10 May 2023: Clinical Research
Surgical Outcomes in 62 Patients with Ulcerative Colitis: A Retrospective, Single-Center Study from Poland
Zofia KampkaDOI: 10.12659/MSM.939412
Med Sci Monit 2023; 29:e939412
Abstract
BACKGROUND: Surgery continues to play an important role in the treatment of ulcerative colitis (UC), which is one of the most common inflammatory diseases of the colon and rectum. This retrospective study from a single center in Poland aimed to evaluate surgical outcomes in 62 patients with ulcerative colitis.
MATERIAL AND METHODS: The study enrolled 62 patients (36 men [58.1%], 26 women [41.9%]), mean age 52.69±16.84 (range, 19-96) years who underwent surgical treatment of UC during the period 2001-2020. The mandatory inclusion criteria were patients with UC, who underwent total intra-abdominal colectomy (n=22, 46.8%), proctocolectomy (n=25, 53.2%), or left-sided hemicolectomy (n=8, 12.9%). The primary endpoint was postoperative death, and secondary endpoints were long hospitalization (>15 days), complications, and relaparotomy.
RESULTS: Postoperative mortality was observed in 8 (12.9%) patients. Older age and low albumin level were associated with longer hospitalization time (P=0.004 and P<0.001, respectively). High C-reactive protein (CRP) level (P=0.003), high CRP/albumin ratio (P=0.023), and malnourishment (P=0.026) were risk factors for complications. Malnutrition (P=0.026), older age (P=0.031), high CRP level (p<0.001), high CRP/albumin ratio (P=0.014), arterial hypertension (P=0.012), and urgent surgeries (P=0.021) were associated with higher risk of postoperative death. Patients who had undergone previous surgeries were more likely to need relaparotomy (P=0.022).
CONCLUSIONS: Preoperative nutritional status was an important factor associated with postoperative outcomes in patients with ulcerative colitis. Correction of malnutrition seems to be a vital part of preoperative preparation.
Keywords: Colectomy, Colitis, Ulcerative, Inflammatory Bowel Diseases, Proctocolectomy, Restorative, Surgical Procedures, Operative, Humans, Colitis, Ischemic, Poland, Postoperative Complications, Retrospective Studies, Treatment Outcome, Male, Female, Middle Aged
Background
Ulcerative colitis (UC) is the most common inflammatory bowel disease. Its prevalence among the Polish population is estimated as 191.4 per 100 000 [1]. Although pharmacotherapy is the therapy of first choice for UC, surgery continues to play a vital role in the treatment of this disease. Over 20% of patients with UC will require at least 1 bowel surgery throughout their life [2,3] and as much as 10% in the first year of illness. Due to the possibility of complete removal of the affected sections of the intestine (ie, the colon and rectum), surgery is the only curative option in UC. It also eliminates the risk of dysplasia and cancer development, whereas pharmacological treatment only allows control of symptoms [3]. The most common indications for surgery are the disease becoming unresponsive to maximal medical therapy or severe medical complications such as toxic megacolon or colonic perforation. A total abdominal colectomy with end-ileostomy is usually performed because of emergency and urgent indications. Regarding elective surgery, 4 options are available: restorative proctocolectomy and ileal pouch-anal anastomosis, total abdominal colectomy with end-ileostomy, total abdominal colectomy with ileorectal anastomosis, and total proctocolectomy with end-ileostomy [4].
A similar study that assessed the most common indications for surgery (ie, fistulae and strictures) and the methods (ie, right hemicolectomy) and results of surgical treatment of another principal type of inflammatory bowel disease, Crohn’s disease, in the same department as our referral Department of Digestive Tract Surgery, University Clinical Center, Medical University of Silesia in Katowice, was performed and the results can be compared with those of the present study [5]. The aim of our research was to determine the most common indications for surgical treatment of ulcerative colitis, along with methods and results of this procedure. We also analyzed the correlations between the obtained data and postoperative complications. Therefore, this retrospective study from a single center in Poland aimed to evaluate surgical outcomes in 62 patients with ulcerative colitis.
Material and Methods
ETHICS STATEMENT:
This was a retrospective study of patient medical records, and all data were fully anonymized before access. Written informed consent was obtained from all participants. All procedures were in accordance with the 1964 Declaration of Helsinki on Medical Research Involving Human Subjects and its subsequent amendments or comparable ethical standards. Our retrospective analysis of patient medical records fell into the category of exempt from Institutional Review Board (IRB) approval according to local regulations.
STUDY POPULATION:
The study was a single-centered retrospective analysis of 62 patients (36 men [58.1%], 26 women [41.9%]), mean age 52.69±16.84 (19–96) years, who underwent surgical treatment for UC in the Department of Digestive Tract Surgery in Katowice during the period 2001–2020. Data were acquired from the database of the hospital and were anonymized.
ANALYZED PARAMETERS:
The collected data included factors such as demographic data (age, gender, body mass index [BMI]) and past medical history (onset of symptoms, implemented treatment, time from diagnosis to surgery, concomitant diseases, surgeries, and substance abuse). We also investigated surgery-related parameters such as: indications for surgery, type and duration of surgery, and postoperative complications. Laboratory blood morphological and biochemical parameters at admission and after the surgery were also included.
The mandatory inclusion criteria were patients aged ≥18 years with K51.0–51.9 code of the International Classification of Diseases, Tenth Revision (ICD-10)-UC, who underwent procedures with codes 45.7 (Open and other partial excision of large intestine), 45.8 (Total intra-abdominal colectomy), 48.5 (Abdominoperineal Resection of Rectum), 48.6 (Other resection of rectum) in International Classification of Diseases, Ninth Revision. Patients with UC require elective surgeries because of pharmacological therapy ineffectiveness, steroid dependency, low compliance, and multifocal or high-grade dysplasia, while emergency surgeries are performed due to acute colitis with severe complications (ie, toxic megacolon, perforation, and severe colorectal bleeding) [2,3]. Exclusion criteria were incomplete data regarding the procedure type and outcome.
STATISTICAL ANALYSIS:
A descriptive analysis was performed. A confidence interval of 95% was used. The distribution of quantitative variables was analyzed. Variables closely following a normal distribution are expressed as means and standard deviation, while non-normally distributed variables are given as medians with interquartile range. To confirm the normality distribution of variables, the distribution of each variable was examined via a quantile-quantile plot (qqplot) and measure of skewness. Associations between different clinical parameters such as age, body mass index, time from diagnosis to treatment, type of surgery, surgery duration, type of stoma, pharmacological treatment, comorbidities and Intensive Care Unit (ICU) stay, length of hospital stay, postoperative complications, and postoperative mortality were analyzed. Additionally, analysis of laboratory test results before and after surgery was performed. The level of statistical significance was set at
Results
STUDY POPULATION CHARACTERISTICS:
The general patient clinical characteristics are presented in Table 1. For surgical characteristics, most procedures (n=37, 63.8%) were elective and 21 (36.2%) were urgent. The most common reasons for elective surgery were: persistence of symptoms despite treatment such as loss of weight, chronic diarrhea, and abdominal pain in 24 (38.7%) patients, severe anemia (n=9, 14.5%), colon stenosis (n=5, 8.1%), and neoplastic lesions in the large intestine (n=5, 8.1%), while for urgent surgery the reasons were: exacerbation of symptoms (n=13, 21%), megacolon toxicum (n=12, 19.4%), and peritonitis (n=6, 9.7%).
SURGICAL CHARACTERISTICS:
The most frequently performed procedure was proctocolectomy (n=25, 40.3%), 17 (27.4%) patients underwent laparoscopic surgery, and 45 (72.6%) underwent open surgery. The average time of surgery was 5 hours 17 minutes. Forty-seven (75.8%) patients required stoma creation. The most common type of stoma was temporary end-ileostomy (n=25, 54.3%) followed by definitive ileostomy (n=18, 39.1%) and double-loop ileostomy (n=3, 6.5%). The differences in selected clinical parameters examined before and after the surgery are presented in Table 2. The increase in red blood cell count after surgery was statistically significant (P=0.028). Decreases in neutrophil count and C-reactive protein level were also statistically significant (P=0.047 and P=0.005 respectively). Twenty-three (37.1%) patients required a longer hospital stay (>15 days).
POSTOPERATIVE COMPLICATIONS:
The complications rate was 40.3% (n=25). The most common complications were wound suppuration (n=14, 22.6%) and wound dehiscence (n=6, 9.7%). Less common complications were: intra-abdominal hemorrhage (n=4, 6.5%), sepsis (n=3, 4.8%), anastomotic leaks (n=1, 1.6%), and intestinal obstruction (n=1, 1.6%). Fourteen (22.6%) patients required reoperation and 2 (3.23%) required rehospitalization. The most common reasons for reoperation were intra-abdominal/pelvic abscess (n=6, 42.9%), wound dehiscence (n=2, 14.3%), hematoma (n=2, 14.3%), obstruction (n=1, 7.1%), and acute pancreatitis with abscess (n=1, 7.1%). Postoperative mortality was observed in 8 (12.9%) patients; the direct cause of death was sudden cardiac arrest and the underlying causes of death were sepsis (n=3, 37.5%), initial serious condition requiring urgent surgery (n=2, 25%), wound dehiscence (n=1, 12.5%), and massive intra-abdominal hemorrhage (n=1, 12.5%).
