27 November 2023: Clinical Research
Effect of Stand-Alone Oblique Lateral Interbody Fusion (OLIF) in Treating Lumbar Spine Lesions
Yongxing Song1ABCDE, Haidong Wang1ABCDEFG*DOI: 10.12659/MSM.940872
Med Sci Monit 2023; 29:e940872
Abstract
BACKGROUND: The aim of this study was to investigate the safety and early clinical results of stand-alone oblique lateral interbody fusion (OLIF) in the fusion of lumbar spine lesions and to explore the indications for surgery.
MATERIAL AND METHODS: A total of 92 cases of lumbar spine lesions treated with stand-alone OLIF in 2 medical centers from October 2014 to December 2018 were retrospectively analyzed. We included 30 males and 62 females, ages 32-83 years.
RESULTS: Our results showed that the operation time was 60.92±27.40 min (average 36.6 min) and the intraoperative blood loss was 68.22±141.6 ml (average 23.8 ml). The height of the intervertebral space was restored – before the operation (9.23±1.94 mm) and (12.68±2.01 mm) after the operation – and it was 10.18±2.14 mm at the last follow-up. There was a significant difference between the postoperative and preoperative values (t=9.27, P<0.0001), and there was also a significant difference between the final follow-up and postoperative comparison value (t=8.43, P<0.0001).
CONCLUSIONS: The use of stand-alone OLIF in treating fusion of lumbar spine lesions showed excellent clinical efficacy and achieved the expected clinical improvements.
Keywords: Diagnostic Imaging, Manipulation, Spinal, Microcephaly Cervical Spine Fusion Anomalies
Background
Oblique lateral interbody fusion (OLIF) has been widely used for treating various degenerative lumbar conditions and it is an effective surgical tool to treat spine-related diseases [1,2]. Lumbar interbody fusion involves insertion of a structural graft into an intervertebral disc space to promote bony arthrodesis [3–5]. Spinal disorders range from degenerative conditions to trauma, and neoplastic diseases and deformities need correction [6–8]. Basic research related to osteoblast function and regulation has progressed over many years and some proteins and signaling pathways have been used in the clinic to treat some bone disorders [9–20]. However, the detailed mechanism is still elusive, and the surgery is still the most commonly used method to correct the potential deformation. At present, there are 3 main methods of OLIF technology in clinical application: stand-alone OLIF, OLIF combined with lateral plate or screw rod fixation, and OLIF combined with posterior pedicle screw fixation [21–24]. According to the results of biomechanical experiments [25–28], OLIF combined with pedicle screw fixation provides the best biomechanical stability, but it requires significant increases in anesthesia and surgical time and requires separate incisions and position.
Placement of a steel plate or nail rod system may require lengthening of the incision and exposure of the lumbar spine blood vessels, and this can cause significant irritation to the lumbar plexus and psoas [29–33]. The plexus nerve is irritated, and the lateral fixation strength is more stable than without fixation. Due to the large volume and area of the cage used in OLIF technology, it can well disperse the stress and conduct the load. Thus, this study aimed to investigate the clinical stability and effect of stand-alone OLIF for the fusion of lumbar spine lesions and aimed to establish a thorough understanding of the indications for surgery. We retrospectively analyzed the data of 92 cases of lumbar spine lesions treated with stand-alone OLIF from October 2014 to December 2018 in our hospital. Stand-alone OLIF in the fusion of lumbar spine lesions achieved good early results and had good clinical advantages, but there was a high rate of complications. It is recommended to choose the method cautiously. Further studies are needed to continue to summarize, explore, and clarify the indications for surgery.
Material and Methods
GENERAL INFORMATION:
There were 30 males and 62 females in this study group. Age ranged from 32 to 83 years, with an average age of 61.2±12.94 years. Disease types were as follows: 20 cases of lumbar spinal stenosis, 15 cases of lumbar disc degeneration and 11 cases of lumbar degenerative spondylolisthesis (I°), 6 cases of discogenic lower back pain, 7 cases of giant lumbar disc herniation, 13 cases of primary lumbar intervertebral interstitial inflammation in the turnaround period, 6 cases of adjacent spondylosis after lumbar internal fixation, and 14 cases of degenerative lumbar kyphosis. The clinical symptoms and signs mainly included severe back and leg pain, intermittent claudication, weakened muscle strength of the lower limbs, and hypoesthesia. Preoperative dual-energy X-ray bone mineral density examination showed that 31 cases had a T value of −1 to −2.4 SD, 8 cases had a T value of −2.5 to −3.5 SD, and the remaining T values were normal. Number of fusion segments were as follows: 68 cases of a single segment, 9 cases of 2 segments, 12 cases of 3 segments, and 3 cases of 4 segments. Specific fusion sites were as follows: L1–2 (1 case), L2–3 (4 cases), L3–4 (10 cases), L4–5 (53 cases), L2–3 L3–4 (3 cases), L3–4 L4–5 (6 cases), L1–2 L2–3 L3–4 (1 case), L1–2 L3–4 L4–5 (1 case), L2–3 L3–4 L4–5 (10 cases), and L1–2 L2–3 L3–4 L4–5 (3 cases).
SURGERY:
All patients were under placed general anesthesia. The patients were placed in a standard right decubitus position, the hip was flexed, and the armpit and hip were fixed with a wide cloth glue. The C-arm machine located and planned the incision. Incision planning was as follows: single-segment fusion was to project the anterior edge of the vertebral body along the body surface of the diseased intervertebral space 2 cm forward and 1 cm backward, and the incision length was 3 cm; 2-segment fusion included 2 segments. The oblique projection of the middle part of the lesion was still the anterior edge of the vertebral body extending 2–3 cm forward and 2 cm backward, making an incision about 4–5 cm long; for 3-segment fusion, a slightly longer oblique incision was made at the center of the 3 segments of approximately 6 cm; for 4-segment fusion, 2 upper and lower incisions were made, each with a length of 4–5 cm. The transversus abdominis was cut and the extraperitoneal fat and abdominal viscera were gently pushed to expose the psoas major muscle. The psoas major was gently pushed to the dorsal side, a retractor was used to pull the psoas major to the dorsal side, and the abdominal organs and extraperitoneal fat were drawn to the ventral side, thus revealing the intervertebral space of the diseased segment obliquely in the anterior middle 1/3 of the intervertebral space. After inserting the guide needle, the C-arm X-ray machine fluoroscopy confirmed that the diseased segment was correct, and then the expansion sleeve and the channel with a light source were placed step by step.
