30 April 2024: Lab/In Vitro Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Restored with Cast Post Cores Using 5 Common Luting (Cement) Agents
Monika SinghDOI: 10.12659/MSM.944110
Med Sci Monit 2024; 30:e944110
Abstract
BACKGROUND: A luting agent is a dental cement used to secure a dental restoration. This study aimed to evaluate retentive strength of 50 endodontically-treated single-rooted mandibular second premolars (extracted) restored using 5 common luting (cement) agents.
MATERIAL AND METHODS: Fifty single-rooted mandibular second premolars with adequate root length and uniform size/shape were decoronated. After completing endodontic biomechanical preparation and obturation, root canals of all specimens were prepared to receive a cast post core. Depending upon cementation type, CPC specimens were divided in 5 groups (10 each) (Gp): Zinc phosphate (Gp ZP), polycarboxylate (Gp PC), glass ionomer (Gp GI), resin-modified glass ionomer (Gp RGI), and resin cement (Gp RC). Retentive strength was determined using the adhesive failure pull-out test. Mean/standard deviations were calculated for tensile forces (in kilograms) and differences were determined using analysis of variance (ANOVA). Multiple comparison was performed using the t test. A P value of ≤0.05 indicated a statistically significant difference.
RESULTS: The order of mean tensile strength from higher to lower was Gp RC (21.46) >Gp RGI (18.17) >Gp GI (16.07) >Gp ZP (15.33) >Gp PC (13.63). Differences in retentive strengths between the cements were significant (P≤0.05). Multiple-group comparisons showed that except for Gp ZP and Gp GI, all groups differed significantly from each other.
CONCLUSIONS: All investigated cements provided optimal retentive strengths, with wide differences between them. Resin cements should be used when CPC removal is not anticipated, while polycarboxylate or zinc phosphate should be used if CPC removal is anticipated.
Keywords: Dental Casting Technique, Dental Prosthesis Retention, Dental Restoration Failure, Dental Restoration, Permanent, Post and Core Technique
Introduction
Use of metal and wood placed within the roots of teeth to retain a bridge dates to the year 1728 and the mid-nineteenth century [1]. Later modifications in the nineteenth century included the ‘Richmond crown’ (single-unit cast metal post and crown) [2] and custom cast post core (CPC). Survival rates of endodontically-treated teeth increased with placement of an intraradicular post [3,4], but some critics have stated that intraradicular posts do not reinforce tooth structure [5,6]. Concerns include further depletion of dentin after endodontic treatment [7], loss of water and collagen [8], post space preparation and post design [7], greater differences in modulus of elasticity between posts (fiber post are 45.7–54.8 gigapascals [Gpa], cast posts are 178.34–198.76 Gpa, and dentin is 18.6 Gpa) [9,10], increased stress within roots and poor esthetics (prefabricated metal and CPC) [11]. Post cores are not essential for all teeth that have received endodontic treatment [12], but are indicated in cases where the remaining coronal tooth structure cannot retain a restoration and all other means or retaining a core have been exhausted [13]. Any tooth that has lost substantial coronal tooth structure due to caries, previous and current restorations, or endodontic treatment preparations (access cavity and root canal space) is likely to be a candidate for a post core, depending on the remaining tooth structure (post crown preparation), tooth position, patient/dentist preference, and core/crown material [14,15]. Metal dowels have been reported to increase fracture resistance of teeth [16], and studies reporting greater risk of root fracture when using a post core have not used the crown (isolated post and core) [17,18]. Recent studies on survival rates of post cores have reported they last for 10.9 years [19] to 11.74 years [20], with a cumulative failure rate of 28%. Root fracture in post core crown teeth in these studies was associated with primary crown retained partial dentures (removable) within the first 5 years [20]. In another study, the annual failure rates of CPC and glass fiber posts were 1.2% and 1.7%, respectively, with the authors concluding that both post systems performed well [21]. The most common failures were, listed from higher to lower prevalence, bonding failure (37%), apical lesions (37%), and crown dislodgement (11%), with a root fracture being only 3% of total failures [22]. Root fracture and root perforation have been reported to be more associated with removal of an intra-canal post [23] than routine functioning. Other recognized failures associated with post cores include secondary caries, periodontitis, cement failure, metal corrosion, post fracture, and post distortion [21,23]. Studies have reported no significant differences between prefabricated and cast post in terms of survival rates [15,24], although factors like crown type, bone attachment, patient age, and material have shown significant influences on survival time [19,20]. Clinically and biomechanically, CPCs offer several advantages over prefabricated posts, including higher rotation resistance [12], better retrievability [15,20], superior success [21], superior and maximum canal adaptation [12,15,21,25], conservative (minimum dentin removal) [26], and passive fit [27], and can be prepared on any canal configuration [10,13,16,21]. Ideally, the post must retain the core without undesirable stress and must have several ideal properties, such as high tensile strength, high resistance to fatigue, and ability to distribute forces, and must be biocompatible and esthetic [28]. Factors that influence post retention include the post itself (length, shape, design, diameter, surface characteristic), cement type, and endodontic sealer [29,30]. The disagreement between authors is primarily on the timing of post space preparation after completion of endodontic obturation and its effect on post retention [30,31]. A specific structural design feature known as ‘ferrule’, which encapsulates restored tooth providing a collar effect (1–2 mm sound tooth preparation) enhances stability and increases survival rate (5–10%) [32].
