05 February 2024: Clinical Research
A Comparative Study of Laparoscopic and Open Approaches for Right Hemihepatectomy in Hepatocellular Carcinoma Patients: Safety and Short-Term Outcomes
Gehui Li12ABCE, Joseph MugaanyiDOI: 10.12659/MSM.942096
Med Sci Monit 2024; 30:e942096
Abstract
BACKGROUND: Hepatocellular carcinoma (HCC) is a leading cause of cancer deaths worldwide, with China reporting over half of global cases. While traditional open liver resection is effective, it often results in large incisions and significant complications. Laparoscopic hepatectomy, particularly for right hemi-hepatectomy, features smaller incisions and quicker recovery, but its widespread adoption is hindered by its procedural complexity and a steep learning curve. This study compares the safety and efficacy of laparoscopic versus open right hemi-hepatectomy with an anterior approach in 57 patients with HCC.
MATERIAL AND METHODS: The data of patients with HCC who underwent treatment at our center from January 2016 to December 2020 were retrospectively analyzed.
RESULTS: We included a total of 57 patients with histopathologically-confirmed HCC – 23 in the laparoscopic group and 34 in the open group. Operation time was significantly shorter in the open group than in the laparoscopic group (234.5±66.9 vs 297.0±74.9, P=0.002). Intraoperative bleeding was significantly less in the laparoscopic group (P=0.042). There were no statistically significant differences in postoperative complications between the 2 groups. Postoperative hospital stay was significantly shorter in the laparoscopic group (12 days vs 15 days, P=0.044). There was no significant difference in postoperative overall survival (OS) and disease-free survival (DFS) between the 2 groups (P>0.05).
CONCLUSIONS: In patients with hepatocellular carcinoma, the laparoscopic right hemi-hepatectomy with the anterior approach technique has the same safety and comparable short-term outcomes as open surgery.
Keywords: Carcinoma, Hepatocellular, Hepatectomy, Laparoscopy, Morbidity, Survival
Background
Hepatocellular carcinoma (HCC) is one of the most common malignancies and ranks fifth in cancer-related deaths worldwide. Data show that the number of primary liver cancer cases in China is increasing yearly, accounting for more than half of all diagnosed cases globally [1]. At present, radical surgical resection is the primary curative treatment approach. Although traditional open surgery has excellent clinical efficacy for patients, the incisions are usually large; intraoperative bleeding may be excessive and postoperative complications may be severe [2]. Recently, with the worldwide adoption of laparoscopic technology, hepatic hepatectomy has been widely used in China. Compared to traditional open surgery, laparoscopic surgery has many advantages, such as small surgical incisions and faster postoperative recovery [3]. In recent years, more centers have gradually transitioned to performing right hemi-hepatectomy laparoscopically whenever possible. First reported by Huscher et al [4], it has been used for both benign and malignant hepatic lesions. However, due to the difficulty of the procedure, steep learning curve, and postoperative complications [5], its adoption has been limited to tertiary surgical centers. Although significant advances have been made in laparoscopic hepatectomy techniques, their clinical efficacy is still controversial [6], especially in laparoscopic right hemi-hepatectomy. More studies are needed to confirm the feasibility and safety of the procedure. In this study, we aimed to investigate the safety and effectiveness of an anterior approach to laparoscopic right hemi-hepatectomy in treating hepatocellular carcinoma by comparing the perioperative indicators and the short-term outcomes of patients who underwent laparoscopic or open right hemi-hepatectomy.
Material and Methods
ETHICS STATEMENT:
This retrospective study has been conducted in accordance with the ethical principles and guidelines set forth by the Helsinki Declaration and our institution’s Ethics Review Board. The study involved the analysis of previously collected and anonymized data, and due to the retrospective research design, the requirement for individual patient informed consent was waived by the Ethics Review Board.
PATIENT DATA:
We reviewed data of patients who underwent right hemi-hepatectomy for HCC at our center from January 2016 to December 2020. Inclusion criteria were: (1) lesions confined to the right hemi-liver; (2) HCC diagnosis confirmed by histopathology; (3) Child-Pugh classification of B or above. Exclusion criteria were: (1) Pathologically confirmed cholangiocarcinoma, mixed cell carcinoma, or extra-hepatic metastasis; (2) Patients with portal vein thrombus or bile duct thrombus; (3) Patients with tumors closely related to the first and second hepatic hilum and not suitable for laparoscopic treatment. Patients were then divided into 2 groups: a laparoscopic group and an open surgery group.
SURGICAL PROCEDURE:
In the laparoscopic group, a standardized procedure was used for the operation. The patient was placed in a supine position, and the operation was conducted under general anesthesia. The camera port was located below the umbilicus, with a 10-mm trocar used. Two ports were used for the lead surgeon; a 10-mm trocar along the right midclavicular line and a 5-mm trocar along the right lateral line. Another 2 ports were used for the assisting surgeon; a 5-mm trocar along the left midclavicular line and a 10-mm port along the left lateral line. The 5 ports form a U/umbrella shape. After exploring the abdominal cavity, the gallbladder was resected. The right hepatic hilar was controlled by the intrathecal or the extrathecal method. After the location of the middle hepatic vein was determined by ultrasound, the liver parenchyma was transected according to the ischemic line to the anterior aspect of the right hepatic hilar. Following the total exposure of the right hepatic hilar tissue, the right hepatic hilar was dissected using ultrasonic shears (HAR36 HARMONIC ACE+ Shears with Adaptive Tissue Technology, Ethicon, Inc.).
The liver tissue was transected up to the anterior aspect of the inferior vena cava, and the right and left hepatic halves were split from the bottom up with the inferior vena cava as a guiding reference. After exposing the right hepatic vein, the right hepatic vein and the right short hepatic vein were dissected. Next, the right perihepatic ligament was dissected to resect the right hemi-liver fully. A single abdominal drainage tube was placed to drain the operation area. Operation procedure images are shown in Figure 1. Video 1 shows the laparoscopic right hemihepatectomy with an anterior approach.
In the open surgery group, the operation was similar to the laparoscopic technique. After the first hepatic hilar sheath was dissected to control blood flow through the posterior hepatic tunnel, leaving a lifting band around the liver, and the right hemi-liver was resected with an anterior approach. Operation procedure images are shown in Figure 2.
