24 June 2023: Clinical Research
New Suggested Enhancing Safe Apneic Time in Edentulous Elderly: A Comparison of Transnasal Humidified Rapid-Insufflation Ventilatory Exchange and Facemask
Yuxi Shen1BCE, Yajie XuDOI: 10.12659/MSM.940044
Med Sci Monit 2023; 29:e940044
Abstract
BACKGROUND: Edentulous elderly patients often face challenges in airway management and are susceptible to hypoxemia. Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE) provides high-flow nasal oxygenation, potentially extending safe apneic time (SAT). This study compared the efficacy of THRIVE versus facemask ventilation in improving oxygenation and extending SAT in edentulous elderly patients.
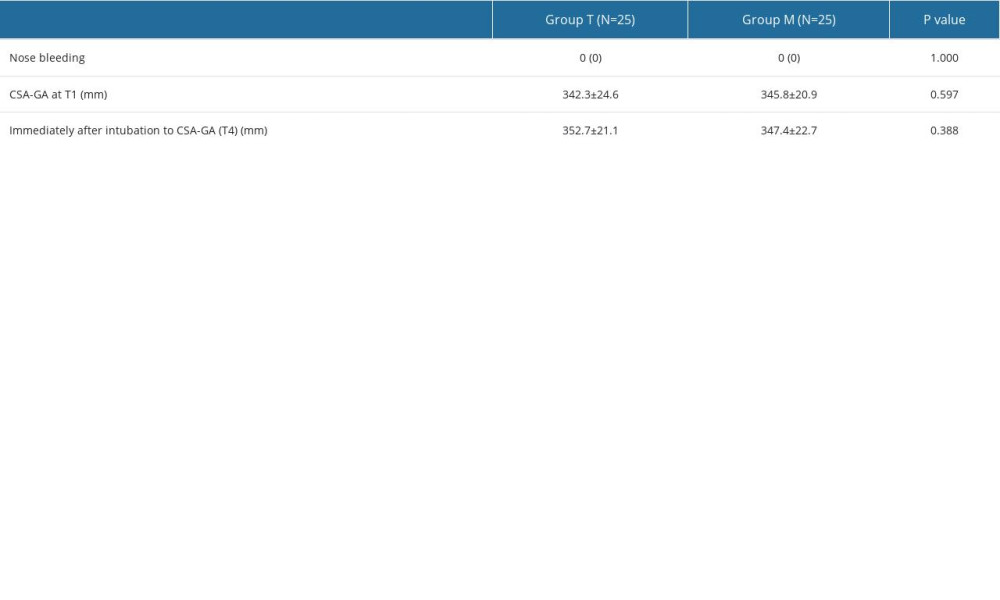
MATERIAL AND METHODS: Patients with more than 10 missing teeth and who were over 65 years old were randomly assigned to the facemask group (Group M, n=25) or the THRIVE group (Group T, n=25). Patients in Group M were pre-oxygenated with a facemask (6 L/min, FiO₂ 100%), while patients in Group T were pre-oxygenated with their mouths closed via THRIVE (30 L/min, FiO₂ 100%). After anesthesia induction, patients in Group M were ventilated with pressure-controlled ventilation. In Group T, the patient's mouth was kept closed, and the flow rate was adjusted to 70 L/min. Four min after cisatracurium administration, ventilation was stopped in Group M while Group T continued to receive oxygen (70 L/min, FiO₂ 100%). The primary outcome was SAT, which was attained at 4 min after injection of cisatracurium and ended when SpO₂ decreased to 95% or when apneic time reached 480 s. A secondary outcome was the reoxygenation time, defined as the time from the beginning of mechanical ventilation to the time when SpO₂ 98% was reached.
RESULTS: An SAT of 480 s was reached by all patients in Group T, but by only 6 patients in Group M (P<0.05). Compared with Group M, the reoxygenation time in Group T was significantly shorter (P<0.05).
CONCLUSIONS: As compared to facemask, THRIVE can extend the SAT, improve oxygenation, and reduce reoxygenation time.
Keywords: Aged, airway management, Hyperbaric Oxygenation, Humans, Masks, Insufflation, personal protective equipment, Respiration, Mouth, Oxygen, Oxygen Inhalation Therapy, Administration, Intranasal
Background
Tooth loss is a common phenomenon in elderly patients and is an independent risk factor for predicting difficult facemask ventilation [1,2]. Loss of teeth in elderly patients often leads to progressive facial morphological changes, leading to cheek indrawing and depression, making it difficult for the mask to fit closely with the face. Therefore, air leakage during facemask ventilation can occur in these patients and is associated with poor oxygenation [3,4]. In addition, elderly patients have reduced static pulmonary compliance, alveolar surface area, and oxygen storage [5]. Therefore, following induction of anesthesia, elderly patients with tooth loss have a shortened safe apneic time (SAT) and are at greater risk of hypoxia. In clinical practice, gauze packing and use of a leakproof facemask can be used to reduce oxygen leakage, but the effect is still poor [6,7]. Some investigators have adopted the method of retaining dentures [8], but this risks denture loss and aspiration. Therefore, it is particularly important to seek a better ventilation method for elderly toothless patients during the induction period of general anesthesia. Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE) provides a high concentration of heated and humidified oxygen through the nasal cannula with a flow of up to 70 L/min for oxygenation. Studies have shown that THRIVE can provide a better oxygen supply and prolong SAT during the induction of general anesthesia [9]. The use of THRIVE during the induction of general anesthesia in edentulous elderly patients, however, has not been studied in detail. Therefore, we designed a randomized controlled study comparing oxygenation and SAT using THRIVE or facemask during the induction of general anesthesia in these elderly patients.
