15 August 2022: Clinical Research
Radiological Assessment of Prevalance and Quality of Periapical Status of Endodontic Treatments
Zeynep AysalDOI: 10.12659/MSM.936569
Med Sci Monit 2022; 28:e936569
Abstract
BACKGROUND: The aim of this study was to determine the current prevalence and quality of endodontic treatments and investigate the relationship of various factors with posttreatment endodontic disease (PTED) in a Turkish subpopulation.
MATERIAL AND METHODS: The cone beam computed tomography (CBCT) images of 1069 patients (male, 50.9%; female, 49.1%; mean age, 45.32±13.50 years) were retrospectively analyzed. A total of 20 646 teeth were examined; 1604 had undergone root canal. Periapical status was assessed using a modified CBCT periapical index. The relationship between periapical status and quality of root canal fillings (RCFs) was analyzed statistically using the chi-square test. Multivariate logistic regression was performed to evaluate the effect of individual parameters by adjusting them for other variables.
RESULTS: A total of 7.8% of all teeth had RCF. The prevalence of poor filling (having at least 1 procedural error) was 54.1%; the prevalence of PTED was 56.8%. The prevalence of PTED was 44.3% in teeth with short RCF, 10.8% with overextended RCF, 35.7% with nonhomogeneous RCF, and 15.5% in teeth with untreated root canals. The rate of RCF teeth with procedural errors associated with PTED was 76.2%. There was no significant difference between sexes in apical periodontitis (P>0.05), which developed more frequently in teeth with procedural errors.
CONCLUSIONS: The overall prevalence of poor fillings (having at least 1 procedural error) among RCF teeth was high (54.1%) in this subpopulation. There is a substantial need to improve the technical quality of endodontic treatment.
Keywords: Cone-Beam Computed Tomography, Epidemiology, Periapical Periodontitis, Tooth, Nonvital, Adult, Female, Humans, Male, Middle Aged, Root Canal Obturation, Root Canal Therapy
Background
Epidemiologic studies bring useful knowledge about trends in the incidence and prevalence of diseases and their risk factors. These data are valuable for planning health care strategies to prevent or decrease the occurrence of considered disorders [1]. The presence of apical periodontitis (AP) is evaluated by clinical symptoms and periapical radiograhps. The radiological assessment is important for diagnosis, especially for different atypical odonalgia [2]. Conventional radiographs, as 2-dimensional (2D) images, show low sensitivity for detecting apical radiolucency [3]. AP is an inflammatory oral disease that can be detected when the destruction of cortical bone is present. Therefore, AP might not be detected in regions with a thick cortical plate [3]. The term “postteatment endodontic disease” (PTED) has been suggested by Friedman and is defined as the disease associated with the radiolucency of endodontically treated teeth. PTED includes all persistent, recurrent, and emerged AP associated with endodontically treated teeth and differentiates these conditions from AP that is associated with untreated teeth [4].
Cone beam computed tomography (CBCT) is a relatively new imaging techique that shows 3D images of structures. CBCT scanning can be useful in endodontics for detecting AP, assesing root canal morphology, detecting procedural errors, and evaluating postoperative healing outcomes [5,6]. Estrela et al [7] evaluated a new periapical index (PAI) based on CBCT for the identification of AP.
Procedural improvements and advances in technology have changed endodontic therapy. However, this has not changed the outcome of endodontic treatment throughout the years [8]. Many observational studies identified the rate of inadequately obturated root canals in relation to periapical health, with results showing various treatment outcomes among different countries. The prevalance of inadequate filling was up to 72.4%, of which 87.0% showed periapical periodontitis [9]. Undoutedly, endodontic treatment quality is not the only parameter assuring a successful root canal treatment [10]. Periodic evalautions of the rate of periapical pathology in different populations can aid in determining treatment need in a particular area and correlate treatment outcomes to different parameters.
The aim of this study was to determine the current prevalence and quality of endodontic treatments and to investigate the relationship of various factors with PTED in a Turkish subpopulation. In addition, the qualities of root canal fillings (RCFs) were evaluated with regard to their impact on periapical health. The null hypothesis (H0) to be tested was there is no difference in the prevalence of periapical lesions in each particular root regarding procedural errors.
Material and Methods
STATISTICAL ANALYSIS:
The statistical analyses were performed using MedCalc Statistical Software version 12.7.7 (MedCalc Software bcba, Ostend, Belgium;
Results
A total of 20 646 teeth from 525 women and 544 men with a mean age of 45.28 years were screened (Table 2). A total of 1604 endodontically treated teeth (7.8%) were identified. Among the endodontically treated teeth, the prevalence of PTED was 56.8% (911 teeth). The distribution of endodontically treated teeth according to sex and age is shown in Table 2: women had more endodontically treated teeth than men.
The apical status of teeth with root canal treatment was evaluated by CBCT PAI, and the score 0 was determined as “no apical lesion” and score 1 to 5 as “with apical lesion”. A significant difference was found between the average age of patients with periapical lesions and the average age of patients without lesions (
Of the 911 teeth that had undergone root canal treatment and were associated with periapical lesions, 59.6% were in the maxilla and 40.4% were in the mandible. Of the 543 endodontically treated teeth in the maxilla and associated with apical lesions, 45.1% were anterior teeth and 54.9% were posterior teeth. According to multivariate logistic regression analysis, the incidence of apical lesions in maxillary posterior teeth was found to be 1.62 times lower than in maxillary anterior teeth (95% CI, odds ratio [OR]=0.617), and this difference was statistically significant (
No procedural errors were detected in 45.9% of the endodontically treated teeth. The prevalence of PTED was 34% in teeth without procedural errors. At least 1 procedural error was detected in 54.1% of the evaluated endodontically treated teeth. The prevalence of PTED was 76.2% in teeth with procedural errors.
Apical lesions were detected in 30 (76.9%) of 39 teeth with a broken instrument, 141 (87%) of 162 teeth with missed canals, 30 (73.2%) of 41 teeth with ledge formation, and 6 (66.7%) of 9 teeth with perforation. When homogeneity and apical extent of root canal treatments were evaluated, 38.1% of 810 (50.5%) teeth with flush and homogenous canal fillings were found to be associated with apical lesions; 98 (78.4%) of 125 teeth with overfillings were associated with apical lesions; and 404 (75.1%) of 538 teeth with short canal filling were associated with apical lesions. In multi-rooted teeth, the shortest or the most extended root filling was used for the evaluation. Apical lesions were detected in 325 (80.2%) of 405 teeth with nonhomogeneous RCF (presenting voids and poor density) (OR=2.748). While the presence of broken instruments (OR=2.746), missed canals (OR=5.809), short canal filling (OR=3.142), and inhomogeneity of canal filling (OR=2.748) in endodontically treated teeth had statistically significant differences (
Discussion
Epidemiological studies provide important information about the prevalence and frequency of AP and endodontically treated teeth. It also provides data on the outcomes of endodontic treatments in the population [1]. There are very few studies that were conducted in large subpopulations and that revealed more generalized and accurate results than the present study. This study was an epidemiological study aimed at evaluating the quality of endodontic treatments in a large subpopulation of the Turkish population.
For a long time, conventional imaging techniques (digital panoramic and periapical radiographs) have been used to diagnose periapical radiolucencies and differentiate them from a healthy periapex. Conventional imaging techniques show some limitations, including 3D compression of the anatomies of structures, geometric alternation, and superposition of anatomical structures [11]. As a new clinical tool, CBCT provides 3D imaging of the pathology under investigation and has a higher sensitivity than conventional radiography, without superposition of adjacent structures [12]. Estrela et al [3] analyzed 1425 root-treated teeth in different imaging modalities and found the periapical lesion percentages were 63.3% for CBCT, 35.3% for periapical radiographs, and 17.6% for panoramic radiographs. The researchers stated that CBCT has a higher sensitivity for identifying periapical lesions than do conventional modalities. Additionally, the 3D evaluation enables a more reliable assessment of other parameters, including extention of RCF, compared with 2D analysis.
