05 May 2023: Meta-Analysis
Benefits of Using Smartphones and Other Digital Methods in Achieving Better Cardiac Rehabilitation Goals: A Systematic Review and Meta-Analysis
Miruna Popovici1ABCEF, Sorin UrsoniuDOI: 10.12659/MSM.939132
Med Sci Monit 2023; 29:e939132
Abstract
BACKGROUND: The importance of introducing digital technology as an alternative to classical cardiac rehabilitation has been discussed in several reviews. The purpose of this systematic review and meta-analysis was to analyze the effectiveness of digital technology use in cardiac rehabilitation to determine whether digital methods like use of smartphones, compared to traditional rehabilitation methods, can improve the overall quality of life and exercise capacity of cardiac patients.
MATERIAL AND METHODS: PubMed, EMBASE, and ScienceDirect were systematically searched in a randomized manner, resulting in 11 randomized controlled trials (RCTs) that met all the inclusion criteria. The inclusion criteria were patients with coronary heart disease, valvular surgery, or post- myocardial revascularization that were in a technology-assisted cardiac rehabilitation program vs traditional standard physical follow-up protocol.
RESULTS: Seven eligible trials including a total of 802 participants examined the effect of interventions on VO2 peak. One of the studies comprised 2-stage analysis for this parameter. We found that VO₂ peak was significantly higher in the intervention group. Three studies analyzed the 6-minute walk test (6MWT) results; significant differences were reported, with better results in the interventional group.
CONCLUSIONS: The results of our meta-analysis support conducting further randomized trials, considering that the development of technology is on the rise. In the past decade there has been an immense increase in the use of smartphones, which can widely be used in healthcare, with promising benefits in having efficient home-based monitoring of the patients and in reducing financial burden.
Keywords: cardiac rehabilitation, Coronary Artery Disease, telerehabilitation, Humans, Smartphone, Quality of Life, Coronary Disease, Myocardial Revascularization
Background
Cardiovascular diseases (CVD) are the most common non-communicable diseases globally [1], even if their incidence and mortality tend to decrease, thanks to new and successful diagnostic methods and treatments [2,3]. They still are a problem for health systems because they are a major cause of disability worldwide [4]. Coronary artery bypass grafting, PTCA, valvular replacement, and other cardiac revascularization procedures are efficient alternatives for the treatment of CVD, causing at the same time important physiological and organic changes. Even though attempts are being made to limit postoperative cardiac complications by introducing minimally invasive techniques, median sternotomy remains the most widely used method of cardiac approach. Postoperatively, the risk of complications increases, especially because this is patient-dependent phase, leading to a significant decrease in patient compliance with recovery programs [5].
Despite various protocols and awareness sessions provided, there is a large void noted worldwide in data on postsurgical patient compliance. Sudden and prolonged interruption from rehabilitation programs can result in serious postsurgical complications, endangering the life of patients. Reduced compliance is either due to financial costs the patient has to bear, or issues related to traveling long distances to reach rehabilitation centers, or simply due to lack of psychological and family support. Use of smartphones and other digital methods can help overcome these hurdles to a large extent. Tailored smartphone applications can help immensely, not only in motivating and reminding patients to adhere to the protocols, but also help in keeping an efficient check on the patients’ health status, avoiding the discomfort of traveling to rehabilitation centers for follow-ups [6].
Cardiac rehabilitation (CR) following a cardiac event or procedure “has been recognized as the most cost-effective intervention to ensure favorable outcomes across a wide spectrum of cardiovascular disease” according to the latest position paper of the European Association of Preventive Cardiology [7]. CR is a Class I recommendation with the level of evidence A of the European Society of Cardiology, which is also highly recommended by the American Heart Association [8]. A typical CR program is prescribed mainly to improve survival and quality of life and to reduce further hospitalizations [9,10]. Other benefits of CR are reducing cardiovascular risk factors and minimizing the psychological impact of the disease. CR helps to regain lost functional capacity and increase exercise capacity. Cardiac recovery protocols in most countries involve performing procedures in hospital units (hospital-based cardiac rehabilitation, HBCR) or special recovery units (center-based cardiac rehabilitation, CBCR). CR takes place through a multidisciplinary, medically supervised program, typically involving healthcare teams that include cardiologists, physiotherapists, dieticians, psychologists, and nurses [11].
Traditionally, cardiac rehabilitation programs have been divided into 3 phases, except for a few countries which have adopted four-phase programs including both in-hospital recovery and home-based rehabilitation [12]. The first phase, known as the in-hospital phase, consists of early mobilization and education, being initialized from the first days after heart surgery, right from the intensive care unit, depending on the clinical condition of the patient [13]. In this phase, the patient performs passive movements to avoid postoperative physical deconditioning due to prolonged rest [12], with a progressive increase in mobilization (emphasizing lower limb movements as early as the patient’s general condition allows), accompanied by respiratory recovery exercises and education about the specific cardiac pathology, risk factors, recommended lifestyle, nutrition, physical exercises, pharmacological therapy, and community resources available for assistance in cardiac rehabilitation. Phase II, known as the early out-patient phase, nowadays is recommended to be started immediately as the patient is discharged if no complications were witnessed during the postoperative period at the hospital. This phase lasts for approximately 3 to 6 months after surgery, during which the sternotomy heals [13]. A tailored approach is used depending on the physical condition of the patient, which helps pre-set the frequency, duration, and intensity goals for exercises [5]. The aim of this phase is to improve cardiac performance and to develop physical activities that stimulate the metabolic expense of everyday activities [13]. The patient should be trained to perform upper and lower limb movements, as well as breathing exercises, in such a manner that no pressure is exerted on the recently operated-on sternum, and at the same time increasing physical activity [5,14]. The delay in the start of these basic exercises can delayed the patient’s overall recovery and lead to more muscle wasting, delay becoming independent again in performing routine daily activities and return to work, and all this can create anxiety and depression for patients who are confined to bed. The third phase of the cardiac rehabilitation program has a variable duration, and it is known as the late out-patient phase [13]. The objective of this phase is to consolidate the results obtained in the previous phases. Phase IV is an adaptation to the patient’s way of life by including recovery exercises in the daily routine. It is well known that cardiac rehabilitation is an underused resource [15], and even more important, the impact of the recommendations to maintain social distance, due to the widespread of the novel coronavirus, has played a major role in reducing the efficacy of cardiac rehabilitation centers. Therefore, home-based cardiovascular recovery is safe for the patient, both by limiting contact with medical staff and other patients, and by providing a comfortable environment with which the patient is already accustomed. In support of this idea are the results of the most recent review published by Stefanakis et al, which showed that HBCR can be as safe as CBCR in terms of the prevalence of adverse effects. Of the 9 studies included in the systematic review by Stefanakis et al, only 1 reported the presence of severe adverse effects. Furthermore, as a result of the restrictions imposed by authorities, many rehabilitation programs have been discontinued or relocated online [16]. Apart from helping to adapt to the pandemic era, home-based online monitoring of patients can increase the success of surgeries requiring periodic follow-ups, as well as dose adjustments based on the patient’s current state of health. The problems faced by many countries, including scarcity of well-trained medical staff and long distances patients must travel to reach specialized medical centers, can be minimized by simple use of digital home-based monitoring devices. They are cost-effective both for the patients and state healthcare budget, save time and energy, and also help in achieving better patient adherence to the set recovery plans in a comfortable environment [17]. The cardiac population for which the home-based exercise interventions were considered applicable comprised coronary and/or valvular patients with revascularization procedures and/or valvular replacement, with different stages of heart failure. An entire recently published work, REACH-HF RCT [18], was dedicated to patients with heart failure; therefore, this paper will not focus mainly on these patients. Since the pre-pandemic period, the importance of introducing digital technology as an alternative to traditional, home-based cardiac rehabilitation was discussed in several reviews. The purpose of our work was to focus on home-based digital recovery rather than continuous visits to cardiac rehabilitation centers, precisely because of the many advantages of the technology in this field, such as the possibility to monitor patients more closely, even remotely, encouraging them when the results are below expectations, and the possibility of being observed by specialized staff regarding the effectiveness of certain physical exercise programs and their improvement, with the ultimate goal of increasing patient compliance with cardiovascular recovery programs. All these benefits to patient health also help improve healthcare systems, which lack personnel specialized in cardiovascular recovery. Eventually, it will be easier to manage the evolution of each patient with the help of new technologies capable of permanently monitoring physical activity and vital functions.
The benefits of mobile health (mHealth) intervention for secondary prevention of CVD were analyzed in a review conducted by Gandhi et al [19], but the analysis did not include the psychological implications of rehabilitation. A review by García-Bravo et al [20] found that virtual reality and video games can be used to improve the adherence of patients in cardiac rehabilitation programs, but the main limitation of this analysis was the small number of papers published on this topic. In their latest published meta-analysis, Antoniou et al [21] highlighted the importance of wearable sensors in transmitting real-time data related to vital signs and electrocardiogram of patients in a cardiac recovery program at home, thus strengthening the idea of a good functioning of digital cardiovascular rehabilitation in addition to traditional methods.
The purpose of the present systematic review and meta-analysis was to analyze the effectiveness of digital technology in cardiac recovery and myocardial revascularization procedures, compared to traditional rehabilitation, in terms of quality of life and exercise capacity.
Material and Methods
STUDY DESIGN:
This paper represents a systematic review and meta-analysis of randomized control trials (RCTs) and is written in accordance with the guidelines from the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) to improve transparency, accuracy, and completeness.
SEARCH STRATEGY:
A systematic electronic database search was performed in PubMed, EMBASE, and ScienceDirect up to December 2021, with a supplementary manual search of references. The search included the following keywords: “cardiac rehabilitation” OR “heart rehabilitation” OR “exercise-based cardiac rehabilitation” OR “coronary heart disease” OR “telerehabilitation”. The literature search was limited to papers published between 2000 and 2021, in English, including only human subjects. Duplicate articles or those containing only the abstract were excluded from the search process, and all the results were managed using the EndNote platform. Two investigators (M.P. and O.T.) were assigned to independently evaluate the titles and abstracts of the research results, verify the fulfillment of inclusion criteria, and perform a quality evaluation. A database that included all the downloaded full texts of the relevant studies was created. Disagreements between the 2 investigators were resolved through consensual discussions with a third reviewer (M.V.).
STUDY SELECTION:
The included studies followed a certain design (randomized controlled trials with a parallel design), representing a comparison between traditional and digital-assisted cardiac rehabilitation. The selected studies presented the following inclusion criteria: 1) patients: men or women, older than 18 years old, diagnosed with coronary heart disease (CHD), acute coronary syndrome (ACS), who have undergone cardiac revascularization procedures (ie, percutaneous coronary intervention (PCI) and coronary artery bypass graft (CABG) surgery) or valvular replacement surgery); 2) interventions: mobile health application (mHealth), website-based application, phone calls, text messages, emails, telemonitoring used individually or in combination as a Phase 2 cardiac rehabilitation alternative; 3) control: traditional cardiac rehabilitation program comprising physical exercises supervised by a specialist, an established local protocol for cardiac rehabilitation with periodic follow-up by an assigned clinician or just a standard care protocol without specific cardiac exercises; and 4) outcomes. Outcome parameters analyzed in the studies were: exercise capacity (6-minute walk test, steps per day, sedentary time, active energy expenditure, duration of physical activity), cardiopulmonary parameters (peak oxygen uptake, ventilatory threshold, peak heart rate, peak respiratory exchange ratio, Borg scale), clinical (systolic blood pressure, diastolic blood pressure, body mass index, waist-to-hip ratio, lipid profile, blood pressure), health quality of life (Short-Form-36 Questionnaire physical and mental health score, Generalized Anxiety Disorder 7-item scale, nine-item Patient Health Questionnaire scale). We excluded from our selection non-randomized studies, those without conclusive results, and those with a lack of reported baseline or follow-up results. We did not impose limits on the number of participants, duration of follow-up, or technologies used for rehabilitation.
