13 April 2023: Clinical Research
Efficacy of Direct Anterior Approach Versus Posterior Lateral Approach for Total Hip Replacement in Patients with Parkinson’s Disease
Meng Yang1ABCDE, Mengxuan Yao1ADE, Kun Chu1D, Congcong Wei2B, Zihang Li1C, Jia Huo1F, Sikai Liu1F, Huijie LiDOI: 10.12659/MSM.939682
Med Sci Monit 2023; 29:e939682
Abstract
BACKGROUND: The present study was performed to evaluate the efficacy of direct anterior approach (DAA) versus posterolateral approach (PLA) for total hip arthroplasty (THA) in patients with Parkinson’s disease (PD). The aim of the study was to compare the speed of recovery of hip function and postoperative complications between the 2 approaches.
MATERIAL AND METHODS: The study included 285 Parkinson’s patients who underwent THA; 209 eligible patients were recruited for analysis as per the inclusion criteria and assigned into DAA group (n=90) and PLA group (n=119) according to the surgical approach. Postoperative Harris Hip Score (HHS), Western Ontario and McMaster University Osteoarthritis Index (WOMAC), and Forgotten joint score (FJS) were collected to assess hip function.
RESULTS: The DAA had a statistically lower incidence of postoperative complications than the PLA, particularly the rate of postoperative dislocation. Perioperative outcomes showed a longer operative time in the DAA than in the PLA group and more intraoperative blood loss in the DAA than in the PLA group. At 3 months postoperatively, the HHS and WOMAC scores in the DAA group showed significantly higher scores compared to the PLA group versus the DAA group. However, these differences disappeared at 6 months postoperatively and the FJS in the DAA group had a statistically higher score compared to the PLA group.
CONCLUSIONS: In patients with Parkinson’s disease complicated with hip disease, the DAA approach exhibited a lower rate of dislocation than the PLA approach and had faster recovery of hip function.
Keywords: Arthroplasty, replacement, Hip, Humans, Arthroplasty, Replacement, Hip, Parkinson Disease, Treatment Outcome, Postoperative Complications, Joint Dislocations
Background
Parkinson’s disease (PD) is the second most prevalent progressive neurodegenerative disease in the elderly. It is caused by pathological loss of dopaminergic neurons in the substantia nigra of the midbrain and enhanced acetylcholine action, resulting in slow movements and tremors of the hands, feet, or other parts of the body [1]. Hayes et al [2] suggested that PD can cause progressive bradykinesia, muscle stiffness, contractures, dystonia, and postural instability, and may be accompanied by resting tremors, leading to a higher risk of falls in patients with PD. Fontalis et al [3] identified a higher incidence of femoral neck fractures and a greater susceptibility to osteoarthritis in PD patients given their older age and abnormal stresses around the hip joint. It has been shown that some PD patients could tolerate surgery after specialized neurological interventions [4]. Total hip arthroplasty (THA) is most recommended for the management of hip diseases in the present stage, including the available direct anterior and posterior lateral approaches, both of which provide a safe and effective reconstruction of the femur and acetabulum. Studies suggest that THA relieves hip pain, improves hip function, and enhances patients’ quality of life [5,6]. Among the causes of soft tissue injuries, surgical access is considered one of the influencing factors [7–9]. Thus, the selection of the optimal approach can significantly reduce the severity of pain and improve the range of motion and function of the hip joint, thereby increasing patient satisfaction with THA. Zhang et al [10] found a high prevalence (9%) of prosthesis dislocation after hip replacement in patients with neuromuscular disorders such as post-hemiplegia, post-polio, and Parkinson’s disease with hip muscle laxity or muscle imbalance. Nevertheless, studies on the efficacy of THA have excluded neuromuscular disorders, and long-term clinical follow-up of patients with PD undergoing THA using different surgical approaches has been sparsely reported. To this end, this study was performed to evaluate the efficacy of DAA versus PLA for THA in patients with PD.
Material and Methods Participants
SURGICAL PROCEDURES:
All procedures were performed by experienced chief surgeons. The prosthesis used was produced by Johnson & Johnson Tri-lock COC (Johnson & Johnson, New Brunswick, NJ, USA), and preoperative template measurements were routinely performed in the included patients.
DAA group: the procedure was performed according to the surgical procedures described by Nakata et al and Lovell et al [11,12]. Patients were placed in the supine position, and a longitudinal incision was made along the gap between the broad fascial tensor and suture muscles starting 2 cm lateral and distal to the anterior superior iliac spine. The skin, subcutaneous tissue, and fascia were incised in sequence, and the Smith-Peterson gap was separated. The lateral femoral cutaneous nerve was protected and the lateral femoral artery was ligated by separating along the broad fascial tensor and rectus femoris gaps. The anterior aspect of the hip capsule was revealed and opened from within the broad fascial tensor and rectus femoris gaps, and the femoral neck was osteotomized to reveal the acetabulum, followed by acetabular preparation and acetabular component implantation. Femoral visualization was performed, followed by femoral preparation, traction, and femoral stem implantation. After the replacement was completed, the wound was closed (Figure 1A, 1B).
PLA group: With the patient in the lateral position, the pelvic positioner was placed posteriorly (sacrum) and anteriorly (pubis). A posterior lateral approach to the hip was performed, and the short external rotators and joint capsule were incised. The hip was dislocated posteriorly to fully expose the acetabulum and proximal femur, and acetabular preparation and acetabular component implantation as well as femoral preparation and distraction of the femoral stem for implantation of the prosthesis were performed sequentially. After the replacement was completed, the wound was closed (Figure 2A, 2B).
POSTOPERATIVE MANAGEMENT:
The patients were given antibiotics and low-molecular-weight heparin sodium postoperatively until discharge, and oral rivaroxaban was administered until 35 days postoperatively. Postoperative rehabilitation was provided by a professional charge nurse and a rehabilitation specialist. After recovery from anesthesia, the patients were instructed to perform ankle pump exercises. Patients were allowed to perform off-bed exercises if they could lift the lower leg off the bed voluntarily with them in a lying position, their knee joint flexed at 30° and the thigh fixed. This was to reduce the risk of falling due to insufficient lower limb strength and reduce the incidence of postoperative prosthesis dislocation and peripheral fracture. Functional exercises were performed in the DAA group after surgery: (1) upright hip flexion exercises for the iliopsoas muscle; (2) hip abduction exercises for the abductor muscle group to strengthen the mobility of the hip joint. PLA group: Excessive flexion, internal retraction, and internal rotation of the affected hip were avoided to avoid posterior dislocation of the hip.
BASELINE PATIENT PROFILES:
Baseline patient profiles were recorded, including sex, age, weight, height, body mass index (BMI), drinking, smoking, etiology, affected side, and postoperative complications. The operative time, intraoperative bleeding, incision length, and discharge time of the patients were recorded.
CLINICAL FUNCTIONAL ASSESSMENT:
All patients were followed up at 3 months, 6 months, and 12 months postoperatively. At each follow-up visit, the Harris Hip Score, McMaster University Osteoarthritis Index Score (WOMAC), and Joint Forgetting Score (FJS) were recorded to evaluate the hip function of patients after THA.
