20 May 2023: Clinical Research
Association Among Complete Blood Count Parameters, Bone Mineral Density, and Cobb Angle in Cases of Adolescent Idiopathic Scoliosis
Mehmet Murat BalaDOI: 10.12659/MSM.940355
Med Sci Monit 2023; 29:e940355
Abstract
BACKGROUND: Improving the quality of life of scoliosis patients with appropriate preventive measures is critical. This study aimed to investigate the relationships among bone mass, Cobb angle, and complete blood count (CBC) parameters in patients with scoliosis.
MATERIAL AND METHODS: This joint study was conducted by the pediatric department and orthopedics clinics, which used the medical records of patients aged 10-18 years between 2018 and 2022. Patients were divided into 3 groups according to the Cobb angle. Patient blood count levels from medical records and bone mineral density (BMD) Z scores (g/cm²) were compared among groups. Notably, BMD Z scores were calculated using a (BMD) dataset from local Turkish children after adjusting for height and age.
RESULTS: A total of 184 individuals (120 females, 64 males) were included in the study. There were statistically significant differences among the groups in platelet-to-lymphocyte ratio (PLR). Significant differences in DXA Z scores among groups were found. There was a significantly strong and positive correlation between DXA Z scores and all CBC parameters in patients with severe scoliosis.
CONCLUSIONS: This study found that CBC parameters can predict BMD in adolescents. Furthermore, the association between vitamin D deficiency and low BMD may contribute to the follow-up of body adaptation in patients with scoliosis receiving conservative treatment.
Keywords: Bone Density, Blood Cell Count, Scoliosis, Male, Child, Female, Humans, Adolescent, Quality of Life, Bone Diseases, Metabolic, Kyphosis
Background
Bone mineral density (BMD) has been increasingly investigated since the 1980s after 2 reports showed that children with adolescent idiopathic scoliosis (AIS) have lower bone mineral density than their peers [1–3]. Various studies have suggested an association between osteoporosis and scoliosis [2–7]. Notably, some studies have reported a significant association between scoliosis and osteopenia [2,6,8–15], and some studies have reported that scoliosis can even develop in adulthood [13]. Patients with osteopenia and AIS have been reported to have twice the risk of curve progression than those with normal BMD [16]. Because osteopenia poses a risk of curve progression and is thought to cause worsening scoliosis, it has been proposed as a potential prognostic factor [16,17].
Clonal hematopoiesis is a somatic mutation caused by various changes in the hematopoietic stem cells [18,19]. Any chronic inflammation in the body causes a suppression of erythropoiesis in the bone marrow and alters red blood cell heterogeneity [20]. Moreover, the inflammation directly or indirectly affects BMD and fracture risk [21].
Osteoimmunology has shown that the immune system and inflammatory factors play important roles in the development of osteoporosis [22]. Several studies of immune diseases have reported that monocyte-to-lymphocyte ratio (MLR) has diagnostic value and can reflect systemic inflammation and the severity of immune system damage [23]. Therefore, MLR has been recognized as a marker of inflammation [23]. Moreover, elevated MLR has been reported to be associated with osteoporosis and bone diseases [24,25].
Notably, neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR), which are novel markers of systemic inflammatory response [26,27], have also been found to be associated with low BMD [28,29].
Appropriate preventive measures are critical in preventing the development of scoliosis and improving the quality of life of patients [30,31]. The present study aimed to investigate the associations among bone mass, Cobb angle, and complete blood count (CBC) parameters in patients with scoliosis.
Material and Methods
EVALUATION OF SPINAL CURVATURE:
The Cobb angle between the most inclined vertebrae was calculated by a single experienced orthopedist using a standard full-spine posteroanterior radiograph [32]. Specifically, scoliosis was defined as the presence of a curvature of ≥10°. Moreover, AIS was confirmed using erect and bending radiographs. Other causes of scoliosis were excluded by examination and investigations at the pediatric endocrinology clinic.
The 2016 Scientific Society on Scoliosis Orthopaedic and Rehabilitation Treatment guidelines define mild and moderate scoliosis as a Cobb angle of <20° and 21–35°, respectively [33,34]. In this study, patients were divided into 3 groups according to the Cobb angle: less than 10 degrees (control group), 10–20 degrees, and over 20 degrees.
DATA COLLECTION:
Demographic data of the patients were extracted from electronic medical records, and based on these data, calcium (CA), phosphorus (P), 25-hydroxyvitamin D (25-OH-D3), alkaline phosphatase (ALP), parathyroid hormone (PTH), NLR, MLR, and PLR were calculated.
