22 July 2023: Clinical Research
Use of a Flexible Ruler in Measuring the Length of Artificial Stapes During Stapedotomy Under Otoendoscopy
Nan Zeng12ABCDEF, Shang Yan1ABCDEF, Qiong Yang2ABCDEF, Chaobing Gao1ABCDEFG*DOI: 10.12659/MSM.940337
Med Sci Monit 2023; 29:e940337
Abstract
BACKGROUND: We explored a new method for measuring the length of artificial stapes during stapedotomy in otoendoscopic middle-ear surgery using a flexible ruler.
MATERIAL AND METHODS: A retrospective analysis was conducted on 56 cases of otosclerosis, comprising 56 ears with a follow-up of over 6 months and complete data. Patients were admitted to the Department of Otology, Huazhong University of Science and Technology Union Shenzhen Hospital from July 2020 to June 2022. SPSS statistical software was used for efficacy analysis. The results of different measurement methods on the implantation time of the prosthesis and postoperative hearing follow-up were compared.
RESULTS: The 56 patients were randomly divided into 2 groups. In 1 case measured by the metal measuring stick, the prosthesis was too short and was replaced during the operation; 2 patients experienced transient dizziness postoperatively, and the other patients had no surgical complications. All 56 patients had varying degrees of hearing improvement after surgery, and no dislocation of the ossicular chain was observed during the follow-up. There was a statistically significant difference in the implantation time of the prosthesis between the different measurement methods (P<0.05). The improvement in hearing in the flexible ruler group was statistically significant (P<0.05).
CONCLUSIONS: The selection of the length of the ossicular prosthesis is a crucial step in the operation and can directly affect hearing outcomes. The use of a flexible ruler to measure prosthesis length can significantly shorten operation time and improve hearing, and the ruler is easily obtainable. It is worth promoting its application in ear endoscopic stapedotomy.
Keywords: Stapes Surgery, Otoscopes, endoscopy, Disposable Equipment, Humans, Stapes, Ossicular Prosthesis, Retrospective Studies, Prosthesis Implantation, Artificial Limbs
Background
Conductive hearing loss results from ossicular chain disruption, which can be secondary to a number of etiologies [1]. In the field of otology, reconstruction of the middle ear ossicular chain is referred to as ossiculoplasty, which is a common otologic procedure used worldwide [2].
Otosclerosis is a progressive disease characterized by abnormal bony remodeling, which includes the formation of new bone and bone resorption in the temporal bone [3,4]. Surgical treatment has evolved through the years. Stapedotomy is considered the most effective and up-to-date surgical technique for the management of otosclerosis [5,6].
Reconstructive surgery of the ossicular chain is an essential method of restoring hearing levels in patients with conductive hearing loss [7]. Various types of artificial ossicular materials are available that ensure good biocompatibility and tissue affinity, and they are widely used in ossicular implantation surgery to effectively improve patients’ hearing levels [8].
The incus-footplate distance in Chinese individuals, like in other populations, can vary depending on individual anatomy and pathological conditions. In general, the normal range of the incus-footplate distance is between 2.5 and 6.0 mm, and studies have reported an average distance of approximately 3.8 to 4.0 mm [9–12]. Therefore, selecting the length of the artificial ossicular prosthesis is a crucial step in the surgery and can directly affect the success rate of the surgery, which is particularly challenging for novice and young doctors. Improper selection of the prosthesis length can be a common cause of unsatisfactory postoperative hearing improvement, especially in the case of artificial stapes implantation. Accurate measurement of the incus-footplate distance is usually done using high-resolution computed tomography (CT) or other imaging techniques [12]. Today, endoscopic surgery provides a broad view to observe the incus and stapes, while limiting the use of one-handed surgical techniques by the surgeon, and the endoscope cannot provide binocular 3-dimensional (3D) and depth perception [13]. Therefore, the measurement tools that we traditionally use in the 3D field of view of the microscope are not accurate in the 2D field of the otoendoscopy. Also, classic measuring tools cannot be bent, and repeated disinfection is costly.
The aim of the present study is to explore the role of a ruler in measuring the length of an artificial ossicular prosthesis during endoscopic stapes surgery.
Material and Methods
GENERAL DATA:
A retrospective analysis was conducted on 56 cases (56 ears) of otosclerosis patients with follow-up of more than 6 months and complete data who were treated in the Department of Otology, Huazhong University of Science and Technology Union Shenzhen Hospital from July 2020 to June 2022. All patients were treated for the first time. Of the 56 patients, 29 were male and 27 were female, with an age range of 7 to 67 years (mean age 34.26±11.20 years); the follow-up time ranged from 7 to 14 months (mean 13.7±2.3 months). All 56 patients underwent surgery performed by the same experienced otolaryngologist, using an ear endoscope, and the length of the prosthesis was measured randomly using a measuring stick or a flexible ruler. Among them, a metal measuring stick was used in 30 cases, and a flexible ruler was used in 26 cases. The group assignment was based on the material used at the time of surgery, since we did not have measurements in every surgical kit. The clinical data, including the implantation time and postoperative hearing level, were retrospectively analyzed.
