02 March 2024: Clinical Research
Early Mobilization in Pediatric Critical Care: Exploring the Gap Between Theory and Practice in Saudi Arabia
Samah Al-Harbi12ABCDEFG*DOI: 10.12659/MSM.942467
Med Sci Monit 2024; 30:e942467
Abstract
BACKGROUND: Because of advancements in critical care, Pediatric Intensive Care Units (PICUs) have experienced improved survival rates. However, PICU-acquired frailty and cognitive deficits continue to be issues. In PICUs, early mobilization is emerging as a useful technique. The present study assesses early mobilization awareness, opinions, and practices among pediatric critical care providers in Saudi Arabia.
MATERIAL AND METHODS: From July 2020 to February 2021, a survey was undertaken in Saudi Arabia, targeting 110 physicians, 200 nurses, 30 respiratory therapists, and 20 physiotherapists. It concentrated on emergency medicine practices, operational issues, initiation time, rehabilitation modalities, and PICU staff strain.
RESULTS: The results showed that 64.7% of the 266 respondents were nurses, usually working in 5- to 15-bed ICUs providing medical and surgical treatment. Early mobilization was evaluated as highly significant by 40.6% of the respondents. Equipment constraints (63.5%), patient medical instability (67.3%), endotracheal intubation complications (65.4%), and personnel limits (56.4%) were major challenges. Non-physicians cited space constraints 38.9% of the time, whereas physicians cited safety concerns 47.4% of the time. Respiratory physiotherapy and passive range-of-motion exercises were the most used rehabilitation techniques (77.8%). Only 38.7% of patients with ICU-acquired weakness were referred for outpatient therapy.
CONCLUSIONS: The study emphasizes the importance of early mobilization in Saudi Arabian pediatric critical care while also recognizing considerable limitations. Addressing these difficulties necessitates a multidisciplinary, strategic approach. Future research should strive to standardize practices to enhance patient outcomes and develop standards in pediatric critical care.
Keywords: Early Ambulation, Intensive Care Units, Pediatric, Muscle Weakness, Rehabilitation, Saudi Arabia
Background
Advances in understanding and technology have significantly improved the survival rate of children in pediatric intensive care units (PICUs) [1]. However, a considerable increase in the number of survivors with moderate or severe disabilities has been observed over the past 3 decades, despite a decline in mortality rates and stability in the length of stays in pediatric critical care units and the severity of illnesses [2]. This has negatively impacted the quality of life for survivors and their families, leading to the phenomenon of post-intensive care syndrome (PICS) [3–6]. PICS is poorly understood in pediatrics, with limited case series and longitudinal studies [7]. However, it is thought that ICU-acquired weakness involves decreased contractility, muscle atrophy, anabolic resistance, mitochondrial dysfunction, and calcium homeostasis issues [8]. Yuan et al cited that more than half of patients who are discharged from critical care units suffer from PICS [9]. Knoester et al (2008), using the Nederlandse Organisatie voor Toegepast-Natuurwetenschappelijk Onderzoek-Academisch Ziekenhuis Leiden (TNO-AZL) Preschool Children Quality of Life Questionnaire, evaluated the health-related quality of life (HRQoL) of social workers specializing in child mental health. In children aged 1–6 years and 6–12 years, the results revealed substantial disparities in lung function abnormalities, problematic behavior, and motor performance [10]. Bone et al reported, in a cohort of 29 352 admissions, 3.4–10.5% of patients developed global functional and cognitive disability following admission to the PICU [11]. PICS is likely caused by several interrelated risk factors, including the critical illness itself, mechanical ventilation, sedation, delirium, prolonged bed rest, and immobility during the illness [12]. It has been published that polyneuropathy [13,14], muscle wasting [13,15], and physical and mental function impairment are common, even among sepsis survivors [8,16]. Our current understanding of PICS in the pediatric population has several holes. Disparate research techniques have hampered a comprehensive approach to screening, preventing, and treating PICs-related morbidity [4]. The PICS paradigm, which incorporates numerous multidimensional morbidities, was developed at the 2010 Society of Critical Care Medicine meeting on improving long-term outcomes following critical illness for survivors and their families [17].
A modern description of early mobilization means engaging in physical activity during the initial 2 to 5 days of a severe illness or injury. In one study, early intervention was described as starting before leaving the intensive care unit (ICU), with an average of 6.6±5.5 days for activities like sitting on the bed [10]. Early physical therapy and mobilization during critical illness is a safe, realistic, and effective technique for reducing long-term morbidity due to PICS [12].The benefits of early mobilization of critically ill patients suggest that it should be included into daily therapeutic practice [11]. In intensive care units, early passive, active, and combined progressive mobilizations can be initiated safely [18–20]. To assess the knowledge, views, and stated practices regarding early mobilization among physicians and physiotherapists in pediatric critical care units in Canada, the United Kingdom, and the USA, surveys were conducted: in Canada, by Choong et al [21]; in the United Kingdom, by Thompson et al [22]; and in the USA, by Bakhru et al [23]. Additionally, an international survey was conducted that indicated that the organization and practice in different international ICUs vary significantly, with characteristics like multidisciplinary rounds, patient goals, specialized physiotherapists, and country-specific staffing ratios influencing early mobilization practice. Published data suggest that the absence of protocols and multidisciplinary team knowledge, concerns about patient safety, degree of sedation, and availability of staff and resources constitute the major barriers to implementing early mobilization in pediatric ICUs [1]. Staffing and practice patterns must be considered for successful implementation of early mobilization practices in pediatric critical care units [24]. A similar survey was conducted in adults, and revealed that the prevalence of early mobilization for mechanically ventilated patients in Saudi Arabia was 47%, even though only 36% of ICU staff had previous early mobilization training [25]. We conducted a nationwide survey on early mobilization in the pediatric population to explore the current gap between theory and practice in Saudi Arabia more deeply, which is critical for developing methods and tactics to reduce PICS and, eventually, improve patient recovery.
Material and Methods
STATISTICAL ANALYSIS:
All analyses were performed using R version 4.1.1 (2021-08-10). We used the tableone R package, to create Table 1, a table of demographic characteristics of our survey data. This package summarized both categorical and numerical variables. Categorical variables were counted or expressed as percentages. We used a non-normal method using medians and interquartile range (IQR) for data that were not normally distributed. We compared perceptions of patient-, institutional-, and healthcare provider-level barriers to early mobilization in the PICU between non-physicians and physicians using a chi-square test or a Fisher exact test where appropriate, with α=0.05 (2-sided) for the level of statistical significance. We did not correct for multiple significance testing because the analyses were primarily exploratory. Categorical variables were visualized by various plots, such a radial bar chart, pie chart, and donut chart using OpenAI data analysis software, written in Python.
Results
RESPONDENTS:
In a comprehensive survey involving 266 participants from Saudi Arabia, we observed a diverse distribution of respondents across various regions (Table 1). Jeddah accounted for the majority (54.1%), followed notably by Riyadh (29.3%), Tabuk (5.6%), and Madinah (3.4%). The professional demographic was predominantly composed of registered nurses, representing 64.7% of respondents. This was followed by consultants and attending physicians, constituting 16.5% of respondents, and physicians in clinical training, comprising 7.1%. Specialists and registrars were more sparsely represented in the survey. Regarding professional experience, a significant portion of the respondents (34.6%) had 1–5 years of experience. Those with 6–10 years, 11–15 years, and 16–20 years of experience made up 28.6%,18.4%, and 8.6% of the respondents, respectively. A smaller percentage of participants had less than a year of experience, 21–25 years of experience, or over 25 years of experience. In terms of workplace settings, 47.7% (127 respondents) reported working in ICUs that provide both medical and surgical care. This was the most common setting, followed by 32.3% who worked in the second-largest group, mixed medical-surgical and cardiac ICUs. Only a minor fraction (1.9%) were employed in exclusively medical ICUs, whereas 16.2% worked in exclusively cardiac ICUs. The survey also revealed that most of these facilities had 5–15 beds (69.2%), with the next most common category being facilities with 16–25 beds (18.8%). Facilities with more than 25 beds accounted for 9.8% of the ICU settings, while a mere 2.3% were in facilities with fewer than 5 beds. The annual patient admission rate predominantly ranged between 200 and 500, with 29.3% of respondents uncertain about the exact numbers. A significant majority of respondents were employed in academic teaching hospitals affiliated with universities, while the remaining 33.8% were based in non-academic hospitals. These insights collectively provide a nuanced understanding of the healthcare landscape and professional demographics within Saudi Arabian medical facilities, particularly in intensive care settings.
PERSONAL VIEW OF EARLY MOBILIZATION IN THE PICU:
The survey outcomes underscore a strong consensus among healthcare professionals on the importance of early mobilization in PICUs. A substantial majority of the respondents, exceeding 80%, categorized early mobilization as a critical component in PICU patient care. This includes 40.6% who deemed it very important, 22.2% who considered it important, and 19.2% who viewed it as crucial.
PERCEPTIONS OF BARRIERS TO EARLY MOBILIZATION:
In exploring the respondents’ perceptions of barriers to early mobilization, the survey highlighted several patient-level impediments. Medical instability (76.1%) and endotracheal intubation (56.3%) emerged as the most prevalent barriers. Other significant obstacles identified were the risk of dislodgement of devices or lines (60.6%) and excessive sedation (45.1%). Additional patient-level barriers include cognitive impairment or cognitive age (28.2%), muscular weakness (35.2%), and inadequate nutritional status (14.1%). Furthermore, physical restraints (28.2%), insufficient analgesia (14.1%), and obesity (7.0%) were recognized as less pronounced but relevant barriers. Interestingly, a small fraction of respondents (5.6%) perceived no patient barriers to early mobilization. These data suggest a consensus among both physicians and non-physicians in Saudi Arabia regarding the recognition of patient-level barriers to early mobilization, with no significant differences detected between these 2 groups. These findings, detailed in Table 2, provide crucial insights into the challenges of implementing early mobilization practices in the PICU setting.
BARRIERS AT THE INSTITUTIONAL AND PROVIDER LEVELS:
Table 3 delineates a comparative analysis of physician and non-physician perspectives on both institutional- and provider-level barriers to early mobilization in PICUs. A notable divergence between physicians and non-physicians was observed in the perception of routine bed rest orders upon ICU admission, with a significant difference (P=0.019) evident between the 2 groups. While 27.2% of non-physicians believed that such orders are routinely issued, only 12.7% of physicians shared this view. Although not reaching statistical significance (P=0.059), there was also a discernible trend towards significance in the belief that physician orders are necessary before mobilization, with 54.9% of non-physicians and 40.8% of physicians holding this opinion. The survey also revealed a difference in the perceived availability of equipment essential for early mobilization, though this difference was not statistically significant (P=0.231). A slightly greater proportion of physicians (42.3%) reported equipment insufficiency compared with non-physicians (33.3%). A significant discrepancy (P<0.001) existed between the groups regarding the absence of established guidelines or protocols, with 59.2% of physicians recognizing this gap, vs 34.0% of non-physicians recognizing it. The variance in perceptions about physical space availability in PICUs was not statistically significant (P=0.241). Moreover, the presence of a clinical advocate or champion was identified as a barrier more frequently by physicians (39.4%) than by non-physicians (24.6%), a difference that was statistically significant (P=0.027). The perceptions regarding cost-effectiveness as a barrier to early mobilization did not show a significant difference (P=0.813), suggesting a consensus on this aspect. Regarding healthcare provider-level barriers, the data indicated no significant variations between the groups in most areas, reflecting a shared recognition of challenges such as limited staffing, prioritization issues, and safety concerns. However, notable differences emerged in the perceptions of the timing of early mobilization initiation (P<0.001) and the adequacy of training (P<0.001). Physicians were more inclined to view these factors as obstacles, highlighting areas that may require targeted interventions for improvement in early mobilization practices. These insights, shown in Table 3, provide a detailed understanding of the multifaceted barriers to early mobilization in PICU settings, as perceived by different healthcare professionals.
TIMING AND THRESHOLDS FOR EARLY MOBILIZATION:
The initiation of early mobilization in PICUs presents a contested issue among healthcare providers. The predominant strategy, endorsed by 61.7% of respondents, is to commence mobilization once the patient’s cardiorespiratory status stabilizes, underscoring a general clinical inclination towards ensuring medical stability before beginning mobilization. Other commonly cited approaches include initiating mobilization when the patient is conscious and cooperative (44.7%), or when they are nearing transfer out of the ICU (33.1%). A notable proportion of respondents (30.1%) advocate for mobilization to start immediately post-admission to the PICU. Additional thresholds identified for starting early mobilization include post-extubation (25.9%), cessation of vasoactive infusions (24.8%), and upon stopping all sedative infusions (24.1%). Most respondents (53.4%) perceived early mobilization in the PICU as mobilization occurring within the initial 0–3 days of admission, while 29.7% consider the timeframe to be between 4 and 7 days, and a smaller group (5.3%) between 8 and 14 days. A minority, 11.7%, did not respond to this query.
