18 June 2024: Clinical Research
Outcomes of Anterior Lateral Approach and Gerdy’s Tubercle Osteotomy for Tibial Plateau Fractures Involving the Posterior Lateral Condyle: A Retrospective Study of 20 Patients
Yanqing Gu1A*, Wengbo Yang1BC, Yan Ren1C, Chenyang Xu1D, Lei Zhao1AEF, Chunzhi Jiang1AEFDOI: 10.12659/MSM.943946
Med Sci Monit 2024; 30:e943946
Abstract
BACKGROUND: The objective of this investigation was to assess the effectiveness of using T-shaped steel plates through the anterior lateral approach and Gerdy’s tubercle osteotomy for treating posterior lateral tibial plateau fractures.
MATERIAL AND METHODS: A retrospective analysis was conducted on clinical data from 20 patients, aged on average 53.9±10.36 years, who were admitted for tibial plateau fractures involving the posterior lateral condyle between January 2019 and October 2022. The fixation and reduction of the posterior lateral bone block were performed using the anterior lateral approach combined with Gerdy’s tubercle osteotomy to address the posterior lateral tibial plateau fracture. Post-surgery assessment was conducted using the Hospital for Special Surgery (HSS) knee combined score.
RESULTS: During the 12-24 (14.2±1.7) month postoperative period, we conducted 20 surgeries. Within 9 to 12 weeks, fracture healing transpired without any complications such as incision infection, nerve injury, or fracture displacement being detected. Assessment of knee joint function at the final follow-up was conducted using the HSS knee combined score, with results indicating 16 cases rated as excellent, 3 cases as good, and 1 case as fair.
CONCLUSIONS: In tibial plateau fractures impacting the posterior lateral condyle, the anterior lateral approach, combined with Gerdy’s tubercle osteotomy, allows for direct exposure and manipulation of the posterior lateral bone block fracture. Using a T-shaped support plate and a lateral locking plate provides a reliable method for fracture fixation, aiding in convenient surgical positioning and intraoperative fluoroscopy. The treatment approach effectively manages fractures located on the posterior lateral aspect of the tibial plateau.
Keywords: Fracture Fixation, Fracture Healing, Tectum Mesencephali
Introduction
High-energy injuries are commonly linked to tibial plateau fractures, which represent around 1% of all fractures. Tibial plateau fractures can occur due to varus or valgus loading on the knee, with or without axial loading. These fractures can manifest in a lateral, medial, or bicondylar orientation [1]. The efficacy of open reduction internal fixation (ORIF) has been established in tibial plateau fractures presenting with prominent articular surface stepover, ligamentous instability, Schatzer type IV, V, and VI injuries, and condylar widening [2].
Studies on the posterior lateral condyle of the tibial plateau have shown that this area is a common site for complex tibial plateau fractures. The intersection of significant posterior lateral condylar splitting and collapse may lead to joint incongruity, causing bone instability and impacting treatment effectiveness, necessitating simultaneous surgical reduction and fixation of the posterior lateral condyle [3,4].
Surgical approaches for knee joint procedures are broadly classified as non-osteotomy and osteotomy. Non-osteotomy approaches, including the posterior lateral, anterior lateral, lateral, posterior medial, and posterior median approaches, each have distinct characteristics. The posterior lateral approach, known for its directness, allows for reduction and supports steel plate fixation under direct visualization. However, challenges arise when attempting to combine the Calson and Frosch approaches, commonly used for repairing the posterior lateral condyle of the tibial plateau, with the medial approach due to issues such as positional placement [5,6]. By employing a floating position alongside a posterior inverted L-shaped approach and an anterior lateral approach, certain scholars have effectively accomplished fracture reduction. Nonetheless, this positioning has been demonstrated to enhance fluoroscopy challenges, escalate the prevalence of soft tissue complications, and impede the retrieval of internal fixation. The anterior lateral approach requires the bamboo raft steel plate to be placed backward for optimal fixation. In contrast, the lateral approach involves a single incision, allowing for simultaneous treatment of tibial anterior lateral and posterior lateral plateau fractures. The anatomy of the posterior medial approach is relatively simple, but it is unable to provide complete direct visualization for comminuted fractures of the posterior lateral platform. Due to its potential to harm the popliteal artery and tibial nerve [7,8], the posterior median approach is used less frequently. Conversely, the osteotomy approach encompasses fibular head osteotomy, femoral condylar osteotomy, and Gerdy’s tubercle osteotomy. While osteotomy of the fibular head provides a clear field of view, it also entails relatively extensive bone damage [9–11].
