18 August 2022: Clinical Research
A 3-Year Clinical Evaluation of Endodontically Treated Posterior Teeth Restored with Resin Nanoceramic Computer-Aided Design/Computer-Aided Manufacture (CAD/CAM)-Fabricated Partial Crowns
Lei Zhang1E, Xiao-Xia Hou2C, Maihefuzi Aishan3B, Meng-Ting Tian3B, Hui-Yu He1A*DOI: 10.12659/MSM.937331
Med Sci Monit 2022; 28:e937331
Abstract
BACKGROUND: We aimed to investigate the clinical effects of resin nanoceramic (RNC) computer-aided design/computer-aided manufacture (CAD/CAM) partial crowns on posterior teeth after root canal treatment over a 3-year period.
MATERIAL AND METHODS: A total of 132 posterior teeth restored with CAD/CAM partial crowns were placed in 128 patients. The observation group (n=66) was restored with RNC restorations, while the control group received lithium disilicate-based glass ceramic (LDGC) CAD restorations. Using Fédération dentaire internationale (FDI) World Dental Federation clinical criteria, 2 calibrated evaluators examined the performance of the restorations at baseline, 6, 12, 18, 24, and 36 months. The Kaplan-Meier method and the log-rank test were adopted to analyze the survival rate. The influence of potential risk factors on the main pattern of failure was studied by univariate Cox regression analysis (α=0.05).
RESULTS: At the 3-year followup, the survival rate of the partial crowns was 83.1% in the RNC group, and 93.5% in the LDGC group (P=0.061). Failures were caused by debonding (66.7%), restoration fracture (26.6%), and tooth fracture (6.7%). No significant differences were found between the 2 materials at 36 months, except for the parameters of “surface luster” (P=0.002) and “occlusal contour and wear” (P=0.009). The RNC group was significantly more likely to debond than the LDGC group (hazard ratio=9.22 [1.17,72.74], P=0.01).
CONCLUSIONS: RNC CAD/CAM-fabricated partial crowns are a potential clinical alternative for endodontically treated posterior teeth, with a survival rate of 83.1% at the 3-year followup. The main pattern of failure was debonding, which might be influenced by surface pretreatment of the RNC material.
Keywords: Composite Resins, Inlays, ProCAD Ceramic, Ceramics, Computer-Aided Design, Computers, Crowns, Dental Porcelain, Dental Prosthesis Design, Humans, Materials Testing, Root Canal Therapy
Background
Endodontically treated posterior teeth have a higher risk of mechanical failure than vital teeth owing to the loss of a large amount of coronal tooth structure, necessitating functional reconstruction [1,2]. The loss of hard tissue may result from the endodontic access preparation or extensive excavation to remove caries [3]. Partial indirect restorations, which have been classified as inlays (covering none of the cusps), onlays (covering at least one cusp), and overlays (covering all cusps), can enable conservation of the remaining dental structure with minimal tooth reduction to reinforce a tooth compromised by caries or fracture [4]. “Onlays” and “overlays” are often referred to as partial crowns and are documented to be more durable in posterior teeth with large defects, especially endodontically treated teeth [5].
Since the current trend for metal-free restorative dentistry, resin-composite and ceramic materials, which provide superior esthetics and clinical longevity, have been increasingly requested by patients [6]. Conventional resin-composite or ceramic restorations have previously involved a series of complicated procedural steps, which waste time and energy; however, CAD/CAM systems with simplified procedures for indirect restorations have improved rapidly and are now used worldwide [7]. CAD/CAM ceramic and resin-composite materials, especially all-ceramic materials, can be used for either partial indirect restorations or monolithic crowns, providing excellent esthetic properties and adequate strength [8]. Lithium disilicate-based glass ceramic (LDGC) CAD/CAM blocks (IPS E. max, Ivoclar Vivadent, Schaan, Liechtenstein) were recently accepted for clinical use because of their high strength and fracture resistance when compared with other CAD/CAM all-ceramic materials, and can be used even for 3-unit dental bridges [9].
However, all-ceramic materials are generally brittle by nature and more vulnerable to fracture [10]. CAD/CAM resin-composite materials exhibit mechanical properties that approximate those of human dentin, with higher flexural strength and modulus of resilience, and lower flexural modulus values, compared with feldspar ceramic [11], but inferior flexural strength, flexural modulus, and fracture toughness when compared with LDGC [12]. Consisting of a particulate-filled composite resin containing nanometer-sized silica and zirconia particles and clusters (80 weight%), RNC (Lava Ultimate; 3M ESPE, St. Paul, MN, USA) is less brittle than LDGC, which suffers more from catastrophic and non-reparable fracture patterns, because of the flexibility of the resin [13].
Clinical researchers have focused on all-ceramic CAD/CAM restorations with observation of their long-term survival [14,15]. However, the studies of RNC blocks have focused on testing the material’s physical and chemical properties in the laboratory, with little investigation of its clinical performance [16,17].
This prospective cohort study aimed to observe the clinical performance of RNC partial crowns in restoring endodontically treated posterior teeth over a 3-year period. The null hypothesis was that (1) there would be no notable difference in the survival rate between RNC and LDGC groups over 3 years; and (2) there would be no notable difference between the 3-year clinical performance of RNC and LDGC restorations, based on Fédération dentaire internationale (FDI) World Dental Federation clinical criteria.
Material and Methods
The present study was approved by the Ethics and Research Committee of the First Affiliated Hospital of Xinjiang Medical University (approval no: 20170309-01). All individuals were enrolled at the dentistry faculty clinic of Xinjiang Medical University from 1 March 2017 to 28 February 2018. Eligible patients were informed about the objectives, procedures, treatment stages, dental materials to be used, potential risks, long-term followup, and their right to decline to participate or withdraw their participation (Table 1).
Sample size was calculated with the use of PASS (NCSS, LLC, Kaysville, UT, USA) software. To obtain the f=0.25 effect difference and reach 80% power and an alpha error <0.05, we required at least 60 restorations in each group.
The randomization process was carried out by a staff member not involved in this study, using a computer-generated form. Details of the teams assigned were recorded on cards, which came in sequentially numbered sealed opaque envelopes. The cards were prepared by a staff member who did not participate in our study.
The shade of teeth was determined using the tooth guide 3D-Master (Vita Zahnfabrik, Rauter GmbH, Bad Sackingen, Germany). Digital photographs (Canon EOS 50D, Tokyo, Japan) were taken with the help of an intraoral photo mirror.
One operator with more than 5 years of clinical experience prepared the endodontically treated posterior teeth for restorations using the same methods and principles [18]. A conical diamond rotary instrument (TF-14/TR-19, Mani, Tokyo, Japan) was used to flatten the cavity floor and remove undercuts. The temporary filling was removed with a round bur (BR-31, Mani, Tokyo, Japan). All caries and unsupported enamel edges were removed. Different patterns of gingival retraction cords (Ultrapack, Ultradent Products Inc., South Jordan, UT, USA) were used before tooth preparation if the enamel margin was below the gingiva. All cavity edges were terminated on the enamel and all internal surfaces were terminated in dentin. The enamel margins were not beveled. Weak walls of less than 2 mm were eliminated. The occlusal surface was reduced by 2-mm over functional cusps and at least 1.5 mm over nonfunctional cusps. Composite resin (FiltekTM Z350XT, 3M ESPE) was used to fill the pulp cavity to a depth of more than 3 mm to ensure a space of 2.0–2.5 mm. It was required that the prepared cavities contain no sharp internal angles, with clear lines and a 1-mm-wide subgingival shoulder.
Digital model impressions were taken using a Cerec Omnicam intraoral scanner (Sirona Dental Systems GmbH, Bensheim, Germany). The data were sent to the laboratory via Sirona Connect software 4.3. The restorations were designed according to the margins drawn by CAD, using identical parameters. All restorations were milled in a Cerec inLab MC XL milling machine (Cerec 3D, Sirona Dental Systems GmbH). LDGC restorations were glazed (Vita Akzent, Vita Zahnfabrik, Rauter GmbH) while the pits and fissures of the RNC restorations were stained, following the manufacturer’s instructions, and polished with discs, polishing rubbers, and polishing paste (Sof-Lex, 3M ESPE).
During the try-in session, the anatomical form, marginal adaptation, and color were assessed. The intaglios of the restorations were pretreated according to the manufacturer’s instructions as follows:
The LDGC restoration was etched with hydrofluoric acid (9% Porcelain Etch; Ultradent Products Inc.) for 20 seconds, then washed with a large amount of flowing water for 60 seconds.
The RNC restoration was sandblasted with air abrasion with Al2O3 (Rønvig Dental Mfg, Daugaard, Denmark) of particle size ≤50 μm at a pressure of 2 bar for a duration of 20 seconds.
Both restorations were placed in the ultrasonic oscillator (Guanboshi, Shenzhen, China) with 95% ethanol, and washed for 10 minutes to fully remove the etch agent and debris on the surface of the restorations. After removal, the surface was washed with copious flowing water for 30 seconds and blown dry with oil-free compressed air.
The surface was spread with a thin layer of silane (Ultradent Products Inc.) which was left in place for 60 seconds, then dried with oil-free compressed air. The restoration was placed in a clean box and set aside.
For cementation, the teeth were isolated with rubber dams (Hygienic Dental Dam, Coltène/Whaledent Inc., OH, USA). The restorations were seated with moderate pressure with adhesive resin cement using an etch-and-rinse adhesive system (Variolink® N; Ivoclar Vivadent, Schaan, Liechtenstein) or a self-etching adhesive system (Multilink® N; Ivoclar Vivadent), and then polymerized for 5 seconds per quarter surface with a light-emitting diode curing unit (Bluephase, VALO Cordless, Ultradent Products Inc.). Excess luting agent was carefully removed with a scaler and dental floss. Finally, each side of the restoration was light-polymerized for 60 seconds.
At the end of the procedure, the occlusion and occlusal contacts were adjusted with marking paper. The restoration was polished using sequential steps of abrasiveness with rubber points using a low-speed handpiece.
The restorations were evaluated by 2 dentists who were not involved in the clinical procedure. The Cohen kappa values between examiners ranged from 0.8 to 0.9. The restorations were examined at baseline and subsequently at 6, 12, 18, 24, and 36 month followup visits by the above 2 trained dentists. All restorations were clinically evaluated with an intraoral mirror, a probe, and images. Each restoration was examined according to FDI World Dental Federation clinical criteria [19,20], including 3 main groups and 15 criteria. Photos of RNC restoration of the maxillary left second premolar can be seen in Figure 1A–1C and photos of LDGC restoration of the maxillary right second molar can be seen in Figure 2A–2C.
All statistical analyses were performed with SPSS statistical software (version 26; IBM Corp., Armonk, NY, USA). The survival rates of the 2 materials, including data relating to fractured restorations or teeth, debonding of restorations, recurrence of caries, and biological complications [21,22], were analyzed by the Kaplan-Meier procedure and the log-rank test.
Descriptive statistics were used to describe patterns of failure and the distributions of the evaluated criteria. Because the 2 groups did not exhibit a normal data distribution (K-S test), non-parametric tests were used. Comparison of the LDGC and RNC restorations for each category of FDI World Dental Federation clinical criteria at baseline and at 36 months was performed with Mann-Whitney tests. Differences in the materials at baseline and at each recall time (6, 12, 18, 24, and 36 months) were tested with Friedman’s repeated measures analysis and significant differences between the different time points were analyzed by the Nemenyi post-hoc test.
To understand the main pattern of failure, several variables were evaluated as possible covariates of the time-dependent survival rates; namely, sex, age, tooth distribution, arch distribution, coverage of cusps, restoration material, and cement. The influence of potential risk factors on the main pattern of failure was studied by univariate analysis including Cox regression or log-rank tests.
In all tests, the probability level for statistical significance was α=0.05.
Results
A total of 132 restorations were placed for 128 participants, including 66 RNC restorations (in 64 participants) and 66 LDGC restorations (in 64 participants). Four participants received 2 restorations each. Seven participants did not take part in the followup examinations. One young participant (1 LDGC) went abroad at the time of the 6-month recall; 1 participant (1 LDGC) moved to another city at the time of the 12-month recall; 2 participants (1 LDGC and 1 RNC) were uncontactable for the 18-month recall; and 3 participants (2 LDGC and 1 RNC) chose not to participate in the 24-month recall. Demographic and baseline data are shown in Table 2.
Fifteen restorations failed (11 RNC and 4 LDGC) due to debonding (n=10, 9 RNC and 1 LDGC), restoration fracture (n=4, 1 RNC and 3 LDGC), or abutment tooth fracture (n=1, 1 RNC) during the followup periods (Table 3). No biological complications or secondary caries were reported.
Kaplan-Meier analysis showed that the 3-year survival rate of the RNC group was 83.1% (95% CI, 78.4–87.8%), and that of the LDGC group was 93.5% (95% CI, 90.4–96.6%) (Figure 3). The log-rank test indicated that there was no significant difference between the 2 groups (chi-square=3.512;
In accordance with FDI World Dental Federation clinical criteria, the clinical properties of the restorations were calibrated at baseline and at followup visits at 6, 12, 18, 24, and 36 months (Table 4). With regard to esthetic properties, the performance of both materials had deteriorated after 3 years of clinical service without statistical significance, except for the parameter of “surface luster” (
For functional properties, no significant differences in the parameters were found in either the RNC or LDGC group, except for the parameter of “occlusal contour and wear” (
There was no notable difference between the 2 groups for the parameter of “patient’s opinion”. For both groups, the scores of this property increased significantly at each recall time.
