19 January 2023: Clinical Research
Determining the Impact of the COVID-19 Pandemic on Dental Care in the Serbian Adult Population: An Online Questionnaire-Based Study
Marija Nikolić1ABCDEF*, Aleksandar Mitić1ABE, Jelena PetrovićDOI: 10.12659/MSM.939238
Med Sci Monit 2023; 29:e939238
Abstract
BACKGROUND: Emergence of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 virus) could lead to an increase in dental anxiety, avoidance of dental visits, and general neglect of oral health. This online questionnaire-based study conducted in April and May of 2021 in Serbia aimed to determine the impact of the coronavirus disease 2019 (COVID-19) pandemic on dental care.
MATERIAL AND METHODS: The study included 2060 adult citizens of the Republic of Serbia who participated in an anonymous online questionnaire based on a 5-point Likert scale. Data were collected on dental care routine prior to and during the pandemic, and the fear of negative consequences for oral health. The results were statistically analyzed using descriptive statistics, Pearson’s correlation coefficient, ANOVA, and the paired t test.
RESULTS: Approximately one-fifth of the respondents postponed dental visits during the pandemic. Concern about postponing dental treatment was expressed by more than one-half of the respondents (57.1%), while 21.4% thought that they were already experiencing the consequences. Avoidance of preventive examinations and improvement of oral hygiene are more common among the elderly compared to younger respondents (P=.000).
CONCLUSIONS: The COVID-19 pandemic did not significantly affect the habit of avoiding dental interventions due to fear, but it did lead to part of the population completely avoiding even urgent dental interventions during the peak of the pandemic, and opting for tooth extraction rather than treatment. The strongest impact on dental care in the pandemic was among people over 64 years old.
Keywords: COVID-19, Dental Anxiety, Dental Care, Adult, Humans, Aged, Middle Aged, COVID-19, SARS-CoV-2, Pandemics, Serbia, Surveys and Questionnaires
Background
The odyssey of dental anxiety probably began in prehistoric times, since dental care can be traced back to the Neolithic era [1]. When we find ourselves in real danger, anxiety and fear are reasonable and useful responses, as is the avoidance which accompanies these emotions. However, if we see danger where there is none, then these emotions no longer have a protective function and are no longer useful [2].
Frightened and worried individuals feel that something terrible will happen during dental treatment, which is why they avoid the dentist [3]. Dental anxiety and dental phobia can be a reflection of complex psychological problems which have significant effects on the life of an individual, whether they cause avoidance, an increased incidence of caries, or poor oral health and quality of life [4]. Individuals experiencing dental anxiety only go to the dentist in case of an emergency, when often complicated and traumatic treatment is needed, which additionally increases their fear and leads to more complete avoidance in the future. Therefore, what ensues is a vicious circle of dental fear [5]. Etiological factors which cause dental anxiety are numerous, and can be aggravated by external factors [3].
The emergence of the COVID-19 pandemic, as one of the biggest health crises, has affected all aspects of people’s lives [6]. Fear for one’s own life, the lives of loved ones, and new living conditions has influenced the emergence of psychological stress, insomnia, and high prevalence of depressive symptoms and generalized anxiety in the population [6–8]. In addition to the impact on people’s mental health, COVID-19 is also associated with other diseases such as psychosomatic obesity and stroke [9–11], as well as complications of medical conditions resulting from the delay of necessary treatment due to the pandemic [12].
The specific nature of the services offered in a dental office can render it a high-risk location for the transmission of viruses. Most interventions include the production of aerosol and close contact with the patient, which places dental staff at much greater risk of infection or transmission [13–15]. During the first few months of the COVID-19 pandemic, most dental offices the world over paused their usual practice, limiting it only to emergency services, and provided patients with telephone consultations [13,16,17]. Unlike the period before the pandemic, during the pandemic, especially in the acute phase, fewer conservative procedures were performed, while the number of tooth extractions increased [18]. An increase in the extent of oral hygiene and preventive dental care are some of the recommendations given to decrease the need for dental interventions during the pandemic [19,20].
Additional measures were also introduced to control infection, which will probably remain in power for a time after the end of the pandemic, or until the fear completely disappears [13]. For dental professionals who have returned to work, implementing preventive measures has been an integral part of returning to their practice [21]. An increase in the number of telephone consultations was noted, while other sources cited a decrease in the flow of patients [22,23]. With new knowledge of the virus, its means of transmission, and with the onset of vaccination, dental practice gradually became available again. The pandemic is still not over, and for one segment of scared patients the reason for avoiding the dentist still exists.
A high level of fear of COVID-19 affects the increase in dental anxiety and decrease of oral health and oral health-related quality of life [24]. In addition to fear of infection, economic deterioration or unemployment can also contribute to neglect of oral health, along with the negative impact the pandemic has on the mental health of individuals [25–27]. No matter the reason, postponing or avoiding dental care and neglecting oral hygiene can have medical consequences, which are becoming a new reason for concern among people and a challenge for their dentists [28]. The consequences of delayed dental care can be expected in those who avoided care only in one part of the pandemic, while those consequences among individuals who still avoid going to the dentist can be severe [5]. Knowing the frequency of these consequences, as well as people’s habits related to dental intervention in a pandemic, can be of great importance to dental professionals to rehabilitate the negative effects of the pandemic together with their patients and to adopt the possible positive things that this negative experience has taught us, such as the importance of preventive examinations and oral hygiene, as well as the implementation of new measures that would make us more prepared for potential future health crises [29].
Therefore, this online questionnaire-based study conducted in April and May 2021 in Serbia aimed to determine the impact of the COVID-19 pandemic on dental care, including the impact on the change in people’s habits related to dental visits, their fear of the consequences of postponing dental treatment, their attitude towards undergoing dental services, and the implementation of preventive measures during the pandemic.
Material and Methods
ETHICS STATEMENT:
The study was granted approval from the Ethics Committee of the Faculty of Medicine, University of Niš (Approval number: 12-2213-2/3). Obtaining ethics approval by the Faculty of Medicine in Niš involved a data protection check in accordance with the Law of the Republic of Serbia assessed by a lawyer on the Ethics Committee. The questionnaire was voluntary and anonymous, and did not contain personal information that would enable identification of the respondents. The study was carried out in accordance with the Declaration of Helsinki. Informed consent was provided before the respondents started to answer the questions in the questionnaire, by clicking on the “I agree” box below the information about the study. If the potential respondents chose the option “disagree”, the questionnaire would close automatically. The respondents had the possibility of dropping out at any phase of the study. In addition to being simpler to apply and quickly providing a large amount of data, the online questionnaire was also chosen due to the pandemic conditions in which it was conducted, which implies avoiding social contact.
STUDY DESIGN AND RESPONDENTS:
The study was carried out via an online questionnaire distributed through social networks and online channels during March and April 2021. A representative sample was determined based on data from the Statistical Office of the Republic of Serbia (for the adult population of the Republic of Serbia in 2021) using a 95% confidence level and margin error of 3%, which included a minimum of 1067 respondents [30]. The study included 2060 adults. The inclusion criterion for the study sample was being an adult citizen of the Republic of Serbia who agreed to participate in the study.
There were 1339 female respondents and 721 male respondents; 45% were age 18–34 years, 35% were 35–49, 15% were 50–64, and 5% were over age 64.
QUESTIONNAIRE:
The questionnaire was developed after analyzing the available literature on the impact of the COVID-19 pandemic on dental care, in accordance with the aims of the study, and following the Stehr-Green steps for designing a questionnaire [31]. The survey questions were prepared using Google Forms. Fourteen closed-ended questions (with categorical response options or ordinal response options) included in the survey were grouped into 3 sections. It took less than 3 min to complete the questionnaire. The reliability of the survey was determined based on the value of Cronbach’s Alpha test of 0.707.
Section 1 of the questionnaire referred to the demographic data (gender and age), and consisted of 2 questions. Section 2 also consisted of 2 questions, both of which were related to the respondents’ dental care routine prior to the pandemic, pertaining to any bad habits the respondents may have, which could be affected by the pandemic. Therefore, these 2 questions were also asked in section 3, which was related to the respondents’ dental care routine during the pandemic. The remaining 8 questions of section 3 referred to consequences of postponing professional dental care (2 questions), to extreme avoidance of dental services (2 questions), and to preventive measures, which could eventually delay the negative consequences of postponing treatment (4 questions). The focus of section 3 was on dental care during the pandemic itself. The questions are shown in Table 1.
Except for 2 questions related to demographic data, all questions were based on a 5-point Likert scale. The answer options for question number 7 (Q7. How would you rate any possible feelings of concern about potential consequences of postponing dental treatment due to the pandemic caused by the SARS-CoV-2 virus?) were Not Anxious, Slightly Anxious, Fairly Anxious, Very Anxious, and Extremely Anxious (ranked from 1 for Not Anxious to 5 for Extremely Anxious). For all the other questions from Q3 to Q14 (except Q7), the respondents stated their level of agreement in 5 points, and the answer options were Strongly Disagree, Disagree, Undecided, Agree, and Strongly Agree (ranked from 1 for Strongly Disagree to 5 for Strongly Agree). The obtained scores were used for statistical analysis.
