06 November 2023: Clinical Research
Improved Outcomes in Distal Tibial Non-Union: A Retrospective Study of 8 Patients Treated with Distal Tibial Nail and Screw Fixation
Celil AlemdarDOI: 10.12659/MSM.942207
Med Sci Monit 2023; 29:e942207
Abstract
BACKGROUND: Non-union of distal tibia fractures is a challenge in orthopedic surgery and can be due to open fractures, osteopenia, infection, or failure of surgical devices. This retrospective study aimed to describe 8 patients with non-union of distal tibial fractures treated with distal tibial nail and screw fixation.
MATERIAL AND METHODS: According to the Gustilo-Anderson classification, 3 patients had type 2 open fractures, 1 had a type 3 open fracture, 1 had a type 1 open fracture, and 3 had closed fractures. The Association of Osteosynthesis AO classified 4 patients as A2, 2 as B2, and 2 as C2. Seven patients received distal supporting bolt-locking-screw nails (DSBLS) and 1 received DSBLS nail and plate in their most recent operation. Clinical outcomes were evaluated with American Orthopaedic Foot and Ankle Society (AOFAS) and Olerud-Molander scores.
RESULTS: All 8 patients were male, with a mean age of 35.5±14.6 years. Six patients had atrophic non-union, 1 had hypertrophic non-union, and 1 had infected non-union. Union was achieved in all patients. The average union time was 25.1 (range, 12-60) months, and the follow-up duration was 3.6 (range, 2-6) years. The mean Olerud-Molander score was 92.5 (range 85-100), and the mean AOFAS score was 91.2 (range, 85-100). There was no evidence of rotational deformity or shortening.
CONCLUSIONS: Distal tibial non-unions benefit from nails with DSBLS system due to their excellent biomechanical properties. These nails facilitate union and allow patients to bear weight early in the postoperative period, enabling a quicker return to normal activities.
Keywords: Tibia, Fracture Fixation, Intramedullary, Pseudarthrosis
Background
One of the most frequent consequences of fracture is fracture non-union. In tibial fractures, the rate of non-union is close to 1.1% if treated nonoperatively and nearly 5% if treated operatively [1]. Delayed union is defined as the absence of radiographic healing 3–5 months following the injury in tibia diaphyseal fractures. For fractures that had not healed after 9 months, non-union was described [2]. The factors contributing to non-union include: high-energy fractures with significant comminution, extensive soft tissue and periosteal stripping, bone loss, fracture gaps, lack of cortical continuity, infection, smoking, diabetes, inadequate blood supply, vitamin D deficiency, inadequate stabilization, and biological factors dependent on the patient host and surgical technique [1,3,4]. Operative and nonoperative treatment options are available. The most often used nonoperative treatments include conservative treatment and early weight-bearing, electrical stimulation in the electromagnetic field, low-intensity pulsed ultrasound, injection of bone marrow aspirate percutaneously, and extracorporeal shock wave therapy. The main factor to consider when developing a surgical plan to treat a case of tibial non-union is whether the non-union is septic or aseptic. When treating septic tibial non-unions, a phased approach is the criterion standard [5,6], while controlling aseptic tibial non-union can be accomplished with just 1 operation. A single-stage technique entails surgical debridement of all non-viable bone ends and tissues, numerous cultures to be collected from the non-union site, canal reaming, revision open reduction, internal fixation, and/or exchange nailing. Debridement, treatment of bone defects, local antibiotic elution, and, ultimately, surgery are the typical 4 steps of a staged approach [7]. Nail dynamization and nail exchange, fibular osteotomy (partial fibulectomy), open reduction and internal fixation with plate and screws, locking compression plates, external fixation, bone grafting, and cell treatment are the most often utilized surgical methods. Amputation may be an option if satisfactory functional results cannot be obtained [8]. In a study comparing the use of plate and screw nails in distal tibia fractures, general complications were found to be similar after 12 months [9].