Material and Methods
STUDY DESIGN:
This randomized controlled trial was approved by the Ethics Committee of Nanjing First Hospital (KY20201102-04) and registered with the Chinese Clinical Trial Center (ChiCTR2100051967) before patient enrollment. All patients signed an informed consent form. The work has been reported in line with Consolidated Standards of Reporting Trials (CONSORT) Guidelines.
PATIENTS:
Patients undergoing elective general anesthesia with endotracheal intubation from October 2021 to December 2021 were selected. The inclusion criteria were as follows: ≥65 year of age; ASA class I–III; Mallampati class I–II; missing more than 10 teeth; and adapt to proper use of THRIVE after instruction. The exclusion criteria included: patient refusal to participate; emergency surgery; known or anticipated airway difficulty as well as history of nasal surgery, epistaxis, and nasopharyngeal cavity abnormalities; gastric hypertension, reflux aspiration, intestinal obstruction, and other digestive system diseases; central nervous system disease (eg, stroke and myopathy); BMI >30 kg/m2; significant cardiac disease such as history or coronary artery or cardiac valvular disease; significant lung disease such as emphysema or COPD; hepatic dysfunction; renal failure (CKD 2–4) and history of anemia; and Cormack and Lehane Grade 3 or 4 larynx identified after initial laryngoscopy. The patients were also excluded in the event of unexpected difficult intubation and managed according to the 2015 British Association of Difficult Airway For Adult Unanticipated Difficult Endotracheal Intubation Guidelines [10].
RANDOMIZATION AND BLINDING:
The patients were randomized using computer randomization software (SPSS 24.0) in a 1: 1 ratio and divided into the facemask group (Group M; n=25) and THRIVE group (Group T; n=25). The randomized schedule was hidden and generated by the anesthesiologist in charge of the case, who was not part of the study. The same anesthesiologist prepared the envelopes, and the envelopes were opened just before anesthesia. Correspondents registered each subject after assessing their eligibility.
INTERVENTION:
The patient’s dentures were removed prior to entering the operating room. The patient was placed in the 25-degree head-up position. Invasive arterial pressure was monitored by radial artery catheterization under local anesthesia. A bispectral index (BIS) monitor, blood pressure (BP), electrocardiogram (ECG), SpO2, heart rate(HR), and arterial blood gases (ABG) were monitored in all patients. The THRIVE device (Fisher & Paykel Health care, New Zealand) was heated and humidified 5 min before use.
Preoxygenation: Patients in Group T were pre-oxygenated with a closed mouth by THRIVE (30 L/min, FiO2 100%, 5 min). However, patients in Group M were pre-oxygenated by a facemask without positive airway pressure (PEEP) (6 L/min, FiO2 100%, 5 min).
Induction of anesthesia: Induction of anesthesia after 5 min of preoxygenation: Anesthesia was induced using Midazolam (0.05 mg/kg), sufentanil (0.3–0.5 μg/kg), propofol (1–2 mg/kg) and cisatracurium (0.2 mg/kg) administered intravenously over a 30–60 s period. Target BIS values were maintained between 40 and 60 in all patients after induction. Following loss of consciousness, the patient’s jaw was supported and 30 degrees head-back tilt was provided to optimize the airway. Oxygenation was then provided for each patient depending on patient group. In Group T, the THRIVE flow rate was increased to 70 L/min 100% oxygen, and the patient’s mouth was kept closed (Figure 1A). In Group M, facemask positive-pressure-controlled ventilation was used (inspiratory pressure: 15 cmH2O; respiratory rate: 16 min−1; oxygen flow rate of 100%: 6 L/min) (Figure 1B).
Four min after cisatracurium administration, the facemask was removed in group M while ventilation was continued in group T. During this stage, a laryngoscope was used to continuously expose the glottis to rule out any airway difficulty. When SpO2 decreased to 95% or the apneic time reached 480 s, we immediately performed endotracheal intubation. After intubation was confirmed by a continuous end-tidal carbon dioxide waveform, mechanical ventilation was initiated. To ensure patient safety, pure oxygen was used during reoxygenation. The oxygen concentration was reduced when SpO2 was above 98% and was stable enough to achieve a protective lung ventilation.
All procedures were performed by the same skilled and experienced anesthesiologist. If the patient’s MAP decreased by more than 20%, ephedrine 6 mg or norepinephrine 50 μg was injected intravenously. If the patient’s heart rate was <50 bpm, atropine 0.3–0.5 mg was injected intravenously.
OUTCOMES AND DATA COLLECTION:
During this study, we defined different time points, including: entering the operating room while breathing room air (T1), 5 min after preoxygenation (T2), 4 min after administration of muscle relaxant (T3), at the time of reaching SAT (T4), and at reoxygenation to SpO2 98% following intubation and ventilation (T5).
The primary outcome was SAT, which was attained at 4 min after injection of cisatracurium and ended when SpO2 decreased to 95% or when apneic time reached 480 s.
Reoxygenation time was defined as the time from the beginning of mechanical ventilation to reaching SpO2 98%. PaO2, PaCO2, HR, and MAP at T1–T4 were recorded.