For patients with head trauma and elevated intracranial pressure, bed rest was predominantly recommended (13.2%) as the minimal activity level by healthcare providers. Other responses included active (44%) and passive (48%) range-of-motion exercises. Notably, 75% of respondents refrained from selecting ambulatory activities, suggesting a consensus on the inappropriateness of such activities for this patient group. Additionally, 11.7% did not provide a response, indicating uncertainty or a lack of consensus on the minimum required activity level. In cases of cardiac shock, bed rest was the most frequently chosen activity, followed by passive range-of-motion exercises (25.6%). A significant proportion of respondents abstained from responding, reflecting a similar uncertainty or lack of agreement on the appropriate minimum activity level for patients experiencing cardiac shock. These data, reflecting diverse clinical opinions and practices, underscore the complexity and variability in approaches to early mobilization in pediatric critical care settings.
SAUDI PRACTICE:
In Saudi PICUs, the duration of passive range-of-motion exercises performed by physiotherapists exhibits considerable variation. The most common duration reported was less than 15 minutes, as indicated by 26.3% of respondents, followed by 16–30 minutes (24.1%), with 18.0% unsure of the duration. Notably, 13.5% of participants did not respond, suggesting potential gaps in knowledge or data availability on this subject (Figure 1). Registered nurses, comprising 82.0% of the workforce, actively participate in patient mobilization in critical care units. The survey indicates that in many institutes, physiotherapists are not regularly involved in patient mobilization (47.4%), and 23.3% of providers were uncertain about their role. A significant majority (61.7%) of healthcare professionals did not answer the question related to physiotherapist involvement. Regarding referrals for patients with suspected ICU-acquired weakness, patients were most often referred to physiotherapists, rehabilitation specialists, neurologists, and pediatricians, in that order. Physiotherapists were the most identified group (14.7%), followed by rehabilitation specialists (5.3%), neurologists (4.1%), and pediatricians (4.9%). Only a small fraction (1.5%) referred patients to family physicians. This pattern indicates variations in referral practices for ICU-acquired weakness, with physiotherapists being the predominant specialists to whom patients were referred (Figure 2).
Concerning the practice of daily sedation interruption or sedation protocols in PICUs, responses varied among the 266 healthcare professionals surveyed. A notable 13.9% did not respond to the query. The prevalent practice, as reported by 33.5% of respondents, is the routine application of daily sedation interruption or sedation regimens. Other responses included “sometimes” (22.2%), “frequently” (12.0%), “unsure” (8.6%), “never” (5.3%), and “infrequently or never” (4.5%). These data indicate varied practices regarding the use of daily sedation interruption or sedation protocols in PICUs, with a majority indicating routine usage. Additionally, there appears to be some uncertainty among healthcare professionals regarding the routine referral of patients with suspected ICU-acquired weakness for long-term rehabilitation in an outpatient setting post-discharge, as 31.2% expressed doubt. However, most respondents (38.7%) reported that these patients are typically referred to an outpatient clinic for ongoing therapy (Figure 3).
Discussion
Early mobilization practice in the ICU can vary greatly based on factors such as nation, multidisciplinary rounds, defining daily goals for patients, the existence of a dedicated physiotherapist, and the nurse/patient staffing ratio. Because of the diversity in worldwide ICU organization and practice, there may be disparities in the hurdles to implementing early mobilization. To successfully execute early mobilization, it is necessary to address multiple aspects of early mobilization practice, including viewpoints, opinions, barriers at various levels, ICU staffing, and individual country practice patterns. This may entail customizing implementation tactics to specific settings, such as through trials or quality-improvement programs sensitive to the local environment [24]. In our national survey on early mobilization in pediatric critical care, we interviewed 266 healthcare professionals to gain a better understanding of the current gap between theory and practice in Saudi Arabia. This understanding is critical for developing methods and tactics to reduce PICS and, eventually, improve pediatric critical care outcomes. The following important conclusions were found from our survey:
To begin with, the distribution of responders among Saudi cities demonstrated a range of levels of engagement. Jeddah had the most responses (54.1%), followed by Riyadh (29.3%), Tabuk (5.6%), and Madinah (3.4%). When formulating practice guidelines for early mobilization in the PICU, these geographical inequalities should be considered. Our poll results also showed the respondents’ professional backgrounds, with registered nurses making up the majority (64.7%). Consultants, attending physicians, and physicians who had undergone clinical training contributed significantly. In contrast, Thompson et al (2022) [22] reported that nurses constituted the largest percentage of respondents (27%), followed by physiotherapists (23%), and physicians (18%), in the UK. Ista (2020) [19] indicated that nurses participated in 72% of the European survey [19], but 59.8% of the Canadian survey respondents were physicians [21]. The majority of respondents had 1 to 5 years of experience. This distribution reflects the diverse range of healthcare professionals involved in pediatric critical care. In terms of the type of ICUs in which respondents worked, a considerable proportion (47.7%) worked in units that provided both medical and surgical care, with the second-largest group (32.3%) working in the second-largest category, mixed medical-surgical and cardiac ICU. The smallest category was medical-only ICUs (1.9%) followed by cardiac-only ICUs (16.2%), indicating that the poll is representative of a wide range of ICUs. This diversity of ICU types can assist in better understanding early mobilization approaches in various patient populations. Moreover, the distribution of the number of beds in facilities reflects the range of healthcare settings. Most facilities (69.2%) had 5–15 beds, followed by 16–25 beds (18.8%). According to Odetola and Folafoluwa (2005), PICUs in the United States have a median of 4.5 pediatric beds (IQR: 2–10 beds) [26]. Another study found that many ICUs (58%) in the United States were either mixed medical/surgical ICUs or medical ICUs (22%), with a median of 16 beds [23]. Our survey found that most of the respondents (66.2%) worked in academic teaching hospitals linked to universities. This suggests that this study will most likely provide feedback from healthcare professionals involved in research and education. According to Bakhru and Wiebe (2015), 51 percent of the hospitals surveyed were linked with an academic institution [24]. The number of patients admitted each year varied, with most responders admitting 200–500 persons (29.3%) and with a substantial minority of responders unsure. This variation in patient numbers may influence the workload and human resources required to perform early mobilization measures. Finally, the baseline features of the Saudi Arabian survey respondents regarding early mobilization in pediatric critical care provide a comprehensive overview of the region’s healthcare landscape and practices. These demographics and institutional circumstances are crucial for comprehending the study’s findings, as well as the potential impact of early mobilization tactics.
Furthermore, the study provides hopeful insights into the utility of early mobilization in PICUs. Most participants recognize its importance. This consensus is consistent with current literature, emphasizing the several advantages of early mobilization in PICU settings [25]. Notably, early mobilization is linked to increased muscle strength, a higher chance of walking, and more days spent outside the hospital [27]. It is also related to decreased delirium rates, lower readmission or mortality rates, and fewer occurrences of ventilator-associated pneumonia and central line and catheter infections [28]. Furthermore, studies show that early mobilization can considerably reduce PICU stays, perhaps restoring children to their pre-illness state more quickly [29]. Our survey confirms these findings, emphasizing Saudi healthcare professionals’ knowledge of the need for early mobilization in minimizing the negative consequences of prolonged immobility in pediatric patients.
Additionally, our data suggested a variety of obstacles for early mobilization in PICUs, with medical instability and endotracheal intubation standing out as the most significant. Other significant impediments include the possibility of dislodging medical devices or lines, severe sedation, and cognitive impairment. Muscular weakness and a poor dietary level were also detected. Physical restrictions, insufficient analgesia, and obesity were also mentioned as minor issues. Surprisingly, a tiny group of responders saw no hurdles at the patient level. This demonstrates a broad agreement among Saudi healthcare professionals, including both physicians and non-physicians, about the challenges of early mobilization. Comparing the data of others with our data, sedation, physiological instability, and endotracheal intubation were recognized as major hurdles in research from Australia and Scotland [30]. This list was enlarged by Nardo et al (2021) to include disease severity, medical orders, human resources, and the availability of mobilization equipment [18]. Staffing difficulties, time constraints, inadequate planning and coordination, and a lack of staff training were also mentioned [31]. Our research aligns with Thompson et al’s findings in the UK. They identified key challenges in pediatric critical care, including physiological instability, limited staff, sedation needs, scarcity of resources and equipment, delayed recognition of patient readiness for treatment, and budget limitations [22]. A Canadian study, likewise, stressed medical problems, probable device dislodgment, and endotracheal tubes as common impediments [21].
Another important element is that the poll findings show a wide range of opinions among healthcare experts on the best time to start early mobilization in PICUs. Most clinicians prefer to prioritize medical stability over mobilization measures. However, a sizable minority advocate for a more proactive strategy, arguing that early mobilization should be evaluated for safety and appropriateness as soon as feasible following PICU admission. This viewpoint is consistent with that of certain specialists, who advocate starting early mobilization soon after PICU admission or after significant medical milestones such as extubation or the discontinuation of sedative and vasoactive infusions. Choong et al proposed that early mobilization begin within the first 2 days of PICU admission [32]. Dubb et al define early mobilization in pediatric contexts as mobility treatments initiated within 72 hours after admission, aimed at children and adolescents obtaining spontaneous or aided ventilation [33]. Tsuboi et al propose initiating early mobilization within 2 to 5 days of the diagnosis of a serious disease or condition necessitating PICU hospitalization [34]. The poll also reveals the preferred exercise levels for various patient categories. Bed rest followed by passive range-of-motion exercises is rated the most recommended initial activity for individuals with head injuries and increased intracranial pressure. Bed rest is the suggested initial activity in situations of cardiac shock, with passive range-of-motion exercises as an alternative option. Notably, ambulatory activities are rarely explored, most likely due to worries about potential patient strain. Surprisingly, a sizable proportion of responders did not provide a firm answer about the recommended exercise level for cardiac shock patients. This ambiguity illustrates the lack of agreement among healthcare professionals and emphasizes the need for additional study and clear standards in this area. Standardized guidelines are critical for ensuring consistent, safe, and successful mobilization activities in PICUs.
Furthermore, the study in Saudi PICUs found that the lengths of physiotherapist-led passive range-of-motion exercises varied. The most often reported duration was “15 minutes” (26.3%), followed by “16–30 minutes” (24.1%), with a sizable proportion of respondents (18.0%) unclear. Betters et al observed that the duration and activity of early mobilization sessions are determined by the patient’s tolerance. The patient may be moved from laying to sitting during the initial early mobilization efforts, and following sessions may progress to sitting at the bed’s edge [35]. Saliski et al underlined the necessity of being active during the day, especially regular mobilization, to improve restorative sleep at night, which aids in healing and recovery. Nardo et al found that the median duration of mobilization sessions increased from 4 to 5.5 minutes [36]. Adel et al outlined a variety of early mobilization activities, including regular turning, passive motion, and sitting in various postures, as well as walking and in-bed cycling [37,38]. Ista et al differentiated between out-of-bed mobility, such as transferring from bed to chair or walking, and in-bed activity, such as passive motion or sitting in bed [19]. Walker et al emphasized the importance of tailoring the frequency and duration of early mobilization, typically recommending 30-minute physiotherapy sessions once daily from Monday to Friday, with the duration and frequency adjusted dependent on patient awareness and participation. Morrow also emphasized the lack of specific data for effective early mobilization dosage in the PICU, advising a 30-minute initial daily activity with future changes based on patient response [3].
Importantly, registered nurses play a substantial role in patient mobilization in Saudi practice, with 82.0% participation. Simpson et al and Nardo et al stressed the importance of a multidisciplinary team in early mobilization in a PICU. This group often consists of physicians, nurses, physical therapists, and other rehabilitation specialists who work together to assess, arrange, and carry out patient mobility exercises [18,39]. The early mobilization procedure, according to Betters et al, is a collaborative effort. When a patient meets the criteria for early mobilization, the attending physician places an order. Physical therapists, occupational therapists, nurses, and respiratory therapists then work together to plan mobilization, with physical therapists and occupational therapists also educating and incorporating parents [35]. Adel et al and Herbsman et al outline the team’s tasks, which include finding eligible patients, managing resources, and integrating patients’ families in the mobility process. Daily meetings between physicians, supervising nurses, and bedside nurses analyze mobilization options for each patient, taking into account their medical status and age [37,38]. According to Treble-Barna et al, a collaborative strategy incorporating several rehabilitation providers is normal practice [40]. According to Choong et al, nurses frequently drive mobility efforts, participating in 74% of events, sometimes with family help. Family participation is significant, occurring in nearly half of the cases [41]. Physiotherapists are primarily in charge of early mobilization in the PICU, according to Walker et al and Morrow, but it is not completely their job. The complete team, including nurses, critical care specialists, respiratory technologists and technicians, and rehabilitation therapists, as well as the child and his or her family, is required for successful implementation [3,42].