Advances in digital dentistry have brought a wide range of new materials and techniques in relation to both prefabricated and CPC systems and luting agents. Traditionally, the various materials that have been used for posts include alloys (eg, gold, titanium, base metal) [10], ceramics (eg, zirconium oxide) [12,22], and composites (eg, glass fiber-reinforced) [12,29]. The materials have been customized using traditional techniques like casting [12,21], computer-aided diagnosis, computer-assisted machining (CADCAM) [33–35], and 3D printing [33,36]. Milled posts have been reported to have better accuracy of fit than CPC in terms of feasibility of impression-taking [37]. However, Hendi et al [38] reported that CPC had better retention than half and full digitally fabricated milled post cores (mean force CPC – 171.6 N, half digital – 91.8 N). Modern alloys containing base metal nickel and chromium have also been reported to cause less post bending, which enhances stress distribution to the roots [39]. There have also been advances in luting agents, and with the introduction of adhesive cements many of the drawbacks of various post systems have been either eliminated or minimized. Earlier studies reported higher retention of CPCs with zinc phosphate [40] and glass ionomer cements [41]. CPC retention was also found to be higher with resin cements (Panavia F) using ultrasonic decementation [42]. Currently, there are a vast range of both adhesive and non-adhesive cements that are available to a dental practitioner that are indicated for either CPC or prefabricated posts (metal-, zirconia-, fiber-reinforced). Resin cements provide additional advantages of being insoluble in fluids and have superior mechanical strength [43]. Within adhesive systems, there are cements that are self-adhesive and do no require tooth etching. However, they are also technique-sensitive and result in development of secondary caries, besides having restricted working time and polymerization sensitivity [44]. Some of these drawbacks have been overcome by resin-modified glass ionomer cements, which have the combined advantages and properties of glass ionomer and resin cement. Amelia et al [45] compared glass ionomer with self-adhesive resin cement but did not find any significant differences in the tensile bond strength of the CPC. Hesarkhani et al [46] found highest retention with resin cement (Panavia SA) as compared to zinc phosphate and glass ionomer. Other studies on CPC retention using zinc phosphate and glass ionomer cement showed significantly higher retention with zinc phosphate cements [47]. Hybrid cements like resin-modified glass ionomer have been compared to zinc phosphate and glass ionomer cement for CPC retention and were found to have significantly higher mean retentive strengths (310.9 N) [48]. Selection of a luting agent can also be based whether it is for short- or long-term use, and certain cements are better for long-term use [49].