Complete blood counts were obtained using an automated hematology analyzer (Abbott, Cell-Dyn Ruby, IL, USA). Moreover, biochemical parameters were measured using a clinical chemistry analyzer (Abbott, c16000, IL, USA). In addition, hormone parameters were measured using chemiluminescence immunoassay (Abbott, i2000sr, IL, USA). MLR, NLR, and PLR were calculated using monocyte count/lymphocyte count, neutrophil count/lymphocyte count, and platelet count/lymphocyte count, respectively.
BONE MINERAL DENSITY MEASUREMENTS:
The T score indicates how much a person’s bone mass differs from the bone mass of an average healthy 30-year-old adult. In contrast, the Z score refers to standard deviations based on a comparison of a child’s BMD to the mean BMD of a standard population of the same sex and age [35]. When calculating age- and sex-adjusted Z scores, DXA measures the density of different bones in the body; however, the lumbar spine (L1–L4) and femoral neck are most commonly used [36]. In the present study, Z scores were obtained for the spine using BMD (g/cm2) from DXA scans. BMD Z scores were calculated using the BMD dataset of local Turkish children after adjustment for height and age [37,38]. All DXA procedures were performed using Lunar Prodigy (General Electric, GE Healthcare, Lunar DPX, NT+150301, USA) at a single institution.
STATISTICAL ANALYSIS:
Descriptive data are presented as number (percentages) or median and interquartile ranges (IQR: 25th–75th percentiles), according to data distribution. The normality of continuous variables was assessed with the Shapiro-Wilk test and histogram plots. Kruskal-Wallis and post hoc Dunn’s tests were used for the comparison of continuous variables among groups. Pearson correlation analysis was conducted to assess the relationship between DXA Z scores and hemogram parameters. The analyses were performed using SPSS 26.0 for Windows (SPSS, Inc., Chicago, Illinois, USA) and R 4.2.1 statistical software. The results were considered to be significant at a level of
Results
A total of 184 individuals (120 females, 64 males) were included in the study. The median age of participants was 14 (IQR: 12–16) years. The comparison of hemogram parameters among the control group with no scoliosis (n=96), patients with mild scoliosis (n=72), and patients with moderate scoliosis (n=16) is presented in Table 1. There were statistically significant differences among the groups in terms of PLR (
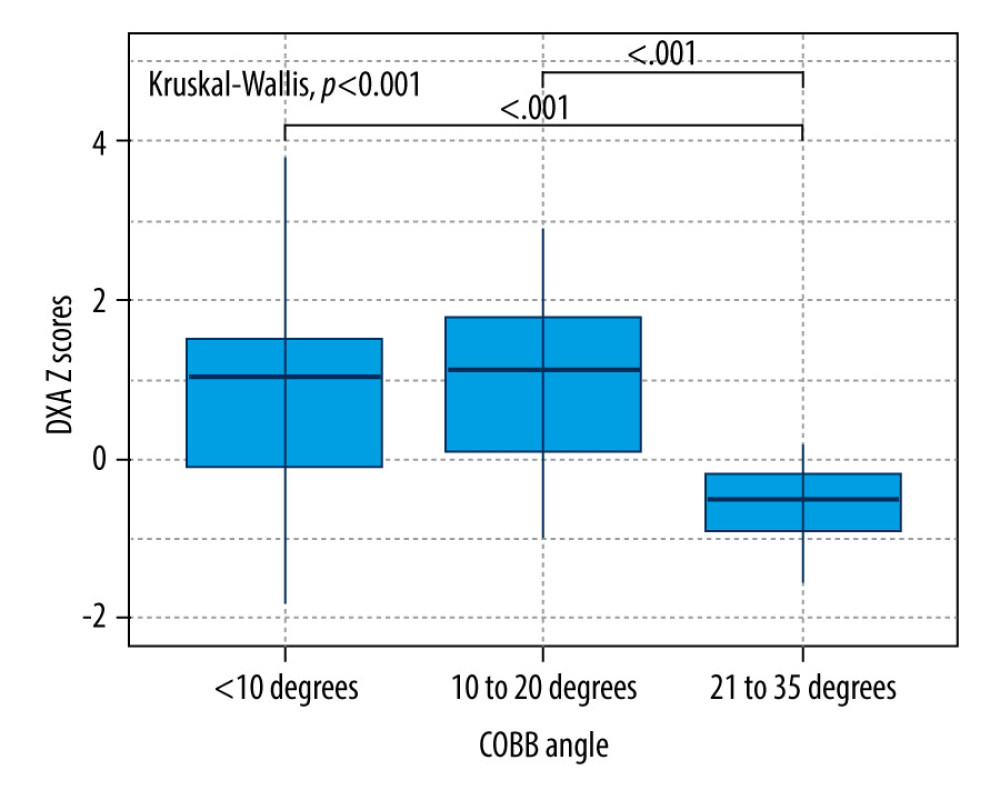
The distribution of DXA Z scores among groups are displayed in Figure 1. Significant differences in terms of DXA Z scores among groups were found (
Correlations between DXA Z scores and hemogram parameters were evaluated separately for groups (Table 2). There was no significant correlation between DXA Z score and hemogram parameters in the control group. In the patients with mild scoliosis, a significant weak positive correlation was found between DXA Z Score and PLR (0.324,