The cannula was removed, the channel was opened and fixed (note: the channel was kept oblique and fixed parallel to the intervertebral space), discectomy was performed, a blunt reamer was inserted perpendicular to the direction of the intervertebral space, and the intervertebral space was determined through C-arm X-ray machine perspective location and endplate orientation. The intervertebral nucleus pulposus and endplate cartilage were removed, and blunt distractors and cage trial models were used to distract and loosen the intervertebral space to further remove the residual nucleus pulposus and endplate cartilage to create a cage bed. The height and length of the fusion device were determined according to the C-arm X-ray machine fluoroscopy. During the process of implanting the intervertebral space, the bone mass was dropped vertically into the intervertebral space, and the C-arm X-ray machine fluoroscopy was used again to determine the position of the fusion cage. After flushing the incision and detecting no active bleeding in the incision, the channel was removed. Those who underwent fusion of 2 or more segments received implantation in the other segments one by one according to this method. After all the segmental fusion cages were implanted, the incision was inspected again to confirm that there was no active bleeding in the incision, and the incision was sutured layer by layer. Except in 2 cases (1 case of left common iliac artery injury for enlarged incision vascular repair and 1 case of left ovarian vein injury for enlarged incision for hemostasis), negative-pressure drainage was placed, and no drainage tube was placed in the incision in the remaining cases.
The fusion device used was the Peek material Clydesdale fusion device (USA) and the bone graft in the fusion device used was artificial bone in 59 cases, xenograft bone in 14 cases, and allogeneic bone in 19 cases. The artificial bone was produced by Wright Medical Technology Co., Ltd. (USA), BMP2 was produced by Hangzhou Jiuyuan Genetic Engineering Co., Ltd. (China), and BMP2 was dissolved in calcium sulfate and was placed into the fusion device. The xenogeneic bone was produced and provided by Tianjin Zhongjin Biological Development Co., Ltd. (China). The dried calf bone (Jinshi Bone Ling) and allogeneic bones were provided by Beijing Xinkangchen Medical Technology Development Co., Ltd.
POSTOPERATIVE TREATMENT:
Routine postoperative treatments included preventive anti-infection, fluid replacement, and bed rest. After awakening from anesthesia, the patient was instructed to actively perform both lower extremity ankle-extension exercises and passively perform both lower extremities straight-leg elevation exercises. In 2 cases where the drainage tube was placed in the incision, the drainage tube was removed 48 to 72 h after the operation according to the drainage volume (24 h drainage volume <50 ml). Except for 3 cases with vertebral fractures, the patients were in bed for 6 weeks. The rest of the patients wore a thoracolumbar brace and got out of bed 3 to 5 days after the operation.
EVALUATION METHODS AND OBSERVATION INDICATORS:
We recorded the amount of blood loss and operation time. For clinical efficacy, visual analog scale (VAS) score and Oswestry disability index (ODI) were used to evaluate the low-back pain and lumbar function preoperatively and at last follow-up.
IMAGING EVALUATION:
Lumbar X-ray positive and lateral examinations were performed at 3 to 5 days, 1.5 months, 3 months, 6 months, and 12 months after surgery. Lumbar spine examinations were performed at the same time 12 months after surgery. X-ray examination of flexion and hyperextension were conducted. Computed tomography (CT) scans and two-dimensional (2D) and three-dimensional (3D) reconstruction were performed to evaluate the initial position of the fusion cage, whether the fusion cage developed subsidence or anteroposterior displacement, intervertebral fusion conditions, and degeneration of the adjacent segments (including degeneration or herniation of intervertebral discs, bone hyperplasia, local deformities, and vertebral slippage). The settlement of the fusion cage was evaluated using the grading standard below: grade 0, intervertebral space height loss 0–24%; grade I, intervertebral space height loss 25–49%; grade II, intervertebral space height loss 50–74%; and grade III, 75–100% loss of intervertebral space height.
COMPLICATIONS:
Intraoperative endplate injury, vertebral fracture, vascular injury, intraoperative and postoperative nerve injury, postoperative incision skin necrosis, and incision infection were assessed.
STATISTICAL ANALYSIS:
The data obtained were processed using SPSS20.0 statistical software, and the data were represented as (x±s). The height of the intervertebral space of the segment during the preoperative and postoperative stages and at the final follow-up, as well as the lower back pain and ODI at the preoperative stage and final follow-up, were analyzed using two-way ANOVA. The index was tested with paired data. The test level was α=0.05, and the difference was considered statistically significant at
Results
CLINICAL AND IMAGING RESULTS:
The operation time was about 40–140 min, with an average time of 60.92±27.40 min; the average time for each fusion segment was 36.6 min; and the intraoperative blood loss was 20–720 ml with an average bleeding volume of 68.22±141.6 ml, and the average bleeding per OLIF segment was 23.8 ml. The bleeding volume of the enlarged incision for vascular repair was 720 ml, and the bleeding volume of the other left ovarian vein injury was 670 ml. The height of the intervertebral space was restored from 9.23±1.94 mm before surgery to 12.68±2.01 mm after surgery, and the height of the intervertebral space was 10.18±2.14 mm at the last follow-up. There was a significant difference between the postoperative and preoperative values (t =9.27, P<0.0001), and there was a significant difference between the final follow-up and postoperative comparison values (t=8.43, P<0.0001) (Figures 1–4). The patient’s low-back pain score ranged from 6.28±2.11 points preoperatively to 1.52±0.73 points at the last follow-up. There was a statistically significant difference (t=8.56, P<0.0001=0.028); the ODI index was 36.3±7.52% preoperatively and it recovered to 10.6±3.29% at the last follow-up, which was significantly different (t=7.79, P<0.0001). Except for 9 cases at the last follow-up, the remaining cases underwent intervertebral fusion, the fusion rate was 90.2%, and no obvious degeneration of adjacent segments was observed (Table 1).
INTRAOPERATIVE AND POSTOPERATIVE COMPLICATIONS:
There were 4 cases of vascular injury during the operation, of which 1 case of left common iliac artery injury was freed, the abdominal aorta temporarily blocked, and the common iliac artery was repaired. One case of ovarian vein injury was compressed and filled to stop bleeding, and 2 cases were segmented. Vascular damage was electro-coagulated to stop bleeding. There were 21 cases of endplate injury: 13 cases were confirmed during the operation, 8 cases were confirmed by postoperative imaging examination, 4 cases of endplate injury were associated with vertebral fractures, and 21 cases of endplate injury included vertebral fractures. There were no necroses or infections in the incision skin in this group. Except for 4 patients with vertebral fractures, which were bedridden for 6 weeks, the remaining patients were out of bed with thoracolumbar braces 3–5 days after surgery. Left sympathetic chain injury occurred in 4 cases after 3–5 days; 4 cases of transient hip flexion weakness recovered after 3 to 5 days; and there were 2 cases of left thigh anterior lateral pain, numbness, and weakness of the quadriceps femoris. One patient with incomplete intestinal obstruction recovered after 5 days. During the follow-up, the fusion cages showed subsidence of varying degrees, including 69 cases with grade 0, 17 cases with grade I, 5 cases with grades II, and 1 case with grade III (Figures 1–4; Table 2).
