. Symptoms often appear on one side, and then later affect both sides. Typically, neurogenic claudication begins bilaterally and is characterized by pain in the lower limbs, numbness, tingling, and reduced muscle strength [31–33]. Neurogenic claudication increases while standing and walking and decreases while sitting and lying down. Although patients cannot walk properly, they can travel relatively comfortably while seated [31–33]. Patients with central stenosis and those with lateral recess stenosis have resting pain and night pain, as well as pain while sneezing [31,33].
Central stenosis is often accompanied by lateral recess stenosis. In a neurological study, 60% of the patients with central stenosis and 43% with mixed stenosis exhibited Lasegue’s syndrome and a reverse Lasegue’s syndrome [33]. The mechanics, motor activity, reactions, and sensation most often reflect the level or levels of pathology. However, many patients either do not experience neurological symptoms or these symptoms are very slight. However, a common symptom of stenosis of the lumbar region of the spine is chronic dysfunction of the urinary bladder [34].
In studies done on animals, it was concluded that constant pressure applied to the nerve elements causes neurological degradation and loss of potential induced in the lower limbs [34]. This is followed by atrophy and demyelination caused by direct pressure onto the nerve roots and the shrinking and decrease of flow in the vessels that supply the nerve roots [34].
Radiculopathy and neurogenic claudication connected with stenosis of the vertebral canal are attributed both to direct and indirect pressure as a result of vascular insufficiency, which leads to ischemia of the nerve elements [35]. Standing and walking temporarily increases spine lordosis, causing stenosis by yellow ligaments bulging out into the central canal and lateral recesses, which increases the symptoms [36]. On the other hand, sitting and lying down decreases lordosis, opening up the vertebral canal, and increasing blood flow, as a result of which symptoms decrease [35,36]. The anthropoid position is characteristic of patients with neurogenic claudication, leaning forwards, decreases lumbar lordosis, and the pressure on the yellow ligaments and joint surfaces [35,36].
Differentiation in Degenerative Stenosis of the Lumbar Spine
Lumbar stenosis manifests itself with neurogenic claudication, which should be differentiated from vascular claudication [37]. Neurogenic claudication is a lateral or bilateral pain of the buttocks, hips, and thighs, especially while standing and sitting (strongly variable), while the pain decreases when the position is changed to sitting or lying down [37], and relief comes very quickly. In vascular claudication, limb pain is connected with muscular ischemia as a result of arteriosclerosis [37]. As opposed to vascular claudication, neurogenic claudication is induced by ischemia of the spinal nerve root, whose vessels are compressed by the surrounding structures [37]. Neurogenic claudication is very specific for lumbar stenosis [38].
Symptoms of trochanteric bursitis are similar to the symptoms of lumbar stenosis [39]. They generally include intermittent pain in the lateral part of the hip, which radiates to the lateral or dorsal part of the thigh [39]. Similarly to neurogenic claudication, it is experienced while standing and sitting, but the pain on the affected side does not recede while lying down [39]. The pain increases while moving in the area of the hip joint, especially in external rotation (positive Patrick test) [40]. Treating trochanteric bursitis is based on using non-steroid anti-inflammatory drugs, local steroid injections, and anesthetic drugs, using manual therapy (muscle stretching), as well as using ice compresses [40]. Prolapse of the nucleus pulposus often accompanies degenerative stenosis of the lumbar spine, and spondylolisthesis [40]. Mediolateral prolapse causes pressure on the dural sac and the nerve roots found within. Lateral prolapse causes a narrowing of the lateral recess and direct pressure on the nerve root [40]. Lateral hernia of the nucleus pulposus occurs in 7–12% of all disc hernias. Far-lateral prolapse of the nucleus pulpous causes pressure on the nerve root in the area of the pedicle of the arch [41,42].
The lumbar region of the spine, especially on the L4/L5 level, is predisposed to spondylolisthesis (the joint surfaces are placed more sagittally than coronally) [43]. The advancing dislocation leads to constriction of the cauda equina and nerve roots [43]. The disease most often affects middle-aged women at an average age of approximately 67 years [43]. Degenerative spondylolisthesis most often occurs on level L4/L5 and then on levels L3/L4, L2/L3, and L5/S1 [43].
Patients with diffuse back or lower-limb pain may suffer from cervical spinal stenosis or thoracic spinal stenosis [44]. However, in elderly patients with stenosis, neurological examination can determine that the symptoms are cephalic [44].
Synovial cyst is a rare pathology, clinically described in 1968, and its etiology is unknown [45]. It develops from the elements of the intervertebral joint, or less commonly the yellow ligament. Surgical treatment is the most common treatment [45]. Ossification of the yellow ligament can be a significant factor in the development of lumbar stenosis. Due to growth factors, the yellow ligament is induced to proliferate and it undergoes hypertrophy and then calcium saturation, and as a result, ossification [44]. Amyloidosis may also contribute to lumbar stenosis, as amyloid deposits were found in a hypertrophied yellow ligament [45].
Patients with diabetic neuropathy, diabetic amyotrophy, or angiopathy may be insufficiently diagnosed and undergo lumbar stenosis surgery [46]. Clinically, a patient with diabetes differs from a patient with lumbar stenosis due to the sudden appearance of pain, especially at night, a burning sensation when urinating, and no improvement as the body position changes [46]. Those suffering from diabetes with lumbar stenosis who have undergone decompression surgery are often less pleased after the surgery, while post-surgical treatment is longer [46].
Tumors in the cervical, thoracic, or lumbar region (especially the cauda equina and conus medullaris) may cause symptoms similar to the symptoms of lumbar stenosis [47,48].
Radiological Diagnosis of Patients with Degenerative Lumbar Stenosis of the Spine
RADIOGRAPHY:
With the aid of radiography (RTG), the outline of the vertebra and the lumbar spine, as well as its curvature, may be determined [62,63]. Dynamic X-ray testing allows us to determine the hypermobility and instability, which manifests itself in a more than 4 mm dislocation and more than 10 to 12 degrees of the angular fold [62,63]. X-ray imaging does not provide any significant information about lumbar stenosis [62,63]. Plain film in anterior-posterior (AP) and lateral projections may be useful, especially when spondylolisthesis is suspected [62,63]. Spot film X-rays of the lumbar spine in a lateral projection allow for an initial estimate of the degree of narrowing of the intervertebral space, facet arthrosis, spine stability, or narrowing of the intervertebral openings [62,63]. It is also possible to diagnose the hypertrophic process, especially pathological fracture. Currently, X-rays in an AP and lateral projections of the whole spine along with the hip joints are predominantly used for evaluation of frontal and sagittal balance [64].
MYELOGRAPHY:
Myelography can show constrictions of the contrast medium, with partial or complete blocking of the flow [65]. This test may be difficult to conduct due to low flow of cerebrospinal fluid and a thick bundle of nerve roots. Myelography is performed in a very few selected cases [65].
COMPUTED TOMOGRAPHY:
Computed tomography (CT) shows the characteristic shape of the spinal canal, which resembles a 3-leaf clover. CT allows for evaluation of the A-P dimension of the spina canal, hypertrophic yellow ligaments, and intervertebral joints, as well as protrusions of the intervertebral discs [66]. CT of the spine supplemented with 2 and 3-dimensional reconstructions allows for an exact diagnosis of recurrent stenosis, dislocation of the nucleus pulposus, fracture, and ossification of the posterior longitudinal ligament and yellow ligament [66]. Three-dimensional CT or CT myelography produce images of each axis of the spinal canal, and evaluation of the lateral and far-lateral regions [66]. Radiological computed tomography is especially useful in the diagnosis of skeletal changes as a supplementary test in the case of diagnostic ambiguities [67].
