18 June 2023: Clinical Research
Lamina Abrasion Caused by High-Speed Drill in Unilateral Door Cervical Laminoplasty: A Clinical Investigation
Jiwei Zou1BCEF, Shuyong Fan1BCE, Xingxing Chen2BCD, Zhibin Wu3CDEF, Yongfeng Chen1ABCE*DOI: 10.12659/MSM.939939
Med Sci Monit 2023; 29:e939939
Abstract
BACKGROUND: The association of laminar opening extent (LOE) with sagittal canal diameter (SCD) and the cross-sectional area (CSA) in unilateral door cervical laminoplasty (UDCL) was previously analyzed. However, the lamina abrasion has been neglected, which could lead to unreliable results. The present study aims to develop the concept of effective laminar opening extent (ELOE) with consideration of the lamina abrasion and to analyze the relationships between ELOE and SCD as well as the CSA of the spinal canal.
MATERIAL AND METHODS: A total of 138 patients treated by UDCL were included. Pre- and postoperative SCDs and CSAs and cervical Japanese Orthopaedic Association (JOA) scores were compared to verify the effectiveness of the surgery. Linear and curvilinear regression models were used to assess the association between postoperative SCD/CSA increases and ELOE.
RESULTS: All surgeries were successfully performed. A total of 602 mini-plates were used, and 12-mm mini-plates was the most often used (n=402, 66.78%), while 16-mm were used the least (n=25, 4.15%). The SCDs, CSAs, and JOA scores were increased significantly after surgery (P<0.01). There was a strong linear correlation between the postoperative SCD/CSA increase and ELOE (SCD: R²>0.939, P<0.01; CSA: R²>0.938, P<0.01).
CONCLUSIONS: This study developed the concept of ELOE considering the lamina abrasion in UDCL. There was a strong linear correlation between ELOE and the postoperative SCD/CSA increase, which might enable the selection of optimal mini-plate size.
Keywords: Cervical Cord, Laminoplasty, Spine, Humans, Orthopedics, Neck, Postoperative Period, Soft Tissue Injuries
Background
Unilateral door cervical laminoplasty (UDCL) is a widely accepted treatment for severe multisegmented cervical spinal stenosis, and mini-plate fixation is currently recognized and used in UDCL [1,2]. Excellent biocompatibility, biomechanical performance, and significant treatment effect have been proved by finite element analysis [3] and many clinical studies [4,5].
During UDCL, the increases in sagittal canal diameter (SCD) and the cross-sectional area (CSA) of the spinal canal were determined by laminar opening extent (LOE), showing an insufficient LOE would lead to insufficient decompression of the spinal cord, while an excessive LOE is a risk factor for complications such as postoperative C5 palsy [6,7]. Moreover, according to LOE, a suitable size of mini-plate should be selected, which is closely related to the stability of the reconstructed cervical spine based on finite element analysis [8]. Therefore, an appropriate LOE as well as a suitable mini-plate size is particularly important for desirable outcomes.
Numerous studies continued to try to improve UDCL, and assessed the association of LOE with SCD and CSA to provide assistance for surgery; however, these findings were too limited to be widely adopted in clinical practice [9,10]. Moreover, the lamina abrasion caused by high-speed drill in UDCL has been neglected in these reports, which could lead to unreliable results [11–13]. The present study aims to develop the concept of effective laminar opening extent (ELOE with consideration of the lamina abrasion extracted by the drill bit in UDCL, and the relationships between ELOE and the SCD as well as the CSA of the spinal canal were analyzed. The results could provide references for the selection of optimally-sized mini-plates prior to surgery and estimate the SCD/CSA increase after surgery, thus further improving the effectiveness and reliability of UDCL.
Material and Methods
SUBJECTS:
We included patients who were previously diagnosed as having cervical spondylosis myelopathy and ossification of the posterior longitudinal ligament, and radiographically confirmed by a spine expert in our institution. The inclusion criteria were as follows: (a) age 18–85 years; (b) magnetic resonance imaging (MRI) showed spinal stenosis or cervical disc herniation involving ≥3 levels and spinal cord compression; (c) patients who have received conservative therapy for at least 3 months before surgery, but without satisfactory effect. The exclusion criteria were as follows: (a) patients with cervical trauma history, cervical deformity, or cervical tumors; (b) patients who underwent posterior-anterior cervical surgery or revision surgery. All participants were instructed to fill out the cervical Japanese Orthopaedic Association (JOA) questionnaire before and after surgery. The present study was approved in advance by the Ethics Committee of our institution (No. XJCR2019-19), and written informed consent was obtained from all participants and their families.
SURGICAL PROCEDURES:
A standard posterior midline approach was performed in each patient. The paravertebral muscles were detached, then we removed the spinous processes. To expand the central spinal canal and relieve compression, the UDCL was performed using a high-speed 2-mm drill according to the modified Hirabayashi method [14] between C3–7 vertebrae. For all patients, we used the left side as the opening side and the lamina was completely cut by the drill; subsequently, the left side was partially cut and formed a hinge. After the left side-opening procedure, the Centerpiece mini-plates (Medtronic, Inc., USA) with mini-screws were used for internal fixation at the opened space. All surgeries were carried out by a same surgery team.
RADIOLOGY:
Computed tomography (CT) scans and three-dimensional reconstruction ranged from C1 to C7 were performed on all subjects preoperatively and 1 week after surgery, using a GE Light Speed 64-slice VCT instrument (GE Healthcare, USA). CT parameters as follows: slice thickness, 0.625 mm; tube current, 220 mA; tube voltage, 120 kV; reconstruction interval, 0.625 mm; pitch, 0.925; gantry rotation time, 0.5 s; matrix, 512×512; FOV, 200×200 mm. Axical CT sections at each pedicle level were obtained for assessment to keep the same measurement position before and after surgery.
The CSA and SCD were assessed using the Picture Archiving and Communication System (PACS) (Carestream Vue; Carestream Health, Rochester, NY, USA), as shown in Figure 1, in which the CSA of the spinal canal was measured using an imaginary red line encircling the area with the intervertebral disc or the posterior edge of the vertebral body as the anterior boundary, the anterior edge of the vertebral arch as the posterior boundary, and the inner edge of the pedicle as the left and right borders. The SCD was measured using an imaginary yellow line connecting the Hridayesh midpoint of the posterior edge of the vertebral body to the top of the vertebral arch. Once the measurement area and distance were manually defined, the software automatically generated the measurement results. All the measurements (accuracy, 0.01 mm2 and 0.01 mm) were performed by 3 radiologists who were unaware of our study design; subsequently, these measurements were averaged for statistical analysis.
During the process of lamina opening, some vertebral laminas were inevitably worn off by the high-speed drill (Figure 2), and the sizes of lamina abrasion corresponding to the drill bit’s diameter (d). We set the mini-plate size to a, then the ELOE equals to the difference value between a and d.
STATISTICAL ANALYSIS:
The statistical analysis was conducted on SPSS software v24.0 (SPSS, Inc., Chicago, IL, USA). All variables were tested by one-sample Kolmogorov-Smirnov test and presented as the mean±SD at a significance level of
Results
GENERAL INFORMATION:
From March 2020 to December 2021, a total of 138 patients (76 males and 62 females) treated by UDCL in our institution were included, aged 38 to 83 (58.3±11.3) years, course of disease 4 to 48 (7.5±5.8) months, and the average duration of follow-up was 18.62±5.88 months. Pathologies of the patients included cervical spondylosis myelopathy (n=92) and ossification of the posterior longitudinal ligament (n=46). The presenting symptoms were: paresthesia in the extremities (n=92), intermittent gait incoordination (n=63), wide-based stance (n=52), radicular pain syndrome (n=43), and clumsiness of fine movements (n=26). All UDCL surgeries were successfully performed, the average operating time was 192.23±75.34 min, and blood loss was 182.36±52.37 ml.