Other serum blood parameters were compared among groups in Table 3. Significant differences were found in 25-OH-D3 (
Discussion
STUDY LIMITATIONS:
This study has some limitations. First, this was a single-center study and included a small number of patients. Longitudinal and molecular biology studies may be required to obtain clearer results. Second, BMD measured using DXA can be confusing because bone growth is three-dimensional and uneven [35,59]. Third, bone microarchitecture, particularly that of trabecular bone, is another critical mechanical quality of bone; however, our study performed a comprehensive and systemic study of BMD but failed to assess trabecular bone microarchitecture. In addition, although physical activity has an effect on bone health, the fact that patients were not classified according to their physical activities is another limitation of our study [60]. Nonetheless, this study used a heterogeneous patient population and attempted to identify the factors that best correlated with low BMD and high Cobb angle.
Conclusions
To the best of our knowledge, this is the first study to provide evidence of an association of PLR with the Cobb angle in patients with AIS. Moreover, this study reported that CBC parameters play a predictive role for BMD in adolescent. Furthermore, the association between vitamin D deficiency and low BMD may contribute to the follow-up of body adaptation in patients with scoliosis receiving conservative treatment.
References
1. Bartal E, Gage JR, Idiopathic juvenile osteoporosis and scoliosis: J Pediatr Orthop, 1982; 2(3); 295-98
2. Burner WL, Badger VM, Sherman FC, Osteoporosis and acquired back deformities: J Pediatr Orthop, 1982; 2(4); 383-85
3. Dede O, Akel I, Demirkiran G, Is decreased bone mineral density associated with development of scoliosis? A bipedal osteopenic rat model: Scoliosis, 2011; 6(1); 24
4. Healey JH, Lane JM, Structural scoliosis in osteoporotic women: Clin Orthop Relat Res, 1985(195); 216-23
5. Thevenon A, Pollez B, Cantegrit F, Relationship between kyphosis, scoliosis, and osteoporosis in the elderly population: Spine (Phila Pa 1976), 1987; 12(8); 744-45
6. Cheng JC, Guo X, Osteopenia in adolescent idiopathic scoliosis. A primary problem or secondary to the spinal deformity?: Spine (Phila Pa 1976), 1997; 22(15); 1716-21
7. Pappou IP, Girardi FP, Sandhu HS, Discordantly high spinal bone mineral density values in patients with adult lumbar scoliosis: Spine (Phila Pa 1976), 2006; 31(14); 1614-20
8. Cook SD, Harding AF, Morgan EL, Trabecular bone mineral density in idiopathic scoliosis: J Pediatr Orthop, 1987; 7(2); 168-74
9. Chen H, Zhang J, Wang Y, Abnormal lacuno-canalicular network and negative correlation between serum osteocalcin and Cobb angle indicate abnormal osteocyte function in adolescent idiopathic scoliosis: FASEB J, 2019; 33(12); 13882-92
10. Diarbakerli E, Savvides P, Wihlborg A, Bone health in adolescents with idiopathic scoliosis: Bone Joint J, 2020; 102-B(2); 268-72
