03 December 2023: Clinical Research
Impact of Long-Term Blood Pressure Variability on Survival Rate in Elderly Maintenance Hemodialysis Patients: A 46-Month Follow-Up Study of 245 Patients
Yue Zhang1ABCDE, Daqing Hong1ABCDE, Qiang He1BCDE, Guisen Li1CDE, Hui Gao1AE*DOI: 10.12659/MSM.940621
Med Sci Monit 2023; 29:e940621
Abstract
BACKGROUND: At present, there are few blood pressure variability (BPV)-related studies of elderly maintenance hemodialysis (MHD) patients. This study aimed to compare the effects of long-term BPV on the 46-month survival rate of MHD patients aged <75 years and ≥75 years between 2000 and 2014, with follow-up until 2018.
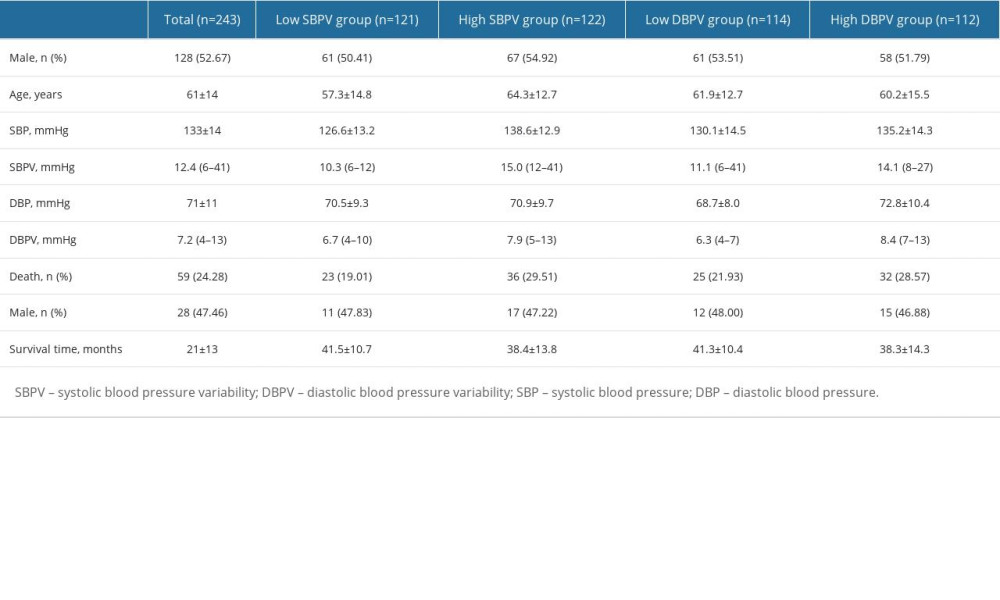
MATERIAL AND METHODS: According to systolic blood pressure variability (SBPV) and diastolic blood pressure variability (DBPV), patients were divided into 4 groups: a low SBPV group (n=121), a high SBPV group (n=122), a low DBPV group (n=114), and a high DBPV group (n=112).
RESULTS: We included 243 patients in the study. All the patients were followed up for 46 months, and 59 patients (28 males) died during follow-up. The survival rate of patients in the high SBPV group was significantly lower than that of the low SBPV group (log rank P=0.049). No significant differences were observed between the high DBPV group and low DBPV group (log rank P=0.167). There were no significant differences in survival rates between the high SBPV group and low SBPV group among patients aged <75 years (log rank P=0.656), and among patients ≥75 years, the survival rate of the high SBPV group was significantly lower than that of the low SBPV group (log rank P=0.041).
CONCLUSIONS: Increased long-term SBPV in MHD patients is associated with a decrease in long-term survival rate, and patients ≥75 years are more susceptible to it.