The cement retention of CPC is difficult to determine in the oral cavity, so traditional methods of evaluating cement retention have been used in vitro studies. The samples are cemented on extracted teeth that are prepared to simulate endodontically-treated teeth, after which they are thermocycled to represent oral conditions. Retentive strength is then tested using tensile tests. Our investigation of the literature found that the retentive strength of hybrid cement has not been compared with the resin and polycarboxylate cement, which would elucidate the properties of luting agents and improve clinicians’ choices regarding luting options for CPC. Therefore, this study aimed to evaluate the retentive strength of cast post core restorations in 50 endodontically-treated single-rooted mandibular second premolars using 5 common luting (cement) agents. The objective of the study was to determine which cements are currently able to provide the minimum required retentive strength for cast post cores. Assessing differences in retentive strength would also improve understanding of the cement strength of cast post cores. We hypothesized that retentive strengths vary between different cements, the basis of which is their ingredients. Alternately, the null hypothesis was that there is no difference in retention between various cements.
Material and Methods
ETHICS:
This research was a part of the postgraduate program and was approved by the college and university ethics committee (university registration number SVSUSDCH/Staff-E000204-Pr). All materials used in this study are regulated and approved by the Central Drugs Standard Control Organisation (CDSCO) (Ministry of Health, India).
STUDY DESIGN:
This in vitro experimental study followed the comparative approach and was conducted in different stages. The primary stage involved designing of the post and core samples, while the secondary stage involved cementation in the cast post and testing of the specimens.
OPERATIONAL DEFINITIONS:
“CPC post” was operationally defined as a single-piece foundation restoration comprising post that fits within a previously endodontically-treated tooth of a root canal, while the core is the portion of the CPC that replaced the missing coronal tooth structure and would allow tooth preparation for retention and supporting the crown [50]. “Luting agent” was operationally defined as a material used to cement the desired indirect restoration (in this case, CPC) to prepare post space within the root canal of the natural tooth. The term “retention” was defined as the ability of CPC to resist dislodgment in the vertical direction or along the path of placement [50]. The term “failure stress” was defined as the bond failure at an interface between 2 materials because of tensile force. Higher failure stress contextually indicates specimens failed at higher stress, while lower failure stress indicates a specimen failing at lower tensile stress. This term was specifically denoted as adhesion failure and is used interchangeably here [51].
SAMPLE SIZE ESTIMATION: The guide for the sample size was taken from earlier studies [46,47], which was verified by determination of sample size using G power software (V3.1.9.7; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany). An effect size of 0.7 with alpha error probability of 0.05 and power of 0.90 yielded a total sample size of 11 for each group (actual power of 0.911) [52]. Five specimens were kept as supplementary to replace specimens that had an error during fabrication or testing.
SAMPLE SELECTION AND PREPARATION: A comprehensive list of various materials and instruments used in the study is presented in Table 1. All experimental procedures were conducted on extracted single-rooted mandibular second premolar human teeth (Figure 1A). The inclusion/exclusion criteria included no evidence of decay/caries/restoration extending apically, adequate root length (minimum mean length 15±1 mm) and diameter, uniform diametrically, no evidence of root surface cracks/fracture/other continuity breaches, and no history of endodontic treatment. Fifty-five similar natural teeth meeting these criteria were cleaned of debris and then chemically sterilized in 5.25% sodium hypochlorite, and then were stored in diluted formalin solution (10%) for 1 day before storing them in saline [53]. Light microscope (10×) magnification ruled out surface cracks and crazing. All teeth were also radiographed to exclude those with extra canals, internal resorption, calcifications, or any abnormal anatomical aberration. A line was marked on the surface of the tooth from labial to lingual cemento-enamel junction traversing the proximal surfaces on each side to guide the axis of decoronation. The teeth were then decoronated at 1 mm above the cemento-enamel junction, using a disc (Carborundum) (Dentorium, New York, NY, USA) on a high-speed handpiece with coolant (compressed air/distilled water), leaving the root length of 15 mm (10 mm for post and 5 mm for apical seal).
