26 June 2023: Database Analysis
Association Between Alcohol Consumption and Cardiovascular Risk Based on Data from the Three Generations for Health Program in Hungary
Gergő József SzőllősiDOI: 10.12659/MSM.940327
Med Sci Monit 2023; 29:e940327
Abstract
BACKGROUND: Alcohol consumption has a significant effect on cardiovascular health, and risk factors, such as excessive alcohol use, should be avoided. Although alcohol consumption has decreased over the last decade in Hungary, it is still significantly higher than the average across the European Union. The objective of this study was to describe the patterns of alcohol use based on the Alcohol Use Disorders Identification Test (AUDIT), with a special focus on cardiovascular risk status (low, moderate, high, or very high).
MATERIAL AND METHODS: The Three Generations for Health program focuses on the development of primary health care in Hungary. One of the key elements of the program is the identification of risk factors of cardiovascular diseases. An ordinal multiple logistic regression analysis was performed with 10 categorical explanatory variables and the outcome was the categorical cardiovascular risk.
RESULTS: The database consisted of patients aged 40-65 years with a sample size of 11 348. A significant relationship was found between alcohol consumption and cardiovascular risk status; people with high-risk drinking patterns had higher a value of odds ratio (OR=1.306 [1.003-1.701]) for having a more serious cardiovascular status. According to multiple regression analysis, alcohol dependence was associated with cardiovascular risk.
CONCLUSIONS: From a public health perspective, the results highlight the importance of reducing alcohol consumption with the help of primary care and preventive services in countries with a high cardiovascular risk profile to reduce the cardiovascular disease-related burden.
Keywords: Alcoholism, Heart Disease Risk Factors, Primary Prevention
Background
THREE GENERATIONS FOR HEALTH PROGRAM:
Three Generations for Health program is managed by the National Directorate General for Hospitals with the support of the Gottsegen György National Cardiovascular Center of Hungary. Its main goals, such as reducing mortality from coronary heart disease and cardiovascular diseases, are in line with the objectives of the Health Sector Strategy of Hungary [27]. The Three Generations for Health program focuses on the development of primary health care and cooperation between the participants involved in primary health care while simultaneously cooperating with the Health Promotion Offices and local governments [27]. One of the key elements of the program is the identification of risk factors of cardiovascular disease, where lifestyle factors, such as alcohol consumption, play an important role. In addition to assessing the population’s cardiovascular risks, this program also aims to introduce healthy lifestyle routines and practical methods of primary prevention.
The first aim of this study was to describe the patterns of alcohol usage based on the Alcohol Use Disorders Identification Test (AUDIT), with a special focus on cardiovascular risk status [28]. The second aim was to identify the adjusted effect of alcohol dependence on cardiovascular risk status based on the database of the Three Generations for Health program.
Material and Methods
ETHICS STATEMENT:
The study was conducted according to the guidelines of the Declaration of Helsinki with the respect of the Regulation 2016/679 – Protection of natural persons with regard to the processing of personal data and on the free movement of such data and repealing Directive 95/46/EC (General Data Protection Regulation). Informed consent was obtained from all subjects participating in the Three Generations for Health program. According to the Medical Research Council, no approval from an ethics committee was needed because all procedures were carried out in compliance with the applicable standards and regulations, paying full regard to the decision made by the government.
DATABASE:
The database consisted of patients aged 40–65 years who participated in the Three Generations for Health program between 2019 and 2022, with an initial sample size of 12 556. The final sample size was 11 348 because we omitted respondents who did not have data related to alcohol consumption (n=51) and for which cardiovascular score could not be calculated due to missing data (n=1157). The program’s sample inclusion was performed consecutively by the participating general practitioners (GPs). This means that patients in the age group of our study who had a consultation with their doctor for any reason were enrolled in the study, as long as they agreed to participate and gave their informed consent after being given all the relevant information.
The anamnestic data of the participating patients, several vital parameters obtained during physical examination performed in the GP practices, and the results of relevant laboratory tests were recorded. The data were provided by the participating practices through a dedicated online interface (Icardio) from which the data were recorded in a non-identifiable way for analysis. Each data set remained linked to the patient who it belonged to, and their identity could be determined by their own GP if necessary. The 2 main outcomes were cardiovascular risk and risk identification related to alcohol consumption.