To assess gastric gas insufflation, the cross-sectional area of the gastric antrum (CSA-GA) was recorded at T1 and T4. This was performed by an experienced operator with the patient in the supine position with high head and low feet, using a Sono ultrasonic low-frequency convex array probe (2–8 MHz). The marker point was headed to the cephalic side, and the sagittal line was slightly to the right in the middle of the inferior epigastric xiphoid process. The left hepatic lobe was in front of the gastric antrum, and the pancreas was in front of the gastric antrum. The ultrasonic free tracing technique was used to calculate the CSA-GA area by tracing the outline of the gastric antrum [11].
Ventilation-related complications, included nose bleeding and gastric insufflation, were recorded 24 h after the operation.
STATISTICAL ANALYSIS:
The sample size of this study was calculated based on a pilot study with 10 patients in each group. The mean safe apneic time was 355 s in Group M and 480 s in Group T. Given a standard deviation of 120 s, a type I error of 5%, and a power of 0.9, an independent sample
Data were statistically analyzed using the SPSS version 24.0 program (SPSS, Inc., Chicago, IL). The data’s normality was assessed using the Shapiro-Wilk test. Levene’s test was used to determine whether the variance was homogeneous. Means±standard deviations were used to represent normally distributed data. The 2 groups were compared using the
In our study, the cut-off period for apnea was set at 480 s, or when SpO2 dropped to 95% during apnea. If the SpO2 levels did not drop to 95% before 480 s, it was initially documented as 480 s. Because there were no patients whose SpO2 fell below 95% within 480 s in the THRIVE group, the outcome was analyzed as a time-to-event analysis (survival framework). For comparison between Group T and Group M, a Kaplan-Meier survival analysis was performed, but not the Mann-Whitney U test. Statistical significance was set at
Results
PRIMARY OUTCOME:
All 25 patients in Group T reached 480 s with their SpO2 maintained at >95%. In Group M, 6 patients (24%) maintained their SpO2 at >95% for 480 s and the other 19 desaturated to below 95% within 480 s. Kaplan-Meier survival curves showed that there were significantly fewer cases with SpO2 >95% in Group M than in Group T (P<0.001, Figure 3). The time to satisfactory reoxygenation was significantly shorter in Group T compared to Group M (P<0.001, Figure 3).
:
When comparing PaO2 within groups, it was found that both groups had significantly higher PaO2 at T2 and T3 than at T1 (P<0.05). However, PaO2 in Group M at T4 was similar to T1, whereas Group T remained considerably higher at the same timepoint (P<0.05). When compared to T2 or T3, both groups demonstrated a substantial decrease in PaO2 at T4 (P<0.05). In comparison to Group M, PaO2 in Group T was significantly greater at T2, T3, and T4 (P<0.05). There was no difference in PaO2 between the 2 groups at T1 (P>0.05). Both groups showed no difference with PaCO2 at T2 compared to T1. After that, PaCO2 levels in both groups kept rising until T4 was at its greatest value. We discovered no statistically significant change in PaCO2 between the 2 groups at either T1 or T2 (P>0.05). However, the PaCO2 was significantly greater in Group T compared to Group M at T3 and T4 (P<0.05, Figure 4).
COMPARISON OF HR AND MAP BETWEEN THE 2 GROUPS AT EACH TIME POINT:
There were no significant differences in MAP or HR between the 2 groups at each time point (P>0.05, Figure 4).
COMPLICATIONS RELATED TO VENTILATION AND GASTRIC INSUFFLATION:
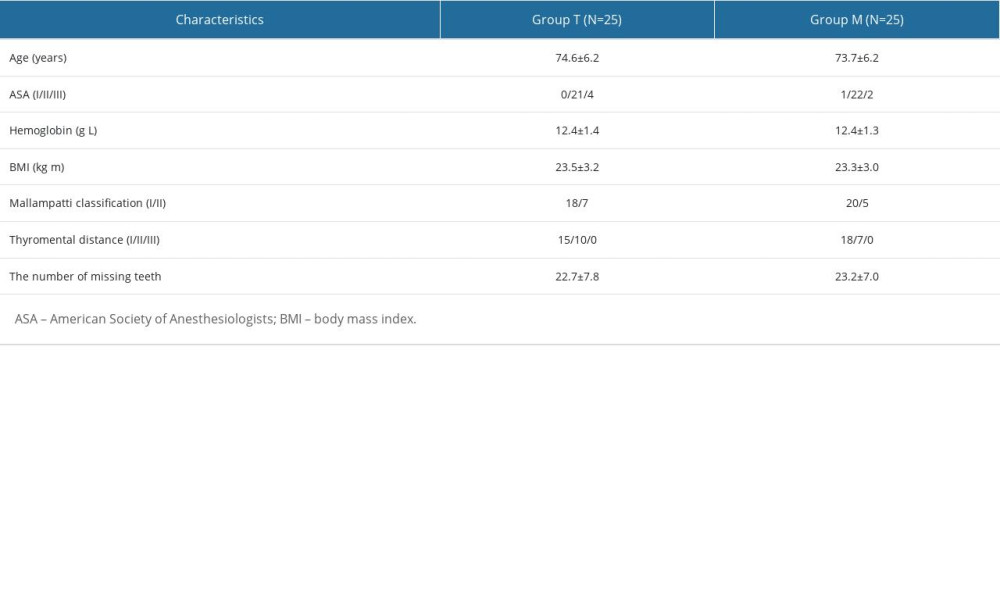
No nose bleeding or other complications occurred in the 2 groups. CSA-GA differences between the 2 groups were not statistically significant at time point T1 and immediately after intubation (P>0.05, Table 2).