SURGICAL MATERIALS:
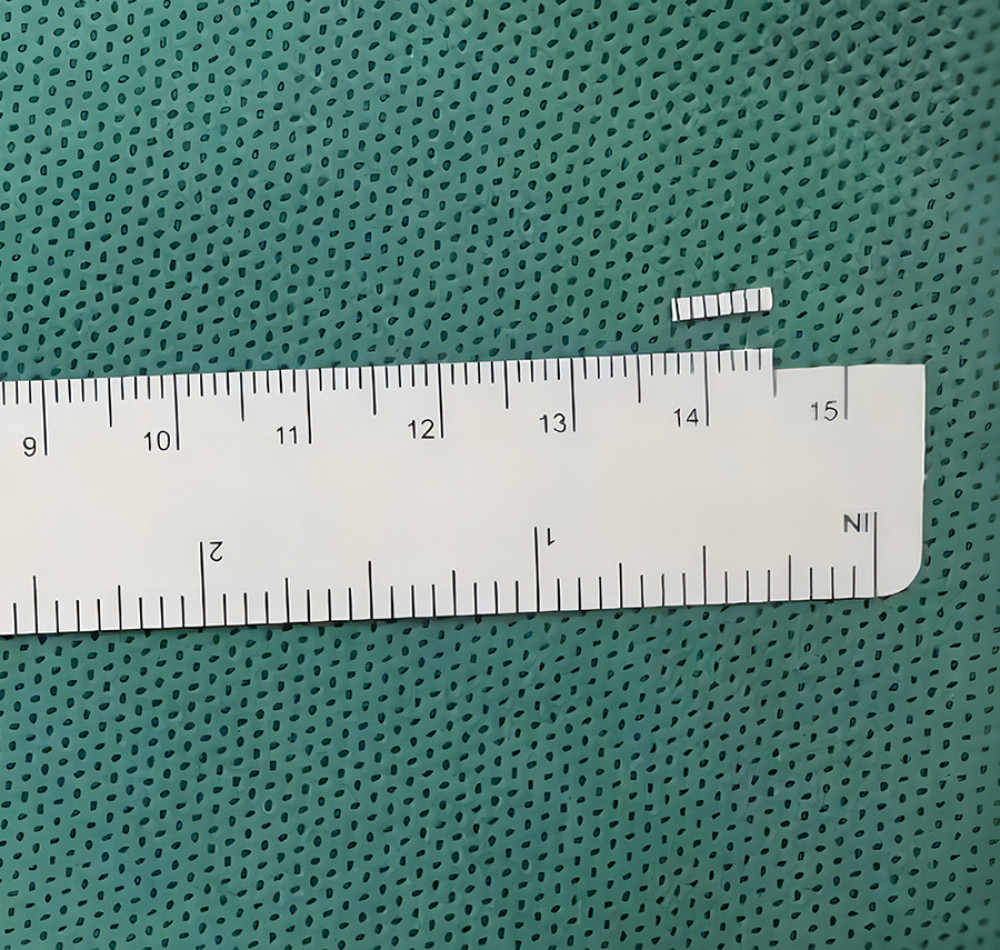
All surgeries were performed using the STORZ ultra-high-definition endoscopy system and recorded. The Piston artificial stapes used during the surgery was a German Spiggle titanium-derived hearing bone, and the CO2 laser used was a German DEKA handheld laser. The measuring stick used was a STORZ otoscope instrument, and the ruler was a disposable medical skin marking pen and ruler used for surgery. The ruler was cut into thin strips approximately 0.5 to 1.0 mm wide and 5 to 6 mm long using ophthalmic scissors, with scales retained.
SURGICAL PROCEDURE:
All surgeries were performed by an experienced ear surgeon using an ear endoscope. The procedure was done under general anesthesia, with controlled hypotension (90/60 mm Hg) maintained during the operation. Under the endoscope, a curved incision was made at the 6 to 12-o’clock position along the posterior wall of the external auditory canal, 5 to 8 mm away from the tympanic sulcus. The external auditory canal skin flap and fibrous annulus were carefully separated to gain access to the middle ear cavity, while ensuring that the tympanic membrane was protected. The external auditory canal skin tympanic flap was lifted and attached to the anterior wall of the external auditory canal.
The surgeon identified the incudostapedial joint, pyramid, stapedius tendon, stapes, vestibule window, and facial nerve in the middle ear cavity under the endoscope. After confirming the fixation of the stapes footplate, the distance among the stapes footplate and the lateral edge of the incus was randomly measured using a measuring stick and ruler. A 600-μm handheld CO2 laser was used to create a hole in the center of the stapes footplate, following which, the Piston artificial stapes was implanted, with one end inserted into the opening and the other end hooked and clamped in the middle and lower third of the incus. The stapedius tendon was cut, and the incudostapedial joint and anterior and posterior feet of the stapes arch was separated to remove the stapes superstructure. After confirming the stability of the artificial stapes and the linkage of the ossicular chain, the external auditory canal skin tympanic flap was restored, and the external auditory canal was filled with appropriate materials to complete the surgery.
