12 July 2023: Clinical Research
Internal Orifice Alloy Closure: A New Procedure for Treatment of Perianal Fistulizing Crohn’s Disease
Xiaoli Fang1CDE, Heng Deng2ABCG*, Ming Li1AGDOI: 10.12659/MSM.940873
Med Sci Monit 2023; 29:e940873
Abstract
BACKGROUND: The high recurrence rate of perianal fistula Crohn’s disease (PFCD) increases the need to protect the anal sphincter during each surgical treatment of fistulas. We aimed to evaluate the safety and efficacy of internal orifice alloy closure in patients with PFCD.
MATERIAL AND METHODS: Fifteen patients with PFCD were enrolled in the study between July 6, 2021, and April 27, 2023. All patients underwent preoperative colonoscopy and anal magnetic resonance examination for diagnosis and evaluation. Internal orifice alloy closure (IOAC) was performed only when Crohn’s disease was in remission. The external sphincter had not been severed. Perianal magnetic resonance imaging examination was used for postoperative evaluation after 6 months. Fistula cure rate, length of stay, perianal pain, and Wexner incontinence score were retrospectively compared between 15 patients treated with IOAC and 40 patients treated with other surgical methods.
RESULTS: Fifteen patients (male/female: 9/6, age: 23.6±14.3 years) with PFCD were included (follow-up: 24 months). In total, 20.0% (3) had multiple tracts, and 13.3% (2) had a high anal fistula. Among them, 10 patients received biologics for induction for mucosal healing before surgery. The fistula healed completely in 80.0% (12/15) and did not heal in 20.0% (3/15). Three patients who did not heal underwent fistulotomy and eventually recovered. IOAC is not superior in terms of fistula healing rates, length of stay, and anal pain, but its Wexner incontinence scores are significantly lower than with other surgical methods.
CONCLUSIONS: IOAC is a novel sphincter-saving surgery that is effective and safe for the treatment of PFCD.
Keywords: Colorectal Surgery, Inflammatory Bowel Disease 7, Rectal Fistula, Humans, Female, Male, Child, Adolescent, young adult, Adult, Crohn Disease, Retrospective Studies, Alloys, Pelvic Pain
Background
Crohn’s disease (CD) is a type of inflammatory bowel disease with unclear etiology and incidence [1,2]. Transmural inflammation of the gastrointestinal tract alternates between chronic remission and recurrence [3]. These characteristics leave patients with chronic immunosuppression and they need repeated surgery to treat the symptoms of the disease [4, 5], but surgery cannot cure the disease [6]. More than a quarter of patients with CD develop perianal fistulizing Crohn’s disease (PFCD) [7], which has been treated with biologics and surgical procedures [8]. These patients experience an endless cycle of perianal abscess, pain, persistent drainage [9], recurrent perianal sepsis [10], and anal stricture [11], which cause ongoing medical costs, negative stress on the family, and a significant burden to the healthcare system [12]. As a result, these conditions leave patients with lost jobs and increased risk of opportunistic infection from biologics. More than 90% of patients with PFCD undergo numerous surgical interventions that put them at risk for incontinence after a sphincter injury [13]. Although fistula healing can be achieved with sphincteroprotective procedures such as displacement flap surgery, these procedures require extensive experience or higher surgical conditions [14].
This frustrating situation has sparked intense interest in research into better treatment options that have the potential to improve outcomes without the risk of incontinence. Internal orifice alloy closure (IOAC) is a protective sphincter surgery used by our team for the treatment of anal fistulas and has been shown to have a positive effect [15]. This study was conducted to evaluate the therapeutic effect of IOAC on PFCD.
Material and Methods
MAGNETIC RESONANCE IMAGING (MRI):
All MRIs scans were performed at the Imaging Department of Anhui University of Chinese Medicine Hospital, using a Philips Ingenia 1.5-T scanner (Philips Medical Systems Nederland B.V.). T2 Kiefer sequences were selected to show the pathological structures [19]. For the T2 Kiefer sequences in the oblique coronal and the oblique transverse plane, the time to echo (TE) was 80 milliseconds and the slice thickness was 5 mm.
PROCEDURE:
All patients underwent routine blood, erythrocyte sedimentation rate (ESR), computed tomography enterography (CTE), colon endoscopy, and intestinal mucosal biopsy examinations. The above examinations revealed anemia, accelerated sedimentation, thickened colonic mucosa, pavers-like nodules, longitudinal ulcers, and acute and chronic mucosal inflammation. Based on perianal MRI, the fistula duct was mapped in detail after a discussion between the radiologist and the surgeon (Figure 2).
After combined subarachnoid and epidural anesthesia was administered, the patient was placed in the left decubitus position. The antibiotics cefoxitin 2 g and metronidazole 500 mg were given intravenously 3 h before surgery. We performed the following steps: (1) Hydrogen peroxide was injected into the fistula from the external orifice, and the internal orifice of the fistula bubbled to confirm the internal orifice. (2) A metal brush was used to clean the epithelium lining the fistula. (3) The mucosa of 1 cm around the internal orifice was removed. (4) Muscle layers were lifted in preparation for closing the internal orifice by exposing and cross-stitching it. (5) The muscular layer was closed through release of the anal fistula clip (Figure 3), at which point the internal orifice was closed. (6) The external opening was enlarged for drainage (Figure 4) [15].
