14 February 2024: Review Articles
Clinical Performance of Glass Ionomer Cement in Load-Bearing Restorations: A Systematic Review
Laura DurrantDOI: 10.12659/MSM.943489
Med Sci Monit 2024; 30:e943489
Abstract
ABSTRACT: Glass ionomer cement (GIC) is a self-adhesive dental restorative material composed of a polyacrylic acid liquid and fluoro-aluminosilicate glass powder. It is commonly used for cementation during dental restoration. This study aimed to systematically review the existing literature regarding the clinical performance of GIC in load-bearing dental restorations. A comprehensive literature search was conducted in EBSCO, PubMed, Embrace, and Cochrane databases. Only randomized controlled trials (RCTs) were included in the search, and a broad search technique was used, where inclusion and exclusion criteria were applied. After a thorough evaluation, 12 RCTs were extensively reviewed, and whether GIC is suitable for load-bearing restorations was determined. Significant variations in staining surface or margin, color match, translucency, esthetic anatomical form, retention, material fracture, marginal adaptation, surface luster, occlusal contour, wear, and approximal anatomical form indicated the unsuitability of GIC. By contrast, significance differences in patient view and periodontal response indicated that GIC is suitable. No significant differences in postoperative sensitivity, recurrence of caries, or tooth integrity were observed. Nevertheless, the results of the review demonstrated that the clinical performance of GIC is comparable to that of traditional restorative materials with regard to the parameters analyzed. GIC is a suitable restorative material for load-bearing restorations regarding surface margin, esthetic anatomical form, material retention and fracture, marginal adaptation, occlusal contour, wear, and approximal anatomical form. It reduces other parameters, such as postoperative sensitivity, recurrence of caries, and tooth integrity.
Keywords: Dental Materials, Glass ionomer
Background
STUDY DESIGN:
This systematic review complied with the standards outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2020 [31,32]. According to the hierarchy of evidence and OLE, the randomized controlled trial (RCTs) is the most widely used study format. Therefore, this review only included results from RCTs.
FORMULATING THE RESEARCH QUESTION:
A total of 5585 studies on the use of GIC in load-bearing restorations were obtained. The preliminary examination of the research topic specified whether the research question (is GIC clinically suitable for loading bearing restoration?) is appropriate for the topic of this review. This question was formulated using the PICO framework, which considers the population (patients requiring load-bearing restoration), intervention (GIC restorations), comparison (other dental restorations), and outcome (clinical direction for GIC use in load-bearing restorations) [33,34]. This framework was selected because it is often used for systematic reviews of clinical trials [35].
KEY TERMS:
For each aspect of PICO, we generated key terms to have a structured and consistent search methodology for all databases. The existing literature underwent screening employing keywords, nesting methods, and Boolean operators. The nesting search method uses synonyms to create themed phrases. The keywords include (Glass Ionomer Cement OR GIC), Restoration and Restorations as Class I and II ‘AND’ and ‘OR’ were used with the nesting method to broaden the search [36,37].
INCLUSION CRITERION:
Including studies published from 2018 and 2022 years ensures that the data collected is accurate and up to date. A Crowe Critical Appraisal Tool (CCAT) of >70% was applied. We included studies that examined dentition type (primary or permanent) and used either GIC or resin-modified GIC. Articles written in a language other than English, systematic reviews, cohort studies, case reports, case series, editorials, expert opinions, gray literature, and restoration of endodontically-involved dentition were excluded.
DATABASES SEARCH:
EBSCOhost (https://library.port.ac.uk), PubMed (https://pubmed.ncbi.nlm.nih.gov), and Embrace and Cochrane databases (https://www.cochranelibrary.com/central/doi/10.1002/central/CN-00978608/full) were searched with the corresponding search terms. The search was implemented in accordance with the PRISMA 2020 statement (Figure 1). An overwhelming result was achieved (52 864 studies), and another overwhelming result was found through the initial broad search. After applying the eligibility criteria and removing duplicates, we selected 37 studies for further screening. The studies were independently screened by reading their titles and abstracts. Finally, 13 studies were deemed suitable for critical appraisal, but only 12 studies met the inclusion criteria (Table 1).
CRITICAL APPRAISAL:
The CCAT is a valid and dependable tool for evaluating the integrity of diverse research designs. It has multiple categories that conclude with a score for interpretation. The literature within the final screening was assessed using the CCAT because it is a widely used tool for RCTs [38,39]. The CCAT score for each appraisal was correlated to a percentage using the CCAT instructions. Only studies with a CCAT score of >70% were included [38,39].
CRITICAL ANALYSIS:
Data collected were subjected to subgroup analysis according to the FDI World Dental Federations’ Clinical Criteria for the Evaluation of Direct and Indirect Restorations [40–42]. These criteria can be used in comprehensive procedures for evaluating dental materials and can be divided into 3 groups: esthetic, functional, and biological properties. Each main group contain 16 subgroups, and each subgroup has scores of 1–5 (1, clinically very good; 2, clinically good; 3, clinically sufficient/satisfactory; 4, clinically unsatisfactory; 5, clinically poor). The last 2 were classified as failures.
The included studies used an alternative criterion, such as USPSH, and we made appropriate amendments to coincide subgroups and achieve evidence-based comparison of homogeneous data. Each subgroup’s dichotomous results are presented in tables and narratively for a comprehensive summary. Subgroups based on participant age, type of dentition (primary or secondary), surface, and material that result in dichotomous outcomes were established (Table 2). Furthermore, as recommended by the PRISMA 2020 statement, we used the WHO’s Grading and Recommendations Assessment, Development, and Evaluation Framework to determine the subjective certainty of evidence, which was rated as very low, low, moderate, or high (Table 2) [43,44].
RISK OF BIAS ASSESSMENT:
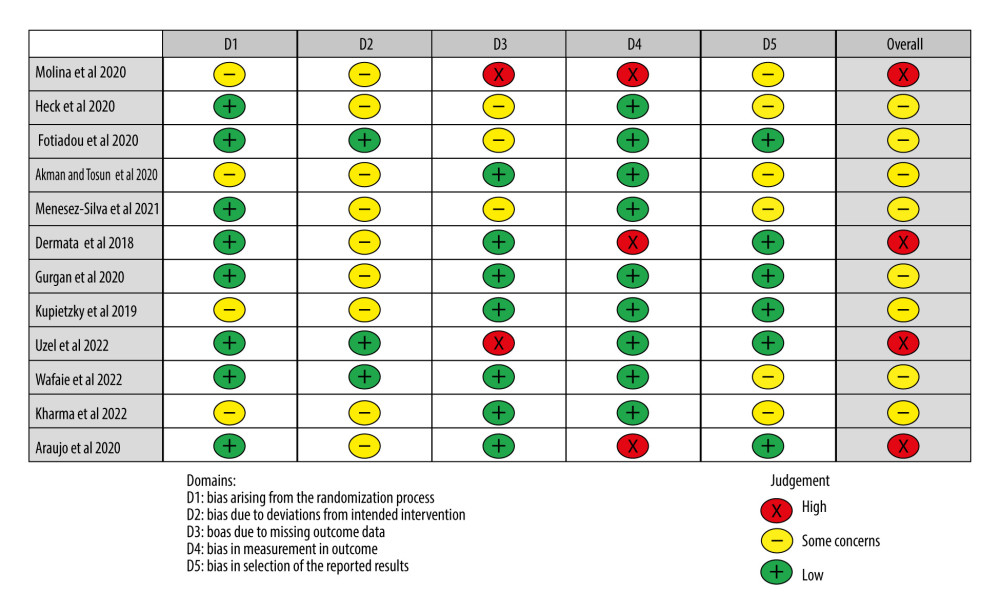
As this systematic review’s contents are RCTs, we indicated the Cochrane risk of bias, which was subjectively rated as “low,” “some concerns,” and “high” and was assessed according to 4 domains (Figure 2): D1, D2, D3, and D4. If a study was marked as high in 1 of the domains, the study was deemed high overall.
Table 2 shows the 12 studies included in this review, showing the characteristics of each study, such as comparison, commercial name, participant age group, number of participants, number of restorations, dentition, class, study length, preferred material, COE, and authors. All the studies have a comparison: GIC versus RC, GIC versus stainless-steel crown, and GIC versus GIC. The outcomes were described as dichotomous outcomes because 2 groups were compared. The investigated GIC materials included in the 12 studies are shown in Table 3, with information on their composition and indications. Some studies were not included in each table because they did not explore all the 16 FDI criteria. Only the studies that produced results for the criterion were included in the table. The top row is the recall period that the results correlate to. It can be used to interpret the results in the tables. For example, a score of 2 for surface luster indicates that the material is slightly dull and contains isolated pores. Fotiadou et al found that 87.5% of EQUIA restorations had an FDI score of 2 for surface luster at 12-month recall. When the difference in results between the baseline and recall periods was insignificant, the column was filled with NA. A P>0.05 indicated that a study explored this criterion [45]. Table 4 shows the parameters evaluated during different recall periods in relation to the type of material used and authors.