IMAGING:
Patients underwent preoperative and postoperative follow-up anteroposterior pelvic radiographs. Anteroposterior pelvic radiographs: Patients stood at a distance of 90 cm from the X-ray tube, with foot spacing equal to shoulder width and toes inward (15°) bilaterally. At the final follow-up, imaging measurements were performed using standardized anatomical landmarks. All imaging measurements (eccentric distance, neck stem angle, and difference in lower limb length) were performed independently by 2 experienced orthopedic surgeons using data obtained from our hospital’s picture archiving and communication system, and the values were averaged between the 2 surgeons. The eccentric distance was measured as the vertical distance between the center of rotation of the femoral head and the long axis of the femur [13]. The lower limb length difference is expressed as the vertical femoral offset measured as the vertical distance between the intertarsal line and the most medially visible point on the lesser trochanter, so the vertical offset of the femur on the operated side relative to the vertical offset of the femur on the healthy side is the lower limb length difference [14]. The cervical stem angle was measured as the angle between the long axis of the femoral stem and the inner and lower femoral neck axis [15]. To assess reproducibility, 20 patients were randomly selected and each measurement was performed twice independently, at an interval of 1 week. All intra-group correlation coefficients used to evaluate reproducibility in this study were >0.9.
STATISTICAL ANALYSIS:
Statistical analyses were performed using SPSS statistical software (IBM Corp., Armonk, NY, USA), version 19. Continuous variables were expressed as mean±standard deviation, and categorical variables were expressed as counts and percentages. Data normality was tested using the Shapiro-Wilk test, and 2 sets of categorical variables were compared using the chi-square test or Fisher’s exact probability method. If the variables were non-normally distributed, the Mann-Whitney test was employed to compare continuous variables. Continuous variables were compared between the 2 groups using the independent samples
Results
BASELINE PATIENT PROFILES:
The 2 groups were well-balanced in terms of baseline patient profiles, including age, gender, BMI, affected side, smoking, alcohol consumption, etiology, follow-up time, and duration of onset (P>0.05) (Table 1).
SURGICAL OUTCOMES:
THA performed through DAA was associated with significantly longer operative time and heavier intraoperative bleeding versus THA through PLA (P<0.05). DAA resulted in a higher incidence of postoperative complications (P<0.05). No incisional infection was reported in either group. The complication rate in the DAA group was 6.6%, including 4 cases of decreased sensation in the lateral thigh skin (due to lateral femoral cutaneous nerve pulling injury) and 2 patients with postoperative hip prosthesis dislocation who were given a reset by manual repositioning and exhibited good recovery. There were 19 cases of complications in the PLA group, with an incidence of 15.9%. Eleven patients had a hip dislocation, and 2 of them failed to be reset by manual repositioning and were prepared for incisional repositioning. However, the patients’ general condition gradually deteriorated and they were transferred to the ICU for treatment. They failed to complete the post-dislocation reset and died of cardiopulmonary complications 3 months after the dislocation. One case of fat liquefaction in the skin incision healed without infection after a wound dressing change. Three patients reported occasional pain during postoperative walking, which was caused by hematoma and skin infection at the surgical incision site. In the 2 patients with thrombosis, no other complications were reported after regular postoperative treatment (Tables 2, 3).
FUNCTIONAL SCORES:
Patients receiving THA via DAA exhibited better-improved hip function versus those with THA by PLA, evidenced by the higher HHS and lower WOMAC scores at 3 months postoperatively (P<0.05); however, this significant difference was absent at 6 months postoperatively (P>0.05) (Tables 4, 5).
FJS SCORES:
The high FJS scores in the DAA group versus the PLA group suggested better postoperative recovery of the patients with THA by DAA, as they tended to forget the existence of the prosthesis (P<0.05). The FJS scores were similar between the 2 arms at 2 years postoperatively and the last follow-up visit (Table 6).
IMAGING OUTCOMES:
There was no significant difference between the 2 groups in terms of neck stem angle, lower limb length difference and eccentric distance (P>0.05) (Table 7; Figures 3, 4).
Discussion
Currently, there are no systematic studies on the efficacy of THA with DAA or PLA in patients with hip disease complicated with Parkinson’s disease. Brendan et al [16] followed 214 patients with hip disease complicated by Parkinson’s disease and found that DAA resulted in lower pain scores, earlier functional recovery, and a lower risk of postoperative dislocation than PLA. The results of the present study showed that DAA was associated with more intraoperative bleeding and longer operative time than PLA, probably because DAA requires special positions as well as special surgical instruments, especially in revealing and installing the lateral femoral prosthesis. Wojtowicz et al [17] reported a 10% mortality rate for patients with Parkinson’s disease undergoing PLA. Despite a lower mortality rate of 1.4% in the present study than in the study by Wojtowicz et al, it is still higher than that of patients without PD undergoing total hip arthroplasty. About 20% of patients develop a severe disability or die within 5 years after disease onset [18]. Berry et al [19] found that the preoperative dislocation rate with PLA was significantly higher in patients with concomitant Parkinson’s disease (6.2%) than in patients without Parkinson’s disease (4.4%), and suggested that decreased muscle strength was responsible for the high dislocation rate. Xu et al [20] used a multifactorial statistical analysis to demonstrate that PLA surgery in patients with Parkinson’s disease was more likely to cause hip instability, leading to a higher incidence of dislocation, which was attributed to excessive destruction of the posterior joint capsule and externally rotated muscle groups by PLA; therefore, an anterior or lateral approach was recommended. Giori et al [21] found that the rate of dislocation with DAA in patients with combined Parkinson’s disease was (2.2%) similar to that of patients without Parkinson’s (1.9%), suggesting a lower postoperative dislocation rate with DAA in patients with concomitant Parkinson’s disease. The results of the present study demonstrated that the incidence of PLA hip dislocation was higher than that of PLA hip dislocation in patients without Parkinson’s disease (4.4%). The reason may be that elderly patients with Parkinson’s disease experience limb tremors, muscle tonicity, and difficulty in maintaining abduction neutral position when lying down, and are prone to internal retraction and internal rotation movements leading to hip dislocation, and PLA may cause periarticular soft tissue injury, resulting in hip instability after hip arthroplasty. The present study showed no statistically significant difference in the postoperative hip prosthesis position between the 2 groups, which was consistent with the research results by Giori et al [21]. The reason may be that DAA separates the deep fascia of the thigh from the gap between the broad fascial tensor and rectus femoris to expose the hip joint without cutting any muscle tendon. DAA preserves the posterior external rotators, posterior joint capsule, and reduces gluteus medius stretch, which reduces hip dislocation due to adductor destruction compared to PLA, thereby facilitating the maintenance of postoperative hip stability. Moreover, patients receiving THA via DAA exhibited better-improved hip function versus those with THA by PLA, evidenced by the higher HHS and lower WOMAC scores at 3 months postoperatively. The reason is that DAA minimized soft tissue and muscle damage and significantly reduced the incidence of dislocation. The high FJS scores in the DAA group versus the PLA group suggested better postoperative recovery of the patients with THA by DAA as they tended to forget the existence of the prosthesis (
The limitations of this study are the short follow-up, small sample size, and failure to identify long-term complications after DAA and PLA, such as aseptic loosening after hip arthroplasty. Studies with larger sample sizes and longer-term follow-ups are required for further evaluation.
