04 March 2024: Clinical Research
Efficacy of Bakri Intrauterine Balloon in Managing Postpartum Hemorrhage: A Comparative Analysis of Vaginal and Cesarean Deliveries with Placenta Accreta Spectrum Disorders
Feifei Chen1BCEF, Chong Zhang1BCEF, Yaping Hu1ADEG*DOI: 10.12659/MSM.943072
Med Sci Monit 2024; 30:e943072
Abstract
BACKGROUND: The incidence of placenta accreta spectrum disorder (PAS) has been increasing in past decades, and women with PAS are a high-risk maternal population. This study aimed to explore the performance of Bakri intrauterine balloon tamponade (IUBT) in the treatment of postpartum hemorrhage (PPH), among those with and without PAS.
MATERIAL AND METHODS: The outcomes of 198 women who underwent treatment for PPH using IUBT were retrospectively analyzed. The demographics and maternal outcomes were analyzed for vaginal and cesarean births, with PAS and without PAS.
RESULTS: Compared to women with vaginal births (n=130), women who underwent cesarean births (n=68) showed a higher proportion of age ≥35 years (χ²=6.85, P=0.013), multiple births (χ²=13.60, P<0.001), preeclampsia (χ²=9.81, P=0.002), use of transabdominal IUBT (χ²=84.12, P<0.001) and pre-IUBT interventions (χ²=41.61, P<0.001), but had less infused volume of physiological saline (t=6.41, P<0.001). Women with PAS (n=105) showed a higher rate of pre-IUBT intervention (χ²=4.96, P=0.029) and transabdominal IUBT placement (χ²=9.37, P=0.002) than non-PAS women (n=93). The 36 women with PAS (n=36) showed a higher rate of preeclampsia (χ²=4.80, P=0.029), pre-IUBT intervention (χ²=5.90, P=0.015), and transabdominal IUBT placement (χ²=14.94, P<0.001) and a shorter duration from delivery to Bakri insertion (χ²=3.31, P=0.002), than non-PAS women (n=32).
CONCLUSIONS: PAS was a major cause of PPH at 198 vaginal and cesarean births. An accurate and timely pre-IUBT intervention and Bakri IUBT placement was critical for controlling PPH in cesarean births, especially in women with PAS.
Keywords: maternal health, Placenta Accreta, Cesarean Section, Treatment Outcome, Uterine Balloon Tamponade, Uterine Hemorrhage
Background
Postpartum hemorrhage (PPH) is still the leading cause of severe maternal morbidity and mortality worldwide [1,2]. Most maternal deaths caused by PPH occur within the first 24 h after birth [3]. To date, there is no criterion standard treatment for PPH at cesarean surgery [4], although there is a criterion standard protocol that effectively prevents PPH > 1000 mL at vaginal birth [5]. Emergency hysterectomy may be performed for PPH, but emergency hysterectomy is not completely effective in controlling PPH, with around 50% requiring additional procedures to stop bleeding [6], and hysterectomy is correlated with high morbidity [7]. Among various conservative procedures, a Bakri IUBT has been recommended to control PPH in second-line treatment, presenting remarkable advantages such as minimal local resource requirements, little required training, and high effectiveness in retaining fertility [8,9]. However, conflicting evidence about the efficacy of Bakri IUBT has been observed, and much evidence was empirical [9,10]. With the recent three-child policy in China, there has been an increase in elderly pregnant women, which may be associated with the increased incidence of PPH [11] and cesarean section [12]. Another cause of increased PPH is placenta accreta spectrum (PAS), which refers to abnormally adherent or invasive placentas [13]. In past decades, the incidence of PAS has been increasing mainly due to the increasing cesarean surgery and other uterine surgery such as curettage for miscarriage births [14]. Recent treatments for PPH mainly focus on the effectiveness of internal iliac artery (IIA) balloon occlusion among patients after cesarean delivery [15,16].
In this study, we aimed to explore the outcomes after the use of Bakri intrauterine tamponade, inserted vaginally or abdominally, in controlling PPH in 198 vaginal and cesarean births. The performance of Bakri IUBT in women with and without PAS was also compared.
Participants
BASELINE CHARACTERISTICS AND MATERNAL OUTCOME MEASURES:
The maternal clinical characteristics and maternal outcomes were collected. All data were de-identified before analyses. The variables between women with vaginal births and cesarean births; women with and without PAS were compared.
STATISTICAL ANALYSIS:
Analyses were performed using SPSS version 22.0 (IBM Corp., Armonk, NY). Measurement data are presented as means±SD, which were analyzed by using the
Results
CHARACTERISTICS ANALYSIS IN WOMEN WITH PPH USING BAKRI IUBT IN 198 VAGINAL AND CESAREAN BIRTHS:
In the study, a total of 198 pregnant women treated for PPH using Bakri IUBT were selected, including 130 women with vaginal births and 68 women with cesarean births (Table 1). Compared with women with vaginal births, women with cesarean births showed a higher proportion of maternal age ≥35 year (χ2=6.85, P=0.013), multiple births (χ2=13.60, P<0.001), and preeclampsia (χ2=9.81, P=0.002). Nineteen women had premature births (<37 weeks), including 10 vaginal births and 9 cesarean births. There were no significant differences in variables such as weight, gestational age, parity, repeat cesarean section, gestational diabetes, gestational hypertension, and uterine atony between the 2 groups (P>0.05).
