10 July 2023: Clinical Research
Effectiveness of Needle Aspiration versus Surgical Excision for Symptomatic Synovial Cysts of the Hip: A Single-Center, Retrospective Study
Kun Chu1ABCDEF, Liying He1B, Yuchuan Wang1C, Mengxuan Yao1D, Meng Yang1E, Sikai Liu1F, Zihang Li1D, Huijie Li1ABCD*DOI: 10.12659/MSM.940187
Med Sci Monit 2023; 29:e940187
Abstract
BACKGROUND: This study was performed to evaluate the clinical effectiveness of needle aspiration vs surgical excision for symptomatic synovial cysts of the hip.
MATERIAL AND METHODS: This retrospective study analyzed the clinical data of patients diagnosed with synovial cysts of the hip and treated in a single-center hospital from January 2012 to April 2022. Patients receiving needle aspiration were assigned to group A and those treated with surgery were assigned to group B. Demographic characteristics, etiology, symptoms, cyst location, postoperative complications and recurrence, Harris Hip Score (HHS) and Visual Analog Scale of Pain (VAS) scores before treatment and at 3, 6, and 12 months after treatment were recorded to assess hip function in both groups.
RESULTS: This study recruited 44 patients, with 18 patients in group A and 26 in group B, and the 2 arms were well-balanced in terms of baseline patient profiles. Needle aspiration resulted in significantly better pain mitigation for patients at 24 h, 48 h, and 72 h after treatment vs surgical interventions (P<0.05). Needle joint aspiration resulted in significantly better function restoration of the hip joint than surgery at 3 months after treatment, as evidenced by the lower HHS score of 85.31±13.16 in group A vs 78.51±11.66 in group B (P=0.002). Surgery was associated with a significantly lower incidence of disease relapse (0.00%) vs needle aspiration (27.7%) (P=0.004).
CONCLUSIONS: Needle aspiration in the treatment of symptomatic synovial cysts of the hip causes less damage to the soft tissue and leads to faster recovery in the short term than surgical resection. Surgical resection has a lower recurrence rate and better long-term efficacy.
Keywords: Synovial Cyst, Endoscopic Ultrasound-Guided Fine Needle Aspiration, Hip Joint, Synovial Fluid, Humans, Retrospective Studies, Neoplasm Recurrence, Local, Cysts, Treatment Outcome, Pain
Background
Synovial cysts commonly occur in the hands, feet, wrists, ankles, and knees but are less common in the hip joint [1]. Synovial cysts of the hip joint are usually diagnosed when patients present with a typical painful groin mass [1,2]. The absence of local clinical manifestations of the hip joint and the presence of unilateral lower-limb symptoms such as edema, abnormal sensation, varicose veins, cold feet, and deep vein thrombosis caused by cyst compression of the surrounding tissues frequently lead to underdiagnosis and misdiagnosis [3]. Synovial cysts that are not clinically evident in the local hip joint require ultrasonography, computed tomography (CT), or magnetic resonance imaging (MRI) of the hip for diagnosis [3]. Currently, research has summarized the characteristics and diagnosis of synovial cysts of the hip [4]. Synovial cysts of the hip are commonly managed by conservative treatment, needle aspiration, and surgical resection [4,5]. For asymptomatic or less symptomatic synovial cysts of the hip, conservative treatment is usually recommended, including reduction of hip movement, medication to reduce swelling and improve blood circulation, and local physiotherapy [5]. Needle aspiration or surgical excision is usually indicated for synovial cysts of the hip that are symptomatic or present with complications. Needle aspiration provides minimal invasiveness, rapid recovery, and easier manipulation. However, in large cysts, the aspirated cavity is difficult to occlude to the extent that long-term compression or even multiple manipulations are required [6]. Moreover, needle aspiration fails to address the underlying problem in synovial cysts that are comorbid with other hip diseases and are prone to recurrence [5,6]. Surgical excision of synovial cysts of the hip allows for complete eradication, but is more invasive, with greater postoperative pain and longer recovery [7,8]. Because of its rarity, the disease is mostly described in case reports, and there is still some controversy regarding the choice of treatment for symptomatic synovial cysts of the hip [6–8]. Few studies have investigated the benefits of needle aspiration and surgical resection for symptomatic synovial cysts of the hip. Therefore, in this study, we collected clinical data on these 2 different treatment options. The patients were divided into 2 groups according to treatment regimen, and the results were retrospectively compared and analyzed to assess them in the treatment of symptomatic synovial cysts of the hip joint. The results demonstrated that this strategy can mitigate the negative psychology of patients, improve the quality of life, and reduce the occurrence of complications.
Material and Methods
ETHICS STATEMENT:
This was a retrospective study with anonymous data and was approved by the Ethics Committee of our hospital (K2018-002-1), which waived the requirement of informed consent. All procedures involving human participants were performed in accordance with the guidelines of the 2013 Declaration of Helsinki.
INCLUSION AND EXCLUSION CRITERIA:
This retrospective study analyzed the clinical data of patients diagnosed with synovial cysts of the hip and treated at the Third Hospital of Hebei Medical University from January 2012 to April 2022. Patients receiving needle aspirations were assigned to group A, and those treated with surgery were assigned to group B.
Inclusion criteria were: (1) patients aged 18–80 years; (2) a final pathological diagnosis consistent with synovial cysts; (3) unilateral onset and treatment with needle aspiration or surgical excision; and (4) a follow-up period of more than 1 year.
Exclusion criteria were: (1) asymptomatic patients with synovial cysts without therapeutic intervention; (2) vital organ failures such as heart, brain, lung and liver; (3) malignant tumors; (4) incomplete medical records or radiological images. See Figure 1.