Perianal pain on day 1, 2, and 3 after surgery was evaluated by numerical scoring [20]. Length of stay (days) was recorded from the first day of hospitalization to discharge. Microscopic inflammation was assessed by histological scores of Pouchitis Disease Activity Index (PDAI) at 1, 4, and 8 weeks after surgery. The clips fell off on its own or was removed within 4–6 weeks after surgery. Repeat perianal MRI was used to assess anal fistula healing, and fistula healing rates were also calculated at 6 months after surgery (Figure 2). No clinical signs plus MRI support was considered complete healing. Wexner incontinence scoring was used for incontinence scoring after fistula healing, which contains incontinence of gas, liquid, and solid; the need for padding and antidiarrhea medications; and the ability to defer defecation for 15 min. Zero denotes no incontinence, and 24 denotes total incontinence. Quality of life of patients following surgery was scored using the Crohn’s Anal Fistula Quality of Life Scale (CAF-QoL), which is an effective patient-reported outcome measure (PROM). Quality of life was scored on a scale of 0 to 108, with higher scores indicating lower the quality of life [21].
STATISTICAL ANALYSIS:
Clinical data were collected from 2 treatment groups: 15 patients with PFCD receiving IOAC and 40 patients with PFCD receiving other surgical treatments. The
Results
Fifteen patients with PFCD underwent surgery. The median follow-up was 11 months (range: 9–24 months). The mean age was 23.6±14.3 years, and the male-to-female ratio was 9/6. In total, 20.0% (3) had multiple tracts and 13.3% (2) had high anal fistula. Among them, 15 patients received biologics for induction for mucosal healing before surgery, 12 patients received infliximab, and 3 patients were switched to Ulinumab or Vedrizol due to non-response to infliximab.
Three patients who did not heal underwent fistulotomy and eventually recovered. The fistula healed completely in 80.0% (12/15) and did not heal in 20.0% (3/15). T2-weighted images demonstrated that the high-signal shadow of fistula and effusion disappeared at 6 months after the operation when the anorectal surgeon considered the fistula to be healed (Figure 2).
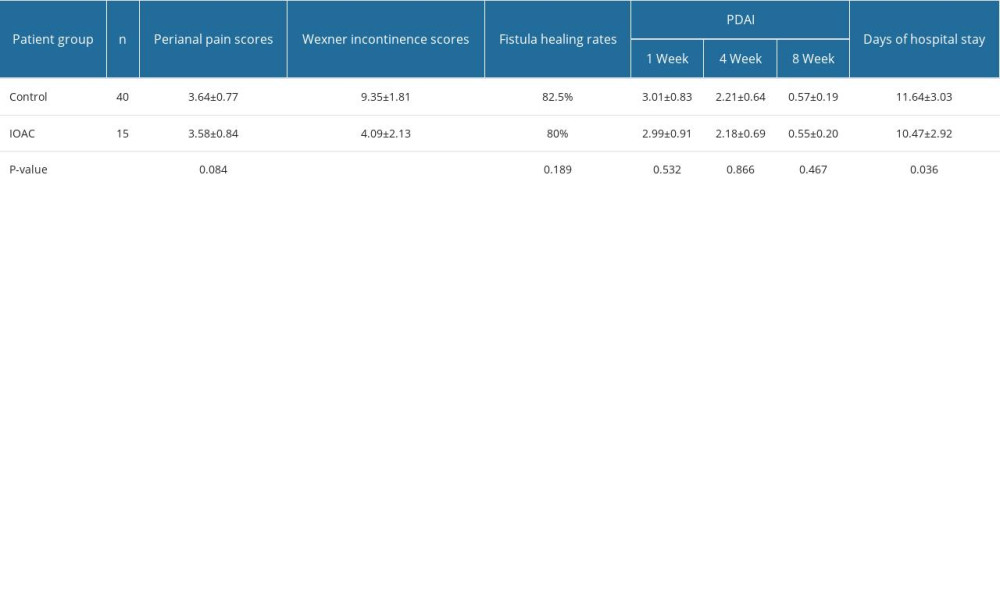
A retrospective comparison was conducted, and 40 patients with PFCD before IOAC was introduced in the hospital were included as a control group. Fistula healing rates, length of hospital stay, perianal pain, Wexner incontinence scores, and quality of life of patients following surgery were compared between the 2 groups (Table 1, Figure 5).
Discussion
One of the most challenging phenotypes of Crohn’s disease is perianal fistula [22]. Up to 50% of patients develop symptoms elsewhere in the gastrointestinal tract, and 5% develop symptoms for the first time [23]. It is associated with severe symptoms such as pain, fecal incontinence, and significantly reduced quality of life [14]. Perianal fistula combined with Crohn’s disease predicts a more severe course of disease [24]. These patients require close monitoring to identify patients at risk of worsening disease, unsatisfactory levels of biologics, and signs of tumor development. Significant progress has been made in the management of PFCD over the past 20 years [25]. Recently, new biologics, cell-based therapies, and new surgical techniques have been introduced in the hope of improving outcomes. However, in refractory cases, many patients face incontinence as a result of repeated surgery and the decision to have an ostomy [26]. In this study, we describe recent advances in modern surgical treatment for PFCD that may impact clinical practice.
According to our analysis of research results, IOAC does not significantly change anal pain and fistula healing rate compared with traditional surgery. In China, the traditional loose seton for drainage is often used in the treatment of PFCD, which can improve perianal comfort and quality of life [27]. However, some patients do not want to be chronically stimulated by foreign bodies around the anus and do not want to accept the loose seton. The fistula healing rate of IOAC treatment for PFCD was comparable to that of conventional surgery, which demonstrated its effectiveness. There was no statistically significant difference in PDAI between the 2 groups, which was related to the medical treatment of the patients during their hospitalization and also suggests that the new surgical approach reduced the local inflammatory response as much as traditional surgery. The reason why IOAC significantly reduces the length of hospital stay may be that the surgical procedure is easy to perform and is minimally invasive. IOAC only involves internal and external orifice and fistulas without additional tissue damage.
