28 December 2023: Clinical Research
Hematologic Parameters as Predictors of Long-Term Mortality in Infective Endocarditis Patients
Sevil Gülaştı1ADEF*, Cemil Zencir1BCFG, Sercan Cayirli2ABC, Berk Mutlu1BCDF, Barcin OzturkDOI: 10.12659/MSM.941758
Med Sci Monit 2023; 29:e941758
Abstract
BACKGROUND: Infective endocarditis (IE) is an endothelial infection that is associated with high mortality and morbidity rates. Early and accurate risk prediction is important in patients with IE. Neutrophil-to-lymphocyte ratio (NLR), which is one of the hematological parameters that can be performed anywhere and is easily accessible, is a predictor of poor prognosis in many infectious and cardiovascular diseases. This study aimed to evaluate the association between laboratory parameters and 3-year mortality in 155 patients with infective endocarditis at a single center in Turkey.
MATERIAL AND METHODS: We retrospectively analyzed the clinical and echocardiographic data of 155 adult patients with definite IE according to the modified Duke Criteria, and we analyzed all laboratory results, such as hemoglobin, white blood cell, neutrophil, lymphocyte, platelet, platelet distribution width, NLR, urea, creatinine, albumin, procalcitonin, and blood culture results.
RESULTS: The median follow-up time was 341 days (range, 2-4003 days). The out-of-hospital mortality rate was 31.6%. Among the discharged patients (n=106), there were 46 non-survivors, with an out-of- hospital mortality rate of 43.4%. The overall mortality rate was 61.3%. During the follow-up, the 1-year mortality rate was 47.1% and the 3-year mortality rate was 54.8%. We detected significant differences in the admission values of NLR between the patients with and without 3-year mortality (P<0.001).
CONCLUSIONS: The NLR on admission to a tertiary center was independently associated with 3-year mortality in IE patients (P<0.001). NLR is a parameter that can be obtained from a simple, widely available and inexpensive hemagroma as a useful marker in predicting long-term mortality in IE.
Keywords: Endocarditis, Hematologic Tests, Mortality
Background
Infective endocarditis (IE) is an endothelial infection that is associated with high mortality and morbidity rates [1]. The diagnosis of IE has increased significantly with the development of echocardiography and nuclear imaging technology in recent years [1]. Despite developments in the diagnosis and treatment of IE, the in-hospital mortality and morbidity rates remain high [1–3]. With early identification of high-risk patients, more aggressive prompt treatment can be initiated for this targeted population, and the prognosis may improve. Comorbidity, cardiac or non-cardiac complications, the microorganism causing the infection, and echocardiographic findings of the patient are the known prognostic markers [1]. Older age, prosthetic valve involvement, heart failure, septic shock, cerebral complications, history of hemodialysis, periannular complications such as abscess, and
Material and Methods
ETHICS STATEMENT:
Approval was obtained from Adnan Menderes University Faculty of Medicine, Non-Invasive Clinical Research Ethics Committee (approval no. 2022/102). The requirement for patient informed consent was waived because of the retrospective nature of this study.
STUDY DESIGN AND PARTICIPANTS:
The patients with definite IE according to the modified Duke Criteria [2], diagnosed between January 2011 and April 2022 in Adnan Menderes University Faculty of Medicine, Aydın, Turkey were screened in the study. Diagnostic categories were defined as follows: direct evidence of vegetative growth in a histologic or bacteriologic study of the involved tissue or satisfying 2 major criteria or 1 major and 3 minor criteria or 5 minor criteria for IE. A total of 225 patients diagnosed with IE were scanned from the system. Seventy patients were excluded from the study because of missing or repetitive data. Finally, data on 155 patients were included in the study. Only those for whom all laboratory and echocardiographic data were available were enrolled. The all-cause mortality was assessed through telephone contact information recorded in the system. Turkish consensus report were used for the diagnosis and management of IE patients [3].
DATA COLLECTION AND MEASUREMENT:
Venous blood samples of all patients were collected at hospital admission, and at least 3 sets of blood cultures were performed for each patient before starting antibiotic treatment. The biochemical analysis results, including glucose, urea, creatinine, total protein, albumin, globulin, and CRP, were measured using an Ar-chitect C8000 analyzer (Abbot Park, IL, USA). CRP was also measured in the collected blood samples. Procalcitonin levels were measured by chemiluminescent immuno-assay using an auto-analyzer (Maglumi 600, Shaanxi, China and Abbott Alınıtyı system, USA). Complete blood count (CBC) parameters were measured using a Sysmex K-1000auto-analyzer (Block Scientific, Bohemia, NY, USA). Neutrophil-to-lymphocyte ratio (NLR) was directly calculated from CBC results.
STATISTICAL ANALYSIS:
For descriptive statistics, mean±standard deviation was used to present continuous data with normal distribution. Median with minimum-maximum values was applied for continuous variables without normal distribution. Numbers and percentages were used for categorical variables. The Shapiro-Wilk, Kolmogorov-Smirnov, and Anderson-Darling tests were used to assess the normal distribution of numerical variables.
The Pearson chi-square and Fisher’s exact tests were used to compare the differences between categorical variables in 2×2 tables. The Fisher Freeman Halton test was used in RxC tables.
The independent-samples
The receiver operating characteristic (ROC) analysis with the Youden index was used to determine the optimum value of the NLR that predicts mortality. The area under the ROC (AUC) curve and corresponding 95% confidence interval (CI) were calculated. Based on the appropriate cut-off value of the NLR, specificity and sensitivity were also calculated for the parameters with AUC value.
Univariate and multivariate Cox proportional hazard models and logistic regression analysis were performed to analyze the factors that impact the development of mortality. Hazard ratio (HR) with 95% CI was calculated.
Jamovi (version 2.2.5.0) and JASP (version 0.16.1) were used for statistical analysis. The significance level (
Results
CHARACTERISTICS OF THE PATIENTS:
There were 155 patients with a mean age of 64.8 ± 14.3 years. The majority of the patients were male (58.7%) (n=91). Hypertension (50.3%) (n=78), diabetes mellitus (41.9%) (n=58), and chronic kidney disease (37.4%) (n=39) were the 3 most common comorbidities in patients with infective endocarditis. Prosthetic heart valves were the most common etiological risk factor in 39 patients (25.2%), the second most common (7.7%, n=12) was history of implantable heart device, and the third most common (7.1%, n=11) was history of infective endocarditis. Other clinical characteristics are detailed in Table 1.
Native valve involvement (69.0%) was more common than prosthetic valve (25.8%) and lead involvement (4.5%). Although we did not detect any microorganism in 89 patients (57.4%),
COMPARISON OF OUTCOMES:
The median NLR was significantly lower in the survivors than in non-survivors (P≤0.001). The receiver operating characteristics (ROC) curve analysis showed that NLR higher than 6.63 had the sensitivity and specificity rates of 56.84% and 81.67% in predicting mortality (AUC=0.706, 95% confidence interval: 0.627–0.776, P≤0.001) (Figure 1). Considering the survival analysis results, the median life expectancy was 2502.4 days (2108.0–2896.9 at 95% CI) for those with an NLR value of 6.63 and above, and 810.7 days (493.2–1128.2 at 95% CI) for those with an NLR value of 6.63 and below, and the 3-year mortality rate was significantly higher in those with an NLR value of 6.63 and below (P<0.001) (Figure 2).
The mitral valve was the most common anatomic location (49.7%) for vegetative lodgment. We detected abscess formation and dehiscence with a leak in 41 (26.5%) and 32 patients (20.6%), respectively.
In 71 patients (45.8%), at least 1 complication developed. Acute renal failure was the most common complication, seen in 41 patients (26.5%). We applied conservative treatment modalities in 109 patients (70.3%), whereas surgical interventions were performed in 46 patients (29.7%). The in-hospital mortality rate was 31.6%. Among the discharged patients (n=106), there were 46 non-survivors, with an out-of-hospital mortality rate of 43.4%. The overall mortality rate was 61.3%.
During the follow-up, the 1-year and 3-year mortality rates were 47.1% and 54.8%, respectively.
Older patients were more likely to die at the end of the 3-year follow-up (P=0.003). The other demographic and clinical characteristics, except for the incidences of chronic renal failure (P=0.010) and previous cancer history (P=0.020), were similar (P>0.05) (Table 2). We detected no significant difference between the patients with and without 3-year mortality regarding disease-related characteristics (Table 3).
We detected significant differences in the values of hemoglobin, white blood cell, neutrophil, lymphocyte, platelet, platelet distribution width, NLR, urea, creatinine, albumin, and procalcitonin between the patients with and without 3-year mortality (P<0.05) (Table 4).
The factors that were associated with 3-year mortality were evaluated with logistic regression analysis. A statistically significant relationship was detected between the NLR values and 3-year mortality after excluding the effects of variables such as age, the presence of CKD, the presence of cancer, and the presence of complications (P=0.006). It was also found that a 1-unit increase in the NLR value caused a 1.136-fold (95% CI, 1.037–1.243) increase in 3-year mortality (Table 5).
The rates of atrial fibrillation in electrocardiography were similar between groups (P=0.968). The vegetations of the patients who died at the end of the three-year follow-up were significantly longer and wider than those in patients who survived (P=0.033 and P=0.028). The other echocardiographic findings were similar (P>0.05) (Table 6).
The 3-year mortality was significantly associated with the development of any complication (p=0.006) and acute renal failure (P=0.003). The other comparisons revealed no significant differences (P>0.05) (Table 7). The duration of the follow-up time was significantly shorter in patients with 3-year mortality (P<0.001).
Discussion
The effects of hematological parameters on mortality in long-term follow-up of patients with definite IE were investigated in this study. The 3-year mortality was 54.8%, with a median follow-up of 341 days (2–4003 days) in 155 patients with IE, whose records were assessed. Neutrophil/lymphocyte level, which was a hematological parameter recorded at the time of admission, is an independent predictor of 3-year all-cause mortality in patients with IE.
Infective endocarditis has a rare but life-threatening morbidity, and the mortality rate has not changed for more than 30 years despite all developments [1,6,8]. The in-hospital mortality rate of patients with IE ranges between 15% and 33% [5,10–12]. However, although the data on long-term mortality are not complete, according to recent studies, mortality rates are estimated to be 80–90% at 1 year, 70–80% at 2 years, and 60–70% at 5 years after the completion of IE treatment [1]. The in-hospital mortality rate was 31.6%, 1-year mortality was 47.1%, and 3-year mortality was 54%. These finding were similer to those of present study. The epidemiology of IE has changed over the years, with healthcare-associated IE now accounting for 25–30% of cases as a result of greater use of intravenous lines and intracardiac devices.