The study was preceded by a pilot study. The final version of the questionnaire was formed after verification of the question construction by 2 experts for the formation of the questionnaire and professional verification by 2 university professors from the corresponding scientific field.
STATISTICAL ANALYSIS:
Statistical analysis was performed using the SPSS, version 22.0 software. For data analysis used descriptive statistics (percentage, mean, standard deviation); Pearson’s correlation coefficient was used to determine the relationship between responses; ANOVA was used to analyze the differences between dependent and independent variables (age); the paired
Results
:
Approximately one-fifth of the respondents (21.8%) postponed dental visits out of fear even prior to the pandemic (mean [M]=2.10, standard deviation [SD]=1.491), while dental visits were postponed during the pandemic by almost the same number of respondents – 21.6% (M=2.11, SD=1.483). The statistical analysis showed that this habit did not change significantly during the pandemic compared to the period before the pandemic (P=0.665) (Table 2). To avoid or postpone a dental visit, 11.2% of the respondents “treated” their dental problems themselves (eg, took medicine, applied compresses, rinses) prior to the pandemic (M=1.65, SD=1.217), while 9.2% of them did the same during the pandemic (M=1.57, SD=1.112). This difference in the percentage of respondents resorting to methods of “treating” their dental problems themselves prior to and during the pandemic was statistically significant (P=.004) (Table 2).
CONSEQUENCES OF POSTPONING DENTAL CARE AND EXTREME AVOIDANCE OF DENTAL TREATMENT (DESCRIPTIVE STATISTICS THE ANOVA TEST FOR QUESTIONS Q7, Q8, Q9, AND Q10):
More than one-half of the respondents (57.1%) stated that they felt some level of concern about the possible consequences of postponing dental treatment due to the COVID-19 pandemic (M=1.89, SD=0.986). More than one-fifth of the respondents (21.4%) believed they were already experiencing the consequences of postponing dental care (M=2.13, SD=1.433). A smaller group of respondents (8.4%) would rather extract a tooth than treat it, so as to avoid the possibility of infection during multiple treatments (M=1.55, SD=1.098). During the peak of infection, 7% of the respondents would not go to see a dentist, even at the cost of enduring strong pain, swelling, and worse dental appearance or function (M=1.48, SD=1.024). Looking at the data in relation to the age of the respondents, in all the studied aspects of extreme avoidance and the consequences of delaying dental care a statistically significant difference was confirmed. Concern about the possible consequences of delaying dental interventions (P=.000), the opinion that they were already experiencing consequences (P=.000), choosing tooth extraction instead of multi-session treatments (P=.000), and extreme avoidance of dentists at the peak of infection (P=.000) were most common among respondents in the oldest age group (over age 64 years) and were least common among the youngest group (age 18–35 years) (Table 3).
PREVENTIVE MEASURES (DESCRIPTIVE STATISTICS AND ANOVA FOR QUESTIONS Q11, Q12, Q13, AND Q14):
During the pandemic, 51.4% of the respondents would receive any kind of dental treatment or go in for preventive check-ups (M=3.36, SD=1.575). In relation to age, a statistically significant difference was confirmed, indicating that majority of younger respondents (most often from the 18–34 age category) would go to the dentist for a preventive check-up during the pandemic (M=3.61, SD=1.485), in contrast to the oldest group of respondents (over 64 years old) who generally would not go to the dentist for a preventive examination under those circumstances (M=2.61, SD=1.567) (Table 4).
An improvement in oral hygiene and habits to prevent the onset or further complication of dental problems during the pandemic was reported by 40% of the respondents (M=3.07, SD=1.517). A statistically significant difference was confirmed in relation to age, whereby the oldest respondents (over 64 years old) improved their oral hygiene the most in order to prevent the occurrence of dental problems (P=.005) (Table 4). Oral hygiene was neglected by 4.4% (M=1.35, SD=.852), while a change in dietary habits, in a negative sense, was reported by approximately one-fifth of the respondents – 21% (M=3.36, SD=1.575).
CORRELATION ANALYSES (PEARSON’S CORRELATION COEFFICIENT):
The correlation analyses led to the following findings in the case of bad habits related to dental care prior to and during the pandemic. A statistically significant positive correlation was noted for postponing dental visits prior to and during the pandemic (Correlation coefficient=.283; P=.000, statistically significant for P<.01). In addition, the respondents resorted to methods of “treating” their dental problems themselves prior to and during the pandemic (correlation coefficient=.441; P=.000, statistically significant for P<.01). The remaining correlation analyses are shown in Tables 5 through 8.
Discussion
At the beginning of the pandemic, studies were primarily concerned with protective measures against the spread of the virus in the dental environment [13,14,32–34]. Given that the pandemic is lasting longer than expected, there have also been studies dealing with its impact on dental practice [23,28,35]; those focusing on the effects on oral health are particularly important [20,36]. Studies conducted in Serbia linking COVID-19 and dental care analyzed the financial burden of dental care, the impact on dental professionals and their practice, and the mental health of dental students [37–39]. The present study focused on dental care in Serbia during the pandemic from the patient’s point of view, with an analysis of the differences in dental care habits before and after the pandemic.
The results in this study indicated that the pandemic did not impact changes in habits regarding postponing dental interventions, since individuals who stated that they avoided dental visits due to the pandemic did so prior to the pandemic as well. Thus, we can assume that the cause of these poor habits is primarily the basic fear which a patient has of dental interventions, while the fear of contracting the SARS-CoV-2 virus represents an additional reason or maybe even justification for avoiding what was already an unpleasant place for these individuals. Resorting to “treating” their dental problems themselves during the pandemic has significantly decreased compared to the period before the pandemic, and the reason could be the fear that unprofessional “treatment” could further worsen their problems.
Medical treatments have been postponed due to fear of COVID-19, which could lead to serious health complications in the near future [12]. Almost 60% of the respondents feel some level of concern regarding the postponement of dental treatment, and one-fifth believed they were already experiencing the consequences. The results indicate that even though more than one-fifth of the respondents stated that they postponed dental treatment due to fear of the virus, almost 3 times as many were afraid of the consequences of postponing. An explanation could be that the reasons for postponing a dental visit during the pandemic were not necessarily caused by fear of COVID-19, but by the various impacts of the pandemic on the life of an individual [6]. Greater fear of the consequences of postponing dental care was found among the respondents who had postponed dental visits due to the pandemic, those who believe they were already experiencing the consequences, and those who would not visit a dentist during the pandemic (Table 5).
The correlation analysis obtained in this study indicated that the opinion “I think I am already experiencing the consequences of postponing dental care” was more frequent among those who postponed dental visits during the pandemic, as well as those who would not visit a dentist during the pandemic for preventive and other treatments (Table 6). These results are expected and logical. On the other hand, considering that the study indicated that individuals who postponed dental visits during the pandemic mostly did so before, the self-evaluation of the respondents who believe they are already experiencing the consequences of postponed care should not be taken at face value, as they could be a consequence of prolonged postponement of dental interventions and not just postponement during the pandemic.
A smaller percentage of the respondents stated that their fear of the SARS-CoV-2 virus led them to have an extreme response when it comes to avoiding dental visits during the pandemic – “I would rather have my tooth extracted than expose myself to repeated possibilities of contracting the SARS-CoV-2 during treatment which requires that I see a dentist more than once” and “I would not go to see the dentist during the peak of infection even if it meant experiencing severe pain, swelling, decayed dental appearance or function” (8.4% and 7%, respectively). These opinions were more frequent among respondents who postponed dental visits during the pandemic, those who feared the consequences of postponing dental care, and those who believed they were already experiencing the consequences (Table 7).
The results indicated that respondents who postponed dental visits due to the pandemic, those worried about the consequences of postponing dental care, and those who believed they were already experiencing the consequences more frequently stated that they changed their dietary habits during the pandemic (they consume more food and of lower quality), that they are neglecting their oral hygiene, but that they have improved their habits and hygiene as well (Table 8). This discrepancy of opposing opinions could mean that they had differing opinions regarding oral hygiene at different times during the pandemic, considering that one response does not preclude the other, and that the pandemic has lasted longer than expected. More than half of the respondents would go for preventive dental check-ups, which is one of the positive effects of the pandemic, even though it is likely dictated by the fear that treatment during the pandemic is a worse option than a dental examination.