TREATMENT METHODS:
All procedures were performed by the same level of senior surgeons in charge. Before surgery, preoperative ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) were routinely performed according to the surgical plan to clarify the size, location, and relationship of the cyst to the surrounding tissue.
NEEDLE ASPIRATION TREATMENT PROCEDURE:
Patients in group A received needle aspiration. Preoperatively, routine sterilization and draping were performed, followed by local anesthesia. Depending on the location of the cyst, the location nearest the cyst to the epidermis was chosen for entry of the needle, and important vascular nerves around the cyst (eg, femoral artery, femoral vein, femoral nerve) were avoided. The injection was performed under Doppler ultrasound guidance. The cyst was aspirated after the needle tip entered the cyst, and the cyst fluid was collected and sent for pathological examinations. Pressure dressing was placed at the puncture site for 24 h.
SURGICAL PROCEDURES:
Patients in group B received surgical resection. Under general anesthesia or epidural anesthesia, a modified S-P incision of approximately 10 cm in length was made in the hip. Through the rectus femoris and broad facialis tensor, the lateral femoral nerve and blood vessels were protected, and the head of the rectus femoris muscle was retracted to reveal the anterior aspect of the joint capsule, where a cystic mass was visible. The cystic mass was removed, and the joint capsule was dissected longitudinally to remove the cystic sinus tract. The incision was closed layer by layer. One patient with rheumatoid arthritis and 1 patient with femoral head necrosis (ARCO stage IV) were treated with a total hip arthroplasty with a posterior-lateral approach to remove the cyst and the cyst wall. All tissues removed during surgery were sent for pathological examination (Figure 2A–2D).
POSTOPERATIVE MANAGEMENT AND REHABILITATION:
For patients treated with needle aspiration, the affected hip was pressure-bandaged for 24 h after treatment control local bleeding and cavity formation. After 24 h, appropriate functional exercise of the affected limb was allowed to prevent deep vein thrombosis of the lower limb.
Patients with surgically removed cysts were given low-molecular-weight heparin and appropriate functional exercises for the affected limbs postoperatively to prevent deep vein thrombosis in the lower limbs. Patients with comorbid rheumatoid arthritis were given methotrexate (15 mg/d orally) and methylprednisolone tablets (4 mg/d orally) postoperatively. Liver and renal function were assessed regularly, and the drug dose was adjusted until the maximum tolerated dose was reached. Patients with coexisting osteoarthritis were given postoperative treatment with celecoxib (200 mg daily orally) and glucosamine hydrochloride (0.75 g twice daily orally) for 3 months.
BASELINE PATIENT PROFILES COLLECTION:
Basic information on all patients before surgery was recorded, including sex, age, weight, height, body mass index (BMI), alcohol consumption, smoking, etiology, side, site of cyst development, ASA score, and complications.
CLINICAL OUTCOMES AND IMAGING ASSESSMENT:
All patients were followed up clinically and by imaging before and at 3, 6, and 12 months postoperatively, and annually thereafter. At each follow-up visit, the Harris Hip Score (HHS) score was measured to assess the patient’s recovery of hip function. Visual analog scale (VAS) results were collected pre- and postoperatively to assess pain. Imaging was performed with Doppler ultrasound to 24-month postoperative follow-up to compare the recurrence rates between the 2 groups. All clinical outcomes and imaging measurements (Doppler, VAS, HHS) were performed independently by 2 experienced orthopedic surgeons. Wang was responsible for the VAS scores at 24 h, 48 h, and 72 h postoperatively and for the measurement of HHS scores preoperatively and at the final follow-up at 3 months, 6 months, 1 year, 2 years, and postoperatively. Yang was responsible for postoperative Doppler imaging and postoperative recurrence statistics.
SAMPLE SIZE CALCULATION:
This experiment mainly took the measurement of VAS score as the main objective index, and used the hypothesis test of 2 groups of overall mean. According to the pre-experiment, the mean VAS scores of group A and group B after treatment were 1.33 and 2.17, respectively, and the standard deviation was 0.8. With α=0.05(2-sided test), power=1−β=0.80, group A: group B=2: 3, the sample size was estimated using PASS 2021 software using the following formula:
(n1: n2=1: k). According to the preset parameters, a total of 33 cases needed to be included after the VAS scores were calculated by using the 2-sample
STATISTICAL METHODS:
All data were statistically analyzed using SPSS 20.0 (IBM, Armonk, USA). Continuous variables were expressed as mean±standard deviation, and categorical variables were expressed as counts and percentages. Data normality was tested using the Shapiro-Wilk test and categorical variables were compared between the 2 groups using the chi-square test or Fisher’s exact probability method, as appropriate. Non-normally distributed variables were analyzed using the Mann-Whitney test. Continuous variables were compared between the 2 groups using the
Results
BASELINE PATIENT PROFILES:
Between January 2012 and April 2022, we collected the clinical data of 18 patients treated with puncture needle aspiration and 26 patients treated with surgical resection. In this study, we retrospectively analyzed the database of patients with a final pathological diagnosis of hip synovial cyst treated with puncture needle aspiration or surgical resection in the Third Hospital of Hebei Medical University, from which 46 patients were extracted, and 2 cases were excluded due to incomplete medical records or radiological images. Finally, a total of 44 patients (24 males and 20 females) were enrolled in this study, with 18 patients treated with puncture needle aspiration (Group A) and 26 patients treated with surgical resection (Group B). The mean age in Group A was 45.88±12.41 years and in Group B it was 42.43±10.60 years. The age distribution in the 2 groups was well-balanced (P=0.351). The BMI in group A and group B was also comparable (25.41±2.25 kg/m2 vs 24.65±3.77, P=0.077). Other baseline data such as smoking, alcohol consumption, affected side, etiology, site of cyst development, ASA score, and follow-up time were also homogenous (P>0.05) (Table 1).