DATA EXTRACTION:
Two reviewers (M.P. and O.T.) independently used standardized forms to extract the following data from the studies that met the inclusion criteria: authors, year of publication, study location, sample size, trial design, follow-up duration, methods used in the control rehabilitation programs, methods used in intervention groups, baseline characteristics, and primary and secondary outcomes.
RISK OF BIAS (QUALITY) ASSESSMENT:
The Cochrane instructions were used to assess the risk of bias in the studies considered in this meta-analysis [22]. Each of the studies was assessed for selection bias, performance bias, attrition bias, detection bias, reporting bias, and other sources of bias that were judged to be high, low, or unclear (Table 1). If the answer to all the questions about the risk of bias is “yes”, it is considered “low” risk. If at least 1 answer is “no”, it is considered “high” risk. If the reported data were insufficient or too poorly explained to allow the formulation of an answer to questions, the risk of bias was classified as “unclear”. The qualitative classification of the studies included in the meta-analysis and the possible sources of heterogeneity were evaluated using the results of the quality assessment.
STATISTICAL ANALYSIS:
Meta-analysis was conducted using Stata version 17.0 software, (StataCorp, Texas, USA) using the meta and metaninf commands. Effect sizes were expressed as mean difference (MD) and its 95% confidence interval (CI). The effect size was calculated as (measure at the end of follow-up in the intervention group − measure at baseline in the intervention group) − (measure at the end of follow-up in the control group − measure at baseline in the control group). Standard deviations (SDs) of the mean difference were calculated using the following formula: SD=square root [(SD preintervention)2+ (SD postintervention)2–(2R×SD preintervention×SD postintervention)], assuming a correlation coefficient (R)=0.5. The proportion of inconsistency across the included studies, which is not attributable to chance (heterogeneity), was quantified using the Cochran Q test and I2 indices [23]. Because I2 values were <50%, fixed models were used. We performed sensitivity analyses in which each study was excluded separately and the overall effect size was re-estimated [24].
The presence of publication bias was explored graphically using funnel plots. Asymmetric funnel plots were further assessed for publication bias using Duval and Tweedie’s ‘trim-and-fill’ method to discover the number of omitted publications, as well as Egger’s regression-based test [25].
Results
SEARCH RESULTS AND TRIAL FLOW:
The search for articles used in this meta-analysis went through several stages. In the first stage, studies that presented topics outside the chosen subject were excluded. We evaluated 124 studies for eligibility, but most were excluded at a later stage of screening because: only the abstract was available (not open-access articles); only the study protocol was available (on-going study); they had an inappropriate design; they referred to irrelevant interventions; they had irrelevant outcomes; or they included inappropriate participants (patients who did not meet the inclusion criteria) (Figure 1).
At the end of the assessment process, 11 RCTs [26–36] with a total of 2152 patients were included in this meta-analysis – 1072 in the intervention group and 1080 in the control group. Two 2 of the 11 studies included in our meta-analysis were conducted with 2 periods of assessment. All the included studies were RCTs with a two-arm design, with 1 exception with a three-arm design [26].
The number of participants included in these studies ranged from 54 to 312, the selected studies were published between 2012 and 2020, and were conducted in China (
Because no limits were imposed on the duration of the rehabilitation programs, they varied between 6 and 48 weeks. Four follow-up trials [28,30,34,36] presented several systematic evaluation steps at 6, 8, or 24 weeks, with the outcomes obtained in all these evaluation stages being described at the end of the studies. Table 1 describes the demographic characteristics and baseline parameters of the included studies.
RISK OF BIAS ASSESSMENT:
An unclear risk of bias with respect to sequence generation and allocation concealment was observed in some trials. Although some studies did not use blindness, they were at low risk in terms of other sources of bias. The systematic assessment of bias in the included studies is shown in Table 2.
QUANTITATIVE DATA SYNTHESIS:
A first meta-analysis included 7 eligible trials with a total of 802 participants (case=395, control=407) and examined the effect of interventions on VO2 peak. The study of Snoek et al [34] had 2 follow-up periods: (a) 24 weeks and (b) 48 weeks. We found that VO2 peak was significantly higher in the intervention group compared to the control (MD: 1.41 mL/kg/min, 95% CI: 0.62 to 2.21, p<0.001), with no heterogeneity among the studies. In the stratified analysis, a significant increase was observed only for studies with a duration of 24 weeks (MD: 1.83 mL/kg/min, 95% CI: 0.72 to 2.94, p=0.001) compared with 12-week studies (MD: 0.48 mL/kg/min, 95% CI: −1.22 to 2.18, p=0.579) and 48-week studies (MD: 1.38 mL/kg/min, 95% CI: −0.16 to 2.91, p=0.078) (Figure 2).
The next meta-analysis included 4 studies that analyzed the 6-minute walk test (6MWT). The study of Dorje et al [28] had 2 follow-up periods: (a) 8 weeks and (b) 24 weeks. The studies included 679 participants (case=351, control=328) who were evaluated for periods between 6 weeks and 24 weeks (Figure 3). Significant differences were reported between studies (MD=14.93 m, 95% Cl.: 4.46 to 25.40, p<0.001), with better results in the intervention group.
To investigate potential bias, we statistically compared the studies that included the supervised and not supervised control group for both VO2 (Figure 4) and 6MWT (Figure 5) parameters. The supervised studies showed no statistically significant differences between intervention and control groups. Three eligible studies from this meta-analysis analyzed the effects of the intervention on VO2 peak compared with the supervised control group, and a single study by Varnfield et al analyzed the effects of the intervention on 6MWT compared to the supervised control group.
:
We analyzed the influence of each study on the overall results. No single study had a large impact on the overall results. The meta-analysis was re-estimated, removing 1 study at a time. The average effect size ranged from a maximum of 1.542 mL/kg/min (95% CI: 0.702, 2.381) when the study by Batalik et al (2019) [27] was excluded to a minimum of 1.234 mL/kg/min (95% CI: 0.380, 2.087) when the study by Frederix et al (2015) [30] was excluded in the fixed-effects model (Figure 6).
Visual inspection of funnel plot asymmetry suggested potential publication bias for the VO2 peak effects (Figure 7).
The mean difference based on the 8 observed studies was 1.414 with a 95% CI of [0.620; 2.208]. One hypothetical study was estimated to be missing and was imputed. If this study would have been included in the meta-analysis, the funnel plot would have been more symmetrical. After inputting the study, we obtain an updated estimate (based on the 9 studies, observed plus imputed) of the mean difference of 1.487 with a 95% CI [0.714; 2.260]. The effect was larger but not statistically significant from the initial estimate.
Regression-based Egger test for small-study effects suggested no evidence of publication bias (
Discussion
CARDIORESPIRATORY FITNESS:
The effects of the cardiac rehabilitation program on the physical activity of patients were analyzed in 9 of the 11 studies included in our analysis, but only 3 of them, including a study with several evaluation periods [28], used the 6-minute walk test. The statistical analysis of the results presented in the 3 studies revealed a mean difference of 14.93 m, which was unexpectedly low, a value well below the 25 m limit, and shown to have significant clinical significance [37]. Two of the studies that analyzed this parameter showed statistically significantly reduced values of 13.43 [29] and 13.00 [36]. We believe that this may be due to the small number of participants included in these studies and to the short follow-up period, both studies being carried out over a period of only 6 weeks. The digital interventions used in these studies included the use of a smartphone strictly to monitor the physical activity of the participants and to provide sustained explanations for performing the exercise training.
Instructions for correctly performing the exercises were given in the form of cartoons in the study of Dorje et al [28], leading to much better results than in the other comparative studies. This is in line with the recommendations of the European Society of Cardiology, which considers that the success of the recovery process also consists in individualizing the rehabilitation programs [7].
The effects of exercise training during the rehabilitation programs were analyzed in 6 other papers included in this meta-analysis in other forms of quantification (eg, steps count/day). These parameters were not included in the meta-analysis because they were considered quite variable depending on many other circumstances in which the study participants were involved.
Because our meta-analysis was based on the evaluation of cardiac function, we chose the maximum volume of oxygen consumed during aerobic exercise (VO2 peak) as the parameter, which is considered to be the criterion standard.
The 8 studies had different evaluation periods – 12, 24, and 48 weeks – thus allowing an analysis of the dynamics of this parameter in relation to the duration of recovery procedures. The additional digital interventions differed in the analyzed studies, even in those with similar duration, making it difficult for us to identify the advantages of one given technique over another. Substantial improvement was seen after 24 weeks, and the least improvement was observed at 12 weeks, most likely due to the short duration of the rehabilitation programs. The study of Snoek et al [34] allowed the observation of peak VO2 evolution after 6 months and 12 months, showing a considerable improvement in favor of the intervention group, thus supporting the idea of allocating a longer time for the rehabilitation program, even in the case of digitized recovery.
The main clinical parameters analyzed in the included studies were max HR, SBP, and DBP. However, they were only included in 2 studies, which rendered their inclusion in a meta-analysis unsatisfactory.
However, the amount of physical exercise is best measured by the amount of daily exercise, but exercise capacity is measured by exercise testing (like 6MWT or exercise ECG). The 6MWT is still very appropriate, but measures exercise capacity rather than amount of exercise. Hence, it can also be stated that physical exercise is not the same as exercise capacity, which might vary.
HEALTH-RELATED QUALITY OF LIFE (HRQOL):
We found heterogeneous results of the SF-36 physical component used to evaluate quality of life. The regression-based Egger test for small-study effects suggested evidence of publication bias (p=0.0061). Similar results were observed in the meta-analysis by Huang et al [38] and as a common cause we can consider the small number of included studies that analyzed this parameter. Just 1 of the studies included in our analyses had heart failure patients, and they were fewer in total number compared to coronary heart disease patients. Hence, we did not include this criterion in our study [30].
Overall, patient adherence was similar among studies. In 4 of the 11 studies, the intervention group had a higher percentage of patients who completed the study, in another 4 studies it was in favor of traditional methods, and another 3 studies had equivocal results. In the studies in which the patients’ adherence percentage was in favor of the intervention, we mention that the control group was an active one, the patients being supervised by qualified personnel. The digitization of the recovery process in these studies included HR monitoring belts and platforms for monitoring and issuing feedback from specialists. The intensity at which the exercises are carried out in the 2 compared groups (traditional vs digital recovery) is difficult to appreciate, especially because in the control group the patients often received only indications regarding the performance of the recovery exercises. In the intervention group, the presence of motion sensors, monitors for vital functions, and careful specialized supervision makes it much easier to determine and adjust the intensity of the exercises performed by patients.
We believe that the results of our meta-analysis support of the idea of conducting further randomized trials, especially because the development of technology is on the rise. Mobile medical applications have proven to be the most used in digital-assisted cardiac rehabilitation, probably because they are user-friendly. Unfortunately, the use of our search criteria did not lead to finding controlled studies on the effects of advanced technologies such as transmissions based on sensors or the use of exoskeletons.
