09 December 2023: Clinical Research
Long-Term Outcomes of Decompression and Grafting in Acute Pathological Proximal Femur Fractures in Children with Unicameral Bone Cysts: A Retrospective Study Utilizing a 120° Fixed-Angle Low-Contact Locking Pediatric Hip Plate
Müjdat Adaş1ABCDEF*, Murat Çakar1ACDEF, İsmail Demirkale1CDEFDOI: 10.12659/MSM.943031
Med Sci Monit 2023; 29:e943031
Abstract
BACKGROUND: Unicameral bone cysts (UBCs) are benign tumor-like lesions that are the most common cause of pathological proximal femur fracture in children. This study aimed to present the outcomes of acute, unstable, pathological proximal femur fractures secondary to UBCs in children.
MATERIAL AND METHODS: We retrospectively reviewed data on 12 patients with a mean age of 9.3 years (7-12 years) who were initially treated with decompression and grafting, followed by stabilization using a 120° fixed-angle low-contact locking pediatric plate (LCLPP). The Musculoskeletal Tumor Society (MSTS) scores, Capanna classification of cyst repair, time to union, collodiaphyseal angle (CDA), and limb length discrepancy (LLD) were evaluated.
RESULTS: The mean follow-up was 33.1 months (range, 13-96 months). The mean union time was 9.5 weeks (8-14 weeks). The mean time for reparation of the cyst was 6.9 months (range 3-9 months). Four patients had Dormans type IB, while the remaining had type IIB fractures. According to the Capanna classification, repairs in 10 cases were grade I and in 2 cases grade II. At the last follow-up, the mean 120.8° of preoperative CDA was corrected to 140.9° (P<0.001) and there was no difference compared to the healthy side (P=0.214). The mean postoperative MSTS score was 97.1% (29.1 points). Two patients experienced LLD at the affected extremities, while the other 10 patients healed without any complications.
CONCLUSIONS: Fixation of acute unstable fractures secondary to UBCs with a 120° fixed-angle LCLPP is a reliable and successful option after decompression and grafting of the lesion.
Keywords: Femur, Bone Cysts, Pediatrics
Background
Unicameral bone cysts (UBCs) are benign entities that typically manifest as cavities filled with interstitial fluid. These cysts are believed to be caused by local circulation abnormalities and predominantly occur in children and adolescents. The diagnosis can be readily established using direct radiographs. Other pathologies such as aneurysmal bone cysts, fibrous dysplasia, and enchondroma are considered in differential diagnosis. For those located in uncommon sites or when assessing fracture risk, T1-weighted magnetic resonance imaging (MRI) combined with measurement of the bone cyst index is usually preferred [1]. Unlike diaphyseal lesions, also termed latent cysts, UBC typically emerges at the proximal ends of tubular bones. They are found most frequently in the humerus, followed by the femur. It has been claimed that UBCs, the actual incidence of which is unknown, constitute approximately 3% of primary bone lesions. UBCs are typically asymptomatic and found incidentally during imaging. Usually the symptoms are pain, swelling, and deformity that occur after pathologic fractures. There is no need to treat unless symptoms develop or there is a risk of fracture [2].
Often, they do not display clinical symptoms unless detected incidentally. For UBCs located in asymptomatic and non-weight-bearing areas, treatments such as alendronate and botulinum toxin have been trialed but have not gained widespread acceptance [3]. Possible interventions for these patients include methylprednisolone injections, applications of autologous bone marrow, or a combination of demineralized bone matrix with bone marrow [4]. It is recognized that UBCs in the pertrochanteric region or those with significant enlargement (where the transverse diameter exceeds 85% or there is less than 0.55 mm of cyst wall remaining during follow-up) necessitate surgical treatment [5]. For those at risk of pathological fractures, ensuring stable fixation, decompressing, and breaking the cyst wall to facilitate bone marrow penetration into the cavity are paramount. The choice of filler post-decompression, be it calcium sulfate, chips allograft, or autologous bone grafts, depends on the cavity size. Close serial monitoring is crucial for asymptomatic cases. However, a definitively accepted treatment or fixation method has still not been found, especially for patients with acute pathological fractures in the proximal femur [5,6].
After such injuries, complications like avascular necrosis, epiphyseal growth arrest, or varus angulation due to mechanical instability after fracture have been noted. This instability arises because the lateral buttress becomes jeopardized by the lesion situated at the base of the neck and the intertrochanteric region [6]. In scenarios where ensuring mechanical stability proves arduous, selecting the right implant is imperative to prevent postoperative complications. Elastic stable intramedullary nails (ESIN) have become popular in recent years, even though they have been associated with complications such as LLD, malunion, and loss of reduction [7,8]. Erol et al have documented their treatment approaches for medium to large UBC cysts in children with acute proximal femur fractures, favoring decompression and grafting and stabilizing the fracture with ESIN [9]. Conversely, Jamshidi et al have chosen Philos plates combined with fibular strut grafting for these intricate situations [10]. While many fixation alternatives, ranging from external fixation to skeletal traction and from Philos plates to intramedullary nails, are available, the optimal approach remains undetermined for such cases [11]. Among these, locked fixed-angle plates, despite the poor bone quality, especially in pathological fractures, provide adequate fixation through multiple fixed-angle points without compromising the blood circulation to the bone surface. Additionally, being made of a titanium alloy and MRI-compatible, they offer a significant advantage in post-treatment tumor monitoring. Therefore, our aim in this study was to present the outcomes of 12 children with acute pathological fractures of the proximal femur due to UBCs, who underwent fixation with a 120° fixed-angle LCLPP following decompression and bone grafting.
