21 June 2023: Database Analysis
The COVID-19 Crisis and the Incidence of Alcohol-Related Deaths in Poland
Andrzej SilczukDOI: 10.12659/MSM.940904
Med Sci Monit 2023; 29:e940904
Abstract
BACKGROUND: Identifying risk and protective factors for excessive alcohol consumption can inform targeted health policies, reducing the impact of potential mental health crises. This study examined the validity and reliability of COVID-19-related death data and explored the correlations among age, sex, residential status, alcohol abuse, and healthcare access.
MATERIAL AND METHODS: This analysis of Polish residents’ mortality relies on individual data from the register of deaths maintained by Statistics Poland. This study examined deviations in the number of deaths between 2020 and 2021 by analyzing specific causes of death.
RESULTS: Alcohol abusers had increased COVID-19 risk factors compared to the general population. F10 values were 22% higher than expected in 2020, aligning with predictions for 2021. Higher mortality rates were observed in the first year of the pandemic. In 2020, women and rural residents were more affected (31% and 25% higher than expected, respectively), while men and urban residents were less affected (21% and 20% higher than expected, respectively). In 2021, the trend reversed, with men 2% higher than predicted and women 4% lower. Urban area residents had a 77% lower than expected value, while rural area residents were similar (8% higher). Overall mortality exceeded expectations in both 2020 (13% higher) and 2021 (23% higher). In 2021, alcohol-related non-mental health problems increased by more than 40% in standardized death rates (SDRs).
CONCLUSIONS: Alcohol-related deaths reflect the hidden effects of the pandemic. Measuring the pandemic’s impact on global excess mortality is hindered by inconsistencies in COVID-19 death reporting.
Keywords: Alcohol-Related Disorders, COVID-19, Mortality, Male, Humans, Female, Incidence, Poland, Reproducibility of Results, COVID-19, Risk Factors
Background
CRISES INCREASE ALCOHOL CONSUMPTION:
In the literature, a crisis is defined as an overwhelming event, such as a breakup of a relationship, the use of violence, the loss of livelihood, or the onset of a serious illness [1]. Authors point to the association of health and economic crises with excessive alcohol consumption and alcohol-related problems. This association also persists several years after a disaster, especially in cases of direct contact with the event. Data indicate that men, single people, and young people are at greater risk of developing such crises [2]. Stressful events contribute to an increase in alcohol-related problems like drinking more, higher frequency of drinking, and abuse disorders. Drinking is a maladaptive coping mechanism for dealing with negative affect, which is associated with an increase in alcohol consumption [3]. Also, studies on subjects with a history of alcohol use disorders have shown that excessive alcohol consumption may be considered a style to cope with a traumatic event within this group of patients. Stressful life events, such as the breakup of a marriage or the loss of a job, increase the risk of alcohol use disorders; however, there is no epidemiological consensus on the specificity of these associations in relation to biological sex [4]. The literature indicates that economic crises as such, or arising from other disasters, affect drinking patterns and the amount of alcohol consumed [3,5]. It is important to analyze the mechanisms that play a role in individuals showing changes in behavioral patterns, as such predictions may help to indicate the potential impact of crises on alcohol consumption. One known mechanism, observed mainly in men, suggests that psychological stress related to unemployment and low income can exacerbate alcohol problems. These reported differences between men and women could potentially reinforce gender inequalities in health during crises [5]. Mateo-Urdiales A et al found that during Spain’s economic crisis between the years 2008 and 2011, excess alcohol-related mortality increased for both men and women. Elevated risk of crisis harm was found for individuals with a higher educational status, and although the risk of death remained higher among those with lower educational status, the increase reduced inequalities in alcohol-related mortality [6].
Economic crises may also result in a decline in alcohol consumption due to insufficient financial resources. In terms of proactive government policies, alcohol consumption during an economic crisis may be influenced or managed by social support and prevention programs, the price and availability of alcohol, and treatment programs in place [3,5]. Epidemic public health crises involve a pairing of a spreading crisis and a severe economic downturn. Such a crisis can affect the drinking pattern in 2 ways, which may coexist, and are not mutually exclusive. On the one hand, abnormal drinking patterns and their exacerbated consequences may be caused by financial difficulties, social isolation, and fear of uncertainties in the future. On the other hand, an economic crisis leads to an increase in unemployment and reduced working hours, leading to a portion of the population receiving lower incomes. As a result, some segments of the population may lack the financial means to purchase alcoholic beverages. In addition, the availability of alcohol during an epidemic is reduced by restrictions on social life and the lesser availability of open drinking establishments [7]. Crises can have both short-term and long-term consequences in distress symptoms. For example, in China after the 2003 SARS outbreak, it was observed that after 1 year and after 3 years, alcohol consumption among those affected was higher compared to the population not directly exposed to the crisis [8]. The variety of mechanisms implied by the crisis, as well as the different timing of their impact on the population and the individual, are important issues in analyzing the relationship between the public health crisis and alcohol consumption.
COVID-19 AND ITS ASSOCIATION WITH INCREASED ALCOHOL CONSUMPTION:
The COVID-19 pandemic represented a major health, social and economic crisis, and its potential threat from increased alcohol consumption has been the subject of debate among many scientists [9–14]. Researchers of the available literature pertaining to the COVID-19 pandemic examined 2 scenarios for changing drinking patterns and the amount of alcohol consumed, based on mechanisms observed during other infection-induced public health crises. One scenario predicted an increase in alcohol consumption resulting from pandemic-related stress. In contrast, the other scenario predicted a decline in consumption associated with reduced, physical and economic availability of alcohol. The second scenario was predicted to dominate during the pandemic period, while the long-term effects would manifest themselves as an increase in alcohol consumption in line with the assumptions of the first scenario [7]. De Goeij et al proved the association between both of the above-mentioned mechanisms and the increase in alcohol consumption associated with the COVID-19 pandemic. The psychological crisis was primarily experienced by men, and the economic crisis resulting in reduced budgets and less availability of alcohol played a role in all countries, regardless of the studied population [5]. Most studies point to an increase in the amount and frequency of alcohol consumption, as well as harmful and hazardous drinking associated with the COVID-19 pandemic. The roles of social isolation, boredom, staying at home, mental disorders, and maladaptive coping methods have been proven in this phenomenon [15]. The increase in alcohol consumption observed during the COVID-19 pandemic was primarily associated with quarantine and social isolation. Wardell et al investigated mechanisms of increased alcohol consumption during the pandemic to find one that is dominant. It turns out that drinking as a way of coping with stress played the most important role. Stress not only increased the frequency of drinking but also led to drinking in solitude [16]. Killgore et al conducted a study to determine whether the restrictions that were implemented for 6 months due to COVID-19 and their resulting isolation caused by stay-at-home orders were associated with changes in risky alcohol use; 5931 people responded to a questionnaire, the Alcohol Use Disorder Identification Test (AUDIT), at 1 of 6 time points between April and September 2020. Over the 6-month period, risky alcohol use and probable addiction increased over the months among those who remained in isolation compared to those who were not subject to restrictions [17]. Studies conducted on the population of various countries prove that the COVID-19 pandemic has had an impact on alcohol consumption. In comparison to the pre-pandemic period, a higher frequency of drinking has been observed in the United States, among others [18]. Similar results were obtained in a study conducted on populations of European countries. Evidence suggested that the amount of alcohol ingested by those in the top 10% of alcohol consumption increased significantly. The change was small for those whose drinking levels were within the other percentiles. Thus, it was concluded that the greater the level of alcohol consumption before the pandemic, the greater the increase during the pandemic [19]. The overall results indicate both a higher number of drinking days and a higher volume of alcohol consumed. There was also a significant increase in the prevalence of daily drinking and moderate or severe alcohol use disorder [9]. The greatest increase in the amount of alcohol consumed was in those who also had symptoms of anxiety and depression [20,21].