Gerdy nodule osteotomy removes a Gerdy nodule bone block parallel to the longitudinal axis of the tibia. After the bone block is reversed, the lateral condyle of the femur can be exposed. EE Johnson introduced a new surgical approach in CORR that can preserve the Gerdy nodule insertion point of the iliotibial tract. In this procedure, a partial anterior tenotomy of the IT band is performed while maintaining the attachment of the posterior iliotibial band to Gerdy’s tubercle. By encircling the fracture lines around Gerdy’s tubercle, osteotomy and external rotation of the tubercle can be carried out, along with excessive joint distraction, to enhance direct visualization of the joint depression. The subsequent procedures, such as joint elevation, grafting, and internal fixation, are performed through this incision [12,13].
Herein, we retrospectively investigated the clinical efficacy of utilizing the Gerdy’s tubercle osteotomy approach in treating posterolateral tibial plateau fractures at our hospital from 2019 to 2022, aiming to enhance exposure and operative access in this area. This study employed an anterior lateral approach to reach the anterior aspect of the tibial plateau, using Gerdy’s tubercle osteotomy to address the posterior lateral bone block. To address complex tibial plateau fractures involving the posterior lateral condyle, a distal radius oblique “T”- or “T”-shaped steel plate was utilized alongside a lateral locking steel plate in the anterior aspect. This approach aimed to construct a “fence-like structure,” thereby circumventing the necessity for intraoperative repositioning. We outline the surgical techniques and precautions pertinent to this approach, serving as a reference for the surgical procedure and selecting internal fixators to treat these fractures.
Material and Methods
INCLUSION AND EXCLUSION CRITERIA:
The inclusion criteria for the study were comprised of adult patients aged 18 years and older with lateral tibial plateau fractures involving the posterior column, as evidenced by preoperative knee CT scans. It was imperative that these patients did not exhibit complications such as vascular or nerve damage, or osteofascial compartment syndrome.
The exclusion criteria involved the presence of multiple fractures in the ipsilateral lower limb, a primary disease affecting the ipsilateral hip and ankle joints, inability to walk normally before the injury, severe degeneration of the knee joint due to osteoarthritis and dysfunction, a history of rheumatoid arthritis, follow-up duration of less than 12 months, and an old fracture.
PREOPERATIVE PREPARATION:
Upon admission, immediate physical therapy, including traction, ice compression, and elevation of the calcaneal nodule, was initiated. The ankle-brachial index was monitored, and sodium saponin was administered to reduce swelling and prevent thrombosis. Antibiotics were prescribed as a prophylactic measure for patients with open wounds. Additionally, CT three-dimensional reconstruction was used to reassess the location of significant fracture blocks and accompanying ligament injuries after traction, to determine the surgical plan, and to exclude lower limb deep vein thrombosis through preoperative vascular ultrasound examination. Among 20 patients, the mean time elapsed from injury to surgery was (7.3±2.8) days, ranging from 5 to 11 days.
SURGICAL PROCEDURE:
When positioned supine, the patient was given a pneumatic tourniquet. In complex tibial plateau fractures, the medial approach was typically employed to address the medial bone block, with the positioning and number of steel plate fixations determined by the specific fracture type. To address the lateral bone block, an anterolateral approach was utilized, involving a longitudinal arc incision made along the lateral aspect of the anterior tibial crest. The incision was 2 cm below the midpoint between the fibular head and the tibial tuberosity. The distal end of the incision was extended along the fracture line. The iliotibial tract was longitudinally split, the joint capsule located below the lateral meniscus was incised, and an L-shaped osteotomy was conducted along the outer edge of the tibial intercondylar spine in the non-load-bearing area of the anterior lateral tibial condyle, adjacent to Gerdy’s tubercle on the inner side. The separated bone block was then outwardly flipped while preserving the integrity of the lateral soft tissue hinge. The posterior lateral collapsed fracture and damaged meniscus were surgically addressed by suturing and repairing the meniscus and releasing and elevating the collapsed bone block located 2 cm below the articular surface using a sharp bone knife. The posterior lateral column fracture block was reduced under direct vision, followed by bone grafting. The lifted fracture block from the anterior lateral column was reduced, and a distal radius T-shaped steel plate was selected, shaped, and used to fix the posterior lateral bone block from the front, followed by fixation with an appropriate anterior lateral anatomical locking steel plate on the tibial plateau. Multiple locking screws were inserted from front to back along the bone below the joint surface, creating a fence-like system to simultaneously stabilize the anterior lateral column and posterior lateral column (Figure 1).