MAGNETIC RESONANCE:
Magnetic resonance imaging (MRI) is a test that better displays the soft tissue and enables the differentiation between scar and disc, while also showing tumors, demyelinating diseases, and infections [68]. An MRI shows pressure on the nerve element and a loss of signal of the cerebrospinal fluid [68]. An MRI also allows imaging of the soft tissues of the spinal canal, especially the nerve structures, and shows damage to the discs and intervertebral joints, yellow ligament hypertrophy, and presence of synovial cysts [68], which is why it is highly recommended for diagnosis of spinal canal narrowing and intervertebral openings [68,69]. MRI should always be carried out in case of suspicion of cancerous and inflammatory changes [70].
Pharmacotherapy, Rehabilitation, and Surgical Treatment of Patients with Degenerative Lumbar Spine Stenosis
PHARMACOTHERAPY TREATMENT OF PATIENTS WITH DEGENERATIVE LUMBAR SPINE STENOSIS:
The introduction of non-steroid anti-inflammatory drugs brings relief to pain caused by inflammation of the spinal joints [71]. On the other hand, in the case of symptomatic central lumbar stenosis, using non-steroid anti-inflammatory drugs, opioids, or non-opioid painkillers, myorelaxants, antidepressants, or tranquilizers yields little benefit in reducing the symptoms of cauda equina claudication [71]. Steroids administered orally or in epidural injections are effective, but they can only be taken for a limited amount of time [71,72].
In the treatment of chronic and neuropathic pain, anticonvulsants such as gabapentin and carbamazepine have had a positive effect [73]. Their multi-factor functioning mechanism includes reducing the experience of pain, increasing the pain threshold, and improving sleep [73]. These drugs should not be used in treating acute pain [73]. Tricyclic antidepressants (eg, amitriptyline) are also used in treating neuropathic pain; however, adverse effects limit their use. Currently, the most often used drug is gabapentin [73].
Opioid drugs are very strong painkillers. Tramadol in combination with paracetamol is most commonly used [74]. Using other strong opioid drugs to treat pain in degenerative spine disease is very limited and are commonly used in treatment of post-surgical pain [74].
Myorelaxants are often used to increase the painkilling activity of non-steroidal anti-inflammatory drugs or painkillers [75]. Typically, they are administered before going to sleep, taking advantage of their slight sedative effect [75].
Selective blocking of spinal structures with the use of painkillers (lidocaine or bupivacaine) and long-acting steroid drugs are used in pain treatment, especially for patients who should not be surgically treated [76]. Injections may be used to treat pain from the facet joints, sacroiliac joints, or intervertebral discs [76]. Furthermore, it is possible to block the nerve roots or perform injections into the epidural space [76]. The effectiveness of the above-mentioned method is estimated at 52–100%, with the highest effectiveness (75–100% in limiting pain in the facet joints [77].
Rehabilitation Treatment of Patients with Degenerative Lumbar Spine Stenosis
SURGICAL TREATMENT OF PATIENTS WITH DEGENERATIVE LUMBAR SPINE STENOSIS:
Surgical procedures enable faster alleviation of symptoms than with behavioral treatment and bring more long-term benefits [90]. From a long-term perspective, surgical treatment is also cheaper than behavioral treatment [90].
Surgical procedures used for degenerative disease of the lumbar spine must be divided into procedures that retain motion as well as surgeries with stiffening that lead to spondylodesis [91]. All may be performed as a single-level or multi-level procedure [91].
Surgical treatment of lumbar stenosis is based on decompression of nerve elements. To properly decompress the nerve elements, decompressive laminectomy is used, which removes the vertebral arch and the yellow ligament and broadens the root canal [36]. This type of treatment is highly effective and decreases the pain that is typical for lumbar stenosis [36]. It is not necessary to remove the skeletal abdominal osteophytes or the calcified protrusions of the intervertebral discs [36]. After surgical treatment, physical fitness is restored and pain tolerance while walking and standing is increased [36]. However, laminectomy does not decrease pain connected with inflammation of the spinal joints and instability [36]. When the spinal joints or the disc space are damaged, the pain resulting from inflammation of the intervertebral joints or instability can increase [36].
In addition to decompression, it may sometimes be necessary to remove the prolapsed nucleus pulposus [92]. Many surgeons, apart from performing decompressions, also perform fusions, which yield the worst results among the oldest patients [92]. Sometime after the surgery, there are both back and limb pain, as well as neurological deficits. Second lumbar stenosis yields worse results, and patients have better treatment results after 1 surgery than after 2 [93,94]. The frequency of repeated decompression is 9.3–28%. For every 100 patients, 16 have experienced recurrent stenosis on the operated level or higher [93,94]. The longer the observation time after the original decompressive laminectomy, the higher the percentage of repeated surgeries [93,94]. Posterolateral stabilization is recommended for patients with lumbar stenosis with coexisting spondylolisthesis requiring decompression [94]. Transpedicular stabilization in addition to posterolateral stabilization may be considered in stenosis and spondylolisthesis if there is preoperative instability or kyphosis on the level of the spondylolisthesis or if there is also iatrogenic instability [94]. Stability may strengthen degeneration in neighboring levels and thus is only recommended on the level of the spondylolisthesis [94].
Younger patients who experience instability after surgery require stability [95]. For older patients, stability is often associated with a higher mortality rate and more complications. Instability after lumbar stenosis surgery via laminectomy seldom requires stabilization [95]. Decompressed of more levels is associated with higher risk of slippage [95].
It is estimated that approximately 5% of patients who have undergone laminectomy require stabilization [96]. Lumbar instability after decompressive laminectomy is quite rare (1%) [96]. Fusion is rarely needed in subluxation and degenerative stenosis. Stability is maintained when 50–66% of the intervertebral joint remains and when the disc space remains intact [96]. Younger and more active patients are more susceptible to instability. Post-surgical instability is verified by functional X-ray images of the lumbosacral spine before and after surgery [96].
Posterolateral stabilization is not recommended for patients with lumbar stenosis after decompressive surgery unless there is evident spondylolisthesis and intraoperative facetectomy [97]. Posterolateral stabilization is recommended for patients with lumbar instability, while transpedicular stabilization is not recommended in combination with posterolateral stabilization [97]. Table 5 summarizes the surgical procedures that allow patients to retain spinal motion on the operated levels or that result in stiffening and spondylodesis [91].