IE is difficult to diagnose and manage since it is a disease involving complex inflammatory processes. Also, with its complexity, it is difficult to identify higher-risk diseases in the early stages. Rapid identification of patients who have high risk of death may offer an opportunity to change the course of the disease [15]. The changes in WBC differential counts during severe infection are well known. In this regard, the progressive increase in neutrophil counts and the simultaneous decrease in lymphocyte counts in neutrophilic leukocytosis constitute the classical cellular shift in the WBC differential in response to acute bacterial infections [16–17]. Lymphocytes have a wide variety of roles in innate and adaptive immune response. T cells can regulate inflammation by interacting with various immune cells and activately suppress other leukocyte inflammatory responses. However, the causes of lymphocytopenia include increased catecholamine and cortisol levels, redistribution of lymphocytes to lymphatic organs, and apoptosis [18,19]. Although neutrophils are generally involved in the rapid response, lymphocytes are more involved in the adaptive and long-term response of the immune system, which is synonymous with physiological stress [20]. T cells are taken to the heart during cardiac inflammation and are involved in the pathophysiology of cardiac disease. Decreased lymphocyte percentage is a common finding in patients who have chronic heart failure and is associated with lower survival rates and increased need for heart transplant [21,22]. NLR in infection provides a higher predictive value than independent leukocyte differential and CRP [23–24]. Interestingly, NLR was shown to be a better predictor of mortality in patients who have advanced heart failure compared to independent absolute neutrophil and lymphocyte counts [25–27]. This can be explained partially by the finding that NLR combines 2 different immune pathways. Recently, elevated NLR levels were reported to be associated with increased mortality in various heart diseases [21–24]. NLR has been shown to be associated with in-hospital mortality in infective endocarditis patients in a few recent studies [6,7,28]. Hashimoto et al, in a study that included patients who were implanted with an intracardiac defibrillator for heart failure in 2016, with a median follow-up of 61.2 weeks, found that NLR was significantly higher in patients who died from all causes vs the surviving group [29]. In a study by Uthamalingam et al, in which 1212 patients who had acute decompensated heart failure were included, the median follow-up period was 26 months and long-term all-cause mortality was significantly higher in the group with high NLR, independent of EF [30]. In the present study, the median follow-up period was 341 days, and NLR was associated with all-cause mortality in IE patients. This marker can be a useful indicator of poor general condition.
NLR thresholds that range between 3.0 and 9.6 were used in studies of advanced heart failure, decompensated heart failure, and cardiac resynchronization therapy [25–27]. There is still no consensus on the cut-off value for identifying an abnormal NLR or when this evaluation should be made. The threshold value for NLR was 6.63 in the ROC analysis performed in the present study.
One of the limitations of the present study was that late referrals may have increased the incidence of morbidity and mortality because it was a retrospective study and was conducted in a single tertiary hospital. The study had a relatively small sample size. Also, other laboratory markers such as fibrinogen, proinflammatory cytokines, and B-type natriuretic peptide could not be evaluated, and factors such as treatment, duration, and use of antibiotics before diagnosis could not be evaluated in patients with IE, which has a wide clinical and etiological spectrum. Only blood test results at admission were analyzed because the relationship between NLR at the time of application and 3-year mortality was evaluated in the study. Further studies can be planned in the future to identify high-risk patients with echocardiography findings such as vegetation diameter and NLR-based risk scores at the time of initial presentation for IE, which has very different clinical presentation and etiology.
Conclusions
NLR was independently associated with 3-year mortality in IE patients. NLR is a parameter that can be obtained from a simple, widely available, and inexpensive test as a useful marker in predicting long-term mortality in IE patients.
Figures
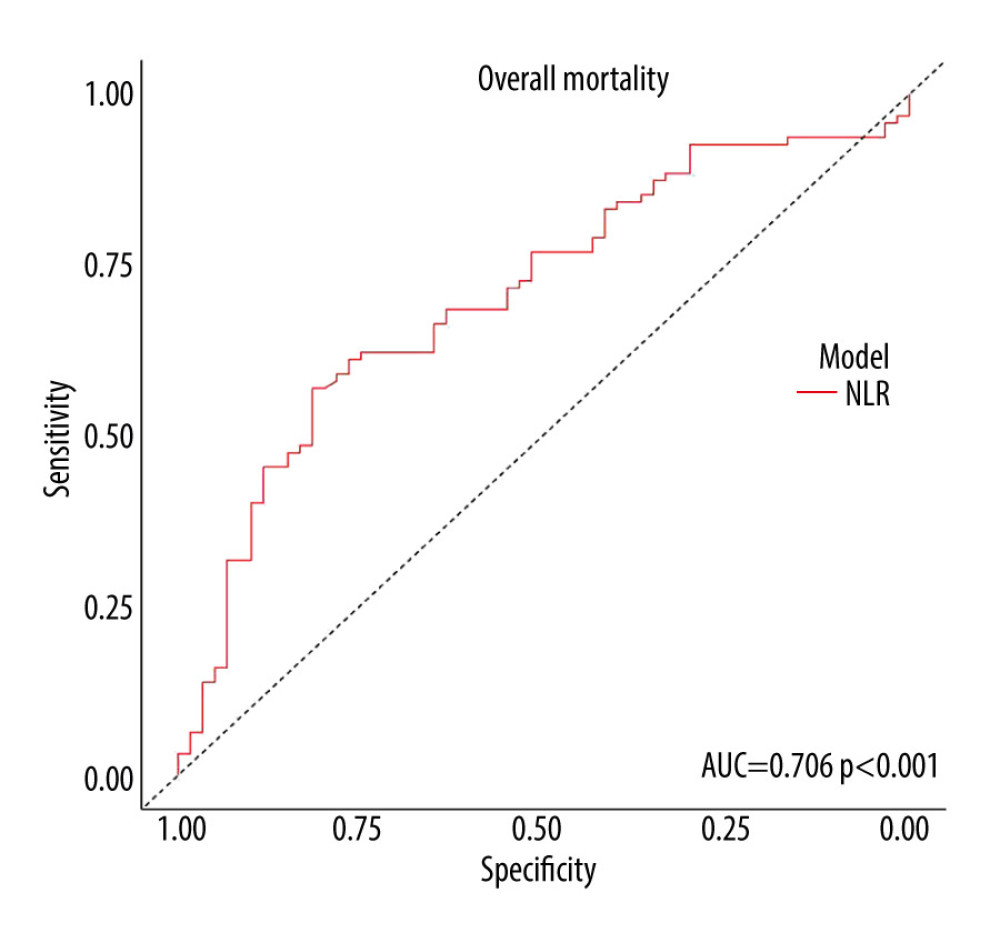 Figure 1. The receiver operating characteristics (ROC) curve analysis showed that neutrophil-to-lymphocyte ratio higher than 6.63 had 56.84% sensitivity and 81.67% specificity in predicting mortality (AUC=0.706, 95% confidence interval: 0.627–0776, P≤0.001)
Figure 1. The receiver operating characteristics (ROC) curve analysis showed that neutrophil-to-lymphocyte ratio higher than 6.63 had 56.84% sensitivity and 81.67% specificity in predicting mortality (AUC=0.706, 95% confidence interval: 0.627–0776, P≤0.001) 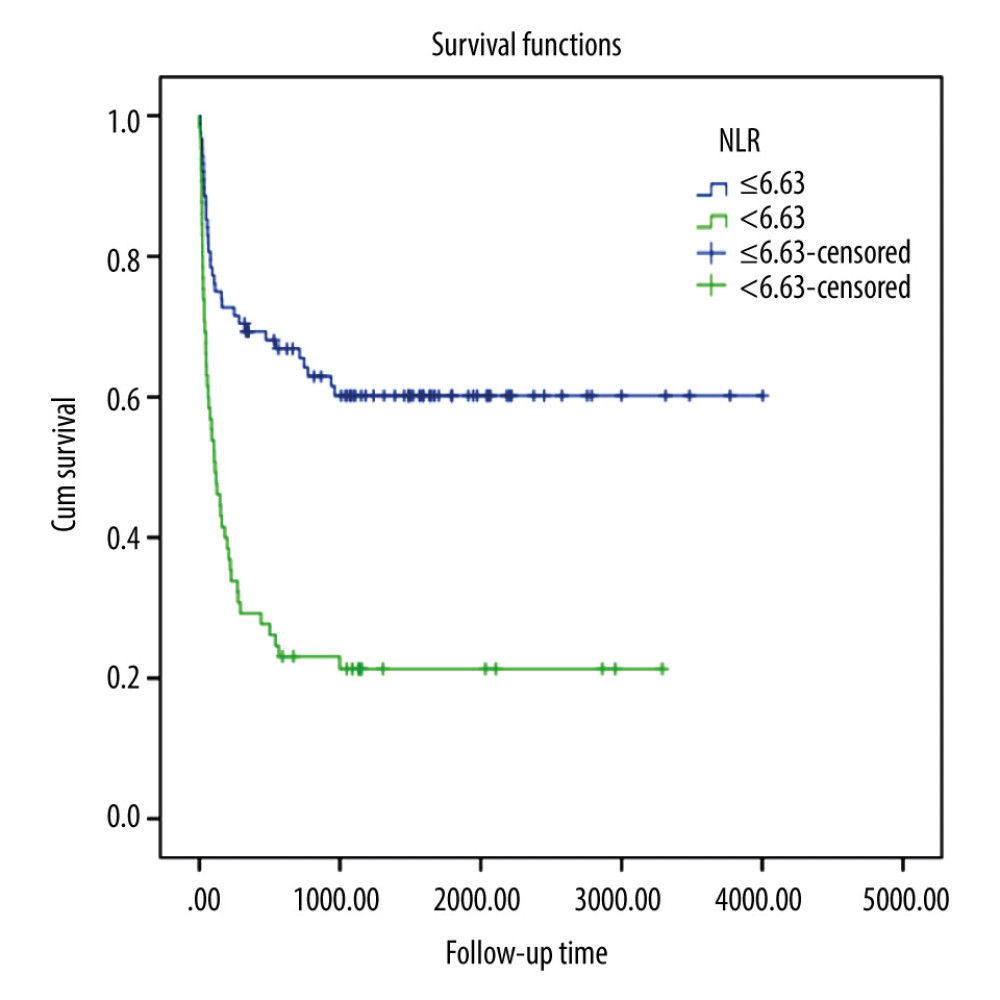 Figure 2. When the survival analysis results were evaluated, the average life expectancy was 2502.4 days (2108.0–2896.9 at 95% CI) for those with an NLR value of 6.63 and above, and 810.7 days (493.2–1128.2 at 95% CI) for those with an NLR value of 6.63 and below, and the 3-year mortality was significantly higher in those with an NLR value of 6.63 and below (P<0.001).