IDENTIFICATION OF CARDIOVASCULAR RISK:
Cardiovascular risk was established by the 2016 European Guidelines on cardiovascular disease prevention in clinical practice and endorsed by the Hungarian Cardiovascular Consensus Conference. The following 4 cardiovascular risk categories were identified: low, moderate, high, and very high. People at low risk had a HeartScore lower than 1%, while people at moderate risk had a HeartScore between 1% and 5% at 10 years. High-risk people had elevated risk factors, such as total cholesterol >8 mmol/l, blood pressure over 180/110 mmHg, diabetes mellitus, glomerular filtration rate 30–59 mL/min/1.73 m2, and HeartScore between 5% and 10%. People at very high risk had a calculated HeartScore over 10%, severe chronic kidney disease (glomerular filtration rate <30 mL/min/1.73 m2), diabetes mellitus with end-organ damage (eg, proteinuria, hypercholesterolemia, hypertension), or documented cardiovascular diseases (eg, acute myocardial infarction or transient ischemic attack).
MEASURE OF ALCOHOL CONSUMPTION:
The self-reported AUDIT was used and calculated among the respondents. The screening tool contains 10 questions; the possible scores are between 0 and 4 per question, and the range of the possible scores is from 0 to 40. Lower scores indicate abstainers and low-risk alcohol consumers, while higher scores indicate harmful alcohol use or alcohol dependence. Regarding the scoring of the questionnaire, people with 0–7 points were considered low risk, 8–14 were considered hazardous, and 15–40 were considered alcohol-dependent.
DATA ANALYSIS:
In the present analysis, the differences between categorical variables were analyzed by Pearson’s chi-squared tests and Fisher’s exact test. Ordinal multiple logistic regression analysis was performed with 10 categorical explanatory variables (gender, age group, smoking status, total cholesterol, HDL cholesterol, LDL cholesterol, body mass index, glomerular filtration rate, systolic blood pressure, and AUDIT score), and the outcome was the categorical cardiovascular risk (low, moderate, high, or very high). The reference level in the model was low cardiovascular risk. Data analysis was performed using Stata software version 9.0 (Stata Corp., College Station, TX, USA). The results were considered significant if
Results
DESCRIPTIVE STATISTICS:
There were 5 043 (44%) males and 6 305 (56%) females in our study. Most people were from the age group of 60–64 years (n=3114, 27%), while 2440 (22%) were from the age group of 55–59 years and 2385 (21%) from the age group of 50–54 years. The lowest proportion of participants were in the age groups of 40–44 and 45–49 years, which contained 1359 (12%) and 2050 (18%) people, respectively. In the sample, 2820 (25%) people were daily smokers and 628 (6%) were considered as occasional smokers. Overweight or obesity affected 8153 (72%) of the respondents. Decreased kidney function measured with glomerular filtration rate lower than 30 mmol/L/1.73 m2 affected 45 participants. Elevated total cholesterol level was observed in 9471 (83%) people, while 1877 (17%) people had total cholesterol <4.5 mmol/l. Elevated blood pressure was noted in 3540 (31%) people, and 7808 (69%) people had normal blood pressure. Regarding cardiovascular risk categories, 3004 (26%) people were low-risk, 2153 (19%) were moderate-risk, 2120 (19%) were high-risk, and 4071 (36%) were very high-risk. There were 10 634 (94%) people with low-risk alcohol use; 471 (4%) belonged to the hazardous group, and 243 (2%) were considered alcohol-dependent, based on self-report.