Results showed that in Poland, alcohol consumption increased in 14% and decreased in 16% of those surveyed in the year 2020 [22]. Previous studies, while attempting to measure changes in alcohol consumption, have excluded alcohol-dependent and in-treatment individuals. Chodkiewicz et al (2022) were the first to examine the impact of the pandemic on the mental state of alcohol-dependent individuals who were participating in drug treatment during the lockdown. They analyzed the mental state of 454 individuals completing drug therapy in July and August 2021. Average scores in the group indicated a mild depressive state, mild anxiety, average alcohol craving, and average life satisfaction, while 18.06% of the subjects exhibited suicidal behavior. It appeared that higher levels of depression, anxiety, post-traumatic stress disorder, and complex post-traumatic stress disorder were associated with individuals participating in day unit treatment compared to inpatient or outpatient treatment. Worse mental status can hinder recovery; less effective therapy may therefore contribute to poorer coping in individuals with a psychiatric condition, which is likely to have contributed to increased alcohol consumption and consequently increased mortality. However, the study showed that the prevalence rate of the aforementioned disorders in the treated patients was less than 20%, which is lower than in earlier studies that included those who consumed alcohol but did not receive treatment [22]. The importance of monitoring and implementation of actions aimed at reducing the potential psychosocial impact of the pandemic, including alcohol-related disorders in general and also in professionals, was also emphasized in other high-impact and highly-cited studies [23,24].
A systematic review of studies to date indicates the presence of heterogeneity. Evidence from reviews suggests a mixed picture, with a general trend toward increased alcohol consumption [25,26]. Some countries are seeing a decline in total alcohol consumption, but it is likely that heavy episodic drinking and the percentage of people with problematic drinking have increased. Although there are suggestions that the aftermath of the crisis may take years to manifest, the literature to date does not provide sufficient results to estimate the long-term impact of the COVID-19 pandemic on alcohol consumption [2,9]. So far, a change in drinking patterns occurring 1 year after the pandemic has been observed in the French population, where 27.64% of the 2491 respondents reported an increase in alcohol consumption, with the phenomenon occurring primarily among men aged 26–44 years old [27].
Material and Methods
ETHICS STATEMENT:
The study was approved by the Ethics Committee for Human Research of the Medical University of Warsaw (no. AKBE/139/23).
The presented analysis of the mortality of Polish residents due to selected causes is based on individual data from the register of deaths of Polish residents kept by Statistics Poland. The register, with some necessary restrictions, is made available to the National Institute of Public Health NIH - National Research Institute to conduct analyses of the health status of Polish residents, following its statutory obligations. The analysis of selected countries’ residents’ mortality is based on raw data from the WHO database [28]. The presented results involve the authors’ own calculations based on data from these databases.
Information on the deaths of Polish citizens (all causes) is collected in a routine death registration system run by Statistics Poland [29]. On the death certificate, the physician confirming the death is obliged to enter 3 causes of death (description in words): the direct cause - description of the disease (injury) that became the final cause of death; secondary – a condition giving rise to the direct cause of death; and the underlying (initial) disease or circumstances of an accident, injury, poisoning, which initiated the chain of morbid events leading directly to death. The physician issuing the death certificate is not authorized to code the causes, he/she is only obliged to describe in words the disease conditions and other circumstances contributing to death.
The initial cause of death indicated above is coded by specially trained physicians, so-called coder doctors. Based on the descriptions (and in case of doubts in medical records or consultations with the physician who filed the death certificate), it is the coder doctor who is obliged to verify the records and resolve the underlying cause of death and assign its code according to ICD-10 5-digit codes. Causes of death statistics are recorded according to the underlying cause of death and the permanent residence of the deceased. The register, with all the records but without personal identifiers, is made available to the National Institute of Public Health NIH - National Research Institute for the purpose of conducting analyses of the health status of the Polish population, in accordance with its statutory obligations. The records contain information on causes of death, date of birth, date of death, sex, and urban or rural place of residence.
A direct method was used to standardize death rates against age. The new European structure, developed and used by Eurostat, was adopted as the standard age structure [30]. We aimed to investigate the norm deviation in the number of deaths occurring between 2020 and 2021, based on analyzing causes of death. To do so, we calculated the expected number of deaths in these years based on mortality in 5-year age groups within the 3 years between 2017 and 2019. Further, we took into account the population of these age groups on June 30th, 2020 and 2021, and calculated the excess percentage of the observed value over the expected one for the total Polish population by biological sex and urban-rural residence.
The calculation of the expected number of deaths was carried out using the following formula:
where:
Thus, the expected number of deaths can be interpreted as the number of deaths that would be expected if the intensity of deaths in 2020 and 2021, in 5-year age groups, were the same as in the 2017–2019 period, with the actual age structure of the population corresponding to 2020 and 2021. After dividing the value of the observed number of deaths by the expected value and multiplying by 100, the excess percentage number of deaths was obtained after eliminating the impact of the change in age structure. The study included mortality data from 3 major causes of death related directly to alcohol consumption: mental and behavioral disorders due to the use of alcohol (ICD10: F10), and 2 external causes of mortality, merged in the study: accidental poisoning by and exposure to alcohol (ICD10: X45) and poisoning by and exposure to alcohol, undetermined intent (ICD10: Y15). Data were divided according to biological sex and place of residence, information present in the death certificate that enabled alternate results for urban and rural areas.
To compare results with other European countries, 2 neighboring countries with higher alcohol consumption than Poland (11.7 L of pure alcohol per capita annually) were included in the study – Czechia (14.4 L) and Germany (12.9 L) [31].
Results
As presented in Figure 1, from 2011 through 2021, standardized death rates (SDR) for F10 had been declining steadily until 2014, when the trend reversed, and since 2015 the rate has increased rapidly, reaching 3-fold larger values in 2020. The increase was more prominent among men, who had 6 times higher SDR for F10 than women. The rates for urban and rural areas were close to the values of the total population; however, since 2017, a noticeable difference had accumulated to around 20% higher value for rural areas in 2020. In 2021, we observed a decrease in SDRs in all groups, on average by 20%, as compared to 2020. The alcohol-use-related deaths are specified according to WHO ICD-10 codes in Table 1.
SDRs for ICD10 codes X45 and Y15 (Figure 2), both of which are considered to be external causes of mortality, had been decreasing steadily in all groups from 2011 to 2016. However, from 2017 to 2018 it escalated, increasing slightly between 2019 and 2020, reaching a level comparable to that observed in 2016. However, in 2021 there was a major shift in previous trends as the SDRs increased by more than 40%. Similar to mortality rates for mental and behavioral disorders due to the use of alcohol (ICD10: F10), the general difference in SDRs observed between groups was 6–7 times higher for men, and 10–15% higher in rural than in urban areas.
To investigate if such differences in trends had been present in other countries, we compared SDRs for all 3 causes of death with those of the Republic of Czechia and Germany, where the consumption of alcohol is higher than in Poland. For a more detailed analysis, we used SDRs for men and women due to large differences in the rates between sexes. As depicted in Figures 3 and 4, F10 as a cause of death showed flat trends for women in both countries, although some alterations had been noted in terms of men – Germany exhibited a slight, approximately 10% increase in the period of 2013–2016, followed by a consequent decrease up until 2020, comparable to levels noted in 2011 (9.1 and 8.8, respectively). In Czechia’s male population, an increase was noticeable from 2019 to 2020, where SDR reached values that were approximately 30% higher than those noted in the previous years (3.1 compared to 2.1 on average).
Regarding mortality from external causes (X45 and Y15), the SDR values were on average 4 times lower than those in Chechia and Poland for both men and women in Germany. The trends in this country had not changed much within the observation period, with a slight decrease in 2012 and return to values from 2011 in 2016. In Czechia, a 25% increase in SDR among men had been observed since 2016, further fluctuating slightly (to around 4.0) in 2020.