STAINING SURFACE OR MARGIN:
Six studies investigated the staining surface [46–51], but only 2 of them found statically significant results regarding staining surface and margin when GIC was compared with RC (P<0.05) [47,48]. The effect was observed only in minor surface staining, which was easily removed and did not exert a detrimental effect. None of the studies found a clinically significant difference in recalls for the materials investigated, and no significant differences in dichotomous outcomes were observed (P>0.05) [49].
COLOR MATCH AND TRANSLUCENCY:
Three of the included studies found statically significant results regarding color match. The results ranged from good color match to distinct deviation, and the latter only affected GIC. One study observed that Filtek Z250 outperformed other GIC materials in terms of color match (P<0.001). EQUIA Forte restoration’s color match was superior to that of Ketac Universal or Riva HV restorations at 5-year recall [47]. Similarly, Gurgan et al [49] observed that Gradia DP outperformed EQUIA Fil. Menezes Silva et al [50] compared Z350-3M with EQUIA Fil (P<0.05). Three studies found no clinical significance in recalls for the materials investigated and no significant differences among dichotomous outcomes (P>0.05) [46,48,51].
ESTHETIC ANATOMICAL FORM:
Two of the included studies found statistical significance regarding the esthetic anatomical form of GIC [47,49], and most of the materials were esthetically acceptable. Menezes et al [50] found a statistically significant difference in esthetic anatomical form between EQUIA Fil and Z350-3M. After 5 years, Ketac Universal and Riva HV restorations displayed a substantial change in esthetic anatomic form relative to the baseline [47]. Two studies found no clinical significance in recalls for the materials investigated and no significant differences in dichotomous outcomes [48,49].
RETENTION AND FRACTURE OF MATERIAL:
The results regarding retention or fracture and retention showed that GIC is frequently minimally retentive with regard to dichotomous outcomes (Table 4) [46–50,52–55]. The 2 studies of dichotomous outcomes showed that EQUIA Fil was superior to Fuji IX GP Fast Set at each recall period [45,56]. Similarly, EQUIA Fil exhibited higher retention performance that Riva Self Cure HV and Ketac Universal Aplicap at 1, 3, and 5 years of recall [47]. Only 1 study yielded significant results regarding fracture alone for EQUIA Fil and Fuji IX Fast Set [45]. Another study found fracture to be the leading cause of failure for EQUIA Fil and Fuji IX Fast Set [56]. However, 5 studies found no clinical significance in recalls for the materials investigated and in dichotomous outcomes [47,49,51,52,54]. Focusing on the average retention of GIC, a study found that at a 3-month recall, the retention of GIC restorations was 97.06% [48]. At a 6-month recall, the retention of GIC averaged 95.6% [46,48,50]. At 12-month recall, the retention of GIC averaged 93.35% [45–50,53]. At 2-year recall, the retention of GIC averaged 91.1% [45–46,50,53,54]. At 3-year recall, the retention of GIC averaged 83.35% [44,47,49,52,54]. One study reported the retention of GIC at a 4-year recall [49].
MARGINAL ADAPTATION:
Four of the included studies found statistically significant marginal adaptation results. The results ranged from harmonious outlines to partial or complete looseness of the restoration and significant gaps and irregularities, and only the last result affected GIC. One study observed irregularities in the EQUIA Fil group. However, the RC groups remained similar at 6 and 12 months of recall (P=0.029 and P=0.034, respectively) [48]. Wafaie et al [47] found that Filtek Z250 underwent no significant change from the baseline to the recall periods, but all GIC groups did (P<0.05). One study found that EQUIA showed statistically significant changes from baseline to 3 years of recall (P=0.039), whereas the changes in Fuji IX GP Fast Set was less notable [45]. However, another study found significant changes from baseline to 6 years of recall for EQUIA Fil and Fuji IX GP Fast Set (P 0.017 and P 0.011, respectively) [56]. Two studies found no clinical significance in recalls for materials investigated and for dichotomous outcomes [49,51].
APPROXIMAL ANATOMICAL FORM, POSTOPERATIVE SENSITIVITY, AND TOOTH VITALITY:
The results ranged from clinically excellent to clinically poor. There was a significantly greater incidence of loss of contact point integrity in Vitremer compared with Filtek Z250 (P=0.03) [53]. Five studies found no clinical significance in recalls for the materials investigated, and no significant differences in dichotomous outcome were observed [45,47,50,54]. In relation to postoperative sensitivity and tooth vitality, no clinical significance was observed at recalls for each material, and no significant differences was found for dichotomous outcomes [45,49,51,56].
SURFACE LUSTER/TEXTURE:
Six of the included studies found deterioration of surface luster as an outcome of GIC at 6-year recall [45–47,50–51,56]. The deterioration varied from slight deviation from enamel to dull surfaces with pores. The most common outcome was a slightly dull appearance. Compared with RC, the results were statistically significant (P<0.05). One study found no significant differences for dichotomous outcomes in recalls for materials investigated with regard to surface luster [49].
RECURRENCE OF CARIES EROSION ABFRACTION AND TOOTH INTEGRITY:
No clinically significant differences were observed at recalls for each of the materials with regard to dichotomous outcomes (P>0.05) in relation to the recurrence of caries and erosion abfraction [45–49,51–54,56] or tooth integrity [45,47,56].
PERIODONTAL RESPONSE/GINGIVAL HEALTH:
Two of the included studies found statically significant results regarding patient satisfaction. The results varied from clinically excellent to clinically poor. One study found a significant decline in patient satisfaction with EQUIA Forte and Riva HV restorations from baseline to 5-year recall [47]. However, the dichotomous comparison of stainless-steel Hall Crown versus EQUIA Forte indicated a preference for EQUIA Forte [52]. Two included studies found no clinical significance observed at recalls for each of the materials investigated, and no significant differences were found for dichotomous outcomes [41,44]. One study found statistically significant results regarding periodontal response [47]. At 12-month recall, Filtek Z250 was associated with significantly more bleeding on probing BOP compared with Vitremer (P=0.005), and no clinical significance observed at recalls for each material investigated, and no significant differences were found for dichotomous outcomes [53].
Discussion
This study collated the results of 12 RCTs, focusing on the clinical suitability of GIC for load-bearing restorations according to the FDI criteria. After analyzing the results, we found significant differences in surface luster, staining surface/margin, color match and translucency, esthetic anatomical form, retention and fracture of material, marginal adaptation, occlusal contour, and approximal anatomical form. No statistically significant differences were found in postoperative sensitivity and recurrence of caries. The present results generally demonstrate that the clinical performance of the GIC materials were similar for most of the above-mentioned parameters. This finding may influence clinicians’ decision-making when considering restoration placement in class II restorations, suggesting that GIC is clinically suitable in appropriate systems. GIC exhibited acceptable performance for posterior teeth after 24 and 36 months [57].
Surface luster, which indicates the ability of a surface to reflect light, is fundamental to the esthetic appearance of restorations and is inversely proportional to surface roughness. The clinical success of a restoration is greatly influenced by the surface texture of a dental material [58]. All surfaces within the oral cavity are covered by the acquired pellicle and undergo biofilm adhesion. Bacteria are associated with dental diseases, such as periodontal disease and dental caries. Accordingly, surface roughness affects a surface’s ability to modulate and limit bacterial attachment and propagate microorganisms [59]. GIC is inferior to RC, but the surface luster of GIC is comparable to that of the enamel. GIC exhibits slight deviation to dull surfaces but can be enhanced by covering it with a film of saliva or multiple pores on more than one-third of its surface. Therefore, no GIC failed for this purpose according to the FDI criteria (4 and 5). Many of the studies used surface coatings and recorded improved surface luster [47,60–62], indicating that resin coatings are effective in transforming restoration surface texture without excessive polishing. However, extended recall periods revealed that the coatings degrade after enduring mastication and show a dull appearance [63]. Therefore, surface texture deterioration may be attributed to the positive correlation between surface roughness and wear [64].
Few GIC groups showed significant differences from RC in surface staining from baseline to recall periods. The lack of profound staining may be due to GIC’s self-adhesion properties to enamel and dentin, eliminating the need for bonding agents [65]. Surface staining may be influenced by the combination of extrinsic stimulus and surface roughness, which correlates with wear [66]. Additionally, fractures, defects, gaps at the margins, and marginal staining in the crevice between the restoration and the cavity wall can be related to pigment absorption [47]. Marginal staining was observed in few cases during 6-year recall period [60]. Despite the minor statistical significance of the results, no GIC was significantly affected by staining or margin criteria because stains can be easily removed by polishing [40].
In relation to color matching of GIC restorations at different recalls, GIC groups performed worse than the RC groups in 3 studies. This result may be related to GIC’s optical properties, which were outperformed by RC because of GIC’s lack of translucency [67,68]. This conclusion contrasts with the findings of other investigations, which found that neither GIC nor RC restorations have a significant color mismatch with the surrounding tooth structure. In 1 study, EQUIA Forte had a better color match with adjacent tooth structures than the other GIC groups because of the small highly reactive glass particles within EQUIA Forte and the coating [47,69]. Two studies revealed an improvement in color matching for the GIC group at 5- and 10-year recall, which may be connected to GIC’s maturation over time [47,49]. This result is congruent with the findings of a 3-year clinical study conducted by Diem et al [70], who found that the color match of GIC restorations improved during the study period.