The periapical index (PAI) has been used in numerous studies and has been accepted as the criterion standard for diagnosing periapical lesions. Ørstavik et al [13] used 2D radiographic images in the PAI scoring they developed, while Estrela et al [7] created CBCT PAI scoring based on the interpretation of 3D CBCT scans. These 2 periapical indices, therefore, have different scoring systems as a result of the characteristics of both imaging methods. The CBCT PAI scoring developed by Estrela et al [7] has some advantages for clinical applications. CBCT PAI scores are calculated by 3D analysis of the lesion, and tomography sections are obtained in the mesiodistal, buccopalatinal, and diagonal directions. Measuring the depth of the lesion contributes to the diagnosis and thus to improving patient prognosis. The purpose of using CBCT PAI scoring in this study was to present a method based on the interpretation of high resolution images that can provide a more accurate measurement of the lesion width, minimize the observer factor, and increase the reliability of the research results.
Regarding age, the ages of the patients included in studies were collected in very different subgroups. In some studies, no significant difference was found in the prevalence of AP and endodontic teratment between different age groups [14,15]. Studies with significant differences in age-related prevalence have reported that patients over 50 years of age are the most affected group [16,17]. In the present study, the age group with the highest PTED rate of 51.6% was in the age group of 25 to 50 years, and was followed by the group above the age of 50 years, with a rate of 41.9%.
Studies have not found a relationship between patient sex and periapical health [18,19]. Similarly, in the present study, the rate of PTED incidence in women was 54.8%, while the rate was 59.6% in men, and this difference was not significant (
The present study showed that 7.8% of all evaluated teeth had undergone endodontic treatment. These data appear to be lower than the results of other studies, which range from 8.8% to 13.4% [14,23]. This is probably because populations in which other studies were conducted had more dental awareness than the population we included in this study. In total, 56.8% of endodontically treated teeth in the present study were associated with AP, which is in accordance with the results of several different studies [17,24]. It can be speculated that root canal treatment is insufficient in controlling disease [25].
Of the 1604 teeth we evaluated, 45.8% of adequate (no procedural error) endodontic treatment was observed, and 34% of these were associated with PTED. These data revealed that the quality of endodontic treatments was below standard; however, our results were clearly above the results of previous studies (9.9–41.9%) that examined the prevalence of adequate root canal therapy [17,26].
Our results revealed a high prevalence of periapical lesions in teeth with short RCFs (more than 2 mm from the radiographic apex). Periapical lesions were observed in 75% of 538 teeth with short RCFs (OR=3.142). These results agree with those of several previous studies [14,23,27]. The flush root filling length (within 0 to 2 mm of the radiographic apex) was associated with a lower prevalence (43%).
Meirinhos et al [14] did not record any difference in terms of AP between canal systems with flush RCFs and long RCFs. Possible reasons for the differences between the results of the studies are differences in clinical protocols, differences between 3D and 2D imaging, and limitations of overextent root filling material in radiographic imaging.
During the endodontic treatment procedure, every loss of canal working length increases the chance of failure. Chugal et al [28] emphasized that shortening of the working length, including ledge formation and canal obstructions, decreases the chance of success, especially in teeth with periapical disease. It has been argued that this is due to the inaccessible microbial infection in the canal section not being controlled and the region not being able to be disinfected. In the present study, it was observed that 73.2% of the teeth in which ledge formation was observed had PTED. The relationship between ledge formation and PTED was not found to be significant (
In the present study, the prevalence of PTED was 80.2% (OR=2.748) in teeth with nonhomogeneous RCF (presenting voids and poor density). Gencoglu et al [23] found the prevalence of AP in teeth with voids in the adaptation of canal filling with canal walls to be 74.7% in their study. Segura-Egea et al [29] reported in their study that 49% of endodotically treated teeth did not have enough adaptation of the canal filling to the canal walls, and that AP was observed in 73.9% of these teeth. However, when comparing the results of the studies, it should be kept in mind that the quality of root canal debridement cannot be evaluated with radiological examinations.
Missed canals can accommodate microorganisms and their byproducts. Therefore, untreated root canals are still one of the main causes of persistent apical lesions of endodontic origin.
Comparing mandibular anterior teeth and maxillary anterior teeth in the present study, similar results with previous studies were obtained: teeth in the mandibular anterior region were more likely to have missed canals than are teeth in the maxillary anterior region. This is because mandibular anterior teeth have more complex anatomy than maxillary anterior teeth [30]. Variations in anatomy should always be considered because having limited knowledge of tooth morphology can increase the likelihood of canals being missed during treatment, which can lead to treatment failure.
Karabucak et al [5] and Costa et al [31] reported that the highest rate of missed canals can be found in the maxillary first molars (44.2% and 59%, respectively). Although these results are similar to our results, in that the maxillary first molars have the highest missed canal prevalence, the values giving the ratio of missed canal (44.2–59%) are higher than the value in the present study (38%). Thus, endodontically treated teeth with missed canals were 5.809 times more likely to be associated with periapical lesions than were endodontically treated teeth without missed canals. The odds ratios noted in the present study are in between those of the studies by Karabucak et al Metin girmek için buraya tıklayın veya dokunun.[5,31] (odds ratios of 4.4 and 6.25, respectively).
In the present study, the prevalence of periapical lesions was found to be 87% in endodontically treated teeth with missed canals. The rate stated in our study was compared with that of Karabucak et al [5] (82.8%) and Costa et al [31] (97.5%). The tight relationship between periapical lesions and missed canals can be explained as a result of the proliferation of bacteria in untreated canals and overriding the body’s immune response in apical tissues [32].
Ng et al [19] found in their prospective study that the presence of a broken instrument has a significant effect on the outcome of root canal treatment. Clinically, the type of the broken instrument, the location of the instrument, and maintaining apical patency correlate significantly with each other. “Maintaining apical patency” has been further analyzed as its direct effect on treatment outcome is more pronounced clinically. In present study, 76.9% of endodontically treated teeth with broken instruments were associated with PTED (95% CI, OR=2.746).
It has been found that the presence of perforation in the middle third or coronal of the root significantly reduces the probability of success. This condition is likely due to bacterial contamination during or after treatment. In our present study, 66.6% of teeth with root perforation were found to be associated with PTED. These data are similar to those of previous studies [19,33].
Considering the long-term success of root canal therapy, coronal leakage can play an important role, perhaps as much as any other step of root canal treatment [34]. However, it should be kept in mind that the time elapsed between the completion of root canal treatment and the placement of the coronal restoration and the conditions in this process are unknown. Gillen et al [35] showed in a meta-analysis study that coronal leakage may not be of clinical significance, as shown in in vitro studies.
Unfortunately, the quality of coronal restorations is difficult to assess due to various image artefacts in CBCT imaging. Clinical examination and intraoral radiographs are considered more reliable methods of evaluating the quality of coronal restorations than is CBCT imaging [36]. In our preliminary study, it was not possible to examine coronal restorations on CBCT images due to artefacts. For these reasons, “compatibility of coronal restorations” was not among the parameters we investigated.
There was limited clinical data regarding some of the root filled teeth assessed in the present study. Additonally, the previous practioners who treated the patients were not mentioned in all of the records. Therefore, there was no sufficient data to determine and assess this aspect properly in the present retrospective study.
A limitation of cross-sectional studies is the inability to determine whether a peripical lesion is healing or progressing [31]. However, it should be noted that the number of cases of healed periapical periodontitis is approximately equal to the number of newly developed lesions. This confirms that large numbers of CBCT evaluations show a realistic scenario in a given population [25].
Endodontic failure includes all teeth that have undergone root canal treatment and are clinically symptomatic and/or have periapical lesions radiographically. However, while terms such as “success” and “failure” refer only to treatment and its various methods, “healed”, “healing”, and “non-healed” lesions accept patient-centered factors, and this is considered an appropriate approach to individualized medicine [37].
Although the superiority of CBCTs over conventional techniques in detecting periapical radiolucencies has been proven in many studies, it should be emphasized that scanning artefacts such as beam hardening (caused by high density materials such as metal posts, metal restorations, and root filling materials) may reduce imaging quality and cause a limitation during CBCT assesment [3,12]. Moreover, recent recommendations are that CBCT should be used strictly for specific indications, not for routine diagnostic imaging in order avoid exposing patients to an unneccessary radiation dose [38].