In Poland, the COVID-19 pandemic and its public health restrictions were major factors that influenced both alcohol consumption during the lockdown period and access to necessary health services. A detailed analysis of expected values of mortality across all causes selected for the study was performed for 2020 and 2021 based on trends observed for 2017–2019. The gathered data were compared with these estimations. Table 2 summarizes major results, which indicate that the mortality across all causes was higher by 13% for 2020 and by 23% for 2021 than their expected values. Such an increase in mortality was attributed mainly to direct and indirect consequences of the COVID-19 pandemic. Meanwhile, the observed values for F10 were 22% higher than expected in 2020, in line with predictions for 2021. Higher than expected mortality was observed within the first year of the pandemic, characterized by the highest scale of lock-down-related limitations, like access to healthcare services. Data show that in 2020, women and residents of rural areas had been affected to a larger extent than men and residents of urban areas (31% vs 21% higher than expected for gender and 25% vs 20% for the place of residence). These differences decreased and showed an opposite trend in 2021, with men ranking 2% above predicted values and women ranking 4% below them. The value for urban area residents was 77% lower than expected, while outcomes for rural residents were similar to those expected (only 8% higher).
Interestingly, the relationship was the opposite for external causes of mortality (X45 and Y15). Overall, in 2020 the observed values were close to those estimated based on trends noticed in 2017–2019 (3% lower for the total population), while in 2021 they had exceeded predictions by 38%. Data for 2020 and 2021 showed that women were more likely to die from external causes than men, as well as those living in urban areas.
Discussion
MORTALITY DURING THE COVID-19 PANDEMIC:
Reported COVID-19 deaths are considered to be an inadequate tool for measuring the pandemic’s impact on excess global mortality. While analyzing these statistics, it is important to note that data reported by many countries may be inconsistent, due to inadequate COVID-19 detection (a problem most prominent in the early stages of the pandemic) or COVID-19 comorbid disease(s) interaction [32].
The WHO guidelines call for the COVID-19 mortality burden indicator to be based on excess mortality, regardless of its cause. Excess mortality is defined as the difference between the total number of deaths within the crisis period and expected mortality under normal conditions. Despite the total number of deaths being reported to the WHO, the fact that COVID-19’s health burden remains somehow uncertain must not be disregarded. On the one hand, underestimations may arise from a lack of testing for COVID-19 prior to death. On the other hand, overestimations may be caused by discrepancies in regulations pertaining to deaths arising from coronavirus infection and comorbid diseases. On May 5th, 2022, the WHO released reports on overestimations of COVID-19-related deaths [33]. Data from 79 countries were analyzed by Shang et al, who assessed cohort and cross-sectional studies published between January 1, 2020, and May 21, 2022 for excess mortality. Collectively, the studied population amounted to nearly 2.23 billion; reports involved almost 18 million deaths, with an estimated mortality value of 15.5 million [34]. Further, mortality data from 103 countries were analyzed by Karlinsky and Kobak, who found that reports exceeded the expected annual mortality by over 50% in Peru, Bolivia, Ecuador, and Mexico. In Peru, Bulgaria, North Macedonia, and Serbia, the excess mortality amounted to over 400 deaths per 100 000 population. In contrast, mortality during the COVID-19 pandemic was lower than expected in Australia and New Zealand, perhaps due to stricter social distancing and hygiene regulations preventing the spread of other infectious diseases [33]. Islam et al estimated excess deaths associated with COVID-19 in 29 high-income countries, suggesting that excess mortality was significant in all of the studied countries with the exceptions of New Zealand, Denmark, and Norway. In 2020, the highest excess mortality was exhibited by the United States (458 000, 95% CI: 454 000–461 000), followed by Italy, England, Wales, Spain, and Poland. Importantly, in many countries, estimated excess mortality surpassed the reported number of COVID-19 deaths, providing support for the pandemic’s indirect impact on healthcare inefficiency [35]. A comprehensive and consistent measurement of excess mortality was provided by a recent study that analyzed monthly data between 2020 and 2021 for 194 WHO member states. Estimates indicate 14.83 million excess deaths globally. This number exceeds the reported number of deaths due to COVID-19 by 2.74 times [36] (5.42 million, as of December 31, 2021; currently (3.2022) it is 6.9 million [37]). However, the number is as high as 18.2 million (95% CI: 17.1–19.6 million) according to some authors. Global excess mortality rate across all age groups averaged 120.3 deaths per 100 000 population (95% CI: 113.1–129.3) [35], while based on data from 79 countries, Shang et al estimated this value at 104.84. However, data from 21 countries show that the excess mortality rate was greater than 300 deaths per 100 000 people [34]. The rates of excess vs expected mortality were highest in Southeast Asia and Africa regions (22% for both), followed by the Middle East and Eastern Europe [34,36]. The highest excess mortality occurred in South America, with 134.02 per 100 000 population (95% CI: 68.24–199.80) per 100 000], while the lowest was in Oceania [−32.15 (95% CI: −60.53 to −3.77) per 100 000] [30]. A global analysis of excess mortality showed that 20 countries with the highest excess mortality accounted for 80% of the estimated excess deaths. Between January 2020 and December 2021, the highest excess mortality occurred in India (4.74 million, CI 95%: 3.31–6.45 million), followed by the Russian Federation, Indonesia, the United States, and Brazil; Poland was ranked 18th. Overall estimates suggest that middle- to low-income countries are responsible for more than 50% of the estimated excess mortality across the studied countries. However, low-income countries’ contributions to global excess mortality may be underestimated due to insufficient data from the African region. The authors estimated the percentage of excess mortality relative to expected mortality based on the p-score value, in turn reducing the effect of population size on the interpretation of the result. The highest p-scores were for Peru, Ecuador, Bolivia, Mexico, and Armenia. In Peru, the value was 97%, nearly doubling the COVID-19 mortality compared to that expected. The p-score was relatively low for India and the United States, indicating that compared to larger ones, smaller countries were less affected by the pandemic. Nevertheless, it was emphasized that the lack of sufficient data from some of the world’s regions required inference with a high degree of uncertainty [36]. The full impact that the pandemic has had on mortality goes far beyond focusing on deaths caused directly by the COVID-19 infection, and has resulted in a significant increase in excess mortality worldwide in almost every country. So far, no evidence of a subsequent compensatory reduction in mortality has been found.
INCREASE IN ALCOHOL-RELATED MORTALITY DURING THE COVID-19 PANDEMIC:
A study by Benzano et al indicates that individuals who abuse alcohol have more COVID-19 risk factors (such as more frequent smoking, liver disease, myocardial hypertrophy, and reduced immunity) than the general population. These individuals are more likely to have poorer prognoses and higher mortality for COVID-19 disease [39]. A study by White et al analyzed data from the National Center for Health Statistics (on mortality in the US), identifying a significant increase in the death rates among people over the age of 16, within the first year of the pandemic. Alcohol-related deaths increased by 25.5% in 2020 compared to 2019 (from 78 927 to 99 017). In contrast, increases in deaths due to other causes were relatively smaller (from 2 823 460 to 3 353 547 [18.8%]). In 2019, deaths due to alcohol consumption accounted for 2.8% of the total number of deaths, increasing to 3.0% in 2020. Rates were elevated in all age groups, with the largest increases found in the 35–44 age group (from 22.9 to 32.0 per 100 000 [39.7%]) and 25–34 age group (from 11.8 to 16.1 per 100 000 [37.0%]). It is worth noting that the increase in rates was similar for women (from 13.7 to 17.5 per 100 000 [27.3%]) and men (from 42.1 to 52.6 per 100 000 [25.1%]) [37]. Alcohol-related deaths reflect the hidden effects of the pandemic. Possible contributing factors involve increased alcohol consumption as a means of coping with pandemic-related problems and impeded access to health care [41]. Moreover, Chaudhry et al found that pancreatitis deaths related to alcohol abuse increased in 2020–2021 compared to 2018–2019. Data from the Centers for Disease Control and Prevention found an increase in the number of deaths from pancreatitis, with 515 and 501 deaths noted in 2019 and 2020, and 747 and 784 deaths noted in 2020 and 2021, respectively. A statistically significant increase in mortality was found among representatives of all age groups except those age 75–84. The increase in mortality was observed in both men and women (48% and 64%, respectively, P<0.001) [42].