ANALYSIS OF THE CERVICAL VERTEBRAE INVOLVED AND THE MINI-PLATE SIZE USED IN IHE SURGERY:
The cervical vertebrae concerned by UDCL were: C3–C7 (n=70, 50.72%), C3–C6 (n=36, 26.09%), C4–C7 (n=12, 8.70%), C4–C6 (n=9, 6.52%), C3–C5 (n=6, 4.35%), and C5–C7 (n=5, 3.62%), and all operations have involved C5. The sizes of the mini-plates used in the operation were: 12 mm (n=402, 66.78%), 14 mm (n=139, 23.09%), 10 mm (n=36, 5.98%), and 16 mm (n=25, 4.15%) (Figure 3). Among the 602 mini-plates used in surgeries, the 12-mm mini-plate was the most often used, while 16-mm plates were least used.
COMPARISON BETWEEN PREOPERATIVE AND POSTOPERATIVE SCD/CSA AND JOA SCORES:
The SCDs (Table 1) and CSAs (Table 2) were increased significantly after surgery in all cases (P<0.01). The JOA scores before and after surgery were 3.22±2.18 and 11.35±4.36, respectively, the improvement rate was 57.68±10.39%, and the JOA scores were significantly increased after surgery (P<0.01).
ANALYSIS OF THE RELATIONSHIP BETWEEN POSTOPERATIVE SCD/CSA AND ELOE:
A strong linear correlation between the ELOE and postoperative SCD increase was found by regression analysis (R2>0.939, P<0.01). The overall calculated postoperative SCD increase was approximately 0.519 times that of ELOE (Table 3).
In addition, the results of regression analysis indicated a strong linear correlation between the postoperative CSA increase and ELOE (CSA: R2>0.938, P<0.01). The overall calculated postoperative CSA increase was approximately 7.727 times that of ELOE (Table 4).
Discussion
After more than 40 years of development, the current trend of laminoplasty is developing toward the goal of muscle preservation and minimum tissue damage [14]. Given this, UDCL is superior to classic laminoplasty due to the biomechanical effect of the posterior musculature reconstruction, with a retained postoperative range of motion and loading response levels of the functional spinal units [3,8]. Several studies have confirmed that the use of the Centerpiece mini-plate can effectively avoid reclosure of the lamina after UDCL and provide adequate protection for the dural sac in the spinal canal, as well as avoid postoperative scar hyperplasia [1,15]. Finite element analysis showed better stability and more motion-sparing using the mini-plate in UDCL [8]. Either insufficient or excessive LOE can result in undesirable treatment outcomes, which is closely related to the mini-plate size [6,7]. Moreover, improper mini-plate used during surgery can also lead to poor biomechanical performance [16]. Therefore, selecting an optimal mini-plate size before surgery is rather important. However, due to the lack of a unified standard, most surgeons often select a mini-plate size based on clinical experience, which increases the possibility of poor treatment outcomes.
Previous studies have confirmed that the recovery of postoperative neurological function is associated with SCD and CSA [17,18]. In addition, for alleviating spinal cord compression, postoperative SCD increase appears to be more important than CSA increase [11]. Lubelski et al [19] considered that the probability of postoperative C5 palsy could decrease by 69% with every 1-mm increase in SCD. Since LOE determines postoperative SCD and CSA, the association between LOE and SCD/CSA has been investigated by numerous clinical studies. Itoh et al [20] suggested that the optimal SCD increase is 4.1 mm and the corresponding LOE is 8 mm. Another study suggested that the optimal SCD increase after UDCL is 4–5 mm [13]. Although the size of the mini-plate plays an important role in LOE, these 2 sizes are not exactly equal. It is worth noting that the above-mentioned related studies ignore the lamina abrasion extracted by drill during the operation, which may lead to unreliable results [1,15]. In addition, due to the irregular geometric structure of the cervical spinal canal, using SCD alone is still insufficient to predict and evaluate the treatment outcome, and postoperative CSA increase is also an important indicator [21]. Relevant research results are complex and limited to clinical application. The present study aimed to develop the concept of ELOE with consideration of the lamina abrasion extracted by the drill (Figure 2), in order to analyze the relationship between LOE and SCD/CSA more accurately.
All surgeries were successfully performed, as verified by a significant increase in SCD, CSA, and JOA scores after surgery. The results of regression analysis indicated a strong linear correlation between the ELOE and postoperative SCD increase, as well as postoperative CSA increase and ELOE. Although there was a linear correlation in each segment, for simplicity’s sake, the equation of C3–7 is recommended for use in clinical practice. According to the equation of C3–7, for each 1 mm increase of ELOE, the SCD would increase by about 0.5 mm. If a 12-mm mini-plate is used during the operation and the diameter of the drill is 2 mm, the ELOE is 10 mm, and the postoperative SCD increase is 5 mm. In the same way, the increase in postoperative CSA could also be estimated according to the size of mini-plate and the diameter of the drill, which provides an effective reference for the selection of intraoperative mini-plate. No standard regarding the most optimal postoperative SCD and CSA increase for UDCL has been proposed previously [9,10], and the finding of the present study only provide a prediction method based on mini-plate size and diameter of the drill, which should be applied flexibly in clinical practice.
It is also found that all operations in this study involved C5, and whether this is related to the occurrence of postoperative C5 palsy warrants further investigate. We performed a statistical analysis of the mini-plate sizes used during surgery, showing that 12-mm mini-plates were most often used (66.78%), while 10-mm and 16-mm mini-plates were least used (5.98% and 4.15%, respectively). Considering that insufficient or excessive LOE may lead to poor treatment outcomes, 10-mm and 16-mm mini-plates should be carefully selected in UDCL.
It is worth noting that there are some limitations in the present study. The lateral hinge location of the lamina is usually on the medial edge of the facet joint [1,6,14], but due to anatomical differences, even when the operations are conducted by a single surgical team, it is still difficult to identify the same hinge location. Besides, due to differences in quality of bone among different patients, the sizes of lamina abrasion extracted in UDCL could also be influenced; therefore, for patients with severe osteoporosis, careful consideration is needed when applying the results of this study. It should also be pointed out that, during the operation, the drill is expected to be perpendicular to the lamina, but this is commonly ignored in clinical practice, causing the lamina abrasion to be slightly larger than the diameter of the drill. To minimize this error, the surgical team should strictly adhere to operating standards to reduce lamina abrasion. Last but not the least, precise implantation of mini-plates is also important; if not, the actual LOE would be larger than the calculated value; therefore, skilled and careful manipulation is also required.
Conclusions
The present study developed the concept of ELOE considering the lamina abrasion in UDCL. A strong linear correlation was found between ELOE and the postoperative SCD/CSA increase. The present study provides a non-invasively tool for the optimal mini-plate selection prior to surgery, reducing the risk of adverse events such as mini-plate deformation or misplacement, and further improving the effectiveness and reliability of UDCL.
