17 March 2023: Clinical Research
Prospective Safety Evaluation of the Femtosecond Laser-Assisted Keratomileusis Procedure in Correcting Residual Ametropia in Patients After Deep Anterior Lamellar Keratoplasty
Dominika Janiszewska-Bil123ABCDEF*, Barbara Czarnota-Nowakowska4ABDE, Katarzyna Krysik13E, Magdalena Mistarz15E, Dariusz Dobrowolski367CD, Beniamin Oskar Grabarek15EF, Anita Lyssek-boroń138CEDOI: 10.12659/MSM.939691
Med Sci Monit 2023; 29:e939691
Abstract
BACKGROUND: This prospective study, from a single center in Poland, aimed to evaluate the correction of residual ametropia, or refractive errors, after corneal grafting using femtosecond laser-assisted in situ keratomileusis (Femto-LASIK) in 60 patients (96 eyes) who had previously undergone deep anterior lamellar keratoplasty (DALK) compared with that achieved in 60 patients (108 eyes) who underwent vision correction using Femto-LASIK alone.
MATERIAL AND METHODS: The study group included 60 patients (96 eyes) whose residual ametropia was corrected using the Femto-LASIK procedure after having previously undergone DALK. The comparison group consisted of 60 patients (108 eyes) who underwent vision correction with the Femto-LASIK procedure without previously having undergone DALK. Uncorrected vision acuity, best-corrected vision acuity, and intraocular pressure were measured for both groups before the procedures and at 3, 6, 12, and 24 months after the procedures. Corneal endothelial cell density was evaluated by non-contact specular microscopy before the procedures and at 6, 12, and 24 months after the procedures.
RESULTS: In the study group, within the 24-month observation period, no transplant rejection, transplant decompensation, or corneal ectasia were noted. Statistical analysis did not show any significant differences between the best-corrected vision acuity values in the study group in the preoperative and postoperative periods (P>0.05). In contrast, uncorrected vision acuity values were significantly higher in patients during the postoperative period than the preoperative period (P>0.05).
CONCLUSIONS: The effects of vision correction with the Femto-LASIK procedure after DALK demonstrate the safety and effectiveness of the procedure for patients.
Keywords: Cornea, Corneal Transplantation, Intraocular Pressure, Keratomileusis, Laser In Situ, Refractive Surgical Procedures, Humans, Prospective Studies, Refractive Errors, Lasers, Treatment Outcome
Background
One of the main reasons for worsening visual acuity and blindness is untreated or badly corrected refractive errors [1–4], with so-called corneal blindness currently the fourth-highest cause of blindness in the world [1–4]. Methods of vision correction include corrective eyeglasses, hard and soft contact lenses, orthocorrection, laser vision correction, and refractive lens exchange (phakic lenses) [5]. Although corrective glasses are advantageous in terms of their low cost and ease of use [6], they have a number of disadvantages, including restricted freedom of movement, reduced visibility in poor weather conditions, a narrower field of vision, and alterations in the size of images [6]. In cases of presbyopia (which also requires correction for myopia, hyperopia, and/or astigmatism), it is often impossible to correct the vision defect with glasses [6]. One alternative to glasses are contact lenses [7,8]. Unfortunately, among the contraindications to their use are tendencies for conjunctivitis, allergies, lens intolerance, and dry eye syndrome [7,8]. While soft contact lenses shorten the period of adaptation of the eyeball, thereby improving comfort [7,8], they also increase the risk of corneal hypoxia and aggravation of dry eye syndrome [7,8]. On the other hand, hard contact lenses are used to correct non-regular corneal astigmatism, such as in the corneal conus and in conditions following keratoplasty, refractive surgery, and corneal trauma [7,8]. The third option for correcting vision defects is orthocorrection surgery, which is used for patients with myopia up to - 6.0 diopters (D) and for astigmatism up to - 1.5 D [9,10]. The underlying mechanism behind specially designed inverted hard contact lenses, which the patient only wears overnight while sleeping, is not yet fully understood [9,10]. The inverted hard contact lenses method is reversible such that when it is discontinued, the cornea returns to its original shape [9,10]. Refractive surgery, including laser vision correction, is a field of ophthalmic surgery that handles the removal of refractive errors and is divided into 2 types: refractive corneal surgery and refractive lens surgery [11]. Laser vision correction procedures are divided into superficial and deep methods [12,13]. Superficial methods involve modulating the outer wall of the corneal dermis using an excimer laser after removing the corneal epithelium [13,14]. These methods include the following: photorefractive keratectomy, laser subepithelial keratomileusis (LASEK), Epi-Bowman keratectomy, epithelial laser-assisted in situ keratomileusis (Epi-LASIK), and transepithelial photo refractive keratectomy [13,14]. These methods account for about 20% of all laser vision correction procedures [13,14]. Deep methods, on the other hand, include laser-assisted in situ keratomileusis (LASIK), femtosecond laser-assisted in situ keratomileusis (Femto-LASIK), and refractive lenticule extraction small incision lenticule extraction (ReLEx Smile) [15–17]. Laser vision correction can be divided into superficial and deep surgical procedures, and the Femto-LASIK procedure is part of the latter [18–20]. The difference between superficial and deep surgical procedures is the way in which the cornea is prepared for the procedure. In Femto-LASIK, a deep laser vision correction procedure, the microkeratome blade cut is replaced by an extremely precise, computer-controlled femtosecond laser [18–20]. This laser is part of the newest generation of lasers used in ophthalmology [18–20]. To qualify patients for the procedure, a topographic map of their corneal epithelium must be created with the aid of coherence tomography, and an evaluation of the tear film must be performed [18–20]. The procedure conducted via this method involves 2 stages [18–20]. In the first stage, a flap with a thickness of 100 to 110 microns is prepared via a femtosecond laser [18–20]. In the second stage, the cornea is ablated, during which, with the aid of an excimer laser, the stroma of the cornea is modeled [18–20]. Thanks to precise computer programming, the location of the ablation does not need to be repositioned in any way and the laser beam falls exactly onto the indicated location of the cornea [18–20].
It is certain that a refractive procedure is safer for patients who have undergone a cornea transplant than another transplant, which carries a much greater burden and poses a higher risk for the patient, especially as refractive procedures do not require corneal tissue [21,22]. In refractive surgery, the most important evaluated parameters are uncorrected vision acuity (UCVA), which is visual acuity expressed in D without any correction, and best-corrected vision acuity (BCVA), which is visual acuity expressed in D after the application of an appropriate vision correction, determined during the eye examination [23–25]. After the laser vision correction procedure, the UCVA value corresponds to the visual acuity the patient would have achieved after correction before the procedure [23–25]. This explains why the UCVA values before and after a successful procedure are significantly different from each other, while the corresponding BCVA values are not statistically significant [23–25]. On the other hand, the small differences between the UCVA and BCVA values after the procedure are attributable to the fact that laser vision correction does not fully correct visual impairment [23–25].
Today, corneal transplantation is a routine surgical procedure performed to restore continuity to the corneal tissue or to restore or bestow the appropriate shape to the cornea when other methods of vision correction, such as corrective glasses with properly selected lenses or contact lenses, fail [26]. Corneal transplantation, or keratoplasty, is one of the most commonly performed and successful forms of tissue transplantation worldwide [27–29]. Among the indications for keratoplasty are bullous keratopathy, corneal dystrophy, Fuchs’ dystrophy, corneal cone, keratitis, traumatic scarring, and decompensation of the graft flap, among others [27–29]. There are basically 2 types of corneal transplantation: (1) penetrating keratoplasty and (2) layered deep anterior lamellar keratoplasty (DALK), Descemet’s stripping automated endothelial keratoplasty, and Descemet membrane endothelial keratoplasty [30–32]. Currently, DALK is an alternative to photorefractive keratectomy [33,34]. The main advantages of DALK are the preservation of the corneal endothelium and lower risk of immune reactions and graft loss [33,34].
The Femto-LASIK procedure has been used in the treatment of refractive errors after penetrating keratoplasty [14]. Studies conducted by Ghoreishi et al on a group of 34 patients during a 12-month observation period after the Femto-LASIK procedure showed that it was a safe, effective, and recommended method for the correction of spherical and cylindrical components of refractive error [35]. Afonso-Bartolozzi et al conducted, on a smaller scale to our study, an evaluation of the results of the Femto-LASIK procedure in patients with residual astigmatism who had previously undergone DALK [36]. They examined 10 eyes, with a follow-up of 30 to 60 months, and reported no intraoperative or postoperative complications [36]. Based on these results, they concluded that Femto-LASIK is a successful and safe method for correcting residual astigmatism in patients after DALK [36].
Our prospective study, from a single center in Poland, was aimed at evaluating the correction of residual ametropia, or refractive errors, after corneal grafting using Femto-LASIK in 60 patients (96 eyes) who had previously undergone DALK compared with that achieved in 60 patients (108 eyes) who underwent vision correction using Femto-LASIK alone.
Material and Methods
ETHICS:
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Institutional Bioethical Committee operating at the Regional Medical Chamber in Krakow, no. 68/KBL/OIL/2020. Each patient who agreed to participate in the study read and signed an informed consent form. Those patients who were unable to willingly decide to participate in the study were excluded.
STUDY DESIGN:
An evaluation of BCVA, UDVA, intraocular pressure (IOP), corneal endothelial cell density (ECD), and central corneal thickness (CCT) was performed on the comparison group before the Femto-LASIK procedure and at 3, 6, 12, and 24 months after the procedure. An evaluation of ECD was performed on both patient groups before the Femto-LASIK procedure and at 6, 12, and 24 months after the procedure.
In the study group and the comparison group, the Femto-LASIK procedure was performed in patients with normal corneas. In patients in the study group, the DALK procedure was performed first, followed by the Femto-LASIK procedure, so there were no contraindications to Femto-LASIK [33,36].
STUDY GROUP:
The study group included 60 patients (96 eyes), of whom 12 were women (40%) and 18 were men (60%), all aged 39.2±4.1 years (range, 31–52 years). These patients had all undergone DALK due to conical cornea, corneal dystrophy, or a corneal injury, in which residual defects were corrected using the Femto-LASIK procedure. The inclusion criteria were as follows: no fewer than 3 years had elapsed since the corneal transplant had been performed, at least 1 year had elapsed since the removal of the corneal stitches, corneal thickness was at its thinnest 540 μm, and informed consent to participate in the study had been provided. Additionally, only those patients whose refractive errors could not be corrected using other methods, such as glasses or soft or hard contact lenses, were included in the study. Thus, those patients with myopia (−6.7±1.2 D; cylinder 5.15±0.87 D) or hyperopia (+2.75±1.1 D; cylinder 5.25±0.90 D) were included in the study. Rule astigmatism was found in 6 patients (3 with myopia, 3 with hyperopia), against-the-rule astigmatism in 22 patients (10 with myopia, 12 with hyperopia), and oblique astigmatism in 10 patients (3 with myopia, 7 with hyperopia).
