17 August 2022: Clinical Research
A Retrospective Study of 98 Elderly Patients with High-Risk Lateral Femoral Wall Intertrochanteric Hip Fractures to Compare Outcomes Following Surgery with Proximal Femoral Nail Antirotation (PFNA) Versus Dynamic Hip Screw (DHS)
Zhi Tian1BCDE, Jia Chen1ABCDE, Yazhou Zhang1CF, Lifang Shi1F, Wenyi Li1AE*DOI: 10.12659/MSM.936923
Med Sci Monit 2022; 28:e936923
Abstract
BACKGROUND: The aim of this study was to evaluate the efficacy of dynamic hip screw (DHS) and femoral nail antirotation (PFNA) in the treatment of lateral-wall high-risk type of intertrochanteric fractures.
MATERIAL AND METHODS: A total of 98 patients with high-risk intertrochanteric fractures of the lateral wall who underwent surgery from January 2019 to December 2020 were selected as the study subjects. Of these, 52 were treated surgically with PFNA (mean age 73.45±5.95 years) and 46 with DHS (71.37±6.22 years). We followed up these patients and compared the occurrence of the 2 surgical methods in terms of perioperative period, complication rate, and functional recovery.
RESULTS: In terms of lateral wall fracture, there were 2 cases of PFNA and 10 cases of DHS, and the difference between groups was statistically significant (P<0.05). Operative time (mean 54.94±7.29 vs 61.17±6.45) and intraoperative blood loss (72.80±9.18 vs 96.12±8.22) was significantly lower in the PFNA group compared to the DHS group (all P<0.05). Efficacy in the PFNA group was significantly better than in the DHS group. The HHS at follow-up was significantly higher in the PFNA group (mean 80.73±9.20 vs 64.19±8.12) than in the DHS group (P<0.001). The VAS score at follow-up was significantly lower in the PFNA group (1.78±0.34 vs 2.65±0.23) than in the DHS group (P<0.001).
CONCLUSIONS: PFNA is more effective than DHS in the treatment of high-risk lateral wall fractures in the elderly, with the advantages of lower incidence of complications and better recovery of hip joint function. PFNA warrants clinical application.
Keywords: Femoral Fractures, Fracture Fixation, Intramedullary, Hip Fractures, Aged, Bone Nails, Bone Screws, Humans, Treatment Outcome
Background
Femoral intertrochanteric fracture (FIF) is a fracture mostly associated with osteoporosis that occurs between the base of the femoral neck and the lesser trochanter and, as a common type of hip fracture in clinical practice, accounts for about 36% of hip fractures [1,2]. In recent years, with population aging, the incidence of FIF has also been increasing year by year and has become a serious traumatic disease threatening the health of the elderly [3], which greatly affects the short-term and long-term quality of life of patients [4,5].
For the treatment of FIF, it has been shown that conservative treatment can easily lead to complications such as coxa vara, osteoporosis, and pulmonary infection [3,6–8]. At present, internal fixation is widely accepted for use in surgical treatment. Internal fixation surgery should be used when the patient’s physical condition allows, as it can ensure that the FIF is reduced in a timely and stable manner, allowing the patient to regain mobility as soon as possible, reducing serious complications caused by long-term bed rest, and ultimately reducing mortality and improving the prognosis [9,10]. At present, there are many surgical methods for the clinical treatment of FIF, including dynamic hip screw (DHS), femoral antirotation intramedullary nail (PFNA), and artificial joint replacement [6,11]. However, for the treatment of high-risk intertrochanteric fractures of the lateral wall, the optimal treatment remains controversial. As early as 2004, Gotfried proposed the concept of the lateral wall of the proximal femur in the clinical application of DHS and defined unstable fractures along the intertrochanteric region as high-risk intertrochanteric fractures of the lateral wall. In this fracture reduction treatment, the structure of the lateral greater trochanter is weak, and there is a rupture, while the medial wall is not supported. Therefore, inappropriate internal fixation can cause damage to the lateral wall, leading to treatment failure.
We hypothesized that PFNA would have better clinical outcomes than DHS for treating patients with high-risk intertrochanteric fractures of the lateral wall. Therefore, 96 patients with high-risk intertrochanteric fractures of the lateral wall treated with PFNA or DHS were retrospectively analyzed in this study. We compared the perioperative period, incidence of complications, and functional recovery to evaluate the therapeutic effect of PFNA and DHS in patients with high-risk intertrochanteric fractures of the lateral wall, and then provide a reference for clinical treatment.