Conclusions
THA with DAA is associated with longer operative time and heavier intraoperative bleeding, provides a lower risk of postoperative complications, and results in better postoperative experience and recovery of patients, as they tend to forget the hip prosthesis.
Figures
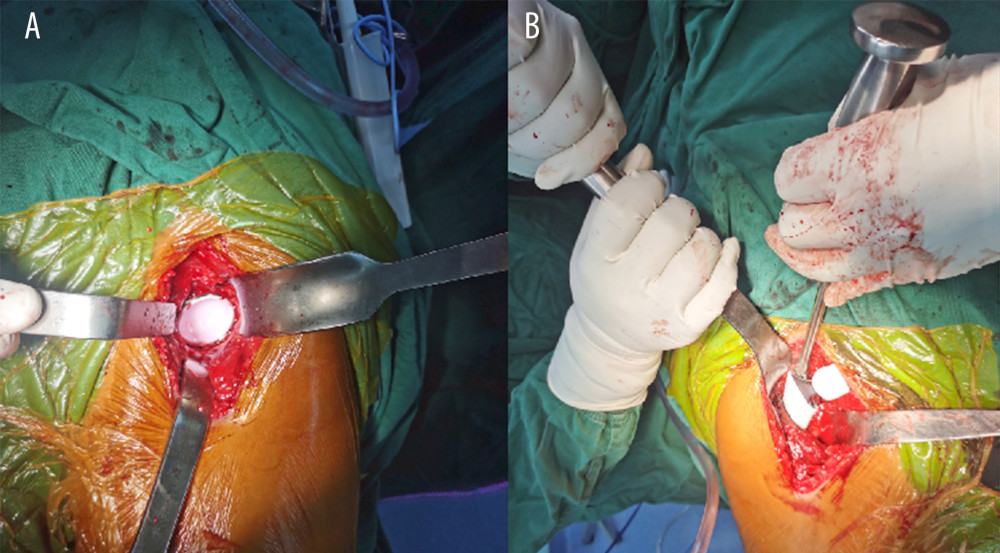 Figure 1. (A, B) Acetabular and femoral stem prostheses during DAA.
Figure 1. (A, B) Acetabular and femoral stem prostheses during DAA. 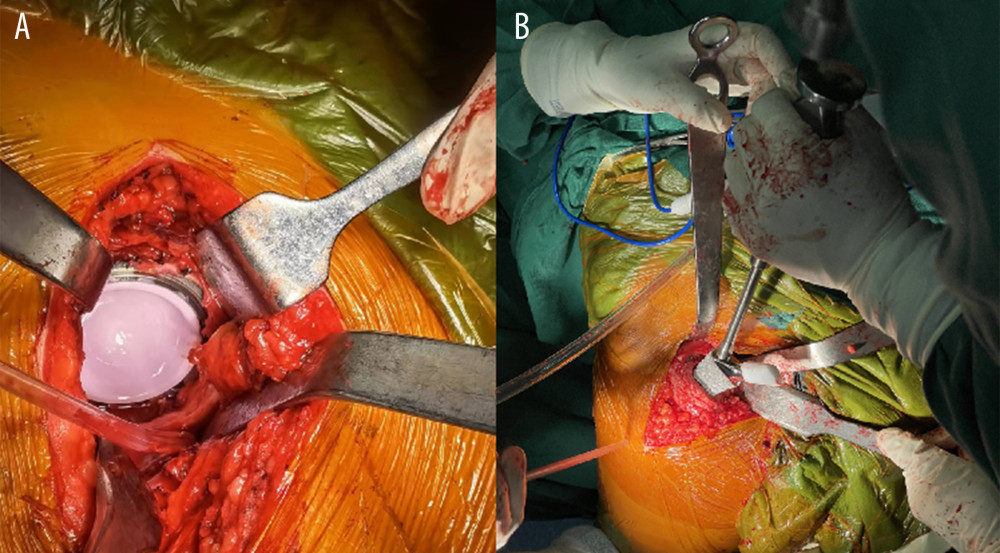 Figure 2. (A, B) Acetabular and femoral stem prosthesis during PLA.
Figure 2. (A, B) Acetabular and femoral stem prosthesis during PLA. 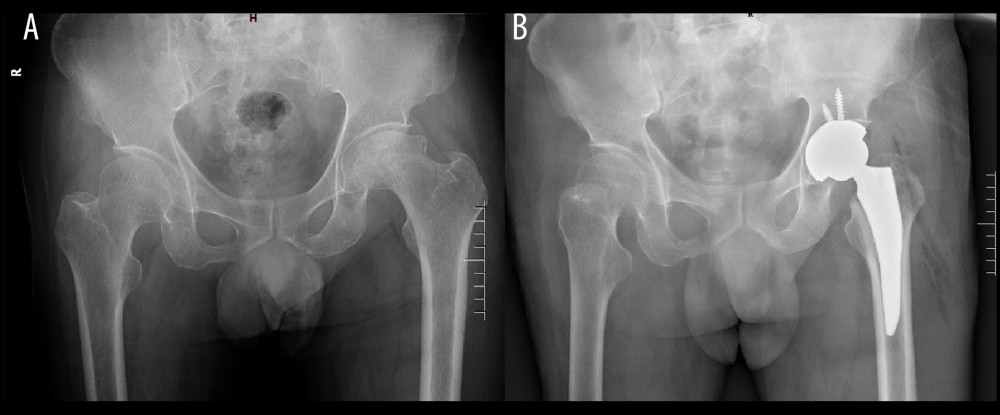 Figure 3. (A, B) Preoperative and postoperative anteroposterior X-rays of patients with DAA.
Figure 3. (A, B) Preoperative and postoperative anteroposterior X-rays of patients with DAA. 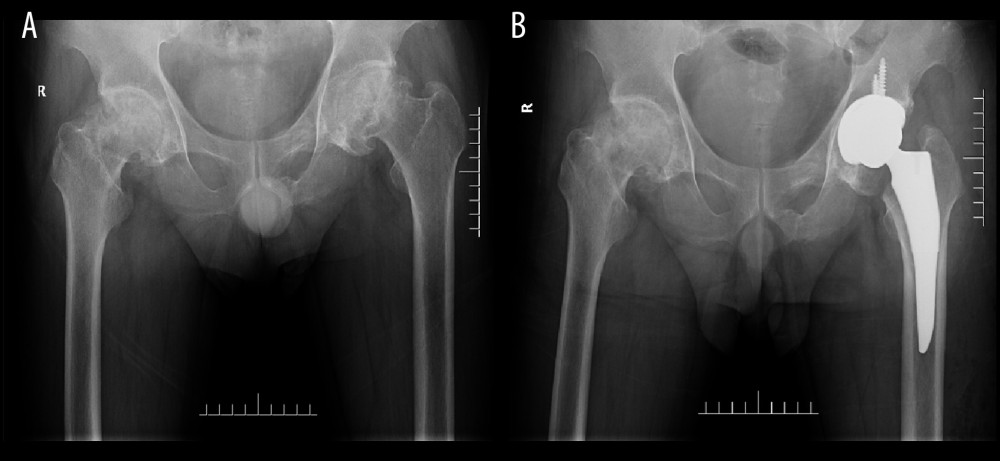 Figure 4. (A, B) Preoperative and postoperative anteroposterior X-rays of patients with PLA.