POSTOPERATIVE TREATMENT AND FOLLOW-UP:
After surgery, negative pressure drainage was utilized until the drainage volume remained below 50 mL for 24 and 48 hours. Elastic bandages were applied to compress and wrap the incision until it was completely dry and free from exudation. The affected limb was elevated, and drainage was ceased before the X-ray examination. Prophylactic antibiotics and low molecular weight heparin were administered 24 hours for thrombosis prevention. On the third day after surgery, partial knee flexion and extension training commenced under the protection of a knee joint fixator. Knee flexion was restricted to 0° to 90° within 6 weeks after surgery, with complete knee extension and flexion training commencing afterward. Partial weight-bearing at the toes began at 8 weeks, with complete weight-bearing avoided until 3 months after surgery. After discharge, it is recommended to adhere to the prescribed rehabilitation plan and attend outpatient follow-up appointments at 1, 2, 3, 6, and 12 months postoperatively. The author performed examinations at each visit, encompassing knee range of motion (ROM), assessment of wound healing, and radiographic evaluation of the healing progress. Assessment of healing included monitoring the gradual bone remodeling, integration of fracture lines, detection of any indications of fixation loosening, and preservation of articular surface reduction. All radiographic images of the 20 patients with posterior plateau fractures were reviewed by 2 authors (Lei Zhao and Chenyang Xu). The assessment of the final radiographs included an evaluation of the level of depression in the anteroposterior and lateral positions of the knee joint, the fusion of fracture lines and bone graft, and the identification of radiolucency or potential hardware loosening. Using the Hospital for Special Surgery (HSS) knee joint scoring system, the recovery of knee joint function was assessed at the 12-month follow-up.
THE HSS KNEE JOINT SCORING SYSTEM:
The HSS knee scoring system was utilized to evaluate the clinical outcome. The HSS score is made up of 6 sections, namely pain (30 scores), function (22 scores), range of motion (18 scores), muscle force (10 scores), flexion-extension deformity (10 scores), and stability (10 scores). Falling within the range of 85–100, a score is classified as excellent, while a rating of 70–84 is deemed good. Acceptable performance is indicated by a score of 60–69, with anything below 60 categorized as poor [14].
STATISTICAL ANALYSIS:
The R language program (version 3.4.4) was employed alongside Empower Stats software for the statistical description and data analysis. Continuous variables were represented as mean±standard deviation (SD), compared using a linear model.
Results
PERIOPERATIVE STATISTICS:
The study cohort comprised 20 patients, 13 females and 7 males; their average age was 53.9±10.36 years. The procedure of anterolateral plateau intraarticular osteotomy was carried out on 20 patients suffering from posterior plateau fractures to access centro-posterior and postero-lateral articular depression. In the study, 50 patients had Schatzker Type II to III fractures, while 15 had Type V to VI fractures, with 8 of the latter located in the right knee and 12 in the left knee.
The follow-up period varied from 14 to 48 months, with an average of 22.4 months ±9.81. Surgical operations had durations ranging from 80 to 140 minutes, with a mean duration of 114 minutes ±24.14. Postoperative X-rays confirmed successful fracture reduction and favorable internal fixation positioning, with no observed complications such as common peroneal nerve paralysis, calf fascia compartment syndrome, or poor wound healing.
RADIOLOGICAL FOLLOW-UP EVALUATION:
Throughout the study, reduction loss did not occur, and the platform width and the lower limb force line were maintained within normal ranges for all patients until the last follow-up.
FUNCTION FOLLOW-UP EVALUATION:
At the final follow-up, the HSS score varied between 74 and 96 (85.33±7.81), and the knee joint exhibited extension from 0° to 22° (8.1°±5.05°) and flexion from 110° to 135° (125°±15°), as shown in Figures 1, 2.