ALCOHOL DRINKING PATTERNS:
A significant association was found between the frequency of alcohol dependence and gender (P<0.001); when comparing men and women the distribution of low risk, low-risk alcohol consumption was noted in 4465 (42%) males and 6169 (58%) females. When comparing hazardous alcohol consumption, hazardous was observed in 381 (81%) males and 90 (19%) females, while alcohol dependence was observed in 197 men (81%) and 46 women (19%). Self-reported alcohol dependence significantly increased with age (P<0.001); 17 (7%) respondents were categorized as alcohol-dependent from the age group of 40–44 years, and this crude case number increased to 36 (15%) in the 45–49 years age group. The rate of alcohol dependence was 19% (n=46) in the 50–54 years age group, and it increased to 27% (n=66) among people aged 55–59 years. Alcohol dependence affected 78 (32%) people in the 60–64 years age group. The same trend was observed in the hazardous category, where the crude rate was 7% (n=34) in the 40–44 years age group, 15% (n=69) in the 45–49 years age group, 23% (n=109) in the 50–54 years age group, and 30% (n=140) in the 55–59 years age group. A slightly lower frequency of hazardous drinking (n=119, 25%) was found in the oldest age group. Smoking status was significantly associated with alcohol dependence (P<0.001). The rate of alcohol dependence was 65% (n=158) among daily smokers, 6% (n=14) among occasional smokers, and 29% (n=71) among non-smokers. Among regular smokers, 23% (n=2452) had low-risk alcohol consumption, 5% among occasional smokers (n=569) and 72% (n=7613) among non-smokers. A significant difference was found between different total cholesterol levels and alcohol dependence (P=0.009). The rate of alcohol dependence among people with total cholesterol <4.5 mmol/l was 22% (n=53), and it was 78% (n=190) among people with total cholesterol ≥4.5 mmol/l. Furthermore, 16% (n=1730) of people with low total cholesterol had low risk of alcohol dependence, and it was 84% (n=8904) among people with high total cholesterol. No significant (P=0.289) difference was found when alcohol consumption risk categories were analyzed regarding HDL cholesterol level, stratified by gender. However, alcohol dependence was more frequent (n=164; 83%) among men with high HDL level compared to men with lower level of HDL level (n=33; 17%). The same non-significant (P=0.589) association was observed among women. Respondents with lower LDL cholesterol level had significantly (P<0.001) lower rates (n=84; 38%) of alcohol dependence compared to participants with high LDL cholesterol level (n=140; 62%). Among respondents with low risk of alcohol dependence, 77% (n=7956) had a higher LDL cholesterol level, while 23% (n=2442) had a lower LDL cholesterol level. A significant association (P=0.017) was found when the prevalence of overweight or obesity was analyzed by alcohol dependence levels. In alcohol-dependent people, respondents with increased BMI were more frequent (n=164; 67%) compared to people who were not obese or overweight (n=79; 33%). Glomerular filtration rate, indicating kidney disease, showed no significant association (P=0.108) with alcohol dependence. Systolic blood pressure was significantly associated with alcohol drinking behavior (P<0.001). In the alcohol-dependent category, 51% (n=124) of respondents had lower blood pressure values and 49% (n=119) had elevated systolic blood pressure. Furthermore, 70% (n=7429) of respondents in the low-risk alcohol consumption group had lower systolic blood pressure and 30% (n=3205) had elevated blood pressure. Regarding cardiovascular risk categories, we found a significant relationship between cardiovascular risk and alcohol consumption risk categories (P<0.001). Among respondents with alcohol dependence, 9% (n=22) had low cardiovascular risk; 13% (n=32) had moderate cardiovascular risk, 23% (n=55) had high cardiovascular risk, and 55% (n=134) had very high cardiovascular risk. In the low-risk alcohol consumption group, 28% (n=2925) had low cardiovascular risk, 19% had moderate (n=2036) or high (n=1981) cardiovascular risk, and 35% (n=3692) had very high cardiovascular risk (Figure 1 and Table 1).
MULTIPLE ORDINAL LOGISTIC REGRESSION RESULTS:
According to the confounder-adjusted multiple ordinal logistic regression model, alcohol dependence was a significant influencing factor (adjusted odds ratio – aOR=1.306 [1.003–1.701]) related to cardiovascular risk; therefore, people with high-risk drinking behavior had higher odds of having a more serious cardiovascular risk status. This association was not significant when we compared high-risk drinkers with low-risk drinkers related to cardiovascular risk category; therefore, it was a non-significant risk factor (aOR=1.189 [0.986–1.435]) (Table 2).
