10 April 2023: Clinical Research
Coracoid Process Fractures of the Scapula Treated by Baseplate Three-Column Glenoid Fixation: A Retrospective Study of 24 Patients
Yanbin Tan1ABCDE*, Hang Li2BC, Jiaqi Wu2CDEF, Deting Xue2AF, Zhijun Pan2BDDOI: 10.12659/MSM.937933
Med Sci Monit 2023; 29:e937933
Abstract
BACKGROUND: This retrospective study from a single center aimed to evaluate 24 patients with coracoid process fractures of the scapula treated by baseplate three-column glenoid fixation of the 3 columns attached to the glenoid, or the scapula-glenoid construct, which includes the base of the coracoid, the scapular spine, and the lateral/scapular pillar.
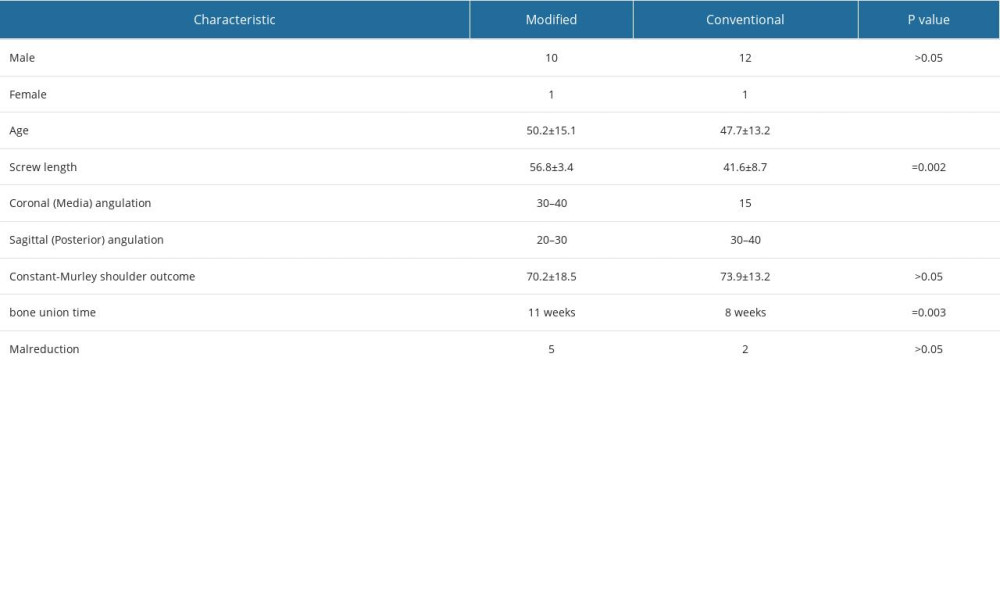
MATERIAL AND METHODS: Twenty-four patients with 24 coracoid process fractures were treated from March 2018 to August 2020 in our hospital; 11 cases were treated with the modified technique and 13 with the conventional technique. The patients had comparable screw length, bone union time, fracture reduction, and Constant-Murley shoulder outcome scores. The significant differences between variables were tested using the t test and Fisher’s exact test, while bone union and reduction position were confirmed with X-ray and CT scans. The average follow-up time was 12 months.
RESULTS: The mean Constant-Murley shoulder outcome score and fracture reduction did not differ significantly (P>0.05), and all patients returned to their previous occupations and levels of activity, with no loss of reduction or surgical revision at the last follow-up. Bone union time for the modified group was longer than that of the conventional group (P<0.05). However, 1 patient had a screw broken at 5 months from heavy manual labor and showed delayed union at 8 months. The lengths of the coracoid process screws in the modified group were longer than in the conventional group (P<0.01).
CONCLUSIONS: The findings from this retrospective study showed that baseplate three-column glenoid fixation of the coracoid process was a good surgical option for coracoid process fractures.