11. Ito M, Ohki M, Hayashi K, Trabecular texture analysis of CT images in the relationship with spinal fracture: Radiology, 1995; 194(1); 55-59
12. Jiang Y, Zhao J, White DL, Genant HK, Micro CT and micro MR imaging of 3D architecture of animal skeleton: J Musculoskelet Neuronal Interact, 2000; 1(1); 45-51
13. Cheng JC, Qin L, Cheung CS, Generalized low areal and volumetric bone mineral density in adolescent idiopathic scoliosis: J Bone Miner Res, 2000; 15(8); 1587-95
14. Roach JW, Adolescent idiopathic scoliosis: Orthop Clin North Am, 1999; 30(3); 353-65
15. Zhu F, Qiu Y, Yeung HY, Trabecular bone micro-architecture and bone mineral density in adolescent idiopathic and congenital scoliosis: Orthop Surg, 2009; 1(1); 78-83
16. Yip BHK, Yu FWP, Wang Z, Prognostic value of bone mineral density on curve progression: A longitudinal cohort study of 513 girls with adolescent idiopathic scoliosis: Sci Rep, 2016; 6; 39220
17. Hung VWY, Qin L, Cheung CSK, Osteopenia: A new prognostic factor of curve progression in adolescent idiopathic scoliosis: J Bone Joint Surg Am, 2005; 87(12); 2709-16
18. Steensma DP, Clinical implications of clonal hematopoiesis: Mayo Clin Proc, 2018; 93(8); 1122-30
19. Jaiswal S, Fontanillas P, Flannick J, Age-related clonal hematopoiesis associated with adverse outcomes: N Engl J Med, 2014; 371(26); 2488-98
20. Lippi G, Turcato G, Cervellin G, Sanchis-Gomar F, Red blood cell distribution width in heart failure: A narrative review: World J Cardiol, 2018; 10(2); 6-14
21. Chandra A, Park SS, Pignolo RJ, Potential role of senescence in radiation-induced damage of the aged skeleton: Bone, 2019; 120; 423-31
22. Limmer A, Wirtz DC, Osteoimmunology: Influence of the immune system on bone regeneration and consumption: Z Orthop Unfall, 2017; 155(3); 273-80
23. Huang Y, Deng W, Zheng S, Relationship between monocytes to lymphocytes ratio and axial spondyloarthritis: Int Immunopharmacol, 2018; 57; 43-46
24. Yapar A, Ulucaköy C, Sezgin EA, Diagnostic role of neutrophil-to-lymphocyte ratio and monocyte-to-lymphocyte ratio in patients with enchondroma and low-grade chondrosarcoma: Jt Dis Relat Surg, 2020; 31(2); 286-90
25. Gao K, Zhu W, Liu W, The predictive role of monocyte-to-lymphocyte ratio in osteoporosis patient: Medicine (Baltimore), 2019; 98(34); e16793
26. Gary T, Pichler M, Belaj K, Platelet-to-lymphocyte ratio: A novel marker for critical limb ischemia in peripheral arterial occlusive disease patients: PLoS One, 2013; 8(7); e67688
27. Grau AJ, Boddy AW, Dukovic DA, Leukocyte count as an independent predictor of recurrent ischemic events: Stroke, 2004; 35(5); 1147-52
28. Öztürk ZA, Yesil Y, Kuyumcu ME, Inverse relationship between neutrophil lymphocyte ratio (NLR) and bone mineral density (BMD) in elderly people: Arch Gerontol Geriatr, 2013; 57(1); 81-85
29. Koseoglu SB, Bone loss & platelet-to-lymphocyte ratio: Biomark Med, 2017; 11(1); 5-10