A total of 8 patients received additional posterior pedicle screw fixation due to fusion cage subsidence and intractable lumbar pain and occurred within 3 months after surgery; 6 of the 8 cases had endplate damage during the initial operation. A total of 6 cases of fusion cage settlement and lateral displacement occurred within 3 months after surgery. Five cases had endplate damage during the initial operation, and 6 cases were fixed with posterior pedicle screws without fusion cage adjustment. The reoperation rate in the group was 15.22%.
Narrow cages (18 mm) and stand-alone cages are associated with increased risk of developing cage subsidence. In this group we noted intraoperative and postoperative complications, such as vascular injury, endplate injury, vertebral fracture, sympathetic chain injury, hip flexor and quadriceps weakness, intestinal obstruction, and fusion cage displacement. There were 60 cases of reoperation, including 12 cases with 2 complications, namely, 4 cases of endplate injury combined with vertebral fracture, 7 cases of endplate injury and reoperation due to fusion cage subsidence after the operation, and 1 case of postoperative fusion cage relocation and reoperation. Thus, according to the actual number of cases, the number of complications in this group was 38 cases, and the incidence was 41.3% (Figures 1–4).
Discussion
Because the OLIF technology involves exposure through blunt separation and stratification of muscle fibers through the anterolateral aspect of the abdomen, and then it enters the intervertebral space through the natural space between the psoas major muscle and the iliac vascular sheath, the exposure is rapid. The intervertebral space operation is performed under the channel with its own light source. The field of view is constant, the illumination is good, and the operation is direct. The operation of the intervertebral space is basically completed under direct vision. One incision can complete the fusion of 3 segments [34–36]. Artificial bone, xenogeneic bone, or allogeneic bone is used for bone grafting in the fusion cage. Autogenous iliac bone is not used, and no lateral or posterior internal fixation is attached [33,35,37–39]. The operation time in this group was 60.92±27.40 min, and the average time used for each fusion segment was 36.6 min; the intraoperative blood loss was (68.22±141.6) ml, and the average bleeding per fusion segment was 23.8 ml. The height of the intervertebral space of the fusion segment achieved good recovery after the operation, which was significantly different from the preoperative value. Of course, the height of the intervertebral space was significantly reduced during the follow-up process, which was also significantly different from the postoperative value.
At the final follow-up, 9 cases that were unclear but all the other cases had intervertebral fusion, with a fusion rate of 90.2%. Low-back pain decreased from 6.28±2.11 points before surgery to 1.52±0.73 points at the last follow-up, and the ODI index recovered from 36.3±7.52% before surgery to 10.6±3.29% at the last follow-up. Compared with the preoperative levels, both the VAS score and ODI index of low-back pain showed significant differences, indicating that low-back pain and lumbar spine function recovered well. In summary, the application of stand-alone OLIF technology in lumbar spine lesions has advantages, such as short operation time, less trauma, less bleeding, fast recovery, good fusion, and accurate results.
As a new technology that has emerged in recent years, OLIF has a clinician learning curve, including complications, especially in the application of the stand-alone method [40–44]. The cases in this group were cases in the early stages of the 2 medical centers. Therefore, the incidence of complications was relatively high: 41.3%, including 21 cases of endplate injury (incidence rate of 22.8%), 4 cases of vertebral fracture (incidence rate of 4.3%), 4 cases of vascular injury (incidence rate of 4.3%), 4 cases of sympathetic chain injury (incidence rate of 4.3%), 6 cases of fusion cage displacement (incidence rate of 6.5%), and 14 cases of reoperation (incidence rate of 15.2%). Complications included severe damage to large blood vessels, reoperation due to sinking or displacement of the fusion cage, and mild transient damage. Overall, our study shows that the complication rate was 41.3%, which was similar to the complication rate reported in the literature for stand-alone LLIF (42.2%). The reoperation rate reported in the literature was 11.1%, and the reoperation rate in our study was 15.22%, which is slightly higher than that of stand-alone LLIF. Our study found the stand-alone OLIF cage subsidence rate was higher than the stand-alone LLIF rate [45–47].
The patient’s individual factors contribute to complications, such as variations in the anatomical structure of the surgical approach, including towering the psoas major, high bifurcation of iliac blood vessels, abnormal iliac lumbar blood vessels, irregular endplate morphology, and high iliac crest [35,48–50]. The surgeon’s experience and surgical technique are also important factors. For example, the surgeon’s inadequate understanding of OLIF technology and lack of rigorous operation training may lead to poor surgical indications and improper selection of surgical methods. Some cases are suitable for OLIF, but not suitable for stand-alone applications, including the following: (1) The patient had bone loss or even osteoporosis; preoperative bone density detection in this group showed 31 cases of bone loss and 8 cases of osteoporosis; and (2) Three-segment or more fusion; 12 cases of three-segment fusion and 3 cases of four-segment fusion were performed in this group.
For the application of stand-alone OLIF, in addition to thoroughly understanding the surgical indications, it is also necessary to perform a meticulous operation during the surgery, strictly protect the endplate, and provide effective treatment after the endplate injury. External protection of the thoracic and lumbar spine should be strengthened after the operation, such as by application of a thoracolumbar brace and close follow-up [51–54].
The present study has certain weaknesses. We only reported the early results of a single surgical method, and did not combine this technique with other fixation and fusion methods, such as posterior pedicle screw fixation and interbody fusion, or OLIF combined with posterior pedicle screw fixation. There was no statistical analysis of the clinical results and complications of different diseases and different fusion segments. In addition, the follow-up time of this group was not long enough, and follow-up observation needs to be strengthened. For osteoporosis patients, greater emphasis is needed on getting patients out of bed under the protection of thoracic and lumbar support after the operation, strengthening anti-osteoporosis treatment, and strengthening lower back and abdominal muscles.
