05 August 2022: Clinical Research
Safety and Efficacy of the Baska Mask Versus Endotracheal Intubation in 64 Women Undergoing Elective Laparoscopic Gynecological Surgery Under General Anesthesia: A Prospective Single-Center Study
Hyoeun AhnDOI: 10.12659/MSM.937630
Med Sci Monit 2022; 28:e937630
Abstract
BACKGROUND: The Baska mask is a supraglottic airway device that has a continuous non-inflatable flexible cuff that mimics an airway, reducing the risk of overinflation and aspiration of gastric contents. This prospective study from a single center aimed to compare the safety and efficacy of the Baska mask vs endotracheal intubation (ET) in 64 women undergoing elective laparoscopic gynecological surgery in Trendelenburg position under general anesthesia.
MATERIAL AND METHODS: This was a prospective randomized study conducted on 64 adult female patients, 32 in each group, undergoing gynecologic surgery under general anesthesia. The study population was divided into 2 groups: the Baska group and the ET group. The respiratory and haemodynamic variables, the degree of gastric distension, and postoperative pharyngolaryngeal symptoms were compared between groups.
RESULTS: After 2 patients dropped out of the study, data from 62 patients were analyzed. The Baska group showed significantly shorter device insertion time (28.4±10.7 vs 46.6±19.8, P=0.001), a significantly lower oropharyngeal leak pressure at all studied time points, and a higher leak fraction at 1 min after the completion of pneumoperitoneum (5.6% vs 2.1%, P=0.031) compared to the ET group. Respiratory and haemodynamic variables, the gastric antrum size, and postoperative pharyngolaryngeal symptoms showed no significant difference.
CONCLUSIONS: This study supports the findings from previous studies in patients undergoing general surgery. The Baska mask was as effective as ET in ventilation during general anesthesia in women undergoing elective laparoscopic gynecological surgery. Respiratory and hemodynamic responses were similar to ET, and no complications were associated with the Baska mask in this study.
Keywords: Anesthesia, Endotracheal, Head-Down Tilt, Intubation, Laparoscopy, Pneumoperitoneum, Adult, Anesthesia, General, Female, Gynecologic Surgical Procedures, Humans, Intubation, Intratracheal, Laryngeal Masks, Prospective Studies
Background
During laparoscopic surgery, CO2 insufflation into the peritoneum increases the load on the respiratory system, as well as the risk of air leakage, insufficient ventilation, and gastric insufflations, which result in aspiration or respiratory complications [1]. Due to the changes caused by pneumoperitoneum, the use of general anesthesia with controlled ventilation has been considered the ideal technique for laparoscopic surgery [2].
Supraglottic airway devices (SADs) are widely used for airway management during general anesthesia and emergency situations. SADs can be used as effectively as endotracheal intubation (ET) in abdominal surgery, including laparoscopic procedures during positive-pressure ventilation [3,4]. Traditionally, SADs have a higher risk of insufficient ventilation and pulmonary aspiration. However, second-generation SADs with gastric channels can maintain appropriate airway pressure and reduce the risk of gastric regurgitation and pulmonary aspiration. Hence, SADs are regarded as reliable alternatives to ET in laparoscopic surgery [5–7].
The Baska mask is one of the second-generation SADs that includes a non-inflatable cuff that molds to the shape of the airway, reducing the risk of overinflation, tissue and nerve damage, and aspiration of gastric contents, and it also includes a side suction channel, and an integrated bite block [8]. The Baska mask provides more efficient ventilation by automatically inflating the cuff during positive-pressure ventilation. As pressure increases with positive-pressure ventilation, the cuff automatically inflates and improves the oropharyngeal leak pressure (OLP) during general anesthesia relative to previous SADs, particularly for laparoscopic surgery [9,10].
Previous studies have shown that the Baska mask is a more suitable alternative airway device than ET for laparoscopic cholecystectomy under positive-pressure ventilation [11,12]. In addition, a recent study reported the Baska mask had comparable ventilatory performance during short-term laparoscopic gynecological surgery [13].
We evaluated the Baska mask vs ET in terms of insertion time, respiratory and hemodynamic variables, the degree of gastric distension by ultrasonography, the incidence and severity of postoperative pharyngolaryngeal symptoms (sore throat, hoarseness and dysphagia), and the presence of nausea and vomiting during laparoscopy in Trendelenburg position. Therefore, this prospective study from a single center aimed to compare the safety and efficacy of the use of the Baska mask vs standard ET in 64 women undergoing elective laparoscopic gynecological surgery under general anesthesia.