VAS SCORES: The preoperative VAS score was 3.57±1.16 in Group A and 3.63±1.29 in Group B (P=0.735). Needle aspiration resulted in significantly better pain mitigation for patients at 24 h (3.76±1.21 vs 4.57±1.32, P=0.003), 48 h (2.74±1.16 vs 3.33±1.27, P=0.001), and 72 h (1.27±0.86 vs 2.23±0.79, P=0.000) after treatment vs surgical interventions, as shown by the lower VAS scores in group A (P<0.05) (Table 2).
HHS SCORES:
The preoperative HHS score was comparable between the 2 groups (74.20±11.45 vs 73.39±12.21) (P>0.05). Needle aspiration resulted in significantly better function restoration of the hip joint than surgery at 3 months after treatment, as evidenced by the lower HHS score of 85.31±13.16 in group A vs 78.51±11.66 in group B (P=0.002). Such significant differences disappeared at 6 months after treatment (P>0.05) and re-emerged at 2 years after interventions (83.26±6.77 vs 94.05±7.29, P<0.05), suggesting good long-term effectiveness of surgery for synovial cysts of the hip in joint function restoration (Table 3).
COMPLICATIONS AND RELAPSE: There was no significant difference in the complication rates between the 2 groups (11.1% vs 11.5%). One case (5.5%) of femoral vein injury in group A presented with postoperative subcutaneous petechiae and soft-tissue hematoma in the groin, which gradually improved after 24 h of wound compression dressing of the affected hip. Subsequent repeat venous ultrasound of the lower limbs also indicated patency of the deep veins of the lower limbs. The remaining complications are shown in Table 4. Surgery was associated with a significantly lower incidence of disease relapse (0.00%) vs needle aspiration (27.7%) (P=0.004) (Table 4).
Discussion
Management of asymptomatic synovial cysts of the hip has largely been established with regular observation and review, whereas the Stiglich optimal regimen for symptomatic synovial cysts of the hip remains debated [9,10]. Studies have shown that for symptomatic synovial cysts of the hip, ultrasound-guided needle aspiration provides less trauma, faster recovery, mild pain, and a significant reduction in cyst size and symptoms [11,12]. However, needle aspiration fails to provide a complete cure for symptomatic synovial cysts of the hip and is prone to recurrence after surgery, especially in patients with other disorders of the hip. Surgical resection is a more reliable technique than needle aspiration for preventing postoperative recurrence [7,8,13]. Because of its rarity, there are few reports about this disease in China and abroad, and most have been case reports. Therefore, we conducted this retrospective study to determine whether needle aspiration in the treatment of symptomatic synovial cysts of the hip is superior to surgical resection in terms of functional recovery and pain control, and whether there are differences in postoperative complications and recurrence rates. The most important finding in our study was that 3-month functional outcomes were better with needle aspiration compared with surgical resection. However, both groups showed similar functional outcomes 6 months after surgery. But at 2 years after surgery, the function of surgical resection was better than that of needle aspiration. In this study, patients treated with needle aspiration had better short-term recovery of hip function, while recurrence was lower in patients treated with surgical excision.
The better functional scores at 3 months postoperatively may be attributed to the minimization of soft tissue and muscle damage by needle aspiration. A study has shown that needle aspiration under ultrasound guidance allows easy differentiation of the relationship between the cystic mass and the surrounding soft tissue, identifying vascularized and non-vascularized areas and minimizing collateral damage. In addition, needle aspiration carries no increased risk of exposure to radiation, frequent bleeding, irreversible damage to neurovascular structures, or the harmful effects of general anesthesia [14]. Another study with similar results to this study showed that the ultrasound-guided needle aspiration method was safe and reliable, simple to perform, less damaging to organ tissue or blood vessels, and caused milder pain [15]. The better functional outcome at 3 months postoperatively with ultrasound-guided needle aspiration vs surgical resection may be attributable to the significantly less serious soft-tissue damage caused by needle aspiration. As the soft tissues recovered, the hip function demonstrated similar functional outcomes at various time points after 6 months postoperatively. In addition, in the early postoperative period, needle aspiration provided better pain relief compared to surgical resection. We reviewed the literature and found no studies comparing needle aspiration with surgical resection for postoperative pain in synovial cysts of the hip. Despite the small number of patients included, this study had the largest sample size of this type of study. The results of the present study showed that needle aspiration gave more significant pain relief than surgical excision at 72 h postoperatively. This may be related to the following factors. Surgical excision requires a layer-by-layer dissection of the skin and subcutaneous tissue and dissection of adjacent structures around the cyst to provide a clear field or to facilitate surgical manipulation, thereby increasing damage to tissue surrounding the cyst. All these will have an adverse impact on postoperative pain recovery of patients. Under the guidance of ultrasound, the best puncture point can be accurately found according to the size, edge, capsule, aspect ratio, and other morphological characteristics of the tumor before puncture needle aspiration, and the percutaneous route direct to the cyst site can minimize the muscle and soft-tissue damage around the cyst. Compared with surgical resection, needle aspiration is simpler, faster, and less traumatic.