Discussion
LIMITATIONS OF THE STUDY:
This large-sample study found a relationship between alcohol consumption and cardiovascular risk in a country with a high-risk rating regarding cardiovascular risk. Alcohol consumption patterns reported in this study may under-represent the reality, and we lacked data regarding blood alcohol levels, thereby distorting our results, which could be considered a weakness; however, we were able to demonstrate an association between alcohol consumption and cardiovascular disease. Furthermore, this was a cross-sectional study; therefore, causality between variables could not be established.
Conclusions
Due to the nature of alcohol consumption, alcohol drinking is highly stigmatized in Hungary; however, our results may under-represent the true proportion of drinkers in the country. It was clear that higher levels of alcohol consumption were associated with increased cardiovascular risk. From a public health perspective, our findings highlight the importance of reducing alcohol consumption with the help of primary care and preventive services in countries with a high cardiovascular risk profile to reduce the cardiovascular-related burden. The present study described alcohol dependence patterns in Hungary, and the association between alcohol dependence and cardiovascular risk was found to be borderline. Therefore, further studies, especially in Hungary, should be conducted to describe the potential effect of alcohol consumption on cardiovascular risk status.
References
1. World Health Organization (WHO): Global Information System on Alcohol and Health https://www.who.int/data/gho/data/themes/global-information-system-on-alcohol-and-health
2. World Health Organization (WHO): Fact Sheet Alcohol https://www.who.int/health-topics/alcohol
3. Arora M, ElSayed A, Beger B, The impact of alcohol consumption on cardiovascular health: Myths and measures: Glob Heart, 2022; 17(1); 45
4. Piano MR, Alcohol’s effects on the cardiovascular system: Alcohol Res, 2017; 38(2); 219-41
5. Obad A, Peeran A, Little JI, Alcohol-mediated organ damages: Heart and brain: Front Pharmacol, 2018; 9; 81
6. Kawano Y, Physio-pathological effects of alcohol on the cardiovascular system: Its role in hypertension and cardiovascular disease: Hypertens Res, 2010; 33(3); 181-91
7. Chiva-Blanch G, Badimon L, Benefits and risks of moderate alcohol consumption on cardiovascular disease: Current findings and controversies: Nutrients, 2019; 12(1); 108