ASSOCIATIVE ANALYSIS:
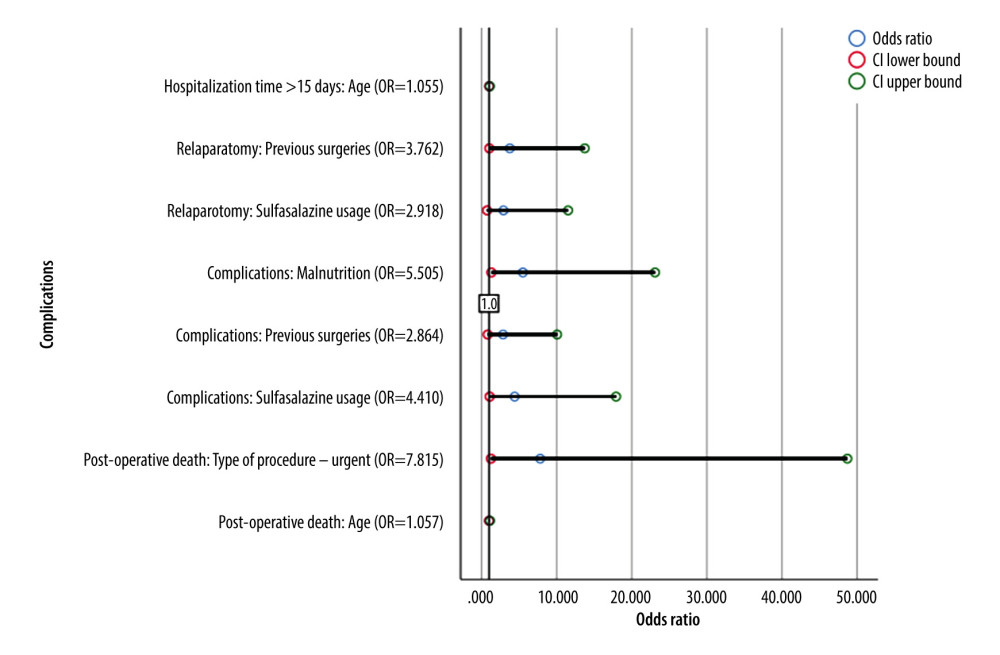
Correlation analyses of preoperative versus perioperative variables are presented in Tables 3–5. Older age was associated with longer hospitalization time (P=0.004, Eta=0.402) and higher risk of postoperative death (P=0.031, Eta=0.275). Patients with low albumin level were more often admitted to the ICU (P=0.004, Eta=0.485) and their hospitalization time was longer (P<0.001, Eta=0.605). High C-reactive protein (CRP) was associated with higher risk of complications (P=0.003, Eta=0.446) and postoperative death (P<0.001, Eta=0.535). The higher the CRP/albumin ratio after surgery, the higher the probability of ICU stay (P=0.005, Eta=0.576), risk of complications (P=0.023, Eta=0.482), and postoperative death (P=0.014, Eta=0.514). Time from diagnosis to surgery did not affect the hospitalization time or the occurrence of complications. Patients taking 5-aminosalicylic acid derivatives (5-ASA) and steroids had longer surgery times (P=0.017, Eta=0.588 and P=0.030, Eta=0.543, respectively). Arterial hypertension was associated with longer hospitalization time (P=0.082, Phi=0.277) and postoperative death (P=0.012, Phi=0.388). Malnourished patients were more likely to have complications (P=0.026, Phi=0.304) and those needing parenteral nutrition were at higher risk of postoperative death (P=0.013, Phi=0.416). Urgent surgeries were associated with higher risk of postoperative death (P=0.021, Phi=0.323) but did not influence the frequency of complications (P>0.05). Patients who had undergone surgeries before were more likely to need a relaparotomy (P=0.022 (Phi=0.310). Binary regression analysis for postoperative complications is presented in Table 6. A forest plot describing the relationship between selected clinical parameters and postoperative complications is presented in Figure 1.
Discussion
Ulcerative colitis is an inflammatory bowel disease. Despite pharmacological treatment, more than 20% of such patients require surgical treatment, mainly due to the ineffectiveness of conservative treatment, exacerbation of symptoms, or neoplastic lesions [2,3]. Postoperative complications are very common, especially infectious complications, obstruction, and rehospitalization [6]. These data are consistent with those obtained in our study. The aim of our research was to evaluate surgical outcomes in patients with UC to determine the most common indications for surgery and factors influencing the frequency of complications. Understanding and modifying these could help improve the outcomes of UC patients undergoing surgery.
We analyzed 62 patients, 41.9% of whom were women and 58.1% were men. In a retrospective analysis of the Polish population in 2012–2020, the incidence of UC in men (52.5%) was also higher than in women (47.5%), but the differences were smaller [1]. Global data show no significant differences in the prevalence of UC by sex (the ratio of women to men ranged from 0.51 to 1.58), which may be due to differences between the geographical regions and the age at diagnosis of the disease [7]. There was an advantage of diagnoses in women over men up to middle age (40–44 years of age), except for the age group of 5–9 years, as well as in Western Europe and North America, while the majority of men are diagnosed after age 45, and at the age of 5–9 and in Central Europe [8,9]. The median age of the patients at the time of surgery in our study was 54 years and was higher than the age reported in the literature [10,11]. The differences may be due to the limited number of observations in our analysis.
Postoperative mortality was observed in 12.9% of our patients, which is a much higher than the data presented by other researchers [10,12–14]. In a study conducted by Majewska et al in our center in patients with Crohn’s disease, no deaths within 30 days after surgery were found [14]. A large meta-analysis published by Singh et al assessed mortality according to the mode of surgery; in elective surgery, the average mortality was 0.7%, while in the case of emergency surgery it was 5.3% [16]. Other analyses also reported higher mortality in the case of emergency surgery (from 2.4% to 13.1%) than in elective surgery (from 0.6% to 2.2%) [17–23]. In our study, the postoperative mortality rate in patients who underwent elective surgery was 25%, while it was 75% patients who underwent emergency surgery. The high postoperative mortality rate in our analysis may be due to the older age of the studied patients and the large number of non-elective surgeries (36.2%).
Admission mode (elective in 63.8% of our patients), the most frequently performed procedure (proctocolectomy in 53.2% patients), and the most common reasons for elective admission in our study were consistent with results reported in the literature [4,24].
Due to common diseases and comorbidities, patients with UC have an increased risk of postoperative complications. In our study, complications occurred in 40.2%. On the report to current evidence-based management consensus ECCO (European Crohn’s and Colitis Organisation) on surgery for UC, emergency laparoscopic surgery as associated with lower risk of infectious complications and a shorter hospital stay, while preoperative steroid use, poor nutritional status, smoking, younger age at colectomy, use of NSAIDs (non-steroidal anti-inflammatory drugs), backwash ileitis, extensive colitis, comorbidities, and extraintestinal manifestations of UC increased the risk of postoperative complications [25].
In our analysis, 28% of patients underwent laparoscopic surgery and 72% underwent open surgery. Sylla et al [26] did not observe significant differences in postoperative complications depending on the type of surgery, which is comparable to the results obtained in our study.
We did not observe any correlation between the type of admission and an increased rate of complications, which is similar to the results reported by other researchers [11].
According to the literature, age, emergency surgery, previous surgery, comorbidities, anemia, and fever are related to increased incidence of postoperative complications in patients following surgery for UC [12,13,27–31]. In our study, no such relationships were found with regard to anemia, previous surgery, and fever, while type of the surgery and older age significantly increased the risk of complications. We found that arterial hypertension was associated with a higher risk of death after surgery and fever was associated with a longer hospitalization time. Majewska et al reported a correlation between smoking and postoperative complications [15], but we did not observe such an association in our patients with UC. In our study, there was no statistically significant association between occurrence of other comorbidities, such as diabetes or cardiovascular diseases, and postoperative complications. Among patients who had undergone surgery in the past, there was an increased risk of reoperation after surgery for UC. The differences between our results and those in the literature may be due to the small size of our sample.
Nutritional status, such as undernutrition, sarcopenia, obesity, and myosteatosis, are important factors that can affect the risk of complications after surgery. Fiorindi et al observed that nutritional prehabilitation reduces the postoperative catabolic effect and found a significant correlation between early oral resumption of feeding and faster recovery of bowel function after surgery and shorter hospital stay. No correlation was observed between early postoperative nutrition and the occurrence of complications, although in the literature such a correlation was described after colorectal cancer surgery [32]. Our study found that undernutrition was related to increased risk of complications, and preoperative parenteral nutrition due to severe malnutrition was associated with higher risk of death after surgery.
The most common postoperative complications described in the literature are wound infections, intestinal obstruction, pelvic abscess, thromboembolic complications, and rehospitalization [11,12,33]. Our study also found a high incidence of wound suppuration and readmissions. Our patients also frequently experienced wound dehiscence, intra-abdominal hemorrhage, and sepsis. The differences may be due to the retrospective nature of our analysis and different definitions in medical records.