LIMITATIONS:
Although we performed a thorough search of 3 databases, our study is limited by the restriction to post-sternotomy status, lack of open-access articles, language barrier (studies written in languages other than English), and limited ability of subjects to use the services provided by the investigators. Many of the included studies had a small number of participants and were heterogeneous concerning the characteristics of patients. However, I2 was zero in VO2 peak and 6MWT meta-analysis, which means there is no between-studies variability. Also, the particular analysis between digital training group with supervised cardiac rehabilitation studies included a small number of studies, and the results did not show significant statistical differences. There was no clear explanation provided on how the blood pressure measurements were obtained at home or was regulation of medical therapy a part of digital rehabilitation. Furthermore, it is advisable to evaluate physical activity by the daily or weekly amount of exercise done by the patients, instead of judging based on a 6-minute walk test. Conducting further trials will also allow the assessment of publication bias as well as the sensitivity of results to any single trial in the case of 6MWT. The HRQOL studies were inconclusive and there was evidence of publication bias. Confirmation of the present findings in additional larger-scale trials is strongly recommended. The differences in duration in the included studies also helped us to observe the dynamics of recovery progression, and it also represented proof for variants of recovery protocols used in different hospital settings. We sought to include in our meta-analysis studies that used more advanced technologies in the recovery process, based on motion sensors and exoskeletons, but few studies met such search criteria. However, the use of technology in the cardiac recovery process has proven to be at least as effective as traditional recovery in physical activity parameters enhancement in these patients.
One major limitation of our analysis is that control groups in the selected studies were strongly heterogeneous as they included supervised cardiac rehabilitation groups or home-based training or used advice for training only. Our findings are thus hypothesis-generating and should be further evaluated in additional larger studies that would include adequately selected control groups.
HANDLING OF MISSING DATA:
The meta-analysis of VO2 peak involved 8 studies and some patients were lost during follow-up. Missing outcome data are a common threat to the validity of randomized trials, as it creates a loss in power and precision and may result in bias at the trial level. These problems subsequently influenced the meta-analysis. The solution is to do a sensitivity analysis to identify how much the results change under different assumptions.
There is no one best approach to handle missing outcome data in meta-analysis with aggregate data. Available cases analysis (ACA) is usually a sensible starting point.
The informative missingness parameter (IMP) relates a summary statistic in the missing group to the corresponding summary statistic in the observed group. Because the IMP parameters cannot be estimated from the observed data, values must be given to them based on judgment. Thus, sensitivity analyses using different plausible values of IMPs are necessary to assess the robustness of results to different assumptions about the missing data.
The sensitivity option in the metamiss2 command sets the IMP means and correlation to zero and gradually increases the IMP standard deviations. This reflects a minor departure from missing at random (MAR). In practice, one would expect the IMP mean to be different from zero. We conducted additional sensitivity analyses by changing the value of both mean and SD (one at a time) of IMP parameters and assuming each of them is common and different across groups and monitor how sensitive results are to these changes.
IMDOM indicates the informative missingness difference of means for continuous outcome data.
We first described the departure from MAR using the IMDOM. We assumed a systematic departure from the MAR assumption where for the intervention group, IMDOM has a mean of −0.5 with SD(IMDOM)=1, and where for the control group, IMDOM has a mean of 1 with SD(IMDOM)=1.5. This means that we think it is likely that missing participants had better outcomes than observed participants in the intervention group, while the opposite is true in the control group (for example, they left the study because of lack of efficacy) (Figure 8).
We also assumed that IMDOMs were correlated between the 2 groups with ρ=0.5, and we compared the results with ACA (that is, when IMP=0 without uncertainty).
To investigate how the summary effect and its variance changes under different levels of uncertainty assumed for the IMP, we ran a sensitivity analysis with IMDOM=1 on a range of different values for SD of IMDOM using the bootstrap method (Figure 9). Increasing the uncertainty of the IMP did not significantly change the confidence interval for the summary effect.
Conclusions
Digitization of the cardiac rehabilitation after sternotomy due to cardiac revascularization or valvular replacement helped obtain better results in most cases compared to traditional rehabilitation programs in patient adherence. To produce clearer outcomes, larger studies on heterogeneous populations are widely required, which could help set future standard protocols. The technological interventions used in these studies included the use of a smartphone or HR belts, strictly to monitor the physical activity of the participants and to provide sustained explanations for performing the exercise training. This suggests that in the process of cardiac rehabilitation, patients need visual and auditory stimulation. Also, the exercise training program associated with nutrition advice, pharmacological therapy, and improvement of the psychological approach to the situation led to better and clinically significant results. This review provides support for future larger studies on cardiac rehabilitation, using several advanced technology methods associated with lifestyle changes in phases 2 and 3 of the rehabilitation process, which can help achieve better patient compliance and decrease the overall financial burden.
Figures
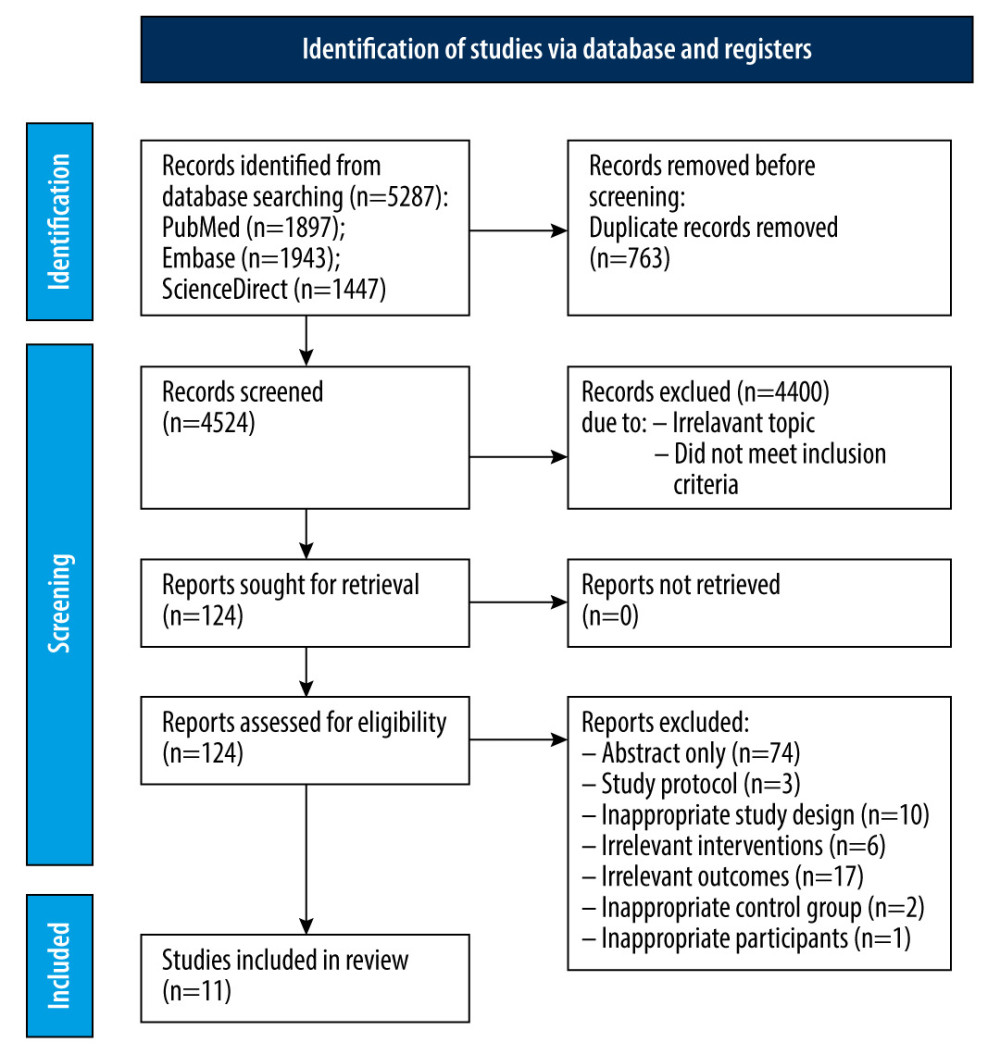 Figure 1. Prisma flow diagram of study selection.
Figure 1. Prisma flow diagram of study selection. 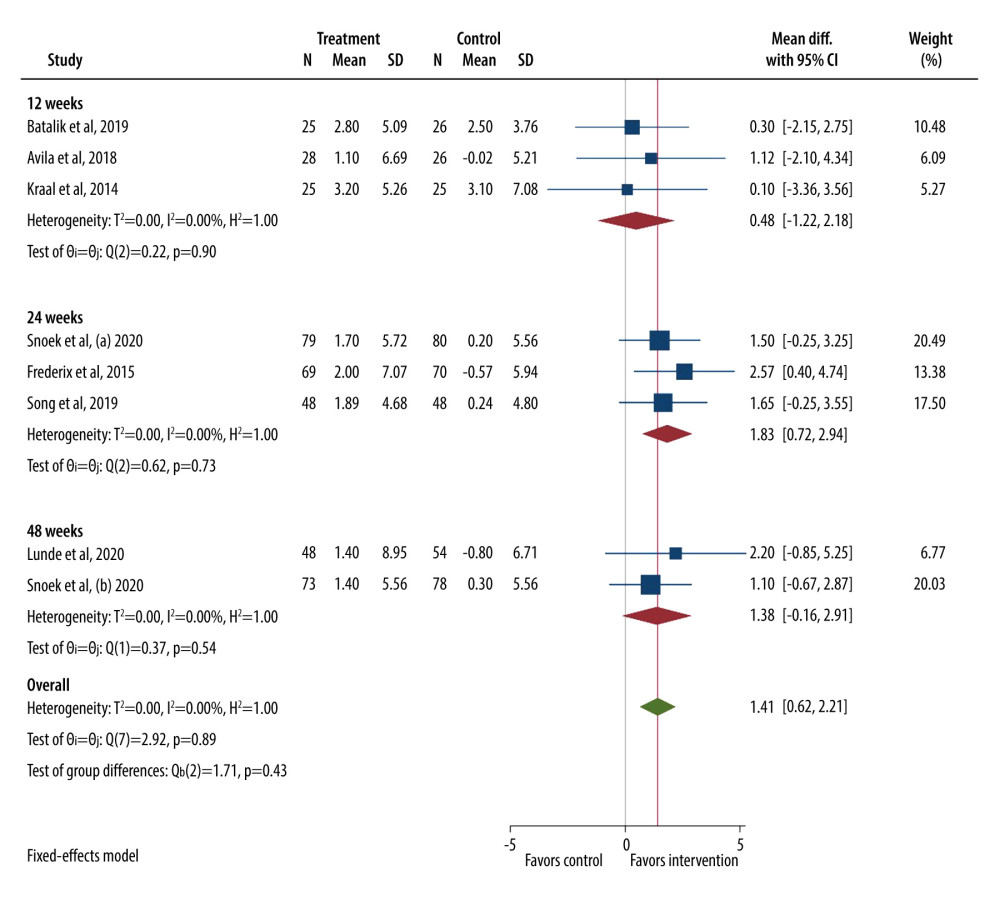 Figure 2. Forest plot for VO2 peak.
Figure 2. Forest plot for VO2 peak. 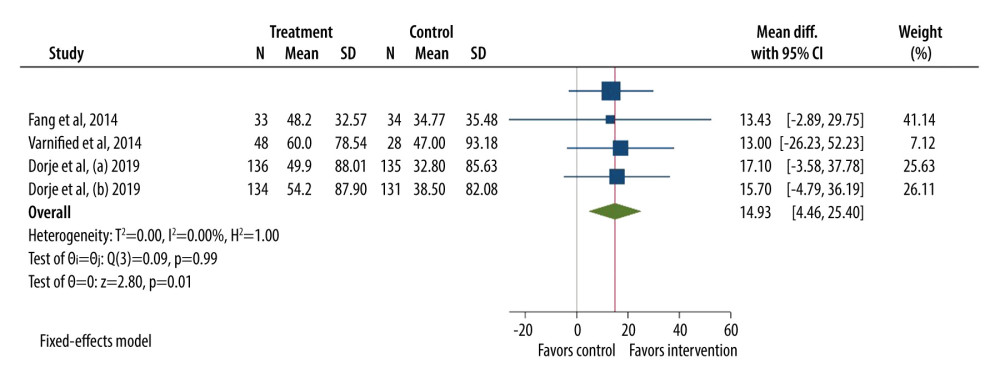 Figure 3. Forest plot for a 6-minute walk test (6MWT).