In terms of biological properties, both materials exhibited increased scores for the parameter of “periodontal response” at the 12-month recall, although this was not statistically significant (
The main pattern of failure was debonding. The survival rates of the restorations, according to various categorical clinical factors, are shown in Table 5. The risk factor of “restoration material” was the only potential risk factor that seemed to influence debonding. RNC restorations were more likely to debond than LDGC restorations (hazard ratio=9.22 [1.17, 72.74],
Discussion
The present study observed the clinical performance of RNC versus LDGC partial crowns, based on FDI criteria, over a 3-year period. It was found that a total of 15 restorations failed, with failure patterns of debonding, restoration fracture, and tooth fracture. There was no difference in the survival rate between the RNC and LDGC groups over the 3-year period, which leads us to accept the first null hypothesis. Systematic reviews [21,22] reported that the 5-year survival rate for ceramic onlays is 71% to 98.5%, with patterns of failure including fracture, debonding (loss of retention), secondary caries, endodontic complications, periodontal complications, and extraction of the restored tooth. Oz et al [23] documented the survival rate of RNC restorations as 86.8% after a mean time of 45 months. Our findings are consistent with these results.
During our followup, the main failure pattern for the RNC group was debonding (n=9). We also analyzed the potential risk factors for debonding of the RNC group. Restoration material was a risk factor for debonding, but sex, age, tooth distribution, arch distribution, coverage of cusps, and cement were not. Meltem et al [24] compared the bonding performance of CAD/CAM restorative materials and found that the LDGC group recorded the highest bond strength (100.31±10.7 MPa) and the RNC group recorded the lowest values (23.63±9.0 MPa). A previous study [25] noted that CAD/CAM resin blocks are manufactured under high pressure and temperature to guarantee their superior physical and mechanical properties. However, this standardized polymerization procedure caused the surface of the RNC blocks to be deficient in carbon–carbon double bonds, to which the resin cement bonds [26]. In 2015, 3M ESPE withdrew the indication of Lava Ultimate RNC for full crowns because of failures resulting from the high debonding rate [27].
For the LDGC group, 3 restoration fractures and 1 debonding occurred. However, one RNC onlay with a relatively high level of toughness fractured in our study. After carefully observing the bulk fracture and the abutment tooth, we found that much cement had been left on the tooth. We presumed that the fractured RNC onlay might have partly debonded at first, then fractured. It is difficult to determine the reason for restoration fracture in terms of physical and mechanical properties because of the multiple factors involved.
CAD/CAM dental materials, whether all-ceramic [28] or resin-composite [29] materials, necessitate adequate surface pretreatment for bonding with resin luting cements. Hydrofluoric acid etching followed by silanization can confer high bond strength to glass-based ceramics [30], while the intaglio of most resin-composite CAD/CAM restoration requires sandblasting followed by silanization [31–33]. Sandblasting increases the surface roughness and surface free energy of RNC, resulting in better mechanical attachment of the luting agent and high bond strength [34]. The silane coupling agent combines with Si-OH on the surface of silica-based material to form siloxane bonds, and polymerizes with double carbon bonds in the luting cement to achieve chemical bonding [35]. However, some literature suggests that silanization on RNC may have less effect on bond strength, possibly owing to the scarcity of silanizable fillers, or its nano-structure [36,37]. Sandblasting in combination with a universal bonding agent [38] or with a resin primer containing methyl-methacrylate [39] is thought to produce a better bond than silane coupling agents. Clinical studies on the comparison between the 2 chemical protocols are still lacking, and further studies are needed.
One tooth with an RNC onlay developed major chipping of the enamel at 28 months in our study. The fracture occurred on a functional cusp with 2 mm of thin-walled dentin. We fabricated a new overlay for the patient, with total cuspal coverage.
In our study, the properties of “surface luster” and “occlusal contour and wear” differed between the 2 groups at the 36-month recall. Thus, the second hypothesis was rejected. We observed variations in the esthetic properties of the RNC group over time. Deterioration of the color match and translucency, margin staining, surface luster, and surface staining were the factors that resulted in the difference. The LDGC material tended to become more brightly opaque, while the RNC material gradually became darker. These findings are in accordance with an in vitro study that found that the changes in color and translucency were affected by the material and the staining solution, with LDGC exhibiting greater color stability than RNC [40]. Souza et al [41] also reported that only 45% of the LDGC and RNC onlays retained a good color match in shade and/or translucency within one year’s observation. They considered that these changes could have resulted from difficulties in imitating the esthetics and optical properties of enamel and dentin. An in vitro study has shown that the bonding interface between the CAD/CAM restoration intaglio and the resin luting cement affected the color stability of LDGC and RNC blocks, and that the color stability of RNC was inferior to that of LDGC at any thickness [42]. After the 3-year observation period, 3 RNC restorations exhibited normal wear only slightly different from that of enamel and another 3 RNC restorations had a wear rate different from that of enamel but within the limits of biological variation. This may be owing to the fact that RNC restorations are more prone to surface wear than all-ceramic restorations [43].
The participants’ periodontal condition had improved at the 12-month recall. This improvement might have occurred because the occlusal function of the defective teeth had been restored. Additionally, instruction about oral health practices and regular periodontal cleaning are necessary. For posterior teeth, the patient needs to feel confident about the functional properties of the restoration so that they feel comfortable chewing with the restoration over time.
Many studies have found no difference in clinical success between direct and indirect resin-composite restorations, regardless of the type of material, whether the tooth was restored or endodontically treated, or whether it was an anterior or posterior tooth [44,45]. Fennis et al [46] reported that the 5-year survival rate of resin-composite restorations was 86.6%, with direct and indirect restorations having rates of 89.9% and 83.2%, respectively, with the main mode of failure being adhesive failure. This is in agreement with our finding that the 3-year survival rate of the RNC group was 83.1%. Both CAD/CAM composites and direct composite materials are prone to varying degrees of discoloration and translucency changes after contact with staining beverages, but CAD/CAM composites are more color stable [47] because they maximize polymer crosslinking due to standardized and controlled industrial processes using high temperature and/or high pressure polymerization [48]. Tunac et al [44] reported that direct composite restorations exhibited worse surface luster than RNC restorations at the end of the second year, but there was no difference in marginal staining.
One limitation of the present study is that it did not use a split-mouth design, which would have meant that the observation group and the control group were influenced by the same oral environment (food, drink, or drugs), thus eliminating inter-subject variability. Another limitation is the loss of patients to followup. Future studies should include a larger number of patients in a long-term investigation.
Conclusions
The survival rate of CAD/CAM partial crowns was similar between the RNC and LDGC groups. All patients were satisfied with their restorations. However, the clinical performance of the 2 groups varied according to esthetic and occlusal wear properties, based on FDI World Dental Federation clinical criteria. The main failure pattern was debonding of the RNC material.
Figures
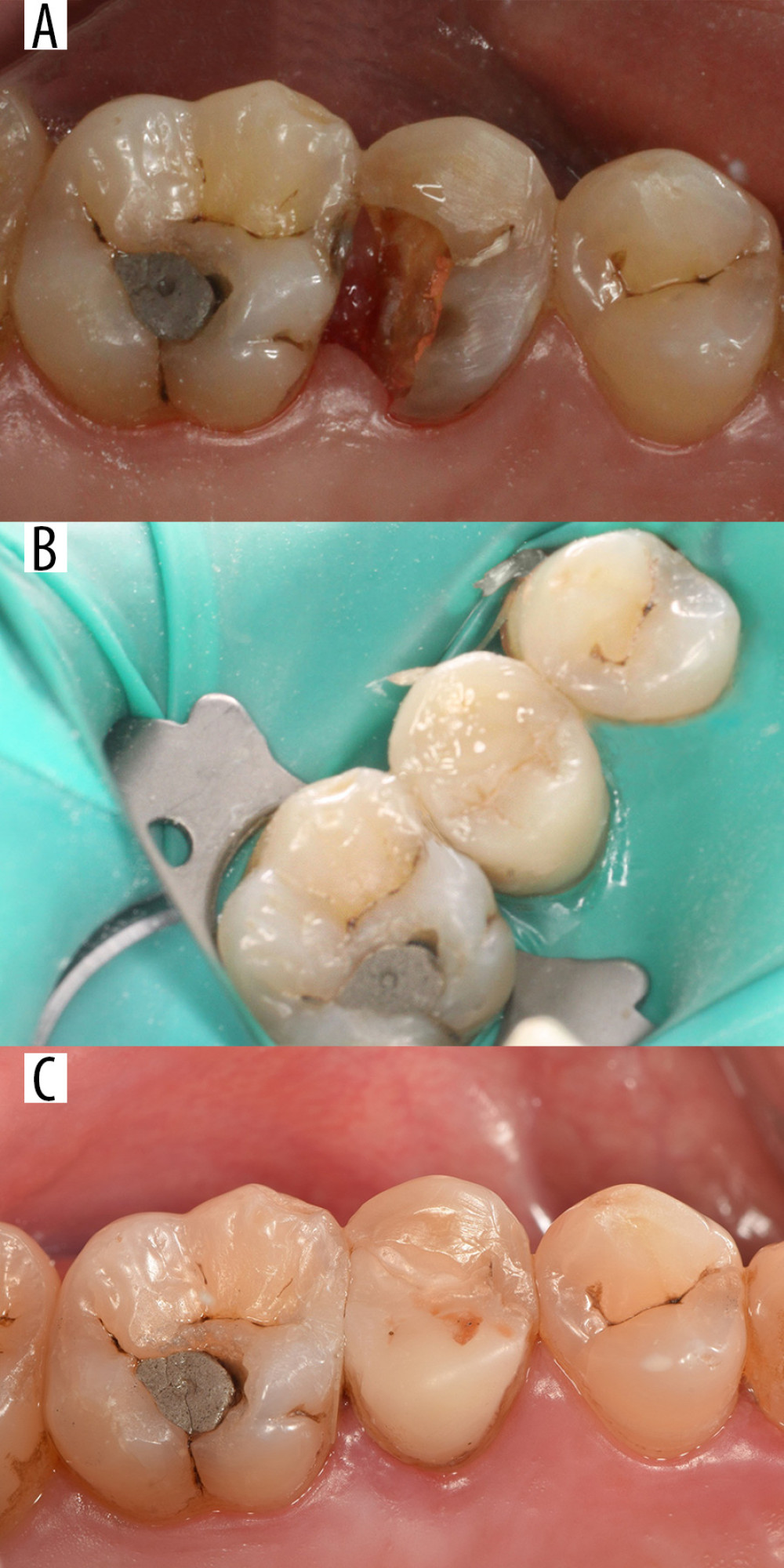 Figure 1. Tooth 25 restored with a resin nanoceramic (RNC) onlay. (A) Before cavity preparation. (B) Restoration after bonding (baseline). (C) Restoration after 36 months.
Figure 1. Tooth 25 restored with a resin nanoceramic (RNC) onlay. (A) Before cavity preparation. (B) Restoration after bonding (baseline). (C) Restoration after 36 months. 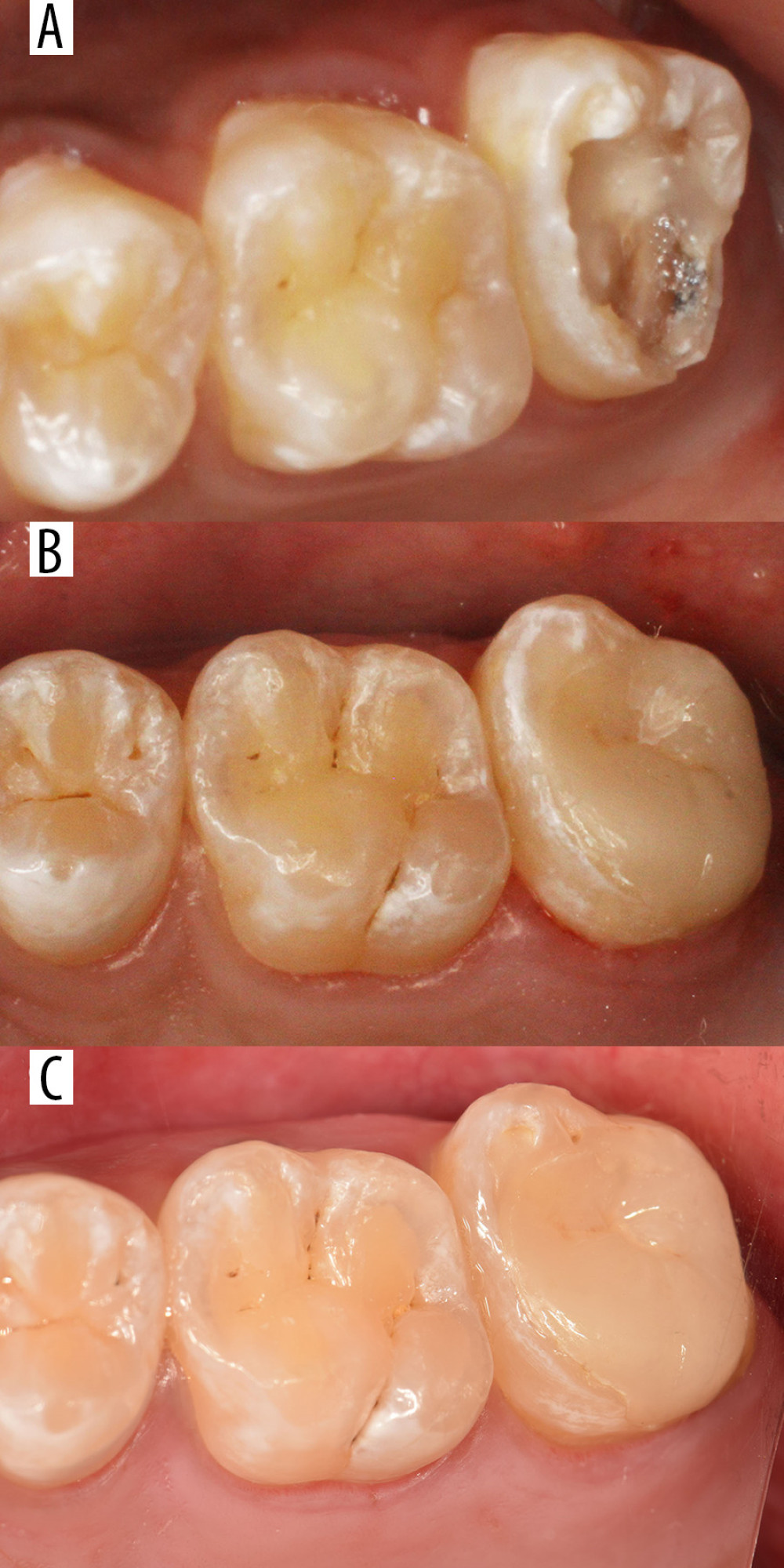 Figure 2. Tooth 27 restored with a lithium disilicate-based glass ceramic (LDGC) onlay. (A) Before cavity preparation. (B)4Restoration after bonding (baseline). (C) Restoration after 36 months.