Some studies show that laboratory parameters, such as hypoalbuminemia, low concentration of hemoglobin, and high concentration of CRP, may be associated with poor outcomes after surgery [11,31]. Rocha et al indicate that low albumin levels and high CRP may be a useful indicator for the diagnosis of sarcopenia in patients with IBD, which is an independent risk factor for postoperative complications [29], but other researchers have found no such correlation [15]. In our analysis, we observed this association in relation to hypoalbuminemia and high CRP concentration. There are also reports that the CRP/albumin ratio may be an independent risk factor for complications after colorectal surgery, and that it is a more precise marker than the level of CRP [34]. In our study, we obtained similar results. Poor postoperative outcomes that are observed in patients may be due to the serious condition on admission, which is associated with low levels of albumin caused by malnutrition and inflammation, as a negative acute-phase protein, as well as high concentration of CRP.
In our study, we compared the biochemical parameters before and after surgery. We observed a statistically significant decline in neutrophil count and CRP level, which may be due to the reduction of inflammation by removal of the inflamed part of the intestine. According to the literature, a high CRP level correlates with clinical and endoscopic disease activity, but its low level may give false-negative results [35–37]. Some researchers showed that CRP level is a good predilection marker of the risk of postoperative abdominal complications, but not a good prognostic factor of recurrence [38–41]. Our analysis also showed a statistically significant postoperative increase in red blood cell count, which may be due to intestinal resection causing a removal of the source of bleeding, as well as being due to transfusions during surgeries.
In some studies, administration of steroids was correlated with the risk of infectious complications, pneumonia, and the need for reoperation [42,43], whereas Khazrei et al did not show a statistically significant effect of using a high dose of prednisolone before proctocolectomy (>20 mg/day) on the risk of postoperative complications [44]. Nguyen et al found that steroids did not significantly increase mortality 30 days after surgery, but did increase the percentage of reoperations and prolonged surgery time [45]. Our analysis showed that the use of steroids and 5-ASA prolonged the operation duration, but did not affect the risk of postoperative complications and reoperation. The literature reports that overall use of immunosuppressants is not correlated with postoperative complications [13,33], which is consistent with our results. According to the latest ECCO guidelines, prolonged immunosuppressive therapy is associated with an increased incidence of postoperative complications [25].
There are also discussions about the preoperative use of biological treatment and the risk of postoperative complications. Some researchers described the lack of a relationship between increased serum anti-TNF alpha levels and adverse effects after surgery or rehospitalization [27,42,46], which correspond with the results obtained during our analysis and with the observations from a similar study in our clinic [15]. Kunitake et al and Bregnbak et al observed only longer hospitalization time in patients treated with infliximab [46,47], while Schluender et al described significantly more frequent occurrence of postoperative complications during the concomitant use of infliximab and cyclosporin A, with no such effect during treatment only with a biological drug [48]. In the case of preoperative use of vedolizumab, no significant differences in the incidence of complications were found [28,49], apart from postoperative leakage of the intestines described by Jeong Yeon Kim et al [50]. Other analyzes, however, showed a correlation between the use of biological drugs and increased risk of postoperative complications [43,51].
Our study has several limitations. First, it was single-center, so the number of patients included in the analysis is limited. Secondly, data were collected retrospectively, so there may be bias due to differences in definitions in medical data and misclassification. Despite several limitations, our study is important because it reveals factors that may contribute to the poor postoperative outcomes of patients with UC, and our results may help provide better control of risk factors in surgical interventions for UC in the future.
Conclusions
Despite the fact that surgery is not the first-line treatment of UC, the complications caused by the illness make it inevitable in many cases. Malnutrition and advanced age were associated with higher risk of postoperative complications. Urgent admission, parenteral nutrition administered due to severe malnutrition, and arterial hypertension were associated with a higher risk of death after surgery. There was a correlation between higher level of CRP and higher CRP/albumin ratio after surgery and the incidence of postoperative complications. The findings from our study show that preoperative nutritional status is an important factor associated with postoperative outcomes in patients with ulcerative colitis. The correction of malnutrition seems to be a vital part of preoperative preparation in patients with UC.
Tables
Table 1. Baseline characteristics.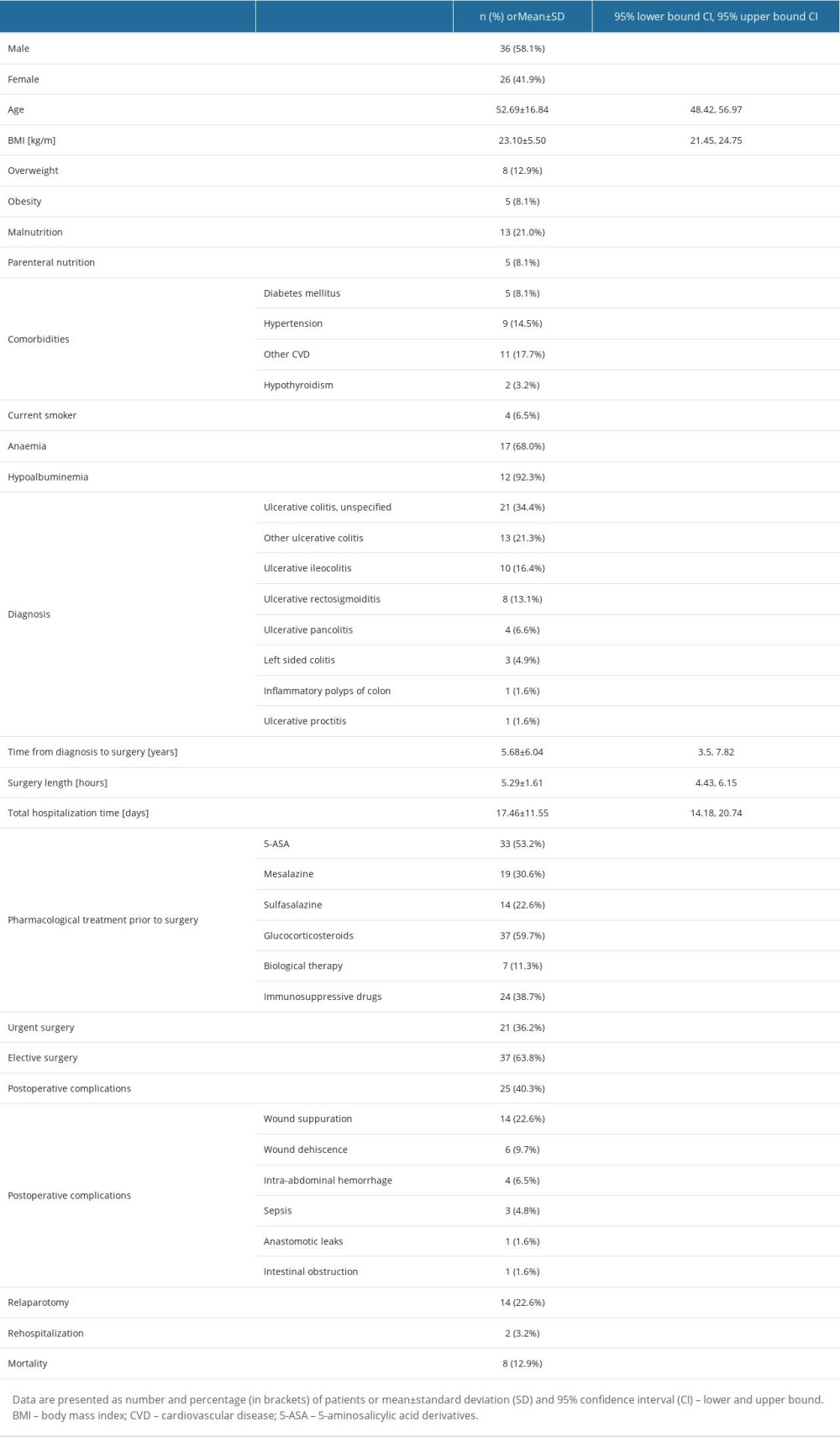 Table 2. Difference in selected laboratory parameters examined before and after surgery.
Table 2. Difference in selected laboratory parameters examined before and after surgery. Table 3. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, quantitative analysis).
Table 3. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, quantitative analysis).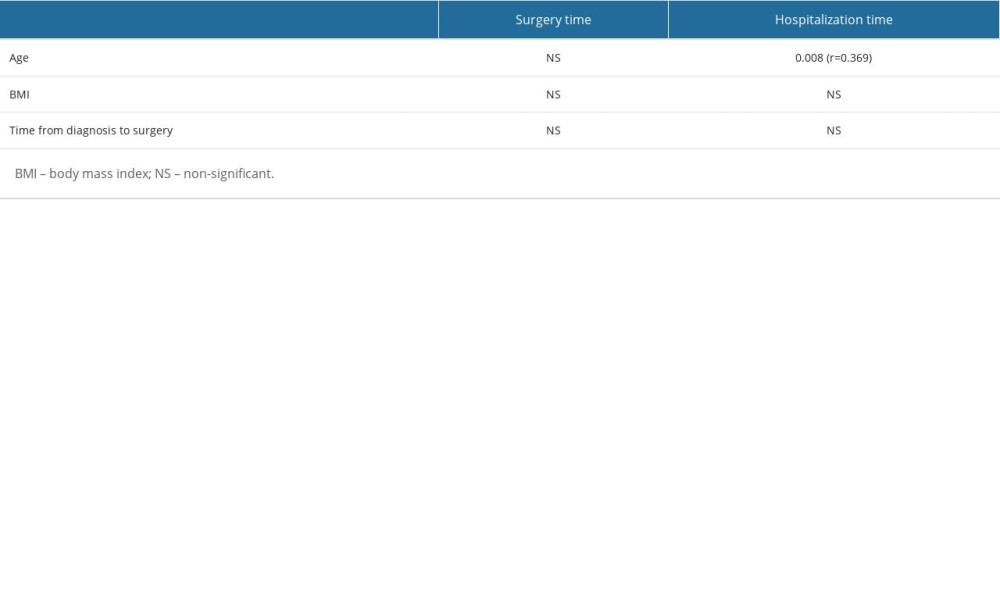 Table 4. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, qualitative-quantitative analysis).