DATA COLLECTION AND FOLLOW-UP METHODS:
All patients underwent preoperative evaluations, including pure tone audiometry, impedance audiometry, temporal bone CT, and otoscopy examination. The surgical procedure was recorded on video, and the implantation time of the ossicular prosthesis was calculated (from the first time the prosthesis was moved into the surgical field to the resetting of the tympanic membrane-ear canal flap, including the time for adjusting the prosthesis, but not the measurement time). After surgery, patients were monitored for complications, such as dizziness, nystagmus, and tinnitus, and underwent follow-up evaluations with pure tone audiometry and otoscopy examination. The preoperative and postoperative air-bone gap (ABG) at speech frequencies of 0.5 kHz, 1 kHz, 2 kHz, and 4 kHz, and surgical time was calculated. Statistical analysis was performed using one-way ANOVA in SPSS software.
Results
GENERAL RESULTS:
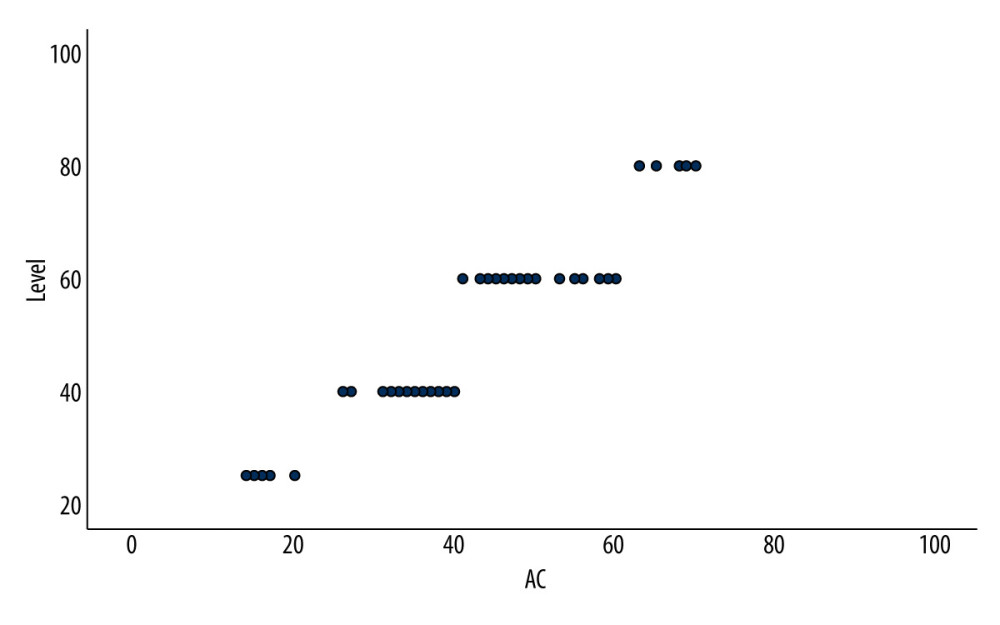
All patients had varying degrees of conductive hearing loss (Figure 1). All surgeries were successful, except for 1 case of intraoperative replacement of metal measuring stick due to it being too short, and 2 cases of dizziness postoperatively in patients undergoing implantation with the metal measuring stick, possibly due to the prosthesis being too long. However, the dizziness disappeared within 3 days after drug treatment. The average incus-footplate distance measured during the procedure was 4.07±0.37 mm, which is consistent with the previous literature. No patients had facial paralysis or new tinnitus after surgery. At the first visit 3 weeks after the surgery, otoendoscopy showed that the tympanic membrane healed well. No ossicular prolapse was found during follow-up. The hearing level was improved in all 56 ears after surgery, to varying degrees.
COMPARISON OF INTRAOPERATIVE IMPLANTATION TIME OF OSSICULAR PROSTHESES:
Patients were divided into 2 groups based on the measurement method used during surgery: in group A, the metal measuring stick was used, and in group B, the flexible ruler was used. The mean implantation time of group A was 300.30±35.13 s, and that of group B was 233.91±20.45 s. Single-factor analysis of variance was performed, with F=154.80 and
POSTOPERATIVE HEARING IMPROVEMENT:
In group A, the preoperative ABG was 34.17±9.66 dB HL, and the postoperative ABG was 12±5.35 dB HL. In group B, the preoperative ABG was 37.50±15.31 dB HL, and the postoperative ABG was 8.08±3.19 dB HL. The preoperative and postoperative hearing results of the 2 groups of patients are shown in Table 1. The postoperative ABG in the 2 groups was analyzed using one-way ANOVA, and the F value was 11.365, with P<0.05. There was no significant difference in the postoperative success rate (ABG within 20 dB) between the 2 groups, with P>0.05. Comparison of functional hearing (air conduction <30 dB) gain between the 2 groups showed that group B was higher than group A, and the difference was statistically significant (P<0.05), indicating that the use of the flexible ruler resulted in a significant improvement in postoperative hearing compared with that of using the metal measurement stick (Table 2).