Intramedullary nails (IMN) may be preferred due to open fracture and history of many operations of patients presenting with non-union, and also because IMN requires less soft-tissue dissection. A three-point fixation inside the diaphysis is required for IMN. However, the IMN will not be able to maintain 3-point fixation in the metaphysis, thus transverse locking screws must be used in place of 1 distal locking screw to maintain stabilization of the fracture reconstruction [10]. In a study examining the effect of the number of distal locking screws on union, Mohammed et al stated that the use of a single screw distally increased the risk of non-union and recommended the use of 2 screws [10], but occasionally the fracture level precludes distal locking in conventional methods. In this aspect, a system created in Turkey and employed in earlier studies is useful. The distal supporting bolt-locking screw (DSBLS), a type of distal locking system, was created to establish a solid anchor point, prevent angulation and rotation, and permit axial compression. This system has been shown to be successful in other studies [11].
We chose this nail for the treatment of non-union of distal tibia fractures due to its high union rates [12] and superior biomechanical properties [13] demonstrated in fracture management. Therefore, this retrospective study describes 8 patients with non-union of distal tibial fractures treated with distal tibial nail and screw fixation.
Material and Methods
PATIENTS AND STUDY DESIGN:
Ethics approval was obtained from the local ethics committee of the university. Written informed consent was obtained from the patients. Eight patients with non-unions of the distal tibia who received intramedullary nails (IMN) with the distal supporting bolt-locking screw DSBLS (TST, Istanbul, Turkey) between 2013 and 2019 at a single facility were included in the study. The demographic characteristics were examined from medical records. Additionally, findings such as types of non-union, follow-up durations, time to full union, deformities, shortening, neurovascular complications, and knee and subtalar joint movements were noted after both radiological and clinical evaluations. The fractures were classified according to the Association of Osteosynthesis (AO) classification, and open fractures were classified using the Gustilo-Anderson classification.
INCLUSION AND EXCLUSION CRITERIA:
Patients needed to have a non-union of the distal tibia and a fracture line that did not penetrate the articular surface to be eligible for the trial. Inclusion required a follow-up time of at least 1 year. All cases were included, regardless of the initial course of action or any side effects, including external fixation or a past infection history. The study excluded patients with insufficient follow-up time, those under the age of 18 years, and those who had surgery for a non-union or malunion in the proximal or middle tibia. Non-union was characterized as either a fracture that failed to heal within 6 months or an internal fixation that failed earlier than this.
SURGERY TECHNIQUE AND IMPLANT FEATURES:
Although surgical procedures may have shown some variations based on previous surgeries and existing implants, the intramedullary nailing method with distal supporting bolt-locking screw DSBLS was consistently applied to all patients as follows:
Approximately 3 cm proximal to the distal tip of the medial malleolus and the midpoint of the tibia in the sagittal plane was chosen as the usual place of application for the DSBLS. The DSBLS was then put into a predrilled channel in the distal tibia from the medial to the lateral side. The chosen unreamed nail was then inserted from the usual location of insertion in the proximal tibia after this. Ahead of the engagement of the nail with the DSBLS, the nail was advanced through the medulla. Fluoroscopy can be used to verify whether the engagement was successful. The nail does not need to precisely align with the distal locking screw. Using a Kirschner wire, another method of confirmation was developed without the use of fluoroscopy. It is impossible to advance the wire in the set screw hole by more than 5 mm if the nail is successfully engaged. The set screw, which was 18 mm shorter than DSBLS, completed distal locking. Two screws were used in all patients, and a proximal guide that was attached to the nail was used to perform the proximal interlocking. There are 2 distal screw holes on the distal nail for those who want to use the conventional nailing method. However, the conventional method was not used in any of our cases (Figure 1). Another technique for distal locking involved inserting the nail up to a few centimeters above the location of the DSBLS, screwing it precisely below the nail’s tip, and then pushing the nail into its ultimate position. One of our cases is shown in Figure 2.
POSTOPERATIVE FOLLOW-UP PROTOCOL:
Ankle and knee exercises began the day following surgery. Follow-up patients were advised to bear weight as tolerated or entirely. AP and lateral radiographs were taken until full union or until the follow-up. An impartial radiologist blinded to therapy measured all radiographic alignment. If the fracture site was not sensitive, full weight-bearing was painless, and orthogonal radiographs showed a bridging callus, the non-union was declared healed. The tuberositas tibia region to the inferior margin of the medial malleolus was the tibia’s length. Greater than 5° ante-/recurvation, greater than 5° varus/valgus deformity, or greater than 15° rotation discrepancy were all considered to be signs of misalignment.