Figure 3. Forest plot for a 6-minute walk test (6MWT). 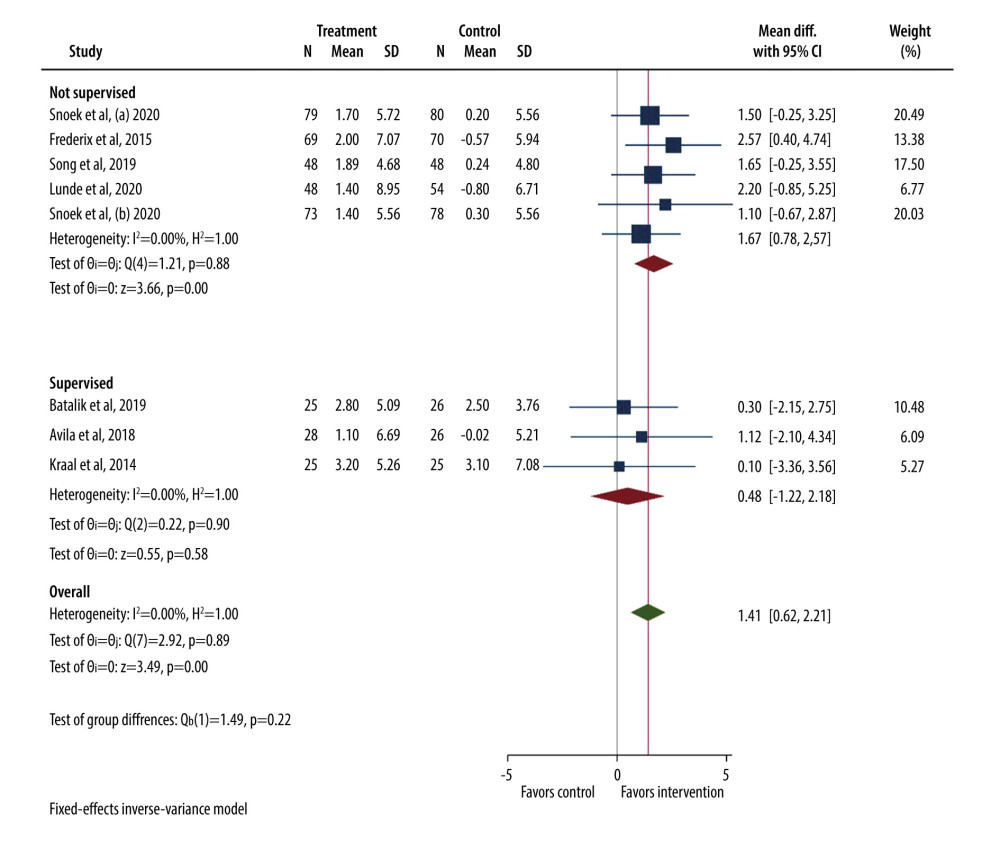 Figure 4. Forest plot for VO2 peak (supervised vs not supervised control group).
Figure 4. Forest plot for VO2 peak (supervised vs not supervised control group). 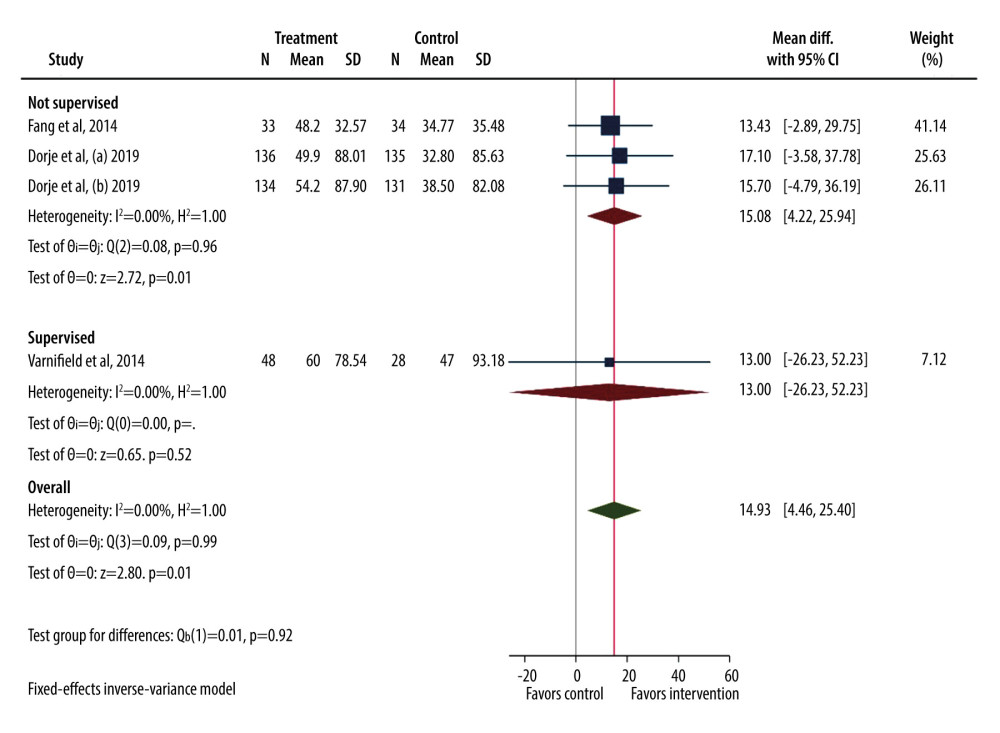 Figure 5. Forest plot for 6MWT (supervised vs not supervised control group).
Figure 5. Forest plot for 6MWT (supervised vs not supervised control group). 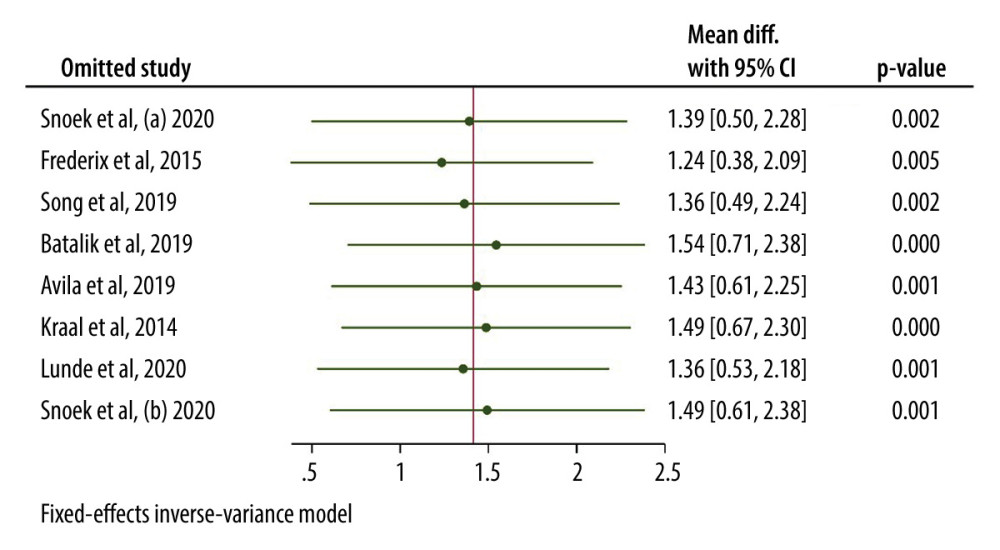 Figure 6. Leave one out sensitivity analysis for VO2 peak.
Figure 6. Leave one out sensitivity analysis for VO2 peak. 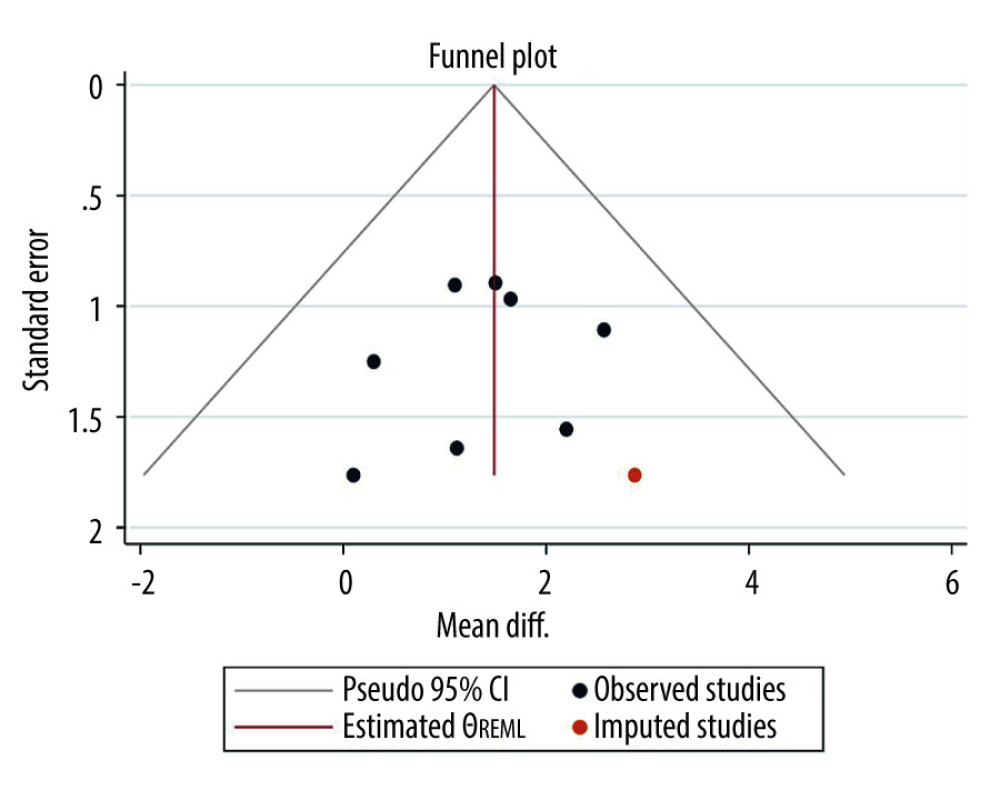 Figure 7. Funnel plot for VO2 peak.
Figure 7. Funnel plot for VO2 peak. 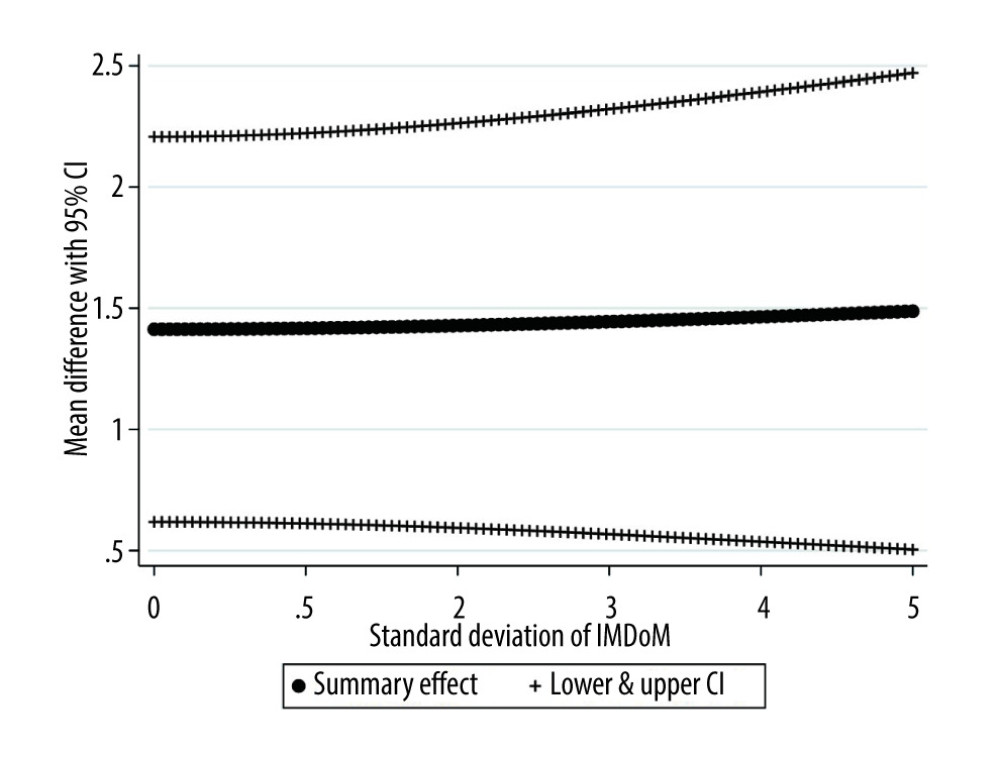 Figure 9. Plot of the summary mean difference of intervention versus control and the respective 95% confidence interval (random-effects meta-analysis) for various values of SD of IMDOM under the IMDOM=1 assumption.