Figure 2. Tooth 27 restored with a lithium disilicate-based glass ceramic (LDGC) onlay. (A) Before cavity preparation. (B)4Restoration after bonding (baseline). (C) Restoration after 36 months. 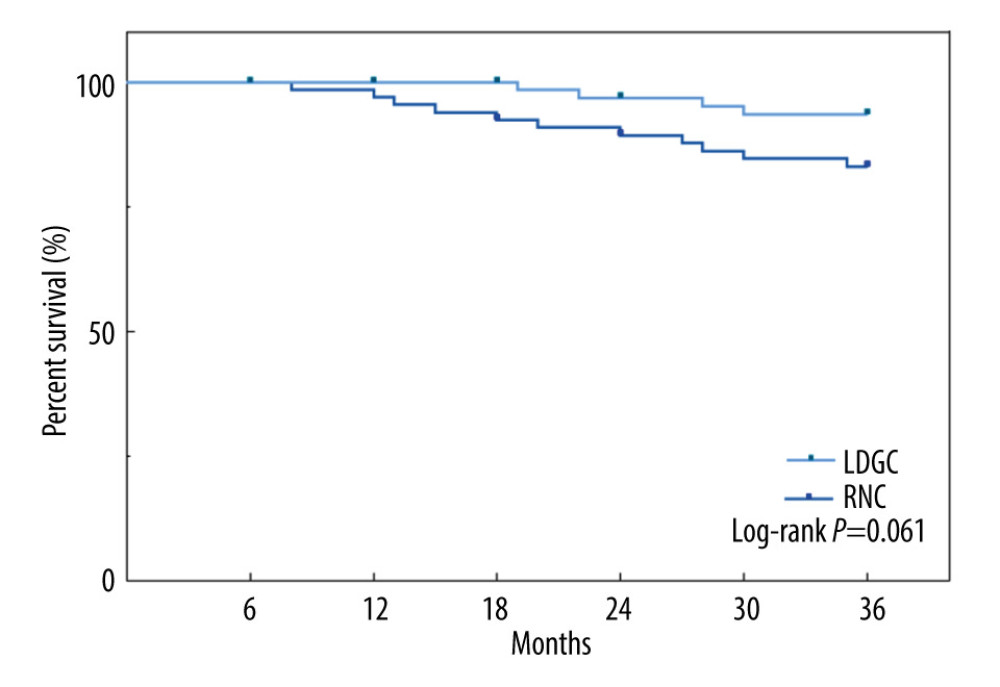 Figure 3. Kaplan-Meier cumulative survival rate over 3 years of partial crowns made of RNC and LDGC (Prism 8.0; GraphPad Software Inc, La Jolla, CA, USA). RNC – resin nanoceramic; LDGC – lithium disilicate-based glass ceramic.
Figure 3. Kaplan-Meier cumulative survival rate over 3 years of partial crowns made of RNC and LDGC (Prism 8.0; GraphPad Software Inc, La Jolla, CA, USA). RNC – resin nanoceramic; LDGC – lithium disilicate-based glass ceramic. 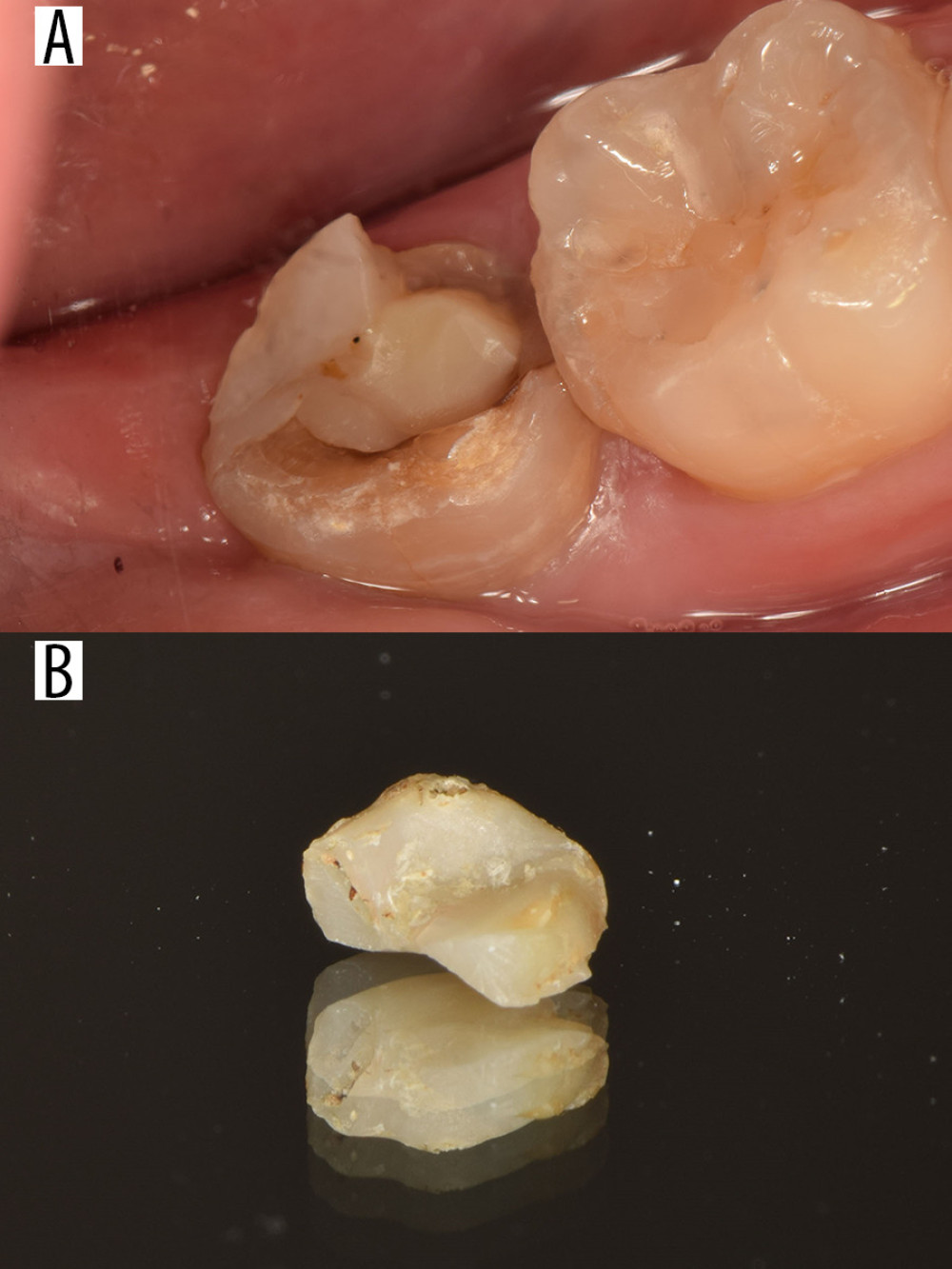 Figure 4. Failed case. Tooth 37 was restored with a resin nanoceramic (RNC) onlay, which fractured after 35 months. (A) Intraoral photograph of the onlay, which fractured after 35 months. (B) Photograph of the fractured onlay.
Figure 4. Failed case. Tooth 37 was restored with a resin nanoceramic (RNC) onlay, which fractured after 35 months. (A) Intraoral photograph of the onlay, which fractured after 35 months. (B) Photograph of the fractured onlay. Tables
Table 1. Eligibility criteria.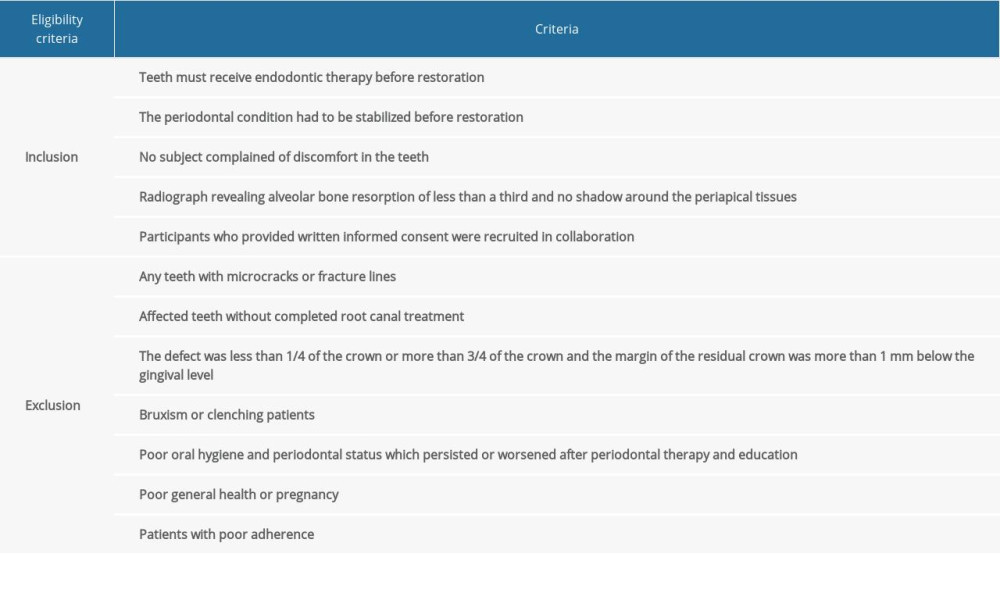 Table 2. Demographic and baseline data.
Table 2. Demographic and baseline data.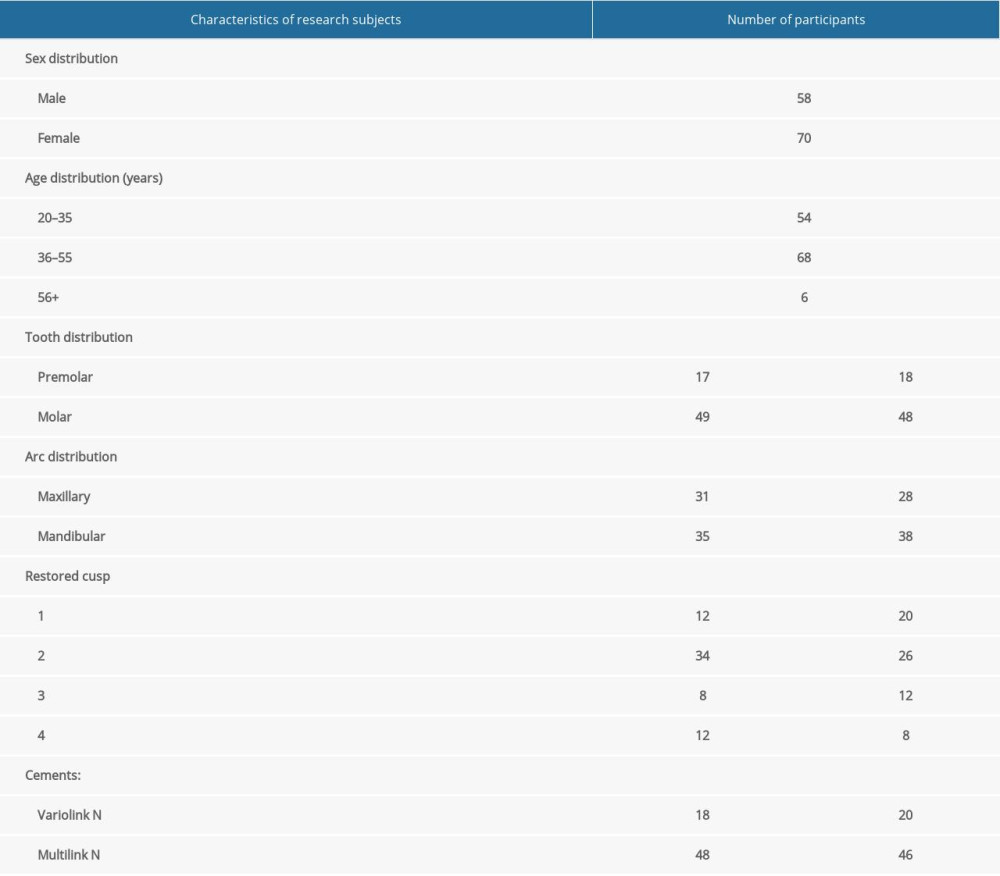 Table 3. Descriptive analysis of failed restorations.