Discussion
Compared with traditional middle ear surgery via a microscopic approach, endoscopic ear surgery has numerous advantages. It improves surgical visibility and accessibility while reducing postoperative pain and increasing the protection of the chorda tympani and stapes footplate [14]. The wide-angle and angled scopes also provide the ability to visualize hidden anatomical structures and distinguish subtle lesions, thereby improving the ability to confirm the coupling of the prosthesis. However, a disadvantage of endoscopic surgery is that it requires 1 hand to hold the endoscope, which limits the surgeon to 1-handed operations. Furthermore, endoscopes cannot provide binocular depth perception, which makes it challenging to accurately measure the length of the stapes prosthesis.
Selecting the correct length of the stapes prosthesis is crucial in achieving successful surgery and improving hearing. Improper selection of stapes prosthesis length is a common cause of unsatisfactory postoperative hearing improvement [15]. If the prosthesis is too short, it cannot provide effective vibration and can easily fall out. If it is too long, it can contribute to dizziness and sensorineural hearing loss [16–18]. Common reasons for reoperation after stapes prosthesis implantation include prosthesis dysfunction, dislocation or displacement, inaccurate prosthesis length, erosion of the incus, fibrous adhesions, or refixation of the stapes footplate [19–22].
Nevertheless, studies on the measurement of the prosthesis length are limited, and the commonly used Piston length is 3.5 to 5.0 mm [23]. Measuring the prosthesis length is frequently judged by experienced ear surgeons based on their experience or is measured by a measuring stick. In patients with ossicular malformations or otosclerosis, the length is often measured by preoperative imaging or direct measurement with a measuring stick during the course of surgery. Nevertheless, different imaging techniques have different evaluation errors for different metal materials. As an example, multi-planar reconstruction CT overestimated the length of a titanium alloy stapes prosthesis by 0.1 mm [24], while cone beam CT overestimated it by 0.2 mm [25]. Multi-slice spiral CT had a greater overestimation value of 0.68 mm for the prosthesis length [26]. Improper selection of prosthesis length is a common cause of surgical failure, with a high incidence of the prosthesis being too short or too long [16].
In this study, all cases were judged with the assistance of imaging examination. Among the 26 cases of stapes implantation measured by a flexible ruler, there were no replacements of prostheses or postoperative complications. In the 30 cases of stapes implantation measured by a measuring stick, 1 patient needed replacement of the prosthesis in the course of the operation due to its short length, and 2 patients had brief dizziness after surgery because the prosthesis was too long. The metal measuring stick is relatively rigid and not easy to bend in the complex anatomy of the middle ear cavity, which can give rise to errors during the measurement process. Moreover, the surgeon must judge the coupling of the prosthesis multiple times, which increases the surgical time.
During ear microsurgery, an ossicular prosthesis is measured using a measuring stick, while the microscope provides binocular 3D images and depth perception. This allows the surgeon to pass the measuring stick through important structures, such as the chorda tympani nerve or residual ossicles, to reach the deepest part of the middle ear for accurate measurement and interpretation. However, an endoscope cannot provide 3D images or depth perception, making it more difficult for surgeons to pass the measuring stick through the chorda tympani nerve or residual ossicles using 1 hand. This can be especially challenging in cases of limited space in the middle ear, such as those with ossicular chain malformation or otosclerosis. Furthermore, straight measuring sticks cannot be perpendicular to the footplate of the stapes, leading to potential inaccuracies in measurements. Although curved measuring sticks can be perpendicular to the footplate, they are prone to deformation in the front section, resulting in further inaccuracies. In the present study, 2 patients who experienced brief dizziness after receiving the Piston artificial stapes implant were found to have been given slightly longer prostheses after measurement was made with the measuring stick. Additionally, the 2D image provided by the ear endoscope can affect the interpretation of the measuring stick’s scale, resulting in incorrect prosthesis length selection.