Figures
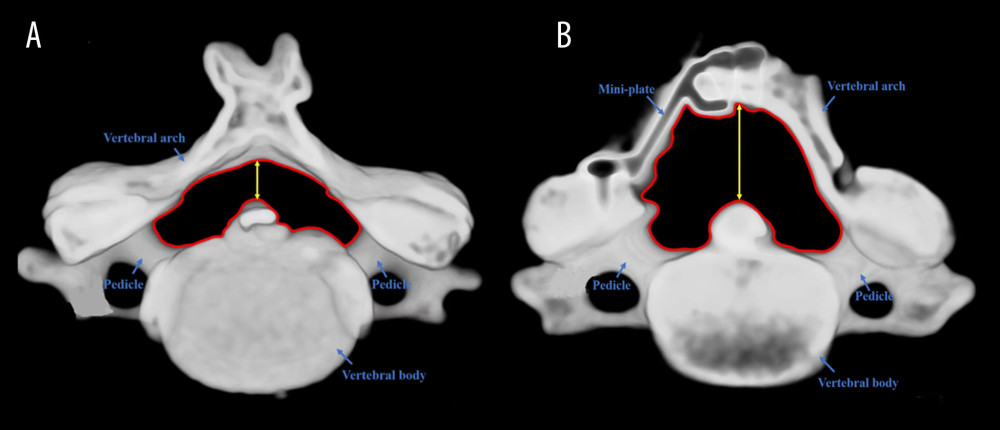 Figure 1. Three-dimensional reconstruction of a patient’s cervical spine(A) Preoperative; (B) Postoperative. Red lines represent the measurement of cross-sectional area, yellow lines represent the measurement of sagittal canal diameter.
Figure 1. Three-dimensional reconstruction of a patient’s cervical spine(A) Preoperative; (B) Postoperative. Red lines represent the measurement of cross-sectional area, yellow lines represent the measurement of sagittal canal diameter. 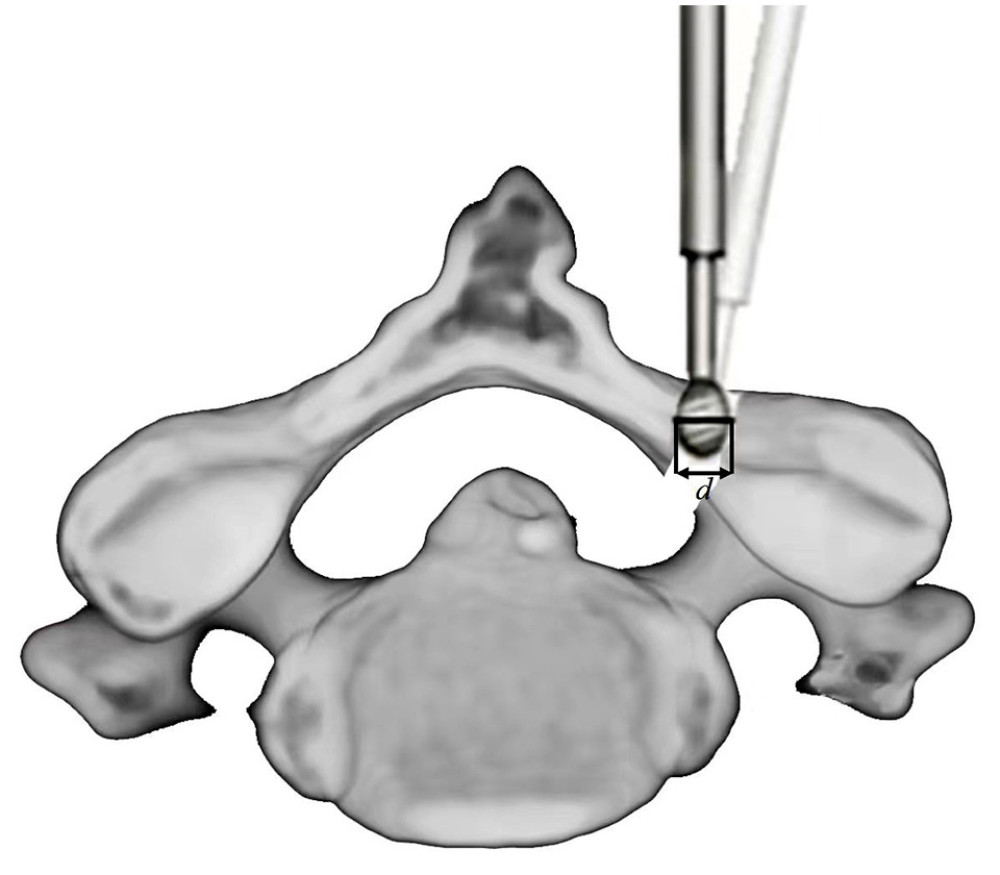 Figure 2. Preparation of the lamina opening with a high-speed drill in unilateral door cervical laminoplastyDuring the surgery, lamina tissues were partly extracted, the sizes of lamina abrasion corresponding to the drill bit’s diameter (d).
Figure 2. Preparation of the lamina opening with a high-speed drill in unilateral door cervical laminoplastyDuring the surgery, lamina tissues were partly extracted, the sizes of lamina abrasion corresponding to the drill bit’s diameter (d). 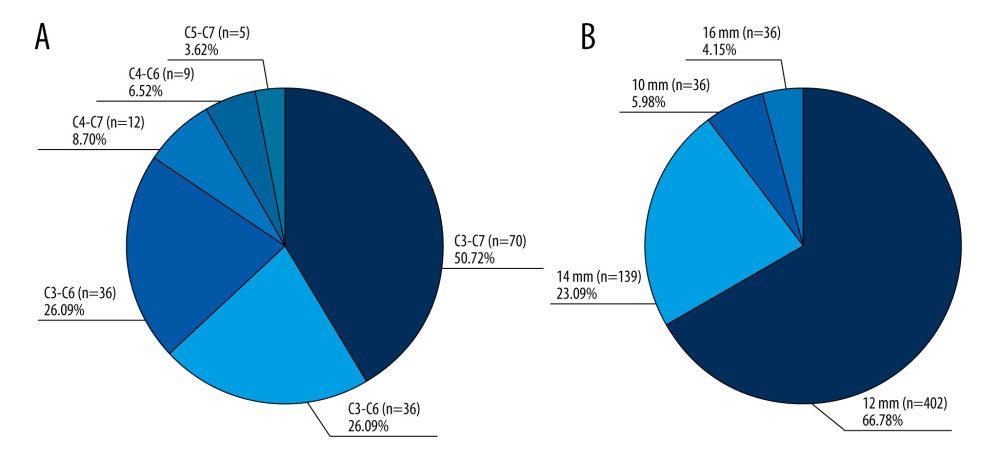 Figure 3. Analysis of the cervical vertebrae involved and the mini-plate size used in the Unilateral door cervical laminoplasty(A) All cervical vertebrae involved in surgery; (B) Sizes of mini-plates used in surgery.