Future Directions
Because of the multifactorial nature of pain and the inability to determine the primary cause of low back pain syndromes based on imaging studies and clinical conditions, including those in the course of spinal canal stenosis, as well as the physical, psychological, and social consequences of LSS, it is necessary to develop a holistic, multidisciplinary approach to patients and their disease [66]. The diagnostic and therapeutic process should include the performance of imaging studies, a neurological examination, a thorough interview with the patient, and provision of pharmaceutical care, as well as care from a physiotherapist, neurologist, orthopedist, or neurosurgeon/neuro-orthopedist [98]. There is also need for psychological support [98]. Only when specialists in various fields jointly assess the patient’s condition is it possible to establish a treatment regimen tailored to each patient, which is part of the trend of personalized medicine [98]. It is also possible that, in addition to the traditionally accepted methods of treatment, the use of “unconventional” methods of treatment, such as acupuncture, herbalism, and folk medicine, should be thoroughly investigated, adding these techniques to the overall arsenal of possibilities [99]. It is also important to establish a registry of patients with LBP or LSS at the local and national, and perhaps international, levels to record and analyze the outcomes of patients at all stages of care, taking into account the various treatment methods, to better assess the effectiveness of various treatment options [100]. An interesting option is to use machine learning to create diagnostic and therapeutic algorithms in patients with LBP or LSS [100].
Conclusions
Back pain is becoming an increasingly common problem, affecting more than just older people. In addition, we live in a time of continuous development in LBP diagnosis and therapy, so it is important to constantly keep up with trends to provide patients with the highest-quality services.
In this literature review, we have turned our attention to the etiopathogenesis of pain accompanying LBP and LSS. The available literature and our own experience indicate that it is impossible to determine the exact reason for the pain syndromes of the lumbar spine region based on imaging and clinical condition tests [8]. Currently, in the neuroimaging diagnosis of LBP and LSS, X-ray imaging is used, which in most cases is the starting point for more advanced imaging studies, such as CT and MRI. MRI, which allows visualization of bony structures and soft tissues, is the criterion standard in diagnosing spinal pain. Finally, treatment should always be tailored to the patient’s clinical condition and reported symptoms and their severity, not just changes visualized on imaging studies. This should be guided by the principle that conservative treatment, including pharmacotherapy and rehabilitation, should be used first and, only later, when necessary, surgical treatment. Therefore, this review has assessed the current knowledge and future research directions.
Tables
Table 1. Causes of pain in the lumbar region of the spine.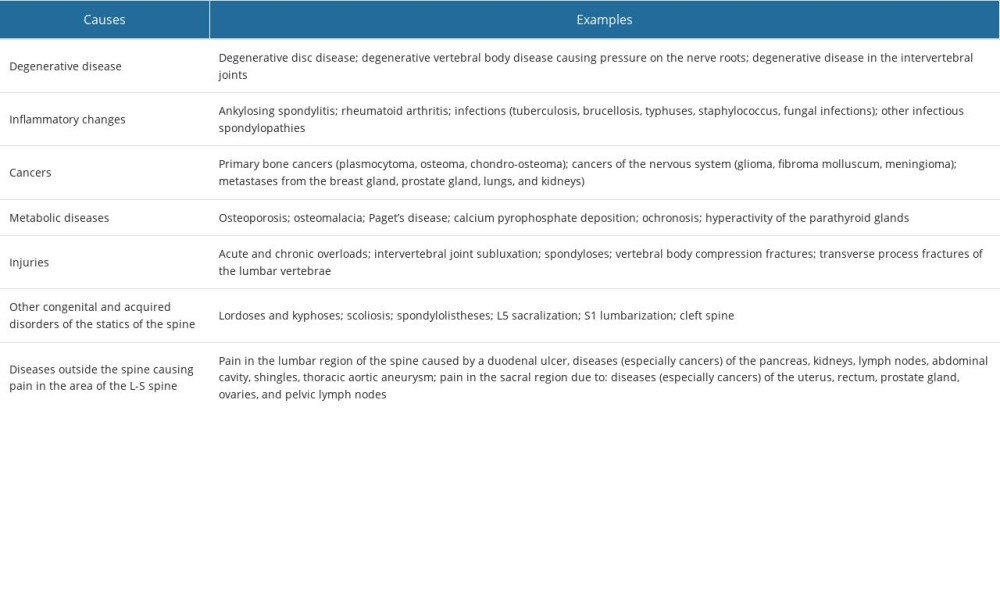 Table 2. Categories of spinal pain according to the location of pain and the type of pathology.
Table 2. Categories of spinal pain according to the location of pain and the type of pathology.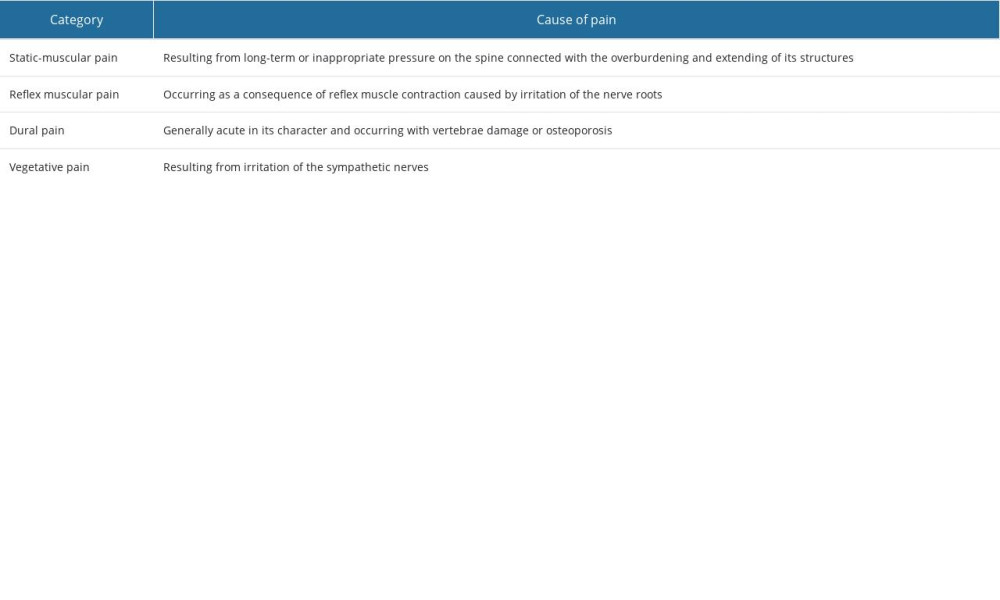 Table 3. Categories of spinal pain according to the structures, which may be the potential source of back pain.
Table 3. Categories of spinal pain according to the structures, which may be the potential source of back pain.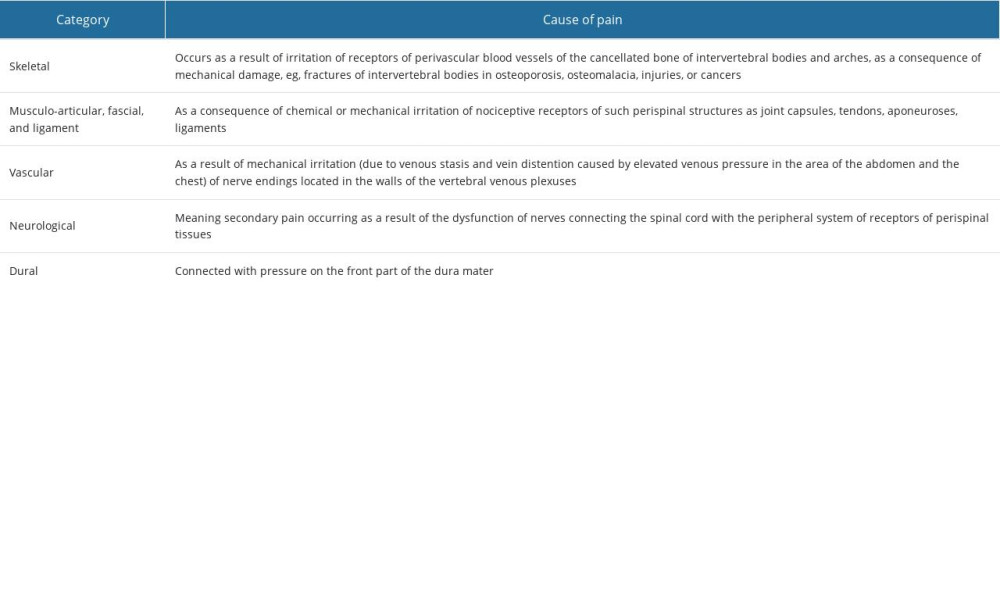 Table 4. Sources of pain in degenerative spine disease.