Keywords: Hemodialysis, Home, Survival
Background
Hypertension is the leading cause of cardiovascular disease and premature death worldwide [1]. Hypertension occurs in 67–92% of patients with chronic kidney disease, which increases with the decline in glomerular filtration rate (GFR) [2]. Blood pressure variability (BPV) refers to the degree of blood pressure variations within a certain period of time, representing the dynamic and characteristic physiological characteristics of cardiovascular system function [3]. It can be divided into inter-cardiac cycle BPV, short-term BPV, and long-term BPV according to the length of observation time [4].
For dialysis patients, short-term variability often refers to the blood pressure variability during dialysis, while long-term variability refers to the degree of blood pressure fluctuations at the beginning of each dialysis session within a certain period of time [5,6]. The NHANES III study suggested that long-term systolic BPV is positively associated with all-cause mortality in the general population [7], and increased long-term BPV is associated with increased cardiovascular mortality in patients with type 2 diabetes [8]. The effects of short-term BPV on the prognosis in hemodialysis patients have been extensively studied. However, the effects of long-term BPV, particularly variability over many years, have been less studied in hemodialysis patients [9,10]. Blood volume fluctuations, vascular calcification, and autonomic dysfunction in maintenance hemodialysis (MHD) patients lead to large and unstable BPV and poor prognosis [11,12]. Greater pre-dialysis BPV among hemodialysis patients was reported to be associated with all-cause mortality [13,14]. At present, there is still some controversy regarding the effects of systemic hypertension on survival in hemodialysis patients [15,16]. Therefore, this retrospective study aimed to compare the effects of long-term systemic blood pressure variability on the 46-month survival rate of 245 patients aged <75 years and ≥75 years on maintenance hemodialysis between 2000 and 2014, with follow-up until 2018.
Material and Methods
ETHICS STATEMENT:
The study was approved by the Medical Ethics Committee of Sichuan Provincial People’s Hospital (2018-167). Written informed consent was obtained from each patient.
PATIENTS:
Patients who entered our center for MHD due to uremia from January 2000 to January 2014 were retrospectively included. The BP data were obtained before each dialysis session of patients from January 2014 to June 2014. Inclusion criteria were patients with: (1) dialysis received for ≥3 months and (2) aged ≥18 years. Exclusion criteria were patients with: (1) BP data records for less than 1 time/month and (2) incomplete BP records.
BPV MEASUREMENT:
BP was measured using a unified electronic sphygmomanometer (OMron HEM 7200) after at least 10 min of quiet rest for each dialysis patient upon arrival at the dialysis room. BP was measured again 5 min later and the was averaged twice.
BPV encompasses broad blood pressure changes that occur within seconds or minutes (very short-term BPV), over 24 h (short-term BPV), and between days (mid-term BPV) [17]. Long-term BPV were obtained from the standard deviation (SD) of BP from January 2014 to June 2014. Long-term BPV is expressed as standard deviation (SD) and was calculated by the following formula:
According to systolic blood pressure variability (SBPV) and diastolic blood pressure variability (DBPV), patients were divided into 4 groups: a low SBPV group, a high SBPV group, a low DBPV group, and a high DBPV group. Follow-up observation was conducted until April 30, 2018 and the end-point was death.
STATISTICAL ANALYSIS:
Statistical analyses were performed using SPSS version 17.0 (SPSS, Chicago, IL, U.S.A.). Quantitative data are described as mean±standard deviation (SD) or median (inter-quartile range). Categorical variables are presented as numbers (percentage). Normally distributed data were compared using the
Results
PARTICIPANT CHARACTERISTICS:
We selected 276 patients registered in the Hemodialysis Remote Terminal System of our center and who had received ≥3 months of MHD treatment. Among them, 10 patients were transferred to transplantation, 2 were transferred to peritoneal dialysis, 11 were transferred to other hospitals, and 10 cases were excluded due to incomplete registration data; the remaining 243 patients were included in the study. There were 121 cases of primary glomerular disease, 44 cases of diabetic nephropathy, 31 cases of hypertensive renal damage, 19 cases of polycystic kidney disease, and 28 cases of other primary diseases. All the patients were followed up for 46 months, and 59 patients (28 males) died during follow-up (Table 1).