TREATMENT OUTCOME MEASURES:
The patients’ ankle clinical scores were assessed using the AOFAS (American Orthopaedic Foot and Ankle Society) and the Olerud-Molander Ankle Score (OMAS) systems. The Olerud-Molander Ankle Score (OMAS) is a self-administered patient questionnaire. The measure is based on 9 separate items, including pain, stiffness, swelling, stair climbing, running, jumping, squatting, supports, and activities of daily living, and ranges from 0 (fully impaired) to 100 (entirely unimpaired).
STATISTICAL ANALYSIS:
We evaluated our data using descriptive statistical techniques (mean, standard deviation, median, and frequency).
Results
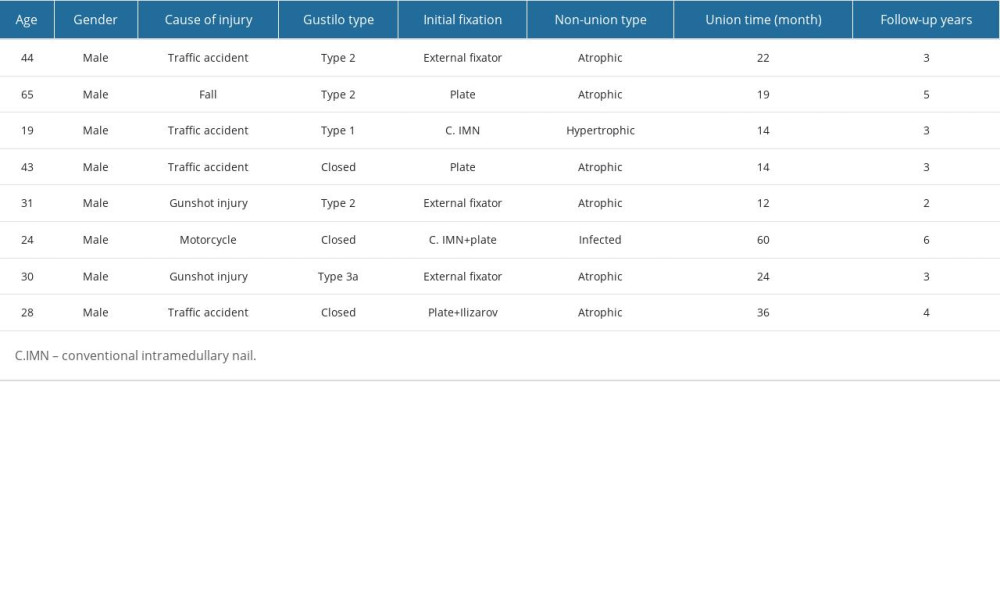
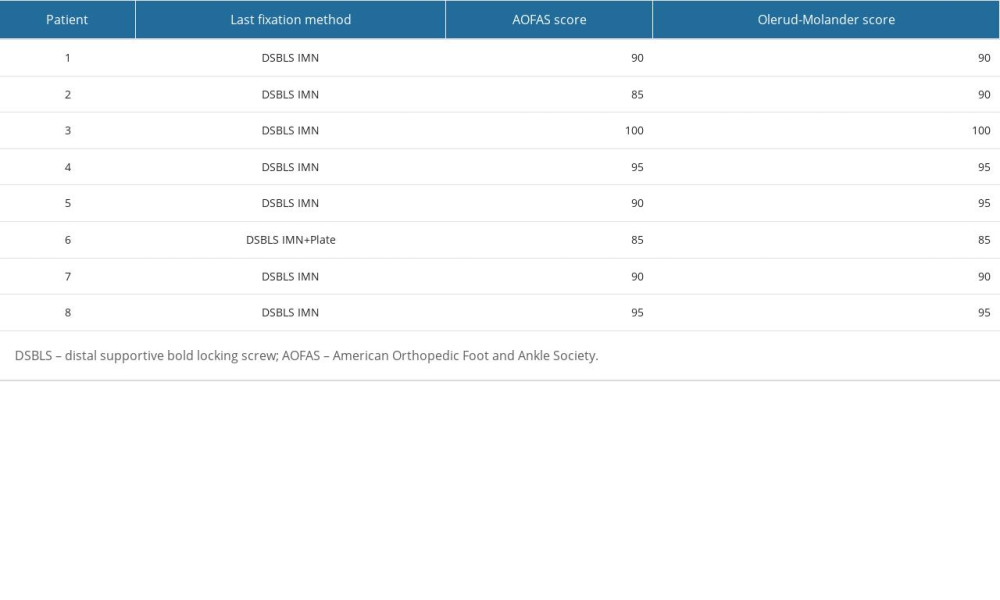
The mean age of the patients was 35.5±14.6 years. All patients were male. According to the Gustilo-Anderson classification, 3 patients had a type 2, 1 patient had a type 1, and 1 patient had a type 3 open fracture, while 3 patients had closed fractures. Based on the Association of Osteosynthesis (AO) classification, 4 patients were classified as A2, 2 as B2, and 2 as C2. Among the patients, 6 had atrophic non-union, 1 had hypertrophic non-union, and 1 had infected non-union. The average follow-up period was 3.6 years (range, 2–6). Complete union was achieved in all patients, with an average union time of 25.1 months (range, 12–60). The initial trauma types of the patients were: 4 cases were due to car accidents (50%), 2 cases were caused by gunshot wounds (25%), 1 case was due to a motorcycle accident (12.5%), and 1 case was a result of a fall from a height. Regarding previous surgeries; 3 patients (37.5%) had external fixators, all of whom presented with open fractures. Two patients (25%) had plates, 1 patient (12.5%) had a plate followed by an Ilizarov fixator, 1 patient (12.5%) had a conventional intramedullary nail (IMN), and 1 patient (12.5%) had undergone a conventional IMN followed by a plate (Table 1). For the patient with infected non-union, the plate was removed, and debridement and a 9-cm bone resection were performed. Limb reconstruction was carried out using the distal supporting bolt-locking screw (DSBLS) system and the limb reconstruction system (LRS). This patient, diagnosed with Fallot tetralogy, had the longest follow-up time (60 months) and received a skin graft. This and another patient who had previously undergone fasciotomy were among the 3 patients with skin problems. In the patient who had previously undergone conventional IMN, the preoperative valgus