Conclusions
The application of stand-alone OLIF has unique clinical advantages in specific clinical cases. The high rate of complications and reoperation when applied to a general population should encourage clinicians to identify key success factors. Our study has demonstrated that protection of the intraoperative endplate, effective treatment after endplate injury, and strict follow-up observation are key in stand-alone OLIF in patients with degenerative lumbar spondylosis.
Figures
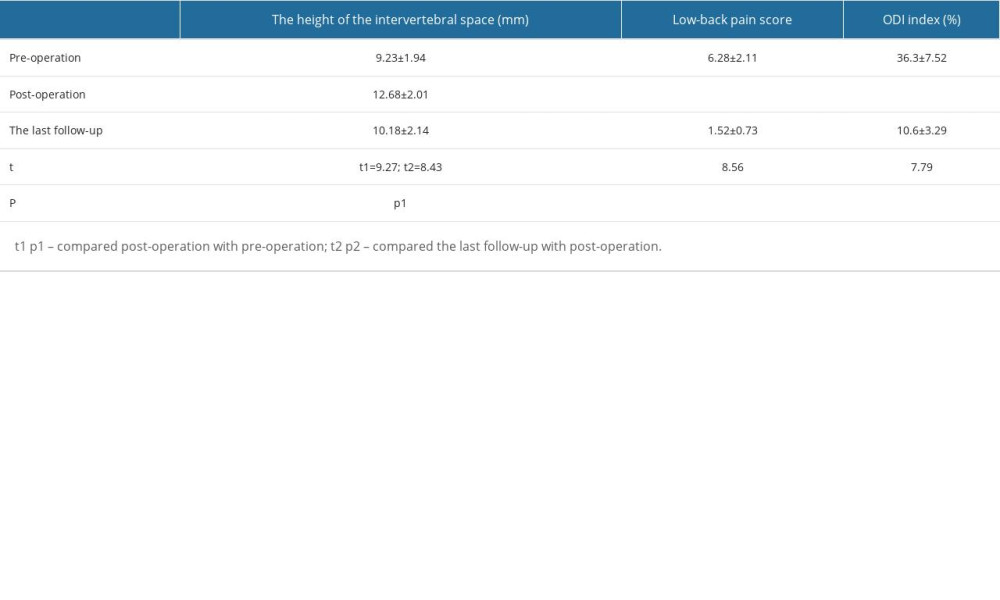
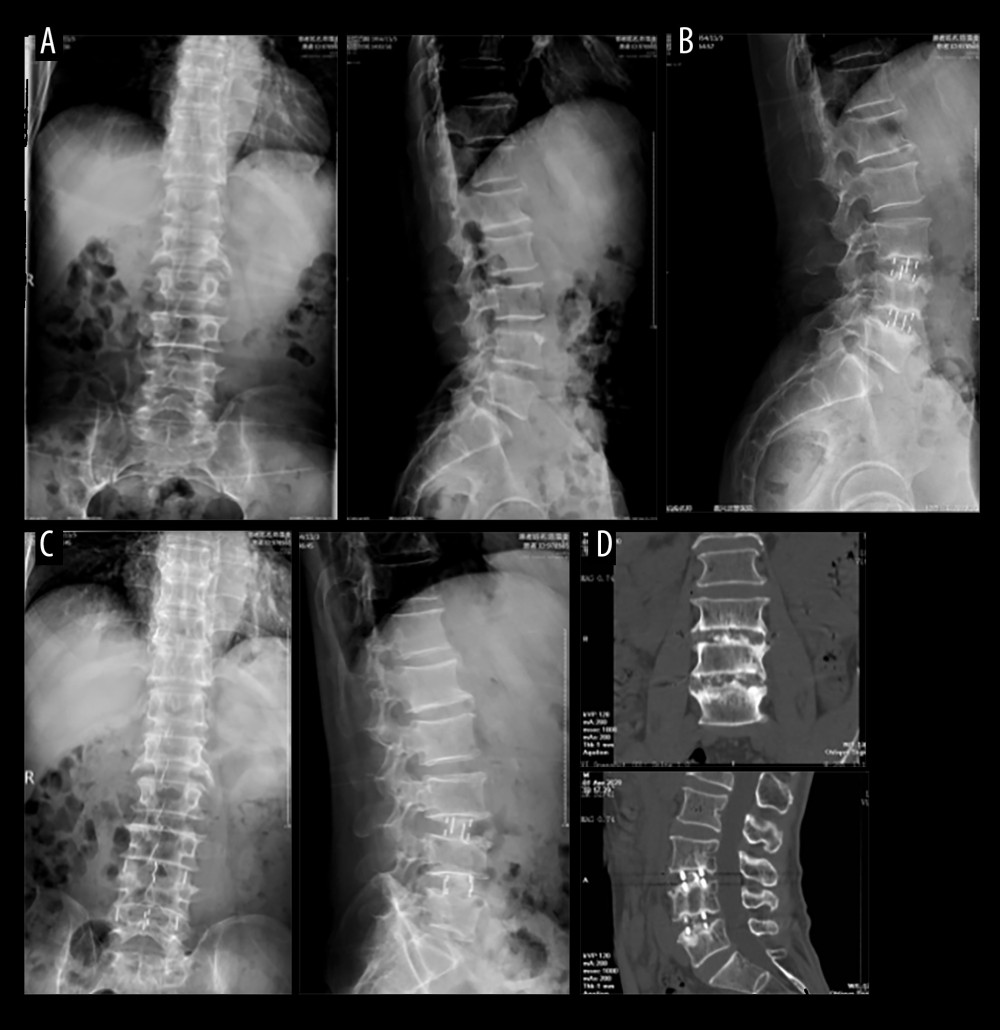 Figure 1. A 63-year-old male patient with diagnosis(A) Lumbar 3/4, lumbar 4/5 intervertebral disc degeneration. (B) Translateral oblique lateral lumbar 3/4, lumbar 4/5 interbody fusion. (C) Postoperative lumbar spine X-ray front and side radiographs. (D) Postoperative 26 months; the lumbar CT plain scan and coronal and sagittal reconstruction.