When the age of the respondents is observed, it seems that the strongest impact of the COVID-19 pandemic on the dantal care was among oldest population. Respondents who would rather extract a tooth than treat it, those with a greater fear of the consequences of postponing dental treatment, those who believe they are already experiencing the consequences, and those who would not visit a dentist during the pandemic are most common among members of the oldest group (over 64 years old), and they are less common with the decrease in the age of the respondents (Table 3). Also, the respondents in the oldest group renounced preventive measures to the greatest extent, but they also reported an improvement in oral hygiene more than the other groups (Table 4). These results are expected, given that the elderly are one of the most vulnerable population groups when it comes to COVID-19, and that preventive examinations are the most delayed of all treatments [6,21]. Avoiding dental treatments leads to consequences and this causes concern for this age group. Although these data are expected, they have a special importance because the elderly as a sensitive group require special attention, and the knowledge that their oral health suffered the greatest negative impact in the pandemic can be useful to dental professionals in their daily practice.
The beginning of the pandemic brought about numerous dilemmas due to the emergence of a previously unknown type of virus. An international questionnaire-based study conducted in 37 countries in the spring of 2020 showed that only 14 countries implemented routine dental treatments, while these services were reduced to emergency services in 13 countries (the findings refer to public and private dental practice) [17]. Dental practice balanced between an obligation to care for one’s patients and the rights of the practitioner to their life and the protection of the lives of their team and loved ones. Initially, the general recommendation was to, if possible, postpone all dental treatments [32]. This might be why dental fear became deeply rooted among frightened patients during the pandemic, even when dental care was available again due to adequate protective measures.
The obtained results that show concern about the consequences of postponing dental treatments are congruent with those of Cotrin et al (a questionnaire-based study conducted in Brazil) who determined that 65.3% of dental patients worry about the impact of postponing treatment during quarantine, and state their most frequent worry to be the delay of the end of treatment. The respondents evaluated the extent of their worry about the impact of the pandemic and quarantine on their treatment on a scale of 1 to 10, whereby a mean level of 4.04 (SD=2.34) was obtained. The same study determined that respondents who did not want to visit an orthodontist due to fear were more worried about the outcome of their treatment, as were those who would only do so in an emergency [27]. The results obtained in the present study indirectly indicate that the reason for postponing was not only the fear of contracting COVID 19 in a dental office because the consequences are of concern to 3 times the number of respondents than the number of respondents who cite the fear of infection with COVID19 as the reason for avoiding treatment. These reasons are confirmed by researchers from Spain who announced that the fear of COVID-19 is the reason for avoiding dental visits in 24.5% of all cases, finances are the reason in 16% of all cases, while in 3.2% of all cases it is some other reason [40]. The current pandemic has, apart from the fear for one’s life and health, also caused an economic crisis, increased unemployment and financial uncertainty, and along with the measures of social distancing and isolation, contributed to the negative impact on the mental health of people [25,36,41]. Analyzing the influence of age on the cancellation of dental treatments, more frequent cancellation of dental treatments in the older group of respondents was noted by researchers from Poland [28], in contrast to Cotrin et al (a questionnaire-based study conducted in Brazil), who did not find a relationship between the age of the respondents and the willingness to go to the dentist during the pandemic. The difference in results is probably due to the fact that their mean age of respondents was 35.49 years.
When it comes to extreme avoidance of dental care in the pandemic and resorting to extraction instead of dental treatment, the prevalence of these phenomena was lower in the present study then in similar studies conducted earlier. Researchers from Italy determined that 15.1% of parents who reported a higher level of fear would not take their children, in even for urgent dental treatment [26], while Cotrin et al found that 14.7% of orthodontic patients in Brazil would not go in for dental treatment during the pandemic and quarantine [27]. The difference in the results could be ascribed to the different study designs and the situations in these countries at the time of the survey. An increase in the number of tooth extractions with a simultaneous decrease in conservative interventions was noted by Nijakowski et al (study conducted in Poland), while Goriuc et al agreed that in order to prevent the transmission of infection, to shorten the intervention time, and to avoid multi-session procedures, the choice of extraction in relation to dental treatment is logical [18,29]. Barabari et al stated that it was expected that dental treatments which were not urgent would be avoided even when the pandemic began to wind down, and that tooth extraction would be the treatment of choice compared to endodontic treatment, as a consequence of the fear of contracting the SARS-CoV-2 virus [19].
When it comes to the implementation of preventive measures, our results are similar to those of Campagnaro et al (a questionnaire-based study conducted in Brazil), showing that 61.5% of the respondents changed their dietary habits during the pandemic and quarantine. Of them, only 33.1% did so for the better, while the others stated that they consumed more food of lower quality, and those who lost their income stated that they consumed less food of lower quality. The same authors determined that 1.8% of parents did not brush their children’s teeth, while 14.7% did so occasionally [26]. Insignificant differences in the results could be ascribed to the different concepts of the studies themselves. Amato et al concluded that 28% of patients from Italy were worried about returning to the dentist and that 71% would only go for urgent treatment [20]. Barbari et al believe that a generalized fear of dental interventions could occur among the population in the post-pandemic period, and that this fear would force some fearful patients to partake in preventive measures and increase their level of oral hygiene [19].
Unfortunately, the pandemic is still ongoing, people and dental practice have adapted to the new circumstances, and there is room for optimism when it comes to the return of patients to dental offices. The existence of patients with dental phobia observed in this study, who would not visit a dentist during the pandemic at any cost, or would resort to radical solutions such as tooth extraction instead of treatment, as well as the fact that they are the most common among the oldest population, should especially concern dentists as professionals. This study also showed that the pandemic did not significantly affect the habits of dental patients, because dental anxiety and bad habits are a problem that exists unrelated to the pandemic and should be the focus of further research.
Although the questions in the questionnaire were formed in such a way so as to refer to the entire period of the pandemic up to the moment of conducting the study, its limitation could be the fact that it was carried out during 2 months (March and April 2021) and that, accordingly, it reflects only a certain period of the pandemic.
The basic limitation of studies with a cross-sectional design is that they are not suitable for determining cause-and-effect relationships. The sample could have been affected by the fact that participation in the study required access to the internet and skill to complete an electronic questionnaire.
Conclusions
The COVID-19 pandemic did not significantly affect the habit of avoiding dental interventions due to fear, but it did lead to a part of the population completely avoiding even urgent dental interventions during the peak of infection, and opting for tooth extraction rather than treatment. The consequences that the pandemic could have on oral health due to postponed treatment worried most people (57.1%), while slightly more than one-fifth believed they were already experiencing the consequences. In an attempt to take preventive measures, 40% of the respondents have opted to improve their dental hygiene, and more than half of the respondents would go for a preventive examination regardless of the pandemic. The strongest impact on dental care in the pandemic was in people over 64 years old. Irrespective of whether the reason for postponing a dental visit is pre-existing fear or the pandemic, the outcome is still the same – avoidance of necessary care, which could have significant consequences on dental practice and human oral health.
Tables
Table 1. The questions included in the questionnaire.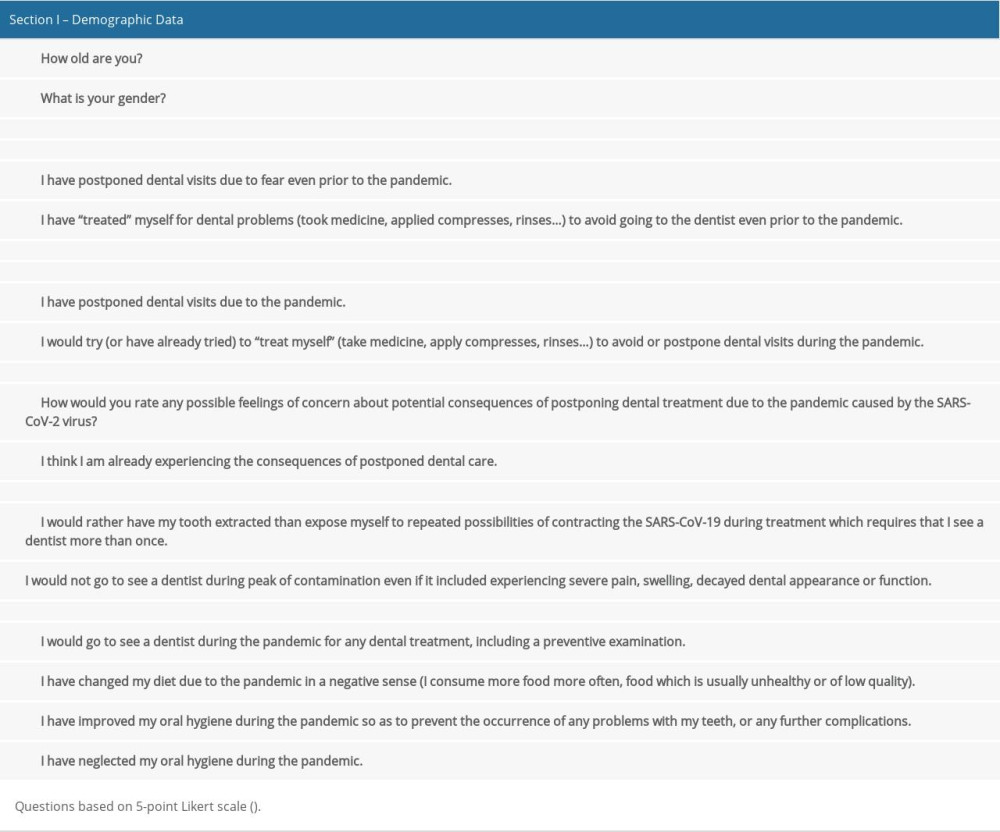 Table 2. The significance of the differences between observed habits related to professional dental care (questions Q3, Q4, Q5, Q6) paired before and during the pandemic (paired t test).