Conclusions
The quality of root canal treatment was poor in this subpopulation. More than half of root canal-treated teeth were demonstrated to have procedural errors. Procedural errors (the presence of a broken instrument, short canal filling length, inhomogenity of canal filling) seems to result in a higher rate of PTED.
The lowest rate of PTED was observed in teeth with homogeneous and flush RCFs. Taken together, these findings suggest that there is a substantial need to improve the technical quality of endodontic treatment.
This study highlights that the AP rate of endodontically treated teeth was highly associated with procedural errors, whereas the lowest rate of AP was observed in teeth with homogeneous and flush RCFs. Our study underlines the substantial need to improve the technical quality of endodontic treatment.
Figures
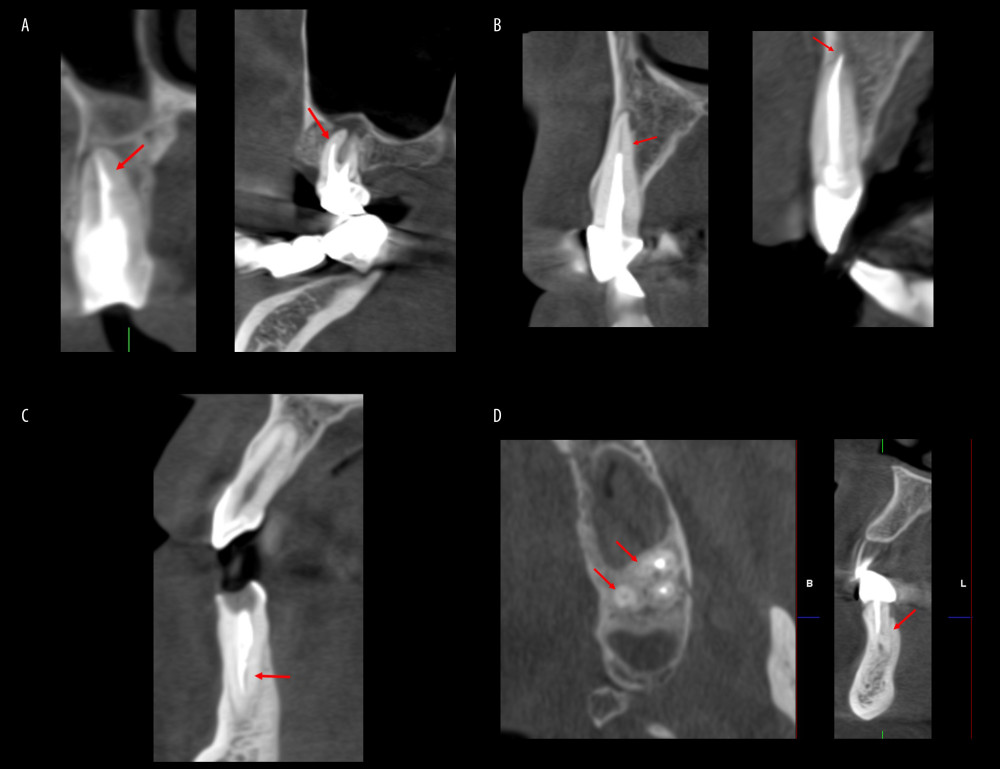 Figure 1. Procedural errors: (A) presence of broken instrument and ledge formation; (B) short root canal filling (RCF) and overextended RCF; (C) nonhomogeneous RCF; and (D) presence of missed canal in maxillary molar tooth andmandibular anterior tooth. Scans were reconstructed using Planmeca Romexis Viewer Software version 4.3.0.R (Planmeca, Helsinki, Finland).
Figure 1. Procedural errors: (A) presence of broken instrument and ledge formation; (B) short root canal filling (RCF) and overextended RCF; (C) nonhomogeneous RCF; and (D) presence of missed canal in maxillary molar tooth andmandibular anterior tooth. Scans were reconstructed using Planmeca Romexis Viewer Software version 4.3.0.R (Planmeca, Helsinki, Finland). 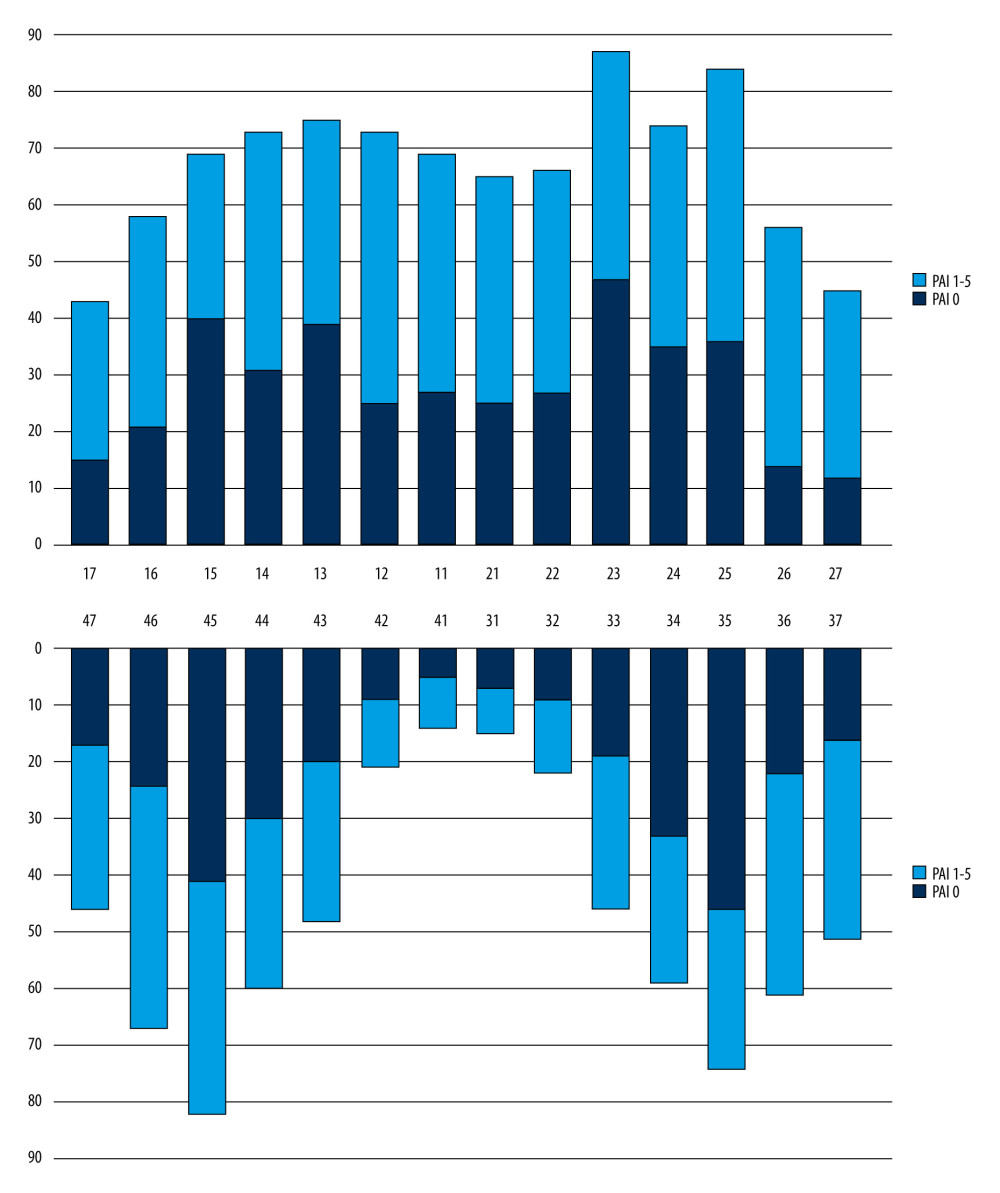 Figure 2. Distribution of the presence of posttreatment endodontic disease in teeth with root canal treatment according to the location of the teeth.
