30 December 2022: Clinical Research
Analysis of Risk Factors of Potentially Difficult Endotracheal Intubation: A Retrospective Observational Study of 154 Patients with Scoliosis at a Single Center in China
Kuan LiBCDEF, Xiao HanBCDEF, Xin ChenB, Zheng LiAG, Shugang LiDOI: 10.12659/MSM.937965
Med Sci Monit 2022; 28:e937965
Abstract
BACKGROUND: Glottic entrance stenosis is an important cause of difficult airway intubation and may be potentially associated with scoliosis. This retrospective study from a single center in China aimed to investigate the parameters and risk factors associated with glottic entrance stenosis by evaluating 154 patients with scoliosis who underwent posterior surgical correction, internal fixation, and fusion.
MATERIAL AND METHODS: A total of 161 patients diagnosed with scoliosis from 2018 to 2020 were included and grouped by classification, and 7 of them were excluded from the risk factor analysis. All patients underwent posterior surgical correction, internal fixation, and fusion. Basic data, scoliosis-related information, and radiological image were collected. Sagittal and transverse diameter and cross-section area were measured. A new definition of glottic entrance stenosis was proposed based on the traditional formula for prediction of tracheal tuba diameter.
RESULTS: The percentage of transverse stenosis in these patients was 35.4%, and the incidence of sagittal stenosis and area stenosis were 9.9% and 12.4% respectively, while 37.9% of scoliosis patients also have at least 1 type of glottic entrance stenosis. Longer course of disease is a proven risk factor for sagittal stenosis (P=0.037). Smaller lumbar lordosis indicates higher risk of transverse stenosis (P=0.024). Wedged vertebrae are a risk factor for area stenosis (P=0.024).
CONCLUSIONS: This study comprehensively measured glottic entrance parameters in patients with scoliosis, proposed a new definition of glottic entrance stenosis, and found that longer course of disease, smaller lumbar lordosis, and wedged vertebrae were risk factors for sagittal stenosis, transverse stenosis, and area stenosis, respectively.
Keywords: airway management, Glottis, Intubation, Scoliosis, Animals, Humans, Lordosis, Constriction, Pathologic, Treatment Outcome, Spinal Fusion, Intubation, Intratracheal, Thoracic Vertebrae, China, Risk Factors, Lumbar Vertebrae
Background
Scoliosis is a major area of interest within the field of spine surgery. Based on characteristics of deformity, scoliosis is classified into adolescent idiopathic scoliosis (AIS), congenital scoliosis (CS), neuromuscular scoliosis (NMS), neurofibromatosis scoliosis (NFS), syndromic scoliosis (SS), and adult degenerative scoliosis (ADS) [1]. Surgery should be considered when the symptoms cannot be managed conservatively [2,3]. Successful general anesthesia is based on full airway evaluation and preparation (air management). Extensive research has shown that scoliosis correlates with abnormal development of cartilage [4], muscular [5], and soft tissue [6], which are involved in degeneration of laryngeal and tracheal tissue [7]. Severe scoliosis can combine with serious deformity of the trachea and cause difficult intubation [8–10]. Preoperative assessment of a patient’s airway enables the anesthesiologist to predict the ease of visualizing the glottis and performing intubation. The term “difficult tracheal intubation” is used when there is difficulty in visualization of the glottic opening or passing of the endotracheal tube, which is common in clinical practice [11].
A variety of methods have been used to assess airway parameters, intending to predict difficult intubation. In the past, X-ray imaging was used to measure tracheal diameter [12]. Recent studies have used ultrasonography to predict the feasibility of endotracheal intubation by measuring the cricoid cartilage diameter [13–16]. However, the glottis is usually located in the narrowest cross-section in the tracheal, which is considered the limiting factor during intubation [17,18]. Research to date has not yet measured glottic parameters in patients with scoliosis, and no studies have determined the condition and risk factors of difficult intubation in various types of scoliosis patients. All surgical patients with scoliosis need to undergo computed tomography (CT) scanning because evaluation of the vertebral body is essential for accurate diagnosis and development of an ideal surgical plan, and CT can help reveal fine structures, including the anatomy of the glottis.
Therefore, we attempted to measure glottic parameters and propose a new definition of glottic entrance stenosis by reviewing CT images of 154 patients who underwent posterior surgical correction, internal fixation, and fusion for scoliosis at our institution. This retrospective study from a single center in China aimed to investigate the parameters and risk factors associated with glottic entrance stenosis in patients with different types of scoliosis. The results may provide valuable information for anesthetists to prepare for difficult intubation and will shed new light on the common pathogenesis of scoliosis and airway abnormality. We hope this report will inspire further clinical and scientific explorations in this field.
Material and Methods
ETHICS STATEMENT:
This study was approved by the Institutional Review Board (IRB) of Peking Union Medical College Hospital (PUMCH), and informed consent was obtained from all participants (Registration code: K22C0277, Approval code: I-22YJ054).
SOURCE OF PATIENTS:
The data were collected from patients who underwent posterior scoliosis correction, internal fixation, and fusion surgery in the Orthopedics Department of Peking Union Medical College Hospital from January 2018 to December 2020. All operations were performed by 1 chief surgeon with over 30 years of clinical experience.
INCLUSION AND EXCLUSION CRITERIA:
Inclusion criteria were: 1) undergoing primary correction, fixation, and fusion surgery due to any type of scoliosis, with sufficient indications for surgical intervention; 2) available for pre-operation all-spine CT and magnetic resonance imaging (MRI) scan; 3) willing to sign written informed consents to approve data collection and publication. Exclusion criteria were: 1) insufficient indication for surgical intervention; 2) secondary scoliosis due to injuries, tumor, or tuberculosis; 3) pure discectomy without internal fixation and/or bone graft fusion; 4) extension of growing rod, revision, or any other history of spine surgery; 5) failure to undergo CT examination for any reason or refusing to be included in the study.
DATA COLLECTED:
A total of 161 patients were included, and 7 of them were excluded from the risk factor analysis due to lack of necessary data.
All patients were grouped according to type of scoliosis: 1) AIS, 2) CS, 3) NMS, 4) NFS, 5) SS, 6) ADS. The CT scanning thickness was 0.625 mm and scanning was continuous. A sagittal reference image was first acquired to guide positioning of the epiglottic cartilage level, then the location of the glottic entrance was determined. In some cases, the glottic entrance is not the narrowest level, so the section of interest might shift, but still represent the major difficulty in intubation under direct vision. Afterwards, 3 parameters of glottic entrance were measured using ImageJ software (http://imagej.net/ImageJ). The measurement was based on a prior study [19]. As shown in Figure 1, the proportional scale was first measured to set the scale based on pixels, then the sagittal diameter and transverse diameter were measured. Subsequently, the image was enlarged and the inner edge of the glottic entrance was split into line segments by linking continuous points. The cross-section area of the glottic entrance was the area enclosed by those lines (Figure 2).
Three kinds of data were collected: basic information, parameters concerning body balance, and condition of spinal deformity. Basic information included age, gender, height, body weight, BMI, course of disease, fixation range, main curve type (thoracic or thoracolumbar/lumbar curve), and combined cardiac structure deformity or pulmonary function abnormity.