Table 4. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, qualitative-quantitative analysis).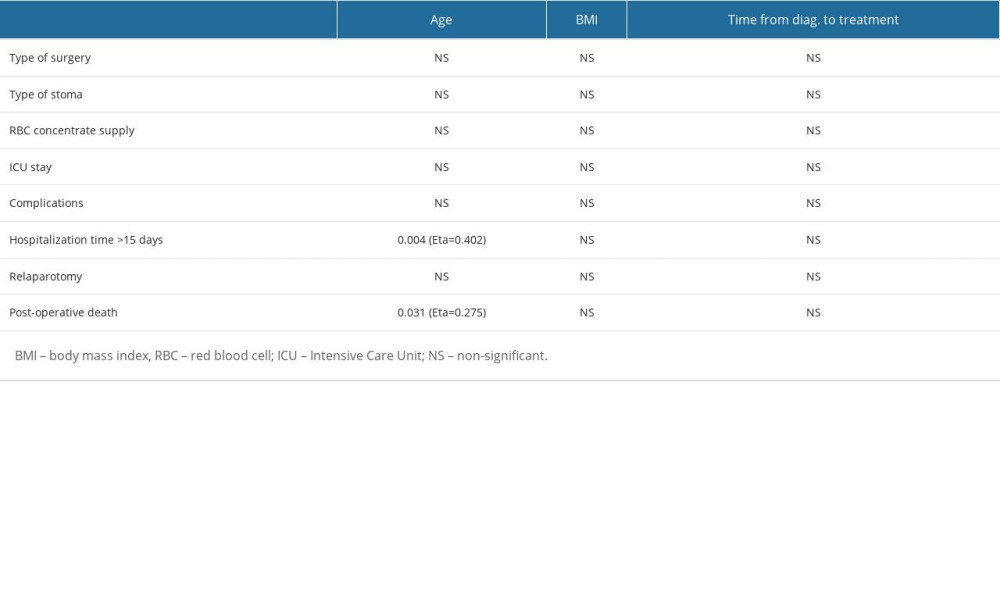 Table 5. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, quantitative-qualitative and qualitative analysis).
Table 5. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, quantitative-qualitative and qualitative analysis).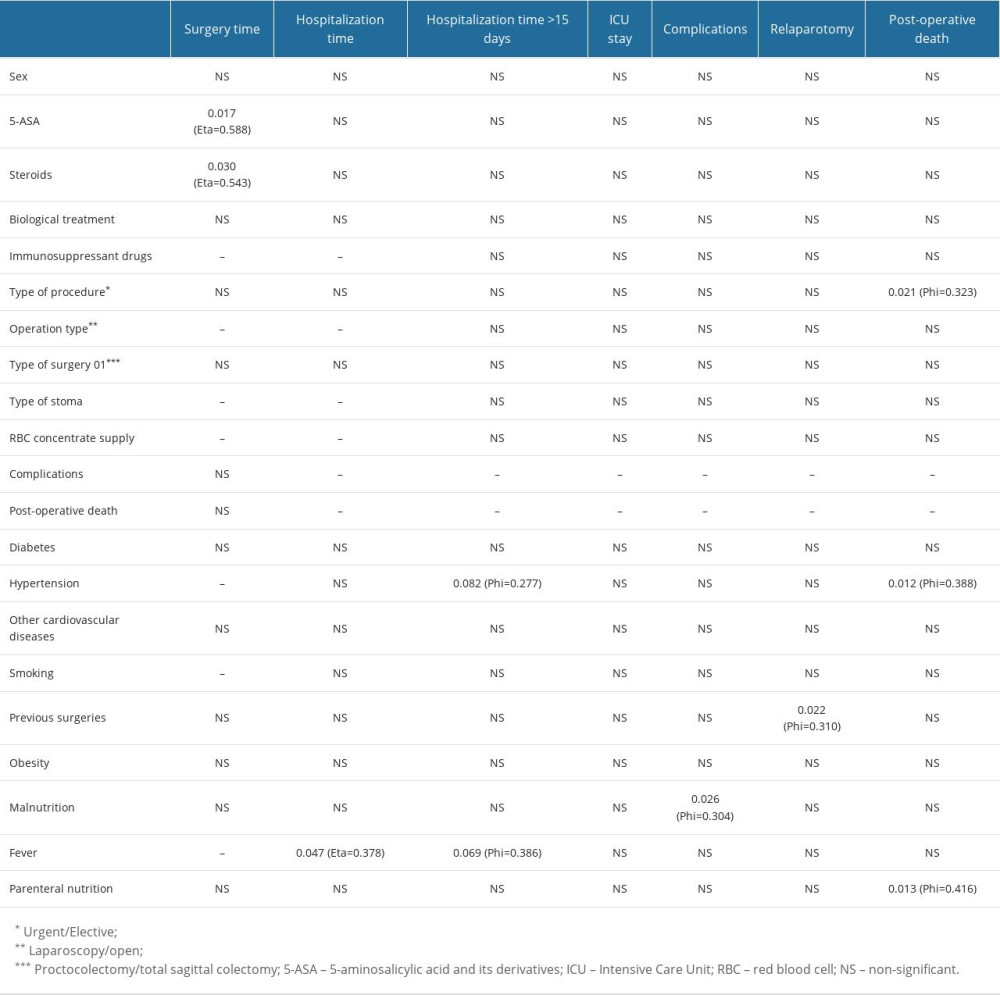 Table 6. Binary regression analysis for postoperative complications.
Table 6. Binary regression analysis for postoperative complications.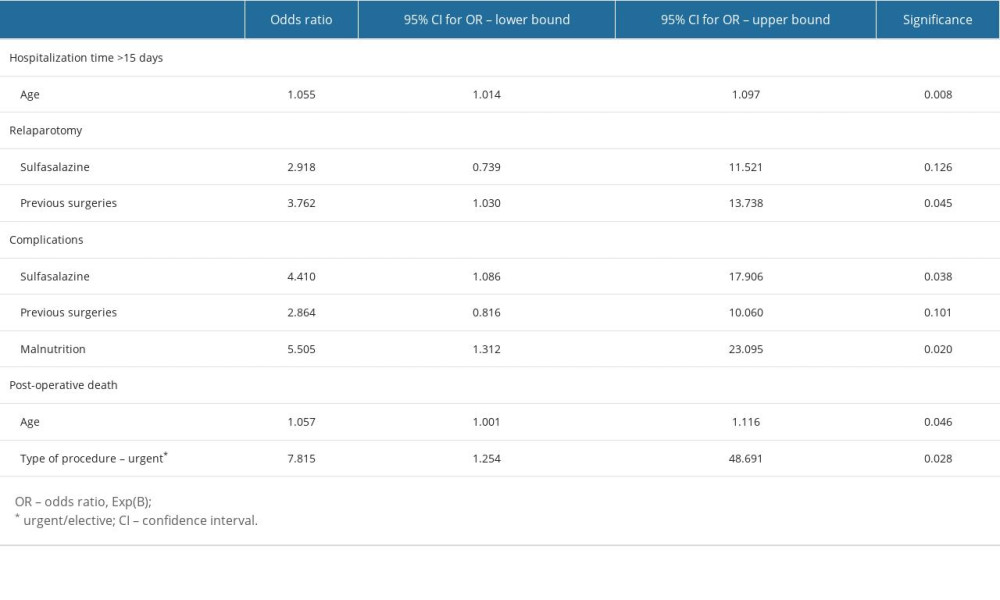
References
1. Zagórowicz E, Walkiewicz D, Kucha P, Nationwide data on epidemiology of inflammatory bowel disease in Poland between 2009 and 2020: Pol Arch Intern Med, 2022; 132(5); 16194
2. Sica GS, Biancone L, Surgery for inflammatory bowel disease in the era of laparoscopy: World J Gastroenterol, 2013; 19(16); 2445-48
3. Andersson P, Söderholm JD, Surgery in ulcerative colitis: indication and timing: Dig Dis, 2009; 27(3); 335-40
4. Frizelle FA, Burt MJ, Review: The surgical management of ulcerative colitis: J Gastroenterol Hepatol, 1997; 12(9-10); 670-77
5. Majewska K, Rusinowski C, Jabłońska B, Retrospective study of surgical outcomes in 60 patients with Crohn disease from a single center in Poland: Med Sci Monit, 2022; 28; e934463
6. Peyrin-Biroulet L, Germain A, Patel AS, Lindsay JO, Systematic review: Outcomes and post-operative complications following colectomy for ulcerative colitis: Aliment Pharmacol Ther, 2016; 44(8); 807-16
7. M’Koma AE, Inflammatory bowel disease: An expanding global health problem: Clin Med Insights Gastroenterol, 2013; 6; 33-47
8. Burisch J, Munkholm P, The epidemiology of inflammatory bowel disease: Scand J Gastroenterol, 2015; 50(8); 942-51
9. Shah SC, Khalili H, Gower-Rousseau C, Sex-based differences in incidence of inflammatory bowel diseases-pooled analysis of population-based studies from Western Countries: Gastroenterology, 2018; 155(4); 1079-89
10. Ma C, Crespin M, Proulx MC, A validation study: BMC Gastroenterol, 2012; 12; 39
11. Feuerstein JD, Curran T, Alosilla M, Mortality is rare following elective and non-elective surgery for ulcerative colitis, but mild postoperative complications are common: Dig Dis Sci, 2018; 63(3); 713-22
12. Gu J, Stocchi L, Remzi F, Factors associated with postoperative morbidity, reoperation and readmission rates after laparoscopic total abdominal colectomy for ulcerative colitis: Colorectal Dis, 2013; 15(9); 1123-29
13. De Silva S, Ma C, Proulx MC, Postoperative complications and mortality following colectomy for ulcerative colitis: Clin Gastroenterol Hepatol, 2011; 9(11); 972-80
14. Abou Khalil M, Boutros M, Nedjar H, Incidence rates and predictors of colectomy for ulcerative colitis in the era of biologics: Results from a provincial database: J Gastrointest Surg, 2018; 22(1); 124-32
15. Majewska K, Rusinowski C, Jabłońska B, Retrospective study of surgical outcomes in 60 patients with Crohn disease from a single center in Poland: Med Sci Monit, 2022; 28; e934463
16. Singh S, Al-Darmaki A, Frolkis AD, A systematic review and meta-analysis of population-based studies: Gastroenterology, 2015; 149(4); 928-37
17. Koudahl G, Kristensen M, Postoperative mortality and complications after colectomy for ulcerative colitis: Scand J Gastroenterol Suppl, 1976; 37; 117-22
18. Bernstein CN, Ng SC, Lakatos PLEpidemiology and Natural History Task Force of the International Organization of the Study of Inflammatory Bowel Disease, A review of mortality and surgery in ulcerative colitis: Milestones of the seriousness of the disease: Inflamm Bowel Dis, 2013; 19(9); 2001-10
