13 March 2023: Clinical Research
Evaluation of Sympathetic Vasomotor Activity of the Brachial Arteries Using Doppler Ultrasound
Omer KazciDOI: 10.12659/MSM.939352
Med Sci Monit 2023; 29:e939352
Abstract
BACKGROUND: The sympathetic nervous system is principally accountable for peripheral artery regulation, and its effect is that vasospasm occurs in the medium and large arteries of the extremities, resulting in decreased flow of blood. Because of this information of how the body works, our goal is to create a noninvasive and repeatable self-test model that uses Doppler ultrasound examination.
MATERIAL AND METHODS: The study was conducted on 31 healthy and active participants who volunteered for the study. Written informed consent was obtained from all participants. The baseline diameter and flow rates of the brachial artery from 2 cm superior to the antecubital fossa were determined using a Doppler probe, which remained stationary throughout the experiment, allowing for continuous measurements. Then, to activate the sympathetic fibers, an electrical stimulus was applied for 5 s with an intensity of 10 mA and frequency of 1 Hz at the level of the median nerve at the wrist via the bipolar stimulation electrode. Immediately following the sixth stimulation, the artery diameter and flow rates were assessed again.
RESULTS: Following the stimulation, a statistically significant decrease in flow rate was observed (P<0.001). Moreover, stimulation resulted in a statistically significant reduction in the diameter of the brachial artery (P<0.001).
CONCLUSIONS: Our research suggests that Doppler ultrasonography can be routinely used to detect the normal and abnormal functioning of the peripheral sympathetic nervous system.
Keywords: Ultrasonography, Doppler, Median Neuropathy, Median Nerve, Median Neuropathy, Diabetic Neuropathies, Median Neuropathy, Brachial Artery, Median Neuropathy, Humans, Ultrasonography, Sympathetic Nervous System, Blood Flow Velocity, Regional Blood Flow
Background
Doppler ultrasound is a noninvasive and cost-effective method for evaluating peripheral vascular pathologies. When a transmitted sound wave is reflected by moving and scattering, the Doppler effect occurs. There are 2 distinct Doppler effects to consider: the first is sound transmission, in which the source is stationary and the observer is moving; the second is the effect of a moving source with a stationary observer. Doppler ultrasound is a technique that is frequently used in clinical practice today to evaluate arterial and venous structures. Along with evaluating intravascular pathologies, such as arterial stenosis and venous thrombosis, it is an effective and readily available method for evaluating calcifications of the arterial wall, atherosclerotic plaques, and peripheral vascular injuries. It is a radiological technique that allows for the rapid measurement of parameters such as blood flow velocity, blood flow rate, and flow direction. Doppler ultrasonography allows effective differentiation of normal and pathological boundaries by performing spectral analyses and waveform detection on the peripheral arterial system.
Numerous physiological factors, such as blood pressure and body temperature, also influence doppler wave parameters, as is well known [1]. As a result of these noticeable physiological effects, the possibility of using the technique to assess the autonomic nervous system’s functions has increased in recent years. For example, some authors used transcranial Doppler ultrasound to record alterations in cerebral blood flow caused by changes in body position and discovered that this technique is useful for evaluating autonomic functions [2]. In one study, investigators utilized the Doppler technique to assess vasomotor activity impairment in patients with carpal tunnel syndrome. The method used in the study was based on the measurement of changes in the radialis indicis artery’s pulsatile index caused by sympathetic activity induced by coughing following deep inspiration. The pulsatile index value in the radialis indicis artery was found to be significantly lower in patients with carpal tunnel syndrome, indicating injury to sympathetic fibers in the median nerve [3].
A careful review of the literature reveals, however, that when Doppler ultrasound examination is used to evaluate autonomic functions, various manipulative processes on the human body are frequently used. These processes include a variety of provocations, such as changes in body position, cold applications, or intrathoracic or intrabdominal pressure changes, all of which are designed to elicit an autonomous response. Furthermore, because such provocations elicit a systemic response, the adrenal gland’s function cannot be excluded, and the peripheral sympathetic nervous system’s activity cannot be measured in isolation. On the other hand, the method we described below focuses exclusively on the activity of the peripheral sympathetic nervous system without resorting to such provocative actions.
The sympathetic nervous system is principally responsible for regulating the arteries and its effect is that vasospasm occurs in the medium and large arteries, resulting in decreased blood flow [4]. By contrast, the vasodilator response is mediated by nitrergic local autoregulation mechanisms, not by the parasympathetic nervous system [5]. In light of this knowledge, measuring sympathetic nervous system activity from a large-diameter artery in the upper extremity is physiologically and clinically appropriate. On the other hand, it is critical to know which peripheral nerve supplies sympathetic innervation to the arteries of the upper extremities. The sympathetic fibers in the median nerve are denser than those in the ulnar nerve, particularly at the elbow level, according to dark-field fluorescence microscopy findings [6].
A study indicated that there is no significant difference between the median and ulnar nerves in terms of the strength of their sympathetic fibers [7]. Thus, electrical stimulation of the median nerve to measure changes in brachial artery flow parameters is consistent with current physiological and anatomical knowledge. Our primary objective was to develop a noninvasive and reproducible autonomous test model that utilized Doppler ultrasound examination, which is quick, does not require provocative actions on the human body, and detects peripheral sympathetic nervous system activities that function independently of adrenal gland activity.
Material and Methods
PARTICIPANTS:
Consent was obtained from each participant and/or their legal guardian(s). The study adhered to the most recent edition of the Declaration of Helsinki, and the Ankara City Hospital No. 2 Clinical Research Ethics Committee authorized the procedures. The Ethics Committee at the Ankara City Hospital is the Turkish Ministry of Health’s most authorized ethics body. We thought it important to acquire ethics approval from the Ankara City Hospital due to the nature and significance of our research (approval no. E3-22-1307).
The study included individuals who were physically active and in good health. Individuals with known polyneuropathy or chronic diseases that could result in autonomic neuropathy, such as amyloidosis and diabetes mellitus, were excluded from the study, as were those with essential hypertension, heart disease, and peripheral arterial disease. Individuals who had sustained a traumatic injury to the median nerve or who had moderate to severe carpal tunnel syndrome were also excluded from the study.