Material and Methods
PATIENTS:
In this retrospective cohort study, we systematically reviewed medical records of all patients with high-risk intertrochanteric fractures of the lateral wall who underwent surgery from January 2019 to December 2020. According to inclusion and exclusion criteria, 98 patients were finally included after screening. All procedures were performed by 2 senior chief physicians with comparable technical experience. According to surgical method, the patients were divided into 2 groups: the PFNA group and the DHS group. Of these, 52 (mean age 73.45±5.95 years) were in the PFNA group and 46 (71.37±6.22 years) were in the DHS group. The sex patio was 22/30 male/females in the PFNA group and 22/24 in the DHS group. The study was approved by the Institutional Review Board of Hebei Provincial People’s Hospital and conducted in accordance with the Declaration of Helsinki and the regulations of the Health Insurance Portability and Accountability Act (HIPAA). The requirement of informed consent was waived by the Ethics Committee of Hebei Provincial People’s Hospital due to the retrospective nature of the study and anonymity of data.
INCLUSION AND EXCLUSION CRITERIA:
Inclusion criteria were: (1) Patients hospitalized in Hebei Provincial People’s Hospital due to intertrochanteric fracture from January 2019 to December 2020, (2) Patients with lateral-wall high-risk type of intertrochanteric fracture confirmed by X-ray and CT, (3) Complete medical records, (4) Patients undergoing PFNA or DHS surgery, and (5) Patients signed the informed consent. Exclusion criteria (to eliminate the impact of other diseases on clinical outcomes) were: (1) Patients with blood diseases, coagulation disorders, or immune system diseases, (2) Pathological fractures and old femoral fractures, (3) Lost to follow-up or follow-up less than 6 months, (4) Patients with consciousness, communication, or mental disorders, and (5) Patients with a history of lower-limb surgery.
SURGICAL PROCESS:
In the PFNA group, epidural anesthesia or general anesthesia was used. The patient was supine on the traction bed, the traction bed was adjusted, the internal rotation was retracted to reduce the fracture, and fluoroscopy confirmed that the fracture reduction fracture was satisfactory. The operation area was disinfected. At 3–4 cm from the apex of the greater trochanter of the femur, a 4-cm longitudinal incision was made, the skin, subcutaneous tissue, and deep fascia were incised, and the lateral femoral muscle group was bluntly separated to fully expose the greater trochanter and cortex of the femur. A guide wire and reamer were placed in the direction of the medullary canal from the anterior third of the apex of the greater tuberosity. We inserted the PFNA staple extension into the medullary cavity. Install the aiming device, we drilled the guide wire in its direction, and placed the helical blade in the direction of the guide wire, which passes through the middle and lower part of the femoral neck near the superior femoral moment. We loosened the traction appropriately, placed the distal locking pin, and installed the tail cap. C-arm fluoroscopy confirmed fracture reduction and good internal fixation position. After repeated flushing, we placed drainage and sutured the incision.
DHS group: The anesthesia and reduction process were the same as in the PFNA group. After acceptable reduction, the skin, subcutaneous tissue, and deep fascia were incised, the lateral femoral muscle group was bluntly separated, and the greater femur and cortex were entirely exposed through a 10-cm incision on the lateral side of the greater trochanter. After reaming and measuring the depth in the direction of the guide wire, the suitable DHS screw was driven in, and a sleeve plate was attached and screwed to the lateral cortex of the femoral shaft. C-arm fluoroscopy confirmed fracture reduction and good internal fixation position. After repeated flushing, we placed drainage and sutured the incision.
POSTOPERATIVE MANAGEMENT:
Patients in both groups received an intravenous infusion of standard antibiotics within 24 hours of surgery to avoid infection. Under the supervision of a doctor, patients were asked to conduct quadriceps stretching contraction exercises as well as flexion and extension activities involving the hip on the second postoperative day. Low-molecular-weight heparin was used to prevent lower-limb thrombosis from the first day of hospitalization until 2 weeks after surgery.
One week after surgery, the patient was required to stand on the ground with crutches (walking aids), bear weight on the unaffected lower limb, and do not bear weight on the surgical limb; partial weight-bearing training was started 4 weeks after surgery, and weight-bearing was gradually increased according to the callus formation shown by X-ray examination, followed by full weight-bearing after complete fracture healing (generally 12–16 weeks after surgery). Balance training and functional motor training were carried out 12 weeks after surgery.
OUTCOMES:
(1) Demographic characteristics and clinical parameters, such as sex, age, body mass index (BMI), alcohol consumption status, smoking status, cause of injury, and fracture type, were recorded for all patients. (2) Intraoperative conditions and postoperative recovery were recorded in all patients in both groups, including: operation time, number of intraoperative fluoroscopies, intraoperative blood loss, and time to start ambulation. Radiographic evaluation was performed to estimate fracture union, hip varus deformity, and internal fixation failure. Anterior and lateral X-rays were taken monthly for 6 months after surgery. After that, X-rays were taken every 3 months for 6 months. Internal fixation failure, delayed fracture union, nonunion, and lateral wall fractures were recorded. (3) We evaluated the functional recovery of patients. Hip joint function recovery was evaluated according to Harris Hip Score (HHS) [12] from 4 aspects: function, pain, deformity, and activity. The total score is 100 points, and the score and corresponding evaluation are as follows: excellent: ≥90 points; good: 80–89 points; fair: 70–79 points; poor: <70 points. The HHS and excellent and good rate were recorded. The visual analog scale (VAS) was used to evaluate the degree of hip pain in the 2 groups during follow-up [12].