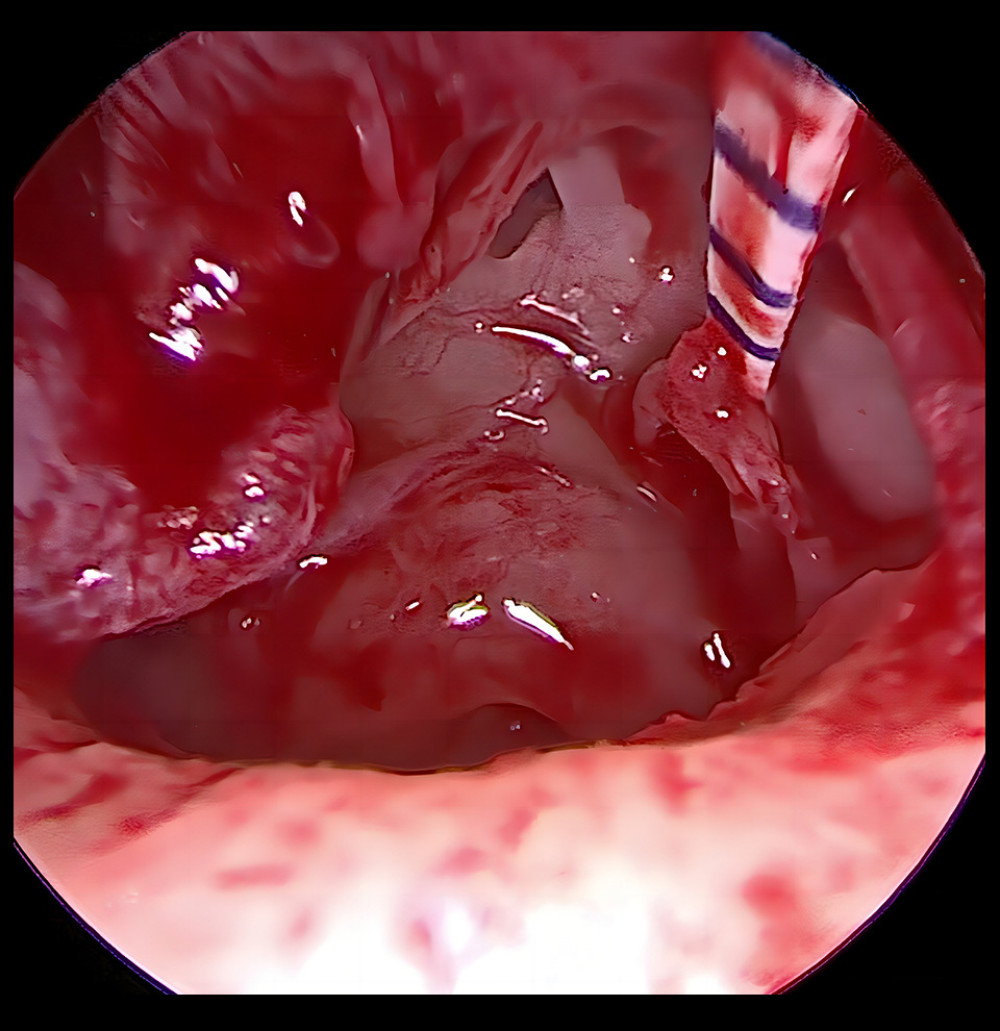
Because the rigid tool is not easy to bend and there is no obvious accurate scale, the incus-footplate distance cannot be assessed immediately and accurately in the 2D field of view provided by otoscopy, and therefore, it sometimes needs to be adjusted 2 or more times. Through long-term clinical exploration, we have found that for patients with otosclerosis, a disposable surgical ruler can be used for measurement during surgery. The ruler is trimmed to a thin strip, with a width of 0.5 to 1.0 mm and a length of 5 to 6 mm, with scale markings retained (Figure 2). The trimmed ruler is placed in the center of the footplate of the stapes with micro tissue forceps or suction, and placed along the long axis of the stapes until the level of the handle of the malleus or the long process of the incus, with the reading taken on the magnified image of the endoscope (Figure 3). The prosthesis implantation time measured with the ruler was 233.91±20.45 s, with no readjustment or postoperative complications. The ruler is cost-efficient, easy to obtain, and can be easily trimmed during surgery. It can be completely placed in the middle ear for measurement, without being affected by external auditory canal stenosis or protrusion. The ruler is also flexible and can be measured more vertically on the footplate of the stapes with the assistance of micro instruments, thus reducing operation time and minimizing postoperative complications.
We did a systematic analysis of the data, but our study still had limitations. For example, the number of patients with otosclerosis was significantly lower than that of patients with chronic suppurative otitis media, resulting in a relatively small sample size. We did not have a very long follow-up, and the effect on the probability of prosthesis prolapse in the long term was not analyzed. We will continue to accumulate and learn to improve our research.
Conclusions
The selection of prosthesis length is critical for the success of hearing reconstruction in patients with otosclerosis. The use of a measuring stick or a disposable surgical ruler by experienced otologists can directly measure prosthesis length. Prosthesis implantation measured using a surgical ruler can significantly reduce implantation time and improve hearing outcomes. The use of a surgical ruler in single-handed ear endoscopic surgery is a simple and easy-to-learn method for beginners, those without measuring tools, and special cases in which the measuring stick cannot be placed vertically owing to limited space. It can improve the accuracy of prosthesis length measurement and reduce surgical complications. The use of a surgical ruler is convenient, cost-efficient, and worth promoting in ear endoscopic stapes surgery.