EXPERIMENTAL DESIGN:
Techniques similar to “sensory nerve conduction research” were modeled. These noninvasive procedures are routinely used in regular clinical electrophysiological examinations to detect peripheral neuropathies. Nicotine, caffeine, alcohol, and physical activity were restricted for 4 h following the trial. At the beginning of the experiment, the participants rested for 10 min in a seated position with their forearms supinated, after which their blood pressure, heart rate, and body temperature were assessed. Those with abnormal results were removed from the study. One male participant had hypertension (>135/85 mmHg). The investigation was conducted at temperatures between 22 and 24°C. After a 10-min break, participants were instructed to remain as still as possible and were briefed verbally at each stage of the test (for example, before the Doppler measurement was performed and before the electrical stimulation began). Using a 9-Hz linear probe of a General Electric LOQIC P9 ultrasound Doppler machine, the baseline diameter and flow rates of the right brachial artery were determined from 2 cm above the antecubital fossa (Figure 1). These measurements were taken by a radiologist with 6 years of experience using Doppler. Throughout the experiment, the Doppler sensor stayed fixed, allowing for continuous measurements. Then, for 5 s, an electrical stimulus of 10 mA strength and 1 Hz frequency was delivered to the median nerve at the level of the wrist through the bipolar stimulus electrode of the Nihon Kohden MEB-9400A EMG/EP system, in the direction of the sensory fibers (orthodromic manner; Figure 2). Immediately following the fifth stimulus, the artery diameter and flow rates were recorded once more.
STATISTICAL ANALYSIS:
Statistical analysis was conducted using version 25 of the Statistical Package for the Social Sciences (SPSS).The variables were investigated using visual (histograms and probability plots) and analytical methods (Kolmogorov-Smirnov and Shapiro-Wilk tests) to determine whether they were normally distributed. Descriptive analyses were presented using means and standard deviations for normally distributed variables and medians and 25th and 75th percentiles for the non-normally distributed variables.
The diameter and flow rate changes prior to and following median nerve stimulation were expressed as percentage changes relative to the initial values. Descriptive analyses were presented using medians (25th–75th percentiles) for the non-normally distributed variables. The Wilcoxon test was used to compare the measurements at 2 time points (before and after stimulation of the median nerve). A result was considered statistically significant if its
In addition to sociodemographic data, such as age and sex, the diameters and flow rates of the brachial arteries were recorded as final values before and after electrical stimulation in a healthy volunteer group.
Results
The age and sex distribution was as follows: 51.6% (n=16) of the 31 participants in the study were women. The participants were between 19 and 61 years of age, with a median age of 27 years. The median age of women was 27.5 years (23.5–34.5), while the median age of men was 27 years (24–39). Similar age distributions existed between men and women (
Vasomotor alterations are shown in Table 1, which shows changes in the flow rate and diameter of the brachial artery following stimulation of the median nerve. Prior to stimulation, the baseline median flow rate of the median nerve was 71.8 ml/min (60.80–110.10), whereas the median flow rate after stimulation was 35.7 ml/min (30.00–53.70). Following the electrical stimulation, a statistically significant decrease in flow rate was observed (
In the whole group, the median brachial artery diameter was 3.40 mm (3.00–3.80) before the nerve was stimulated, while the measured diameter after stimulation was 2.90 mm (2.10–3.40) on average. After stimulation, a statistically significant reduction in the diameter of the brachial artery was seen (
Table 2 displays the differences by sex in brachial artery flow rate and diameter after stimulation of the median nerve. The absolute decrease in flow rate following stimulation of the median nerve was 28.90 mL/min (21.80–38.10) in women and 41 mL/min (37.50–69.80) in men. Men had a significantly greater decrease in flow rate following stimulation (
Table 3 shows the percentages of change in the brachial artery’s flow rate and diameter following stimulation of the median nerve by sex. When the decreases in flow rate following median nerve stimulation were expressed as a percentage change from the initial value, it was discovered that the decrease in flow rate of 49.70% (39.03–57.74%) in women was not significantly different from the decrease in flow rate of 50.13% (38.33–55.97%) in men (
Discussion
Our findings corroborate the view that the Doppler ultrasound technique is an effective tool for assessing autonomic nervous system functions. In our investigation, both the diameter and flow rate of the brachial artery decreased significantly following electrical stimulation of the median nerve; in other words, when the peripheral sympathetic fibers were activated. Figures 3 and 4 depict the Doppler results of 4 randomly selected participants before and after the stimulation.
Furthermore, the Doppler-guided autonomic test, which we developed and first announced, has the potential to be useful in clinical practice by avoiding provocative methods of measuring sympathetic nervous system functions. There is no such advantage in other autonomic tests that also utilize Doppler ultrasound. For instance, a study demonstrated that the arterial blood flow was significantly lower in the cold-applied group than in the control group during the cold pressor test. In this case, sympathetic activation was induced by immersing both lower extremities of healthy volunteers in iced water [8]. Similarly, several investigators found via Doppler ultrasound that applying ice to the forehead significantly decreases forearm arterial flow [9]. On the other hand, a study noted that the diameter of the brachial artery is narrower during mental stress than in the stress-free state. Sympathetic activation is induced in this experiment by performing arithmetic tasks on 3-digit numbers [10]. Furthermore, in some studies that take advantage of Doppler ultrasound, sympathetic activation has been induced by coughing following deep inspiration, that is, artificial intrathoracic pressure manipulation [11–13].
The sympathetic skin response and quantitative sudomotor axonal reflex testing, on the other hand, are tests that measure sympathetic sudomotor function without using provocative methods but rather by using the electrical stimulation of the peripheral nerves. The tests have found broader use in clinical practice. However, Doppler ultrasound is redundant for these tests, and there are also concerns about their reproducibility [14–16].
