26 August 2022: Clinical Research
Effect of Positive End-Expiratory Pressure (PEEP) Titration in Elderly Patients Undergoing Lobectomy
Wenyu Yao1AE*, Bo Yang2B, Wenlong Wang3B, Qian Han1D, Fenghai Liu4D, Shiqiang Shan1G, Chao Wang1E, Mengliang Zheng1FDOI: 10.12659/MSM.938225
Med Sci Monit 2022; 28:e938225
Abstract
BACKGROUND: Currently, one-lung ventilation in thoracoscopic lobectomy adopts mostly a protective ventilation mode, which includes low tidal volume (a tidal volume of 6 mL/kg predicted body weight), positive end-expiratory pressure (PEEP), and intermittent lung inflation. However, there is no clear conclusion regarding the value of PEEP in elderly patients undergoing lobectomy.
MATERIAL AND METHODS: Fifty patients who underwent video-assisted thoracoscopic unilateral lobectomy, aged 65 to 78 years, with a body mass index of 18 to 29 kg/m² and ASA grades I to III, were randomly divided into 2 groups (n=25 each): optimal oxygenation titration group (group O) and optimal compliance titration group (group C). Mean arterial pressure (MAP), heart rate (HR), and central venous pressure (CVP) were recorded in both groups at different time points. The radial artery blood samples were collected at 3 time points for blood gas analysis, and the void volume/tidal volume ratio was calculated. The peak airway pressure and PEEP values were recorded at 4 min after the completion of one-lung ventilation titration (T2), and the driving pressure was calculated.
RESULTS: The best PEEP value of titration in the best compliance group was lower than that of the best oxygenation method, the peak was lower, and the dynamic lung compliance was higher; however, this had no effect on MAP and HR. The CVP was lower than optimal oxygenation at T2.
CONCLUSIONS: Dynamic lung compliance-guided PEEP titration improved lung function in elderly patients undergoing lobectomy.
Keywords: Thoracic Surgery, Video-Assisted, Aged, Respiration, Artificial, Respiratory Function Tests, Humans, Positive-Pressure Respiration, Tidal Volume, one-lung ventilation, Lung, Blood Gas Analysis
Background
There is no consensus on how to choose the appropriate positive end-expiratory pressure (PEEP) value during one-lung ventilation (OLV) in current research reports. Improper PEEP levels have an impact on patient physiology. If the setting level is too low to achieve the desired purpose, it cannot produce the effect of applying PEEP. If the setting level is too high, the pulmonary vascular resistance increases, venous return blood volume decreases, intrapulmonary shunt increases, and arterial oxygen partial pressure level is reduced [1]. When the PEEP is too high, the alveoli can produce excessive expansion at the end of exhalation, resulting in mechanical or biological damage to the lung tissue [2]. Therefore, determining how to individualize the optimal PEEP level according to the respiratory condition of elderly patients has gradually attracted the attention of clinicians. The methods to determine the best PEEP levels include computed tomography scanning, electrical impedance tomography, ultrasound, P-V curve method, best oxygenation titration method, and best lung compliance titration method. Each method has its advantages and disadvantages [3–5]. There are few studies on the selection of PEEP values during OLV in elderly patients and the protective effect of PEEP values titrated by different titration methods on the lungs of elderly patients. Therefore, the effect of PEEP titrated by different methods during OLV on lung protection needs to be further confirmed.
Material and Methods
STUDY DESIGN AND OBJECTIVES:
This single-center randomized controlled study was approved by the Cangzhou Central Hospital, China (ethics approval no. 2018-024-01, Clinical Trial Registration Identifier: ChiCTR1800017835). Informed consent was obtained from the patients or their relatives. Fifty patients with video-assisted thoracoscopic unilateral lobectomy who were aged 65 to 78 years and had a body mass index of 18 to 29 kg/m2 and ASA grade I to III were enrolled. The inclusion criteria were as follows: (1) without circulatory system diseases, (2) without acute or chronic pulmonary inflammation, (3) without a history of chest surgery and trauma, (4) without a history of psychosis or nervous system diseases, and (5) without serious liver or kidney dysfunction. The random number table method was used to divide the patients into 2 groups (n=20 each): the best oxygen titration group (group O) and best compliance titration group (group C).