ROOT CANAL FILLING:
After extirpation of the dead pulp (barbed broach [Dentsply, Switzerland]) and cleaning of the root canal. Patency of each canal was determined using conventional endodontic files (#10K) followed by determination of canal length. The working length of endodontic treatment was standardized for all specimens using rubber stops. A jig fixed to the work table helped to align each tooth vertically, with any discrepancy between the tooth and the jig filled by laboratory putty-consistency elastomer (Reprosil, Dentsply/Caulk; USA). Biomechanical endodontic root canal preparation was accomplished by using NiTi (nickel titanium) rotary files (ProTaper next, Dentsply-Maillefer) attached to the corresponding endo-motor (contra angle, Endo-Mate DT, Japan). The preparation was standardized by keeping a constant torque (200 gcm), speed (300 rpm), irrigating solution (5.25% sodium hypochlorite) (Chloraxid, Poland), distilled water rinsing, and paper points (Pro Taper next size X3) (Dentsply-Maillefer) drying. For all teeth, the smear layer from within the root canal was accomplished using a 17% ethylene diamine tetra-acetic acid (EDTA, PD, Vevey, Switzerland). A standard clinical procedure for biomechanical preparation was followed for instrumentation until Pro Taper next file size X3. Obturation of the canals was standardized by filling with gutta percha (Meta Biomed; South Korea) and root canal sealer (AD; Meta Biomed; South Korea) with thermal (cold) lateral compaction technique. Once obturation was completed, the canal orifice was sealed with a temporary restoration (light cure; Temp. It, Korea), which prevented seepage of setting sealer. All samples were then stored at 37°C with 100% relative humidity for 2 weeks.
CAST POST CORE PREPARATION/CEMENTATION: The temporary restoration over the canal orifice was dismantled with a round (initial penetration) and straight fissure bur (bulk) in a high-speed air rotor handpiece under air/water coolant. The visible gutta percha was then pierced through with a Gates Glidden drill (Dentsply-Maillefer, Ballaigues, Vallorbe, Switzerland) used from size #1 to #5 to remove the gutta percha using a slow-speed contra-angled handpiece. The post space was then prepared using a Pesso reamer (size 1 to 5) (Dentsply-Maillefer, Ballaigues, Vallorbe, Switzerland) up to the root canal length of 10 mm. The diameter of the post space was standardized by preparing each post up to size 4 of the Pesso reamer, followed by final enlargement by size 5 up to 10 rotations at the minimum speed of the control box. The canals were then cleaned by rinsing with a syringe containing distilled water. A ferrule 2 mm high and 2 mm wide was kept at the coronal end by preparing the tooth using a high-speed round bur. Another standard feature incorporated was anti-rotational groove towards the cervical portion of the post space preparation using a tapered bur. For all specimens, the posts and cores were fabricated by direct technique using autopolymerizing resin (Duralay; Reliance, Dental Mfg. Co., USA). Layers of pattern resin were carried on the corrugated plastic pin provided by the manufacturer. The direct pattern within the canal was further extended by 1 mm from the height of the ferrule, after which it was further extended by 4 mm towards the coronal direction (Figure 1B, 1C). A loop was prepared extending 2 mm above the canal orifice to assist in engaging the key during testing. The entire pattern was provided with a sprue so that it could be cast directly without any addition of material (Figure 1C). After completing the pattern, the roots were filled with dry sterile cotton within the canal while the orifice was sealed temporarily until post fabrication and testing. All patterns were then invested using a phosphate-bonded investment (Bellasun, Bego, Bremer Goldschlägerei Wilh Herbst GmbH & Co) manipulated according to the manufacturer’s recommendations. All the specimens were cast using nickel-chromium alloy (Wiron 99, BEGO) in an induction casting machine. Once the investment material cooled, the CPCs were retrieved and the investment was cleaned from the casting using sandblasting (alumina 200 μm). The fit of the dowel in the respective root preparation was evaluated with light finger pressure. Verification of the fit was confirmed by evaluation of the margins at the cervical end. Castings that were not accurate in fit were rejected and the process repeated. The portion of the sprue inside the loop was cut off so that only the loop for testing would remain (Figure 1D). Each casting was then finished from the outside leaving the root canal portion untouched. Before cementation of CPC for each group, the root canals of each tooth were washed with triple-distilled water and dried with paper absorbent points. Cement manipulation was performed according to each individual cement manufacturer’s instruction using recommended instruments and parameters (mixing time, working time, excess removal) (Table 1). A load of 5 kg was applied during the setting of the cement until the dowel was stable. Wherever desired, the cement was carried into the canal using the clinically recommended Lentulo spiral (Mani Co., Tokyo, Japan). All cemented CPCs were thus divided into 5 groups: zinc phosphate (Gp ZP), glass ionomer (Gp GI), resin cement (Gp RC), polycarboxylate (Gp PC), and resin-bonded glass ionomer (Gp RGI). To simulate clinical conditions, the samples were then stored in an incubator (37°C, 100% humidity, 1 week duration).