Table 4. Sources of pain in degenerative spine disease.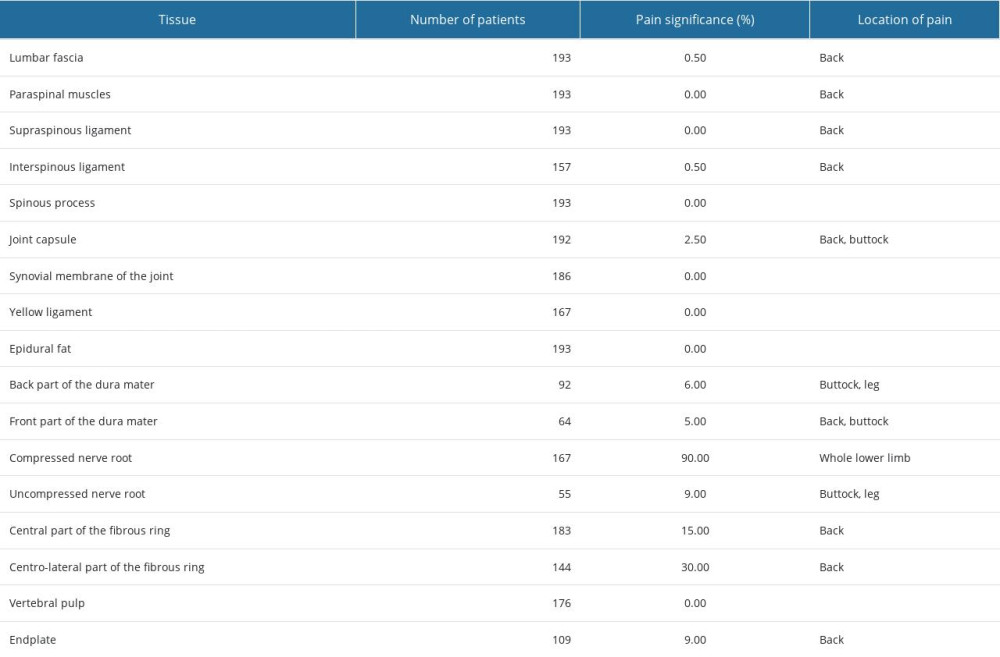 Table 5. Surgical procedures that allow patients to retain spinal motion on the operated levels or that result in stiffening and spondylodesis.
Table 5. Surgical procedures that allow patients to retain spinal motion on the operated levels or that result in stiffening and spondylodesis.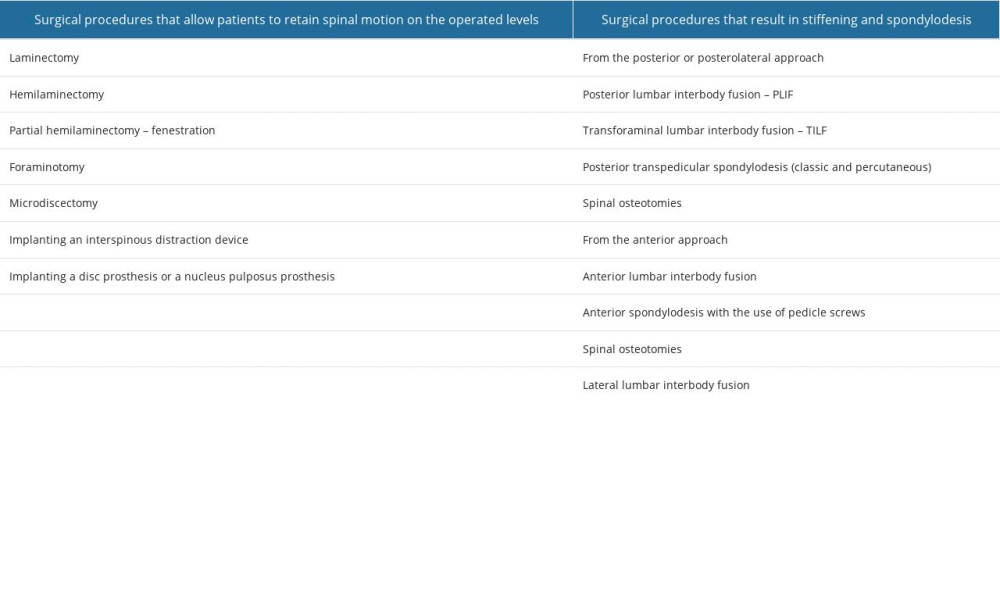
References
1. Kahere M, Hlongwa M, Ginindza TG, A scoping review on the epidemiology of chronic low back pain among adults in Sub-Saharan Africa: Int J Environ Res Public Health, 2022; 19(5); 2964
2. Knezevic NN, Candido KD, Vlaeyen JWS, Low back pain: Lancet, 2021; 398(10294); 78-92
3. Jana A, Paul A, Epidemiology of low back pain: A literature review: Int J Phys Educ Sports Heal, 2019; 6(3); 233-37
4. Carregaro RL, Tottoli CR, da Silva Rodrigues D, Low back pain should be considered a health and research priority in Brazil: Lost productivity and healthcare costs between 2012 to 2016: PLoS One, 2020; 15(4); e0230902
5. Jensen RK, Jensen TS, Koes B, Hartvigsen J, Prevalence of lumbar spinal stenosis in general and clinical populations: a systematic review and meta-analysis: Eur Spine J, 2020; 29(9); 2143-63
6. Wei Q, Zhang X, Zhou C, Roles of large aggregating proteoglycans in human intervertebral disc degeneration: Connect Tissue Res, 2019; 60(3); 209-18
7. Martin BI, Mirza SK, Spina N, Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015: Spine, 2019; 44(5); 369-76
8. Hall AM, Aubrey-Bassler K, Thorne B, Maher CG, Do not routinely offer imaging for uncomplicated low back pain: BMJ, 2021; 372; n291
9. Boden SD, Davis DO, Dina TS, Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation: J Bone Joint Surg Am, 1990; 72(3); 403-8
10. Zytkowski A, Sosnowski S, Wrodycka BSpondylarthrosis etiopathogenesis: Pol Merkur Lekarski, 2006; 21(125); 498-501 [in Polish]
11. Emami F, Yoosefinejad AK, Razeghi M, Correlations between core muscle geometry, pain intensity, functional disability and postural balance in patients with nonspecific mechanical low back pain: Med Eng Phys, 2018; 60; 39-46
12. Will JS, Bury DC, Miller JA, Mechanical low back pain: Am Fam Physician, 2018; 98(7); 421-28
13. Handa R, Low back pain-myths and facts: J Clin Orthop Trauma, 2019; 10(4); 828-30
14. Izzo R, Popolizio T, D’Aprile P, Muto M, Spinal pain: Eur J Radiol, 2015; 84(5); 746-56
15. Jagucka-Mętel W, Machoy-Mokrzyńska A, Nowicki A, Sobolewska E, Lumbosacral ailments of the spine in workers of Szczecin Universities – functional anatomy, diagnostics, and selected forms of physiotherapy: Pomeranian J Life Sci, 2018; 64(2); 69-73
16. Spivak JM, Degenerative lumbar spinal stenosis: J Bone Joint Surg Am, 1998; 80(7); 1053-66
17. Kachonkittisak K, Kunakornsawat S, Pluemvitayaporn T, Congenital spinal canal stenosis with ossification of the ligamentum flavum in an achondroplastic patient: A case report and literature review: Asian J Neurosurg, 2019; 14(4); 1231-35
18. Kamska V, Daley M, Badri-Spröwitz A, 3D Anatomy of the quail lumbosacral spinal canal-implications for putative mechanosensory function: Integr Org Biol, 2020; 2(1); obaa037
19. Marcia S, Zini C, Bellini M, Image-guided percutaneous treatment of lumbar stenosis and disc degeneration: Neuroimaging Clin N Am, 2019; 29(4); 563-80
20. Murata K, Akeda K, Takegami N, Morphology of intervertebral disc ruptures evaluated by vacuum phenomenon using multi-detector computed tomography: Association with lumbar disc degeneration and canal stenosis: BMC Musculoskelet Disord, 2018; 19(1); 164
21. Rauschning W, Pathoanatomy of lumbar disc degeneration and stenosis: Acta Orthop Scand Suppl, 1993; 251; 3-12
22. Kirkaldy-Willis WH, Wedge JH, Pathology and pathogenesis of lumbar spondylosis and stenosis: Spine, 1978; 3(4); 319-28
23. Kuslich SD, Ulstrom CL, Michael CJ, The tissue origin of low back pain and sciatica: A report of pain response to tissue stimulation during operations on the lumbar spine using local anesthesia: Orthop Clin North Am, 1991; 22(2); 181-87
24. Wyke BD, Neurological aspects of pain therapy: The therapy of pain. Current Status of Modern Therapy, 1981; 1-30, Netherlands, Springer
25. Chapman KB, Groenen PS, Vissers KC, The pathways and processes underlying spinal transmission of low back pain: Observations from dorsal root ganglion stimulation treatment: Neuromodulation J Int Neuromodulation Soc, 2021; 24(4); 610-21
26. Hoeritzauer I, Pronin S, Carson A, The clinical features and outcome of scan-negative and scan-positive cases in suspected cauda equina syndrome: a retrospective study of 276 patients: J Neurol, 2018; 265(12); 2916-26