8. Rosoff DB, Davey Smith G, Evaluating the relationship between alcohol consumption, tobacco use, and cardiovascular disease: A multivariable Mendelian randomization study: PLoS Med, 2020; 17(12); e1003410
9. Powell L, Feng Y, Duncan MJ, Does a physically active lifestyle attenuate the association between alcohol consumption and mortality risk? Findings from the UK biobank: Prev Med, 2020; 130; 105901
10. Lu Y, Xu Z, Georgakis MK, Smoking and heart failure: A Mendelian randomization and mediation analysis: ESC Heart Fail, 2021; 8(3); 1954-65
11. Khoramdad M, Vahedian-Azimi A, Karimi L, Association between passive smoking and cardiovascular disease: A systematic review and meta-analysis: IUBMB Life, 2020; 72(4); 677-86
12. Francula-Zaninovic S, Nola IA, Management of measurable variable cardiovascular disease’ risk factors: Curr Cardiol Rev, 2018; 14(3); 153-63
13. Smyth A, Teo KK, Rangarajan S, Alcohol consumption and cardiovascular disease, cancer, injury, admission to hospital, and mortality: A prospective cohort study: Lancet, 2015; 386(10007); 1945-54
14. Bell S, Daskalopoulou M, Rapsomaniki E, Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: Population based cohort study using linked health records: BMJ, 2017; 356; j909
15. Biddinger KJ, Emdin CA, Haas ME, Association of habitual alcohol intake with risk of cardiovascular disease: JAMA Network Open, 2022; 5(3); e223849
16. Wakabayashi I, A U-shaped relationship between alcohol consumption and cardiometabolic index in middle-aged men: Lipids Health Dis, 2016; 15(1); 50
17. Zhang X, Liu Y, Li S, Alcohol consumption and risk of cardiovascular disease, cancer and mortality: A prospective cohort study: Nutr J, 2021; 20(1); 13
18. Minzer S, Losno RA, Casas R, The effect of alcohol on cardiovascular risk factors: Is there new information?: Nutrients, 2020; 12(4); E912
19. Hoek AG, van Oort S, Mukamal KJ, Beulens JWJ, Alcohol consumption and cardiovascular disease risk: Placing new data in context: Curr Atheroscler Rep, 2022; 24(1); 51-59
20. Mihailovic N, Szőllősi GJ, Rancic N, Alcohol consumption among the elderly citizens in Hungary and Serbia – comparative assessment: Int J Environ Res Public Health, 2020; 17(4); 1289
21. , Hungary: Most frequent causes of death 2021: Statista https://www.statista.com/statistics/1094534/hungary-most-frequent-causes-of-death/
22. World Bank Data: Life expectancy at birth, total (years) – Hungary | Data https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=HU