Figure 4. (A, B) Preoperative and postoperative anteroposterior X-rays of patients with PLA. References
1. Lotankar S, Prabhavalkar KS, Bhatt LK, Biomarkers for Parkinson’s disease: Recent advancement: Neurosci Bull, 2017; 33(5); 585-97
2. Hayes MT, Parkinson’s disease and Parkinsonism: Am J Med, 2019; 132(7); 802-7
3. Fontalis A, Kenanidis E, Bnennet-Brown K, Clinical outcomes in elective total hip arthroplasty in Parkinson’s disease: A systematic review of the literature: EFORT Open Rev, 2020; 5(12); 856-65
4. Chen Y-Y, Cheng P-Y, Wu S-L, Lai C-H, Parkinson’s disease and risk of hip fracture: An 8-year follow-up study in Taiwan: Parkinsonism Relat Disord, 2012; 18(5); 506-9
5. Wang Z, Hou J-Z, Wu C-H, A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty: J Orthop Surg Res, 2018; 13(1); 229-37
6. Xianquan W, Efficacy analysis of total hip arthroplasty with lateral femoral priority and combined anterior tilt angle techniques: Chinese Journal of Surgery, 2018; 56(04); 279-83
7. Sutphen SA, Berend KR, Morris MJ, Direct anterior approach has lower deep infection frequency than less invasive direct lateral approach in primary total hip arthroplasty: J Surg Orthop Adv, 2018; 27(1); 21-24
8. Petis S, Howard J, Lanting B, Comparing the anterior, posterior and lateral approach: Gait analysis in total hip arthroplasty: Can J Surg, 2018; 61(1); 50-57
9. Winther SB, Foss OA, Husby OS, Muscular strength and function after total hip arthroplasty performed with three different surgical approaches: One-year follow-up study: HIP Int, 2019; 29(4); 125-31
10. Yinchang Z, Hip prosthesis replacement in femoral neck fractures with neuromuscular lesions of the hip: Journal of Wannan Medical College, 2019; 38(04); 320-22
11. Nakata K, Nishikawa M, Yamamoto K, A clinical comparative study of the direct anterior with mini-posterior approach: Two consecutive series: J Arthroplasty, 2009; 24(5); 698-704
12. Lovell TP, Single-incision direct anterior approach for total hip arthroplasty using a standard operating table: J Arthroplasty, 2008; 23(7); 34-42
13. Parry MC, Povey J, Blom AW, Whitehouse MR, Comparison of acetabular bone resection, offset, leg length and post operative function between hip resurfacing arthroplasty and total hip arthroplasty: J Arthroplasty, 2015; 30(10); 799-803
14. Mahmood SS, Mukka SS, Crnalic S, Sayed-Noor AS, The influence of leg length discrepancy after total hip arthroplasty on function and quality of life: A prospective cohort study: J Arthroplasty, 2015; 30(9); 215-20
15. Yao M, Wang Y, Wei C, Greater increase in femoral offset with use of collum femoris-preserving stem than Tri-Lock stem in primary total hip arthroplasty: J Int Med Res, 2020; 48(5); 326-31
16. Higgins BT, Barlow DR, Heagerty NE, Lin TJ, Anterior vs. posterior approach for total hip arthroplasty, a systematic review and meta-analysis: J Arthroplasty, 2015; 30(3); 107-12
17. Wojtowicz AL, Mohaddes M, Odin D, Is Parkinson’s disease associated with increased mortality, poorer outcomes scores, and revision risk after THA? Findings from the Swedish Hip Arthroplasty Register: Clin Orthop Relat Res, 2019; 477(6); 1347-55
18. Wood BH, Bilclough JA, Walker RW, Incidence and prediction of falls in Parkinson’s disease: A prospective multidisciplinary study: J Neurol Neurosurg Psychiatry, 2002; 72(6); 721-25
19. Berry DJ, von Knoch M, Schleck CD, Harmsen WS, The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty: J Bone Joint Surg Am, 2004; 86(1); 9-14
20. Xu WD, Wu YS, Problems of artificial hip replacement surgery in Parkinson’s patients: Modern Rehabilitation, 2001; 19(16); 54-55
21. Giori NJ: Clin Orthop Relat Res, 2019; 477(6); 1356-57
Figures
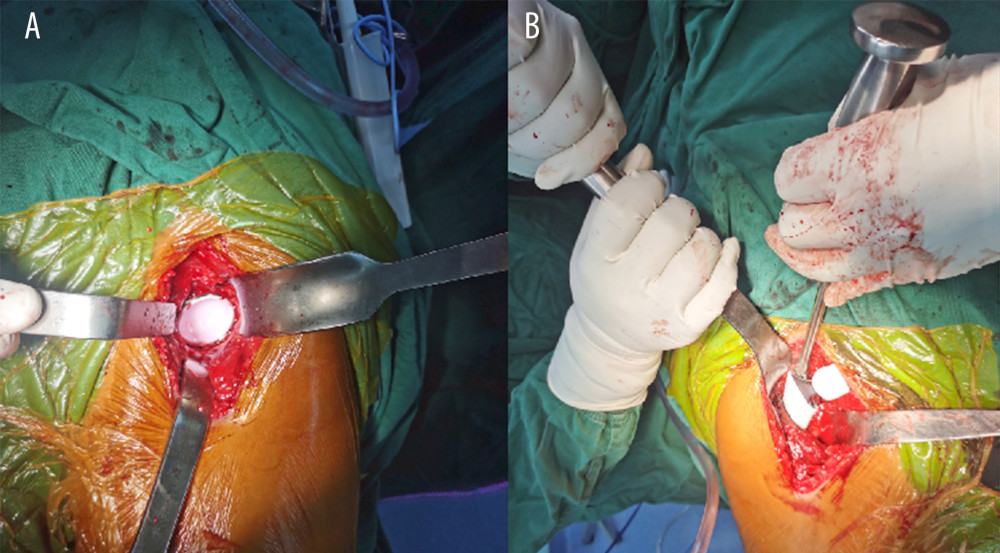 Figure 1. (A, B) Acetabular and femoral stem prostheses during DAA.
Figure 1. (A, B) Acetabular and femoral stem prostheses during DAA.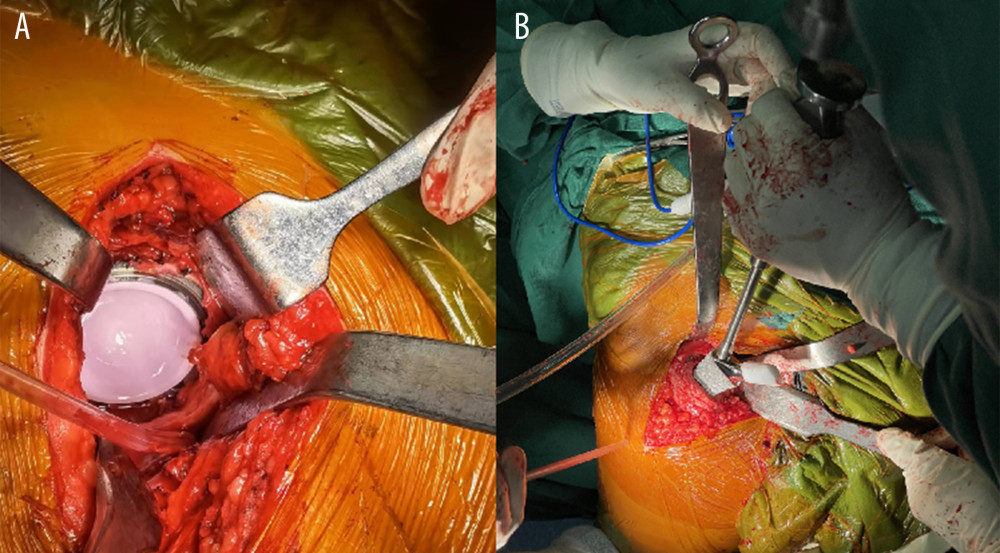 Figure 2. (A, B) Acetabular and femoral stem prosthesis during PLA.