CLINICOPATHOLOGICAL DATA:
Preoperative characteristics, including age, sex, BMI, hypertension, and diabetes mellitus diagnosis; intraoperative characteristics, such as operation time, intraoperative bleeding, and transfusion rate; and postoperative data, including postoperative hospital stay, overall survival (OS) and disease-free survival (DFS) were compared between the 2 groups.
STATISTICAL ANALYSIS:
Statistical analysis was performed using SPSS version 26.0. All Normally distributed variables are presented as mean±standard deviation. Categorical variables are presented as median (range). Continuous variables were compared using the
Results
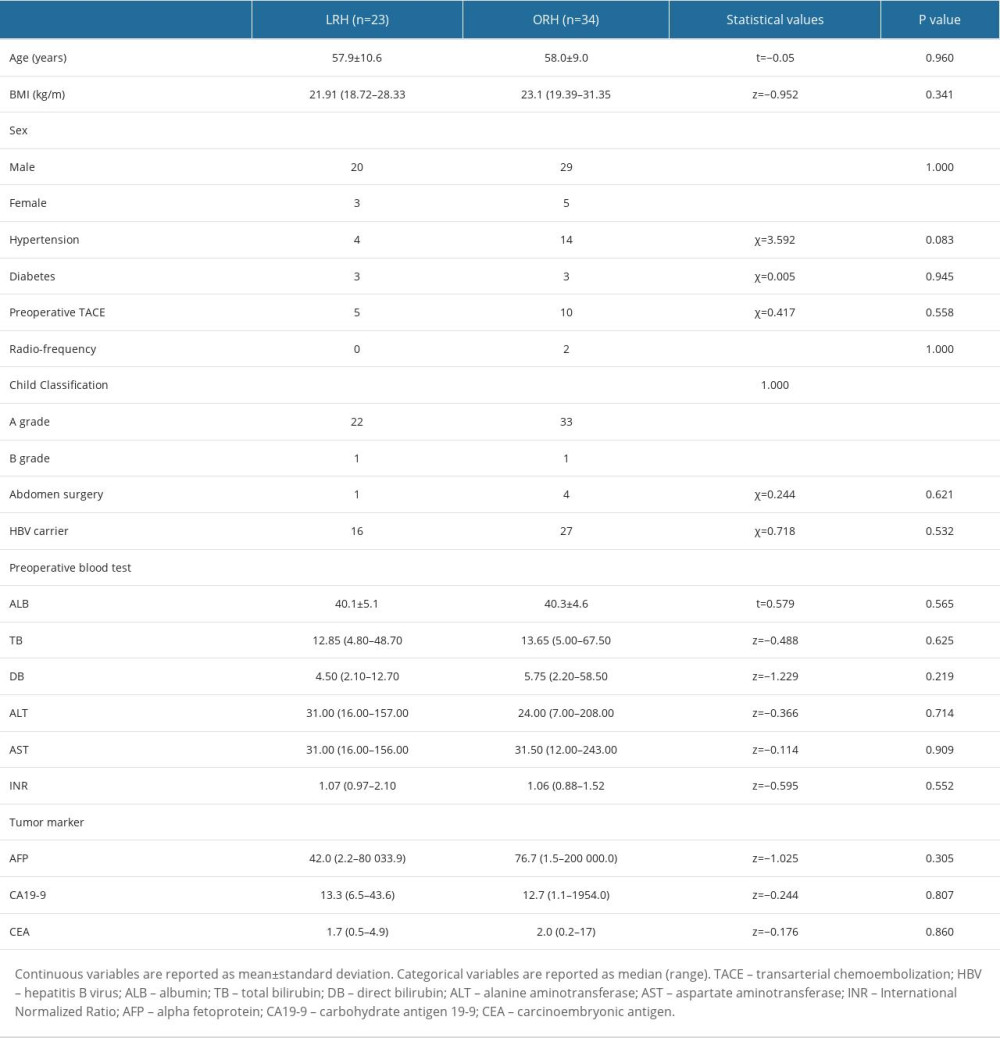
BASELINE CHARACTERISTICS:
The 57 patients were divided into 2 groups; a laparoscopic group (n=23) and an open surgery group (n=34). There was no statistically significant difference in the demographics data of the 2 groups nor in serology results such as ALB, ALT, and tumor markers (P>0.05). The baseline characteristics of the patients are summarized in Table 1.