27. Long B, Koyfman A, Gottlieb M, Evaluation and management of cauda equina syndrome in the emergency department: Am J Emerg Med, 2020; 38(1); 143-48
28. van Gorp EJJAA, Teernstra OPM, Gültuna I, Subcutaneous stimulation as ADD-ON therapy to spinal cord stimulation is effective in treating low back pain in patients with failed back surgery syndrome: A multicenter randomized controlled trial: Neuromodulation Technol Neural Interface, 2016; 19(2); 171-78
29. Mendenhall SK, Parker SL, Adogwa O, Long-term outcomes after revision neural decompression and fusion for same-level recurrent lumbar stenosis: Defining the effectiveness of surgery: J Spinal Disord Tech, 2014; 27(7); 353-57
30. Lall MP, Restrepo E, Predictors of weeks to opioid cessation after lumbar fusion: A prospective cohort study: Pain Manag Nurs, 2018; 19(5); 525-34
31. Kaito T, Yamato Y, The essence of clinical practice guidelines for lumbar disc herniation, 2021: 3. Diagnosis: Spine Surg Relat Res, 2022; 6(4); 325-28
32. Ekedahl H, Jönsson B, Annertz M, Frobell RB, Accuracy of clinical tests in detecting disk herniation and nerve root compression in subjects with lumbar radicular symptoms: Arch Phys Med Rehabil, 2018; 99(4); 726-35
33. Haro H, Ebata S, Inoue G, Japanese Orthopaedic Association (JOA) clinical practice guidelines on the management of lumbar disc herniation, third edition – secondary publication: J Orthop Sci, 2022; 27(1); 31-78
34. Abdin AJ, Early Surgical management for Neurological intermittent claudication: Damascus Univ J Health Sci, 2015; 31(1); 51-58
35. Ammendolia C, Hofkirchner C, Plener J, Non-operative treatment for lumbar spinal stenosis with neurogenic claudication: an updated systematic review: BMJ Open, 2022; 12(1); e057724
36. Deer T, Sayed D, Michels J, A review of lumbar spinal stenosis with intermittent neurogenic claudication: Disease and diagnosis: Pain Med, 2019; 20(Suppl 2); S32-S44
37. Ko S, Oh T, Comparison of bilateral decompression via unilateral laminotomy and conventional laminectomy for single-level degenerative lumbar spinal stenosis regarding low back pain, functional outcome, and quality of life – a randomized controlled, prospective trial: J Orthop Surg Res, 2019; 14(1); 252
38. De Biase G, Gruenbaum SE, Quiñones-Hinojosa A, Abode-Iyamah KO, Spine surgery under spinal vs general anesthesia: Prospective analysis of quality of life, fatigue, and cognition: Neurosurgery, 2022; 90(2); 186-91
39. Lozano AM, Gildenberg PL, Tasker RR: Textbook of stereotactic and functional neurosurgery, 2009; 1 & 2
40. Carpenter K, Decater T, Iwanaga J, Revisiting the vertebral venous plexus – a comprehensive review of the literature: World Neurosurg, 2021; 145; 381-95
41. Nicoletti GF, Umana GE, Chaurasia B, Navigation-assisted extraforaminal lumbar disc microdiscectomy: Technical note: J Craniovertebr Junction Spine, 2020; 11(4); 316-20
42. Kim SK, Kang SS, Hong YH, Clinical comparison of unilateral biportal endoscopic technique versus open microdiscectomy for single-level lumbar discectomy: A multicenter, retrospective analysis: J Orthop Surg Res, 2018; 13(1); 22
43. Covaro A, Vilà-Canet G, de Frutos AG, Management of degenerative lumbar spinal stenosis: An evidence-based review: EFORT Open Rev, 2017; 1(7); 267-74
44. Epstein NE, Epstein JA, Carras R, Coexisting cervical and lumbar spinal stenosis: Diagnosis and management: Neurosurgery, 1984; 15(4); 489-96
45. Bergström J, Gustavsson A, Hellman U, Amyloid deposits in transthyretin-derived amyloidosis: Cleaved transthyretin is associated with distinct amyloid morphology: J Pathol, 2005; 206(2); 224-32
46. Maruf MH, Suzuki A, Hayashi K, Increased advanced glycation end products in hypertrophied ligamentum flavum of diabetes mellitus patients: Spine J, 2019; 19(10); 1739-45
47. LoRusso S, Disorders of the cauda equina: Continuum (Minneap Minn), 2021; 27(1); 205-24
48. Diehn FE, Krecke KN, Neuroimaging of spinal cord and cauda equina disorders: Continuum (Minneap Minn), 2021; 27(1); 225-63
49. Verbiest H, Pathomorphologic aspects of developmental lumbar stenosis: Orthop Clin North Am, 1975; 6(1); 177-96
50. Schonstrom NS, Bolender NF, Spengler DM, The pathomorphology of spinal stenosis as seen on CT scans of the lumbar spine: Spine (Phila Pa 1976), 1985; 10(9); 806-11
51. Schönström N, Hansson T, Pressure changes following constriction of the cauda equina. An experimental study in situ: Spine (Phila Pa 1976), 1988; 13(4); 385-88