Figure 2. Distribution of the presence of posttreatment endodontic disease in teeth with root canal treatment according to the location of the teeth. Tables
Table 1. Parameters for classification.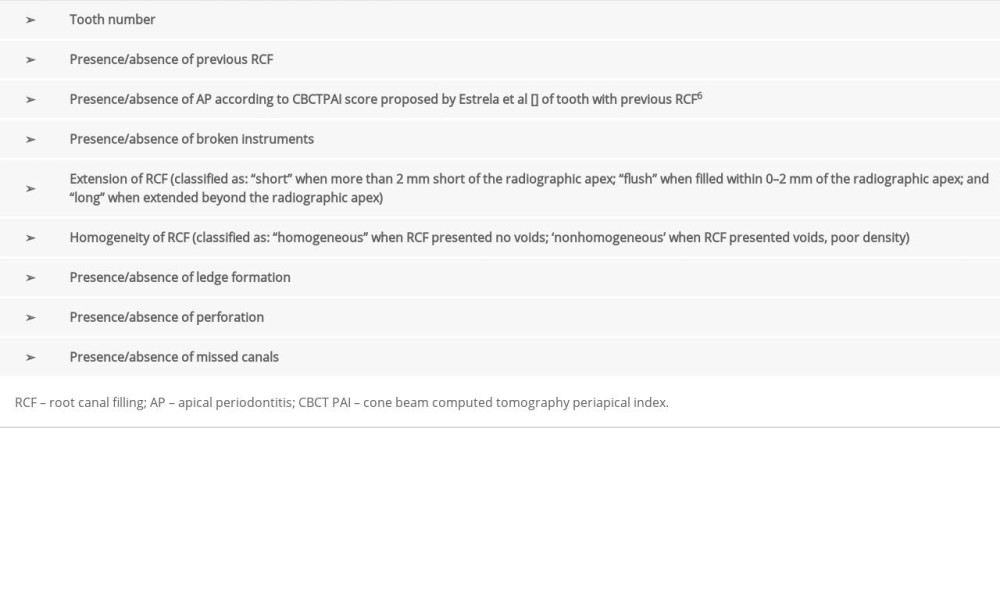 Table 2. Distribution of demographic variables.
Table 2. Distribution of demographic variables.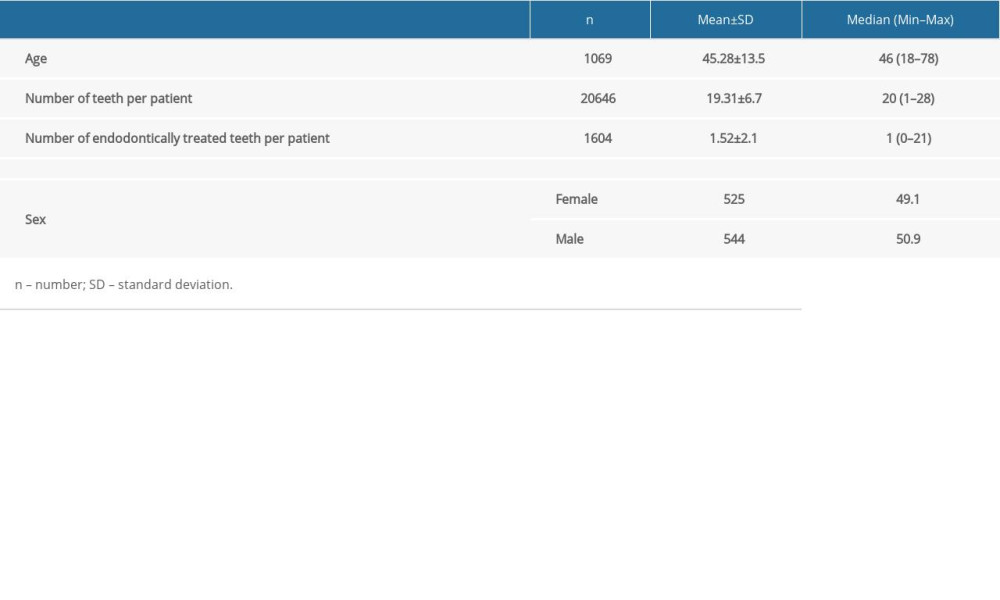 Table 3. Distribution of the presence of posttreatment endodontic disease according to age and sex.
Table 3. Distribution of the presence of posttreatment endodontic disease according to age and sex.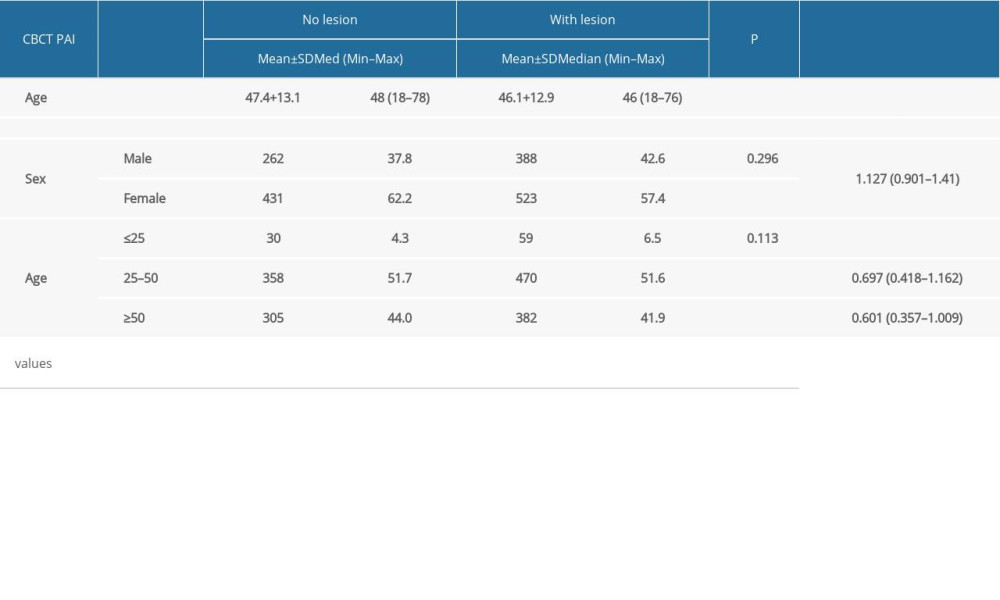 Table 4. Bivariate and multivariate analyses of posttreatment endodontic disease in association with procedural errors.