Keywords: coracoid process, Fracture Fixation, Orthopedic Procedures, Humans, Scapula, Fractures, Bone, Shoulder Joint
Background
Coracoid process (CP) fractures constitute 3% to 13% of scapular fractures and 5% of all shoulder fractures [1]. Many methods of treatment for coracoid fractures have been described. Of these, metallic screw fixation from the CP into the neck of the scapula is the standard surgical approach and is believed to be effective [2–4].
Moreover, many CP fractures are associated with fractures of the glenoid, scapular spine, and scapular neck/body [5,6]. These types of cases are extremely challenging for the orthopedic surgeon.
A new scapular bone stock consisting of a baseplate three-column glenoid construct has been described in recent years, which could be a surgically relevant technique in the fixation of these complex types of scapular fractures [7].
The purpose of this study was to introduce a modified fixation technique utilizing the “baseplate three-column glenoid construct” for CP fractures, including complex types with scapular neck/body or intra-articular glenoid fractures, and we also discuss the main characteristics of the technique. This retrospective study from a single center aimed to evaluate 24 patients with coracoid process fractures of the scapula treated by baseplate three-column glenoid fixation of the 3 columns attached to the glenoid, or the scapula-glenoid construct, which includes the base of the coracoid, the scapular spine, and the lateral/scapular pillar.
Material and Methods
PATIENTS IDENTIFICATION:
Twenty-four patients with CP fractures were treated from March 2018 to August 2020 in our hospital. Eleven patients (1 female, 10 male) with an average age of 50.2 years (range, 27 to 67 years) were placed in the modified technique group; the etiologies of the injuries were fall (4 cases), direct blow to shoulder (5 cases), and motor vehicle accident (2 cases). Thirteen patients (1 female, 12 male) with an average age of 47.7 years (range, 29 to 65 years) were in the conventional group; the etiologies of their injuries were fall (3 cases), direct blow to shoulder (2 cases), and motor vehicle accident (9 cases).
INDICATIONS:
All injuries were confirmed with shoulder X-rays. In addition, computed tomography (CT) scans were used to delineate the distribution and displacement of the fracture fragments. Indications for surgical fixation were the following: 1) ≥ 1-cm displacement on radiographic evaluation, 2) active patients requiring normal shoulder function and wishing to return to work sooner, 3) multi-trauma patients requiring function of the shoulder to mobilize.
TREATMENT METHODS:
All patients received general anesthesia and were placed in lateral or beach-chair position according to the surgical plan. An approximately 4-cm vertical incision was made through the Langer’s lines. Blunt dissection was then performed with an elevator from the tip of the CP down the cephalad slope. Under fluoroscopic guidance, a guidewire was inserted to the glenoid neck at the coracoid base anterior and lateral to the coracoid clavicle ligament with 30- to 40-degree medial angulation and 20- to 30-degree posterior angulation in the modified group (Figure 1). Fifteen medial angulations with 30 to 40 posterior angulations were used in the conventional group [8].
After the position and depth of the guide wire were confirmed, a 4.5-mm partially-threaded cannulated lag screw (Synthes, Paoli, Pennsylvania), 55 to 60 mm in the modified group and 30 to 60 mm in the conventional group, was inserted over the guide wire. The wound was then irrigated thoroughly and the soft tissues were closed in layers, then the arm was immobilized in a sling.
POSTOPERATIVE MANAGEMENT AND EVALUATION:
Pendulum shoulder exercises and active-assisted motions of the shoulder were initiated during the first 3 weeks after surgery. In the following 3 weeks, the focus shifted to achieving strength and resistance training beginning with 3 to 5 lb weights and advancing as tolerated. After 6 weeks, the patients were encouraged to have complete movement of the shoulder joint. Once full range of motion was achieved, the patient was instructed in performing a series of progressive resistance strengthening exercises for the rotator cuff, deltoid, and scapular stabilizing muscles.
Patients were followed up and functions of the shoulder joints were evaluated using the Constant-Murley shoulder outcome score [4]. Bone union and reduction position were confirmed with X-ray and CT scans.