Discussion
We found that use of THRIVE resulted in a significantly better PaO2 than facemask ventilation during the induction of general anesthesia, and that the SAT was prolonged and the reoxygenation time was shortened. Patients in the THRIVE group maintained a PaO2 that was greatly elevated when compared to their baseline throughout the study period, including the end of the safe apneic period. All of the patients using THRIVE reached an SAT of 480 s, but just 6 of the patients did so when using a facemask. However, the average time for re-saturation to the SpO2 of 98% was much longer in the facemask group (45 s) compared to the THRIVE group (11 s); this result may be related to the lower SpO2 on commencement of intubation in the facemask group compared with the THRIVE group.
In edentulous elderly patients, cheek sinking leads to reduced facemask tightness, with serious air leakage during facemask ventilation and reduced facemask ventilation efficiency [2,3]. Liu and Chu have found that when the number of missing teeth accounts for more than 1/4 of the total number of teeth, the oral structure of elderly patients will change, hindering masticatory function and changing facial morphology, resulting in mask ventilation difficulties [12]. Moreover, elderly patients have lower oxygen reserves, which shortens the SAT during the general anesthesia intubation period. Therefore, it is particularly important to seek a better ventilation strategy in elderly toothless patients. THRIVE uses a relatively constant concentration, temperature, and humidity at a high flow rate of up to 70 L/min via the nasal cannula. Studies have shown that THRIVE can extend the asphyxia window for patients under general anesthesia to 65 min for patients with difficult airway management [13]. Hua and colleagues found that THRIVE significantly extended the SAT in elderly patients after rapid sequence induction of anesthesia compared to facemask [5], which is consistent with our results. Our findings demonstrated that patients with THRIVE had significantly greater PaO2, longer SAT, and shorter reoxygenation time during induction of general anesthesia than in patients using mask ventilation. Possible reasons are as follows: (1) THRIVE uses a nasal catheter to administer high-concentration and high-flow oxygen and is unaffected by tooth loss. (2) THRIVE facilitates oxygenation by delivering high-flow pure oxygen with a maximum velocity of 70 L/min and a small amount of CPAP, which opens the upper respiratory tract and even the distal airway, decreasing ventilatory dead space and reducing the likelihood of atelectasis [13]. (3) The facemask usually needs to be removed during endotracheal intubation, which leads to an interruption of oxygenation. THRIVE allows continuous oxygen supply during intubation, which may make it a better choice for oxygenation maintenance during intubation. During simulated asphyxia intubation, THRIVE provides higher PaO2, establishes relatively higher oxygen partial pressure difference, promotes oxygen diffusion from respiratory tract to alveolar capillaries, and thus maintains satisfactory oxygenation during the asphyxia stage, prolongs safe ventilation time, and shortened the reoxygenation time.
It is important to note that SAT in this study was still computed from 4 min after muscle relaxant treatment, even if respiration in the THRIVE group gradually stopped after the termination of muscle relaxant administration. The primary reason is that THRIVE’s effects on both the induction process and the asphyxiation phase were going to be evaluated. Clinically, the time when SpO2 drops to 90% after ventilation cessation is usually defined as the safe apneic duration after induction of general anesthesia [14]. However, elderly patients are often complicated with cardiovascular and cerebrovascular diseases and decreased respiratory function, making them more vulnerable to hypoxic episodes and less tolerant of low SpO2. Therefore, to ensure patient safety, this study defined the time when SpO2 decreased to 95% after ventilation cessation as the safe apneic duration. In addition, to avoid serious hypercapnia and other potential complications in our elderly patients, we set the safe apneic duration as 480 s [14].
PaCO2 significantly increased in both groups during the apneic period. However, the THRIVE group experienced a much larger increase in PaCO2 than the facemask group. The longer SAT time and insufficient gas scour may be to blame for the greater PaCO2 in the THRIVE group. PaCO2 rose, but it remained within the acceptable range. THRIVE creates a cascade of vortex flows from the larger to the smaller airways, while promoting gas exchange through the alveoli-capillary surface and flushing the carbon dioxide still present in the nasal cavity, oral cavity, and throat. Even without formal positive-pressure ventilation, the heart’s oscillation mechanism works to remove carbon dioxide [15].
Positive-pressure ventilation using the facemask can lead to gastric insufflation and increase the risk of reflux aspiration [16]. Studies have shown that when the pressure setting in the pressure control mode increases from 10 cmH2O to 25 cmH2O, the incidence of bloating increases from 0% to 41% [17]. Ultrasonic monitoring of the gastric antrum cross-sectional area can reflect the gastric volume [18]. In line with the findings of earlier research [17], our investigation revealed that CSA-GA did not increase following facemask pressure control ventilation with a 15 cmH2O pressure. After 480 s of THRIVE use, CSA-GA did not rise. The lower esophageal sphincter is a high-pressure region at the junction between the lower esophagus and the stomach, with a pressure of 17.5–40.7 cmH2O [19]. Relevant studies have shown that with the increase in oxygen flow, THRIVE increases the average pressure in the main trachea, main bronchus, and pharynx to varying degrees, but the pressure generated is always less than 10 cmH2O, far lower than the pressure of the lower esophageal sphincter [20].
In comparison with the facemask group, no increased occurrence of complications, including hemodynamic instability, resistant arrhythmia, or nasal discomfort, was reported in this study until the preset endpoint. These results suggest that use of THRIVE in elderly patients was as safe as using a facemask.
