18 July 2023: Clinical Research
Risk Factors for New Vertebral Compression Fracture After Percutaneous Vertebral Augmentation: A Retrospective Study
Yunfeng Zhang1ABCE, Jiayang J. Sun1BCD, Zhuo Zhang1BCD, Fei Huang1CDF, Jiayin Lv1CDF, Qingsan Zhu1AG*DOI: 10.12659/MSM.940134
Med Sci Monit 2023; 29:e940134
Abstract
BACKGROUND: Percutaneous vertebral augmentation is the mainstream treatment of osteoporotic vertebral compression fracture (OVCF). New vertebral compression fracture (NVCF) after percutaneous vertebral augmentation may be an issue that cannot be ignored. Nevertheless, the risk factors for NVCF are still uncertain. This research aimed to study the risk factors for NVCF after percutaneous vertebral augmentation.
MATERIAL AND METHODS: All patients who underwent percutaneous vertebral augmentation for OVCF from January 2019 to December 2020 were enrolled in the study. These patients were divided into NVCF and control groups according to whether they had NVCF. The covariates including sex, age, BMI, diabetes, hypertension, smoking, alcohol, fracture level, surgical method, cement leakage, cement volume, preoperative anterior vertebral height ratio, and Hounsfield unit (HU) value were reviewed. Univariate and multivariate analyses were performed to identify risk factors.
RESULTS: A total of 279 patients were included in this study, of which 47 had NVCF after percutaneous vertebral augmentation. Univariate analysis demonstrated that there were significant differences in age (OR=1.040, 95% CI=1.003-1.078, P=0.033), BMI (OR=0.844, 95% CI=0.758-0.939, P=0.002) and HU value (OR=0.945, 95% CI=0.929-0.962, P<0.001) between the 2 groups. Multivariate regression analysis revealed that HU value (OR=0.942, 95% CI=0.924-0.960, P<0.001) were independent risk factor for NVCF after percutaneous vertebral augmentation.
CONCLUSIONS: Hounsfield unit value was an independent risk factor for new vertebral compression fracture after percutaneous vertebral augmentation, whereas age and BMI were not.
Keywords: Fractures, Compression, Osteoporosis, Osteoporotic Fractures, Risk Factors, Humans, Spinal Fractures, Retrospective Studies, kyphoplasty, Treatment Outcome, vertebroplasty, Bone Cements
Background
Osteoporotic vertebral compression fracture (OVCF) usually occurs in elderly people with osteoporosis [1]. Patients with OVCF may have spinal kyphosis, serious back pain, and even mortality [2]. Conservative treatment, including anti-inflammatory drugs (NSAID), bed rest, and brace fixation, is the first treatment option.
Percutaneous vertebral augmentation, including percutaneous vertebroplasty (PVP) and percutaneous kyphoplasty (PKP), is the mainstream treatment for patients with OVCF after conservative treatment failure. Several studies have demonstrated the safety and efficacy of PVP and PKP in the treatment of OVCF [3,4]. Nevertheless, some adverse events, including new vertebral compression fracture (NVCF), pulmonary cement embolism, and bone cement leakage, after percutaneous vertebral augmentation were reported [5–7].
NVCF occurring in patients treated by percutaneous vertebral augmentation for OVCF may be an issue that cannot be ignored [8]. Some possible risk factors including age, cement leakage, body mass index (BMI), and bone mineral density (BMD) were reported [9,10]. Nevertheless, the risk factors for NVCF are still unclear. The above studies did not include the factor of Hounsfield unit (HU) value. HU value is considered as an indicator to the assessment of bone mineral density (BMD) and can be used in the diagnosis of osteoporosis [11,12]. There exists an association between HU value of L1 vertebral body on CT and T-score obtained by dual X-ray absorptiometry. Previous research revealed that the incidence of NVCF was as high as 20% [13]. NVCF has become a worldwide public health issue, bringing huge economic burden to patients, their families, and even society [14,15]. Therefore, it is necessary and significant for clinicians, patients, and researchers to conduct a comprehensive study on NVCF percutaneous vertebral augmentation. Our hypothesis is that age, BMI, and HU value may be potential risk factors for NVCF. The purpose of this study was to retrospectively study NVCF patients after percutaneous vertebral augmentation and to analyze the risk factors for NVCF. Clinicians could obtain some valuable guidance, and patients with risk factors could receive preventive interventions, which may reduce the occurrence of NVCF in patients after percutaneous vertebral augmentation. Future researchers can also draw inspiration and conduct further research based on this study.