MATERNAL OUTCOMES AFTER THE USE OF BAKRI IUBT IN CONTROLLING PPH AT 198 VAGINAL AND CESAREAN BIRTHS:
The maternal outcomes in 198 women with vaginal and cesarean births were analyzed (Table 2). The women with cesarean births had more use of transabdominal IUBT placement (χ2=84.12, P<0.001) and pre-IUBT interventions (χ2=41.61, P<0.001), but less infused volume of physiological saline (t=6.41, P<0.001). In vaginal births, a pre-IUBT intervention of toothless oval cervical clamp was used before Bakri IUBT balloon in 9.2% (12/130) of women. In cesarean births, single or combined use of “8” suture and arterial ligation were employed for 50.0% (34/68) of women. Women after cesarean section required fewer blood transfusions than women with vaginal births (P<0.001), but needed a higher volume of blood components: red blood cells, cryoprecipitate, and plasma transfused (P<0.05). The Bakri IUBT success rate was 81.31% (108/130) in vaginal births and 86.8% (59/68) in cesarean births. None required a hysterectomy, and only 2 women delivering vaginally had puerperal fever after the use of Bakri IUBT. Among the 7 cases with previous cesarean section, there were 3 cases of successful VBACs (vaginal birth after cesarean).
COMPARISON OF PERFORMANCE OF BAKRI IUBT IN WOMEN WITH PAS AND THOSE WITHOUT PAS:
The performance of Bakri IUBT in women with PAS (n=105) and those without PAS (n=93) was also compared (Figure 1). Compared to women without PAS, women with PAS showed a higher rate of pre-IUBT intervention (χ2=4.96, P=0.029) and transabdominal IUBT placement (χ2=9.37, P=0.002). However, women with PAS showed no significant differences in delivery mode, gestational age, repeat cesarean section, total EBL, pre-/post-IUBT EBL, infused volume of IUBT, IUBT indwelling duration, or rate of hemostasis, and had less genital tract trauma, blood transfusion, post-IUBT intervention, and puerperal fever than women without PAS (P>0.05).
OUTCOMES AFTER THE USE OF BAKRI IUBT IN CONTROLLING PPH IN WOMEN WITH PAS AND CESAREAN BIRTHS:
In cesarean births (n=68), the outcomes after the use of Bakri IUBT in controlling PPH between women without PAS (47.1%, n=32) and women with PAS (52.9%, n=36) were further compared (Figure 2). The women with PAS had a higher rate of preeclampsia (χ2=4.80, P=0.029), transabdominal IUBT placement (χ2=14.94, P<0.001), and pre-IUBT intervention (χ2=5.90, P=0.015), and a shorter time from delivery to Bakri insertion (χ2=3.31, P=0.002). Among the 36 cases with PAS, there were 7 cases with premature births (28w ≤ gestational age <37w, 19.4%, 7/36) and 2 cases with previous cesarean (5.6%, 2/36). There were no significant differences in other variables (all P>0.05).
Discussion
In obstetrics, PPH remains the predominant cause of severe maternal morbidity and mortality. This retrospective cohort study analyzed the characteristics and maternal outcomes after the use of Bakri IUBT in controlling PPH in 198 vaginal and cesarean births of women with and without PAS from Jan 2016 to Dec 2020 in a single center. Our findings demonstrated that PAS was a major cause of PPH among in 198 vaginal and cesarean births. An accurate and timely pre-IUBT intervention and Bakri IUBT placement was critical for controlling PPH in cesarean births, especially in women with PAS. Women with cesarean births accounted for 34% of the women treated with Bakri and women with PAS accounted for 53.0%. Among the women delivering by cesarean section, 52% also had PAS, including 2 women with history of previous cesarean section. Moreover, the women with PAS (n=36) had higher rates of preeclampsia, pre-IUBT intervention, and transabdominal IUBT placement and a shorter time from delivery to Bakri insertion, than those without PAS (n=32).
The demographic characteristics analysis revealed that women with cesarean births had a higher proportion of maternal age ≥35, multiple births, and preeclampsia than those delivering vaginally. The results were consistent with previous studies [18–20]. Advanced maternal age increased risks for preeclampsia, cesarean section, and adverse pregnancy outcomes [18–20]. Further analysis of the maternal outcomes of cesarean births demonstrated more use of transabdominal IUBT placement and pre-IUBT interventions, but less infused volume of physiological saline than vaginal births. Transabdominal IUBT placement was more common at cesarean births. Considering the risks of physiological saline infusion, it should be used only in an emergency. In the present study, 34 women received a pre-IUBT intervention at cesarean births, which was correlated with transabdominal IUBT placement. The fact that 26 women with transabdominal IUBT placement received a pre-IUBT intervention verified our speculations that accurate and timely pre-IUBT intervention and Bakri IUBT placement can contribute to controlling PPH in cesarean births.