MEASURES, DATA COLLECTION, EVALUATION, AND ANALYSIS: The specimens of each group were then placed in a hollow rectangular metal block (3/2/2 centimeter) (Figure 2A) as preparation for testing. A mixture of autopolymerizing acrylic resin was poured into these metal blocks leaving 5 mm of root exposed to the outside to hold the specimens during testing (Figure 2B). A cast surveyor was used to hold the exposed portion of the sprue and embed the specimens perpendicular to the base of the blocks to ensure that tensile loading occurred along the long axis of the root canal during testing (Figure 2C). After proper alignment of each CPC assembly, the clamp of the machine was placed into the loops of each sample. Positive contact of the loop with the machine was obtained with the help of locking pliers. The samples were finally tested (pilot test) by connecting the assembly to a calibrated universal testing machine (Instron, model 4511, Brucks, United Kingdom) using a crosshead speed of 1 mm/min until cement failure. The force required for cement failure or dislodgment of CPC was automatically recorded by the machine in kilograms.
STATISTICAL ANALYSIS:
Data obtained for individual specimens in each group were entered in Microsoft Excel, where it was refined, cleaned, and then coded to be analyzed using SPSS (Chicago, IL, USA, V25.0). For each specimen within each group, the mean values and standard deviations were calculated. Differences between the groups were determined using one-way analysis of variance (ANOVA) with the
Results
RETENTIVE STRENGTH:
The mean force (tensile) that caused an adhesive failure between CPC restoration and the root canal surface within the natural tooth is presented in Table 2 along with the overall differences between various investigated groups. CPCs specimens in Gp RGI showed the highest forces (m=21.46) required to dislodge the CPC restoration, indicating that CPC cemented with resin cement is more retentive than other cements. The lowest forces to dislodge CPCs were observed in Gp PC (m=13.63), indicating that the lowest retention for CPC to tooth was with polycarboxylate cement.
GROUP DIFFERENCES:
A statistically significant difference in the mean adhesive failure values existed between different cement groups (P≤0.05) (Table 2). A multiple-group comparison of adhesive failure between CPC and natural root surface between different groups is presented in Table 3 and graphically depicted in Figure 3. The differences between the groups were statistically determined at 2 different levels – (significant (P≤0.05) and highly significant (P≤0.01) – to differentiate the levels of differences between 2 different cements. No difference in means was observed in groups cemented with zinc phosphate and glass ionomer, although both had higher retentive values than polycarboxylate cement. Significant differences were observed in 2 group comparisons (Gp ZP vs Gp PC and Gp PC vs Gp GI) (P≤0.05), while all other group differences were highly significant (Figure 3).
Discussion
STRENGTH AND LIMITATIONS OF THE STUDY:
The main strength of the study includes investigating a wide variety of chemically different luting agents that are commonly used for cementation of CPC. The limitation of the study is related to in vitro design which cannot be the exact replica of a clinical situation. The influence of periodontal ligament to bear some of the tensile force is also lacking in such studies. There are also many manufacturers of a particular cement which have not been included in this study. In vivo bonding failure occurs in different clinical conditions which are difficult to replicate in laboratory studies. A CPC may undergo bonding failure after serving for a long period of time during which the influence of other variables plays a role. Our study replicated that condition for only a week which may be considered less of a CPC that serves 4 years.
Conclusions
We found that the cements investigated had wide variations in mean retentive strengths (range 13.63 to 21.46 kg), with resin cement showing the highest and polycarboxylate cement showing the lowest strengths. Significant differences in retentive strength of cements existed among these 5 cements for CPC cementation. These values may be considered sufficient for a CPC, although the issue of having a cutoff standard needs attention. Clinically, our results suggest that if for some reason the clinician feels that the endodontic treatment may require intervention in the future, then polycarboxylate cement should be used for CPC cementation. For long-term, trouble-free cementation, resin cement shows higher retentive strengths, but other factors must be weighed to determine its feasibility.