SURVIVAL:
According to the median of SBPV (12.4 mmHg) and the median of DBPV (7.2 mmHg), patients were divided into 4 groups: a low SBPV group, a high SBPV group, a low DBPV group, and a high DBPV group. Survival analysis showed that the survival rate of patients in the high SBPV group was significantly lower than that of the low SBPV group (log rank P=0.049). No significant differences were observed between the high DBPV group and low DBPV group (log rank P=0.167) (Table 1, Figure 1).
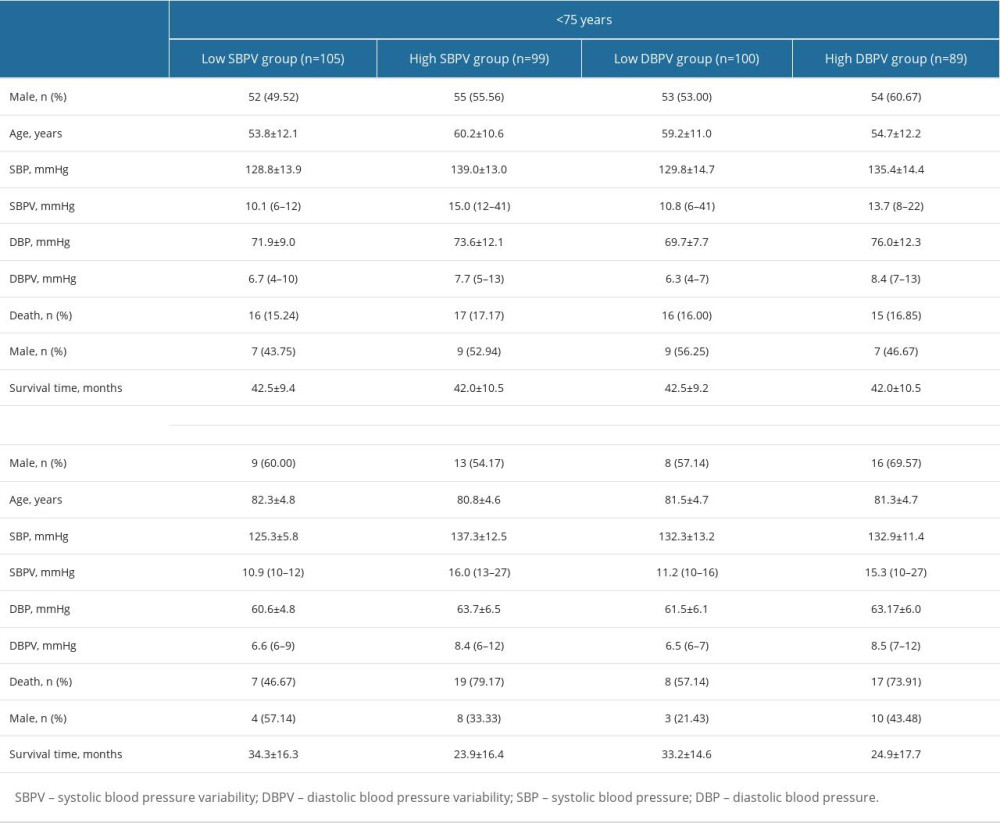
There were no significant differences in survival rates between the high SBPV group and low SBPV group among patients aged <75 years (log rank P=0.656), and among patients ≥75 years, the survival rate of high SBPV group was significantly lower than that of the low SBPV group (log rank P=0.041) (Table 2, Figure 2A, 2B). There was no significant difference in survival rates between the high DBPV group and low DBPV group in patients aged <75 years (log rank P=0.875) and patients aged ≥75 years (log rank P=0.190) (Table 2, Figure 2C, 2D).