STATISTICAL ANALYSIS:
The results are presented as mean±standard deviation (SD). Statistical evaluation of the data was carried out using SPSS Statistics for Windows, version 21.0 (IBM Corp., Armonk, NY, USA). The Mann-Whitney test was used for normally distributed data. The significant differences between variables were tested using the
Results
In all patents, the surgical wounds healed with primary closure, and no infections or neurovascular injuries were observed. The patients were followed for a mean duration of 12 months (range: 10 to 16 months). In the modified group, 10 patients showed bone union with a mean time from surgery to union of 11 weeks (range: 8 to 16 weeks), and 1 patient had screw broken at 5 months from heavy manual labor and showed delayed union at 8 months (Figure 2). Five patients had incomplete reduction with up to 3 mm displacement. The mean Constant-Murley shoulder outcome score was 70.2±18.5 at last follow-up.
In the conventional group, 12 patients showed bone union with a mean time from surgery to union of 8 weeks (range: 6 to 10 weeks). Two patients had incomplete reduction with up to 3 mm displacement. The mean Constant-Murley shoulder outcome score was 73.9±13.2 at last follow-up. All patients returned to their previous occupations and levels of activity, and no loss of reduction or surgical revision occurred.
When comparing the 2 groups, we found the mean Constant-Murley shoulder outcome score did not differ significantly (
Discussion
The CP is an important structure for the attachment of the limb flexion muscles and ligaments, especially those stabilizing the clavicle [9]. Unstable CP fractures as part of multiple shoulder fractures are usually best treated by surgical fixation. Some complex types of CP fractures, including Eyres type IV, type V associated with comminuted fractures or glenoid neck (Miller type II and type III), or with extension to the inferior glenoid (Ideberg type V and type IV), are extremely challenging for the orthopedic surgeon. The fixation technique should be customized and selected based on the size of the fragment, the degree of comminution, and the extent of articular involvement to ensure adequate stabilization [8]. This retrospective study describes a “baseplate three-column glenoid construct” fixation technique used in simple and complex types of CP fractures with cannulated screws, which can be considered as a surgical option for patients with coracoid process fractures.
The parameters of scapular anatomy and the intact screw zone are essential for the fixation of CP fractures. The baseplate three-column glenoid construct is a supportive bony framework formed by the lateral scapular border, scapular spine, and the inferior coracoid pillar [7]. The junctional construct of baseplate three-column glenoid construct can be described as the center of the scapular bone stock, and the maximal length of coracoid fixation screw can be achieved from the superior coracoid pillar to the center of baseplate three-column glenoid construct.