ANESTHESIA METHOD:
After the patient entered the operating room, a patient monitor (model 866066, Philips, Germany) was used to monitor the electrocardiogram, heart rate (HR), mean arterial pressure (MAP), SpO2, bilateral bispectral index, and muscle relaxation. The venous channel was opened, and a catheter was placed through the radial artery under local anesthesia to monitor the invasive arterial blood pressure. The patient inhaled pure oxygen through the mask, and anesthesia induction was started. Midazolam 0.05 mg/kg, sufentanil 0.4 to 0.6 μg/kg, propofol 1 to 2 mg/kg, and cisatracurium 0.2 mg/kg were used to induce general anesthesia. When the train-of-four count was 0 and the post-tetanic count was ≥1, the trachea was intubated with a double lumen tube (Willy Rusch Gmbh, Germany). The location of the double lumen tube was confirmed by fiberoptic bronchoscopy before and after the patient’s lateral positioning. During OLV, the non-ventilated side was opened, and the Drager anesthesia machine (Perseus A500) was connected for intermittent positive pressure ventilation. Respiratory parameters during bilateral lung ventilation were as follows: inhaled oxygen concentration of 100%, tidal volume of 8 mL/kg, predicted body weight, ventilation frequency of 12 times/min, and inspiratory respiratory ratio of 1: 1.5. The end-expiratory carbon dioxide partial pressure (ETCO2) was adjusted between 35 and 40 mmHg (1 mmHg=0.133 kPa). To maintain the anesthesia, 1% to 2% sevoflurane was inhaled and an intravenous pump of dexmedetomidine 0.01 μg*kg−1*min−1, remifentanil 0.1 to 0.3 μg*kg−1*min−1, and cisatracurium 5 mg/h was administered. The bispectral index value was maintained between 40 and 60. The fluctuation of the intraoperative MAP should not exceed 20% of the baseline value, and the train-of-four count should be ≤2. A double-lumen central venous catheter was inserted into the right internal jugular vein to monitor the central venous pressure (CVP) and infusion. During the operation, target-guided fluid therapy, mainly crystalloid fluid, was used. When the reduction in MAP exceeded 20% before induction, ephedrine 6 mg or methoxyamine 2 mg was injected intravenously, as appropriate. Based on the patient’s response to the drug and volume status, continuous infusion of vasoactive drugs or the use of glue body fluid volume expansion was determined. HR, MAP, arterial oxygen saturation, and ETCO2 were continuously monitored (Datexengstrom, Finland).
During OLV, the best oxygenation method titration group (group O) had a tidal volume of 6 mL/kg, respiratory rate of 14 to 16 breaths/min, PEEP increase from 3 cmH2O, and increase of 1 cmH2O every 4 min until the arterial partial pressure of oxygen (PaO2) was the highest. The best method of lung compliance (group C) was a tidal volume of 6 mL/kg, respiratory rate of 14 to 16 breaths/min, PEEP of 3 cmH2O, and 1 cmH2O every 4 min until the best lung compliance was achieved.
DATA COLLECTION AND MEASUREMENT:
MAP, HR, and CVP were recorded in both groups at the time of bilateral ventilation (T1), 4 min after the completion of OLV titration (T2), and 10 min after the resumption of bilateral ventilation after intubation (T3). Radial artery blood samples were collected at 3 the time points, and a cobqsb221 blood gas analyzer (Roche, Switzerland) was used for blood gas analysis, recording PaO2 and PaCO2, calculating the void volume/tidal volume ratio (VD/VT), recording the peak airway pressure (PIP) and PEEP values at T2, and calculating the driving pressure. The formula was as follows:
Operation time, OLV time, intraoperative volume, and use of vasoactive drugs were recorded.