Material and Methods
ETHICS STATEMENT:
This prospective randomized study was approved by the Institutional Review Board of Ajou University Hospital (approval no. AJIRB-MED-INT-19-463). The clinical trial was registered at Clinical Research Information Service (CRIS) of Korea (identifier: KCT0004624). All participants provided written informed consent before the start of the study.
STUDY DESIGN:
Adult patients, aged between 19 and 70 years, with an American Society of Anesthesiologists (ASA) physical status of I to II, who underwent elective laparoscopic gynecological surgery under general anesthesia were enrolled in this study. Written informed consent was obtained from all patients. The exclusion criteria were: high risk of aspiration (hiatal hernia, gastroesophageal reflux disease, and non-fasting status), difficult airway to intubation (limitation of mouth opening, limitation of neck extension, and Mallampati class IV), body mass index (BMI) ≥35 kg/m2, and previous gastrectomy history.
ANESTHESIA PROTOCOL:
All patients fasted for at least 8 h before surgery. Airway evaluation, including the Mallampati score, was performed preoperatively. On arrival at the operating room, patients were monitored (CARESCAPE B850® monitor, GE Healthcare, USA) by using an electrocardiogram, noninvasive blood pressure measurement, pulse oximetry, and the bispectral index (BIS) (BISTM, Covidien LLC, USA). For each patient, after 3 min of pre-oxygenation, general anesthesia was induced using a target-controlled infusion (Orchestra® Base Primea device, Fresenius Kabi, France) of propofol and remifentanil, with an effect-site concentration of 4–6 μg/ml and 3–4 ng/ml, respectively. After checking the patient’s loss of response to verbal commands, rocuronium 0.6 mg/kg was administered and positive-pressure ventilation via an oxygen mask was delivered. Two minutes after rocuronium injection, a Baska® mask (Logikal Health Products PTY Ltd., Australia) or ET (Profile Soft Seal® Cuff, Sims Portex, UK) was inserted when the BIS was below 60. In the Baska mask group, appropriate mask insertion was confirmed by the absence of audible leak with peak airway pressures of 12 cmH2O or greater, during gentle manual ventilation [14].
Patients were excluded from the study if the number of attempts at Baska mask insertion was more than 3. In addition, the Baska mask was removed, and ET was intubated if any of the following occurred: respiratory obstruction, persistent oropharyngeal leak with inadequate ventilation (end-tidal CO2 [EtCO2]) ≥39 mmHg before peritoneal insufflation and ≥45 mmHg during peritoneal insufflation), and gastric distension interfering with the surgical field [15].
During the operation, mechanical ventilation (Primus®, Dräger, Germany) was initiated by maintaining a tidal volume of 8 mL/kg, respiratory rate of 10–12/min with an inspiratory/expiratory ratio of 1: 2, and a mixture of O2 and air with an 0.5 fraction of inspired oxygen, and EtCO2 pressure of 35–45 mmHg.
Oropharyotic suction was performed through the Baska mask-side suction channel or rubber catheter (ET group) every 15 min during the operation. All procedures were performed by a single anesthesiologist.
CLINICAL PERFORMANCE MEASUREMENT:
Basic patient characteristics were collected, including age, height, weight, BMI, ASA status, and Mallampati score. The anesthetic profiles we collected included: device insertion time, operation time, insufflation time, and device removal time. The time taken for effective device insertion was defined as the time from the initial use of the laryngoscope (or picking up of the Baska mask) to the appearance of a square-wave capnographic tracing [14].
During the operation, hemodynamic and respiratory variables of patients were also recorded, including mean arterial pressure, heart rate, saturation of peripheral oxygen (SpO2), BIS, EtCO2, tidal volume, peak airway pressure, mean airway pressure, OLP, and leak fraction.
The OLP was measured by adjusting the expiratory valve of the breathing circle to 40 cmH2O (fixed gas flow, 3 L/min). After the pressure equilibrium was reached, the OLP was recorded when audible gas leakage was detected with a stethoscope at the throat site [16].