Esthetic anatomic form is the acceptability of the esthetics of a restoration [40]. Significant results for GIC’s esthetic anatomical form were found in studies that compared GIC with RC, ranging from an ideal form to a form that deviates from the norm but is still acceptable. This deviation can be related to the high wear rate or material fracture for GIC [71]. By contrast, 2 studies found no appreciable deviation in the form of the anatomical esthetic [47,49], which is supported by a systematic review by Dias et al [28], who found no deficiency for this parameter.
In relation to fracture and retention of GIC materials, only 1 study found significant differences I fracture rates, and another found fracture as the leading cause of failure, despite yielding no significant results. The remaining studies investigating material fracture found no significant difference from baseline to recall periods and in comparisons with RC. These findings contradict the existing literature, which suggests that CGIC is highly prone to fracture, especially compared with RC [72]. The studies included in this review used reinforced restorative systems indicated for load-bearing restorations (Table 3). This may increase the fracture toughness and durability of the restorations we explored. These restorative systems frequently included a paired surface coating, such as EQUIA Fil and EQUIA COAT, improving mechanical properties, such as fracture resistance. Increased fracture resistance and high strength were observed after the application of coating agents, which prevented contamination caused by intra-oral fluids before hardening. This type of contamination can lead to loss of matrix-forming ions, weakens a material, and degrades reinforcing properties within a coating’s matrix [73–75]. A review of material longevity shows that GIC typically has a success rate of 93–98% within the primary dentition for the tooth’s lifespan and 5 years within the adult dentition [76]. Therefore, the result from this study exceeds this expectation because many restorations have been retained for up to 10 years. The existing literature regarding the lifespan of GIC within load-bearing restorations was created 13 years ago. Therefore, developments in the composition of different brands of GIC may account for the improvement in retention.
Concerning marginal adaptation, an acid- or base-resistant layer is created by the chemical adhesion of GIC to the tooth structure, creating a long-lasting marginal seal [77]. Furthermore, the dimensional stability of GIC is due to its hydrophilicity, which promotes the absorption of any fluid produced from the cavity prep, and adhesion to enamel ensures that the seal is fixed [13]. Additionally, GIC has the same coefficient of thermal expansion as the tooth structure, and the microgap between a restoration and a tooth is small [78]. Coatings reduce the formation of marginal gaps and were applied in the included studies [79]. Reducing the risk of marginal gaps is necessary, as the dentin pulp complex is exposed to the oral environment by restorations with poor marginal adaptation, and restorations are vulnerable to microleakage and plaque retention [80]. These results varied, and 2 studies showed failures for this subgroup; both compared Fuji IX and EQUIA, but reported contradictory results. Thus, both materials may be at risk of marginal gaps after 3-year recall [70].
Clinical evaluation of wear is performed to determine how materials behave when subjected to challenging masticatory changes in the mouth. All the restorations were clinically acceptable in terms of wear resistance according to the findings of this study. This might be explained by the modern GIC’s increased flexural strength and wear resistance. Additionally, the coating agent permeates the pores and stops cracks in restorations from spreading [81]. Only 1 study stated that the participant’s occlusion was normal, preventing excessive wear rates caused by clenching or bruxism habits [70]. Progressive occlusal wear was reported in all studies despite the absence of failure. The impact of coarse particles in dietary components and the strong occlusal forces in the posterior region may reflect pitting and wear [82].
The tightness and durability of the proximal contact points of restorations are crucial because poor contact results in food impaction and discomfort during mastication [83]. Small changes in approximal anatomical form occurred in Vitremer and Filtek after a 2-year recall [53]. Cyclic loads generated occlusal-proximal marginal fractures and damaged the proximal point [84]. Given that only 1 study produced significant results, GIC may fit the requirements for approximal anatomical shape. However, a recent RCT identified approximal anatomical shape as one of the primary causes of a class II GIC restoration failure [85].
In relation to periodontal response, a single study found a significant difference in gingival health between Vitremer and Z250. At 12- and 24-month recalls, Santos et al [86] found that RMGIC positively affected subgingival biofilm composition more than RC. According to Atieh, open-sandwich restorations exposing Vitremer in their proximal aspect resulted in considerable improvement in gingival health when compared to SSC [87].
Despite the success of outcomes regarding GIC within this review, most of the included studies covered less than 5 years of recall. Therefore, large studies with long follow-up times are required. Attention should be placed on approximal restorations. In addition, the guidelines in the WHO’s Prevention and Treatment of Dental Caries with Mercury-Free Products and Minimal Interventions have recommended GIC for single-surface occlusal restorations [88]. The heterogeneity of the studies can be considered another limitation of this review, and the GIC and RMGIC have distinct compositions and microstructures.
This review did not focus on surface coatings within GIC systems. However, the GIC and surface coating are promising materials at appropriate indications and cavity geometries when mechanical factors are considered. Further research may be required, especially long-term clinical studies that evaluate the efficacy of surface coatings in enhancing the mechanical properties of GIC in load-bearing restorations.
Conclusions
Our study found that GIC is suitable for load-bearing restorations. Notably, RC is superior to most subgroups with regard to dichotomous outcomes. However, the differences were considerable. Notable differences in surface luster, color match, translucency, and marginal adaptation were observed.
Tables
Table 1. Included studies with their title, year, author (s), outcomes, and Crowe Critical Appraisal Tool score.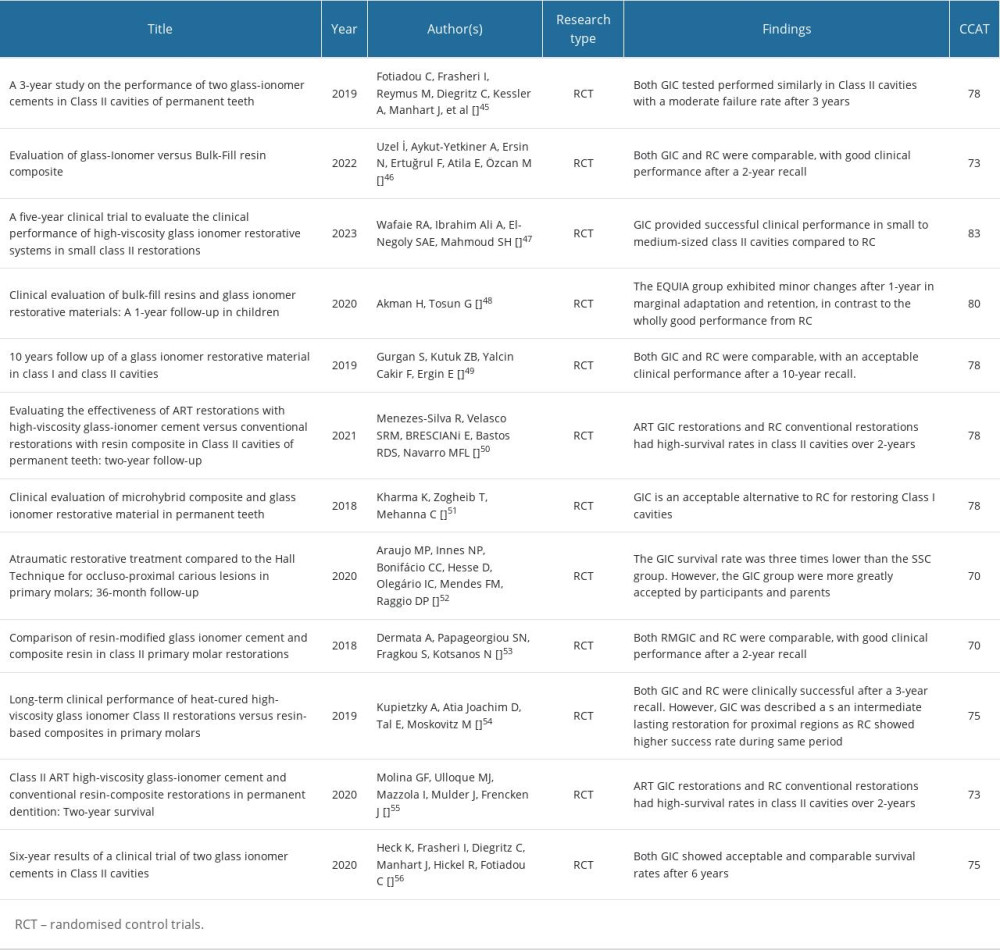 Table 2. Characteristics of the 12 included studies.