Figure 2. When the survival analysis results were evaluated, the average life expectancy was 2502.4 days (2108.0–2896.9 at 95% CI) for those with an NLR value of 6.63 and above, and 810.7 days (493.2–1128.2 at 95% CI) for those with an NLR value of 6.63 and below, and the 3-year mortality was significantly higher in those with an NLR value of 6.63 and below (P<0.001). Tables
Table 1. Demographic and clinical characteristics of the patients with infective endocarditis.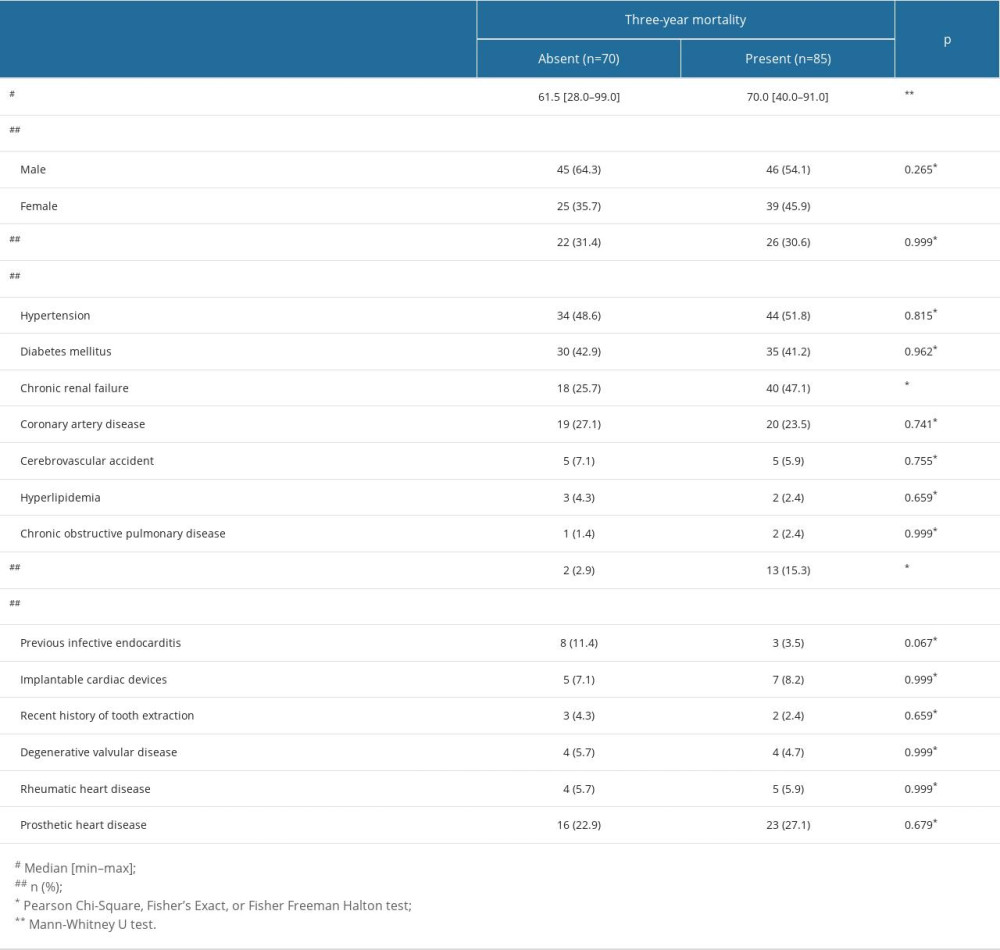 Table 2. Demographic and clinical characteristics of the patients with and without 3-year mortality.
Table 2. Demographic and clinical characteristics of the patients with and without 3-year mortality.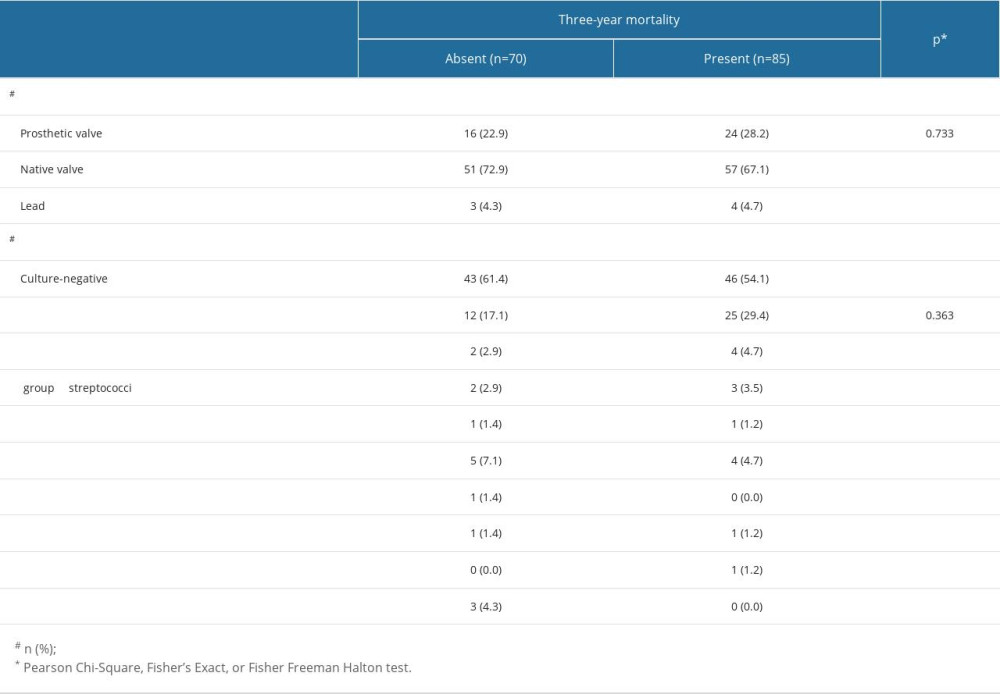 Table 3. Comparison of the disease-related characteristics in patients with and without three-year mortality.
Table 3. Comparison of the disease-related characteristics in patients with and without three-year mortality.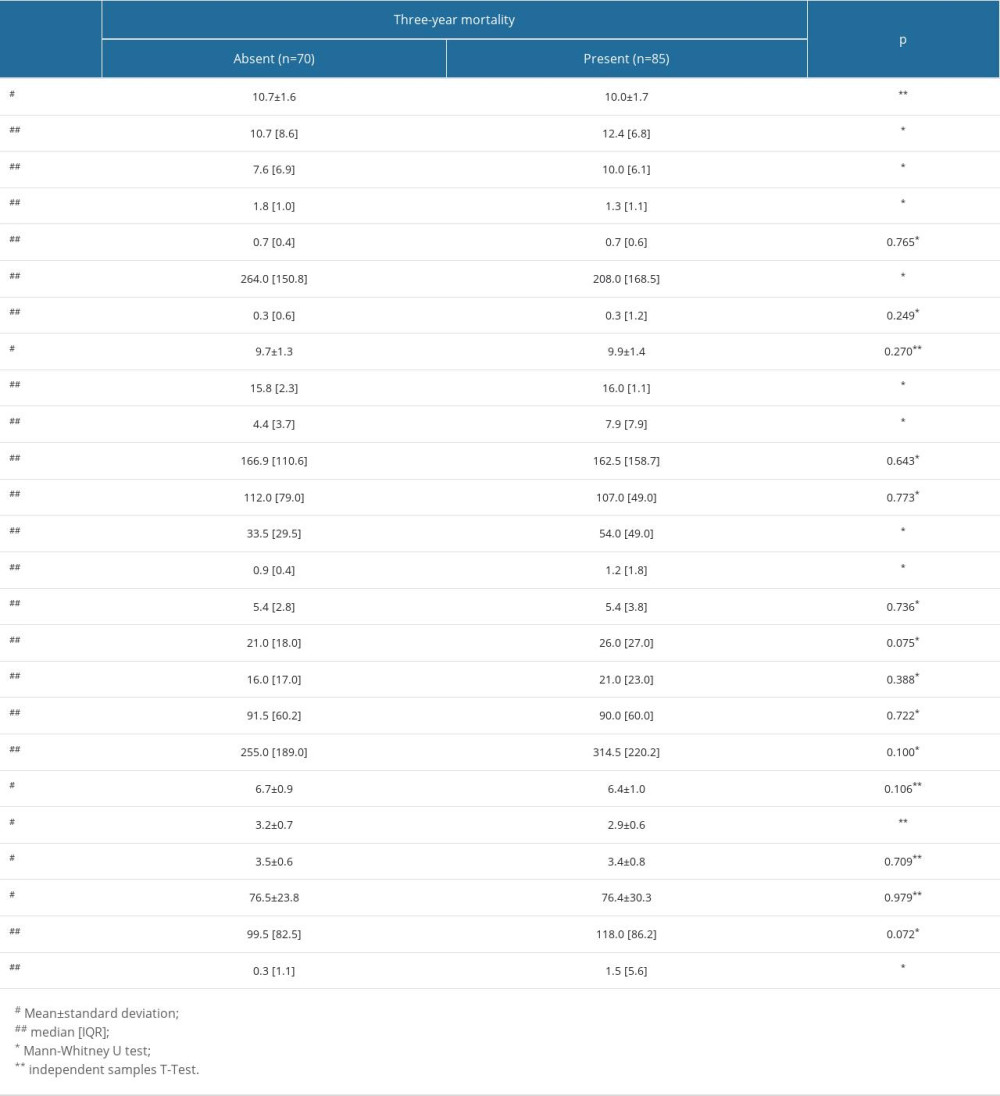 Table 4. Laboratory investigations of the patients with and without 3-year mortality.
Table 4. Laboratory investigations of the patients with and without 3-year mortality.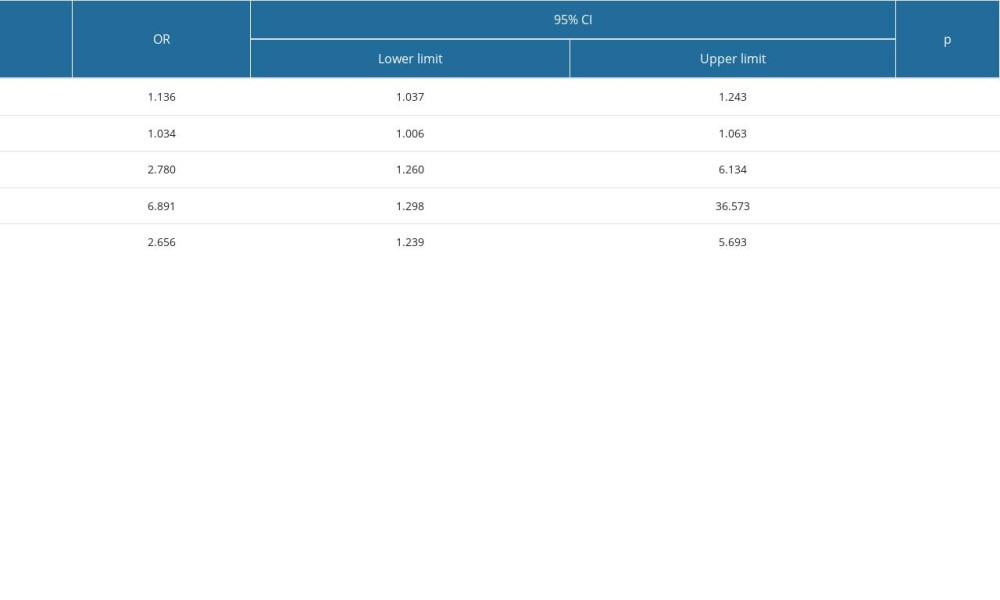 Table 5. The evaluation of the factors that may be associated with 3-year mortality with logistic regression analysis.