The hemodynamic, respiratory, and ventilator variables were estimated and recorded at T1, T2, T3, and T4 (T1, 1 min after device insertion; T2, 10 min after pneumoperitoneum initiation; T3, 30 min after pneumoperitoneum initiation; and T4, 1 min after pneumoperitoneum completion).
To compare the gastric distension degree data between the 2 groups, the surgical field of vision, the presence of gastric air, and the size of antral CSA were measured. The surgical field of vision was graded on a 10-point grading system (0=empty stomach and 10=gastric distension interfering with the surgical field) 2 separate times (after the completion of pneumoperitoneum and before the end of pneumoperitoneum) by the surgeon. Assessment of the antral CSA and the presence of gastric air (irregular bright white structures in ultrasonography) was performed for each patient lying in the supine position using ultrasonography before anesthesia was induced and after the surgery. Air artifact longitudinal and anteroposterior diameters of a single section of the gastric antrum were determined and recorded [17].
After the operation was completed, the presence of blood staining on the device surface, continuous coughing, gastric content regurgitation, and bronchospasm were checked during device removal and recorded as YES/NO. Postoperative pharyngolaryngeal symptoms (the incidence of sore throat, hoarseness, and dysphagia) were evaluated at 1 h and 24 h after surgery. The severity of the symptoms was assessed using a numerical rating scale (NRS) as a follow: NRS 1–3=mild, NRS 4–7=moderate, and NRS≥8=severe symptom. The presence of nausea and vomiting was recorded as YES/NO and assessed twice, as described above.
STATISTICS:
The sample size was calculated according to results of a previous study [11] in which the standard deviation of the intubation time was an estimated 11.8 s. An intergroup difference of 10 s in the intubation time was assumed to be clinically significant. With an α-error of 0.05, and a power of 0.9, 31 patients were required in each group. The sample size was increased to 64 patients to compensate for potential attrition.
The data were statistically analyzed by using SPSS version 21.0 (IBM Corp., Armonk, NY, USA). Continuous variables were expressed as mean±standard deviation or median with interquartile range and analyzed using the
Results
BASIC PATIENTS CHARACTERISTICS AND ANESTHESIA PROFILES DATA:
In total, 64 patients were enrolled in this study. Two patients were excluded: 1 due to a lack of seal in the Baska mask (in the Baska mask group) and 1 due to increased airway pressure with bronchospasm (in the ET group).
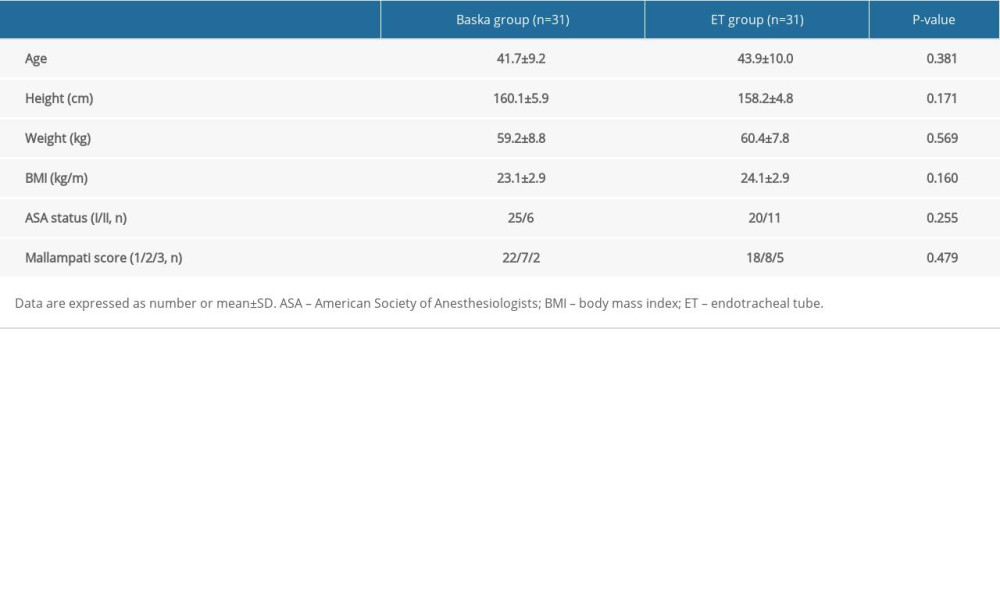
Of the remaining 62 patients, no significant differences in age, height, weight, BMI, ASA classification, or Mallampati score between the 2 groups were detected (Table 1). Moreover, the anesthetic and operational times did not differ between the 2 groups. The Baska mask group showed a significantly shorter device insertion time (s) than the ET group (28.4±10.7 vs 46.6±19.8, P=0.001). The insufflation and device removal times were similar between the groups (Table 2).