The “baseplate three-column glenoid construct” fixation technique re-establishes a firm connection between the coracoid and the center of the scapula bone stock. This technique was successfully used in simple and complex types of CP fractures in this study, and the mean Constant-Murley score did not differ significantly (
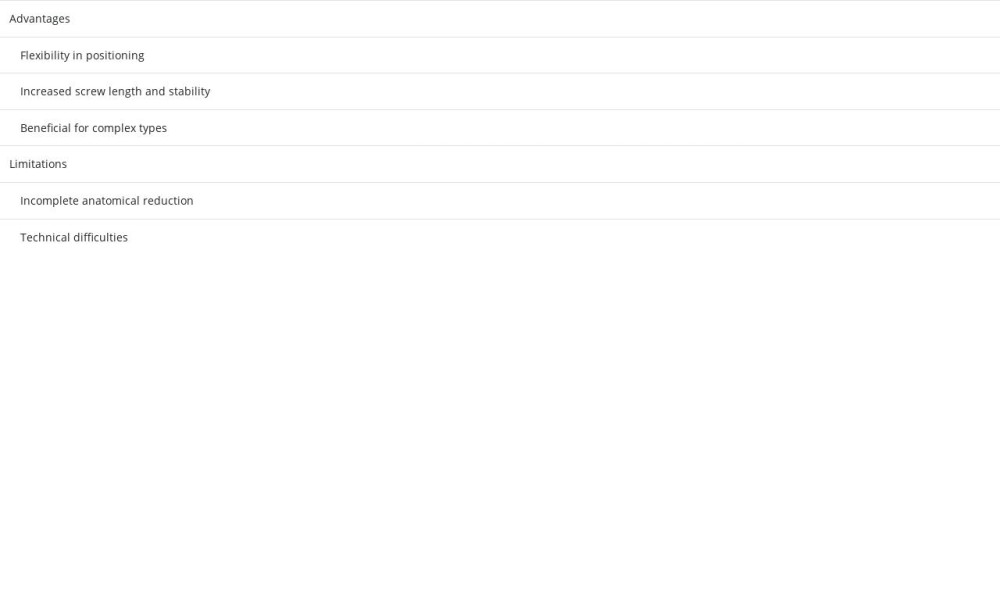
There are several differences between the modified fixation method and the conventional technique (Table 2). In the conventional technique, the screw used to fix the CP to the scapular neck has a 15-degree medial angulation and 30- to 40-degree posterior angulation [8]; we utilized a screw with 30- to 40-degree medial angulation and 20- to 30-degree posterior angulation in the modified technique. The insertion site is at the anterior and lateral rim of the coracoid base with the modified technique, which could offer more working space, allowing more flexibility in surgical positioning in lateral or even supine positions.
The length of the screw used in the modified group varied between 55 and 60 mm, and the average length was longer than in the conventional group (
There are some limitations of this modified fixation method. Without exposing the fractured ends, complete anatomical reduction was difficult to achieve for the complex cases (5 cases). However, compared with the conventional group (2 cases), the fracture malreduction rate did not differ significantly (
The baseplate three-column glenoid construct fixation method provides a customized solution to the surgeon, but most cases in the modified group were combined with other fixation of the scapular components, which could influence the evaluation of the technique. Further clinical and biomechanical studies are required to support these results.
Conclusions
The findings from this retrospective study show that baseplate three-column glenoid fixation of the coracoid process is a good surgical option for coracoid process fractures. This technique can be considered as a surgical option for coracoid process fractures, but further studies are required to explore the efficacy of the modified technique.
Figures
 Figure 1. The direction of the screw for coracoid process fracture. The direction (↖) has increased coronal plane with anterior posterior view (A) and decreased sagittal plane (B) angulation compared to the conventional method. (C) Coronal plane with posterior anterior view.
Figure 1. The direction of the screw for coracoid process fracture. The direction (↖) has increased coronal plane with anterior posterior view (A) and decreased sagittal plane (B) angulation compared to the conventional method. (C) Coronal plane with posterior anterior view. 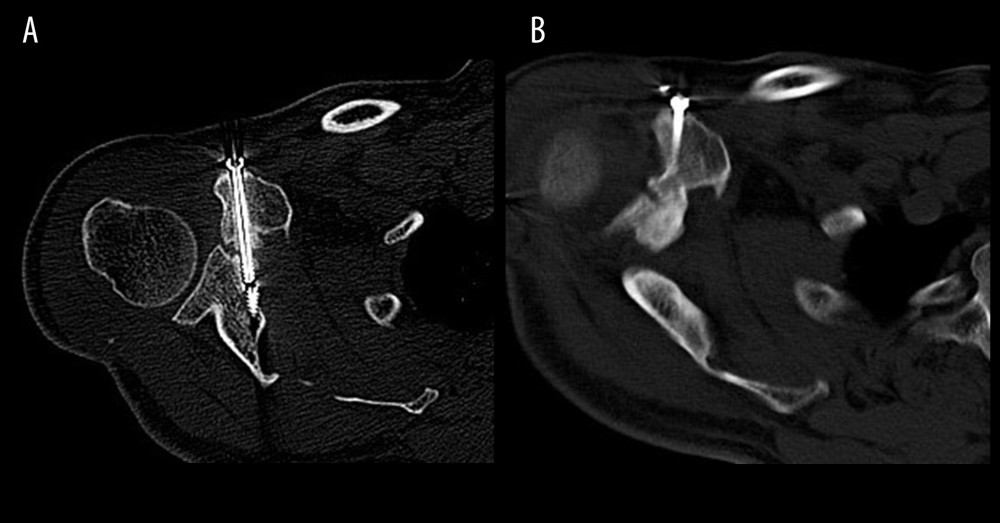 Figure 2. CT scan coracoid process fracture. (A) Delayed union was noted at 5 months, and (B) the fracture healed at 8 months.