The higher incidence of recurrence with needle aspiration compared to surgical resection may be attributed to the pathogenesis of synovial cysts of the hip. A study has shown that synovial cysts of the hip develop as a result of subtle congenital or developmental defects in the hip joint capsule. Fluid accumulation in the joint (eg, active synovitis or joint injury) leads to increased intra-articular pressure, which consequently causes progressive formation and enlargement of synovial cysts in weak areas [16]. Another study has demonstrated that when pressure increases around the hip joint, an abnormal increase in synovial fluid can flow into the iliopsoas muscle bursa, resulting in enlargement of the hip bursa, bursal hypertrophy, and synovial villous hyperplasia [17]. In the absence of a direct connection between the hip and the iliopsoas muscle capsule, periarticular tissue necrosis due to degenerative and rheumatoid changes in the hip may lead to communication between the hip and the iliopsoas muscle capsule, resulting in synovial cysts of the hip [17]. This suggests that synovial cysts of the hip are comparable to a herniation of the joint capsule. The significantly higher recurrence rate of needle aspiration vs surgical resection may be attributed to the fact that needle aspiration fails to intervene in the hernia sac, and the increased pressure and abnormal increase in synovial fluid in the joint capsule at a later stage may lead to recurrence. Surgical excision allows complete removal of the synovial cyst and closure of the hernia sac and minimizes recurrence of the cyst, which is consistent with the results of previous studies [7,8,13]. Colasanti et al [18], in a study of treatment for 27 symptomatic synovial cysts, found that surgical excision had a lower recurrence rate (5%) than puncture needle aspiration (37%). However, the sample size of their study was smaller than ours, and the evidence in the present study is more convincing. Other studies suggest that puncture needle aspiration therapy in the treatment of symptomatic hip synovial cysts associated with other diseases of the hip (eg, osteoarthritis, rheumatoid arthritis, femoral head necrosis) can alleviate patients’ symptoms [19]. Nevertheless, the recurrence rate in these patients was not calculated in these studies, and the clinical efficacy of puncture needle aspiration was not compared with surgical excision. The present study concluded that 5 patients with postoperative recurrence were all found in the needle aspiration group, with the time of recurrence was 14–24 months postoperatively. This may also account for the lower functional scores of needle aspiration compared to surgical resection at 2 years postoperatively. Of the 5 patients who relapsed after needle aspiration, 3 had femoral head necrosis, 1 had rheumatoid arthritis, and 1 had no apparent cause. Despite targeted and systematic treatment of the primary disease in patients with a clear etiology before and after needle aspiration, the long-term outcome was unsatisfactory, with recurrence after 1 year. This suggests that puncture needle aspiration in symptomatic hip synovial cysts with other diseases of the hip joint is associated with a higher recurrence rate. On the whole, the present study demonstrates that surgical resection in the treatment of symptomatic synovial cysts of the hip is associated with a lower incidence of recurrence and a more favorable long-term outcome than needle aspiration.
With the development of medicine, the concept of minimally invasive and rapid rehabilitation is increasingly accepted. Although surgical resection is currently preferred in management of symptomatic hip synovial cyst, puncture needle aspiration is still superior to surgical resection in short-term functional recovery of the hip joint, and there is a possibility of being cured with puncture needle aspiration. Moreover, it is easy to perform and only causes minor soft-tissue damage, hence puncture needle aspiration is a potential strategy for patients with synovial cysts with no other hip joint diseases. In patients with symptomatic synovial cysts with osteoarthritis, rheumatoid arthritis, or other hip diseases, surgery provides favorable long-term outcomes for hip function and remains the preferred option for improving hip function and preventing recurrence.
Several limitations to this study should be mentioned. First, the sample size was small due to the characteristic of retrospective design. Prospective studies with larger sample sizes and longer follow-ups are needed to determine whether puncture needle aspiration is superior or equivalent to surgical resection. In addition, all procedures in this study were performed by surgeons with equivalent qualifications, which may bias the results due to their surgical experience. Given these limitations, the results must be interpreted with caution. The strength, however, should also be highlighted. To the best of our knowledge, the present study is one of a handful of retrospective comparative studies on the clinical efficacy of puncture needle aspiration and surgical resection. It might provide a novel choice of treatment modality for symptomatic synovial cysts.
Conclusions
In the management of symptomatic synovial cysts of the hip, needle aspiration causes less damage to the soft tissues than surgical excision, results in a faster early postoperative recovery, and provides significant short-term relief of symptoms, but has a higher incidence of recurrence. Although surgical resection has a slower recovery of hip function than needle aspiration in the short term, the risk of recurrence is lower and the treatment effect is better.
Figures
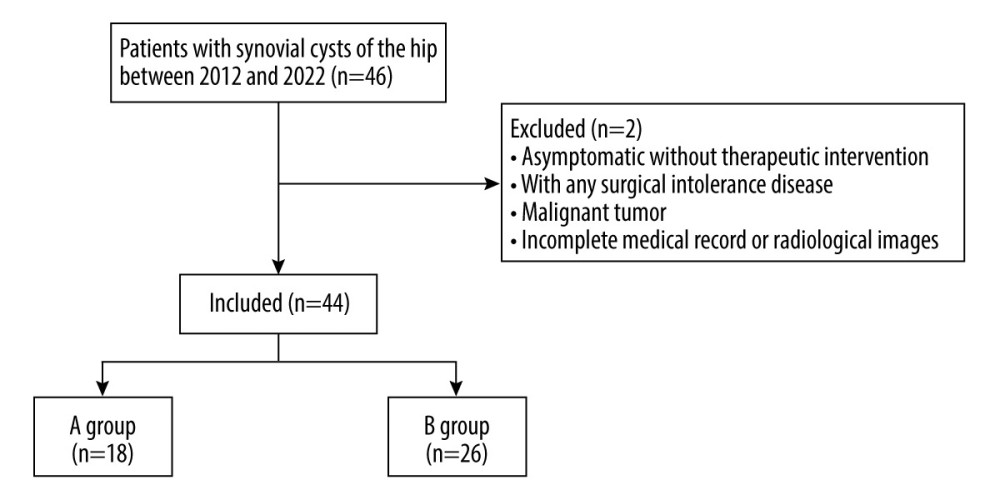 Figure 1. The process of screening patients.