In addition, our survey found a varied landscape in the application of daily sedation interruptions or sedation regimes. In 33.5% of cases, respondents indicated routine use of these treatments, while others reported less frequent use, showing a variety of approaches to sedation management. Given the recognized impact of sedative modalities on early mobilization in pediatric critical care, this disparity is a major concern. According to Cameron et al and Betters et al, sedation vacations, which are part of the ABCDE package (which includes awakening and breathing coordination of daily sedation and ventilator removal trials, delirium monitoring and management, and early mobility and exercise), are critical for allowing active involvement in early mobilization treatments. The importance of minimizing sedation-related delirium and enhancing patient movement is emphasized in the current sedation regimens, which rely less on benzodiazepines [12,35]. Simpson et al underline the sensitive relationship between sedation, mechanical breathing, and mobilization time [39], emphasizing the significance of a balanced strategy in sedation management. Saliski et al and Herbsman et al investigate the challenges of finding the right balance between oversedation and undersedation. While sedation interruption can minimize total drug consumption and ICU stays, the risks of consequences such as inadvertent extubation must be considered [36,37]. Nardo et al expand on these concerns, stressing the logistical and safety constraints that prevent them from including daily sedation breaks in their benzodiazepine-sparing regimen [18]. On the other hand, Akinremi et al advocate for daily sedation interruption as a strategy for reducing ICU-acquired weakness, demonstrating differing perspectives on sedation management in the setting of early mobilization [43]. Walker et al concur, citing a lack of consistent sedation criteria as a barrier to the early implementation of early mobilization in PICUs [42]. While there is theoretical consensus on the benefits of early mobilization and the role of sedation management in facilitating it, our findings show that practice differs substantially. This variance could be attributed to differences in clinical settings, patient populations, and logistical constraints. Sedation can be managed in a variety of ways in pediatric critical care. These range from not using it daily to being more cautious and not utilizing benzodiazepines. This is since there are numerous elements that influence early mobilization in this situation. Our study investigates the need for a more consistent approach to sedation management in Saudi PICUs to promote successful and safe early mobilization.
Finally, our study found that healthcare providers aren’t always clear on how to refer patients who have developed a weakness in the ICU to long-term rehabilitation in outpatient settings after they leave the hospital. Although around 31.2% of respondents were perplexed by such referrals, the vast majority (38.7%) responded that these patients are commonly sent to outpatient clinics for ongoing treatment. Bakhru’s findings corroborate our findings, emphasizing the significance of referring such patients to physical therapists or physiotherapists following discharge [24]. Choong’s research highlights the importance of post-discharge rehabilitation. Children with obvious ICU-acquired weakness are typically referred to rehabilitation, mostly physiotherapy (46.6%). Other common referrals include rehabilitation medicine (37.5%), neurology (26.1%), and occupational therapy (19.3%) [21]. These numbers support our findings, highlighting the significance of a comprehensive approach to post-PICU treatment for overall rehabilitation. Furthermore, Barros’ study offers an intriguing point of view, revealing that more than half of respondents (51.6%) had processes or protocols in place for continuing rehabilitation after ICU discharge [44]. This figure indicates a growing recognition of the significance of structured, ongoing rehabilitation interventions for children recovering from ICU stays. Our Saudi Arabian study parallels these global trends and emphasizes a comparable need for established referral systems for post-PICU rehabilitation.
The findings of a national assessment on early mobilization in pediatric critical care in Saudi Arabia have important clinical implications. Due to geographic and professional variety, it emphasizes the necessity for region-specific guidelines, advocating personalized approaches in pediatric critical care units with a focus on multidisciplinary collaboration. Common challenges such as medical instability, resource restrictions, and mobilization timing highlight the importance of worldwide collaborative efforts and evidence-based recommendations to standardize care. According to the study, specific guidelines for physiotherapist-led interventions and a uniform manner to handle sedation are also required to ensure that patient needs are satisfied while also allowing for early mobilization. It also emphasizes the significance of developing defined protocols for post-ICU rehabilitation to promote continuity of care and improve long-term results for pediatric patients.
The study has various limitations, including the possibility of a lack of generalizability due to a concentration of responses from specific regions and types of institutions. The use of self-reported data may introduce biases since respondents may submit answers that are socially desirable or not totally factual. The lack of a direct association between the impressions of healthcare personnel and actual patient outcomes is a key constraint, impeding the capacity to conclusively link early mobilization techniques with clinical gains. Given the professional backgrounds of most respondents, the study may also have a response bias toward nursing perspectives, potentially overshadowing findings from other experts. Furthermore, the survey’s cross-sectional form makes it difficult to track changes over time or evaluate the success of various early mobilization initiatives.
Conclusions
By presenting a detailed study of the healthcare landscape, views, and challenges regarding early mobilization, this research contributes to the field of pediatric critical care in Saudi Arabia. Recognizing the importance of early mobilization and understanding the challenges involved with its implementation allows healthcare organizations to progress toward a consistent and evidence-based approach, ultimately leading to better patient outcomes and greater quality of care. A future study should focus on finding the best timing and activity levels for certain patient groups to encourage evidence-based early mobilization in the PICU. This study’s findings have far-reaching consequences for pediatric critical care clinical practice, legislation, and future research. Addressing the identified barriers and taking a multidisciplinary approach to early mobility would help healthcare personnel bridge the gap between theory and reality, ensuring that pediatric patients in the PICU receive the greatest care and achieve the best outcomes. Finally, these programs have the potential to improve pediatric critical care while also raising healthcare quality in Saudi Arabia and worldwide.
Figures
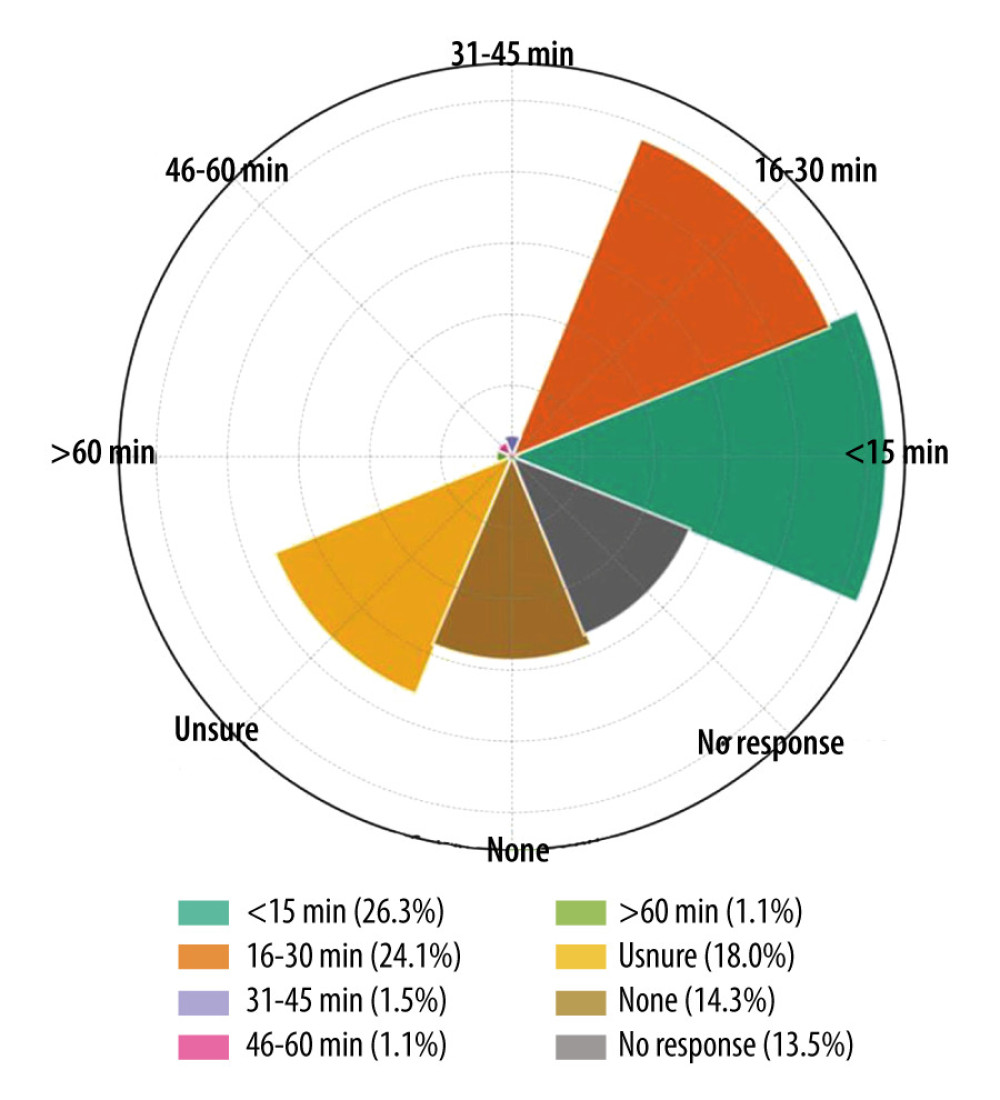 Figure 1. Radial bar chart (also known as a circular bar plot) representing the data on the daily duration of active motion performed by physiotherapists in a pediatric intensive care unit. Each segment of the chart corresponds to a different time duration category, with the extent of the fill within each segment indicating the proportion of responses for that category. Percentage labels are included on each bar, and a legend is positioned at the bottom to aid in identifying each category. This figure was created with the help of openAI data analysis.
Figure 1. Radial bar chart (also known as a circular bar plot) representing the data on the daily duration of active motion performed by physiotherapists in a pediatric intensive care unit. Each segment of the chart corresponds to a different time duration category, with the extent of the fill within each segment indicating the proportion of responses for that category. Percentage labels are included on each bar, and a legend is positioned at the bottom to aid in identifying each category. This figure was created with the help of openAI data analysis. 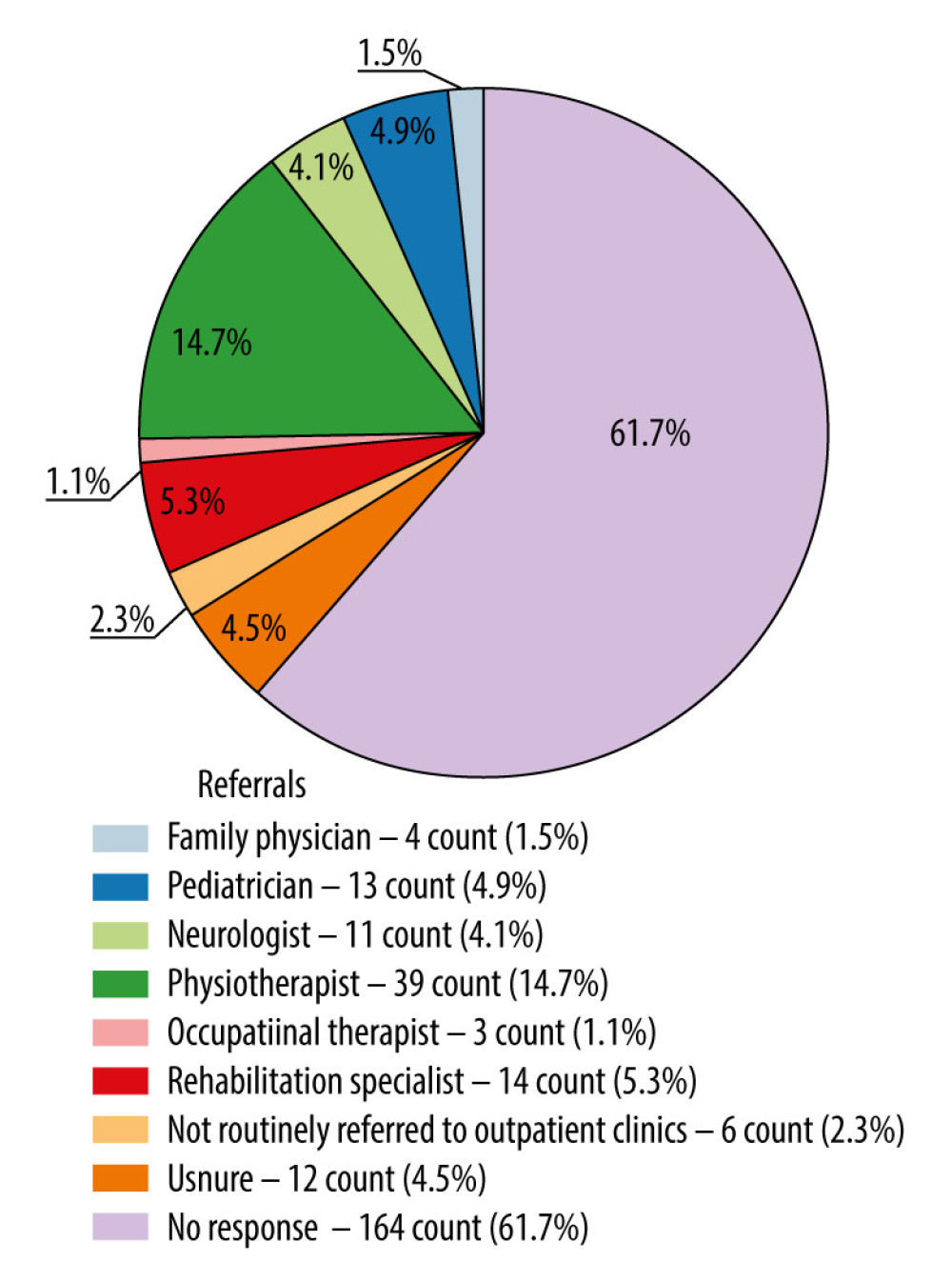 Figure 2. Pie chart representing the distribution of referrals for patients with suspected acquired weakness to various healthcare professionals. The chart is color-coded, and the legend includes both count and percentage, providing a clear and detailed description.