An alternative to the performed procedure was another corneal transplant. However, the waiting time for corneal tissue in Poland is quite long, at a minimum of 2 years. Patients who had undergone DALK fewer than 3 years prior to the Femto-LASIK procedure, whose corneal thickness at its thinnest was less than 540 μm, and/or who did not provide informed consent to participate in the study were excluded.
COMPARISON GROUP OF PATIENTS:
The comparison group included 60 patients (108 eyes), of whom 24 were women (40%) and 36 were men (60%), all aged 36.1±3.8 years (range, 28–49 years) after vision correction using the Femto-LASIK procedure. The inclusion criteria were as follows: diagnosed myopia (up to −10 D), hyperopia (up to +4 D), no astigmatism, lack of other diseases of the cornea, appropriate IOP, no damage to the eyeball in the past, and informed consent to participate in the study.
EVALUATION OF UCVA AND BCVA:
The test of visual acuity for distance was used to assess retinal resolving ability – that is, the perception of 2 points in close proximity as separate points.
The UCVA and BCVA tests were conducted using a Snell array at a distance of 6 m to eliminate the effect of eyeball accommodation. Snell arrays contain signs, for example, numbers and letters (optotypes), of decreasing size but of the same angular size (5 minutes). Next to each row, the distance from which the elements of the optotypes in that row are visible at an angle of 1 minute is also given. Optotypes are 5 angular minutes in size in their entirety, and the distinguishing elements of each are 1 angular minute in size, for example, the numbers 1 and 7 or 5 and 6 differ only by single small elements in typography, similar to the letters U and V, or I and L. This optotype size makes them easier to distinguish and communicate with the patient. Visual acuity is recorded as a fraction. In the numerator is written the distance from which the examinee reads the optotypes (in Poland, it is 5 m). In the denominator is entered the value appearing next to the last row of optotypes that is correctly recognized by the patient (ie, the distance from which the optotype elements are seen at an angle of 1 minute, or, ie, the distance from which examinees should recognize them if they have full visual acuity). If a patient correctly recognizes optotypes from the last, lowest row, his or her visual acuity is 5/5, or, in decimal notation, 1.0. If the patient recognizes only the optotype in the first, highest row on the board, his or her visual acuity is 5/50, or, in decimal notation, 0.1. The test does not require special preparation; although, like any psychophysical test, this will depend on the patient’s mental state. Therefore, it is advisable that the patient be fully rested and properly focused during the test.
An automatic RT-3100 Phoropter (Nidek, Tokyo, Japan) was used to determine BCVA prior to Femto-LASIK surgery. The phoropter examination, which is completely painless, requires patients to answer questions posed by the ophthalmologist conducting the examination. One eye is examined first, after which, once the best correction has been selected, the other eye is examined. Finally, the patient’s level of comfort is checked against the final settings for both eyes.
EVALUATION OF CORNEAL TOPOGRAPHY:
Corneal topography assessments were performed using the Pentacam Oculus camera (Oculus Sp z o.o., Warsaw, Poland). This examination allows the physician to identify abnormal corneal structure, which is a contraindication to laser vision correction. Using a high-resolution rotating Scheimpfung camera (360°), cross-sectional images of the cornea are created, which are then assembled into a 3-dimensional model of the anterior segment of the cornea and analyzed. The topography of the cornea is visualized as color maps from stubble to stubble. The anterior corneal surface is also described by the central rays, central corneal astigmatism, and its axis value. Finally, the following are obtained: (1) four corneal refractive maps (axial, elevation of the anterior corneal surface, elevation of the posterior corneal surface, pachymetric map), (2) a map with corneal thickness profiles and corneal irregularity indices, and (3) a map with the Berlin/Ambrosio Enhanced Ectasia report.
OPTICAL SPECTRAL COHERENCE TOMOGRAPHY:
Optical spectral coherence tomography (OCT) is a noninvasive and non-contact technique that allows the imaging of 2-dimensional tissue cross-sections via the measurement of the delayed echo and intensity of light reflected or back-scattered from internal tissue structures. The method uses light wavelengths of 820 nm. The OCT interferometer measures the delay between when the light beam is sent and reflects off the eye structures and returns to the camera. Based on this delay, an image of the eyeball structures is created.
In the present study, OCT was employed to evaluate the corneal transplant flap as well as to measure the flap after the Femto-LASIK procedure using the Casia apparatus (Tomey Corp, Nagoya, Japan). The study used a pachymetry map scan (8 lines of 128 scans each) and Visante time-domain OCT (Carl Zeiss Meditec, Inc, Dublin, CA, USA) to evaluate CCT.
IOP ANALYSIS:
To assess IOP, Goldman applanation tonometry was used with a special prism with which the cornea was flattened after anesthesia and the corneal image was viewed under a slit lamp. The measurement itself was based on the Imbert-Fick rule, according to which the pressure inside the sphere is equal to the force needed to flatten it, divided by the size of the flattening area. Seated patients face a slit lamp while the surface of their eye is anesthetized and the tear film is stained with a solution of fluorescein, which begins to glow (exhibits fluorescence) when exposed to cobalt-blue light. With the tip of the prism, the top of the cornea is pressed. Upon contact with the cornea, the tinted film produces a meniscus around the circular tip of the prism, which is visible in the form of 2 yellow semicircles. The scale of the tonometer is set so that these half-circles make contact with the inner edges, after which the pressure value is read. IOP values in the range 11 to 21 mmHg were assumed to be correct.
CORNEAL ENDOTHELIAL EXAMINATION:
Corneal endothelial examination involves analyzing corneal endothelial cells for their number, density, shape, and surface area. The examination is performed using a specular microscope (Conan, SP-3000, Japan) via a non-contact method that is painless and noninvasive. The examination counts the number of endothelial cells with the aid of a computer and performs corneal thickness measurements (pachymetry).
The morphometric evaluation in the current study included: (1) the number of cells analyzed, (2) the average size of the analyzed endothelial cells, (3) the density of the analyzed endothelial cells presented as the number of cells per 1 square mm, (4) the variability of cell co-occurrence derived by dividing the average size by the standard size, and (5) size of the largest and smallest cell.
DALK SURGICAL PROCEDURE:
All procedures were performed under general anesthesia. After placing the dilation and marking the center of the cornea, the cornea was incised with a Hesburg-Baron vacuum trephine (7.5 mm) at about 80% thickness. Then, a 27G needle was bent in the distal one-third at an angle of 30°, with the incision pointing downward, after which it was placed on a syringe filled with sterile air. The needle was inserted para centrally interstitially so that the end of the needle could be seen in the center of the cornea, after which interstitially sterile air was injected to detach Descemet’s membrane. The next step in the procedure involved interstitially inserting a spatula and incising the corneal parenchyma above it, after which paracentesis was performed to lower the IOP and detach Descemet’s membrane. Subsequently, the posterior parenchyma was systematically detached from Descemet’s membrane and cut out with scissors. Descemet’s membrane presented as a shiny, smooth surface, resembling a sheet of ice.
The previously hand-dilated donor flap (7.5 mm) was placed on a Teflon block with the endothelium facing upward. Using tweezers, Descemet’s membrane was separated from the endothelium. The flap, prepared in this way, was applied to the lamina of the recipient’s dissected eyeball. A double continuous suture of 10.0 nylon was used. The various stages of the procedure are presented in Figure 1.
All patients received 8 mg of dexamethasone phosphate sodium intravenously on the day of surgery. This dose was maintained for the first 3 days after surgery, after which, on the fourth postoperative day, the dose was reduced to 4 mg of the preparation. On average, on the seventh postoperative day, patients were discharged with recommendations to continue treatment, with a dose of 4 mg of methylprednisolone acetate administered orally for an average of 1 month. All patients also received, from the day of surgery, orally administered ciprofloxacin, an antibiotic from the fluoroquinolone group, at a daily dose of 1 g (2×500 mg). Treatment was continued for 10 days. In the first 7 days after surgery, while still hospitalized, patients were administered a topical treatment according to the regimen listed in Table 1.
On average, patients were discharged on the seventh postoperative day. The qualification criterion for successful surgery was complete coverage of the transplanted flap with the recipient’s epithelium. The local and general treatment scheme is shown in Table 2.
LASER VISION CORRECTION USING THE FEMTO-LASIK PROCEDURE:
Patients were treated with Femto-LASIK, a vision correction procedure, during which 2 separate lasers were used: a femtosecond laser with which a corneal flap is created, and an excimer laser, which corrects vision defects inside the cornea. Femto-LASIK began by preparing the site for the procedure. Then, the patient’s eye socket was washed with a special disinfectant fluid, while local anesthesia was administered to the eyeballs in the form of lignocaine eye drops. Next, with the use of the Carl Zeiss VisuMax femtosecond laser, the flap was entirely raised. The incision was made using energy from the femtosecond laser, which allowed for the separation of collagen fibers and the creation of a flap with a thickness of 100 to 110 μm. The corneal flap created during a corneal transplant generally has a diameter of 8.5±0.05 μm (minimum 8.3 μm, maximum up to 8.7 μm), depending on the diameter of the ablation. However, flaps that are transplanted most often have a diameter of 8.3 μm. In the following stage, the ablation of the corneal stroma was conducted with a laser, which was entirely painless for the patient. After modeling the cornea, the flap was repositioned.
After the procedure, the patient was instructed to wear an eye shield. To create the corneal flap, the Visu Max Femtosecond Laser (Carl Zeiss Meditec Jena, Germany) was used. At the same time, the ablation was conducted with the Mel 80 laser (Carl Zeiss Meditec, Jena, Germany).
After the procedure, the patients received dexamethasone sodium phosphate (Tea, France) 4 times a day for 7 days, after which a progressively reduced dose was given: 3 times for 7 days, 2 times for 7 days, and 1 time for 7 days. In addition, the antibiotic levofloxacin was used 4 times a day for 7 days, as well as moisturizing drops with an active sodium hyaluronate at a concentration of 0.15% every hour. Neither oral immunosuppression nor general steroid therapy was used. Figure 2 shows a graphical interpretation of the various stages of the Femto-LASIK procedure.