Table 2. Characteristics of the 12 included studies.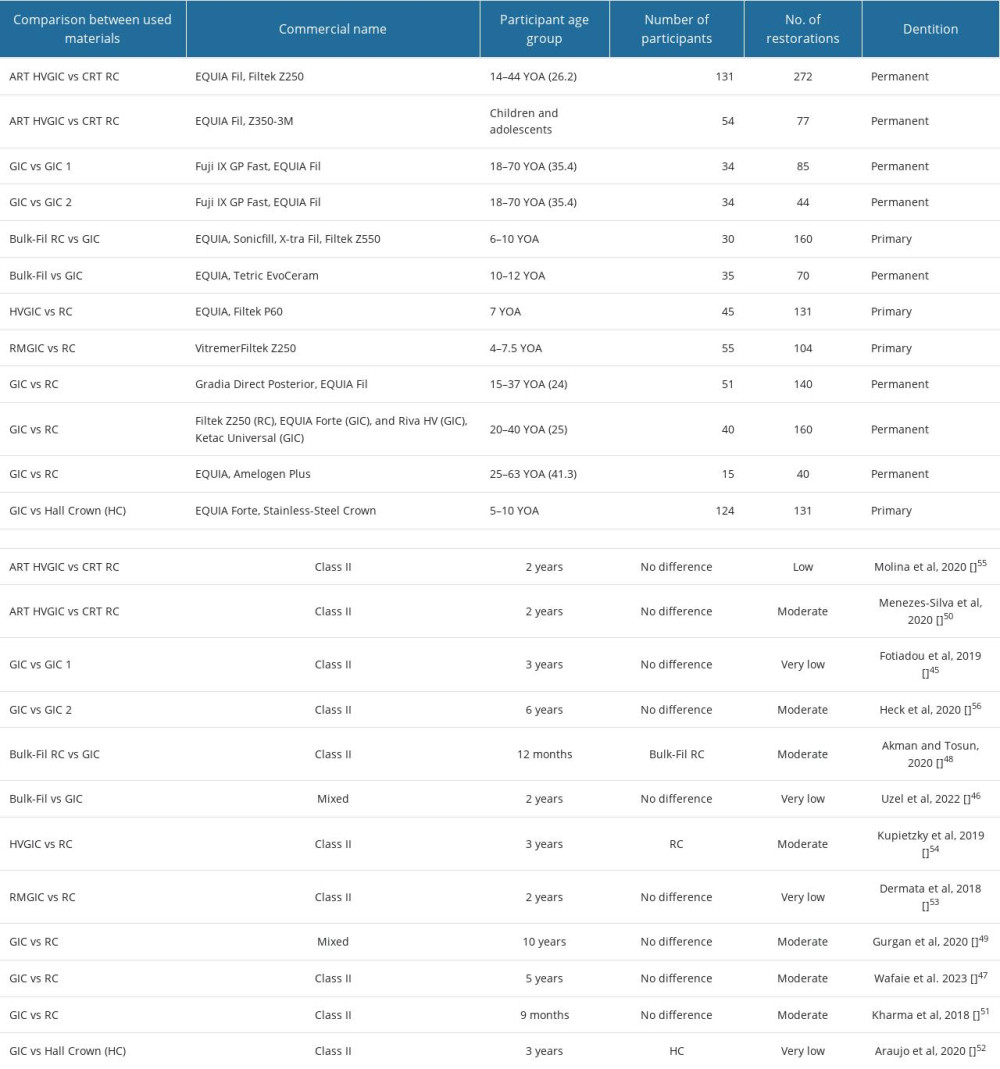 Table 3. Included materials and their types, indications, composition, and authors.
Table 3. Included materials and their types, indications, composition, and authors.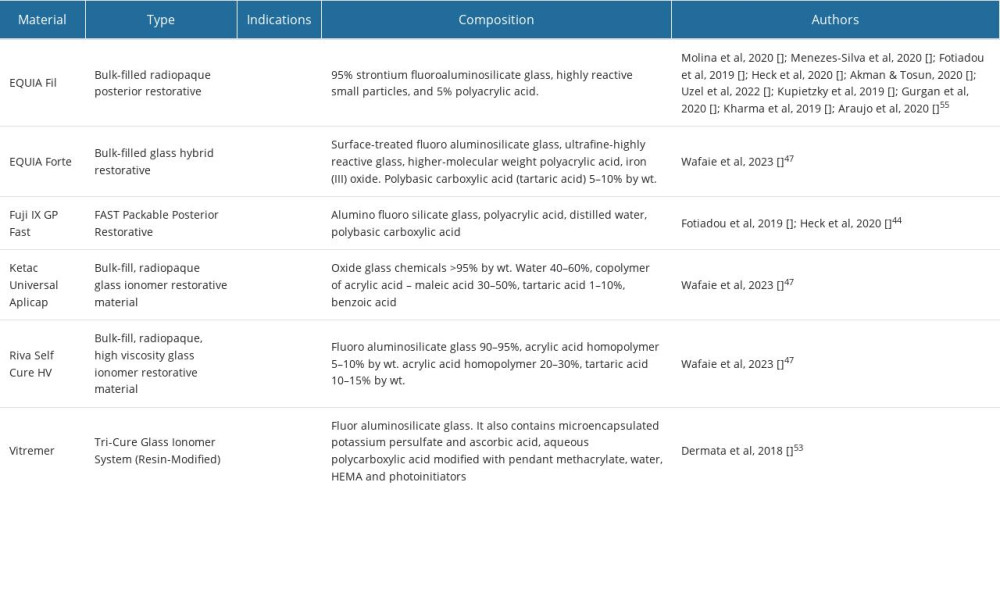 Table 4. Characteristics of the studies during different recall periods and their relation to esthetics, functions, and biological behavior (n=12).
Table 4. Characteristics of the studies during different recall periods and their relation to esthetics, functions, and biological behavior (n=12).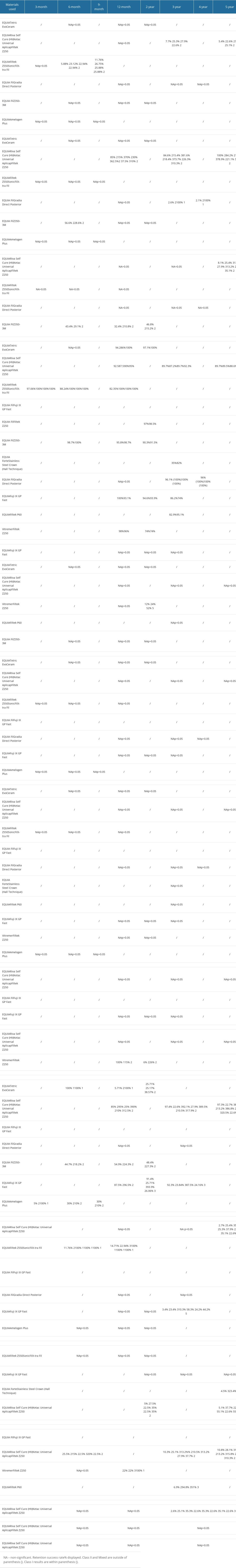
References
1. Francisconi LF, Scaffa PM, de Barros VR, Glass ionomer cements and their role in the restoration of non-carious cervical lesions: J Appl Oral Sci, 2009; 17(5); 364-69
2. Hill R, Glass ionomer polyalkenoate cements and related materials: Past, present and future: Brit Dent J, 2022; 232(9); 653-57
3. British Dental Association: John-McLean. Bda.org, 2019 https://bda.org/McLeanArchive/john-mclean
4. McLean JW, Glass-ionomer cements: Br Dent J, 1988; 164(9); 293-300
5. Khurshid Z, Zafar M, Qasim S, Advances in nanotechnology for restorative dentistry: Materials (Basel), 2015; 8(2); 717-31
6. Aliyu MB, Efficiency of Boolean Search strings for Information Retrieval: AJER, 2017; 6(11); 216-22
7. Ortiz M, Olvera D, Reyes J, Evolution of glass ionomer cements biocompatibility vs cytotoxicity: Acta Microscopica, 2019; 28(1); 19-31
8. Wilson PM, Petticrew M, Calnan MW, Nazareth I, Disseminating research findings: What should researchers do? A systematic scoping review of conceptual frameworks: Implement Sci, 2010; 5; 91
9. Abbasi R, Nodehi A, Atai M, Synthesis of poly (acrylic-co-itaconic acid) through precipitation photopolymerization for glass-ionomer cements: Characterization and properties of the cements: Dent Mater, 2020; 36(6); e169-e83
10. Mylonas P, Zhang J, Banerjee A, Conventional glass-ionomer cements: A guide for practitioners: Dental Update, 2021; 48(8); 643-50
11. Nicholson JW, Brookman PJ, Lacy OM, Wilson AD, Fourier transform infrared spectroscopic study of the role of tartaric acid in glass-ionomer dental cements: J Dent Res, 1988; 67(12); 1451-54
12. Nicholson JW, Maturation processes in glass-ionomer dental cements: Acta Biomater Odontol Scand, 2018; 4(1); 63-71
13. Sidhu SK, Nicholson JW, A Review of glass-ionomer cements for clinical dentistry: J Funct Biomater, 2016; 7(3); 16
14. Sauro S: Bioactive and therapeutic dental materials, 2019, MDPI https://doi.org/10.3390/books978-3-03921-420-4
15. Ngo HC, Mount G, Mc Intyre J, Chemical exchange between glass-ionomer restorations and residual carious dentine in permanent molars: An in vivo study: J Dent, 2006; 34(8); 608-13
16. Ireland R: A Dictionary of dentistry, 2010, Oxford University Press https://doi.org/10.1093/acref/9780199533015.001.0001
17. Singh P, Sehgal P, G.V Black dental caries classification and preparation technique using optimal CNN-LSTM classifier: Multimed Tools Appl, 2020; 80(4); 5255-72
18. Martin J, Fernandez E, Estay J, Management of Class I and Class II amalgam restorations with localized defects: Five-year results: Int J Dent, 2013; 2013; 450260
19. Kateeb ET, Warren JJ, The transition from amalgam to other restorative materials in the U.S. predoctoral pediatric dentistry clinics: Clin Exp Dent Res, 2019; 5(4); 413-19
20. Department of Health and Social Care: National plan to phase down use of Dental Amalgam in England Contents, 2019 https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/811635/phasing-down-use-of-dental-amalgam-in-england.pdf
21. Chan KH, Mai Y, Kim H, Review. Resin composite filling: Materials, 2010; 3(2); 1228-43
22. Menezes-Silva R, Cabral RN, Pascotto RC, Mechanical and optical properties of conventional restorative glass-ionomer cements – a systematic review: J Appl Oral Sci, 2019; 27; e2018357
23. Sikka N, Brizuela M, Glass ionomer cement [Updated 2023 Nov 13]: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing
24. Hamdy TM, Evaluation of compressive strength, surface microhardness, solubility and antimicrobial effect of glass ionomer dental cement reinforced with silver doped carbon nanotube fillers: BMC Oral Health, 2023; 23; 777
25. Wan Jusoh WN, Matori KA, Mohd Zaid MH, Incorporation of hydroxyapatite into glass ionomer cement (GIC) formulated based on alumino-silicate-fluoride glass ceramics from waste materials: Materials (Basel), 2021; 14(4); 954
26. Ghilotti J, Mayorga P, Sanz JL, Remineralizing ability of resin modified glass ionomers (RMGICs): A systematic review. J. Funct: Biomater, 2023; 14(8); 421
27. : OCEBM Levels of evidence – Centre for Evidence-Based Medicine (CEBM), 2011, University of Oxford . Www.cebm.ox.ac.uk
28. Dias AGA, Magno MB, Delbem ACB, Clinical performance of glass ionomer cement and composite resin in Class II restorations in primary teeth: A systematic review and meta-analysis: J Dent, 2018; 73; 1-13
29. Pilcher L, Pahlke S, Urquhart O, Direct materials for restoring caries lesions: Systematic review and meta-analysis – a report of the American Dental Association Council on Scientific Affairs: J Am Dent Assoc, 2023; 154(2); e1-e98
30. Murad MH, Asi N, Alsawas M, Alahdab F, New evidence pyramid: Evid Based Med, 2016; 21(4); 125-27
31. Page MJ, McKenzie JE, Bossuyt PM, The PRISMA 2020 statement: An updated guideline for reporting systematic reviews: BMJ, 2021; 372; n71
32. Sarkis-Onofre R, Catalá-López F, Aromataris E, Lockwood C, How to properly use the PRISMA Statement: Syst Rev, 2021; 10(1); 117