Although the medical or surgical treatment of PFCDS is controversial, the actual surgical treatment available has a relatively limited success rate. Gastroenterologists and colorectal surgeons use similar methods for the management of PFCD. The results of surgery (mesenchymal stem cells, LIFT, rectal mucosal propulsion flap technique) plus biologics in the safety and efficacy of PFCD treatment are encouraging. Direct injection of mesenchymal stem cells (MSC) does not cause injury to the internal sphincter; therefore, there is no risk of fecal incontinence, but the most common adverse events are perianal pain or abscess formation at the injection site and it is expensive. LIFT, a rectal mucosal propulsion flap technique, requires more surgical experience. Although there is no visible improvement in efficiency, IOAC has obvious advantages such as sphincter retention, simple operation, and low cost. The reason why the postoperative Wexner incontinence scores in IOAC group were not 0 may that some patients had received other surgical methods before this treatment.
However, a retrospective historical control group represents a limitation, and the stability of the therapeutic effect of IOAC on PFCD still needs a large sample size to be verified.
Conclusions
IOAC has a high potential value in the treatment of PFCD. This procedure is a sphincter-preserving operation, which is one of the factors guaranteeing postoperative quality of life of patients.
Figures
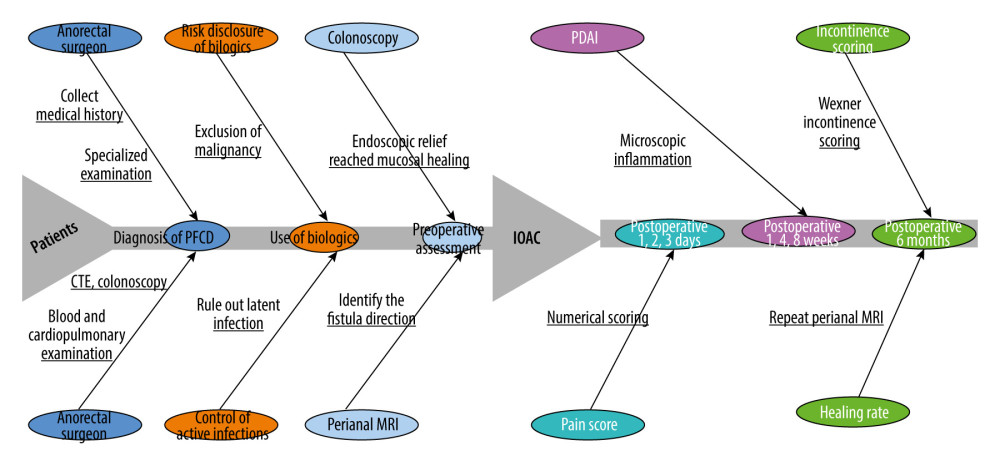 Figure 1. The general process of the patient from presentation to surgery and postoperative testing. Because patients have different conditions before surgery and need to meet the standards for endoscopic mucosal healing, the time of use of biological agents and the waiting time before surgery are different.
Figure 1. The general process of the patient from presentation to surgery and postoperative testing. Because patients have different conditions before surgery and need to meet the standards for endoscopic mucosal healing, the time of use of biological agents and the waiting time before surgery are different. 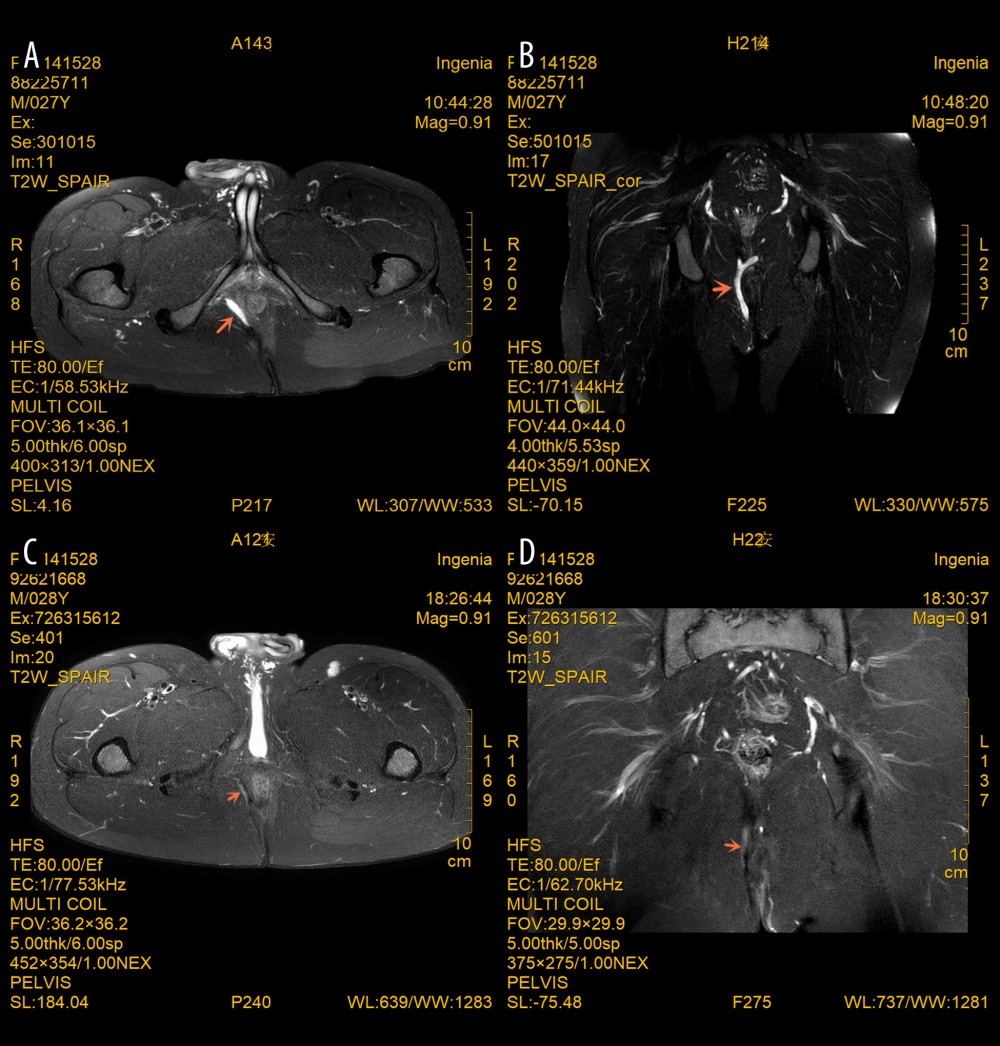 Figure 2. (A–D) MRI images of a perianal fistula in a young male patient with PFCD before and 6 months after IOAC. Note that the inflammatory component (T2 hyperintensity and collections) markedly improved and the fistula track disappeared. The oblique coronal plane and oblique transverse plane are parallel and perpendicular to the longitudinal axis of the anal canal, respectively. The orange arrows indicate changes in the site of the lesion.