Figures
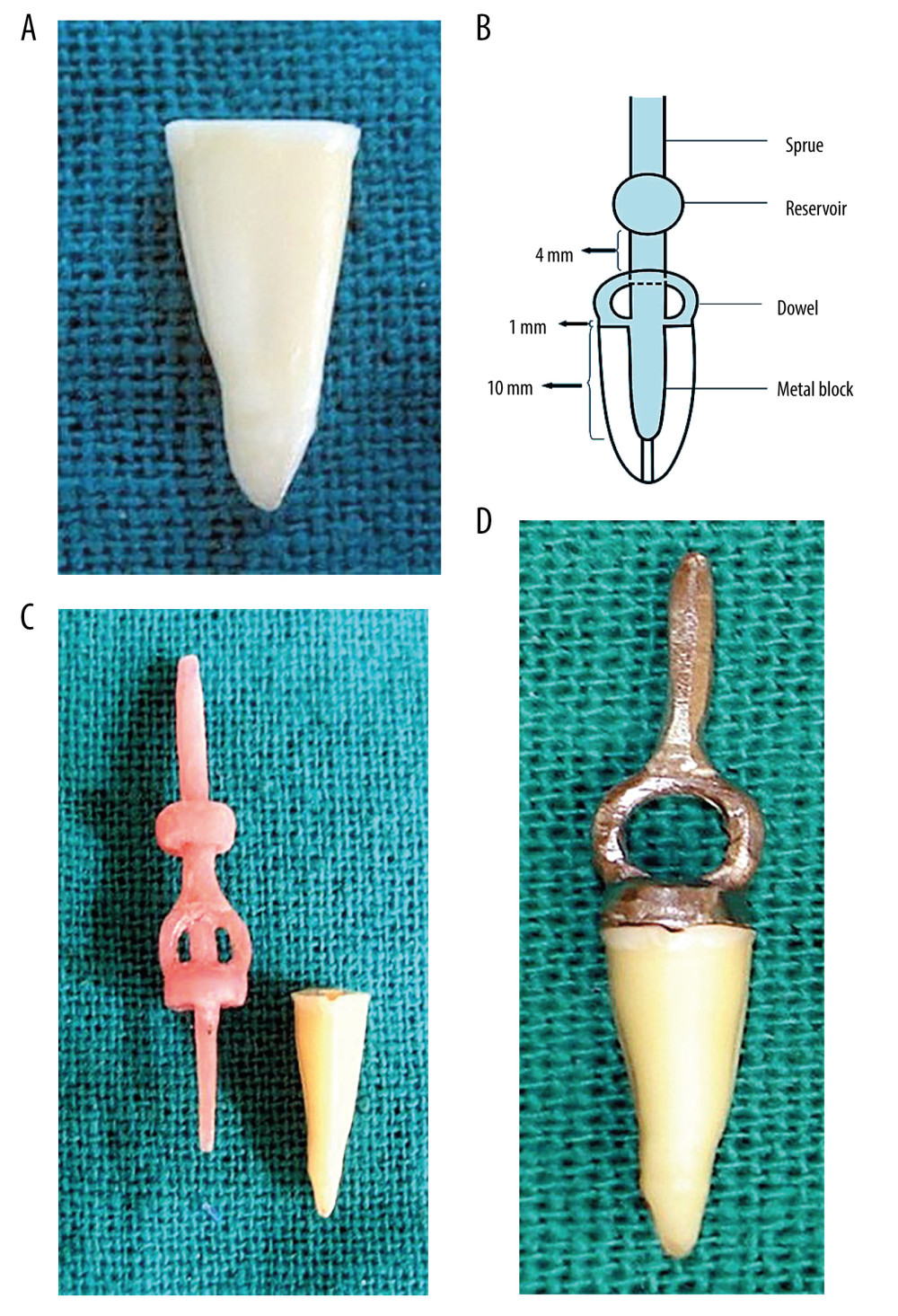 Figure 1. (A) Extracted mandibular second premolar after decoronation. (B) Schematic diagram showing the design of the cast post core and its various dimensions relative to the length of the root. (C) Prepared pattern for cast post core against the back drop of its specimen. (D) Raw cast post core seated on the extracted tooth showing marginal adaptation. Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft corporation).
