28 July 2023: Clinical Research
Emergency Response and Clinical Insights from a Non-Epicenter Hospital during the 2023 Turkey-Syria Earthquake: A Retrospective Analysis
Selahattin Gürü1ABCDEF*, Süeda Zaman2ABCEF, Mehmet Akif Karamercan3AEFDOI: 10.12659/MSM.941226
Med Sci Monit 2023; 29:e941226
Abstract
BACKGROUND: The Turkey-Syria earthquake of February 6, 2023, impacted 11 provinces and necessitated widespread emergency medical support. Although not at the disaster’s epicenter, Ankara Mamak State Hospital in Ankara, Turkey, offered critical multidisciplinary support. This retrospective study evaluates the factors that drove 124 admissions to the hospital’s Emergency Department (ED) following the earthquake.
MATERIAL AND METHODS: We recorded patient demographic data, dates of arrival at the ED, provinces of origin, diagnoses, treatments, consultations during the ED visit, and patient outcomes. The majority of the 124 admissions were due to trauma and multi-organ damage, and the primary diagnostic tools were physical examination and radiological imaging. Of these patients, 85.5% (106) recovered and were discharged directly from the ED, 11 were admitted for continued care, and 7 were referred to another hospital.
RESULTS: The 124 cases consisted of adults injured within the first 20 days post-earthquake, with a mean age of 46.5±17.4 years, and a higher number of females. A peak in admissions was observed on the third and fourth days following the earthquake, with the most cases originating from the Hatay province. The most frequently injured body region was the lower extremity, and orthopedic consultations significantly outnumbered other surgical consultations.
CONCLUSIONS: Our findings underscore the vital role of robust, multidisciplinary disaster preparedness in all EDs, especially in regions prone to natural disasters.
Keywords: Disaster Planning, Disaster Victims, Emergency Medicine, Earthquakes, Crush Injuries, Adult, Female, Humans, Middle Aged, Emergency Service, Hospital, Hospitals, Retrospective Studies, Syria, Turkey, Male
Background
Earthquakes, which are natural disasters, cause life-threatening injuries in short periods of time [1]. Turkey is a world earthquake zone, located on many active faults [2]. On February 6, 2023, the south and southeast regions of the country were affected by 2 massive earthquakes with moment magnitudes (Mw) of 7.8 and 7.5, which had 2 different epicenters (37.05°E 37.23°N and 37.23°E 38.11°N) close to each other [3–5]. The earthquake was followed approximately 9 h later by a 7.5-Mw event and more than 200 aftershocks. The earthquake and aftershocks flattened buildings and sent rescuers to dig through the concrete rubble to find survivors [6]. These 2 consecutive earthquakes affected 9.1 million people in 11 provinces and caused 44 000 deaths and 108 000 injuries. After this disaster, 2.2 million people were displaced among the affected population [7]. These earthquakes were felt in a very large area, especially in Turkey, Syria, Lebanon, and Cyprus, up to a distance of 2000 km from the epicenters [3]. A total of 4500 deaths and 8700 injuries were also reported in neighboring Syria [8]. Earthquakes caused temporary disruptions in the healthcare system of Turkey. Some hospitals and emergency response systems were also damaged. Healthcare workers had to work long and tiring shifts [9]. In the early days of the disaster, 74 000 healthcare workers struggled to treat many injuries and practice disaster medicine. Temporary hospitals were built, with tents in outdoor areas [10]. A large number of patients were transferred to hospitals in provinces outside the disaster area by highways, airlines, and maritime lines [11]. Therefore, this retrospective study aimed to report the causes of 124 admissions to the Emergency Department (ED) of Ankara Mamak State Hospital, Ankara, Turkey, following the February 2023 Turkey-Syria earthquake.
Material and Methods
STUDY DESIGN AND ETHICS:
Approval for the study was obtained from the local clinical research ethics committee with the number 2023/282. A signed informed consent form was obtained from the participants. After this approval, adult victims presented to ED on the first 20 days of massive earthquakes were scanned from the database of the hospital retrospectively.
DATA COLLECTION:
Data about the patients’ age, sex, days presented after disaster, provinces they came from, hemodynamic parameters (stable or not), injury types (penetrating or blunt), body zones injured, diagnoses in ED, treatments in ED, results of ED visit, duration of hours in ED, and consultations, if any, were recorded. Exclusion criteria were patients younger than 18 years old, patients with missing data, and patients with injuries not related with the earthquakes.
STATISTICAL ANALYSES:
Statistical analyses were conducted using SPSS 24.0 (Statistical Package for the Social Sciences; IBM Corp, Armonk, NY, USA) program. Descriptive statistics are presented as mean±standard deviation (minimum–maximum), frequency distribution, and percentage.
Results
DEMOGRAPHIC CHARACTERISTICS OF VICTIMS:
The mean age of patients was 46.5±17.4 years (min: 18, max: 98); 75 (60.5%) were female and 49 (39.5%) were male patients. Patients arrived to our ED from 6 different provinces in the disaster area. These provinces are very far from Ankara. The average distance between the centers of these 6 provinces and our ED is 715 km (min: 557, max: 827). Among them, according to the number of cases, Hatay had a higher percentage, with 45.1% (n=56; Figure 1).
CLINICAL RESULTS:
The hemodynamic parameters of all patients were stable. In addition to 13 (10.5%) of patients with penetrating trauma, 113 (91.1%) of them had blunt trauma, and 2 patients had both. There were 52 lower extremity injuries (41.9%) and 28 upper extremity injuries (22.6%) at most, among the affected body zones. Soft tissue injuries (n=74) were the most common diagnoses, and wound dressing (n=75) was the most common treatment in the ED. A total of 106 of patients were discharged from the ED (85.5%) with recovery. None of them died in the ED. The mean of duration of stay in the ED was 2.6±1.4 h (min: 1, max: 7). Body zones injured, diagnoses, treatments, and results of ED visit are presented in Table 2.