Figure 2. (A–D) MRI images of a perianal fistula in a young male patient with PFCD before and 6 months after IOAC. Note that the inflammatory component (T2 hyperintensity and collections) markedly improved and the fistula track disappeared. The oblique coronal plane and oblique transverse plane are parallel and perpendicular to the longitudinal axis of the anal canal, respectively. The orange arrows indicate changes in the site of the lesion. 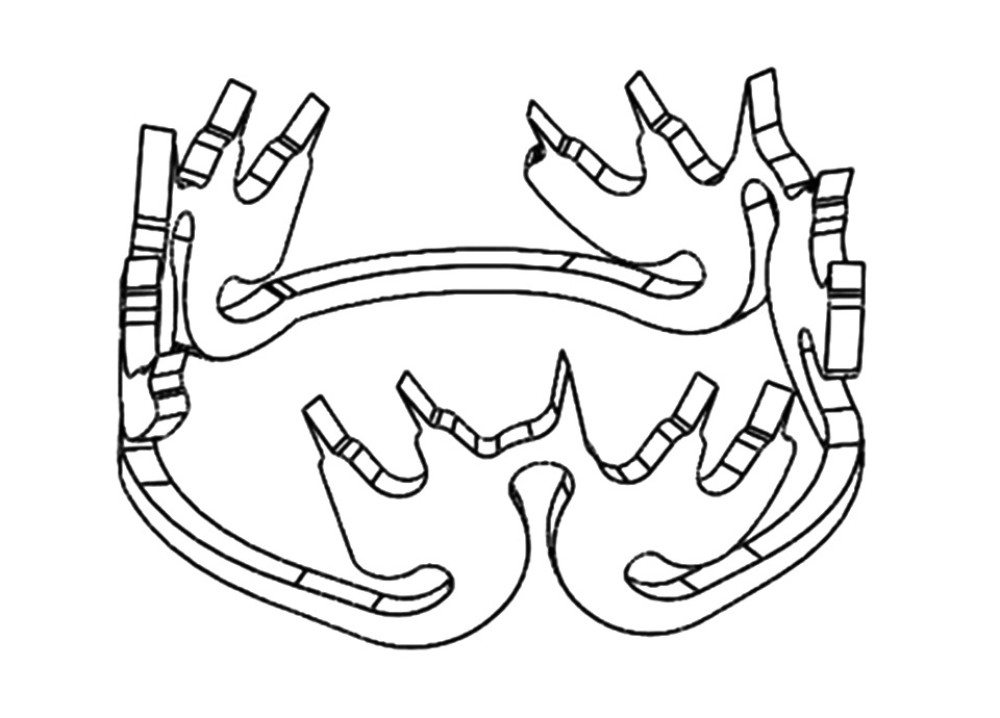 Figure 3. Schematic diagram of the anal fistula clip. The anal fistula clip has a three-lobe design, and the alloy is soft at 0°C. At 36°C, the alloy has a strong centripetal force and can clamp the central tissue.
Figure 3. Schematic diagram of the anal fistula clip. The anal fistula clip has a three-lobe design, and the alloy is soft at 0°C. At 36°C, the alloy has a strong centripetal force and can clamp the central tissue.  Figure 4. IOAC surgery was performed on a young male PFCD patient with repeated perianal surgery. (A) Confirmation of the internal orifice of the fistula. (B) Clean the epithelium lining the fistula. (C) The mucosa 1 cm around the internal orifice was removed. (D) The muscular layer was closed by the anal fistula clip (blue arrowheads).