STATISTICAL ANALYSIS:
Data analysis was performed using SPSS Statistics, Version 21 (SPSS, Inc., Chicago, IL, USA). Results are expressed as mean±standard deviation (m±SD). Categorical variable data were analyzed by chi-square test. The independent samples
Result
DEMOGRAPHIC DATA:
Demographic data, including sex, age, side of injury, cause of injury, smoking status, alcohol consumption status, fracture type, and follow-up time, showed no statistical difference (all P>0.05) (Table 1).
INCIDENCE OF COMPLICATIONS:
There was no significant difference in incision infection, bedsores, delayed fracture healing, deep venous thrombosis, pulmonary infection, urinary tract infection, internal fixation failure, and nonunion between the PFNA and DHS groups (all P>0.05). In terms of lateral wall fractures, PFNA occurred in 2 patients and DHS occurred in 10 patients, with a statistically significant difference (P<0.05) (Table 2).
PERIOPERATIVE CONDITIONS:
The PFNA group had a significantly shorter operative time (54.94±7.29 min vs 61.17±6.45 min) and less intraoperative blood loss (72.80±9.18 ml vs 96.12±8.22 ml) compared to the DHS group (all P<0.05). No significant difference was found between groups in the number of intraoperative fluoroscopies (38.40±10.17 vs 37.18±8.26) (P=0.516) (Table 3).
CLINICAL OUTCOMES:
Fracture healing time was not significantly different between the PFNA and DHS groups (14.78±4.76 weeks vs 15.53±3.16 weeks) (P=0.367). The PFNA group had a considerably shorter time to ambulation than the DHS group (8.51±3.23 days vs 13.87±2.74 days) (P<0.001) (Table 4).
There was no significant difference in preoperative HHS between the PFNA and DHS groups (45.50±6.49 vs 44.73±7.89) (P=0.598). However, HHS at follow-up was significantly higher in the PFNA group (80.73±9.20 vs 64.19±8.12; P<0.001). There was a significant increase in HHS before follow-up in both groups (P<0.05) (Table 5). There was no significant difference in preoperative VAS scores between the PFNA and DHS groups (6.54±2.76 vs 6.43±2.44) (P=0.836). However, the VAS score at follow-up was significantly lower in the PFNA group (1.78±0.34 vs 2.65±0.23) (P<0.001). The VAS scores at follow-up were significantly lower in both groups (P<0.05) (Table 6).
In the PFNA group, the treatment outcome was excellent in 18 cases and good in 26 cases, and the excellent and good rate of the treatment outcome was 84.62%. In the DHS group, the treatment outcome was excellent in 10 cases and good in 15 cases, with an excellent and good rate of 54.35%. The treatment effect in the FNA group was significantly better than that of the DHS group (P=0.001) (Table 7).
Discussion
With population aging in recent years, the incidence of FIF has increased [13,14]. The notion of the lateral femoral wall was first developed by Israeli surgeon Gotfried, who introduced it into the surgical treatment of fractures in 2004, stating that it plays an important role in maintaining the integrity of internal fixation of fractures [15]. The extent of the lateral femoral wall remains controversial. According to some research, the lateral femoral wall is the location where the lateral femoral cortex joins the lateral femoral cortex along the tangent line of the femoral neck’s upper and lower edges [16]. According to some research, the lateral femoral ridge is the upper boundary of the lateral wall, while the junction point between the lateral femoral cortex and the tangent of the lower neck of the femur is the lower boundary [17].
It has been confirmed that the lateral wall of the femur plays an important mechanical stabilization role in the treatment of femoral fractures, and that the integrity of the lateral wall can provide rotational stability for the femur, support the bone of the head and neck, and effectively resist its varus, rotation, and diaphyseal displacement, which can avoid the cut-out of screws [16,18]. The helical blade must be implanted in the femoral head neck through the lateral wall for FIF, whether treated with extramedullary fixation or intramedullary nailing, and maintaining the integrity of the lateral wall is critical to the stability of FIF internal fixation [19,20]. However, Palm et al [21] found that 74% of lateral wall fractures were due to intraoperative manipulation, while patients with lateral wall fractures had a 22% re-operation revision rate. Therefore, how to select the appropriate fixation method and make the fracture well fixed while protecting the lateral wall is a very critical clinical problem. In addition, compared with intertrochanteric fractures in general, the lateral wall danger type of intertrochanteric fractures is more severe, and fracture reduction is more difficult due to severe comminuted fractures and involvement of the lesser trochanter.