Material and Methods
PATIENTS:
Before conducting this study, institutional review board and ethics committee approval were obtained (EC approval no: 90-27/03/2023) and only participants who signed a written consent form were included. A retrospective review of the digital patient database from the authors’ institution was conducted to identify patients who experienced a pathological fracture of the pertrochanteric femur due to UBC between September 2015 and January 2022. The diagnosis was established for all patients through direct radiographs. Transparent unicameral lesions were present in all cases, characterized by well-defined margins with sclerotic edges, accompanied by separated fracture ends and a narrow transition zone from adjacent normal bone. Additionally, for documentation and differential diagnosis, all patients underwent MRI. CT scans were performed to assess the bone fracture morphology and the preserved area of the posteromedial neck. To be included in this study, patients had to meet the following criteria: age 12 years or younger, a minimum of 1 year of follow-up, and present an unstable pathological fracture of the proximal femur attributed to UBC.
SURGICAL TECHNIQUE:
All surgeries were performed under general anesthesia with patients in the supine position. Fluoroscopy guided the procedures, and the same senior surgeon conducted all operations. Utilizing a direct lateral approach, the intertrochanteric region was accessed and the femur was exposed. After confirming the cyst’s unicameral nature via fluoroscopic examination with a radio-opaque substance, meticulous curettage was undertaken on the bone defect in either the lateral or anterior cortex. The material extracted during this process was forwarded for intraoperative frozen section analysis. Additionally, samples were collected for culture. Upon confirming UBC through the frozen section, the cystic cavity was filled with cancellous chips allograft. Temporary reduction of the fracture was achieved using K-wires. A 120° titanium alloy 3.5-mm or 4.5-mm locking LCPP was employed for fracture stabilization. Attention was paid to position the plate’s proximal end slightly below the trochanter major and to ensure the proximal screws did not harm the trochanteric epiphysis. In every case, the pre-bent 120
FOLLOW-UP AND POSTOPERATIVE CARE:
Patients underwent scheduled follow-up visits in the third and sixth weeks, followed by monthly visits up to the sixth month. Those who exhibited no complications during the ninth and twelfth months were subsequently followed annually until skeletal maturity was reached. At each follow-up session, the union of the fracture and the consolidation of the cyst were assessed using plain radiographs. For the initial 6 weeks after surgery, patients were advised to walk with the assistance of crutches, ensuring no weight was placed on the operated extremity. Once the post-surgical pain had entirely dissipated and at least 3 cortices of radiological callus formation were evident, patients were permitted partial weight-bearing.
DATA COLLECTION:
Details such as the patient’s age, sex, side of injury, injury mechanism, follow-up duration, radiographic time to fracture union, cyst reparation time, CDA, and ranges of motion (ROM) were meticulously recorded.
EVALUATION AND CLASSIFICATION:
The functional outcomes were gauged using the Musculoskeletal Tumor Society (MSTS) score [12]. The cyst type was categorized as per the Dormans classification system, while the cyst repair was assessed based on the Capanna classification [13,14]. Fractures were further classified based on anatomical location using the Delbet-Colonna classification system [15].
COMPLICATION RECORDS:
Any complications encountered were sourced from hospital records. Specific complications were duly noted, including avascular necrosis of the femoral head, LLD, infections, and heterotopic ossification.
STATISTICAL ANALYSIS:
Statistical analyses were conducted using SPSS version 25.0 software. Descriptive statistics, including mean, standard deviation, median and interquartile range (IQR), were utilized to present the data. The normality of the variables was assessed through histogram graphs and the Kolmogorov-Smirnov test. For normally distributed variables between groups, the independent group
Results
DEMOGRAPHIC CHARACTERISTICS:
There were 12 patients (9 boys and 3 girls) with a mean age of 9.3 years (range, 7–12 years) and a mean follow-up of 33.1 months (range, 13–96 months). The dominant side was fractured in 6 patients. Eight of the fractures were caused by simple falls while playing, 2 were due to sports injuries, 1 was due to a motor vehicle accident, and 1 patient was admitted after a fall from a bicycle. The demographic characteristics of the cases, fracture type, cyst classification, cyst reparation time, follow-up periods, and complications are shown in Table 1.
HEALING AND FUNCTIONAL OUTCOMES:
The mean time to union of the fractures was 9.5 weeks (range, 8–14 weeks). The mean time for reparation of the cyst was 6.9 months (range, 3–9 months). According to the Capanna classification, repairs in 10 cases were grade I, and were grade II in 2 cases, where minimal residual radiolucency is observed on the radiograph. There was no grade III or IV improvement in any patient. The mean 120.8° of preoperative CDA was corrected to 140.9° (P<0.001) (Table 2). The anatomical union was permanent at the last follow-up (mean CDA=138.7°), and there was no statistically significant difference when compared to the healthy side (P=0.214) (Figure 1). The mean MSTS score was 97.1% (29.1 points) (Table 2).