HEMODYNAMIC AND RESPIRATORY VARIABLES:
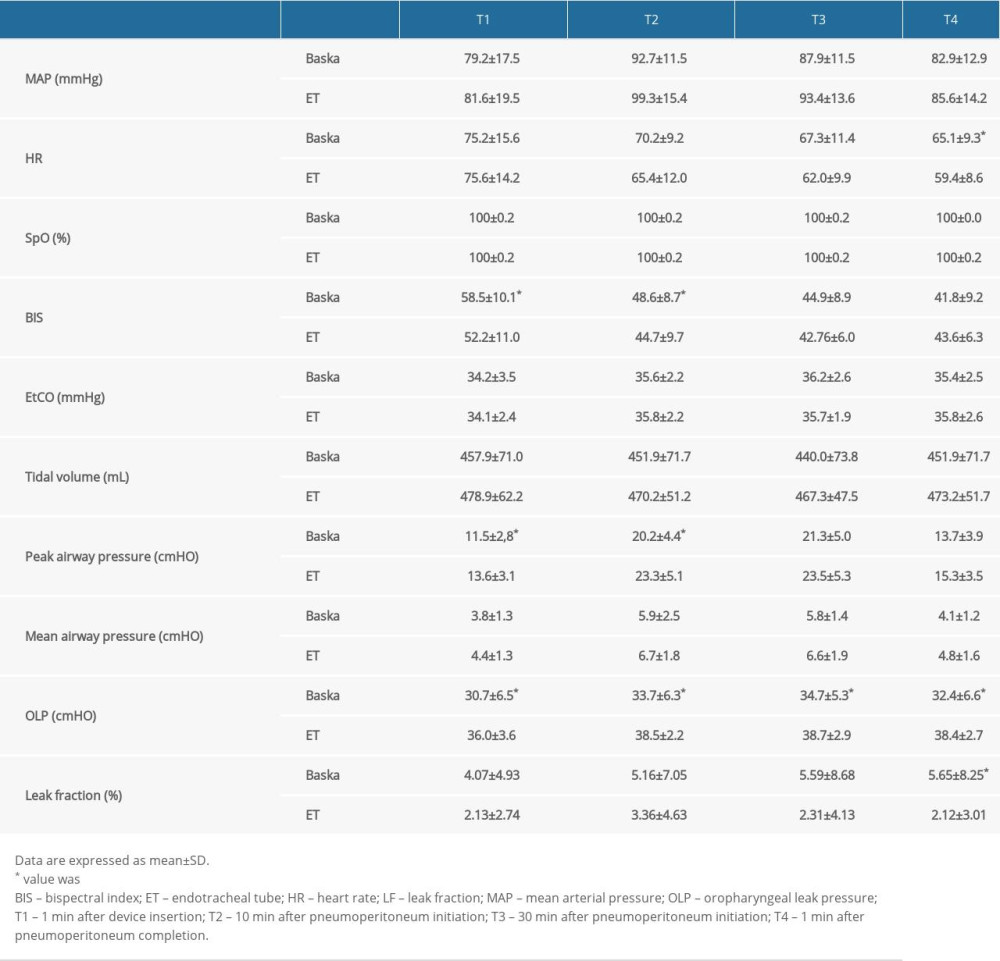
Hemodynamic and respiratory variables are presented in Table 3. The mean arterial pressure and heart rate were stably maintained during the operation in both groups. Although the heart rate at T4 in the Baska mask group was significantly higher than that in the ET group, there was no significant time-dependent change from T1 to T4 in either group. The O2 saturation was well maintained throughout the operation, and the BIS was maintained at under 60 at all time points in both groups.