30. Tomé-Bermejo F, Piñera AR, Alvarez L, Osteoporosis and the management of spinal degenerative disease (II): Arch bone Jt Surg, 2017; 5(6); 363-74
31. McCoy S, Tundo F, Chidambaram S, Baaj AA, Clinical considerations for spinal surgery in the osteoporotic patient: A comprehensive review: Clin Neurol Neurosurg, 2019; 180; 40-47
32. Engelke K, Stampa B, Timm W, Short-term in vivo precision of BMD and parameters of trabecular architecture at the distal forearm and tibia: Osteoporos Int, 2012; 23(8); 2151-58
33. Negrini S, Donzelli S, Aulisa AG, 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth: Scoliosis Spinal Disord, 2018; 13; 3
34. Horng M-H, Kuok C-P, Fu M-J, Cobb angle measurement of spine from X-ray images using convolutional neural network: Comput Math Methods Med, 2019; 2019; 6357171
35. Harindhanavudhi T, Petryk A, Jones R, Lumbar spine bone mineral density Z-score discrepancies by dual X-ray absorptiometry do not predict vertebral fractures in children: J Investig Med, 2018; 66(6); 980-85
36. Syed Z, Khan A, Bone densitometry: Applications and limitations: J Obstet Gynaecol Can, 2002; 24(6); 476-84
37. Goksen D, Darcan S, Coker M, Kose T, Bone mineral density of healthy Turkish children and adolescents: J Clin Densitom, 2006; 9(1); 84-90
38. Demir K, Konakci E, Ozkaya G, New features for child metrics: further growth references and blood pressure calculations: J Clin Res Pediatr Endocrinol, 2020; 12(2); 125-29
39. Wang H, Zou D, Sun Z, Hounsfield unit for assessing vertebral bone quality and asymmetrical vertebral degeneration in degenerative lumbar scoliosis: Spine (Phila Pa 1976), 2020; 45(22); 1559-66
40. Gorissen BMC, Wolschrijn CF, van Vilsteren AAM, Trabecular bone of precocials at birth; Are they prepared to run for the wolf(f)?: J Morphol, 2016; 277(7); 948-56
41. Johnson KA, Wolff’s law continues to inspire orthopaedic research: Vet Comp Orthop Traumatol, 2014; 27(1); V-VI
42. Teichtahl AJ, Wluka AE, Wijethilake P, Wolff’s law in action: A mechanism for early knee osteoarthritis: Arthritis Res Ther, 2015; 17(1); 207
43. Lill CA, Fluegel AK, Schneider E, Sheep model for fracture treatment in osteoporotic bone: A pilot study about different induction regimens: J Orthop Trauma, 2000; 14(8); 556-59
44. Parfitt AM, Drezner MK, Glorieux FH, Bone histomorphometry: Standardization of nomenclature, symbols, and units. Report of the ASBMR Histomorphometry Nomenclature Committee: J Bone Miner Res, 1987; 2(6); 595-610
45. Siu WS, Qin L, Cheung WH, Leung KS, A study of trabecular bones in ovariectomized goats with micro-computed tomography and peripheral quantitative computed tomography: Bone, 2004; 35(1); 21-26
46. Kapadia RD, Stroup GB, Badger AM, Applications of micro-CT and MR microscopy to study pre-clinical models of osteoporosis and osteoarthritis: Technol Heal Care, 1998; 6(5–6); 361-72
47. Lencel P, Magne D, Inflammaging: The driving force in osteoporosis?: Med Hypotheses, 2011; 76(3); 317-21