Figure 3. Analysis of the cervical vertebrae involved and the mini-plate size used in the Unilateral door cervical laminoplasty(A) All cervical vertebrae involved in surgery; (B) Sizes of mini-plates used in surgery. Tables
Table 1. Pre- and postoperative SCD of patients who underwent unilateral door cervical laminoplasty (x±s, mm).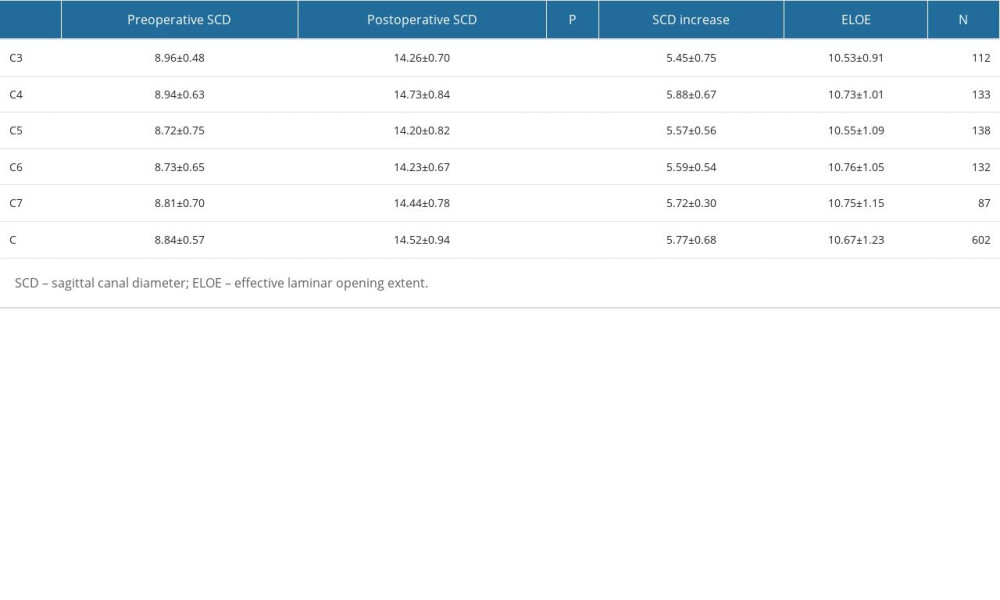 Table 2. Pre- and postoperative CSA of patients underwent unilateral door cervical laminoplasty (x±s, mm2).
Table 2. Pre- and postoperative CSA of patients underwent unilateral door cervical laminoplasty (x±s, mm2).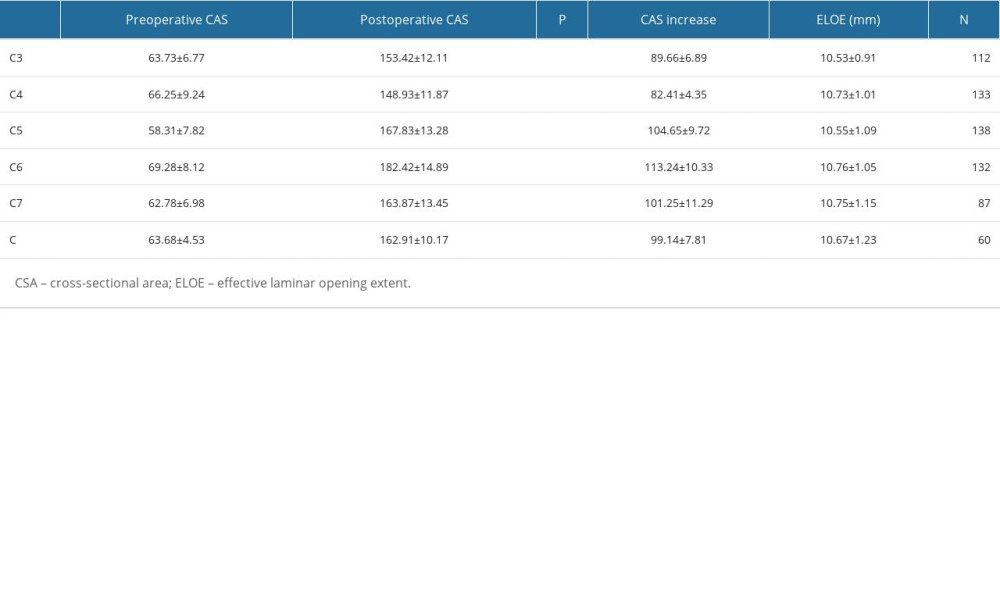 Table 3. Linear regression of effective laminar opening extent against the postoperative sagittal canal diameter increase for unilateral door cervical laminoplasty.
Table 3. Linear regression of effective laminar opening extent against the postoperative sagittal canal diameter increase for unilateral door cervical laminoplasty.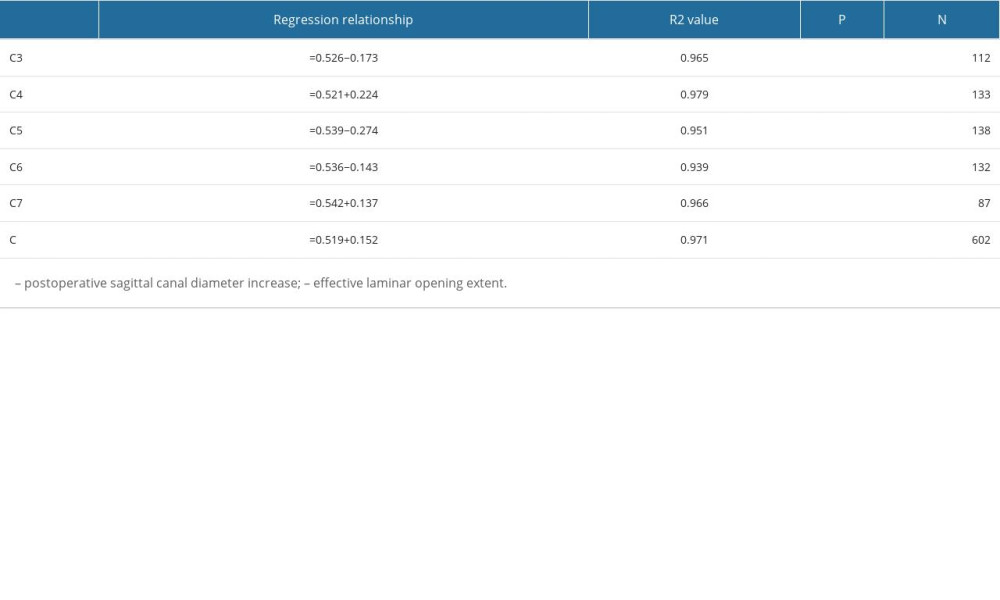 Table 4. Linear regression of effective laminar opening extent against the postoperative cross-sectional area increase for unilateral door cervical laminoplasty.