Tidal volume and EtCO2 were maintained throughout the operation in both groups, and there were no time-dependent changes. The peak and mean airway pressures demonstrated a trend of increase at T2 and decrease at T4 in both groups (
COMPARISON OF GASTRIC DISTENSION DEGREE AND PHARYNGOLARYNGEAL COMPLICATIONS BETWEEN BASKA AND ET GROUPS:
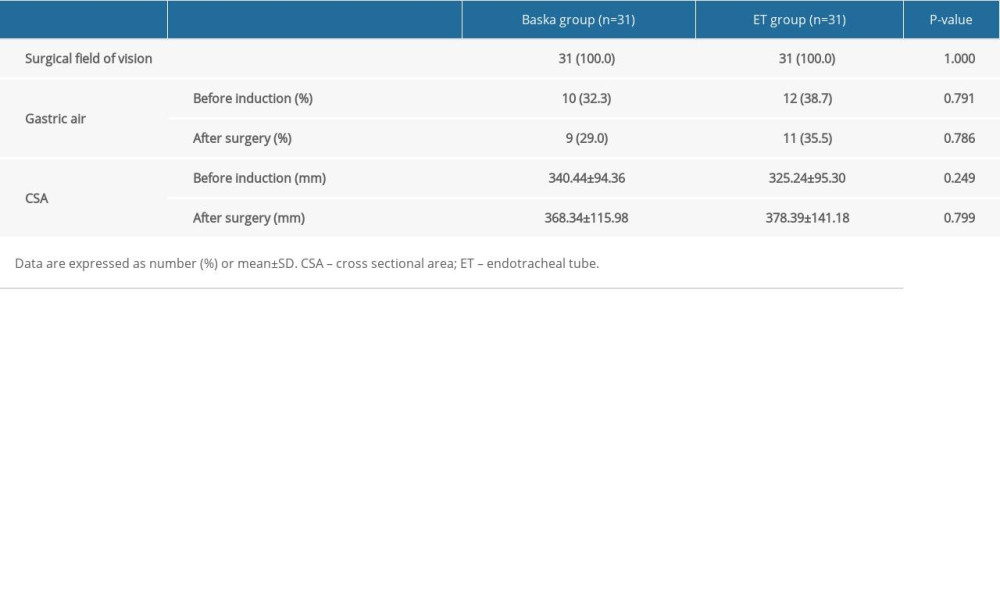
All surgeons graded a zero (no disturbance) for surgical field of vision. The incidence of the presence of gastric air was 10 (32.3%) in the Baska mask group and 12 (38.7%) in the ET group before induction (9 [29%] and 11 [35.5%] after surgery). The measured size of antral CSA before and after surgery showed no significant difference between the 2 groups (Table 4).
After the operation, the presence of blood staining on the Baska mask and ET was assessed. Blood staining was observed in 7 patients in the Baska group (22.6%) and 1 patient in the ET group (3.2%) (
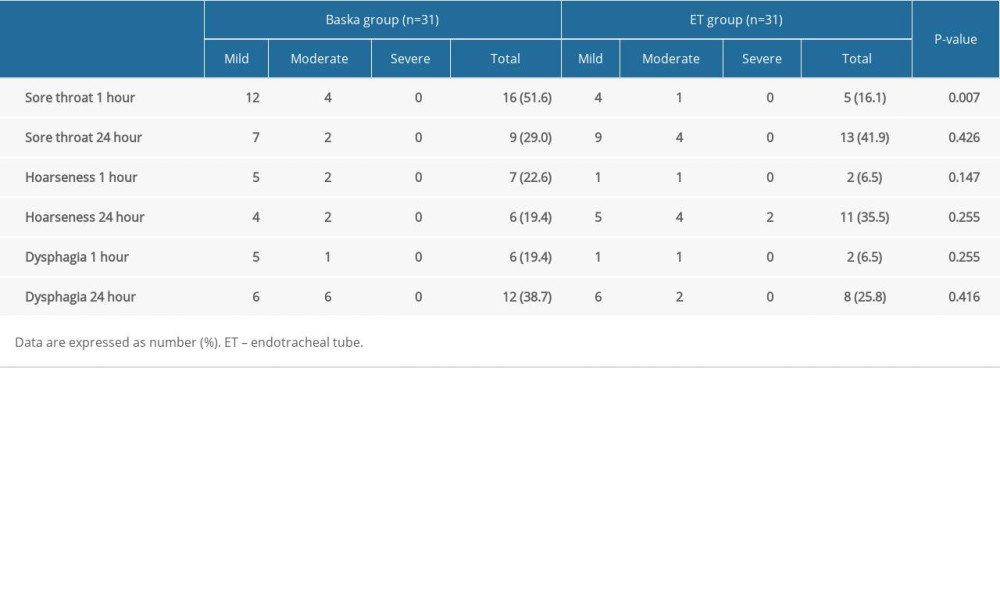
The incidence and severity of postoperative hoarseness and dysphagia generally did not differ between the Baska and ET groups. For sore throat 1 h after surgery, the Baska mask group had a higher incidence than the ET group (P=0.007) (Table 5). There was no difference between the 2 groups in the presence or absence of nausea and vomiting measured at 1 h and 24 h after surgery (both P=1.000).