STATISTICAL ANALYSIS:
SPSS version 17.0 was used for the analysis. The measurement data of normal distribution are expressed as mean±standard deviation. The group
Results
There was no significant difference between the 2 groups in the relevant indicators of the general preoperative and intraoperative conditions (
In the comparison of circulation indices, CVP in group O was significantly higher than that in group C at T2 (9.36±1.66 cmH2O vs 5.64±1.19 cmH2O,
The results of respiratory mechanics showed that at T2, the driving pressure value of group O (12.88±2.47 cmH2O) was higher than that of group C (10.80±1.73 cmH2O) (
Regarding the gas exchange indices, at T2, PaO2 in group O was significantly higher than that in group C (202.28±59.66 mmHg vs 112.23±8.74 mmHg). Compared with T1,the PaO2 at T2 and T3 decreased significantly in both groups. The value of VD/VT in group C was significantly higher than that in group O at T2 and T3 (0.09±0.03 vs 0.07±0.02 and 0.13±0.04 vs 0.11±0.04, respectively). The VD/VT of the 2 groups were significantly higher at T3 than at T1 (Table 4).
Discussion
We studied the PEEP levels of the 2 titration methods in elderly patients undergoing thoracotomy and compared the effects of the methods on respiration and circulation. The PEEP value of optimal oxygenation titration (11.24±1.71 cmH2O) was significantly higher than that of optimal lung compliance titration (7.68±1.28 cmH2O;
Some studies [7] used dynamic lung compliance titration to measure the PEEP value, starting from 20 cmH2O and gradually reducing the titration. However, considering that 20 cmH2O in elderly patients with OLV can cause hemodynamic changes, an excessively high PEEP can lead to decreased blood pressure [8]. Therefore, in the present study, we adopted the method of gradually increasing the PEEP value after pulmonary dilatation, starting from 3 cmH2O. However, due to the limitations of the experimental conditions and the lack of postoperative follow-up, no differences in postoperative pulmonary complications related to patients’ surgical conditions were observed.
Peak airway pressure and driving pressure are respiratory mechanics indices related to ventilation in elderly patients during anesthesia in surgery [9]. Peak airway pressure is the maximum airway pressure reached by ventilation during inhalation, and the value can indicate the degree of alveolar dilatation [10]. Driving pressure is the result of tidal volume corrected by dynamic lung compliance, which may indicate alveolar injury caused by the change in respiratory phase during ventilation. An increase in the driving pressure can increase the risk of postoperative respiratory complications [11]. The results of this study showed that compared with group O, the driving pressure decreased, PIP decreased, and dynamic lung compliance increased in group C 10 min after the completion of OLV titration, indicating that PEEP titration guided by dynamic lung compliance can have a positive effect on the respiratory mechanics of elderly patients during anesthesia in surgery.
Owing to anatomical and mechanical lung changes that occur with age, maintaining normal PaCO2 levels depends on the increase in the total minutes of ventilation, that is, the sum of alveolar ventilation and dead space ventilation (VD) [12]. The VD/VT index can show alveolar closure and ventilation and it can reflect the ratio of non-oxygenated gas in the lung to total ventilation [13]. During OLV, we should avoid the increase of VD/VT, try to increase arterial oxygen partial pressure, improve oxygenation, and reduce cardiovascular complications. An increase in VD/VT often indicates poor prognosis [14]. However, the abnormal increase of VD/VT indicates the imbalance of pulmonary ventilation and blood flow, which becomes the main mechanism of respiratory failure [15]. Therefore, VD/VT is helpful to judge the prognosis of acute respiratory distress. In addition, the level of VD/VT is closely related to the formation of pulmonary and microvascular thrombosis. Spece et al [16] also believe that the increase of VD/VT level is an independent high risk factor of pulmonary embolism, increasing the risk of death.
The results of the present study showed that there was no difference between the 2 groups in terms of the change in VD/VT. However, VD/VT increased significantly after OLV.
Conclusions
In summary, the PEEP value titrated by the best compliance method was lower than that titrated by the best oxygenation method. The peak was lower and the dynamic lung compliance was higher but had no effect on MAP and HR, and the CVP was also lower than that titrated by the best oxygenation method. Therefore, dynamic lung compliance-guided PEEP titration can improve lung function in elderly patients undergoing lobectomies.