STATISTICAL ANALYSIS:
In the first step, after implementing the database from an Excel spreadsheet into a statistical program, we assessed whether the distribution of the analyzed data met the assumptions of a normal distribution. To do this, we used the Shapiro-Wilk test, which showed that the distribution of our data conformed to the assumptions of a normal distribution. As the null hypothesis was not rejected, we performed the statistical analysis using parametric methods. Accordingly, the data were presented as a mean±standard deviation. We further checked the homogeneity of the variance with the Leven test. Confirmation of homogeneity of variance permitted us to use one-way and two-factor ANOVA for further statistical analysis. When the
Results
CHANGES IN UCVA AND BCVA DURING 24-MONTH OBSERVATION:
One-way ANOVA showed that there were statistically significant differences in UCVA values (
In contrast, the changes in BCVA values in the study and comparison groups were not statistically significant (one-way ANOVA analysis;
However, when a two-factor ANOVA analysis was performed, taking into account the timing of the evaluation (months) as well as the type of group (study, comparison), statistically significant differences were found when comparing the UCVA and BCVA values (P<0.05). This indicates that the changes in BCVA and UCVA values were dependent not just on the Femto-Lasik procedure itself but also on whether a DALK procedure had been previously performed (P<0.05). Detailed UCVA and BCVA values for both groups are shown in Table 3.
CHANGES IN CCT DURING 24-MONTH OBSERVATION IN THE STUDY GROUP:
CCT thickness before the Femto-LASIK procedure in the study group was 591 m±9 μm; whereas, at 3, 6, and 12 months after the procedure, CCT thickness was 489 μm±12 μm. At the 24-month follow-up, a CCT thickness of 485 μm±7 μm was recorded. One-way ANOVA indicated the presence of statistically significant differences in CCT thickness (P<0.05). Therefore, a Tukey post-hoc test was performed, which showed that CCT thickness was different between the period before the Femto-LASIK procedure was performed and at each month following the procedure, during which CCT was assessed (P<0.001; Tukey post-hoc test). Changes in CCT values in the study group during the 24-month follow-up are shown in Figure 3.
CHANGES IN IOP DURING 24-MONTH OBSERVATION:
One-factor ANOVA did not generate any statistically significant findings concerning IOP during the follow-up in either the study or comparison group (P>0.05). In both groups, the IOP values were comparable, as confirmed by the results of the two-factor ANOVA (P>0.05). In both groups, IOP values were within the normal range (11–21 mmHg) during the entire 24-month follow-up period. Detailed IOP results by period for both groups are shown in Table 4.
ANALYSIS OF ECD DURING THE 24-MONTH OBSERVATION:
One-factor ANOVA did not generate any statistically significant findings concerning ECD during the follow-up in either the study or comparison group (P>0.05). Nevertheless, lower ECD was observed in the study group than in the comparison group. Two-factor ANOVA confirmed that ECD density was dependent on whether the patient had undergone a DALK procedure before the Femto-Lasik procedure (P<0.001). Detailed ECD results by period for both groups are shown in Table 5.
Discussion
Laser vision correction using the Femto-LASIK procedure is a less invasive method of visual acuity correction than undergoing yet another corneal transplant for patients who had already undergone cornea transplantation due to conical cornea, corneal dystrophy, or another injury. In addition, concerning the corneal tissue needed to perform a transplant, it is easier to employ refractive surgery [37,38]. Refractive surgery can also occasionally be used to alleviate adverse effects from other conditions, such as cataracts [39,40].
The effectiveness of the Femto-LASIK procedure for patients who had previously undergone corneal transplantation was confirmed by studies conducted by Ghoreishi et al in which 16 of 34 patients underwent the Femto-LASIK and Zyoptix Personalized Treatment Advanced procedures, while 18 patients underwent the tissue-saving Femto-LASIK procedure. Ghoreishi et al showed that, during a year-long observation, the preoperative myopic spherical equivalent refraction decreased from -6.50±2.8 D to −1.6±1.8 D and the mean hyperopic spherical equivalent refraction decreased from +3.2±2.20 D to 0.37±1.2 D [35]. Similarly, Guccione et al demonstrated the effectiveness of correcting visual defects via the Femto-LASIK procedure among 31 patients. These researchers noted a correction of the preoperative astigmatic topographic cylinder of 56% and of the preoperative refractive error of over 42%, as well as an approximate 20% improvement in BCVA and UCVA values [41]. Chuprov et al also confirmed the safety and effectiveness of the Femto-LASIK procedure during the correction of astigmatism while operating on cataracts among a group of patients for whom the implantation of toric intraocular lenses or peripheral femtolaser corneal incision were used. In the early postoperative phase, Chuprov et al noted the visual acuity in both groups to be at the level of 0.8 to 1.0, which remained constant up to 6 months after the procedure. The observed vision acuity they observed was similar to that of the present study [42]. Therefore, based on the UCVA and BCVA values obtained in the present study, we can conclude that vision correction with the Femto-LASIK procedure in patients after undergoing DALK is a safe and effective method, one characterized by long-term improvement in the patients’ quality of life. Our conclusion is further supported by observations made by Klokova et al, who demonstrated a significant improvement in the quality of life of patients over a period of 2 years following the laser vision correction procedure [43]. That said, when evaluating the safety and effectiveness of vision correction via the Femto-LASIK procedure in patients after undergoing DALK, CCT results must be considered.
In this regard, Pateras et al evaluated CCT values before and after myopia correction that employed the Femto-LASIK procedure, obtaining statistically significant results of 552.43±27.82 μm vs 493.21±36.30 μm (
During the Femto-LASIK procedure, a small cut must be made on the surface of the cornea in order to create a flap. Doing so, however, causes temporary nerve damage on the surface of the cornea, consequently leading to a decrease in the release of the tear film. This in turn leads to dry eye syndrome [46–48]. However, it should be noted that patients who qualified for inclusion in the present study had a corneal flap of a thickness of 110 to 100 μm, which significantly reduced the risk of dry eye syndrome.
Recent studies on the treatment of dry eye syndrome have been targeted at developing biological therapies that can be used to reduce inflammation – the fundamental cause of dry eye syndrome – as well as to moisturize the surface of the eyeball [49].
To reduce adverse effects following the Femto-LASIK procedure, the eyes must be moisturized with eye drops containing the appropriate concentration of hyaluronic acid. Directly after the procedure, special attention must be paid to recommendations and eye hygiene. Above all, at the beginning of recovery, the eyes must not be subjected to unnecessary pressure. Swimming is strictly forbidden for about 1 month after the procedure, as is the use of eye cosmetics or visits to a solarium or sauna. It is also recommended that exposure to smoke-filled and/or dusty places be limited and that intense physical effort be avoided. It is extremely important to ensure that the eyes are properly moisturized and that pharmaceuticals are used as recommended by a physician [46,50].
In the case of our patients, neither oral immunosuppression nor steroid therapy was used; instead, sodium hyaluronate at a concentration of 0.15% was administered every hour to adequately moisturize the eyes and thereby avoid the adverse effects that can otherwise occur after such procedures. During control visits, patients were asked whether they followed the doctor’s recommendations, with the responses always being in the affirmative.
In the case of the Femto-LASIK procedure, the corneal flap is designed to be as thin as possible to minimize nerve damage and avoid the risk of the procedure failing. These steps were also taken to prevent or minimize dry eye symptoms or, if they occurred, to make them easy to alleviate with the aid of proper pharmacological treatment, such as moisturizing drops.
It was also essential to evaluate ECD in the comparison and study groups during the 24-month observation period. Based on the results of the present study, it can be stated that although, in the study group, ECD was significantly lower than in the comparison group, the percentage of ECD loss in both groups was comparable and therefore did not statistically differ between the groups (
Determining changes in the number of ECD cells that comprise the monolayer of endothelium with a thickness of 4 to 6 μm was extremely important since this layer plays a significant role in maintaining optical transparency and also because these cells possess limited regenerative potential. Therefore, the loss of these cells may be only partially compensated for by the migration of endothelial cells, their growth, and heterogeneity. It must, therefore, be considered that a drop in ECD is a physiological phenomenon and decreases with age from approximately 4000/mm2 at the time of birth to approximately 1000/mm2 for people 80 years and older. Factors that significantly accelerate the loss of endothelial cells include intraocular surgery, injury, and glaucoma [52,53. It should come as no surprise that the number of endothelial cells in the study group was significantly lower than that in the comparison group (
Our work had strengths and weaknesses. First, it was essential for us to conduct these studies because few studies in this area have been conducted. As such, there is a lack of published results concerning the safety and effectiveness of vision correction via the Femto-LASIK procedure in patients after undergoing DALK. Another strength of our study was the 24-month observation period after the vision correction procedure had been performed. However, our analysis was limited to a single center in Poland, which is partly attributable to the lack of specialist facilities and ophthalmologists specializing in vision correction procedures via the Femto-LASIK procedure in the country. Clearly, the findings of our study would be of greater value if more patients had been eligible for inclusion. Thus, in future studies, we plan to include a larger number of patients, which is feasible given the prospective nature of the present study. Despite our study’s limitations and the need for further research, our results remain cognitively and clinically significant.
Conclusions
Our 24-month observation period of the effects of vision correction via the Femto-LASIK procedure in patients after having undergone DALK showed that this method is safe and effective for these patients.
Figures
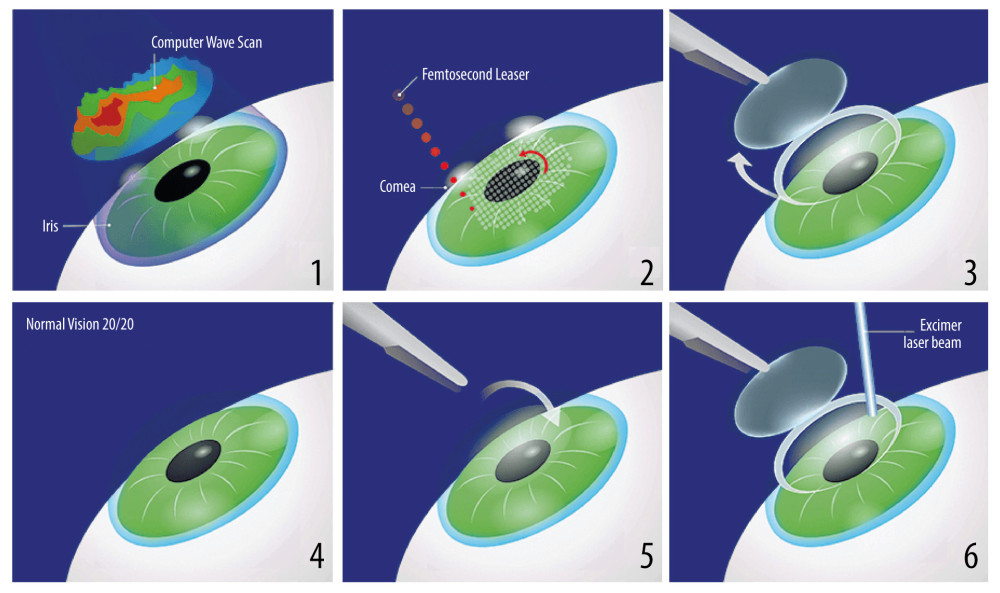 Figure 1. Stages of the deep anterior lamellar keratoplasty (DALK) surgical procedure. (1) Hesburg-Baron vacuum trepan applied to the center of the cornea; (2) cornea incised to a depth of 80% of the corneal dermis; (3) 27G needle bent at a 30° angle before insertion into the corneal dermis; (4) corneal dermis dissected with air; (5) Descemet’s membrane dissected; (6) patient’s eye after completed anterior layered corneal transplantation.