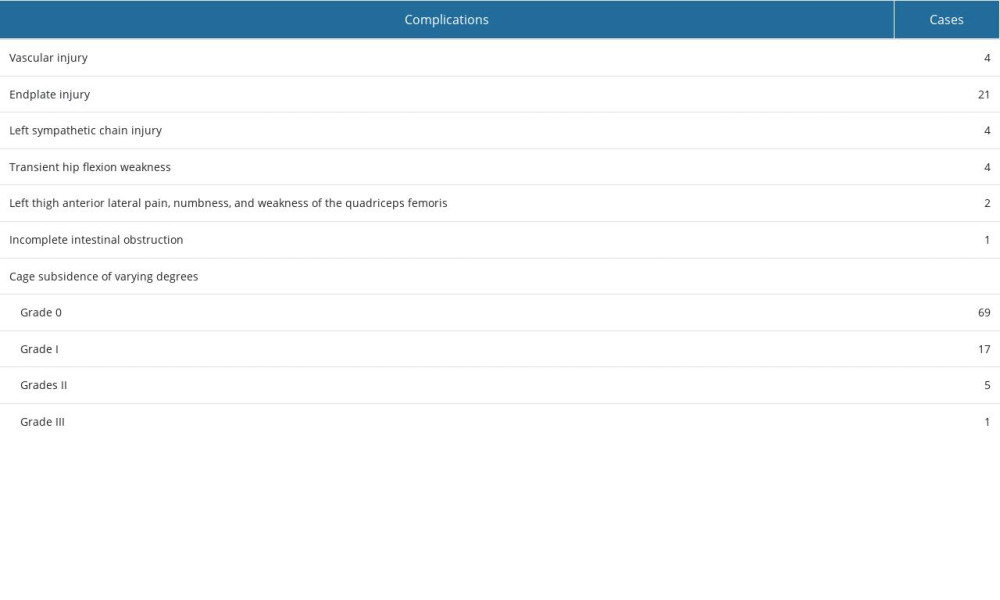
Figure 1. A 63-year-old male patient with diagnosis(A) Lumbar 3/4, lumbar 4/5 intervertebral disc degeneration. (B) Translateral oblique lateral lumbar 3/4, lumbar 4/5 interbody fusion. (C) Postoperative lumbar spine X-ray front and side radiographs. (D) Postoperative 26 months; the lumbar CT plain scan and coronal and sagittal reconstruction. 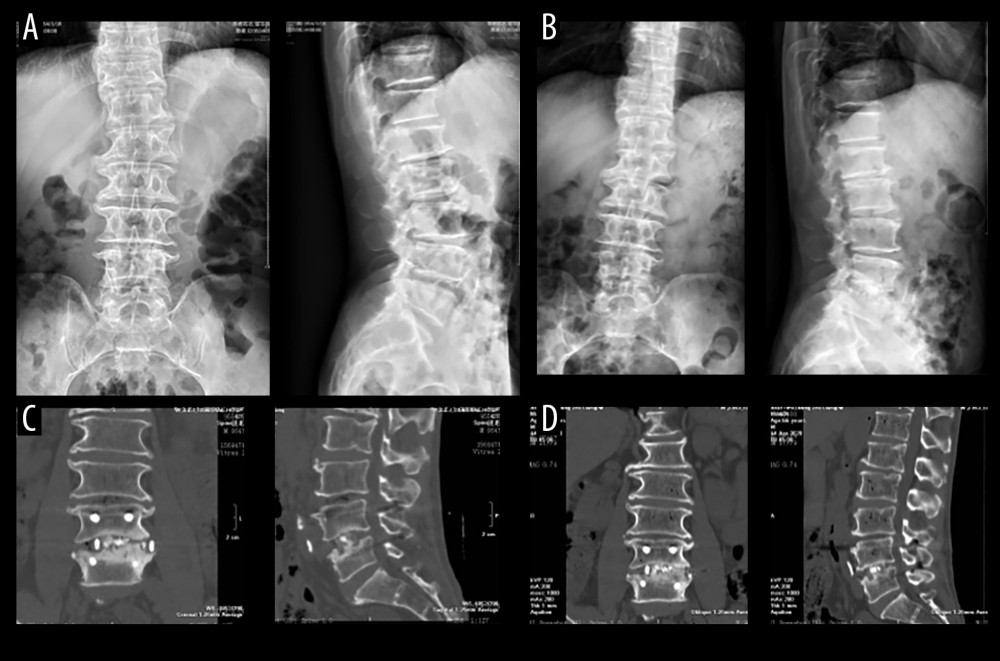 Figure 2. A 63-year-old male patient with diagnosis(A) The X-ray front and side view of the lumbar spine before operation. (B) At 1 month after the operation, the lumbar spine X-ray front and side radiographs. (C) Lumbar spine CT scan and coronary scan 1 year after reconstruction of the facial and sagittal planes. (D) CT plain scan of the lumbar spine 2.5 years after surgery and reconstruction of the coronal and sagittal planes.
Figure 2. A 63-year-old male patient with diagnosis(A) The X-ray front and side view of the lumbar spine before operation. (B) At 1 month after the operation, the lumbar spine X-ray front and side radiographs. (C) Lumbar spine CT scan and coronary scan 1 year after reconstruction of the facial and sagittal planes. (D) CT plain scan of the lumbar spine 2.5 years after surgery and reconstruction of the coronal and sagittal planes.  Figure 3. A 51-year-old female patient with diagnosis(A) Preoperative lumbar spine X-ray front and lateral view. (B) Postoperative lumbar CT plain scan and sagittal reconstruction. (C) At 2 years and 10 months after surgery, lumbar spine X-ray front and side view.
Figure 3. A 51-year-old female patient with diagnosis(A) Preoperative lumbar spine X-ray front and lateral view. (B) Postoperative lumbar CT plain scan and sagittal reconstruction. (C) At 2 years and 10 months after surgery, lumbar spine X-ray front and side view.  Figure 4. A 61-year-old female patient with diagnosis(A) Preoperative lumbar X-ray positive and lateral radiographs. (B) At 2 years and 8 months after surgery, lumbar spine X-ray hyperflexion and extension lateral view. (C) Two years after surgery, lumbar CT plain scan and reconstruction of the coronal and sagittal planes. (D) Lumbar CT plain scan at 2 years and 8 months after surgery.