A study using Doppler ultrasound to assess peripheral vasomotor activity in patients with carpal tunnel syndrome concluded that an impaired sympathetic response resulted in insufficient vasoconstriction and lower pulsatile index values in the radialis indicis artery [3]. This result is consistent with our findings and suggests that vasomotor activity can be measured by the Doppler ultrasound technique. By contrast, the method we described is the first autonomous test to combine peripheral electrical stimulation with the Doppler ultrasound technique; thus, it has the potential to be used in clinical practice as a low-cost, quick, and useful method without putting the body or mind under artificial stress.
The Doppler ultrasound technique has been on the agenda for the last decade as a radiological tool capable of measuring the autonomic nervous system’s functions. However, because the tests developed to date are difficult and time-consuming to administer, they have been used exclusively in scientific research and have not found a place in clinical practice. As a result, the utilization of traditional methods that do not rely on Doppler ultrasound to detect autonomic and small fiber neuropathies continued. The test we developed, on the other hand, paves the way for the routine use of Doppler ultrasound in detecting autonomic neuropathy conditions that are common in neurology and endocrinology clinics.
The limitation of this study is that, while the physiological response to peripheral sympathetic activation was demonstrated in healthy volunteers, the boundaries between normal and pathological values could not be deciphered since the study was not extended to disease groups. Even when low levels of electrical stimulation were administered to healthy volunteers, their worry and fear were taken into account, and they were instructed to relax. Those who could not get over their worries and fears were excluded from the study. Further studies are necessary to determine pathological values in autonomous neuropathy groups.
Conclusions
Doppler ultrasound scanning is a radiological technique that is frequently used to assess arterial and venous pathologies. Our research suggests that this radiological technique can be routinely used to detect not only vascular but also neurological and endocrine autonomous pathologies. It can be routinely used to detect the normal and abnormal functioning of the peripheral sympathetic nervous system.
Finally, our findings show that a new Doppler-based method can successfully detect sympathetic autonomic dysfunction in patients. This method is thought to be more user-friendly and comfortable than other methods described in the literature.
Figures
 Figure 1. Positioning of Doppler ultrasound probe.
Figure 1. Positioning of Doppler ultrasound probe.  Figure 2. Positioning of bipolar stimulus electrode.
Figure 2. Positioning of bipolar stimulus electrode. 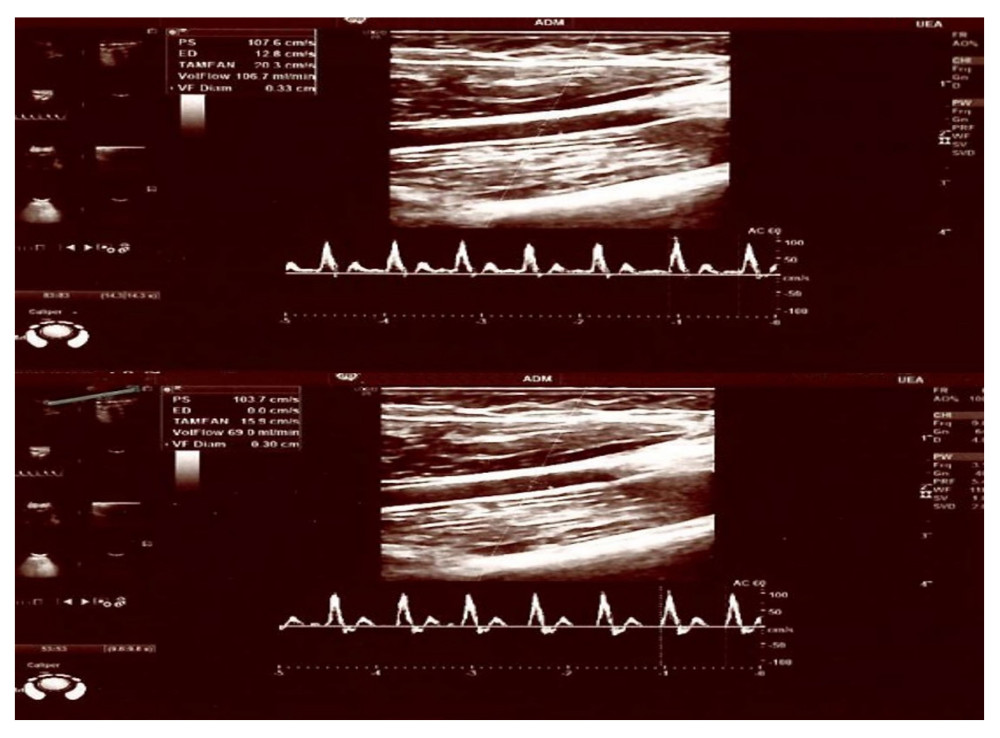 Figure 3. A 27-year-old male healthy volunteer with a pre-stimulation flow/diameter of 106.3 mL/min, 0.33 cm and post-stimulus flow/diameter of 69 mL/min, 0.30 cm.