Figure 2. CT scan coracoid process fracture. (A) Delayed union was noted at 5 months, and (B) the fracture healed at 8 months. 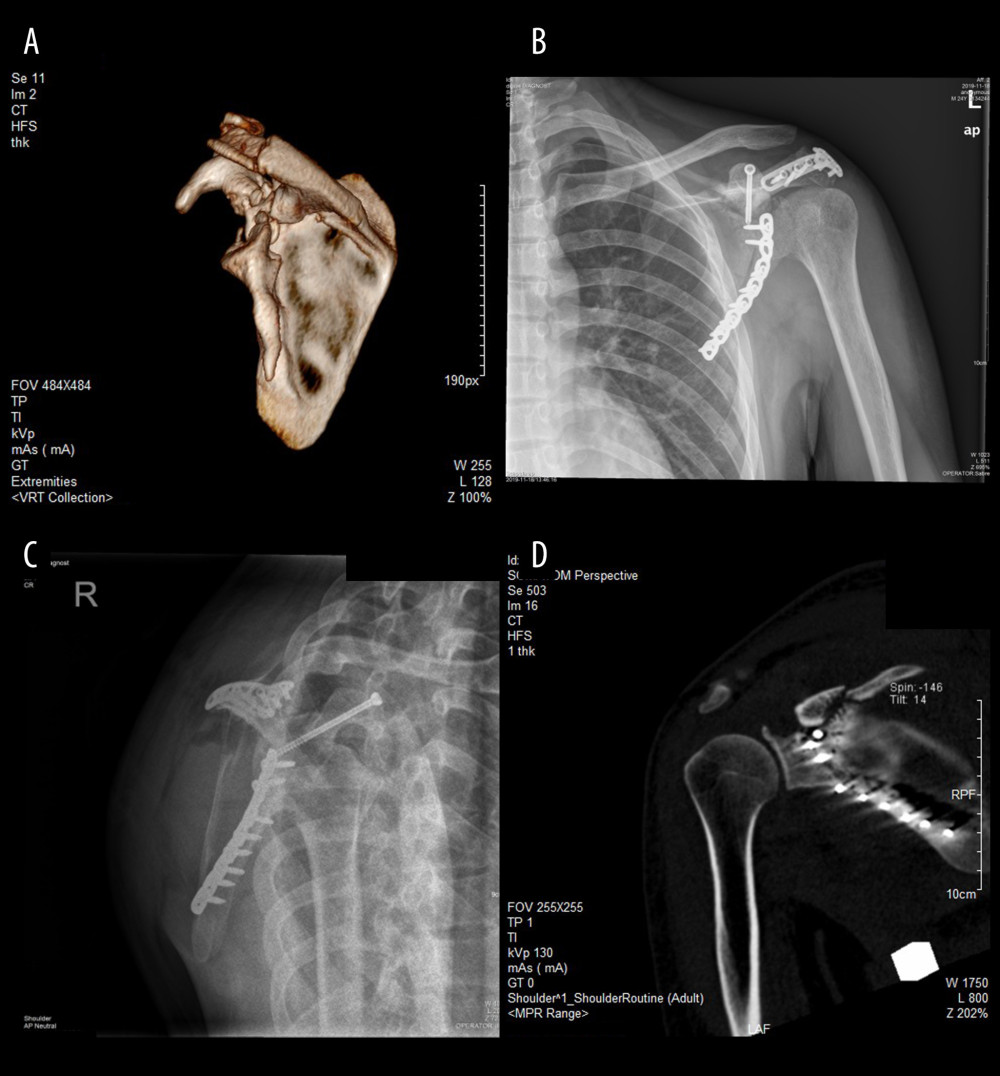 Figure 3. Case 1, coracoid process fracture with Eyres type V associated with Miller type III and Ideberg type IV. (A) 3D reconstruction of a CT scan. (B, C) Postoperative X-ray showing screw fixation of the coracoid process and plate fixation of the scapular neck, scapular body and acromion. CT scan with coronal (D), and anterior views showing the tip of the screw.