Material and Methods
STUDY SUBJECTS:
All patients treated with percutaneous vertebral augmentation for OVCF at our institution from January 2019 to December 2020 were enrolled in the study. The calculation method for sample size in this study was from previous research [16]. To further clarify the risk factors for vertebral compression fractures after percutaneous vertebral augmentation, logistic regression analysis was designed to retrospectively analyze patients with OVCF admitted to our hospital over a 2-year period. The sample of this study has a certain representativeness, the data collected are mostly objective data, the measurement results obtained are objective results, and the accuracy is high. In accordance with the Helsinki Declaration, the study was supported by the Ethics Committee of our institution and we obtained written informed consent of the participants. The inclusion criteria were as follows: 1) back pain; 2) PVP or PKP; 3) single-level vertebral compression fracture; 4) complete imaging data; 5) follow-up time >1 year. The exclusion criteria were as follows: 1) back pain caused by non-fracture diseases; 2) multi-level vertebral compression fracture; 3) vertebral fractures caused by high-energy trauma or pathological diseases; 4) VCF with deformity; 5) non-PVP or PKP; 6) previous history of vertebral augmentation; 7) incomplete imaging data; 8) follow-up time <1 year.
SURGICAL PROCEDURE:
With the patient in prone position, local anesthesia was administered. Fluoroscopy was performed to identify the fractured vertebral body. A working channel was established after the puncture needle was inserted into the fractured vertebral body with the help of C-arm fluoroscopy. The use of a balloon was sometimes necessary to restore the fractured vertebral body height prior to cement injection. The bone cement was slowly injected into the fractured vertebral body under C-arm fluoroscopy to avoid bone cement leakage. The procedure was immediately stopped if the bone cement overfilled the fractured vertebral body or if cement leakage was found.
ASSESSMENT:
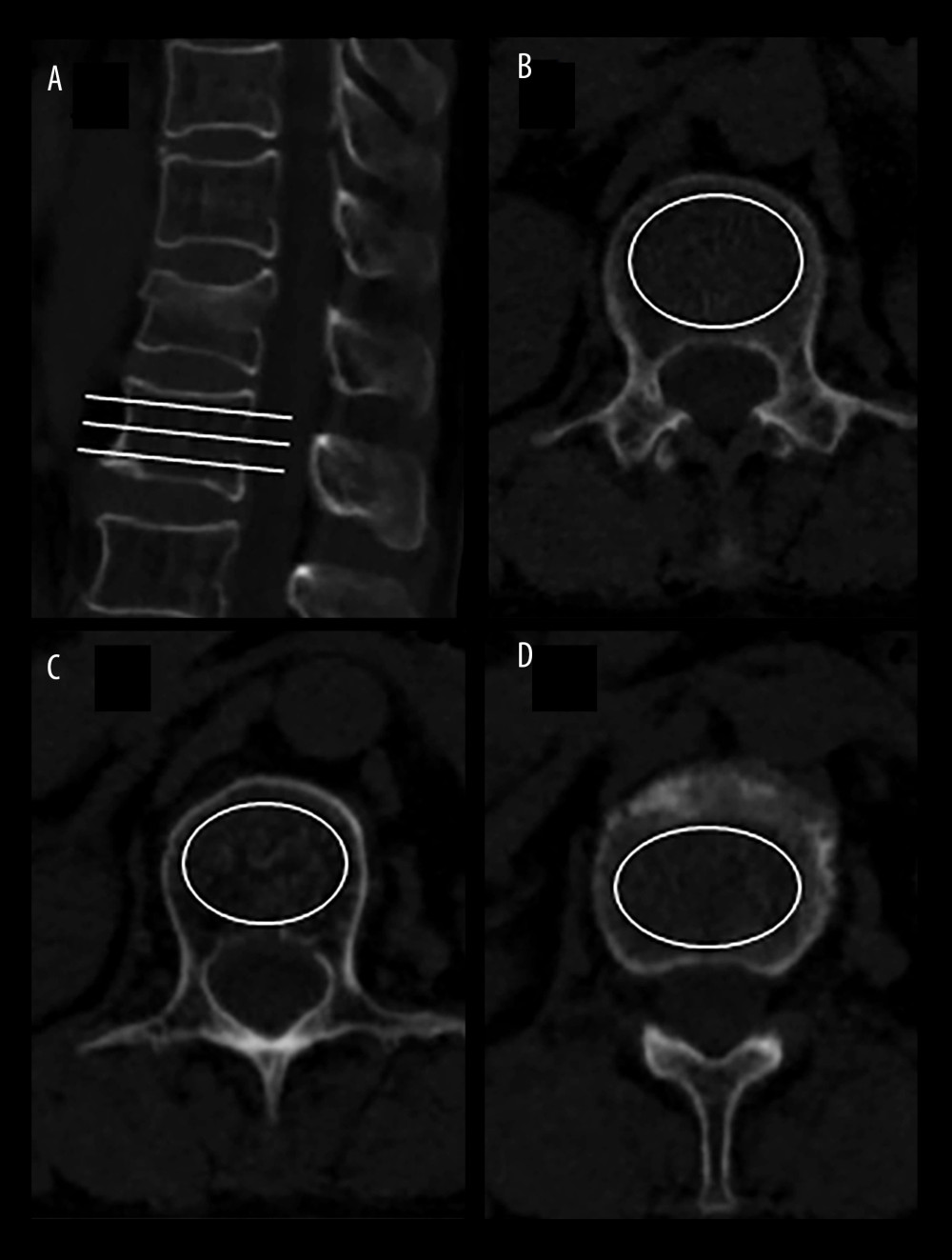
The parameters including sex, age, BMI, diabetes, hypertension, history of smoking, history of alcohol, fracture level, surgical method, bone cement leakage, bone cement volume, preoperative anterior vertebral height ratio (AVHR), and HU value were reviewed. Surgical methods included PVP and PKP, and fracture level included thoracolumbar (TL) junction and non-TL junction. AVHR of the fractured vertebral body was calculated by dividing the anterior vertebral height (AVH) by the average of the anterior vertebral height (AVH1) of the upper vertebra of the fractured vertebrae and the anterior vertebral height (AVH2) of 1 vertebra below the fractured vertebra. HU value is considered as an indicator to the assessment of bone mineral density (BMD) and can be used in the diagnosis of osteoporosis [11,12]. HU value was measured on the axial CT imaging. HU value of the L1 vertebra is equal to the average value of the largest elliptical region of interest (ROI) of inferior to the superior endplate and the middle of the vertebral body and superior to the inferior endplate layers [17] (Figure 1). Osteoporosis is diagnosed as L1 CT value ≤110 HU [18].