When interpreting the results of the current study, several limitations should be considered. First, this study selected patients with ≥10 missing teeth, and whether the different locations and numbers of missing teeth would have different effects was not specifically assessed. Second, the optimal flow rate of THRIVE has not been discussed, and further research will be carried out in the future.
Conclusions
In conclusion, during the induction period of general anesthesia, THRIVE can improve oxygenation, prolong safe apneic time, and reduce reoxygenation time in edentulous elderly patients.
Figures
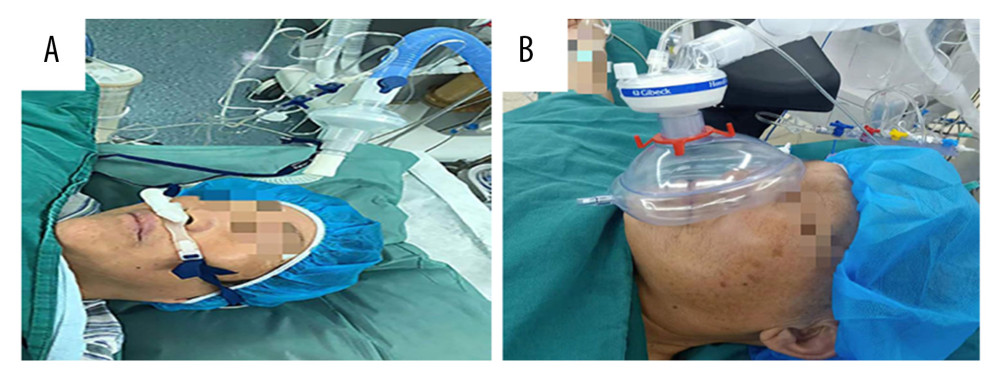 Figure 1. (A) The use of transnasal humidified rapid-insufflation ventilatory exchange. (B) The use of facemask. This figure was created using Office Word (version 16.16.27 by Microsoft).
Figure 1. (A) The use of transnasal humidified rapid-insufflation ventilatory exchange. (B) The use of facemask. This figure was created using Office Word (version 16.16.27 by Microsoft). 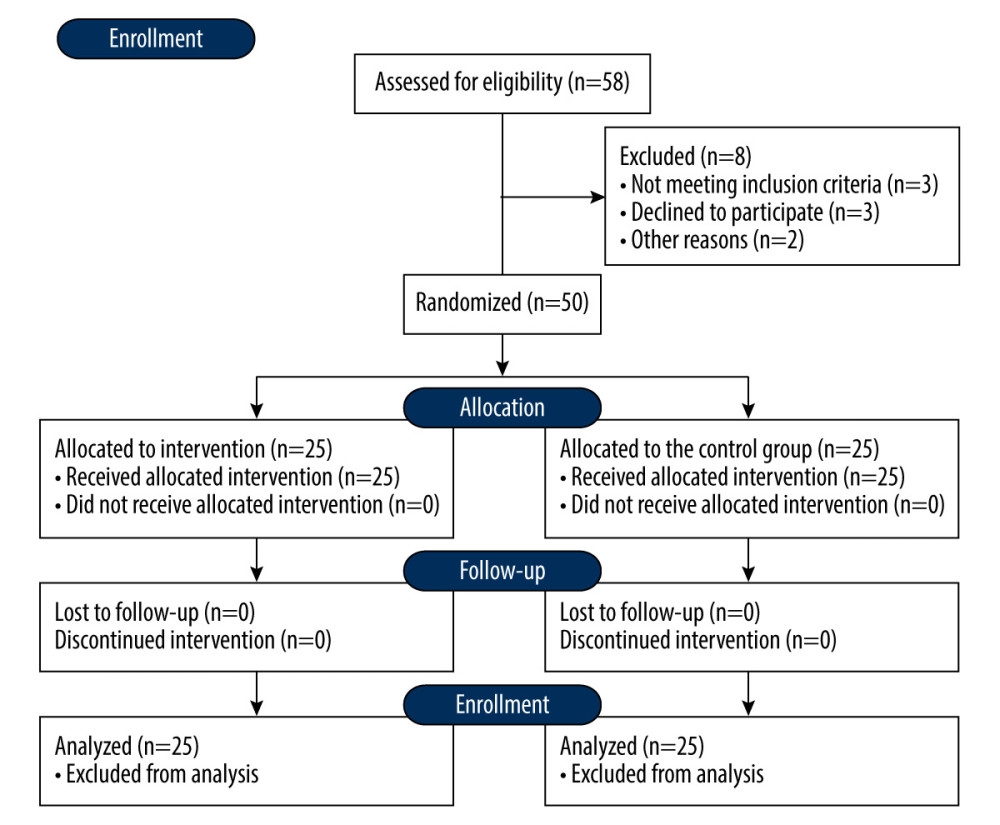 Figure 2. CONSORT diagram of recruitment. This figure was created using Office Word (version 16.16.27 by Microsoft).