33. Fandino W, Formulating a good research question: Pearls and pitfalls: Indian J Anaesth, 2019; 63(8); 611-16
34. Aslam S, Emmanuel P, Formulating a researchable question: A critical step for facilitating good clinical research: Indian J Sexu Transm Diseases AIDS, 2010; 31(1); 47-5
35. Tawfik GM, Dila KAS, Mohamed MYF, A step-by-step guide for conducting a systematic review and meta-analysis with simulation data: Trop Med Health, 2019; 47; 46
36. Aliyo M, Efficiency of Boolean Search strings for information retrieval: ResearchGate, 2019 https://www.researchgate.net/publication/321314341_Efficiency_of_Boolean_Search_strings_for_Information_Retrieval
37. Hornberger B, Rangu S: Designing inclusion and exclusion criteria, 2020 https://repository.upenn.edu/cgi/viewcontent.cgi?article=1000&context=crp
38. Morrison K: Dissecting the literature: the Importance of Critical Appraisal, 2017, Royal College of Surgeons https://www.rcseng.ac.uk/library-and-publications/library/blog/dissecting-the-literature-the-importance-of-critical-appraisal/
39. Crowe M, Sheppard L, Campbell A, Comparison of the effects of using the Crowe Critical Appraisal Tool versus informal appraisal in assessing health research: A randomised trial: International J Evidence-Based Healthcare, 2011; 9(4); 444-49
40. Hickel R, Mesinger S, Opdam N, Revised FDI criteria for evaluating direct and indirect dental restorations-recommendations for its clinical use, interpretation, and reporting: Clin Oral Investig, 2023; 27(6); 2573-92
41. Marquillier T, Doméjean S, Le Clerc J, The use of FDI criteria in clinical trials on direct dental restorations: A scoping review: J Dent, 2018; 68; 1-9
42. Cavalheiro CP, de Souza PS, de Oliveria Rocha R, Choosing the Criteria for Clinical Evaluation of Composite Restorations: An Analysis of Impact on Reliability and Treatment Decision: Pesquisa Brasileira Em Odontopediatria E Clínica Integrada, 2020; 20; e5088
43. British Medical Journal, What is GRADE? – BMJ Best Practice: Bmj.com, 2011 https://bestpractice.bmj.com/info/toolkit/learn-ebm/what-is-grade/
44. Pannucci CJ, Wilkins EG, Identifying and avoiding bias in research: Plast Reconstr Surg, 2010; 126(2); 619-25
45. Fotiadou C, Frasheri I, Reymus M, A 3-year controlled randomized clinical study on the performance of two glass-ionomer cements in Class II cavities of permanent teeth: Quintessence International, 2019; 50(8); 592-602
46. Uzel İ, Aykut-Yetkiner A, Ersin N, Evaluation of glass-ionomer versus bulk-fill resin composite: A two-year randomized clinical study: Materials, 2022; 15(20); 7271
47. Wafaie RA, Ibrahim Ali A, El-Negoly SAE, Mahmoud SH, Five-year randomized clinical trial to evaluate the clinical performance of high-viscosity glass ionomer restorative systems in small class II restorations: J Esthet Restor Dent, 2023; 35(3); 538-55
48. Akman H, Tosun G, Clinical evaluation of bulk-fill resins and glass ionomer restorative materials: A 1-year follow-up randomized clinical trial in children: Niger J Clin Pract, 2020; 23(4); 489-97
49. Gurgan S, Kutuk ZB, Yalcin Cakir F, Ergin E, A randomized controlled 10 years follow up of a glass ionomer restorative material in class I and class II cavities: J Dent, 2020; 94; 103175
50. Menezes-Silva R, Velasco SRM, Bresciani E, A prospective and randomized clinical trial evaluating the effectiveness of ART restorations with high-viscosity glass-ionomer cement versus conventional restorations with resin composite in Class II cavities of permanent teeth: Two-year follow-up: J Appl Oral Sci, 2021; 29; e20200609
51. Kharma K, Zogheib T, Mehanna C, Clinical evaluation of microhybrid composite and glass ionomer restorative material in permanent teeth: J Contemporary Dental Practice, 2018; 19(2); 226-32
52. Araujo MP, Innes NP, Bonifácio CC, Atraumatic restorative treatment compared to the Hall Technique for occluso-proximal carious lesions in primary molars; 36-month follow-up of a randomised control trial in a school setting: BMC Oral Health, 2020; 20(1); 318
53. Dermata A, Papageorgiou SN, Fragkou S, Kotsanos N, Comparison of resin modified glass ionomer cement and composite resin in class II primary molar restorations: A 2-year parallel randomised clinical trial: Eur Arch Paediatr Dent, 2018; 19(6); 393-401
54. Kupietzky A, Atia Joachim D, Tal E, Moskovitz M, Long-term clinical performance of heat-cured high-viscosity glass ionomer class II restorations versus resin-based composites in primary molars: A randomized comparison trial: Eur Arch Paediatr Dent, 2019; 20(5); 451-56
55. Molina GF, Ulloque MJ, Mazzola I, Randomized controlled trial of Class II ART high-viscosity glass-ionomer cement and conventional resin-composite restorations in permanent dentition: Two-year survival: J Adhes Dent, 2020; 22(6); 555-65
56. Heck K, Frasheri I, Diegritz C, Manhart J, Six-year results of a randomized controlled clinical trial of two glass ionomer cements in class II cavities: J Dent, 2020; 97; 103333
57. Cribari L, Madeira L, Roeder RBR, High-viscosity glass-ionomer cement or composite resin for restorations in posterior permanent teeth? A systematic review and meta-analyses: J Dent, 2023; 137; 104629
58. Heintze SD, Forjanic M, Surface roughness of different dental materials before and after simulated toothbrushing in vitro: Oper Dent, 2005; 30(5); 617-26
59. Sterzenbach T, Helbig R, Hannig C, Hannig M, Bioadhesion in the oral cavity and approaches for biofilm management by surface modifications: Clin Oral Investig, 2020; 24(12); 4237-60