In past decades, the incidence of PAS has been increasing due to the in vitro fertilization techniques and increased rates of elective cesarean sections [16,21]. PAS can result in massive bleeding or peripartum hysterectomy [14]. In our study, characteristics analysis in women with PPH using Bakri IUBT revealed that PAS was present in 53% of women delivering vaginally and by cesarean, which was slightly higher than the 42% rate of uterine atony. It is suggested that PAS was a major cause of PPH, and the primary cause in this study, which was consistent with Li’s study [22]. The high rate of PAS may be due to the large number of critically ill patients referred from other hospitals, including a high proportion of women with PAS. Besides a second cesarean, a previous history of other uterine surgery, curettage, uterine fibroleiomyoma, uterine cavity infection, and endometritis can result in PAS [23]. PAS was mainly diagnosed by checking the integrity of the discharged placenta after placental detachment or manual delivery of the placenta, in combination B mode ultrasound. Ultrasound was highly sensitive and specific in the prenatal diagnosis of placenta accreta when performed by skilled operators [24]. An accurate prenatal diagnosis of PAS was confirmed by a multidisciplinary team to avoid over-diagnosis or misdiagnosis of PAS.
The maternal outcomes after the use of Bakri IUBT in women with PAS were further analyzed. Notably, the women with PAS among the 68 cesarean births had a higher rate of pre-IUBT intervention and transabdominal IUBT placement than those with non-PAS. This may be due to the high PAS rate in both vaginal and cesarean births, suggesting a positive correlation with pre-IUBT intervention and transabdominal IUBT placement. It was reported that most PPH-related deaths are considered preventable, which highlights the critical importance of risk assessment and early intervention [25,26]. Previous research has assessed use of pre-IUBT intervention such as toothless oval cervical clamp, gauze compression, figure-of-8 closure, artery ligation, and UAE. Temporary uterine artery occlusion is associated with a theoretical fertility advantage [27]. In vaginal births, a toothless, oval cervical clamp was used but was not effective before Bakri IUBT balloon in 9.2% (12/130) of women [28]. In our study, after cesarean births, single or combined use of a figure-8 suture and arterial ligation were applied in 50.0% (34/68) of women. The massive pre-IUBT EBL suggests that pre-IUBT hemostatic impairment and hemodynamic instability at the early phase of PPH caused women with PAS to lose more blood. Our results suggest that a pre-IUBT intervention may contribute to sufficient hemodynamic stability for delivery of the placenta. In our study, women with PAS in cesarean births also had a shorter time from delivery to Bakri insertion. The 5 cases with preeclampsia were all accompanied by PAS and delivered by cesarean birth. In our clinical practice, manual removal of the placenta is usually performed 30 min after delivery. However, the subsequent postpartum bleeding was very rapid in some cases, especially among those who had manual delivery of the placenta after 30 min. Cohain suggests waiting only 15 min for better results [5]. According to guidelines, IUBT was applied after the failed first-line conservative treatment (uterotonic agent and uterine massage), which resulted in a mean delivery/insertion duration of ≥1 h. Women with PAS had a significantly higher proportion of delivery/insertion duration <1 h than those without PAS in our study (75.0%, 27/36 vs 34.4%, 11/32; χ2=11.34, P=0.001). Wang et al found that timely insertion of IUBT after delivery could effectively improve the perinatal outcome of PPH and reduce the cesarean section rate [29]. Similarly, Wang et al reported that the combination of rapid diagnosis of PPH with early use of the IUBT was more effective for PPH management [30]. The evidence here suggests that a pre-IUBT intervention can prevent a significant amount of bleeding. A pre-IUBT contributed to controlling PPH. An accurate and timely pre-IUBT intervention and Bakri IUBT placement was critical for controlling PPH in cesarean births, especially in women with PAS.
In our study, women with IUBT failure immediately received a post-IUBT intervention (UAE or IIAE), and none required postpartum hysterectomy. This suggests an immediate post-IUBT intervention is an effective alternative to hysterectomy. Embolization, such as UAE, has been previously shown to be an effective PPH treatment [31,32], even in women with PAS [33]. In addition, in contrast to other countries such as Israel [34], blood transfusion was more commonly used in China. In our study, blood loss was estimated mainly through gravimetric measurement, in which blood loss volume is determined by subtracting the dry weight of items from the weight of blood-soaked items. We also collect blood in calibrated canisters using a negative-pressure aspirator after birth of the neonate, avoiding the problem of measuring non-blood fluids. We found that 80.30% (159/198) of women received blood transfusions, including 96.67% (115/130) of vaginal births and 64.7% (44/68) of cesarean births. A higher average transfusion of red blood cells, cryoprecipitate, and plasma may reflect a more critically ill status in cesarean births than vaginal births. Similarly, the need for blood transfusion in women with PAS also showed an increasing trend compared to those without PAS. The reason for the high blood transfusion rate was multifactorial, including prenatal anemia, unstable vital signs, and postpartum anemia. The technique of autologous blood transfusion in our hospital also provides a portion of the blood supply [35]. To cope with emergency situations, IUBT insertion/indwelling duration and hemostatic volume should be the top considerations.