Table 3. Descriptive analysis of failed restorations.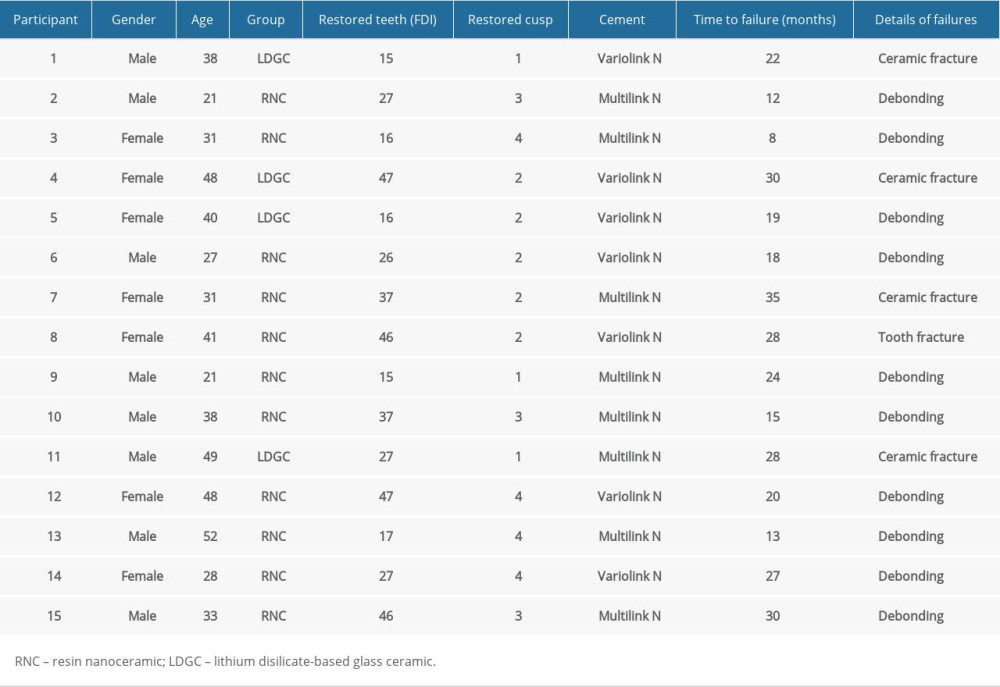 Table 4. Number of restorations evaluated for each group, classified according to the FDI Criteria, at baseline and at followup visits, at 6, 12, 18, 24, and 36 months.
Table 4. Number of restorations evaluated for each group, classified according to the FDI Criteria, at baseline and at followup visits, at 6, 12, 18, 24, and 36 months.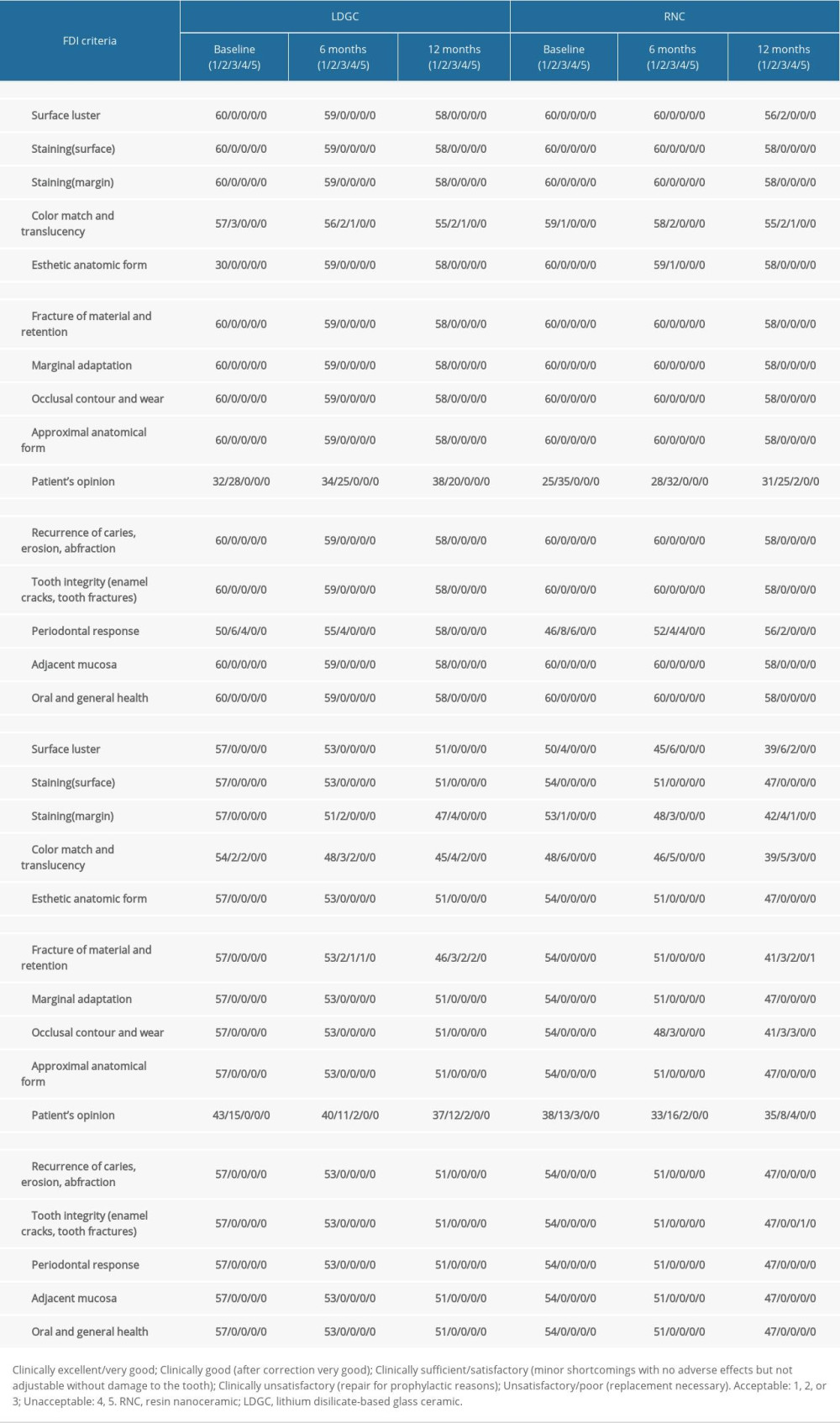 Table 5. Survival (failure=debonding) distributions and test results according to categorical clinical factors.
Table 5. Survival (failure=debonding) distributions and test results according to categorical clinical factors.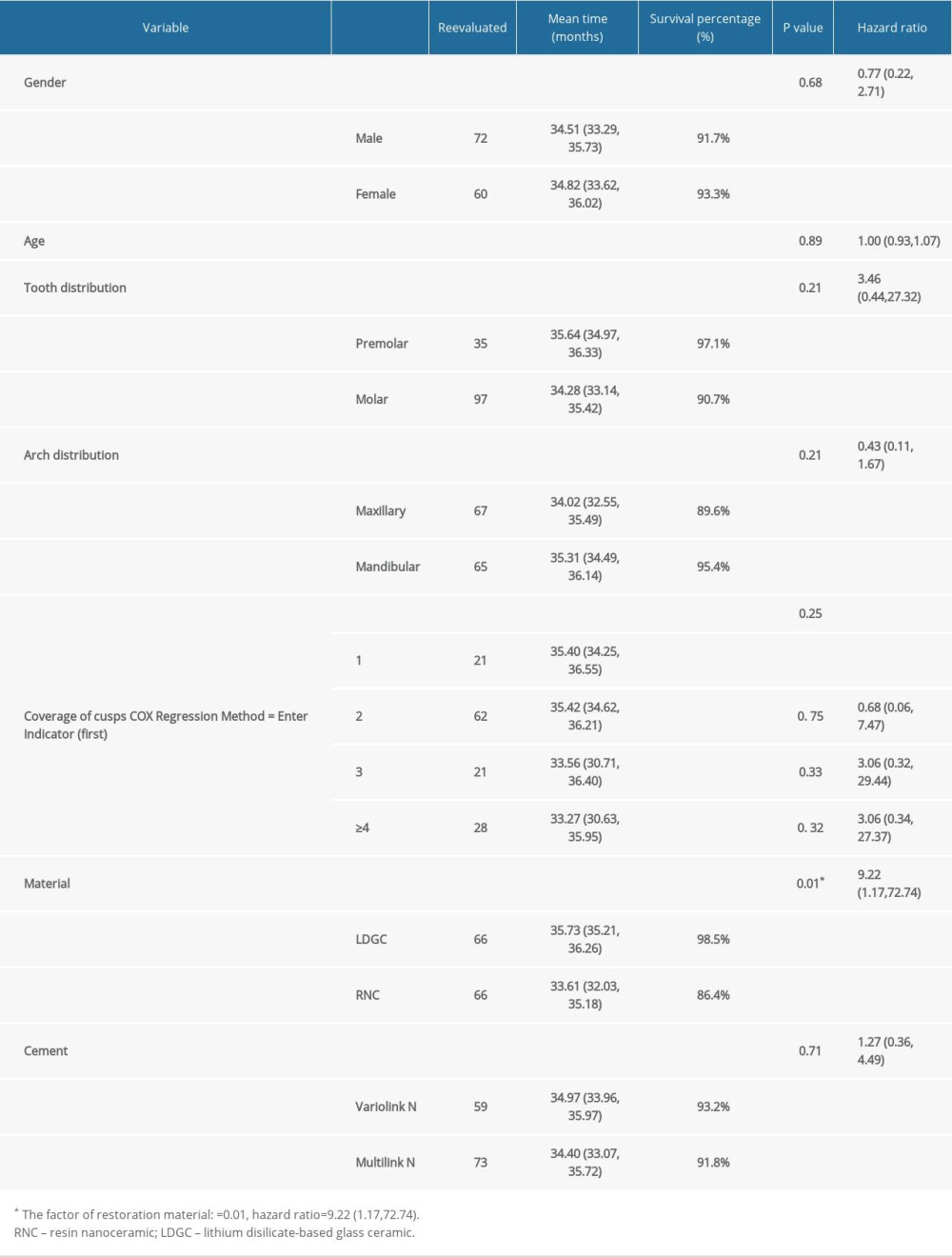
References
1. Faria AC, Rodrigues RC, de Almeida Antunes RP, Endodontically treated teeth: Characteristics and considerations to restore them: J Prosthodont Res, 2011; 55(2); 69-74
2. Bitter K, Meyer-Lueckel H, Fotiadis N, Influence of endodontic treatment, post insertion, and ceramic restoration on the fracture resistance of maxillary premolars: Int Endod J, 2010; 43(6); 469-77
3. de V, Habekost L, Camacho GB, Azevedo EC, Demarco FF, Fracture resistance of thermal cycled and endodontically treated premolars with adhesive restorations: J Prosthet Dent, 2007; 98(3); 186-92
4. Politano G, Van Meerbeek B, Peumans M, Nonretentive bonded ceramic partial crowns: concept and simplified protocol for long-lasting dental restorations: J Adhes Dent, 2018; 20(6); 495-510
5. Kassis C, Khoury P, Mehanna CZ, Effect of inlays, onlays and endocrown cavity design preparation on fracture resistance and fracture mode of endodontically treated teeth: An in vitro study: J Prosthodont, 2021; 30(7); 625-31
6. Angeletaki F, Gkogkos A, Papazoglou E, Kloukos D, Direct versus indirect inlay/onlay composite restorations in posterior teeth. A systematic review and meta-analysis: J Dent, 2016; 53; 12-21
7. Marchesi G, Camurri Piloni A, Nicolin V, Chairside CAD/CAM materials: Current trends of clinical uses: Biology (Basel), 2021; 10(11); 1170
8. Li RW, Chow TW, Matinlinna JP, Ceramic dental biomaterials and CAD/CAM technology: State of the art: J Prosthodont Res, 2014; 58(4); 208-16
9. Pieger S, Salman A, Bidra AS, Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: A systematic review: J Prosthet Dent, 2014; 112(1); 22-30
10. Kassem AS, Atta O, El-Mowafy O, Fatigue resistance and microleakage of CAD/CAM ceramic and composite molar crowns: J Prosthodont, 2012; 21(1); 28-32
11. Awada A, Nathanson D, Mechanical properties of resin-ceramic CAD/CAM restorative materials: J Prosthet Dent, 2015; 114(4); 587-93
12. Lucsanszky IJR, Ruse ND, Fracture toughness, flexural strength, and flexural modulus of new CAD/CAM resin composite blocks: J Prosthodont, 2020; 29(1); 34-41
13. Goujat A, Abouelleil H, Colon P, Mechanical properties and internal fit of 4 CAD-CAM block materials: J Prosthet Dent, 2018; 119(3); 384-89
14. Otto T, Up to 27-years clinical long-term results of chairside Cerec 1 CAD/CAM inlays and onlays: Int J Comput Dent, 2017; 20(3); 315-29
15. Malament KA, Margvelashvili-Malament M, Natto ZS, Comparison of 16.9-year survival of pressed acid etched e.max lithium disilicate glass-ceramic complete and partial coverage restorations in posterior teeth: Performance and outcomes as a function of tooth position, age, sex, and thickness of ceramic material: J Prosthet Dent, 2021; 126(4); 533-45
16. Chen C, Trindade FZ, de Jager N, The fracture resistance of a CAD/CAM Resin Nano Ceramic (RNC) and a CAD ceramic at different thicknesses: Dent Mater, 2014; 30(9); 954-62
17. Pivetta Rippe M, Monaco C, Missau T, Survival rate and load to failure of premolars restored with inlays: An evaluation of different inlay fabrication methods: J Prosthet Dent, 2019; 121(2); 292-97
18. Goodacre CJ, Campagni WV, Aquilino SA, Tooth preparations for complete crowns: An art form based on scientific principles: J Prosthet Dent, 2001; 85(4); 363-76
19. Hickel R, Roulet JF, Bayne S, Recommendations for conducting controlled clinical studies of dental restorative materials. Science Committee Project 2/98 – FDI World Dental Federation study design (Part I) and criteria for evaluation (Part II) of direct and indirect restorations including onlays and partial crowns: J Adhes Dent, 2007; 9(Suppl 1); 121-47 Erratum in: J Adhes Dent. 2007;9(6):546
20. Hickel R, Peschke A, Tyas M, FDI World Dental Federation: Clinical criteria for the evaluation of direct and indirect restorations-update and clinical examples: Clin Oral Investig, 2010; 14(4); 349-66