23. Csákvári T, Elmer D, Németh N, EPH85 mortality and health care utilization trends of cardiovascular diseases: Comparing Hungary to OECD average: Value in Health, 2022; 25(7); S450
24. : EAPC Country of the month – Hungary , https://www.escardio.org/Sub-specialty-communities/European-Association-of-Preventive-Cardiology-(EAPC)/Advocacy/Prevention-in-your-country/country-of-the-month-hungary
25. European Observatory on Health Systems and Policies: Country health profiles https://eurohealthobservatory.who.int/publications/country-health-profiles
26. Năsui BA, Ungur RA, Talaba P, Is alcohol consumption related to lifestyle factors in Romanian university students?: Int J Environ Res Public Health, 2021; 18(4); 1835
27. : Három generációval az egészségért program, Gokvi [in Hungarian]https://gokvi.hu/harom-generacioval-az-egeszsegert-program
28. : AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care https://www.who.int/publications-detail-redirect/WHO-MSD-MSB-01.6a
29. Erol A, Karpyak VM, Sex and gender-related differences in alcohol use and its consequences: Contemporary knowledge and future research considerations: Drug Alcohol Depend, 2015; 156; 1-13
30. Becker U, Tolstrup JAlcohol-related morbidity and mortality: Ugeskr Laeger, 2021; 183(14); V11200854 [in Danish]
31. El O, Jj D, Jh O, Cj L, Alcohol and CV health: Jekyll and Hyde J-curves: Prog Cardiovasc Dis, 2018; 61(1); 68-75
32. Varvasovszky Z, McKee M, Problem drinking among hospitalized patients in Hungary: Alcohol Alcohol, 2000; 35(6); 574-79
33. Rigler SK, Alcoholism in the elderly: Am Fam Physician, 2000; 61(6); 1710-16 passim
34. Britton M, Derrick JL, Shepherd JM, Associations between alcohol consumption and smoking variables among Latinx daily smokers: Addict Behav, 2021; 113; 106672
35. O’Keefe JH, Bhatti SK, Bajwa A, Alcohol and cardiovascular health: The dose makes the poison… or the remedy: Mayo Clin Proc, 2014; 89(3); 382-93
36. Day E, Rudd JHF, Alcohol use disorders and the heart: Addiction, 2019; 114(9); 1670-78
37. Gruenewald PJ, Regulating availability: How access to alcohol affects drinking and problems in youth and adults: Alcohol Res Health, 2011; 34(2); 248-56
38. CDC: CDC’s alcohol screening and brief intervention efforts, Centers for Disease Control and Prevention Published June 15, 2021
Tables
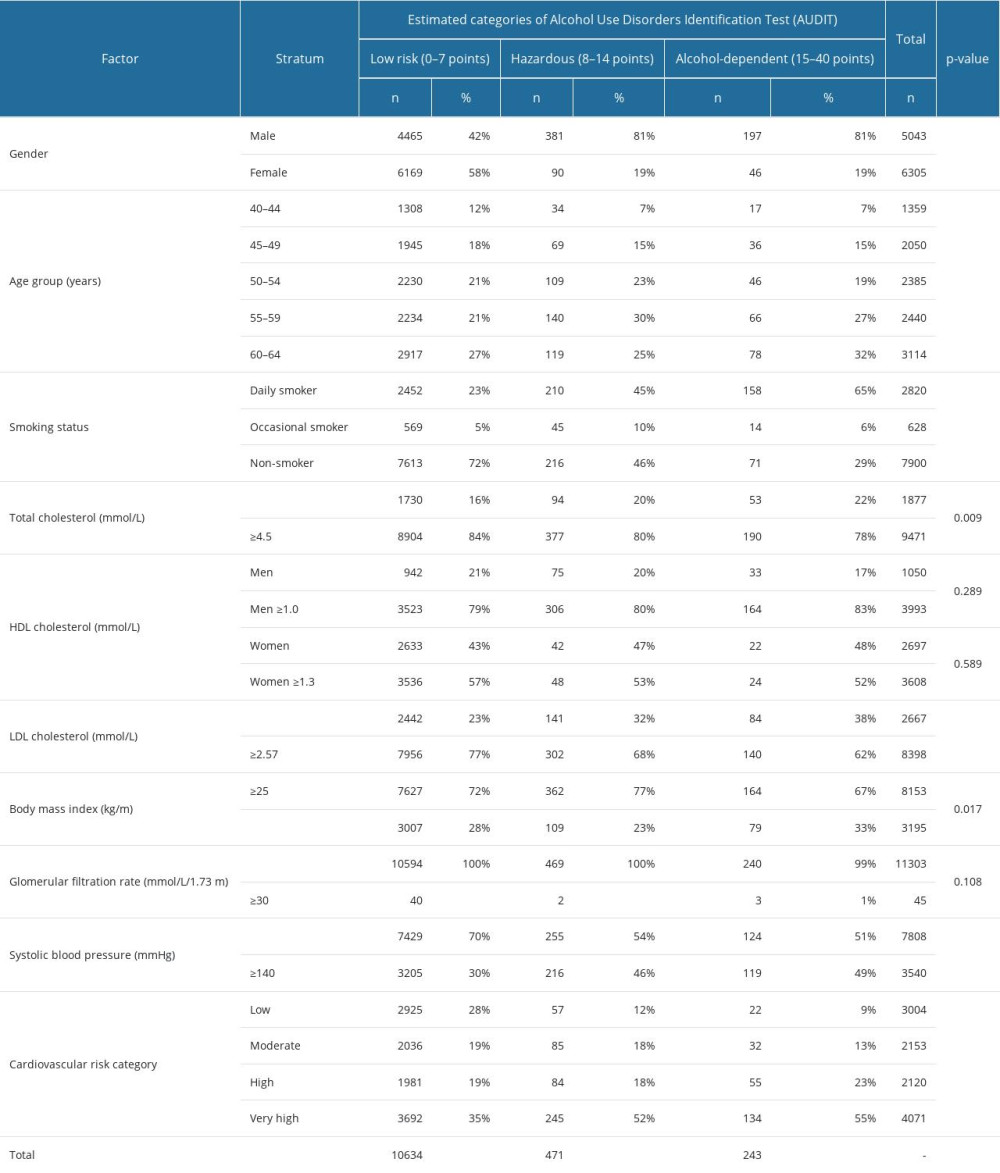 Table 1. Descriptive characteristics of the patients regarding alcohol consumption categories estimated by Alcohol Use Disorders Identification Test (AUDIT).