Discussion
In this prospective randomized study, the Baska mask provided a shorter insertion time, a lower OLP, and a higher leak fraction than ET during laparoscopic gynecological surgery in the Trendelenburg position. In terms of respiratory and hemodynamic responses, gastric distension degree, incidence and severity of postoperative pharyngolaryngeal symptoms, nausea and vomiting, the Baska mask was comparable to ET.
A previous study reported that the Baska mask demonstrated a level of utility comparable to that of SAD. Many studies have also been conducted to evaluate the effectiveness of the Baska mask compared to other airway devices [7–9,17–24]. In most studies, the Baska mask was considered an appropriate SAD for maintaining stable hemodynamics, effective tidal volume, and suitable airway pressures. Our results indicated that the insertion time for the Baska mask was shorter than with ET, and the mean device insertion time decreased by 18 s (39%). This result is consistent with that reported in a previous study [11], in which the mean of device insertion time decreased by 20 s (44%). Thus, the apnea period and hypoxic risk may be reduced during airway device insertion using the Baska mask. The hemodynamic and respiratory variables were suitably maintained during laparoscopic gynecological surgery with Baska mask ventilation compared to ET ventilation in our study. There was no significant difference in the tidal volume, EtCO2, and mean airway pressure between the Baska and ET groups in our study. These results suggest that the Baska mask performed as adequately as ET. Moreover, the peak airway pressure was significantly lower immediately after device insertion and 10 min after pneumoperitoneum in the Baska mask group. This is not surprising, because in general, a higher peak airway pressure is detected with the use of ET than with SADs [7].
During laparoscopic surgery, CO2 insufflation for pneumoperitoneum increases the load on the respiratory system, and the risk of air leakage, insufficient ventilation, or gastric insufflation, which results in aspiration or respiratory complications [25]. In particular, most laparoscopic gynecological surgeries are performed in the Trendelenburg position, which raises airway pressure and may lead to problems when using SADs. However, a meta-analysis reported that SADs showed similar efficacy and fewer pharyngolaryngeal complications than ET, and concluded that SADs were clinically useful as effective airways in laparoscopic surgery [26]. Several studies using the Baska mask have also shown that airway pressure and ventilation were well maintained during laparoscopic cholecystectomy [10,11,27].
The measurement of OLP, analyzed in previous studies, showed that the OLP of the Baska mask was higher than that of other SADs, such as laryngeal mask Supreme™ (Teleflex, Inc., Wayne, PA, USA), and slightly lower than that of ET ventilation [7,9,12,15,28]. According to a previous study, the reported OLP of the Baska mask ranged from 33.3 to 36.6 cmH2O [12,22]. In our study, the mean OLP of the Baska mask was maintained at over 30 cmH2O throughout the operation. This is consistent with a previous study, in which median OLP was maintained at over 30 cmH2O during laparoscopy in the Trendelenburg position [13].
In our study, the leak fraction of the Baska mask group ranged from 4.1% to 5.6% during surgery. This result is consistent with the finding of a previous study, in which the median leak fraction in the Baska mask was 5% (range, 3% to 15%) [8]. Our results in the Baska mask group implied that there was a low and stable air leakage, with the leak fraction increasing during surgery. Based on this observation, the effectiveness of ventilation may decrease due to an increasing leak fraction with prolonged surgical time. Taken together, our results showed that the Baska mask is effective for use during general anesthesia in short-duration laparoscopic surgeries in the Trendelenburg position.