19. Hovde Ø, Småstuen MC, Høivik ML, Mortality and causes of death in ulcerative colitis: Results from 20 years of follow-up in the IBSEN study: Inflamm Bowel Dis, 2016; 22(1); 141-45
20. Nguyen GC, Bernstein CN, Benchimol EI, Risk of surgery and mortality in elderly-onset inflammatory bowel disease: A population-based cohort study: Inflamm Bowel Dis, 2017; 23(2); 218-23
21. Negrón ME, Rezaie A, Barkema HW, Ulcerative colitis patients with clostridium difficile are at increased risk of death, colectomy, and postoperative complications: A population-based inception cohort study: Am J Gastroenterol, 2016; 111(5); 691-704
22. Bitton A, Vutcovici M, Sewitch M, Mortality trends in Crohn’s disease and ulcerative colitis: A population-based study in Québec, Canada: Inflamm Bowel Dis, 2016; 22(2); 416-23
23. Kaplan GG, McCarthy EP, Ayanian JZ, Impact of hospital volume on postoperative morbidity and mortality following a colectomy for ulcerative colitis: Gastroenterology, 2008; 134(3); 680-87
24. Gallo G, Kotze PG, Spinelli A, Surgery in ulcerative colitis: When? How?: Best Pract Res Clin Gastroenterol, 2018; 32–33; 71-78
25. Øresland T, Bemelman WA, Sampietro GM, European evidence-based consensus on surgery for ulcerative colitis: J Crohns Colitis, 2015; 9(1); 4-25
26. Sylla P, Chessin DB, Gorfine SR, Comparison with the open approach: Dis Colon Rectum, 2009; 52(3); 394-99
27. Gainsbury ML, Chu DI, Howard LA, Preoperative infliximab is not associated with an increased risk of short-term postoperative complications after restorative proctocolectomy and ileal pouch-anal anastomosis: J Gastrointest Surg, 2011; 15(3); 397-403
28. Ward ST, Mytton J, Henderson L, Anti-TNF therapy is not associated with an increased risk of post-colectomy complications, a population-based study: Colorectal Dis, 2018; 20(5); 416-23
29. Telemi E, Trofymenko O, Venkat R, Frailty predicts morbidity after colectomy for ulcerative colitis: Am Surg, 2018; 84(2); 225-29
30. Rocha R, de J, Santos G, Santana G, Influence of nutritional status in the postoperative period of patients with inflammatory bowel disease: World J Gastrointest Pharmacol Ther, 2021; 12(5); 90-99
31. Sofo L, Caprino P, Schena CA, Machine learning preliminary approach: Eur Rev Med Pharmacol Sci, 2020; 24(24); 12781-87
32. Fiorindi C, Cuffaro F, Piemonte G, Effect of long-lasting nutritional prehabilitation on postoperative outcome in elective surgery for IBD: Clin Nutr, 2021; 40(3); 928-35
33. Nelson R, Liao C, Fichera A, Rescue therapy with cyclosporine or infliximab is not associated with an increased risk for postoperative complications in patients hospitalized for severe steroid-refractory ulcerative colitis: Inflamm Bowel Dis, 2014; 20(1); 14-20
34. Ge X, Cao Y, Wang H, Diagnostic accuracy of the postoperative ratio of C-reactive protein to albumin for complications after colorectal surgery: World J Surg Oncol, 2017; 15(1); 15
35. Henriksen M, Jahnsen J, Lygren I, A predictive factor and marker of inflammation in inflammatory bowel disease. Results from a prospective population-based study: Gut, 2008; 57(11); 1518-23
36. Schoepfer AM, Beglinger C, Straumann A, Fecal calprotectin more accurately reflects endoscopic activity of ulcerative colitis than the Lichtiger Index, C-reactive protein, platelets, hemoglobin, and blood leukocytes: Inflamm Bowel Dis, 2013; 19(2); 332-41
37. Chang S, Malter L, Hudesman D, Disease monitoring in inflammatory bowel disease: World J Gastroenterol, 2015; 21(40); 11246-59