COMPLICATIONS:
No major complication was observed in any patient during the recovery period and until the end of the follow-up. In 1 case (patient 3), a deep infection developed after 3 months and required short-term intravenous treatment followed by oral antibiotic. In this case, the implants were removed at the 10th month (Figure 2). In this case, whose fracture was achieved full union and complete cyst repair, CDA decreased by 17° compared to the healthy side at the last follow-up, but the patient did not have any concerns. There was no problem with the implant in other patients and there was no request from the families for the removal of the implants. We did not have any patients who required revision surgery. In another case, we noticed an LLD that became evident from the 3rd month and developed a 3-cm LLD at last follow. In this case with a Dormans Type IIB cyst (patient 4), the CDA at the last follow-up was 117.4°, which meant that there was a difference of 21 degrees between legs with evidence of coxa vara. In other cases, there were no LLDs. Hip ROM on the operated side was within normal ranges in 10 patients. Only 2 patients had 10–20° less internal than the healthy side. The loss of internal rotation was evident in the patient with LLD.
Discussion
A pivotal discovery of this research was the anatomical side plate’s suitability as a fixation material in acute pathologic fractures of the proximal femur due to UBCs, primarily because of its capability to ensure correct screw placement in the posteromedial metaphysis region with the aid of 120 degrees of fixed-angle screw purchase where the bone typically remains intact.
For individuals who have achieved skeletal maturity, sliding hip screws or intramedullary nails are deemed the criterion standard for fixation in pathological proximal femur fractures [13]. However, securing acute proximal femur fractures attributed to UBCs presents a challenge for children and adolescents with an open epiphysis. Various fixation methods, such as ESIN, Philos plates (a type of side plate), and cannulated screws, have been employed [3,7,9,11]. Each method comes with its respective advantages and disadvantages. Notably, the Philos plate, when compared to other methods, is viewed as an off-label application for this specific region and does not align well with the anatomy of the proximal femur [11]. In parallel with our study, Jiang et al evaluated the suitability of fixation of acute pathologic fractures secondary to UBC using locking plates in 6 of 28 patients and found that fixation with locking plates was highly successful [16]. However, the study investigated the effectiveness of compressive locking plating without mentioning the fixed angle of proximal screws in this context [16].
A universally accepted criterion standard for fixation does not exist for these patients. Therefore, in addition to meticulous curettage and bone grafting, we evaluated results of application of the 120° fixed-angle LCLPP for these cases presenting with unstable fractures where the lateral buttress was lost. Of the study participants, 2 exhibited LLD: one resulting from varus malunion caused by a severe infection that required premature implant extraction, while the cause for the other remains undetermined. The remaining 10 cases manifested no complications.
The management of proximal femoral UBCs presents a challenge due to the weight-bearing nature of the region, the potential for recurrence, and the intricacies associated with securing stable fixation [10,17]. Particularly in Dormans Type IB and Type IIB UBC presenting with acute pathological fractures, the limited availability of intact bone stock for proximal screw anchorage elevates the risks of varus malunion, avascular necrosis, and nonunion [18]. In such scenarios, it is imperative to ensure prompt mobilization and prevention of deformity through anatomical realignment and steadfast fixation. Although numerous techniques have been proposed to achieve this, a consensus on the ideal treatment remains elusive [10]. Contrary to other regions where the spontaneous healing of fractures might be anticipated, the emphasis in this area leans more towards addressing the fracture rather than the cyst when considering the fixation of pathological fractures, as corroborated by the existing literature [9,10,19].
Following anatomical realignment, we employed a 120° fixed-angle locking LCLPP as a fixation technique. This method neither compromises the epiphysis nor harms the weakened lateral buttress, directing the uppermost screws toward the posterior-medial metaphyseal zone, frequently found intact in these cases. Although 2 patients in our study exhibited a deep infection and a LLD of undetermined origin, the remaining subjects demonstrated no fixation-associated complications. These outcomes underscore the viability of this fixation approach for such intricate cases. In contemporary orthopedic practice, ESIN has gained attention as a fixation alternative. While its intramedullary placement seemingly offers robust resistance against external forces, this method poses certain drawbacks in these cases, such as the potential for neck perforation and the lack of sturdy proximal fixation points, resulting in complications like loss of reduction [20]. Although it is deemed suitable for impending subtrochanteric fractures, the timeline for early weight-bearing remains constrained [21]. Our findings, which show the almost unaltered shaft-neck angle during postoperative assessments, indicate that this fixation modality offers superior mechanical backing by effectively countering rotational and bending forces.
Notably, our cohort had no recurrences, and we observed no signs of graft resorption during follow-up assessments. The absence of UBC recurrence among our patients cannot be solely attributed to the choice of osteosynthesis material. We posit that cyst drainage due to fracture formation at the cyst base and thorough tumor excision using a burr significantly influenced this outcome. Urakawa et al previously highlighted the enhanced healing propensity of UBC post-pathological fracture, hypothesizing that post-fracture callus osteogenesis might expedite cyst healing [22]. Similarly, in a study comparing the treatment of bone cysts in 129 patients using 3 different intralesional techniques, it was demonstrated that open surgery, involving removal of the intracystic membrane and filling the lesion with a graft, was the most successful treatment method [23].
We concur with the consensus that premature closure of the femoral head epiphysis is plausible in these fractures. As such, we advocate for periodic leg length radiographic evaluations every 3 months for the first 2 years and semi-annually thereafter until growth cessation. Our data reveal that discrepancies in limb lengths adversely impact the MSTS score. However, with a monitoring duration exceeding 1 year, our patients’ MSTS scores closely resembled those of unaffected individuals, save for a solitary case presenting a 3-cm shortening.