Figure 3. A 27-year-old male healthy volunteer with a pre-stimulation flow/diameter of 106.3 mL/min, 0.33 cm and post-stimulus flow/diameter of 69 mL/min, 0.30 cm. 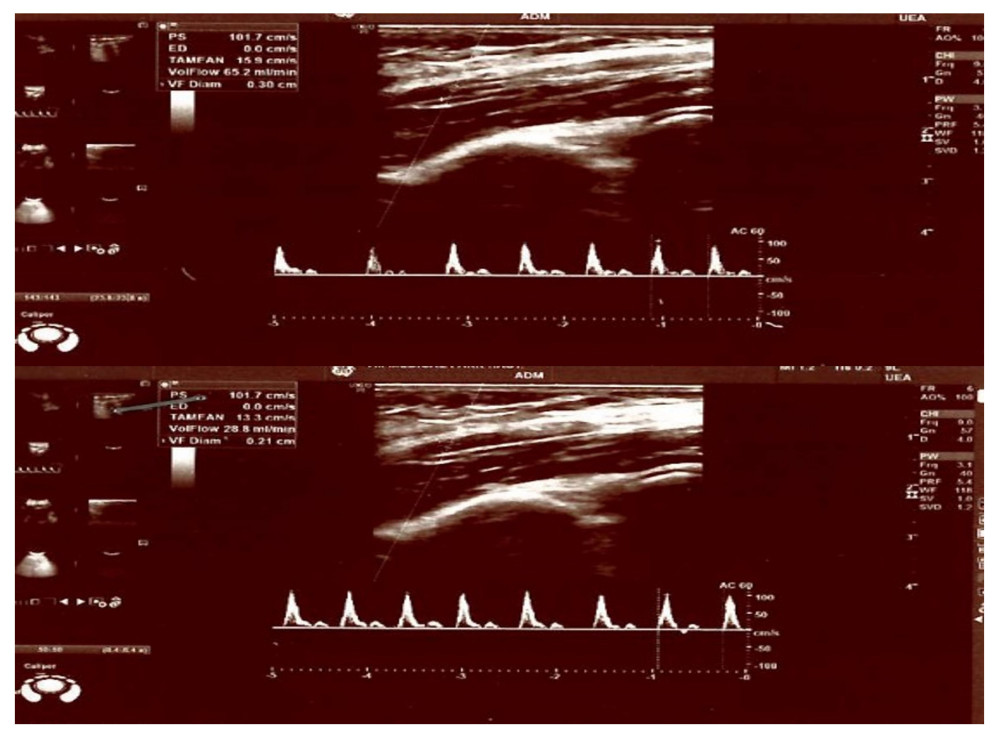 Figure 4. A 22-year-old female healthy volunteer with a pre-stimulation flow/diameter of 81.9 mL/min, 0.35 cm and post-stimulus flow/diameter of 55 mL/min, 0.30 cm.
Figure 4. A 22-year-old female healthy volunteer with a pre-stimulation flow/diameter of 81.9 mL/min, 0.35 cm and post-stimulus flow/diameter of 55 mL/min, 0.30 cm. Tables
Table 1. Changes in the brachial artery’s flow rate and diameter following median nerve stimulation.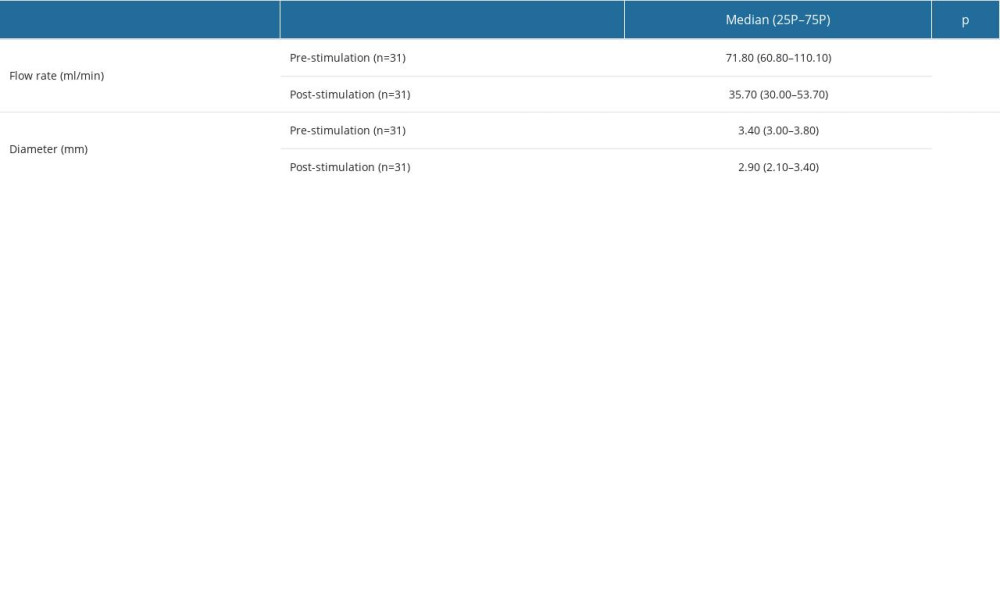 Table 2. Changes in the brachial artery’s flow rate and diameter following median nerve stimulation, by sex.
Table 2. Changes in the brachial artery’s flow rate and diameter following median nerve stimulation, by sex.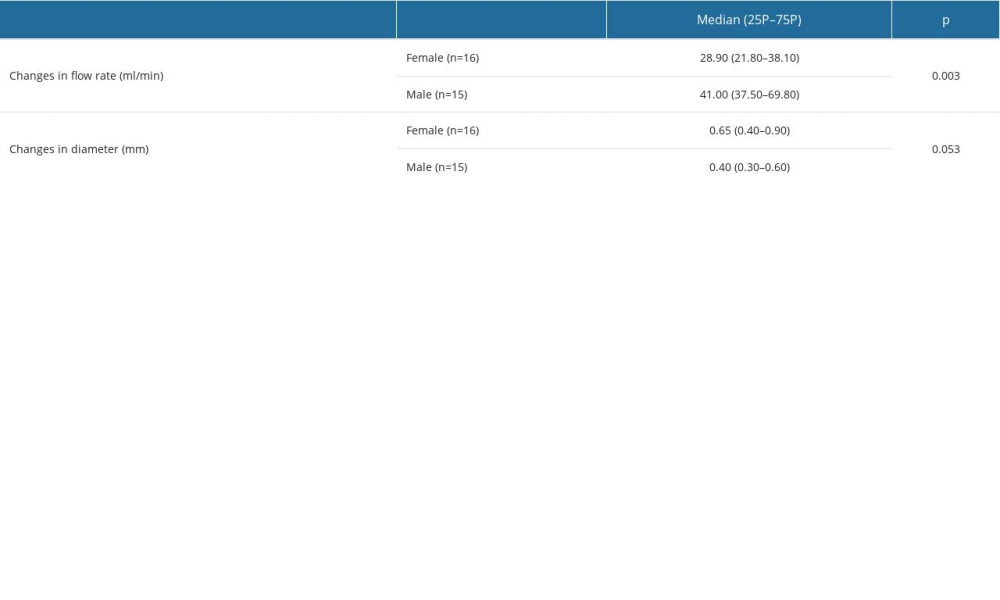 Table 3. The percentages of change in the brachial artery’s flow rate and diameter following median nerve stimulation, by sex.