48. Weitzmann MN, Ofotokun I, Physiological and pathophysiological bone turnover – role of the immune system: Nat Rev Endocrinol, 2016; 12(9); 518-32
49. Bozan N, Alpaycı M, Aslan M, Mean platelet volume, red cell distribution width, platelet-to-lymphocyte and neutrophil-to-lymphocyte ratios in patients with ankylosing spondylitis and their relationships with high-frequency hearing thresholds: Eur Arch Otorhinolaryngol, 2016; 273(11); 3663-72
50. Tang Y, Peng B, Liu J, Systemic immune-inflammation index and bone mineral density in postmenopausal women: A cross-sectional study of the national health and nutrition examination survey (NHANES) 2007–2018: Front Immunol, 2022; 13; 975400
51. Nishida M, Yagi M, Suzuki S, Persistent low bone mineral density in adolescent idiopathic scoliosis: A longitudinal study: J Orthop Sci, 2022 [Online ahead of print]
52. Sadat-Ali M, Al-Othman A, Bubshait D, Al-Dakheel D, Does scoliosis causes low bone mass? A comparative study between siblings: Eur Spine J, 2008; 17(7); 944-47
53. Lee WTK, Cheung CSK, Tse YK, Generalized low bone mass of girls with adolescent idiopathic scoliosis is related to inadequate calcium intake and weight bearing physical activity in peripubertal period: Osteoporos Int, 2005; 16(9); 1024-35
54. Cheung CSK, Lee WTK, Tse YK, Generalized osteopenia in adolescent idiopathic scoliosis--association with abnormal pubertal growth, bone turnover, and calcium intake?: Spine (Phila Pa 1976), 2006; 31(3); 330-38
55. Caţan L, Cerbu S, Amaricai E, Assessment of static plantar pressure, stabilometry, vitamin D and bone mineral density in female adolescents with moderate idiopathic scoliosis: Int J Environ Res Public Health, 2020; 17(6); 2167
56. Batista R, Martins DE, Hayashi LF, Association between vitamin D serum levels and adolescent idiopathic scoliosis: Scoliosis, 2014; 9(Suppl 1); O45
57. Ng S-Y, Bettany-Saltikov J, Cheung IYK, Chan KKY, The role of vitamin D in the pathogenesis of adolescent idiopathic scoliosis: Asian Spine J, 2018; 12(6); 1127-45
58. Balioglu MB, Aydin C, Kargin D, Vitamin-D measurement in patients with adolescent idiopathic scoliosis: J Pediatr Orthop B, 2017; 26(1); 48-52
59. Ryan PJ, Blake GM, Herd R, Parker J, Fogelman I, Distribution of bone mineral density in the lumbar spine in health and osteoporosis: Osteoporos, 1994; 4(2); 67-71
60. Lau RW, Cheuk KY, Ng BK, Effects of a home-based exercise intervention (E-Fit) on bone density, muscle function, and quality of life in girls with adolescent idiopathic scoliosis (AIS): A pilot randomized controlled trial: Int J Environ Res Public Health, 2021; 18(20); 10899
Tables
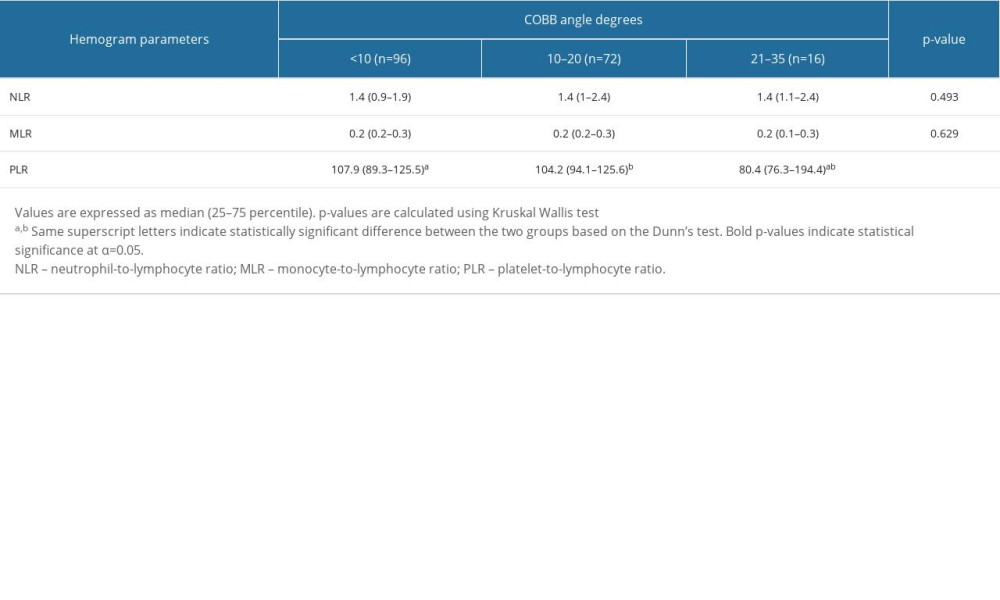 Table 1. The comparison of hemogram parameters across scoliosis groups.
Table 1. The comparison of hemogram parameters across scoliosis groups.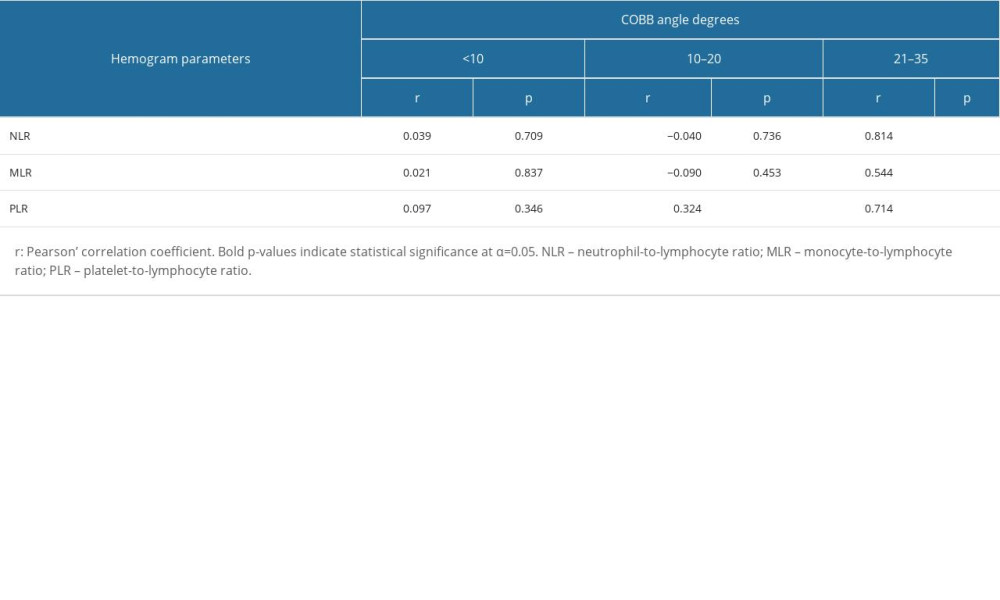 Table 2. Correlation analysis between DXA Z scores and hemogram parameters according to severity of scoliosis.