From a stability point of view, it is very important to select the appropriate fixation treatment [14]. In clinical practice, there are still many disagreements about the best internal fixation procedure for hazardous lateral femoral wall fractures in the elderly [22]. For the treatment of hazardous lateral femoral wall fractures, both PFNA and DHS are common surgical options [20]. In this study, patients with serious lateral femoral wall fractures were compared to the efficacy of DHS internal fixation and minimally invasive PFNA internal fixation. The results of this study suggest that the PFNA internal fixation technique has significant advantages over the DHS technique. The PFNA group had a shorter operation duration, less intraoperative blood loss, quicker ambulation, better hip function, and a lower incidence of complications than the DHS group. The PFNA group had a significantly lower rate of lateral femoral wall fractures than the DHS group, which could be due to the DHS’s excessive dissection of the lateral wall’s soft tissue during fracture treatment, causing the lateral wall to lose its soft tissue protection and be more likely to fracture perioperatively. PFNA is a minimally invasive internal fixation approach characterized by short operation time and less intraoperative bleeding [23]. These were also the main reasons for the early ambulation and high hip function scores in the PFNA group. In addition, in stable intertrochanteric 31-A1 and 31-A2 fractures, the absence of distal blocking screws does not compromise bone healing and may prevent multiple clinical complications. Palm et al [21] evaluated and examined the clinical efficacy of PFNA and DHS in the treatment of patients with femoral fractures, and discovered that DHS was more likely to cause perioperative fracture of the lateral wall of the greater trochanter, and that the re-operation revision rate of patients in the PFNA group was much lower than that of patients in the DHS group. Other studies have found that PFNA reduces injury and complications in the treatment of risky lateral wall fractures in older people, which is effective in reducing fracture healing time and promoting hip joint function recovery [27–29]. These findings show the feasibility and efficacy of closed reduction and minimally invasive internal fixation with PFNA for the treatment of hazardous aneurysms. For the high-risk type of lateral wall of femoral fracture with high stability requirement, DHS fixation method is not effective.
Several limitations of this study should be considered. First, this was a retrospective cohort study, and the data were not comprehensive enough, which may cause bias. Second, each study group had a small number of patients, which resulted in inadequate statistical power. Future research that improves these factors may provide further information to validate the findings presented here.
Conclusions
In conclusion, PFNA is more effective than DHS in the treatment of hazardous lateral wall fractures in the elderly, with the benefits of a lower risk of complications, shorter operation duration, less intraoperative blood loss, and better hip joint function recovery.
Tables
Table 1. General information of the patients in the 2 groups.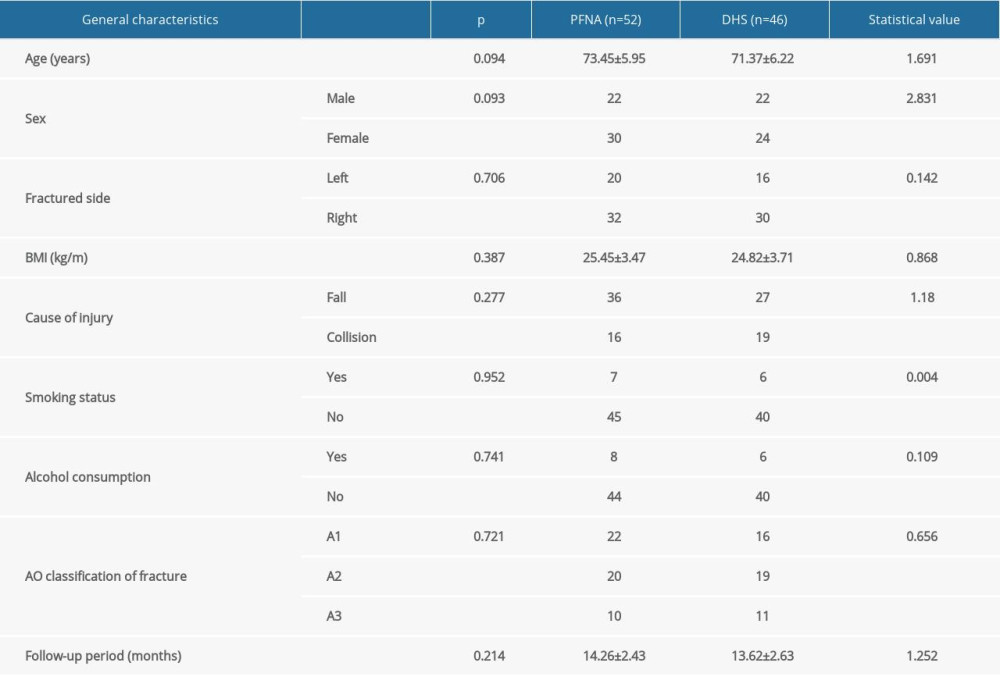 Table 2. Incidence of complications of the patients in the 2 groups.