Figure 4. IOAC surgery was performed on a young male PFCD patient with repeated perianal surgery. (A) Confirmation of the internal orifice of the fistula. (B) Clean the epithelium lining the fistula. (C) The mucosa 1 cm around the internal orifice was removed. (D) The muscular layer was closed by the anal fistula clip (blue arrowheads). 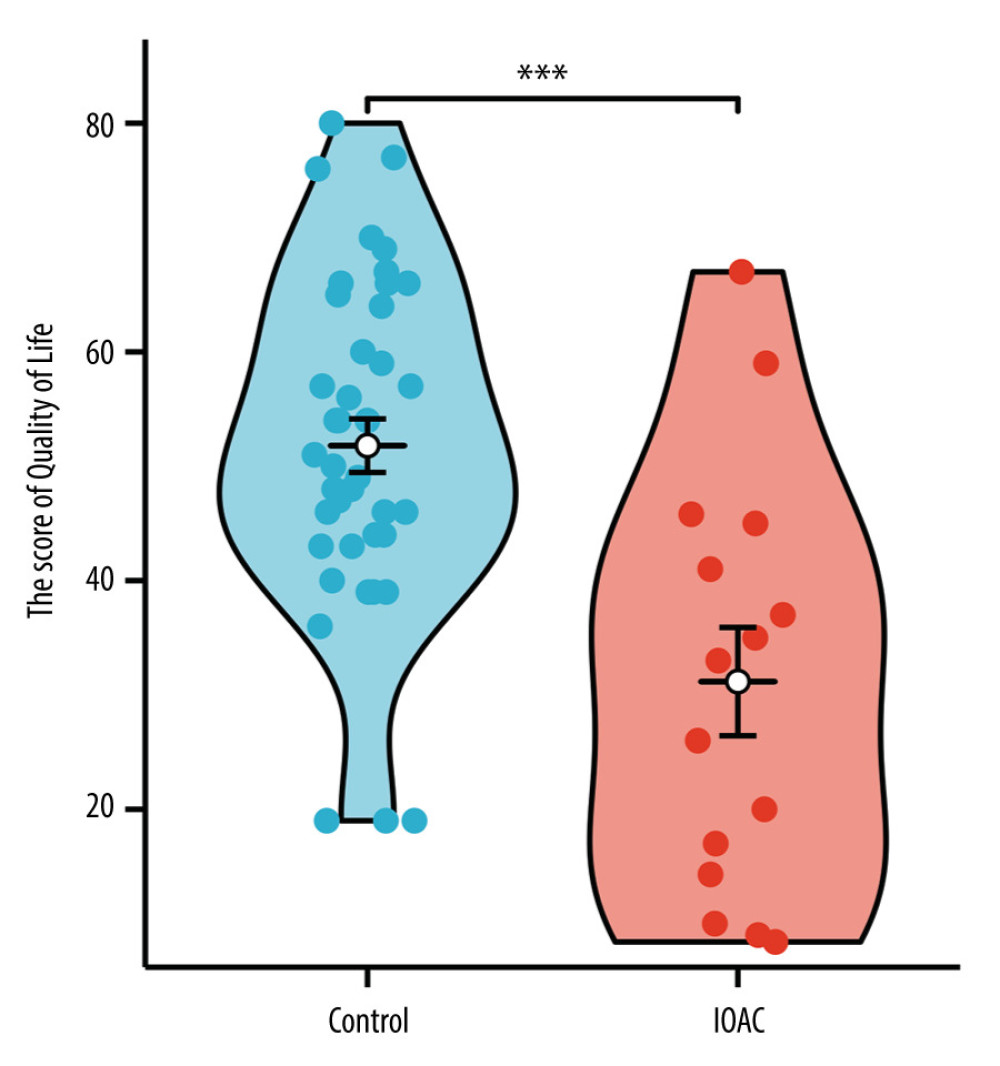 Figure 5. The comparison of quality of life of patients between the 2 groups. Questionnaire data from 15 patients in study groups showed scores of 8–67, while the control group had scores of 19–80 (possible range from 0 to 108). The scores were approximately normally distributed, and the average score of the study group and control group was 31.1 and 51.8, and the standard deviation was 18.3 and 14.8, respectively. *** P<0.001
Figure 5. The comparison of quality of life of patients between the 2 groups. Questionnaire data from 15 patients in study groups showed scores of 8–67, while the control group had scores of 19–80 (possible range from 0 to 108). The scores were approximately normally distributed, and the average score of the study group and control group was 31.1 and 51.8, and the standard deviation was 18.3 and 14.8, respectively. *** P<0.001 References
1. Jakubczyk D, Leszczyńska K, Górska S, The effectiveness of probiotics in the treatment of inflammatory bowel disease (IBD) – a critical review: Nutrients, 2020; 12(7); 1973
2. Le Berre C, Ananthakrishnan AN, Danese S, Ulcerative colitis and Crohn’s disease have similar burden and goals for treatment: Clin Gastroenterol Hepatol, 2020; 18(1); 14-23
3. Li Y, Chen J, Bolinger AA, Target-based small molecule drug discovery towards novel therapeutics for inflammatory bowel diseases: Inflamm Bowel Dis, 2021; 27(Suppl 2); S38-62
4. Clough JN, Omer OS, Tasker S, Regulatory T-cell therapy in Crohn’s disease: Challenges and advances: Gut, 2020; 69(5); 942-52
5. Colombo F, Frontali A, Baldi C, Repeated surgery for recurrent Crohn’s disease: Does the outcome keep worsening operation after operation? A comparative study of 1224 consecutive procedures: Updates Surg, 2022; 74(1); 73-80
6. Nam K, Jung WB, Lee SB, Predictors of reoperation for perianal fistula in Crohn’s disease: J Dig Dis, 2021; 22(6); 334-41
7. Vasudevan A, Bruining DH, Loftus EV, Approach to medical therapy in perianal Crohn’s disease: World J Gastroenterol, 2021; 27(25); 3693-704
8. Kotze PG, Shen B, Lightner A, Modern management of perianal fistulas in Crohn’s disease: Future directions: Gut, 2018; 67(6); 1181-94
9. Herissay A, Siproudhis L, Le Balc’h E, Combined strategies following surgical drainage for perianal fistulizing Crohn’s disease: Failure rates and prognostic factors: Colorectal Dis, 2021; 23(1); 159-68
10. Malian A, Rivière P, Bouchard D, Pedictors of perianal fistula relapse in Crohn’s disease: Inflamm Bowel Dis, 2020; 26(6); 926-31 [Erratum in: Inflamm Bowel Dis. 2021;27(8):1365]
11. Mutanen A, Pakarinen MP, Perianal Crohn’s disease in children and adolescents: Eur J Pediatr Surg, 2020; 30(5); 395-400