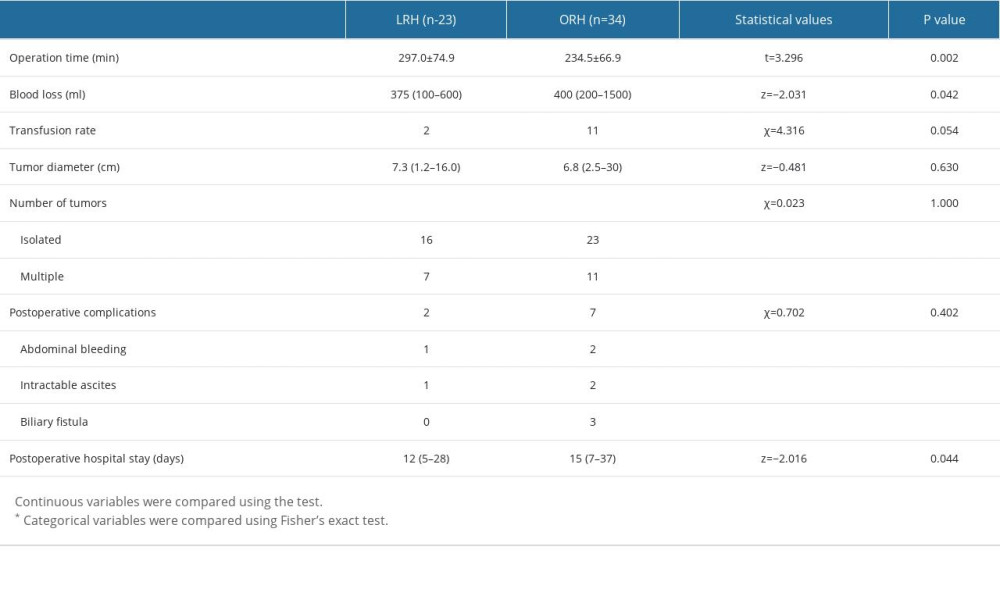
INTRAOPERATIVE AND POSTOPERATIVE CHARACTERISTICS:
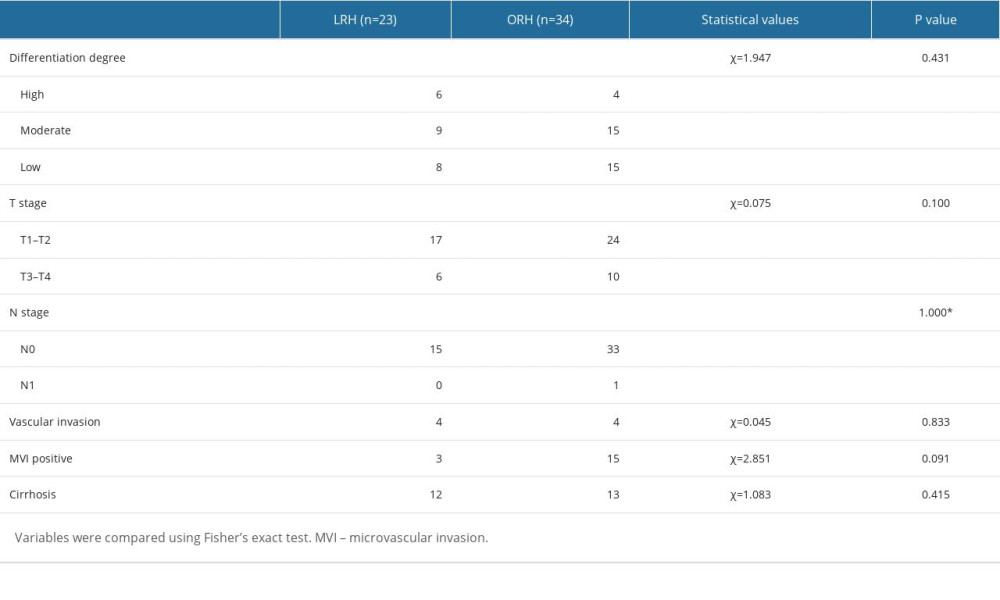
Intraoperative and postoperative data are reported in Table 2. The operation time was significantly shorter in the open group than in the laparoscopic group [(234.5±66.9) min vs (297.0±74.9) min, P=0.002]. Intraoperative bleeding was significantly less in the laparoscopic group than in the open group [375 (100–600) ml vs 400 (200–1500) ml, P=0.042]. There was a significant difference in postoperative complications between the 2 groups (8.7% vs 20.6%, P=0.402). There was 1 case of abdominal bleeding and 1 case of intractable ascites in the laparoscopic group. There were 2 cases of abdominal bleeding, 2 of intractable ascites, and 3 of biliary fistula in the open group. Hospital stay was significantly shorter in the laparoscopic group than in the open group [12 (5–28) vs 15 (7–37), P=0.05]. The pathological data of the 2 groups are detailed in Table 3. There was also no statistically significant difference in tumor differentiation (TNM stage, vascular invasion) between the 2 groups (P>0.05).
FOLLOW-UP DATA:
The last patient follow-up was in June 2022, with a follow-up period of 3–72 months. The 1-year, 2-year, and 3-year OS were 91.3% vs 82.4%, 68.5% vs 70.6%, and 68.5% vs 61.0% in the laparoscopic and open groups, respectively. The 1-year, 2-year, and 3-year DFS were 65.2% vs 78.4%, 65.2% vs 65.3%, 59.8% vs 61.2%, in the laparoscopic and open groups, respectively. There was a statistically significant difference in the OS of the 2 groups based on Kaplan-Meier survival curves (P=0.689, P=0.678). Kaplan-Meier survival curves are shown in Figure 3.
Discussion
In this study that included 57 participants, 23 in the laparoscopic group and 34 in the open surgery group, we found that baseline characteristics were significantly different between the 2 groups. The operation time was significantly shorter in the open surgery group while intraoperative bleeding was significantly less in the laparoscopic group. Hospital stay was significantly shorter in the laparoscopic group. In 1996 Edward et al first proposed an anterior approach to right hemi-hepatectomy [7]. This surgical approach involves pre-emptive control of right hepatic blood inflow, followed by right and left hemi-liver dissection and control of hepatic vein bleeding before right hemi-liver dissection. This approach to surgery avoids squeezing and pulling the tumor, thus preventing tumor cells from entering the body’s circulation through the hepatic vein. Studies have demonstrated that the open anterior approach to right hemi-hepatectomy has been widely used for treating hepatocellular carcinoma and has a better prognosis than the conventional approach [8]. Wang et al found laparoscopic hemi-hepatectomy to be safe procedure in patients with HCC [9]. Therefore, this study confirms the feasibility and safety of an anterior approach to laparoscopic right hemi-hepatectomy for hepatocellular carcinoma.
The liver is an essential organ with a very high blood supply. In laparoscopic hepatectomy, reasonable and adequate control of hepatic bleeding is a critical factor for successful completion of the operation [10]. In 1908, James Hogarth Pringle first proposed a method of portal vascular blockage in liver dissection, called the first portal blood flow block (Pringle maneuver), which is an effective method to reduce bleeding. Over the past 100 years, as technology has improved, there are now many methods of hepatic blood flow block, including the original total access maneuver (Pringle maneuver) [11], regional access maneuver, hepatic vein block, inferior hepatic vena cava block, and total hepatic blood flow block [12]. During our procedure, the right hepatic portal is first controlled by the intrathecal or extrathecal method to establish a selective right hepatic inflow control, which helps control bleeding during liver dissection and can reduce ischemia-reperfusion injury in the residual liver. It also allows for obtaining an ischemic line on the liver surface, ensuring a proper incision margin. It has been demonstrated in previous studies that in open right hepatectomy, controlling right hepatic blood flow before dissection of the liver parenchyma by using an anterior approach to the surgery helps to reduce intraoperative blood loss, which is beneficial to the patient [8,13]. In our study, intraoperative bleeding was significantly less in the laparoscopic group [375 (100–600) ml vs 400 (200–1500) ml,
Many studies have reported complications ranging from 5.4% to 35.7% after laparoscopic right hemi-hepatectomy [16,17]. Our study data showed no significant difference in postoperative complications between the laparoscopic and open groups (8.7% vs 20.6%). Chen et al found no significant difference in postoperative complications between laparoscopic right hepatectomy and conventional open surgery for hepatocellular carcinoma [18], which is similar to our findings. Similar results were reported in other studies. Komatsu et al compared laparoscopic hemi-hepatectomy for HCC to open surgery and concluded that the postoperative complication incidence rate was less in laparoscopic than in open surgery (31.6% vs 60.5%). In comparing postoperative hospital stay, it was significantly shorter in the laparoscopic group. This may translate into an overall reduction in hospital-stay-related costs for the patient. Riquelme et al also found a shorter hospital stay in patients who underwent laparoscopic hemi-hepatectomy [19] and also found a significant reduction in postoperative complications.