52. Ogikubo O, Forsberg L, Hansson T, The relationship between the cross-sectional area of the cauda equina and the preoperative symptoms in central lumbar spinal stenosis: Spine (Phila Pa 1976), 2007; 32(13); 1423-29
53. Bolender NF, Schönström NS, Spengler DM, Role of computed tomography and myelography in the diagnosis of central spinal stenosis: J Bone Joint Surg Am, 1985; 67(2); 240-46
54. Ullrich CG, Binet EF, Sanecki MG, Kieffer SA, Quantitative assessment of the lumbar spinal canal by computed tomography: Radiology, 1980; 134(1); 137-43
55. Schizas C, Theumann N, Burn A, Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images: Spine (Phila Pa 1976), 2010; 35(21); 1919-24
56. Lee BH, Moon SH, Suk KS, Lumbar spinal stenosis: Pathophysiology and treatment principle: A narrative review: Asian Spine J, 2020; 14(5); 682-93
57. Sartoretti E, Wyss M, Alfieri A, Introduction and reproducibility of an updated practical grading system for lumbar foraminal stenosis based on high-resolution MR imaging [published correction appears in Sci Rep. 2021 Sep 15;11(1): 18732]: Sci Rep, 2021; 11(1); 12000
58. Haleem S, Malik M, Guduri V, The Haleem-Botchu classification: A novel CT-based classification for lumbar foraminal stenosis: Eur Spine J, 2021; 30(4); 865-69
59. Telfeian AE, Oyelese A, Fridley J, Gokaslan ZL, Transforaminal endoscopic decompression in the setting of lateral lumbar spondylolisthesis: World Neurosurg, 2018; 117; 321-25
60. Ploumis A, Transfeldt EE, Gilbert TJ, Degenerative lumbar scoliosis: Radiographic correlation of lateral rotatory olisthesis with neural canal dimensions: Spine (Phila Pa 1976), 2006; 31(20); 2353-58
61. Machino M, Yukawa Y, Ito K, Dynamic changes in dural sac and spinal cord cross-sectional area in patients with cervical spondylotic myelopathy: Cervical spine: Spine (Phila Pa 1976), 2011; 36(5); 399-403
62. Wáng YXJ, Wu AM, Ruiz Santiago F, Nogueira-Barbosa MH, Informed appropriate imaging for low back pain management: A narrative review: J Orthop Translat, 2018; 15; 21-34
63. van den Bosch MA, Hollingworth W, Evidence against the use of lumbar spine radiography for low back pain: Clin Radiol, 2004; 59(1); 69-76
64. Widmer J, Fornaciari P, Senteler M, Kinematics of the spine under healthy and degenerative conditions: A systematic review: Ann Biomed Eng, 2019; 47(7); 1491-522
65. Kim DK, Brinjikji W, Morris PP, Lateral decubitus digital subtraction myelography: Tips, tricks, and pitfalls: Am J Neuroradiol, 2020; 41(1); 21-28
66. da Costa RC, De Decker S, Lewis MJ, Volk HCanine Spinal Cord Injury Consortium (CANSORT-SCI), Diagnostic imaging in intervertebral disc disease: Front Vet Sci, 2020; 7; 588338
67. Gellad F, Rao KC, Joseph PM, Vigorito RD, Morphology and dimensions of the thoracic cord by computer-assisted metrizamide myelography: Am J Neuroradiol, 1983; 4(3); 614-17
68. Ogon I, Takebayashi T, Takashima H, Imaging diagnosis for intervertebral disc: JOR Spine, 2019; 3(1); e1066
69. Han Z, Gao L, Shi Q, Quantitative magnetic resonance imaging for diagnosis of intervertebral disc degeneration of the cervico-thoracic junction: A pilot study: Am J Transl Res, 2018; 10(3); 925-35
70. Khodjaeva DI, Magnetic-resonance imaging in the diagnosis of breast cancer and its metastasis to the spinal column: Sci Prog, 2021; 2(6); 540-47
71. Greeff OBW, The pharmacotherapy of lower back pain: SA Pharm J, 2022; 89(2); 13-15
72. Schreijenberg M, Koes BW, Lin CC, Guideline recommendations on the pharmacological management of non-specific low back pain in primary care – is there a need to change?: Expert Rev Clin Pharmacol, 2019; 12(2); 145-57
73. Coles S, Dabbs W, Wild S, Pharmacologic management of chronic pain: Prim Care, 2022; 49(3); 387-401
74. Tucker HR, Scaff K, McCloud T, Harms and benefits of opioids for management of non-surgical acute and chronic low back pain: A systematic review: Br J Sports Med, 2020; 54(11); 664
75. Csiba L, Zhussupova AS, Likhachev SAA systematic review of using myorelaxants in treatment of low back pain: Zh Nevrol Psikhiatr Im S S Korsakova, 2018; 118(12); 100-13 [in Russian]
76. Boswell MV, Trescot AM, Datta S, Interventional techniques: Evidence-based practice guidelines in the management of chronic spinal pain: Pain Physician, 2007; 10(1); 7-111
77. Parr AT, Manchikanti L, Hameed H, Caudal epidural injections in the management of chronic low back pain: A systematic appraisal of the literature: Pain Physician, 2012; 15(3); E159-98
78. Jacobi S, Beynon A, Dombrowski SU, Effectiveness of conservative nonpharmacologic therapies for pain, disability, physical capacity, and physical activity behavior in patients with degenerative lumbar spinal stenosis: A systematic review and meta-analysis: Arch Phys Med Rehabil, 2021; 102(11); 2247-60e7