Discussion
Tibial plateau fractures are a common type of fracture, accounting for approximately 1% of all body fractures [5]. The incidence is slightly higher in males than in females, with females being more susceptible between the ages of 60 and 90. The “Three Pillars Theory Classification of Tibial Plateau,” introduced by Luo et al [4] in 2010, classifies the tibial plateau into lateral, medial, and posterior columns based on CT imaging data and knee joint injury mechanisms. Positioned on the lateral side of the posterior column, the posterior lateral tibial plateau is pivotal for knee joint motion, particularly in knee flexion [12]. Fractures of the posterior lateral tibial plateau are a prevalent occurrence, constituting around 35.9% of AO/OTA 41B fractures [6], 44.32% of AO/OTA 41C fractures [13], and around 15% of all tibial plateau fractures [15–17]. This area is anatomically complex, being obstructed by significant structures such as the fibular head, numerous muscles and ligaments, as well as important popliteal blood vessels and nerves passing through the posterior popliteal fossa [7–8], making surgical exposure quite challenging. Consequently, the treatment of fractures in this area poses significant challenges [9–11]. Recently, there has been a rising interest in managing posterior lateral tibial plateau fractures.
The anterior steel plate lacks the strength to withstand axial loading forces, increasing the risk of failure of traditional anterior-posterior tension screws. Hence, the arrangement of screws in various steel plate setups often deviates from the necessary alignment with the supporting joint surface, especially in cases of fractures affecting the posterior lateral or posterior medial column of the tibial plateau [18–19]. Bermúdez et al [20] devised a solution for this problem by creating a “horizontal rafting plate.” This plate, made by bending a 3.5 mm reconstructive steel plate with flexibility, is designed to encircle the posterior lateral edge of the tibial plateau and provide reinforcement for the posterior bone block. Similarly, Cho et al [21] treated 7 patients with posterior lateral tibial plateau fractures using a modified anterior lateral surgical approach and transformed a 2.7 mm clover-shaped universal compression steel plate into “rim plates” to cover most of the posterior lateral tibial plateau, achieving satisfactory surgical reduction and postoperative functional recovery. While this type of edge steel plate may be more suitable for cases with individual posterior lateral fracture fragments, it may not effectively stabilize fractures with comminuted posterior lateral articular surfaces. By Chen HW et al and Mao W et al, an extended anterolateral approach has been created, showcasing outstanding visualization potential. Through this approach, the plate can be placed in a more posterior position [22,23]. Additionally, Giordano et al [24] proposed the “hoop plate” technique, involving the insertion of a horizontally preformed 1/3 tubular steel plate from the outer to inner sides through the posterior lateral surgical approach (Lobenhoffer approach) of fibular head osteotomy, providing support and embracing effects for fractures resulting from posterior lateral cortical rupture, displacement, and comminuted articular surfaces. The transfibular osteotomy approach presents a key benefit in facilitating intuitive anatomical reduction of the joint, particularly advantageous for managing certain types of tibial plateau posterolateral column fractures. Nonetheless, this approach is theoretically linked to complications, including common fibular nonunion, peroneal nerve injury, and potential compromise of upper tibiofibular joint stability. Moreover, the utility of hoop plates in reinforcing the fixation of epiphyseal fractures is constrained.
Based on previous studies, our fixation method effectively reduces posterior lateral bone mass using the anterior lateral approach under direct vision. Hence, this retrospective study enrolled 20 patients with tibial plateau fractures affecting the posterior lateral condyle. Between January 2019 and October 2022, they underwent fixation and reduction of the posterior lateral bone block through the anterior lateral approach, along with Gerdy’s tubercle osteotomy. The objective was to assess knee function using the HSS scoring system at the 1-year postoperative follow-up. Gerdy’s tubercle osteotomy, or the original fracture line osteotomy, is the most suitable method for accessing and realigning the region near the intercondylar spine on the lateral side after reduction. The combination of these approaches offers a comprehensive solution for addressing a wide spectrum of lateral condylar fractures. Gerdy’s tubercle osteotomy is performed in the bare area near the intercondylar spine on the lateral condyle of the tibial plateau, extending backward to the fracture line, with minimal impact on the weight-bearing joint surface in direct contact with the femoral condyle. Following osteotomy, the anterior lateral bone block can be rotated outward to fully expose the coronal surface of the posterior lateral condyle fracture under direct visual inspection. For patients with severe flour fragmentation and collapse of the posterior lateral joint, Gerdy’s tubercle osteotomy can create sufficient space below the front of the fracture to expose the deep surface of the fracture. Subsequently, healthy trabecular bone can be cut from the area far from the collapse and lifted and reduced as a whole under direct visual inspection, thereby avoiding the separation and poor reduction of crushed bone fragments, which is the main advantage of Gerdy’s tubercle osteotomy. After osteotomy, the posterior lateral fracture is reduced under direct vision. The T-shaped steel plate is affixed to the front of the tibial plateau, and the screws above the T-shaped steel plate secure the fracture from front to back. We integrated it into a cohesive unit, merging the lateral “L” shape with the anterolateral “T” shape in a dual plate fixation. The screws, along with those of the anterior lateral locking steel plate, form a fence-like structure, ensuring the entire lateral bone block of the tibial plateau. Follow-up results indicate favorable postoperative fixation and functional recovery.