This study is not without limitations, chief among them being the modest sample size and the comparatively brief monitoring period. The retrospective design might seem like a constraint, but the ethical implications tied to randomization can impinge upon the inception of a more rigorous study. Nevertheless, observational retrospective comparative therapeutic studies encompassing a broader patient pool could furnish a more nuanced understanding of such cases.
Conclusions
Our study underscores the potential of meticulous curettage, grafting, and using a 120° fixed-angle locking LCPP for fixation to yield successful results in UBC cases with acute unstable fractures where lateral cortical support is compromised.
Figures
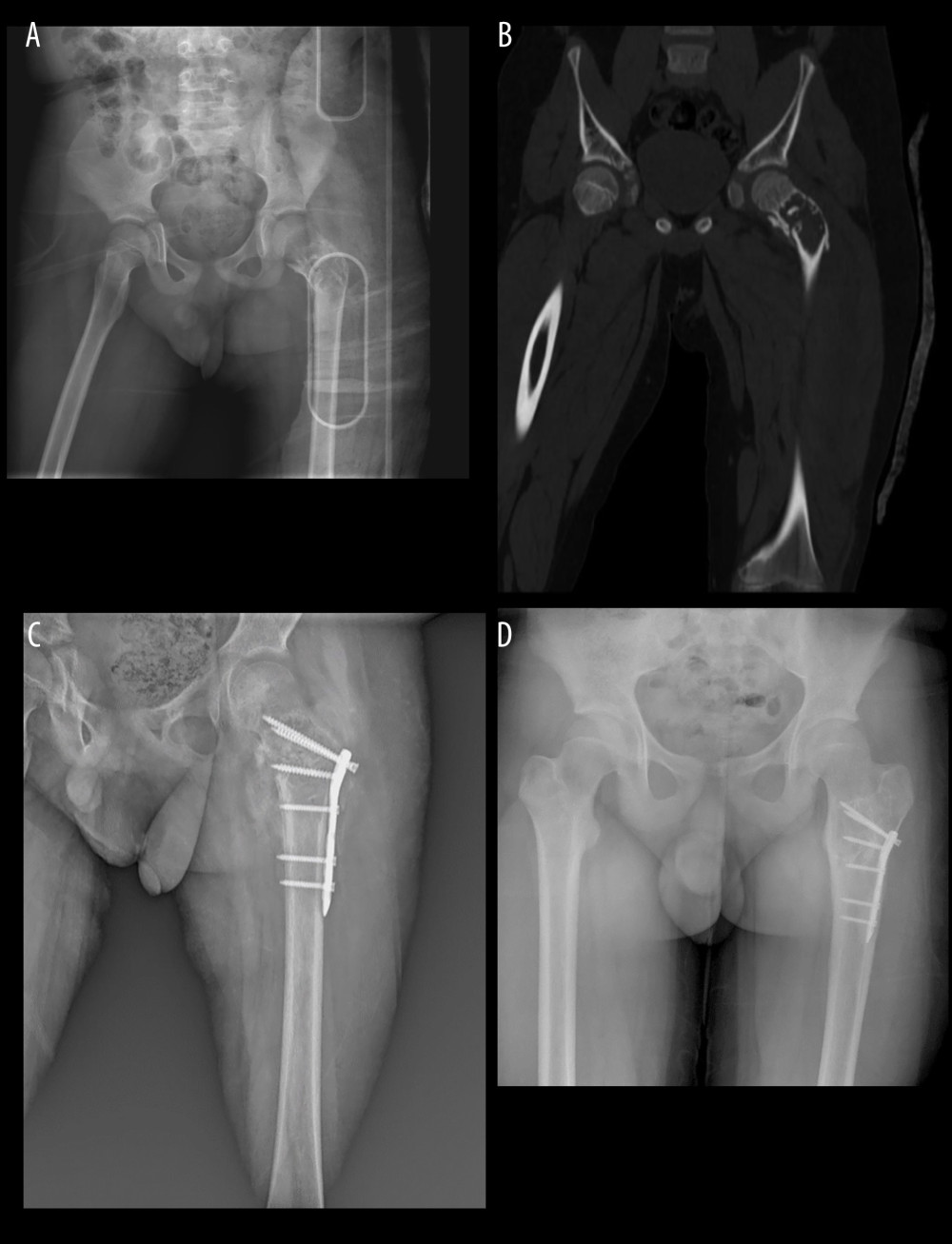 Figure 1. (A) Preoperative X-ray of an 8-year-old boy (Case 1). (B) Preoperative CT of Case 1. (C) Early postoperative X-Ray of Case 1. (D) Postoperative 8. year X-ray Case 1.