Figure 4. A 61-year-old female patient with diagnosis(A) Preoperative lumbar X-ray positive and lateral radiographs. (B) At 2 years and 8 months after surgery, lumbar spine X-ray hyperflexion and extension lateral view. (C) Two years after surgery, lumbar CT plain scan and reconstruction of the coronal and sagittal planes. (D) Lumbar CT plain scan at 2 years and 8 months after surgery. References
1. Park SC, Chang SY, Mok S, Risk factors for postoperative ileus after oblique lateral interbody fusion: A multivariate analysis: Spine J, 2021; 21(3); 438-45
2. Zhao R, Huo Y, Yeo T, Application of stand-alone oblique lateral interbody fusion in L4-5 lumbar diseases: J Vis Exp, 2023(195); 65351
3. Xu DS, Walker CT, Godzik J, Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: A literature review: Ann Transl Med, 2018; 6(6); 104
4. Zhao L, Hou W, Shi H, Risk factors for postoperative sympathetic chain dysfunction following oblique lateral lumbar interbody fusion: A multivariate analysis: Eur Spine J, 2023; 32(7); 2319-25
5. Zhang X, Wang Y, Zhang W, Perioperative clinical features and long-term prognosis after oblique lateral interbody fusion (OLIF), OLIF with anterolateral screw fixation, or OLIF with percutaneous pedicle fixation: A comprehensive treatment strategy for patients with lumbar degenerative disease: Neurospine, 2023; 20(2); 536-49
6. Ricciardi L, Piazza A, Capobianco M, Lumbar interbody fusion using oblique (OLIF) and lateral (LLIF) approaches for degenerative spine disorders: A meta-analysis of the comparative studies: Eur J Orthop Surg Traumatol, 2023; 33(1); 1-7
7. Razzouk J, Ramos O, Mehta S, CT-based analysis of oblique lateral interbody fusion from L1 to L5: Location of incision, feasibility of safe corridor approach, and influencing factors: Eur Spine J, 2023; 32(6); 1947-52
8. Qiu MG, Zhou SG, Lin SS, Early effect of standalone oblique lateral interbody fusion vs. combined with lateral screw fixation of the vertebral body on single-level lumbar degenerative disc disease: A pilot study: J Back Musculoskelet Rehabil, 2023; 36(3); 709-19
9. Hu B, Wu T, Zhao Y, Physiological signatures of dual embryonic origins in mouse skull vault: Cell Physiol Biochem, 2017; 43(6); 2525-34
10. Zhang X, Shi G, Sun X, Factors influencing the outcomes of artificial hip replacements: Cells Tissues Organs, 2018; 206(4–5); 254-62
11. Chen G, Yao Y, Xu G, Zhang X, Regional difference in microRNA regulation in the skull vault: Dev Dyn, 2019; 248(10); 1009-19
12. Chen G, Xu H, Yao Y, BMP signaling in the development and regeneration of cranium bones and maintenance of calvarial stem cells: Front Cell Dev Biol, 2020; 8; 135
13. Chen G, Ishan M, Yang J, Specific and spatial labeling of P0-Cre versus Wnt1-Cre in cranial neural crest in early mouse embryos: Genesis, 2017; 55(6); dvg.23034
14. Chen G, Deng C, Li YP, TGF-beta and BMP signaling in osteoblast differentiation and bone formation: Int J Biol Sci, 2012; 8(2); 272-88
15. Wu T, Chen G, Tian F, Liu HX, Contribution of cranial neural crest cells to mouse skull development: Int J Dev Biol, 2017; 61(8–9); 495-503
16. Maruyama T, Stem cells of the suture mesenchyme in craniofacial bone development, repair and regeneration: Keio J Med, 2019; 68(2); 42
17. Wilk K, Yeh SA, Mortensen LJ, Postnatal calvarial skeletal stem cells expressing PRX1 reside exclusively in the calvarial sutures and are required for bone regeneration: Stem Cell Reports, 2017; 8(4); 933-46
18. Vlashi R, Zhang X, Wu M, Chen G, Wnt signaling: Essential roles in osteoblast differentiation, bone metabolism and therapeutic implications for bone and skeletal disorders: Genes Dis, 2023; 10(4); 1291-317
19. Juma SN, Liao J, Huang Y, Osteoarthritis versus psoriasis arthritis: Physiopathology, cellular signaling, and therapeutic strategies: Genes & Diseases, 2023 [in Press]
20. Huang Y, Liao J, Vlashi R, Chen G, Focal adhesion kinase (FAK): Its structure, characteristics, and signaling in skeletal system: Cell Signal, 2023 [Online ahead of print]
21. Woods KR, Billys JB, Hynes RA, Technical description of oblique lateral interbody fusion at L1–L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates: Spine J, 2017; 17(4); 545-53
22. Zhang X, Shi G, Sun X, Factors influencing the outcomes of artificial hip replacements: Cells Tissues Organs, 2018; 206(4–5); 254-62
23. Pan Q, Yu H, He X, Lumbar sympathetic trunk injury: An underestimated complication of oblique lateral interbody fusion: Orthop Surg, 2023; 15(4); 1053-59
24. Lee KH, Son DW, Oh BK, Incidental ureteral complication in single-center consecutive oblique lateral interbody fusion cases: Turk Neurosurg, 2023 [Online ahead of print]
25. Ohtori S, Mannoji C, Orita S, Mini-open anterior retroperitoneal lumbar interbody fusion: Oblique lateral interbody fusion for degenerated lumbar spinal kyphoscoliosis: Asian Spine J, 2015; 9(4); 565-72
26. Zhu L, Wang JW, Zhang L, Feng XM, Outcomes of oblique lateral interbody fusion for adult spinal deformity: A systematic review and meta-analysis: Global Spine J, 2022; 12(1); 142-54
27. Wang W, Xiao B, Wang H, Oblique lateral interbody fusion stand-alone vs. combined with percutaneous pedicle screw fixation in the treatment of discogenic low back pain: Front Surg, 2022; 9; 1013431
28. Lee JS, Son DW, Lee SH, Surgical outcome of minimal invasive oblique lateral interbody fusion with percutaneous pedicle screw fixation in the treatment of adult degenerative scoliosis: Medicine (Baltimore), 2022; 101(48); e31879