Table 4. Linear regression of effective laminar opening extent against the postoperative cross-sectional area increase for unilateral door cervical laminoplasty.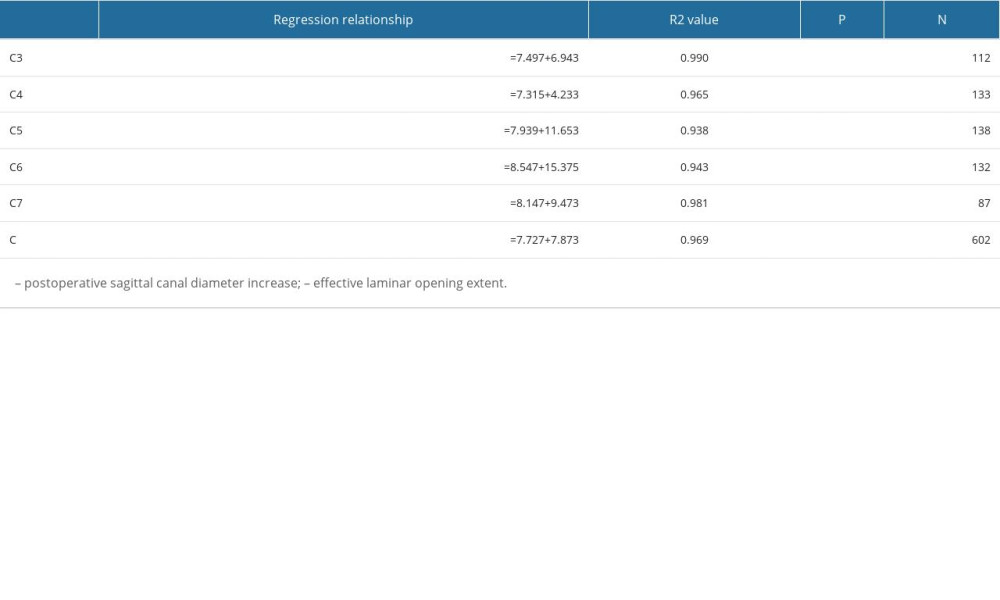
References
1. Kothe R, Schmeiser G, Papavero L, Open-door laminoplasty: What can the unilateral approach offer?: Oper Orthop Traumatol, 2018; 30(1); 3-12
2. Cho SK, Kim JS, Overley SC, Cervical laminoplasty: Indications, surgical considerations, and clinical outcomes: J Am Acad Orthop Surg, 2018; 26; e142-e52
3. Xu H, Wu J, Xie H, Biomechanical behaviour of tension-band-reconstruction titanium plate in open-door laminoplasty: A study based on finite element analysis: BMC Musculoskelet Disord, 2022; 23(1); 851
4. Hoti YUD, Aziz A, Ishaque K, Clinical outcome of laminoplasty in cervical myelopathy: J Coll Physicians Surg Pak, 2018; 28; 466-69
5. Chen C, Yang C, Yang S, Clinical and radiographic outcomes of modified unilateral open-door laminoplasty with posterior muscle-ligament complex preservation for cervical spondylotic myelopathy: Spine, 2019; 44; 1697-704
6. Weinberg DS, Rhee JM, Cervical laminoplasty: Indication, technique, complications: J Spine Surg, 2020; 6; 290-301
7. Zhu L, Miao Y, Mao Y, Analysis of the risk factors for C5 nerve palsy after cervical posterior open-door laminoplasty for patients with cervical spondylotic myelopathy – from the perspective of cervical sagittal parameters: World Neurosurg, 2022; 165; e169-e74
8. Tadepalli SC, Gandhi AA, Fredericks DC, Cervical laminoplasty construct stability: An experimental and finite element investigation: Iowa Orthop J, 2011; 31; 207-14
9. Hradil J, Horak Z, Henys P, The opening size of the laminoplasty is dependent on the groove size: A numerical study: Clin Biomech (Bristol, Avon), 2021; 89; 105479
10. Gu Z, Zhang A, Shen Y, Relationship between the laminoplasty opening size and the laminoplasty opening angle, increased sagittal canal diameter and the prediction of spinal canal expansion following open-door cervical laminoplasty: Eur Spine J, 2015; 24; 1613-20
11. Yang XJ, Tian RJ, Su X, Relationship of actual laminoplasty opening size and increase of the cross-sectional area based on single-door cervical laminoplasy: Medicine, 2018; 97; e0216
12. Shrestha D, Jun M, Jidong Z, Effect of titanium miniplate fixation on hinge fracture and hinge fracture displacement following cervical open-door laminoplasty: Int J Spine Surg, 2020; 14; 462-75
13. Wang H, Zhang L, Expansion of spinal canal with lift-open laminoplasty: A new method for compression cervical myelopathy: Orthop Surg, 2021; 13; 1673-81
14. Kurokawa R, Kim P, Cervical laminoplasty: The history and the future: Neurol Med Chir (Tokyo), 2015; 55(7); 529-39
15. Zhong H, Xu C, Wang R, Anterior cervical discectomy and fusion, open-door laminoplasty, or laminectomy with fusion: Which is the better treatment for four-level cervical spondylotic myelopathy?: Front Surg, 2023; 9; 1065103
16. Liu FJ, Ding XK, Chai Y, Influence of fixed titanium plate position on the effectiveness of open-door laminoplasty for cervical spondylotic myelopathy: J Orthop Surg Res, 2022; 17(1); 297
17. Wang H, Zhang L, Expansion of spinal canal with lift-open laminoplasty: A new method for compression cervical myelopathy: Orthop Surg, 2021; 13(5); 1673-81
18. Shimizu T, Fujibayashi S, Otsuki B, Residual anterior cord compression after laminoplasty for cervical spondylotic myelopathy: Evaluation of risk factors according to the most severely stenotic vertebral segment: J Neurosurg Spine, 2022; 37(6); 794-801
19. Lubelski D, Derakhshan A, Nowacki AS, Predicting C5 palsy via the use of preoperative anatomic measurements: Spine J, 2014; 14; 1895-901
20. Itoh T, Tsuji H, Technical improvements and results of laminoplasty for compressive myelopathy in the cervical spine: Spine, 1985; 10; 729-36
21. Yang XJ, Sang HX, Liu CX, A new method for calculating the desired laminoplasty opening size based on the target sagittal canal diameter before single-door cervical laminoplasty: Eur Spine J, 2019; 28; 2302-10
Figures
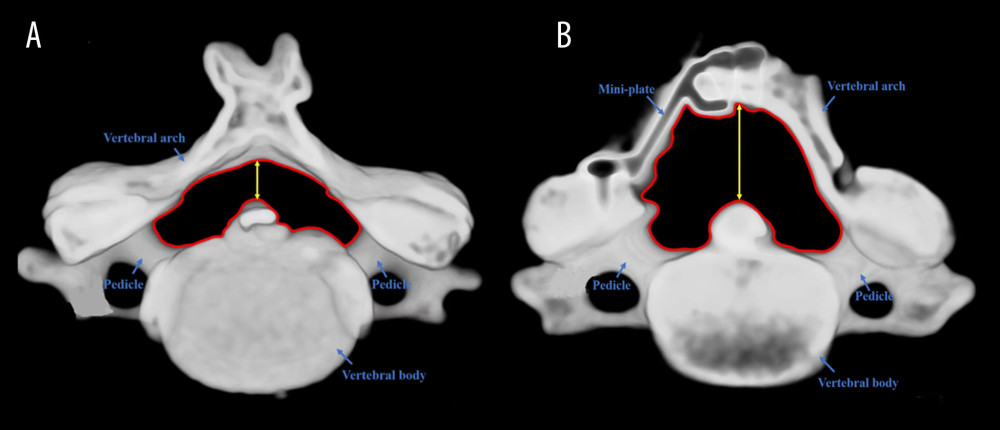 Figure 1. Three-dimensional reconstruction of a patient’s cervical spine(A) Preoperative; (B) Postoperative. Red lines represent the measurement of cross-sectional area, yellow lines represent the measurement of sagittal canal diameter.