Figure 1. (A) Preoperative X-ray of an 8-year-old boy (Case 1). (B) Preoperative CT of Case 1. (C) Early postoperative X-Ray of Case 1. (D) Postoperative 8. year X-ray Case 1. 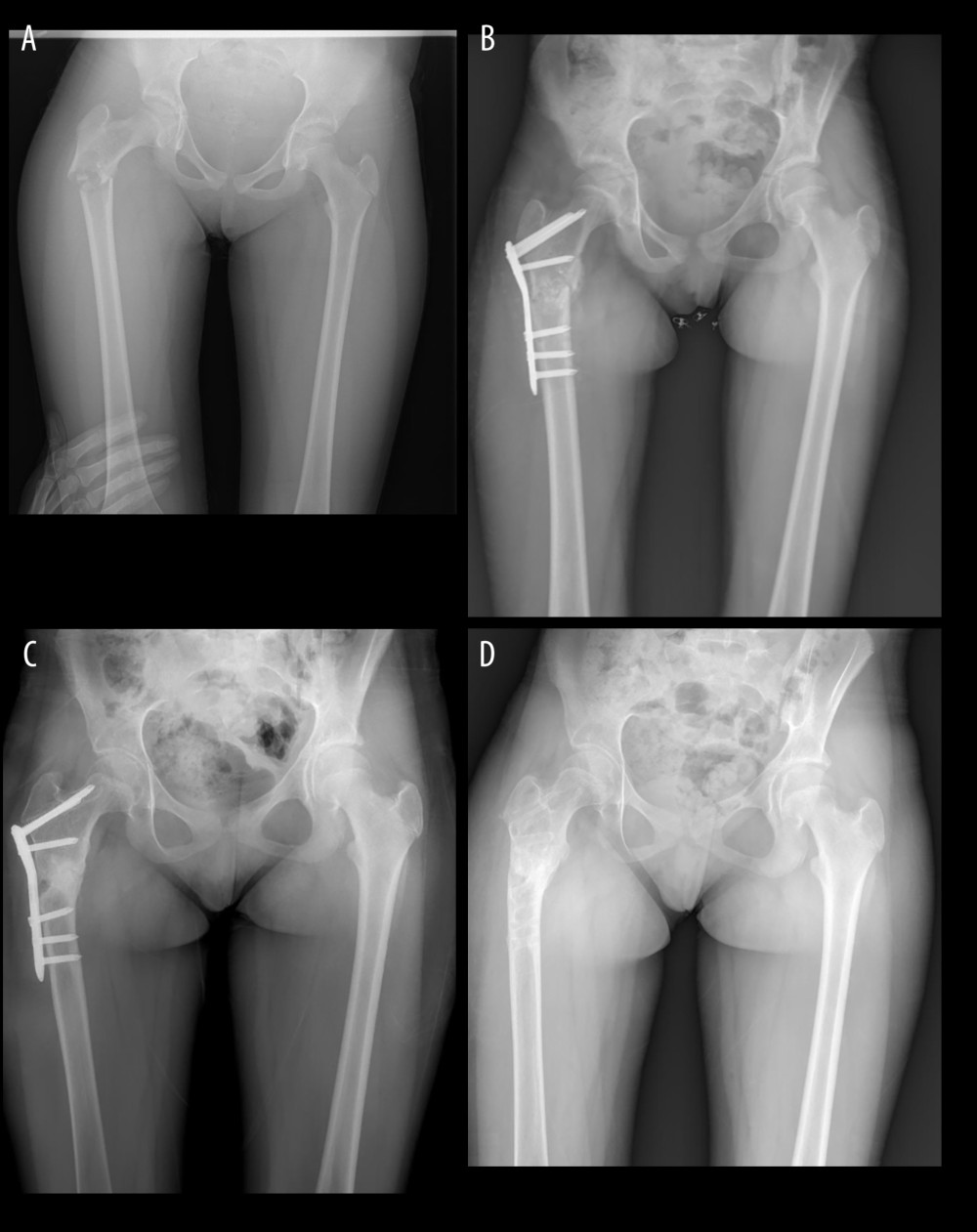 Figure 2. (A) Preoperative X-ray of a 12-year-old girl (Case 3). (B) Early postoperative X-ray of Case 3. (C) Postoperative 10. Month X-ray of Case 3. (D) Postoperative 2. year X-ray of Case 3.
Figure 2. (A) Preoperative X-ray of a 12-year-old girl (Case 3). (B) Early postoperative X-ray of Case 3. (C) Postoperative 10. Month X-ray of Case 3. (D) Postoperative 2. year X-ray of Case 3. References
1. Pireau N, De Gheldere A, Mainard-Simard L, Fracture risk in unicameral bone cyst: Is magnetic resonance imaging a better predictor than plain radiography? Acta Orthop Belg, 2011; 77(2); 230-38
2. Evans J, Shamrock AG, Blake J, Unicameral bone cyst: StatPearls, 2023, StatPearls Publishing www.ncbi.nlm.nih.gov/books/NBK470587/
3. Donaldson S, Chundamala J, Yandow S, Wright JG, Treatment for unicameral bone cysts in long bones: An evidence based review: Orthop Rev (Pavia), 2010; 2(1); e13
4. Çakar M, Bülbül AM, Triple methylprednisolone injections for simple humerus cysts at one-month intervals: Eur Arc Med Res, 2018; 34; 132-36
5. Rajasekaran RB, Krishnamoorthy V, Gulia A, Unicameral bone cysts: Review of etiopathogenesis and current concepts in diagnosis and management: Indian J Orthop, 2022; 56(5); 741-51
6. Noordin S, Allana S, Umer M, Unicameral bone cysts: Current concepts: Ann Med Surg (Lond), 2018; 34; 43-49
7. Ho CA, Skaggs DL, Tang CW, Kay RM, Use of flexible intramedullary nails in pediatric femur fractures: J Pediatr Orthop, 2006; 26(4); 497-504
8. Chen X, Chen K, Su Y, Evaluation of immediate and delayed surgery for pathological fracture due to unicameral bone cysts in children: J Child Orthop, 2020; 14(4); 335-42
9. Erol B, Topkar MO, Aydemir AN, A treatment strategy for proximal femoral benign bone lesions in children and recommended surgical procedures: Retrospective analysis of 62 patients: Arch Orthop Trauma Surg, 2016; 136(8); 1051-61
10. Jamshidi K, Mirkazemi M, Izanloo A, Mirzaei A, Locking plate and fibular strut-graft augmentation in the reconstruction of unicameral bone cyst of proximal femur in the paediatric population: Int Orthop, 2018; 42(1); 169-74