In radical tumor resection, an adequate surgical margin must be ensured for both laparoscopic and open surgery. In laparoscopic surgery, the inability to directly palpate the liver and magnify the operation field view can result in an inadequate resection margin. Therefore, more care should be taken to determine the resection margin. However, studies have shown that R0 resection and adequate margins can be achieved in laparoscopic anatomical hepatectomy, non-anatomical hepatectomy, or partial hepatectomy [20,21]. Furthermore, indocyanine green fluorescence imaging techniques and intraoperative ultrasound can be used to better assess and obtain adequate resection margins.
The anterior approach also follows the principle of radical tumor treatment by moving the tumor as little as possible during resection to reduce tumor dissemination and metastasis. Compared with the open anterior approach to right hepatectomy, the laparoscopic anterior approach technique requires better guidance of the hepatic plane during hepatectomy. Open surgery often uses a suspension around the liver to ensure adequate hepatic resection, which is not very effective or necessary in laparoscopy. We have adopted a standardized hepatic resection procedure based on prior experience to simplify the operation and ensure adequate resection. The standardized approach includes the following: (1) Dissection of the first hepatic hilar, using intrathecal or extrathecal method to control the blood flow into the right liver; (2) After determining the extent of the liver to be resected, transection of the liver parenchyma, paying particular attention to the dissection of the hepatic parenchyma of the caudate lobe in the front of the inferior vena cava; (3) Transecting the right hepatic hilar; (4) Expose the inferior vena cava, using the inferior vena cava as a guide, to dissect the liver tissue; (5) Finally, expose the right short hepatic and right hepatic veins and the transection of the associated veins and ligaments. The right half of the liver and the tumor are removed. The intra- and extra-hepatic ducts are used as guides during hepatic resection. In our study, R0 resection was achieved in both the laparoscopic and open groups. Based on our findings, laparoscopic hemi-hepatectomy can also ensure negative surgical margins and meet oncological requirements to achieve a curative effect.
There were several limitations to this study. This was a single-center retrospective study and as such selection bias is a limitation. The sample size of the study was relatively small; therefore, the findings of the study may have been affected by the limited sample size. To mitigate these issues, a large-sample-size multi-center study with a prospective study design is needed to validate the findings. Future studies should also include an analysis of the learning curve of laparoscopic right hemi-hepatectomy.
Conclusions
In patients with hepatocellular carcinoma, the laparoscopic right hemi-hepatectomy with the anterior approach technique has comparable safety and comparable short-term outcomes compared to open right hemi-hepatectomy. However, the operation time is comparatively longer in laparoscopic right hemi-hepatectomy.
Figures
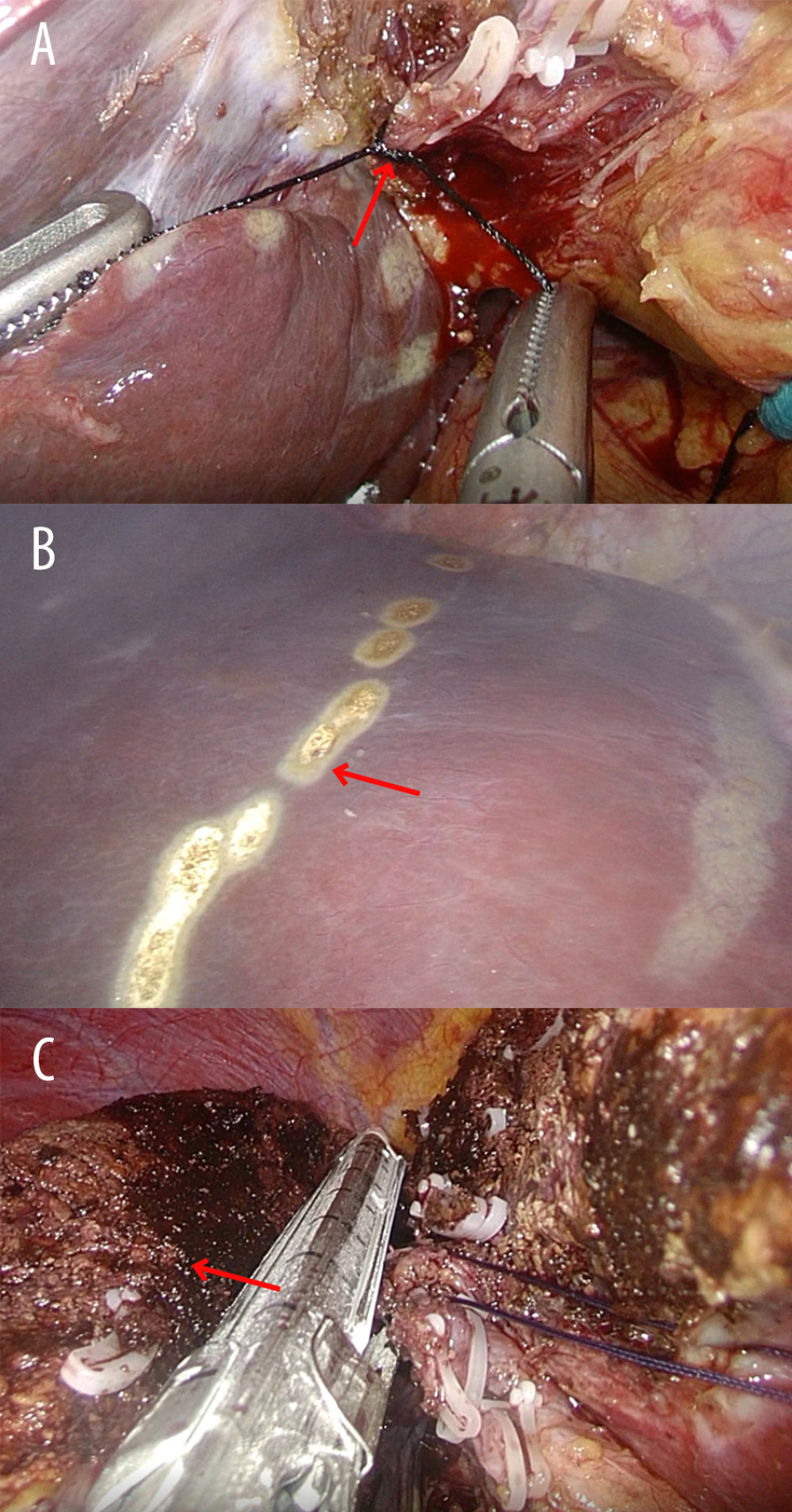 Figure 1. Intraoperative images of the laparoscopic right hemi-hepatectomy. (A) The right hepatic hilar was controlled (red arrow). (B) The resection guideline was based on the ischemic boundary (red arrow). (C) The hepatic parenchyma was transected and the right hemi-liver (red arrow) removed.