Table 1. Descriptive characteristics of the patients regarding alcohol consumption categories estimated by Alcohol Use Disorders Identification Test (AUDIT).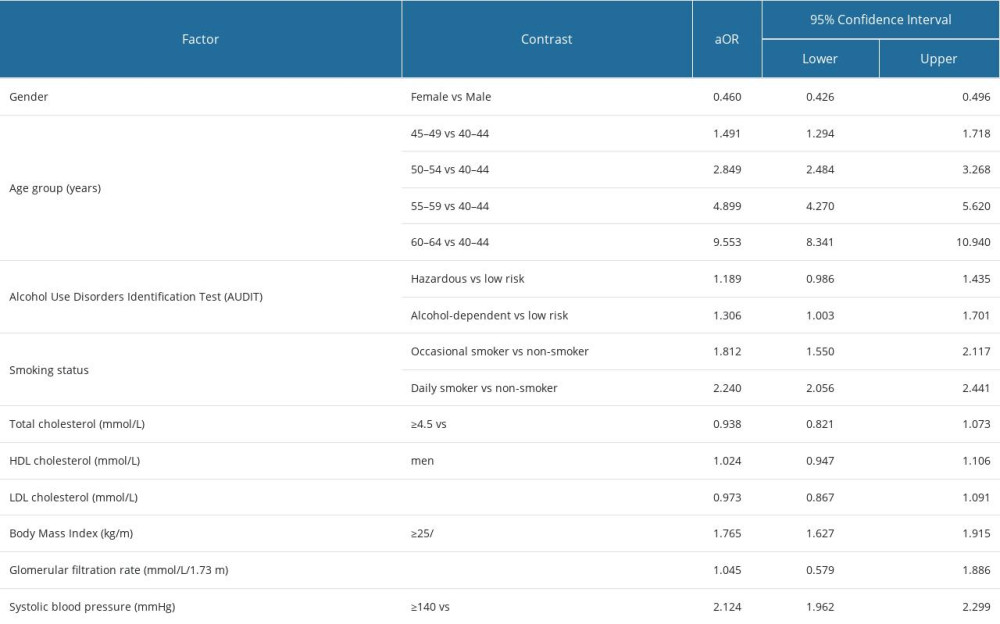 Table 2. Factors that influenced cardiovascular risk status among respondents based on a multiple ordinal logistic regression model.
Table 2. Factors that influenced cardiovascular risk status among respondents based on a multiple ordinal logistic regression model.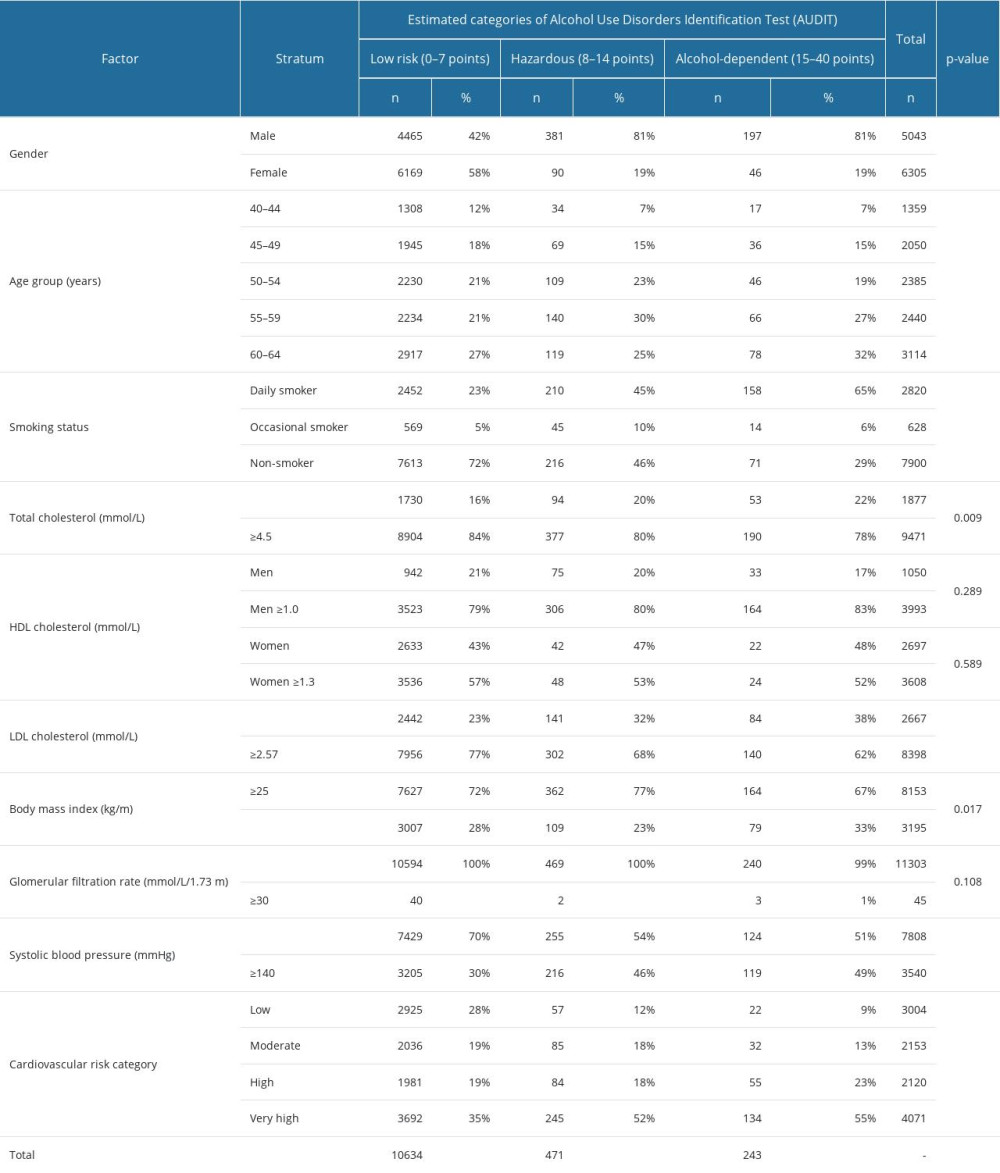 Table 1. Descriptive characteristics of the patients regarding alcohol consumption categories estimated by Alcohol Use Disorders Identification Test (AUDIT).