Table 2. Correlation analysis between DXA Z scores and hemogram parameters according to severity of scoliosis.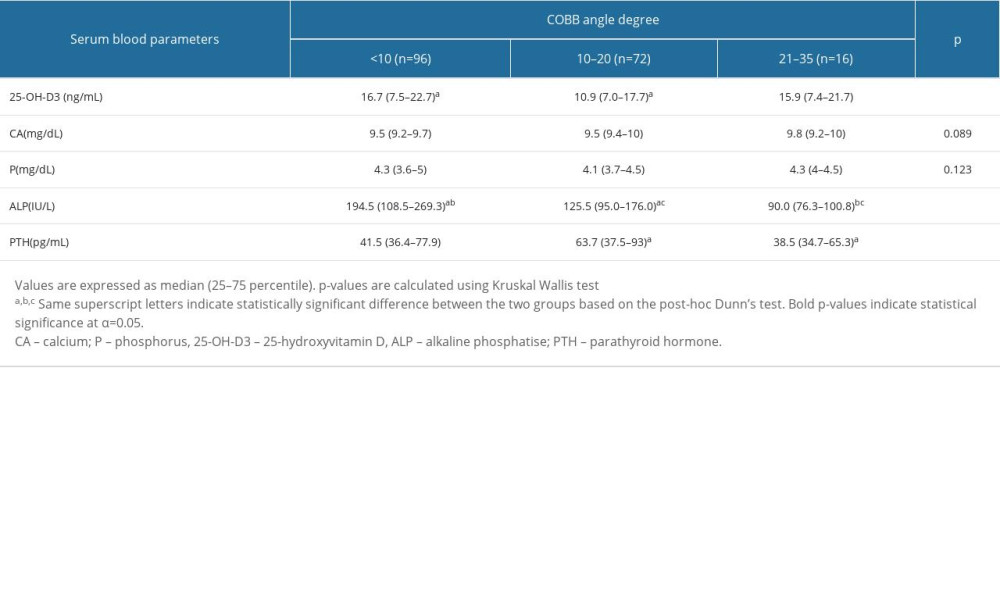 Table 3. Comparison of serum blood parameters across scoliosis groups.
Table 3. Comparison of serum blood parameters across scoliosis groups.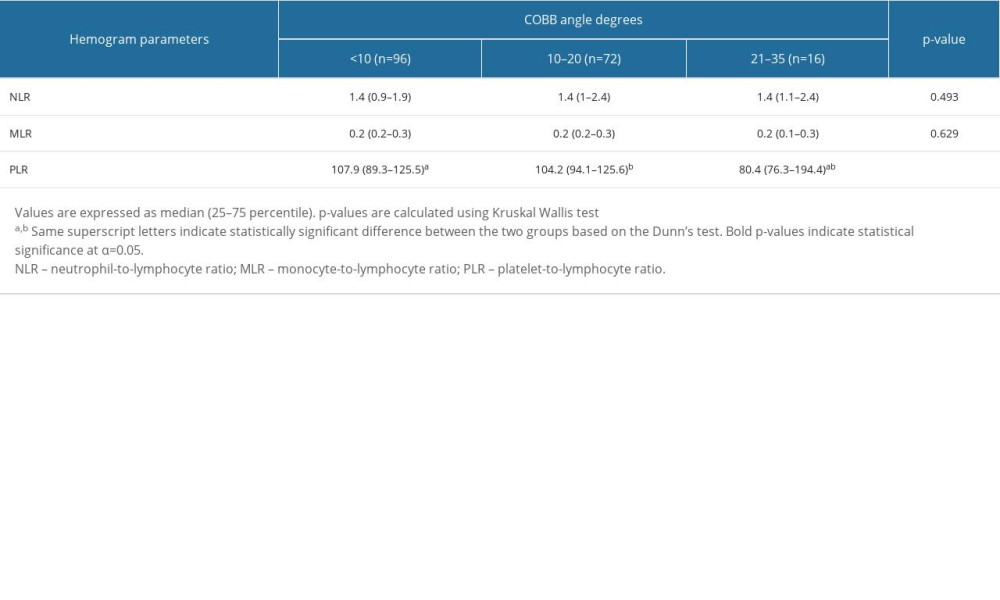 Table 1. The comparison of hemogram parameters across scoliosis groups.