Several limitations in our study should be addressed. The women were from 1 hospital in a 4-year period, which resulted in a relatively small sample size. Due to our study’s retrospective nature, sample selection bias was inevitable. However, the data about the outcomes of IUBT in women with PAS supplemented the existing limited evidence. More research is still needed to assess the potential effect of premature births, pre-IUBT intervention, and the timing of balloon insertion on maternal outcomes. To minimize postpartum bleeding, genital tract trauma, and blood transfusion postpartum, more techniques such as Judy’s 3,4,5 minute third-stage protocol [5] should be promoted.
Conclusions
An accurate and timely pre-IUBT intervention and Bakri IUBT placement was critical for controlling PPH in cesarean births, especially in women with PAS. PAS may be a major cause of PPH in China due to higher rates of history of curettage, uterine fibroleiomyoma, or previous uterine cavity infection. Blood transfusion was commonly used in women with massive postpartum bleeding. A pre-IUBT intervention may be considered in an urgent situation to increase the hemostasis success rate in women with PAS. Our study expands the evidence on IUBT in controlling PPH, providing support for balloon placement in clinical practice.
Figures
References
1. Say L, Chou D, Gemmill A, Global causes of maternal death: A WHO systematic analysis: Lancet Glob Health, 2014; 2(6); e323-33
2. , Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017: Lancet, 2018; 392(10159); 1736-88
3. Khan KS, Wojdyla D, Say L, WHO analysis of causes of maternal death: A systematic review: Lancet, 2006; 367(9516); 1066-74
4. Collins P, Abdul-Kadir R, Thachil J, Management of coagulopathy associated with postpartum hemorrhage: Guidance from the SSC of the ISTH: J Thromb Haemost, 2016; 14(1); 205-10
5. Cohain JS: Eur J Obstet Gynecol Reprod Biol, 2022; 278; 29-32