Tables
Table 1. Comparison of general conditions and intraoperative conditions of patients (n=25).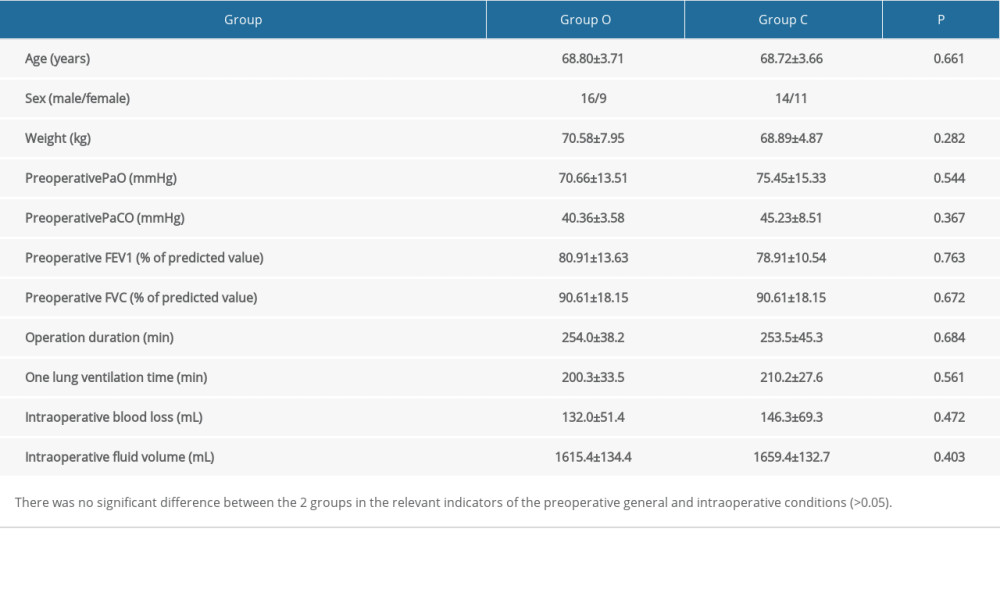 Table 2. Comparison of 2 groups of circulation indexes (n=25).
Table 2. Comparison of 2 groups of circulation indexes (n=25).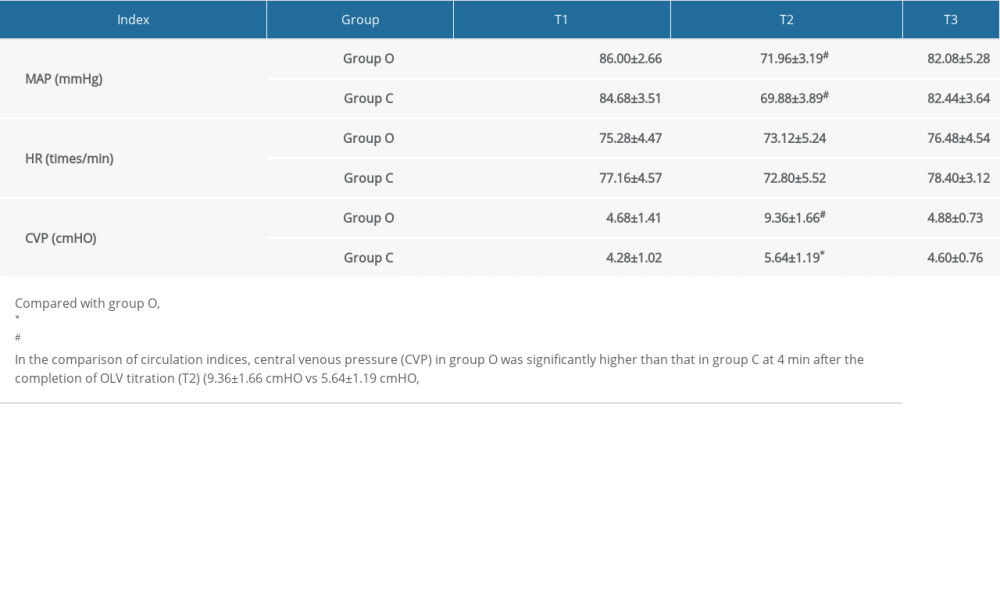 Table 3. Comparison of respiratory mechanics indexes at 4 min after the completion of the one-lung ventilation titration (T2) time point.