29. Wang K, Zhang C, Cheng C, Radiographic and clinical outcomes following combined oblique lumbar interbody fusion and lateral instrumentation for the treatment of degenerative spine deformity: A preliminary retrospective study: Biomed Res Int, 2019; 2019; 5672162
30. He W, He D, Sun Y, Quantitative analysis of paraspinal muscle atrophy after oblique lateral interbody fusion alone vs. combined with percutaneous pedicle screw fixation in patients with spondylolisthesis: BMC Musculoskelet Disord, 2020; 21(1); 30
31. Wakita H, Shiga Y, Ohtori S, Less invasive corrective surgery using oblique lateral interbody fusion (OLIF) including L5-S1 fusion for severe lumbar kyphoscoliosis due to L4 compression fracture in a patient with Parkinson’s disease: A case report: BMC Res Notes, 2015; 8; 126
32. Hu S, Chen S, Zeng H, Ap-2beta regulates cranial osteogenic potential via the activation of Wnt/beta-catenin signaling pathway: Dev Biol, 2023; 501; 81-91
33. Kim H, Chang BS, Chang SY, Pearls and pitfalls of oblique lateral interbody fusion: A comprehensive narrative review: Neurospine, 2022; 19(1); 163-76
34. Zhang YW, Xiong LY, Huang ZT, Deng L, WITHDRAWN: Minimally invasive treatment of lumbar tuberculosis via the oblique lateral interbody fusion combined with posterior percutaneous screws placement: Asian J Surg, 2020 [Online ahead of print]
35. Liao J, Huang Y, Wang Q, Gene regulatory network from cranial neural crest cells to osteoblast differentiation and calvarial bone development: Cell Mol Life Sci, 2022; 79(3); 158
36. Iwasaki M, Hayase H, Takamiya S, Yamazaki K, Preoperative dorsal disc height is a predictor of indirect decompression effect through oblique lateral interbody fusion in lumbar degenerative stenosis: Medicine (Baltimore), 2022; 101(41); e31020
37. Park SW, Ko MJ, Kim YB, Le Huec JC, Correction of marked sagittal deformity with circumferential minimally invasive surgery using oblique lateral interbody fusion in adult spinal deformity: J Orthop Surg Res, 2020; 15(1); 13
38. Juma SN, Gong X, Hu S, Shark new antigen receptor (IgNAR): Structure, characteristics and potential biomedical applications: Cells, 2021; 10(5); 1140
39. Abbasi H, Storlie NR, Aya KL, Transfacet oblique lateral lumbar interbody fusion: Technical description and early results: Cureus, 2022; 14(7); e26533
40. Xie T, Wang C, Yang Z, Minimally invasive oblique lateral lumbar interbody fusion combined with anterolateral screw fixation for lumbar degenerative disc disease: World Neurosurg, 2020; 135; e671-e78
41. Wu T, Xiao L, Liu C, Anatomical study of the lumbar segmental arteries in relation to the oblique lateral interbody fusion approach: World Neurosurg, 2020; 138; e778-e86
42. Shimizu T, Fujibayashi S, Otsuki B, Indirect decompression through oblique lateral interbody fusion for revision surgery after lumbar decompression: World Neurosurg, 2020; 141; e389-e99
43. Robertson SC, Shaikh Y, Sharif S, Perspective on variation in lumbar segmental arteries and their importance on oblique lateral interbody fusion: World Neurosurg, 2020; 139; 453-55
44. Chen GQ, Hu XF, Sugahara K: J Zhejiang Univ Sci B, 2007; 8(11); 839-44
45. Manzur MK, Steinhaus ME, Virk SS, Fusion rate for stand-alone lateral lumbar interbody fusion: A systematic review: Spine J, 2020; 20(11); 1816-25
46. Shimizu T, Fujibayashi S, Otsuki B, Indirect decompression via oblique lateral interbody fusion for severe degenerative lumbar spinal stenosis: A comparative study with direct decompression transforaminal/posterior lumbar interbody fusion: Spine J, 2021; 21(6); 963-71
47. Park SC, Chang SY, Mok S, Risk factors for postoperative ileus after oblique lateral interbody fusion: A multivariate analysis: Spine J, 2021; 21(3); 438-45
48. Ng JP, Kaliya-Perumal AK, Tandon AA, Oh JY, The oblique corridor at L4-L5: A radiographic-anatomical study into the feasibility for lateral interbody fusion: Spine (Phila Pa 1976), 2020; 45(10); E552-E59
49. Liu M, Hu Y, Chen G, The antitumor effect of gene-engineered exosomes in the treatment of brain metastasis of breast cancer: Front Oncol, 2020; 10; 1453
50. Oh BK, Son DW, Lee SH, Learning curve and complications experience of oblique lateral interbody fusion: A single-center 143 consecutive cases: J Korean Neurosurg Soc, 2021; 64(3); 447-59
51. Liu J, Feng H, Oblique lateral interbody fusion (OLIF) with supplemental anterolateral screw and rod instrumentation: A preliminary clinical study: World Neurosurg, 2020; 134; e944-e50
52. Inoue M, Orita S, Inage K, Radiological assessment of damage to the iliopsoas muscle by the oblique lateral interbody fusion approach: Spine Surg Relat Res, 2020; 4(2); 152-58
53. Feng S, Tian W, Wei Y, Clinical effects of oblique lateral interbody fusion by conventional open versus percutaneous robot-assisted minimally invasive pedicle screw placement in elderly patients: Orthop Surg, 2020; 12(1); 86-93
54. Masuda S, Fujibayashi S, Kimura H, Salvage oblique lateral interbody fusion for pseudarthrosis after posterior/transforaminal lumbar interbody fusion: A technical note: World Neurosurg, 2021; 152; 107-12
Figures
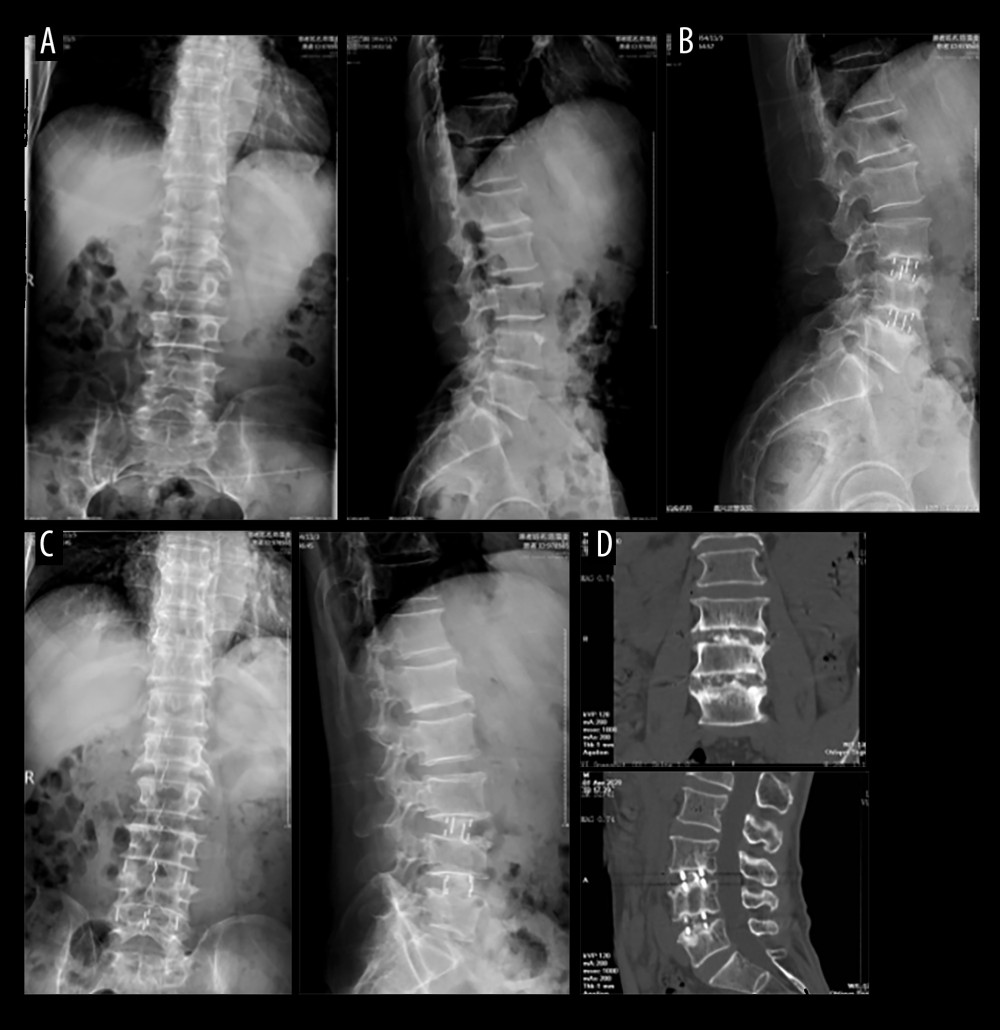 Figure 1. A 63-year-old male patient with diagnosis(A) Lumbar 3/4, lumbar 4/5 intervertebral disc degeneration. (B) Translateral oblique lateral lumbar 3/4, lumbar 4/5 interbody fusion. (C) Postoperative lumbar spine X-ray front and side radiographs. (D) Postoperative 26 months; the lumbar CT plain scan and coronal and sagittal reconstruction.