6. Michelet D, Ricbourg A, Gosme C, Emergency hysterectomy for life-threatening postpartum haemorrhage: Risk factors and psychological impact: Gynecol Obstet Fertil, 2015; 43(12); 773-79
7. Huque S, Roberts I, Fawole B, Risk factors for peripartum hysterectomy among women with postpartum haemorrhage: Analysis of data from the WOMAN trial: BMC Pregnancy Childbirth, 2018; 18(1); 186
8. Doumouchtsis SK, Papageorghiou AT, Arulkumaran S, Systematic review of conservative management of postpartum hemorrhage: What to do when medical treatment fails: Obstet Gynecol Surv, 2007; 62(8); 540-47
9. Said Ali A, Faraag E, Mohammed M, The safety and effectiveness of Bakri balloon in the management of postpartum hemorrhage: A systematic review: J Maternal Fetal Neonatal Med, 2021; 34(2); 300-7
10. Suarez S, Conde-Agudelo A, Borovac-Pinheiro A, Uterine balloon tamponade for the treatment of postpartum hemorrhage: A systematic review and meta-analysis: Am J Obstet Gynecol, 2020; 222(4); 293e1-93.e52
11. Sheen JJ, Wright JD, Goffman D, Maternal age and risk for adverse outcomes: Am J Obstet Gynecol, 2018; 219(4); 390.e1-90.e15
12. Kadour-Peero E, Sagi S, Awad J, Vitner D, The maternal age cut-off for an increase in composite adverse outcomes: J Obstet Gynaecol Can, 2022; 44(4); 372-77
13. Liu CN, Yu FB, Xu YZ, Prevalence and risk factors of severe postpartum hemorrhage: A retrospective cohort study: BMC Pregnancy Childbirth, 2021; 21(1); 332
14. Abdelwahab M, Cackovic M, Placenta accreta spectrum and postpartum hemorrhage: Clin Obstet Gynecol, 2023; 66(2); 399-407
15. Wang Y, Zhou Y, Zeng L, Analysis of risk factors for massive intraoperative bleeding in patients with placenta accreta spectrum: BMC Pregnancy Childbirth, 2022; 22(1); 116
16. Hong L, Chen A, Chen J, The clinical evaluation of IIA balloon occlusion in caesarean delivery for patients with PAS: A retrospective study: BMC Pregnancy Childbirth, 2022; 22(1); 103