11. Danişman M, Özdemir E, Dursun G, An alternative fixation option for subtrochanteric femur fractures in children: Adult proximal humerus plate: J Pediatr Orthop, 2022; 42(8); e828-e32
12. Enneking WF, Dunham W, Gebhardt MC, A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system: Clin Orthop Relat Res, 1993(286); 241-46
13. Dormans JP, Pill SG, Fractures through bone cysts: Unicameral bone cysts, aneurysmal bone cysts, fibrous cortical defects, and nonossifying fibromas: Instr Course Lect, 2002; 51; 457-67
14. Capanna R, Dal Monte A, Gitelis S, Campanacci M, The natural history of unicameral bone cyst after steroid injection: Clin Orthop Relat Res, 1982(166); 204-11
15. Miu A, Pathological fractures of the proximal femur due to solitary bone cyst: Classification, methods of treatment: J Med Life, 2015; 8(4); 536-43
16. Jiang X, Application of the Locking Compression Pediatric Hip Plate™ in children with proximal femoral tumors: J Orthop Surg Res, 2022; 17(1); 536
17. Dong C, Klimek P, Abächerli C, Percutaneous cyst aspiration with injection of two different bioresorbable bone cements in treatment of simple bone cyst: J Child Orthop, 2020; 14(1); 76-84
18. Li J, Ze R, Rai S, Is elastic stable intramedullary nail a good choice for pathological fractures of the proximal femur due to simple bone cyst in pediatric population?: Medicine (Baltimore), 2020; 99(39); e22364
19. Tomaszewski R, Rutz E, Mayr J, Dajka J, Surgical treatment of benign lesions and pathologic fractures of the proximal femur in children: Arch Orthop Trauma Surg, 2022; 142(4); 615-24
20. Roposch A, Saraph V, Linhart WE, Treatment of femoral neck and trochanteric simple bone cysts: Arch Orthop Trauma Surg, 2004; 124(7); 437-42
21. Li W, Xu R, Du M, Chen H, Comparison of titanium elastic intramedullary nailing versus injection of bone marrow in treatment of simple bone cysts in children: A retrospective study: BMC Musculoskelet Disord, 2016; 17(1); 343
22. Urakawa H, Tsukushi S, Hosono K, Clinical factors affecting pathological fracture and healing of unicameral bone cysts: BMC Musculoskelet Disord, 2014; 15; 159
23. Bukva B, Vrgoč G, Abramović D, Treatment of unicameral bone cysts in children: A comparative study: Acta Clin Croat, 2019; 58(3); 403-9
Figures
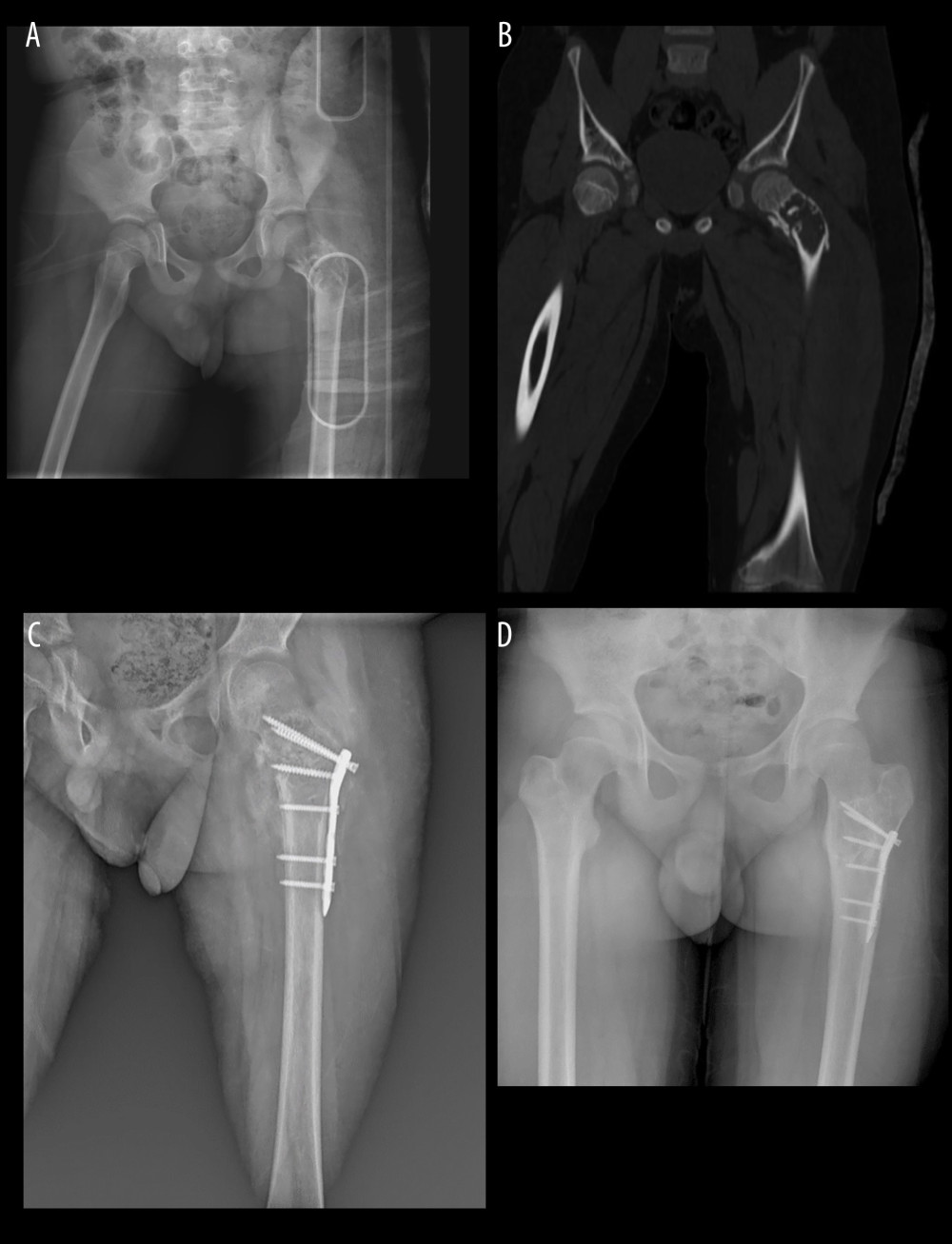 Figure 1. (A) Preoperative X-ray of an 8-year-old boy (Case 1). (B) Preoperative CT of Case 1. (C) Early postoperative X-Ray of Case 1. (D) Postoperative 8. year X-ray Case 1.