Figure 2. Pie chart representing the distribution of referrals for patients with suspected acquired weakness to various healthcare professionals. The chart is color-coded, and the legend includes both count and percentage, providing a clear and detailed description. 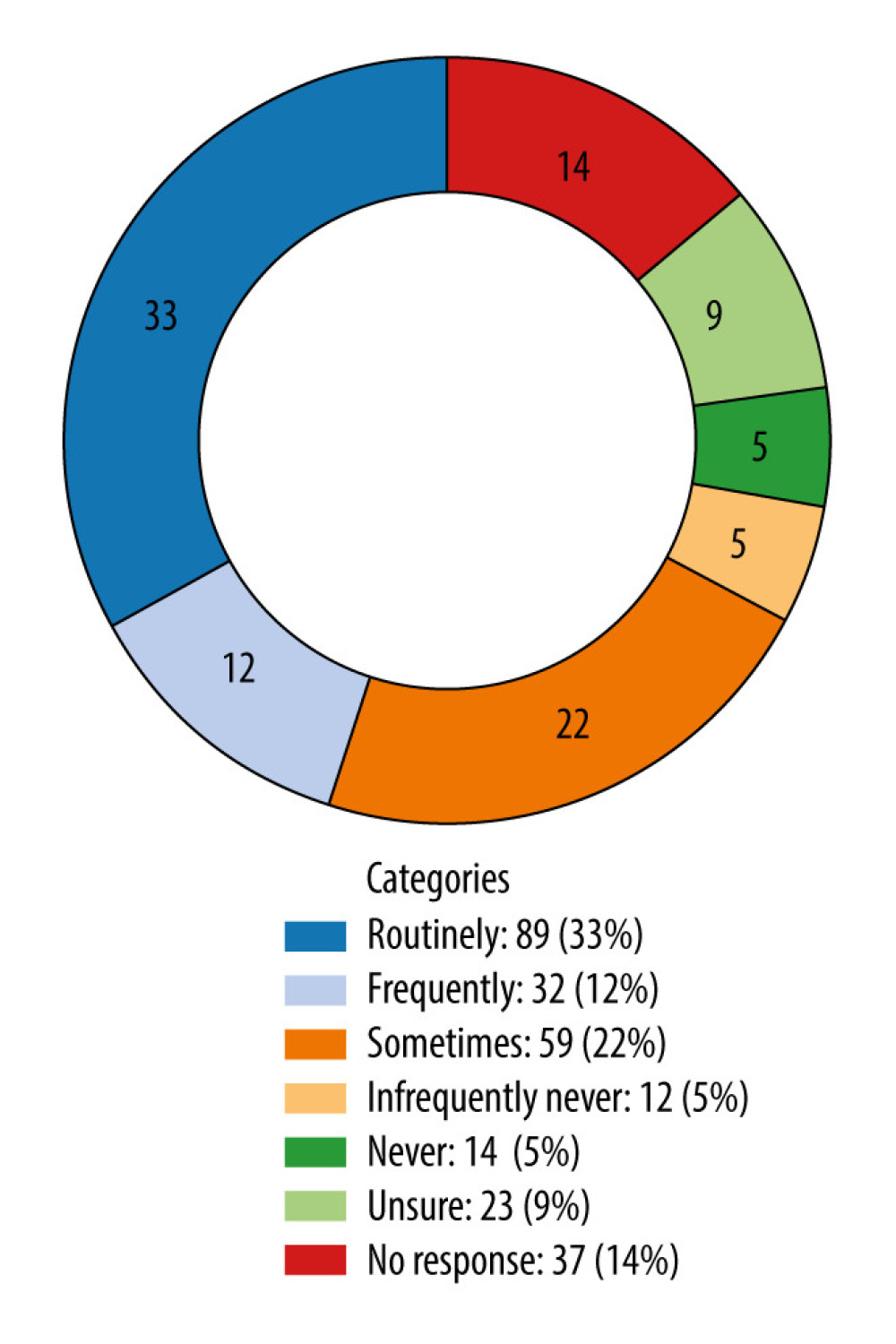 Figure 3. Donut chart visualizing the sedation vacation practice or protocols in the pediatric intensive care unit, with labels indicating both the count and the percentage for each category.
Figure 3. Donut chart visualizing the sedation vacation practice or protocols in the pediatric intensive care unit, with labels indicating both the count and the percentage for each category. Tables
Table 1. Demographic characteristics of survey data.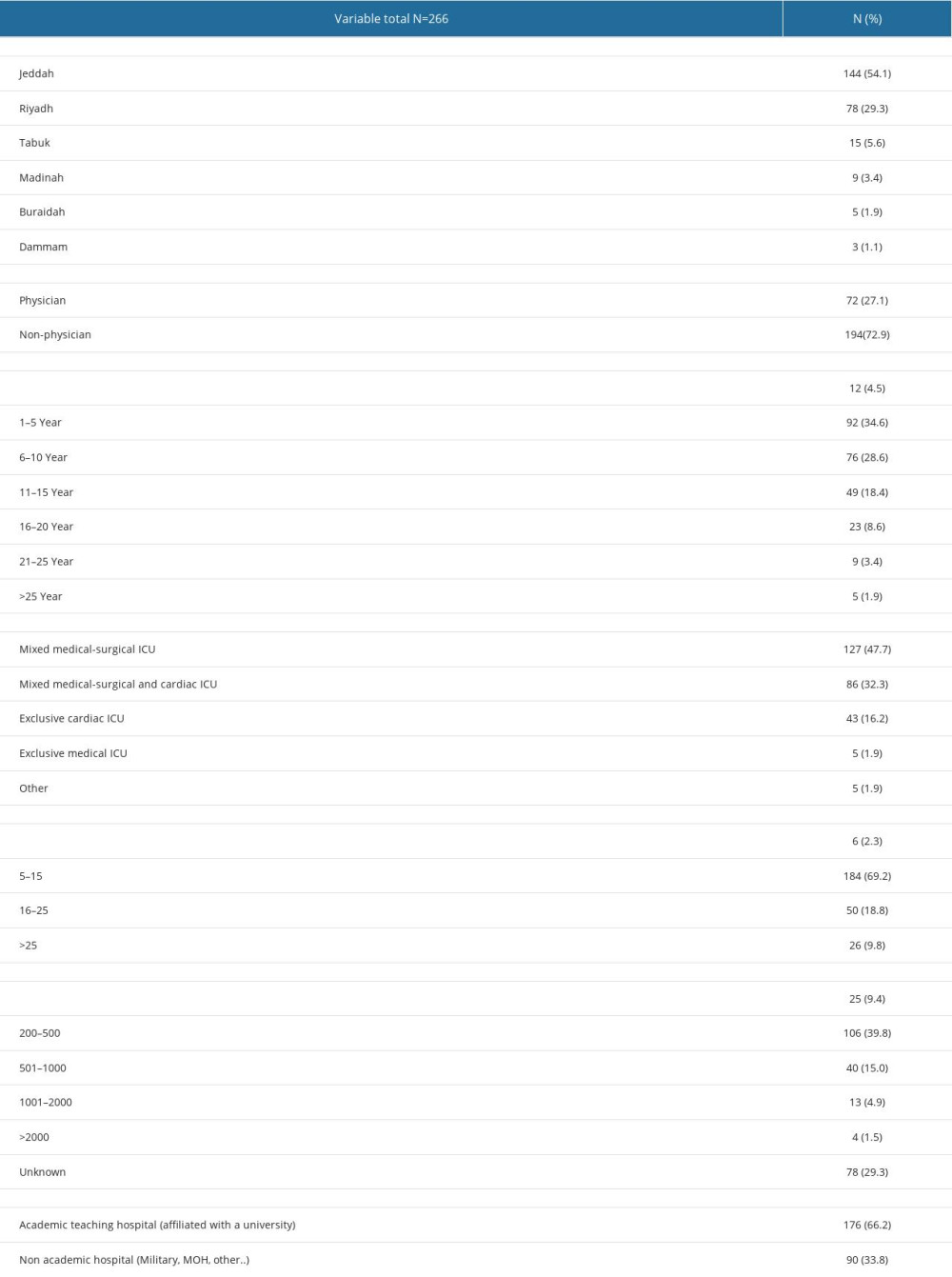 Table 2. Perception of patient-level barriers regarding early mobilization in the pediatric intensive care unit: comparison of opinion between non-physicians and physicians.
Table 2. Perception of patient-level barriers regarding early mobilization in the pediatric intensive care unit: comparison of opinion between non-physicians and physicians.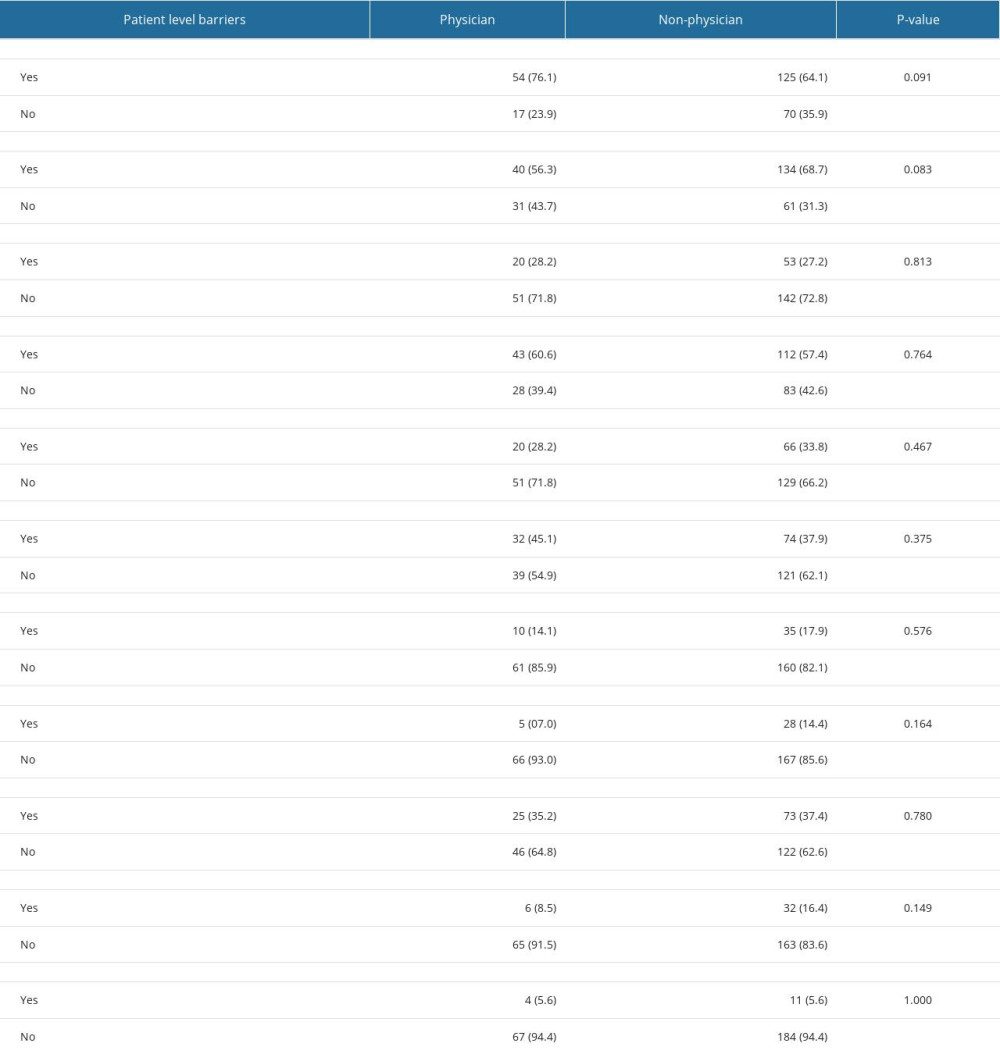 Table 3. Perception of institutional and healthcare provider-level barriers regarding early mobilization in pediatric intensive care units: comparison of opinion between non-physicians and physicians.