Figure 1. Stages of the deep anterior lamellar keratoplasty (DALK) surgical procedure. (1) Hesburg-Baron vacuum trepan applied to the center of the cornea; (2) cornea incised to a depth of 80% of the corneal dermis; (3) 27G needle bent at a 30° angle before insertion into the corneal dermis; (4) corneal dermis dissected with air; (5) Descemet’s membrane dissected; (6) patient’s eye after completed anterior layered corneal transplantation. 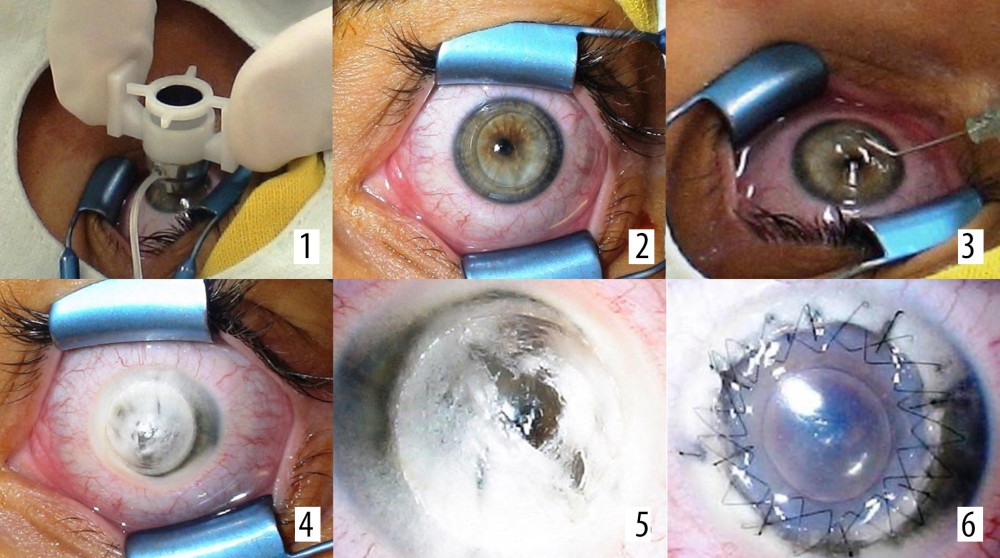 Figure 2. (1–6) Stages of the Femto-LASIK procedure.
Figure 2. (1–6) Stages of the Femto-LASIK procedure. 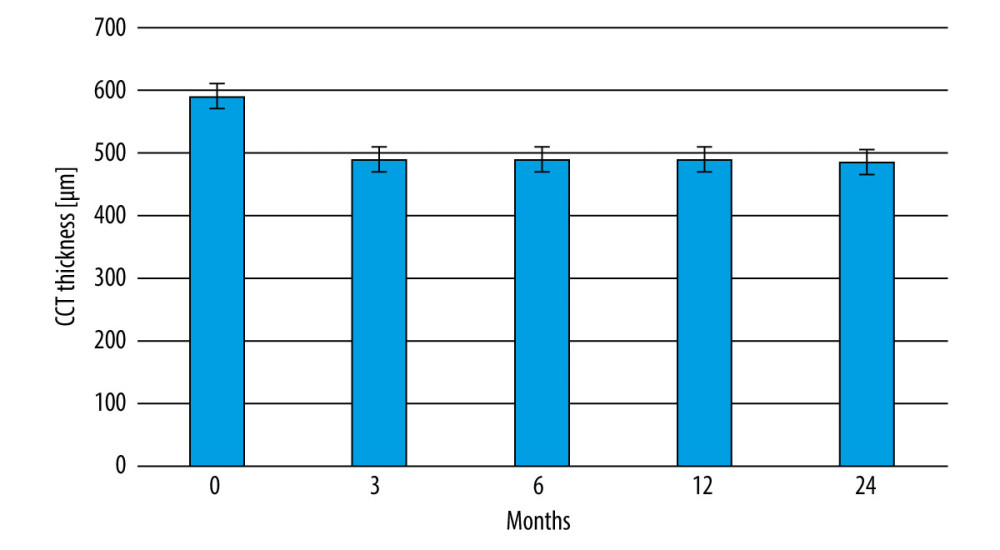 Figure 3. Changes in central corneal thickness before and after the Femto-LASIK procedure in the study group.
Figure 3. Changes in central corneal thickness before and after the Femto-LASIK procedure in the study group. Tables
Table 1. Local treatment for 7 days during hospital stay after deep anterior lamellar keratoplasty (DALK) surgery.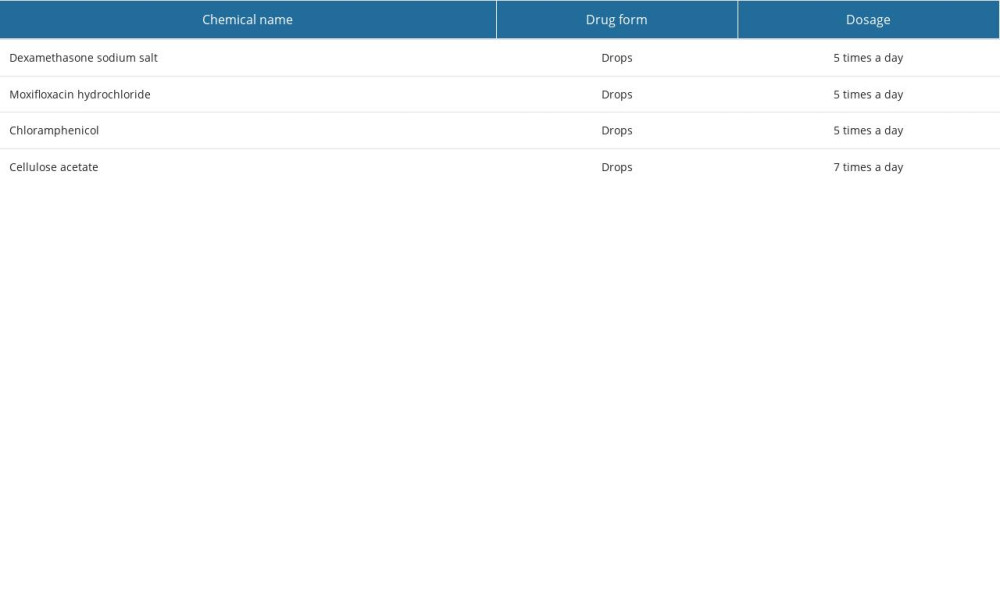 Table 2. Topical and general treatment scheme after deep anterior lamellar keratoplasty (DALK).
Table 2. Topical and general treatment scheme after deep anterior lamellar keratoplasty (DALK).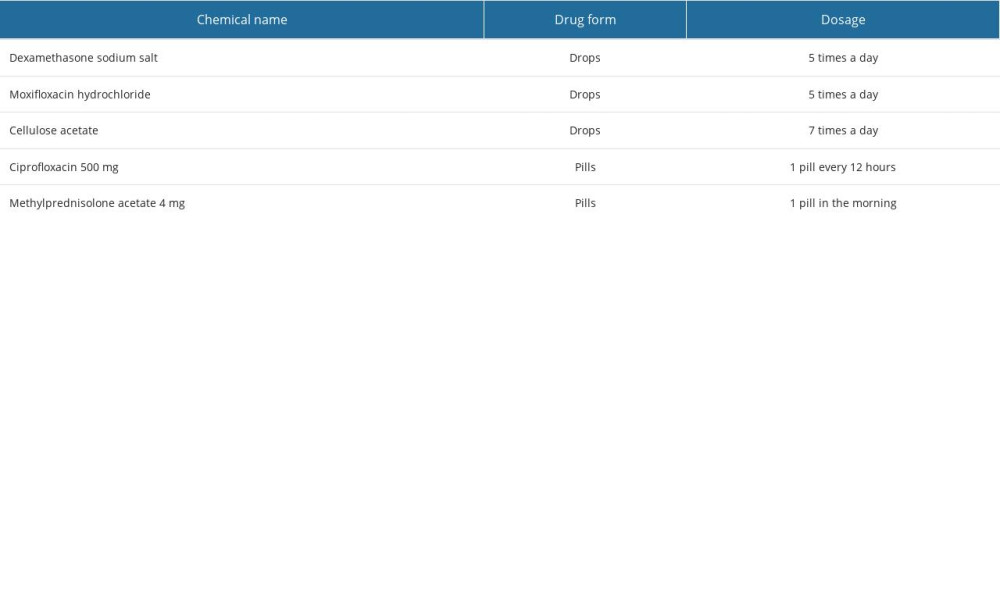 Table 3. Changes in the UCVA and BCVA values in patients of the study and comparison groups before and after Femto-LASIK procedure.
Table 3. Changes in the UCVA and BCVA values in patients of the study and comparison groups before and after Femto-LASIK procedure.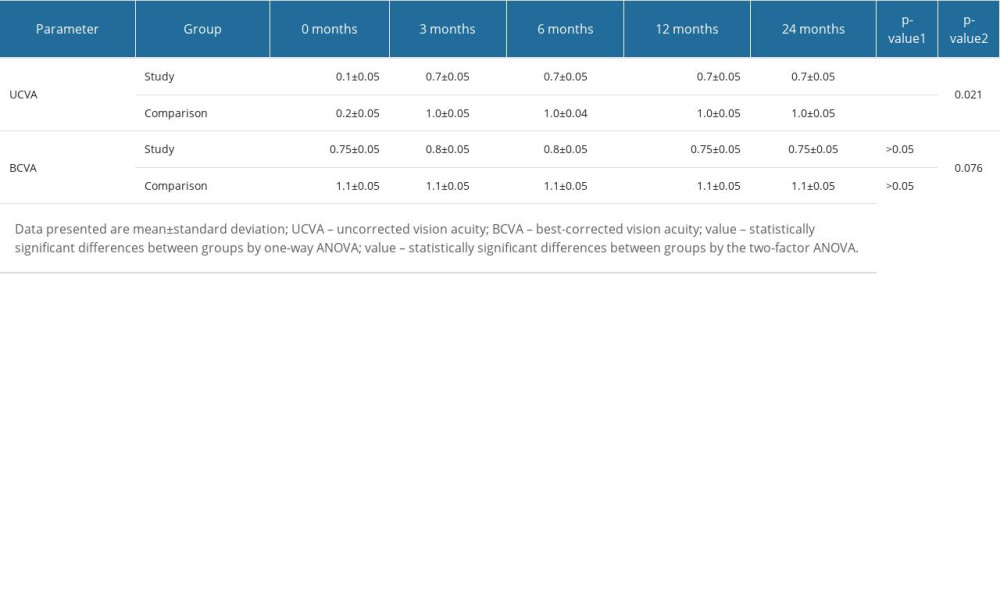 Table 4. Changes in the value of intraocular pressure of the study and comparative groups before and after the Femto-LASIK procedure.