angle of the 18-degree fracture was corrected to 2° postoperatively. In 1 patient with a preoperative malalignment apex anterior of 14°, the postoperative malalignment was reduced to 3°. Similarly, in another patient who had undergone previous fixation, the apex anterior angle, which was initially 15°, was reduced to 0°, and the valgus angle was decreased from 6° to 2°. Unfortunately, in the patient with a previous plate, the preoperative 10° apex posterior angle increased to 12° postoperatively, but no symptoms or additional complications were observed during the follow-up. Two patients experienced infection – 1 had anterior knee pain and 1 had ankle motion limitation. No rotational deformity or shortening was observed. The average American Orthopaedic Foot and Ankle Society (AOFAS) score was 91.2 (range, 85–100), and the average Olerud-Molander score was 92.5 (range, 85–100) (Table 2).
Discussion
In this study, we examined 8 cases of distal tibial pseudoarthrosis. All patients were male and had previously experienced high-energy injuries. Among them, 5 had open fractures, 3 had closed fractures, and all had undergone prior surgeries with different implants. All patients were treated using an intramedullary nail (IMN) system featuring a screw system known as the distal supporting bolt-locking screw (DSBLS). Early weight-bearing was permitted, and early physical therapy was initiated. Follow-up assessments revealed successful union in all patients, with no need for implant removal. Previous deformities have been largely corrected. No cases showed shortening or rotational deformity. The 2 patients with infections had undergone the most prior surgeries. The lengthy mean time to a union may be a result of the fact that the duration of complete union and the duration of patients’ full functional capacity overlap to some extent. It was seen that the complications were not caused by the implant.
The principal benefits of this technique include a short learning curve, the ability to lock even distal tibia fractures just above the joint, the use of percutaneous placement for skin issues common in non-union patients with a history of multiple surgeries, the preservation of vascular support without the need for a new incision, and the ability to immediately resume postoperative ankle movements. Patient can also bear their entire weight on the first postoperative day because DSBLS and a nail together make a load-bearing structure that resembles an inverted “T” inside of a bone and has a set angle [14].