Figure 1. Three-dimensional reconstruction of a patient’s cervical spine(A) Preoperative; (B) Postoperative. Red lines represent the measurement of cross-sectional area, yellow lines represent the measurement of sagittal canal diameter.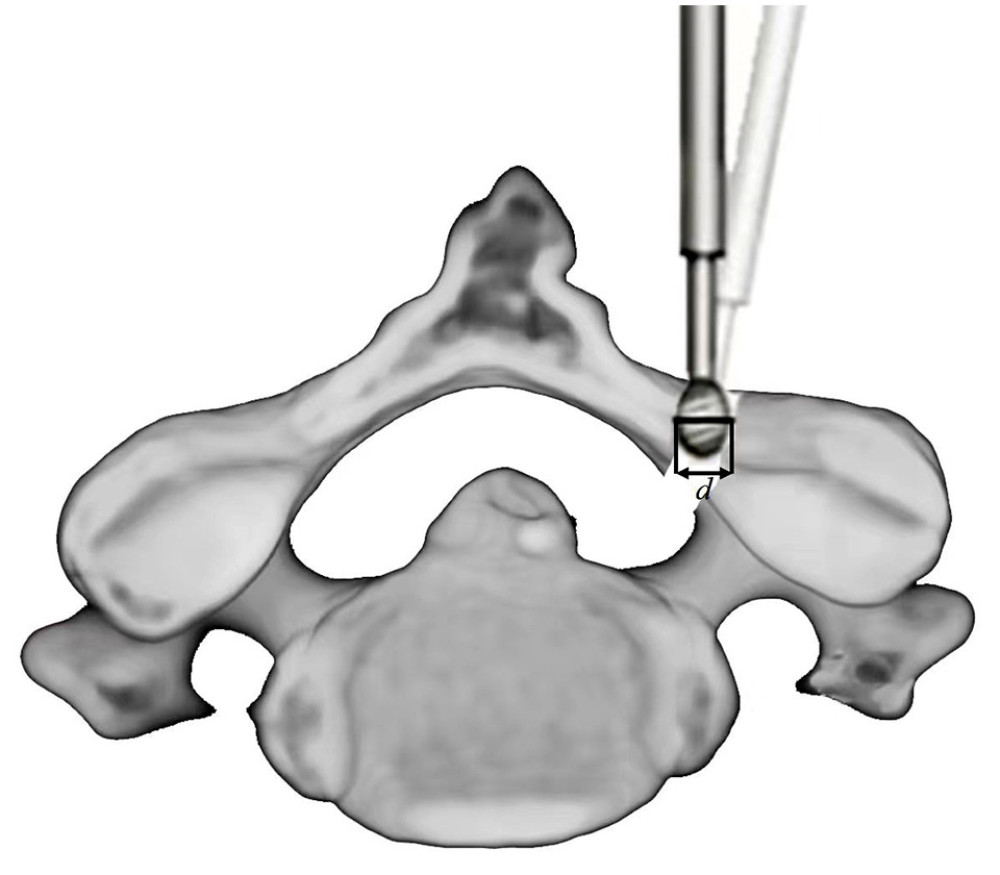 Figure 2. Preparation of the lamina opening with a high-speed drill in unilateral door cervical laminoplastyDuring the surgery, lamina tissues were partly extracted, the sizes of lamina abrasion corresponding to the drill bit’s diameter (d).
Figure 2. Preparation of the lamina opening with a high-speed drill in unilateral door cervical laminoplastyDuring the surgery, lamina tissues were partly extracted, the sizes of lamina abrasion corresponding to the drill bit’s diameter (d).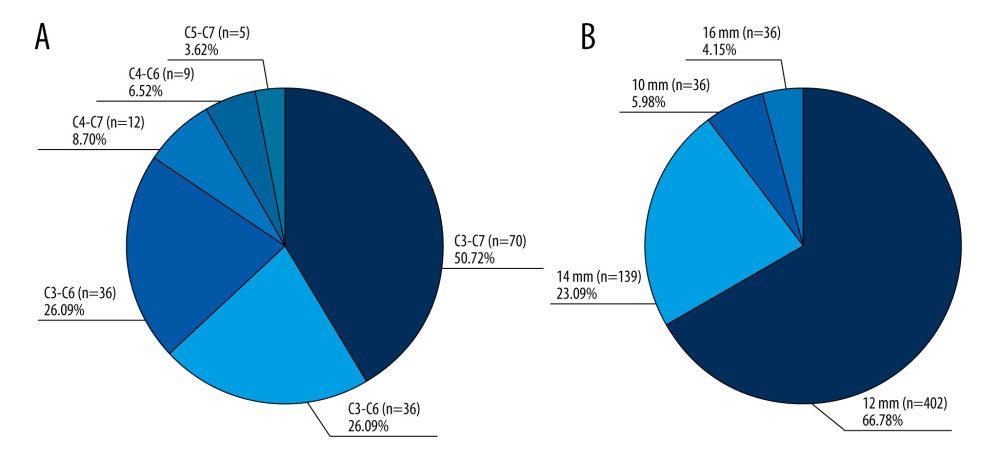 Figure 3. Analysis of the cervical vertebrae involved and the mini-plate size used in the Unilateral door cervical laminoplasty(A) All cervical vertebrae involved in surgery; (B) Sizes of mini-plates used in surgery.
Figure 3. Analysis of the cervical vertebrae involved and the mini-plate size used in the Unilateral door cervical laminoplasty(A) All cervical vertebrae involved in surgery; (B) Sizes of mini-plates used in surgery. Tables
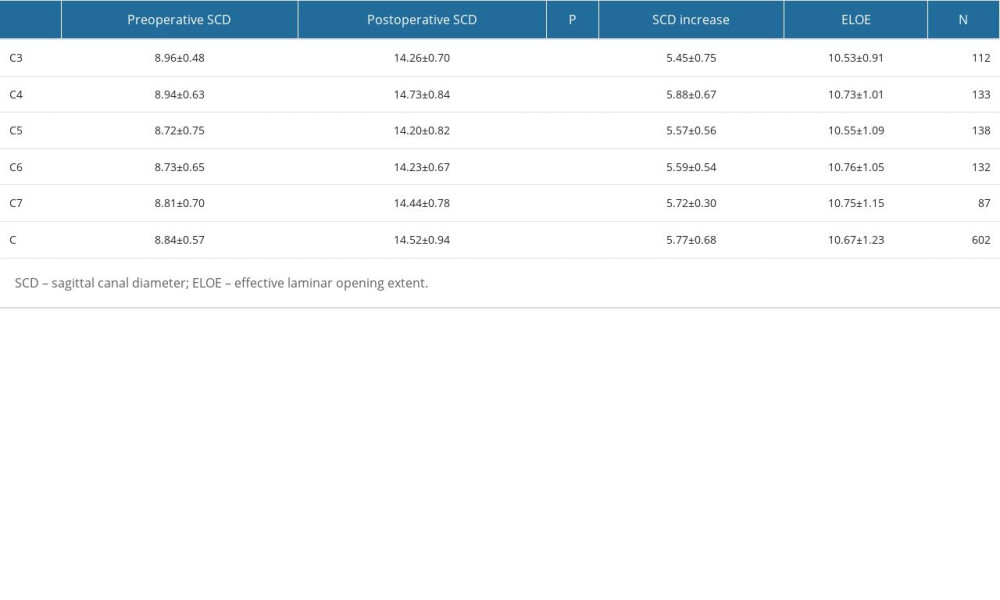 Table 1. Pre- and postoperative SCD of patients who underwent unilateral door cervical laminoplasty (x±s, mm).