Balance-related parameters were measured in sagittal and coronal all-spine X-rays. Those parameters were directly recorded as continuous variables and transferred into classified variables to solve abnormal distribution and improve goodness of fit. All sagittal spino-pelvic parameters were recorded to describe sagittal balance, including upper thoracic kyphosis angle (T2–T5), lower thoracic kyphosis angle (T5–T12), thoracolumbar lordosis angle (T10-L2), lumbar lordosis angle (T12-S1), sagittal vertical axis (SVA), sacral inclination (SS), pelvic inclination (PT), and pelvic inclination (PI). Measurement criteria for these parameters have been provided in previous articles [20]. T2-T5 is described as normal (within 0–20°) or abnormal (over 20°). T5–T12 is presented as flat back (0–10°), normal (10–40°), and kyphosis (over 40°). T10-L2 is classified as 0, 0–20°, 20–40°, 40–60°, and over 60°. T12-S1 is divided into under 30°, 30~70°, and over 70°. SVA is presented as normal (0–4 cm) or unbalanced (over 4 cm). Using the formula of PI (PT+SS), and the principle of independent variables in statistical analysis of risk factors, only PI was included, and the level was set as 0–20°, 20–40°, 40-60°, and 60–80°. Coronal parameters include Cobb angle, flexibility, and trunk shift (TS). Flexibility= (Cobb angle-bending Cobb angle)/Cobb angle*100%. Flexibility is divided into 0%, 0–25%, 25–50%, 50–75%, 75–100%, and 100%. The TS value is equally divided into 6 levels from 0 to 6 cm.
Spinal deformity is diagnosed by X-ray and CT, including butterfly vertebrae, wedge vertebrae, rachischisis, hemivertebra, and vertebrae dyssegmentation. Spinal cord malformation includes syringomyelia and diastematomyelia, which are verified by all-spine MRI.
In this study we have proposed the term “glottic entrance stenosis”, based on the theoretical tracheal tube diameter (age/4+4 cm for children and adolescent and 8.5 cm for adults) [21]. Patients with sagittal glottic entrance diameter less than the theoretical value are defined as sagittal stenosis transverse stenosis, and area stenosis is defined in the same way. Glottic entrance stenosis is defined as meeting any of the criteria for stenosis.
STATISTICAL ANALYSIS:
The first step was the comparison among 6 groups. The Shapiro-Wilk normality test was performed to determine the distribution normality of all data. Normally distributed data were presented as means ± standard deviation (SD) and analyzed using the variance analysis of multiple independent samples. Skewed distributed data were shown as medians (range) and analyzed using the nonparametric Wilcoxon rank-sum test for multiple independent samples. Afterwards, the incidence of sagittal, transverse, area, and glottic entrance stenosis were compared using the R*C chi-square test. Risk factor analysis was performed using logistic regression. Statistical analysis was performed using SPSS software (version 20). The difference was considered statistically significant at
Results
DEMOGRAPHIC DATA:
The study consisted of 161 patients who met the inclusion and exclusion criteria, including 42 males and 119 females, with an average number of fixed segments of 10.78±3.32. The mean age of patients was 16.87±6.70 years. The mean BMI was 18.95±3.82. The mean course of disease was 6.09±6.95 years. The main curve type of 100 patients was thoracolumbar or lumbar curve, and 61 patients had thoracic curve.
GLOTTIC ENTRANCE PARAMETERS AND INCIDENCE OF GLOTTIC ENTRANCE STENOSIS:
According to normality testing, data are shown in proper form in Table 1. The mean sagittal diameter, transverse diameter, and glottic entrance area of all scoliosis patients were 15.67±28.89 mm, 8.32 (0.00~15.65) mm and 103.50 (0.00~292.92) mm2, respectively. Overall incidences of sagittal stenosis, transverse stenosis, and area stenosis were 9.9%, 35.4%, and 12.4%, respectively. Glottic entrance stenosis was present in 37.9% of scoliosis patients. There was no significant difference among the 6 groups.
RISK FACTORS OF GLOTTIC ENTRANCE STENOSIS:
In this section, we excluded 7 patients due to lack of necessary data. These patients had serious spinal deformation and were unable to complete some physical and radiological examinations. To minimize analysis error, we finally included 154 patients with complete data into risk factor analysis.
In the analysis of sagittal diameter stenosis, all 154 patients were divided into either the sagittal stenosis group or the no sagittal stenosis group. The subsequent analysis used a similar grouping method. As shown in Table 2, 12 factors were included in bivariate logistic regression analysis. Course of disease was positively correlated with the incidence of sagittal stenosis (P=0.037, OR=1.099). Table 3 provides an overview of risk factors of transverse stenosis. Seven factors were included into analysis. Smaller angle from T12 to S1 was a risk factor of transverse stenosis (P=0.024, OR=0.554). Table 4 shows that wedged vertebrae are the risk factor of area stenosis (P=0.024, OR=7.992).
The results of the correlational analysis for any type of stenosis are displayed in Table 5. After summing up all types of stenosis and analyzing the correlation, 5 factors were selected and brought into calculation. There was no significant correlation between gender, wedged vertebrae, hemivertebrae, diplomyelia, main curve Cobb, and any type of glottic entrance stenosis.
Discussion
The study found that 37.9% of scoliosis patients also have at least 1 type of glottic entrance stenosis, which is a significant proportion for anesthetists to consider. In addition, we found that longer course of disease, smaller lumbar lordosis, and wedged vertebrae were risk factors for glottic entrance stenosis. These results will remind anesthetists to better prepare for intubation in certain patients.
Some studies have used ultrasonography to predict the feasibility of endotracheal intubation by measuring the cricoid cartilage diameter [13–16]. Hao et al used ultrasonography to measure the transverse diameter of cricoid cartilage in 50 patients with congenital scoliosis to predict the size of endotracheal intubation, but the measurement was biased due to cone rotation [16]. The glottic entrance is usually the narrowest area of the trachea [17,18]. In a prospective study involving 95 children, a correlation was found between the glottis diameter measured by ultrasonography and endotracheal intubation size [17], but generalizability of that study is confined to only healthy children with no previous airway abnormalities. We chose to use CT to measure glottic parameters for better accuracy. In addition, CT is required in patients undergoing surgery for scoliosis if anesthetists want to obtain glottic parameters to assess the difficulty of intubation, so the patient will not need to undergo an additional procedure. In our study, transverse stenosis was the most common type, which occurred in 35.4% of patients, and sagittal stenosis was relatively rare (9.9%), which may indicate that glottic entrance stenosis is mainly associated with intensive tension of the glottis. Since there was no difference among groups, and the overall incidence of glottic entrance stenosis was high, we suggest that anesthetists need to be vigilant and regard all types of scoliosis cases as potentially difficult airway intubation. It is necessary to prepare by having on hand all sizes of endotracheal tubes and GlideScopes.
No study has determined the risk factors for difficult intubation of various types of scoliosis patients. These factors were carefully chosen for the present study. Some general information is relevant to body development, including height, body weight, BMI, and gender. Previous research has indicated that cardiac malformation and ventilation disorder might be associated with developmental vertebrae deformation [22,23]. Previous surgery may affect the airway structure [24]. The present classification of scoliosis is only suitable for adolescent idiopathic scoliosis [25], so in this study we only analyzed the main curve, including curve type (thoracic or thoracolumbar/lumbar curve), curve angle, and flexibility. The feature of the main curve may reflect the seriousness of scoliosis, and this might be related to deformation of other systems. Trunk balance parameters ere also analyzed, including TS, SVA, PI, upper thoracic kyphosis angle, lower thoracic kyphosis angle, thoracolumbar lordosis angle and lumbar lordosis angle, lower limb discrepancy, shoulder discrepancy, and hip discrepancy. Vertebrae and spinal cord abnormalities are considered specific features of spine malformation, so we included these in our research.