Inherent disadvantages of plate fixation include substantial soft-tissue removal, disruption of periosteal blood flow, wound complications, infection, and postoperative ankle stiffness. In their randomized controlled multicenter trial, Costa et al compared using plates and nails to treat distal tibial fractures. At the 3-month evaluation, the disability rating index was higher in patients in the plaque group. At 6 months, there was no discernible difference between the outcomes, but the plaque group experienced more secondary surgeries. Nailed group patients began to bear their entire weight earlier. At 6 months, it was discovered that the nail group had a higher Olerud-Molander Ankle Score (OMAS) score. At 3 and 6 months, the secondary outcome measures overall were better in the nail group, but at 12 months, there was not a significant difference [9]. As in the Costa et al study, our patients were able to initiate early physical therapy despite soft-tissue damage due to previous surgeries. Additionally, they had the opportunity for early full weight-bearing, thereby increasing the stimulation for union and allowing them to return to their normal lives sooner. In the present study and in the study by Costa et al, OMAS scores were satisfactory during follow-up.
IMN is the preferred line of action for tibial non-unions [15]. However, if the fracture line extends too far distally, conventional IMNs might not be adequate. Reamed nails improve endosteal circulation and have positive impacts on biomechanics. Unreamed nails provide less stability while preserving endosteal circulation. Both systems are incapable of supporting a patient’s full weight right away due to distal interlocking-related instability. Distal locking is also to blame for a significant loss of surgical time and most of the necessary fluoroscopy. Attempts have been made to treat fractures close to the joint by cutting the nail tip from the last distal locking screw. However, the outcome unexpected, because this technique did not permit early loading [16]. The impact of the number of screws used in distal locking on union in distal tibia fractures was investigated by Mohammed et al. In their study, among 65 patients who underwent nail fixation, non-union was observed in 15 of them. Among the patients with non-union, 80% had experienced high-energy trauma, and 10 had a history of open fractures. It was observed that in 12 of these 15 patients, a single screw was used distally. The study indicated that the use of a single screw distally significantly increased the risk of non-union [10]. Our patients also experienced high-energy trauma, and 5 of them had open fractures. The DSBLS IMN system we used is biomechanically superior to conventional nails that use a single screw. The distal locking of nails has been examined biomechanically. In the first group the IMN nail was fixed with 2 screws from the distal, 3 screws from the distal in the second group, a DSBLS screw from the distal in the third group, and 3 screws of varying diameters in the fourth group. In terms of axial loading force, DSBLS was discovered to be noticeably better when compared to triple and double distal locking options [13]. This IMN system allows for robust fixation using an unreamed technique that allows for immediate full weight-bearing and needs just minimal fluoroscopy for distal locking. As far as we are aware, this design IMN with DSBLS offers the most remote interlocking option among the IMNs that are now on the market [12].
Forthy-eight patients who had distal tibia dia-metaphyseal fractures treated with IMNs distally locked with DSLBS were assessed in a study. All fractures consequently healed together. Six patients had a satisfactory functional evaluation, whereas 42 patients received an excellent evaluation. None of the patients had any DSLBS loosening, migration, or breaking [11]. In a study examining the treatment of distal tibial fractures, including Gustilo type I and II fractures, 24 patients were treated with the DSBLS IMN nail system and 22 patients were treated with conventional IMN. Patients who received DSBLS IMN treatment were able to bear their entire weight faster and for longer, and their fractures healed more quickly. In the DSBLS group, patients had higher OMAS scores (93.96±6.91) and AOFAS scores (93.46±8.09) compared to the conventional IMN group [17]. These clinical scores are similar to our patients’ scores. Union was achieved in all patients in both studies, as well as in our study. No implant-related problems were observed.
The findings of this study need to be interpreted considering certain limitations, such as the small sample size and the single-center, retrospective design. Due to the limited number of patients, statistical calculations are limited; therefore, the generalizability of the results is low. Retrospective studies can sometimes introduce bias risks. Additionally, as a limitation in the methodology, not comparing the patient group with the same concern but with a different implant could be considered. The metabolic factors and lifestyles that may affect bone union in patients were not thoroughly examined. Due to the larger distal screw of this nail system compared to standard screws, caution must be exercised during application to avoid fracture, but such a complication has not been reported yet. A prospective, multicenter, randomized, controlled trial would make the results more objective and generalizable.
Conclusions
The non-union of distal tibia fractures is a significant concern for both patients and surgeons. When treating these fractures, it is crucial to use methods and implants that minimize complications, facilitate union, and allow for an earlier return to normal life. The nail and screw system we used in this study provided these features.