Table 3. The percentages of change in the brachial artery’s flow rate and diameter following median nerve stimulation, by sex.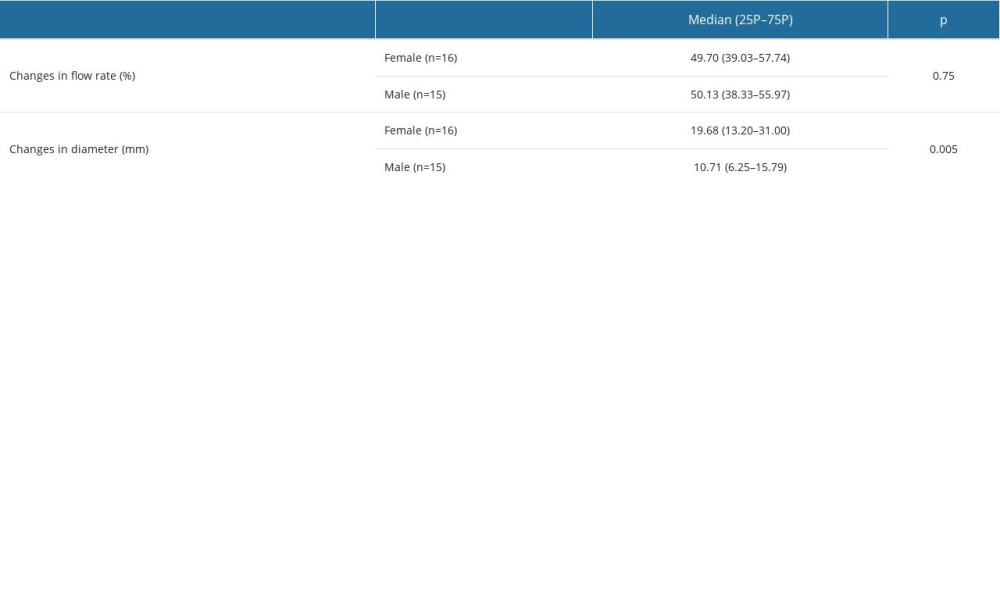
References
1. Kim ES, Sharma AM, Scissons R, Interpretation of peripheral arterial and venous Doppler waveforms: A consensus statement from the Society for Vascular Medicine and Society for Vascular Ultrasound: Vasc Med, 2020; 25(5); 484-506
2. Norcliffe-Kaufmann L, Galindo-Mendez B, Garcia-Guarniz AL, Transcranial Doppler in autonomic testing: Standards and clinical applications: Clin Auton Res, 2018; 28(2); 187-202
3. Ghasemi-Esfe AR, Morteza A, Khalilzadeh O, Color Doppler ultrasound for evaluation of vasomotor activity in patients with carpal tunnel syndrome: Skeletal Radiol, 2012; 41(3); 281-86
4. LeBouef T, Yaker Z, Whited L, Physiology, autonomic nervous system: StatPearls [Internet], 2022, Treasure Island (FL), StatPearls Publishing
5. Karemaker JM, An introduction into autonomic nervous function: Physiol Meas, 2017; 38(5); R89-R118
6. Morgan RF, Reisman NR, Wilgis EF, Anatomic localization of sympathetic nerves in the hand: J Hand Surg Am, 1983; 8(3); 283-88
7. Balogh B, Auterith A, Behrus R, The sympathetic axons of the nerves of the hand: Handchir Mikrochir Plast Chir, 2002; 34(6); 369-73
8. Dyson KS, Shoemaker JK, Hughson RL, Effect of acute sympathetic nervous system activation on flow-mediated dilation of brachial artery: Am J Physiol Heart Circ Physiol, 2006; 290(4); H1446-53
9. Sinoway LI, Wilson JS, Zelis R, Sympathetic tone affects human limb vascular resistance during a maximal metabolic stimulus: Am J Physiol, 1988; 255(4 Pt 2); H937-46
10. Harris CW, Edwards JL, Baruch A, Effects of mental stress on brachial artery flow-mediated vasodilation in healthy normal individuals: Am Heart J, 2000; 139(3); 405-11
11. Galea LA, Mercieca A, Sciberras C, Evaluation of sympathetic vasomotor fibres in carpal tunnel syndrome using continuous wave Doppler ultrasonography: J Hand Surg Br, 2006; 31(3); 306-10
12. Eicke BM, Milke K, Schlereth T, Comparison of continuous wave Doppler ultrasound of the radial artery and laser Doppler flowmetry of the fingertips with sympathetic stimulation: J Neurol, 2004; 251(8); 958-62
13. Chang KV, Wu CH, Yeh TS, Application of pulsed-wave Doppler ultrasound to exploration of the peripheral vasomotor response by gender and hand dominance: J Med Ultrason (2001), 2011; 38(4); 195
14. Kucera P, Goldenberg Z, Kurca E, Sympathetic skin response: Review of the method and its clinical use: Bratisl Lek Listy, 2004; 105(3); 108-16
15. Giza E, Katsarou Z, Georgiadis G, Bostantjopoulou S, Sympathetic skin response in Parkinson’s disease before and after mental stress: Neurophysiol Clin, 2012; 42(3); 125-31
16. Berger MJ, Kimpinski K, Test-retest reliability of quantitative sudomotor axon reflex testing: J Clin Neurophysiol, 2013; 30(3); 308-12
Figures
 Figure 1. Positioning of Doppler ultrasound probe.
Figure 1. Positioning of Doppler ultrasound probe. Figure 2. Positioning of bipolar stimulus electrode.