Table 3. Comparison of respiratory mechanics indexes at 4 min after the completion of the one-lung ventilation titration (T2) time point.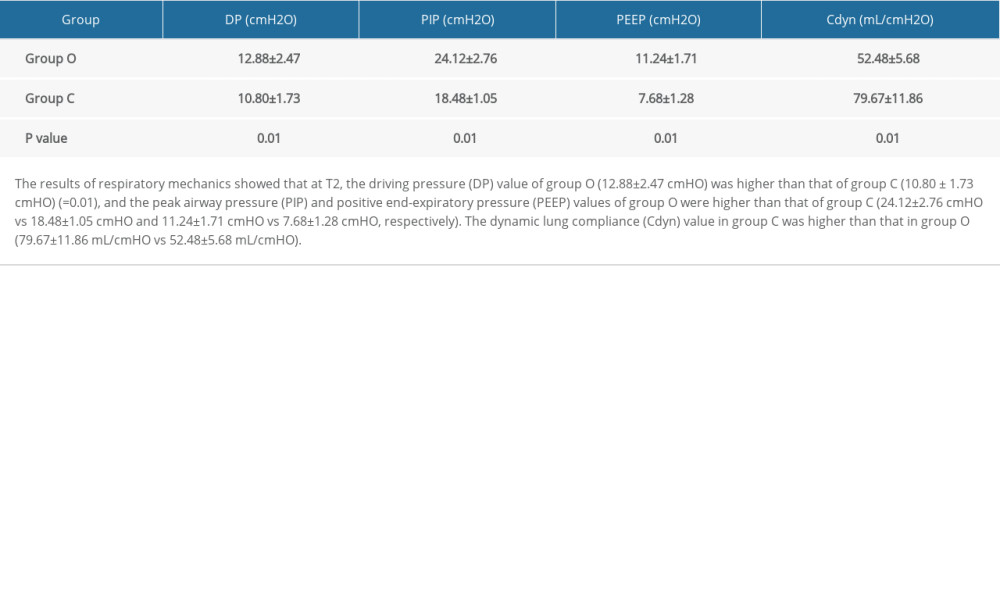 Table 4. Comparison of gas exchange indexes.
Table 4. Comparison of gas exchange indexes.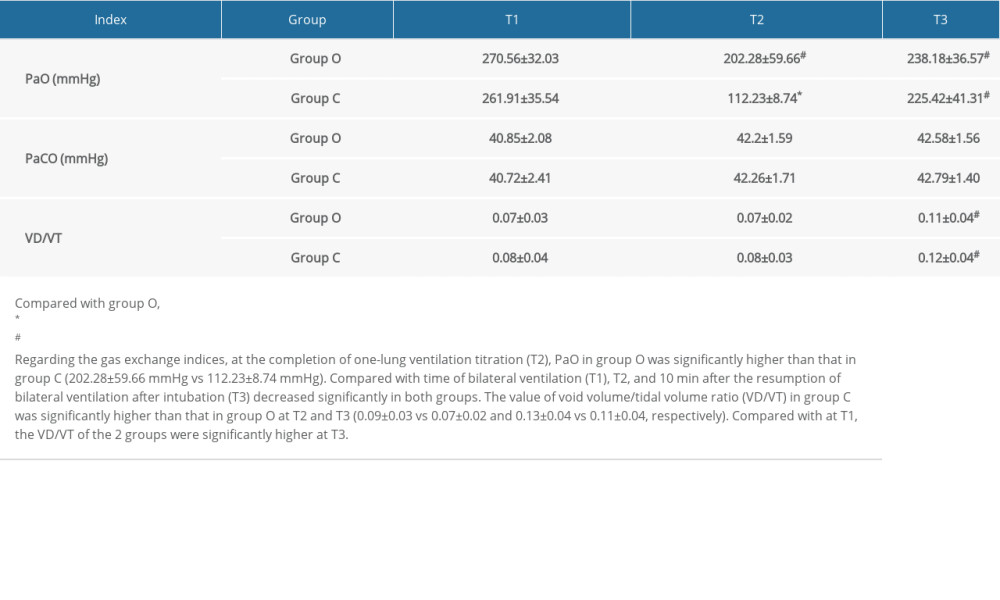
References
1. Zick G, Elke G, Becher T, Effect of PEEP and tidal volume on ventilation distribution and end – expiratory lung volume: A prospective experimental animal and pilot clinical study: PLoS One, 2013; 8(8); 72-75
2. Bluth T, Serpa Neto A, Schultz MJ, Effect of intraoperative high positive end-expiratory pressure (PEEP) with recruitment maneuvers vs low PEEP on postoperative pulmonary complications in obese patients: JAMA, 2019; 321(23); 2292-305
3. Liu K, Huang C, Xu M, PEEP guided by electrical impedance tomography during one-lung ventilation in elderly patients undergoing thoracoscopic surgery: Ann Transl Med, 2019; 7(23); 757
4. Zhaoxia W, Xianjie W, Progress in clinical application of positive end-expiratory pressure: J Pharm Res Int, 2021; 526-37
5. Shen P, Luo R, Gao Y, Assessment of positive end-expiratory pressure induced lung volume change by ultrasound in mechanically ventilated patients: Zhonghua Jie He He Hu Xi Za Zhi, 2014; 37(5); 332-36