Consultations to surgeons was requested from the ED staff 22 times for all patients included in this study. Of them, 12 cases were consultations to the Orthopedics Department and 6 cases were to the Neurosurgery Department (Figure 2).
Discussion
In this study, we evaluated 124 cases of adult patients injured in the first 20 days after the earthquakes. The mean patient age was 46.5±17.4 years, and there were more female than male patients. The number of cases peaked on the third and fourth days after the earthquake. In the last decade, 2.6 billion people worldwide have been affected by natural disasters. Many injuries have occurred as a result of this exposure. These injuries lead to an excessive workload, which makes it difficult to provide a comprehensive and effective healthcare system [12]. While disasters are a precursor of the workload of local healthcare providers, they can actually exceed the emergency care capacity of local organizations and institutions due to their size [13]. Therefore, the healthcare providers far from the disaster area can also experience difficulties because of this increased workload. The goal of this study was to describe and examine the increased workload in an ED very far from the disaster area.
When the arrival dates of the 124 patients were examined, we found there were almost no cases of arrival to the ED in the first 2 days of the earthquakes, and the number of cases peaked on the third and fourth days. In a previous review examining the effects of the 2015 Nepal earthquake at hospitals, Moitinho de Almeida et al mentioned that the peak admission day after the earthquake is the fifth day [14]. Our result on the peak day is similar to the conclusion reported by this review. Çağıran et al reported the arrival time peaks of the 2020 Aegean Sea earthquake victims to their hospitals near the disaster area within the first 12 h. In addition, they found that the time of admission was significantly earlier in their mortal cases [1]. Since there were no mortal cases in this study, a result in this sense cannot be reported. However, unlike that study, the fact that almost no patients arrived in this study in the first 2 days may have been due to the high distance from the disaster area.
In the present study, the mean age of patients was 46.5±17.4 years (min: 18, max: 98), and 75 (60.5%) were women and 49 (39.5%) were men. In their study, Uz et al reported 313 earthquake victims in their emergency services, with a mean age of 38.0 years and the same percentage of women as the present study, 60.4% [15]. Çağıran et al found the mean age to be 38.13 years and the percentage of female patients to be 60.5% in their study [1]. Both studies include data on victims of the 2020 Aegean Sea earthquake in local hospitals in Turkey. Ergen et al reported the average age of the patients from the 2020 Elazığ earthquake in Turkey was 37.3 years, and they reported more male patients, at 55.88% [12]. When discussed together with the results of those studies reporting the victims of earthquakes in the same country with similar demographic structures, it can be predicted that the different mean age data in the present study may be due to the exclusion of children. Although the percentage of female patients was higher in this study and in some studies above, it is not thought that it has a significant medical outcome. A total of 11 provinces were affected by the massive February 2023 earthquakes [7]. In this study, when the cases were examined according to the provinces they came from, it was determined that cases came to the ED from 6 of these 11 provinces. Hatay was dominant among these 6 provinces. With potential future data to be published on patient referrals and human migrations after these earthquakes in Turkey, this data about Hatay may also become meaningful and valuable.
In their review, MacKenzie et al reported that extremity injuries as the affected body area due to earthquakes were significantly higher, at 87%. They also reported that lower extremity injuries were more common, with 59% among extremity injuries [16]. In their review of 147 reports on earthquake injuries over a 30-year period, Missair et al reported that extremity injuries were leading, with a range of 29% to 98%. According to this review, lower extremity injuries were more common than upper extremity injuries [17]. Ergen et al classified the fractures in the cases they examined after the 2020 Aegean Sea earthquake according to body region and found the percentage of lower extremity fractures to be 56.07% and the percentage of upper extremity fractures to be 33.64% [2]. In the data of the present study, among all injuries, according to the affected body zone injured, the percentage of lower extremity injuries was higher, at 41.9%, and that of upper extremity injuries was lower, at 22.6%. In this study, in which we reported the data of a hospital far from the disaster area, the lower extremity dominance was similar to that found in the literature. The present study and many reports in the literature show that the rate of lower extremity injuries is significantly higher in earthquakes. In this study, the main diagnosis in the ED was soft tissue injury. There were no cases of mortality. In an ED far from the disaster area, where the number of cases seen was very low in the first 2 days, it can be expected that injuries related to earthquakes will be moderate and mortality will remain low. In their study, Uz et al reported that soft tissue injuries were the leading diagnosis in ED cases in the disaster area [15]. However, mortality was not zero in studies designed in hospitals in disaster areas, such as those of Uz et al and Çağıran et al [1,15]. It seems reasonable that acute mortal cases were seen in hospitals located in the disaster area where the data of these studies were collected. The low mortality in the present study can be explained by the fact that patients with milder cases arrived to distant hospitals by their own efforts, and more mortal cases to local hospitals, without wasting time. When more comprehensive data has been published, this possibility can be discussed in the future.
The duration of stay in the ED of the patients in this study was 2.6±1.4 h. Most of the patients were treated in the ED and discharged. A large part of the treatment in the ED was wound dressing. In the report of Uz et al, the duration of the earthquake victims’ stay in the ED was reported as 1.84±3.04 h. In the present report, most of the patients were discharged after being treated in the ED. Both this study and the report of Uz et al, which is about an ED in the earthquake area, show that most of the patients after the earthquake were treated in the ED and discharged within a few hours. After disasters, changes can be observed in the tendency of patients to apply to emergency services and hospitals, and to be hospitalized. A decrease was observed in the number of hospital admission s and emergency service admissions [18]. In another study, it was shown that after the earthquake, especially in the acute and subacute period, the number of applications due to injury to the emergency services increased, the applications related to pregnancy continued, and the maternity care services should continue [19].