38. Azad S, Sood N, Sood A, Biological and histological parameters as predictors of relapse in ulcerative colitis: A prospective study: Saudi J Gastroenterol, 2011; 17(3); 194-98
39. Bitton A, Peppercorn MA, Antonioli DA, Clinical, biological, and histologic parameters as predictors of relapse in ulcerative colitis: Gastroenterology, 2001; 120(1); 13-20
40. Bouteloup G, Lefevre JH, Challine A, Is it still a good marker for intra-abdominal complication? A retrospective cohort study of 347 procedures: CRP after inflammatory bowel disease surgery: Int J Colorectal Dis, 2022; 37(11); 2347-56
41. Holl S, Fournel I, Orry D, Should CT scan be performed when CRP is elevated after colorectal surgery? Results from the inflammatory markers after colorectal surgery study: J Visc Surg, 2017; 154(1); 5-9
42. Ferrante M, D’Hoore A, Vermeire S, Corticosteroids but not infliximab increase short-term postoperative infectious complications in patients with ulcerative colitis: Inflamm Bowel Dis, 2009; 15(7); 1062-70
43. Selvasekar CR, Cima RR, Larson DW, Effect of infliximab on short-term complications in patients undergoing operation for chronic ulcerative colitis: J Am Coll Surg, 2007; 204(5); 956-62
44. Khazraei H, Bananzadeh A, Hosseini SV, Early outcome of patient with ulcerative colitis who received high dose of steroid and underwent two staged total proctocolectomy: Adv Biomed Res, 2018; 7; 11
45. Nguyen GC, Elnahas A, Jackson TD, The impact of preoperative steroid use on short-term outcomes following surgery for inflammatory bowel disease: J Crohns Colitis, 2014; 8(12); 1661-67
46. Kunitake H, Hodin R, Shellito PC, Perioperative treatment with infliximab in patients with Crohn’s disease and ulcerative colitis is not associated with an increased rate of postoperative complications: J Gastrointest Surg, 2008; 12(10); 1730-36
47. Bregnbak D, Mortensen C, Bendtsen F, Infliximab and complications after colectomy in patients with ulcerative colitis: J Crohns Colitis, 2012; 6(3); 281-86
48. Schluender SJ, Ippoliti A, Dubinsky M, Does infliximab influence surgical morbidity of ileal pouch-anal anastomosis in patients with ulcerative colitis?: Dis Colon Rectum, 2007; 50(11); 1747-53
49. Ferrante M, de Buck van Overstraeten A, Schils N, Perioperative Use of vedolizumab is not associated with postoperative infectious complications in patients with ulcerative colitis undergoing colectomy: J Crohns Colitis, 2017; 11(11); 1353-61
50. Kim JY, Zaghiyan K, Lightner A, Fleshner P, Risk of postoperative complications among ulcerative colitis patients treated preoperatively with vedolizumab: A matched case-control study: BMC Surg, 2020; 20(1); 46
51. Mor IJ, Vogel JD, da Luz Moreira A, Infliximab in ulcerative colitis is associated with an increased risk of postoperative complications after restorative proctocolectomy: Dis Colon Rectum, 2008; 51(8); 1202-7
Tables
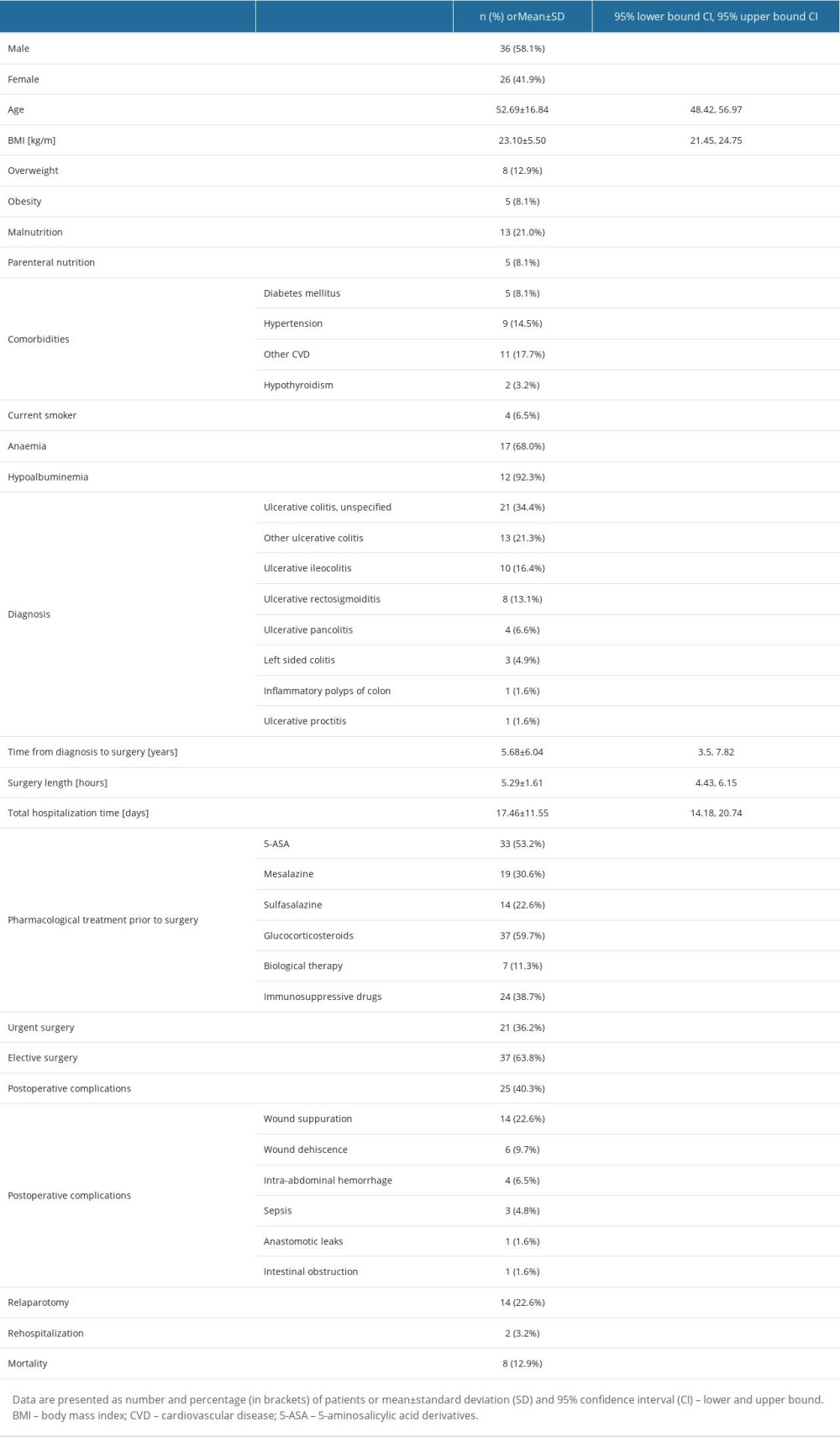 Table 1. Baseline characteristics.
Table 1. Baseline characteristics. Table 2. Difference in selected laboratory parameters examined before and after surgery.
Table 2. Difference in selected laboratory parameters examined before and after surgery.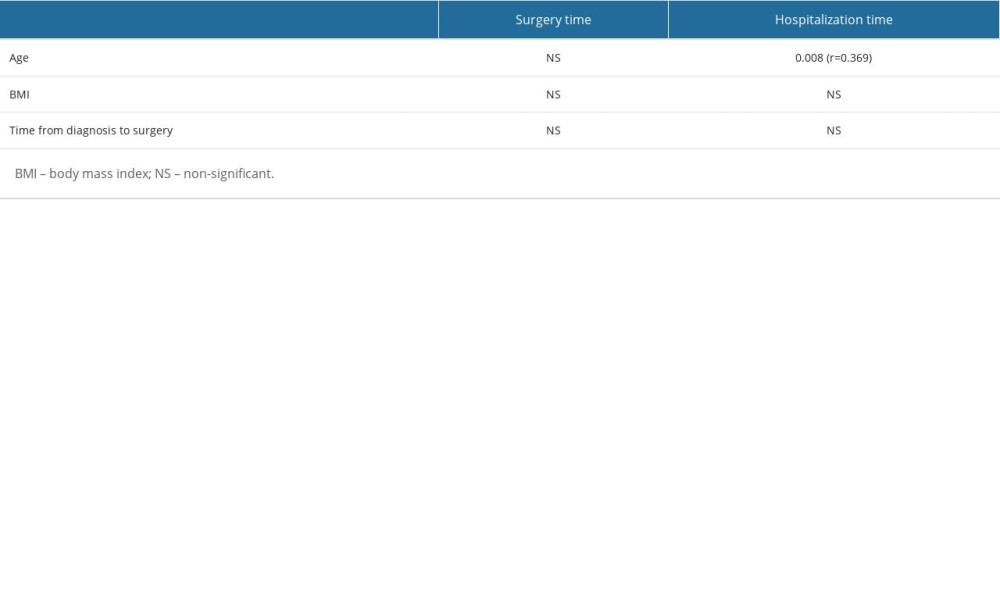 Table 3. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, quantitative analysis).
Table 3. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, quantitative analysis).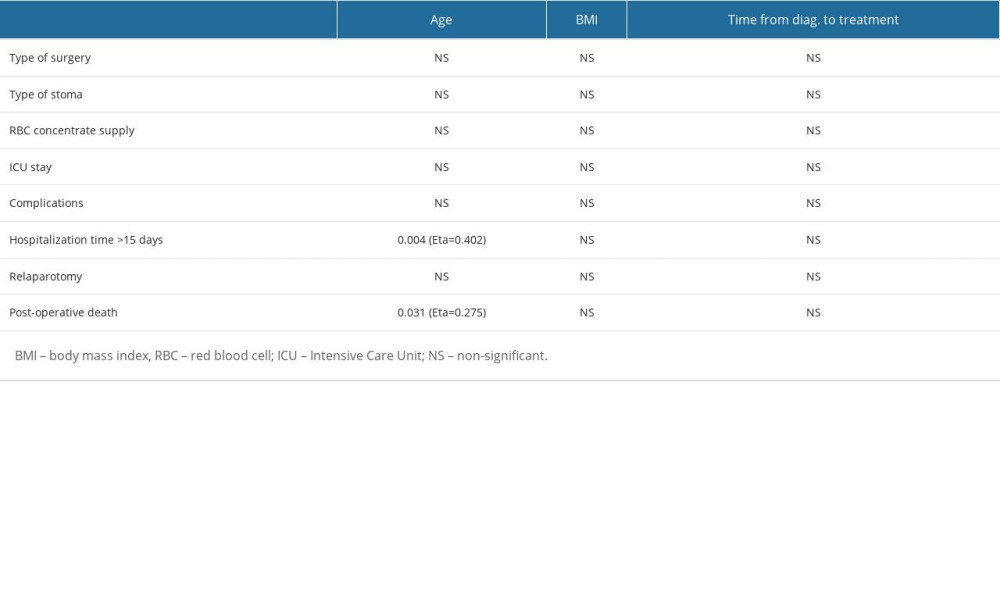 Table 4. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, qualitative-quantitative analysis).