STATISTICAL ANALYSIS:
The data were statistically analyzed using SPSS 25 (IBM Corp., Armonk, NY, USA). Categorical variables were described as the number with the percentages, whereas continuous variables were expressed as the mean with standard deviation. Univariate logistic regression analysis was used to compare the control and NVCF groups. Multivariate logistic regression analysis was conducted with variables that had a
Results
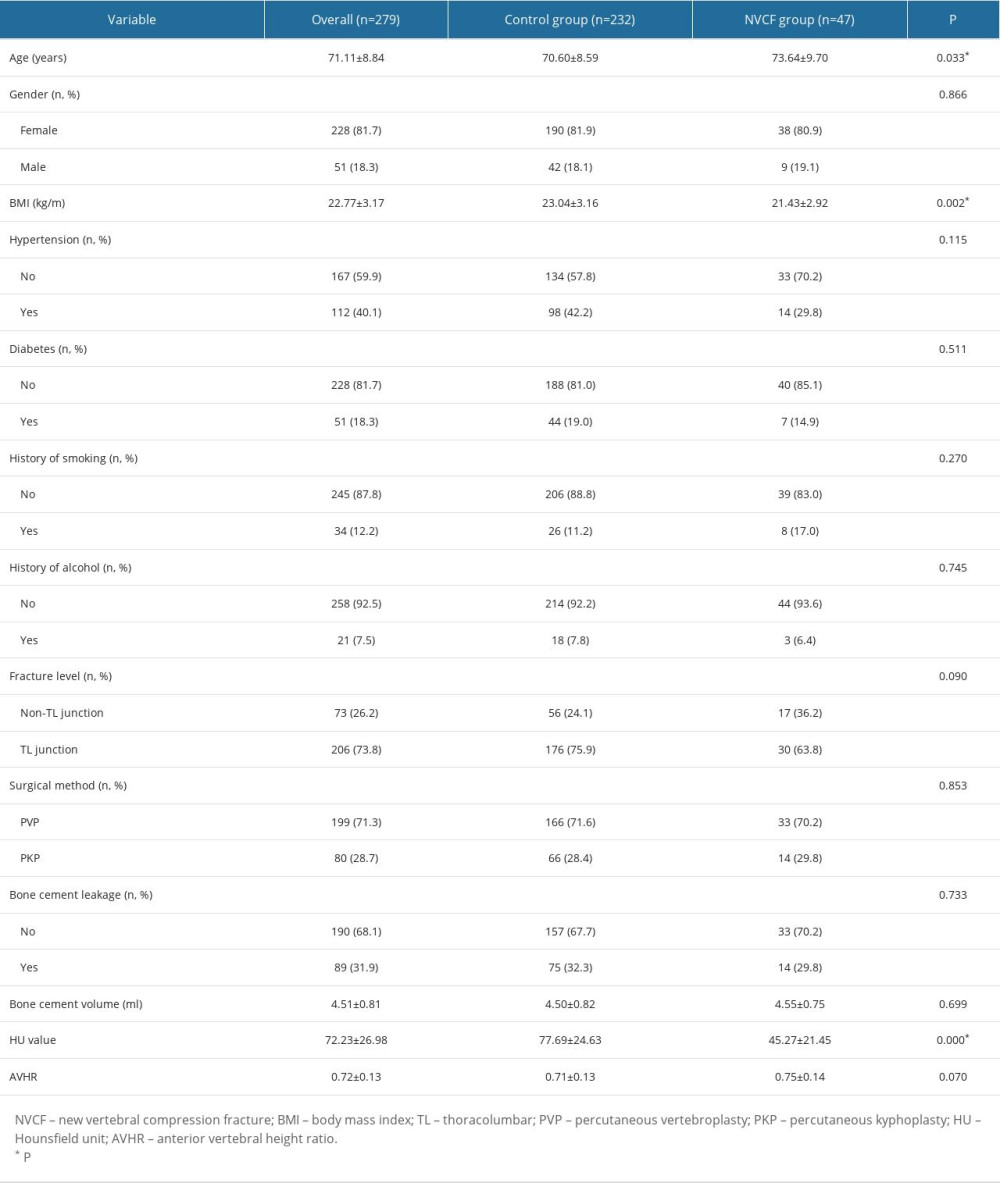
In this study, 279 patients, including 228 females and 51 males, were enrolled. The mean age was 71.11±8.84 years, the average of BMI was 22.77 ±3.17 kg/m2, and the mean HU value was 72.23±26.98. Among the overall patients, 47 (16.8%) patients with NVCF were included in the NVCF group, whereas 232 (83.2%) patients with no NVCF were enrolled in the control group. In the NVCF group, the mean age, BMI, and HU value of 47 patients, including 38 females and 9 males, were 73.64±9.70 years, 21.43±2.92 kg/m2 and 45.27±21.45, respectively. Of the 47 patients with NVCF, 30 patients fractured at the TL junction, whereas 17 cases fractured at the non-TL junction (Table 1).