17. Guideline of prevention and treatment about postpartum hemorrhage (2023): Zhonghua Fu Chan Ke Za Zhi, 2023; 58(6); 401-9 [in Chinese]
18. Rydahl E, Declercq E, Juhl M, Maimburg RD, Cesarean section on a rise-Does advanced maternal age explain the increase? A population register-based study: PLoS One, 2019; 14(1); e0210655
19. Frick AP, Advanced maternal age and adverse pregnancy outcomes: Best Pract Res Clin Obstet Gynaecol, 2021; 70; 92-100
20. Kim S, Song E, Park YH, Association between cesarean section rate and maternal age in twin pregnancies: J Perinat Med, 2022; 50(4); 438-45
21. Capriglione S, Ettore C, Terranova C, Analysis of ultrasonographic and hystopathologic features of placental invasiveness in Vitro Fertilization (IVF) pregnancies: A prospective study: J Matern Ftal Neonatal Med, 2022; 35(25); 5631-38
22. Li S, Gao J, Liu J, Incidence and risk factors of postpartum hemorrhage in China: A multicenter retrospective study: Front Med (Lausanne), 2021; 8; 673500
23. Jauniaux E, Collins S, Burton GJ, Placenta accreta spectrum: Pathophysiology and evidence-based anatomy for prenatal ultrasound imaging: Am J Obstet Gynecol, 2018; 218(1); 75-87
24. Jauniaux E, Bhide A, Prenatal ultrasound diagnosis and outcome of placenta previa accreta after cesarean delivery: A systematic review and meta-analysis: Am J Obstet Gynecol, 2017; 217(1); 27-36
25. Main EK, McCain CL, Morton CH, Pregnancy-related mortality in California: Causes, characteristics, and improvement opportunities: Obstet Gynecol, 2015; 125(4); 938-47
26. Ruppel H, Liu VX, Gupta NR, Validation of postpartum hemorrhage admission risk factor stratification in a large obstetrics population: Am J Perinatol, 2021; 38(11); 1192-200
27. Brown M, Hong M, Lindquist J, Uterine artery embolization for primary postpartum hemorrhage: Tech Vasc Interv Radiol, 2021; 24(1); 100727
28. Tang P, Xu P, Clinical analysis of 38 cases of postpartum hemorrhage treated with toothless oval forceps through vagina: Journal of Practical Obstetrics and Gynecology, 2013; 29(3); 226-28