In the regression analysis, when analyzing risk factors of any type of stenosis, none of the involved factors shows significant relevance, but after exploring 3 types of stenosis individually, we achieved some meaningful results. Course of disease is a risk factor for sagittal stenosis. This may not be explained by the increase of age, as this factor had been excluded in primary correlation analysis. One reasonable speculation is the increasing great influence of scoliosis on sagittal development of the glottis. Lumbar lordosis angle (T12-S1) is negatively correlated with transverse stenosis. Considering the translated form of data, this indicates that smaller lumbar lordosis angle (<30°) is a risk factor for transverse stenosis. Lumbar lordosis angle is regarded as a compensatory indicator of scoliosis, which increases when scoliosis worsens, and larger T12-S1 reflects better compensatory ability of the spine [26]. A smaller lumbar lordosis angle may indicate more difficulty in maintaining sagittal trunk balance and a loss of bearing capacity of the lumbar spine. It is confusing that this association has not been found in the thoracic kyphosis angle, which is anatomically closer to the airway. This may be a consequence of overall imbalance. Wedged vertebrae are positively associated with area stenosis. Chen’s research has revealed that deactivation of osterix (an important transcriptional factor for bone formation) contributes to wedged vertebrae and scoliosis in mice [27], and this factor is also involved in regulation of cartilage development [28]. Since cartilage is an important component of tracheal tissue, some regulators may have simultaneous effects on airway development and scoliosis progress. Furthermore, it has been proved that serotonin can help maintain muscle tone to keep posture balance [29], and serotonin is widely recognized as an important regulatory factor in the respiratory airway. Serotonin contributes to redistribution of pulmonary blood flow, regulation of bronchomotor tone, and regulation of lung growth and development [30], and this might be a common mechanism of respiratory deformation and scoliosis. Future research should focus on revealing the common mechanism of glottic entrance stenosis and scoliosis, so as to provide a theoretical basis for identifying scoliosis patients with potentially difficult intubation.
A number of limitations need to be noted regarding the present study. Firstly, the sample size included in the analysis of risk factors does not meet the requirements of Event Per Variable, which will unavoidably affect the reliability of the statistical results. However, due to the scarcity of scoliosis cases, we believe that the results of this study have some value and provide a new direction for future research. This is the first study on this topic, and further studies with larger sample sizes are needed to generate higher-quality results. Secondly, the definition of “glottic entrance stenosis” has not been tested in anesthesia practice, so the accuracy and specificity remain unclear. However, it is widely accepted that the glottic entrance is the narrowest plane in the process of intubation, and measurement based on CT scan is feasible, so these parameters combined with other physical examinations could provide anesthetists with supplementary information in prediction of difficult airway intubation.
Conclusions
This study comprehensively measured glottic entrance parameters in patients with scoliosis, proposed a new definition of glottic entrance stenosis, and found that longer course of disease, smaller lumbar lordosis, and wedged vertebrae were risk factors for sagittal stenosis, transverse stenosis, and area stenosis, respectively. These findings will provide a meaningful reference to predict potential difficult intubation and help to prevent accidents and complications in general anesthesia.
Figures
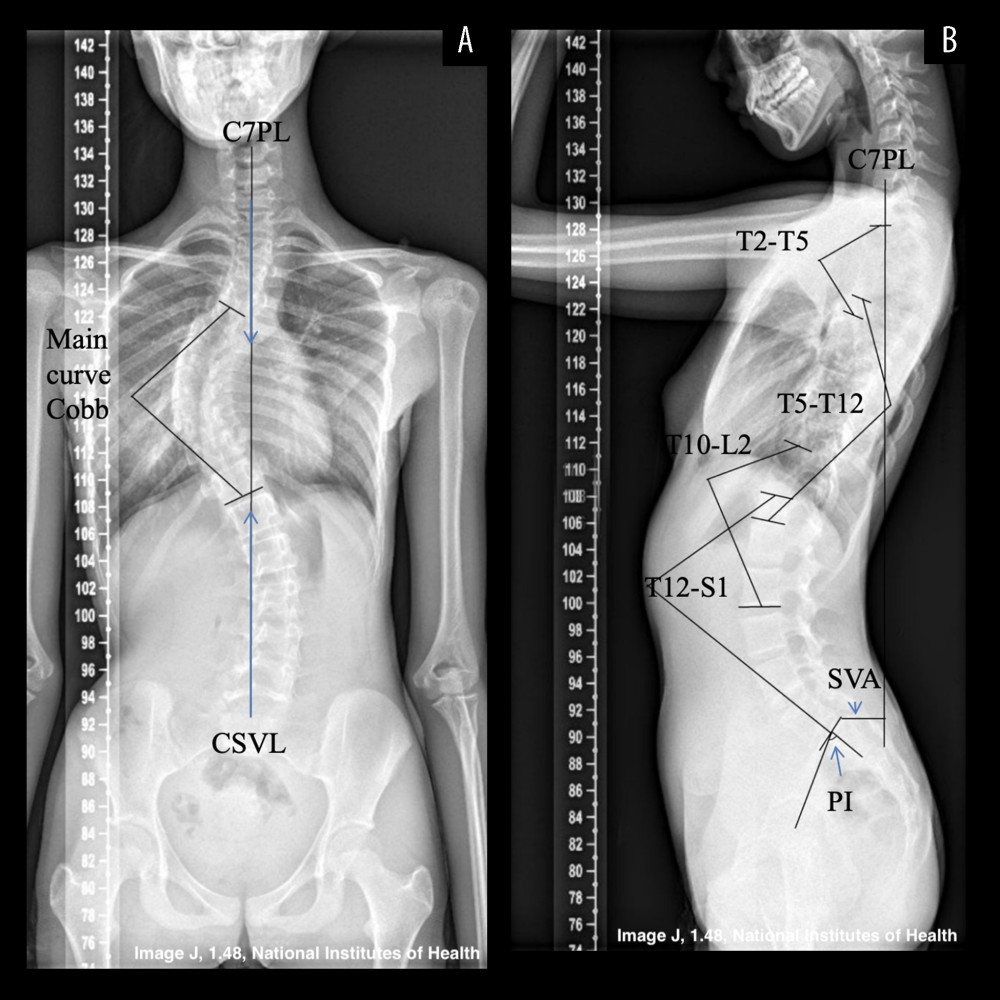 Figure 1. Coronal and sagittal parameters in all-spine X-ray. Case 1, an 11-year-old female diagnosed with AIS. (A) Anterior-posterior radiograph. The main curve was thoracic curve from T7 to T11, and the Cobb angle is 61°. Shoulder discrepancy and hip discrepancy were noted. No obvious vertebrae malformation was found. C7PL (C7 Plumb Line) and CSVL (Center Sacral Vertical Line) coincide, so TS (trunk shift) is 0 mm. (B) Lateral all-spine radiograph. Pelvic incidence (PI): the angle between center sacral vertical line and center of femur head. Upper thoracic kyphosis: the angle between upper endplate of T2 and lower plate of T5. Lower thoracic kyphosis: the angle between upper endplate of T5 and lower endplate of T12. Thoracolumbar lordosis: the angle between upper endplate of T10 and lower endplate of L2. Lumbar lordosis: the angle between upper endplate of T12 and upper endplate of S1. SVA (sagittal vertebrae axis): the vertical distance from C7PL to posterior border of S1 upper endplate.