Figure 2. CONSORT diagram of recruitment. This figure was created using Office Word (version 16.16.27 by Microsoft). 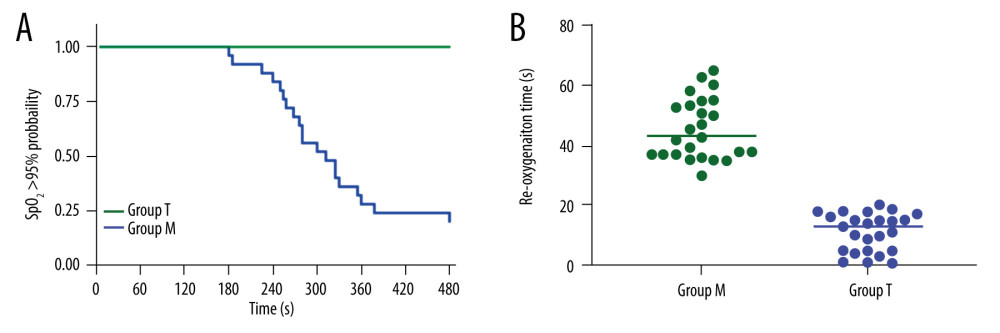 Figure 3. Kaplan-Meier survival curves and reoxygenation time of the 2 groups. This figure was created using Prosm 9 for macOS (version 9.5.0, GraphPad Software).
Figure 3. Kaplan-Meier survival curves and reoxygenation time of the 2 groups. This figure was created using Prosm 9 for macOS (version 9.5.0, GraphPad Software). 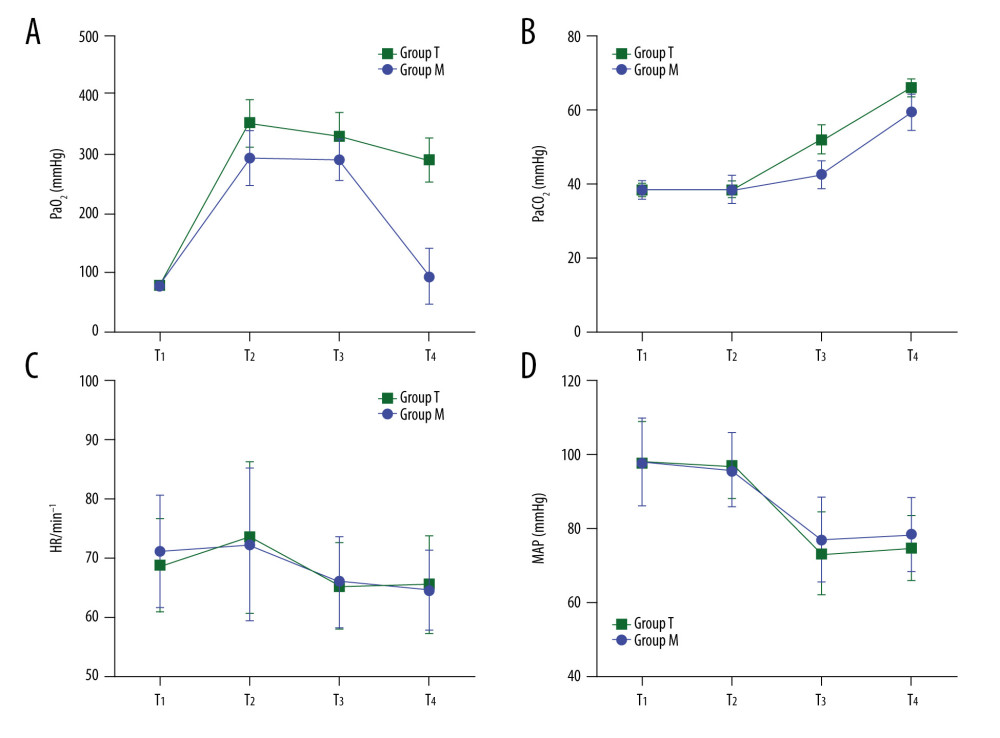 Figure 4. PaO2, PaCO2, HR, and MAP at different time points. This figure was created using Prosm 9 for macOS (version 9.5.0, GraphPad Software).
Figure 4. PaO2, PaCO2, HR, and MAP at different time points. This figure was created using Prosm 9 for macOS (version 9.5.0, GraphPad Software). References
1. Heidegger T, Management of the difficult airway: N Engl J Med, 2021; 384(19); 1836-47
2. Schäuble JC, Heidegger TErratum to: Management of the difficult airway: Overview of the current guidelines: Der Anaesthesist, 2019; 68(1); 29 [in German]
3. Johnson KN, Botros DB, Groban L, Anatomic and physiopathologic changes affecting the airway of the elderly patient: Implications for geriatric-focused airway management: Clin Interv Aging, 2015; 10; 1925-34
4. Shi Z, Wu Z, Zha B, Efficacy of WEI JET for supraglottic ventilation before tracheal intubation in patients with tooth less: Chin J Anesthesiol, 2019(08); 985-88
5. Hua Z, Liu Z, Li Y, Transnasal humidified rapid insufflation ventilatory exchange vs. facemask oxygenation in elderly patients undergoing general anaesthesia: A randomized controlled trial: Sci Rep, 2020; 10(1); 5745
6. Cai D, Chen S, Ling Y, Observation after intubation edentulous gauze packing: Modem Hospital, 2015; 15(02); 62-63
7. Zhang H, Application of leakproof mask in induction of general anesthesia in elderly patients: J Clin Anesthesiol, 2013; 29(1); 88-89
8. Conlon NP, Sullivan RP, Herbison PG, The effect of leaving dentures in place on bag-mask ventilation at induction of general anesthesia: Anesth Analg, 2007; 105(2); 370-73
9. Mir F, Patel A, Iqbal R, A randomised controlled trial comparing transnasal humidified rapid insufflation ventilatory exchange (THRIVE) pre-oxygenation with facemask pre-oxygenation in patients undergoing rapid sequence induction of anaesthesia: Anaesthesia, 2017; 72(4); 439-43
10. Frerk C, Mitchell VS, McNarry AF, Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults: Br J Anaesth, 2015; 115(6); 827-48