12. Kotsafti A, Scarpa M, Angriman I, Fistula-related cancer in Crohn’s disease: A systematic review: Cancers (Basel), 2021; 13(6); 1445
13. Wiseman J, Chawla T, Morin F, A multi-disciplinary approach to perianal fistulizing Crohn’s disease: Clin Colon Rectal Surg, 2022; 35(1); 51-57
14. Zabot GP, Cassol O, Saad-Hossne R, Bemelman W, Modern surgical strategies for perianal Crohn’s disease: World J Gastroenterol, 2020; 26(42); 6572-81
15. Li M, Fang X, Zhang J, Deng H, Internal orifice alloy closure – a new procedure to treat anal fistula: Front Surg, 2022; 9; 881060
16. Geldof J, Iqbal N, LeBlanc JF, Classifying perianal fistulising Crohn’s disease: An expert consensus to guide decision-making in daily practice and clinical trials: Lancet Gastroenterol Hepatol, 2022; 7(6); 576-84
17. Schwartz DA, Peyrin-Biroulet L, Lasch K, Efficacy and safety of 2 vedolizumab intravenous regimens for perianal fistulizing Crohn’s disease: ENTERPRISE study: Clin Gastroenterol Hepatol, 2022; 20(5); 1059-67e9
18. Attauabi M, Burisch J, Seidelin JB, Efficacy of ustekinumab for active perianal fistulizing Crohn’s disease: A systematic review and meta-analysis of the current literature: Scand J Gastroenterol, 2021; 56(1); 53-58
19. Azzam N, Alharbi O, Almadi M, Predictors of long-term outcomes of radiologically defined perianal fistulizing Crohn’s disease treated with antitumor necrosis factor-alpha agents based on Parks’ classification: Eur J Gastroenterol Hepatol, 2020; 32(2); 187-92
20. Deng H, Zhang J, Yuan X, The effects of phellodendron decoction on wound healing of anal fistula after anal fistulotomy: Evid Based Complement Alternat Med, 2022; 2022; 7363006
21. Adegbola SO, Dibley L, Sahnan K, Development and initial psychometric validation of a patient-reported outcome measure for Crohn’s perianal fistula: The Crohn’s Anal Fistula Quality of Life (CAF-QoL) scale: Gut, 2021; 70(9); 1649-56
22. Truong A, Zaghiyan K, Fleshner P, Anorectal Crohn’s disease: Surg Clin North Am, 2019; 99(6); 1151-62
23. Mitchel EB, Rosh JR, Pediatric management of Crohn’s disease: Gastroenterol Clin North Am, 2022; 51(2); 401-24
24. Rackovsky O, Hirten R, Ungaro R, Colombel JF, Clinical updates on perianal fistulas in Crohn’s disease: Expert Rev Gastroenterol Hepatol, 2018; 12(6); 597-605
25. Short SS, Dubinsky MC, Rabizadeh S, Distinct phenotypes of children with perianal perforating Crohn’s disease: J Pediatr Surg, 2013; 48(6); 1301-5
26. Spinelli A, Armuzzi A, Ciccocioppo R, Management of patients with complex perianal fistulas in Crohn’s disease: Optimal patient flow in the Italian clinical reality: Dig Liver Dis, 2020; 52(5); 506-15
27. Haennig A, Staumont G, Lepage B, The results of seton drainage combined with anti-TNFα therapy for anal fistula in Crohn’s disease: Colorectal Dis, 2015; 17(4); 311-19
Figures
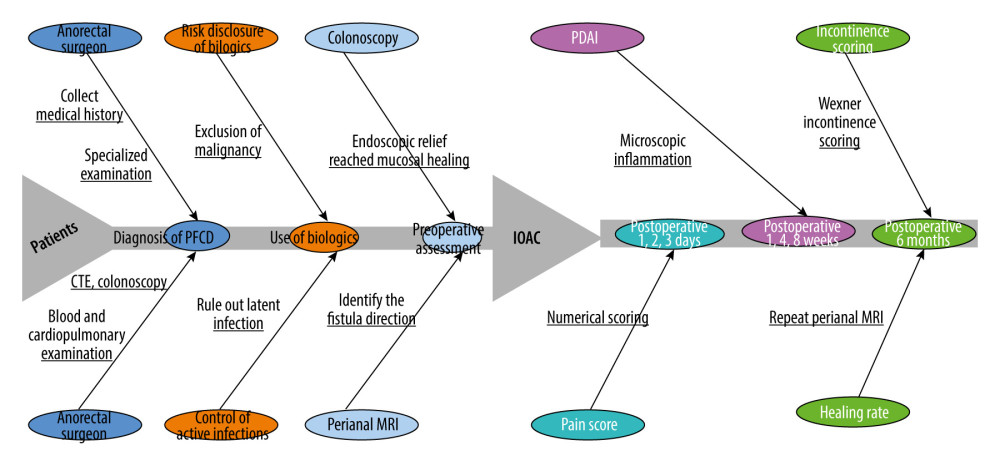 Figure 1. The general process of the patient from presentation to surgery and postoperative testing. Because patients have different conditions before surgery and need to meet the standards for endoscopic mucosal healing, the time of use of biological agents and the waiting time before surgery are different.