Figure 2. Positioning of bipolar stimulus electrode.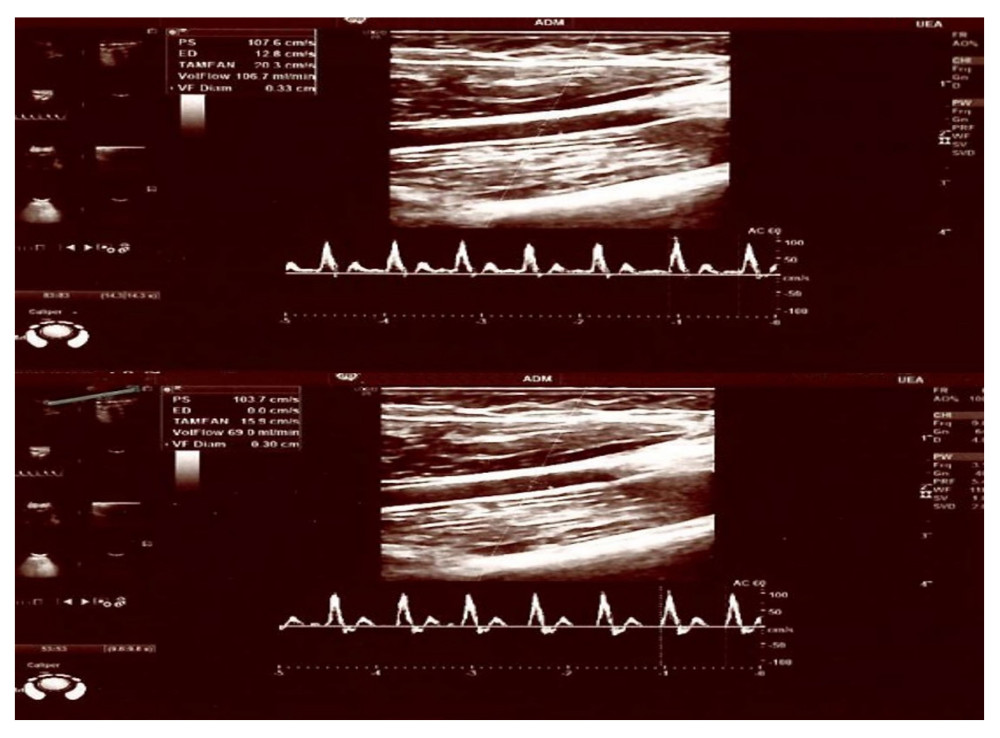 Figure 3. A 27-year-old male healthy volunteer with a pre-stimulation flow/diameter of 106.3 mL/min, 0.33 cm and post-stimulus flow/diameter of 69 mL/min, 0.30 cm.
Figure 3. A 27-year-old male healthy volunteer with a pre-stimulation flow/diameter of 106.3 mL/min, 0.33 cm and post-stimulus flow/diameter of 69 mL/min, 0.30 cm.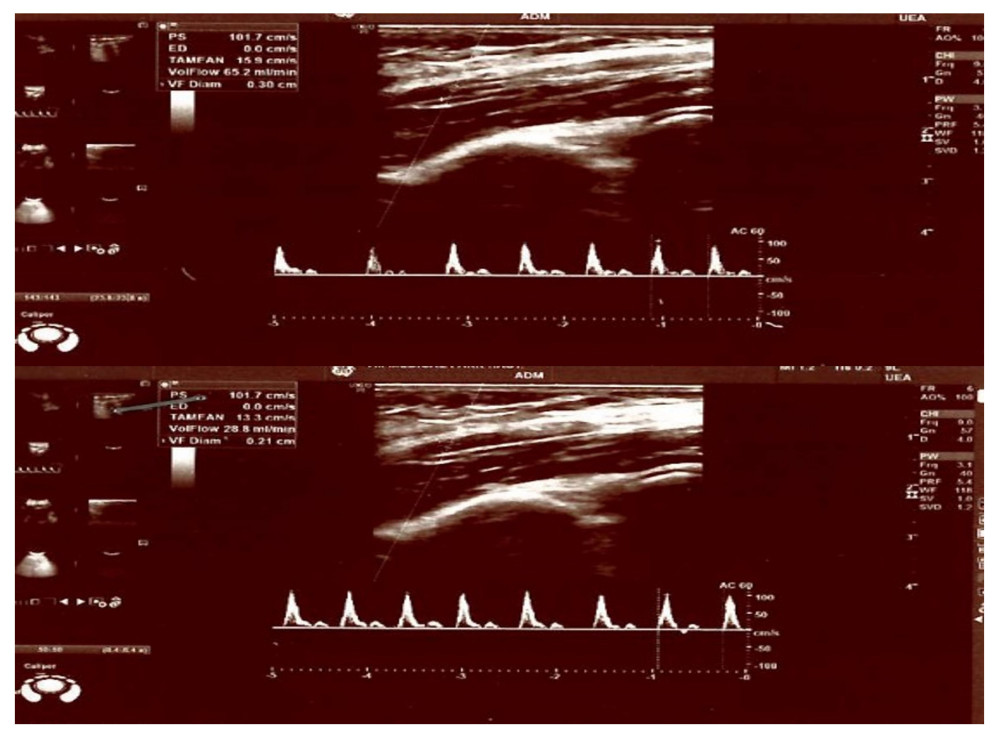 Figure 4. A 22-year-old female healthy volunteer with a pre-stimulation flow/diameter of 81.9 mL/min, 0.35 cm and post-stimulus flow/diameter of 55 mL/min, 0.30 cm.