21. Abduo J, Sambrook RJ, Longevity of ceramic onlays: A systematic review: J Esthet Restor Dent, 2018; 30(3); 193-215
22. Vagropoulou GI, Klifopoulou GL, Vlahou SG, Complications and survival rates of inlays and onlays vs complete coverage restorations: A systematic review and analysis of studies: J Oral Rehabil, 2018; 45(11); 903-20
23. Oz FD, Bolay S, Canatan S, A clinical evaluation of resin nanoceramic CEREC Omnicam restorations associated with several factors: J Esthet Restor Dent, 2021; 33(4); 583-89
24. Kömürcüoğlu MB, Sağırkaya E, Tulga A, Influence of different surface treatments on bond strength of novel CAD/CAM restorative materials to resin cement: J Adv Prosthodont, 2017; 9(6); 439-46
25. Ruse ND, Sadoun MJ, Resin-composite blocks for dental CAD-CAM applications: J Dent Res, 2014; 93; 1232-34
26. Stawarczyk B, Krawczuk A, Ilie N, Tensile bond strength of resin composite repair in vitro using different surface preparation conditionings to an aged CAD/CAM resin nanoceramic: Clin Oral Investig, 2015; 19(2); 299-308
27. http//www.3m.com/3M/enUS/Dental/Products/Catalog/~?N=5144788+3294776545&rt=rud
28. Krämer N, Lohbauer U, Frankenberger R, Adhesive luting of indirect restorations: Am J Dent, 2000; 13(Spec); 60D-76D
29. Peumans M, Valjakova EB, De Munck J, Bonding effectiveness of luting composites to different CAD/CAM materials: J Adhes Dent, 2016; 18(4); 289-302
30. Kim BK, Bae HE, Shim JS, Lee KW, The influence of ceramic surface treatments on the tensile bond strength of composite resin to all-ceramic coping materials: J Prosthet Dent, 2005; 94(4); 357-62
31. http//www.gcamerica.com/lab/products/CERASMART/CERASMART12IFU.pdf
32. http//multimedia.3m.com/mws/media/747392O/lava-ultimate-restorative-instructions-for-use-english.pdf
33. http//www.shofu.de/wp-content/uploads/2016/03/BPZSHOFUBlockHC2014-09AXDEESFRGBITLTNLPLRORU.pdf
34. Yano HT, Ikeda H, Nagamatsu Y, Effects of alumina airborne-particle abrasion on the surface properties of CAD/CAM composites and bond strength to resin cement: Dent Mater J, 2021; 40(2); 431-38
35. Matinlinna JP, Lung CYK, Tsoi JKH, Silane adhesion mechanism in dental applications and surface treatments: A review: Dent Mater, 2018; 34(1); 13-28
36. Emsermann I, Eggmann F, Krastl G, Influence of pretreatment methods on the adhesion of composite and polymer infiltrated ceramic CAD-CAM blocks: J Adhes Dent, 2019; 21(5); 433-43
37. Yano HT, Ikeda H, Nagamatsu Y, Correlation between microstructure of CAD/CAM composites and the silanization effect on adhesive bonding: J Mech Behav Biomed Mater, 2020; 101; 103441
38. Castro EF, Azevedo VLB, Nima G, Adhesion, mechanical properties, and microstructure of resin-matrix CAD-CAM ceramics: J Adhes Dent, 2020; 22(4); 421-31
39. Reymus M, Roos M, Eichberger M, Bonding to new CAD/CAM resin composites: Influence of air abrasion and conditioning agents as pretreatment strategy: Clin Oral Investig, 2019; 23(2); 529-38
40. Eldwakhly E, Ahmed DRM, Soliman M, Color and translucency stability of novel restorative CAD/CAM materials: Dent Med Probl, 2019; 56(4); 349-56
41. Souza J, Fuentes MV, Baena E, Ceballos L, One-year clinical performance of lithium disilicate versus resin composite CAD/CAM onlays: Odontology, 2021; 109(1); 259-70
42. Acar O, Yilmaz B, Altintas SH, Color stainability of CAD/CAM and nanocomposite resin materials: J Prosthet Dent, 2016; 115(1); 71-75
43. Zhi L, Bortolotto T, Krejci I, Comparative in vitro wear resistance of CAD/CAM composite resin and ceramic materials: J Prosthet Dent, 2016; 115(2); 199-202
44. Tunac AT, Celik EU, Yasa B, Two-year performance of CAD/CAM fabricated resin composite inlay restorations: A randomized controlled clinical trial: J Esthet Restor Dent, 2019; 31(6); 627-38
45. de Kuijper MCFM, Cune MS, Özcan M, Gresnigt MMM, Clinical performance of direct composite resin versus indirect restorations on endodontically treated posterior teeth: A systematic review and meta-analysis: J Prosthet Dent, 2021 [Online ahead of print]
46. Fennis WM, Kuijs RH, Roeters FJ, Randomized control trial of composite cuspal restorations: Five-year results: J Dent Res, 2014; 93(1); 36-41
47. Quek SHQ, Yap AUJ, Rosa V, Tan KBC, Teoh KH, Effect of staining beverages on color and translucency of CAD/CAM composites: J Esthet Restor Dent, 2018; 30(2); E9-E17
48. Giordano R, Materials for chairside CAD/CAM-produced restorations: J Am Dent Assoc, 2006; 137(Suppl); 14S-21S
Figures
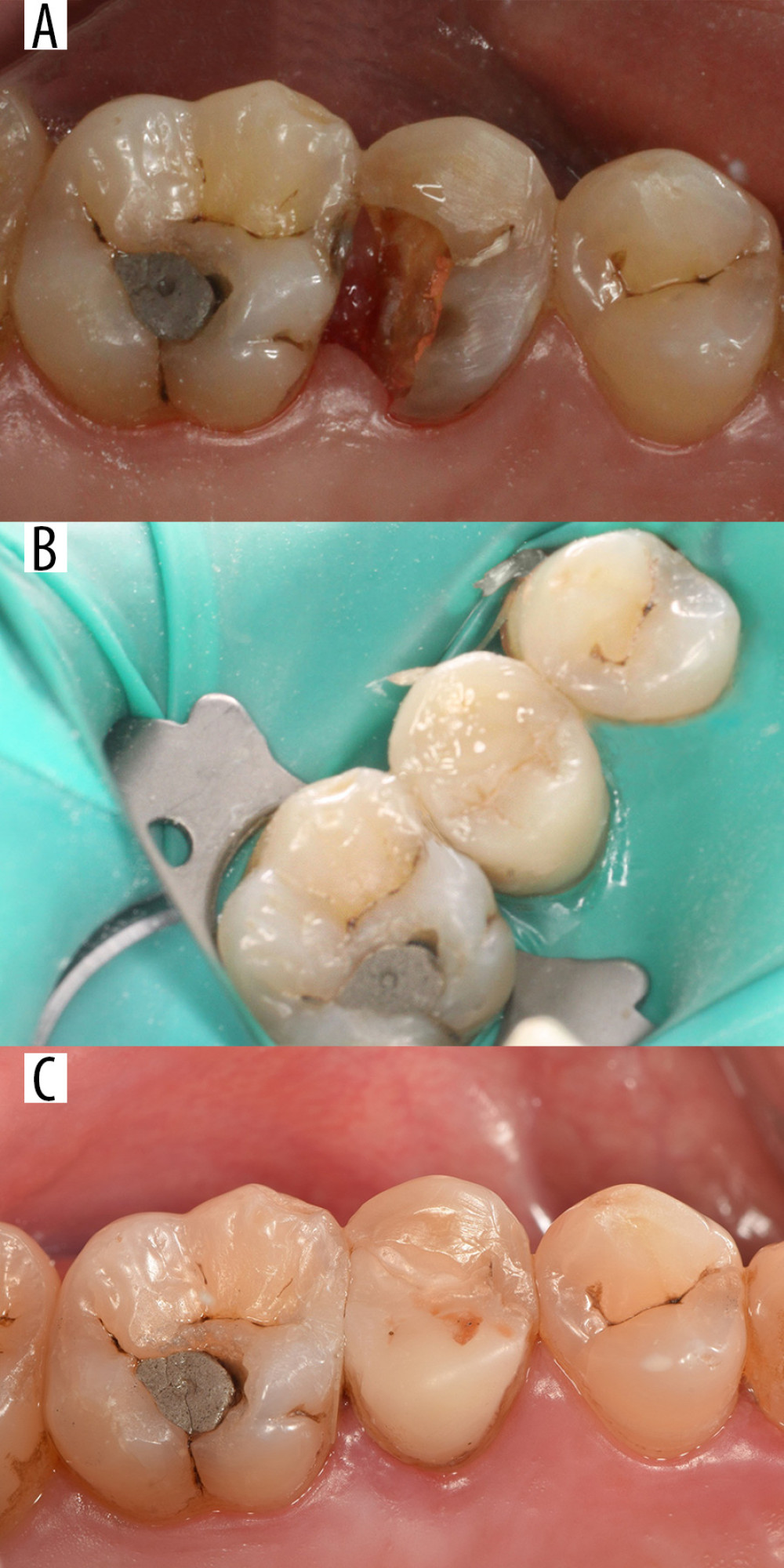 Figure 1. Tooth 25 restored with a resin nanoceramic (RNC) onlay. (A) Before cavity preparation. (B) Restoration after bonding (baseline). (C) Restoration after 36 months.