Table 1. Descriptive characteristics of the patients regarding alcohol consumption categories estimated by Alcohol Use Disorders Identification Test (AUDIT).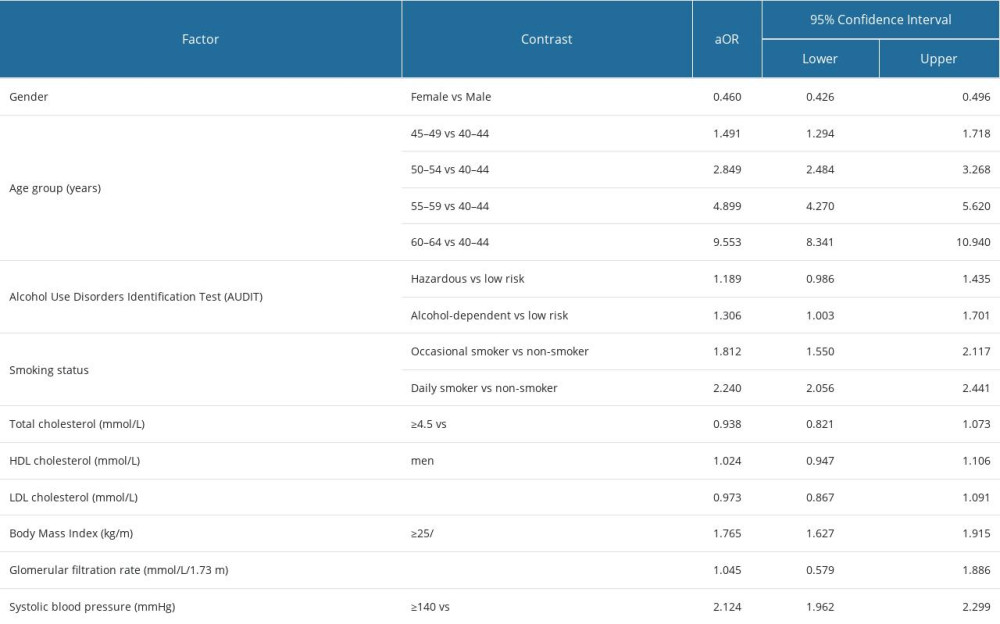 Table 2. Factors that influenced cardiovascular risk status among respondents based on a multiple ordinal logistic regression model.
Table 2. Factors that influenced cardiovascular risk status among respondents based on a multiple ordinal logistic regression model. In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952