Figure 4. A 22-year-old female healthy volunteer with a pre-stimulation flow/diameter of 81.9 mL/min, 0.35 cm and post-stimulus flow/diameter of 55 mL/min, 0.30 cm. Tables
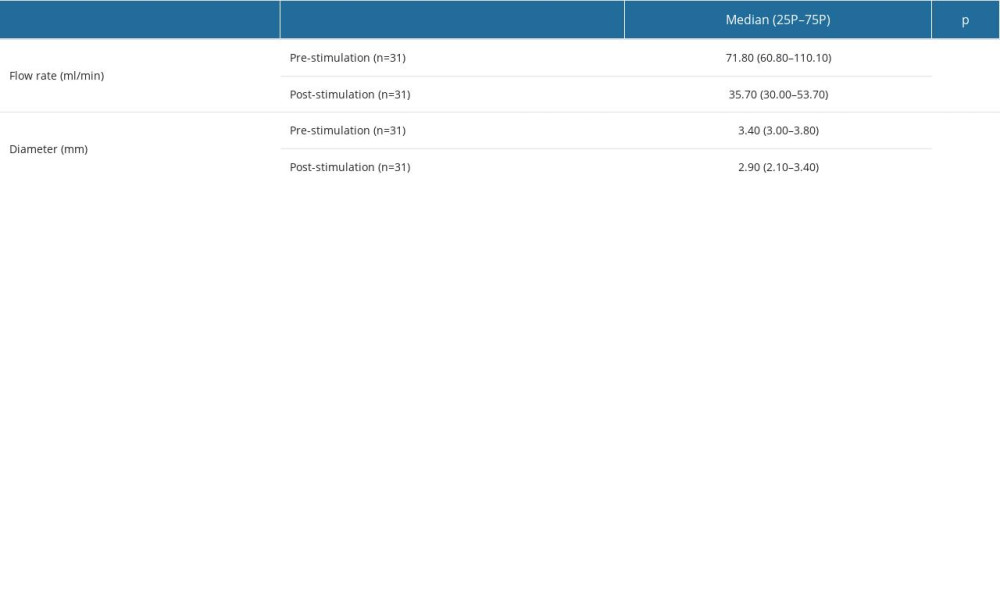 Table 1. Changes in the brachial artery’s flow rate and diameter following median nerve stimulation.
Table 1. Changes in the brachial artery’s flow rate and diameter following median nerve stimulation.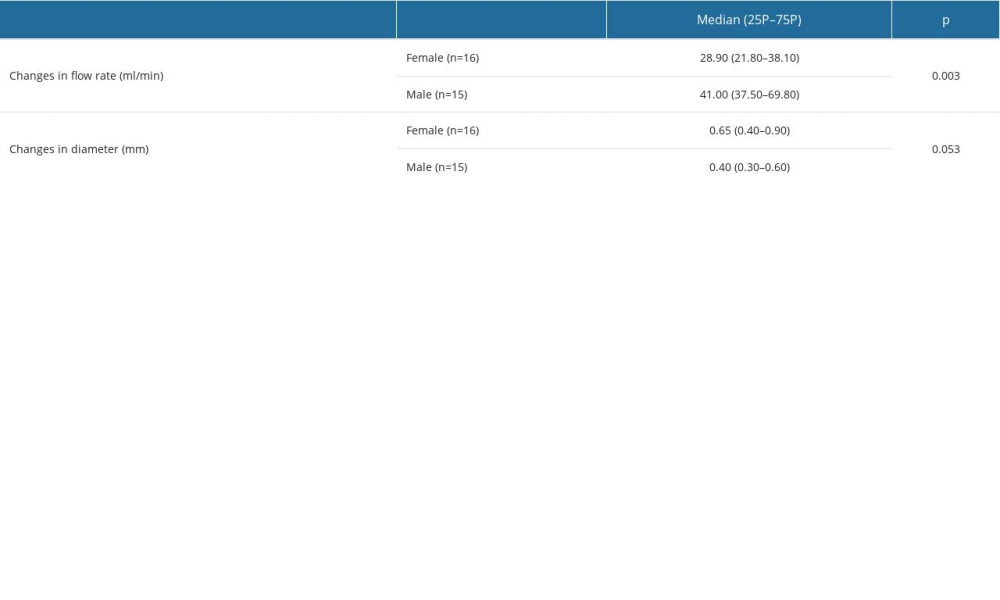 Table 2. Changes in the brachial artery’s flow rate and diameter following median nerve stimulation, by sex.
Table 2. Changes in the brachial artery’s flow rate and diameter following median nerve stimulation, by sex.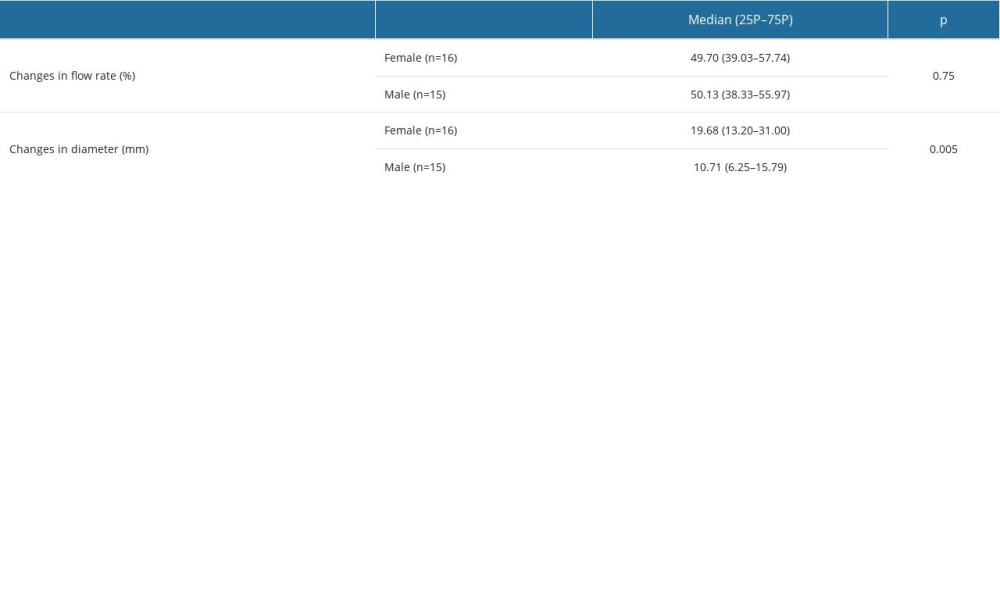 Table 3. The percentages of change in the brachial artery’s flow rate and diameter following median nerve stimulation, by sex.