To evaluate gastric regurgitation and aspiration, we analyzed the degree of gastric distension by estimating the size of antral CSA using ultrasonography. Ultrasonographic measurement of the CSA is a well-described technique that is currently used for the assessment of gastric emptying, since the gastric antrum is visible in almost all patients, irrespective of the gas content in the fundus [17,29]. A previous study reported that the surgeon’s visual access and the degree of gastric distension did not differ significantly between the laryngeal mask and ET during laparoscopic cholecystectomy, according to the surgeon’s visual scoring [3]. However, this previous study could not determine the statistical significance because of the subjectivity of the measurements. In the present study, accurate measurements of the size of antral CSA by ultrasonography contributed to improving the quality of analysis of the degree of gastric distension during Baska mask ventilation. In our study, the CSAs of the Baska mask group did not differ from those of the ET group until the operation was completed. This may be due to the unique feature of the Baska mask, in which a cylindrical tube with a high-pressure and flow-suction system is available to remove oropharyngeal and gastric secretions and fluids. Tosh et al [12] also reported no difference in the regurgitation and aspiration of gastric contents between the Baska mask and ET in laparoscopic cholecystectomy, which was evaluated by bronchoscopic detection of methylene blue in the trachea and bronchus at the end of the operation.
This study has several limitations. First, the Baska mask group did not demonstrate fewer pharyngolaryngeal complications than the ET group. Tosh et al [27] reported that the Baska mask significantly reduced the incidence and severity of postoperative sore throat and hoarseness compared with ET in short-duration laparoscopic surgery. However, the results remain unclear. A possible explanation for this is the unique shape of the Baska mask. The Baska mask has a relatively large cuff and induces periodic cuff inflation and deflation during positive-pressure-controlled ventilation, leading to frequent stimulation of the adjacent pharyngolaryngeal tissue. In our study, most pharyngolaryngeal symptoms were mild, and no rescue analgesics were needed for postoperative sore throat in the Baska mask group, suggesting that this is of low clinical significance. Further large-scale studies of pharyngolaryngeal complications of the Baska mask are needed. Second, most intraoperative data were measured in an unblinded manner, which increased the risk of possible bias. However, bias is inevitable owing to the study design and the shapes of the different airway devices.
Conclusions
This study supports the findings from previous studies in patients undergoing general surgery. The Baska mask was as effective as ET in ventilation during general anesthesia in women undergoing elective laparoscopic gynecological surgery. Respiratory and hemodynamic responses were similar to ET, and no complications were associated with the Baska mask in this study.
References
1. Doyle MT, Twomey CF, Owens TM, McShane AJ, Gastroesophageal reflux and tracheal contamination during laparoscopic cholecystectomy and diagnostic gynecological laparoscopy: Anesth Analg, 1998; 86(3); 624-28
2. Bajwa SJ, Kulshrestha A, Anaesthesia for laparoscopic surgery: General vs regional anaesthesia: J Minim Access Surg, 2016; 12(1); 4-9
3. Maltby JR, Beriault MT, Watson NC, Fick GH, Gastric distension and ventilation during laparoscopic cholecystectomy: LMA-Classic vs. tracheal intubation: Can J Anaesth, 2000; 47(7); 622-26
4. Ho BY, Skinner HJ, Mahajan RP, Gastro-oesophageal reflux during day case gynaecological laparoscopy under positive pressure ventilation: Laryngeal mask vs. tracheal intubation: Anaesthesia, 1998; 53(9); 921-24
5. Hong SJ, Ko KM, Park JH, Effectiveness of the Streamlined Liner of the Pharynx Airway (SLIPATM) in allowing positive pressure ventilation during gynaecological laparoscopic surgery: Anaesth Intensive Care, 2011; 39(4); 618-22
6. Maltby JR, Beriault MT, Watson NC, The LMA-ProSeal is an effective alternative to tracheal intubation for laparoscopic cholecystectomy: Can J Anaesth, 2002; 49(8); 857-62