6. Chen Zhigang C, Baojin LL, Xin L, Use of dynamic compliance identify the positive end-expiratory pressure level in the video-assisted pulmonary lobectomy: Int J Anesth Resus, 2016; 37(3); 197-201
7. Huang L-P, Fu H, Wand Q-S, The hemodynamic influence of positive end expiratory pressures titrated by different methods on patients with acute respiratory distress syndrome: Guangdong Medical Journal, 2017; 38(14); 2141-46
8. Santa Cruz R, Villarejo F, Irrazabal C, High versus low positive end-expiratory pressure (PEEP) levels for mechanically ventilated adult patients with acute lung injury and acute respiratory distress syndrome: Cochrane Database Syst Rev, 2021; 2021(3); CD009098
9. Ji J, Chun Y, The effect of individualized PEEP guided by driving pressure on pulmonary function in elderly patients undergoing surgery and postoperative pulmonary complications: Chin J Hemorh, 2021; 31(3); 363-64
10. Beyoglu CA, Teksoz S, Ozdilek A, A comparison of the efficacy of three different peak airway pressures on intraoperative bleeding point detection in patients undergoing thyroidectomy: a randomized, controlled, clinical trial: BMC Surg, 2020; 20(1); 69
11. Sahetya SK, Hager DN, Stephens RS, PEEP titration to minimize driving pressure in subjects with ARDS: A prospective physiological study: Resp Care, 2020; 65(5); 583-89