Figure 1. Coronal and sagittal parameters in all-spine X-ray. Case 1, an 11-year-old female diagnosed with AIS. (A) Anterior-posterior radiograph. The main curve was thoracic curve from T7 to T11, and the Cobb angle is 61°. Shoulder discrepancy and hip discrepancy were noted. No obvious vertebrae malformation was found. C7PL (C7 Plumb Line) and CSVL (Center Sacral Vertical Line) coincide, so TS (trunk shift) is 0 mm. (B) Lateral all-spine radiograph. Pelvic incidence (PI): the angle between center sacral vertical line and center of femur head. Upper thoracic kyphosis: the angle between upper endplate of T2 and lower plate of T5. Lower thoracic kyphosis: the angle between upper endplate of T5 and lower endplate of T12. Thoracolumbar lordosis: the angle between upper endplate of T10 and lower endplate of L2. Lumbar lordosis: the angle between upper endplate of T12 and upper endplate of S1. SVA (sagittal vertebrae axis): the vertical distance from C7PL to posterior border of S1 upper endplate. 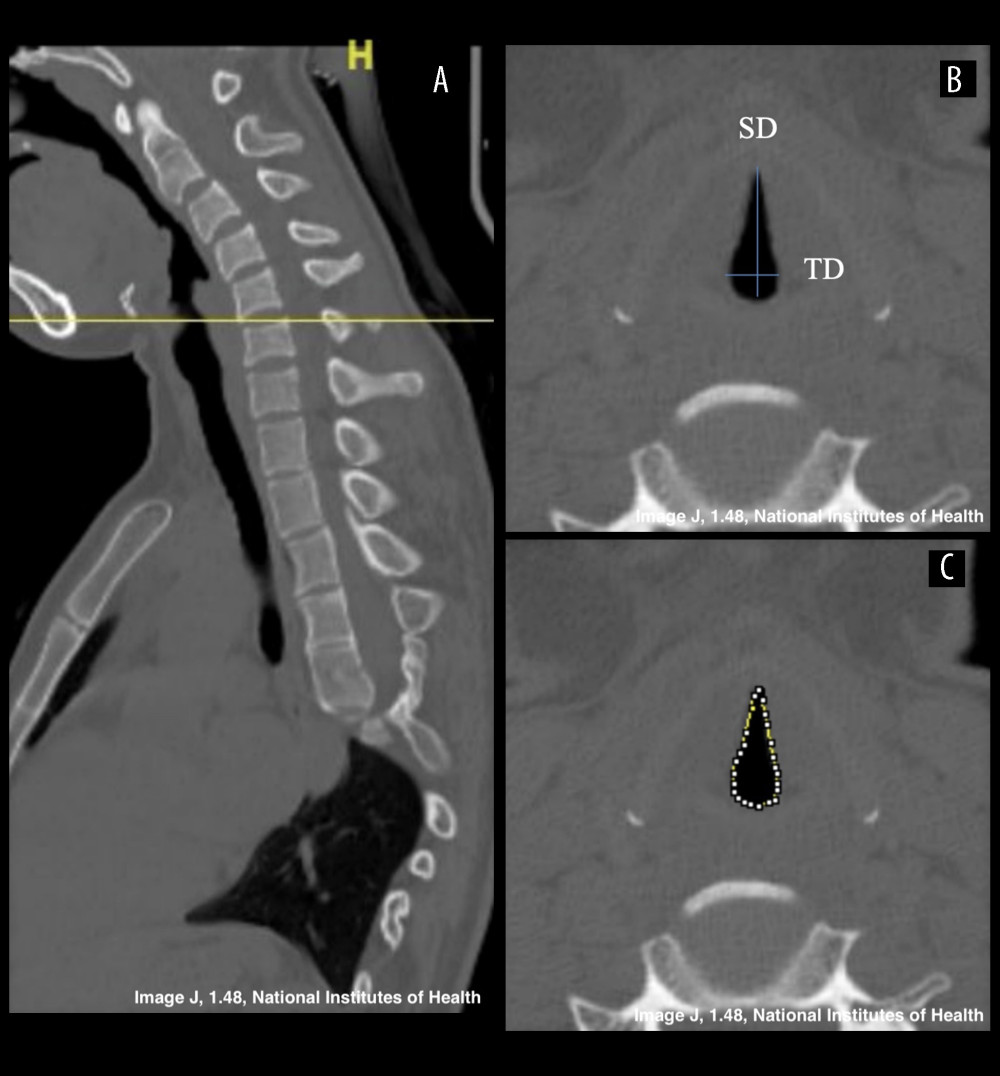 Figure 2. Measurement of glottic entrance parameters. (A) Cross-reference of sagittal image helps to find location of glottic entrance. Most of them are located at the level of epiglottic cartilage, but in some patients the narrowest plane is regarded as the glottic entrance. (B) Sagittal diameter is the distance from anterior end and posterior end of glottic entrance (line a). Transverse diameter is the broadest distance between lateral sides. (C) Cross-section area is measured by linking points on the medial wall of the glottic entrance.
Figure 2. Measurement of glottic entrance parameters. (A) Cross-reference of sagittal image helps to find location of glottic entrance. Most of them are located at the level of epiglottic cartilage, but in some patients the narrowest plane is regarded as the glottic entrance. (B) Sagittal diameter is the distance from anterior end and posterior end of glottic entrance (line a). Transverse diameter is the broadest distance between lateral sides. (C) Cross-section area is measured by linking points on the medial wall of the glottic entrance. Tables
Table 1. Comparison of glottic entrance parameters and incidence of stenosis in different types of scoliosis. Table 2. Risk factors for sagittal glottic entrance stenosis.
Table 2. Risk factors for sagittal glottic entrance stenosis.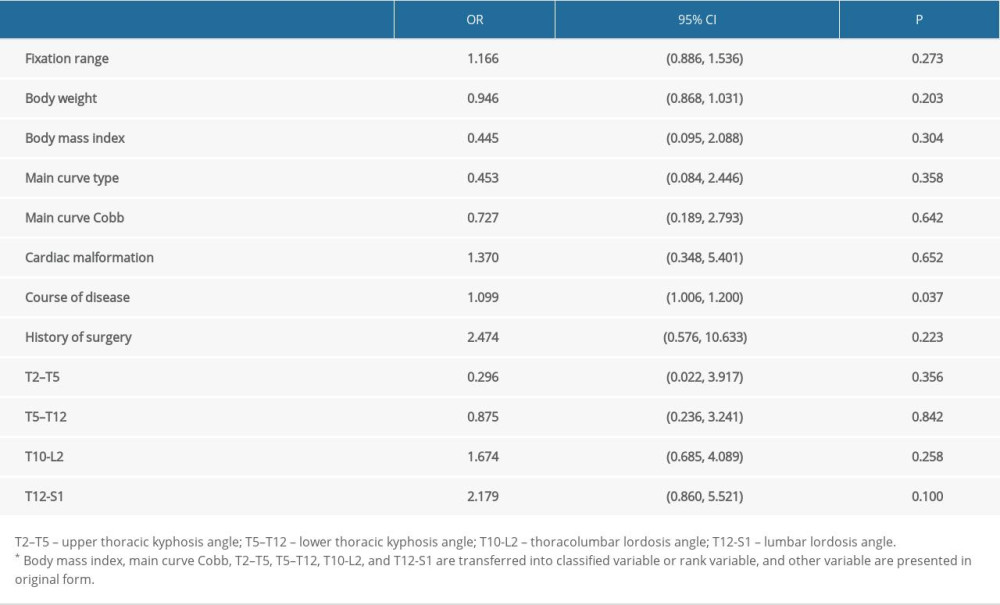 Table 3. Risk factors for transverse glottic entrance stenosis.
Table 3. Risk factors for transverse glottic entrance stenosis. Table 4. Risk factors for area glottic entrance stenosis.
Table 4. Risk factors for area glottic entrance stenosis.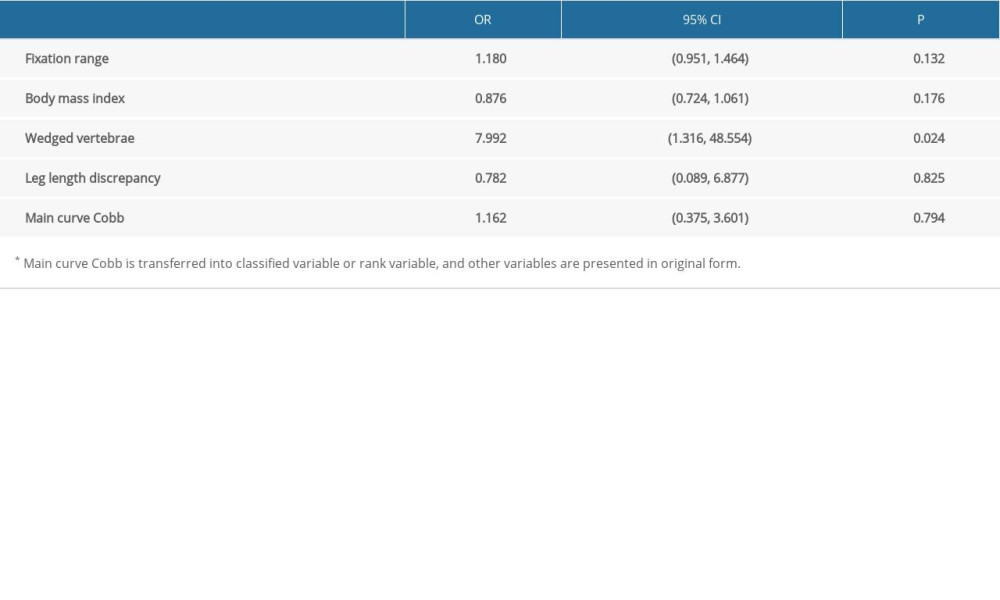 Table 5. Risk factors for all type of glottic entrance stenosis.