Discussion
LIMITATIONS OF THE STUDY:
The small sample size and short study duration are limitations of this study. Therefore, a multicenter, prospective clinical study with a large sample size and long-term follow-up is needed.
Conclusions
In conclusion, increased long-term SBPV in MHD patients is associated with a decrease in long-term survival rate, and patients ≥75 years are more susceptible to it.
Figures
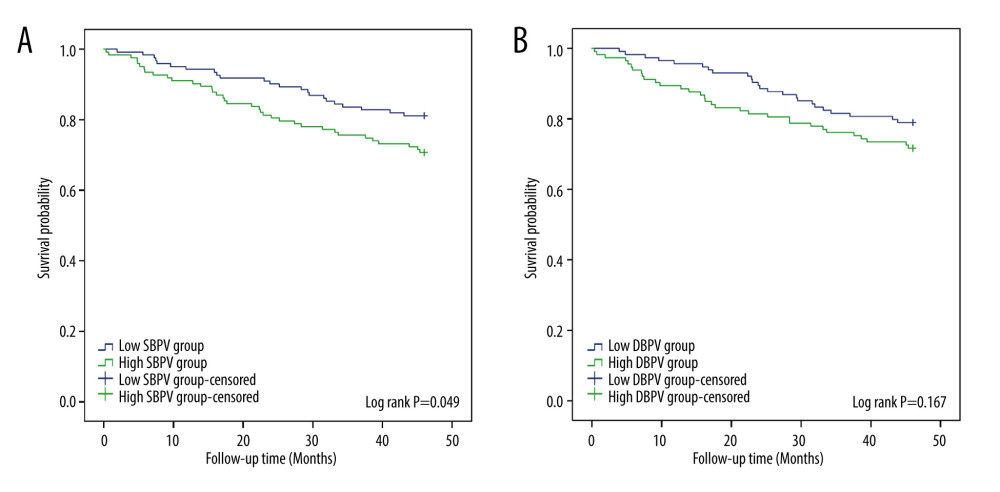 Figure 1. The relationship between blood pressure variability (BPV) and survival time in maintenance hemodialysis (MHD) patients. (A) The relationship between systolic blood pressure variability (SBPV) and survival time. (B) The relationship between diastolic blood pressure variability (DBPV) and survival time.
Figure 1. The relationship between blood pressure variability (BPV) and survival time in maintenance hemodialysis (MHD) patients. (A) The relationship between systolic blood pressure variability (SBPV) and survival time. (B) The relationship between diastolic blood pressure variability (DBPV) and survival time. 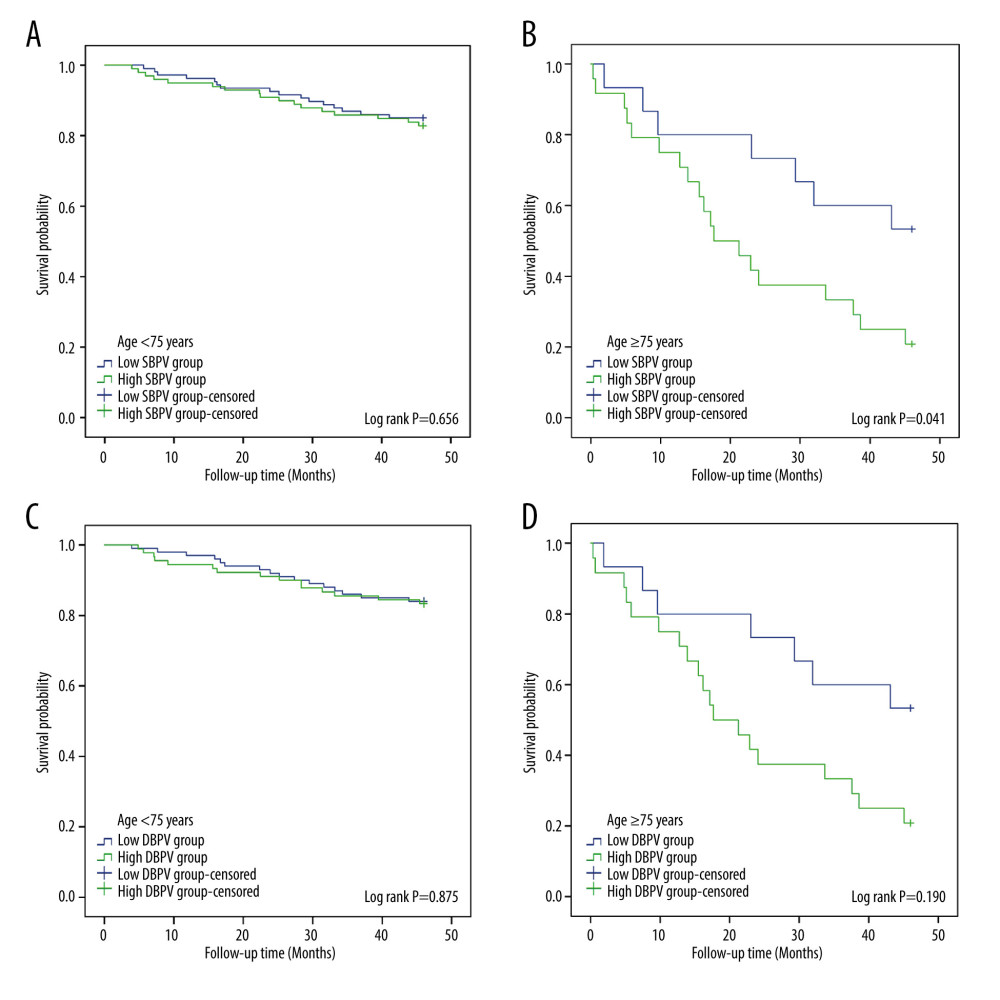 Figure 2. Maintenance hemodialysis (MHD) patients were grouped as patients aged <75 years and patients aged ≥75 years, and the relationship between BPV and survival time in each group is shown. (A) The relationship between systolic blood pressure variability (SBPV) and survival time of MHD patients <75 years. (B) The relationship between SBPV and survival time of MHD patients ≥75 years. (C) The relationship between diastolic blood pressure variability (DBPV) and survival time of MHD patients <75 years. (D) The relationship between DBPV and survival time of MHD patients ≥75 years.