Table 3. Perception of institutional and healthcare provider-level barriers regarding early mobilization in pediatric intensive care units: comparison of opinion between non-physicians and physicians.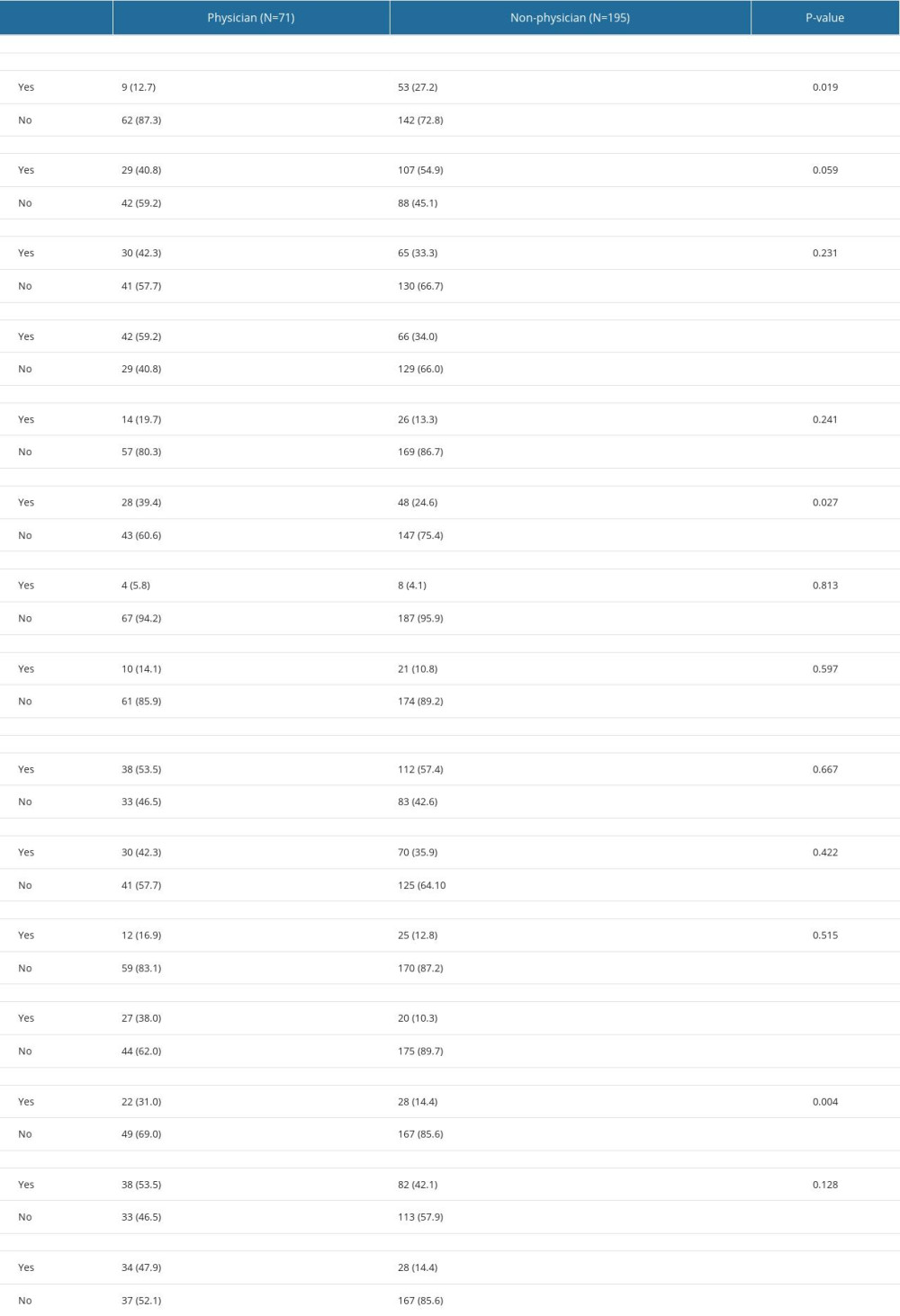
References
1. Piva TC, Ferrari RS, Schaan CW, Early mobilization protocols for critically ill pediatric patients: Systematic review: Rev Bras Terapia Intensiva, 2019; 31(2); 248-57
2. Namachivayam P, Shann F, Shekerdemian L, Three decades of pediatric intensive care: Who was admitted, what happened in intensive care, and what happened afterward: Pediatr Crit Care Med, 2010; 11(5); 549-55
3. Morrow BM, Building a culture of early mobilization in the Pediatric Intensive Care Unit – a nuts and bolts approach: Transl Pediatr, 2021; 10(8); 2845-57
4. Woodruff AG, Choong K, Long-term outcomes and the post-intensive care syndrome in critically ill children: A North American perspective: Children (Basel), 2021; 8(3); 254
5. Hartman ME, Williams CN, Hall TA, Post-intensive-care syndrome for the pediatric neurologist: Pediatr Neurol, 2020; 108; 47-53
6. Ekim A, The post-intensive care syndrome in children: Compr Child Adolesc Nurs, 2020; 43(1); 15-21
7. Field-Ridley A, Dharmar M, Steinhorn D, Intensive Care Unit-Acquired Weakness (ICU-AW) is associated with differences in clinical outcomes in critically ill children: Pediatr Crit Care Med, 2017; 176(3); 139-48
8. Voiriot G, Oualha M, Pierre A, Chronic critical illness and post-intensive care syndrome: From pathophysiology to clinical challenges: Ann Intensive Care, 2022; 12(1); 58
9. Yuan C, Timmins F, Thompson DR, Post-intensive care syndrome: A concept analysis: Int J Nurs Stud, 2021; 114; 103814
10. Knoester H, Bronner MB, Bos AP, Grootenhuis MA, Quality of life in children three and nine months after discharge from a Paediatric Intensive Care Unit: A prospective cohort study: Health Qual Life Outcomes, 2008; 6; 21
11. Bone MF, Feinglass JM, Goodman DM, Risk factors for acquiring functional and cognitive disabilities during admission to a PICU: Pediatr Crit Care Med, 2014; 15(7); 640-48
12. Cameron S, Ball I, Cepinskas G, Early mobilization in the Critical Care Unit: A review of adult and pediatric literature: J Crit Care, 2015; 30; 664-72
13. Zhou C, Wu L, Ni F, Ji W, Wu J, Zhang H, Critical illness polyneuropathy and myopathy: A systematic review: Neural Regen Res, 2014; 9(1); 101-10
14. Hermans G, De Jonghe B, Bruyninckx F, Van den Berghe G, Clinical review: Critical illness polyneuropathy and myopathy: Crit Care, 2008; 12; 238
15. Puthucheary ZA, Rawal J, McPhail M, Acute skeletal muscle wasting in critical illness: JAMA, 2013; 310(15); 1591-600
16. Farris RW, Weiss NS, Zimmerman JJ, Functional outcomes in pediatric severe sepsis: Further analysis of the researching severe sepsis and organ dysfunction in children: A global perspective trial: Pediatr Crit Care Med, 2013; 14(9); 835-42
17. Elliott D, Davidson JE, Harvey MA, Exploring the scope of post-intensive care syndrome therapy and care: Crit Care Med, 2014; 42(12); 2518-26
18. Di Nardo M, Boldrini F, Broccati F, The LiberAction Project: Implementation of a pediatric liberation bundle to screen delirium, reduce benzodiazepine sedation, and provide early mobilization in a human resource-limited Pediatric Intensive Care Unit: Front Pediatr, 2021; 9; 788997
19. Ista E, Scholefield BR, Manning JC, Mobilization practices in critically ill children: A European point prevalence study (EU PARK-PICU): Crit Care, 2020; 24(1); 368
20. Wieczorek B, Ascenzi J, Kim Y, PICU Up!: Impact of a quality improvement intervention to promote early mobilization in critically ill children: Pediatr Crit Care Med, 2016; 17(12); e559-e66
21. Choong K, Koo KKY, Clark H, Early mobilization in critically Ill children: A survey of Canadian practice: Crit Care Med, 2013; 41; 1745-53
22. Thompson JY, Menzies JC, Manning JC, Early mobilization and rehabilitation in the PICU: A UK survey: BMJ Paediatr Open, 2022; 6(1); e001300
23. Bakhru RN, Wiebe DJ, McWilliams DJ, An environmental scan for early mobilization practices in U.S. ICUs: Crit Care Med, 2015; 43(11); 2360-69
24. Bakhru RN, McWilliams DJ, Wiebe DJ, Intensive Care Unit structure variation and implications for early mobilization practices: An international survey: Ann Am Thorac Soc, 2016; 13(9); 1527-37
25. Alqahtani JS, Alahamri MD, Alqahtani AS, Early mobilization of mechanically ventilated ICU patients in Saudi Arabia: Results of an ICU-wide national survey: Heart Lung, 2022; 56; 167-74
26. Odetola FO, Clark SJ, Freed GL, Bratton SL, Davis MM, A national survey of pediatric critical care resources in the United States: Pediatrics, 2005; 115(4); e382-e86
27. Tipping CJ, Harrold M, Holland A, The effects of active mobilisation and rehabilitation in ICU on mortality and function: A systematic review: Intensive Care Med, 2017; 43; 171-83