79. Lv B, Sun S, Wang H, Clinical efficacy and rehabilitation of microscopic “over the top” for bilateral decompression in degenerative lumbar stenosis: A retrospective study: Biomed Res Int, 2020; 2020; 7174354
80. Schott C, Zirke S, Schmelzle JM, Effectiveness of lumbar orthoses in low back pain: Review of the literature and our results: Orthop Rev (Pavia), 2018; 10(4); 7791
81. Keller A, Hayden J, Bombardier C, van Tulder M, Effect sizes of non-surgical treatments of non-specific low-back pain: Eur Spine J, 2007; 16(11); 1776-88
82. Mills DS, Demontigny-Bédard I, Gruen M, Pain and problem behavior in cats and dogs: Animals (Basel), 2020; 10(2); 318
83. Coppock JA, Zimmer NE, Englander ZA, In vivo intervertebral disc mechanical deformation following a treadmill walking “stress test” is inversely related to T1rho relaxation time: Osteoarthritis Cartilage, 2023; 31(1); 126-33
84. Belavý DL, Quittner MJ, Ridgers N, Running exercise strengthens the intervertebral disc: Sci Rep, 2017; 7; 45975
85. Lam OT, Strenger DM, Chan-Fee M, Effectiveness of the McKenzie method of mechanical diagnosis and therapy for treating low back pain: Literature review with meta-analysis: J Orthop Sports Phys Ther, 2018; 48(6); 476-90
86. Namnaqani FI, Mashabi AS, Yaseen KM, Alshehri MA, The effectiveness of McKenzie method compared to manual therapy for treating chronic low back pain: A systematic review: J Musculoskelet Neuronal Interact, 2019; 19(4); 492-99
87. Halliday MH, Pappas E, Hancock MJ, A randomized controlled trial comparing the mckenzie method to motor control exercises in people with chronic low back pain and a directional preference: J Orthop Sports Phys Ther, 2016; 46(7); 514-22
88. Tagliaferri SD, Miller CT, Ford JJ, Randomized trial of general strength and conditioning versus motor control and manual therapy for chronic low back pain on physical and self-report outcomes: J Clin Med, 2020; 9(6); 1726
89. Verburg AC, van Dulmen SA, Kiers H, Development of a standard set of outcome measures for non-specific low back pain in Dutch primary care physiotherapy practices: A Delphi study: Eur Spine J, 2019; 28(7); 1550-64
90. Medress ZA, Jin MC, Feng A, Medical malpractice in spine surgery: A review: Neurosurg Focus, 2020; 49(5); E16
91. Postacchini F, Cinotti G, Perugia D, Gumina S, The surgical treatment of central lumbar stenosis. Multiple laminotomy compared with total laminectomy: J Bone Joint Surg Br, 1993; 75(3); 386-92
92. Schneider MJ, Ammendolia C, Murphy DR, Comparative clinical effectiveness of nonsurgical treatment methods in patients with lumbar spinal stenosis: A randomized clinical trial: JAMA Netw Open, 2019; 2(1); e186828
93. Ulrich NH, Burgstaller JM, Valeri F, Incidence of revision surgery after decompression with vs without fusion among patients with degenerative lumbar spinal stenosis: JAMA Netw Open, 2022; 5(7); e2223803
94. Katz JN, Lipson SJ, Lew RA, Lumbar laminectomy alone or with instrumented or noninstrumented arthrodesis in degenerative lumbar spinal stenosis: Patient selection, costs, and surgical outcomes: Spine, 1997; 22(10); 1123-31
95. Müller SJ, Burkhardt BW, Oertel JM, Management of dural tears in endoscopic lumbar spinal surgery: A review of the literature: World Neurosurg, 2018; 119; 494-99
96. Spina NT, Moreno GS, Brodke DS, Biomechanical effects of laminectomies in the human lumbar spine: A finite element study: Spine J, 2021; 21(1); 150-59
97. Resnick DK, Watters WC, Mummaneni PV, Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 10: Lumbar fusion for stenosis without spondylolisthesis: J Neurosurg Spine, 2014; 21(1); 62-66
98. van Dieën JH, Reeves NP, Kawchuk G, Analysis of motor control in patients with low back pain: A key to personalized care?: J Orthop Sports Phys Ther, 2019; 49(6); 380-88
99. Nisa U, Triyono A, Ardiyanto D, Ethnopharmacological study of medicinal plants indigenous knowledge about low back pain therapy in Sumatra, Indonesia: J Appl Pharm Sci, 2022; 12(9); 178-88
100. Senders JT, Staples PC, Karhade AV, Machine learning and neurosurgical outcome prediction: A systematic review: World Neurosurg, 2018; 109; 476-86e1
Tables
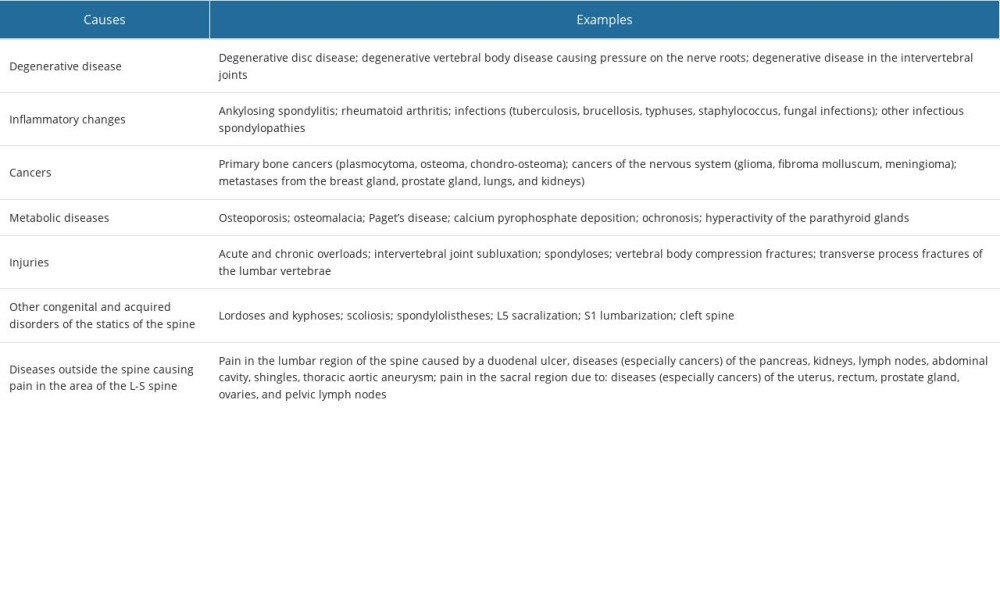 Table 1. Causes of pain in the lumbar region of the spine.
Table 1. Causes of pain in the lumbar region of the spine.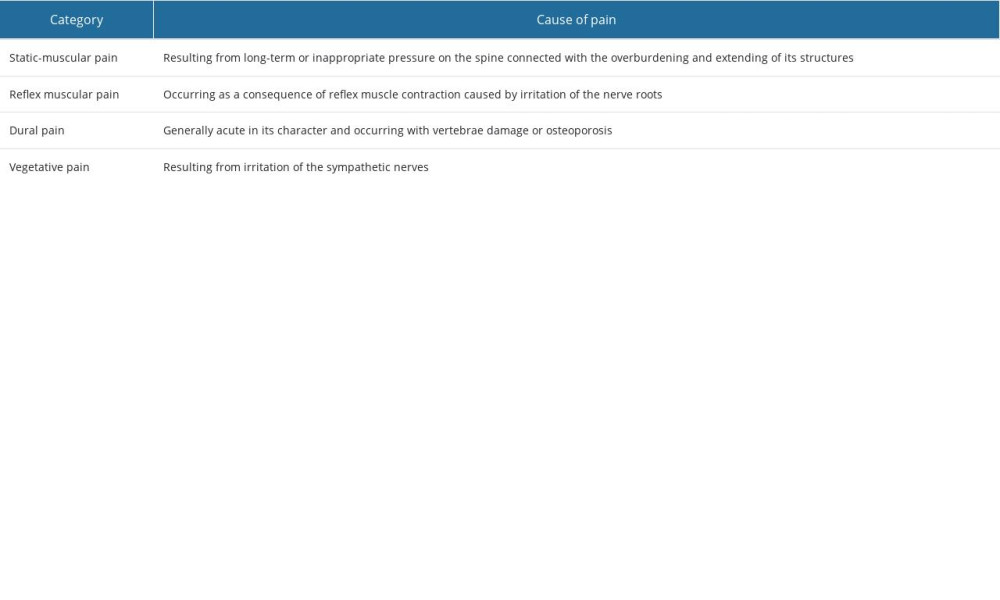 Table 2. Categories of spinal pain according to the location of pain and the type of pathology.