References
1. Deklerck AN, Acke FR, Janssens S, Etiological approach in patients with unidentified hearing loss: Int J Pediatr Otorhinolaryngol, 2015; 79(2); 216-22
2. Faramarzi M, Roosta S, Faramarzi A, Kherad M, Comparison of partial vs. total ossicular chain reconstruction using titanium prosthesis: A retrospective cohort study: Eur Arch Otorhinolaryngol, 2023 [Online ahead of print]
3. Quesnel AM, Ishai R, McKenna MJ, Otosclerosis: Temporal bone pathology: Otolaryngol Clin North Am, 2018; 51(2); 291-303
4. Wolfovitz A, Luntz M, Impact of imaging in management of otosclerosis: Otolaryngol Clinic North Am, 2018; 51(2); 343-55
5. Poutoglidis A, Tsetsos N, Vardaxi C, Conventional microscopic stapedotomy: An obsolete technique or still the gold standard for the management of otosclerosis?: Cureus, 2021; 13(3); e14126
6. De Vito A, Mandalà M, Soprani F, Conventional approaches versus laser CO2 surgery in stapes surgery: A multicentre retrospective study: Eur Arch Otorhinolaryngol, 2022; 279(5); 2321-27
7. Gu FM, Chi FL, Titanium ossicular chain reconstruction in single stage canal wall down tympanoplasty for chronic otitis media with mucosa defect: Am J Otolaryngol, 2019; 40(2); 205-8
8. Kálmán J, Horváth T, Liktor B, Limitations of non-echo planar diffusion weighted magnetic resonance imaging (non-EPI MRI) in cholesteatoma surveillance after ossicular chain reconstruction. A prospective study: Auris Nasus Larynx, 2021; 48(4); 630-35
9. Marchica CL, Saliba I, The relationship between stapes prosthesis length and rate of stapedectomy success: Clin Med Insights Ear Nose Throat, 2015; 8; 23-31
10. Zhang G, Sun L, Wang XClinical study of a single congenital stapes malformation with possible X-linked dominant inheritance: Lin Chuang Er Bi Yan Hou Ke Za Zhi, 2005; 19(16); 745-47 [in Chinese]
11. Liu Y, Liu S, Wang B, Measurements of the middle ear in Chinese adults with normal hearing using high-resolution computed tomography: JAMA Otolaryngol Head Neck Surg, 2017; 143(10); 983-88
12. Li J, Li Y, Chen X, Analysis of the distance between the incus and stapes footplate for the design of a prosthesis: J Otolaryngol Head Neck Surg, 2019; 48(1); 36
13. Bartel R, Sanz JJ, Clemente I, Endoscopic stapes surgery outcomes and complication rates: A systematic review: Eur Arch Otorhinolaryngol, 2021; 278(8); 2673-79