Table 5. Risk factors for all type of glottic entrance stenosis.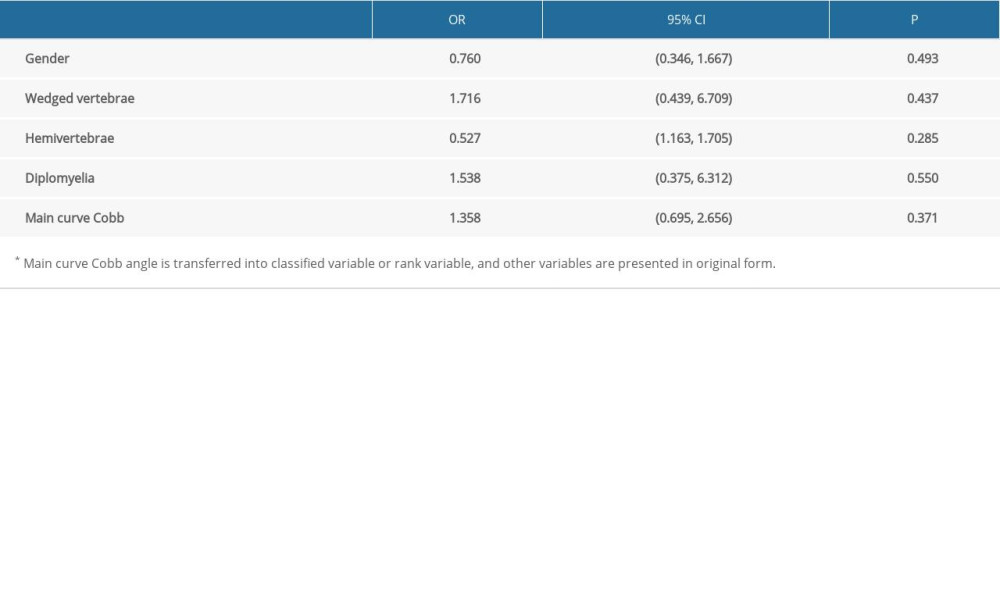
References
1. Shakil H, Iqbal ZA, Al-Ghadir AH, Scoliosis: Review of types of curves, etiological theories and conservative treatment: J Back Musculoskelet Rehabil, 2014; 27(2); 111-15
2. Bettany-Saltikov J, Turnbull D, Ng S, Management of spinal deformities and evidence of treatment effectiveness: Open Orthop J, 2017; 11; 1521-47
3. Hardesty C, Huang R, El-Hawary R, Early-onset scoliosis: Updated treatment techniques and results: Spine Deform, 2018; 6(4); 467-72
4. Ulici V, Kelley KL, Longobardi L, Impaired annulus fibrosus development and vertebral fusion cause severe scoliosis in mice with deficiency of c-Jun NH2-terminal kinases 1 and 2: Am J Pathol, 2019; 189(4); 868-85
5. Li J, Tang M, Yang G, Muscle injury associated elevated oxidative stress and abnormal myogenesis in patients with idiopathic scoliosis: Int J Biol Sci, 2019; 15(12); 2584-95
6. Hefti F, Pathogenesis and biomechanics of adolescent idiopathic scoliosis (AIS): J Child Orthop, 2013; 7(1); 17-24
7. Arora R, Metzger RJ, Papaioannou VE, Multiple roles and interactions of Tbx4 and Tbx5 in development of the respiratory system: PLoS Genet, 2012; 8(8); e1002866
8. Wang J, Zhou B, Yang X, Computed tomography-based bronchial tree three-dimensional reconstruction and airway resistance evaluation in adolescent idiopathic scoliosis: Eur Spine J, 2020; 29(8); 1981-92
9. Furutani K, Kodera Y, Hiruma M, Difficult tracheal intubation in a patient with maternal uniparental disomy 14: JA Clin Rep, 2016; 2(1); 25
10. Hilton G, Mihm F, Butwick A, Anesthetic management of a parturient with VACTERL association undergoing Cesarean delivery: Can J Anaesth, 2013; 60(6); 570-76
11. Ahmed A, Azim A, Difficult tracheal intubation in critically ill: J Intensive Care, 2018; 6; 49
12. Corbett M, Hughes I, O’Shea J, X-ray and CT scan based prediction of best fit tracheostomy tube – a pilot study, 2020; 10(8); 506
13. Alonso Quintela P, Oulego Erroz I, Mora Matilla MUsefulness of bedside ultrasound compared to capnography and X-ray for tracheal intubation: An Pediatr (Barc), 2014; 81(5); 283-88 [in Spanish]
14. Altun D, Sungur M, Ali A, Ultrasonographic measurement of subglottic diameter for paediatric cuffed endotracheal tube size selection: Feasibility report: Turk J Anaesthesiol Reanim, 2016; 44(6); 301-5
15. Shibasaki M, Nakajima Y, Ishii S, Prediction of pediatric endotracheal tube size by ultrasonography: Anesthesiology, 2010; 113(4); 819-24
16. Hao J, Zhang J, Dong B, The accuracy of ultrasound to predict endotracheal tube size for pediatric patients with congenital scoliosis: BMC Anesthesiol, 2020; 20(1); 183
17. Deekiatphaiboon C, Oofuvong M, Karnjanawanichkul O, Ultrasonography measurement of glottic transverse diameter and subglottic diameter to predict endotracheal tube size in children: A prospective cohort study: Sci Rep, 2022; 12(1); 15215
18. Dalal P, Murray D, Messner A, Pediatric laryngeal dimensions: An age-based analysis: Anesth Analg, 2009; 108(5); 1475-79
19. Wani T, Bissonnette B, Rafiq Malik M, Age-based analysis of pediatric upper airway dimensions using computed tomography imaging: Pediatr Pulmonol, 2016; 51(3); 267-71
20. Schroeder J, Schaar H, Mattes K, Spinal alignment in low back pain patients and age-related side effects: A multivariate cross-sectional analysis of video rasterstereography back shape reconstruction data: Eur Spine J, 2013; 22(9); 1979-85
21. Khine H, Corddry D, Kettrick R, Comparison of cuffed and uncuffed endotracheal tubes in young children during general anesthesia: Anesthesiology, 1997; 86(3); 627-31 discussion 27A
22. Zhu L, Peng JL, Harutyunyan KG, Craniofacial, skeletal, and cardiac defects associated with altered embryonic murine Zic3 expression following targeted insertion of a PGK-NEO cassette: Front Biosci, 2007; 12; 1680-90