Moitinho et al and Bortolin et al reported significantly over-reported orthopedic interventions in earthquake injuries that underwent a surgical procedure [14,20]. Ergen et al also revealed the dominance of orthopedic interventions in ED earthquake victims [2]. When the 22 consultations made in the present study were evaluated, it was shown that most of the cases were referred to orthopedists. These results are quite consistent, considering that mostly extremity injuries occur in earthquakes.
This study had some limitations. Since the hospital where the data were collected is far from the disaster area, no inference can be made about earthquake-related mortality. It can be considered as a limitation that the psychiatric conditions of the patients were not evaluated while evaluating the physical examination and medical data. In addition, long-term medical follow-up of patients in different hospitals in the country can be considered as a methodological limitation. On the other hand, no mortality was observed in the data set. Therefore, the patients had a relatively better prognosis. Of course, different results can be obtained with more comprehensive studies evaluating the data of the hospitals in the disaster area together.
Conclusions
An extraordinary workload can occur in EDs far from the disaster area in cases of massive earthquakes. In the first days of the disaster, such EDs are not as crowded as the EDs in the disaster area. Injuries of earthquake victims in EDs far from the disaster area may be diagnosed more moderately and mortality may be lower. Similar to EDs in disaster areas, extremity injuries are more common in EDs far from disaster. After massive earthquakes, precautions should be taken in terms of the number of health workers, equipment, and physical conditions in EDs far from the disaster area. The findings from this study showed the importance of multidisciplinary emergency disaster preparedness in all EDs, particularly in countries where natural disasters occur.
Figures
 Figure 1. Number of cases according to the provinces they came from after the February 2023 Turkey-Syria earthquake to Emergency Department of Ankara Mamak State Hospital.
Figure 1. Number of cases according to the provinces they came from after the February 2023 Turkey-Syria earthquake to Emergency Department of Ankara Mamak State Hospital. 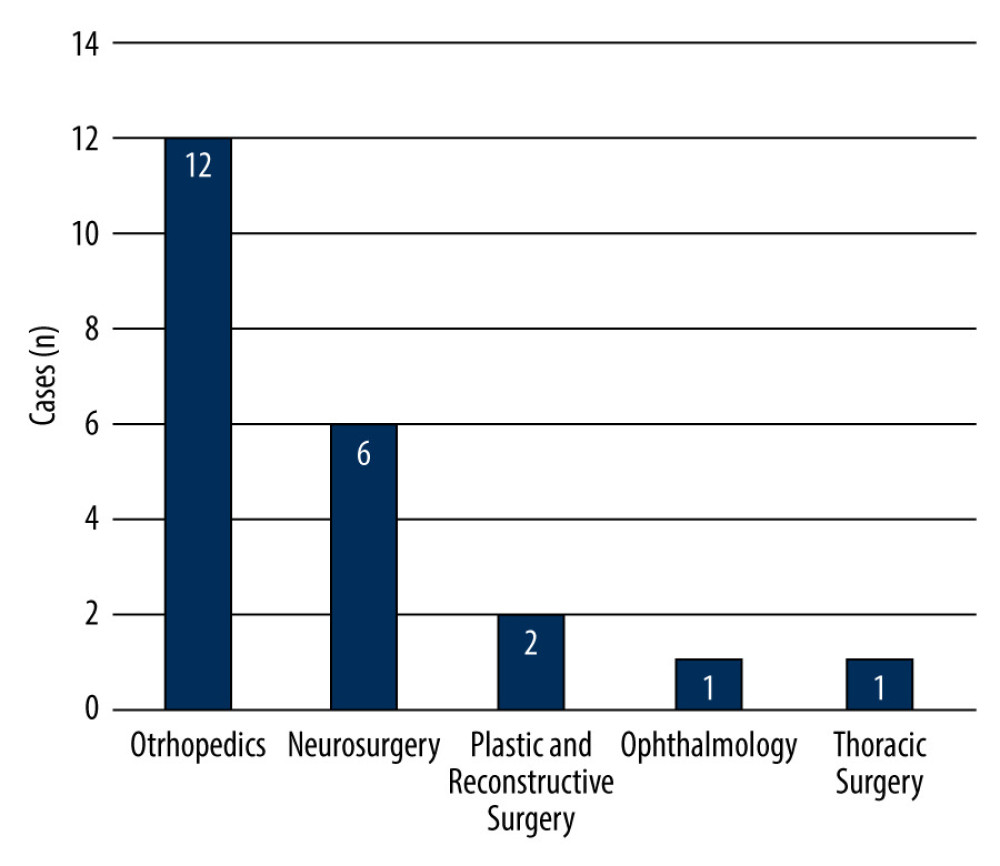 Figure 2. Distribution of surgical consultations requested from Emergency Department of Ankara Mamak State Hospital for patients admitted following the February 2023 Turkey-Syria earthquake.