28. Hunter A, Johnson L, Coustasse A, Reduction of intensive care unit length of stay: The case of early mobilization: Health Care Manager, 2014; 33(2); 128-35
29. Rennick JE, Childerhose JE, Redefining success in the PICU: New patient populations shift targets of care: Pediatrics, 2015; 135; e289-e91
30. Harrold ME, Salisbury LG, Webb SA, Allison GT, Early mobilisation in Intensive Care Units in Australia and Scotland: A prospective, observational cohort study examining mobilisation practises and barriers: Crit Care, 2015; 19; 336
31. Mostafa B, Salem S, Mohammed S, Perceived barriers to early mobilization of patients admitted to the Intensive Care Unit (ICU): The Egyptian Journal of Intensive Care and Emergency Medicine, 2022; 2(1); 8-19
32. Choong K, Foster G, Fraser DD, Acute rehabilitation practices in critically ill children: A multicenter study: Pediatric Critical Care Medicine, 2014; 15(6); e270-e79
33. Dubb R, Nydahl P, Hermes C, Barriers and strategies for early mobilization of patients in Intensive Care Units: Ann Am Thorac Soc, 2016; 13(5); 724-30
34. Tsuboi N, Hiratsuka M, Kaneko S, Benefits of early mobilization after pediatric liver transplantation: Pediatric Critical Care Medicine, 2019; 20(2); E91-E97
35. Betters KA, Hebbar KB, Farthing D, Development and implementation of an early mobility program for mechanically ventilated pediatric patients: J Crit Care, 2017; 41; 303-8
36. Saliski M, Kudchadkar S, Optimizing sedation management to promote early mobilization for critically ill children: J Pediatr Intensive Care, 2015; 04(4); 188-93
37. Herbsman JM, D’Agati M, Klein D, Early mobilization in the Pediatric Intensive Care Unit: A quality improvement initiative: Pediatr Qual Saf, 2020; 5(1); e256
38. Van den Adel TZ, van Dijk M, de Heer M, Quality improvement intervention to stimulate early mobilisation of critically ill children: Nurs Crit Care, 2023; 28(4); 545-53
39. Simpson CEM, Esterman AJ, Ganu SS, Early mobilisation in critically ill children: Does routine patient screening reduce time to commencing mobilisation?: Australian Critical Care, 2023; 36(2); 208-14
40. Treble-Barna A, Beers SR, Houtrow AJ, PICU-based rehabilitation and outcomes assessment: A survey of pediatric critical care physicians: Pediatric Critical Care Medicine, 2019; 20(6); e274-e82
41. Choong K, Zorko DJ, Awojoodu R, Prevalence of acute rehabilitation for kids in the PICU: A Canadian multicenter point prevalence study: Pediatric Critical Care Medicine, 2021; 22(2); 181-93
42. Walker TC, Kudchadkar SR, Early mobilization in the pediatric intensive care unit: Transl Pediatr, 2018; 7(4); 308-13
43. Akinremi A, Erinle O, Hamzat T, ICU-acquired weakness: A multicentre survey of knowledge among ICU clinicians in South-Western Nigeria: Niger J Clin Pract, 2019; 22(9); 1229-35
44. Barros-Poblete M, Bernardes Neto SC, Benavides-Cordoba V, Early mobilization in intensive care unit in Latin America: A survey based on clinical practice: Front Med (Lausanne), 2022; 9; 1005732
Figures
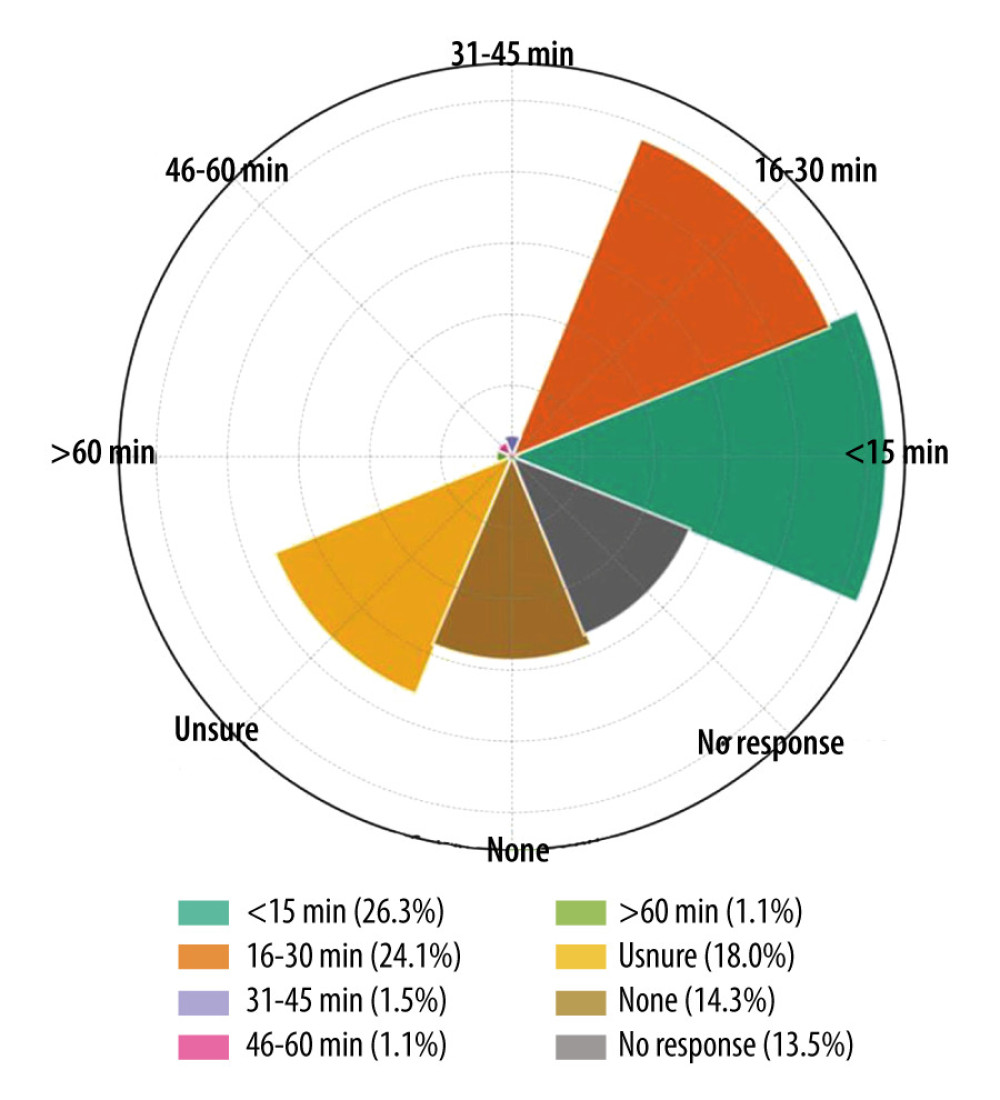 Figure 1. Radial bar chart (also known as a circular bar plot) representing the data on the daily duration of active motion performed by physiotherapists in a pediatric intensive care unit. Each segment of the chart corresponds to a different time duration category, with the extent of the fill within each segment indicating the proportion of responses for that category. Percentage labels are included on each bar, and a legend is positioned at the bottom to aid in identifying each category. This figure was created with the help of openAI data analysis.
Figure 1. Radial bar chart (also known as a circular bar plot) representing the data on the daily duration of active motion performed by physiotherapists in a pediatric intensive care unit. Each segment of the chart corresponds to a different time duration category, with the extent of the fill within each segment indicating the proportion of responses for that category. Percentage labels are included on each bar, and a legend is positioned at the bottom to aid in identifying each category. This figure was created with the help of openAI data analysis.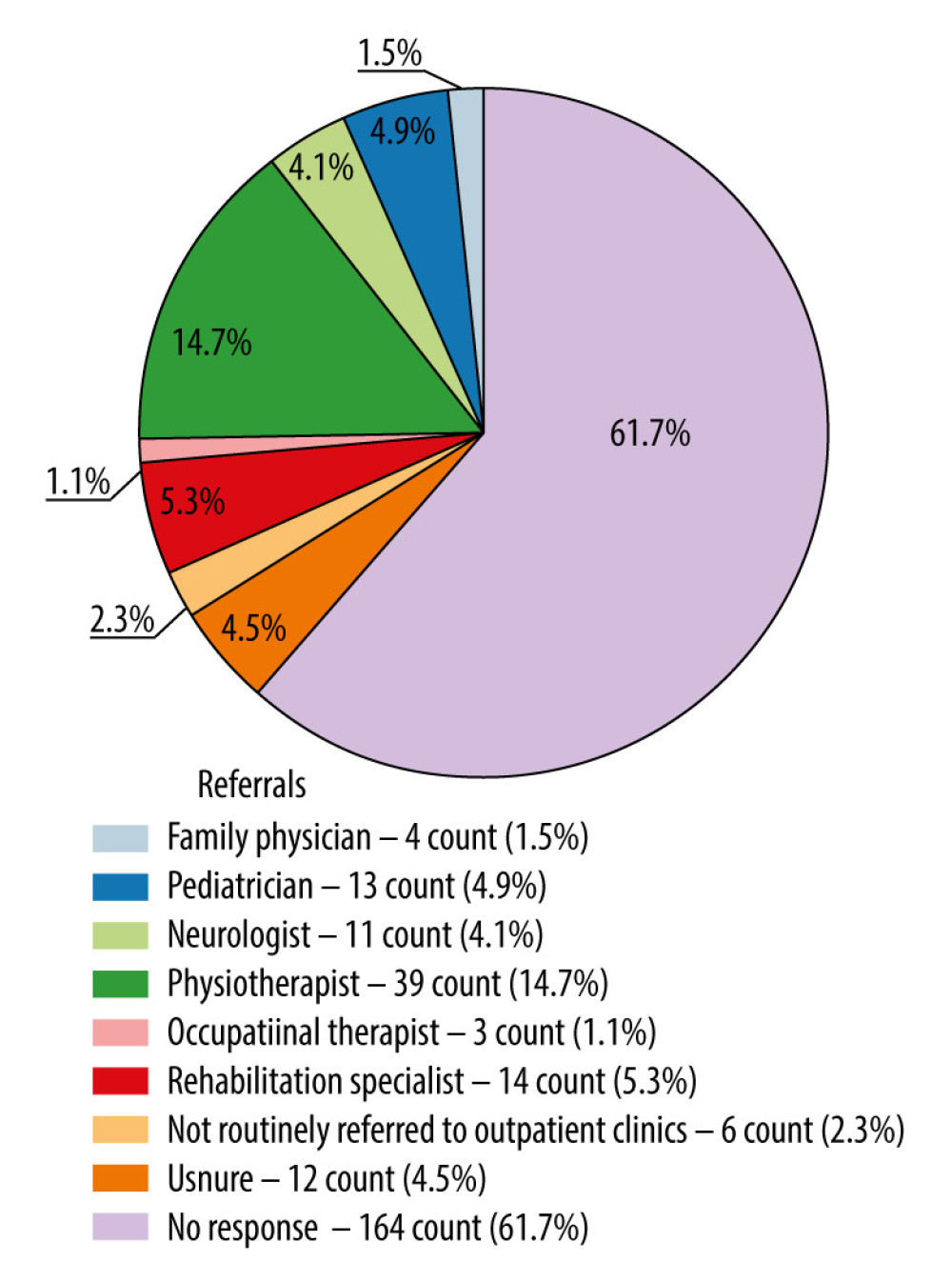 Figure 2. Pie chart representing the distribution of referrals for patients with suspected acquired weakness to various healthcare professionals. The chart is color-coded, and the legend includes both count and percentage, providing a clear and detailed description.
Figure 2. Pie chart representing the distribution of referrals for patients with suspected acquired weakness to various healthcare professionals. The chart is color-coded, and the legend includes both count and percentage, providing a clear and detailed description.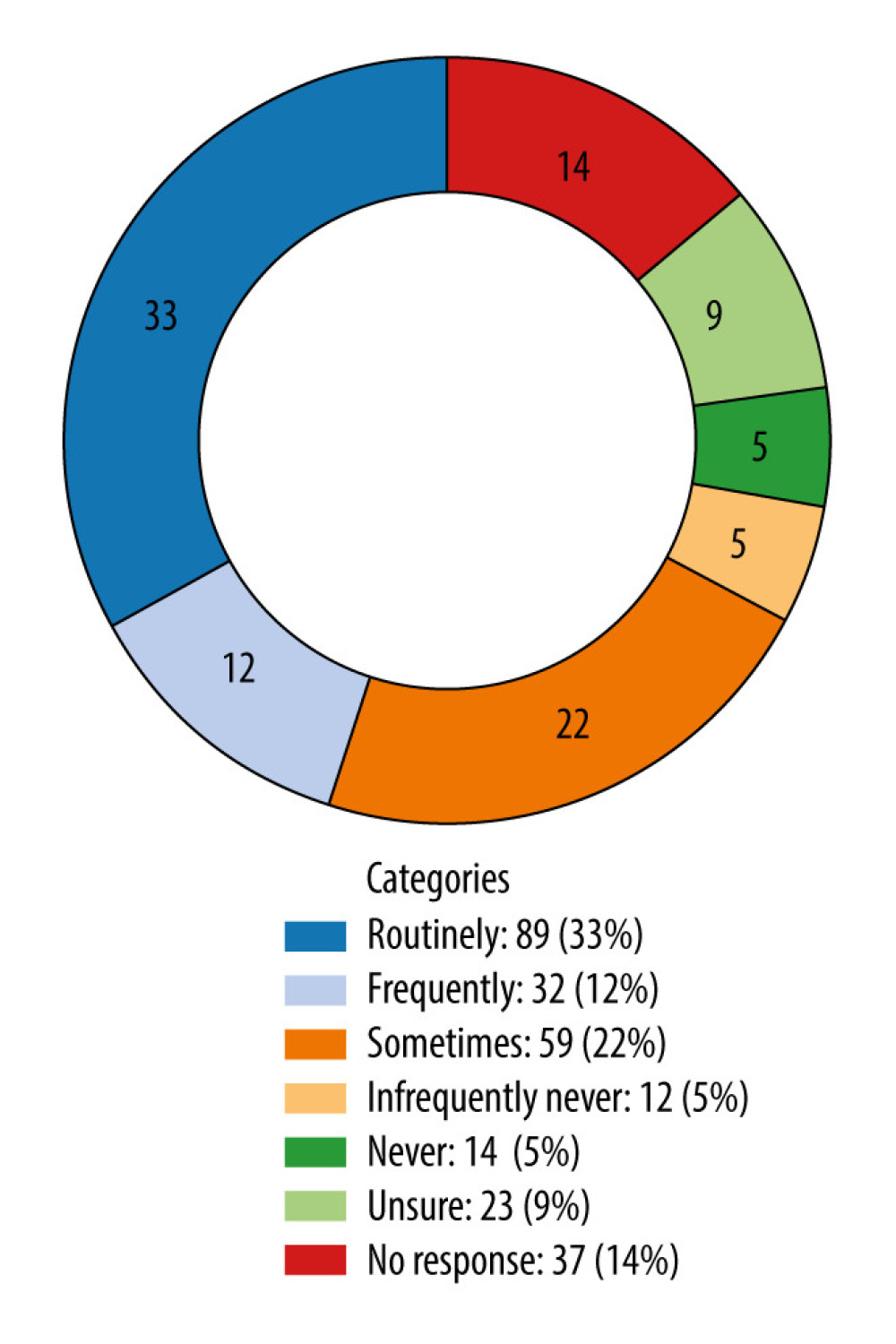 Figure 3. Donut chart visualizing the sedation vacation practice or protocols in the pediatric intensive care unit, with labels indicating both the count and the percentage for each category.