23. Sakić K, Pećina M, Pavicić F, Cardiorespiratory function in surgically treated thoracic scoliosis with respect to degree and apex of scoliotic curve: Respiration, 1992; 59(6); 327-31
24. Aday U, Impact of prior different abdominal or pelvic surgery on cecal intubation time: A prospective observational study: Acta Gastroenterol Belg, 2020; 83(4); 541-48
25. Lenke LG, Lenke classification system of adolescent idiopathic scoliosis: Treatment recommendations: Instr Course Lect, 2005; 54; 537-42
26. Lafage V, Schwab F, Patel A, Pelvic tilt and truncal inclination: Two key radiographic parameters in the setting of adults with spinal deformity: Spine (Phila Pa 1976), 2009; 34(17); E599-606
27. Chen S, Feng J, Zhang H, Key role for the transcriptional factor, osterix, in spine development: Spine J, 2014; 14(4); 683-94
28. Nishimura R, Hata K, Matsubara T, Regulation of bone and cartilage development by network between BMP signalling and transcription factors: J Biochem, 2012; 151(3); 247-54
29. Machida M, Miyashita Y, Murai I, Role of serotonin for scoliotic deformity in pinealectomized chicken: Spine (Phila Pa 1976), 1997; 22(12); 1297-301
30. Van Lommel A, Pulmonary neuroendocrine cells (PNEC) and neuroepithelial bodies (NEB): Chemoreceptors and regulators of lung development: Paediatr Respir Rev, 2001; 2(2); 171-76
Figures
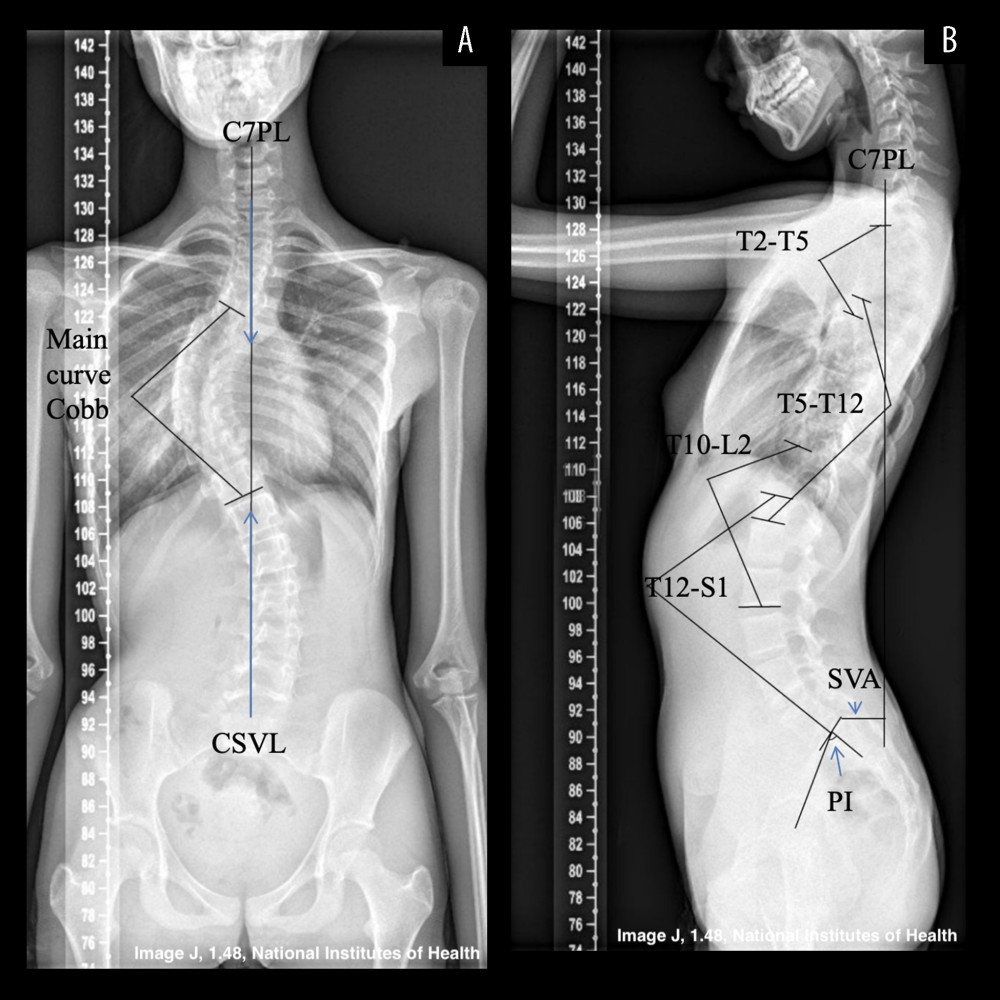 Figure 1. Coronal and sagittal parameters in all-spine X-ray. Case 1, an 11-year-old female diagnosed with AIS. (A) Anterior-posterior radiograph. The main curve was thoracic curve from T7 to T11, and the Cobb angle is 61°. Shoulder discrepancy and hip discrepancy were noted. No obvious vertebrae malformation was found. C7PL (C7 Plumb Line) and CSVL (Center Sacral Vertical Line) coincide, so TS (trunk shift) is 0 mm. (B) Lateral all-spine radiograph. Pelvic incidence (PI): the angle between center sacral vertical line and center of femur head. Upper thoracic kyphosis: the angle between upper endplate of T2 and lower plate of T5. Lower thoracic kyphosis: the angle between upper endplate of T5 and lower endplate of T12. Thoracolumbar lordosis: the angle between upper endplate of T10 and lower endplate of L2. Lumbar lordosis: the angle between upper endplate of T12 and upper endplate of S1. SVA (sagittal vertebrae axis): the vertical distance from C7PL to posterior border of S1 upper endplate.
Figure 1. Coronal and sagittal parameters in all-spine X-ray. Case 1, an 11-year-old female diagnosed with AIS. (A) Anterior-posterior radiograph. The main curve was thoracic curve from T7 to T11, and the Cobb angle is 61°. Shoulder discrepancy and hip discrepancy were noted. No obvious vertebrae malformation was found. C7PL (C7 Plumb Line) and CSVL (Center Sacral Vertical Line) coincide, so TS (trunk shift) is 0 mm. (B) Lateral all-spine radiograph. Pelvic incidence (PI): the angle between center sacral vertical line and center of femur head. Upper thoracic kyphosis: the angle between upper endplate of T2 and lower plate of T5. Lower thoracic kyphosis: the angle between upper endplate of T5 and lower endplate of T12. Thoracolumbar lordosis: the angle between upper endplate of T10 and lower endplate of L2. Lumbar lordosis: the angle between upper endplate of T12 and upper endplate of S1. SVA (sagittal vertebrae axis): the vertical distance from C7PL to posterior border of S1 upper endplate.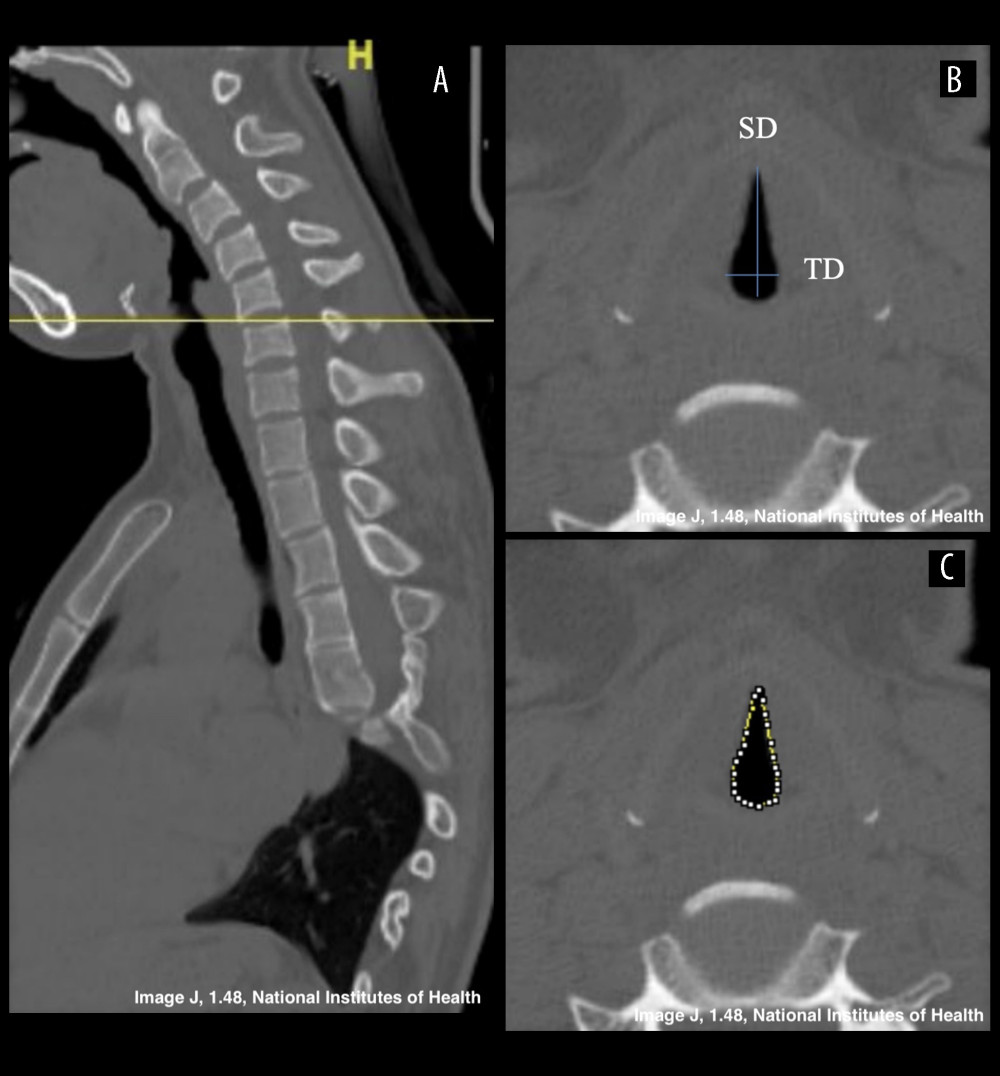 Figure 2. Measurement of glottic entrance parameters. (A) Cross-reference of sagittal image helps to find location of glottic entrance. Most of them are located at the level of epiglottic cartilage, but in some patients the narrowest plane is regarded as the glottic entrance. (B) Sagittal diameter is the distance from anterior end and posterior end of glottic entrance (line a). Transverse diameter is the broadest distance between lateral sides. (C) Cross-section area is measured by linking points on the medial wall of the glottic entrance.