Table 1. Pre- and postoperative SCD of patients who underwent unilateral door cervical laminoplasty (x±s, mm).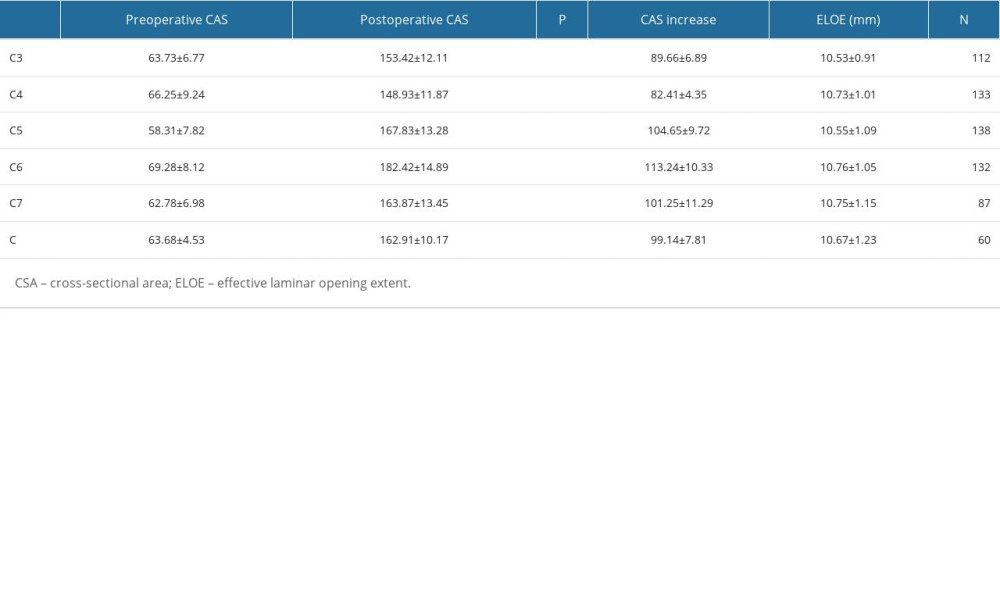 Table 2. Pre- and postoperative CSA of patients underwent unilateral door cervical laminoplasty (x±s, mm2).
Table 2. Pre- and postoperative CSA of patients underwent unilateral door cervical laminoplasty (x±s, mm2).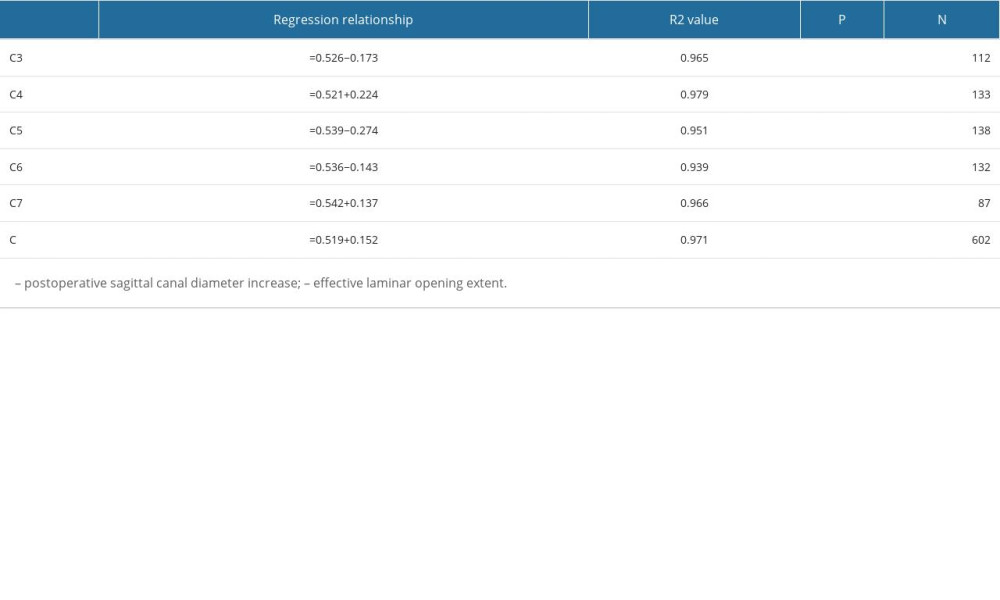 Table 3. Linear regression of effective laminar opening extent against the postoperative sagittal canal diameter increase for unilateral door cervical laminoplasty.
Table 3. Linear regression of effective laminar opening extent against the postoperative sagittal canal diameter increase for unilateral door cervical laminoplasty.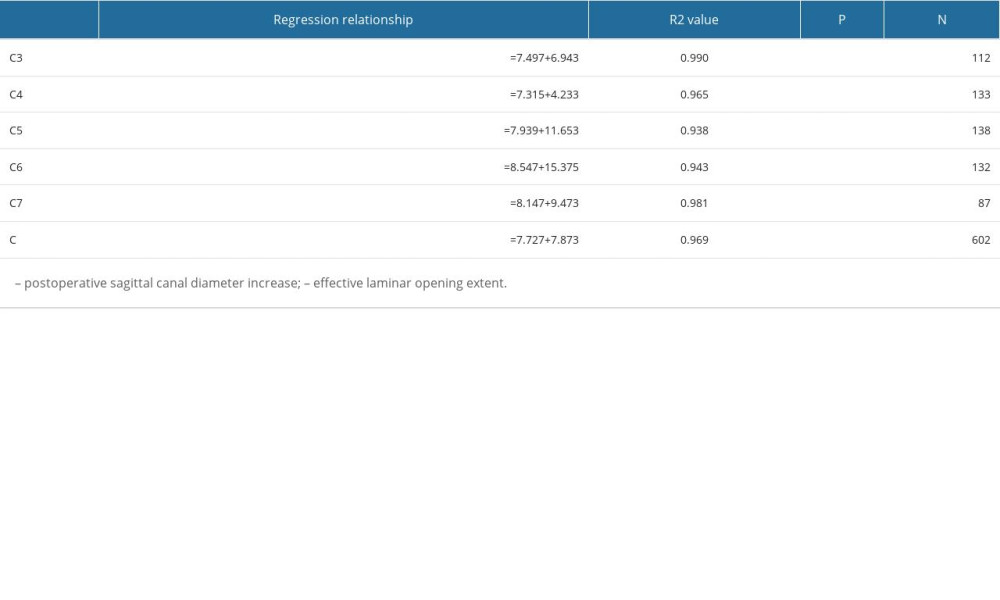 Table 4. Linear regression of effective laminar opening extent against the postoperative cross-sectional area increase for unilateral door cervical laminoplasty.
Table 4. Linear regression of effective laminar opening extent against the postoperative cross-sectional area increase for unilateral door cervical laminoplasty.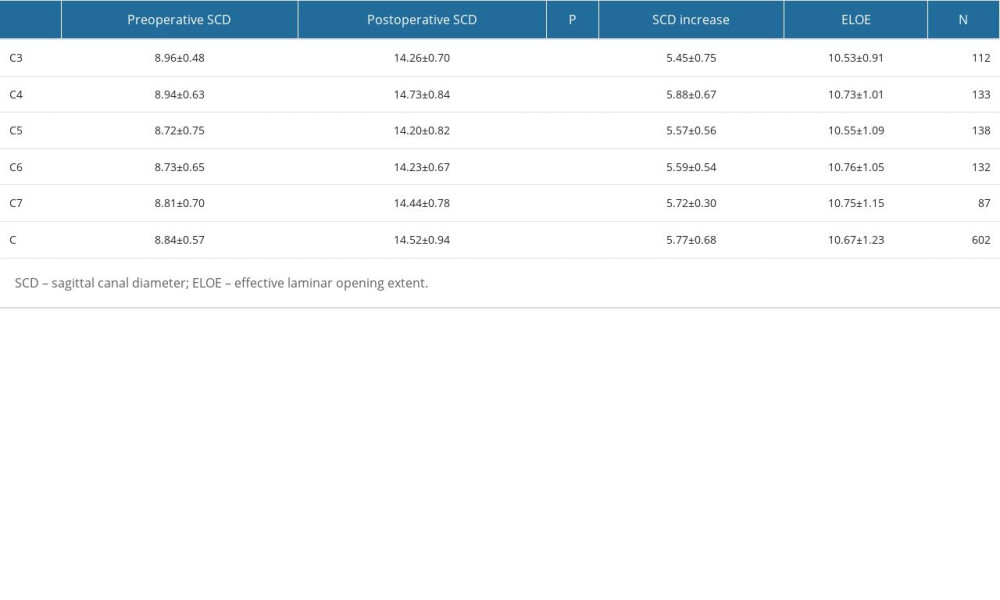 Table 1. Pre- and postoperative SCD of patients who underwent unilateral door cervical laminoplasty (x±s, mm).