Figure 1. Intraoperative images of the laparoscopic right hemi-hepatectomy. (A) The right hepatic hilar was controlled (red arrow). (B) The resection guideline was based on the ischemic boundary (red arrow). (C) The hepatic parenchyma was transected and the right hemi-liver (red arrow) removed. 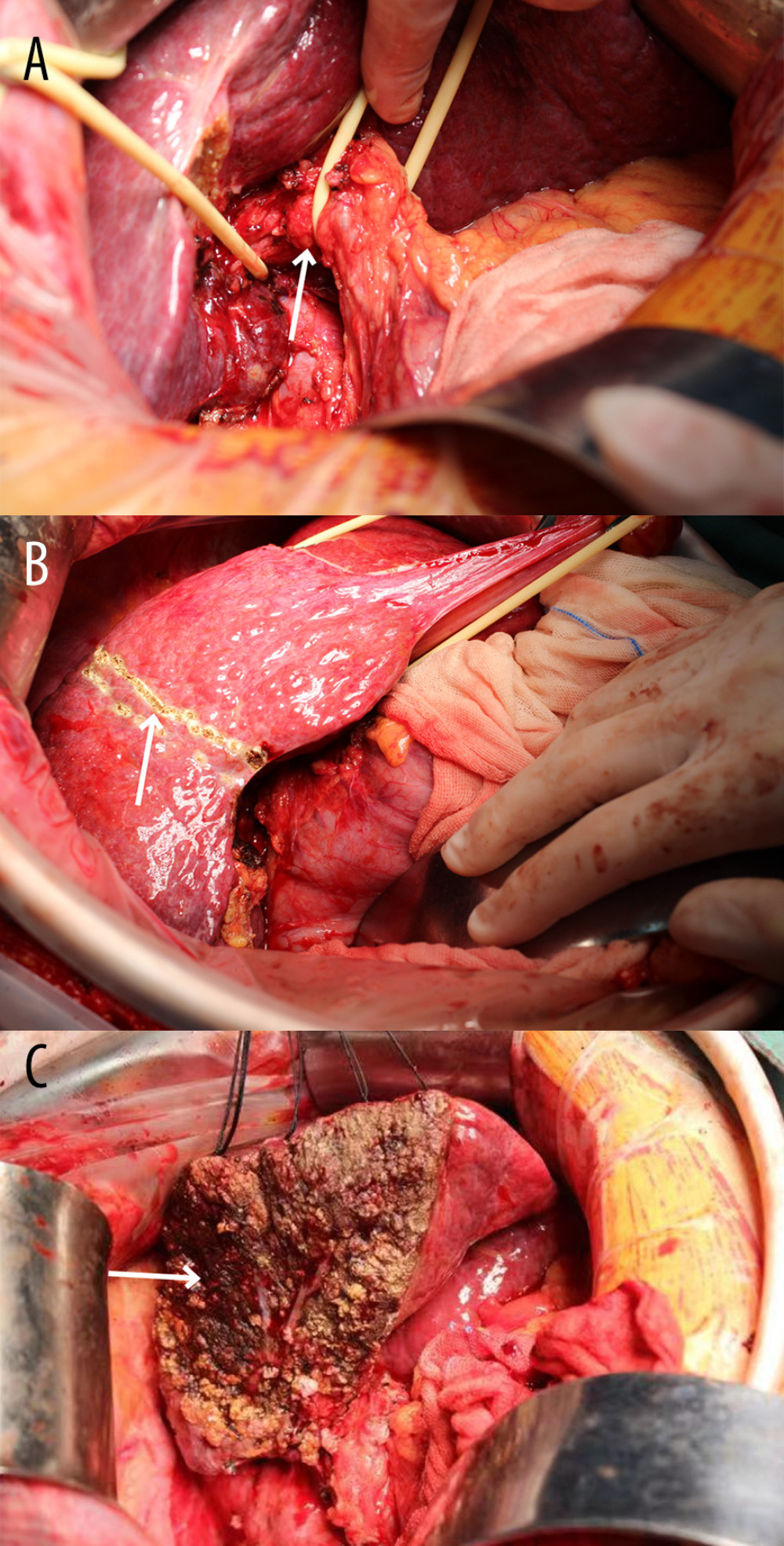 Figure 2. Intraoperative images of the open right hemi-hepatectomy. (A) Control of the first hepatic portal (white arrow). (B) Resection guideline based on the ischemic boundary (white arrow). (C) The right hemi-liver is resected and removed. The left hemi-liver remains (white arrow).