Table 5. The evaluation of the factors that may be associated with 3-year mortality with logistic regression analysis.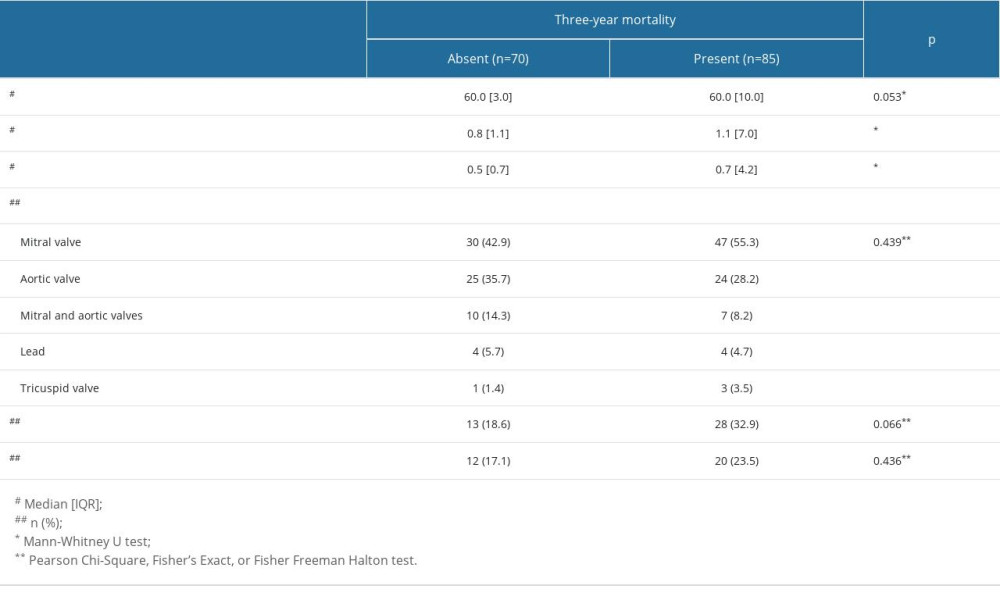 Table 6. Echocardiographic findings in patients with and without 3-year mortality.
Table 6. Echocardiographic findings in patients with and without 3-year mortality.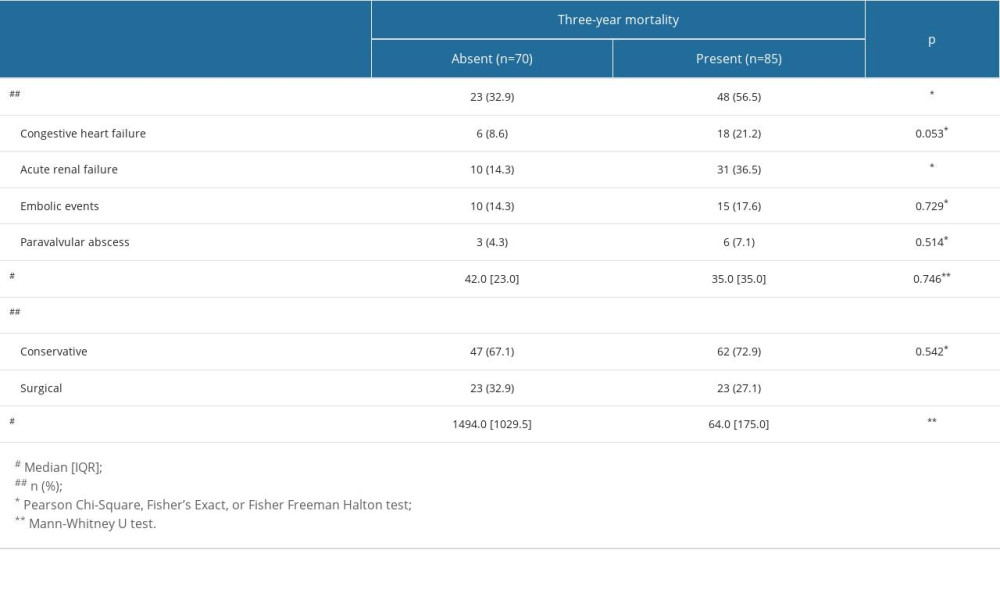 Table 7. Morbidity and outcomes of patients with and without 3-year mortality.
Table 7. Morbidity and outcomes of patients with and without 3-year mortality.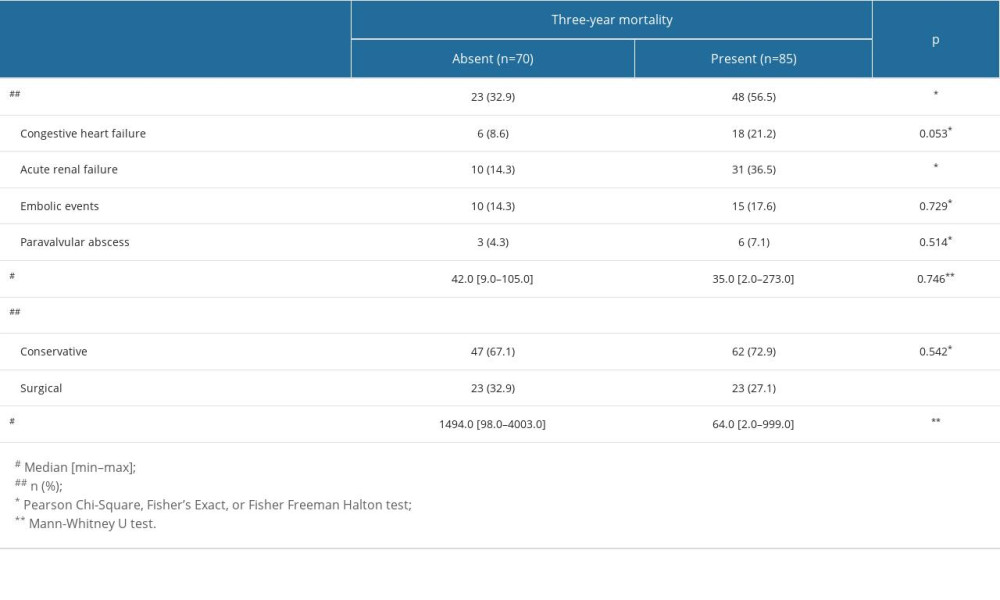
References
1. Delgado V, Ajmone Marsan N, de Waha SESC Scientific Document Group, 2023 ESC Guidelines for the management of endocarditis: Eur Heart J, 2023; 44(39); 3948-4042
2. Baddour LM, Wilson WR, Bayer ASAmerican Heart Association Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease of the Council on Cardiovascular Disease in the Young, Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and Stroke Council, Infective endocarditis in adults: Diagnosis, antimicrobial therapy, and management of complications: A scientific statement for healthcare professionals from the American Heart Association: Circulation, 2015; 132(15); 1435-86
3. Şimşek-Yavuz S, Akar AR, Aydoğdu S, Diagnosis, treatment and prevention of infective endocarditis: Turkish consensus report: Klimik Derg, 2019; 32(Suppl 1); 2-116
4. Habib G, Erba PA, Iung B, Clinical presentation, aetiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: A prospective cohort study: Eur Heart J, 2019; 40; 3222-32
5. Ris T, Teixeira-Carvalho A, Coelho RMP, Inflammatory biomarkers in infective endocarditis: machine learning to predict mortality: Clin Exp Immunol, 2019; 196(3); 374-82
6. Turak O, Özcan F, İşleyen A, Usefulness of neutrophil-to-lymphocyte ratio to predict in-hospital outcomes in infective endocarditis: Can J Cardiol, 2013; 29(12); 1672-78
7. Zencir C, Akpek M, Senol S, Association between hematologic parameters and in-hospital mortality in patients with infective endocarditis: Kaohsiung J Med Sci, 2015; 31(12); 632-38
8. Shah ASV, McAllister DA, Gallacher P, Incidence, microbiology, and outcomes in patients hospitalized with ınfective endocarditis: Circulation, 2020; 141(25); 2067-77
9. Leone S, Ravasio V, Durante-Mangoni E, Epidemiology, characteristics, and outcome of infective endocarditis in Italy: The Italian Study on Endocarditis: Infection, 2012; 40(5); 527-35
10. Meshaal MS, Labib D, Said K, Aspergillus endocarditis: Diagnostic criteria and predictors of outcome. A retrospective cohort study: PLoS One, 2018; 13(8); e0201459
11. Meshaal MS, Kassem HH, Samir A, Impact of routine cerebral CT angiography on treatment decisions in infective endocarditis: PLoS One, 2015; 10(3); e0118616
12. Selton-Suty C, Célard M, Le Moing VAEPEI Study Group, Preeminence of Staphylococcus aureus in infective endocarditis: A 1-year population-based survey: Clin Infect Dis, 2012; 54; 1230-39
13. Fernandez-Hidalgo N, Almirante B, Tornos P, Contemporary epidemiology and prognosis of health care-associated infective endocarditis: Clin Infect Dis, 2008; 47; 1287-97
14. Olmos C, Vilacosta I, Fernandez C, Contemporary epidemiology and prognosis of septic shock in infective endocarditis: Eur Heart J, 2012; 34(26); 1999-2006
15. Menges T, Engel J, Welters I, Changes in blood lymphocyte populations after multiple trauma: association with posttraumatic complications: Crit Care Med, 1999; 27; 733-40
16. Wyllie DH, Bowler IC, Peto TE, Relation between lymphopenia and bacteraemia in UK adults with medical emergencies: J Clin Pathol, 2004; 57; 950-95
17. Zahorec R, Ratio of neutrophil to lymphocyte countsdrapid and simple parameter of systemic inflammation and stress in critically ill: Bratisl Lek Listy, 2001; 102; 5-14