Table 2. The significance of the differences between observed habits related to professional dental care (questions Q3, Q4, Q5, Q6) paired before and during the pandemic (paired t test).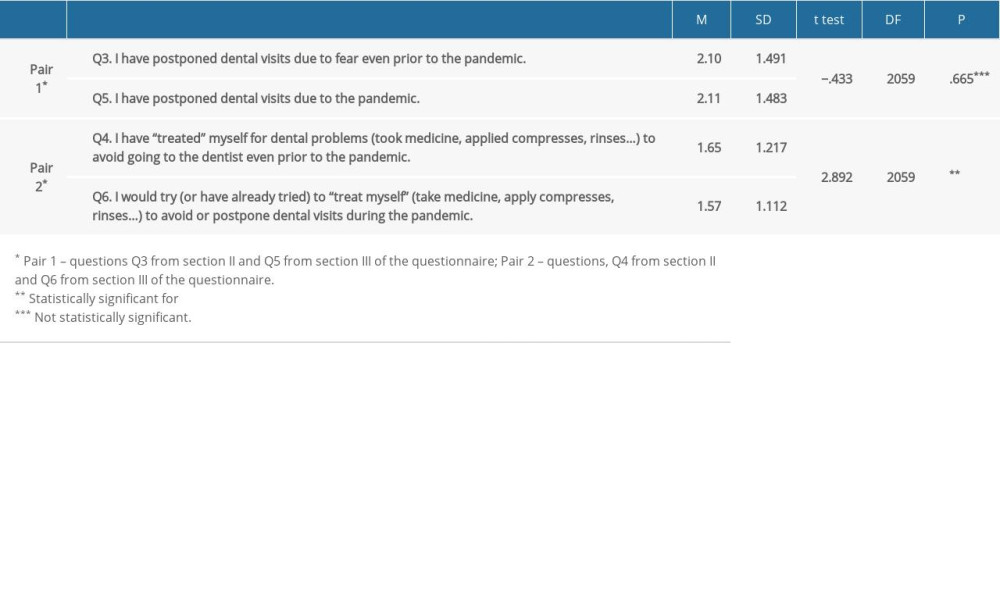 Table 3. The differences in the consequences of postponed dental treatments (questions Q7 and Q8) and extreme avoidance regarding the respondents’ age (questions Q9 and Q10) from section III of the questionnaire).
Table 3. The differences in the consequences of postponed dental treatments (questions Q7 and Q8) and extreme avoidance regarding the respondents’ age (questions Q9 and Q10) from section III of the questionnaire).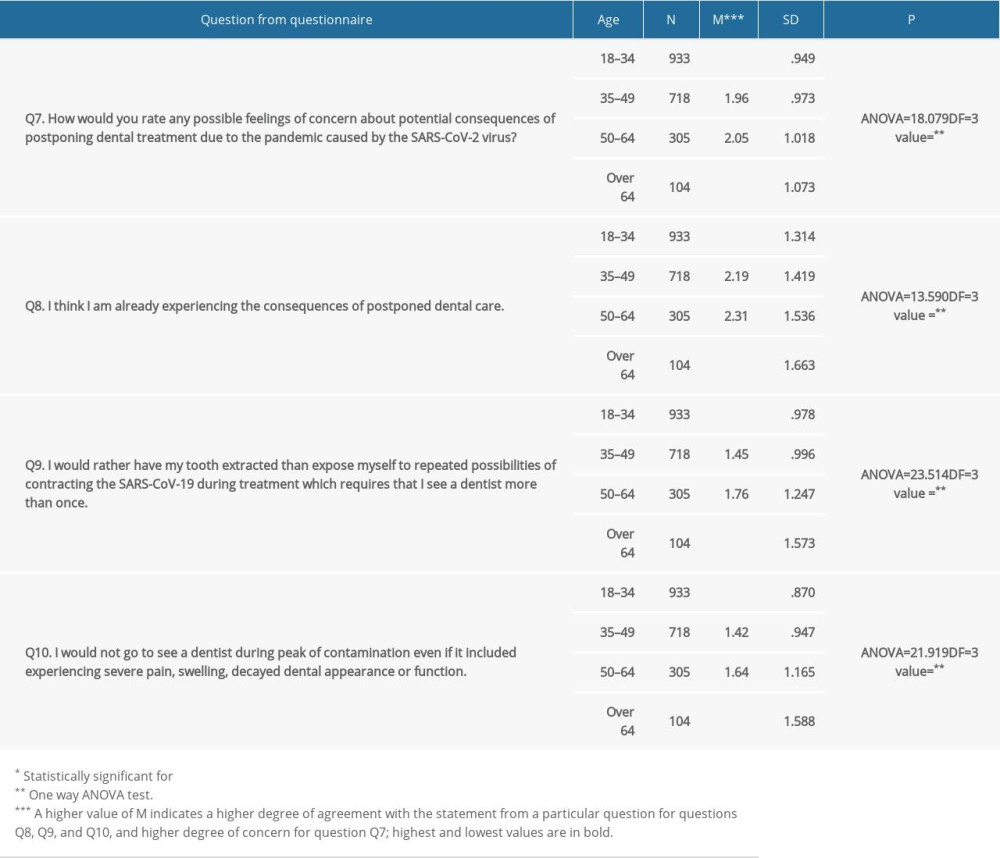 Table 4. The differences in the observed preventive measures during the pandemic regarding the respondents’ age (questions Q11 and Q13).
Table 4. The differences in the observed preventive measures during the pandemic regarding the respondents’ age (questions Q11 and Q13).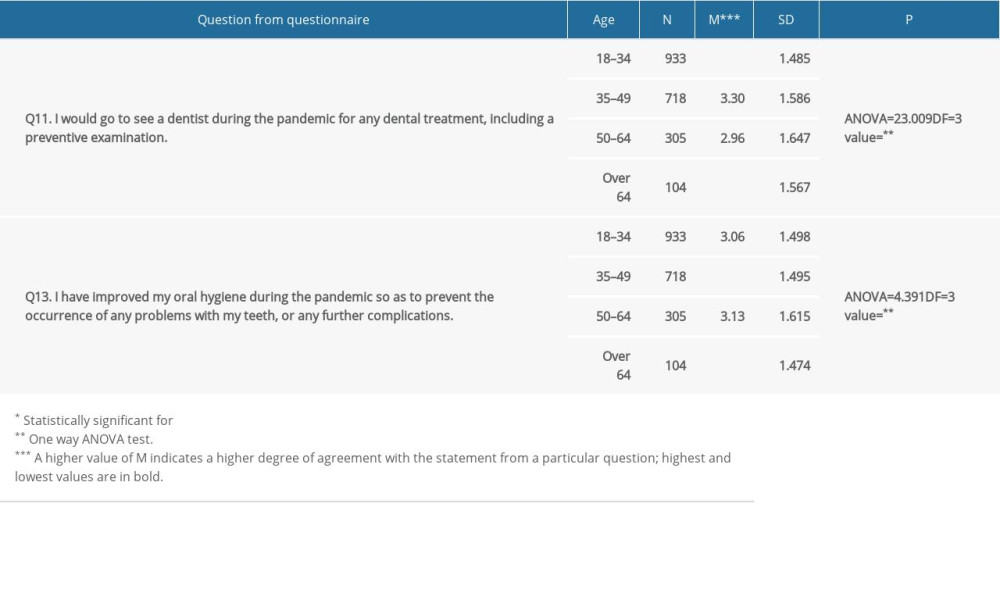 Table 5. Correlation analysis – correlation coefficients for the responses to question Q7 and questions Q5, Q8, and Q11.