Table 2. Incidence of complications of the patients in the 2 groups.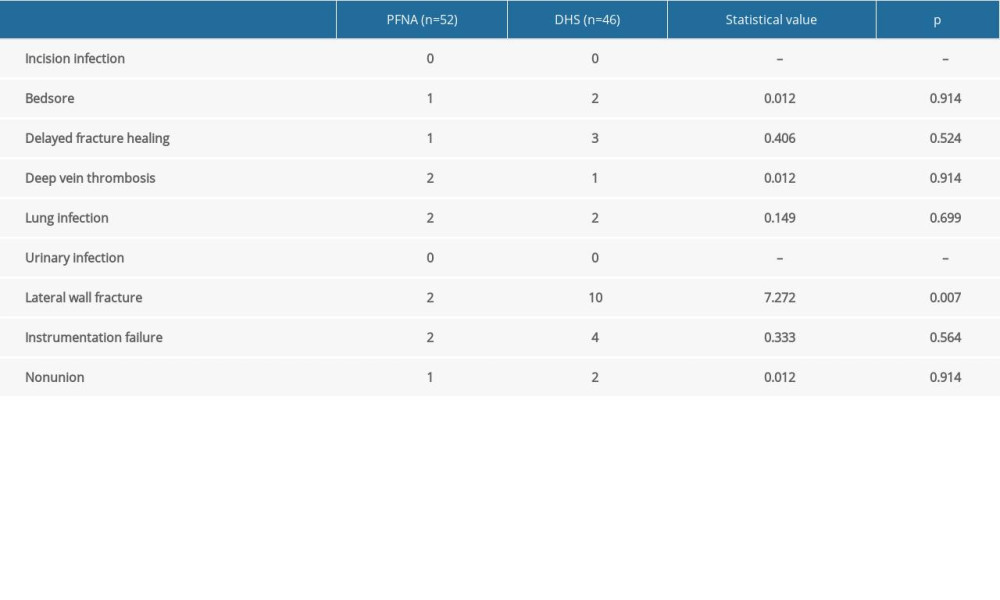 Table 3. Perioperative conditions of the patients in the 2 groups.
Table 3. Perioperative conditions of the patients in the 2 groups. Table 4. Comparison of postoperative recovery between the 2 groups (x±s).
Table 4. Comparison of postoperative recovery between the 2 groups (x±s). Table 5. Comparison of preoperative and postoperative HHS between the 2 groups (x±sd).
Table 5. Comparison of preoperative and postoperative HHS between the 2 groups (x±sd). Table 6. VAS score of hip joint pain before and after operation in both groups (x±sd).
Table 6. VAS score of hip joint pain before and after operation in both groups (x±sd). Table 7. The excellent and good rate of the 2 groups.
Table 7. The excellent and good rate of the 2 groups.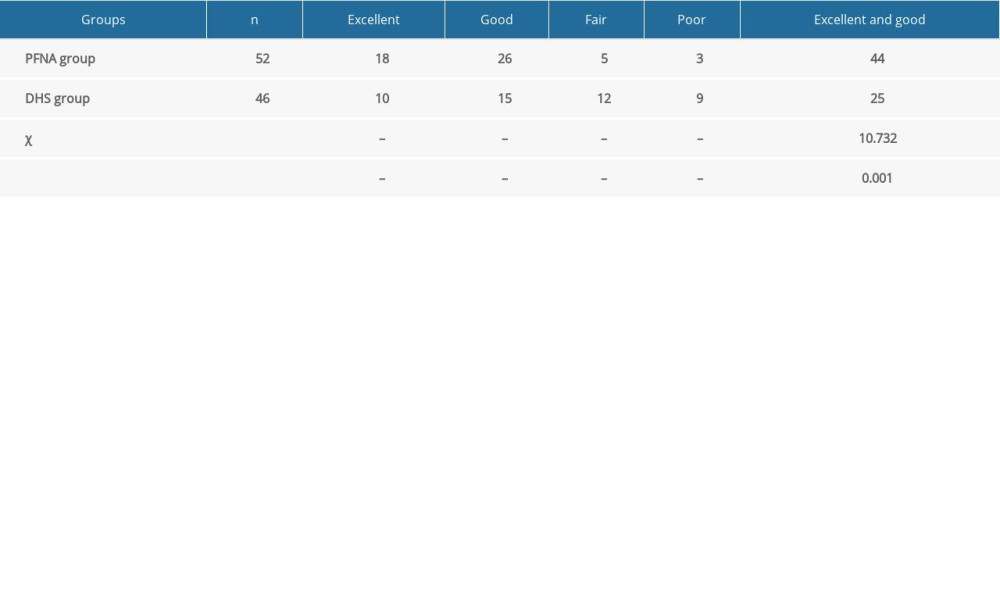
References
1. Cheng YX, Sheng X, Optimal surgical methods to treat intertrochanteric fracture: A Bayesian network meta-analysis based on 36 randomized controlled trials: J Orthop Surg Res, 2020; 15; 402
2. Nie B, Wu D, Yang Z, Liu Q, Comparison of intramedullary fixation and arthroplasty for the treatment of intertrochanteric hip fractures in the elderly: A meta-analysis: Medicine, 2017; 96; e7446
3. Tu DP, Liu Z, Yu YK, Internal fixation versus hemiarthroplasty in the treatment of unstable intertrochanteric fractures in the elderly: A systematic review and meta-analysis: Orthop Surg, 2020; 12; 1053-64
4. Mohan H, Kumar P, Surgical treatment of type 31-a1 two-part intertrochanteric femur fractures: Is proximal femoral nail superior to dynamic hip screw fixation?: Cureus, 2019; 11; e4110
5. Zelle BA, Webb AJ, Matson C, Safety and efficacy of a two-screw cephalomedullary nail for intertrochanteric femur fracture fixation: A retrospective case series in 264 patients: Patient Saf Surg, 2018; 12; 31
6. Luo X, He S, Zeng D, Proximal femoral nail antirotation versus hemiarthroplasty in the treatment of senile intertrochanteric fractures: Case report: Int J Surg Case Rep, 2017; 38; 37-42
7. Wang W, Yu J, Tranexamic acid reduces blood loss in intertrochanteric fractures: A meta-analysis from randomized controlled trials: Medicine, 2017; 96; e9396