Several limitations are present in this study, such as a limited number of sample cases, the absence of a control group, a short follow-up duration, and the retrospective nature of the case analysis, which could impact the study’s conclusions. Further research focusing on injury mechanisms, fracture morphology, and biomechanical assessments is essential to establish the surgical techniques employed, ascertain the actual complication rates, and confirm their safety and efficacy.
Conclusions
In conclusion, employing T-shaped steel plates through the anterior lateral approach, along with Gerdy’s tubercle osteotomy, is deemed a secure and efficient strategy for managing intricate tibial plateau fractures encompassing the posterior lateral condyle, leading to favorable treatment results. The approach demonstrates minimal postoperative complications and favorable clinical efficacy, warranting its promotion in clinical practice. However, the study’s limited sample size necessitates further research to enhance understanding in clinical practice and establish a control group.
Figures
 Figure 1. Schematic diagram of steel plate position. (A) 3D-printed tibial model illustrating the positioning of the T-shaped steel plate on the outer side of the tibial plateau fracture. (B) Diagram illustrating the front steel plate, an outer steel plate with a screw distribution resembling a fence, and the fixation of the outer and rear outer bone blocks.
Figure 1. Schematic diagram of steel plate position. (A) 3D-printed tibial model illustrating the positioning of the T-shaped steel plate on the outer side of the tibial plateau fracture. (B) Diagram illustrating the front steel plate, an outer steel plate with a screw distribution resembling a fence, and the fixation of the outer and rear outer bone blocks. 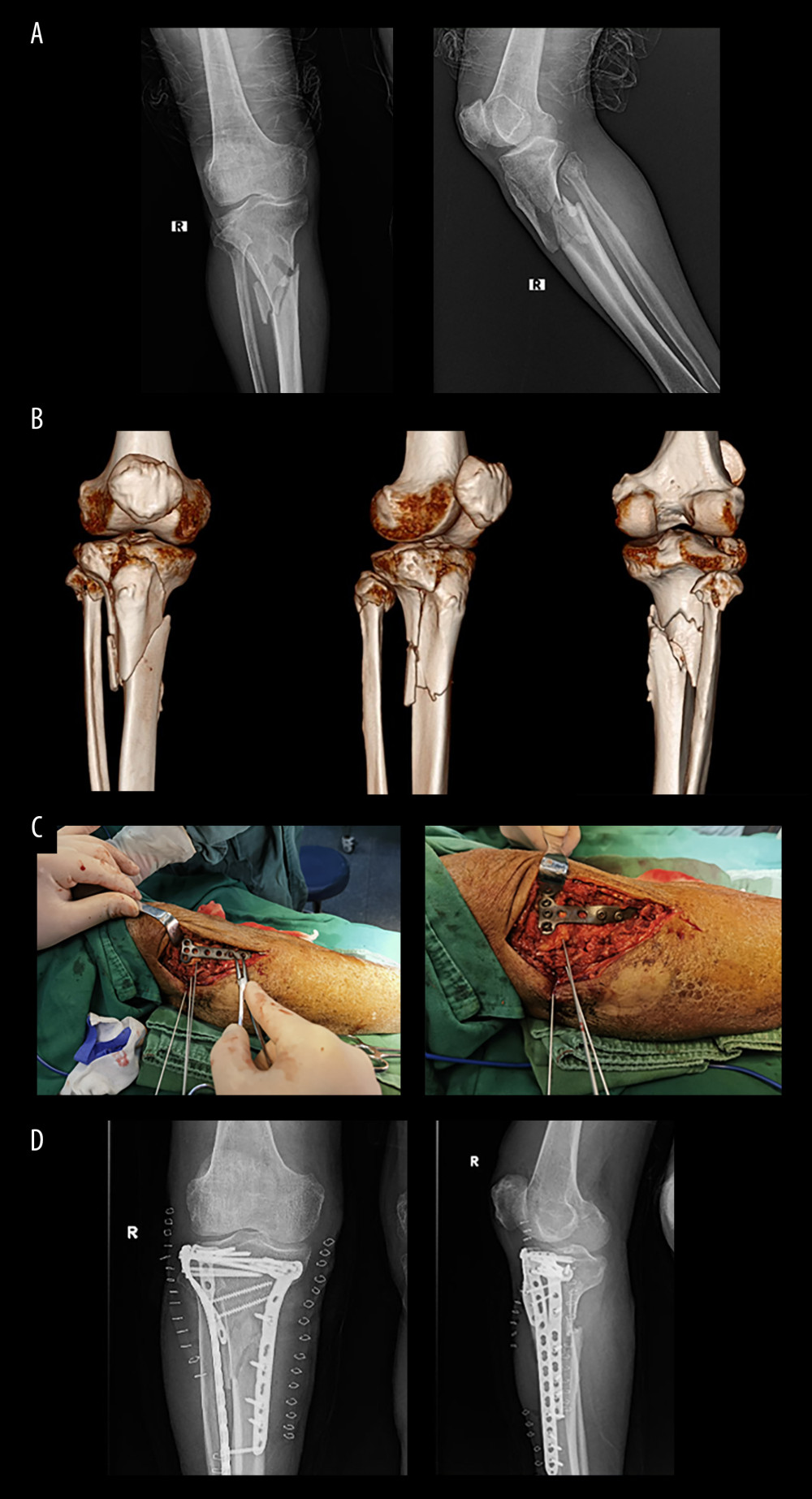 Figure 2. Typical surgical case images. Typical surgical procedure: (A) X-ray and (B) 3D CT examination of a typical surgical case prior to surgery, (C) Sharing of a typical case’s operation process, and (D) X-ray examination of a typical case 3 months after surgery.