Table 5. Correlation analysis – correlation coefficients for the responses to question Q7 and questions Q5, Q8, and Q11.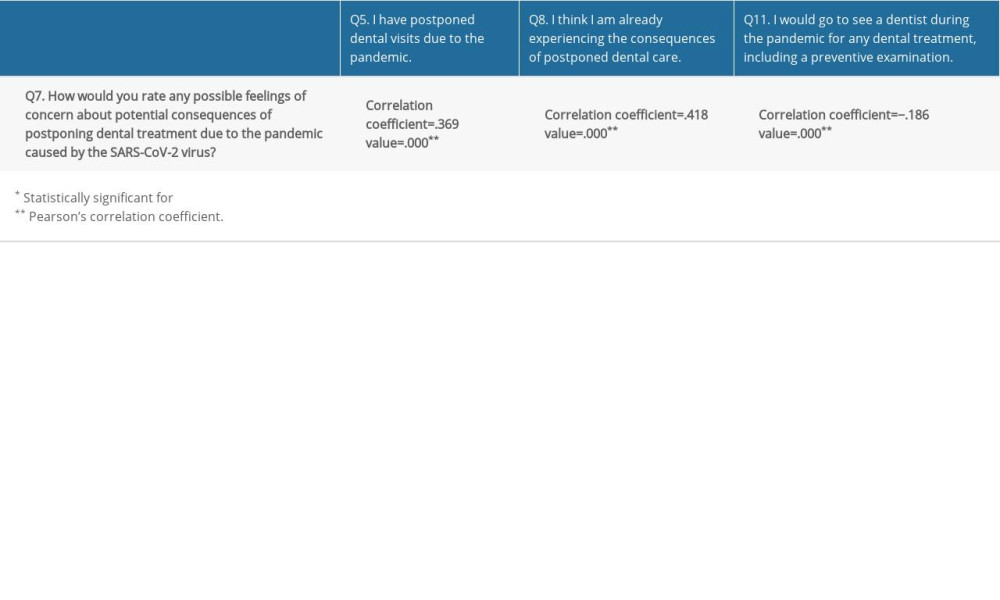 Table 6. Correlation analysis – correlation coefficients for the responses to question Q8 and questions Q5 and Q11.
Table 6. Correlation analysis – correlation coefficients for the responses to question Q8 and questions Q5 and Q11.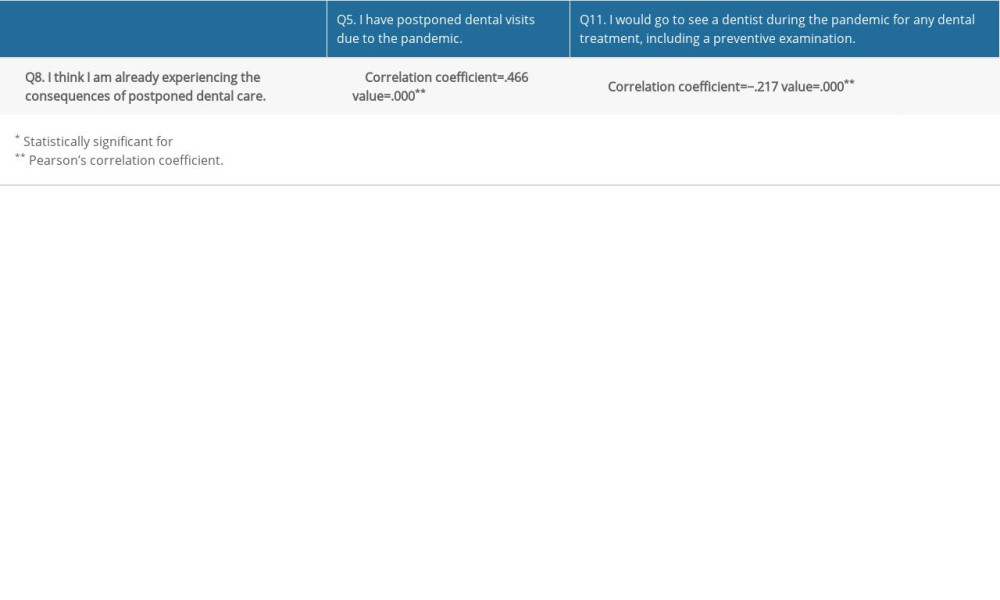 Table 7. Correlation analysis – correlation coefficients for the responses to questions Q6, Q9 and Q10 and questions Q5, Q7 and Q8.
Table 7. Correlation analysis – correlation coefficients for the responses to questions Q6, Q9 and Q10 and questions Q5, Q7 and Q8.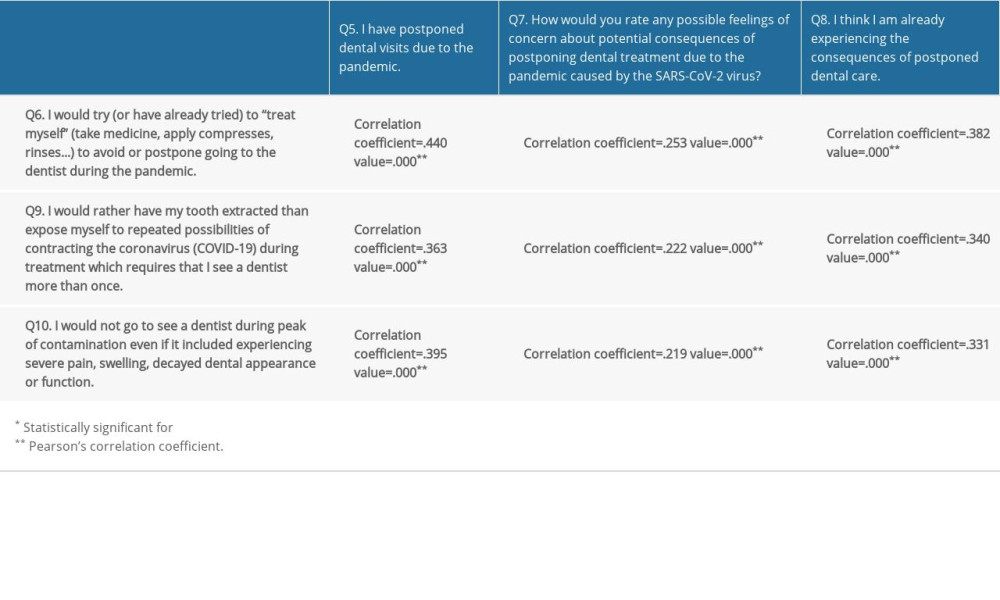 Table 8. Correlation analysis – correlation coefficients for the responses to questions Q12, Q13, and Q14 and questions Q5, Q7, and Q8.
Table 8. Correlation analysis – correlation coefficients for the responses to questions Q12, Q13, and Q14 and questions Q5, Q7, and Q8.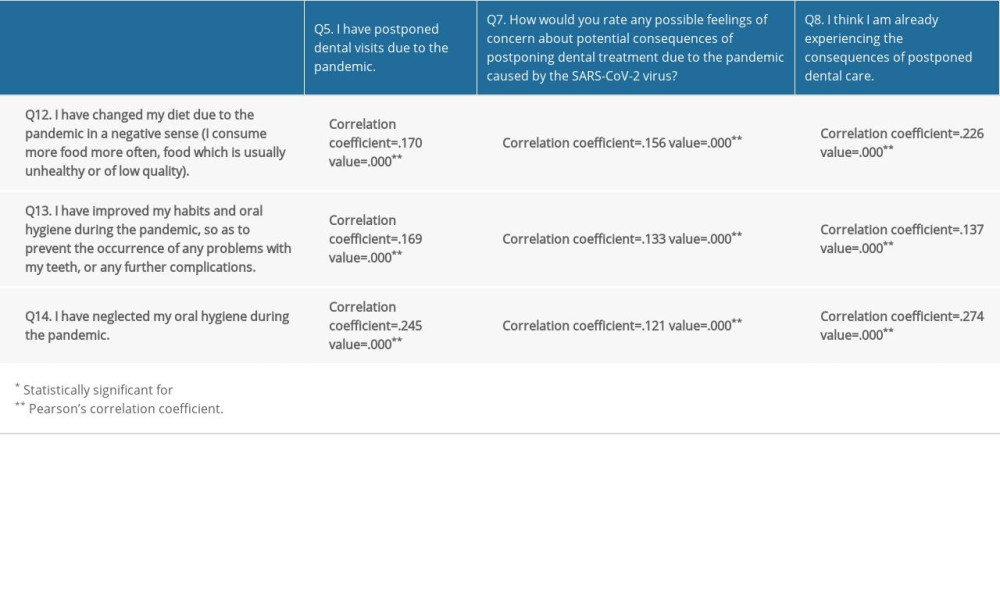
References
1. Facco E, Zanette G, The odyssey of dental anxiety: From prehistory to the present. A narrative review: Front Psychol, 2017; 8; 1155
2. Michael Tompkins: Anxiety avoidance disorders anxiety, 2013; 11-22, Oakland, New Harbinger Publications
3. Appukuttan DP, Strategies to manage patients with dental anxiety and dental phobia: literature review: Clin Cosmet Investig Dent, 2016; 8; 35-50
4. Beaton L, Freeman R, Humphris G, Why are people afraid of the dentist? Observations and explanations: Med Princ Pract, 2014; 23(4); 295-301
5. Armfield JM, Stewart JF, Spencer AJ, The vicious cycle of dental fear: Exploring the interplay between oral health, service utilization and dental fear: BMC Oral Health, 2007; 7; 1
6. Ornell F, Schuch JB, Sordi AO, Kessler FHP, “Pandemic fear” and COVID-19: mental health burden and strategies: Braz J Psychiatry”, 2020; 42(3); 232-35
7. Lin CY, Broström A, Griffiths MD, Pakpour AH, Investigating mediated effects of fear of COVID-19 and COVID-19 misunderstanding in the association between problematic social media use, psychological distress, and insomnia: Internet Interv, 2020; 21; 100345
8. Bäuerle A, Teufel M, Musche V, Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany: J Public Health (Oxf), 2020; 42(4); 672-78
9. Burnatowska E, Surma S, Olszanecka-Glinianowicz M, Relationship between mental health and emotional eating during the COVID-19 pandemic: A systematic review: Nutrients, 2022; 14(19); 3989
10. Gebreegziabher EG, Mekonnen NG, Amogne MT, Clinical characteristics and outcomes of patients with COVID-19 infection and acute ischemic stroke at Eka Kotebe General Hospital in Addis Ababa. Ethiopia: Ethiop J Health Sci, 2022; 32(2); 229-34
11. Akhtar N, Abid F, Singh R, Ischemic stroke in patients that recover from COVID-19: Comparisons to historical stroke prior to COVID-19 or stroke in patients with active COVID-19 infection: PLoS One, 2022; 17(6); e0270413
12. Omarini C, Maur M, Luppi G, Cancer treatment during the coronavirus disease 2019 pandemic: Do not postpone, do it!: Eur J Cancer, 2020; 133; 29-32
13. Kanathila H, Pangi A, Bharathi B, COVID-19 – threat to dentistry – how to overcome?: J Evol Med Dent Sci, 2020; 9(37); 2746-51
14. Volgenant CMC, Persoon IF, de Ruijter RAG, de Soet JJ, Infection control in dental health care during and after the SARS-CoV-2 outbreak: Oral Dis, 2021; 27(3); 674-83
15. Gambarini E, Galli M, Di Nardo D, A survey on perceived COVID-19 risk in dentistry and the possible use of rapid tests: J Contemp Dent Pract, 2020; 21(7); 718-22
16. Walter E, von Bronk L, Hickel R, Huth KC, Impact of COVID-19 on dental care during a national lockdown: A retrospective observational study: Int J Environ Res Public Health, 2021; 18(15); 7963
17. COVIDental Collaboration Group, The COVID-19 pandemic and its global effects on dental practice. An International survey: J Dent, 2021; 114; 103749
18. Nijakowski K, Cieślik K, Łaganowski K, The impact of the COVID-19 pandemic on the spectrum of performed dental procedures: Int J Environ Res Public Health, 2021; 18(7); 3421