Table 2. Categories of spinal pain according to the location of pain and the type of pathology.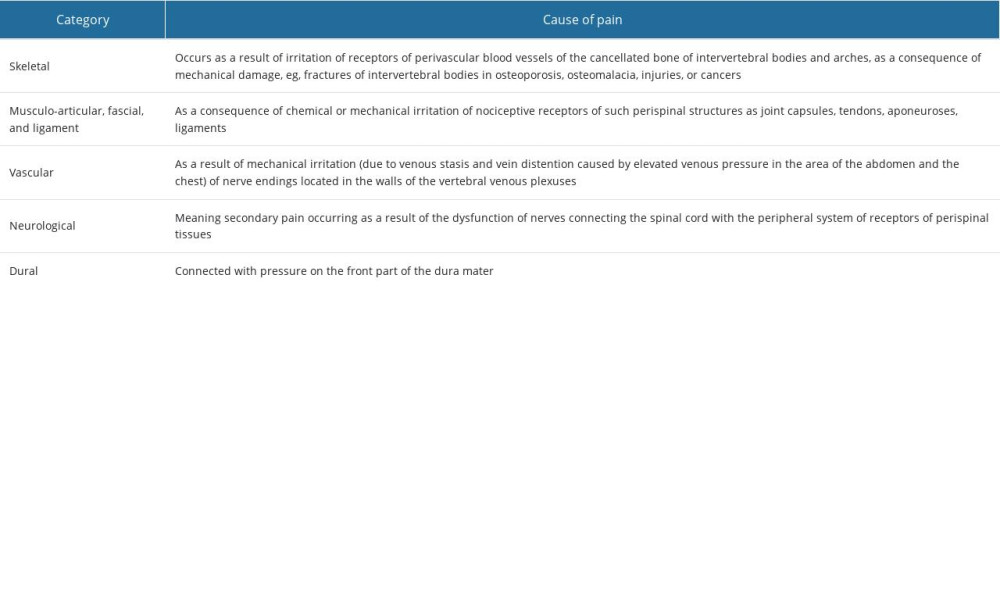 Table 3. Categories of spinal pain according to the structures, which may be the potential source of back pain.
Table 3. Categories of spinal pain according to the structures, which may be the potential source of back pain.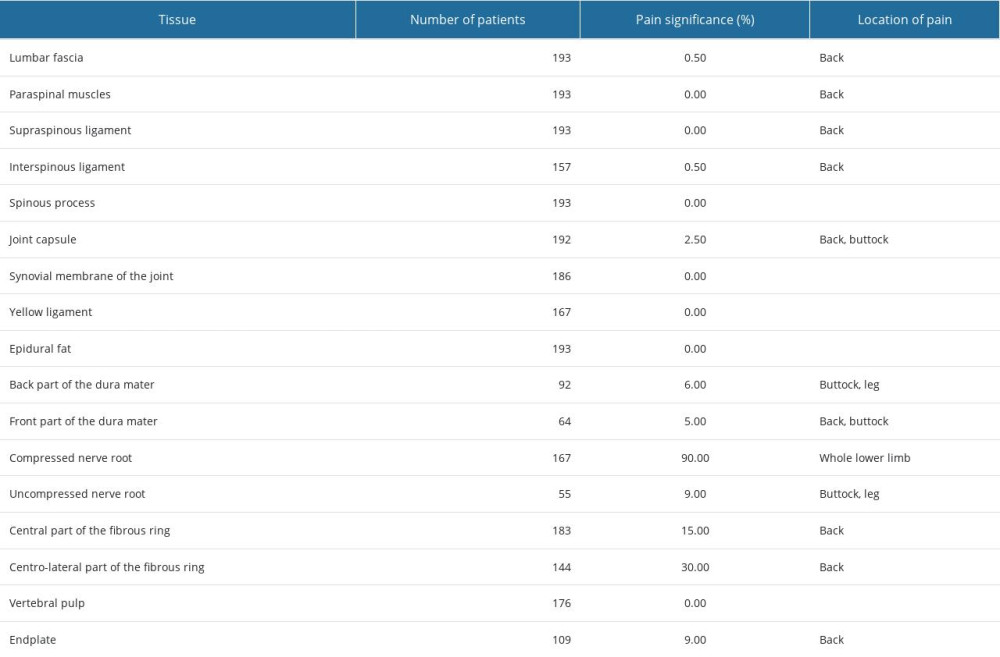 Table 4. Sources of pain in degenerative spine disease.
Table 4. Sources of pain in degenerative spine disease.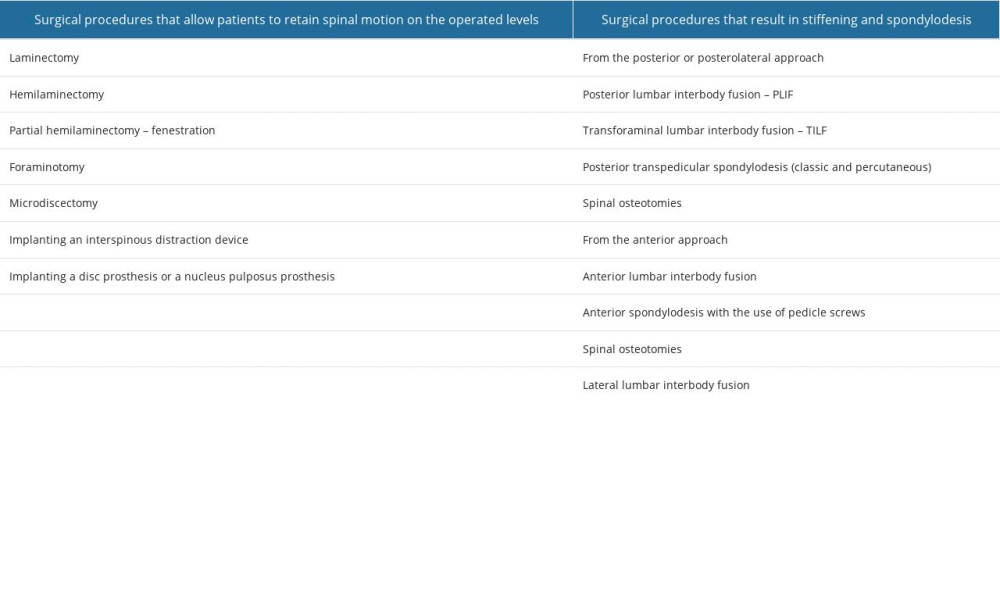 Table 5. Surgical procedures that allow patients to retain spinal motion on the operated levels or that result in stiffening and spondylodesis.
Table 5. Surgical procedures that allow patients to retain spinal motion on the operated levels or that result in stiffening and spondylodesis. In Press
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