Table 4. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, qualitative-quantitative analysis).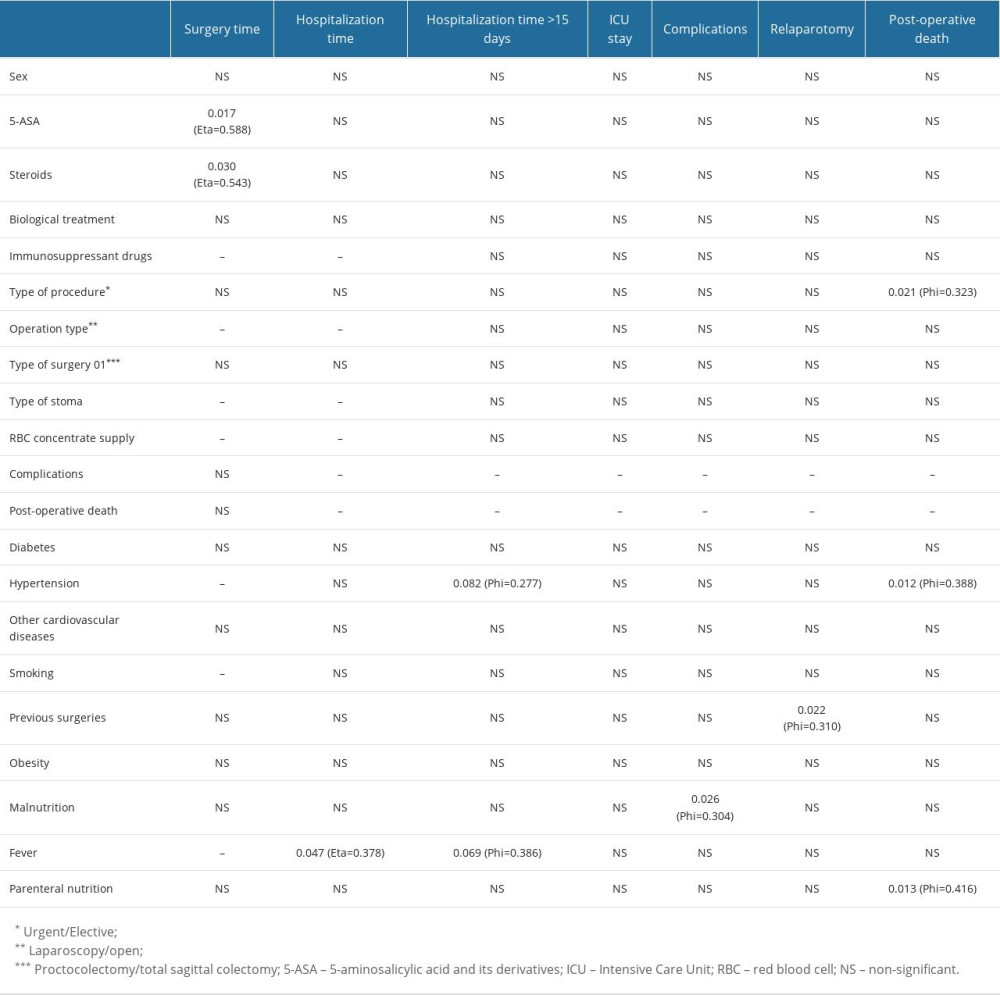 Table 5. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, quantitative-qualitative and qualitative analysis).
Table 5. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, quantitative-qualitative and qualitative analysis).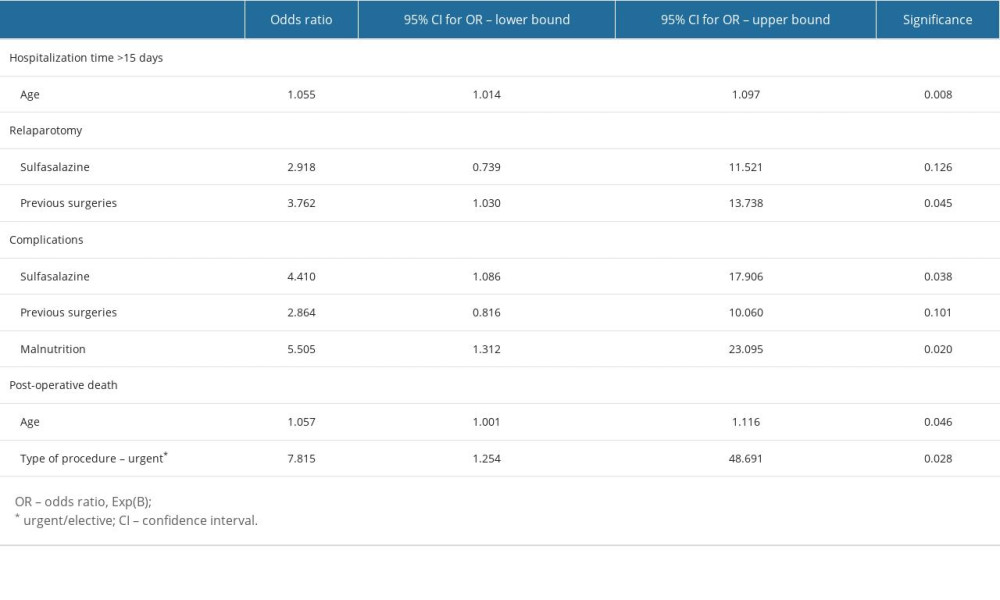 Table 6. Binary regression analysis for postoperative complications.
Table 6. Binary regression analysis for postoperative complications.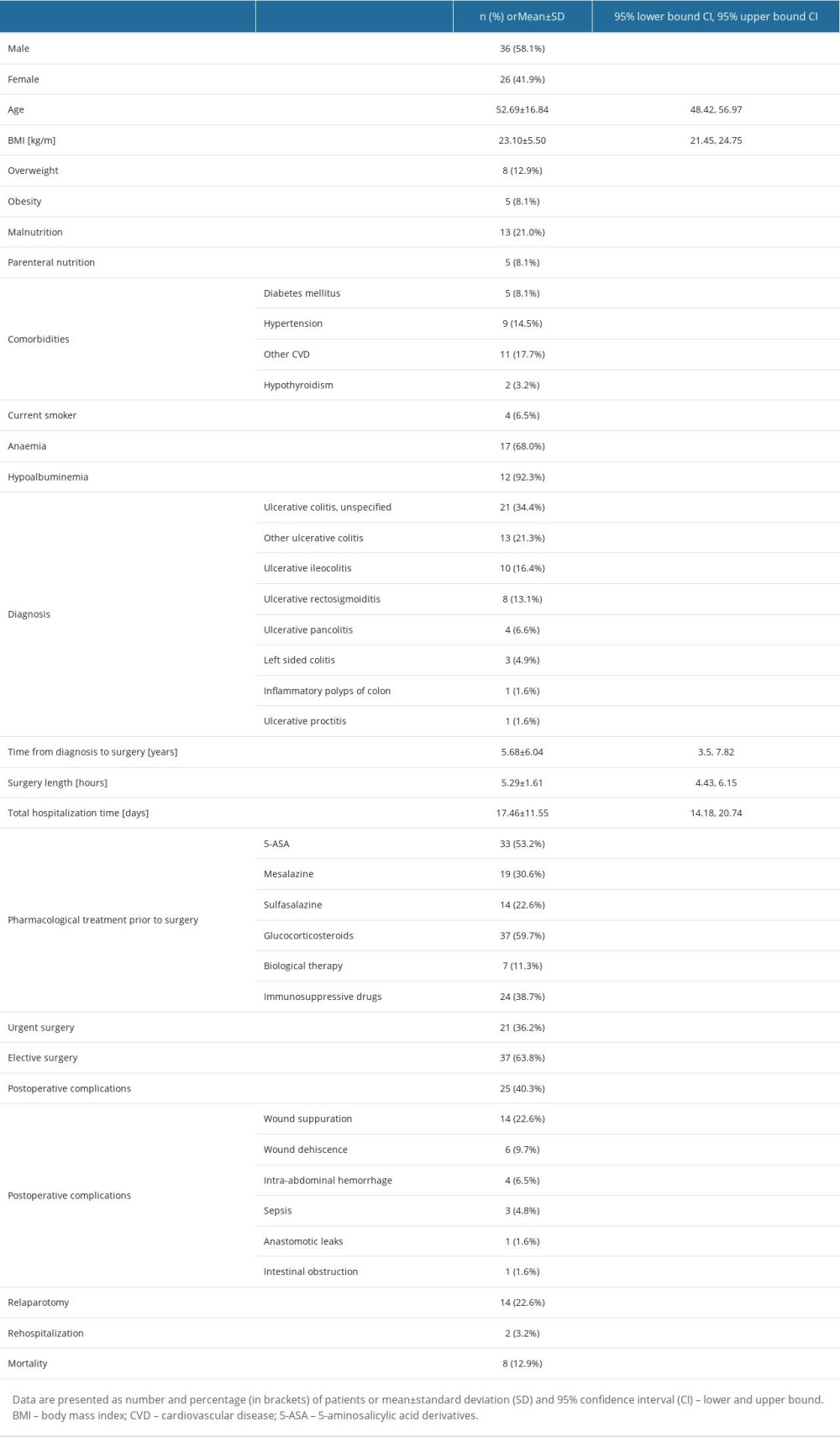 Table 1. Baseline characteristics.
Table 1. Baseline characteristics. Table 2. Difference in selected laboratory parameters examined before and after surgery.