19. Barabari P, Moharamzadeh K, Novel coronavirus (COVID-19) and dentistry – a comprehensive review of literature: Dent J (Basel), 2020; 8(2); 53
20. Amato A, Iandolo A, Scelza G, COVID-19: The patients’ perceived impact on dental care: Eur J Dent, 2022; 16(2); 333-38
21. Expósito-Delgado AJ, Ausina-Márquez V, Mateos-Moreno MV, Delivery of health care by Spanish dental hygienists in private and public dental services during the COVID-19 de-escalation phase (June 2020): A cross-sectional study: Int J Environ Res Public Health, 2021; 18(16); 8298
22. Ahmadi H, Ebrahimi A, Ghorbani F, The impact of COVID-19 pandemic on dental practice in Iran: A questionnaire-based report: BMC Oral Health, 2020; 20(1); 354
23. Jum’ah AA, Elsalem L, Loch C, Perception of health and educational risks amongst dental students and educators in the era of COVID-19: Eur J Dent Educ, 2021; 25(3); 506-15
24. Tofangchiha M, Lin CY, Scheerman JFM, Associations between fear of COVID-19, dental anxiety, and psychological distress among Iranian adolescents: BDJ Open, 2022; 8(1); 19
25. Knipe D, Evans H, Marchant A, Mapping population mental health concerns related to COVID-19 and the consequences of physical distancing: A Google trends analysis: Wellcome Open Res, 2020; 5; 82
26. Campagnaro R, Collet GO, Andrade MP, COVID-19 pandemic and pediatric dentistry: Fear, eating habits and parent’s oral health perceptions: Child Youth Serv Rev, 2020; 118; 105469
27. Cotrin P, Peloso RM, Oliveira RC, Impact of coronavirus pandemic in appointments and anxiety/concerns of patients regarding orthodontic treatment: Orthod Craniofac Res, 2020; 23(4); 455-61
28. Migas K, Marczak M, Kozłowski R, Impact of the COVID-19 pandemic on the dental preferences of patients in the private sector: Int J Environ Res Public Health, 2022; 19(4); 2183
29. Goriuc A, Sandu D, Tatarciuc M, Luchian I, The impact of the COVID-19 pandemic on dentistry and dental education: A narrative review: Int J Environ Res Public Health, 2022; 19(5); 2537
30. : Republički zavod za statistiku Srbije [Internet] Available from: [in Bosnian]https://www.stat.gov.rs/sr-Latn/oblasti/stanovnistvo
31. Nardi MP, Developing a questionnaire: Doing Surv Res, 2020; 2(2); 80-121
32. Gurzawska-Comis K, Becker K, Brunello G, Recommendations for dental care during COVID-19 pandemic: J Clin Med, 2020; 9(6); 1833
33. Jamal M, Shah M, Almarzooqi SH, Overview of transnational recommendations for COVID-19 transmission control in dental care settings: Oral Dis, 2021; 27(3); 655-64
34. Deana NF, Seiffert A, Aravena-Rivas Y, Recommendations for safe dental care: A systematic review of clinical practice guidelines in the first year of the COVID-19 pandemic: Int J Environ Res Public Health, 2021; 18(19); 10059
35. Cagetti MG, Cairoli JL, Senna A, Campus G, COVID-19 outbreak in North Italy: An overview on dentistry. A questionnaire survey: Int J Environ Res Public Health, 2020; 17(11); 3835
36. Ciardo A, Simon MM, Sonnenschein SK, Impact of the COVID-19 pandemic on oral health and psychosocial factors: Sci Rep, 2022; 12(1); 1-12
37. Vojvodic K, Terzic-Supic Z, Todorovic J, Financial burden of medical care, dental care, and medicines among older-aged population in Slovenia, Serbia, and Croatia: Int J Environ Res Public Health, 2022; 19(6); 3325
38. Kolak V, Pavlovic M, Aleksic E, Probable bruxism and psychological issues among dental students in Serbia during the COVID-19 pandemic: Int J Environ Res Public Health, 2022; 19(13); 7729
39. Milošević Marković M, Latas MB, Milovanović S, Mental health and quality of life among dental students during COVID-19 pandemic: A cross-sectional study: Int J Environ Res Public Health, 2022; 19(21); 14061
40. González-Olmo MJ, Delgado-Ramos B, Ortega-Martínez AR, Fear of COVID-19 in Madrid: Will patients avoid dental care? Int Dent J, 2022; 72(1); 76-82
41. Oshima K, Miura H, Tano R, Fukuda H, Factors associated with regular dental checkups’ discontinuation during the COVID-19 pandemic: A Nationwide Cross-Sectional Web-Based Survey in Japan: Int J Environ Res Public Health, 2022; 19(5); 2917
Tables
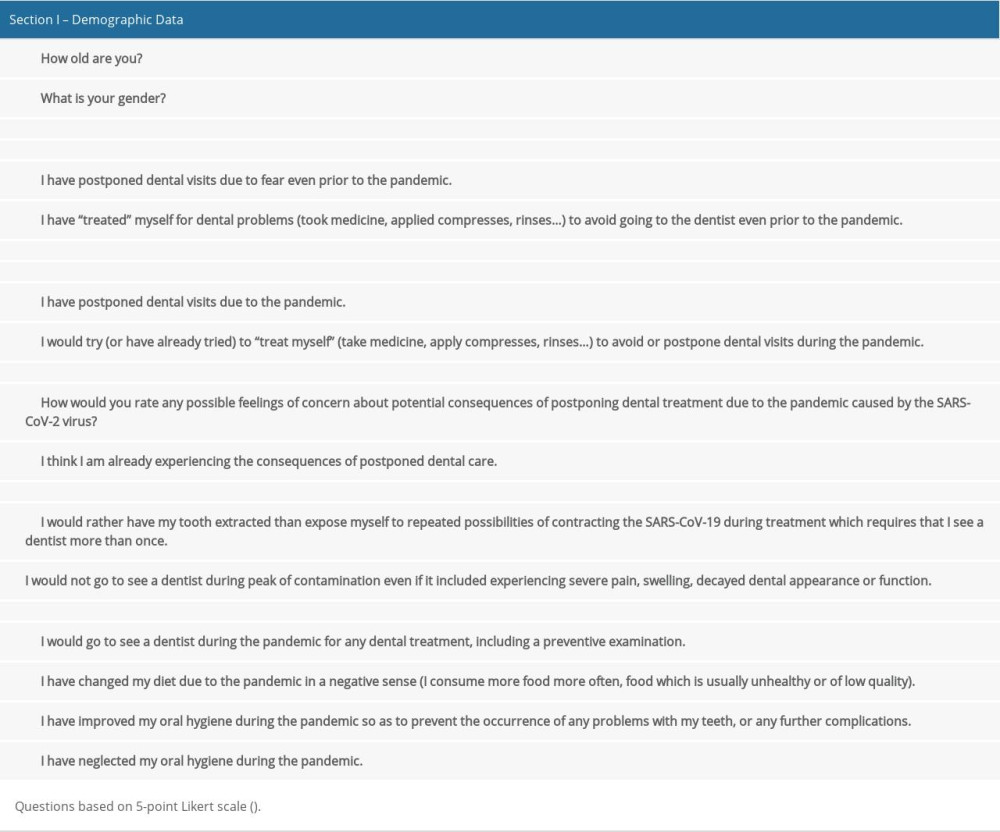 Table 1. The questions included in the questionnaire.