Figure 1. The general process of the patient from presentation to surgery and postoperative testing. Because patients have different conditions before surgery and need to meet the standards for endoscopic mucosal healing, the time of use of biological agents and the waiting time before surgery are different.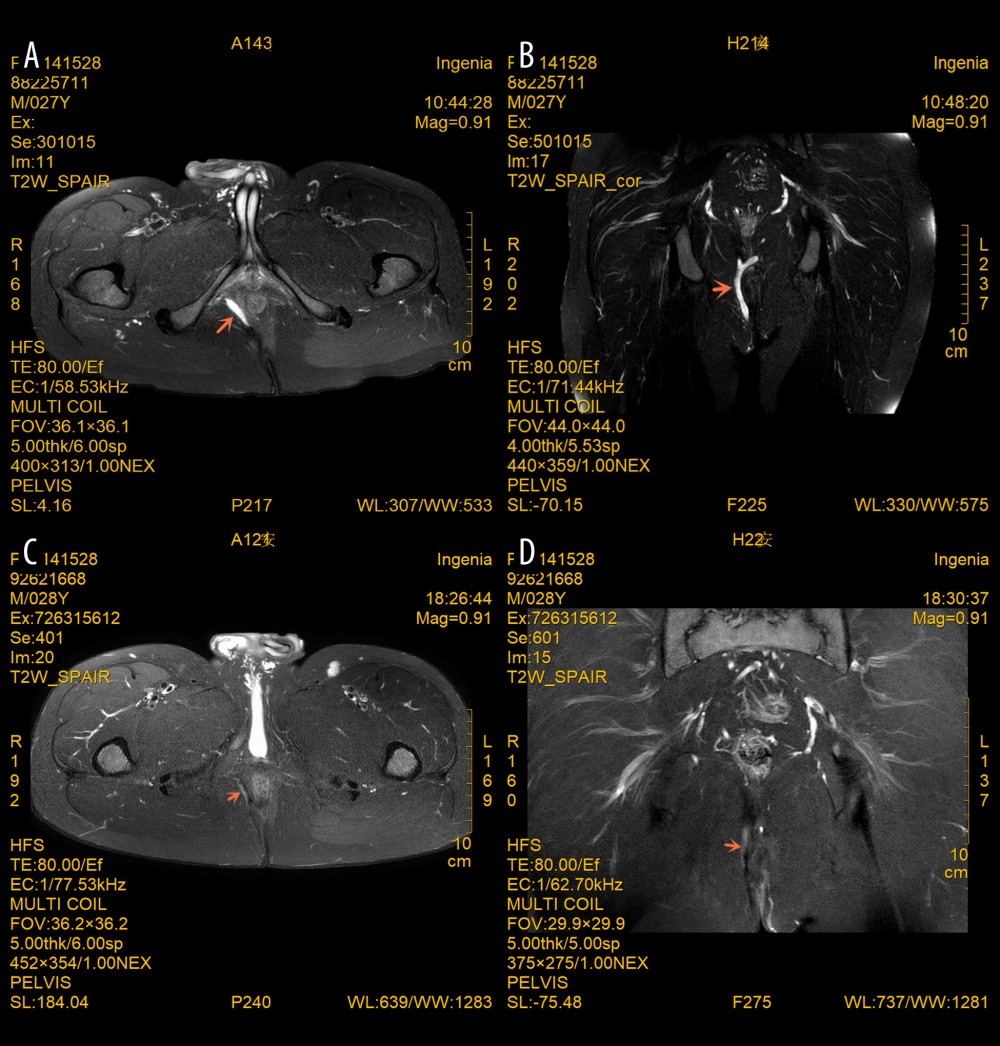 Figure 2. (A–D) MRI images of a perianal fistula in a young male patient with PFCD before and 6 months after IOAC. Note that the inflammatory component (T2 hyperintensity and collections) markedly improved and the fistula track disappeared. The oblique coronal plane and oblique transverse plane are parallel and perpendicular to the longitudinal axis of the anal canal, respectively. The orange arrows indicate changes in the site of the lesion.
Figure 2. (A–D) MRI images of a perianal fistula in a young male patient with PFCD before and 6 months after IOAC. Note that the inflammatory component (T2 hyperintensity and collections) markedly improved and the fistula track disappeared. The oblique coronal plane and oblique transverse plane are parallel and perpendicular to the longitudinal axis of the anal canal, respectively. The orange arrows indicate changes in the site of the lesion.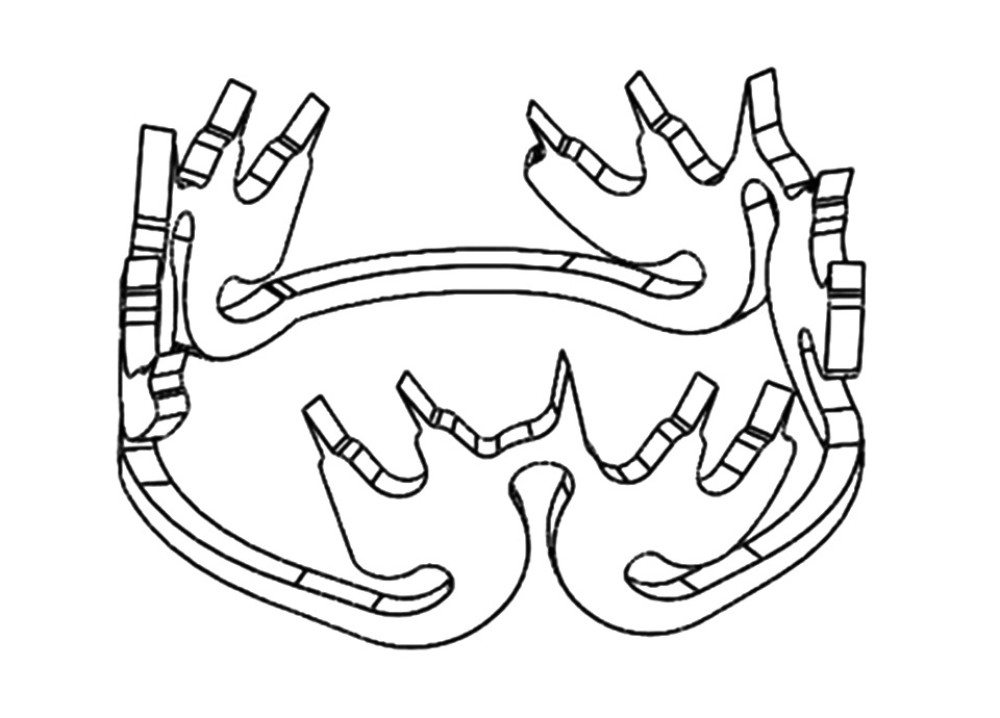 Figure 3. Schematic diagram of the anal fistula clip. The anal fistula clip has a three-lobe design, and the alloy is soft at 0°C. At 36°C, the alloy has a strong centripetal force and can clamp the central tissue.