INCREASE IN DEATHS DUE TO LACK OF ACCESSIBILITY TO MEDICAL CARE:
The restrictions that arose as a consequence of the pandemic may have presented a unique threat to those in recovery from alcohol-related disorders. Stress and negative affect are primary triggers for relapse [43]. Restrictions that imposed social distances, while consistent with public health guidelines, have resulted in hindered access to alcohol addiction treatments and recovery assistance. Given that millions of individuals are burdened with current or past addiction problems, the confluence of these indirect threats has made limited access to services a key public health concern during the pandemic [44]. The number of patients treated in outpatient mental health care facilities because of mental and behavioral disorders due to use of alcohol (F-10) in Poland rapidly decreased in 2020 by 14% as compared to 2019 (374 per 100 000 population and 425, respectively). Similarly, the number of first-time treated patients in 2020 for the same diagnosis decreased by 30% as compared to 2019 [45]. Despite the fact that the COVID-19 pandemic provided opportunities for one-on-one sessions or mutual support groups via the Internet, face-to-face therapy sessions and in-person support group meetings, which are often critical to the effectiveness of the therapeutic process and recovery, were unavailable to many during the worst part of the pandemic, in turn underscoring extreme difficulties in treatment [41]. As a result of restrictions that aimed to prevent COVID-19 transmission, the vast majority of SMART Recovery groups (supporting people with alcohol problems around the world) had been halted. SMART Recovery groups adjusted to these circumstances by providing online support groups to ensure treatment continuity, though the solution took time to implement and was not available immediately. According to information provided by the SMART Recovery country offices, prior to the onset of the COVID-19 pandemic, a relatively small number of SMART Recovery online groups were in operation in the United States (40 groups), England (5 groups), and Australia (6 groups). Nevertheless, the focus was on rapidly increasing the number of available online groups. However, in countries where such groups were not previously accessible, the transition was made more difficult and required establishing local infrastructure to support online groups, as well as training online facilitators. Therefore, the transition was hindered, resulting in fewer opportunities for needing to find help and support [46]. In addition, a study by Tu et al found that a decline in personal primary care visits during the pandemic was a global phenomenon. Estimates of excess deaths due to the COVID-19 pandemic suggest that the health consequences of the pandemic are not limited to direct COVID-19 infections but extend to deaths from a variety of other, seemingly unrelated causes, as well as numerous negative indirect effects, which may have arisen from limited access to healthcare [47]. Wu et al indicated that between March 2 and June 30, 2020, the number of deaths increased by 57 860 in England and Wales, 35% above normative predictions. Out of the 57 860 deaths, 50 603 (87% of excess deaths) were related to COVID-19. Finally, a significant increase in the number of at-home deaths was noted, suggesting that those who needed help had either had difficulty accessing healthcare or avoided it due to fear of infection [48].
LIMITATIONS:
This study has several limitations. The primary drawbacks include: (1) the questionable reliability of evidence (data aggregated in the routine death registration system by Statistics are from different sources); (2) although all physicians in Poland underwent the same programme of medical training, the indicated causes of death on the death certificate are filled in by different physicians and may become a source of diversity in collected data. The physician issuing the death certificate is not authorized to code the causes, he/she is only obliged to describe in words the disease conditions and other circumstances contributing to death. Despite these limitations in the study, these results are objectified by a physician authorized to assign the appropriate code for statistical purposes, which significantly reduced the risk of methodological errors.
Conclusions
Individuals who abuse alcohol have more COVID-19 risk factors (such as more frequent smoking, liver disease, myocardial hypertrophy, and reduced immunity) than the general population. Measuring the pandemic’s impact on global excess mortality is hindered by inconsistencies present in COVID-19 death reports. Across all causes, the mortality was higher than expected for 2020 and 2021, by 13% and 23%, respectively. The values observed for alcohol-related deaths due to mental health problems were higher than expected, by 22% in 2020, in line with predictions for 2021. However, in 2021 there was a major shift in previous trends as the SDRs increased by more than 40% in alcohol-related non-mental health-related problems (like poisoning by alcohol). In 2020, women and residents of rural areas had been affected to a larger extent than men and residents of urban areas. Higher than expected mortality was observed within the first year of the pandemic, characterized by the highest scale of lock-down-related limitations, like access to healthcare services.
Figures
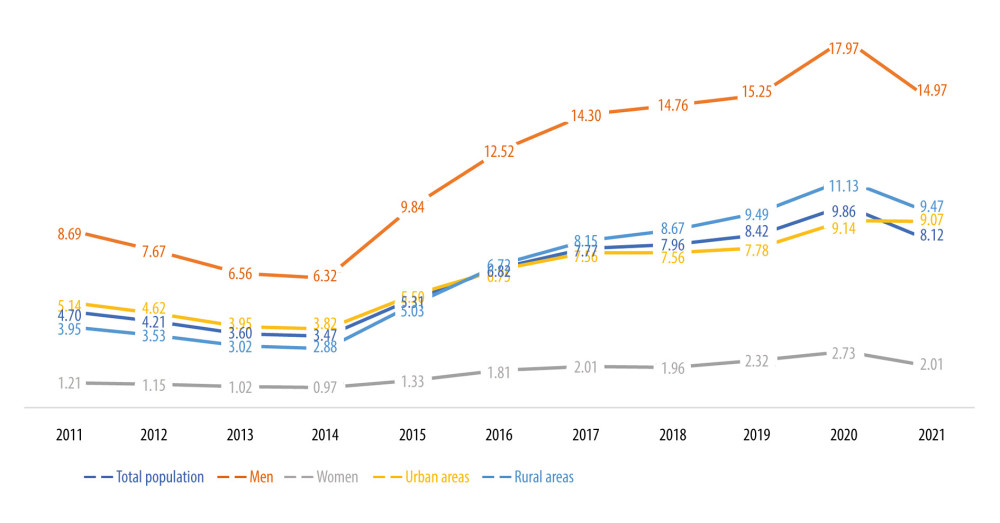 Figure 1. Standardized death rate (SDR) per 100 000 population for ICD-10 code F10 in Poland.
Figure 1. Standardized death rate (SDR) per 100 000 population for ICD-10 code F10 in Poland. 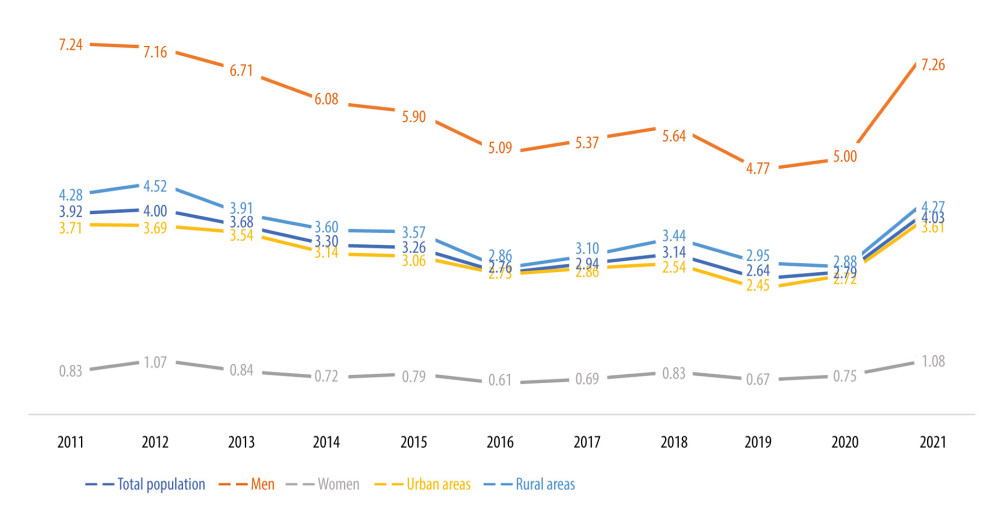 Figure 2. Standardized death rate (SDR) per 100 000 population for ICD-10 codes X45 and Y15 in Poland.