Figure 2. Distribution of surgical consultations requested from Emergency Department of Ankara Mamak State Hospital for patients admitted following the February 2023 Turkey-Syria earthquake. Tables
Table 1. Number of victims presented to the Emergency Department of Ankara Mamak State Hospital by date, in the first 20 days after February 2023 Turkey-Syria Earthquake.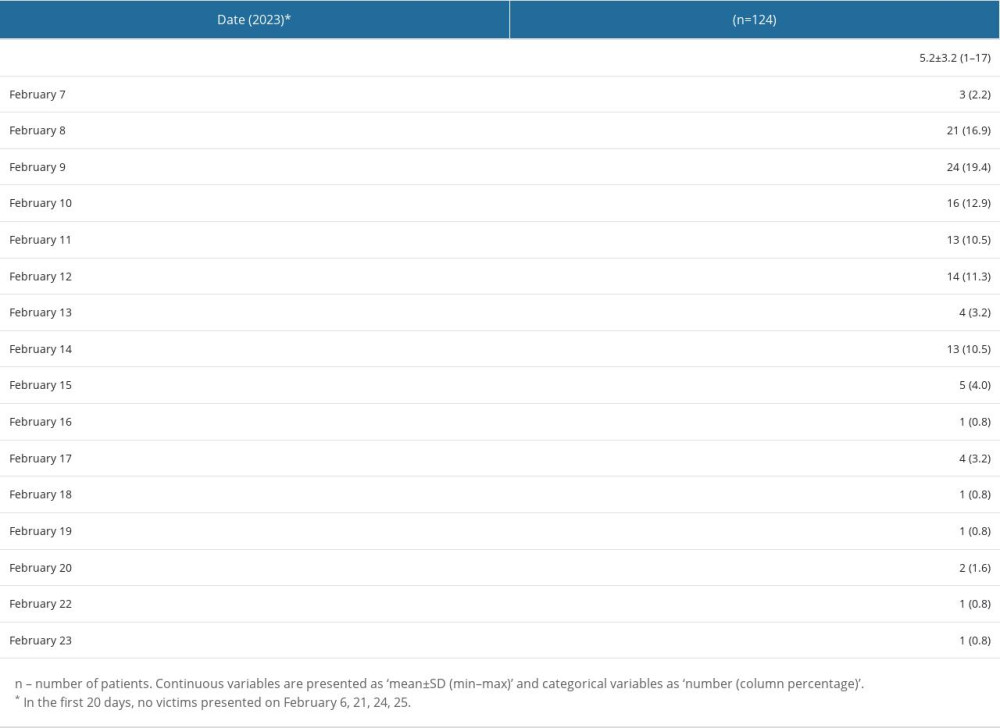 Table 2. Injury type, body zone injured, diagnosis, treatment, and result of Emergency Department visit of victims admitted to Ankara Mamak State Hospital following the February 2023 Turkey-Syria earthquake.
Table 2. Injury type, body zone injured, diagnosis, treatment, and result of Emergency Department visit of victims admitted to Ankara Mamak State Hospital following the February 2023 Turkey-Syria earthquake.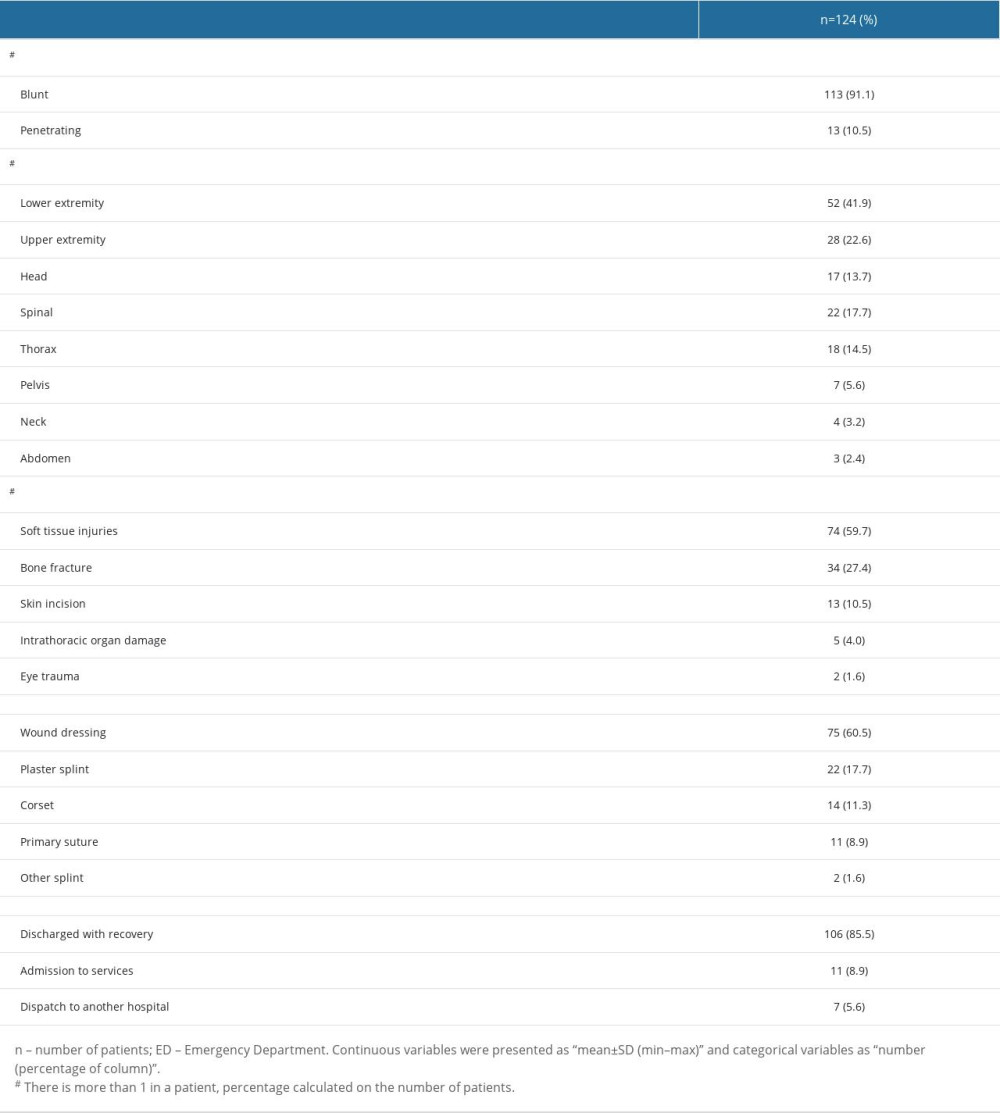
References
1. Çağıran Z, Sertöz N, Karaman S, Our clinical experiences in the earthquake victims who came to our university after the 2020 Aegean Sea earthquake during the COVID-19 pandemic: Ulus Travma Acil Cerrahi Derg, 2023; 29(3); 310-15
2. Ergen E, Kaya O, Yılmaz Ö, Which is more dangerous, earthquake, or the panic? Evaluation of the 24 January 2020 Elazig/Türkiye earthquake related musculoskeletal injuries: Ulus Travma Acil Cerrahi Derg, 2022; 28(9); 1335-39
3. Taymaz T, Ganas A, Melgar D: Earthquake sequence in Turkey February 6, 2023 Available from: https://www.emsc-csem.org/Earthquake/271/Earthquake-sequence-in-Turkey-February-6th-2023
4. : Events near Turkey-Syria border February, 2023 Available from: and http://geofon.gfz-potsdam.de/eqinfo/event.php?id=gfz2023cnwr
5. Yılmaz S, Karakayali O, Yilmaz S: Prehosp Disaster Med, 2023(1); 1-4
6. Naddaf M, Turkey-Syria earthquake: What scientists know: Nature, 2023; 614(7948); 398-99
7. World Health Organization: Turkey earthquake: External situation report no 2 February 20–26, 2023, World Health Organization Regional Office for Europe
8. : Earthquakes: North-west Syria Situation Report No 1 (As of 7 March 2023) Available from: https://reliefweb.int/report/syrian-arab-republic/earthquakes-north-west-syria-situation-report-no-1-7-march-2023