7. Kuvaki B, Ozbilgin S, Gunenc SF, Kucuk BA, Comparison of LM-Supreme and endotracheal tube in patients undergoing gynecological laparoscopic surgery: J Clin Monit Comput, 2020; 34(2); 295-301
8. Alexiev V, Salim A, Kevin L, Laffey J: Anaesthesia, 2012; 67(6); 640-45
9. Alexiev V, Ochana A, Abdelrahman D: Anaesthesia, 2013; 68(10); 1026-32
10. Choi SR, Lee TY, Kim SW, Comparison of clinical performance of i-gel and Baska Mask during laparoscopic cholecystectomy: Korean J Anesthesiol, 2019; 72(6); 576-82
11. Ng CC, Sybil Shah MHB, Chaw SH, Baska mask versus endotracheal tube in laparoscopic cholecystectomy surgery: A prospective randomized trial: Expert Rev Med Devices, 2021; 18(2); 203-10
12. Tosh P, Kumar RB, Sahay N, Suman S, Bhadani UK, Efficacy of Baska mask as an alternative airway device to endotracheal tube in patients undergoing laparoscopic surgeries under controlled ventilation: J Anaesthesiol Clin Pharmacol, 2021; 37(3); 419-24
13. Abdel-Ghaffar HS, Kamel HE, Mohamed KH, Ventilatory performance of BASKA mask as an alternative to endotracheal intubation in short-term gynecologic laparoscopic procedures: A prospective randomized clinical trial: Minerva Anestesiol, 2022 [Online ahead of print]
14. Brimacombe J, Keller C, Fullekrug B, A multicenter study comparing the ProSeal and Classic laryngeal mask airway in anesthetized, nonparalyzed patients: Anesthesiology, 2002; 96(2); 289-95
15. Maltby JR, Beriault MT, Watson NC, LMA-Classic and LMA-ProSeal are effective alternatives to endotracheal intubation for gynecologic laparoscopy: Can J Anaesth, 2003; 50(1); 71-77
16. Keller C, Brimacombe JR, Keller K, Morris R, Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients: Br J Anaesth, 1999; 82(2); 286-87
17. Bouvet L, Albert ML, Augris C, Real-time detection of gastric insufflation related to facemask pressure-controlled ventilation using ultrasonography of the antrum and epigastric auscultation in nonparalyzed patients: A prospective, randomized, double-blind study: Anesthesiology, 2014; 120(2); 326-34
18. Bindal M, Demir A, Koculu R, Comparison of new generation baska mask with i-gel and classical laryngeal mask in outpatient urological interventions: Saudi Med J, 2019; 40(7); 694-700
19. Kang SH, Park M, Comparison of early postoperative recovery between laryngeal mask airway and endotracheal tube in laparoscopic cholecystectomy: A randomized trial: Medicine, 2019; 98(25); e16022
20. Kara D, Sarikas CM, Comparison of the Baska and I-gel supraglottic airway devices: A randomized controlled study: Ann Saudi Med, 2019; 39(5); 302-8
21. Sachidananda R, Shaikh SI, Mitragotri MV: Turk J Anaesthesiol Reanim, 2019; 47(1); 24-30
22. Jayalekshmi S, Paul C, Thomas MK, Efficacy of Baska mask and Laryngeal mask airway supreme during positive pressure ventilation – a comparative study: J Anaesthesiol Clin Pharmacol, 2020; 36(1); 31-36
23. Kusderci HS, Torun MT, Oterkus M: Prague Med Rep, 2021; 122(1); 5-13
24. Priya H, Sripriya R, Ravishankar M, Baska Mask is non-inferior to tracheal tube in preventing airway contamination during controlled ventilation in elective nasal surgeries: A randomised controlled trial: Indian J Anaesth, 2021; 65(8); 586-92
25. Doyle MT, Twomey CF, Owens TM, McShane AJ, Gastroesophageal reflux and tracheal contamination during laparoscopic cholecystectomy and diagnostic gynecological laparoscopy: Anesth Analg, 1998; 86(3); 624-28
26. Park SK, Ko G, Choi GJ, Comparison between supraglottic airway devices and endotracheal tubes in patients undergoing laparoscopic surgery: A systematic review and meta-analysis: Medicine, 2016; 95(33); e4598
27. Tosh P, Rajan S, Kumar L, Incidence and severity of postoperative pharyngolaryngeal complications following use of baska mask versus endotracheal intubation: Anesth Essays Res, 2019; 13(3); 481-85
28. Abdi W, Amathieu R, Adhoum A, Sparing the larynx during gynecological laparoscopy: A randomized trial comparing the LMA Supreme™ and the ETT: Acta Anaesthesiol Scand, 2010; 54(2); 141-46
29. Perlas A, Chan VW, Lupu CM, Ultrasound assessment of gastric content and volume: Anesthesiology, 2009; 111(1); 82-89
In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952