Figure 1. (A) Preoperative X-ray of an 8-year-old boy (Case 1). (B) Preoperative CT of Case 1. (C) Early postoperative X-Ray of Case 1. (D) Postoperative 8. year X-ray Case 1.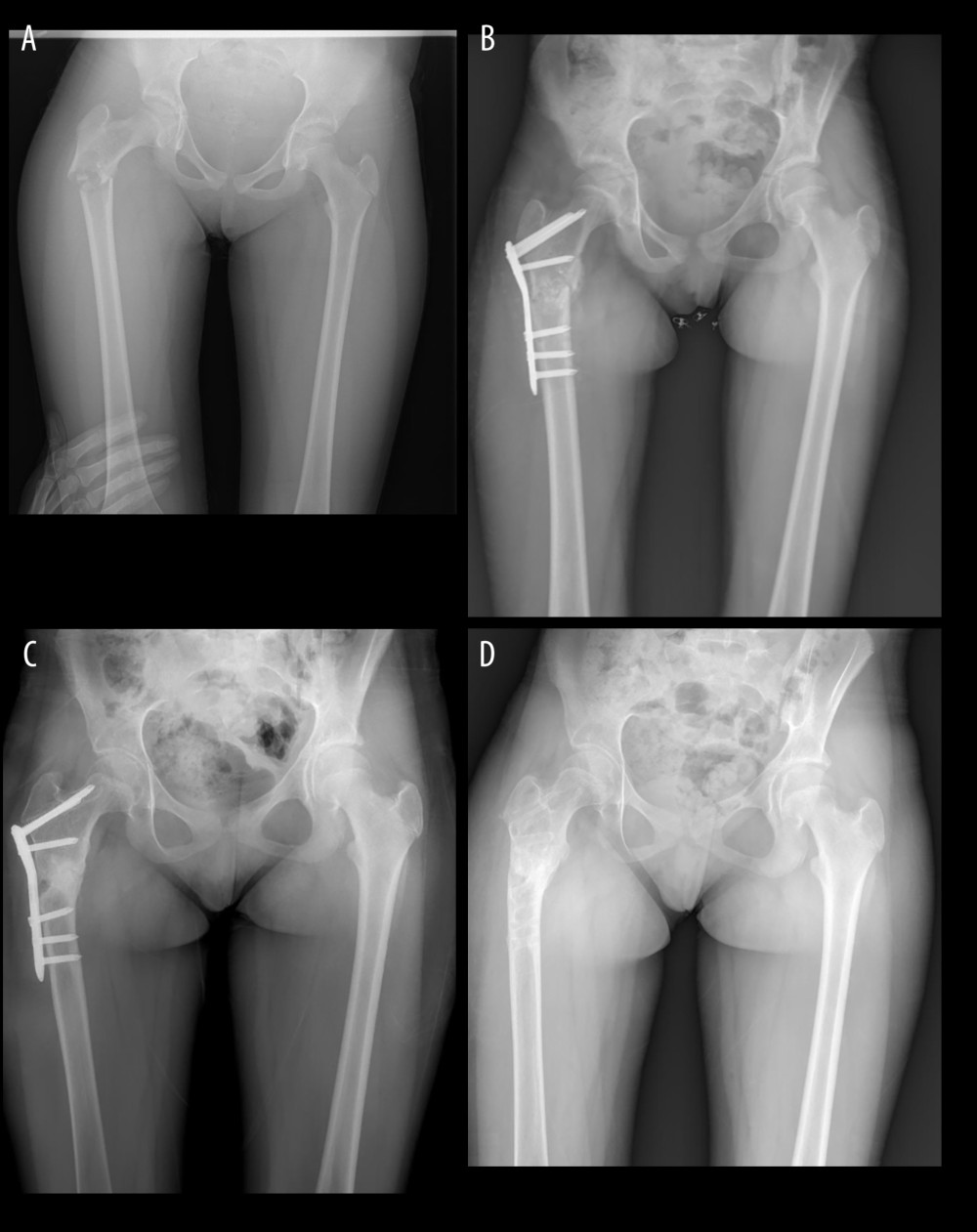 Figure 2. (A) Preoperative X-ray of a 12-year-old girl (Case 3). (B) Early postoperative X-ray of Case 3. (C) Postoperative 10. Month X-ray of Case 3. (D) Postoperative 2. year X-ray of Case 3.