8. Ma SQ, Wang CX, Liu XJSurgical technique and effect of proximal femoral nail anti-rotation internal fixation assisted with large retractor for the treatment of femoral intertrochanteric fractures: Zhongguo Gu Shang, 2019; 32; 165-69 [in Chinese]
9. Sun Y, Huang T, Lin J, Autogenous fibula graft and cannulated screw fixation to cephalic cut out after DHS fixation: A retrospective study: J Orthop Surg Res, 2020; 15; 11
10. Hsieh PH, Chang YH, Chen SH, Shih CH, Staged arthroplasty as salvage procedure for deep hip infection following intertrochanteric fracture: Int Orthop, 2006; 30; 228-32
11. Ju JB, Zhang PX, Jiang BG, Hip replacement as alternative to intramedullary nail in elderly patients with unstable intertrochanteric fracture: A systematic review and meta-analysis: Orthopaedic surgery, 2019; 11; 745-54
12. Yao M, Wang Y, Wei C, Greater increase in femoral offset with use of collum femoris-preserving stem than Tri-Lock stem in primary total hip arthroplasty: J Int Med Res, 2020; 48; 300060520925999
13. Chen WH, Guo WX, Gao SH, Arthroplasty vs proximal femoral nails for unstable intertrochanteric femoral fractures in elderly patients: A systematic review and meta-analysis: World journal of clinical cases, 2021; 9; 9878-88
14. Lan H, Tan Z, Li KN, Gao JH, Liu TH, Intramedullary nail fixation assisted by orthopaedic robot navigation for intertrochanteric fractures in elderly patients: Orthop Surg, 2019; 11; 255-62
15. Gotfried Y, The lateral trochanteric wall: A key element in the reconstruction of unstable pertrochanteric hip fractures: Clin Orthop Relat Res, 2004(425); 82-86
16. Haq RU, Manhas V, Pankaj A, Proximal femoral nails compared with reverse distal femoral locking plates in intertrochanteric fractures with a compromised lateral wall; A randomised controlled trial: Int Orthop, 2014; 38; 1443-49
17. Wu J, Shi Z, Li JResearch progress of lateral wall injury of intertrochanteric fracture: Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi, 2018; 32; 1605-10 [in Chinese]
18. Nie B, Chen X, Li J, The medial femoral wall can play a more important role in unstable intertrochanteric fractures compared with lateral femoral wall: A biomechanical study: J Orthop Surg Res, 2017; 12; 197