Figure 9. Plot of the summary mean difference of intervention versus control and the respective 95% confidence interval (random-effects meta-analysis) for various values of SD of IMDOM under the IMDOM=1 assumption. 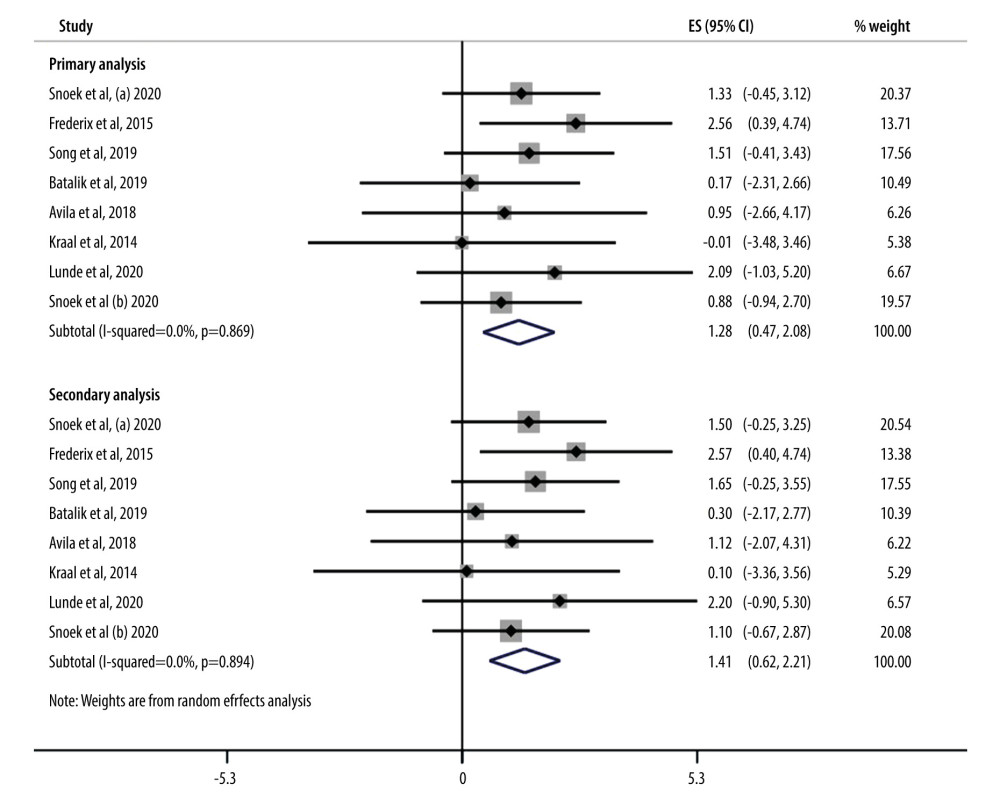 Figure 8. Forrest plot showing results of primary and secondary analysis.
Figure 8. Forrest plot showing results of primary and secondary analysis. References
1. WHO CVD Risk Chart Working Group, World Health Organization cardiovascular disease risk charts: Revised models to estimate risk in 21 global regions: Lancet Glob Health, 2019; 7(10); e1332-e45
2. Poortaghi S, Baghermia A, Golzari SEJ, The effect of home-based cardiac rehabilitation program on self efficacy of patients referred to cardiac rehabilitation center: BMC Res Notes, 2013; 6; 287
3. Visseren FLJ, March F, Smulders YM, 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Eur Heart J, 2021; 42(34); 3227-37
4. de Araújo Pio CS, Interventions to promote patient utilization of cardiac rehabilitation: Cochrane systematic review and meta-analysis: J Clin Med, 2019; 8(2); 189
5. Winkelmann ER, Dallazen F, Steinke Bronzatii AB, Analysis of steps adapted protocol in cardiac rehabilitation in the hospital phase: Rev Bras Cir Cardiovasc, 2015; 30(1); 40-48
6. Pinto R, Lemos Pires M, Borges M, Digital home-based multidisciplinary cardiac rehabilitation: the way to counteract physical inactivity during the COVID-19 pandemic?: Eur J Prev Cardiol, 2021; 28(Suppl 1) zwab061.329
7. Ambrosetti M, Abreu A, Corrá U, Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology: Eur J Prev Cardiol, 2020 [Online ahead of print]
8. Céspedes N, Irfan B, Senft E, A socially assistive robot for long-term cardiac rehabilitation in the real world: Front Neurorobot, 2021; 15; 633248
9. Clark RA, Conway A, Poulsen V, Alternative models of cardiac rehabilitation: A systematic review: Eur J Prev Cardiol, 2015; 22(1); 35-74
10. Barnason S, Zimmerman L, Nieveen J, Influence of a symptom management telehealth intervention on older adults’ early recovery outcomes after coronary artery bypass surgery: Heart Lung, 2009; 38(5); 364-76
11. Wongvibulsin S, Habeos EE, Huynh PP, Digital health interventions for cardiac rehabilitation: Systematic literature review: J Med Internet Res, 2021; 23(2); e18773
12. Lara JS, Cases J, Aguirre A, Human-robot sensor interface for cardiac rehabilitation: IEEE Int Conf Rehabil Robot, 2017; 2017; 1013-18
13. de Macedo RM, Faria-Neto JR, Otriz Constantini C, Phase I of cardiac rehabilitation: A new challenge for evidence based physiotherapy: World J Cardiol, 2011; 3(7); 248-55
14. Freene N, van Berlo S, McNanus M, A behavioral change smartphone app and program (ToDo-CR) to decrease sedentary behavior in cardiac rehabilitation participants: Prospective feasibility cohort study: JMIR Form Res, 2020; 4(11); e17359
15. Moulson N, Bewick D, Selway T, Cardiac rehabilitation during the COVID-19 era: Guidance on implementing virtual care: Can J Cardiol, 2020; 36(8); 1317-21
16. de Melo Ghisi GL, Xu Z, Liu X, Impacts of the COVID-19 pandemic on cardiac rehabilitation delivery around the world: Glob Heart, 2021; 16(1); 43
17. Brouwers RWM, van Exel HJ, van Hal JMC, Cardiac telerehabilitation as an alternative to centre-based cardiac rehabilitation: Neth Heart J, 2020; 28(9); 443-51
18. Dalal HM, Taylor RS, Jolly K, The effects and costs of home-based rehabilitation for heart failure with reduced ejection fraction: The REACH-HF multicentre randomized controlled trial: Eur J Prev Cardiol, 2019; 26(3); 262-72
19. Gandhi S, Chen S, Hong L, Effect of mobile health interventions on the secondary prevention of cardiovascular disease: Systematic review and meta-analysis: Can J Cardiol, 2017; 33(2); 219-31
20. García-Bravo S, Cuesta-Gómez A, Campuzano-Ruiz R, Virtual reality and video games in cardiac rehabilitation programs. A systematic review: Disabil Rehabil, 2021; 43(4); 448-57
21. Antoniou V, Davos CH, Kapreli E, Effectiveness of home-based cardiac rehabilitation, using wearable sensors, as a multicomponent, cutting-edge intervention: A systematic review and meta-analysis: J Clin Med, 2022; 11(13); 3772
22. Higgins JPT, Thomas J, Chandler J: Cochrane handbook for systematic reviews of interventions, 2019, Chichester, John Wiley & Sons