Figure 2. Measurement of glottic entrance parameters. (A) Cross-reference of sagittal image helps to find location of glottic entrance. Most of them are located at the level of epiglottic cartilage, but in some patients the narrowest plane is regarded as the glottic entrance. (B) Sagittal diameter is the distance from anterior end and posterior end of glottic entrance (line a). Transverse diameter is the broadest distance between lateral sides. (C) Cross-section area is measured by linking points on the medial wall of the glottic entrance. Tables
 Table 1. Comparison of glottic entrance parameters and incidence of stenosis in different types of scoliosis.
Table 1. Comparison of glottic entrance parameters and incidence of stenosis in different types of scoliosis.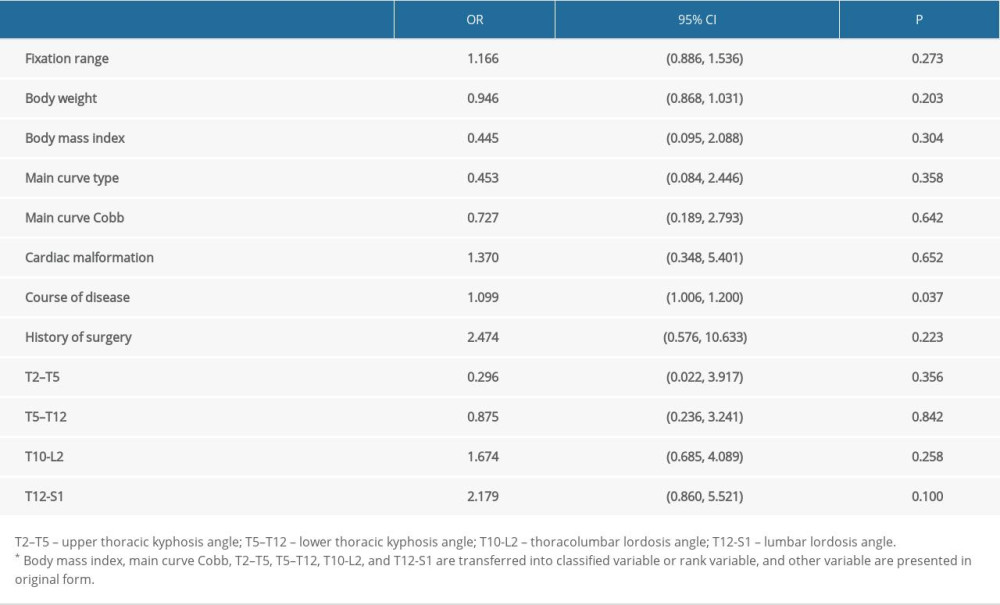 Table 2. Risk factors for sagittal glottic entrance stenosis.
Table 2. Risk factors for sagittal glottic entrance stenosis. Table 3. Risk factors for transverse glottic entrance stenosis.
Table 3. Risk factors for transverse glottic entrance stenosis.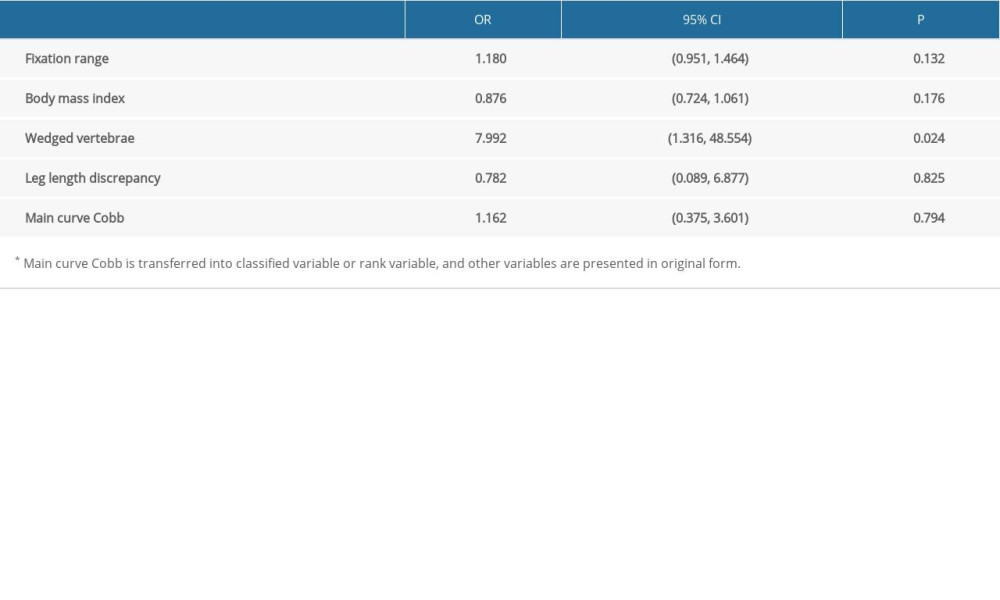 Table 4. Risk factors for area glottic entrance stenosis.