Figures
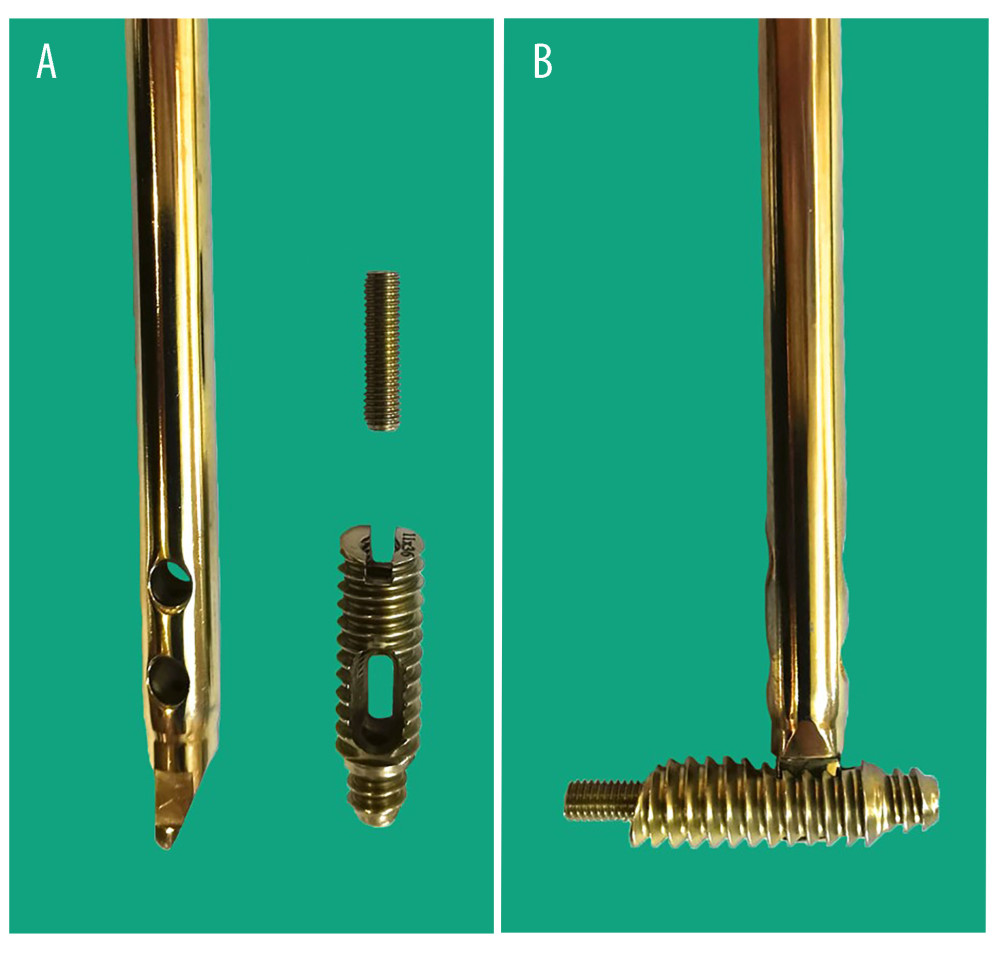 Figure 1. (A) The distal supportive bold locking screw (DSBLS), set screw, and set screw hole are shown. The distal end of the intramedullary nail has a unique design that allows contact with the DSBLS. (B) After the engagement, the design enables strong fixing of the nail within the DSBLS using a set screw. Figure 1 was taken with a smartphone and transferred to the computer. The background color was adjusted using Photoshop CC 2019.
Figure 1. (A) The distal supportive bold locking screw (DSBLS), set screw, and set screw hole are shown. The distal end of the intramedullary nail has a unique design that allows contact with the DSBLS. (B) After the engagement, the design enables strong fixing of the nail within the DSBLS using a set screw. Figure 1 was taken with a smartphone and transferred to the computer. The background color was adjusted using Photoshop CC 2019.  Figure 2. (A–D) Distal supportive bold locking screw nail (DSBLS) system and autograft were used to treat a 44-year-old male patient who had previously received an external fixator and plaster treatment for a Gustilo type 2 open fracture but failed to achieve union. Figure 2 was captured as a screenshot from the PACS Infinitt system used in the hospital and transferred to the computer. No additional processing was performed.