Figure 2. Standardized death rate (SDR) per 100 000 population for ICD-10 codes X45 and Y15 in Poland. 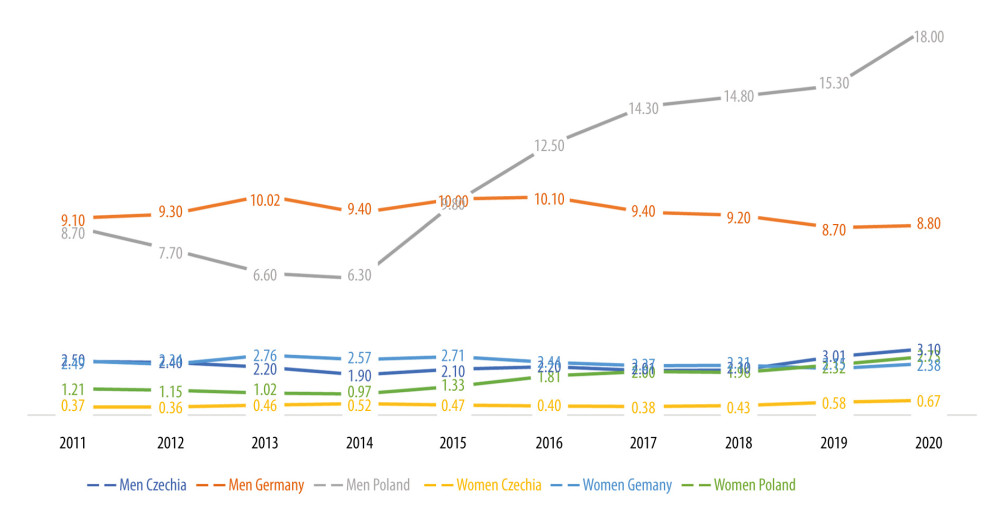 Figure 3. Standardized death rate (SDR) per 100 000 population in selected European countries for ICD-10 code F10.
Figure 3. Standardized death rate (SDR) per 100 000 population in selected European countries for ICD-10 code F10. 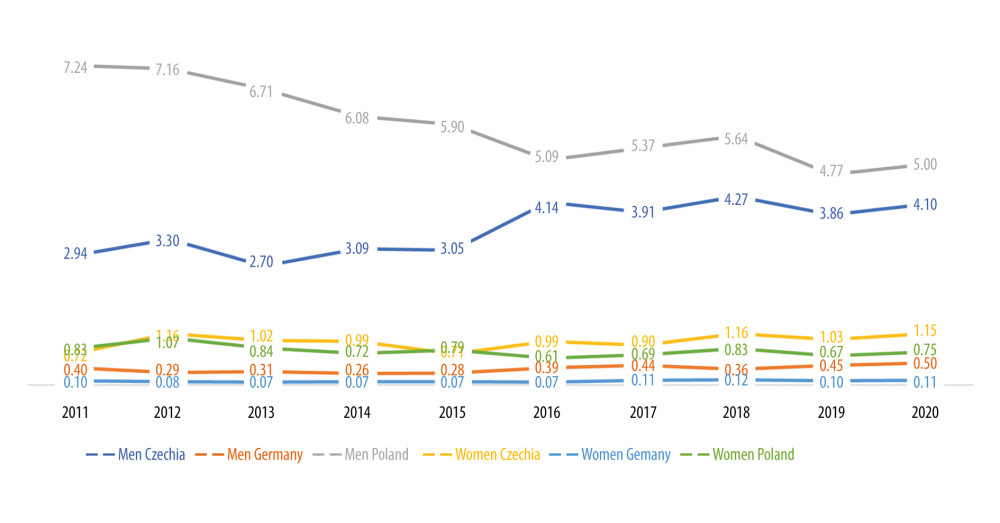 Figure 4. Standardized death rate (SDR) per 100 000 population in selected European countries for ICD-10 codes X45 and Y15.
Figure 4. Standardized death rate (SDR) per 100 000 population in selected European countries for ICD-10 codes X45 and Y15. References
1. Wang D, Gupta V, Crisis Intervention: StatPearls, 2023, Treasure Island (FL), StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC
2. Gonçalves PD, Moura HF, do Amaral RA: Front Psychiatry, 2020; 11; 581113
3. Karanikolos M, Mladovsky P, Cylus J, Financial crisis, austerity, and health in Europe: Lancet, 2013; 381; 1323-31
4. Keyes KM, Hatzenbuehler ML, Hasin DS, Stressful life experiences, alcohol consumption, and alcohol use disorders: The epidemiologic evidence for four main types of stressors: Psychopharmacology (Berl), 2011; 218; 1-17
5. de Goeij MC, Suhrcke M, Toffolutti V, How economic crises affect alcohol consumption and alcohol-related health problems: A realist systematic review: Soc Sci Med, 2015; 131; 131-46
6. Mateo-Urdiales A, Barrio Anta G, José Belza M, Changes in drug and alcohol-related mortality by educational status during the 2008–2011 economic crisis: Results from a Spanish longitudinal study: Addict Behav, 2020; 104; 106255
7. Rehm J, Kilian C, Ferreira-Borges C, Alcohol use in times of the COVID 19: Implications for monitoring and policy: Drug Alcohol Rev, 2020; 39; 301-4
8. Wu P, Liu X, Fang Y, Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak: Alcohol Alcohol, 2008; 43; 706-12
9. Bollen Z, Pabst A, Creupelandt C, Fontesse S, Longitudinal assessment of alcohol consumption throughout the first COVID-19 lockdown: Contribution of age and pre-pandemic drinking patterns: Eur Addict Res, 2022; 28; 48-55
10. Capasso A, Jones AM, Ali SH, Foreman J, Increased alcohol use during the COVID-19 pandemic: The effect of mental health and age in a cross-sectional sample of social media users in the U.S: Prev Med, 2021; 145; 106422
11. Evans S, Alkan E, Bhangoo JK, Tenenbaum H, Ng-Knight T, Effects of the COVID-19 lockdown on mental health, wellbeing, sleep, and alcohol use in a UK student sample: Psychiatry Res, 2021; 298; 113819
12. Fatke B, Hölzle P, Frank A, Förstl HCOVID-19 crisis: Early observations on a pandemic’s psychiatric problems: Dtsch Med Wochenschr, 2020; 145; 675-81 [in German]
13. Jones EAK, Mitra AK, Bhuiyan AR, Impact of COVID-19 on mental health in adolescents: A systematic review: Int J Environ Res Public Health, 2021; 18; 2470
14. Kilian C, Rehm J, Allebeck P, Alcohol consumption during the COVID-19 pandemic in Europe: A large-scale cross-sectional study in 21 countries: Addiction, 2021; 116; 3369-80
15. Boylan J, Seli P, Scholer AA, Danckert J, Boredom in the COVID-19 pandemic: Trait boredom proneness, the desire to act, and rule-breaking: Personality and Individual Differences, 2021; 171; 110387
16. Wardell JD, Kempe T, Rapinda KK: Drinking to cope during COVID-19 pandemic: The role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems, 2020; 2073-83, Wiley-Blackwell Publishing Ltd
17. Killgore WDS, Cloonan SA, Taylor EC, Alcohol dependence during COVID-19 lockdowns: Psychiatry Res, 2021; 296; 113676
18. Pollard MS, Tucker JS, Green HD, Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US: JAMA Netw Open, 2020; 3; e2022942
19. Rossow I, Bartak M, Bloomfield K, Changes in alcohol consumption during the COVID-19 pandemic are dependent on initial consumption level: Findings from eight European countries: Int J Environ Res Public Health, 2021; 18; 10547
20. Rodriguez LM, Litt DM, Stewart SH, Drinking to cope with the pandemic: The unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women: Addict Behav, 2020; 110; 106532
21. Lechner WV, Laurene KR, Patel S, Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings: Addict Behav, 2020; 110; 106527
22. Chodkiewicz J, Talarowska M, Miniszewska J, Alcohol consumption reported during the COVID-19 pandemic: The initial stage: Int J Environ Res Public Health, 2020; 17; 4677