19. Fu CW, Chen JY, Liu YC, Dynamic hip screw with trochanter-stabilizing plate compared with proximal femoral nail antirotation as a treatment for unstable AO/OTA 31-A2 and 31-A3 intertrochanteric fractures: Biomed Res Int, 2020; 2020; 1896935
20. Xu JW, Han L, Hu YGA medium term therapeutic effects of anatomic locking plate for femoral intertrochanteric with lateral femoral wall fractures: Zhongguo Gu Shang, 2017; 30; 256-60 [in Chinese]
21. Palm H, Lysén C, Krasheninnikoff M, Holck K, Jacobsen S, Gebuhr P, Intramedullary nailing appears to be superior in pertrochanteric hip fractures with a detached greater trochanter: 311 consecutive patients followed for 1 year: Acta Orthop, 2011; 82; 166-70
22. Hao Y, Zhang Z, Zhou F, Risk factors for implant failure in reverse oblique and transverse intertrochanteric fractures treated with proximal femoral nail antirotation (PFNA): J Orthop Surg Res, 2019; 14; 350
23. Zhu LJ, Li XF, Liu C, Lyu CYClinical analysis of LPFP, PFNA and BPH in treating femoral intertrochanteric fractures in elderly patients: Zhongguo Gu Shang, 2017; 30; 607-11
24. Rollo G, Tartaglia N, Falzarano G, The challenge of non-union in subtrochanteric fractures with breakage of intramedullary nail: Evaluation of outcomes in surgery revision with angled blade plate and allograft bone strut: Eur J Trauma Emerg Surg, 2017; 43; 853-61
25. Lanzetti RM, Caraffa A, Lupariello D, Comparison between locked and unlocked intramedullary nails in intertrochanteric fractures: Eur J Orthop Surg Traumatol, 2018; 28; 649-58
26. Maiettini D, Bisaccia M, Caraffa A, Feasibility and value of radiographic union score hip fracture after treatment with intramedullary nail of stable hip fractures: Acta Inform Med, 2016; 24; 394-96
27. Mu W, Zhou J, PFNA-II internal fixation helps hip joint recovery and improves quality of life of patients with lateral-wall dangerous type of intertrochanteric fracture: Biomed Res Int, 2021; 2021; 5911868
28. Hao Z, Wang X, Zhang X, Comparing surgical interventions for intertrochanteric hip fracture by blood loss and operation time: A network meta-analysis: J Orthop Surg Res, 2018; 13; 157
29. Huang CG, Ye JJComparison of three methods for the treatment of aged femoral intertrochanteric fracture: Zhongguo Gu Shang, 2012; 25; 549-53
Tables
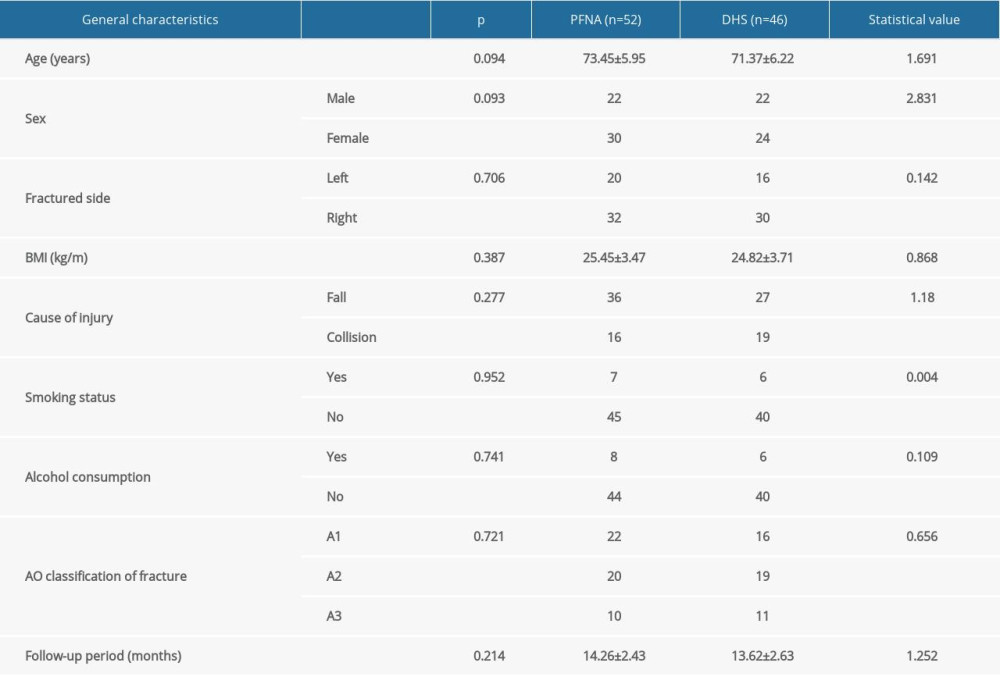 Table 1. General information of the patients in the 2 groups.