9. Uwishema O, Addressing the effects of the earthquakes on Türkiye’s health-care system: Lancet, 2023; 401(10378); 727
10. : Sağlık bakanı Koca, deprem bölgelerindeki sağlık hizmetlerine ilişkin son durumu paylaştı Available from: [in Turkish]https://www.saglik.gov.tr/TR,94838/saglik-bakani-koca-deprem-bolgelerindeki-saglik-hizmetlerine-iliskin-son-durumu-paylasti.html
11. : Bakan Koca, Deprem Bölgesinde Son Durumu Değerlendirdi Available from: [in Turkish]https://www.saglik.gov.tr/TR,94749/bakan-koca-deprem-bolgesinde-son-durumu-degerlendirdi.html
13. Klein TA, Irizarry L, EMS Disaster Response: StatPearls, 2023, Treasure Island (FL), StatPearls Publishing
14. Moitinho de Almeida M, “Recovering, not recovered” Hospital disaster resilience: A case-study from the 2015 earthquake in Nepal: Glob Health Action, 2022; 15(1); 2013597
15. Uz İ, Çetin M, Songur Kodik M, Emergency Department management after the 2020 Aegean Sea – Izmir earthquake: Ulus Travma Acil Cerrahi Derg, 2022; 28(3); 361-68
16. MacKenzie JS, Banskota B, Sirisreetreerux N, A review of the epidemiology and treatment of orthopaedic injuries after earthquakes in developing countries: World J Emerg Surg, 2017; 12; 9
17. Missair A, Pretto EA, Visan A, A matter of life or limb? A review of traumatic injury patterns and anesthesia techniques for disaster relief after major earthquakes: Anesth Analg, 2013; 117(4); 934-41
18. Schluter PJ, Hamilton GJ, Deely JM, Ardagh MW, Impact of integrated health system changes, accelerated due to an earthquake, on Emergency Department attendances and acute admissions: A Bayesian change-point analysis: BMJ Open, 2016; 6(5); e010709
19. Moitinho de Almeida M, Schlüter B-S, van Loenhout JAF, Changes in patient admissions after the 2015 Earthquake: A tertiary hospital-based study in Kathmandu, Nepal: Sci Rep, 2020; 10(1); 4956
20. Bortolin M, Morelli I, Voskanyan , Earthquake-related orthopedic injuries in adult population: A systematic review: Prehosp Disaster Med, 2017; 32(2); 201-8
Figures
 Figure 1. Number of cases according to the provinces they came from after the February 2023 Turkey-Syria earthquake to Emergency Department of Ankara Mamak State Hospital.