11. Kaydu A, Gokcek E, Preoperative assessment of ultrasonographic measurement of antral area for gastric content: Med Sci Monit, 2018; 24; 5542-48
12. Liu H, Chu B, Oral health is the foundation of the general health of the elderly: Chinese Journal of Geriatric Dentistry, 2013; 11(3); 129-31
13. Upperman L, Gildea T, Galway U, Transnasal humidified rapid insufflation ventilatory exchange during bronchoscopy in severe pulmonary hypertension due to Gerbode defect: Respirol Case Rep, 2020; 8(3); e00519
14. Rajan S, Joseph N, Tosh P, Effects of preoxygenation with tidal volume breathing followed by apneic oxygenation with and without continuous positive airway pressure on duration of safe apnea time and arterial blood gases: Anesth Essays Res, 2018; 12(1); 229-33
15. Patel A, Nouraei SA, Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE): A physiological method of increasing apnoea time in patients with difficult airways: Anaesthesia, 2015; 70(3); 323-29
16. Savary D, Drennan IR, Badat B, Gastric insufflation during cardiopulmonary resuscitation: A study in human cadavers: Resuscitation, 2020; 146; 111-17
17. Bouvet L, Albert ML, Augris C, Real-time detection of gastric insufflation related to facemask pressure-controlled ventilation using ultrasonography of the antrum and epigastric auscultation in nonparalyzed patients: A prospective, randomized, double-blind study: Anesthesiology, 2014; 120(2); 326-34
18. Mahmood F, Matyal R, Skubas N, Perioperative ultrasound training in anesthesiology: A call to action: Anesth Analg, 2016; 122(6); 1794-804
19. Fournier MR, Kerr PD, Shoenut JP, Effect of nasal continuous positive airway pressure on esophageal function: J Otolaryngol, 1999; 28(3); 142-44
20. Riva T, Meyer J, Theiler L, Measurement of airway pressure during high-flow nasal therapy in apnoeic oxygenation: A randomised controlled crossover trial: Anaesthesia, 2021; 76(1); 27-35
Figures
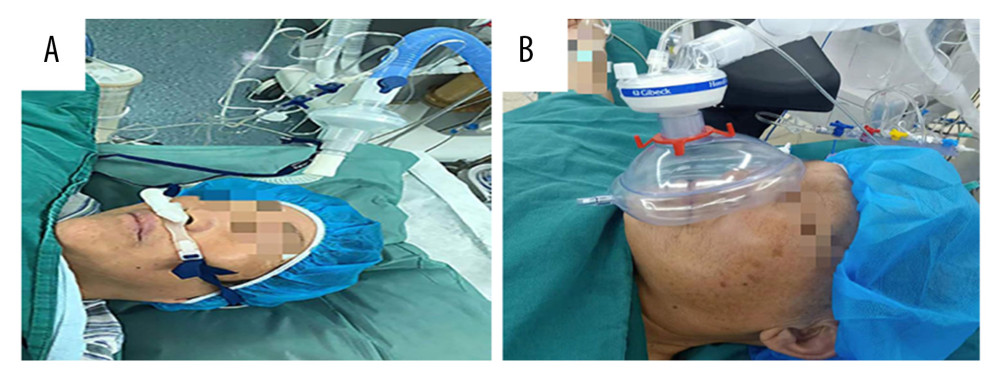 Figure 1. (A) The use of transnasal humidified rapid-insufflation ventilatory exchange. (B) The use of facemask. This figure was created using Office Word (version 16.16.27 by Microsoft).
Figure 1. (A) The use of transnasal humidified rapid-insufflation ventilatory exchange. (B) The use of facemask. This figure was created using Office Word (version 16.16.27 by Microsoft).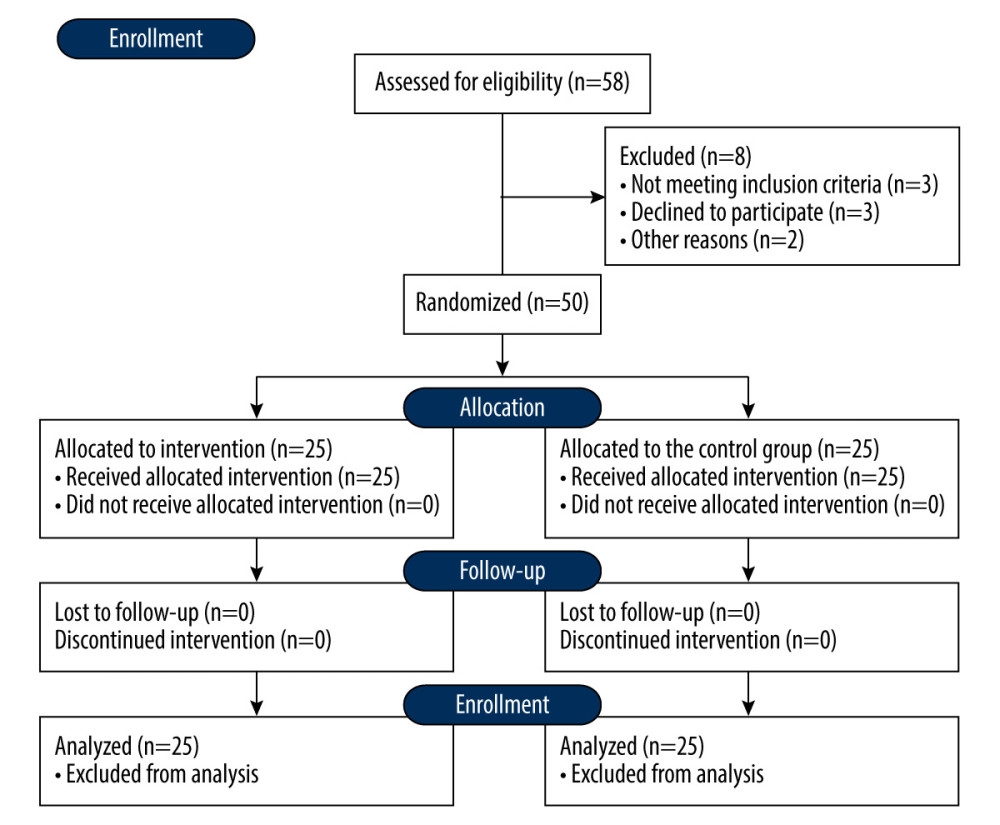 Figure 2. CONSORT diagram of recruitment. This figure was created using Office Word (version 16.16.27 by Microsoft).