Figure 2. (A) Preoperative X-ray of a 12-year-old girl (Case 3). (B) Early postoperative X-ray of Case 3. (C) Postoperative 10. Month X-ray of Case 3. (D) Postoperative 2. year X-ray of Case 3. Tables
 Table 1. Data on 12 pediatric patients with pathological proximal femur fractures.
Table 1. Data on 12 pediatric patients with pathological proximal femur fractures.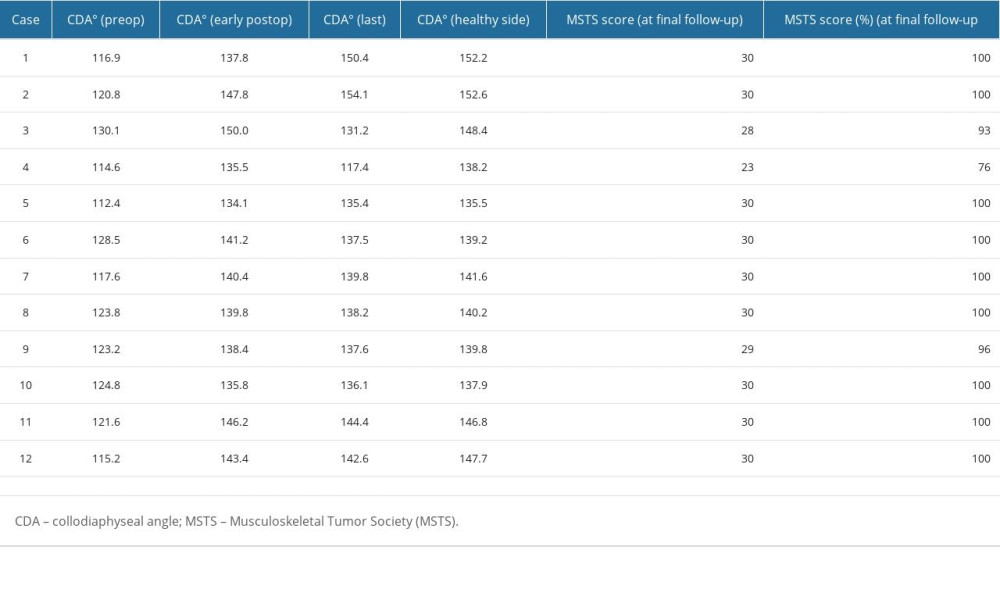 Table 2. CDA changes in the damaged hip preoperatively, postoperatively, and at final follow-up. MSTS scores at the last follow-up.
Table 2. CDA changes in the damaged hip preoperatively, postoperatively, and at final follow-up. MSTS scores at the last follow-up. Table 1. Data on 12 pediatric patients with pathological proximal femur fractures.
Table 1. Data on 12 pediatric patients with pathological proximal femur fractures.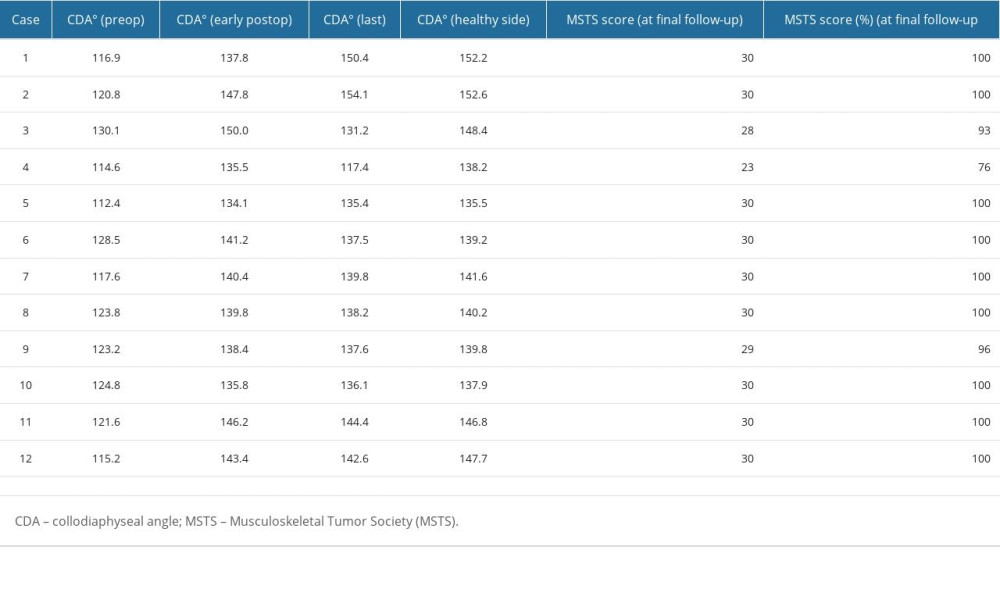 Table 2. CDA changes in the damaged hip preoperatively, postoperatively, and at final follow-up. MSTS scores at the last follow-up.
Table 2. CDA changes in the damaged hip preoperatively, postoperatively, and at final follow-up. MSTS scores at the last follow-up. In Press
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