Figure 1. Number of cases according to the provinces they came from after the February 2023 Turkey-Syria earthquake to Emergency Department of Ankara Mamak State Hospital.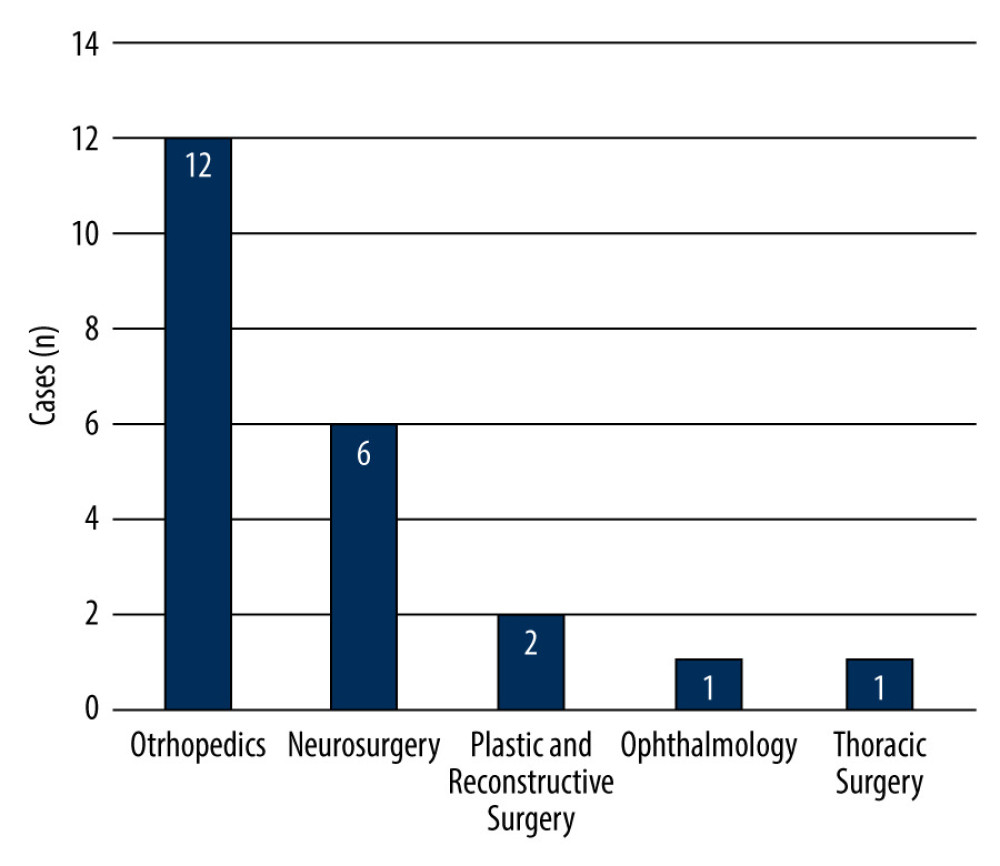 Figure 2. Distribution of surgical consultations requested from Emergency Department of Ankara Mamak State Hospital for patients admitted following the February 2023 Turkey-Syria earthquake.
Figure 2. Distribution of surgical consultations requested from Emergency Department of Ankara Mamak State Hospital for patients admitted following the February 2023 Turkey-Syria earthquake. Tables
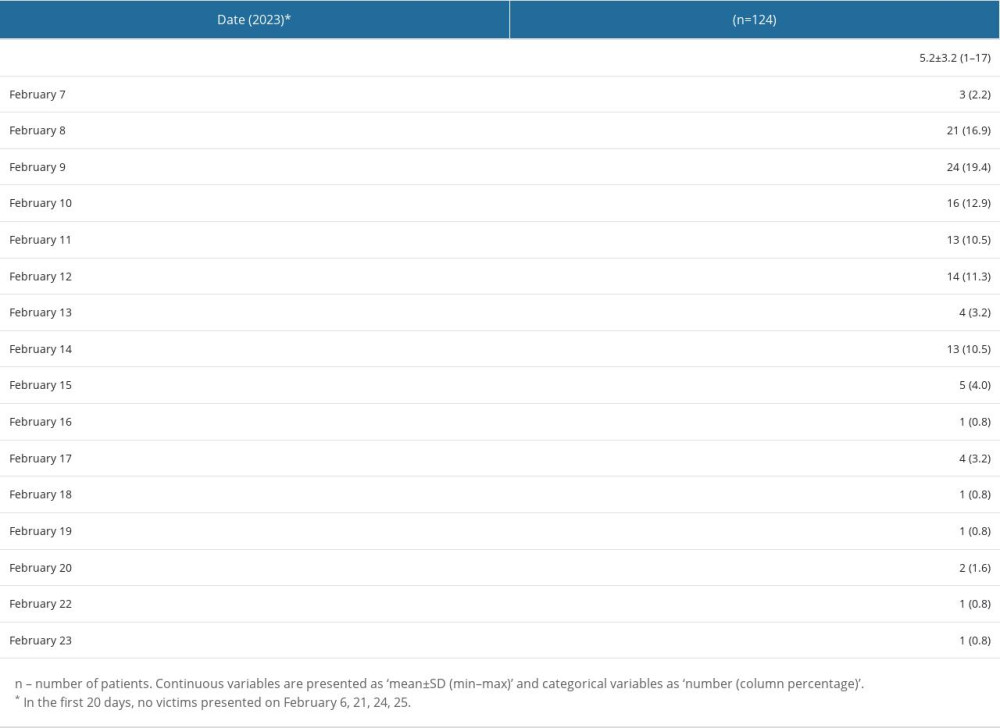 Table 1. Number of victims presented to the Emergency Department of Ankara Mamak State Hospital by date, in the first 20 days after February 2023 Turkey-Syria Earthquake.