Figure 3. Case 1, coracoid process fracture with Eyres type V associated with Miller type III and Ideberg type IV. (A) 3D reconstruction of a CT scan. (B, C) Postoperative X-ray showing screw fixation of the coracoid process and plate fixation of the scapular neck, scapular body and acromion. CT scan with coronal (D), and anterior views showing the tip of the screw.  Figure 4. Case 2, coracoid process fracture with Eyres type V associated with Miller type III and Ideberg type V. (A) 3D reconstruction of a CT scan. (B) Postoperative X-ray showing screw fixation of the coracoid process and plate fixation of the scapular neck, scapular body, acromion, and clavicle. CT scan with axial (C), and sagittal (D) views showing the tip of the screw.
Figure 4. Case 2, coracoid process fracture with Eyres type V associated with Miller type III and Ideberg type V. (A) 3D reconstruction of a CT scan. (B) Postoperative X-ray showing screw fixation of the coracoid process and plate fixation of the scapular neck, scapular body, acromion, and clavicle. CT scan with axial (C), and sagittal (D) views showing the tip of the screw. References
1. Frankle MA, Teramoto A, Luo ZP, Glenoid morphology in reverse shoulder arthroplasty: Classification and surgical implications: J Shoulder Elbow Surg, 2009; 18(6); 874-85
2. Formaini NT, Everding NG, Levy JC, Glenoid baseplate fixation using hybrid configurations of locked and unlocked peripheral screws: J Orthop Traumatol, 2017; 18(3); 221-28
3. Ogawa K, Matsumura N, Ikegami H, Coracoid fractures: Therapeutic strategy and surgical outcomes: J Trauma Acute Care Surg, 2012; 72; E20-E26
4. Vrotsou K, Ávila M, Machón M, Mateo-Abad M, Constant-Murley Score: Systematic review and standardized evaluation in different shoulder pathologies: Qual Life Res, 2018; 27(9); 2217-26
5. Plachel F, Schanda JE, Ortmaier R, The “triple dislocation fracture”: Anterior shoulder dislocation with concomitant fracture of the glenoid rim, greater tuberosity and coracoid process – a series of six cases: J Shoulder Elbow Surg, 2017; 26; e278-e85
6. Kim KC, Rhee KJ, Shin HD, Displaced fracture of the coracoid process associated with acromioclavicular dislocation: A two-bird-one-stone solution: J Trauma, 2009; 67; 403-5
7. Bhatia DN, de Beer JF, du Toit DF, Coracoid process anatomy: Implications in radiographic imaging and surgery: Clin Anat, 2007; 20(7); 774-84
8. Hill BW, Jacobson AR, Anavian J, Cole PA, Surgical management of coracoid fractures: Technical tricks and clinical experience: J Orthop Trauma, 2014; 28(5); e114-22
9. Mohammed H, Skalski MR, Coracoid process: The lighthouse of the shoulder: Radiographics, 2016; 36; 2084-101
10. Anavian J, Wijdicks CA, Schroder LK, Surgery for scapula process fractures: good outcome in 26 patients: Acta Orthop, 2009; 80; 344-50
11. Hak DJ, Johnson EE, Avulsion fracture of the coracoid associated with acromioclavicular dislocation: J Orthop Trauma, 1993; 7; 381-83
12. Lädermann A, Denard PJ, Burkhart SS, Injury of the suprascapular nerve during latarjet procedure: An anatomic study: Arthroscopy, 2012; 28; 316-21
13. Chuaychoosakoon C, Suwanno P, Klabklay P, Proximity of the coracoid process to the neurovascular structures in various patient and shoulder positions: A cadveric study: Arthroscopy, 2019; 35; 372-37
Figures
 Figure 1. The direction of the screw for coracoid process fracture. The direction (↖) has increased coronal plane with anterior posterior view (A) and decreased sagittal plane (B) angulation compared to the conventional method. (C) Coronal plane with posterior anterior view.