Figure 2. Intraoperative images of the open right hemi-hepatectomy. (A) Control of the first hepatic portal (white arrow). (B) Resection guideline based on the ischemic boundary (white arrow). (C) The right hemi-liver is resected and removed. The left hemi-liver remains (white arrow). 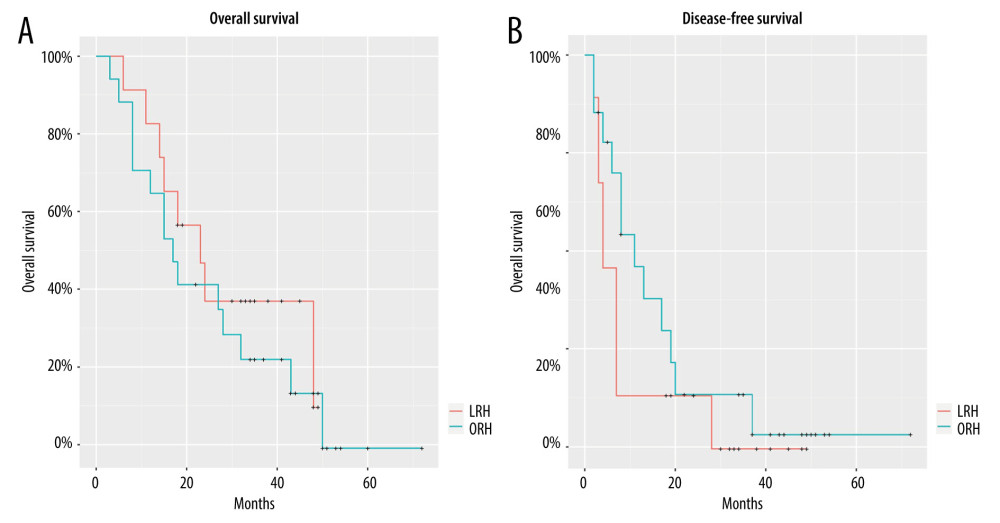 Figure 3. Kaplan-Meier survival curves. (A) Overall survival (OS) curve. (B) Disease-free survival (DFS) curve. LRH – laparoscopic right hemi-hepatectomy; ORH – open right hemi-hepatectomy.
Figure 3. Kaplan-Meier survival curves. (A) Overall survival (OS) curve. (B) Disease-free survival (DFS) curve. LRH – laparoscopic right hemi-hepatectomy; ORH – open right hemi-hepatectomy.  Video 1. Anterior approach to laparoscopic right hemi-hepatectomy.
Video 1. Anterior approach to laparoscopic right hemi-hepatectomy. References
1. Kocarnik JM, Compton KGlobal Burden of Disease 2019 Cancer Collaboration, Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 Cancer Groups from 2010 to 2019: A systematic analysis for the global burden of disease study 2019: JAMA Oncol, 2022; 8(3); 420-44
2. Basaranoglu M, Canbakan B, Yildiz K, Nonalcoholic fatty liver may increase the risk of operation in patients with fatty liver and the frequency of cancer in their first-degree relatives: Wien Klin Wochenschr, 2016; 128(19–20); 691-94
3. Boogerd LS, Handgraaf HJ, Lam HD, Laparoscopic detection and resection of occult liver tumors of multiple cancer types using real-time near-infrared fluorescence guidance: Surg Endosc, 2017; 31(2); 952-61
4. Hüscher CG, Lirici MM, Chiodini S, Recher A, Current position of advanced laparoscopic surgery of the liver: JR Coll Surg Edinb, 1997; 42(4); 219-25
5. Sultana A, Nightingale P, Marudanayagam R, Sutcliffe RP, Evaluating the learning curve for laparoscopic liver resection: A comparative study between standard and learning curve CUSUM: HPB (Oxford), 2019; 21(11); 1505-12
6. Kawaguchi Y, Honda G, Endo I, Current technical issues for surgery of primary liver cancer: Liver Cancer, 2016; 6(1); 51-58
7. Lai EC, Fan ST, Lo CM, Anterior approach for difficult major right hepatectomy: World J Surg, 1996; 20(3); 314-18
8. Liu CL, Fan ST, Cheung ST, Anterior approach versus conventional approach right hepatic resection for large hepatocellular carcinoma: A prospective randomized controlled study: Ann Surg, 2006; 244(2); 194-203
9. Wang Y, Fang J, Lin L, Laparoscopic versus open hemihepatectomy: A 1: 1 matched analysis: Ann Transl Med, 2020; 8(7); 431
10. Mizuguchi T, Kawamoto M, Nakamura Y, New technique of extracorporeal hepatic inflow control for pure laparoscopic liver resection: Surg Laparosc Endosc Percutan Tech, 2015; 25(1); e16-e20