Figure 3. Donut chart visualizing the sedation vacation practice or protocols in the pediatric intensive care unit, with labels indicating both the count and the percentage for each category. Tables
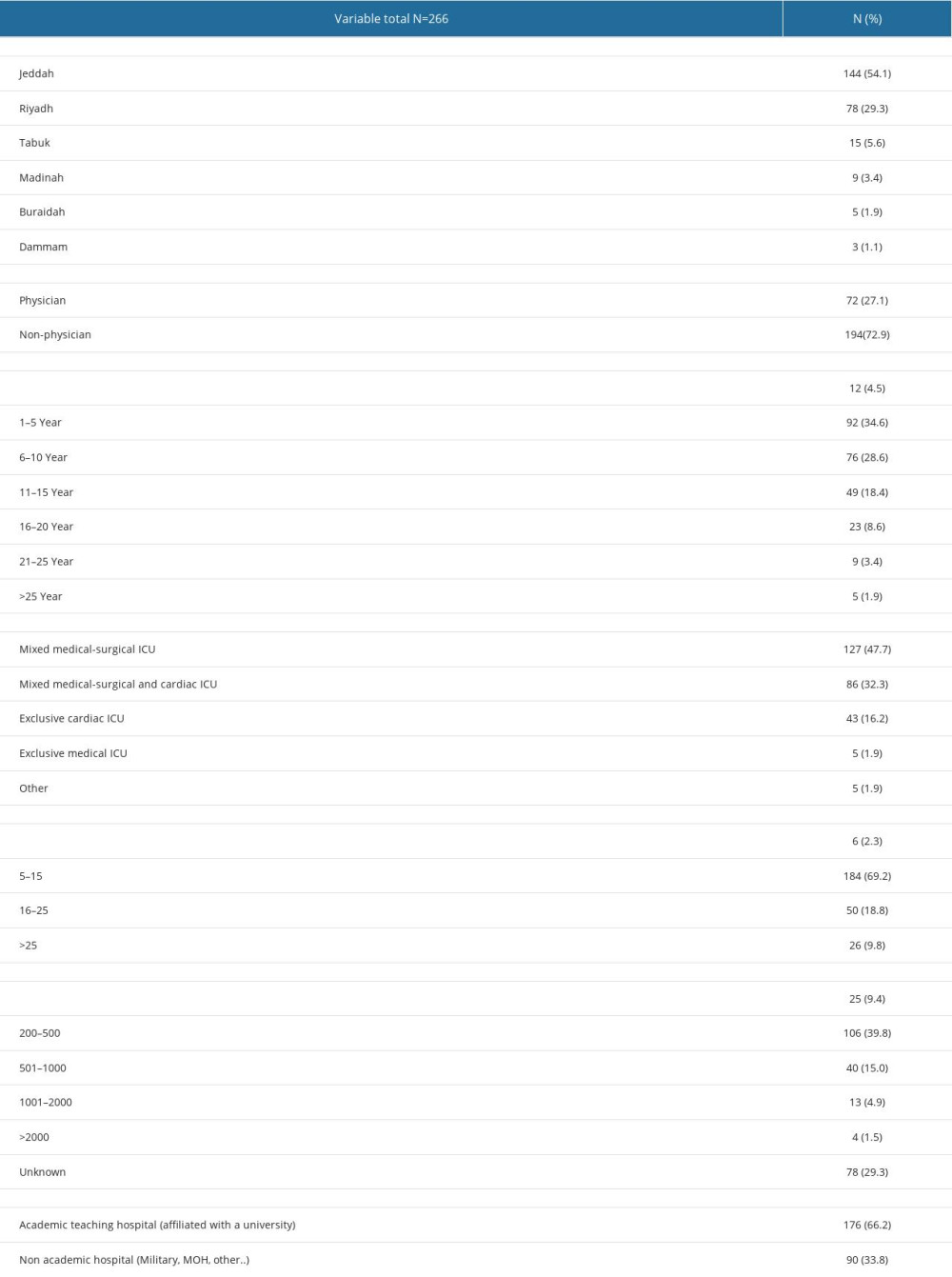 Table 1. Demographic characteristics of survey data.
Table 1. Demographic characteristics of survey data.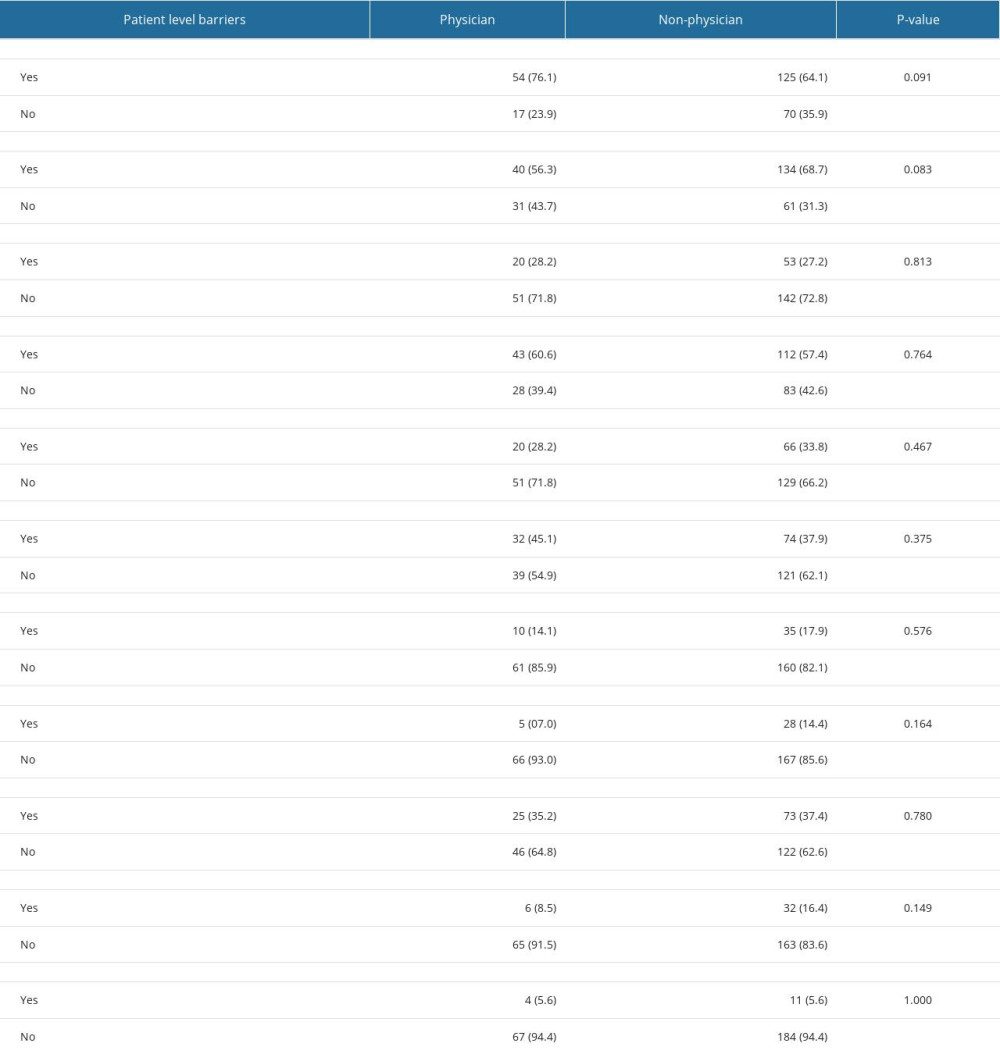 Table 2. Perception of patient-level barriers regarding early mobilization in the pediatric intensive care unit: comparison of opinion between non-physicians and physicians.
Table 2. Perception of patient-level barriers regarding early mobilization in the pediatric intensive care unit: comparison of opinion between non-physicians and physicians.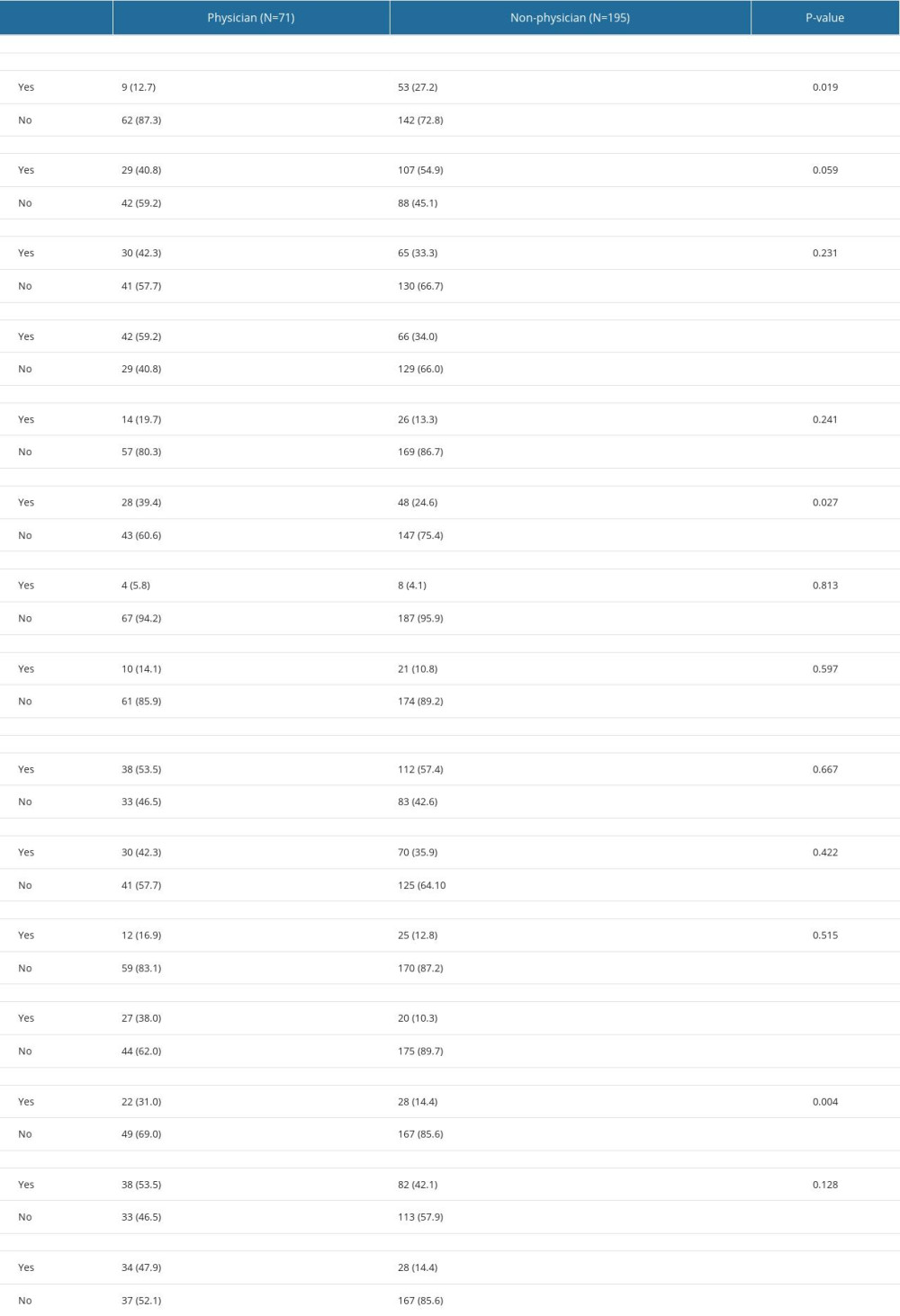 Table 3. Perception of institutional and healthcare provider-level barriers regarding early mobilization in pediatric intensive care units: comparison of opinion between non-physicians and physicians.