There were no significant differences in sex (odds ratio [OR]=0.933, 95% confidence interval [CI]=0.419–2.077,
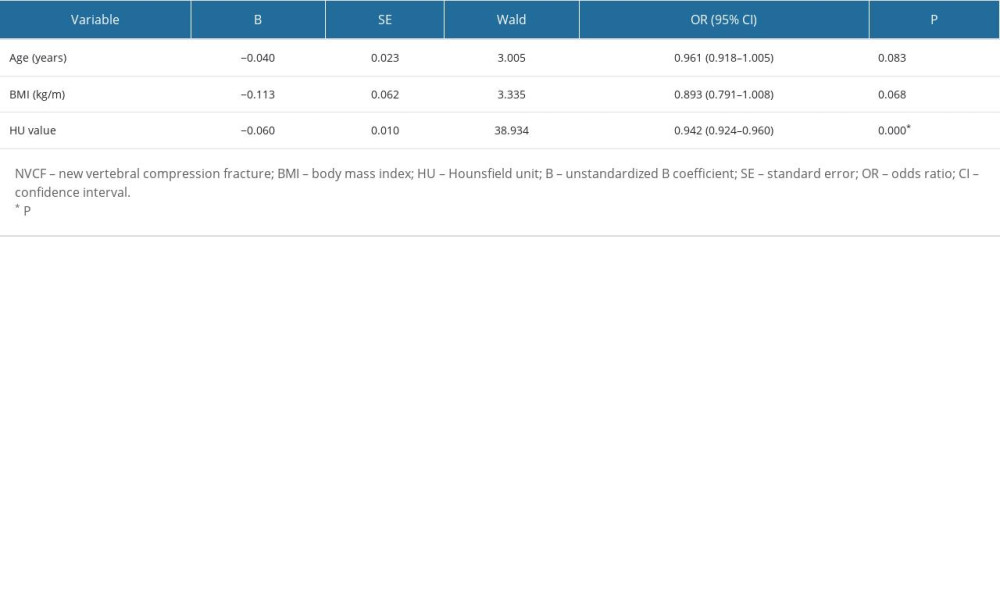
Multivariate regression analysis demonstrated that HU value (OR=0.942, 95% CI=0.924–0.960,
Discussion
NVCF after percutaneous vertebral augmentation may be a severe adverse event that cannot be ignored. According to the literature, the incidence of NVCF after percutaneous vertebral augmentation ranged from 6.5% to 34.8% [19–22]. The results of our study are similar to previous ones; there was 47 patients with NVCF after percutaneous vertebral augmentation for OVCF, and the incidence of NVCF was 16.8% in our study. Li et al [23] proved that the independent risk factors of NVCF after percutaneous vertebral augmentation were age, bone cement volume, bone cement leakage, and anti-osteoporotic treatment, but not BMI, HU value, and augmentation segment. However, in the current study, HU value was an independent risk factor for NVCF after percutaneous vertebral augmentation.
The mean age of the NVCF group was significantly older than that of the control group. However, age was not an independent risk factor for NVCF after percutaneous vertebral augmentation based on multivariate regression analysis. Some studies reported that age significantly increased the risk of NVCF [24,25], but Li et al [26] reported that no statistical difference was observed in age by logistic regression analysis. There may be a risk of bias in our study due to the limited sample size and retrospective design.
The results of this study demonstrated that the mean BMI of the NVCF group was significantly lower than that of the control group. Nevertheless, multivariate regression analysis revealed that BMI was not an independent risk factor for NVCF after percutaneous vertebral augmentation. Patients with low BMI have less bone mass, which seems to be associated with refracture. However, some studies revealed that BMI was not correlated with NVCF after percutaneous vertebral augmentation for OVCF [10,19]. A meta-analysis conducted by Zhai et al [27] showed that there was no association between BMI and secondary fracture in OVCF patients after percutaneous vertebral augmentation, which was consistent with the results of our study.
Previous studies showed that fracture level was not correlated with NVCF after percutaneous vertebral augmentation for OVCF [19,28,29]. However, a study of 371 patients demonstrated that TL junction fracture was an independent risk factor for NVCF development after PKP according to univariate and multivariate logistic analysis [30]. The TL junction is regarded as a transitional region in biomechanical anatomy [31], which seems to increase the risk of subsequent fracture. In our study, the results revealed that TL junction fracture was not a risk factor for NVCF after percutaneous vertebral augmentation.