Table 4. Changes in the value of intraocular pressure of the study and comparative groups before and after the Femto-LASIK procedure.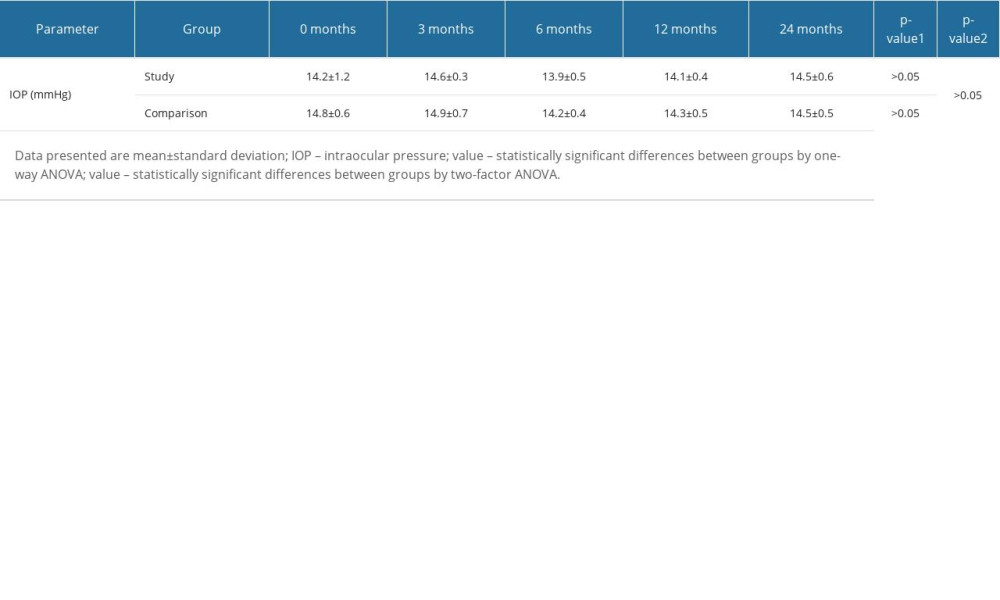 Table 5. Changes in corneal endothelial cell density in the study and comparison groups before and after the Femto-LASIK procedure.
Table 5. Changes in corneal endothelial cell density in the study and comparison groups before and after the Femto-LASIK procedure.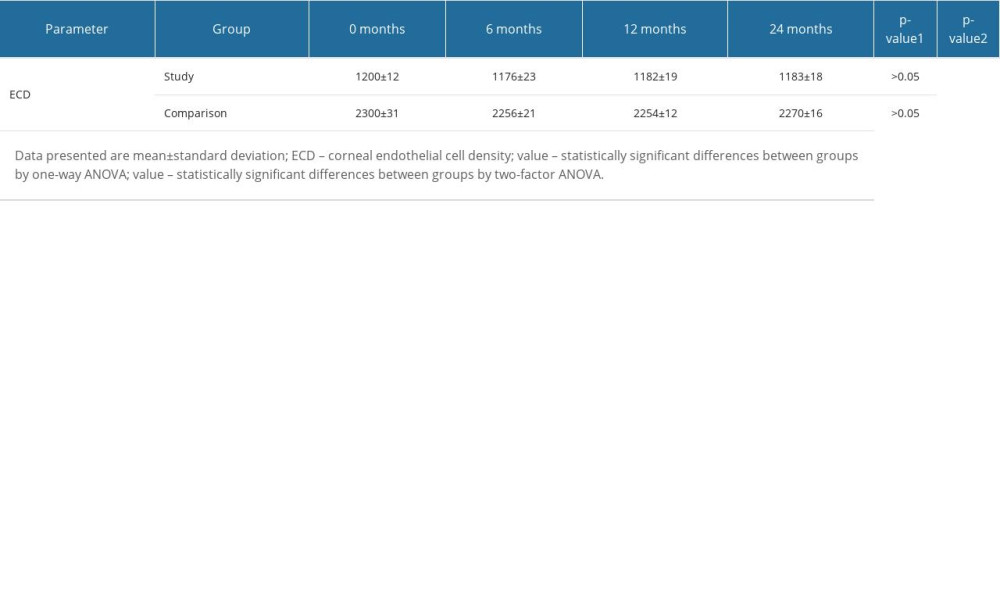
References
1. Mathews PM, Lindsley K, Aldave AJ, Akpek EK, Etiology of global corneal blindness and current practices of corneal transplantation: A focused review: Cornea, 2018; 37(9); 1198-203
2. Porth JM, Deiotte E, Dunn M, Bashshur R, A review of the literature on the global epidemiology of corneal blindness: Cornea, 2019; 38(12); 1602-9
3. Tran TM, Duong H, Bonnet C, Kashanchi A, Corneal blindness in Asia: A systematic review and meta-analysis to identify challenges and opportunities: Cornea, 2020; 39(9); 1196-205
4. Prost M, Rymgayłło-Jankowska B, Treatment of conjunctivitis: OphthaTher Ther Ophthalm, 2021; 8(4); 249-52
5. Riza NA, Amin MJ, Riza MN, Eye vision testing system and eyewear using micromachines: Micromachines, 2015; 6(11); 1690-709
6. Jones RM, Bleasdale SC, Maita D, A systematic risk-based strategy to select personal protective equipment for infectious diseases: Am J Infect Control, 2020; 48(1); 46-51
7. Moreddu R, Vigolo D, Yetisen AK, Contact lens technology: From fundamentals to applications: Adv Healthc Mater, 2019; 8(15); 1900368
8. Musgrave CSA, Fang F, Contact lens materials: A materials science perspective: Materials, 2019; 12(2); 261
9. Chen J, Mi L, Chen CP, Liu H, Design of foveated contact lens display for augmented reality: Opt Express, 2019; 27(26); 38204-19
10. Mutlu Z, Shams Es-haghi S, Cakmak M, Recent trends in advanced contact lenses: Adv Healthc Mater, 2019; 8(10); 1801390
11. Ang M, Gatinel D, Reinstein DZ, Refractive surgery beyond 2020: Eye, 2021; 35(2); 362-82
12. Joffe SN: Clin Ophthalmol, 2021; 15; 1163
13. Lim EWL, Lim L, Review of laser vision correction (LASIK, PRK and SMILE) with simultaneous accelerated corneal crosslinking-long-term results: Curr Eye Res, 2019; 44(11); 1171-80
14. Siddiqui AA, Dubey AK, Recent trends in laser cladding and surface alloying: Opt Laser Technol, 2021; 134; 106619
15. Miraftab M, Hashemi H, Aghamirsalim M, Matched comparison of corneal higher order aberrations induced by SMILE to femtosecond assisted LASIK and to PRK in correcting moderate and high myopia: 3.00 mm vs. 6.00 mm: BMC Ophthalmol, 2021; 21(1); 216
16. Shah R, History and results; Indications and contraindications of SMILE compared with LASIK: Asia Pac J Ophthalmol (Phila), 2019; 8(5); 371
17. Breyer DR, Beckers L, Hagen P, Comparison of long-term results with small incision refractive Lenticule extraction (ReLEX SMILE) vs. Femto-LASIK: Klin Monbl Augenheilkd, 2019; 236(10); 1201-7
18. Mihai C, Ivana TO, Tataru CP, The assessment of postprocedure results in the case of patients operated on using the femtolasik method with the Alcon/Wavelight FS00 Femto & EX500 Excimer Refractive Suite: Res Sci Today, 2014; 7; 132
19. Pavkova Z, Kacerovska J, Kacerovsky M, Comparison of the efficiency of femtoLASIK and ReLEx SMILE in terms of dioptric error reduction: Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub, 2018 [Online ahead of print]
20. Lan G, Zeng J, Li W, Customized eye modeling for optical quality assessment in myopic femto-LASIK surgery: Sci Rep, 2021; 11(1); 16049
21. Bashir ZS, Ali MH, Anwar A, Femto-lasik: The recent innovation in laser assisted refractive surgery: J Pak Med Assoc, 2017; 67(4); 609-15
22. Tomczak M, Chomicka A, Dmitriew A, Dry eye syndrome in the postoperative period after laser vision correction: OphthaTher, 2021; 8(1); 66-70
23. Pazo EE, Huang H, Fan Q, Intense pulse light for treating post-LASIK refractory dry eye: Photobiomodul Photomed Laser Surg, 2021; 39(3); 155-63
24. Yalçınkaya G, Yıldız BK, Çakır İ, Evaluation of peripapillary-macular microvascularity and choroidal vascularity index after refractive surgery: Photodiagnosis Photodyn Ther, 2022; 37; 102714
25. Pasha H, Palazzolo L, Prakash G, Jhanji V, Update on corneal collagen crosslinking for ectasia: Curr Opin Ophthalmol, 2021; 32(4); 343-47
26. Joo J, Kim B, Chun H, Application of computational modeling to improve cornea transplant surgery: J Korean Phys Soc, 2021; 79(9); 874-81
27. Singh R, Gupta N, Vanathi M, Tandon R, Corneal transplantation in the modern era: Indian J Med Res, 2019; 150(1); 7
28. Armitage WJ, Goodchild C, Griffin MD, High-risk corneal transplantation: Recent developments and future possibilities: Transplant, 2019; 103(12); 2468
29. Hori J, Yamaguchi T, Keino H, Immune privilege in corneal transplantation: Prog Retin Eye Res, 2019; 72; 100758
30. Anshu A, Li L, Htoon HM, Long-term review of penetrating keratoplasty: A 20-year review in Asian eyes: Am J Ophthalmol, 2021; 224; 254-66