Figure 1. The process of screening patients. 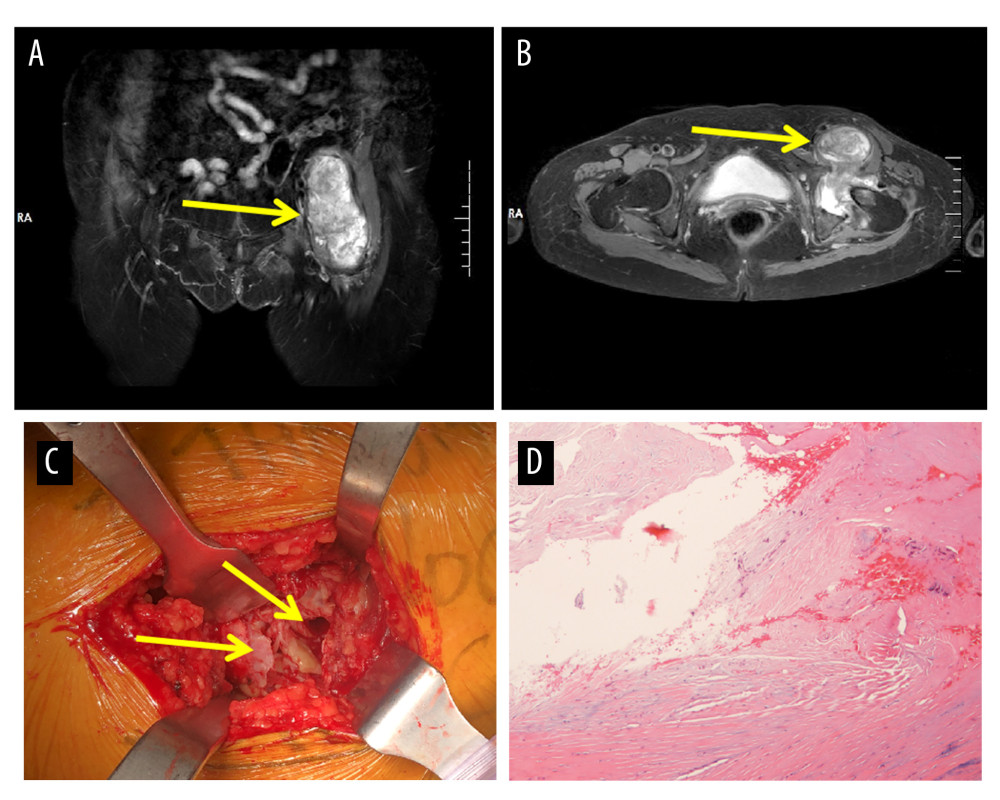 Figure 2. (A) A large cystic mass anterior to the joint capsule is seen in the coronal view of the preoperative hip MRI. (B) A large cystic mass in the anterior aspect of the joint capsule is visible in the preoperative MRI level of the hip joint. (C) Intraoperatively, a large amount of abnormally enlarged synovial membrane is seen around the hip joint, communicating with the joint capsule. (D) Postoperative pathological findings showing synovial cysts of the hip.
Figure 2. (A) A large cystic mass anterior to the joint capsule is seen in the coronal view of the preoperative hip MRI. (B) A large cystic mass in the anterior aspect of the joint capsule is visible in the preoperative MRI level of the hip joint. (C) Intraoperatively, a large amount of abnormally enlarged synovial membrane is seen around the hip joint, communicating with the joint capsule. (D) Postoperative pathological findings showing synovial cysts of the hip. References
1. Coventry MB, Polley HF, Weiner AD, Rheumatoid synovial cyst of the hip; Report of three cases: J Bone Joint Surg Am, 1959; 41-A(4); 721-30 passim
2. Ehrlich GE, Antecubital cysts in rheumatoid arthritis – a corollary to popliteal (Baker’s) cysts: J Bone Joint Surg Am, 1972; 54(1); 165-69
3. Stuplich M, Hottinger AF, Stoupis C, Sturzenegger M, Combined femoral and obturator neuropathy caused by synovial cyst of the hip: Muscle Nerve, 2005; 32(4); 552-54
4. Angelini A, Zanotti G, Berizzi A, Synovial cysts of the hip: Acta Biomed, 2018; 88(4); 483-90
5. Wang HC, Current status of clinical research on Chinese and Western medicine in hip synovitis: Rheumatology and Arthritis, 2013; 2(5); 63-66
6. Yukata K, Arai K, Yoshizumi Y, Obturator neuropathy caused by an acetabular labral cyst: MRI findings: Am J Roentgenol, 2005; 184(3 Suppl); S112-14
7. Diel R, Tuschick B, Hamborg V, Krüger CEnlarged iliopsoas bursa. Possible significance and place of computed tomography and sonography: Der Radiologe, 1990; 30(11); 547-49 [in German]
8. Mori S, Tamura T, Komatsubara S, A case of femoral nerve palsy caused by iliopectineal bursitis associated with rheumatoid arthritis: Mod Rheumatol, 2004; 14(3); 274-78
9. Binek R, Levinsohn EM, Enlarged iliopsoas bursa. An unusual cause of thigh mass and hip pain: Clin Orthop Relat Res, 1987(224); 158-63