Table 1. Pre- and postoperative SCD of patients who underwent unilateral door cervical laminoplasty (x±s, mm).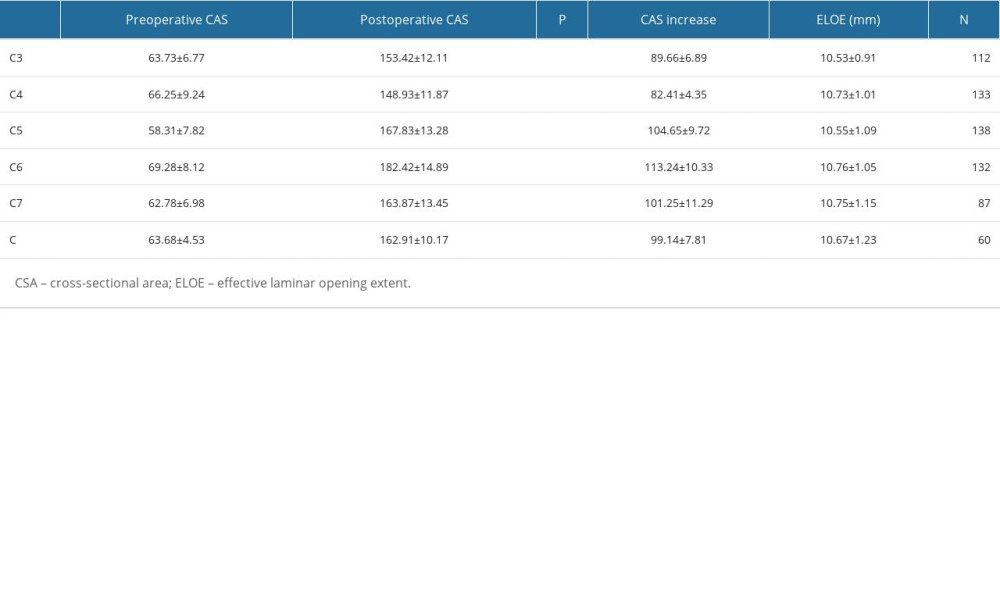 Table 2. Pre- and postoperative CSA of patients underwent unilateral door cervical laminoplasty (x±s, mm2).
Table 2. Pre- and postoperative CSA of patients underwent unilateral door cervical laminoplasty (x±s, mm2).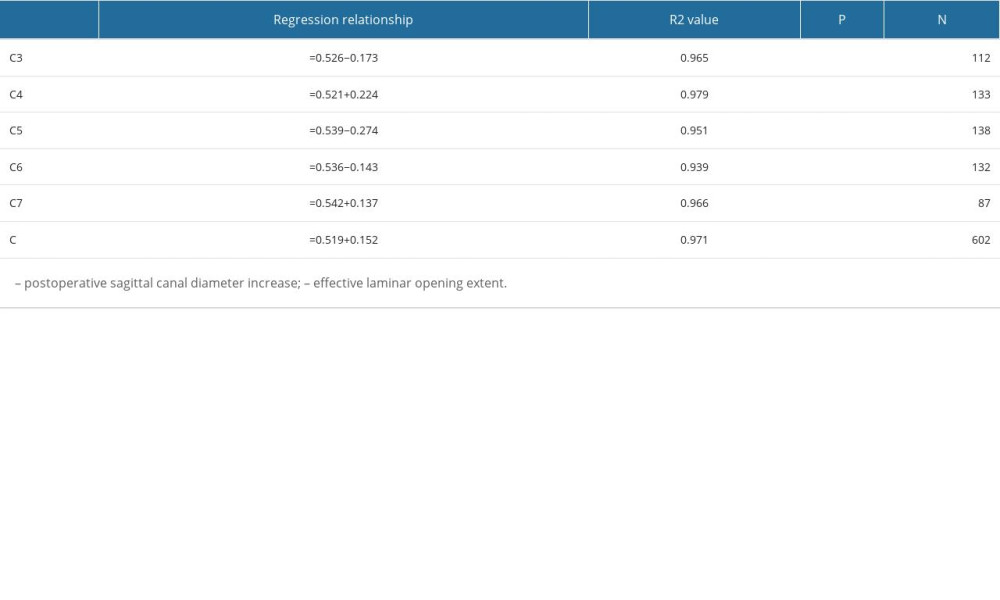 Table 3. Linear regression of effective laminar opening extent against the postoperative sagittal canal diameter increase for unilateral door cervical laminoplasty.
Table 3. Linear regression of effective laminar opening extent against the postoperative sagittal canal diameter increase for unilateral door cervical laminoplasty.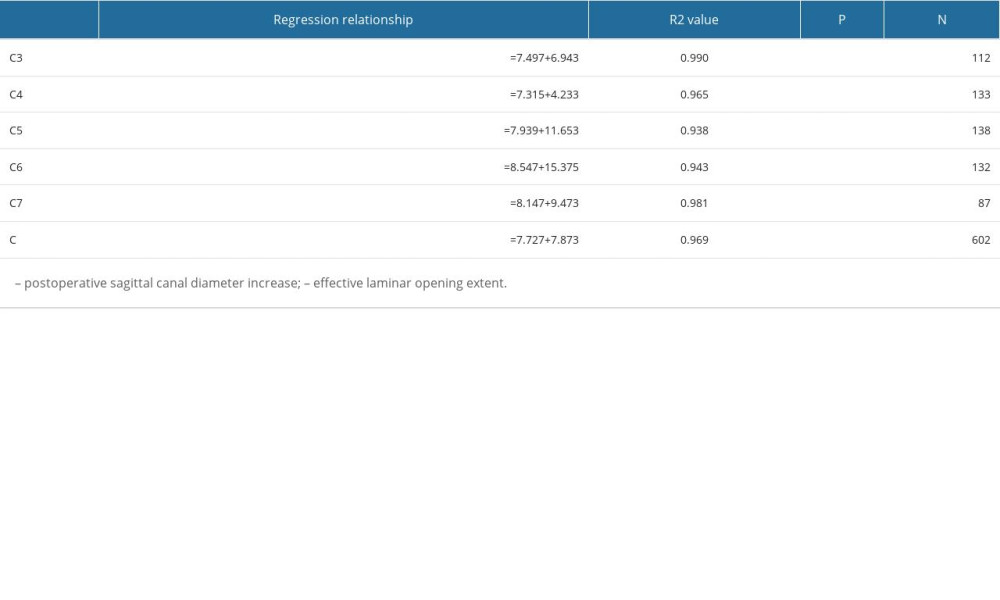 Table 4. Linear regression of effective laminar opening extent against the postoperative cross-sectional area increase for unilateral door cervical laminoplasty.
Table 4. Linear regression of effective laminar opening extent against the postoperative cross-sectional area increase for unilateral door cervical laminoplasty. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