23. Silczuk A, Threatening increase in alcohol consumption in physicians quarantined due to coronavirus outbreak in Poland: the ALCOVID survey: J Public Health (Oxf), 2020; 42(3); 461-65
24. Szajnoga D, Klimek-Tulwin M, Piekut A, COVID-19 lockdown leads to changes in alcohol consumption patterns. Results from the Polish national survey: J Addict Dis, 2021; 39(2); 215-25
25. Roberts A, Rogers J, Mason R, Alcohol and other substance use during the COVID-19 pandemic: A systematic review: Drug Alcohol Depend, 2021; 229; 109150
26. Sohi I, Chrystoja BR, Rehm J, Changes in alcohol use during the COVID-19 pandemic and previous pandemics: A systematic review: Alcohol Clin Exp Res, 2022; 46; 498-513
27. Villette PA, Lyonnard O, Trehu C, Changes in alcohol consumption after 1 year of the COVID-19 pandemic: A cross-sectional study in a region of France: Int J Environ Res Public Health, 2022; 19; 15049
28. WHO: Mortality Database https://www.who.int/data/data-collection-tools/who-mortality-database
29. [in Polish]https://stat.gov.pl/obszary-tematyczne/ludnosc/statystyka-przyczyn-zgonow/jak-gus-prowadzi-statystyke-zgonow,8,1.html
30. Pace M, Lanzieri G, Glickman M, Revision of the European standard population: Eurostat Methodologies and Working Papers, 2013
31. OECD: Preventing harmful alcohol use, OECD health policy studies, 2021, Paris, OECD Publishing https://.org/10.1787/6e4b4ffb-en
32. Karlinsky A, Kobak D, Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset: Elife, 2021; 10; e69336
33. : Global excess deaths associated with COVID-19 (modelled estimates) https://www.who.int/data/sets/global-excess-deaths-associated-with-covid-19-modelled-estimates
34. Shang W, Wang Y, Yuan J, Global excess mortality during COVID-19 pandemic: A systematic review and meta-analysis: Vaccines (Basel), 2022; 10; 1702
35. Islam N, Shkolnikov VM, Acosta RJ, Excess deaths associated with COVID-19 pandemic in 2020: Age and sex disaggregated time series analysis in 29 high income countries: BMJ, 2021; 373; n1137
36. Msemburi W, Karlinsky A, Knutson V, The WHO estimates of excess mortality associated with the COVID-19 pandemic: Nature, 2023; 613; 130-37
37.
38. , Estimating excess mortality due to the COVID-19 pandemic: A systematic analysis of COVID-19-related mortality, 2020-21: Lancet, 2022; 399; 1513-36
39. Benzano D, Ornell F, Schuch JB, Clinical vulnerability for severity and mortality by COVID-19 among users of alcohol and other substances: Psychiatry Res, 2021; 300; 113915
40. White AM, Castle IP, Powell PA, Alcohol-related deaths during the COVID-19 pandemic: JAMA, 2022; 327; 1704-6
41. Koob GF, Powell P, White A, Addiction as a coping response: Hyperkatifeia, deaths of despair, and COVID-19: Am J Psychiatry, 2020; 177; 1031-37
42. Chaudhry H, Sohal A, Sharma R, Increased mortality in patients with alcohol-induced pancreatitis during the COVID-19 pandemic: Ann Gastroenterol, 2023; 36(1); 68-72
43. McCaul ME, Hutton HE, Stephens MA, Anxiety, anxiety sensitivity, and perceived stress as predictors of recent drinking, alcohol craving, and social stress response in heavy drinkers: Alcohol Clin Exp Res, 2017; 41; 836-45
44. Bergman BG, Kelly JF, Fava M, Eden Evins A, Online recovery support meetings can help mitigate the public health consequences of COVID-19 for individuals with substance use disorder: Addict Behav, 2021; 113; 106661
45. Wojtyniak B, Gorynski P: Health status of Polish population and its determinants, 2022; 290, Poland, National Institute of Public Health NIH – National Research Institute access: https://www.pzh.gov.pl/download/32702/
46. Kelly PJ, McCreanor K, Beck AK, SMART Recovery International and COVID-19: Expanding the reach of mutual support through online groups: J Subst Abuse Treat, 2021; 131; 108568
47. Tu K, Sarkadi Kristiansson R, Gronsbell J, Changes in primary care visits arising from the COVID-19 pandemic: An international comparative study by the International Consortium of Primary Care Big Data Researchers (INTRePID): BMJ Open, 2022; 12; e059130
48. Wu J, Mafham M, Mamas MA, Place and underlying cause of death during the COVID-19 pandemic: Retrospective cohort study of 3.5 million deaths in England and Wales, 2014 to 2020: Mayo Clin Proc, 2021; 96; 952-63
Figures
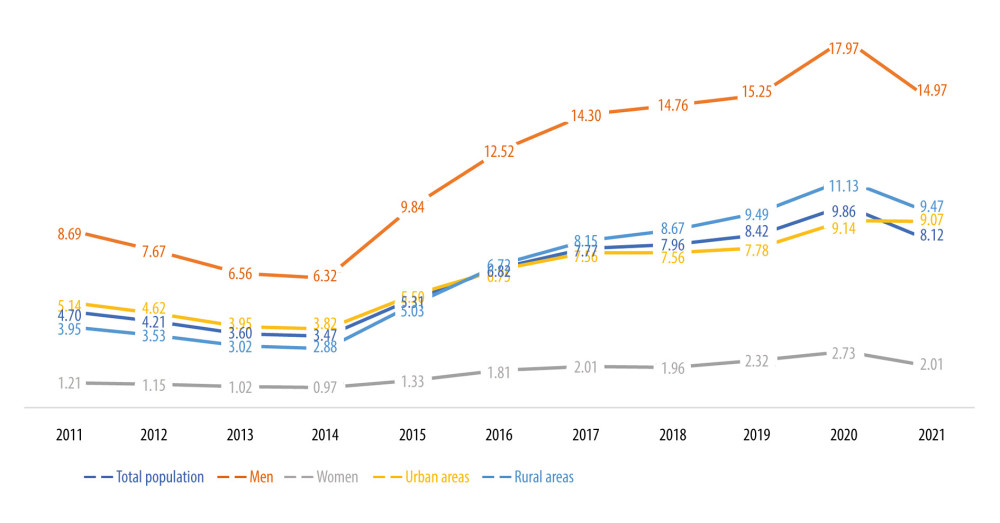 Figure 1. Standardized death rate (SDR) per 100 000 population for ICD-10 code F10 in Poland.