Figure 2. Maintenance hemodialysis (MHD) patients were grouped as patients aged <75 years and patients aged ≥75 years, and the relationship between BPV and survival time in each group is shown. (A) The relationship between systolic blood pressure variability (SBPV) and survival time of MHD patients <75 years. (B) The relationship between SBPV and survival time of MHD patients ≥75 years. (C) The relationship between diastolic blood pressure variability (DBPV) and survival time of MHD patients <75 years. (D) The relationship between DBPV and survival time of MHD patients ≥75 years. References
1. Mills KT, Stefanescu A, He J, The global epidemiology of hypertension: Nat Rev Nephrol, 2020; 16(4); 223-37
2. Magvanjav O, Cooper-DeHoff RM, McDonough CW, Antihypertensive therapy prescribing patterns and correlates of blood pressure control among hypertensive patients with chronic kidney disease: J Clin Hypertens (Greenwich), 2019; 21(1); 91-101
3. Parati G, Stergiou GS, Dolan E, Bilo G, Blood pressure variability: Clinical relevance and application: J Clin Hypertens (Greenwich), 2018; 20(7); 1133-37
4. Schillaci G, Pucci G, The importance of instability and visit-to-visit variability of blood pressure: Expert Rev Cardiovasc Ther, 2010; 8(8); 1095-97
5. Feng Y, Li Z, Liu J, Association of short-term blood pressure variability with cardiovascular mortality among incident hemodialysis patients: Ren Fail, 2018; 40(1); 259-64
6. Liao R, Li J, Lin L, The association between long- and intra-dialytic blood pressure variability with all-cause mortality in hemodialysis patients: Blood Purif, 2019; 48(1); 43-50
7. Muntner P, Shimbo D, Tonelli M, The relationship between visit-to-visit variability in systolic blood pressure and all-cause mortality in the general population: Findings from NHANES III, 1988 to 1994: Hypertension, 2011; 57(2); 160-66
8. Hsieh YT, Tu ST, Cho TJ, Visit-to-visit variability in blood pressure strongly predicts all-cause mortality in patients with type 2 diabetes: A 5•5-year prospective analysis: Eur J Clin Invest, 2012; 42(3); 245-53
9. Sarafidis PA, Loutradis C, Karpetas A, The association of interdialytic blood pressure variability with cardiovascular events and all-cause mortality in haemodialysis patients: Nephrol Dial Transplant, 2020; 35(7); 1277