60. Türkün L, Kanik Ö, A Prospective six-year clinical study evaluating reinforced glass ionomer cements with resin coating on posterior teeth: Quo vadis?: Oper Dent, 2016; 41(6); 587-98
61. Ratnayake J, Veerasamy A, Ahmed H, Clinical and microbiological evaluation of a chlorhexidine-modified glass ionomer cement (GIC-CHX) restoration placed using the atraumatic restorative treatment (ART) Technique: Materials (Basel), 2022; 15(14); 5044
62. Klinke T, Daboul A, Turek A, Clinical performance during 48 months of two current glass ionomer restorative systems with coatings: A randomized clinical trial in the field: Trials, 2016; 17; 239
63. Friedl K, Hiller KA, Friedl KH, Clinical performance of a new glass ionomer-based restoration system: A retrospective cohort study: Dent Mater, 2011; 27(10); 1031-37
64. Bonifácio CC, Werner A, Kleverlaan CJ, Coating glass-ionomer cements with a nanofilled resin: Acta Odontol Scand, 2011; 70(6); 471-77
65. Perdigão J, Current perspectives on dental adhesion: (1) Dentin adhesion – not there yet: Japanese Dental Science Review, 2020; 8; 004
66. Ghinea R, Ugarte-Alvan L, Yebra A, Influence of surface roughness on the color of dental-resin composites: J Zhejiang Univ Sci B, 2011; 12(7); 552-62
67. Balkaya H, Arslan S, Pala K, A randomized, prospective clinical study evaluating effectiveness of a bulk-fill composite resin, a conventional composite resin and a reinforced glass ionomer in Class II cavities: One-year results: J Appl Oral Sci, 2019; 27; e20180678
68. Balkaya H, Arslan S, A Two-year clinical comparison of three different restorative materials in Class II cavities: Oper Dent, 2020; 45(1); E32-E42
69. Pitel ML, An improved glass ionomer restorative system: Stress-bearing Class I and II indications: Dent Today, 2017; 36(2); 130-34
70. Diem VT, Tyas MJ, Ngo HC, The effect of a nano-filled resin coating on the 3-year clinical performance of a conventional high-viscosity glass-ionomer cement: Clin Oral Investig, 2014; 18(3); 753-59
71. Alvanforoush N, Wong R, Burrow M, Palamara J, Fracture toughness of glass ionomers measured with two different methods: J Mech Behav Biomed Mater, 2019; 90; 208-16
72. Stefanac SJ, Nesbit SP: Diagnosis and treatment planning in dentistry, 2017; 423-31, St. Louis, Missouri, Elsevier https://www.who.int/publications-detail-redirect/9789240046184
73. Novrizal A, Soufyan A, Irawan B, Matram N, In vitro application of a nano-filled coating agent to improve the diametral tensile strength of glass ionomer cement: J Phys Confer Ser, 2018; 1073; 062025
74. Faraji F, Heshmat H, Banava S, Effect of protective coating on microhardness of a new glass ionomer cement: Nanofilled coating versus unfilled resin: J Conserv Dent, 2017; 20(4); 260-63
75. Ugurlu M, Effects of surface coating on the flexural strength of fluoride-releasing restorative materials after water aging for one year: European Oral Research, 2020; 45(2); 62-68
76. Goldstein GR, The longevity of direct and indirect posterior restorations is uncertain and may be affected by a number of dentist-, patient-, and material-related factors: J Evid Based Dent Pract, 2010; 10(1); 30-31
77. Gjorgievska E, Nicholson JW, Iljovska S, Slipper IJ, Marginal adaptation and performance of bioactive dental restorative materials in deciduous and young permanent teeth: J Appl Oral Sci, 2008; 16(1); 1-6
78. Pinto-Sinai G, Brewster J, Roberts H, Linear coefficient of thermal expansion evaluation of glass ionomer and resin-modified glass ionomer restorative materials: Oper Dent, 2018; 43(5); E266-E72
79. Lohbauer U, Dental glass ionomer cements as permanent filling materials? – properties, limitations and future trends: Materials, 2009; 3(1); 76-96
80. Neppelenbroek KH, The clinical challenge of achieving marginal adaptation in direct and indirect restorations: J Applied Oral Science, 2015; 23(5); 448-53
81. Hesse D, Bonifácio CC, Kleverlaan CJ, Raggio DP, Clinical wear of approximal glass ionomer restorations protected with a nanofilled self-adhesive light-cured protective coating: J Applied Oral Science, 2018; 26; 94
82. Palaniappan S, Elsen L, Lijnen I, Nanohybrid and microfilled hybrid versus conventional hybrid composite restorations: 5-year clinical wear performance: Clin Oral Investig, 2011; 16(1); 181-90
83. Cheng Y, Wang Z, Shi Y, Research on the characteristics of food impaction with tight proximal contacts based on deep learning: Comput Math Methods Med, 2021; 2021; 1000820
84. Shahmoradi M, Wan B, Zhang Z, Mechanical failure of posterior teeth due to caries and occlusal wear – a modelling study: J Mech Behav Biomed Mater, 2022; 125; 104942
85. Klinke T, Daboul A, Turek A, Clinical performance during 48 months of two current glass ionomer restorative systems with coatings: A randomized clinical trial in the field: Trials, 2016; 17(1); 1339
86. Santos VR, Lucchesi JA, Cortelli SC, Effects of glass ionomer and microfilled composite subgingival restorations on periodontal tissue and subgingival biofilm: A 6-month evaluation: J Periodontology, 2007; 78(8); 1522-28
87. Atieh M, Stainless steel crown versus modified open-sandwich restorations for primary molars: A 2-year randomized clinical trial: Inter J Paediatric Dent, 2008; 18(5); 325-32
88. World Health Organisation: Prevention and treatment of dental caries with mercury-free products and minimal intervention, 2022, World Health Organization https://www.who.int/publications-detail-redirect/9789240046184
Tables
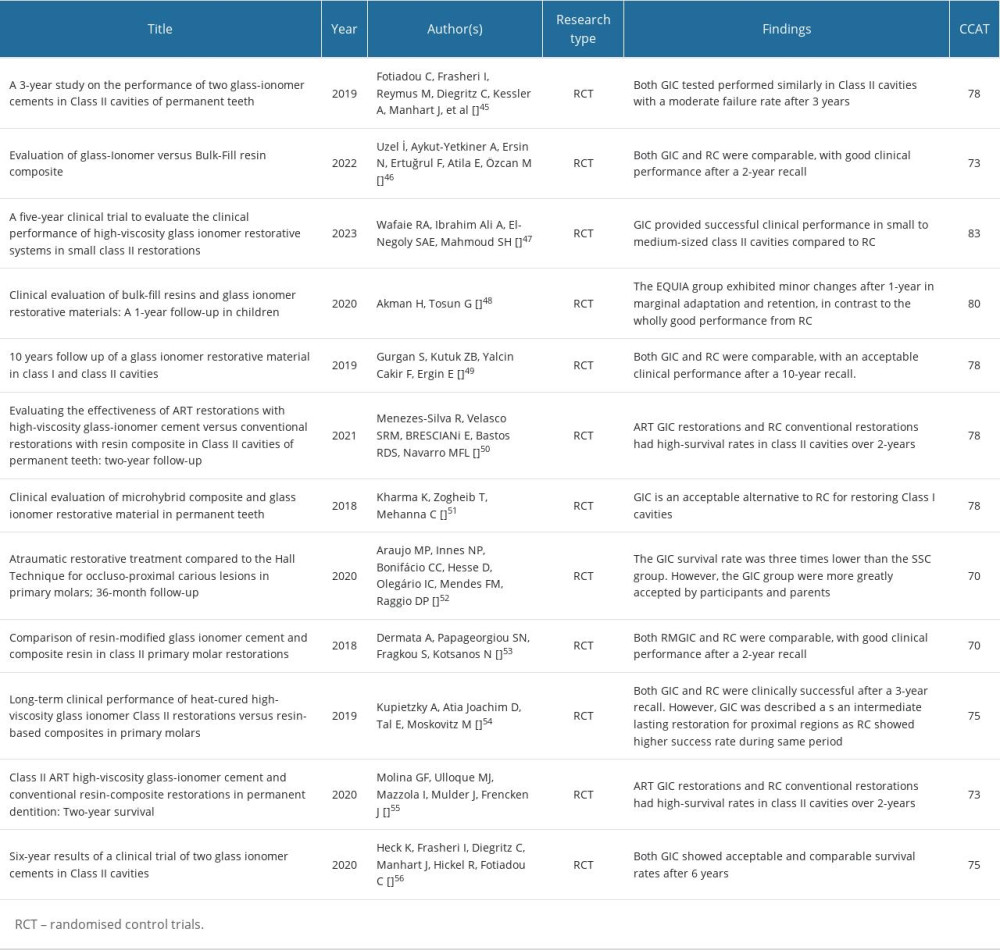 Table 1. Included studies with their title, year, author (s), outcomes, and Crowe Critical Appraisal Tool score.