Figure 2. (A, B) Acetabular and femoral stem prosthesis during PLA.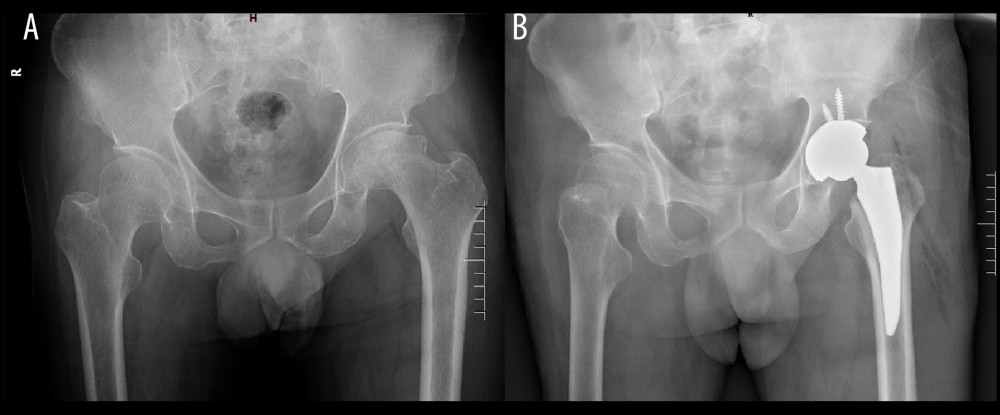 Figure 3. (A, B) Preoperative and postoperative anteroposterior X-rays of patients with DAA.
Figure 3. (A, B) Preoperative and postoperative anteroposterior X-rays of patients with DAA.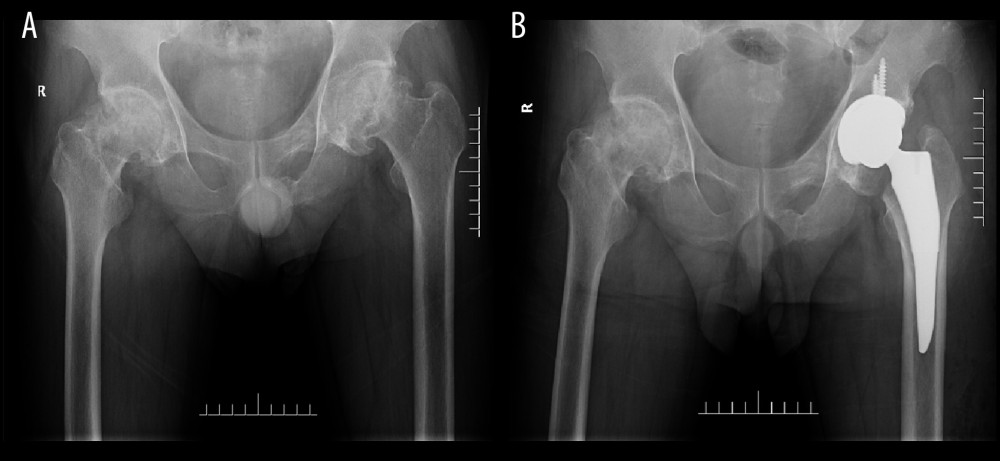 Figure 4. (A, B) Preoperative and postoperative anteroposterior X-rays of patients with PLA.
Figure 4. (A, B) Preoperative and postoperative anteroposterior X-rays of patients with PLA. Tables
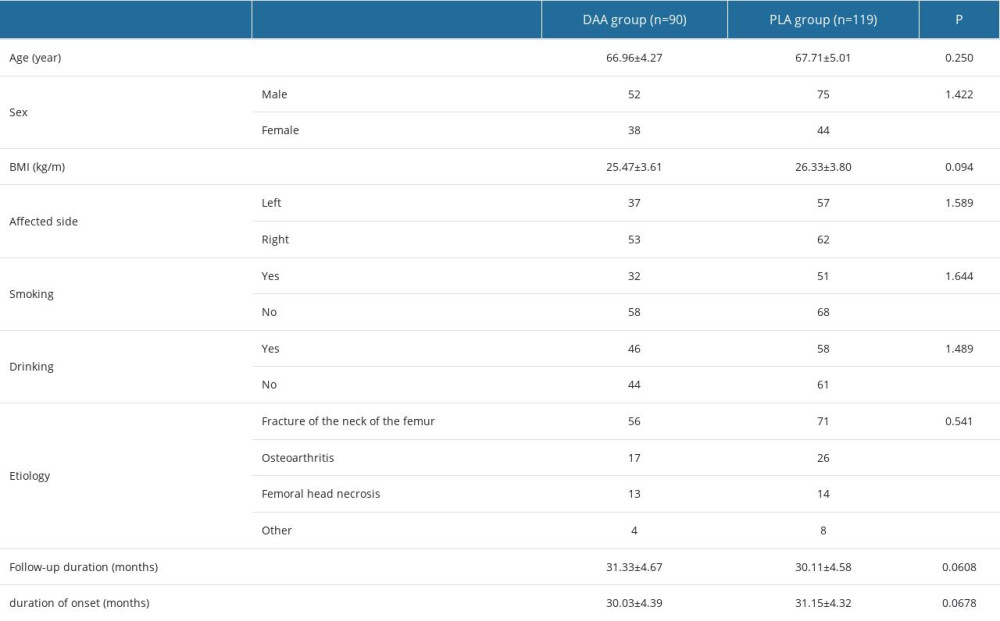 Table 1. Baseline patient profiles.
Table 1. Baseline patient profiles.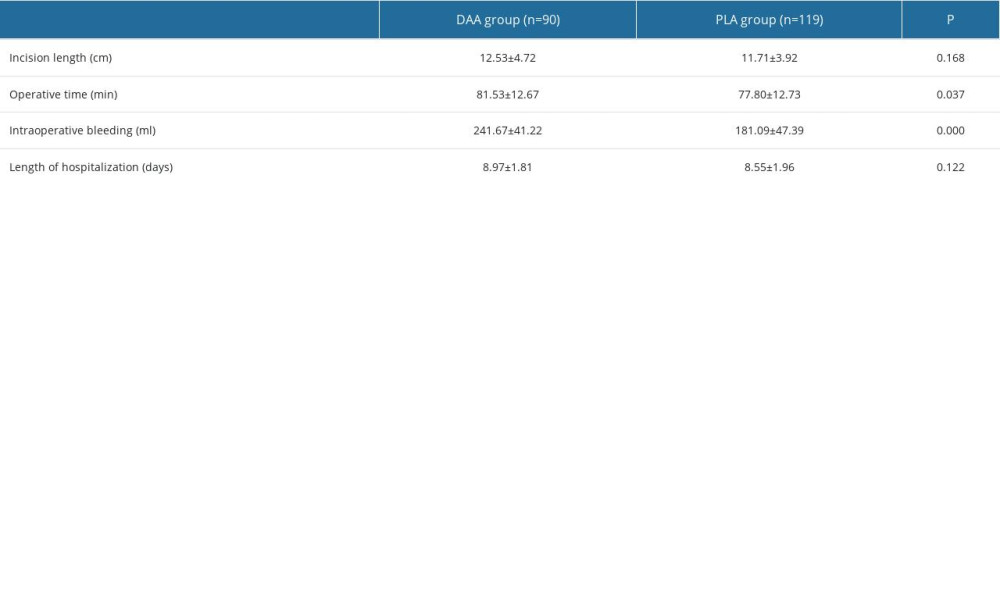 Table 2. Surgical outcomes.