10. Tebib JG, Dumontet C, Carret JP, Synovial cyst of the hip causing iliac vein and femoral nerve compression: Clin Exp Rheumatol, 1987; 5(1); 92-93
11. Armstrong P, Saxton H, Ilio-psoas bursa: Br J Radiol, 1972; 45(535); 493-95
12. Savarese RP, Kaplan SM, Calligaro KD, DeLaurentis DA, Iliopectineal bursitis: An unusual cause of iliofemoral vein compression: J Vasc Surg, 1991; 13(5); 725-27
13. Tokita A, Ikari K, Tsukahara S, Iliopsoas bursitis-associated femoral neuropathy exacerbated after internal fixation of an intertrochanteric hip fracture in rheumatoid arthritis: A case report: Mod Rheumatol, 2008; 18(4); 394-98
14. Scattergood S, Moore S, Prior A, Percutaneous drainage of a parotid gland abscess under contrast-enhanced ultrasound guidance: A case report: Ultrasound, 2018; 26(3); 182-86
15. Chen LL, Chen LD, Study on the value of ultrasound-guided puncture biopsy in the diagnosis of superficial organ disease: Electronic Journal of Clinical Medicine Literature, 2014; 1(14); 2842-43
16. Sartoris DJ, Danzig L, Gilula L, Synovial cysts of the hip joint and iliopsoas bursitis: A spectrum of imaging abnormalities: Skeletal Radiol, 1985; 14(2); 85-94
17. Warren R, Kaye JJ, Salvati EA, Arthrographic demonstration of an enlarged iliopsoas bursa complicating osteoarthritis of the hip. A case report: J Bone Joint Surg Am, 1975; 57(3); 413-15
18. Colasanti M, Sapienza P, Moroni E, An unusual case of synovial cyst of the hip joint presenting as femoral vein compression and severe lower limb edema: Eur J Vasc Endovasc Surg, 2006; 32(4); 468-70
19. Byström S, Adalberth G, Milbrink J, Giant synovial cyst of the hip: An unusual presentation with compression of the femoral vessels: Can J Surg, 1995; 38(4); 368-70
Figures
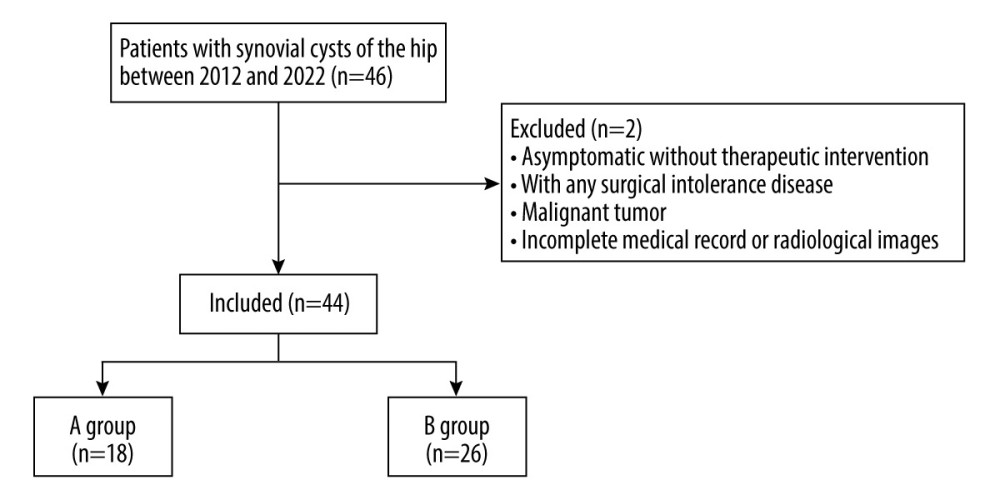 Figure 1. The process of screening patients.
Figure 1. The process of screening patients.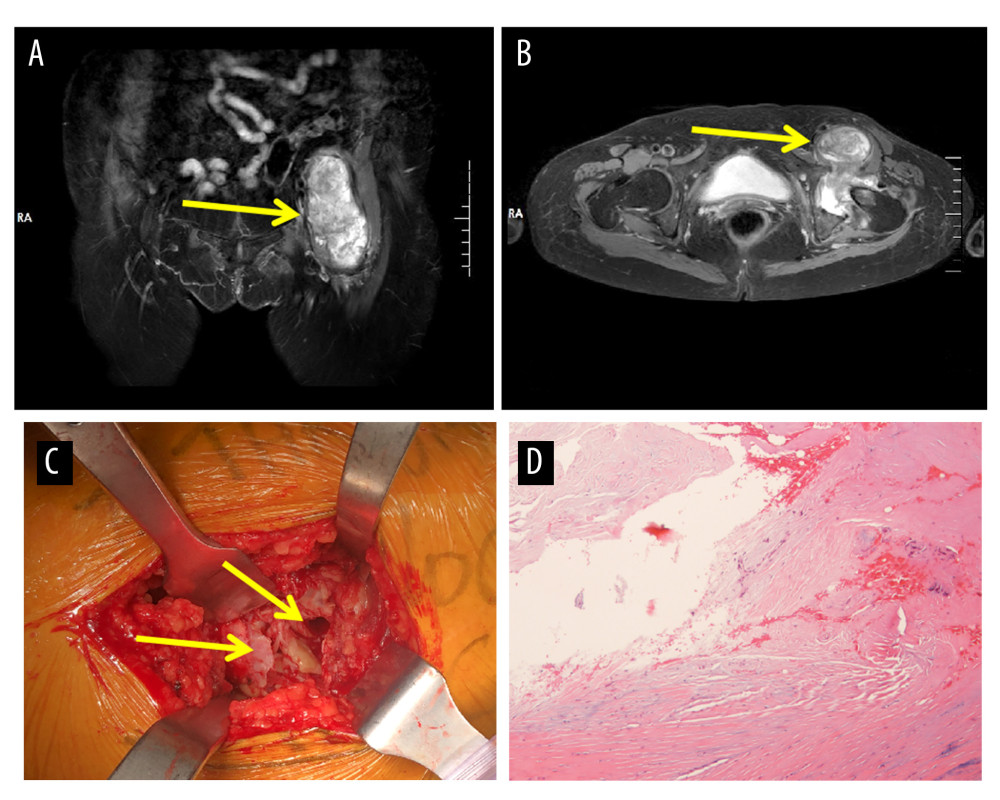 Figure 2. (A) A large cystic mass anterior to the joint capsule is seen in the coronal view of the preoperative hip MRI. (B) A large cystic mass in the anterior aspect of the joint capsule is visible in the preoperative MRI level of the hip joint. (C) Intraoperatively, a large amount of abnormally enlarged synovial membrane is seen around the hip joint, communicating with the joint capsule. (D) Postoperative pathological findings showing synovial cysts of the hip.