Table 1. Included studies with their title, year, author (s), outcomes, and Crowe Critical Appraisal Tool score.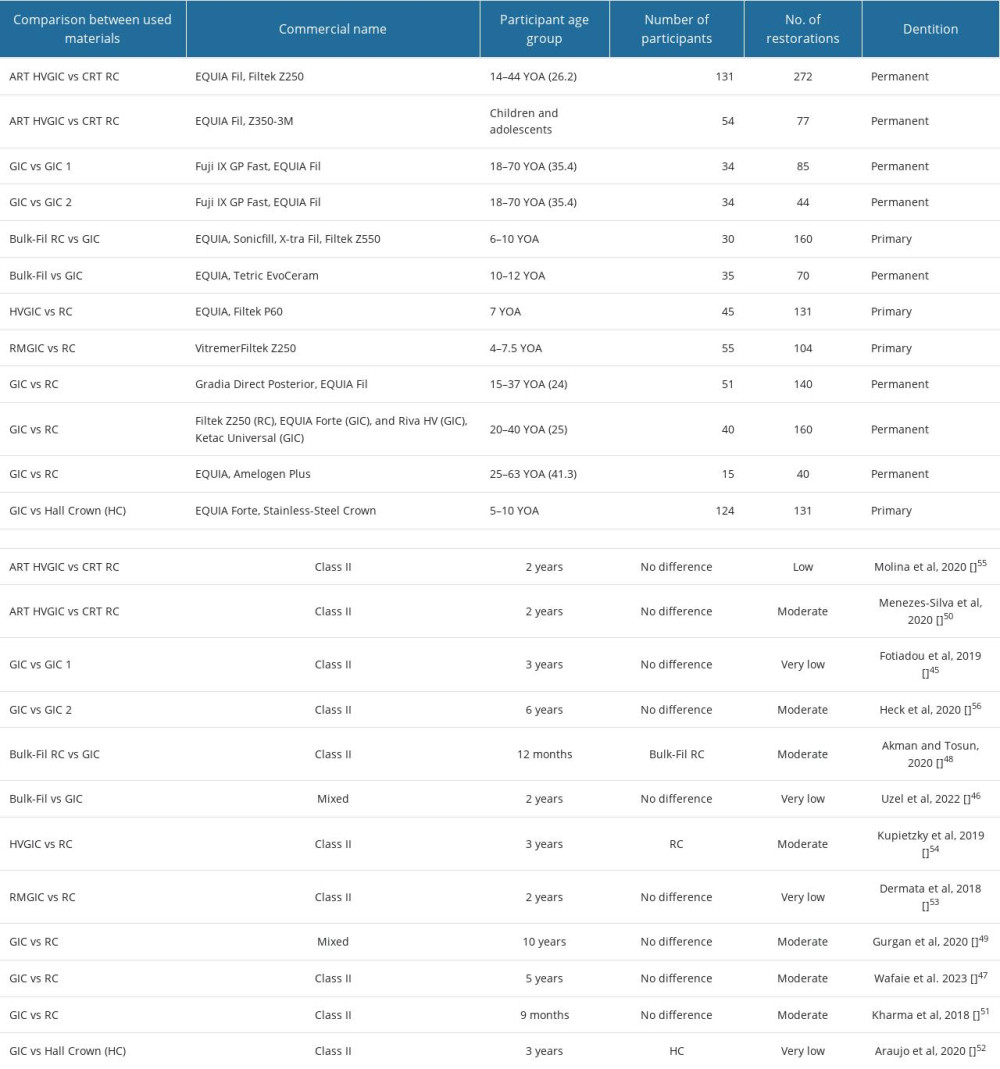 Table 2. Characteristics of the 12 included studies.
Table 2. Characteristics of the 12 included studies.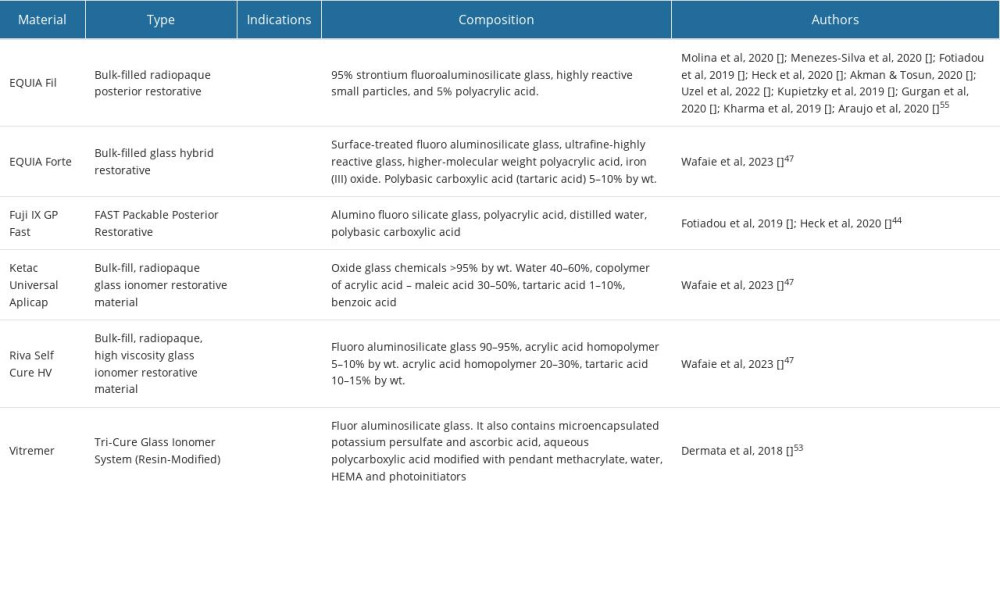 Table 3. Included materials and their types, indications, composition, and authors.
Table 3. Included materials and their types, indications, composition, and authors.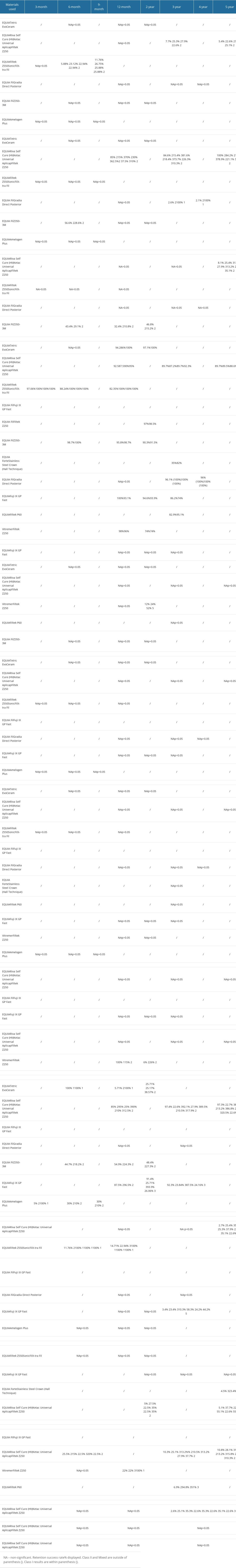 Table 4. Characteristics of the studies during different recall periods and their relation to esthetics, functions, and biological behavior (n=12).
Table 4. Characteristics of the studies during different recall periods and their relation to esthetics, functions, and biological behavior (n=12).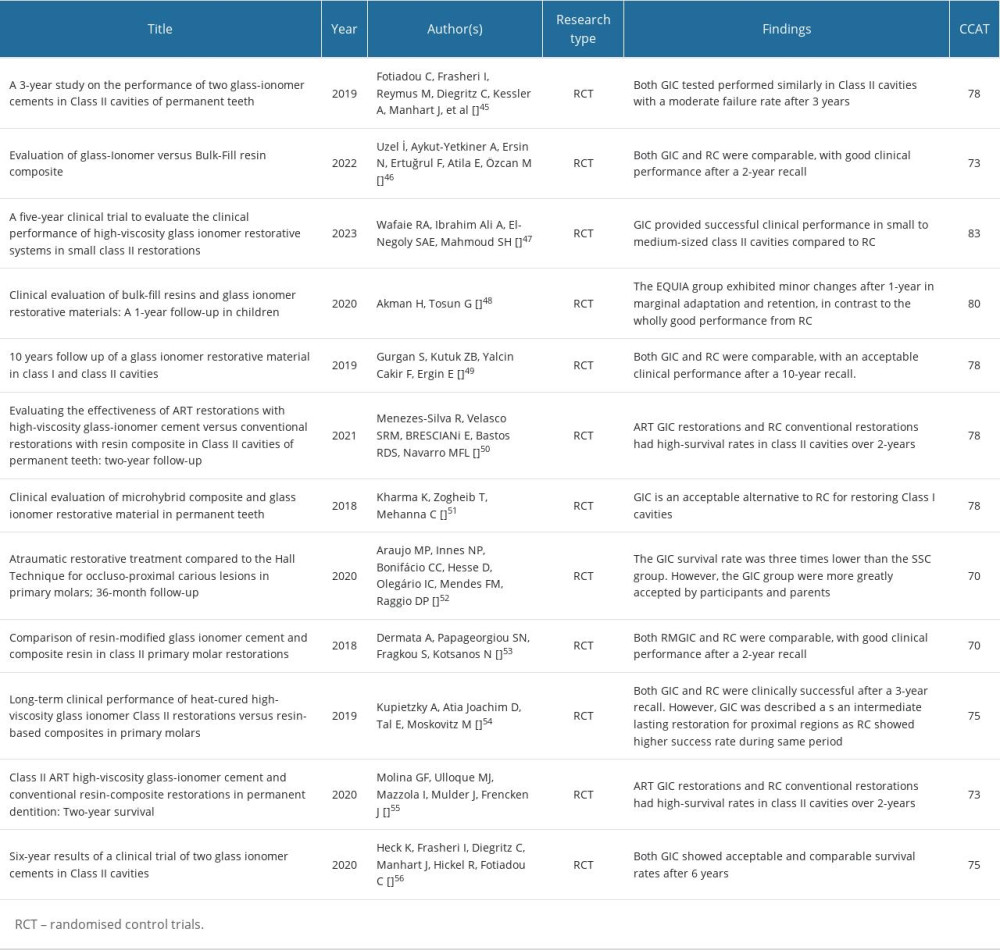 Table 1. Included studies with their title, year, author (s), outcomes, and Crowe Critical Appraisal Tool score.