HU value has been considered to be related to the occurrence of NVCF after percutaneous vertebral augmentation. In a retrospective review of 317 patients, Ji et al [32] found a significant correlation between HU value and refracture, and the HU value was also an independent risk factor of secondary fracture in patients treated by PVP or PKP for OVCF. Moreover, a clinical study conducted by Zhong et al [33] showed that lower HU value was an independent risk factor of NVCF in patients who underwent PVP based on multivariate regression analysis. The results of the present study revealed that low HU value was significantly associated with NVCF development and increased the risk of occurrence of NVCF after percutaneous vertebral augmentation.
The superiority of this study is that logistic regression analysis was used to test both risk factors with clear hypotheses and to explore the many suspected factors that are still unclear, and the study was relatively extensive. However, some limitations of this study are its retrospective study, including the small sample size, the risk of bias, and the significant dispersion of HU values. A prospective trial with large sample size will be conducted to further identify the risk factors for NVCF after percutaneous vertebral augmentation.
Conclusions
Hounsfield unit value was an independent risk factor for new vertebral compression fracture after percutaneous vertebral augmentation, whereas age and BMI were not.
References
1. Johnell O, Kanis JA, An estimate of the worldwide prevalence and disability associated with osteoporotic fractures: Osteoporos Int, 2006; 17(12); 1726-33
2. Bliuc D, Nguyen ND, Milch VE, Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women: JAMA, 2009; 301; 513-21
3. Kamei S, Noguchi T, Shida Y, The safety and efficacy of percutaneous vertebroplasty for patients over 90 years old: Jpn J Radiol, 2019; 37(2); 178-85
4. Clark W, Bird P, Gonski P, Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): A multicentre, randomised, double-blind, placebo-controlled trial: Lancet, 2016; 388; 1408-16
5. Sun HB, Jing XS, Shan JL, Risk factors for pulmonary cement embolism associated with percutaneous vertebral augmentation: A systematic review and meta-analysis: Int J Surg, 2022; 101; 106632
6. Xie W, Jin D, Ma H, Cement leakage in percutaneous vertebral augmentation for osteoporotic vertebral compression fractures: Analysis of risk factors: Clin Spine Surg, 2016; 29(4); E171-76
7. Xie W, Jin D, Wan C, The incidence of new vertebral fractures following vertebral augmentation: A meta-analysis of randomized controlled trials: Medicine, 2015; 94(37); e1532
8. Li HM, Zhang RJ, Gao H, New vertebral fractures after osteoporotic vertebral compression fracture between balloon kyphoplasty and nonsurgical treatment PRISMA: Medicine, 2018; 97(40); e12666
9. Dai C, Liang G, Zhang Y, Risk factors of vertebral re-fracture after PVP or PKP for osteoporotic vertebral compression fractures, especially in Eastern Asia: A systematic review and meta-analysis: J Orthop Surg Res, 2022; 17(1); 161
10. Mao W, Dong F, Huang G, Risk factors for secondary fractures to percutaneous vertebroplasty for osteoporotic vertebral compression fractures: A systematic review: J Orthop Surg Res, 2021; 16(1); 644
11. Jang S, Graffy PM, Ziemlewicz TJ, Opportunistic osteoporosis screening at routine abdominal and thoracic CT: Normative L1 trabecular attenuation values in more than 20 000 adults: Radiology, 2019; 291(2); 360-67
12. Pickhardt PJ, Pooler BD, Lauder T, Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications: Ann Intern Med, 2013; 158(8); 588-95
13. Zhao JG, Zeng XT, Wang J, Association between calcium or vitamin D supplementation and fracture incidence in community-dwelling older adults: A systematic review and meta-analysis: JAMA, 2017; 318(24); 2466-82
14. Krappinger D, Kastenberger TJ, Schmid R, Augmented posterior instrumentation for the treatment of osteoporotic vertebral body fractures: Oper Orthop Traumatol, 2012; 24(1); 4-12