14. Gilberto N, Custodio S, Colaco T, Middle ear congenital cholesteatoma: Systematic review, meta-analysis and insights on its pathogenesis: Eur Arch Otorhinolaryngol, 2020; 277(4); 987-98
15. Skinner M, Honrado C, Prasad M, The incudostapedial joint angle: Implications for stapes surgery prosthesis selection and crimping: Laryngoscope, 2003; 113(4); 647-53
16. Sudhoff H, Gehl HB, Boga E, Stapes prosthesis length: One size fits all?: Audiol Neurootol, 2019; 24(1); 1-7
17. Koopmann M, Weiss D, Savvas E, Outcome measures in stapes surgery: Postoperative results are independent from preoperative parameters: Eur Arch Otorhinolaryngol, 2015; 272(9); 2175-81
18. Vandevoorde A, Williams MT, Ukkola-Pons E, Early postoperative imaging of the labyrinth by cone beam CT after stapes surgery for otosclerosis with correlation to audiovestibular outcome: Otol Neurotol, 2017; 38(2); 168-72
19. Thiel G, Mills R, Persistent and recurrent conductive deafness following stapedotomy: J Laryngol Otol, 2011; 125(5); 460-66
20. Bakhos D, Lescanne E, Charretier C, A review of 89 revision stapes surgeries for otosclerosis: Eur Ann Otorhinolaryngol Head Neck Dis, 2010; 27(5); 177-82
21. Babighian GG, Albu S, Failures in stapedotomy for otosclerosis: Otolaryngol Head Neck Surg, 2009; 141(3); 395-400
22. Gros A, Vatovec J, Zargi M, Success rate in revision stapes surgery for otosclerosis: Otol Neurotol, 2005; 26(6); 1143-48
23. Marchica CL, Saliba I, The relationship between stapes prosthesis length and rate of stapedectomy success: Clin Med Insights Ear Nose Throat, 2015; 8; 23-31
24. Fang Y, Wang B, Galvin JJ, MPR-CT imaging for stapes prosthesis: Accuracy and clinical significance: Otol Neurotol, 2016; 37(4); 321-23
25. Bozzato A, Struffert T, Hertel V, Analysis of the accuracy of high-resolution computed tomography techniques for the measurement of stapes prostheses: Eur Radiol, 2010; 20(3); 566-71
26. Hahn Y, Diaz R, Hartman J, Assessing stapes piston position using computed tomography: A cadaveric study: Otol Neurotol, 2009; 30(2); 223-30
Figures
Tables
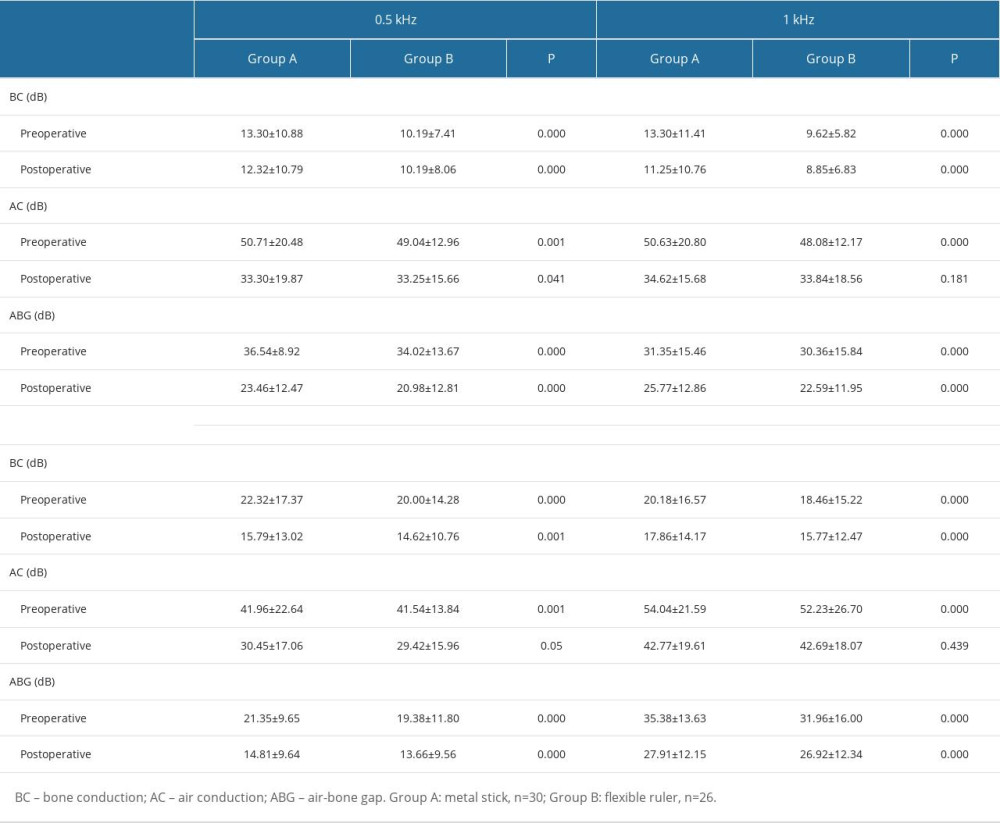 Table 1. Comparison of audiometric results between the 2 groups.
Table 1. Comparison of audiometric results between the 2 groups.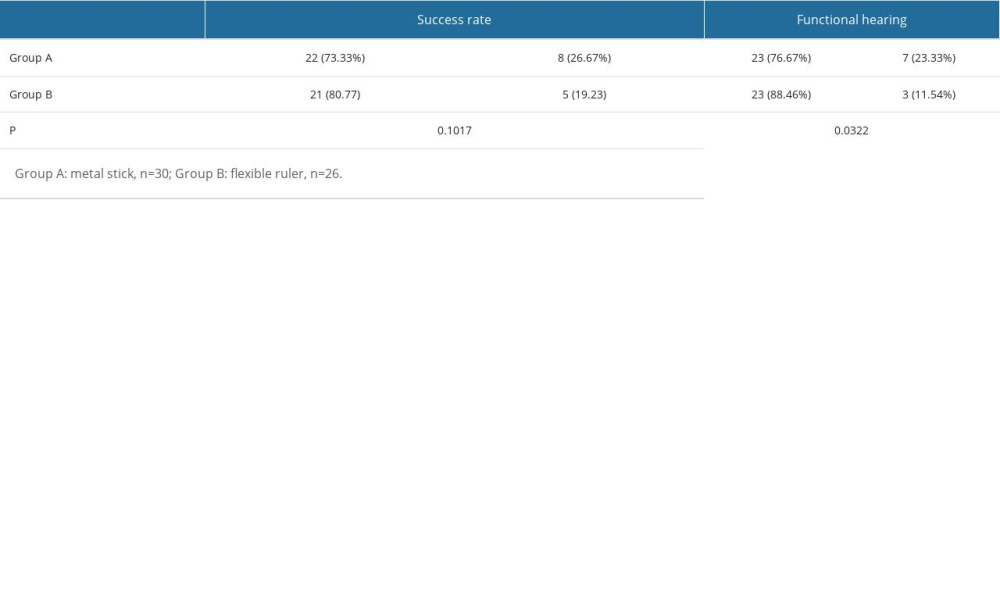 Table 2. Comparison of the success rate of surgery and the proportion of functional hearing.