23. Higgins J, Thompson S, Deeks J, Altman D, Statistical heterogeneity in systematic reviews of clinical trials: A critical appraisal of guidelines and practice: J Health Serv Res Policy, 2002; 7(1); 51-61
24. Greenhouse JB, Iyengar S, Sensitivity analysis and diagnostics: The handbook of research synthesis and meta-analysis, 2009; 417-33, New York, NY, US, Russell Sage Foundation
25. Egger M, Davey Smith G, Schneider M, Minder C, Bias in meta-analysis detected by a simple, graphical test: BMJ, 1997; 315(7109); 629-34
26. Avila A, Claes J, Goetschalckx K, Home-based rehabilitation with telemonitoring guidance for patients with coronary artery disease (short-term results of the TRiCH study): Randomized controlled trial: J Med Internet Res, 2018; 20(6); e225
27. Batalik L, Dosbaba F, Hartman M, Benefits and effectiveness of using a wrist heart rate monitor as a telerehabilitation device in cardiac patients: A randomized controlled trial: Medicine (Baltimore), 2020; 99(11); e19556
28. Dorje T, Zhao G, Tso K, Smartphone and social media-based cardiac rehabilitation and secondary prevention in China (SMART-CR/SP): A parallel-group, single-blind, randomised controlled trial: Lancet Digit Health, 2019; 1(7); e363-e74
29. Fang J, Huang B, Xu D, Innovative application of a home-based and remote sensing cardiac rehabilitation protocol in Chinese patients after percutaneous coronary intervention: Telemed J E Health, 2019; 25(4); 288-93
30. Frederix I, Hansen D, Coninx K, Medium-term effectiveness of a comprehensive internet-based and patient-specific telerehabilitation program with text messaging support for cardiac patients: Randomized controlled trial: J Med Internet Res, 2015; 17(7); e185
31. Hawkes AL, Patrao TA, Atherton J, Effect of a telephone-delivered coronary heart disease secondary prevention program (proactive heart) on quality of life and health behaviours: Primary outcomes of a randomised controlled trial: Int J Behav Med, 2013; 20(3); 413-24
32. Kraal JJ, Peek N, Van den Akker-Van Martie Elske, Effects of home-based training with telemonitoring guidance in low to moderate risk patients entering cardiac rehabilitation: Short-term results of the FIT@Home study: Eur J Prev Cardiol, 2014; 21(2 Suppl); 26-31
33. Lunde P, Bye A, Bergland A, Long-term follow-up with a smartphone application improves exercise capacity post cardiac rehabilitation: A randomized controlled trial: Eur J Prev Cardiol, 2020; 27(16); 1782-92
34. Snoek JA, Prescott EI, van der Velde A, Effectiveness of home-based mobile guided cardiac rehabilitation as alternative strategy for nonparticipation in clinic-based cardiac rehabilitation among elderly patients in Europe: A randomized clinical trial: JAMA Cardiol, 2021; 6(4); 463-68
35. Song Y, Ren C, Liu P, Effect of smartphone-based telemonitored exercise rehabilitation among patients with coronary heart disease: J Cardiovasc Transl Res, 2020; 13(4); 659-67
36. Varnfield M, Karunanithi M, Lee C-K, Smartphone-based home care model improved use of cardiac rehabilitation in postmyocardial infarction patients: Results from a randomised controlled trial: Heart, 2014; 100(22); 1770-79
37. Gremeaux V, Troisgros O, Benaïm S, Determining the minimal clinically important difference for the six-minute walk test and the 200-meter fast-walk test during cardiac rehabilitation program in coronary artery disease patients after acute coronary syndrome: Arch Phys Med Rehabil, 2011; 92(4); 611-19
38. Huang K, Liu W, He D, Telehealth interventions versus center-based cardiac rehabilitation of coronary artery disease: A systematic review and meta-analysis: Eur J Prev Cardiol, 2015; 22(8); 959-71
Figures
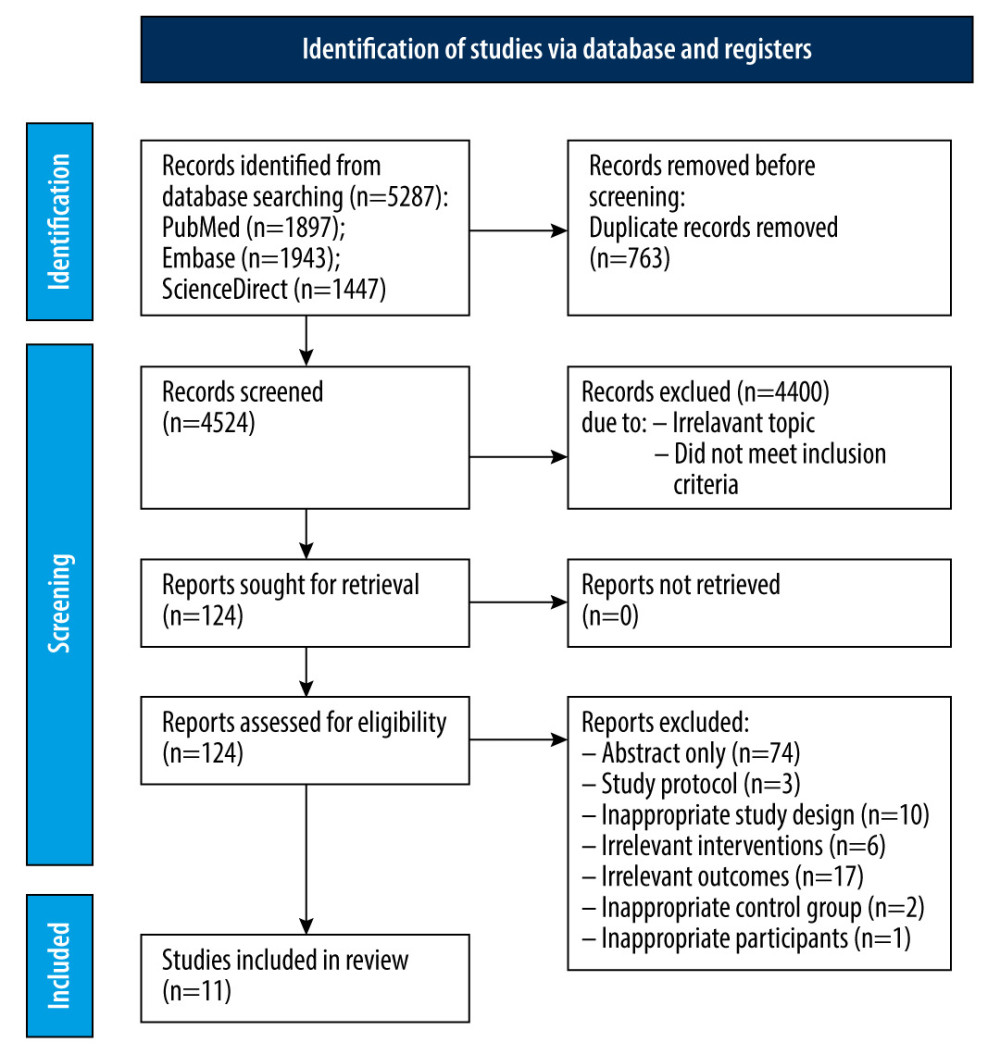 Figure 1. Prisma flow diagram of study selection.
Figure 1. Prisma flow diagram of study selection.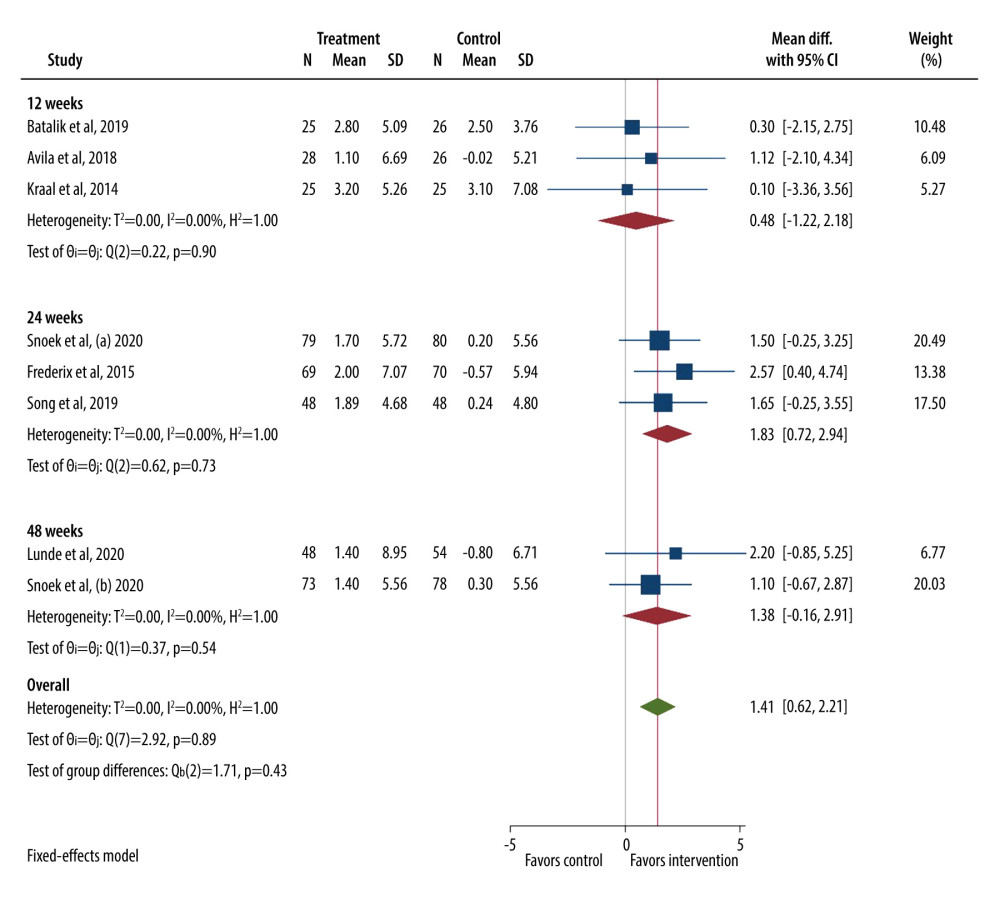 Figure 2. Forest plot for VO2 peak.
Figure 2. Forest plot for VO2 peak.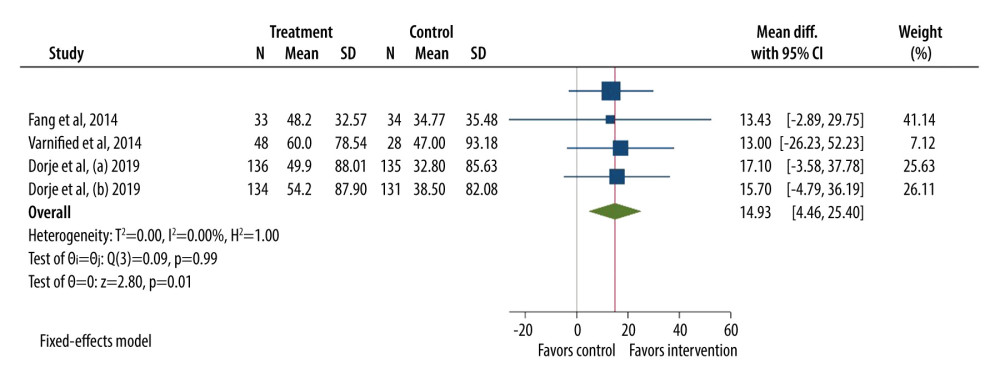 Figure 3. Forest plot for a 6-minute walk test (6MWT).
Figure 3. Forest plot for a 6-minute walk test (6MWT).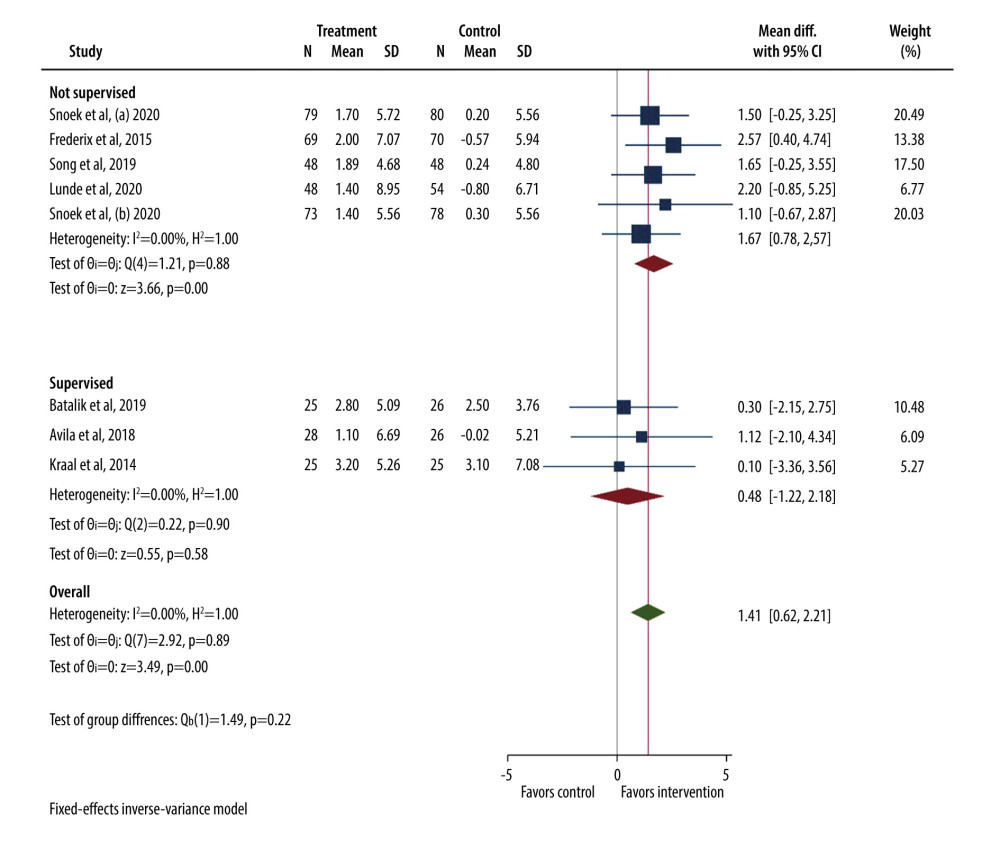 Figure 4. Forest plot for VO2 peak (supervised vs not supervised control group).