Figure 1. Tooth 25 restored with a resin nanoceramic (RNC) onlay. (A) Before cavity preparation. (B) Restoration after bonding (baseline). (C) Restoration after 36 months.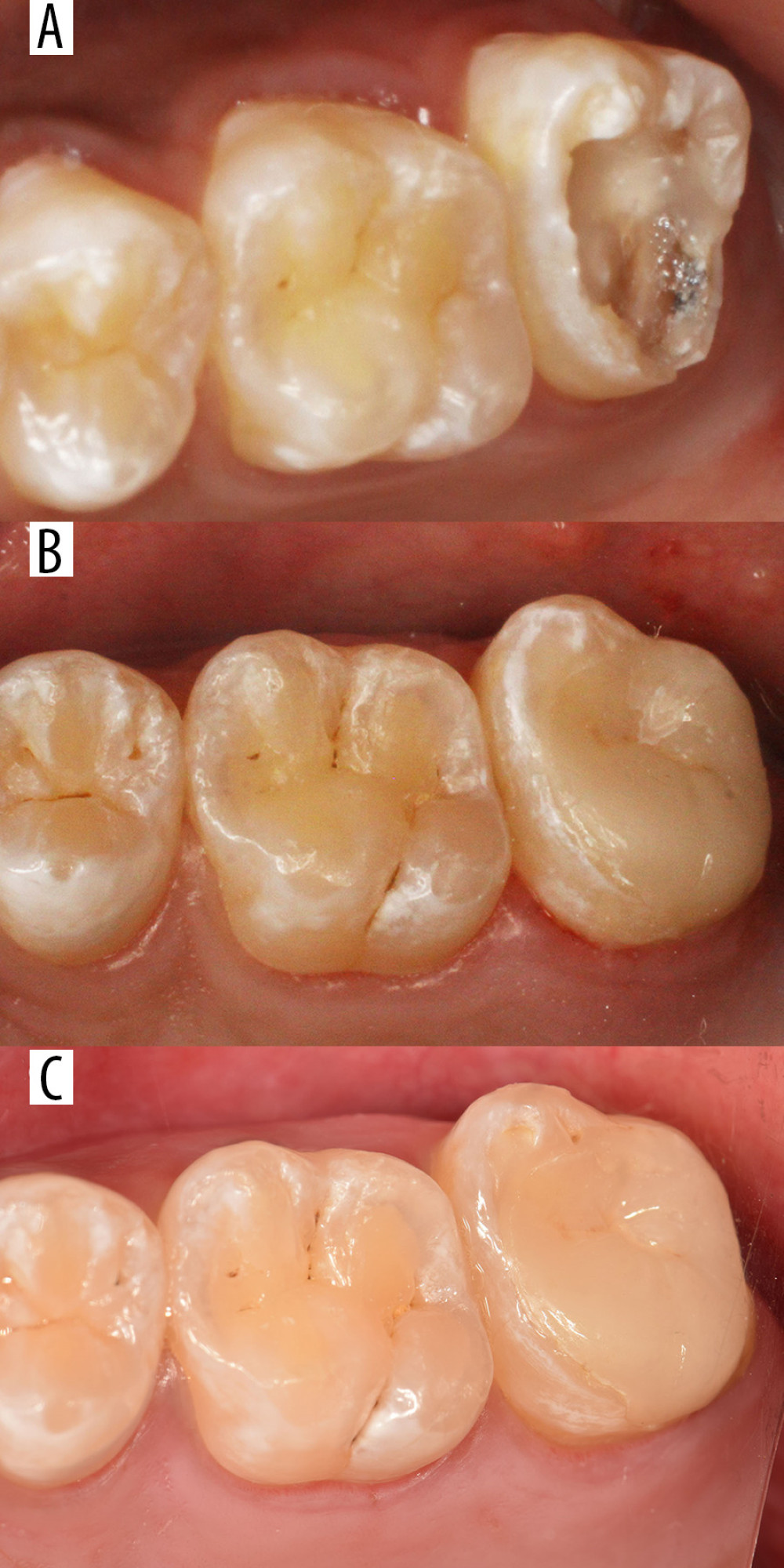 Figure 2. Tooth 27 restored with a lithium disilicate-based glass ceramic (LDGC) onlay. (A) Before cavity preparation. (B)4Restoration after bonding (baseline). (C) Restoration after 36 months.
Figure 2. Tooth 27 restored with a lithium disilicate-based glass ceramic (LDGC) onlay. (A) Before cavity preparation. (B)4Restoration after bonding (baseline). (C) Restoration after 36 months.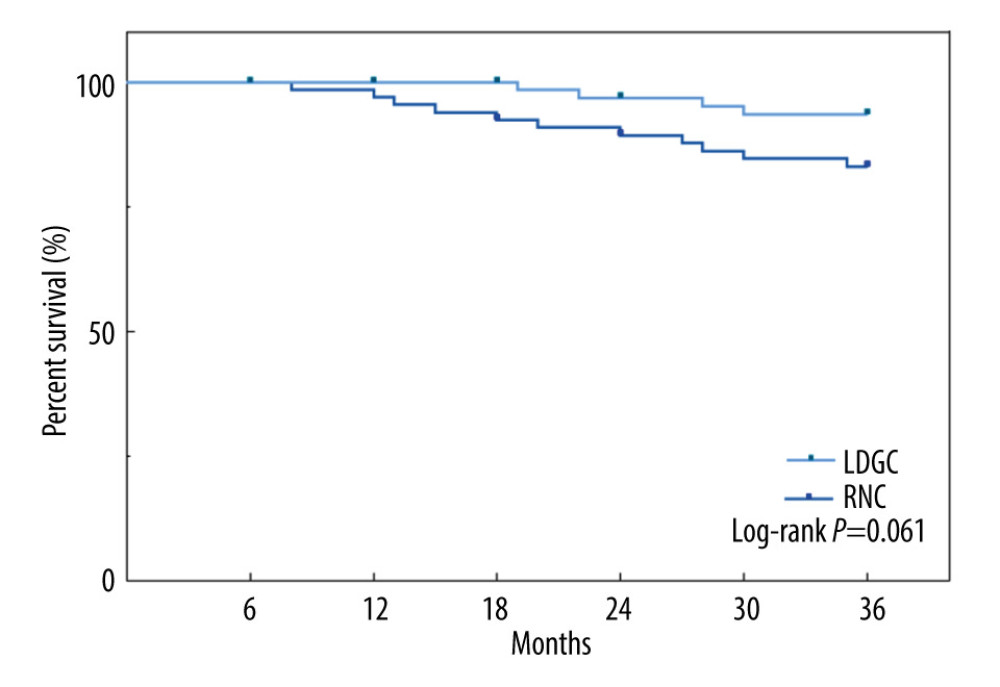 Figure 3. Kaplan-Meier cumulative survival rate over 3 years of partial crowns made of RNC and LDGC (Prism 8.0; GraphPad Software Inc, La Jolla, CA, USA). RNC – resin nanoceramic; LDGC – lithium disilicate-based glass ceramic.
Figure 3. Kaplan-Meier cumulative survival rate over 3 years of partial crowns made of RNC and LDGC (Prism 8.0; GraphPad Software Inc, La Jolla, CA, USA). RNC – resin nanoceramic; LDGC – lithium disilicate-based glass ceramic.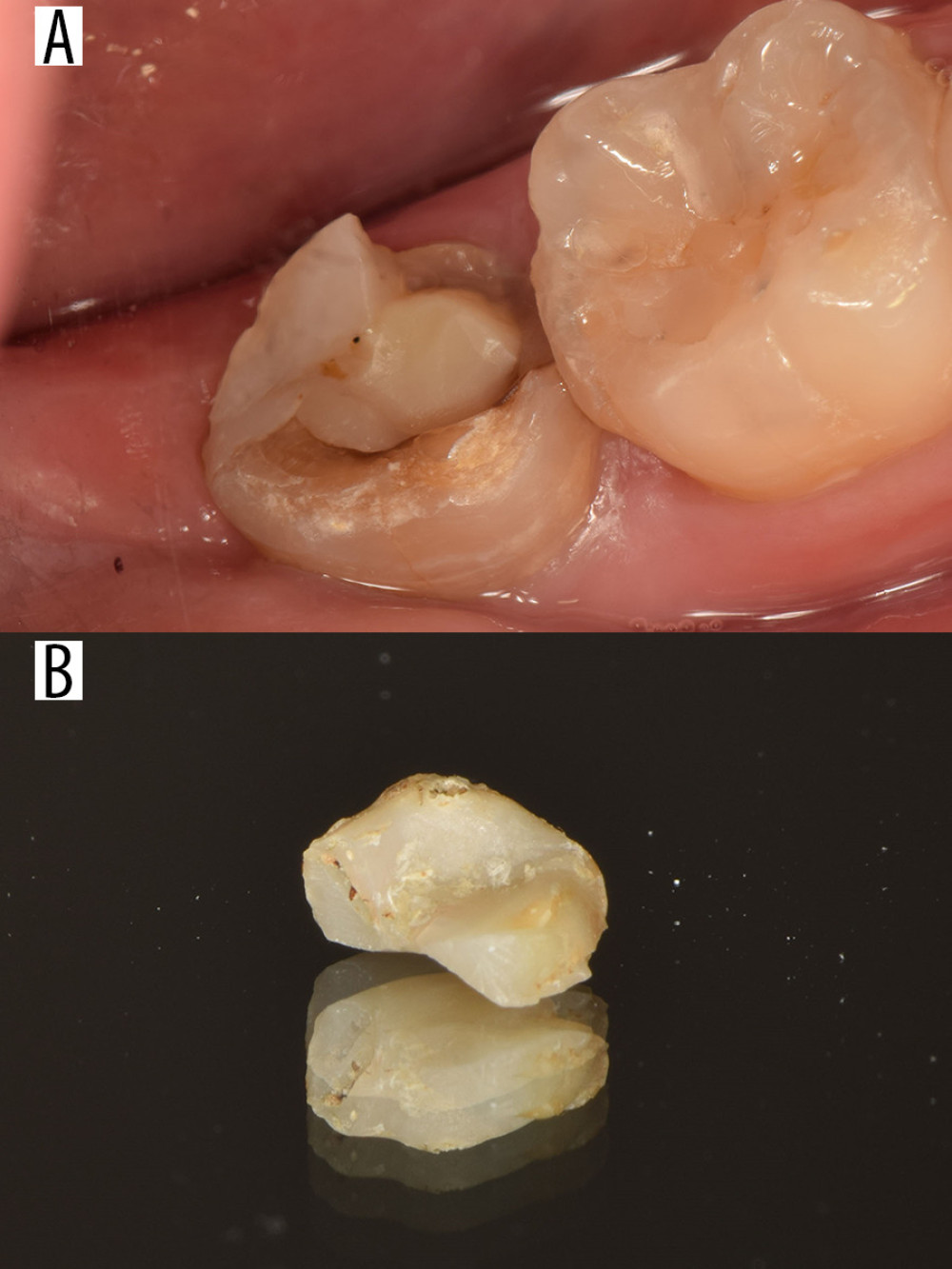 Figure 4. Failed case. Tooth 37 was restored with a resin nanoceramic (RNC) onlay, which fractured after 35 months. (A) Intraoral photograph of the onlay, which fractured after 35 months. (B) Photograph of the fractured onlay.
Figure 4. Failed case. Tooth 37 was restored with a resin nanoceramic (RNC) onlay, which fractured after 35 months. (A) Intraoral photograph of the onlay, which fractured after 35 months. (B) Photograph of the fractured onlay. Tables
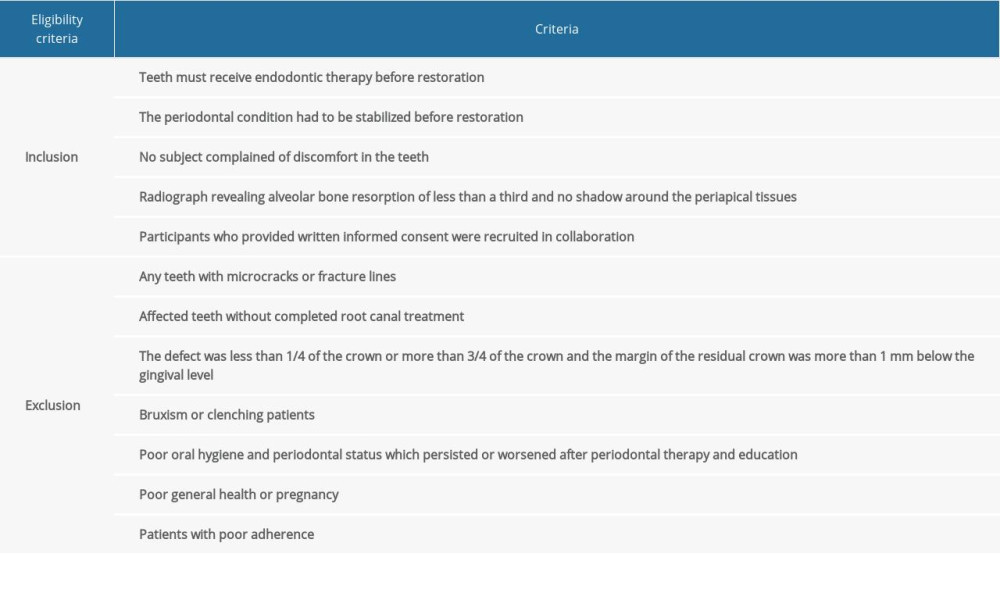 Table 1. Eligibility criteria.
Table 1. Eligibility criteria.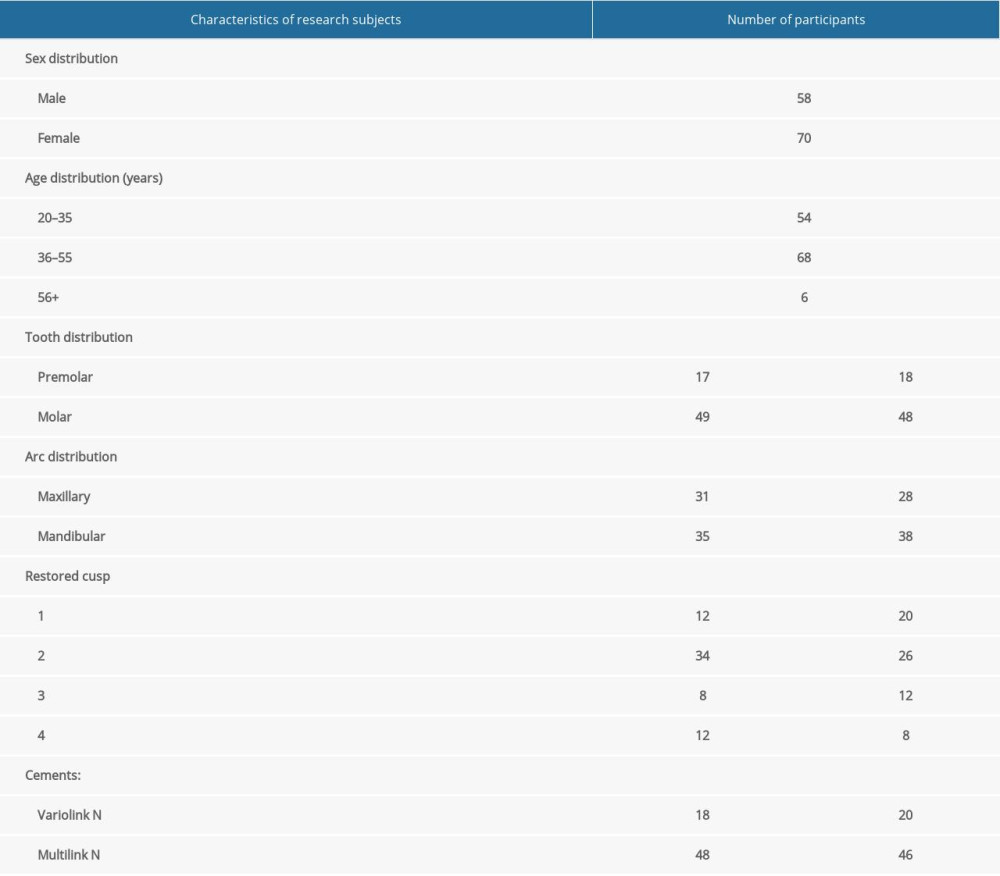 Table 2. Demographic and baseline data.