Table 4. Bivariate and multivariate analyses of posttreatment endodontic disease in association with procedural errors.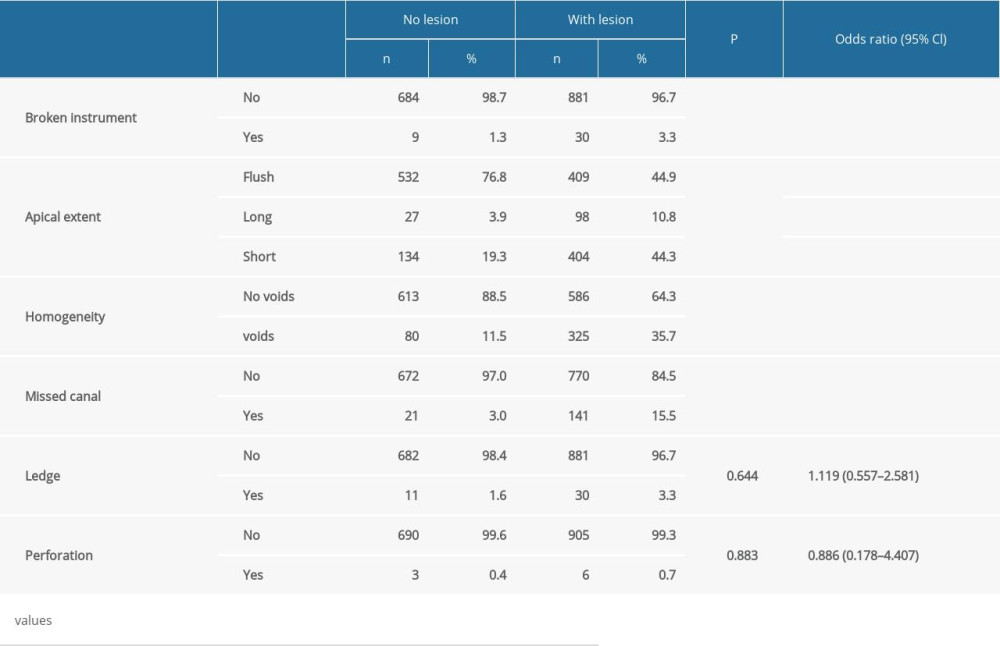
References
1. Cimmino MA, Hazes JM, Introduction: Value of epidemiological research for clinical practice: Best Pract Res Clin Rheumatol, 2002; 16(5); vii-xii
2. Pigg M, List T, Petersson K, Diagnostic yield of conventional radiographic and cone-beam computed tomographic images in patients with atypical odontalgia: Int Endod J, 2011; 44(12); 1092-101
3. Estrela C, Bueno MR, Leles CR, Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis: J Endod, 2008; 34(3); 273-79
4. Friedman S, Considerations and concepts of case selection in the management of post-treatment endodontic disease (treatment failure): EndodTopics, 2002; 1(1); 54-78
5. Karabucak B, Bunes A, Chehoud C, Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: A cone-beam computed tomography study: J Endod, 2016; 42(4); 538-41
6. Sui H, Zhao B, Nie H, Comparing the traditional versus conservative endodontic access cavities design of the maxillary first molar: Using Cone-Beam computed tomography: Med Sci Monit, 2021; 27; e932410
7. Estrela C, Reis Bueno M, Correa Azevedo B: A new periapical ındex based on cone beam computed tomography Available from: https://pubmed.ncbi.nlm.nih.gov/18928840/
8. Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K, Outcome of primary root canal treatment: Systematic review of the literature – Part 1. Effects of study characteristics on probability of success: Int Endod J, 2007; 40(12); 921-39
9. Pak JG, Fayazi S, White SN, Prevalence of periapical radiolucency and root canal treatment: A systematic review of cross-sectional studies: J Endod, 2012; 38(9); 1170-76
10. Al-Omari MA, Hazaa A, Haddad F, Frequency and distribution of root filled teeth and apical periodontitis in a Jordanian subpopulation: Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2011; 111(1); e59-65
11. Lo Giudice R, Nicita F, Puleio F, Accuracy of periapical radiography and CBCT in endodontic evaluation: Int J Dent, 2018; 2018; 2514243
12. Patel S, Brown J, Pimentel T, Cone beam computed tomography in endodontics – a review of the literature: Int Endod J, 2019; 52(8); 1138-52
13. Orstavik D, Kerekes K, Eriksen HM, The periapical index: A scoring system for radiographic assessment of apical periodontitis: Dent Traumatol, 1986; 2(1); 20-34
14. Meirinhos J, Martins JNR, Pereira B, Prevalence of apical periodontitis and its association with previous root canal treatment, root canal filling length and type of coronal restoration – a cross-sectional study: Int Endod J, 2020; 53(4); 573-84
15. Ureyen Kaya B, Kececi AD, Guldas HE, Orhan H, A retrospective radiographic study of coronal-periapical status and root canal filling quality in a selected adult turkish population: Med Princ Pract, 2013; 22(4); 334-39
16. Alrahabi M, Younes H, A cross-sectional study of the quality of root canal treatment in Al-Madinah Al-Munawwarah: Saudi Endod J, 2016; 6(1); 31
17. Kielbassa AM, Frank W, Madaus T, Radiologic assessment of quality of root canal fillings and periapical status in an Austrian subpopulation – an observational study: PLoS One, 2017; 12(5); e0176724
18. Nascimento EHL, Gaêta-Araujo H, Andrade MFS, Freitas DQ, Prevalence of technical errors and periapical lesions in a sample of endodontically treated teeth: A CBCT analysis: Clin Oral Investig, 2018; 22(7); 2495-503
19. Ng YL, Mann V, Gulabivala K, A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: Periapical health: Int Endod J, 2011; 44(7); 583-609
20. Gomes AC, Nejaim Y, Silva AIv, Influence of endodontic treatment and coronal restoration on status of periapical tissues: A cone-beam computed tomographic study: J Endod, 2015; 41; 1614-18
21. Nur BG, Ok E, Altunsoy M, Evaluation of technical quality and periapical health of root-filled teeth by using cone-beam ct: J Appl Oral Sci, 2014; 22(6); 502-8