Figure 3. Schematic diagram of the anal fistula clip. The anal fistula clip has a three-lobe design, and the alloy is soft at 0°C. At 36°C, the alloy has a strong centripetal force and can clamp the central tissue. Figure 4. IOAC surgery was performed on a young male PFCD patient with repeated perianal surgery. (A) Confirmation of the internal orifice of the fistula. (B) Clean the epithelium lining the fistula. (C) The mucosa 1 cm around the internal orifice was removed. (D) The muscular layer was closed by the anal fistula clip (blue arrowheads).
Figure 4. IOAC surgery was performed on a young male PFCD patient with repeated perianal surgery. (A) Confirmation of the internal orifice of the fistula. (B) Clean the epithelium lining the fistula. (C) The mucosa 1 cm around the internal orifice was removed. (D) The muscular layer was closed by the anal fistula clip (blue arrowheads).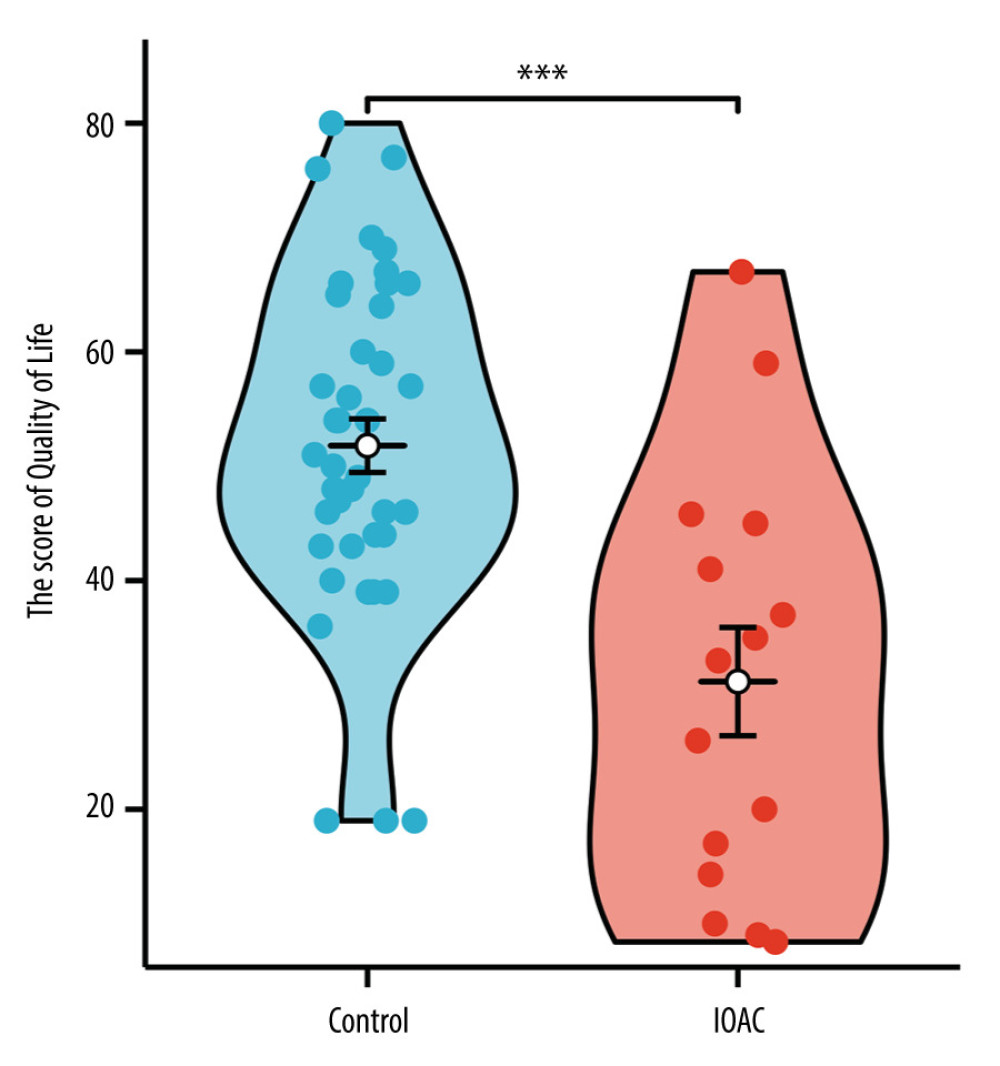 Figure 5. The comparison of quality of life of patients between the 2 groups. Questionnaire data from 15 patients in study groups showed scores of 8–67, while the control group had scores of 19–80 (possible range from 0 to 108). The scores were approximately normally distributed, and the average score of the study group and control group was 31.1 and 51.8, and the standard deviation was 18.3 and 14.8, respectively. *** P<0.001
Figure 5. The comparison of quality of life of patients between the 2 groups. Questionnaire data from 15 patients in study groups showed scores of 8–67, while the control group had scores of 19–80 (possible range from 0 to 108). The scores were approximately normally distributed, and the average score of the study group and control group was 31.1 and 51.8, and the standard deviation was 18.3 and 14.8, respectively. *** P<0.001 In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952