Figure 4. Forest plot for VO2 peak (supervised vs not supervised control group).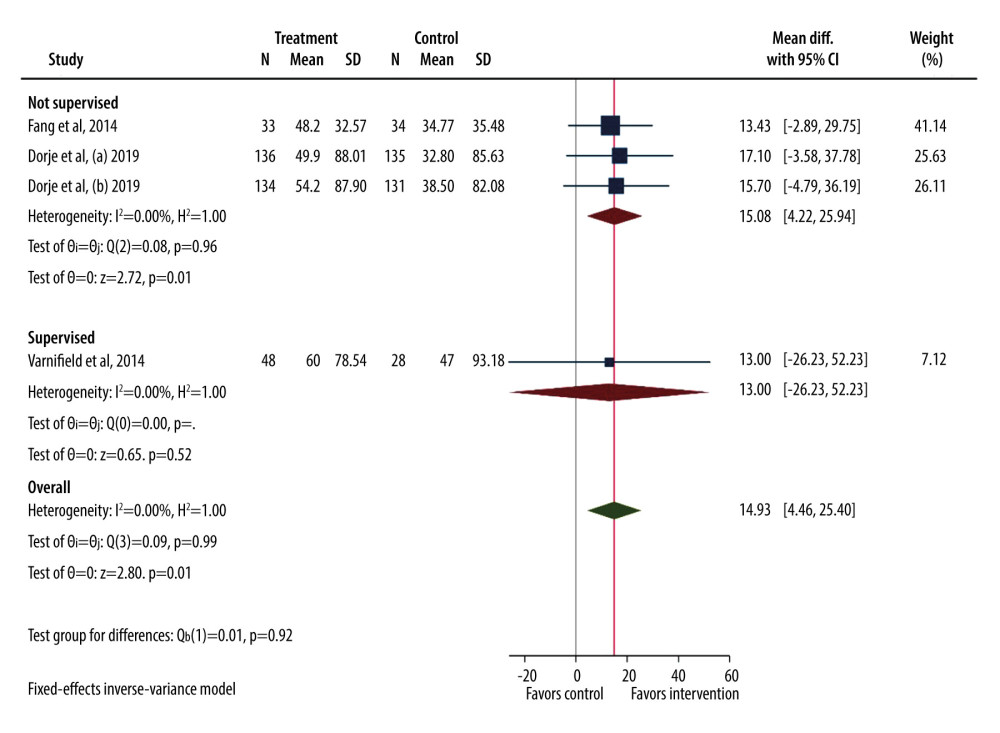 Figure 5. Forest plot for 6MWT (supervised vs not supervised control group).
Figure 5. Forest plot for 6MWT (supervised vs not supervised control group).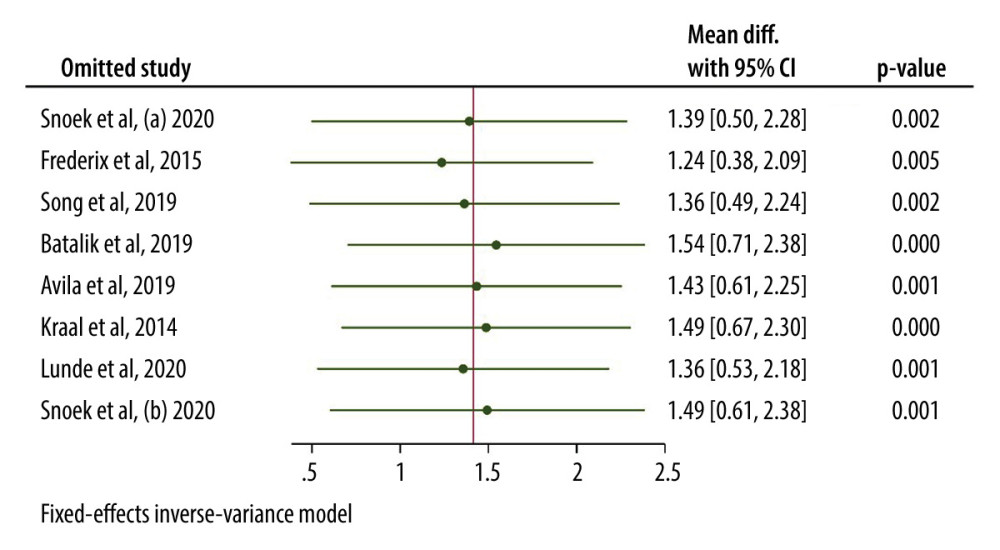 Figure 6. Leave one out sensitivity analysis for VO2 peak.
Figure 6. Leave one out sensitivity analysis for VO2 peak.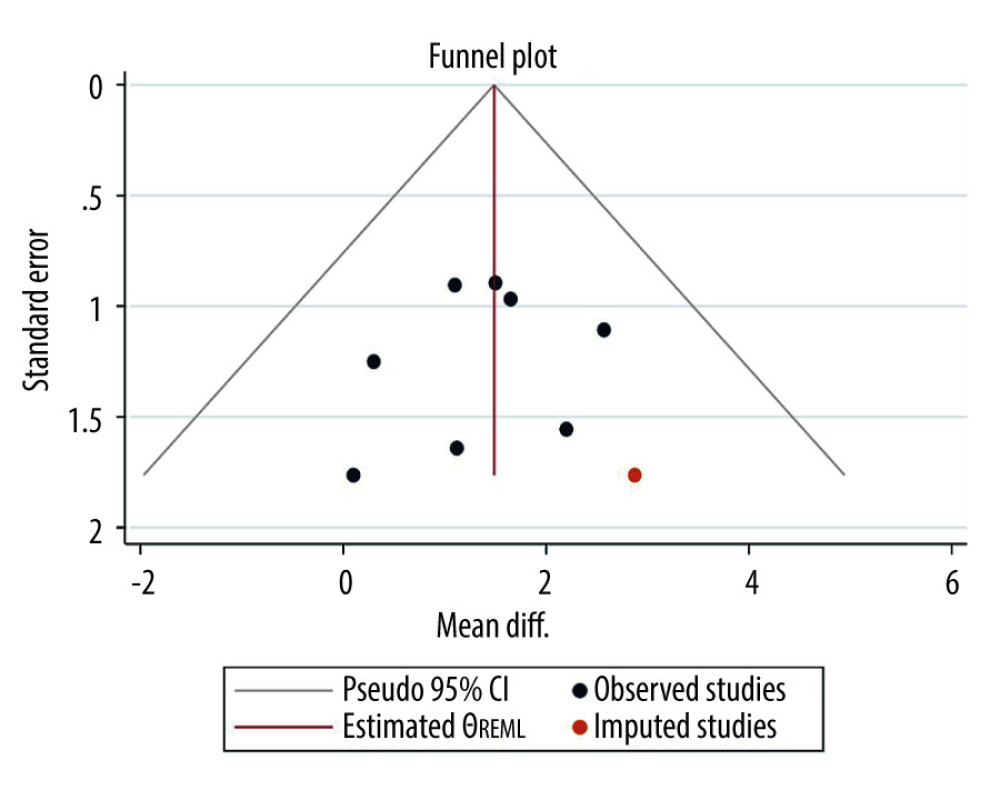 Figure 7. Funnel plot for VO2 peak.
Figure 7. Funnel plot for VO2 peak.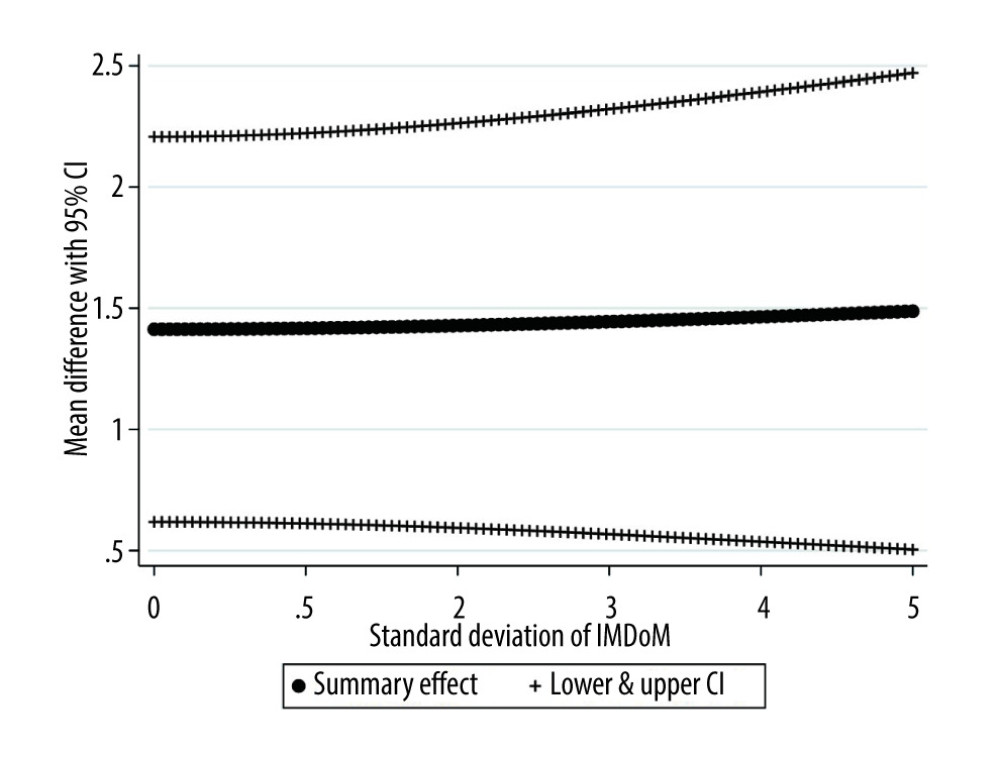 Figure 9. Plot of the summary mean difference of intervention versus control and the respective 95% confidence interval (random-effects meta-analysis) for various values of SD of IMDOM under the IMDOM=1 assumption.
Figure 9. Plot of the summary mean difference of intervention versus control and the respective 95% confidence interval (random-effects meta-analysis) for various values of SD of IMDOM under the IMDOM=1 assumption.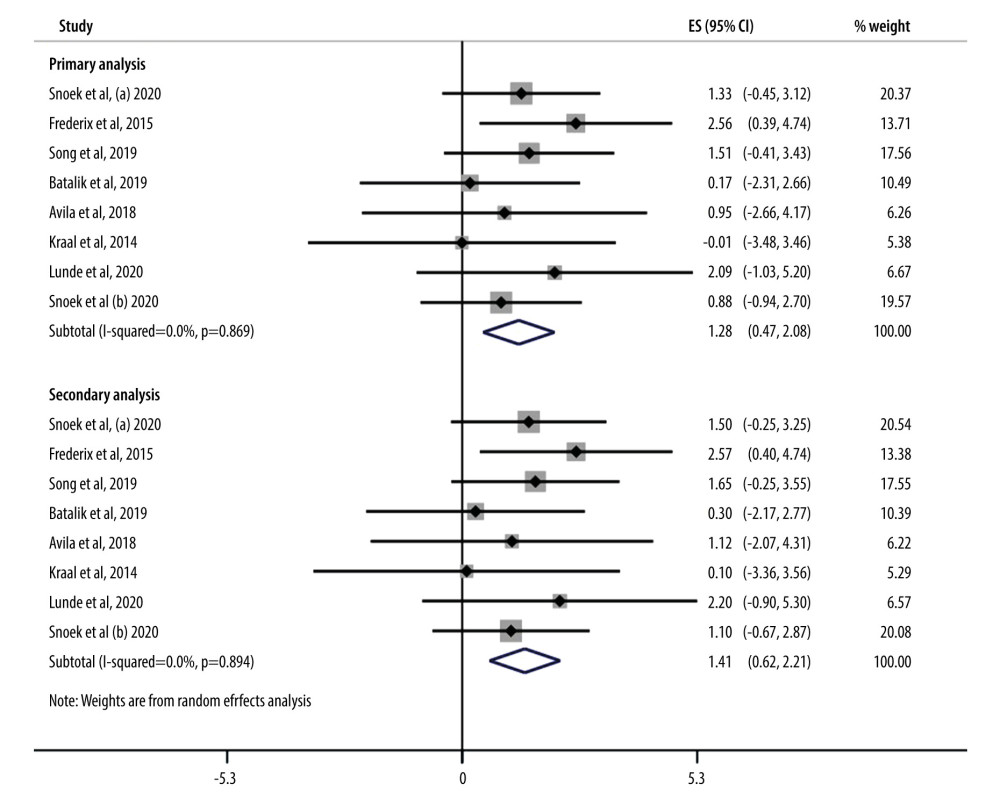 Figure 8. Forrest plot showing results of primary and secondary analysis.