15. Zou D, Zhang K, Ren Y, Therapeutic effects of PKP on chronic painful osteoporotic vertebral compression fractures with or without intravertebral cleft: Int J Clin Exp Med, 2015; 8(9); 15780-86
16. Vaeth M, Skovlund E, A simple approach to power and sample size calculations in logistic regression and Cox regression models: Stat Med, 2004; 23(11); 1781-92
17. Schreiber JJ, Anderson PA, Rosas HG, Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management: J Bone Joint Surg Am, 2011; 93; 1057-63
18. Lee SJ, Binkley N, Lubner MG, Opportunistic screening for osteoporosis using the sagittal reconstruction from routine abdominal CT for combined assessment of vertebral fractures and density: Osteoporos Int, 2016; 27(3); 1131-36
19. Lee BG, Choi JH, Kim DY, Risk factors for newly developed osteoporotic vertebral compression fractures following treatment for osteoporotic vertebral compression fractures: Spine J, 2019; 19(2); 301-5
20. Movrin I, Vengust R, Komadina R, Adjacent vertebral fractures after percutaneous vertebral augmentation of osteoporotic vertebral compression fracture: A comparison of balloon kyphoplasty and vertebroplasty: Arch Orthop Trauma Surg, 2010; 130(9); 1157-66
21. Ko BS, Cho KJ, Park JW, Early adjacent vertebral fractures after balloon kyphoplasty for osteoporotic vertebral compression fractures: Asian Spine J, 2019; 13(2); 210-15
22. Harrop JS, Prpa B, Reinhardt MK, Primary and secondary osteoporosis’ incidence of subsequent vertebral compression fractures after kyphoplasty: Spine, 2004; 29(19); 2120-25
23. Li Q, Long X, Wang Y, Development and validation of a nomogram for predicting the probability of new vertebral compression fractures after vertebral augmentation of osteoporotic vertebral compression fractures: BMC Musculoskelet Disord, 2021; 22(1); 957
24. Bergh C, Wennergren D, Möller M, Fracture incidence in adults in relation to age and gender: A study of 27,169 fractures in the swedish fracture register in a well-defined catchment area: PLoS One, 2020; 15(12); e0244291
25. Kanis JA, Johansson H, Harvey NC, The effect on subsequent fracture risk of age, sex, and prior fracture site by recency of prior fracture: Osteoporos Int, 2021; 32(8); 1547-55
26. Li W, Wang H, Dong S, Establishment and validation of a nomogram and web calculator for the risk of new vertebral compression fractures and cement leakage after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures: Eur Spine J, 2022; 31(5); 1108-21
27. Zhai G, Li A, Liu B, A meta-analysis of the secondary fractures for osteoporotic vertebral compression fractures after percutaneous vertebroplasty: Medicine, 2021; 100(16); e25396
28. Rho YJ, Choe WJ, Chun YI, Risk factors predicting the new symptomatic vertebral compression fractures after percutaneous vertebroplasty or kyphoplasty: Eur Spine J, 2012; 21(5); 905-11
29. Zhong BY, He SC, Zhu HD, Risk prediction of new adjacent vertebral fractures after PVP for patients with vertebral compression fractures: Development of a prediction model: Cardiovasc Intervent Radiol, 2017; 40(2); 277-84
30. Bian F, Bian G, Zhao L, Risk factors for recollapse of new vertebral compression fractures after percutaneous kyphoplasty in geriatric patients: Establishment of a nomogram: BMC Musculoskelet Disord, 2022; 23(1); 458
31. Holmes JF, Miller PQ, Panacek EA, Epidemiology of thoracolumbar spine injury in blunt trauma: Acad Emerg Med, 2011; 8(9); 866-72
32. Ji C, Rong Y, Wang J, Risk factors for refracture following primary osteoporotic vertebral compression fractures: Pain Physician, 2021; 24(3); E335-E40
33. Zhong BY, Wu CG, He SC, ANVCFV score system: Assessment for probability of new vertebral compression fractures after percutaneous vertebroplasty in patients with vertebral compression fractures: Pain Physician, 2015; 18(6); E1047-57
In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952