Figure 2. (A) A large cystic mass anterior to the joint capsule is seen in the coronal view of the preoperative hip MRI. (B) A large cystic mass in the anterior aspect of the joint capsule is visible in the preoperative MRI level of the hip joint. (C) Intraoperatively, a large amount of abnormally enlarged synovial membrane is seen around the hip joint, communicating with the joint capsule. (D) Postoperative pathological findings showing synovial cysts of the hip. Tables
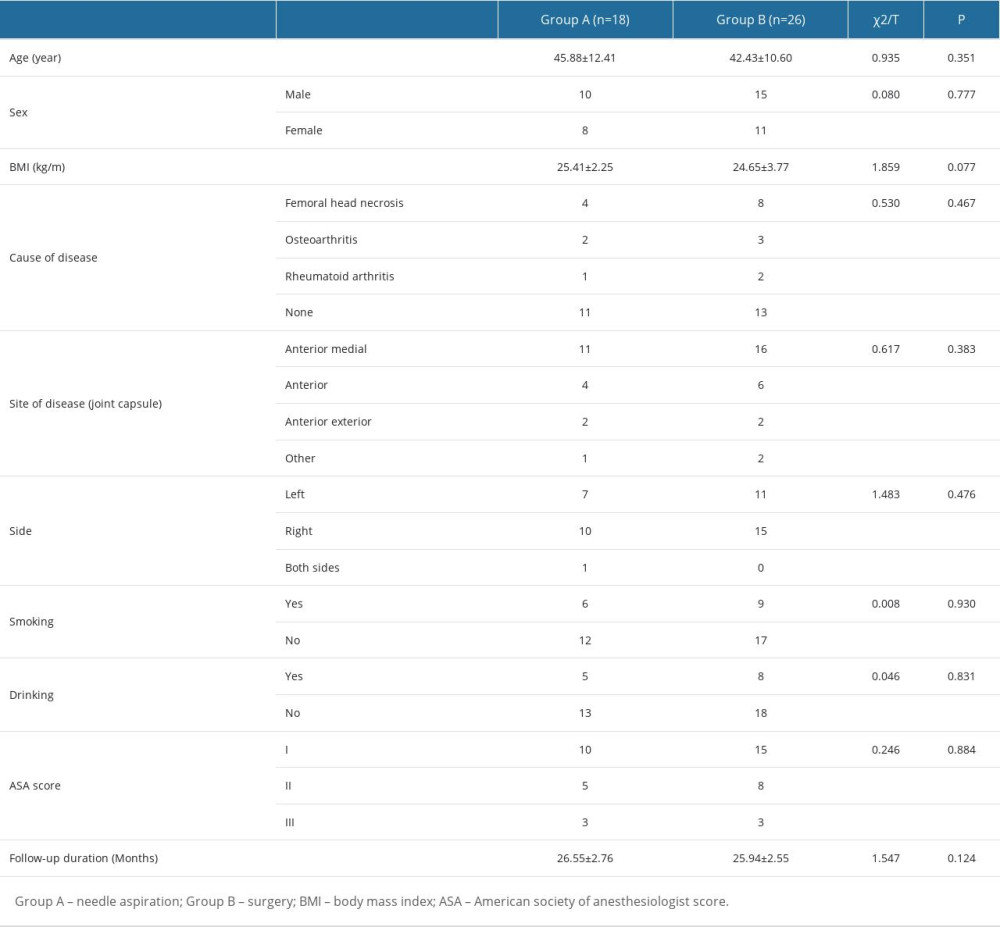 Table 1. Baseline patient profiles.
Table 1. Baseline patient profiles.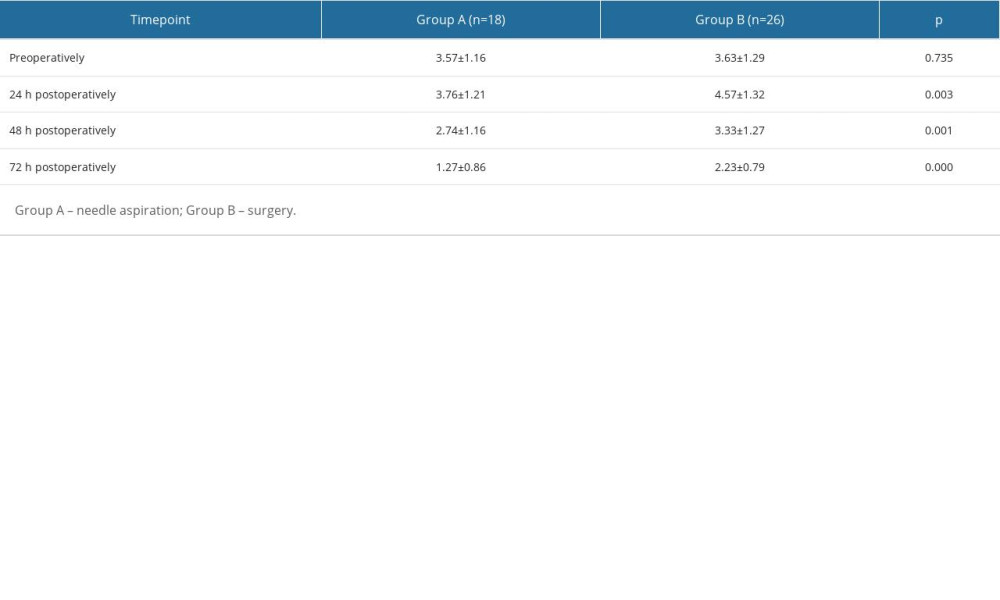 Table 2. Preoperative and postoperative VAS scores.