Figure 2. (A–D) Distal supportive bold locking screw nail (DSBLS) system and autograft were used to treat a 44-year-old male patient who had previously received an external fixator and plaster treatment for a Gustilo type 2 open fracture but failed to achieve union. Figure 2 was captured as a screenshot from the PACS Infinitt system used in the hospital and transferred to the computer. No additional processing was performed. References
1. Rodriguez-Buitrago AF, Mabrouk A, Jahangir A, Tibia nonunion: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing [cited 2023 Sep 3]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK526050/
2. Wiss DA, Stetson WB, Tibial nonunion: Treatment alternatives: J Am Acad Orthop Surg, 1996; 4(5); 249-57
3. Rivera-Saldívar G, Martínez-González CA, Manejo y presentación de las fracturas transtrocantéricas de cadera durante la pandemia de COVID-19 en un hospital de tercer nivel de atención: Cir Cir, 2023; 91(3); 368-74 [in Spanish]
4. Yiğit Ş, Arslan H, Akar MS, şahin MA, Mid-term outcomes of surgical treatment in fractures in patients with osteopetrosis: Bone Jt J, 2020; 102-B(8); 1082-87
5. Bose D, Kugan R, Stubbs D, McNally M, Management of infected nonunion of the long bones by a multidisciplinary team: Bone Jt J, 2015; 97-B(6); 814-17
6. Akar MS, Ulus SA, Durgut F, Dönmez S, Complications and difficulties due to bonesetter in the treatment of pediatric distal humerus fractures: J Clin Trials Exp Investig, 2023; 2(1); 38-44
7. Chaudhary MM, Infected nonunion of tibia: Indian J Orthop, 2017; 51(3); 256-68
8. Devnani AS, Simple approach to the management of aseptic non-union of the shaft of long bones: Singapore Med J, 2001; 42(1); 20-25
9. Costa ML, Achten J, Griffin J, Effect of locking plate fixation vs intramedullary nail fixation on 6-month disability among adults with displaced fracture of the distal tibia: The UK FixDT randomized clinical trial: JAMA, 2017; 318(18); 1767-76
10. Mohammed A, Saravanan R, Zammit J, King R, Intramedullary tibial nailing in distal third tibial fractures: Distal locking screws and fracture non-union: Int Orthop, 2008; 32(4); 547-49
11. Sağlam N, Söylemez MS, Türkmen I, Akpınar F, Dia-metaphyseal fractures of the distal tibia treated with intramedullary nails distally locked with an innovative locking system: A retrospective clinical study: Eur J Trauma Emerg Surg, 2021; 47(4); 1249-57
12. Küçükdurmaz F, Akpınar F, Saka G, A newly designed intramedullary nail with distal interlocking system for tibia fractures in adults – the clinical results, 2012; 18(3); 243-49
13. Kaya YE, Celik M, Kuru T, Biomechanical comparison of distal interlocking methods in sheep tibia models, used in fixation of distal tibia shaft fractures with intramedullary nails: Abant Med J, 2019; 8(2); 52-64