18. Ayala A, Herdon CD, Lehman DL, Differential induction of apoptosis in lymphoid tissues during sepsis: Variation in onset, frequency, and the nature of the mediators: Blood, 1996; 87; 4261-75
19. Afari ME, Bhat T, Neutrophil to lymphocyte ratio (NLR) and cardiovascular diseases: An update: Expert Rev Cardiovasc Ther, 2016; 14(5); 573-77
20. Levy WC, Mozaffarian D, Linker DT, The Seattle Heart Failure Model: Prediction of survival in heart failure: Circulation, 2006; 113; 1424-33
21. Mozaffarian D, Anker SD, Anand I, Prediction of mode of death in heart failure: The Seattle Heart Failure Model: Circulation, 2007; 116; 392-98
22. Terradas R, Grau S, Blanch J, Eosinophil count and neutrophillymphocyte count ratio as prognostic markers in patients with bacteremia: A retrospective cohort study: PLoS One, 2012; 7; e42860
23. De Jager CP, van Wijk PT, Mathoera RB, Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an Emergency Care Unit: Crit Care, 2010; 14; R192
24. Uthamalingam S, Patvardhan EA, Subramanian S, Utility of the neutrophil to lymphocyte ratio in predicting long-term outcomes in acute decompensated heart failure: Am J Cardiol, 2011; 107; 433-38
25. Boros AM, Szeplaki G, Perge P, The ratio of the neutrophil leucocytes to the lymphocytes predicts the outcome after cardiac resynchronization therapy: Europace, 2016; 18; 747-54
26. Benites-Zapata VA, Hernandez AV, Nagarajan V, Usefulness of neutrophil-to-lymphocyte ratio in risk stratification of patients with advanced heart failure: Am J Cardiol, 2015; 115; 57-61
27. Tasal A, Erturk M, Uyarel H, Utility of the neutrophil to lymphocyte ratio for predicting in-hospital mortality after levosimendan infusion in patients with acute decompensated heart failure: J Cardiol, 2014; 63; 418-23
28. Bozbay M, Ugur M, Uyarel H, Neutrophil-to-lymphocyte ratio as a prognostic marker in infective endocarditis: In-hospital and long-term clinical results: J Heart Valve Dis, 2014; 23(5); 617-23
29. Hashimoto N, Arimoto T, Narumi T, The neutrophil-to-lymphocyte ratio predicts all-cause mortality in patients with ımplantable cardioverter defibrillators: Pacing Clin Electrophysiol, 2017; 40(2); 135-44
30. Uthamalingam S, Patvardhan EA, Subramanian S, Utility of the neutrophil to lymphocyte ratio in predicting long-term outcomes in acute decompensated heart failure: Am J Cardiol, 2011; 107(3); 433-38
Figures
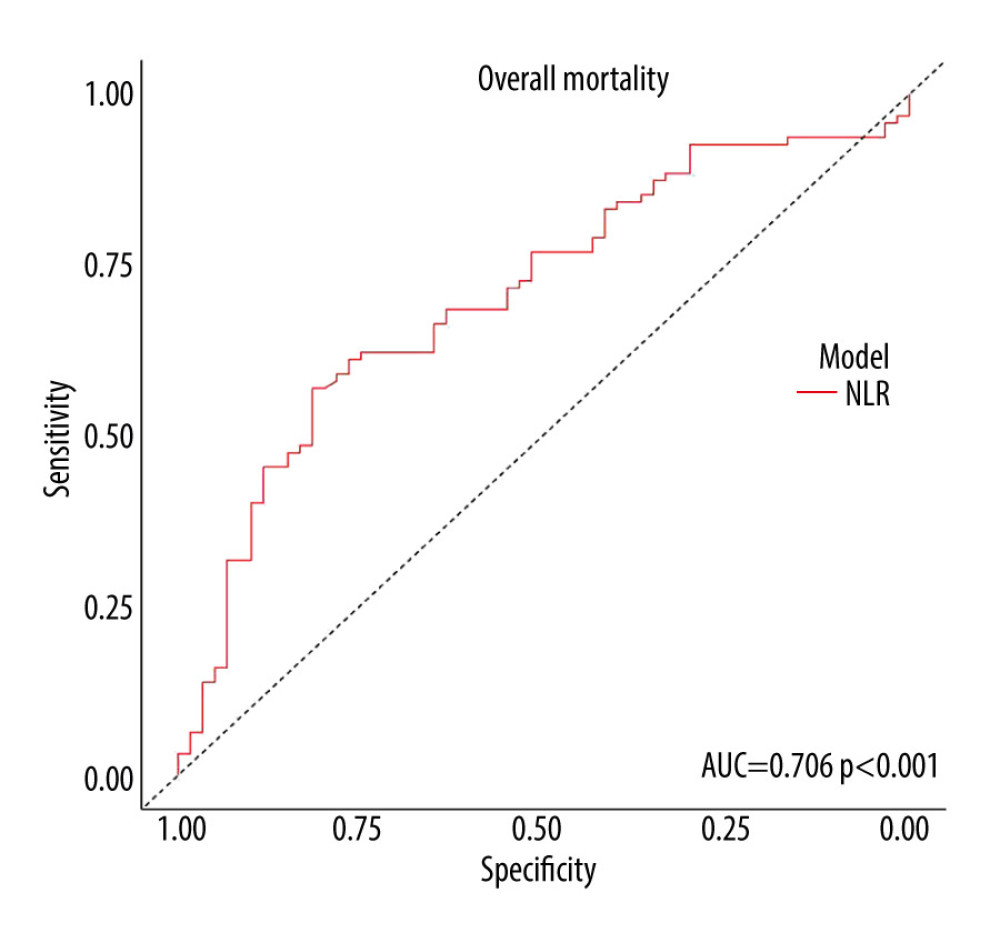 Figure 1. The receiver operating characteristics (ROC) curve analysis showed that neutrophil-to-lymphocyte ratio higher than 6.63 had 56.84% sensitivity and 81.67% specificity in predicting mortality (AUC=0.706, 95% confidence interval: 0.627–0776, P≤0.001)
Figure 1. The receiver operating characteristics (ROC) curve analysis showed that neutrophil-to-lymphocyte ratio higher than 6.63 had 56.84% sensitivity and 81.67% specificity in predicting mortality (AUC=0.706, 95% confidence interval: 0.627–0776, P≤0.001)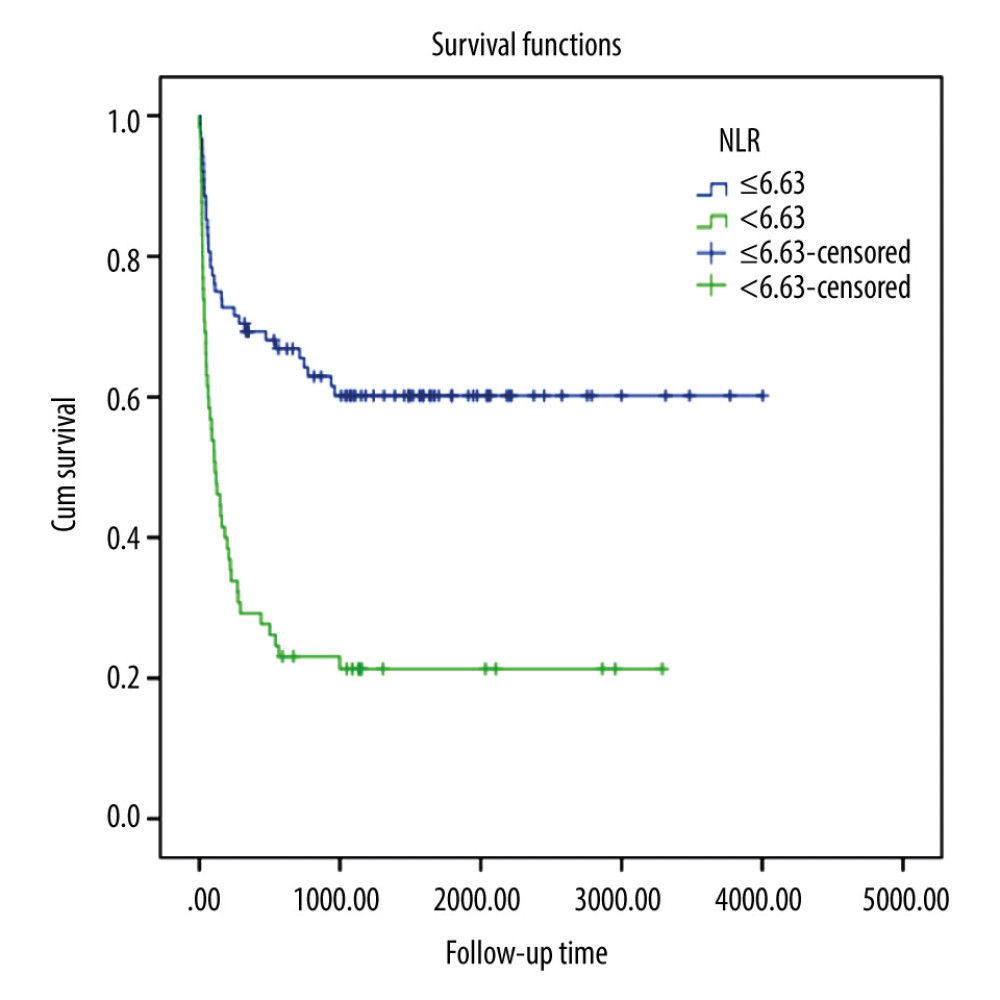 Figure 2. When the survival analysis results were evaluated, the average life expectancy was 2502.4 days (2108.0–2896.9 at 95% CI) for those with an NLR value of 6.63 and above, and 810.7 days (493.2–1128.2 at 95% CI) for those with an NLR value of 6.63 and below, and the 3-year mortality was significantly higher in those with an NLR value of 6.63 and below (P<0.001).
Figure 2. When the survival analysis results were evaluated, the average life expectancy was 2502.4 days (2108.0–2896.9 at 95% CI) for those with an NLR value of 6.63 and above, and 810.7 days (493.2–1128.2 at 95% CI) for those with an NLR value of 6.63 and below, and the 3-year mortality was significantly higher in those with an NLR value of 6.63 and below (P<0.001). Tables
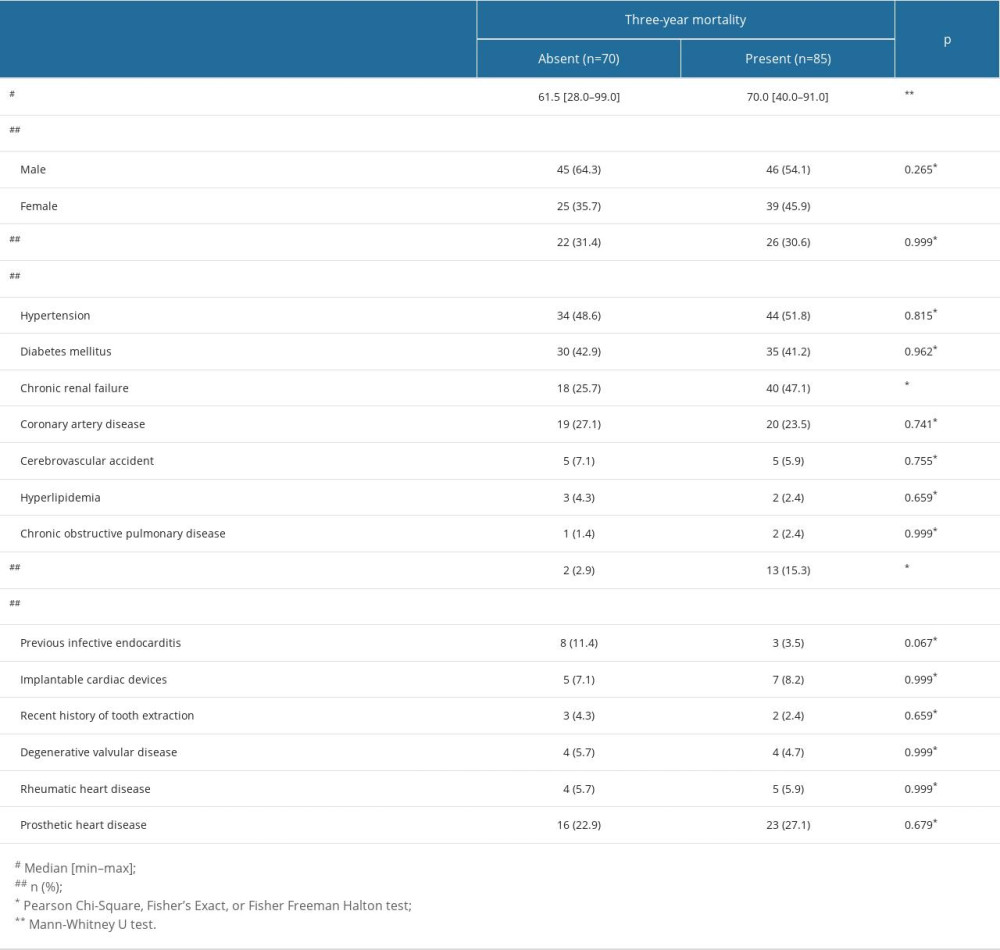 Table 1. Demographic and clinical characteristics of the patients with infective endocarditis.