Table 1. Number of victims presented to the Emergency Department of Ankara Mamak State Hospital by date, in the first 20 days after February 2023 Turkey-Syria Earthquake.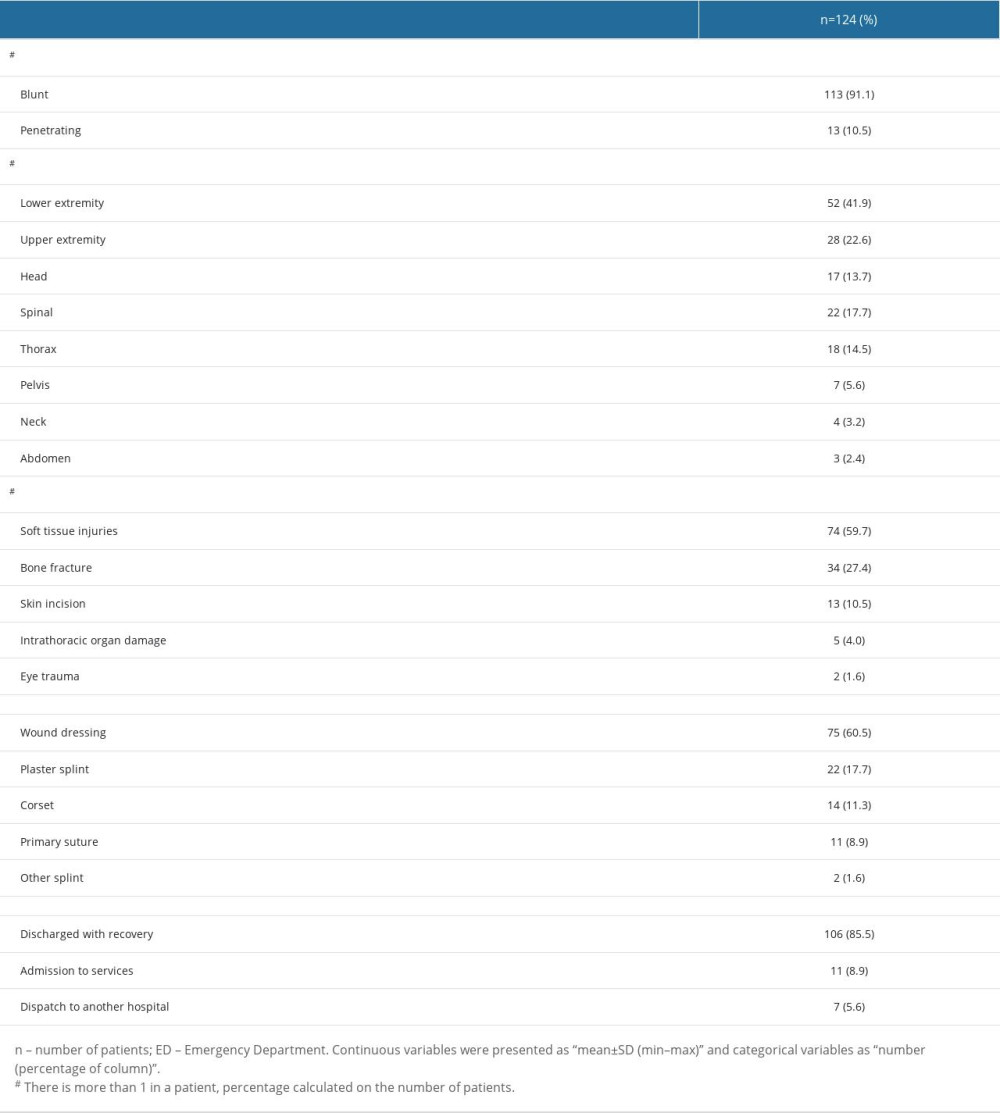 Table 2. Injury type, body zone injured, diagnosis, treatment, and result of Emergency Department visit of victims admitted to Ankara Mamak State Hospital following the February 2023 Turkey-Syria earthquake.
Table 2. Injury type, body zone injured, diagnosis, treatment, and result of Emergency Department visit of victims admitted to Ankara Mamak State Hospital following the February 2023 Turkey-Syria earthquake.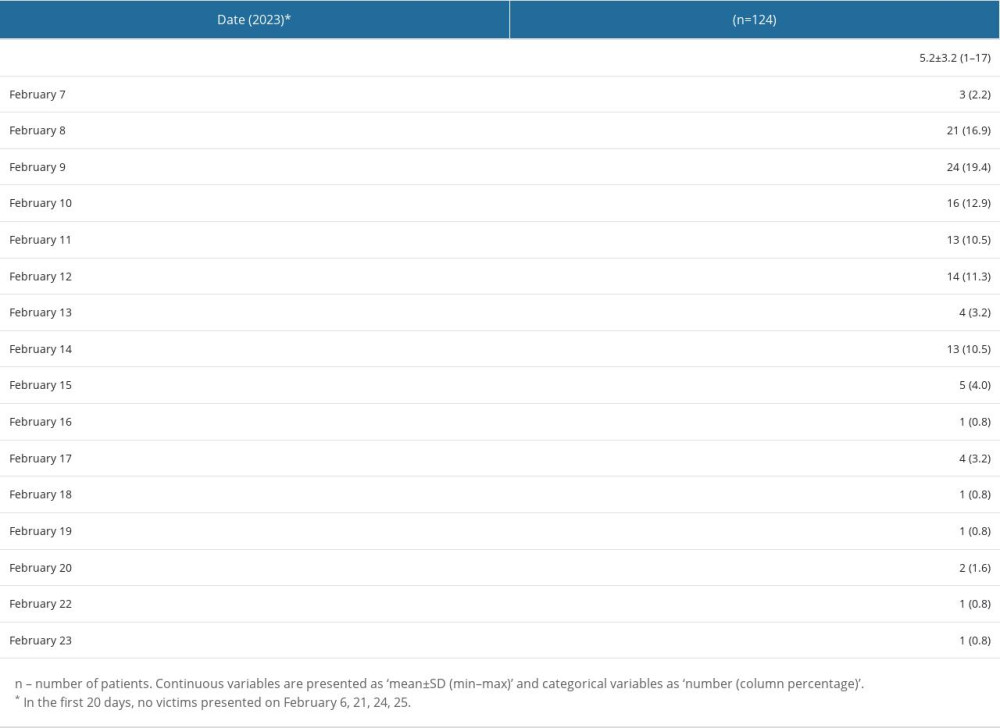 Table 1. Number of victims presented to the Emergency Department of Ankara Mamak State Hospital by date, in the first 20 days after February 2023 Turkey-Syria Earthquake.