Table 2. Difference in selected laboratory parameters examined before and after surgery.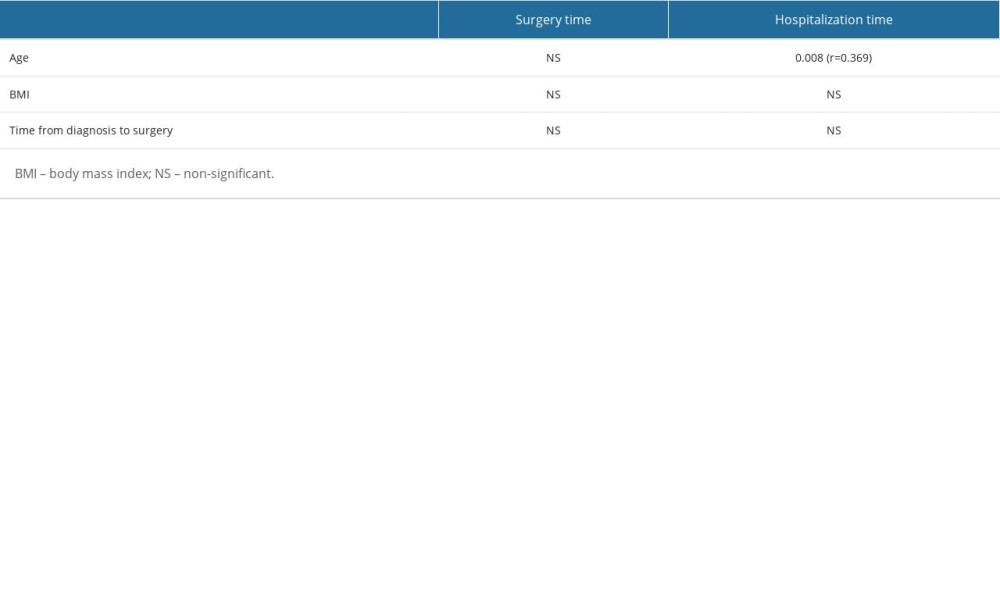 Table 3. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, quantitative analysis).
Table 3. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, quantitative analysis).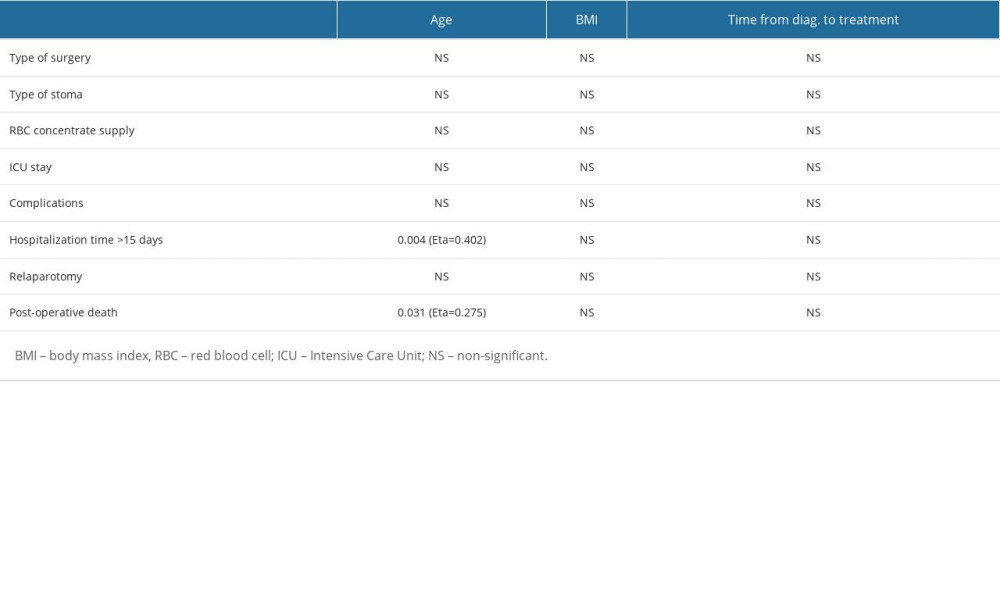 Table 4. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, qualitative-quantitative analysis).
Table 4. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, qualitative-quantitative analysis).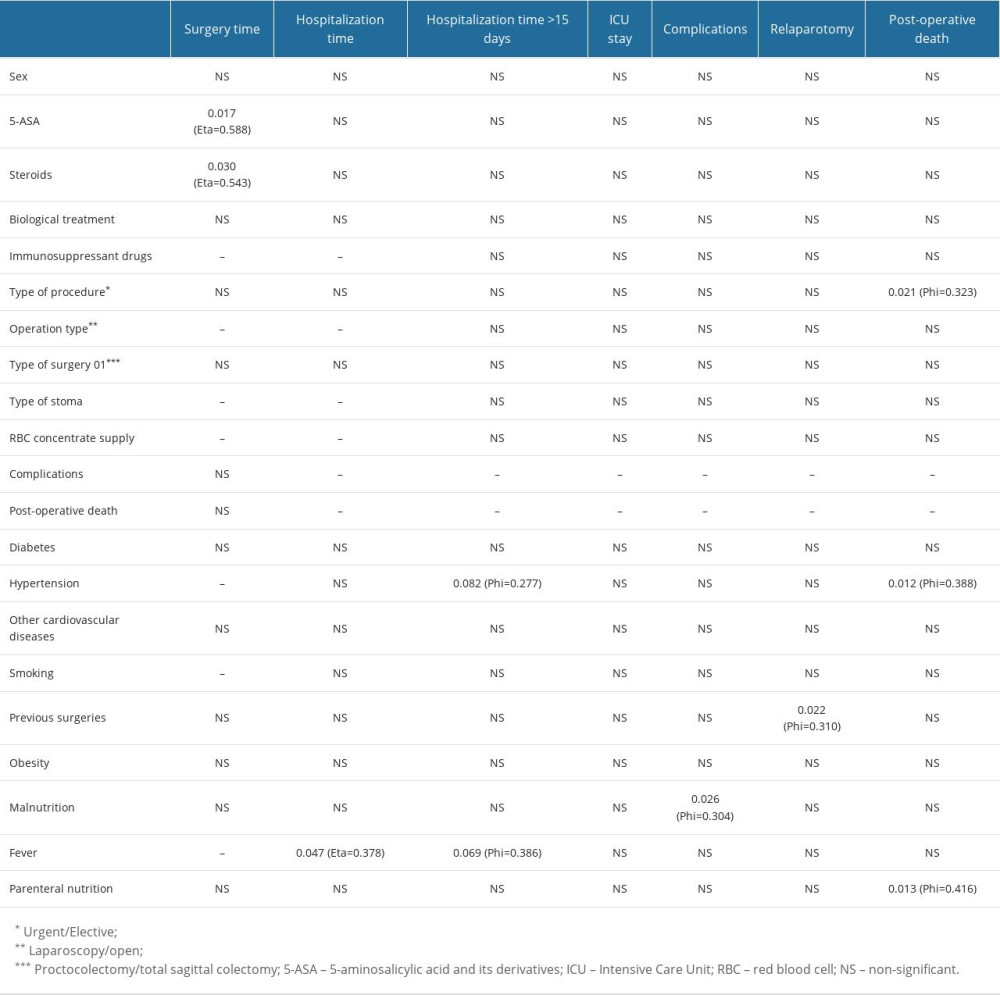 Table 5. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, quantitative-qualitative and qualitative analysis).
Table 5. Correlation analysis of preoperative versus perioperative variables (numerical data in the table represent P value, quantitative-qualitative and qualitative analysis).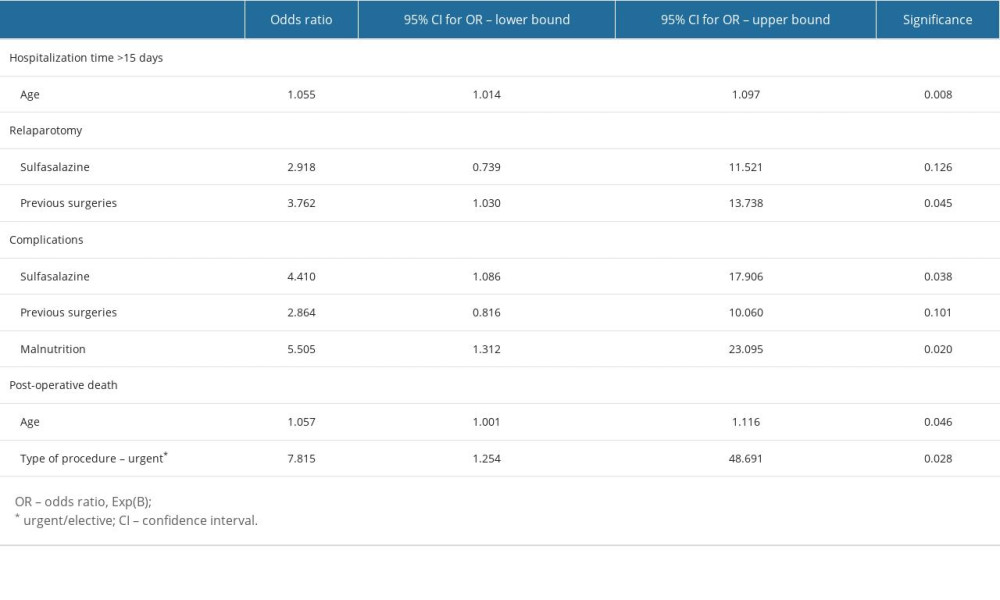 Table 6. Binary regression analysis for postoperative complications.
Table 6. Binary regression analysis for postoperative complications. In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952