Table 1. Demographic and clinical characteristics of the patients with infective endocarditis.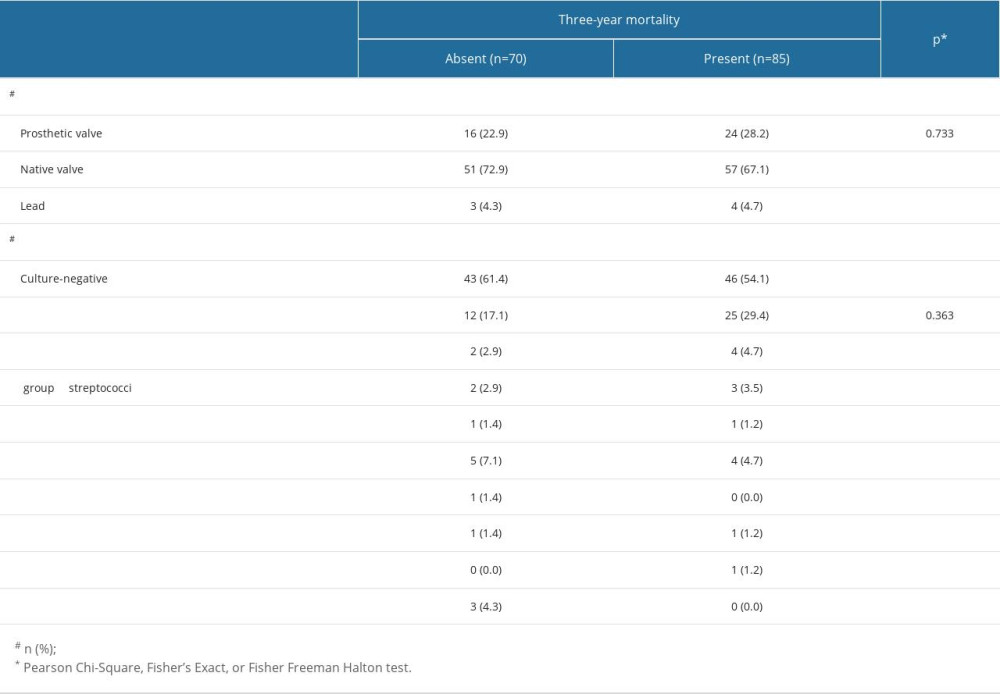 Table 2. Demographic and clinical characteristics of the patients with and without 3-year mortality.
Table 2. Demographic and clinical characteristics of the patients with and without 3-year mortality.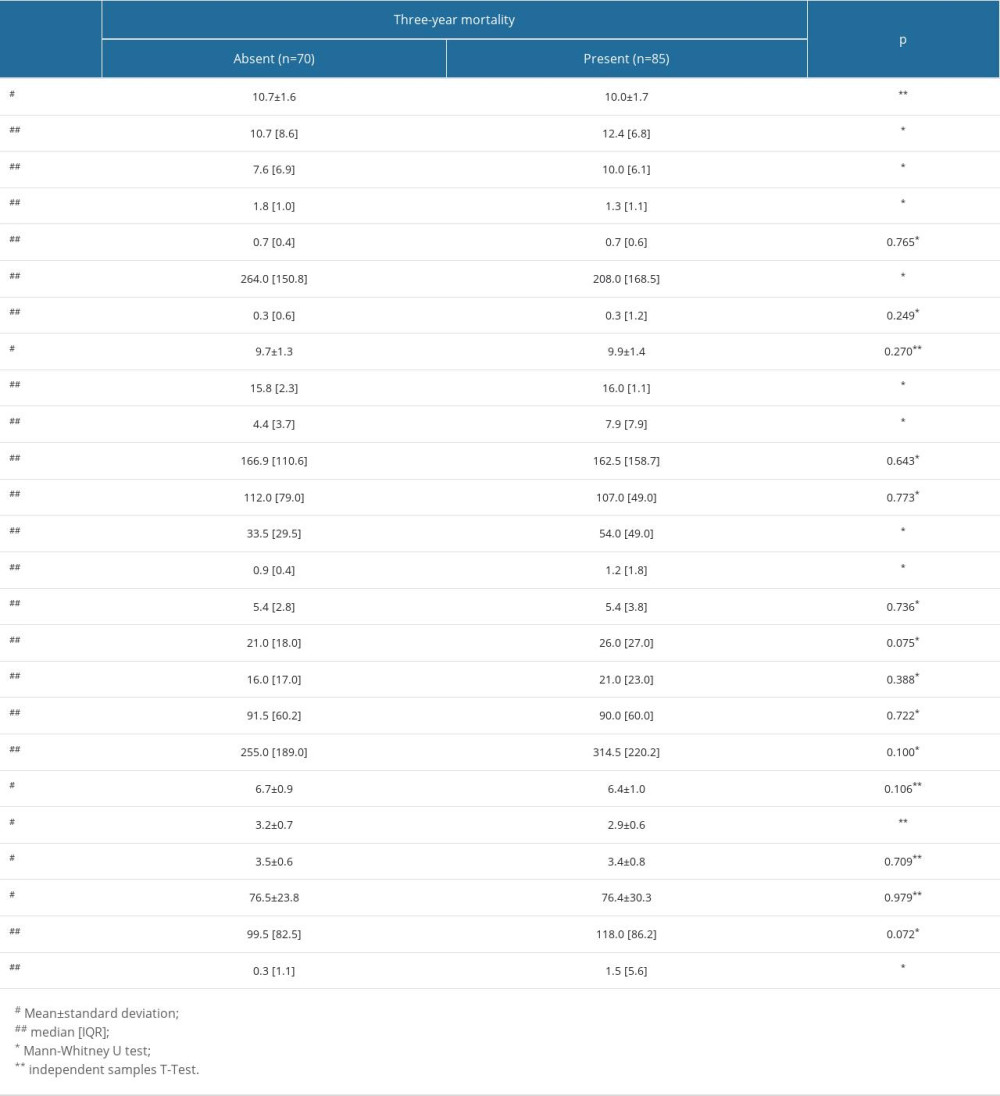 Table 3. Comparison of the disease-related characteristics in patients with and without three-year mortality.
Table 3. Comparison of the disease-related characteristics in patients with and without three-year mortality.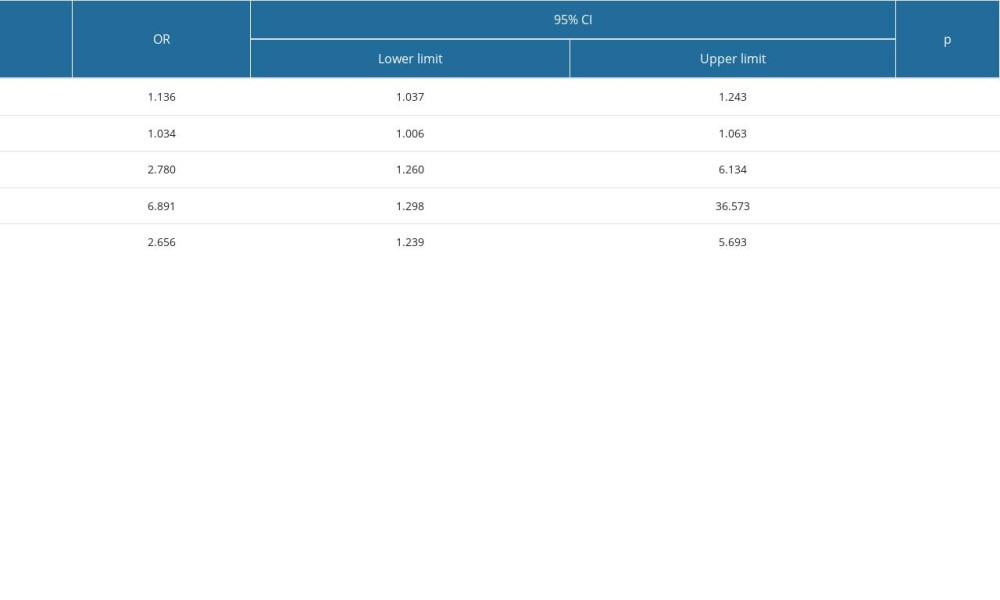 Table 4. Laboratory investigations of the patients with and without 3-year mortality.
Table 4. Laboratory investigations of the patients with and without 3-year mortality.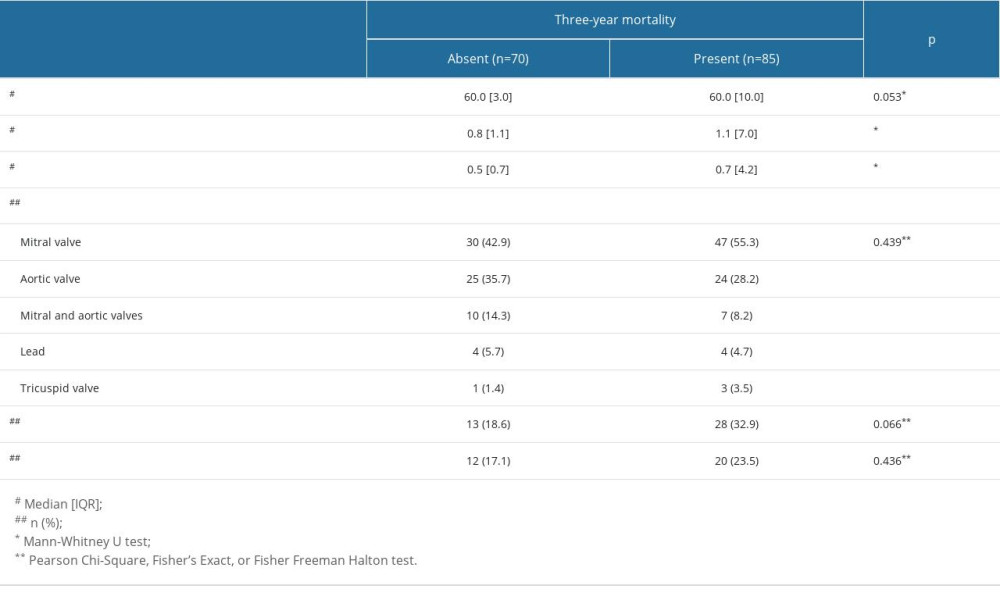 Table 5. The evaluation of the factors that may be associated with 3-year mortality with logistic regression analysis.