11. Pringle JHV, Notes on the arrest of hepatic hemorrhage due to trauma: Ann Surg, 1908; 48(4); 541-49
12. Tan J, Tan Y, Zhu Y, Perioperative analysis of laparoscopic liver resection with different methods of hepatic inflow occlusion: J Laparoendosc Adv Surg Tech A, 2012; 22(4); 343-48
13. Capussotti L, Ferrero A, Russolillo N, Routine anterior approach during right hepatectomy: Results of a prospective randomised controlled trial: J Gastrointest Surg, 2012; 16(7); 1324-32
14. Cheung TT, Dai WC, Tsang SH, Pure laparoscopic hepatectomy versus open hepatectomy for hepatocellular carcinoma in 110 patients with liver cirrhosis: A propensity analysis at a single center: Ann Surg, 2016; 264(4); 612-20
15. Ryu T, Honda G, Kurata M, Perioperative and oncological outcomes of laparoscopic anatomical hepatectomy for hepatocellular carcinoma introduced gradually in a single center: Surg Endosc, 2018; 32(2); 790-98
16. Yoon YI, Kim KH, Kang SH, Pure laparoscopic versus open right hepatectomy for hepatocellular carcinoma in patients with cirrhosis: A propensity score matched analysis: Ann Surg, 2017; 265(5); 856-63
17. Landi F, De’ Angelis N, Scatton O, Short-term outcomes of laparoscopic vs. open liver resection for hepatocellular adenoma: A multicenter propensity score adjustment analysis by the AFC-HCA-2013 study group: Surg Endosc, 2017; 31(10); 4136-44
18. Chen K, Pan Y, Wang YF, Laparoscopic right hepatectomy for hepatocellular carcinoma: A propensity score matching analysis of outcomes compared with conventional open surgery: J Laparoendosc Adv Surg Tech A, 2019; 29(4); 503-12
19. Riquelme F, Muñoz C, Ausania F, Laparoscopic versus open hemihepatectomy: Comprehensive comparison of complications and costs at 90 days using a propensity method: Updates Surg, 2020; 72(4); 1041-51
20. Yoon SY, Kim KH, Jung DH, Yu A, Lee SG, Oncological and surgical results of laparoscopic versus open liver resection for HCC less than 5 cm: Case-matched analysis [published correction appears in Surg Endosc. 2015;29(9):2635]: Surg Endosc, 2015; 29(9); 2628-34
21. Sposito C, Battiston C, Facciorusso A, Propensity score analysis of outcomes following laparoscopic or open liver resection for hepatocellular carcinoma: Br J Surg, 2016; 103(7); 871-80
Figures
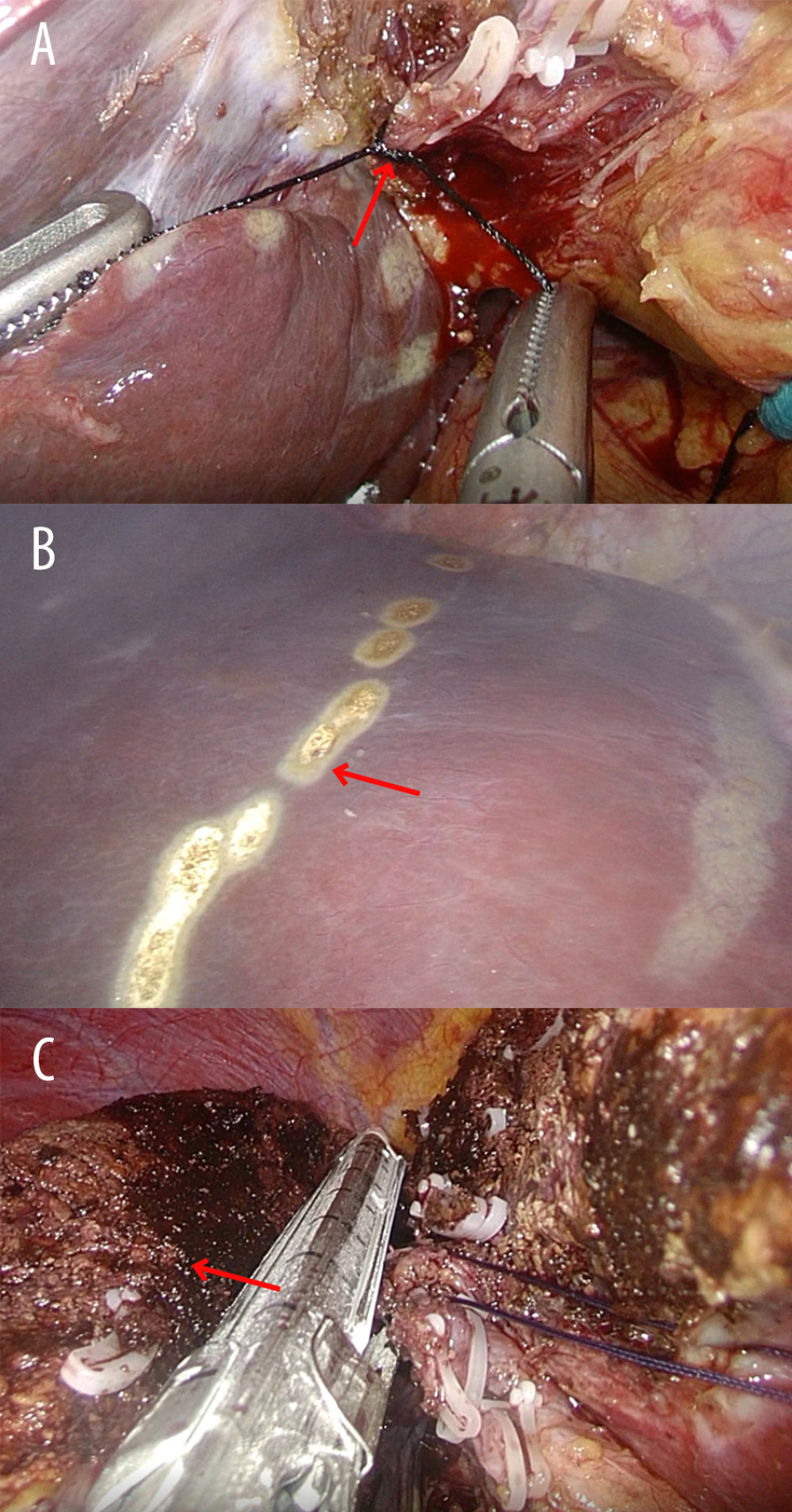 Figure 1. Intraoperative images of the laparoscopic right hemi-hepatectomy. (A) The right hepatic hilar was controlled (red arrow). (B) The resection guideline was based on the ischemic boundary (red arrow). (C) The hepatic parenchyma was transected and the right hemi-liver (red arrow) removed.