Table 3. The percentages of change in the brachial artery’s flow rate and diameter following median nerve stimulation, by sex.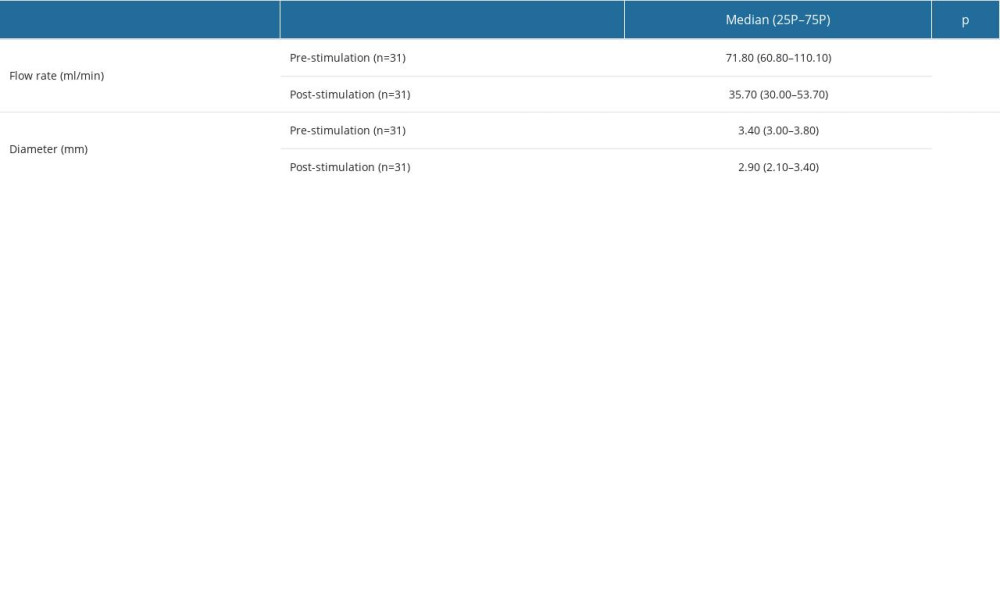 Table 1. Changes in the brachial artery’s flow rate and diameter following median nerve stimulation.
Table 1. Changes in the brachial artery’s flow rate and diameter following median nerve stimulation.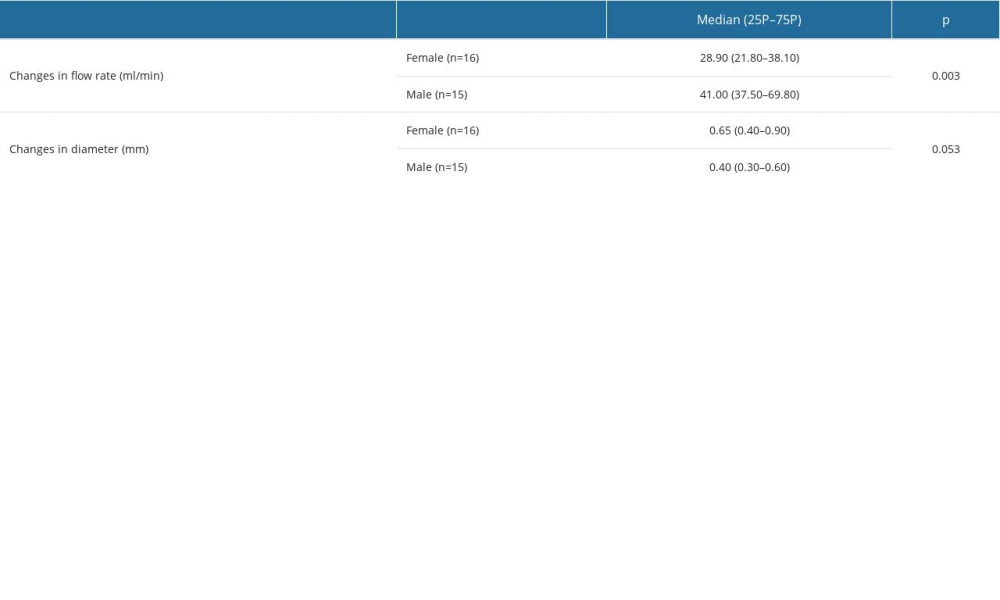 Table 2. Changes in the brachial artery’s flow rate and diameter following median nerve stimulation, by sex.
Table 2. Changes in the brachial artery’s flow rate and diameter following median nerve stimulation, by sex.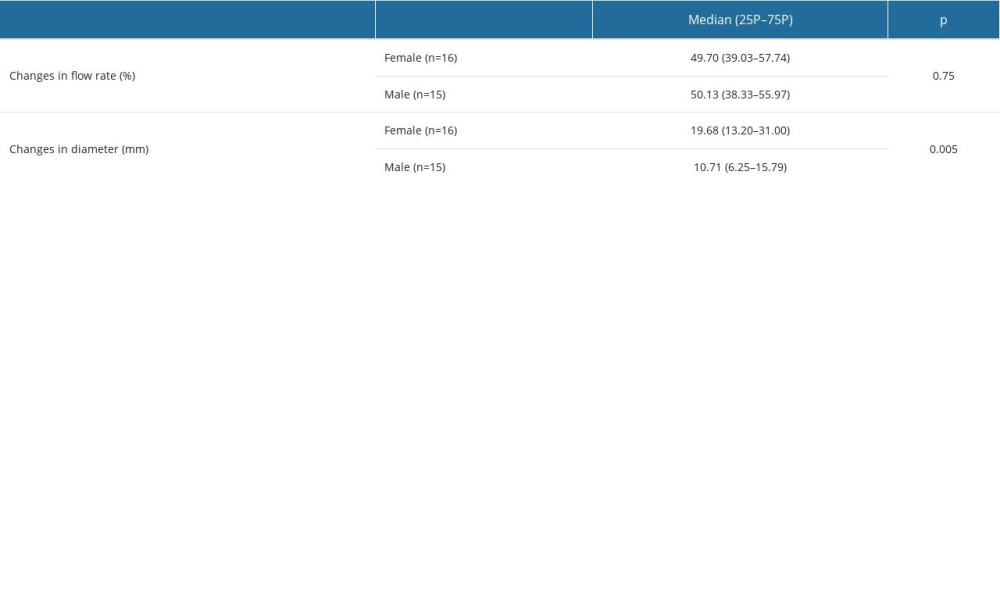 Table 3. The percentages of change in the brachial artery’s flow rate and diameter following median nerve stimulation, by sex.
Table 3. The percentages of change in the brachial artery’s flow rate and diameter following median nerve stimulation, by sex. In Press
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