Table 2. Preoperative and postoperative VAS scores. Table 3. Preoperative and postoperative HHS scores.
Table 3. Preoperative and postoperative HHS scores. Table 4. Complications and relapse.
Table 4. Complications and relapse.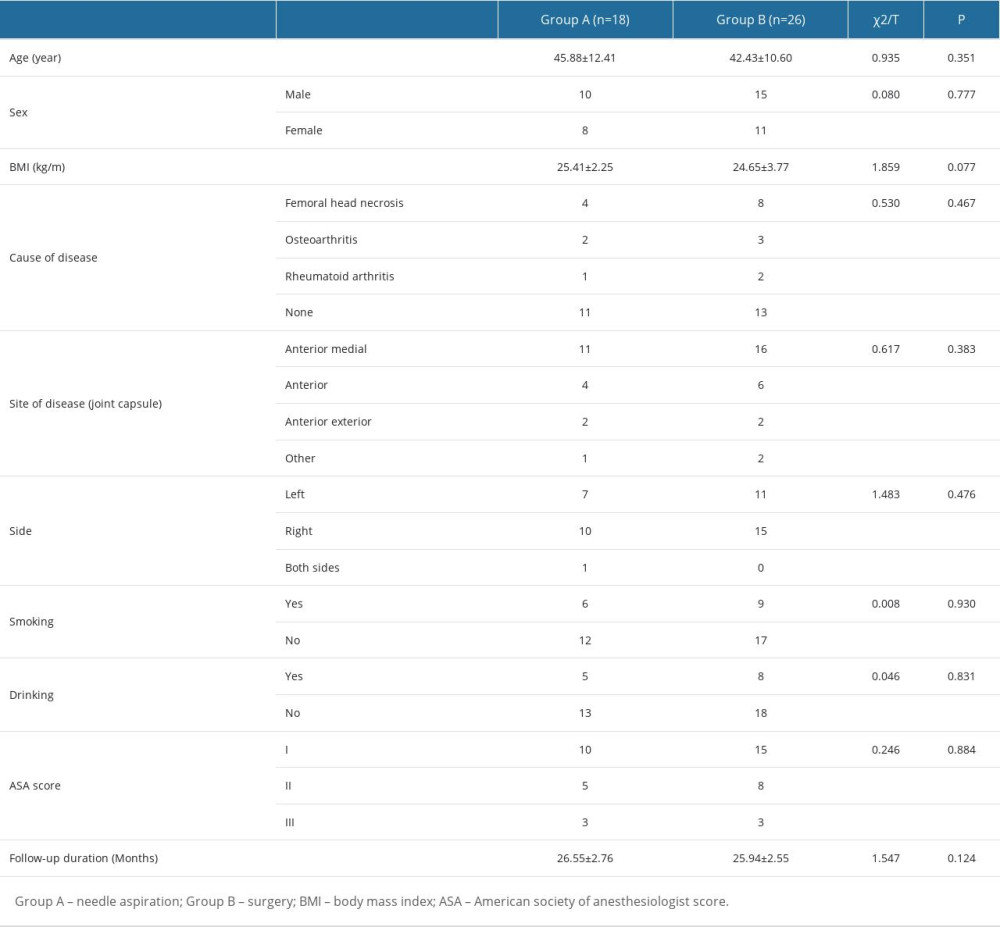 Table 1. Baseline patient profiles.
Table 1. Baseline patient profiles.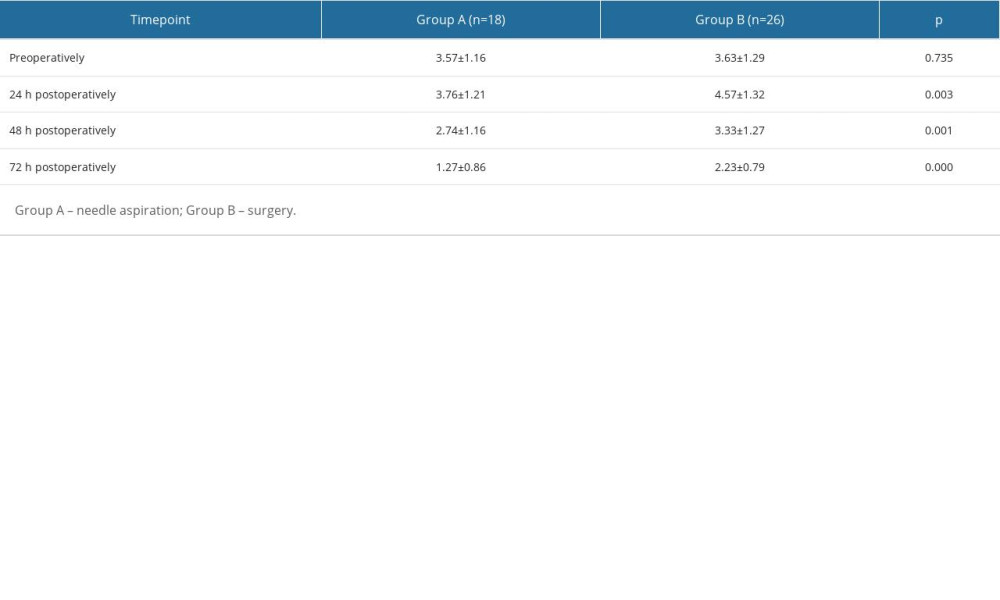 Table 2. Preoperative and postoperative VAS scores.
Table 2. Preoperative and postoperative VAS scores. Table 3. Preoperative and postoperative HHS scores.
Table 3. Preoperative and postoperative HHS scores. Table 4. Complications and relapse.
Table 4. Complications and relapse. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