Figure 1. Intraoperative images of the laparoscopic right hemi-hepatectomy. (A) The right hepatic hilar was controlled (red arrow). (B) The resection guideline was based on the ischemic boundary (red arrow). (C) The hepatic parenchyma was transected and the right hemi-liver (red arrow) removed.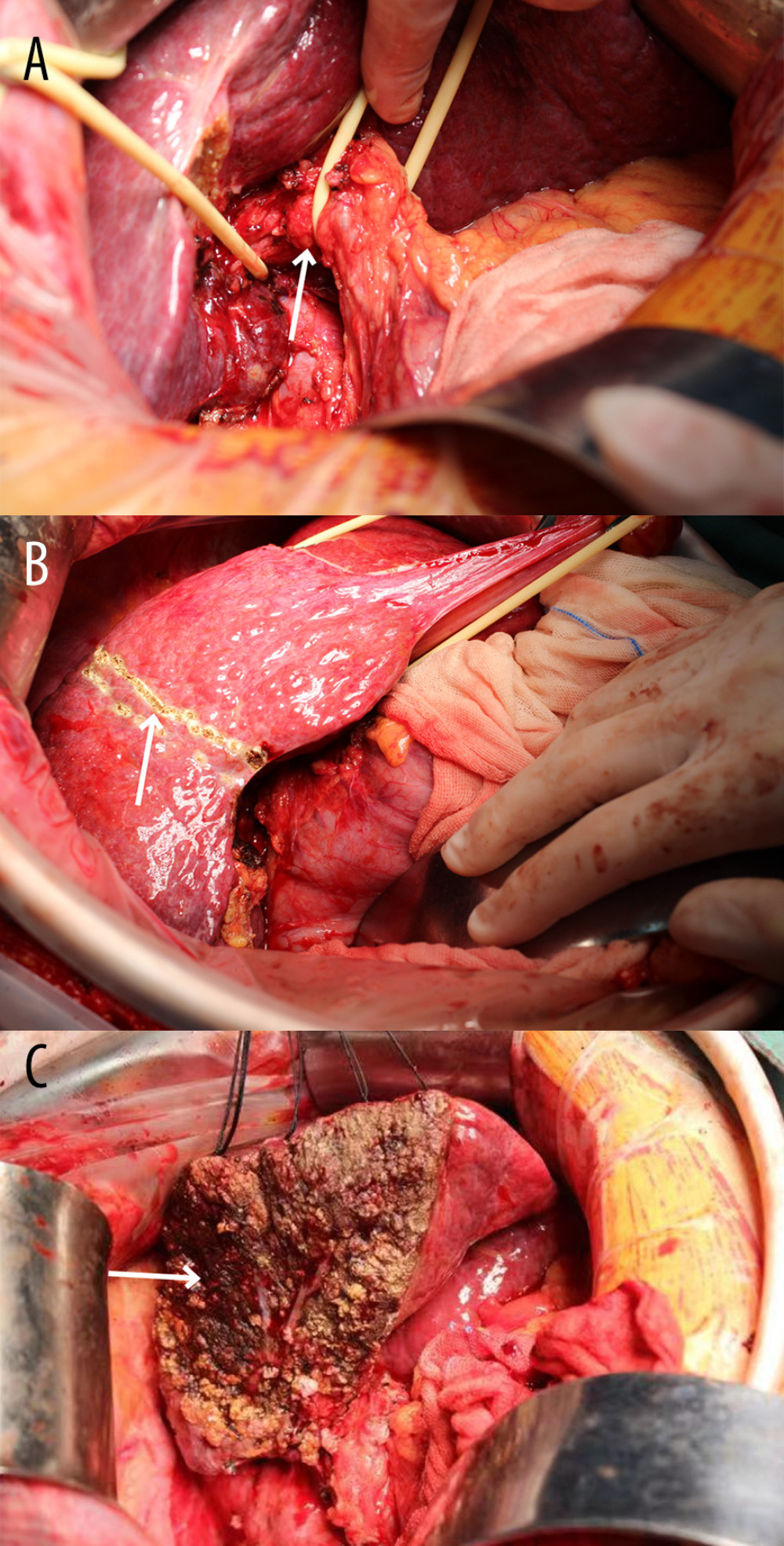 Figure 2. Intraoperative images of the open right hemi-hepatectomy. (A) Control of the first hepatic portal (white arrow). (B) Resection guideline based on the ischemic boundary (white arrow). (C) The right hemi-liver is resected and removed. The left hemi-liver remains (white arrow).
Figure 2. Intraoperative images of the open right hemi-hepatectomy. (A) Control of the first hepatic portal (white arrow). (B) Resection guideline based on the ischemic boundary (white arrow). (C) The right hemi-liver is resected and removed. The left hemi-liver remains (white arrow).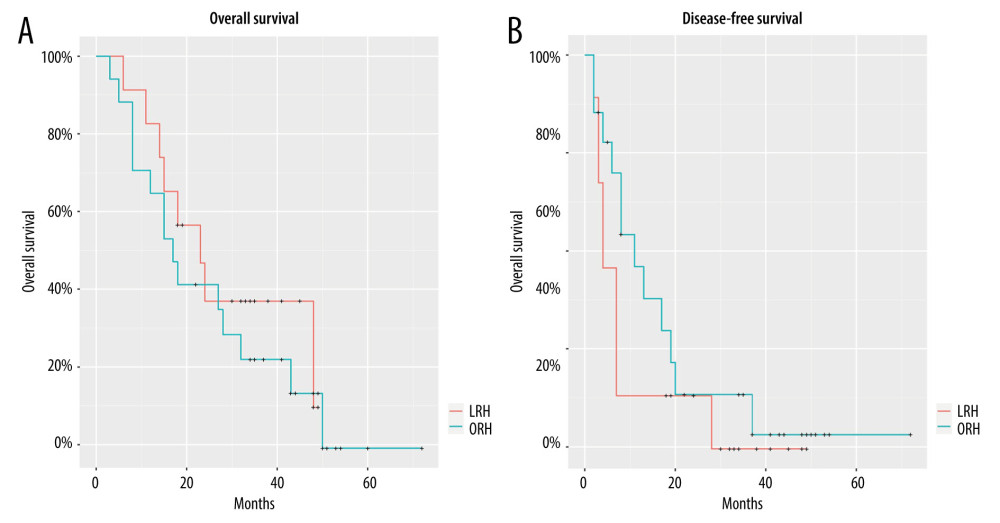 Figure 3. Kaplan-Meier survival curves. (A) Overall survival (OS) curve. (B) Disease-free survival (DFS) curve. LRH – laparoscopic right hemi-hepatectomy; ORH – open right hemi-hepatectomy.
Figure 3. Kaplan-Meier survival curves. (A) Overall survival (OS) curve. (B) Disease-free survival (DFS) curve. LRH – laparoscopic right hemi-hepatectomy; ORH – open right hemi-hepatectomy. Video 1. Anterior approach to laparoscopic right hemi-hepatectomy.
Video 1. Anterior approach to laparoscopic right hemi-hepatectomy. In Press
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952