12. Hasan H, Maranatha RLung function alteration in geriatric patients: Jurnal Respirasi (Journla of Respirology), 2019; 3(2); 52
13. Kallet RH, Zhuo H, Ho K, Lung injury etiology and other factors influencing the relationship between dead-space fraction and mortality in ARDS: Resp Care, 2017; 62(10); 1241-48
14. Wang Y, Wang H, Wang H, Exploring the intraoperative lung protective ventilation of different positive end-expiratory pressure levels during abdominal laparoscopic surgery with Trendelenburg position: Ann Transl Med, 2019; 7(8); 171
15. Zhang Y, Huang X, Gao X, Investigation and analysis of quality index of emergency examination in Chinese PLA General Hospital Sixth Medical Center in 2017: Journal of Modern Laboratory Medicine, 2019; 34(3); 158-60
16. Spece LJ, Mitchell KH, Caldwell ES, Rate of low tidal volume ventilation use remains low in patients with acute respiratory distress syndrome despite improvement efforts at a single center: J Crit Care, 2018; 44; 72-76
Tables
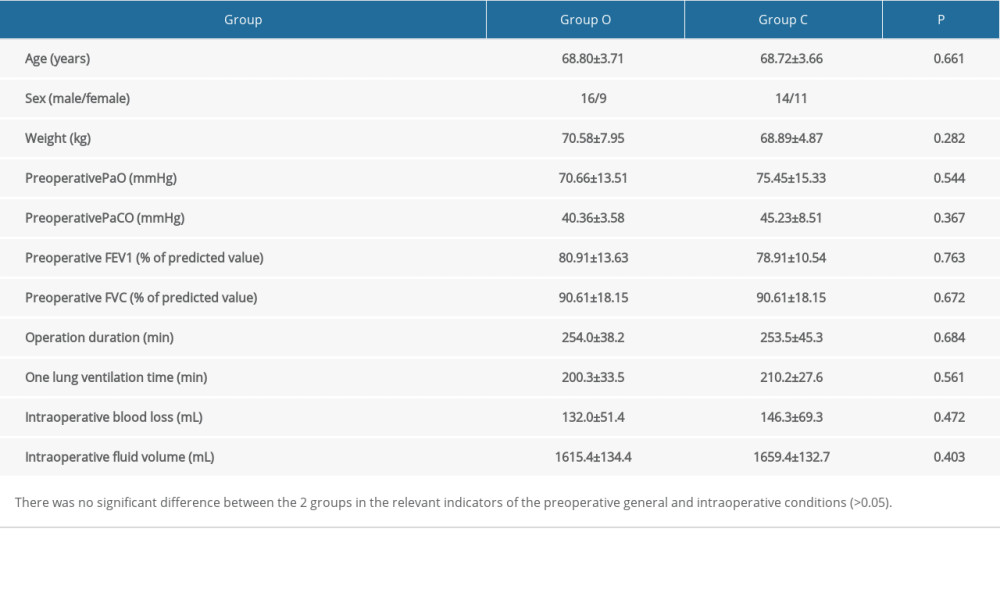 Table 1. Comparison of general conditions and intraoperative conditions of patients (n=25).
Table 1. Comparison of general conditions and intraoperative conditions of patients (n=25).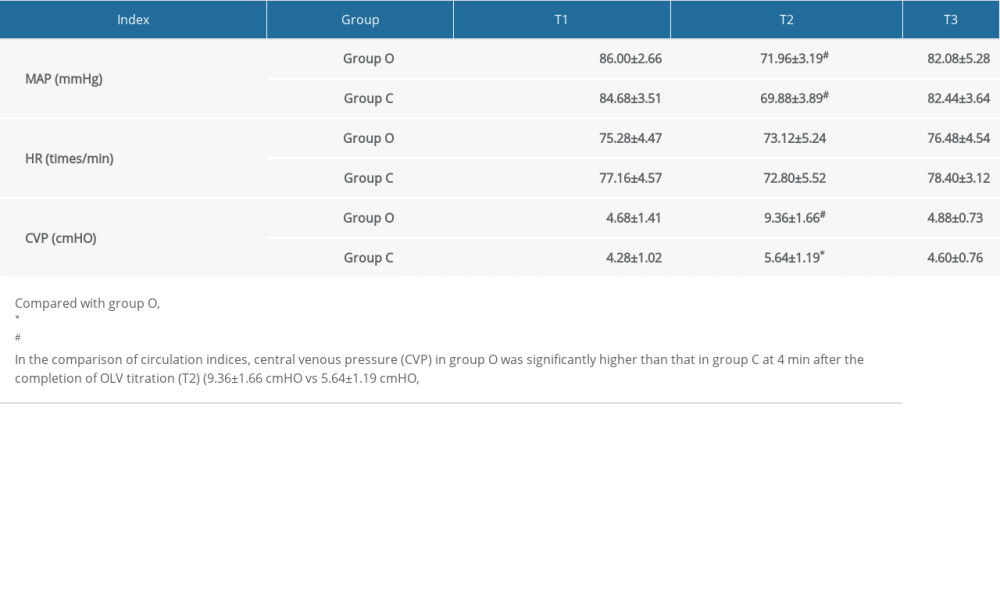 Table 2. Comparison of 2 groups of circulation indexes (n=25).