22. Bartley EJ, Fillingim RB, Sex differences in pain: A brief review of clinical and experimental findings: Br J Anaesth, 2013; 111(1); 52-58
23. Gencoglu N, Pekiner FN, Gumru B, Helvacioglu D, Periapical status and quality of root fillings and coronal restorations in an adult Turkish subpopulation: Eur J Dent, 2010; 4(1); 17-22
24. Gupta S, Khatri RK, Khullar P, A survey report on effect of root canal fillings and coronal restorations on the periapical status of endodontically treated teeth in a selected group of population: Int J Clin Pediatr Dent, 2013; 6(2); 89-94
25. Moreno JO, Flávio Alves FR, Lúcio Gonçalves LS, Periradicular status and quality of root canal fillings and coronal restorations in an urban Colombian population: J Endod, 2013; 39(5); 600-4
26. Gündüz K, Avsever H, Orhan K, Demirkaya K, Cross-sectional evaluation of the periapical status as related to quality of root canal fillings and coronal restorations in a rural adult male population of Turkey: BMC Oral Health, 2011; 11(1); 20
27. de Sousa Gomide Guimarães MRF, Samuel RO, Guimarães G, Evaluation of the relationship between obturation length and presence of apical periodontitis by CBCT: An observational cross-sectional study: Clin Oral Investig, 2019; 23(5); 2055-60
28. Chugal NM, Clive JM, Spångberg LSW, Endodontic infection: Some biologic and treatment factors associated with outcome: Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2003; 96(1); 81-90
29. Segura-Egea JJ, Jiménez-Pinzón A, Poyato-Ferrera M, Periapical status and quality of root fillings and coronal restorations in an adult Spanish population: Int Endod J, 2004; 37(8); 525-30
30. Kartal N, Yanikolu FÇ, Root canal morphology of mandibular incisors: J Endod, 1992; 18(11); 562-64
31. Costa FFNP, Pacheco-Yanes J, Siqueira JF, Association between missed canals and apical periodontitis: Int Endod J, 2019; 52(4); 400-6
32. Baumgartner JC, Siqueira JF, Sedgley CM, Microbiology of endodontic disease: Ingle’s Endodontics, 2008
33. de Chevigny C, Dao TT, Basrani BR, Treatment outcome in endodontics: The Toronto Study-Phases 3 and 4: Orthograde retreatment: J Endod, 2008; 34(2); 131-37
34. Ray HA, Trope M, Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration: Int Endod J, 1995; 28(1); 12-18
35. Gillen BM, Looney SW, Gu LS, Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: A systematic review and meta-analysis: J Endod, 2011; 37(7); 895-902
36. Tyndall DA, Rathore S, Cone-beam CT diagnostic applications: Ccaries, periodontal bone assessment, and endodontic applications: Dent Clin North Am; 52(4); 825-41
37. Messer HH, Yu VSH, Terminology of endodontic outcomes: Int Endod J, 2013; 46(3); 289-91
38. Patel S, Durack C, Abella F, European Society of Endodontology position statement: The use of CBCT in endodontics: Int Endod J, 2014; 47(6); 502-4
Figures
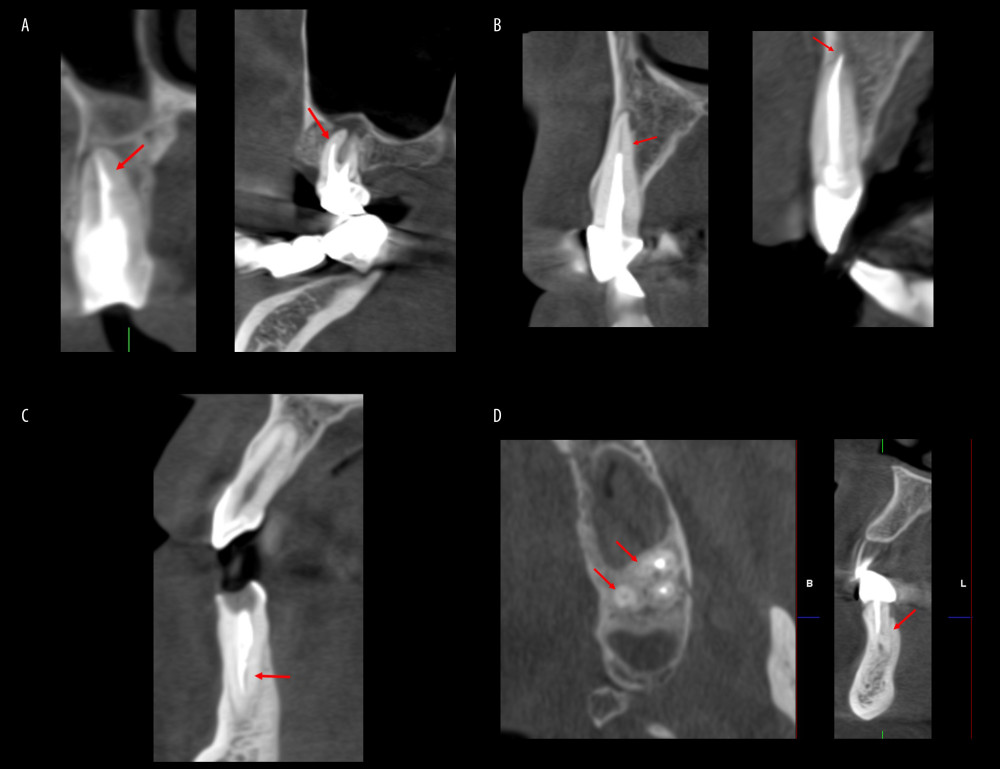 Figure 1. Procedural errors: (A) presence of broken instrument and ledge formation; (B) short root canal filling (RCF) and overextended RCF; (C) nonhomogeneous RCF; and (D) presence of missed canal in maxillary molar tooth andmandibular anterior tooth. Scans were reconstructed using Planmeca Romexis Viewer Software version 4.3.0.R (Planmeca, Helsinki, Finland).
Figure 1. Procedural errors: (A) presence of broken instrument and ledge formation; (B) short root canal filling (RCF) and overextended RCF; (C) nonhomogeneous RCF; and (D) presence of missed canal in maxillary molar tooth andmandibular anterior tooth. Scans were reconstructed using Planmeca Romexis Viewer Software version 4.3.0.R (Planmeca, Helsinki, Finland).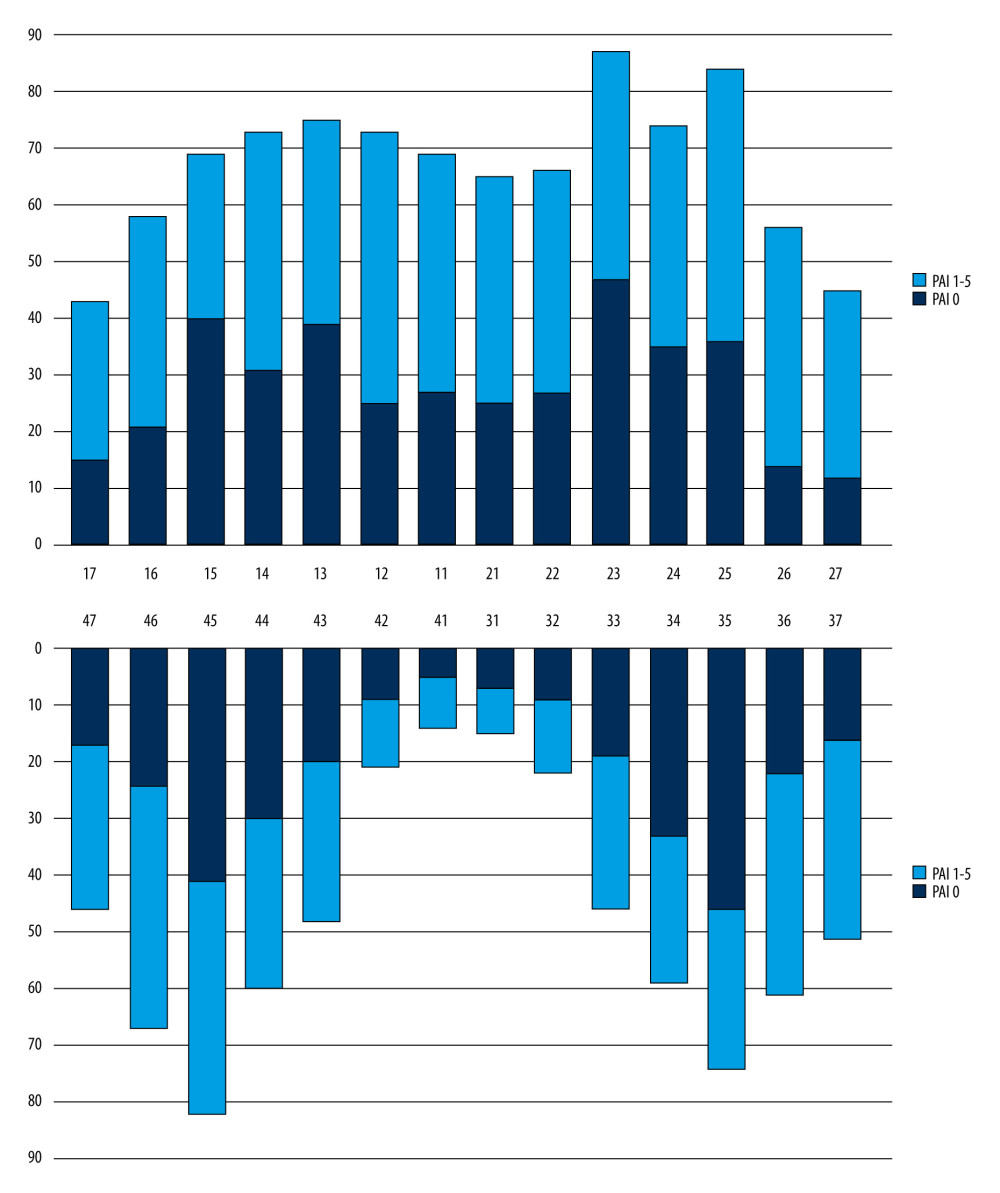 Figure 2. Distribution of the presence of posttreatment endodontic disease in teeth with root canal treatment according to the location of the teeth.
Figure 2. Distribution of the presence of posttreatment endodontic disease in teeth with root canal treatment according to the location of the teeth. Tables
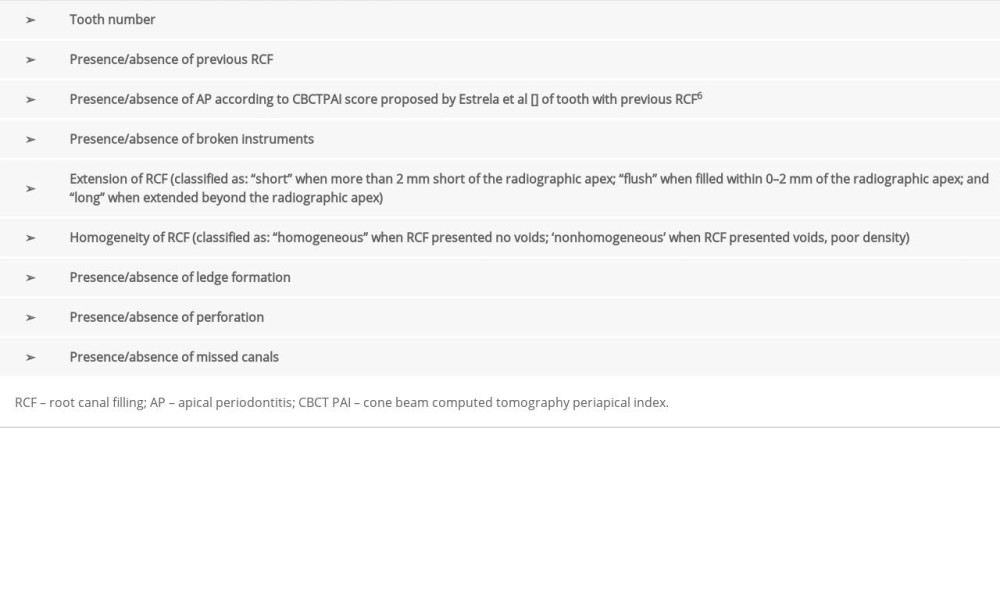 Table 1. Parameters for classification.