Figure 2. Typical surgical case images. Typical surgical procedure: (A) X-ray and (B) 3D CT examination of a typical surgical case prior to surgery, (C) Sharing of a typical case’s operation process, and (D) X-ray examination of a typical case 3 months after surgery. References
1. Mthethwa J, Chikate A, A review of the management of tibial plateau fractures: Musculoskelet Surg, 2018; 102(2); 119-27
2. Hall JA, Beuerlein MJ, McKee MDCanadian Orthopaedic Trauma Society, Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures. Surgical technique: J Bone Joint Surg Am, 2009; 91(Suppl 2 Pt 1); 74-88
3. Xie X, Zhan Y, Wang Y, Comparative analysis of mechanism associated 3-Dimensional tibial plateau fracture patterns: J Bone Joint Surg Am, 2020; 102(5); 410-18
4. Luo CF, Sun H, Zhang B, Three-column fixation for complex tibial plateau fractures: J Orthop Trauma, 2010; 24(11); 683-92
5. Carlson DA, Posterior bicondylar tibial plateau fractures: J Orthop Trauma, 2005; 19(2); 73-78
6. Frosch KH, Balcarek P, Walde T, A new posterolateral approach without fibula osteotomy for the treatment of tibial plateau fractures: J Orthop Trauma, 2010; 24(8); 515-20
7. Heidari N, Lidder S, Grechenig W, The risk of injury to the anterior tibial artery in the posterolateral approach to the tibia plateau: A cadaver study: J Orthop Trauma, 2013; 27(4); 221-25
8. Dee M, Sojka JM, Daccarett MS, Evaluation of popliteal artery injury risk with locked lateral plating of the tibial plateau: J Orthop Trauma, 2011; 25(10); 603-7
9. Solomon LB, Stevenson AW, Baird RP, Posterolateral transfibular approach to tibial plateau fractures: Technique, results, and rationale: J Orthop Trauma, 2010; 24(8); 505-14
10. Solomon LB, Stevenson AW, Lee YC, Posterolateral and anterolateral approaches to unicondylar posterolateral tibial plateau fractures: A comparative study: Injury, 2013; 44(11); 1561-68
11. Frosch KH, Korthaus A, Thiesen D, The concept of direct approach to lateral tibial plateau fractures and stepwise extension as needed: Eur J Trauma Emerg Surg, 2020; 46(6); 1211-19
12. Liebergall M, Wilber JH, Mosheiff R, Gerdy’s tubercle osteotomy for the treatment of coronal fractures of the lateral femoral condyle: J Orthop Trauma, 2000; 14(3); 214-15