Figure 1. The direction of the screw for coracoid process fracture. The direction (↖) has increased coronal plane with anterior posterior view (A) and decreased sagittal plane (B) angulation compared to the conventional method. (C) Coronal plane with posterior anterior view.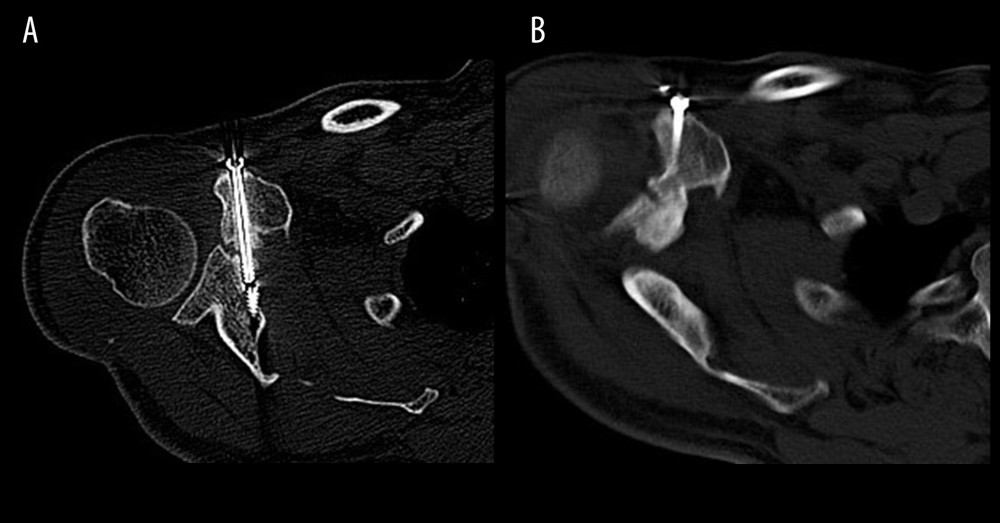 Figure 2. CT scan coracoid process fracture. (A) Delayed union was noted at 5 months, and (B) the fracture healed at 8 months.