Figure 2. CONSORT diagram of recruitment. This figure was created using Office Word (version 16.16.27 by Microsoft).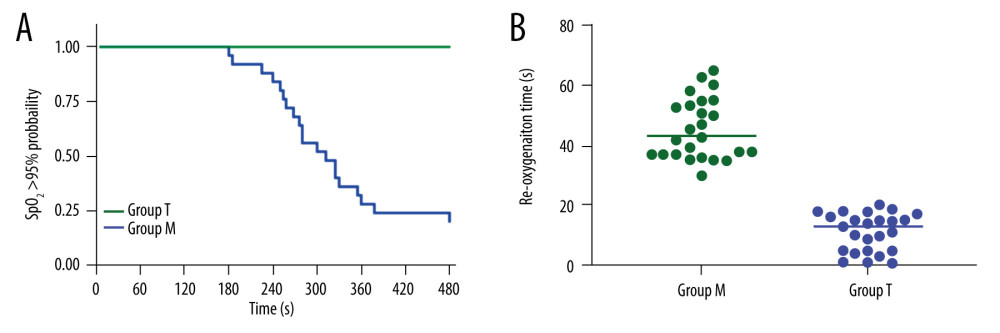 Figure 3. Kaplan-Meier survival curves and reoxygenation time of the 2 groups. This figure was created using Prosm 9 for macOS (version 9.5.0, GraphPad Software).
Figure 3. Kaplan-Meier survival curves and reoxygenation time of the 2 groups. This figure was created using Prosm 9 for macOS (version 9.5.0, GraphPad Software).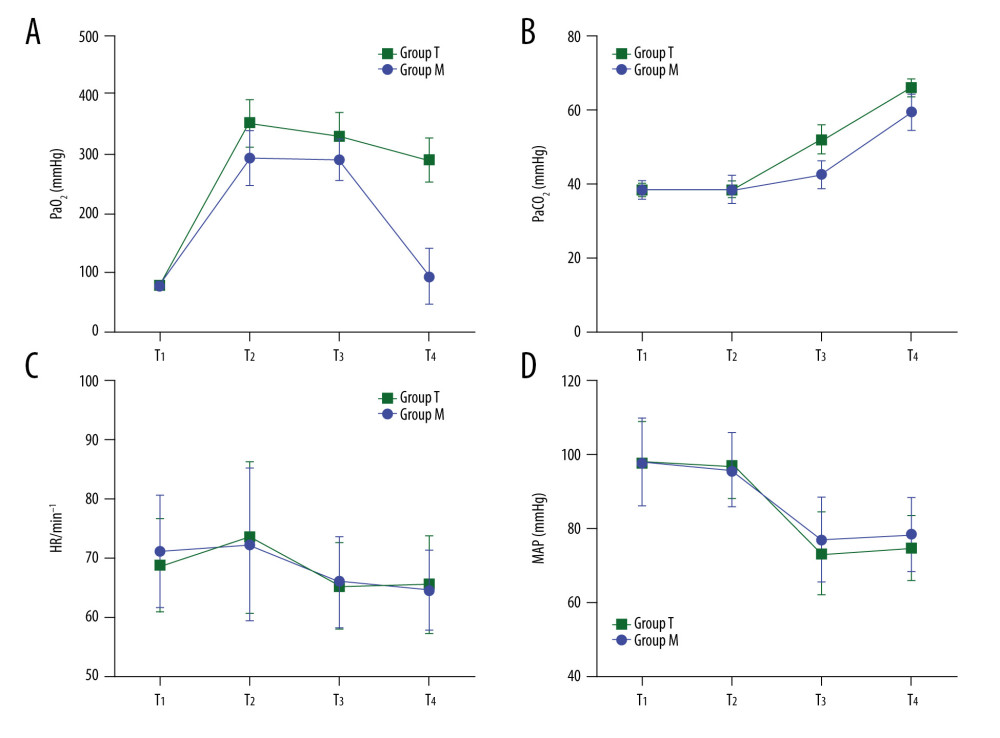 Figure 4. PaO2, PaCO2, HR, and MAP at different time points. This figure was created using Prosm 9 for macOS (version 9.5.0, GraphPad Software).
Figure 4. PaO2, PaCO2, HR, and MAP at different time points. This figure was created using Prosm 9 for macOS (version 9.5.0, GraphPad Software). In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952