Table 2. Comparison of the success rate of surgery and the proportion of functional hearing.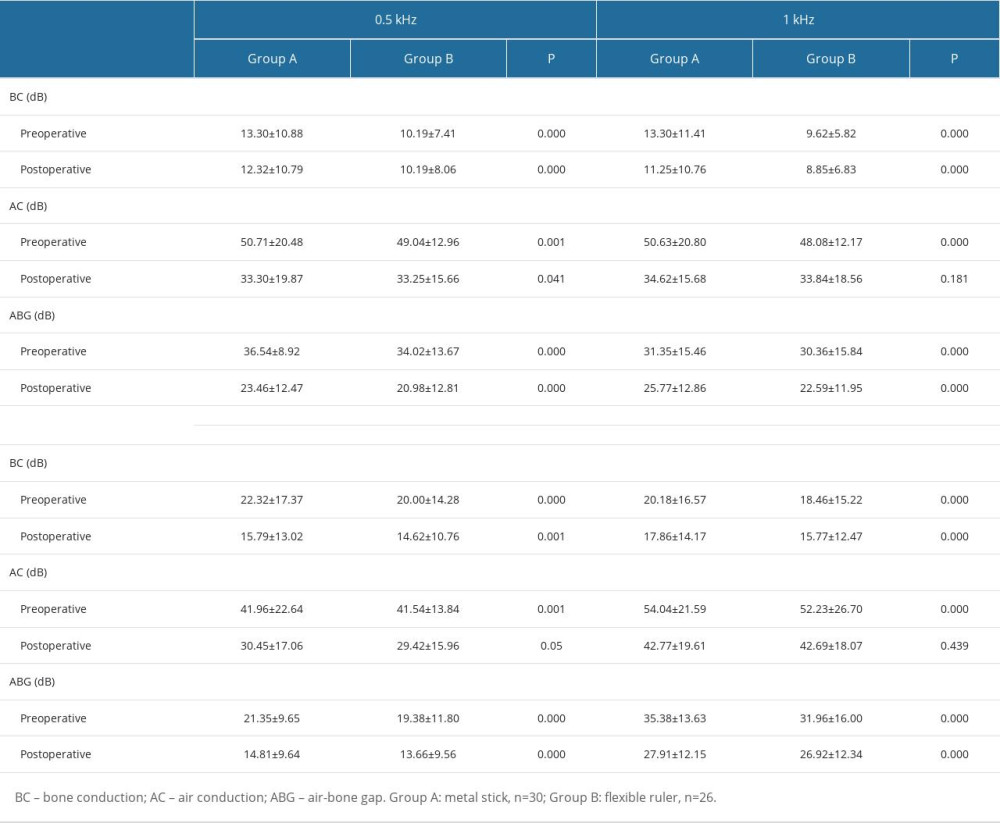 Table 1. Comparison of audiometric results between the 2 groups.
Table 1. Comparison of audiometric results between the 2 groups.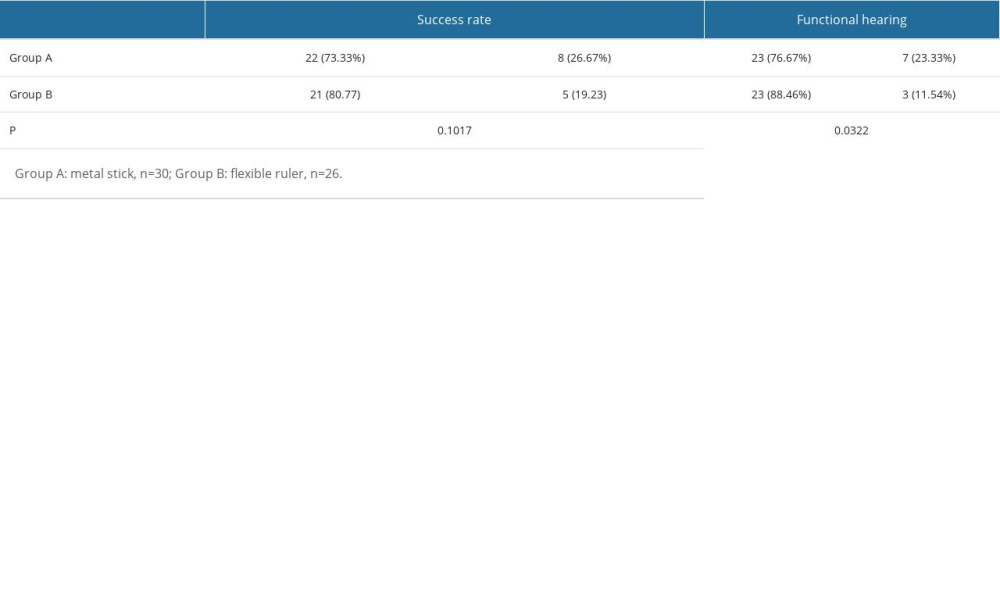 Table 2. Comparison of the success rate of surgery and the proportion of functional hearing.
Table 2. Comparison of the success rate of surgery and the proportion of functional hearing. In Press
14 Mar 2024 : Clinical Research
Differential DHA and EPA Levels in Women with Preterm and Term Births: A Tertiary Hospital Study in IndonesiaMed Sci Monit In Press; DOI: 10.12659/MSM.943895
15 Mar 2024 : Clinical Research
Evaluation of an Optimized Workflow for the Radiofrequency Catheter Ablation of Paroxysmal Atrial FibrillationMed Sci Monit In Press; DOI: 10.12659/MSM.943526
09 May 2024 : Review article
A Review of the Current Status of Disease-Modifying Therapies and Prevention of Alzheimer’s DiseaseMed Sci Monit In Press; DOI: 10.12659/MSM.945091
09 Apr 2024 : Clinical Research
Correlation between Thalamocortical Tract and Default Mode Network with Consciousness Levels in Hypoxic-Isc...Med Sci Monit In Press; DOI: 10.12659/MSM.943802
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952