Figure 1. A 63-year-old male patient with diagnosis(A) Lumbar 3/4, lumbar 4/5 intervertebral disc degeneration. (B) Translateral oblique lateral lumbar 3/4, lumbar 4/5 interbody fusion. (C) Postoperative lumbar spine X-ray front and side radiographs. (D) Postoperative 26 months; the lumbar CT plain scan and coronal and sagittal reconstruction.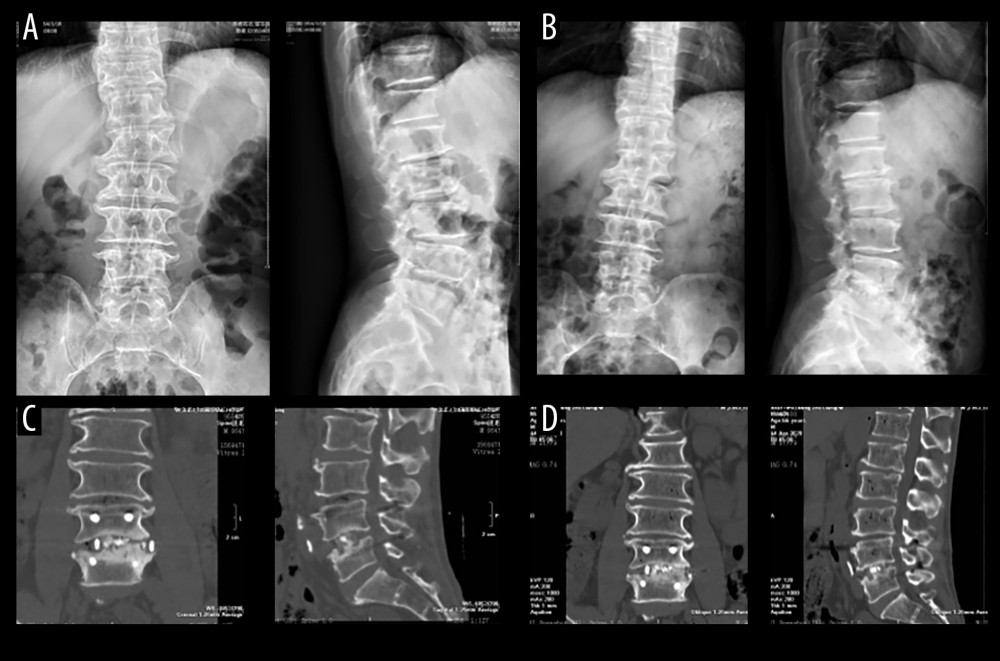 Figure 2. A 63-year-old male patient with diagnosis(A) The X-ray front and side view of the lumbar spine before operation. (B) At 1 month after the operation, the lumbar spine X-ray front and side radiographs. (C) Lumbar spine CT scan and coronary scan 1 year after reconstruction of the facial and sagittal planes. (D) CT plain scan of the lumbar spine 2.5 years after surgery and reconstruction of the coronal and sagittal planes.
Figure 2. A 63-year-old male patient with diagnosis(A) The X-ray front and side view of the lumbar spine before operation. (B) At 1 month after the operation, the lumbar spine X-ray front and side radiographs. (C) Lumbar spine CT scan and coronary scan 1 year after reconstruction of the facial and sagittal planes. (D) CT plain scan of the lumbar spine 2.5 years after surgery and reconstruction of the coronal and sagittal planes. Figure 3. A 51-year-old female patient with diagnosis(A) Preoperative lumbar spine X-ray front and lateral view. (B) Postoperative lumbar CT plain scan and sagittal reconstruction. (C) At 2 years and 10 months after surgery, lumbar spine X-ray front and side view.
Figure 3. A 51-year-old female patient with diagnosis(A) Preoperative lumbar spine X-ray front and lateral view. (B) Postoperative lumbar CT plain scan and sagittal reconstruction. (C) At 2 years and 10 months after surgery, lumbar spine X-ray front and side view. Figure 4. A 61-year-old female patient with diagnosis(A) Preoperative lumbar X-ray positive and lateral radiographs. (B) At 2 years and 8 months after surgery, lumbar spine X-ray hyperflexion and extension lateral view. (C) Two years after surgery, lumbar CT plain scan and reconstruction of the coronal and sagittal planes. (D) Lumbar CT plain scan at 2 years and 8 months after surgery.
Figure 4. A 61-year-old female patient with diagnosis(A) Preoperative lumbar X-ray positive and lateral radiographs. (B) At 2 years and 8 months after surgery, lumbar spine X-ray hyperflexion and extension lateral view. (C) Two years after surgery, lumbar CT plain scan and reconstruction of the coronal and sagittal planes. (D) Lumbar CT plain scan at 2 years and 8 months after surgery. In Press
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952