Figure 2. CT scan coracoid process fracture. (A) Delayed union was noted at 5 months, and (B) the fracture healed at 8 months.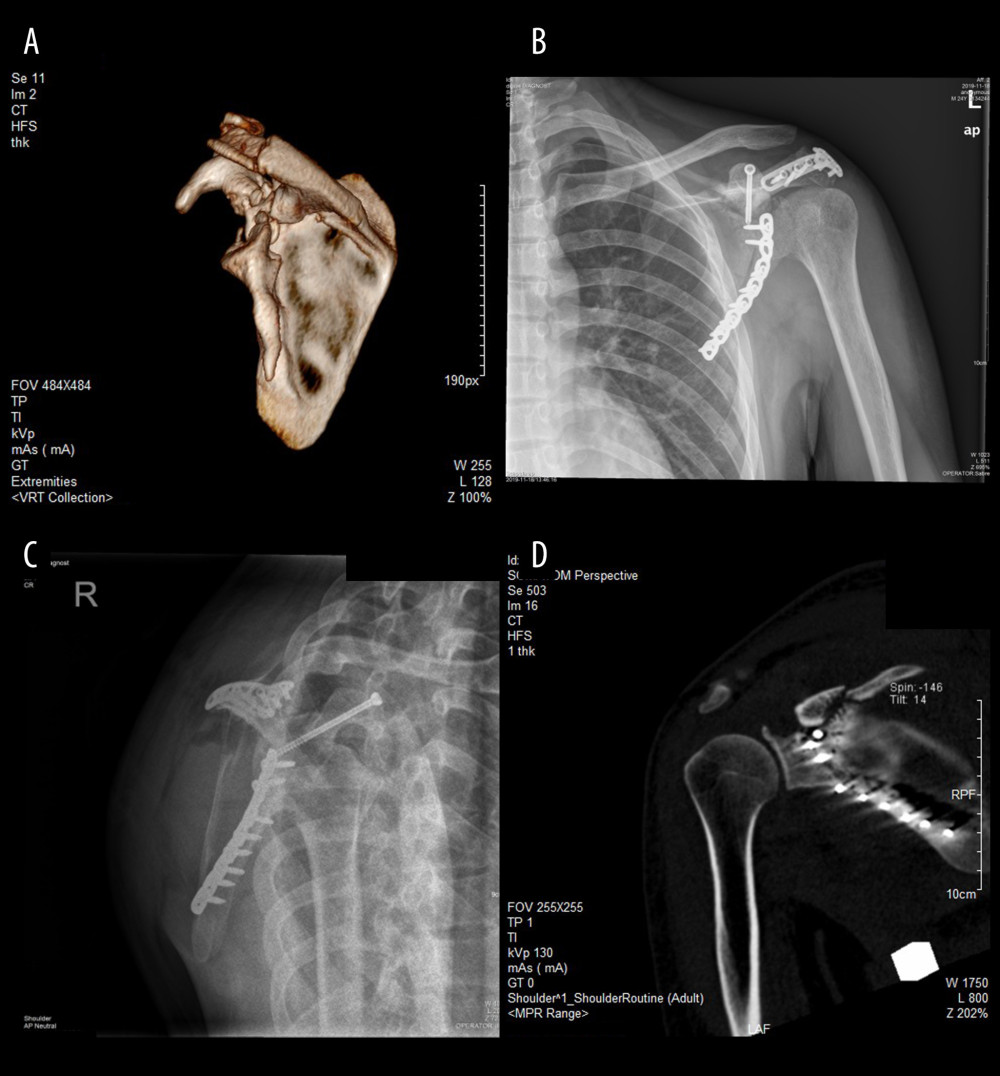 Figure 3. Case 1, coracoid process fracture with Eyres type V associated with Miller type III and Ideberg type IV. (A) 3D reconstruction of a CT scan. (B, C) Postoperative X-ray showing screw fixation of the coracoid process and plate fixation of the scapular neck, scapular body and acromion. CT scan with coronal (D), and anterior views showing the tip of the screw.
Figure 3. Case 1, coracoid process fracture with Eyres type V associated with Miller type III and Ideberg type IV. (A) 3D reconstruction of a CT scan. (B, C) Postoperative X-ray showing screw fixation of the coracoid process and plate fixation of the scapular neck, scapular body and acromion. CT scan with coronal (D), and anterior views showing the tip of the screw. Figure 4. Case 2, coracoid process fracture with Eyres type V associated with Miller type III and Ideberg type V. (A) 3D reconstruction of a CT scan. (B) Postoperative X-ray showing screw fixation of the coracoid process and plate fixation of the scapular neck, scapular body, acromion, and clavicle. CT scan with axial (C), and sagittal (D) views showing the tip of the screw.
Figure 4. Case 2, coracoid process fracture with Eyres type V associated with Miller type III and Ideberg type V. (A) 3D reconstruction of a CT scan. (B) Postoperative X-ray showing screw fixation of the coracoid process and plate fixation of the scapular neck, scapular body, acromion, and clavicle. CT scan with axial (C), and sagittal (D) views showing the tip of the screw. In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952