Table 1. Parameters for classification.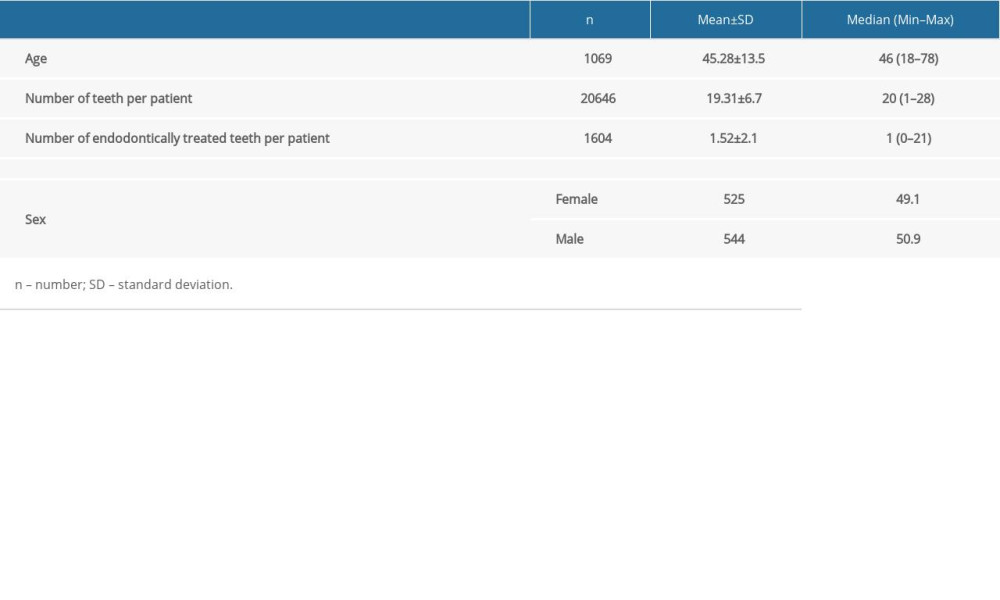 Table 2. Distribution of demographic variables.
Table 2. Distribution of demographic variables.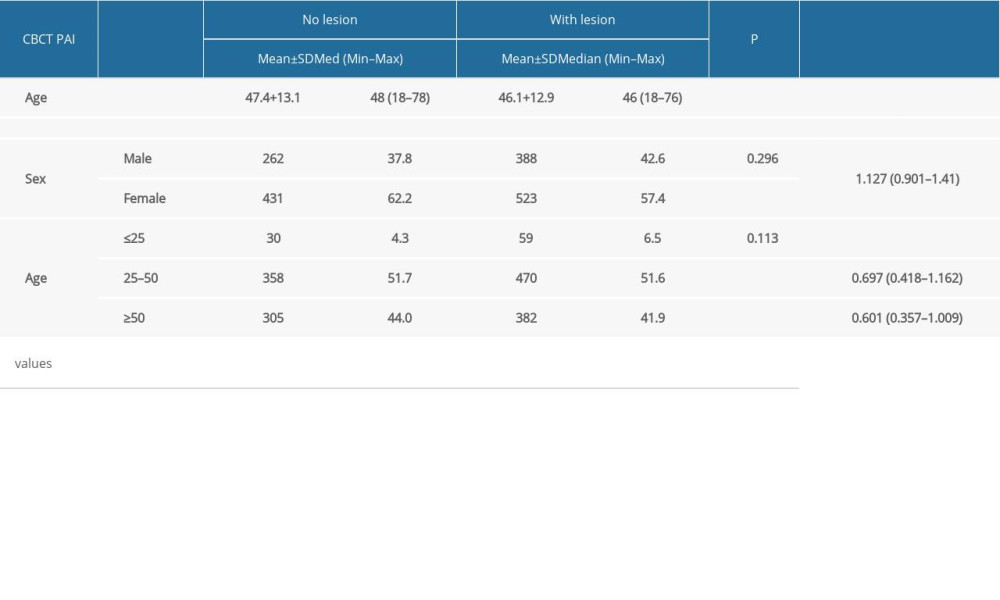 Table 3. Distribution of the presence of posttreatment endodontic disease according to age and sex.
Table 3. Distribution of the presence of posttreatment endodontic disease according to age and sex.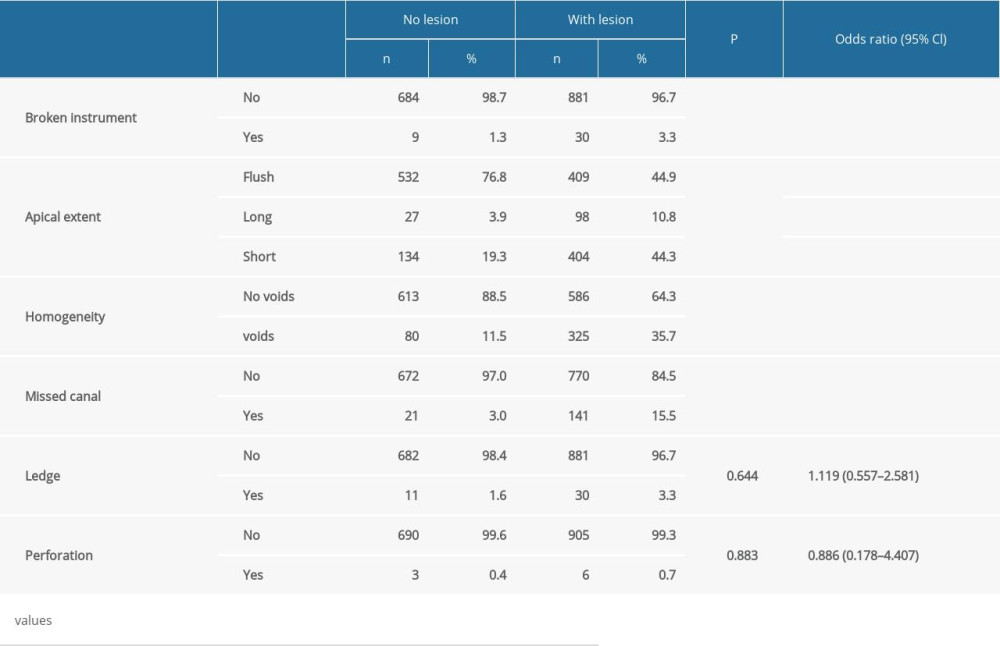 Table 4. Bivariate and multivariate analyses of posttreatment endodontic disease in association with procedural errors.