Table 2. Demographic and baseline data.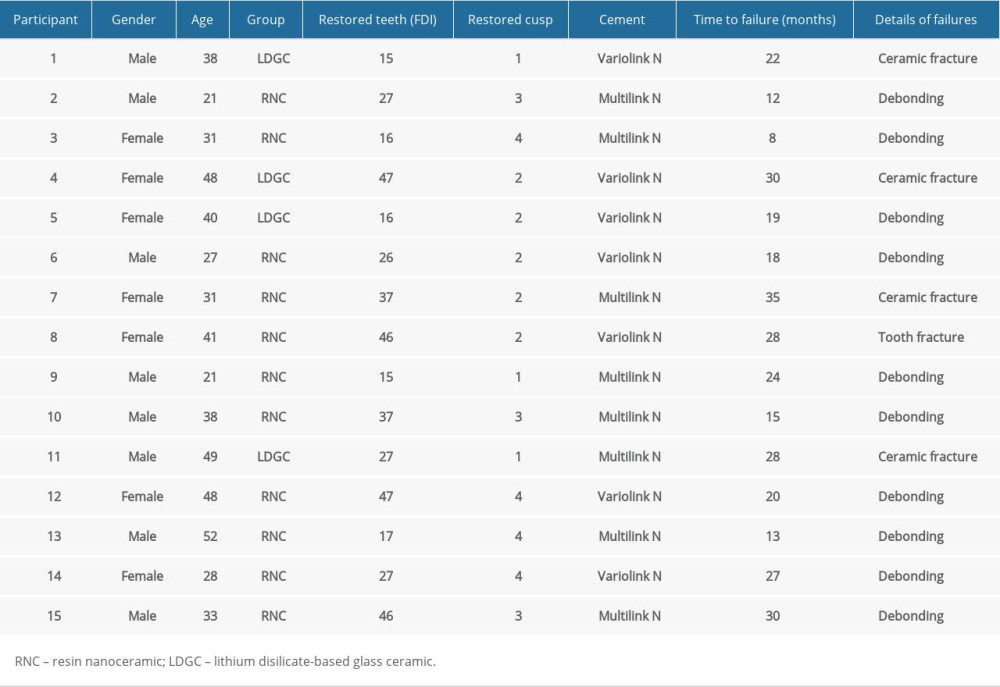 Table 3. Descriptive analysis of failed restorations.
Table 3. Descriptive analysis of failed restorations.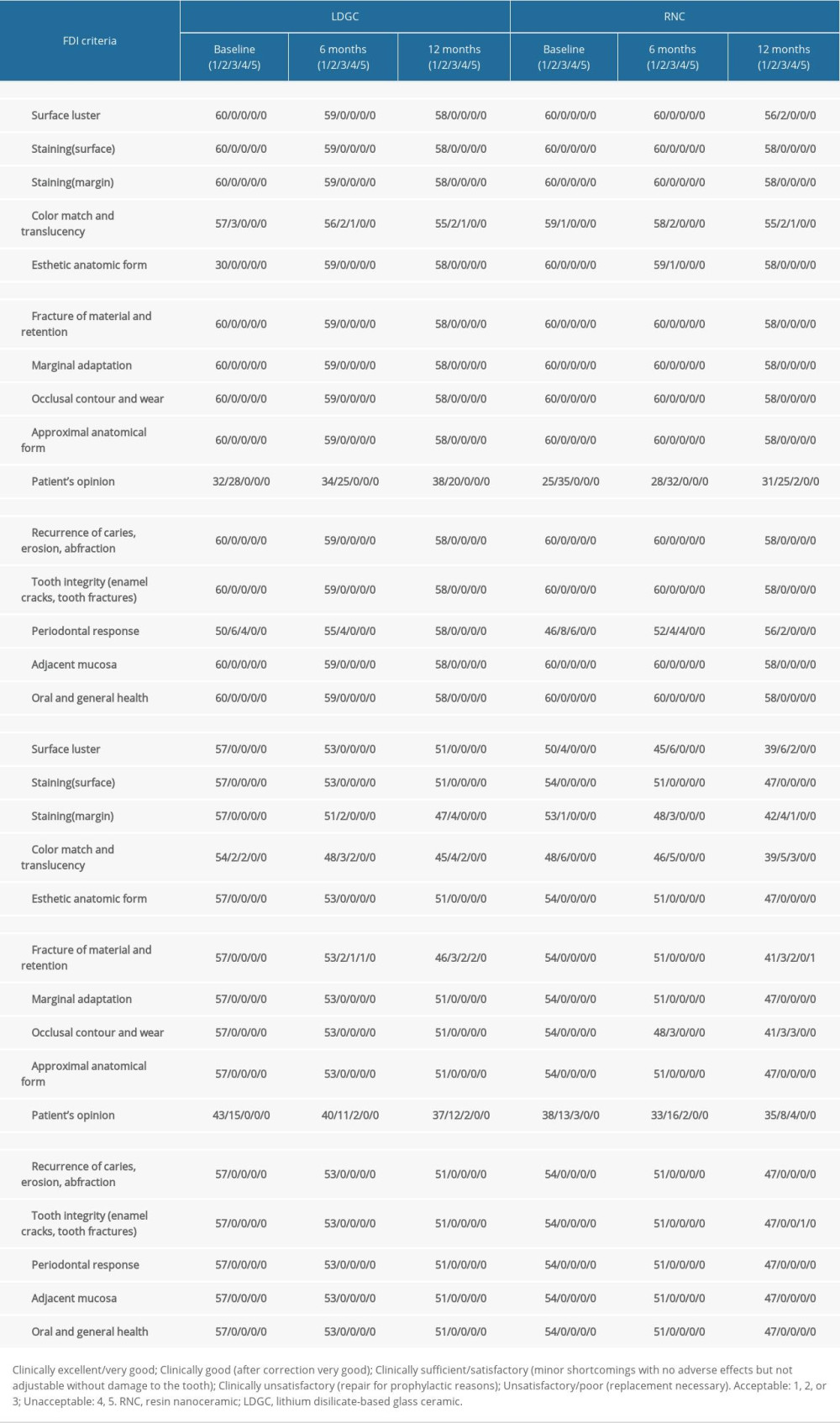 Table 4. Number of restorations evaluated for each group, classified according to the FDI Criteria, at baseline and at followup visits, at 6, 12, 18, 24, and 36 months.
Table 4. Number of restorations evaluated for each group, classified according to the FDI Criteria, at baseline and at followup visits, at 6, 12, 18, 24, and 36 months.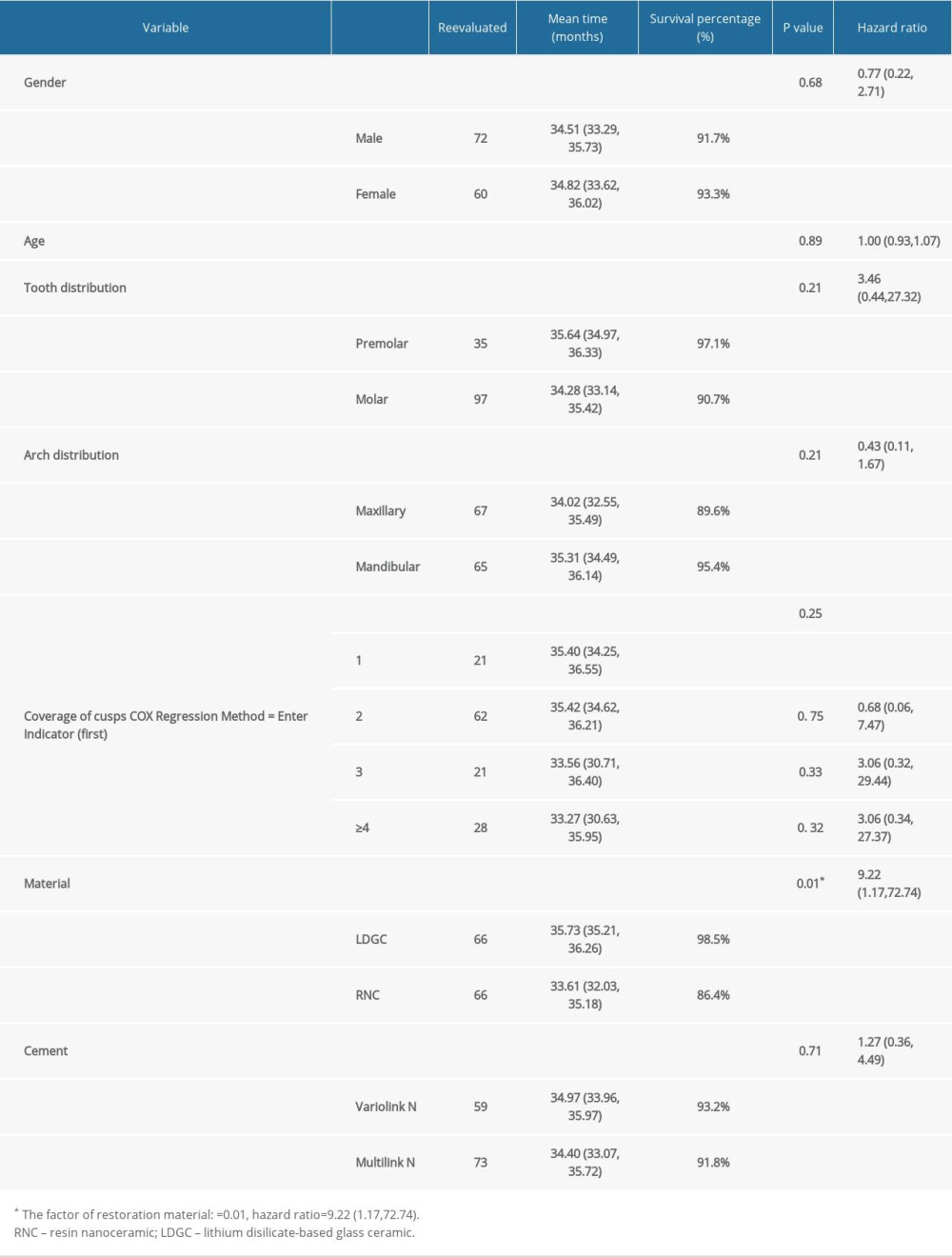 Table 5. Survival (failure=debonding) distributions and test results according to categorical clinical factors.
Table 5. Survival (failure=debonding) distributions and test results according to categorical clinical factors.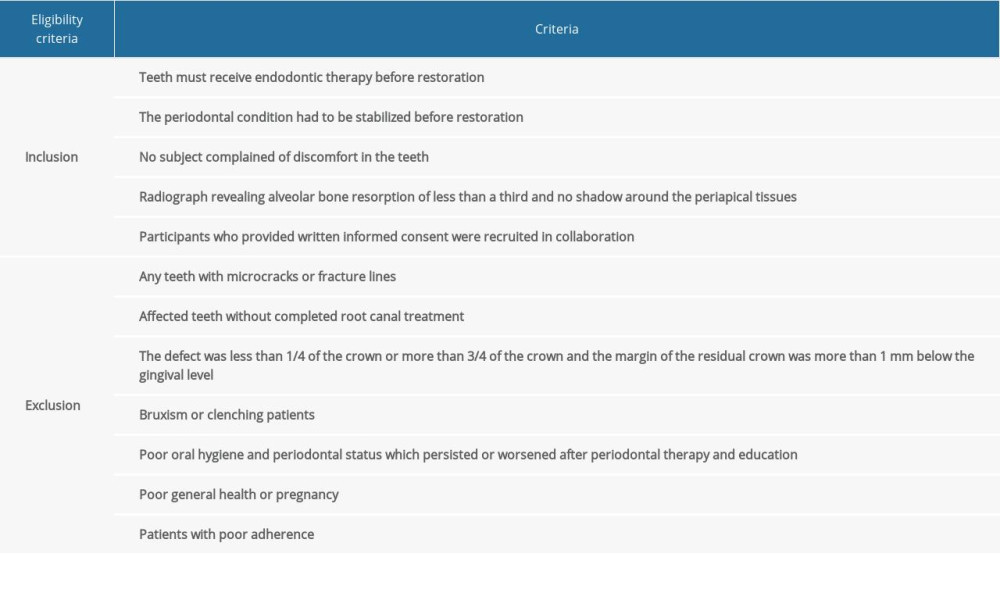 Table 1. Eligibility criteria.