Table 4. Risk factors for area glottic entrance stenosis.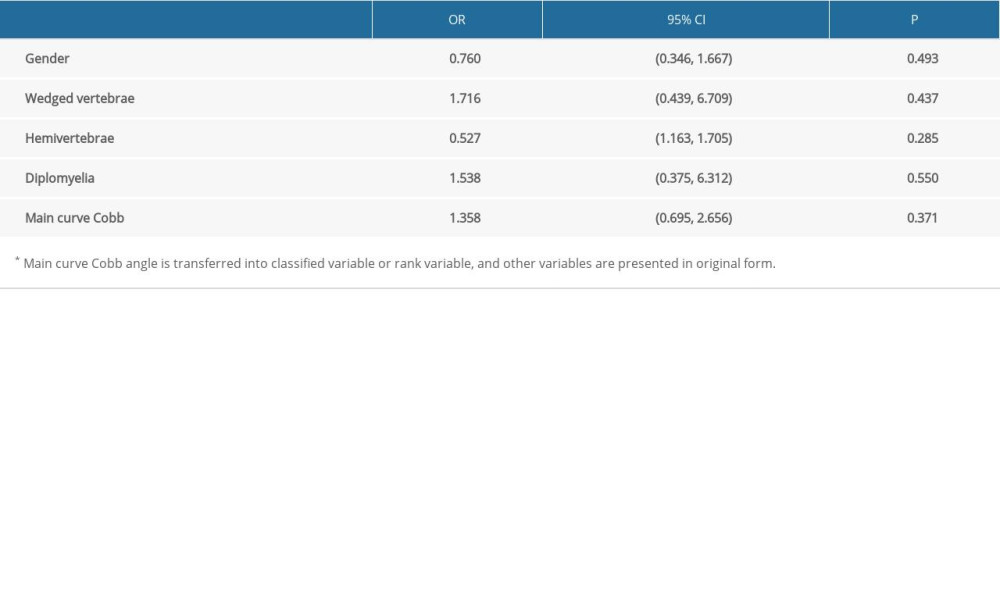 Table 5. Risk factors for all type of glottic entrance stenosis.
Table 5. Risk factors for all type of glottic entrance stenosis. Table 1. Comparison of glottic entrance parameters and incidence of stenosis in different types of scoliosis.
Table 1. Comparison of glottic entrance parameters and incidence of stenosis in different types of scoliosis.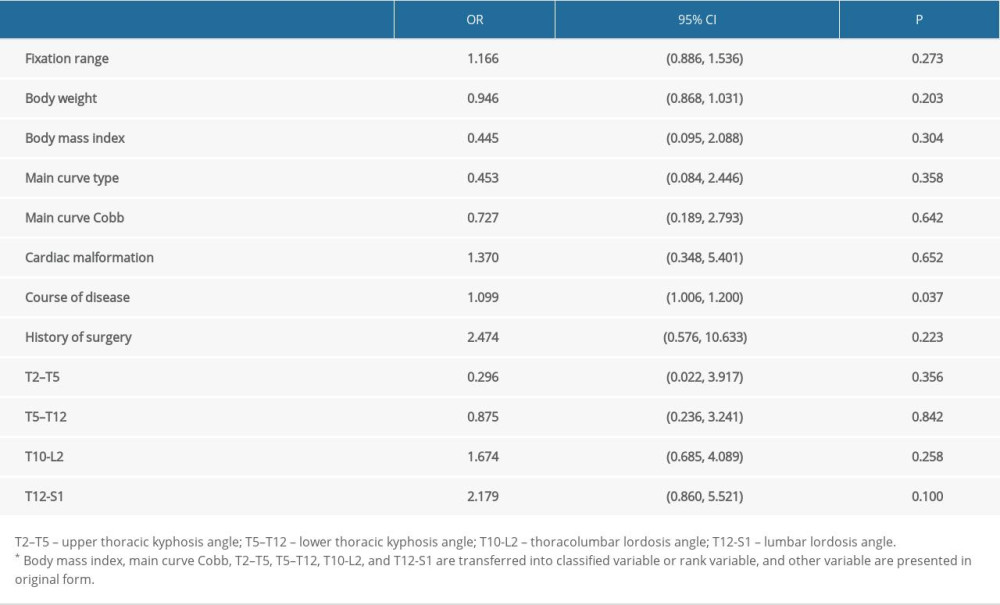 Table 2. Risk factors for sagittal glottic entrance stenosis.
Table 2. Risk factors for sagittal glottic entrance stenosis. Table 3. Risk factors for transverse glottic entrance stenosis.
Table 3. Risk factors for transverse glottic entrance stenosis.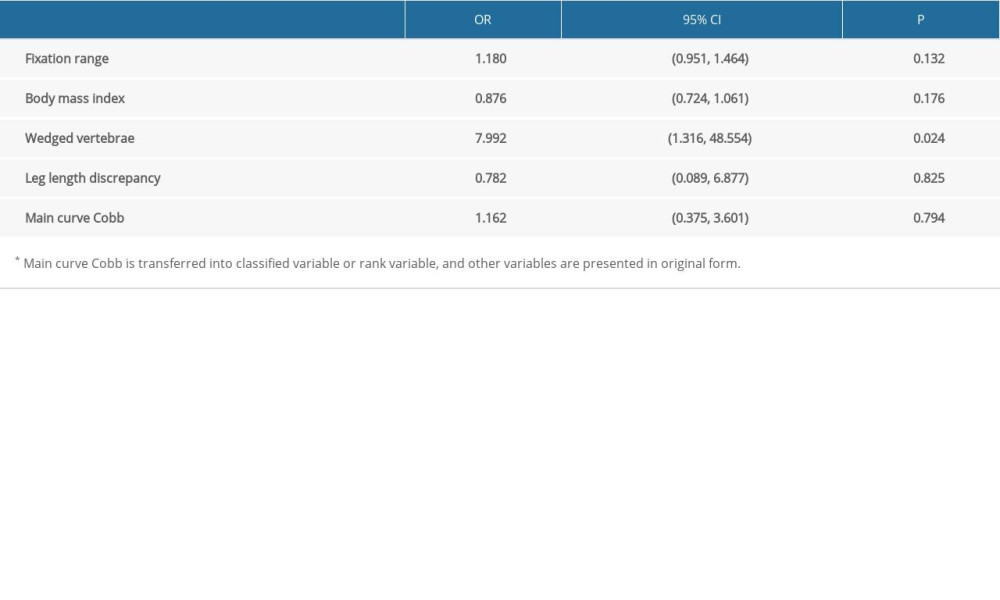 Table 4. Risk factors for area glottic entrance stenosis.
Table 4. Risk factors for area glottic entrance stenosis.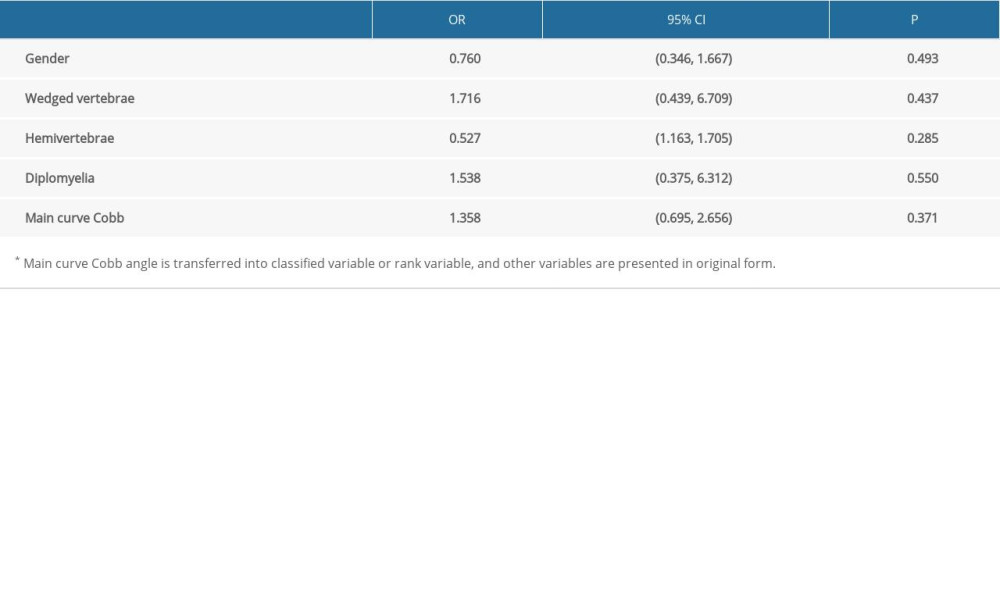 Table 5. Risk factors for all type of glottic entrance stenosis.
Table 5. Risk factors for all type of glottic entrance stenosis. In Press
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