Table 4. Bivariate and multivariate analyses of posttreatment endodontic disease in association with procedural errors.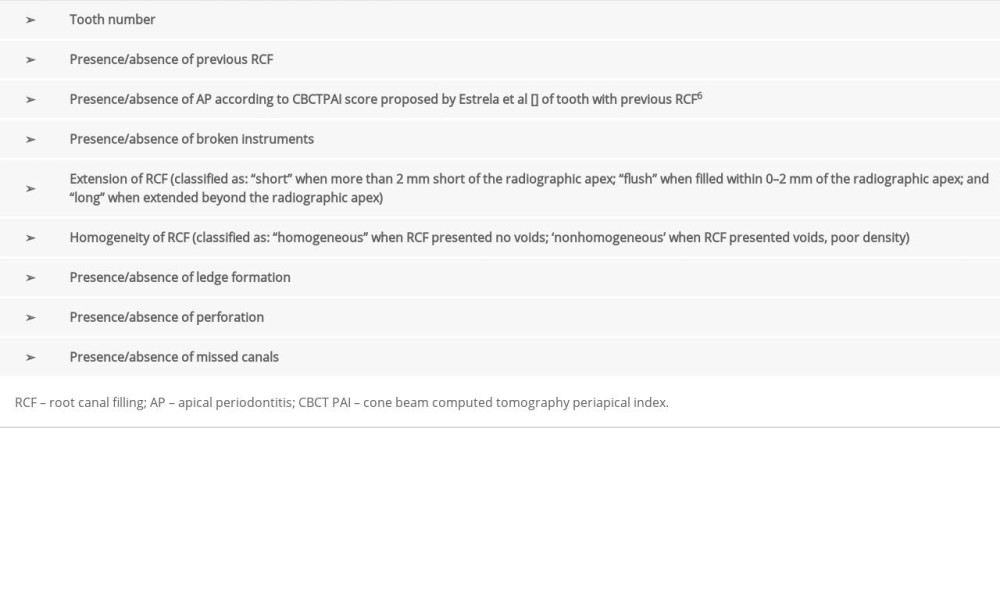 Table 1. Parameters for classification.
Table 1. Parameters for classification.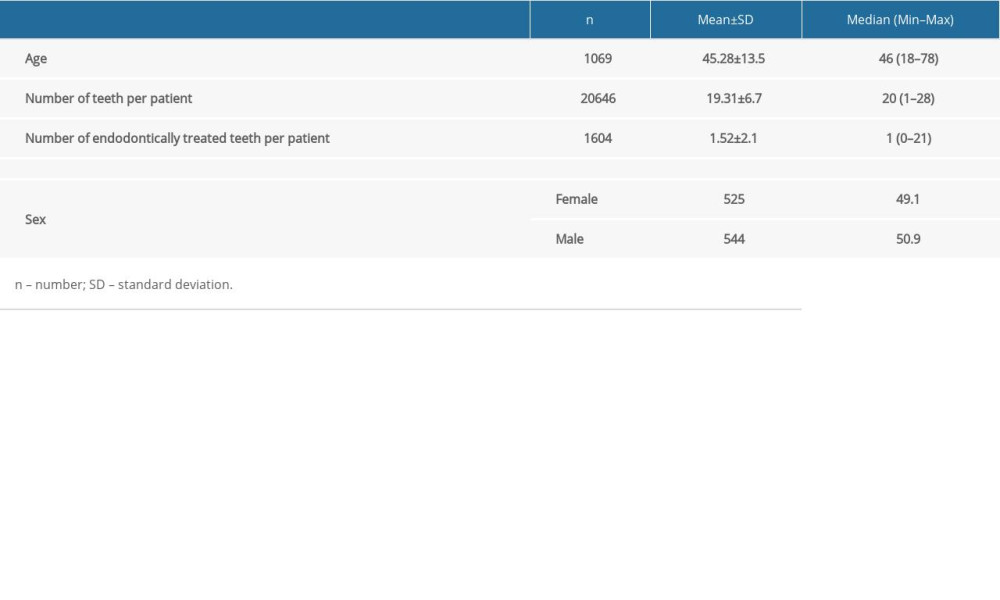 Table 2. Distribution of demographic variables.
Table 2. Distribution of demographic variables.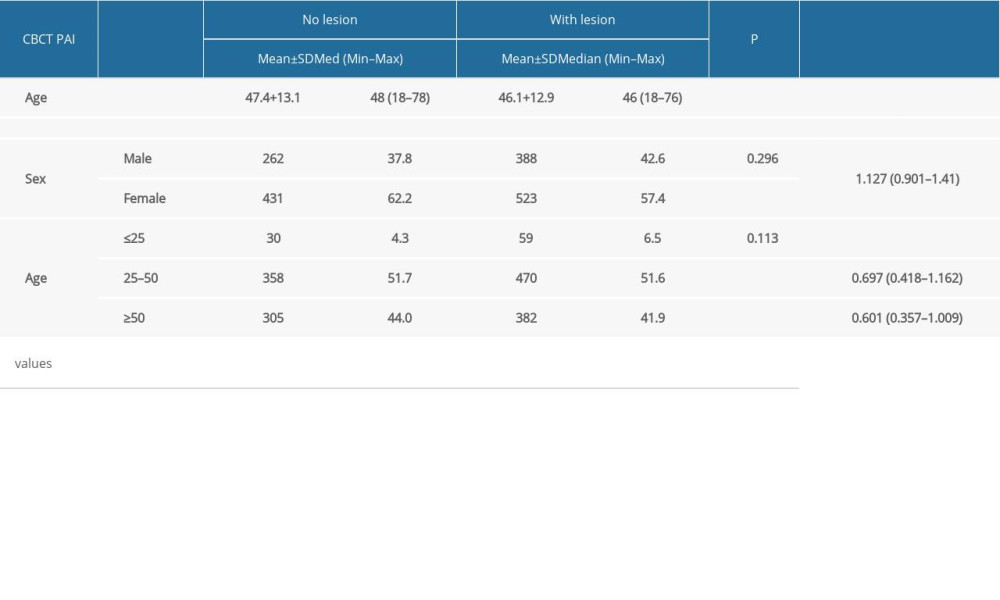 Table 3. Distribution of the presence of posttreatment endodontic disease according to age and sex.
Table 3. Distribution of the presence of posttreatment endodontic disease according to age and sex.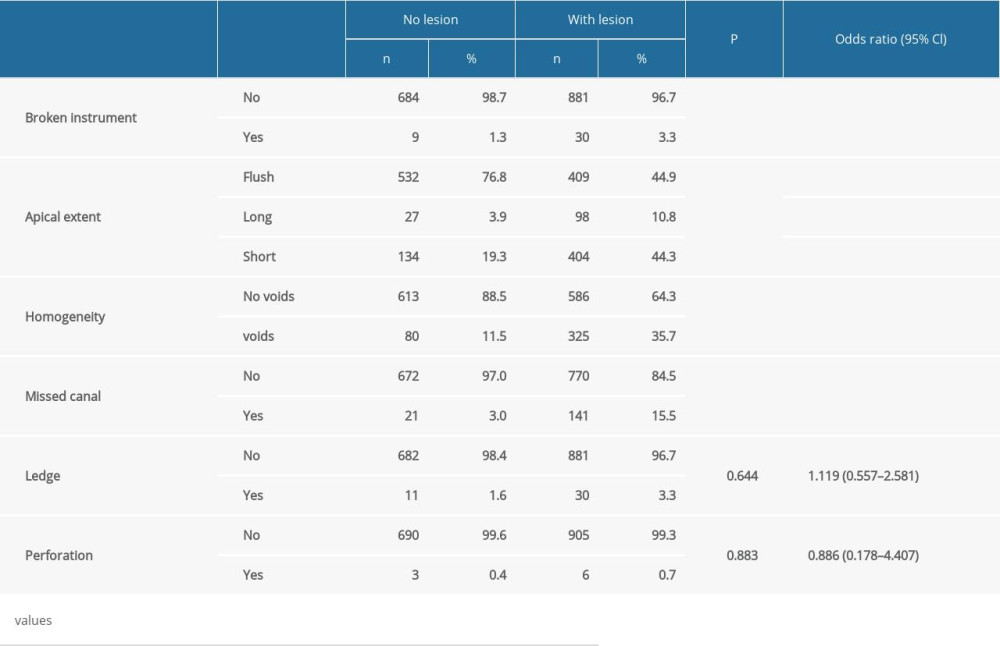 Table 4. Bivariate and multivariate analyses of posttreatment endodontic disease in association with procedural errors.
Table 4. Bivariate and multivariate analyses of posttreatment endodontic disease in association with procedural errors. In Press
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