31. Wu J, Wu T, Li J, DSAEK or DMEK for failed penetrating keratoplasty: A systematic review and single-arm meta-analysis: Int Ophthalmol, 2021; 41(7); 2315-28
32. Song Y, Zhang J, Pan Z, Systematic review and meta-analysis of clinical outcomes of penetrating keratoplasty versus deep anterior lamellar keratoplasty for keratoconus: Exp Clin Transplant, 2020; 18(4); 417-28
33. Alfonso-Bartolozzi B, Martínez-Alberquilla I, Baamonde B, Refractive surgery after deep anterior lamellar keratoplasty: A review of the literature: Int Ophthalmol, 2022 [Online ahead of print]
34. Alio JL, Editorial: Regenerative surgery of the cornea: Front Med, 2022; 9; 1099876
35. Ghoreishi M, Naderi Beni A, Naderi Beni Z, Visual outcomes of Femto-LASIK for correction of residual refractive error after corneal graft: Graefes Arch Clin Exp Ophthalmol, 2013; 251(11); 2601-8
36. Alfonso-Bartolozzi B, Lisa C, Fernández-Vega-Cueto L, Femto-LASIK after deep anterior lamellar keratoplasty to correct residual astigmatism: A long-term case series study: Medicina, 2022; 58(8); 1036
37. Hecht I, Achiron A, Ben Haim L, Refractive surgery in the late adulthood and adolescent age groups: Graefes Arch Clin Exp Ophthalmol, 2019; 257(9); 2057-63
38. Wierzbowska J, Smorawski M, Uram D, Individualizing approach to management of refractive errors: OphthaTher, 2021; 8(1); 58-64
39. Chean CS, Yong BKA, Comely S, Refractive outcomes following cataract surgery in patients who have had myopic laser vision correction: BMJ Open Ophthalmol, 2019; 4(1); e000242
40. Smith LF, Stevens JD, Larkin F, Restori M, Errors leading to unexpected pseudophakic ametropia: Eye, 2001; 15(6); 728-32
41. Guccione L, Mosca L, Scartozzi L, Correction of refractive errors after corneal transplantation: Vision correction and eye surgery, 2022
42. Chuprov AD, Mal’gin KV, Correction of corneal astigmatism during single-step phacoemulsification: Femtolaser archuat incisions and implantation of toric intraocular lenses: Russian Military Medical Academy Reports, 2018; 37(2); 88-91
43. Klokova OA, Sakhnov SN, Geydenrikh MS, Damashauskas RO, Quality of life after refractive surgery: ReLEx SMILE vs Femto-LASIK: Clin Ophthalmol, 2019; 13; 561-70
44. Hemida AY, Said OM, Abdel-Meguid AAE, Changes in corneal biomechanics and intraocular pressure following Femto-LASIK using Goldman applanation tonometry and ocular response analyzer: Int J Ophthalmol, 2020; 13(5); 782-87
45. Pateras E, Kontogeorgou E: Ophthalmology Research: An International Journal, 2020; 13(3); 20-27
46. Denoyer A, Landman E, Trinh L, Dry eye disease after refractive surgery: Comparative outcomes of small incision lenticule extraction versus LASIK: Ophthalmol, 2015; 122(4); 669-76
47. Ambroziak AM, Wpływ chirurgii refrakcyjnej na zespół suchego oka: Optyka, 2019; 6; 52 [in Polish]
48. Guo H, Hosseini-Moghaddam SM, Hodge W, Corneal biomechanical properties after SMILE versus FLEX, LASIK, LASEK, or PRK: A systematic review and meta-analysis: BMC Ophthalmol, 2019; 19(1); 167
49. Holland EJ, Darvish M, Nichols KK, Efficacy of topical ophthalmic drugs in the treatment of dry eye disease: A systematic literature review: Ocul Surf, 2019; 17(3); 412-23
50. Wolniewińska M, Czarnota-Nowakowska B, Wolniewińska J, SMILE – charakterystyka zabiegu i jakość życia pacjentów: Ophthatherapy, 2021; 8(2); 133-41 [in Polish]
51. Fernández-Vega-Cueto L, Lisa C, Naveiras M, FemtoLASIK after descemet membrane endothelial keratoplasty: Cornea, 2020; 39(4); 468-72
52. Bang SP, Yoo YS, Jun JH, Joo CK, Effects of residual anterior lens epithelial cell removal on axial position of intraocular lens after cataract surgery: J Ophthalmol, 2018; 2018; 9704892
53. Joyce NC, Cell cycle status in human corneal endothelium: Exp Eye Res, 2005; 81(6); 629-38
Figures
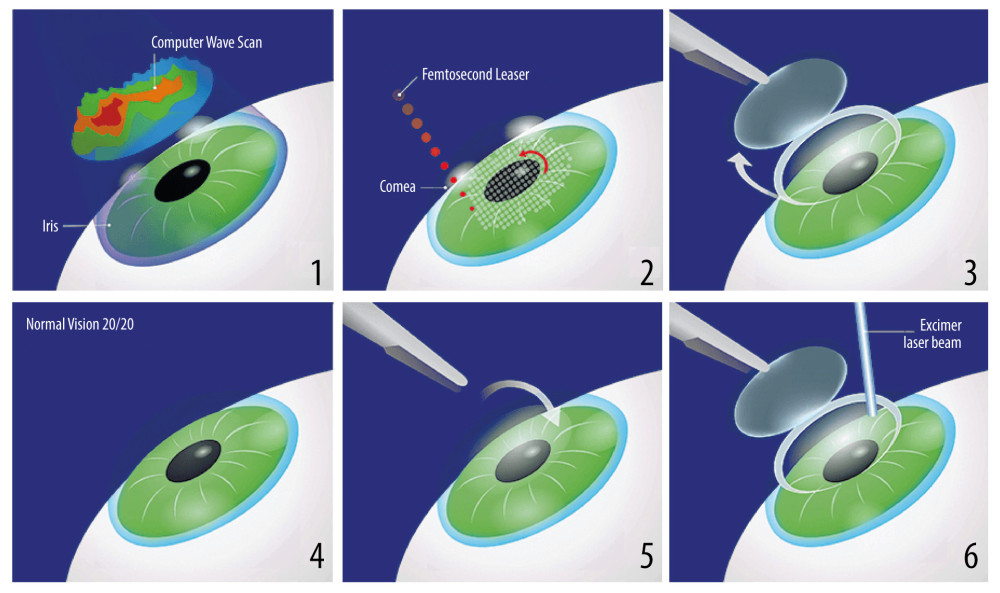 Figure 1. Stages of the deep anterior lamellar keratoplasty (DALK) surgical procedure. (1) Hesburg-Baron vacuum trepan applied to the center of the cornea; (2) cornea incised to a depth of 80% of the corneal dermis; (3) 27G needle bent at a 30° angle before insertion into the corneal dermis; (4) corneal dermis dissected with air; (5) Descemet’s membrane dissected; (6) patient’s eye after completed anterior layered corneal transplantation.
Figure 1. Stages of the deep anterior lamellar keratoplasty (DALK) surgical procedure. (1) Hesburg-Baron vacuum trepan applied to the center of the cornea; (2) cornea incised to a depth of 80% of the corneal dermis; (3) 27G needle bent at a 30° angle before insertion into the corneal dermis; (4) corneal dermis dissected with air; (5) Descemet’s membrane dissected; (6) patient’s eye after completed anterior layered corneal transplantation.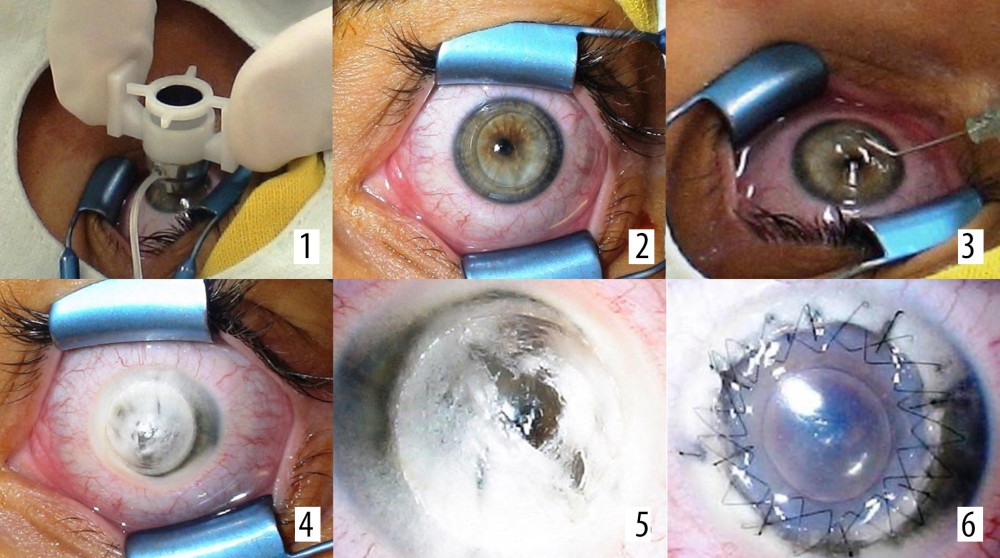 Figure 2. (1–6) Stages of the Femto-LASIK procedure.
Figure 2. (1–6) Stages of the Femto-LASIK procedure.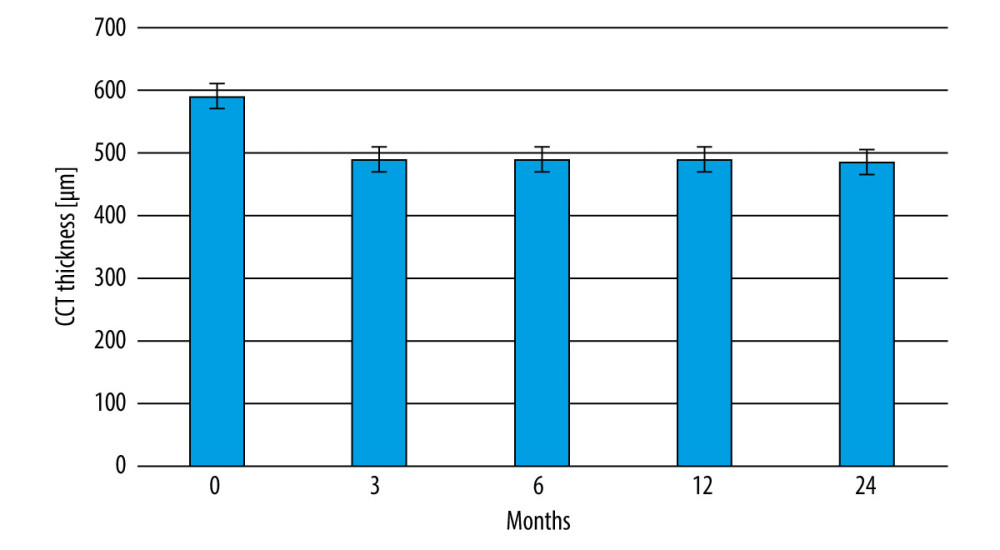 Figure 3. Changes in central corneal thickness before and after the Femto-LASIK procedure in the study group.