13. Johnson EE, Timon S, Osuji C, Surgical technique: Tscherne-Johnson extensile approach for tibial plateau fractures: Clin Orthop Relat Res Sep, 2013; 471(9); 2760-67
14. Insall JN, Ranawat CS, Aglietti P, A comparison of four models of total knee-replacement prostheses: J Bone Joint Surg Am, 1976; 58; 754-65
15. Freeman MA, Pinskerova V, The movement of the normal tibio femoral joint: J Biomech, 2005; 38(2); 197-208
16. Zhu Y, Meili S, Dong MJ, Pathoanatomy and incidence of the posterolateral fractures in bicondylar tibial plateau fractures: Aa clinical computed tomography-based measurement and the associated biomechanical model simulation: Arch Orthop Trauma Surg, 2014; 134(10); 1369-80
17. Sohn HS, Yoon YC, Cho JW, Incidence and fracture morphology of posterolateral fragments in lateral and bicondylar tibial plateau fractures: J Orthop Trauma, 2015; 29(2); 91-97
18. Barei DP, Nork SE, Mills WJ, Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique: J Orthop Trauma, 2004; 18(10); 649-57
19. Georgiadis GM, Combined anterior and posterior approaches for complex tibial plateau fractures: J Bone Joint Surg Br, 1994; 76(2); 285-89
20. Bermúdez CA, Ziran BH, Barrette-Grischow MK, Use of horizontal rafting plates for posterior elements of complex tibial plateau fractures: description and case reports: J Trauma, 2008; 65(5); 1162-67
21. Cho JW, Samal P, Jeon YS, Rim plating of posterolateral fracture fragments (PLFs) through a modified anterolateral approach in tibial plateau fractures: J Orthop Trauma, 2016; 30(11); e362-e68
22. Chen HW, Luo CF, Extended anterolateral approach for treatment of posterolateral tibial plateau fractures improves operative procedure and patient prognosis: Int J Clin Exp Med, 2015; 8(8); 13708-15
23. Mao W, Chen G, Zhu Y, Treatment of tibial plateau fractures involving the posterolateral column using the extended anterolateral approach: Medicine (Baltimore), 2021; 100(38); e27316
24. Giordano V, Schatzker J, Kfuri M, The “hoop” plate for posterior bicondylar shear tibial plateau fractures: Description of a new surgical technique: J Knee Surg, 2017; 30(6); 509-13
Figures