Table 1. General information of the patients in the 2 groups.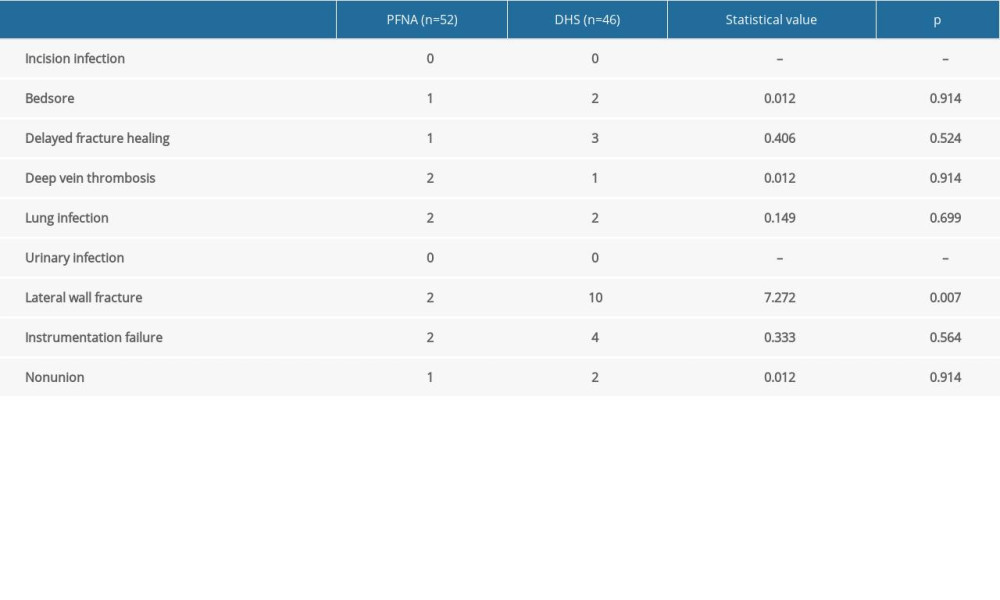 Table 2. Incidence of complications of the patients in the 2 groups.
Table 2. Incidence of complications of the patients in the 2 groups. Table 3. Perioperative conditions of the patients in the 2 groups.
Table 3. Perioperative conditions of the patients in the 2 groups. Table 4. Comparison of postoperative recovery between the 2 groups (x±s).
Table 4. Comparison of postoperative recovery between the 2 groups (x±s). Table 5. Comparison of preoperative and postoperative HHS between the 2 groups (x±sd).
Table 5. Comparison of preoperative and postoperative HHS between the 2 groups (x±sd). Table 6. VAS score of hip joint pain before and after operation in both groups (x±sd).
Table 6. VAS score of hip joint pain before and after operation in both groups (x±sd).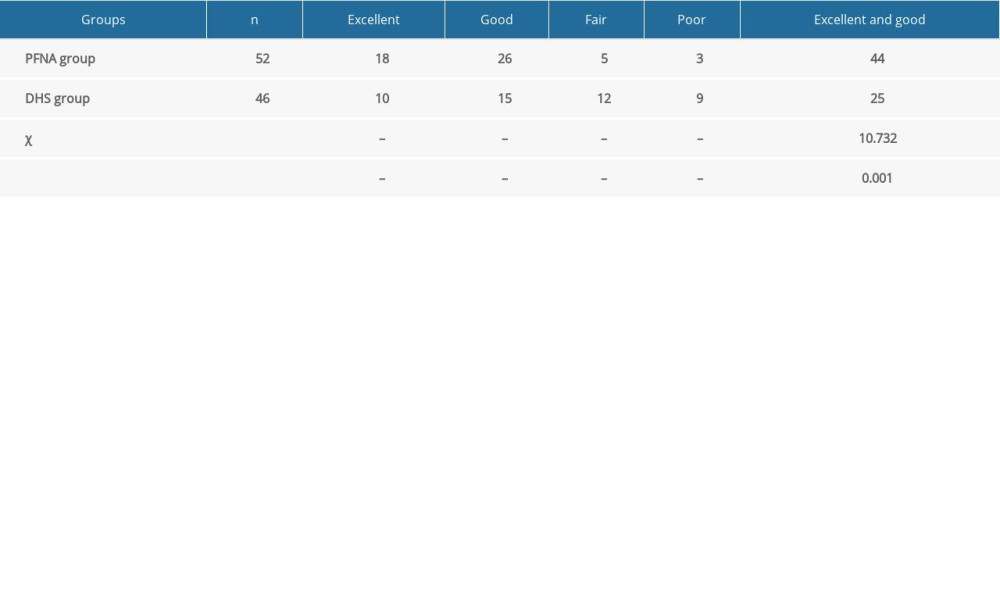 Table 7. The excellent and good rate of the 2 groups.
Table 7. The excellent and good rate of the 2 groups. In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