Table 5. The evaluation of the factors that may be associated with 3-year mortality with logistic regression analysis.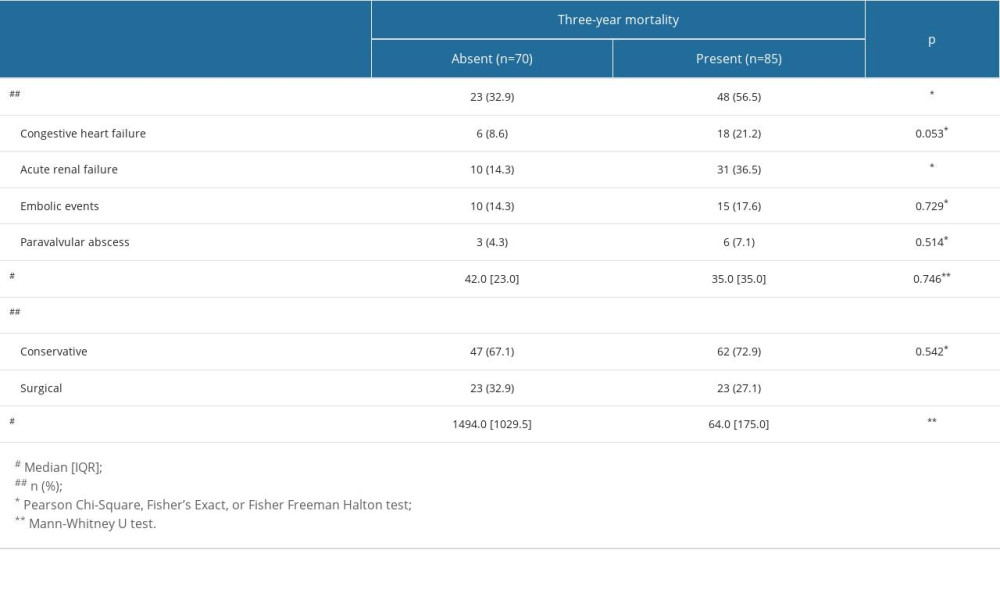 Table 6. Echocardiographic findings in patients with and without 3-year mortality.
Table 6. Echocardiographic findings in patients with and without 3-year mortality.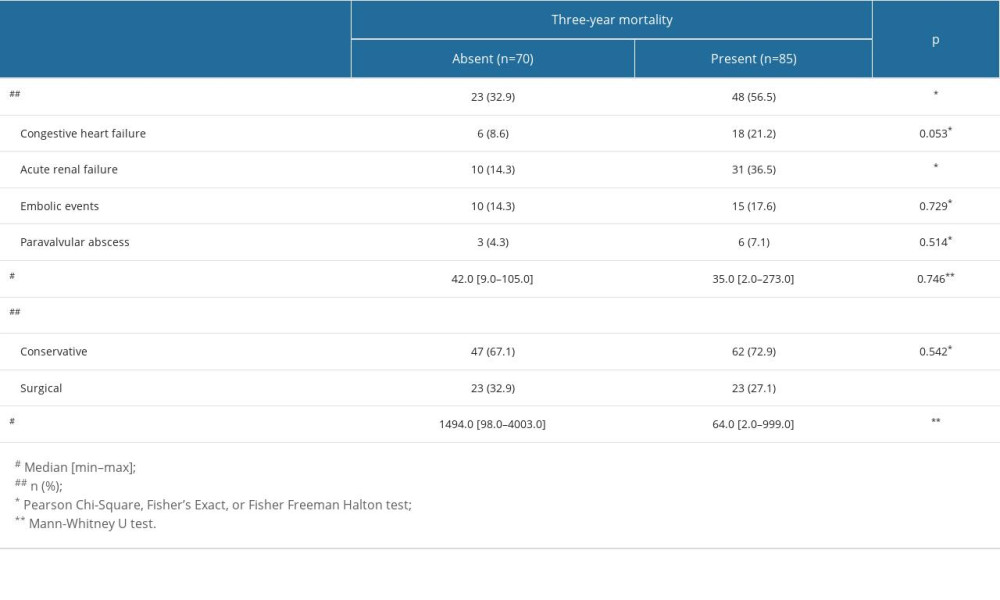 Table 7. Morbidity and outcomes of patients with and without 3-year mortality.
Table 7. Morbidity and outcomes of patients with and without 3-year mortality.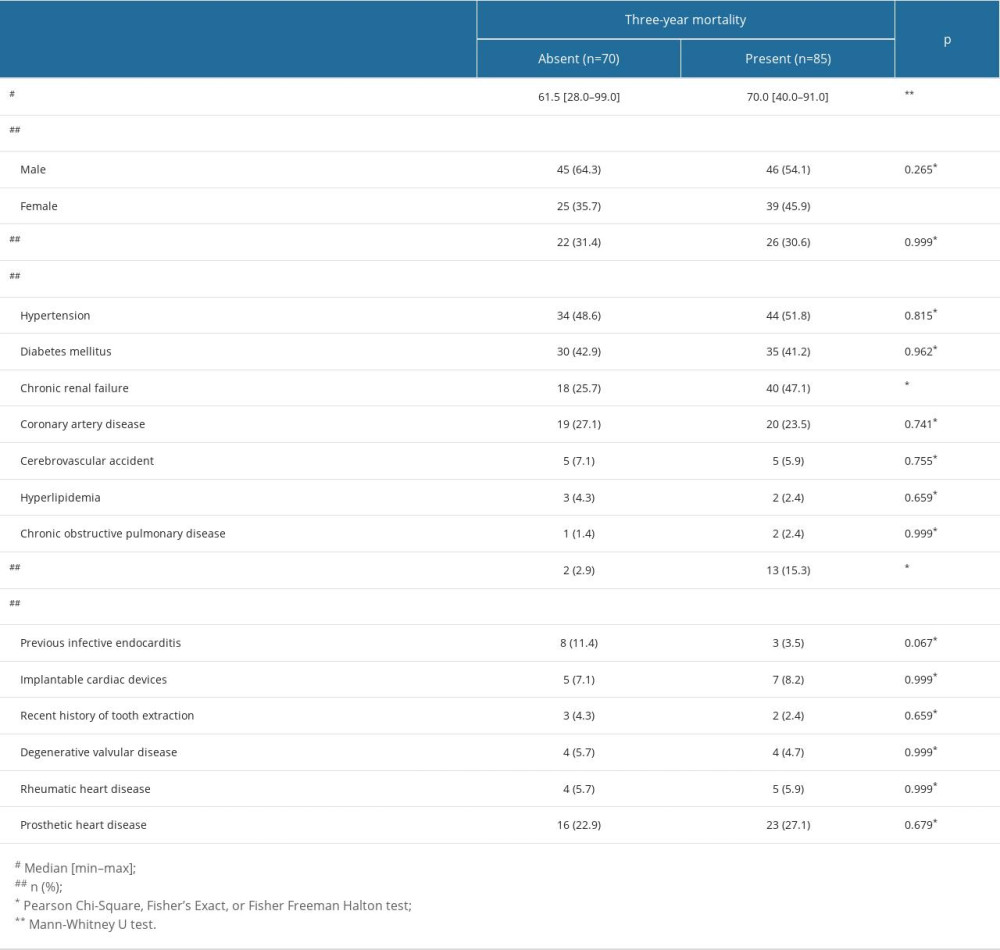 Table 1. Demographic and clinical characteristics of the patients with infective endocarditis.
Table 1. Demographic and clinical characteristics of the patients with infective endocarditis.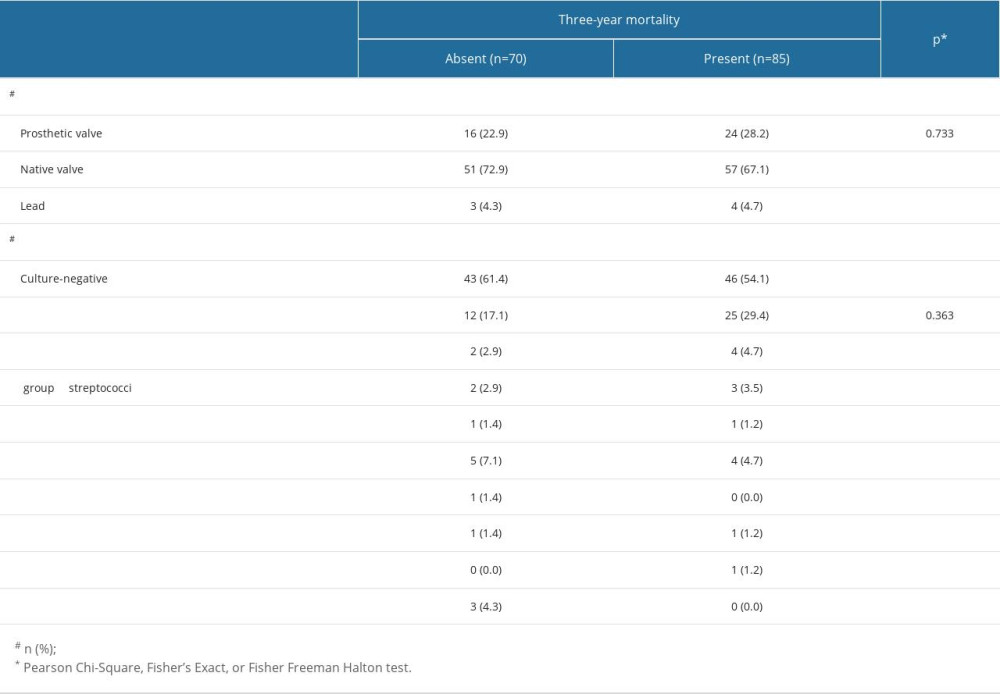 Table 2. Demographic and clinical characteristics of the patients with and without 3-year mortality.