Table 1. Eligibility criteria.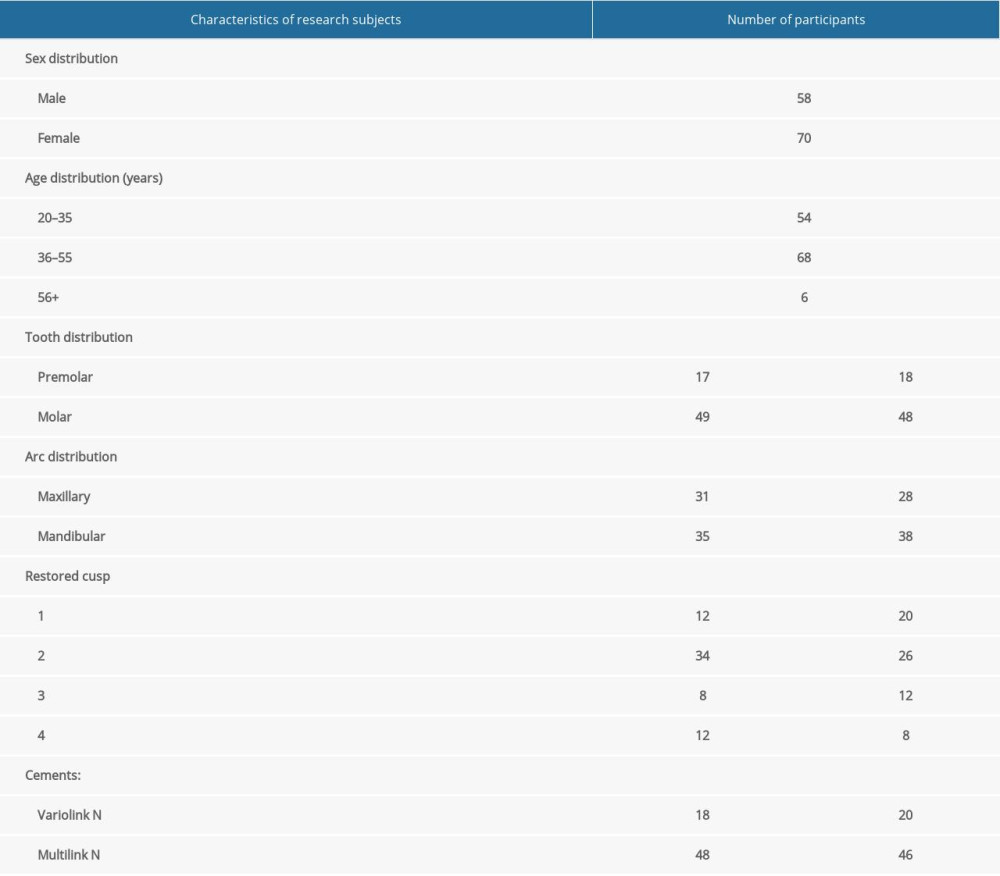 Table 2. Demographic and baseline data.
Table 2. Demographic and baseline data.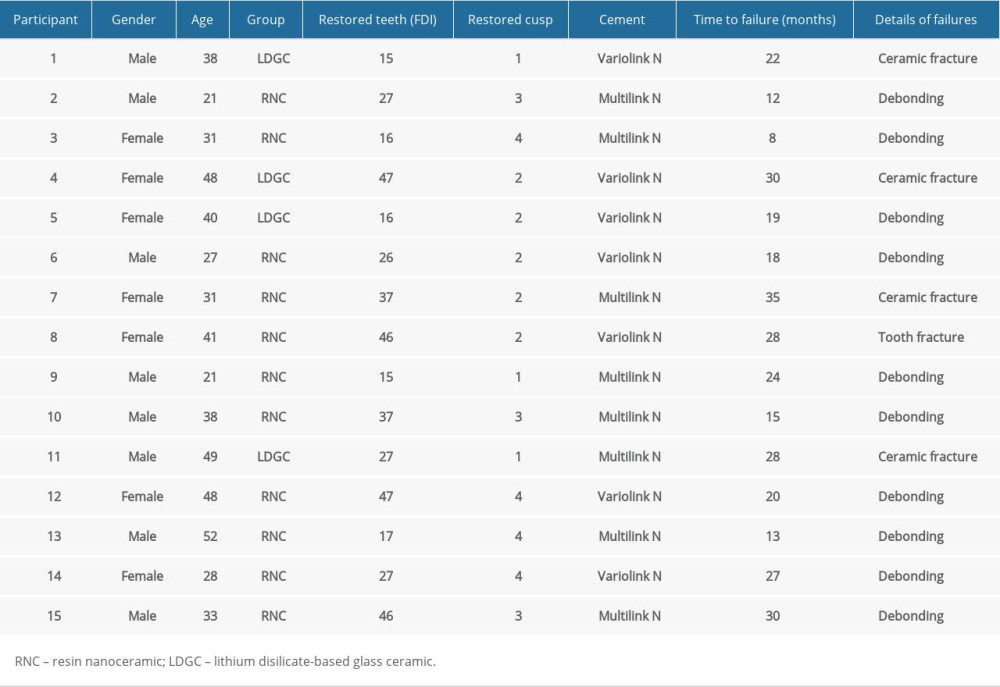 Table 3. Descriptive analysis of failed restorations.
Table 3. Descriptive analysis of failed restorations.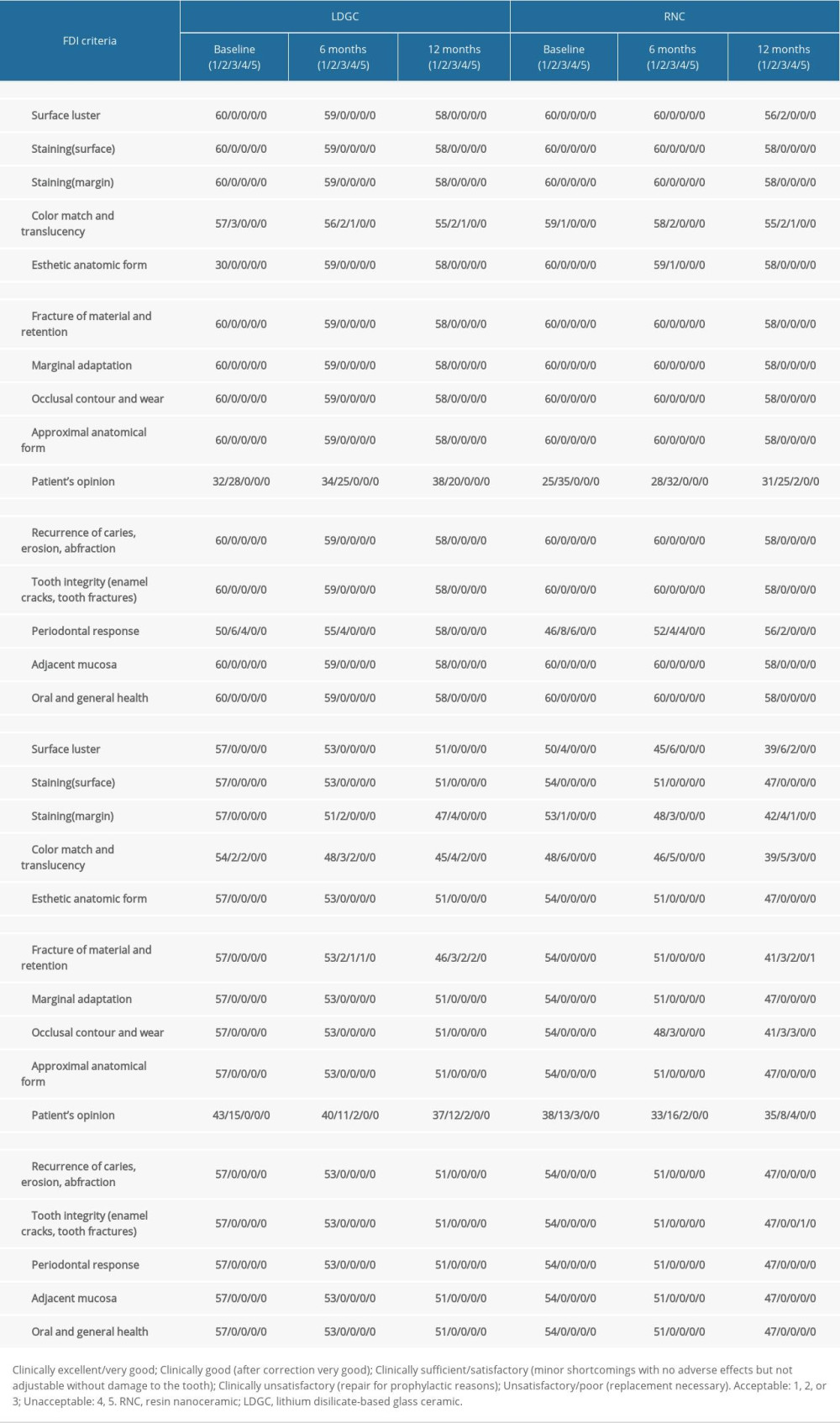 Table 4. Number of restorations evaluated for each group, classified according to the FDI Criteria, at baseline and at followup visits, at 6, 12, 18, 24, and 36 months.
Table 4. Number of restorations evaluated for each group, classified according to the FDI Criteria, at baseline and at followup visits, at 6, 12, 18, 24, and 36 months.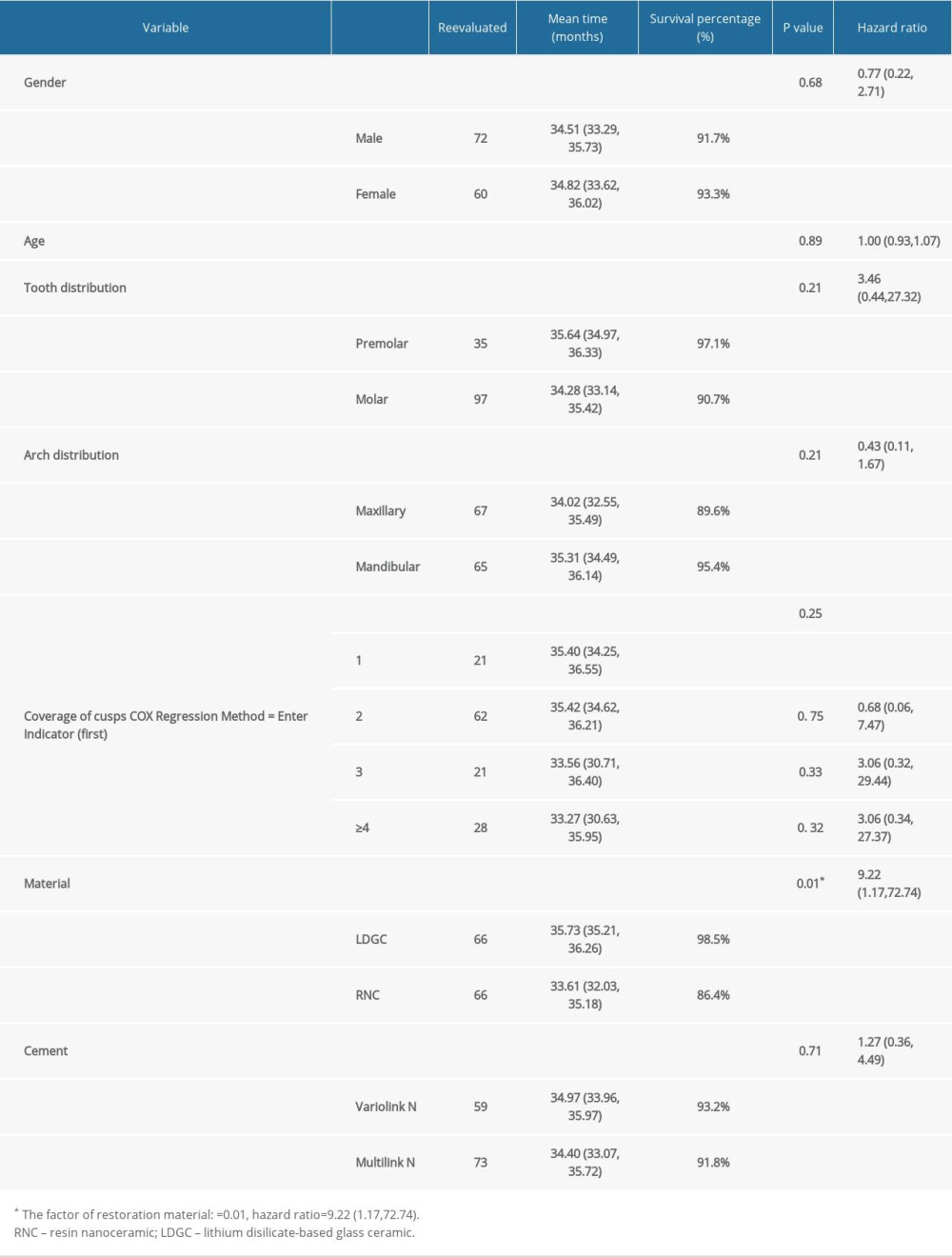 Table 5. Survival (failure=debonding) distributions and test results according to categorical clinical factors.
Table 5. Survival (failure=debonding) distributions and test results according to categorical clinical factors. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