 Figure 1. Schematic diagram of steel plate position. (A) 3D-printed tibial model illustrating the positioning of the T-shaped steel plate on the outer side of the tibial plateau fracture. (B) Diagram illustrating the front steel plate, an outer steel plate with a screw distribution resembling a fence, and the fixation of the outer and rear outer bone blocks.
Figure 1. Schematic diagram of steel plate position. (A) 3D-printed tibial model illustrating the positioning of the T-shaped steel plate on the outer side of the tibial plateau fracture. (B) Diagram illustrating the front steel plate, an outer steel plate with a screw distribution resembling a fence, and the fixation of the outer and rear outer bone blocks.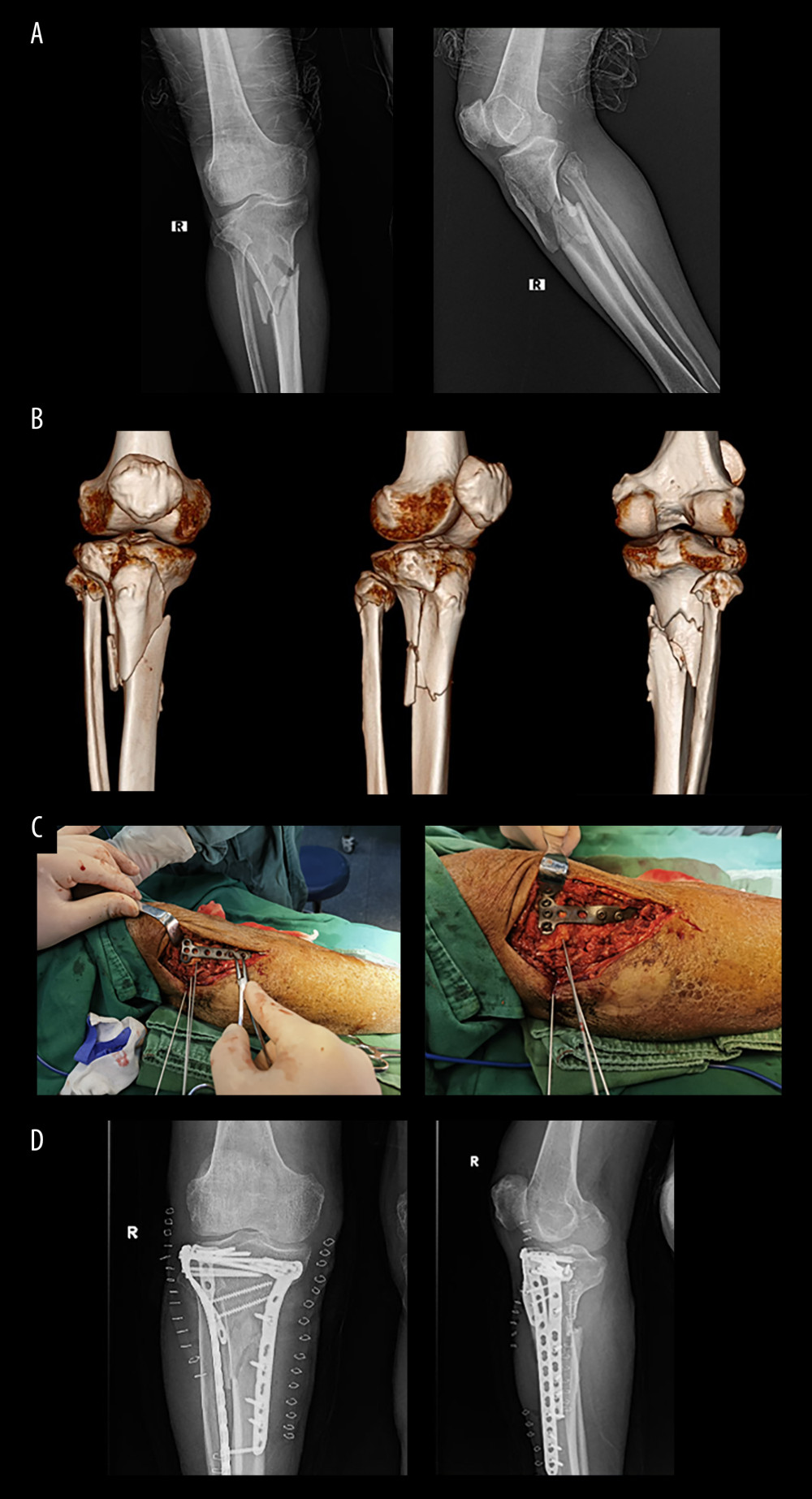 Figure 2. Typical surgical case images. Typical surgical procedure: (A) X-ray and (B) 3D CT examination of a typical surgical case prior to surgery, (C) Sharing of a typical case’s operation process, and (D) X-ray examination of a typical case 3 months after surgery.
Figure 2. Typical surgical case images. Typical surgical procedure: (A) X-ray and (B) 3D CT examination of a typical surgical case prior to surgery, (C) Sharing of a typical case’s operation process, and (D) X-ray examination of a typical case 3 months after surgery. In Press
Clinical Research
Surgical Reconstruction of Type IV Hypoplasia of the Thumb (Floating Thumb) in Infants: A Retrospective Ana...Med Sci Monit In Press; DOI: 10.12659/MSM.943686
Clinical Research
Effect of COVID-19 on Thrombosis Incidence and Patient Prognosis in Kidney Transplant RecipientsMed Sci Monit In Press; DOI: 10.12659/MSM.944285
Review article
The Influence of Acid-Base Balance on Anesthetic Muscle Relaxants: A Comprehensive Review on Clinical Appli...Med Sci Monit In Press; DOI: 10.12659/MSM.944510
Clinical Research
Enhancement of Pulmonary Function and Reduction of Complications Through EIT-Guided Yoga Breathing Exercis...Med Sci Monit In Press; DOI: 10.12659/MSM.942954
Most Viewed Current Articles
17 Jan 2024 : Review article 2,459,040
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research 1,560,914
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research 690,569
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial 50,460
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