Table 1. The questions included in the questionnaire.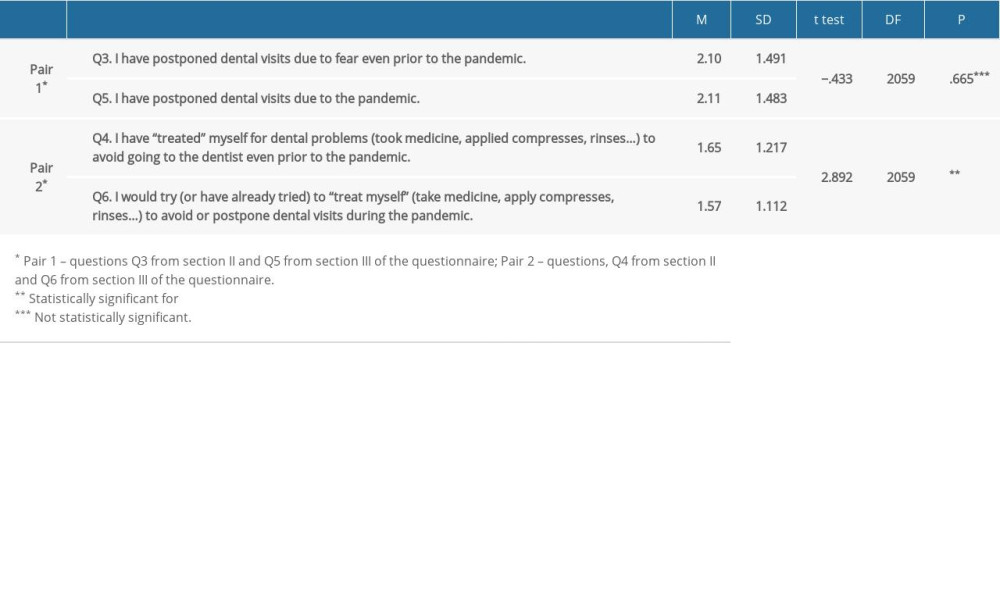 Table 2. The significance of the differences between observed habits related to professional dental care (questions Q3, Q4, Q5, Q6) paired before and during the pandemic (paired t test).
Table 2. The significance of the differences between observed habits related to professional dental care (questions Q3, Q4, Q5, Q6) paired before and during the pandemic (paired t test).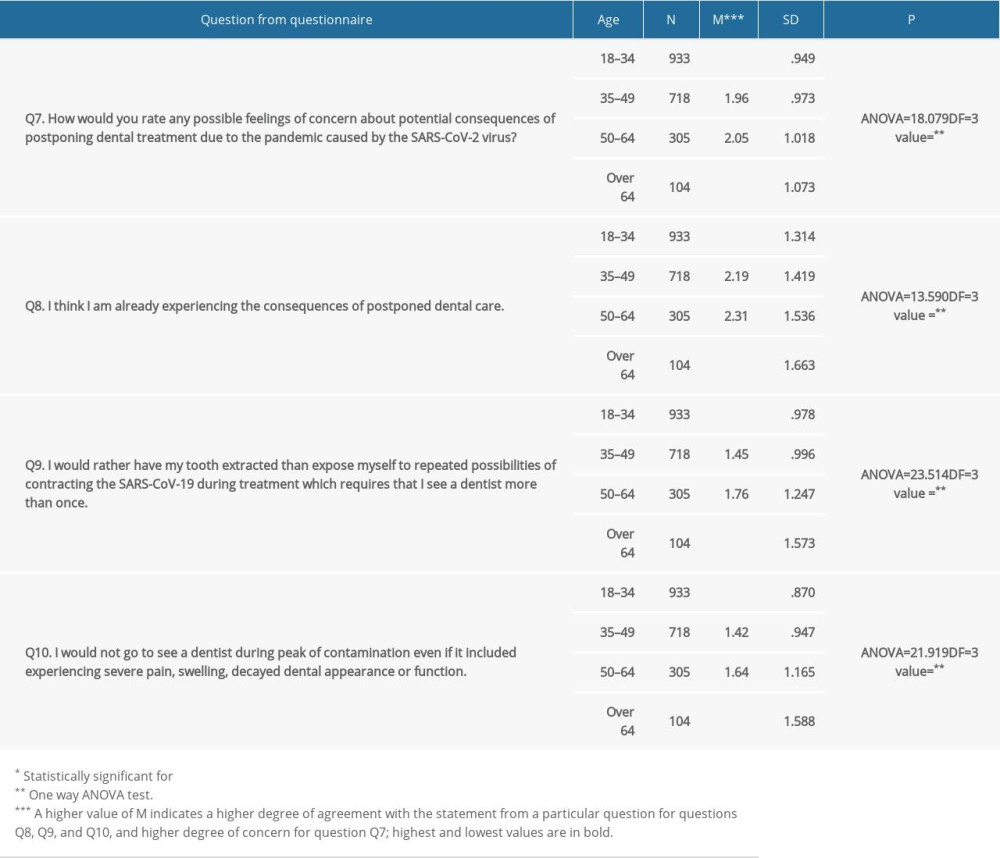 Table 3. The differences in the consequences of postponed dental treatments (questions Q7 and Q8) and extreme avoidance regarding the respondents’ age (questions Q9 and Q10) from section III of the questionnaire).
Table 3. The differences in the consequences of postponed dental treatments (questions Q7 and Q8) and extreme avoidance regarding the respondents’ age (questions Q9 and Q10) from section III of the questionnaire).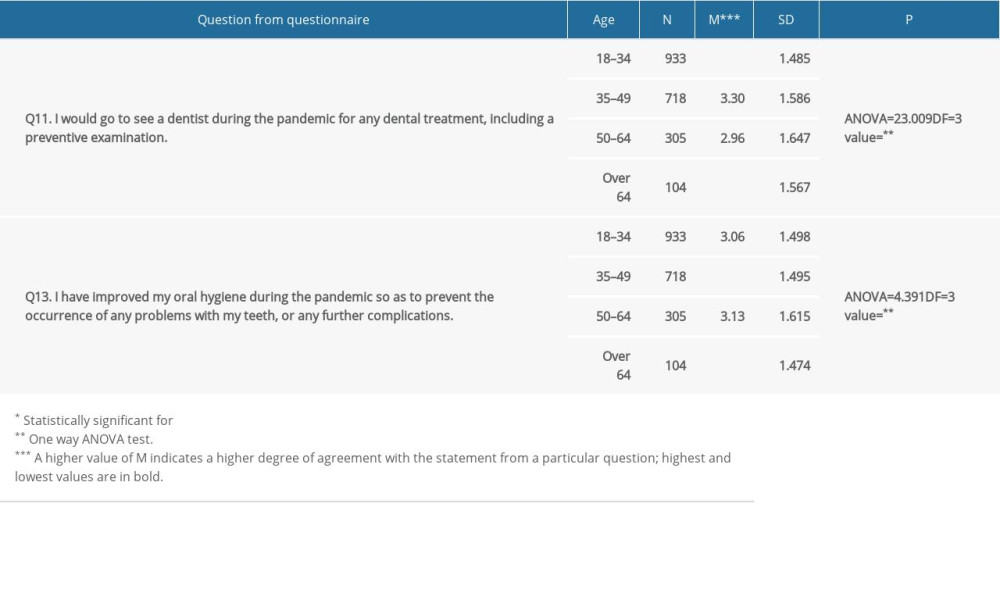 Table 4. The differences in the observed preventive measures during the pandemic regarding the respondents’ age (questions Q11 and Q13).