Figure 1. Standardized death rate (SDR) per 100 000 population for ICD-10 code F10 in Poland.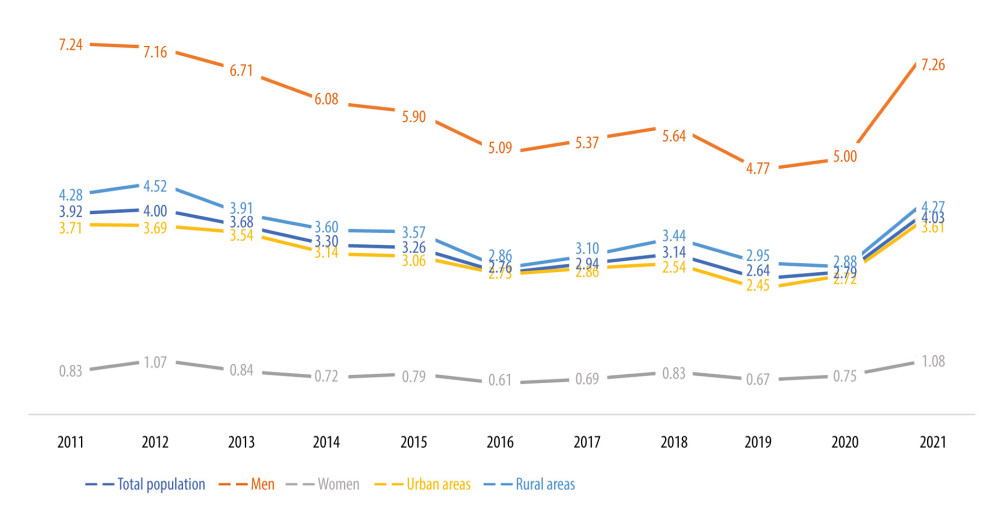 Figure 2. Standardized death rate (SDR) per 100 000 population for ICD-10 codes X45 and Y15 in Poland.
Figure 2. Standardized death rate (SDR) per 100 000 population for ICD-10 codes X45 and Y15 in Poland.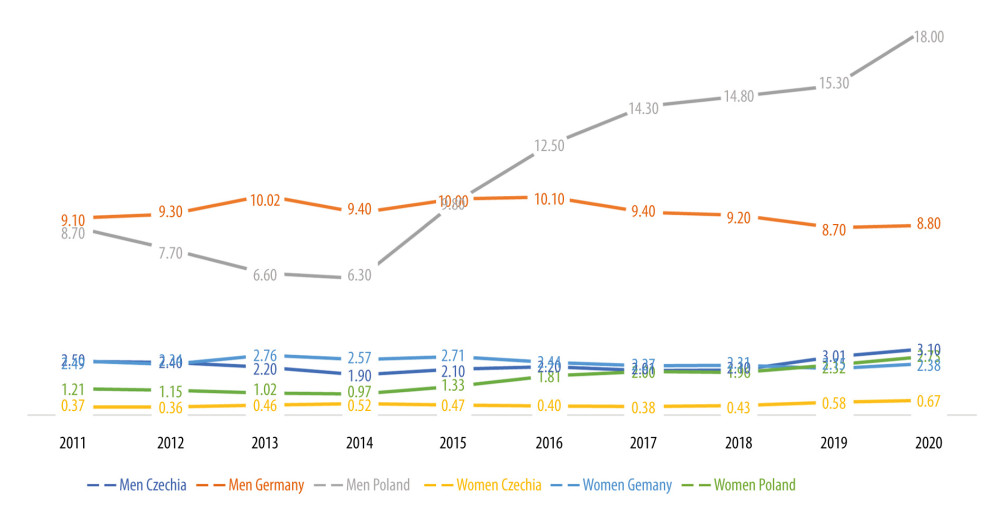 Figure 3. Standardized death rate (SDR) per 100 000 population in selected European countries for ICD-10 code F10.
Figure 3. Standardized death rate (SDR) per 100 000 population in selected European countries for ICD-10 code F10.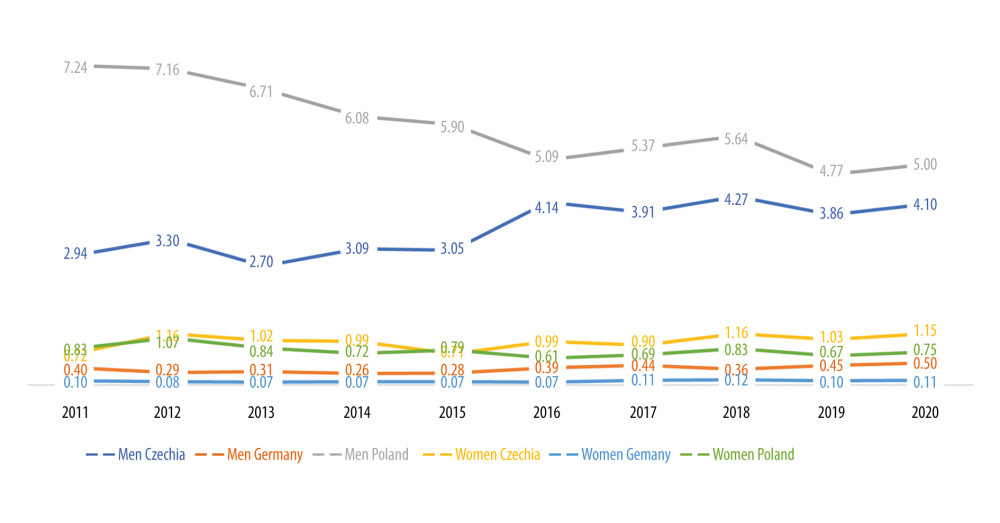 Figure 4. Standardized death rate (SDR) per 100 000 population in selected European countries for ICD-10 codes X45 and Y15.
Figure 4. Standardized death rate (SDR) per 100 000 population in selected European countries for ICD-10 codes X45 and Y15. Tables
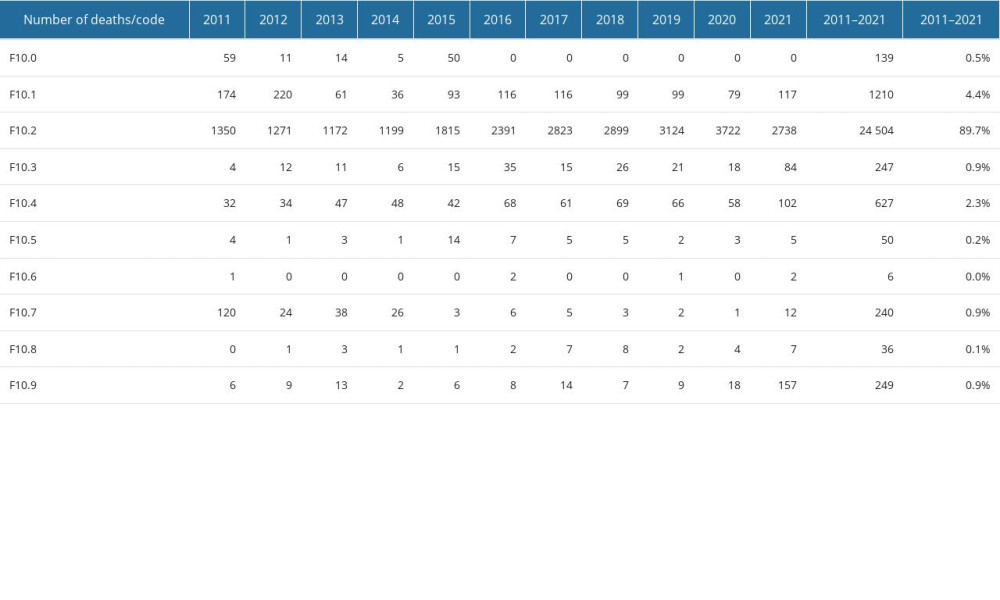 Table 1. Alcohol-use-related deaths according to WHO ICD-10 codes (F10.x).