Table 2. Comparison of 2 groups of circulation indexes (n=25).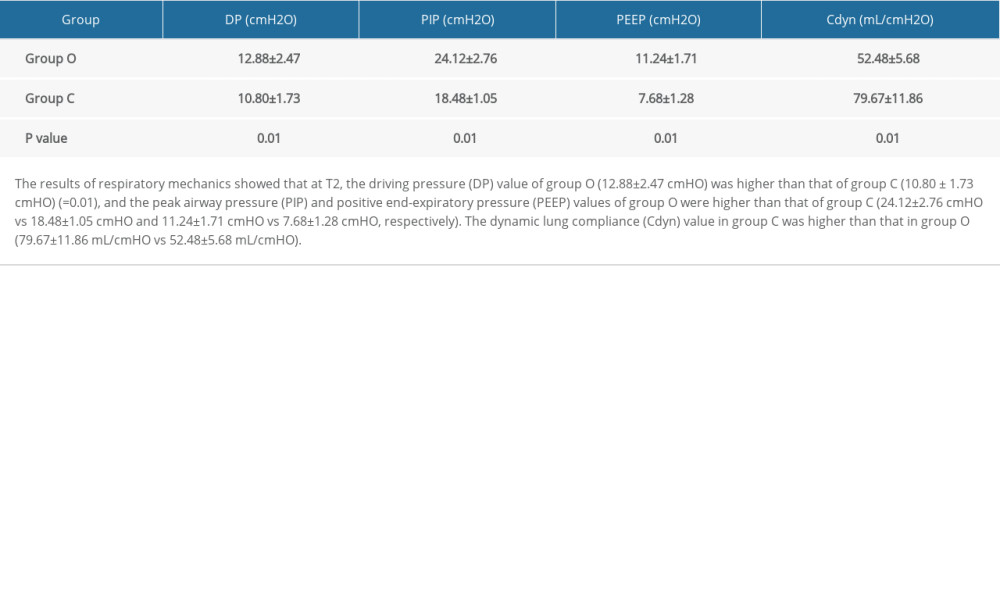 Table 3. Comparison of respiratory mechanics indexes at 4 min after the completion of the one-lung ventilation titration (T2) time point.
Table 3. Comparison of respiratory mechanics indexes at 4 min after the completion of the one-lung ventilation titration (T2) time point.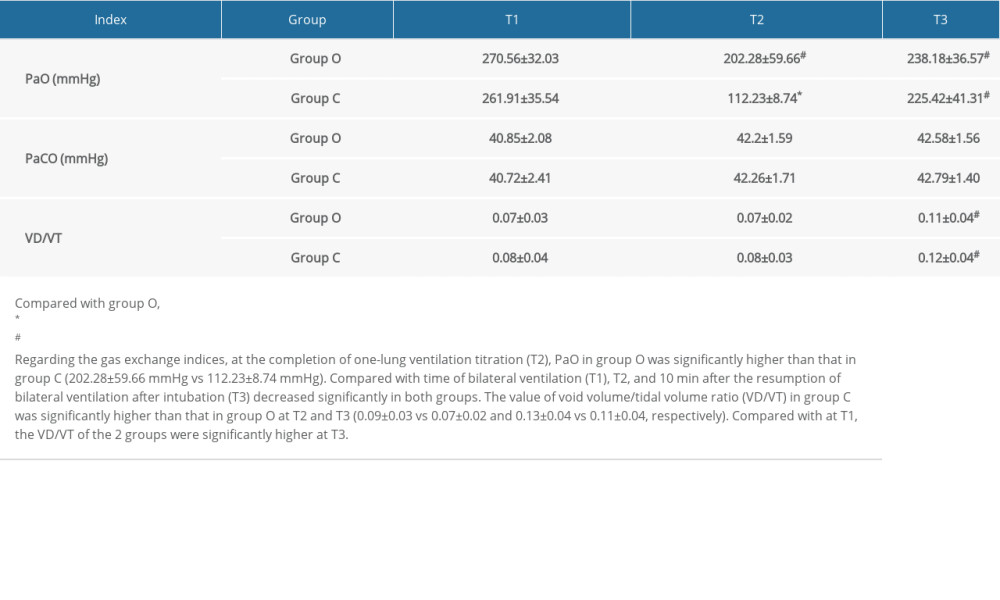 Table 4. Comparison of gas exchange indexes.
Table 4. Comparison of gas exchange indexes. In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