Table 1. The comparison of hemogram parameters across scoliosis groups.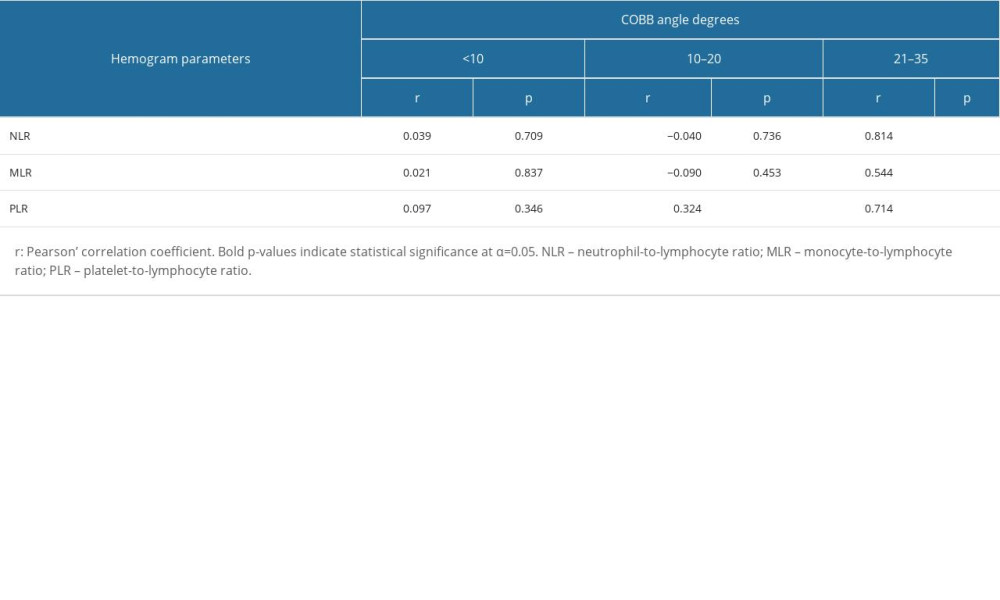 Table 2. Correlation analysis between DXA Z scores and hemogram parameters according to severity of scoliosis.
Table 2. Correlation analysis between DXA Z scores and hemogram parameters according to severity of scoliosis.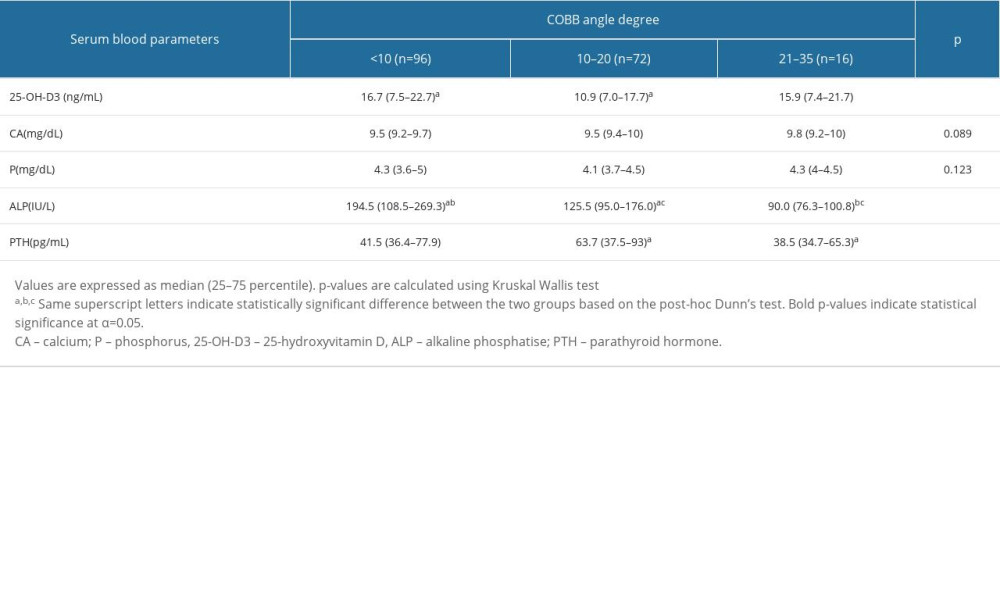 Table 3. Comparison of serum blood parameters across scoliosis groups.
Table 3. Comparison of serum blood parameters across scoliosis groups. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952