Table 1. Included studies with their title, year, author (s), outcomes, and Crowe Critical Appraisal Tool score.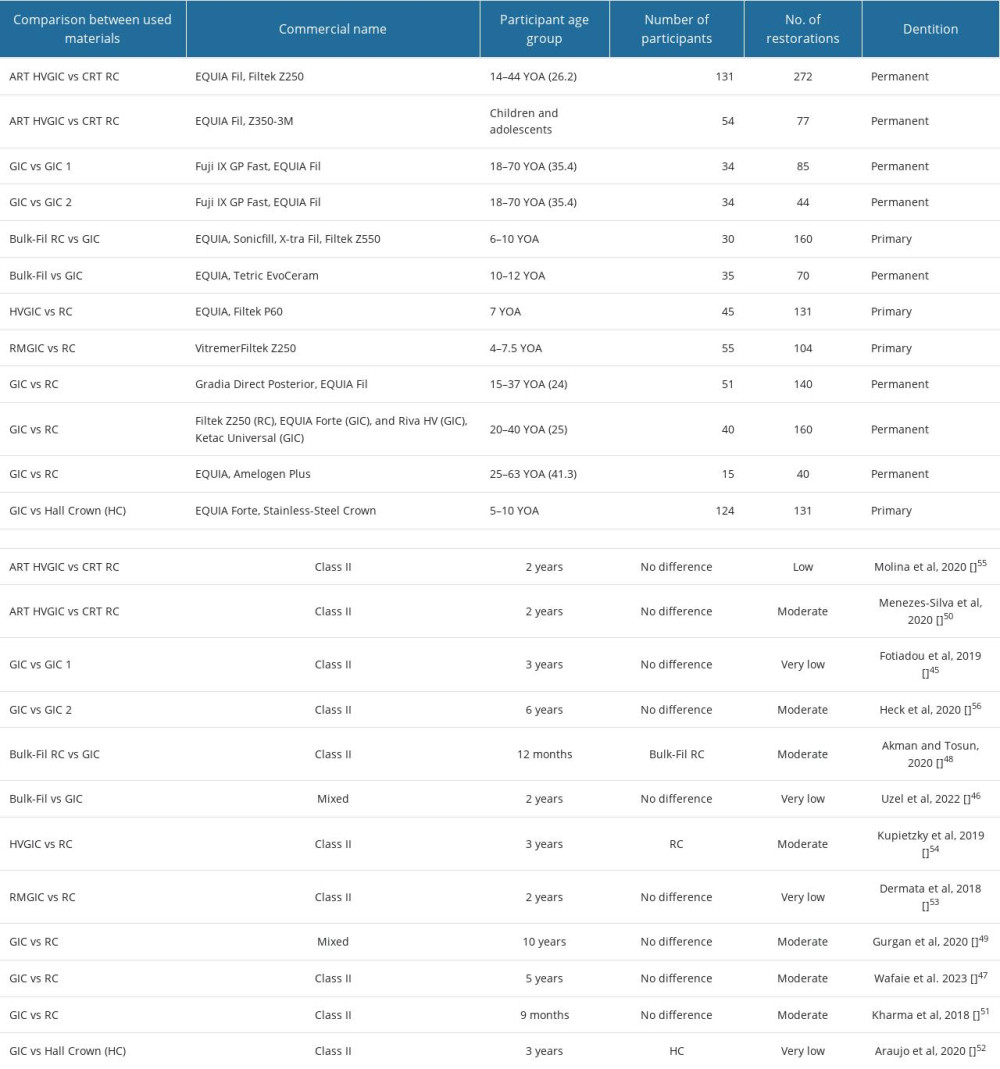 Table 2. Characteristics of the 12 included studies.
Table 2. Characteristics of the 12 included studies.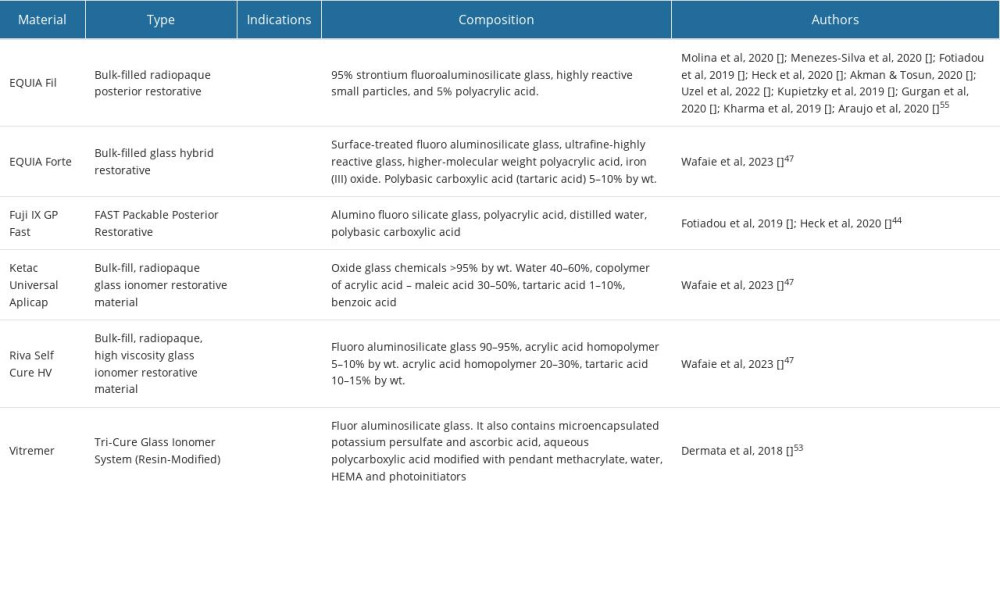 Table 3. Included materials and their types, indications, composition, and authors.
Table 3. Included materials and their types, indications, composition, and authors.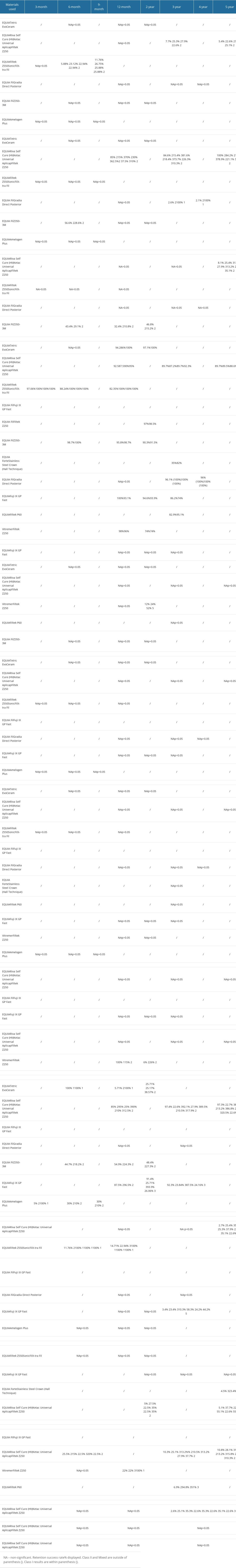 Table 4. Characteristics of the studies during different recall periods and their relation to esthetics, functions, and biological behavior (n=12).
Table 4. Characteristics of the studies during different recall periods and their relation to esthetics, functions, and biological behavior (n=12). In Press
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952









![PRISMA flow diagram [31,32].](https://jours.isi-science.com/imageXml.php?i=medscimonit-30-e943489-g001.jpg&idArt=943489&w=1000)