10. Wang Q, Wang Y, Wang J, Short-term systolic blood pressure variability and kidney disease progression in patients with chronic kidney disease: Results from C-STRIDE: J Am Heart Assoc, 2020; 9(12); e015359
11. Burton JO, Jefferies HJ, Selby NM, McIntyre CW, Hemodialysis-induced cardiac injury: Determinants and associated outcomes: Clin J Am Soc Nephrol, 2009; 4(5); 914-20
12. Yamamoto K, Kobayashi N, Kutsuna T, Excessive fall of blood pressure during maintenance hemodialysis in patients with chronic renal failure is induced by vascular malfunction and imbalance of autonomic nervous activity: Ther Apher Dial, 2012; 16(3); 219-25
13. Yang J, Huang J, Yu B, Long-term predialysis blood pressure variability and outcomes in hemodialysis patients: J Clin Hypertens (Greenwich), 2022; 24(2); 148-55
14. Wang Y, Qin Y, Fan X, Variability in predialysis systolic blood pressure and long-term outcomes in hemodialysis patients: Kidney Blood Press Res, 2018; 43(1); 115-24
15. Khan YH, Sarriff A, Adnan AS, Blood pressure and mortality in hemodialysis patients: a systematic review of an ongoing debate: Ther Apher Dial, 2016; 20(5); 453-61
16. Turner JM, Peixoto AJ, Blood pressure targets for hemodialysis patients: Kidney Int, 2017; 92(4); 816-23
17. Parati G, Stergiou GS, Dolan E, Bilo G, Blood pressure variability: Clinical relevance and application: J Clin Hypertens (Greenwich), 2018; 20(7); 1133-37
18. Cahan A, Ben-Dov IZ, Bursztyn M, Association of heart rate with blood pressure variability: Implications for blood pressure measurement: Am J Hypertens, 2012; 25(3); 313-18
19. Chang JY, Jeon SB, Jung C, Postreperfusion blood pressure variability after endovascular thrombectomy affects outcomes in acute ischemic stroke patients with poor collateral circulation: Front Neurol, 2019; 10; 346
20. Selvarajah V, Pasea L, Ojha S, Pre-dialysis systolic blood pressure-variability is independently associated with all-cause mortality in incident haemodialysis patients: PLoS One, 2014; 9(1); e86514