14. Küçükdurmaz F, Sağlam N, Kurtulmuş T, Akpınar F, A novel intramedullary nail for use in the treatment of supramalleolar malunion and nonunion: A preliminary report of three cases: Acta Orthop Traumatol Turc, 2016; 50(5); 578-83
15. Gálvez-Sirvent E, Ibarzábal-Gil A, Rodríguez-Merchán EC, Treatment options for aseptic tibial diaphyseal nonunion: A review of selected studies: EFORT Open Rev, 2020; 5(11); 835-44
16. Gorczyca JT, McKale J, Pugh K, Pienkowski D, Modified tibial nails for treating distal tibia fractures: J Orthop Trauma, 2002; 16(1); 18-22
17. Koca H, Duman S, Sağlam N, Radiographic and clinical outcomes of distal tibia fractures (3 to 12 cm proximal to the plafond): Comparison of two intramedullary nailing: Ulus Travma Acil Cerrahi Derg, 2022; 28(5); 686-92
Figures
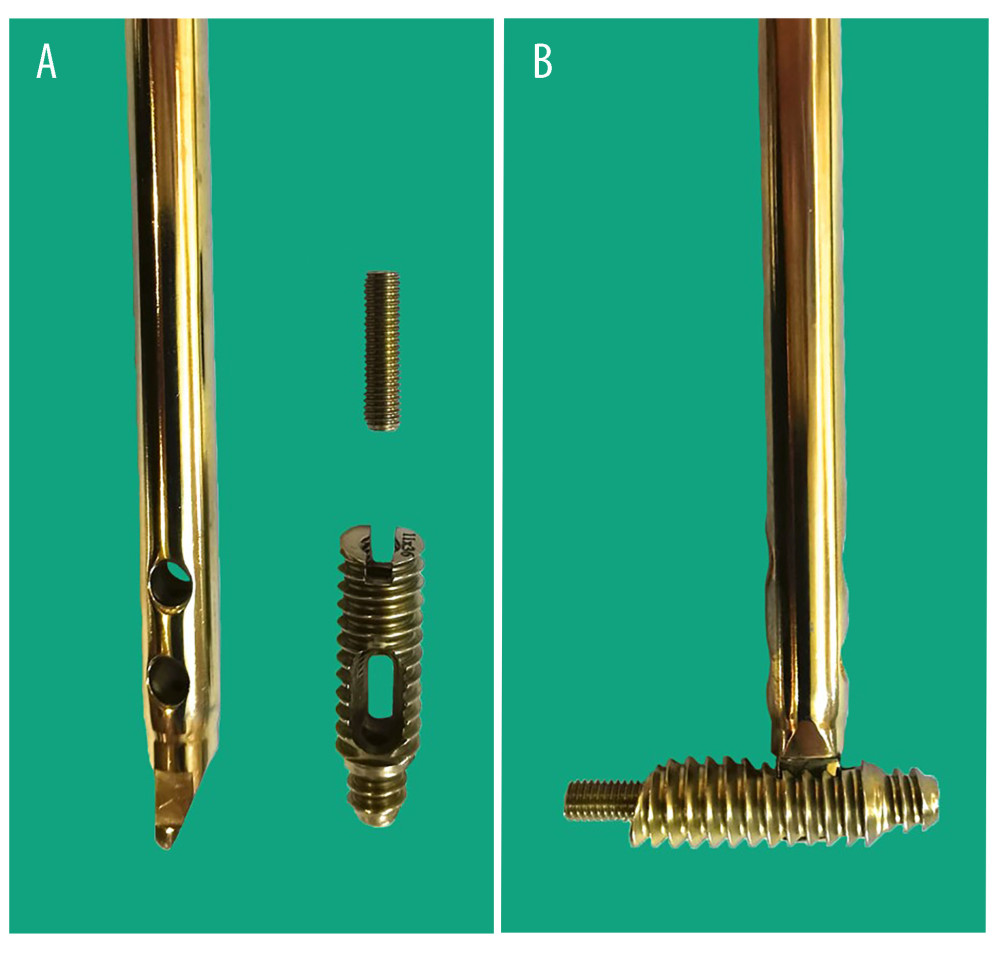 Figure 1. (A) The distal supportive bold locking screw (DSBLS), set screw, and set screw hole are shown. The distal end of the intramedullary nail has a unique design that allows contact with the DSBLS. (B) After the engagement, the design enables strong fixing of the nail within the DSBLS using a set screw. Figure 1 was taken with a smartphone and transferred to the computer. The background color was adjusted using Photoshop CC 2019.
Figure 1. (A) The distal supportive bold locking screw (DSBLS), set screw, and set screw hole are shown. The distal end of the intramedullary nail has a unique design that allows contact with the DSBLS. (B) After the engagement, the design enables strong fixing of the nail within the DSBLS using a set screw. Figure 1 was taken with a smartphone and transferred to the computer. The background color was adjusted using Photoshop CC 2019. Figure 2. (A–D) Distal supportive bold locking screw nail (DSBLS) system and autograft were used to treat a 44-year-old male patient who had previously received an external fixator and plaster treatment for a Gustilo type 2 open fracture but failed to achieve union. Figure 2 was captured as a screenshot from the PACS Infinitt system used in the hospital and transferred to the computer. No additional processing was performed.
Figure 2. (A–D) Distal supportive bold locking screw nail (DSBLS) system and autograft were used to treat a 44-year-old male patient who had previously received an external fixator and plaster treatment for a Gustilo type 2 open fracture but failed to achieve union. Figure 2 was captured as a screenshot from the PACS Infinitt system used in the hospital and transferred to the computer. No additional processing was performed. In Press
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952