Table 2. Demographic and clinical characteristics of the patients with and without 3-year mortality.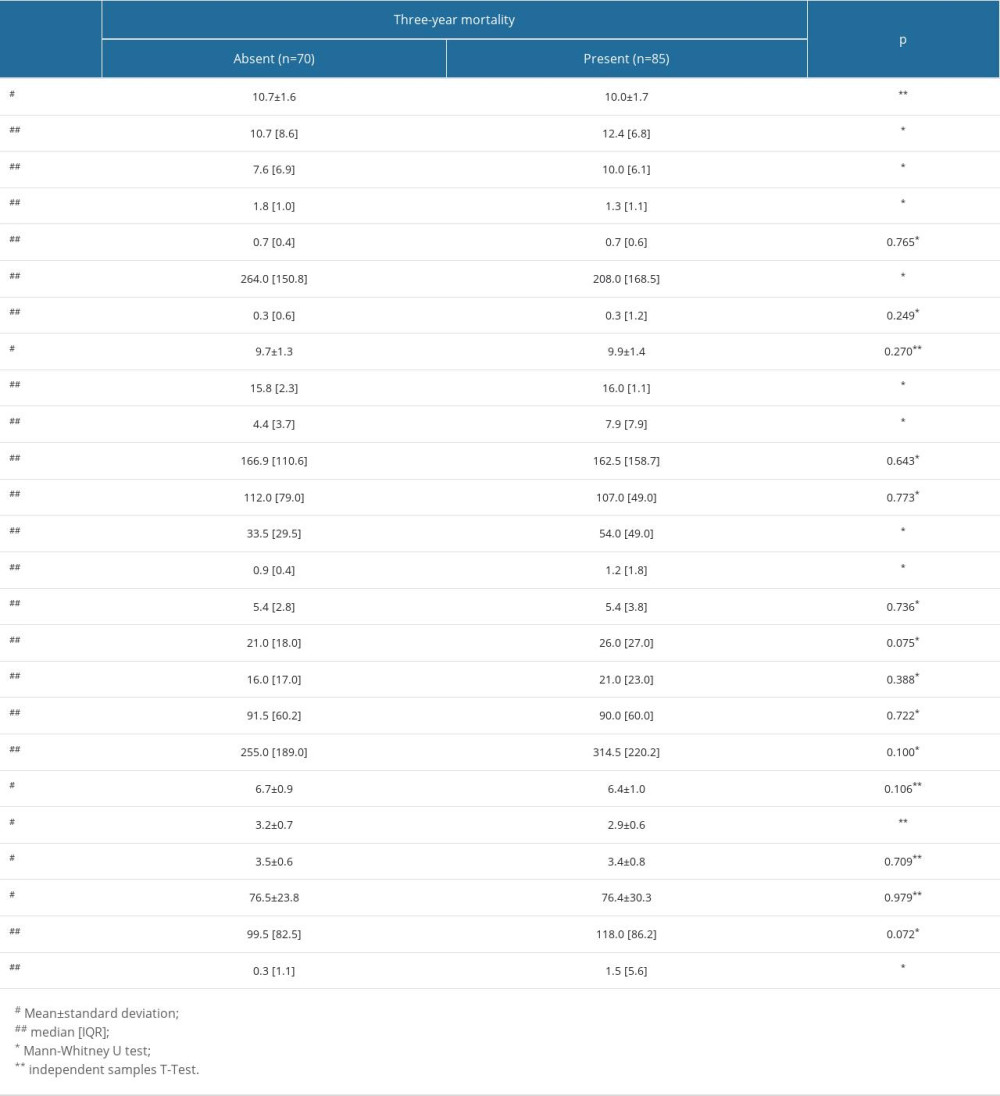 Table 3. Comparison of the disease-related characteristics in patients with and without three-year mortality.
Table 3. Comparison of the disease-related characteristics in patients with and without three-year mortality.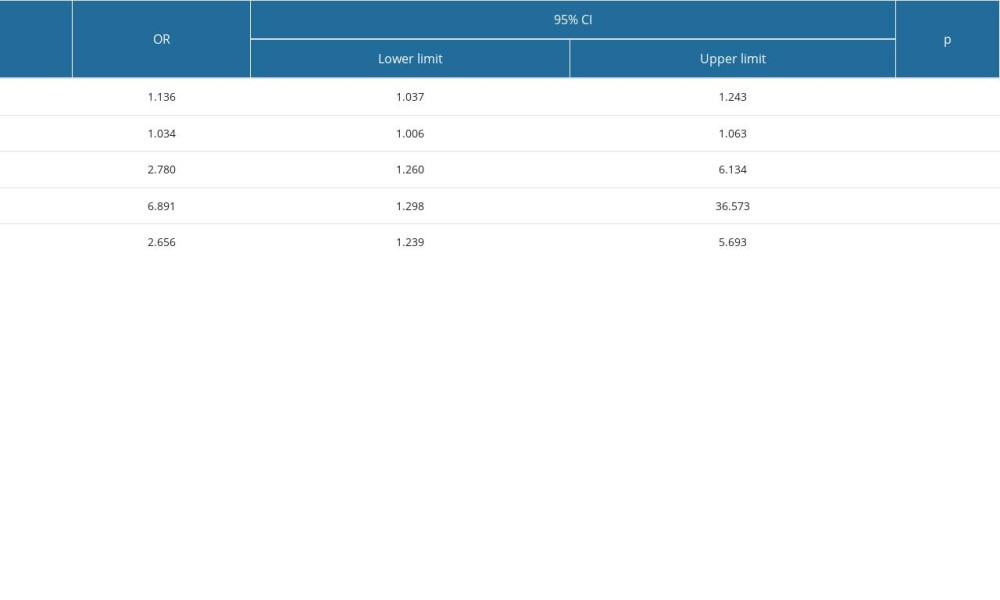 Table 4. Laboratory investigations of the patients with and without 3-year mortality.
Table 4. Laboratory investigations of the patients with and without 3-year mortality.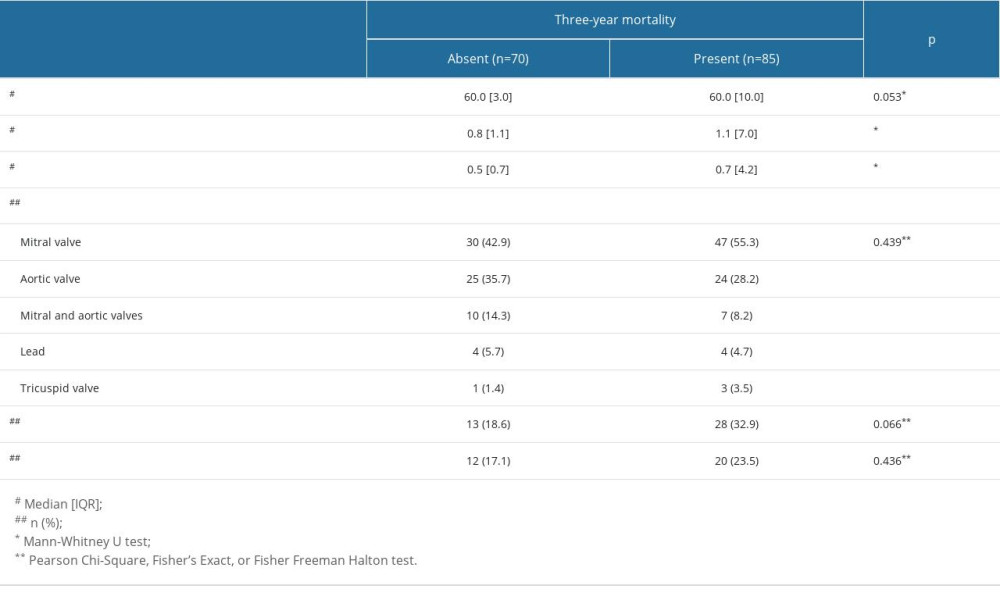 Table 5. The evaluation of the factors that may be associated with 3-year mortality with logistic regression analysis.
Table 5. The evaluation of the factors that may be associated with 3-year mortality with logistic regression analysis.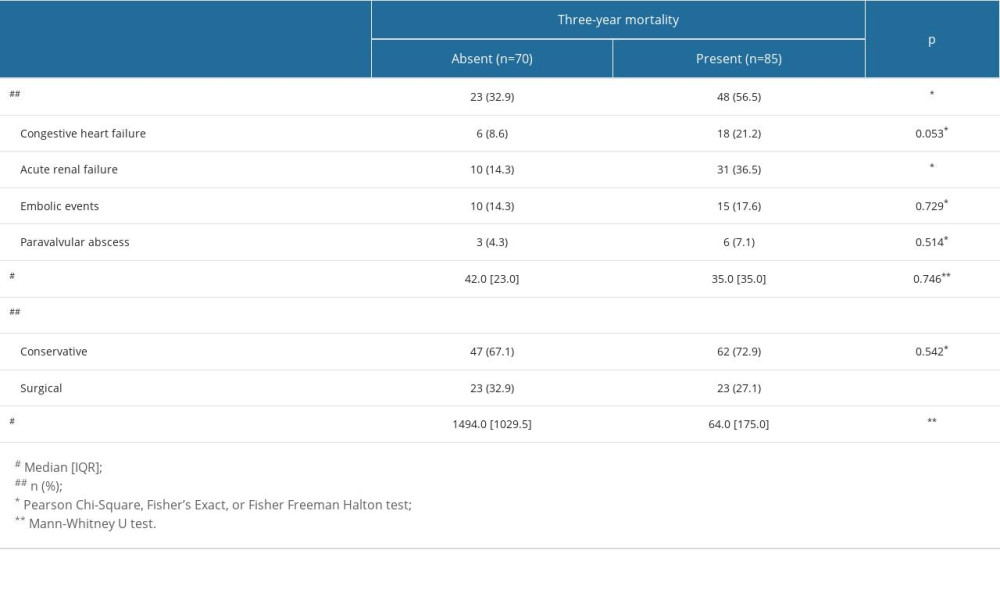 Table 6. Echocardiographic findings in patients with and without 3-year mortality.
Table 6. Echocardiographic findings in patients with and without 3-year mortality.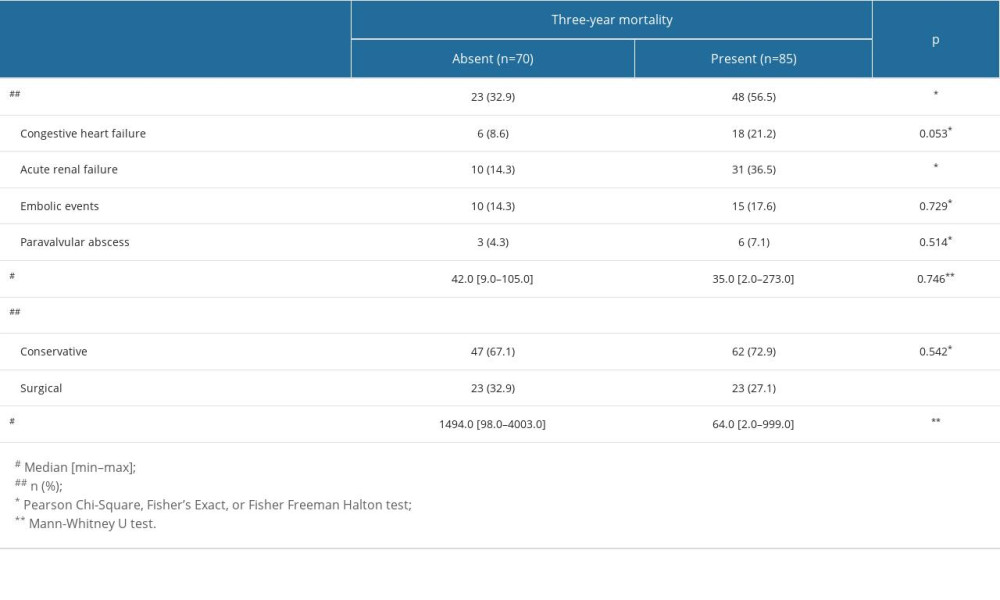 Table 7. Morbidity and outcomes of patients with and without 3-year mortality.
Table 7. Morbidity and outcomes of patients with and without 3-year mortality. In Press
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