Table 1. Alcohol-use-related deaths according to WHO ICD-10 codes (F10.x).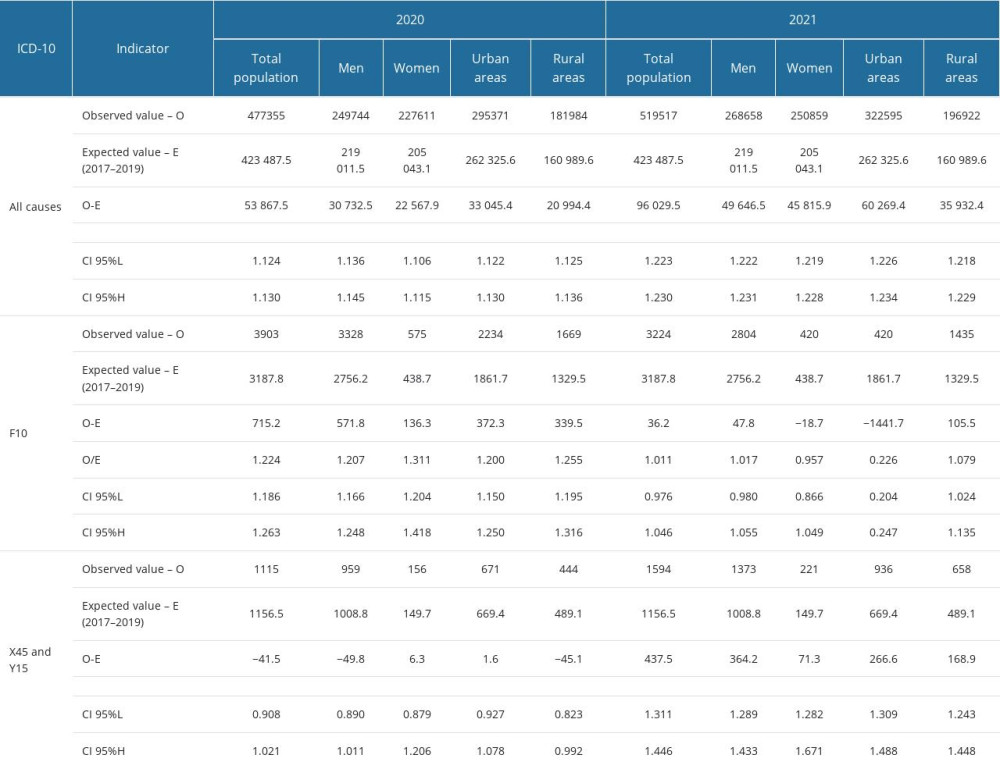 Table 2. Expected and observed deaths related to alcohol consumption in 2020 and 2021 in Poland.
Table 2. Expected and observed deaths related to alcohol consumption in 2020 and 2021 in Poland.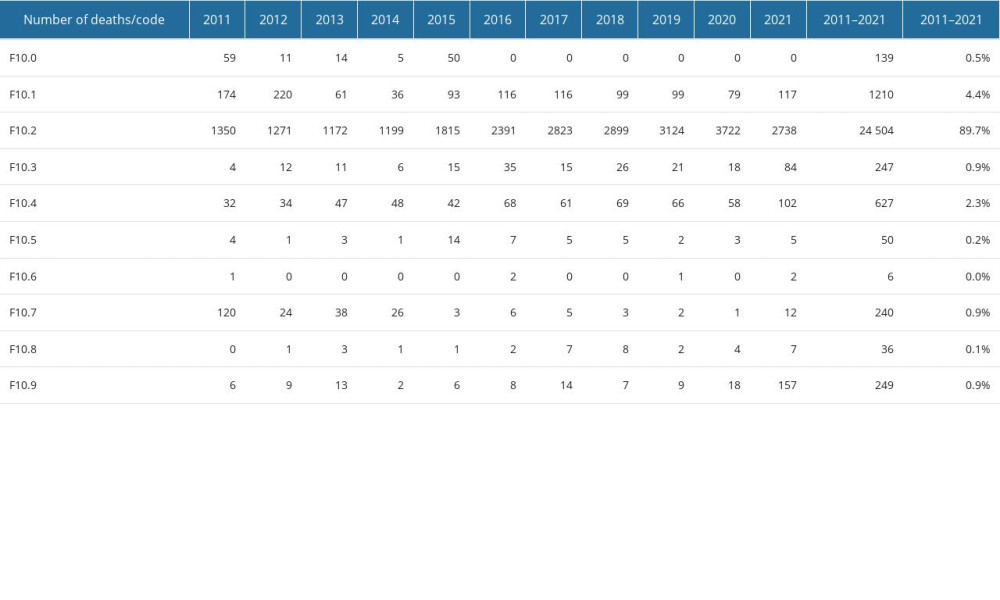 Table 1. Alcohol-use-related deaths according to WHO ICD-10 codes (F10.x).
Table 1. Alcohol-use-related deaths according to WHO ICD-10 codes (F10.x).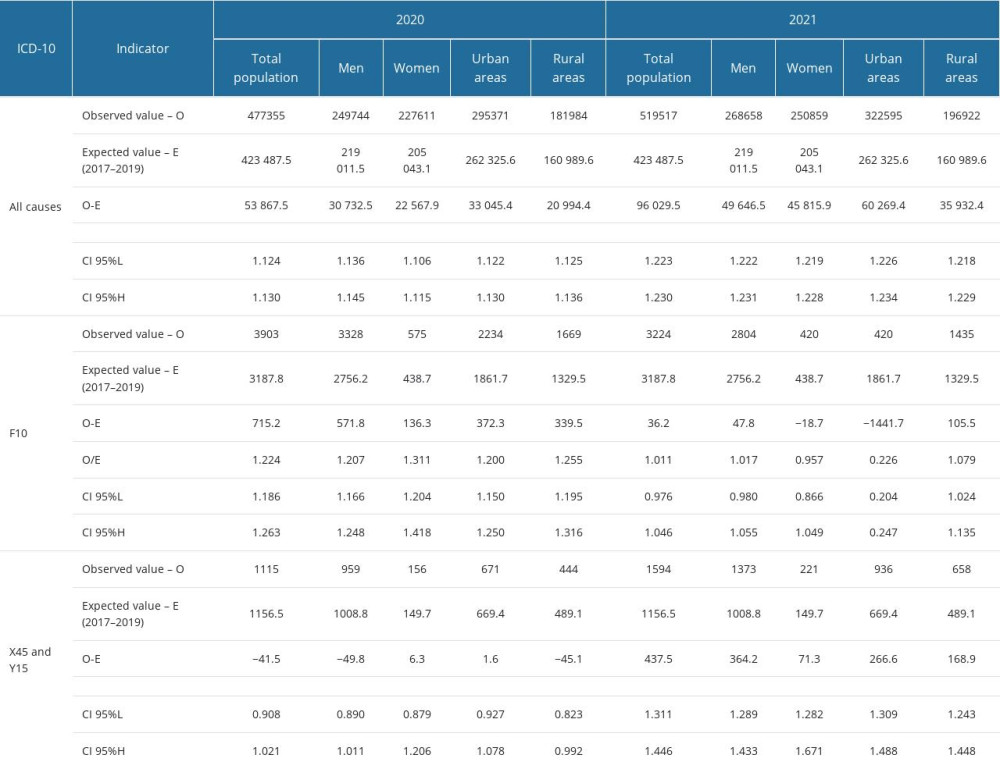 Table 2. Expected and observed deaths related to alcohol consumption in 2020 and 2021 in Poland.
Table 2. Expected and observed deaths related to alcohol consumption in 2020 and 2021 in Poland. In Press
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