21. Kikuya M, Hozawa A, Ohokubo T, Prognostic significance of blood pressure and heart rate variabilities: The Ohasama study: Hypertension, 2000; 36(5); 901-6
22. Rossignol P, Cridlig J, Lehert P, Visit-to-visit blood pressure variability is a strong predictor of cardiovascular events in hemodialysis: insights from FOSIDIAL: Hypertension, 2012; 60(2); 339-46
23. Tozawa M, Iseki K, Yoshi S, Fukiyama K, Blood pressure variability as an adverse prognostic risk factor in end-stage renal disease: Nephrol Dial Transplant, 1999; 14(8); 1976-81
24. Brunelli SM, Thadhani RI, Lynch KE, Association between long-term blood pressure variability and mortality among incident hemodialysis patients: Am J Kidney Dis, 2008; 52(4); 716-26
25. Li H, Xue J, Dai W, Blood pressure variability and outcomes in end-stage renal disease patients on dialysis: A systematic review and meta-analysis: Kidney Blood Press Res, 2020; 45(5); 631-44
26. Nording HM, Seizer P, Langer HF, Platelets in inflammation and atherogenesis: Front Immunol, 2015; 6; 98
27. Coccina F, Pierdomenico AM, Cuccurullo C, Pierdomenico SD, Prognostic value of average real variability of systolic blood pressure in elderly treated hypertensive patients: Blood Press Monit, 2019; 24(4); 179-84
28. Qin X, Zhang Q, Yang S, Blood pressure variability and morning blood pressure surge in elderly Chinese hypertensive patients: J Clin Hypertens (Greenwich), 2014; 16(7); 511-17
29. Wang T, Li Y, Wu H, Optimal blood pressure for the minimum all-cause mortality in Chinese ESRD patients on maintenance hemodialysis: Biosci Rep, 2020; 40(8); BSR20200858
Figures
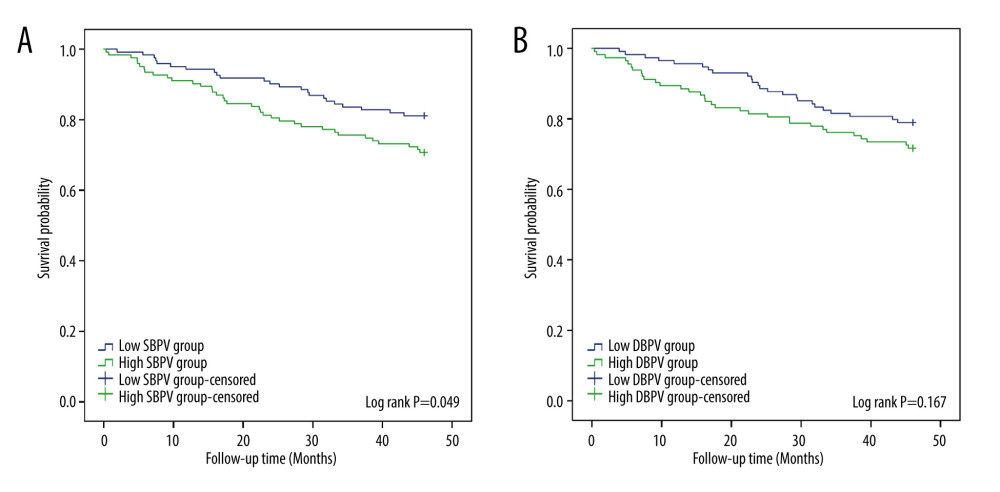 Figure 1. The relationship between blood pressure variability (BPV) and survival time in maintenance hemodialysis (MHD) patients. (A) The relationship between systolic blood pressure variability (SBPV) and survival time. (B) The relationship between diastolic blood pressure variability (DBPV) and survival time.