Table 2. Surgical outcomes.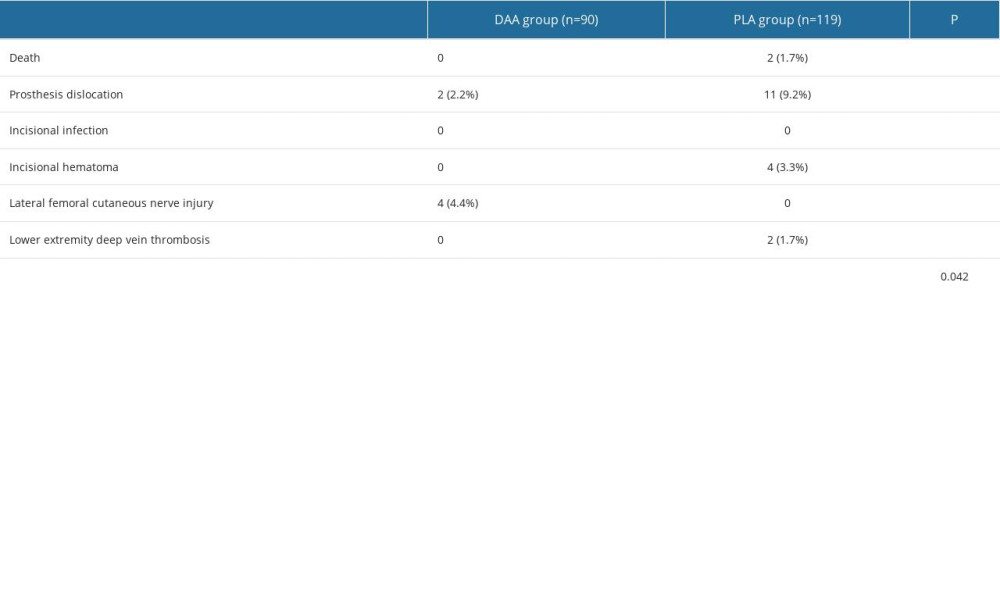 Table 3. Complications [n(%)].
Table 3. Complications [n(%)].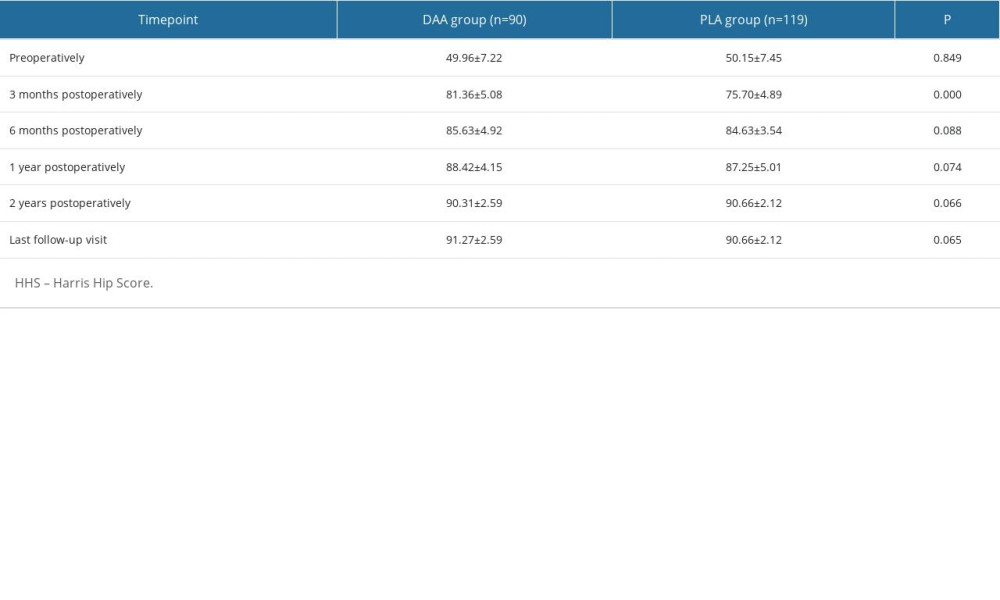 Table 4. HHS scores.
Table 4. HHS scores. Table 5. WOMAC scores.
Table 5. WOMAC scores.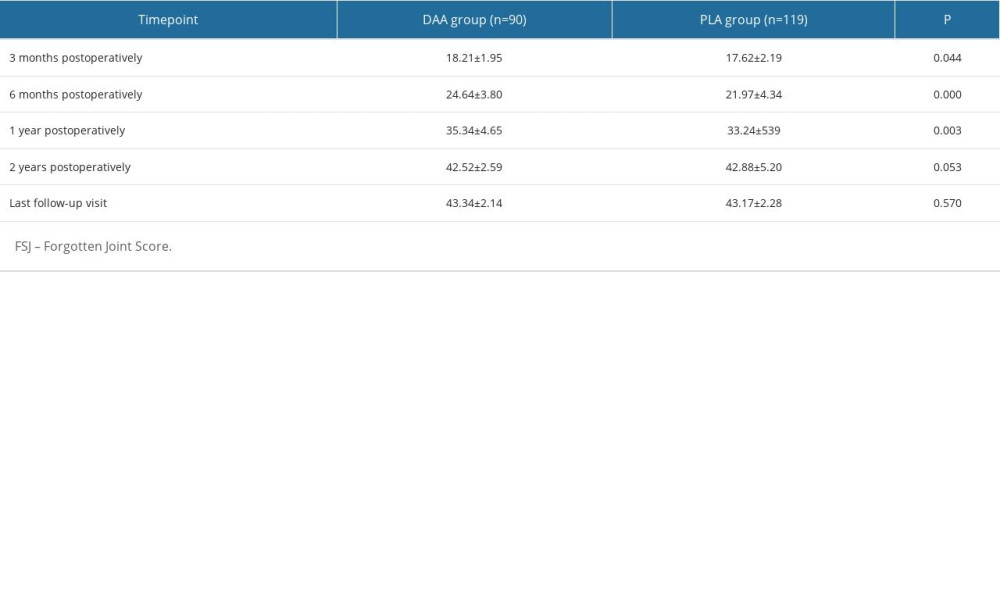 Table 6. FJS scores.