Figure 8. Forrest plot showing results of primary and secondary analysis. Tables
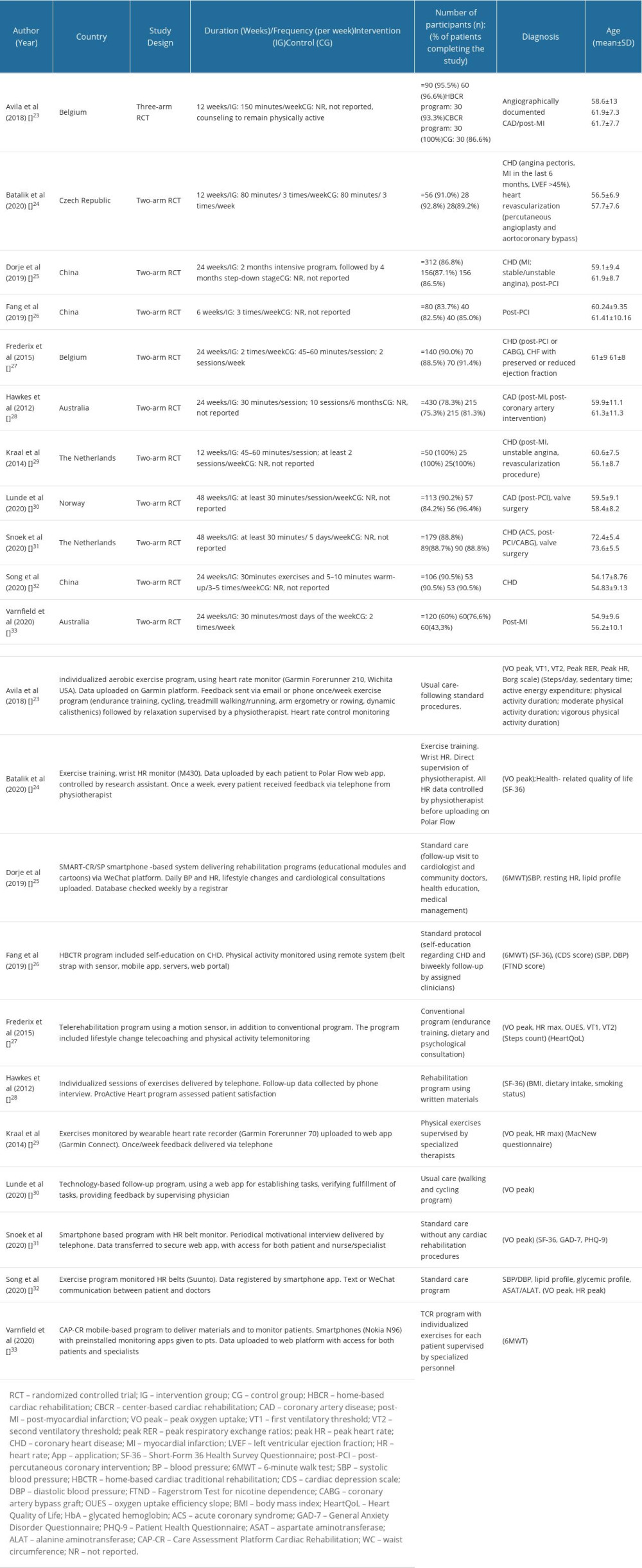 Table 1. Demographic characteristics and baseline parameters description of included studies (n=11).
Table 1. Demographic characteristics and baseline parameters description of included studies (n=11).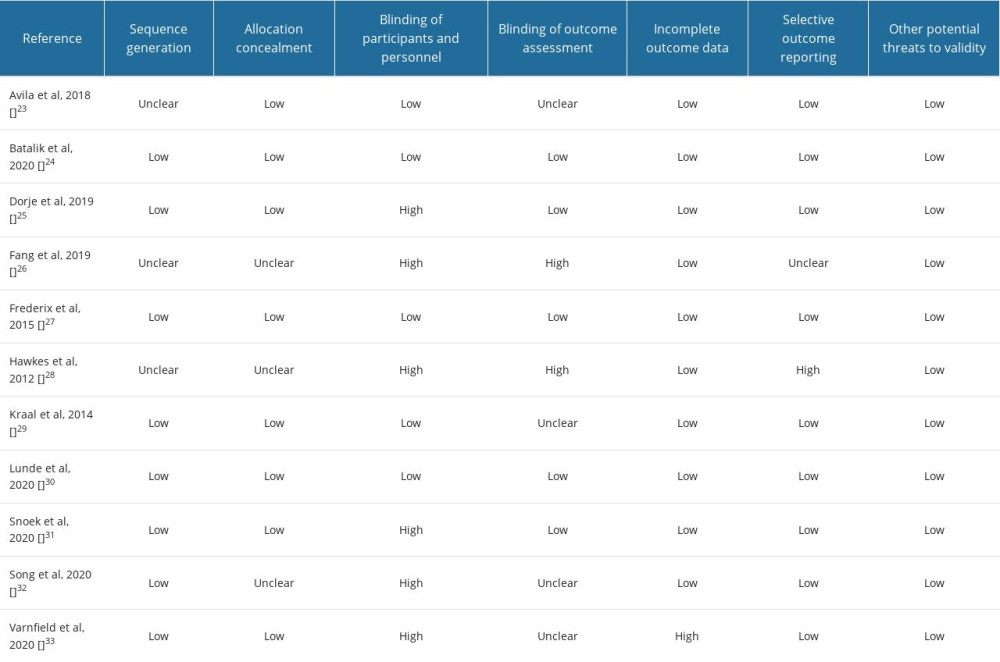 Table 2. Risk of bias assessment of the included studies.
Table 2. Risk of bias assessment of the included studies.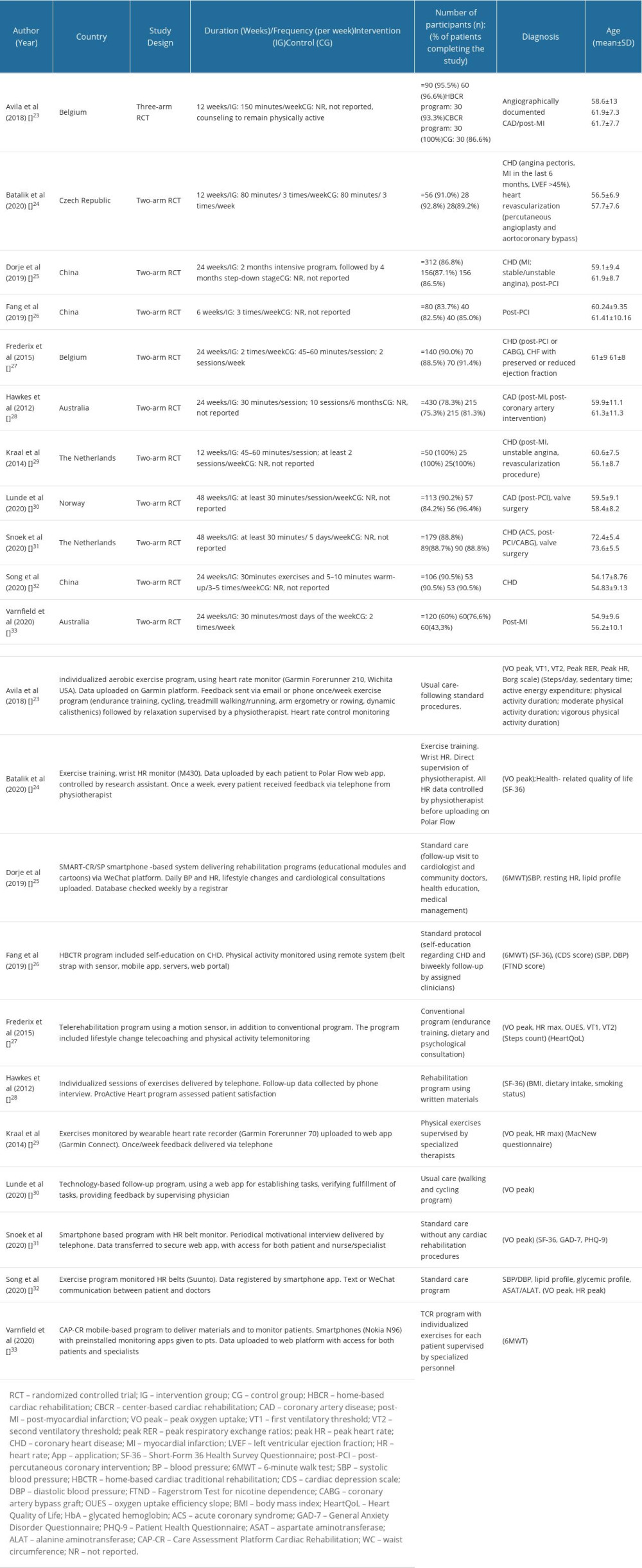 Table 1. Demographic characteristics and baseline parameters description of included studies (n=11).
Table 1. Demographic characteristics and baseline parameters description of included studies (n=11).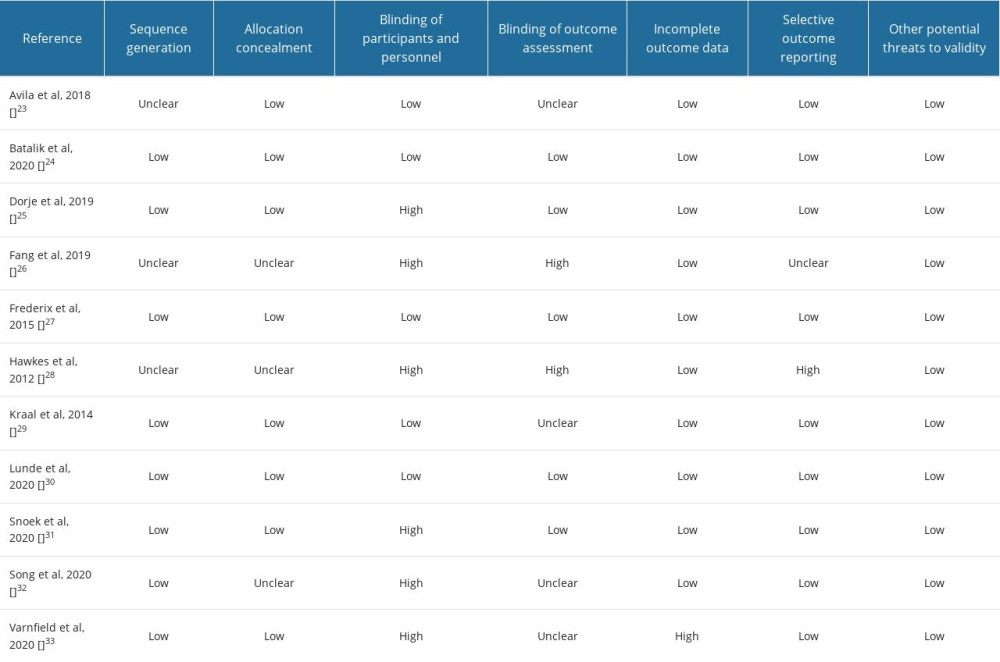 Table 2. Risk of bias assessment of the included studies.
Table 2. Risk of bias assessment of the included studies. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