Table 1. Number of victims presented to the Emergency Department of Ankara Mamak State Hospital by date, in the first 20 days after February 2023 Turkey-Syria Earthquake.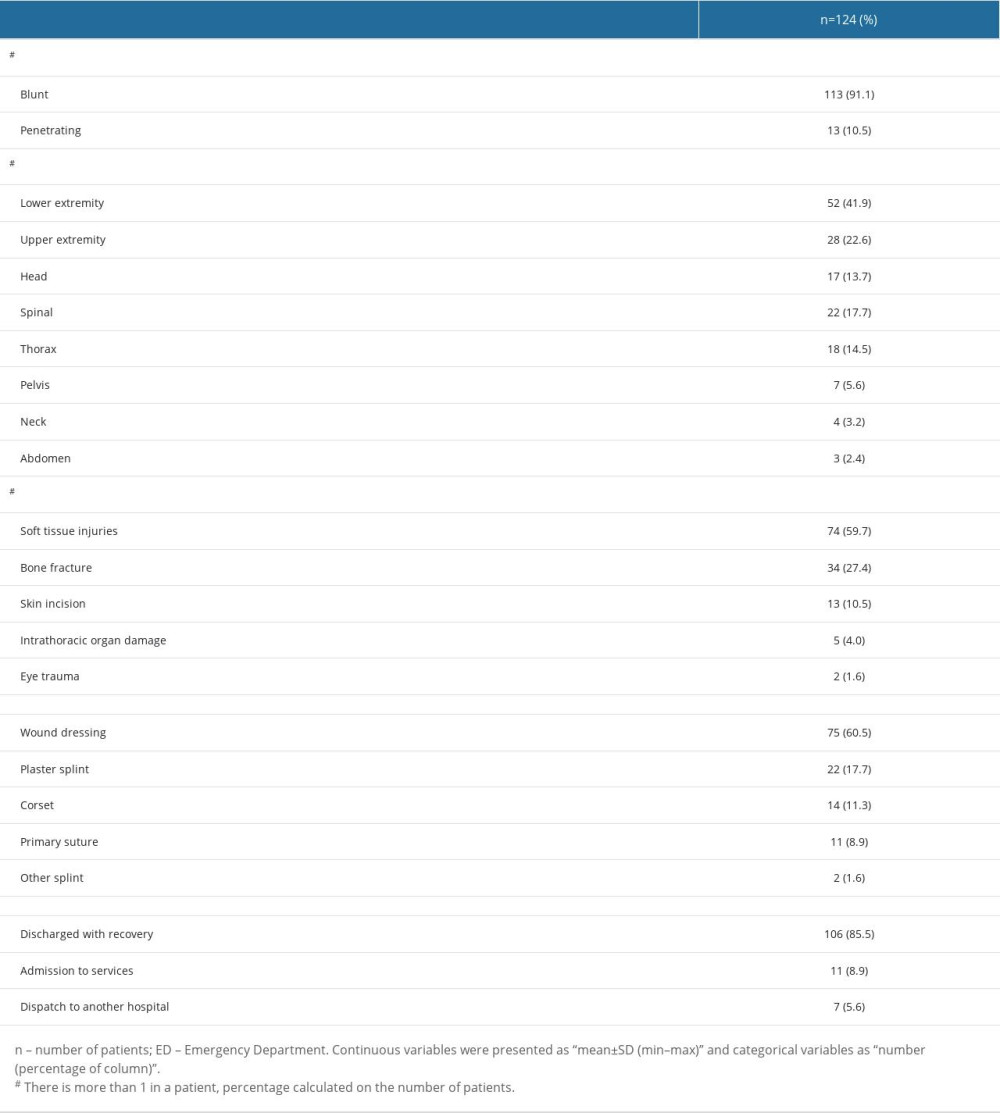 Table 2. Injury type, body zone injured, diagnosis, treatment, and result of Emergency Department visit of victims admitted to Ankara Mamak State Hospital following the February 2023 Turkey-Syria earthquake.
Table 2. Injury type, body zone injured, diagnosis, treatment, and result of Emergency Department visit of victims admitted to Ankara Mamak State Hospital following the February 2023 Turkey-Syria earthquake. In Press
15 Mar 2024 : Clinical Research
Impact of One-Lung Ventilation on Oxygenation and Ventilation Time in Thoracoscopic Heart Surgery: A Compar...Med Sci Monit In Press; DOI: 10.12659/MSM.943089
14 Mar 2024 : Clinical Research
Differential DHA and EPA Levels in Women with Preterm and Term Births: A Tertiary Hospital Study in IndonesiaMed Sci Monit In Press; DOI: 10.12659/MSM.943895
15 Mar 2024 : Clinical Research
Evaluation of an Optimized Workflow for the Radiofrequency Catheter Ablation of Paroxysmal Atrial FibrillationMed Sci Monit In Press; DOI: 10.12659/MSM.943526
09 Apr 2024 : Clinical Research
Correlation between Thalamocortical Tract and Default Mode Network with Consciousness Levels in Hypoxic-Isc...Med Sci Monit In Press; DOI: 10.12659/MSM.943802
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