Table 6. FJS scores.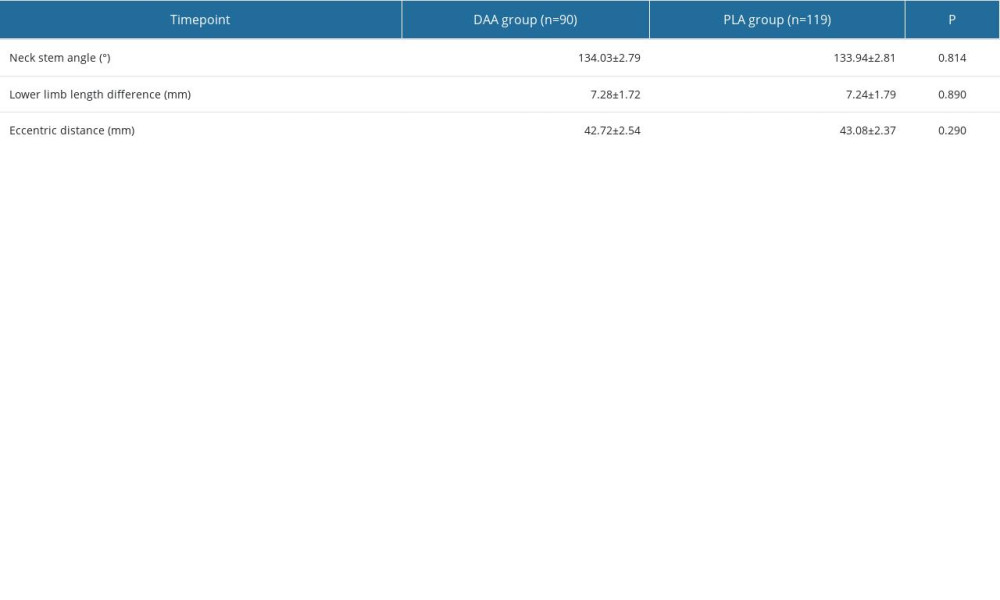 Table 7. Radiological indices of prosthesis position in both groups.
Table 7. Radiological indices of prosthesis position in both groups.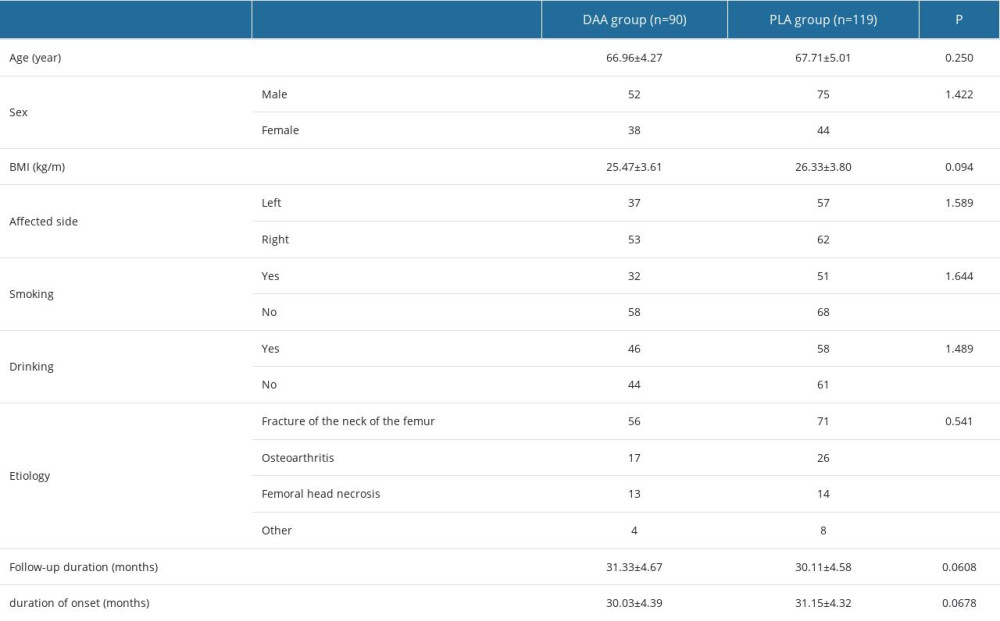 Table 1. Baseline patient profiles.
Table 1. Baseline patient profiles.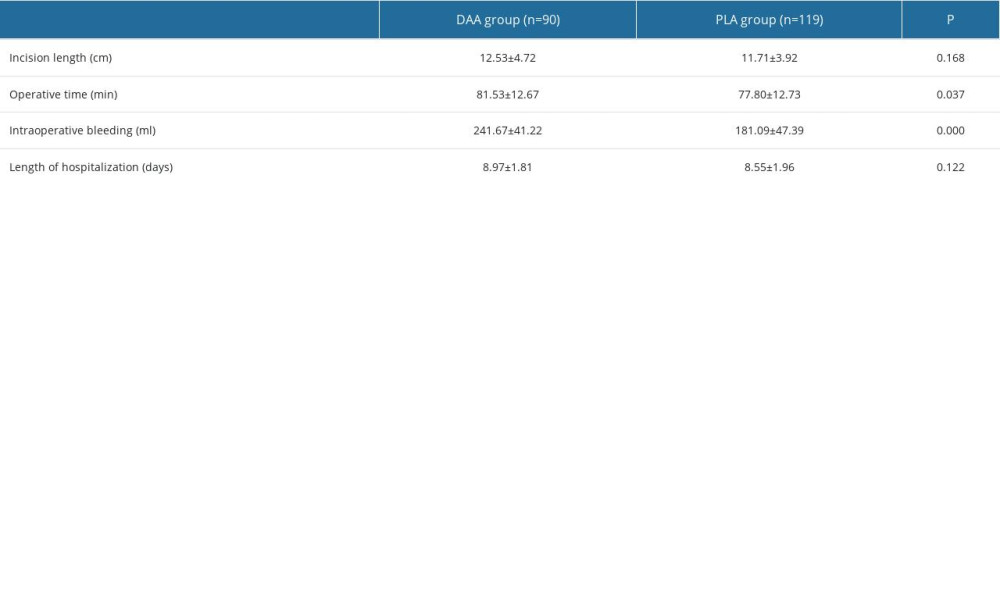 Table 2. Surgical outcomes.
Table 2. Surgical outcomes.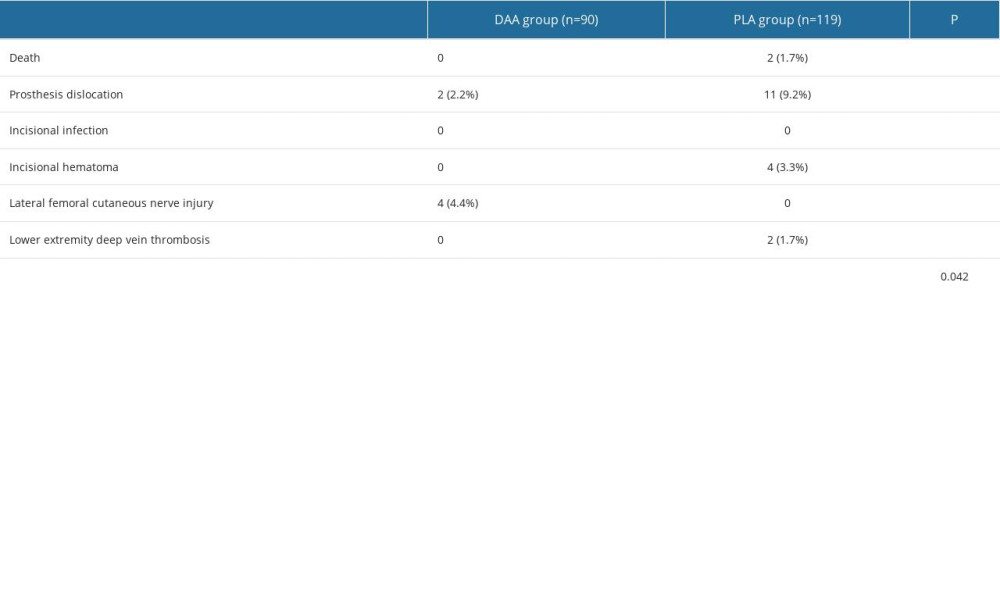 Table 3. Complications [n(%)].