Table 4. The differences in the observed preventive measures during the pandemic regarding the respondents’ age (questions Q11 and Q13).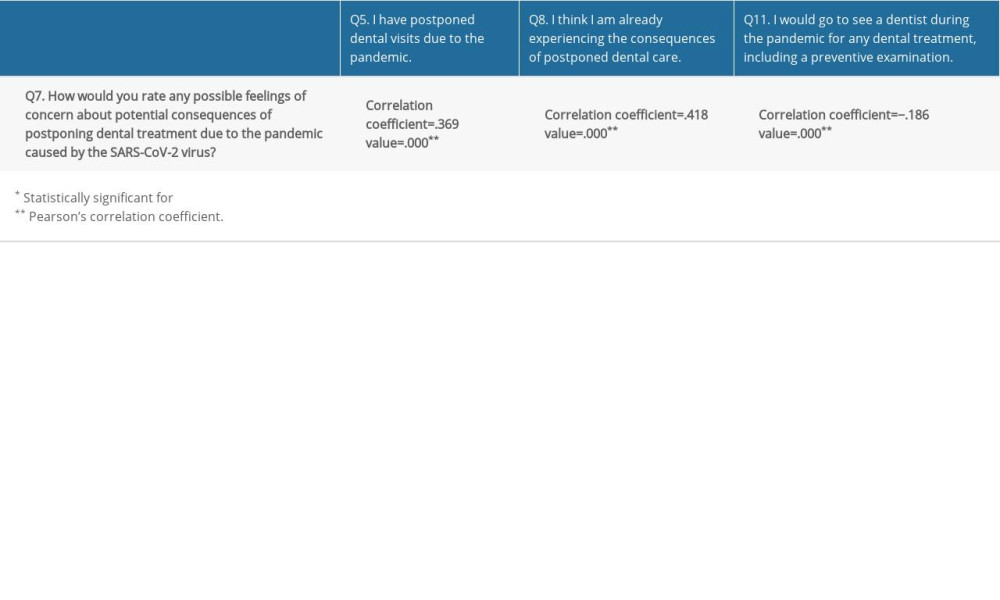 Table 5. Correlation analysis – correlation coefficients for the responses to question Q7 and questions Q5, Q8, and Q11.
Table 5. Correlation analysis – correlation coefficients for the responses to question Q7 and questions Q5, Q8, and Q11.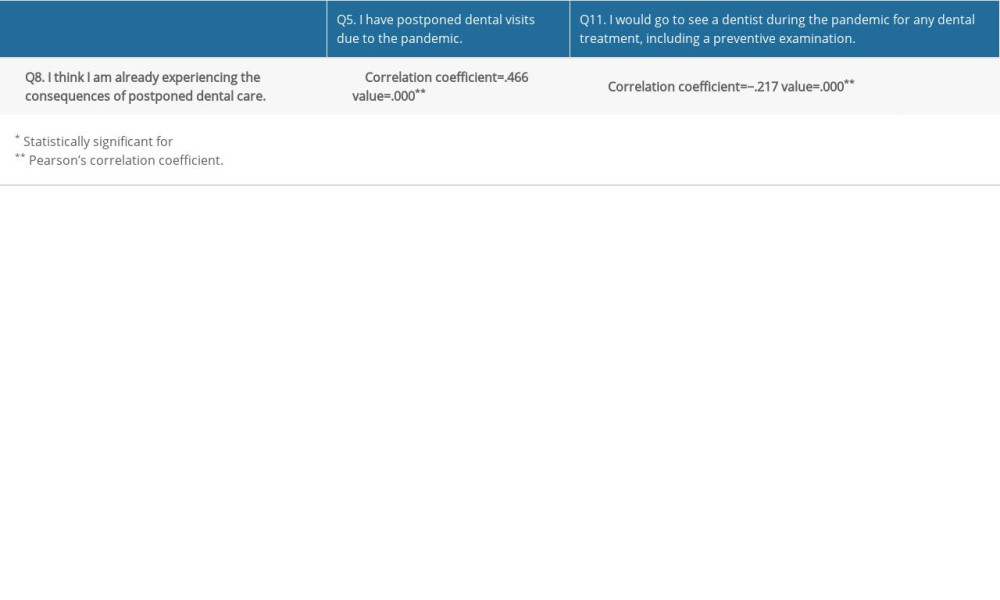 Table 6. Correlation analysis – correlation coefficients for the responses to question Q8 and questions Q5 and Q11.
Table 6. Correlation analysis – correlation coefficients for the responses to question Q8 and questions Q5 and Q11.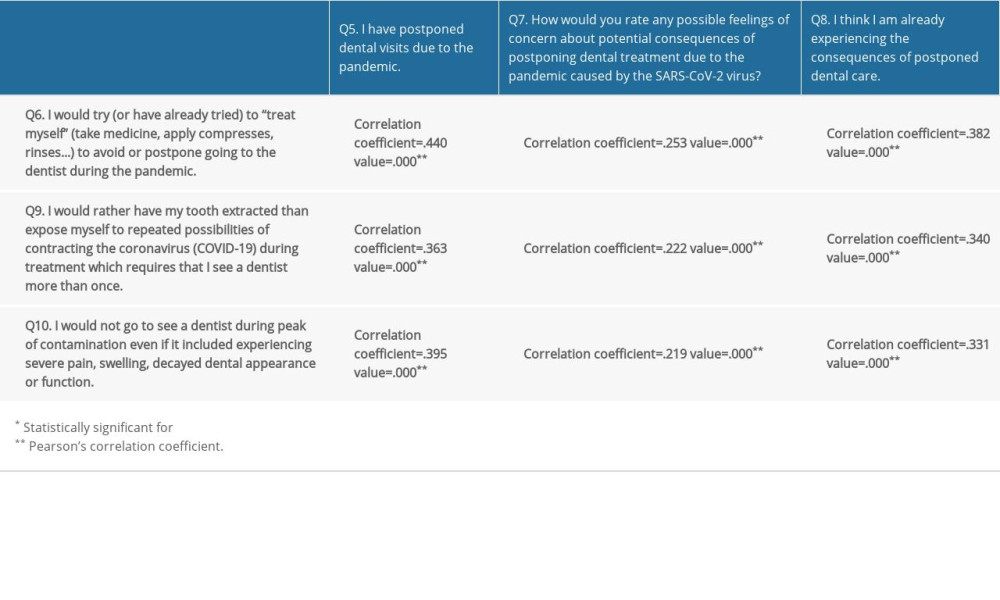 Table 7. Correlation analysis – correlation coefficients for the responses to questions Q6, Q9 and Q10 and questions Q5, Q7 and Q8.
Table 7. Correlation analysis – correlation coefficients for the responses to questions Q6, Q9 and Q10 and questions Q5, Q7 and Q8.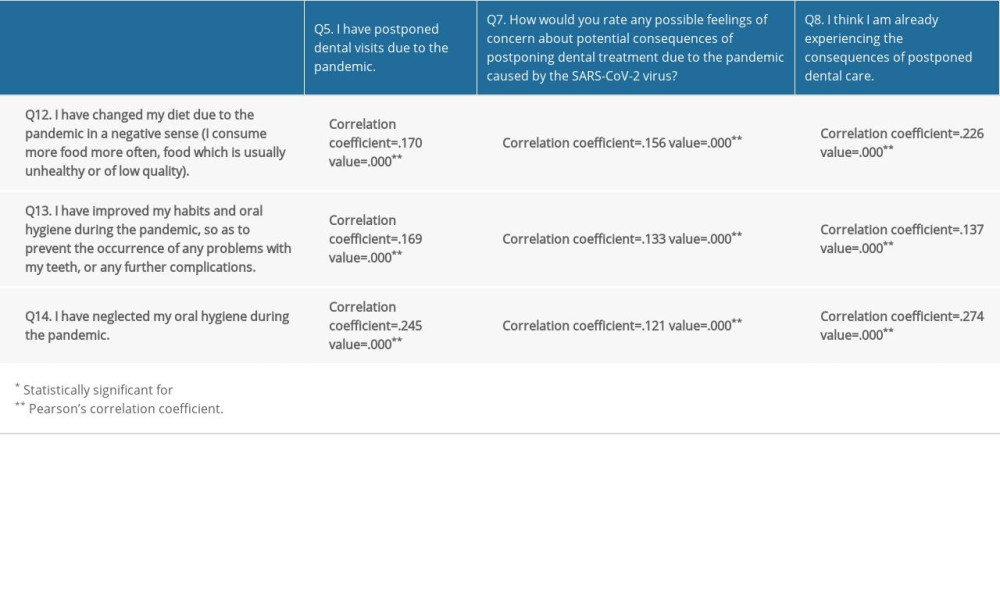 Table 8. Correlation analysis – correlation coefficients for the responses to questions Q12, Q13, and Q14 and questions Q5, Q7, and Q8.
Table 8. Correlation analysis – correlation coefficients for the responses to questions Q12, Q13, and Q14 and questions Q5, Q7, and Q8. In Press
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