29. Wang Y, Xiao C, Zhang N, Sun G, Performance of Bakri balloon tamponade in controlling postpartum hemorrhage: Am J Transl Res, 2023; 15(3); 2268-79
30. Wang D, Xu S, Qiu X, Early usage of Bakri postpartum balloon in the management of postpartum hemorrhage: A large prospective, observational multicenter clinical study in South China: J Perinat Med, 2018; 46(6); 649-56
31. Sathe NA, Likis FE, Young JL, Procedures and uterine-sparing surgeries for managing postpartum hemorrhage: A systematic review: Obstet Gynecol Survy, 2016; 71(2); 99-113
32. Kim MJ, Kim IJ, Kim S, Park IY, Postpartum hemorrhage with uterine artery embolization: The risk of complications of uterine artery embolization: Minim Invasive Ther Allied Technol, 2022; 31(2); 276-83
33. Jeon GU, Jeon GS, Kim YR, Uterine artery embolization for postpartum hemorrhage with placenta accreta spectrum: Acta Radiol, 2023; 64(7); 2321-26
34. Attali E, Many A, Kern G, Predicting the need for blood transfusion requirement in postpartum hemorrhage: J Maternal Fetal Neonatal Med, 2022; 35(25); 7911-16
35. Greenawalt JA, Zernell D, Autologous blood transfusion for postpartum hemorrhage: MCN Am J Matern Child Nurs, 2017; 42(5); 269-75
Figures
Tables
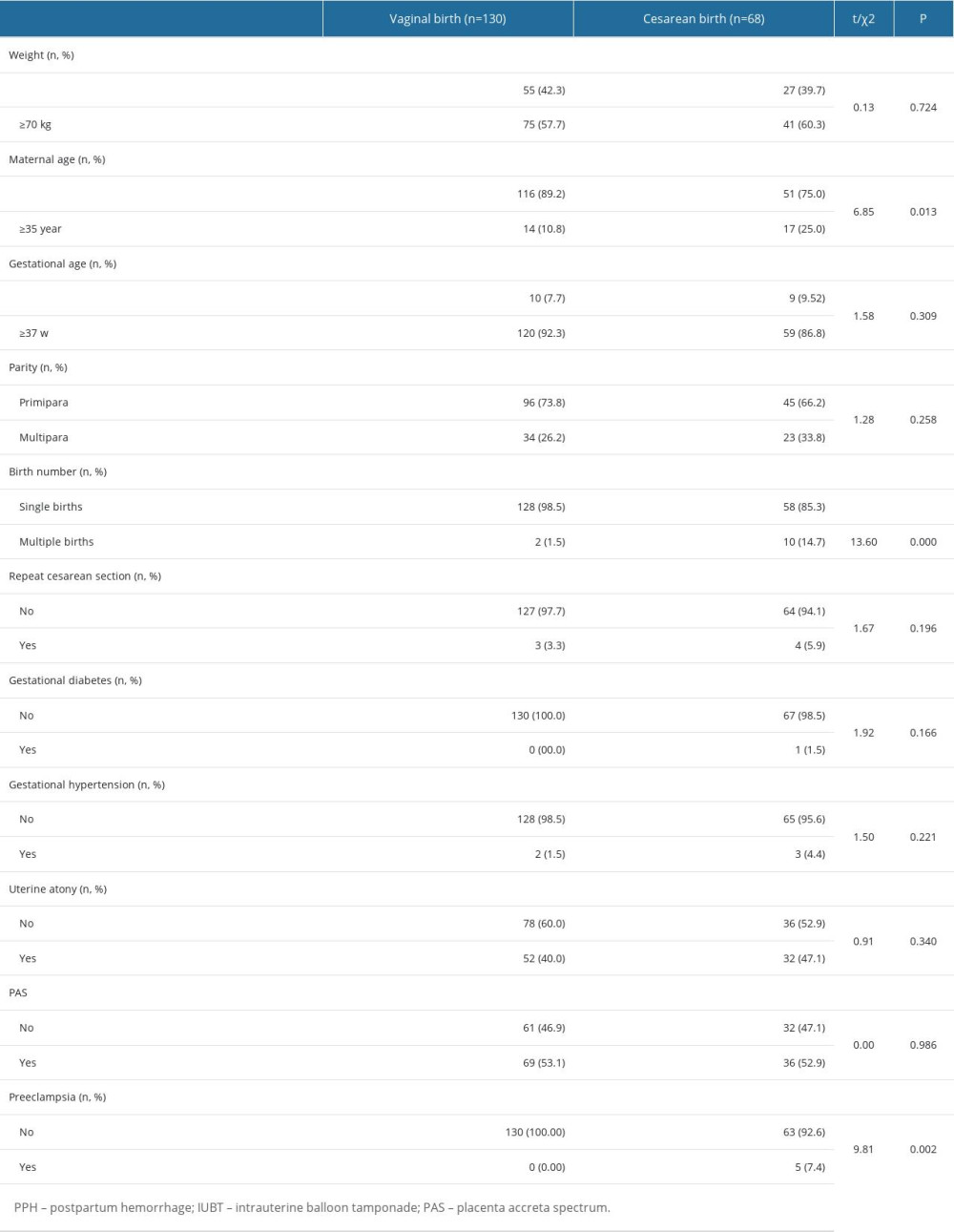 Table 1. Characteristics analysis of women with PPH using Bakri IUBT in 198 vaginal and cesarean births.
Table 1. Characteristics analysis of women with PPH using Bakri IUBT in 198 vaginal and cesarean births.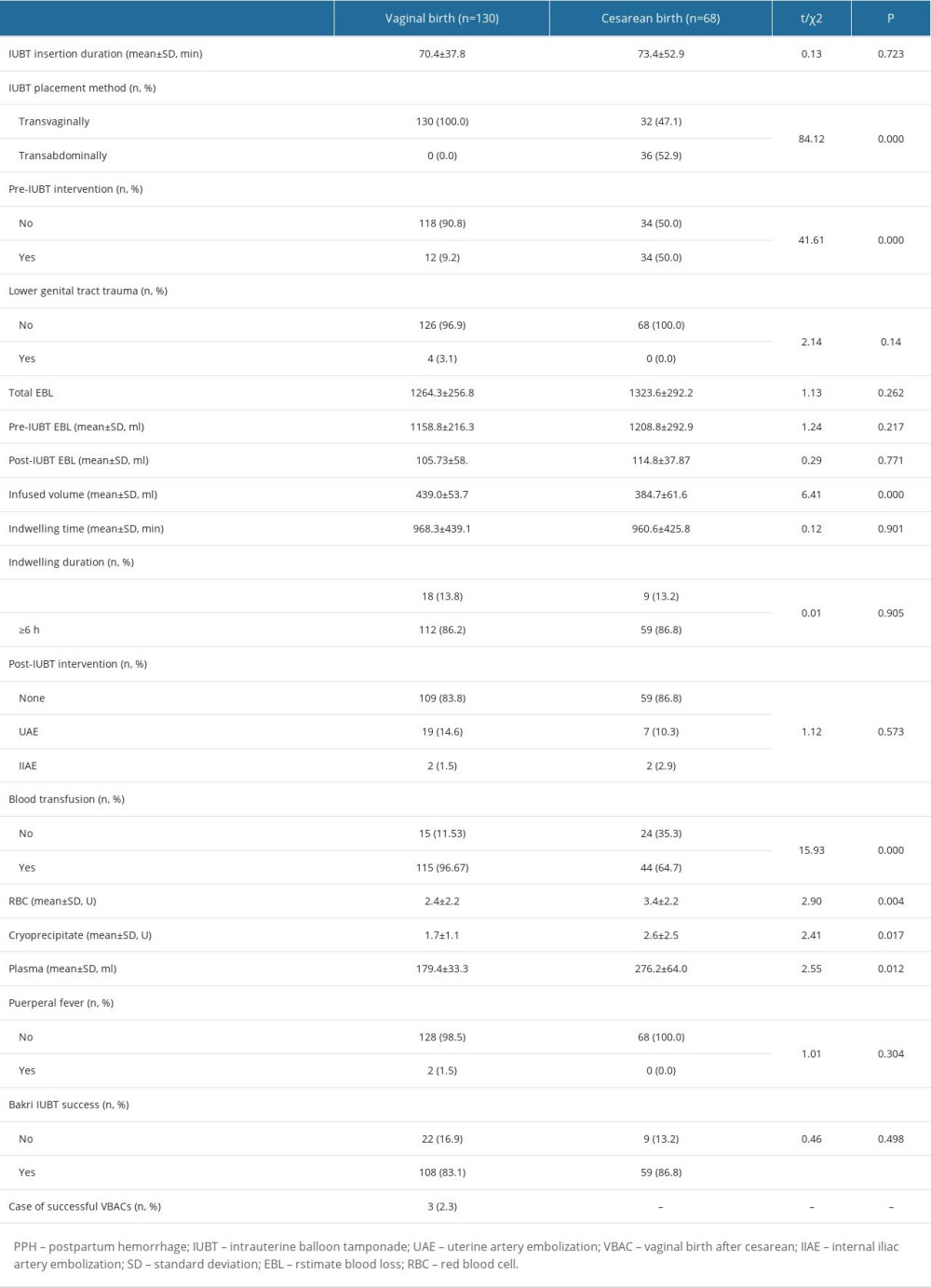 Table 2. Outcomes after the use of Bakri IUBT in controlling PPH in 198 vaginal and cesarean births.
Table 2. Outcomes after the use of Bakri IUBT in controlling PPH in 198 vaginal and cesarean births.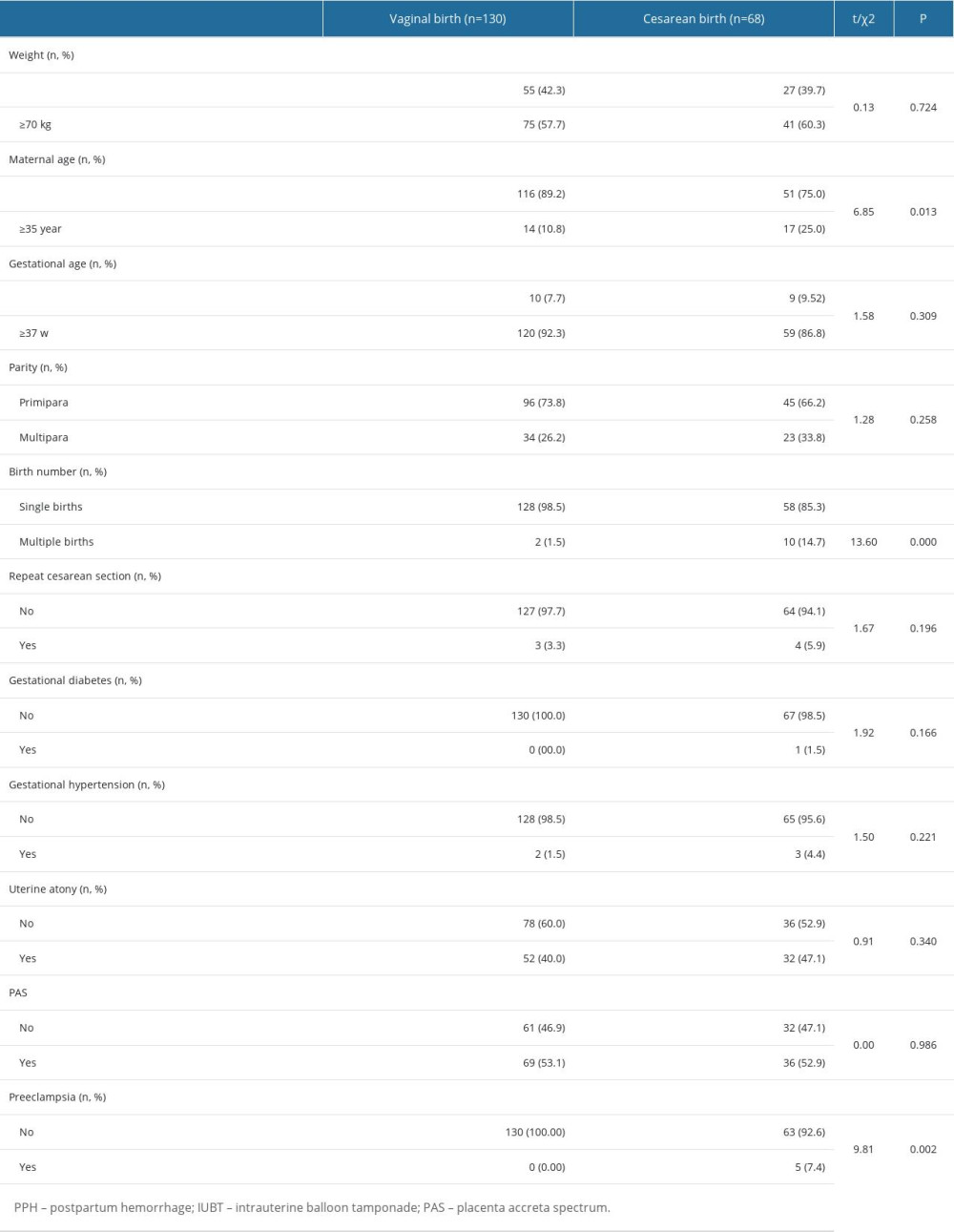 Table 1. Characteristics analysis of women with PPH using Bakri IUBT in 198 vaginal and cesarean births.