Figure 3. Changes in central corneal thickness before and after the Femto-LASIK procedure in the study group. Tables
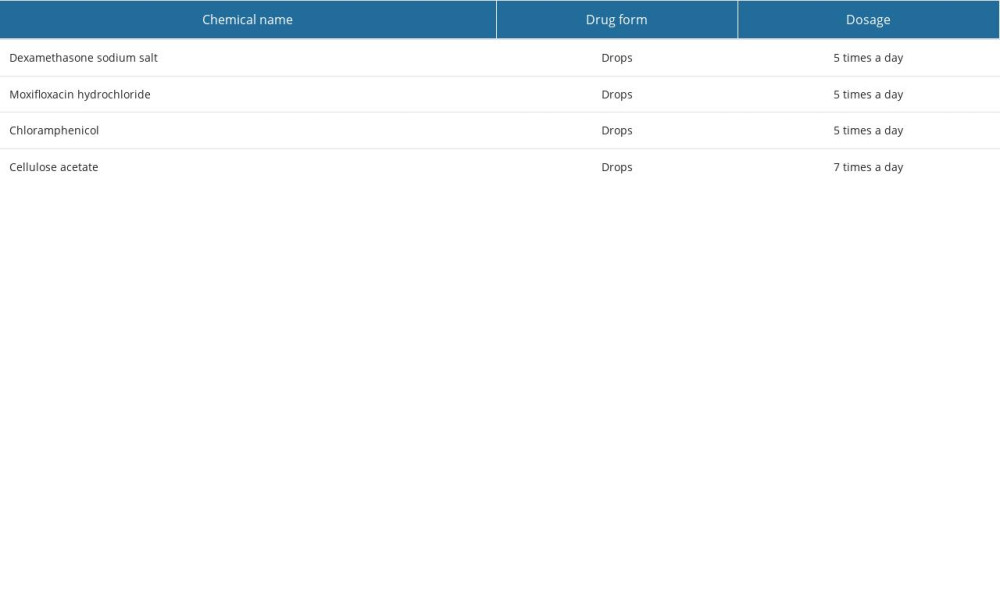 Table 1. Local treatment for 7 days during hospital stay after deep anterior lamellar keratoplasty (DALK) surgery.
Table 1. Local treatment for 7 days during hospital stay after deep anterior lamellar keratoplasty (DALK) surgery.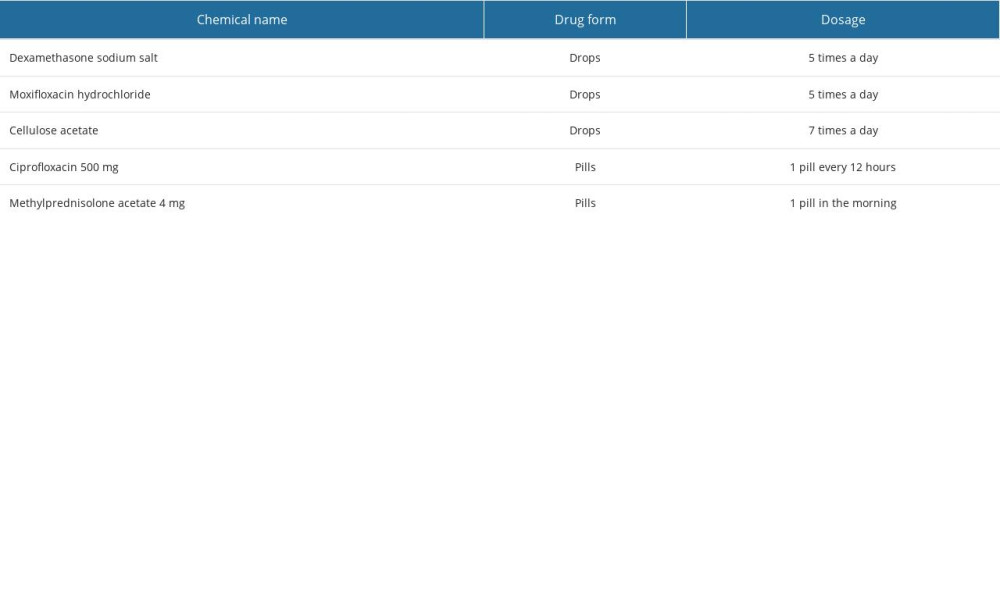 Table 2. Topical and general treatment scheme after deep anterior lamellar keratoplasty (DALK).
Table 2. Topical and general treatment scheme after deep anterior lamellar keratoplasty (DALK).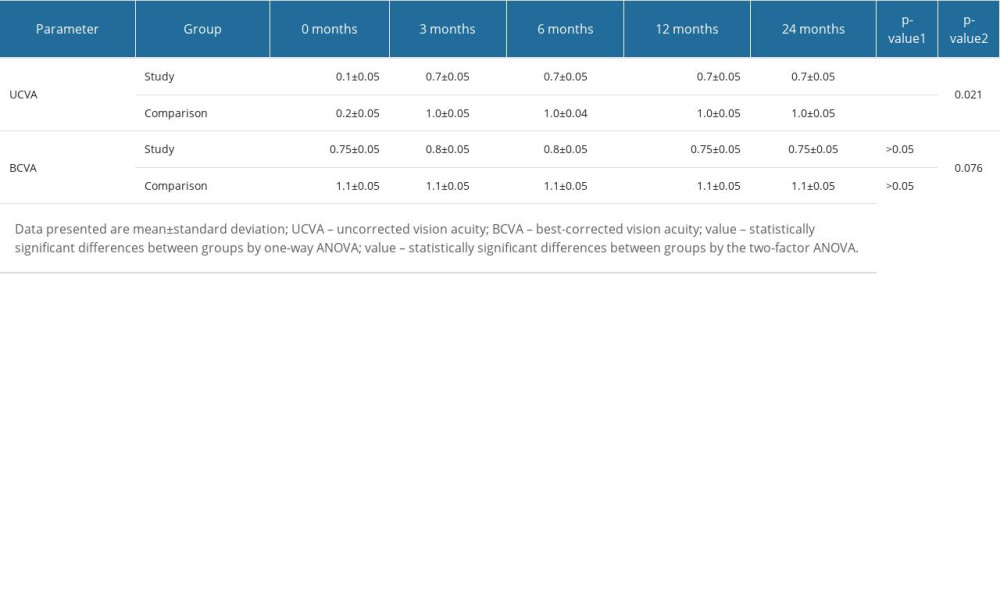 Table 3. Changes in the UCVA and BCVA values in patients of the study and comparison groups before and after Femto-LASIK procedure.
Table 3. Changes in the UCVA and BCVA values in patients of the study and comparison groups before and after Femto-LASIK procedure.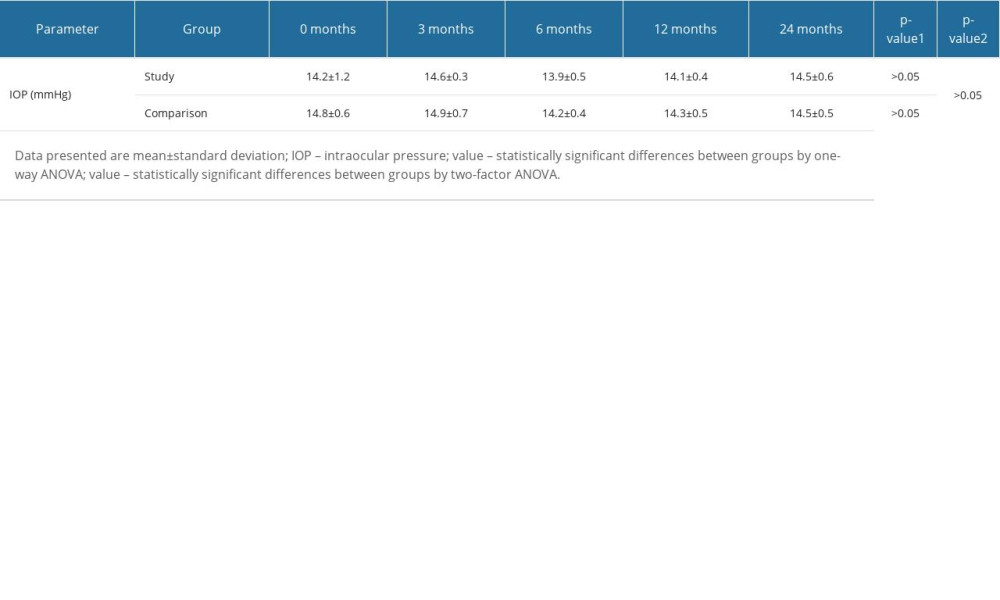 Table 4. Changes in the value of intraocular pressure of the study and comparative groups before and after the Femto-LASIK procedure.
Table 4. Changes in the value of intraocular pressure of the study and comparative groups before and after the Femto-LASIK procedure.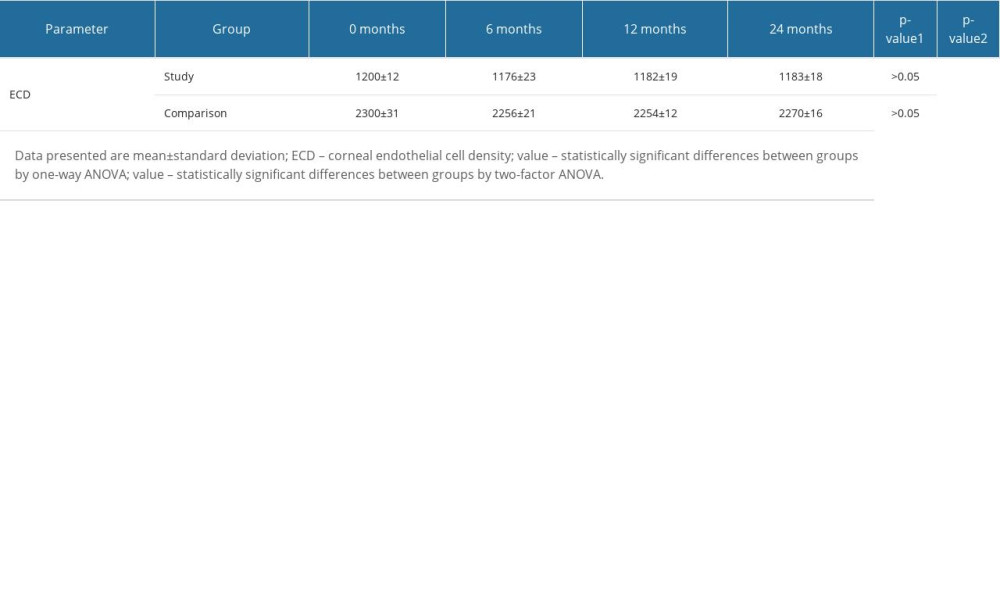 Table 5. Changes in corneal endothelial cell density in the study and comparison groups before and after the Femto-LASIK procedure.