Figure 1. The relationship between blood pressure variability (BPV) and survival time in maintenance hemodialysis (MHD) patients. (A) The relationship between systolic blood pressure variability (SBPV) and survival time. (B) The relationship between diastolic blood pressure variability (DBPV) and survival time.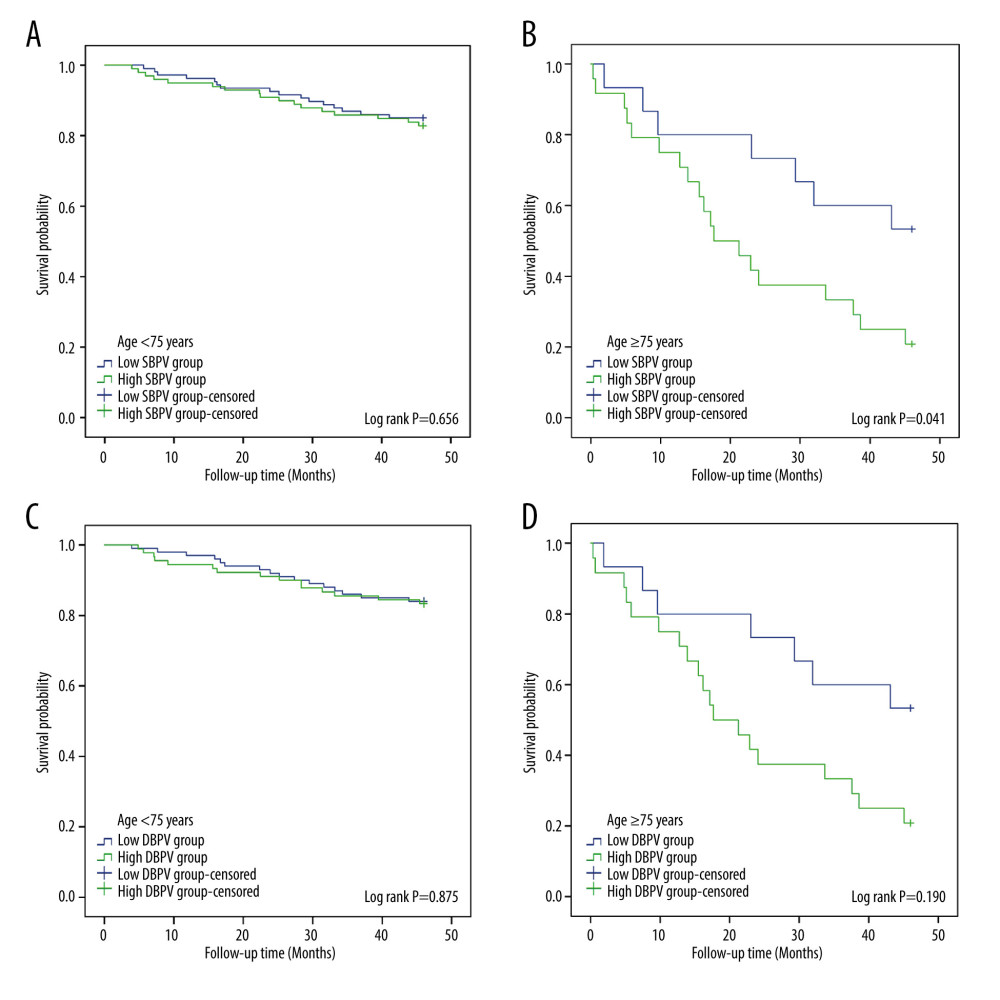 Figure 2. Maintenance hemodialysis (MHD) patients were grouped as patients aged <75 years and patients aged ≥75 years, and the relationship between BPV and survival time in each group is shown. (A) The relationship between systolic blood pressure variability (SBPV) and survival time of MHD patients <75 years. (B) The relationship between SBPV and survival time of MHD patients ≥75 years. (C) The relationship between diastolic blood pressure variability (DBPV) and survival time of MHD patients <75 years. (D) The relationship between DBPV and survival time of MHD patients ≥75 years.
Figure 2. Maintenance hemodialysis (MHD) patients were grouped as patients aged <75 years and patients aged ≥75 years, and the relationship between BPV and survival time in each group is shown. (A) The relationship between systolic blood pressure variability (SBPV) and survival time of MHD patients <75 years. (B) The relationship between SBPV and survival time of MHD patients ≥75 years. (C) The relationship between diastolic blood pressure variability (DBPV) and survival time of MHD patients <75 years. (D) The relationship between DBPV and survival time of MHD patients ≥75 years. In Press
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952