Table 3. Complications [n(%)].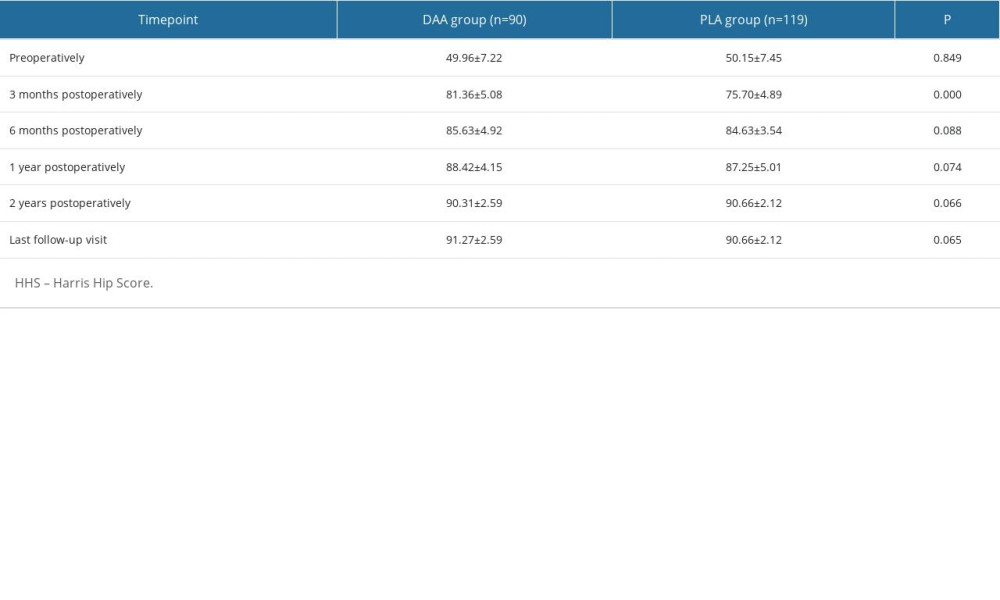 Table 4. HHS scores.
Table 4. HHS scores. Table 5. WOMAC scores.
Table 5. WOMAC scores.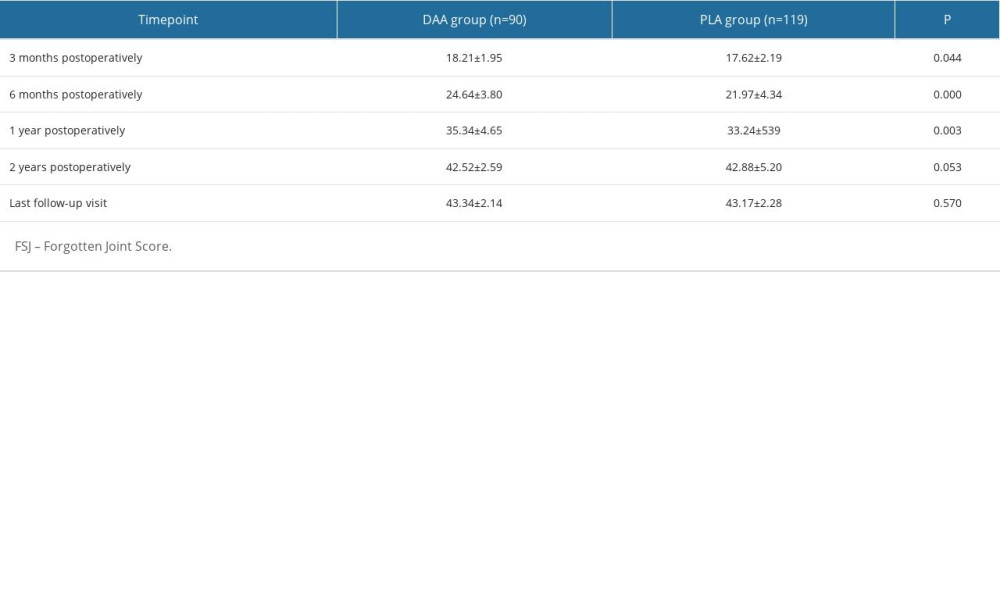 Table 6. FJS scores.
Table 6. FJS scores.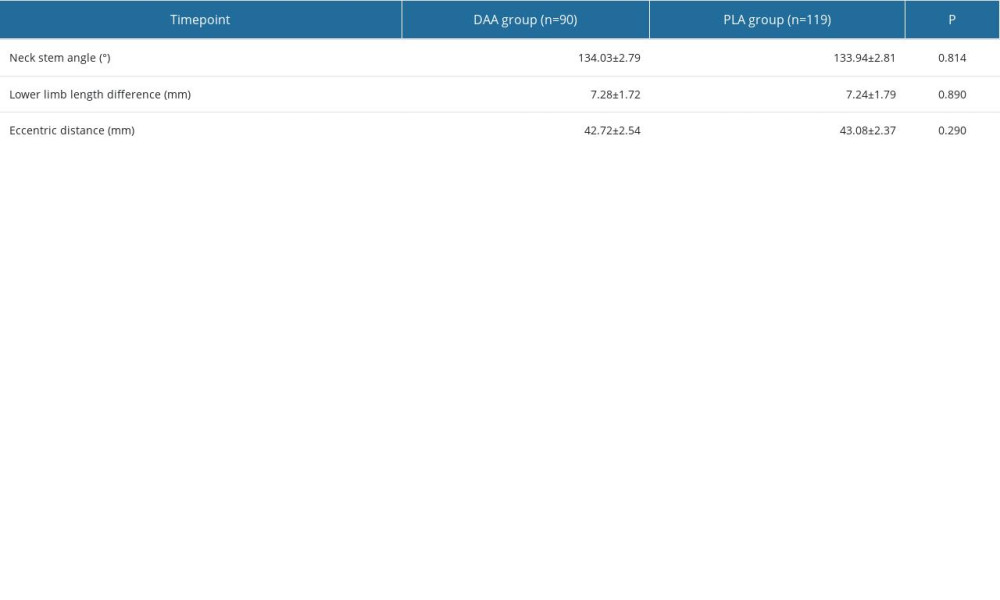 Table 7. Radiological indices of prosthesis position in both groups.
Table 7. Radiological indices of prosthesis position in both groups. In Press
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