Table 3. Perception of institutional and healthcare provider-level barriers regarding early mobilization in pediatric intensive care units: comparison of opinion between non-physicians and physicians.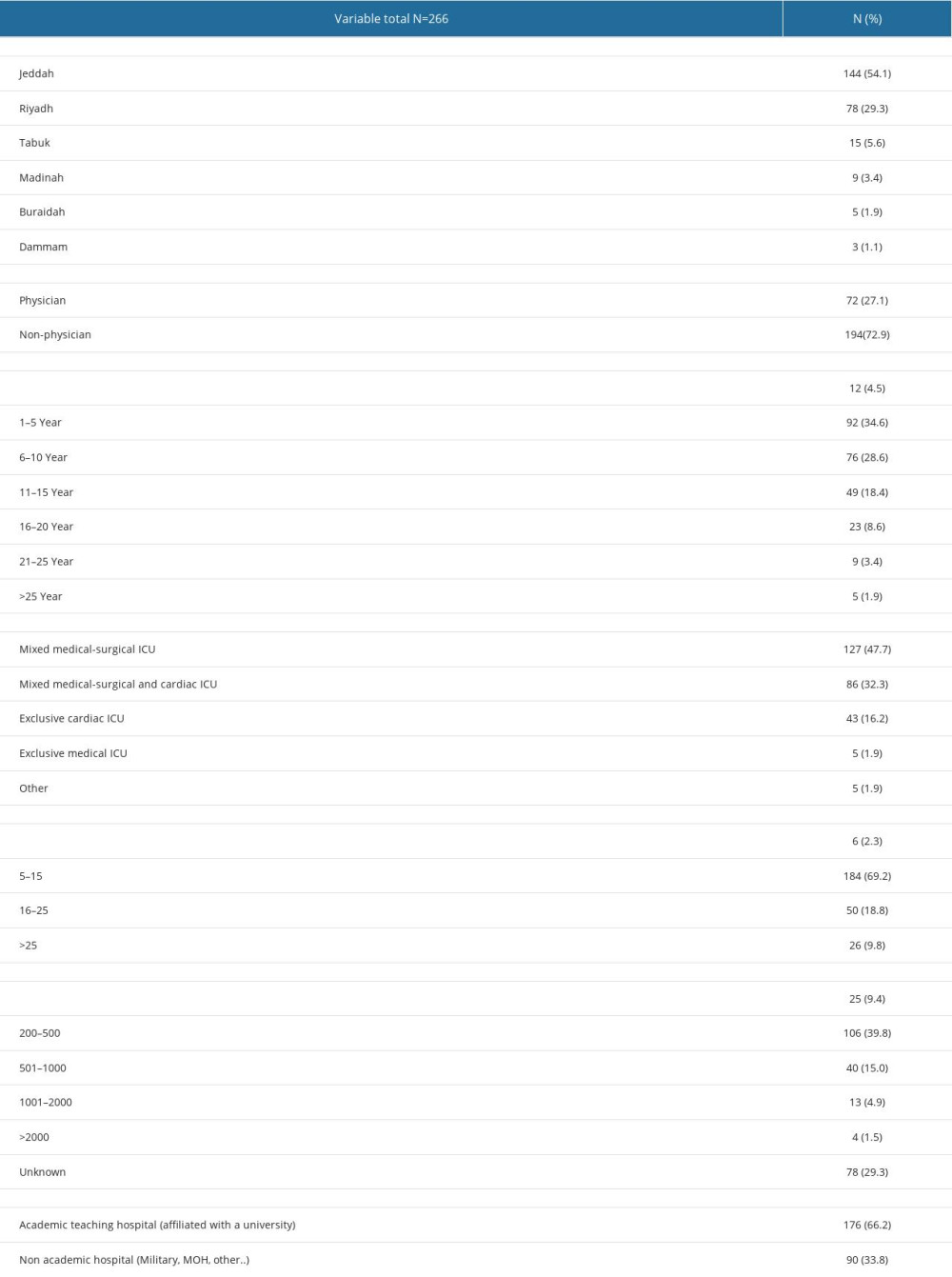 Table 1. Demographic characteristics of survey data.
Table 1. Demographic characteristics of survey data.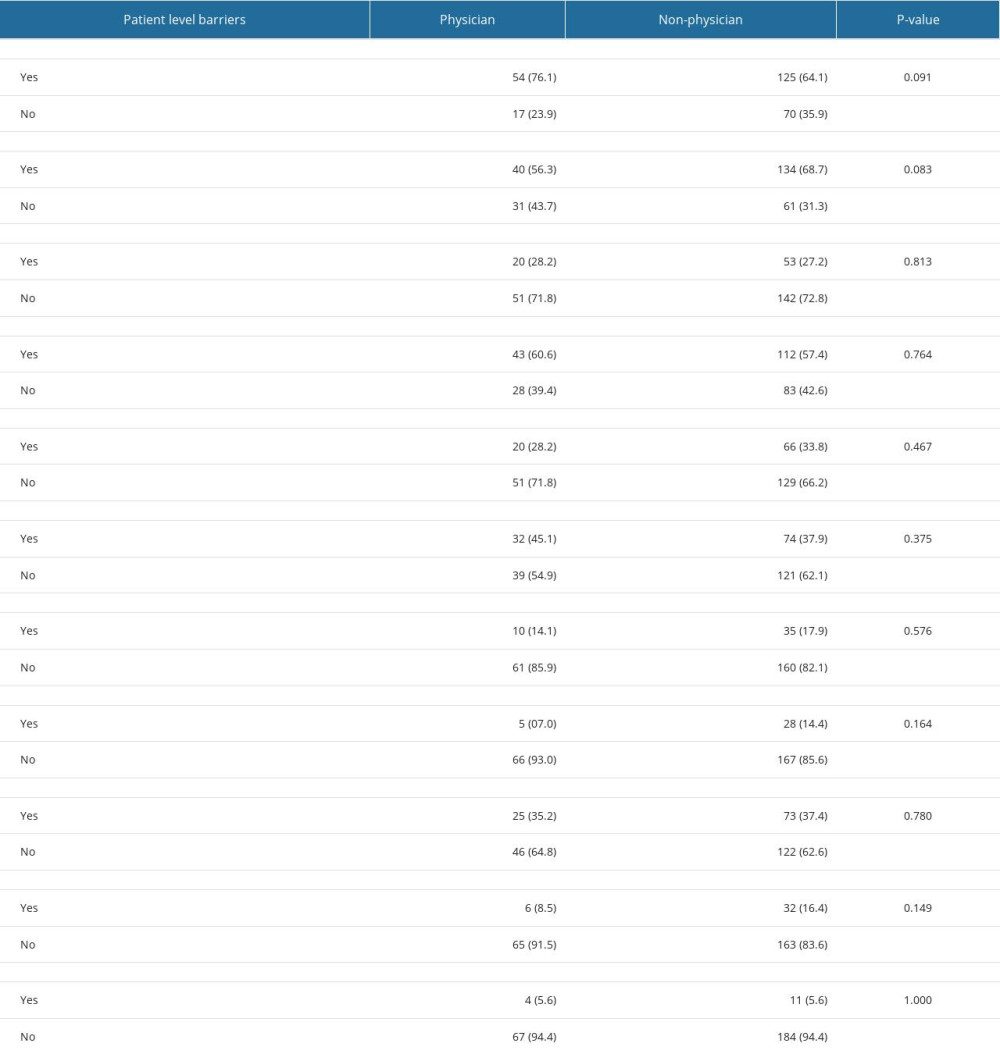 Table 2. Perception of patient-level barriers regarding early mobilization in the pediatric intensive care unit: comparison of opinion between non-physicians and physicians.
Table 2. Perception of patient-level barriers regarding early mobilization in the pediatric intensive care unit: comparison of opinion between non-physicians and physicians.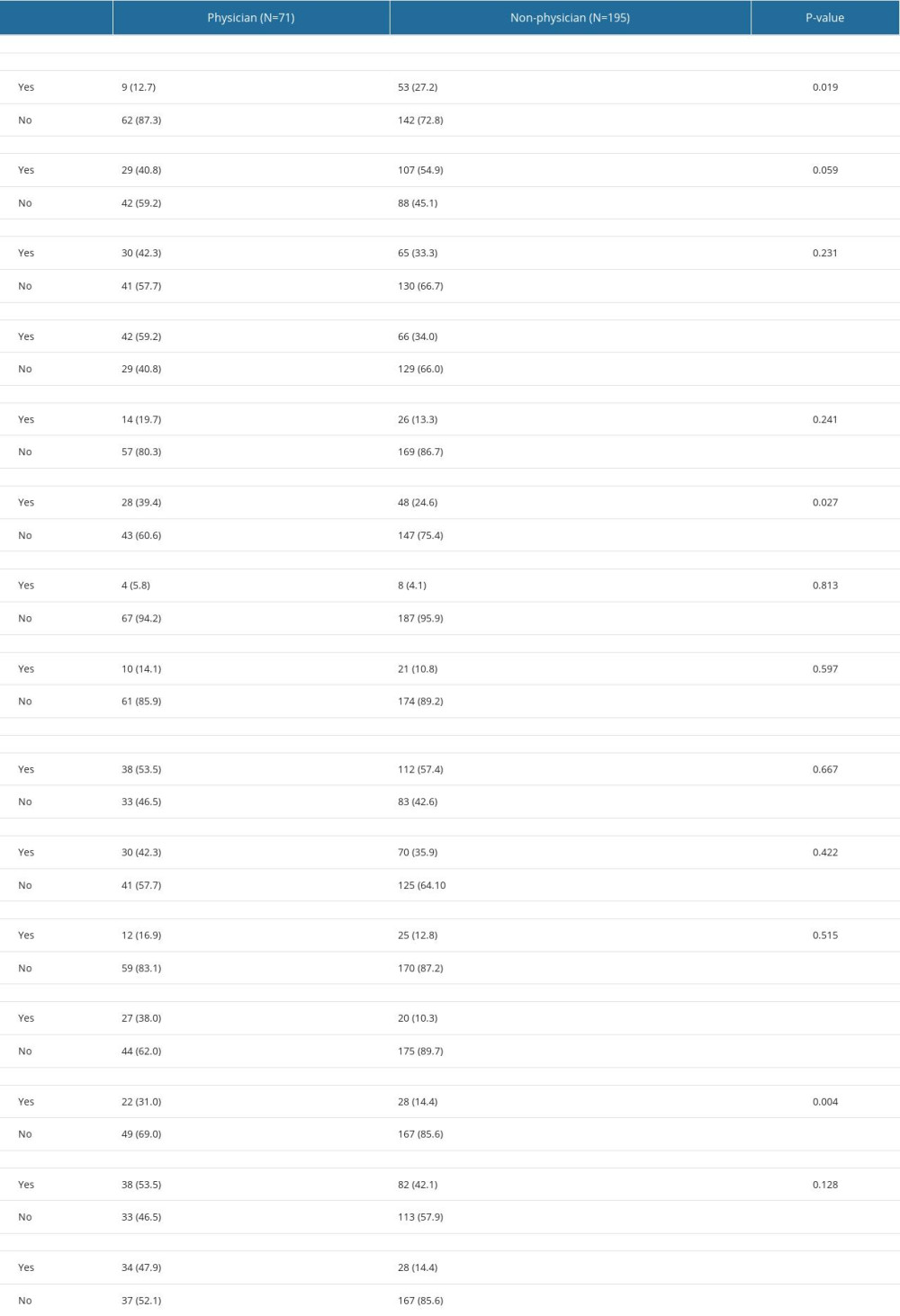 Table 3. Perception of institutional and healthcare provider-level barriers regarding early mobilization in pediatric intensive care units: comparison of opinion between non-physicians and physicians.
Table 3. Perception of institutional and healthcare provider-level barriers regarding early mobilization in pediatric intensive care units: comparison of opinion between non-physicians and physicians. In Press
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