Table 1. Characteristics analysis of women with PPH using Bakri IUBT in 198 vaginal and cesarean births.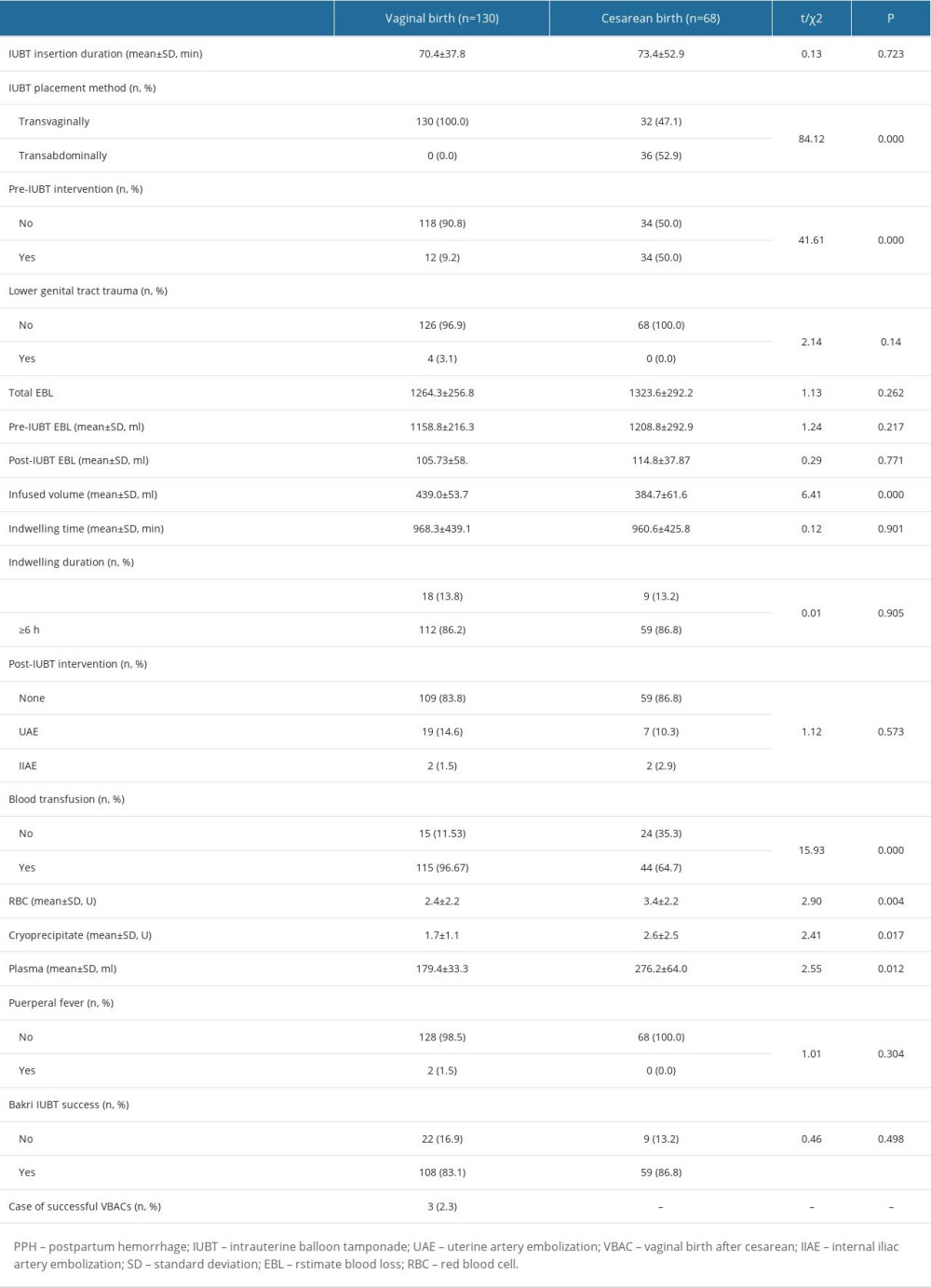 Table 2. Outcomes after the use of Bakri IUBT in controlling PPH in 198 vaginal and cesarean births.
Table 2. Outcomes after the use of Bakri IUBT in controlling PPH in 198 vaginal and cesarean births. In Press
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