Table 5. Changes in corneal endothelial cell density in the study and comparison groups before and after the Femto-LASIK procedure.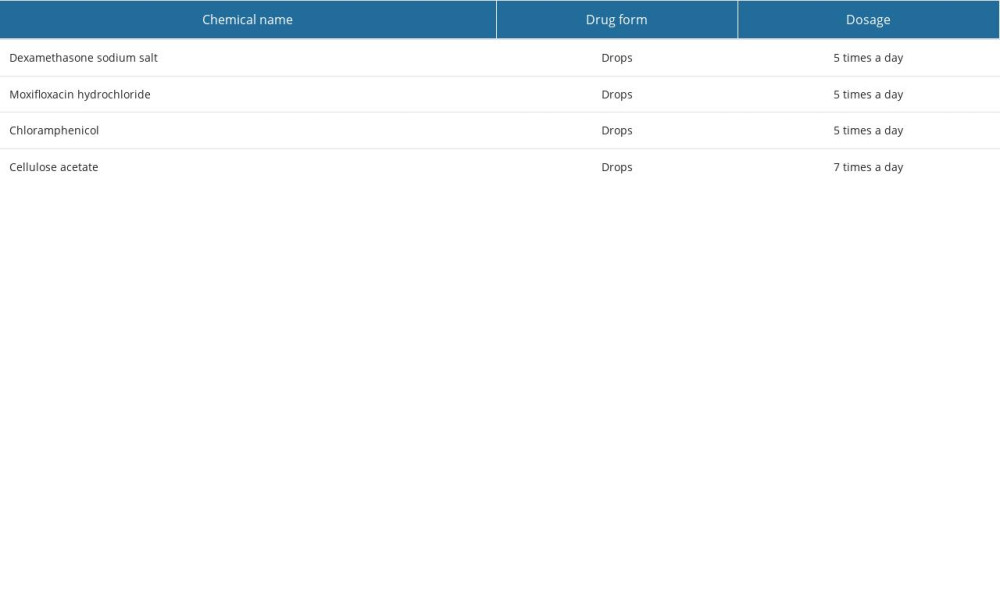 Table 1. Local treatment for 7 days during hospital stay after deep anterior lamellar keratoplasty (DALK) surgery.
Table 1. Local treatment for 7 days during hospital stay after deep anterior lamellar keratoplasty (DALK) surgery.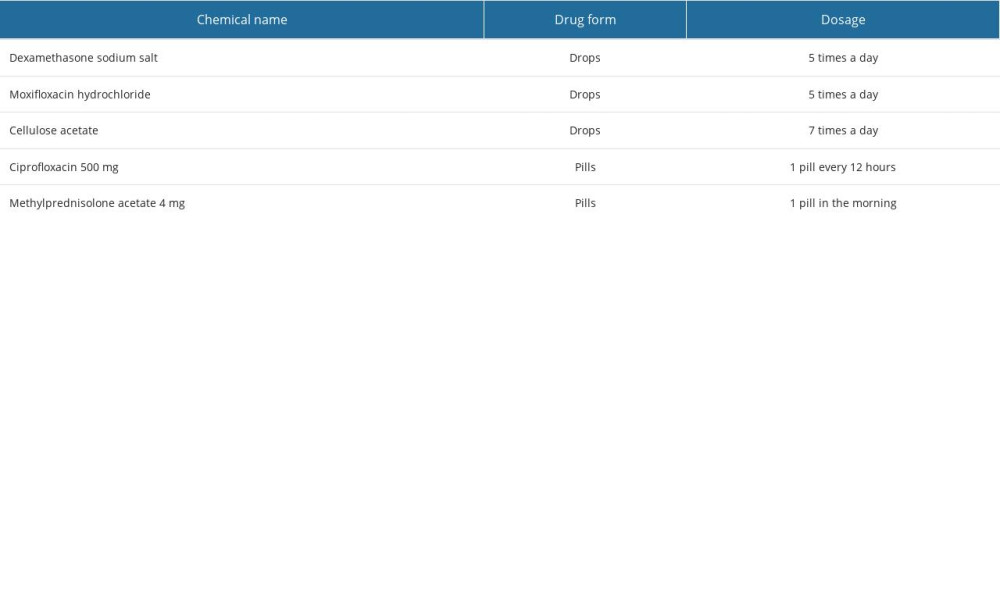 Table 2. Topical and general treatment scheme after deep anterior lamellar keratoplasty (DALK).
Table 2. Topical and general treatment scheme after deep anterior lamellar keratoplasty (DALK).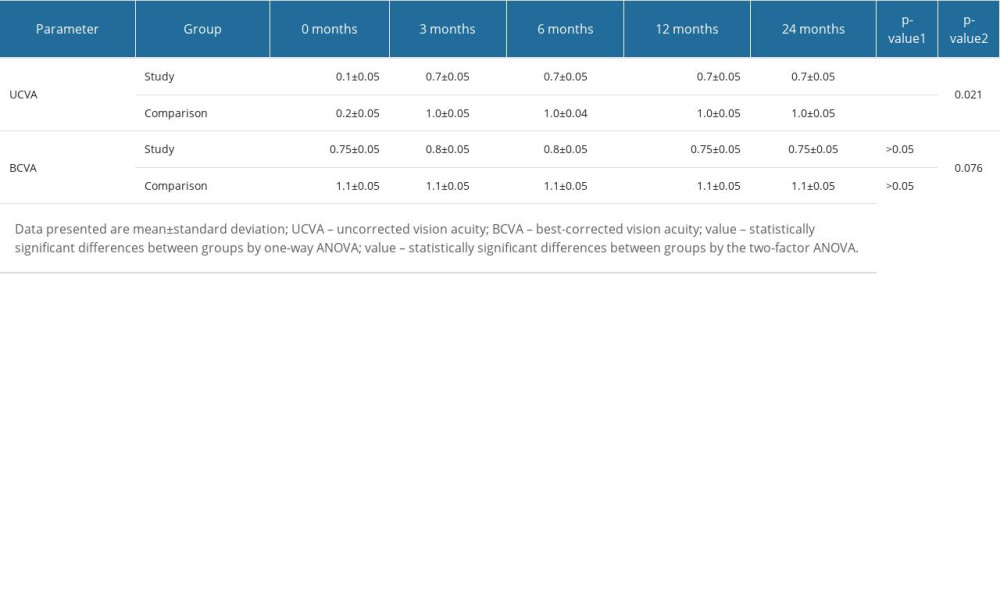 Table 3. Changes in the UCVA and BCVA values in patients of the study and comparison groups before and after Femto-LASIK procedure.
Table 3. Changes in the UCVA and BCVA values in patients of the study and comparison groups before and after Femto-LASIK procedure.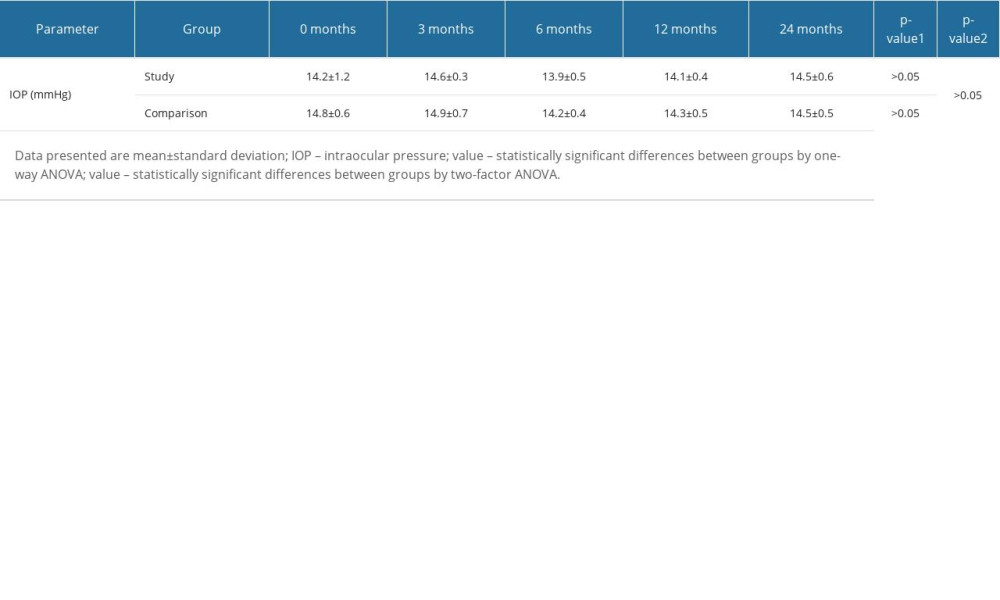 Table 4. Changes in the value of intraocular pressure of the study and comparative groups before and after the Femto-LASIK procedure.
Table 4. Changes in the value of intraocular pressure of the study and comparative groups before and after the Femto-LASIK procedure.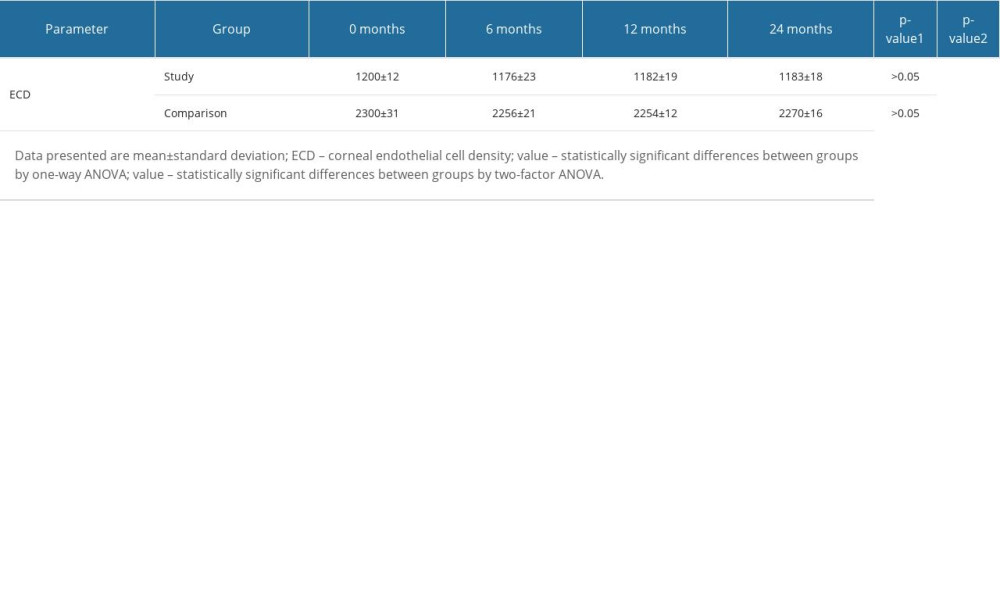 Table 5. Changes in corneal endothelial cell density in the study and comparison groups before and after the Femto-LASIK procedure.
Table 5. Changes in corneal endothelial cell density in the study and comparison groups before and after the Femto-LASIK procedure. In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