Figure 1. (A) Extracted mandibular second premolar after decoronation. (B) Schematic diagram showing the design of the cast post core and its various dimensions relative to the length of the root. (C) Prepared pattern for cast post core against the back drop of its specimen. (D) Raw cast post core seated on the extracted tooth showing marginal adaptation. Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft corporation). 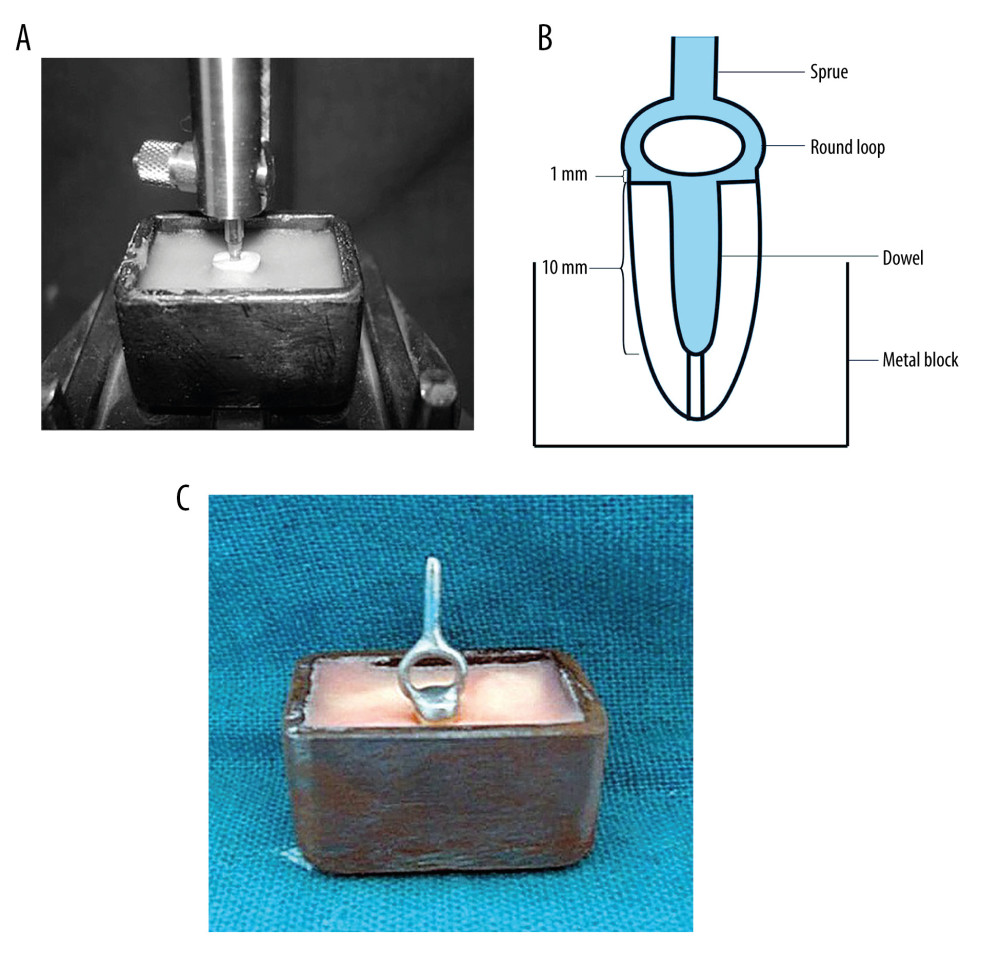 Figure 2. (A) Dental cast surveyor holding the specimen within the customized mold for testing. (B) Schematic diagram showing the design of the customized testing apparatus. (C) Final specimen with cemented cast post core before testing. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100-mm macro lens) with/without ring flash. Figure edited and labelled using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 2. (A) Dental cast surveyor holding the specimen within the customized mold for testing. (B) Schematic diagram showing the design of the customized testing apparatus. (C) Final specimen with cemented cast post core before testing. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100-mm macro lens) with/without ring flash. Figure edited and labelled using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation). 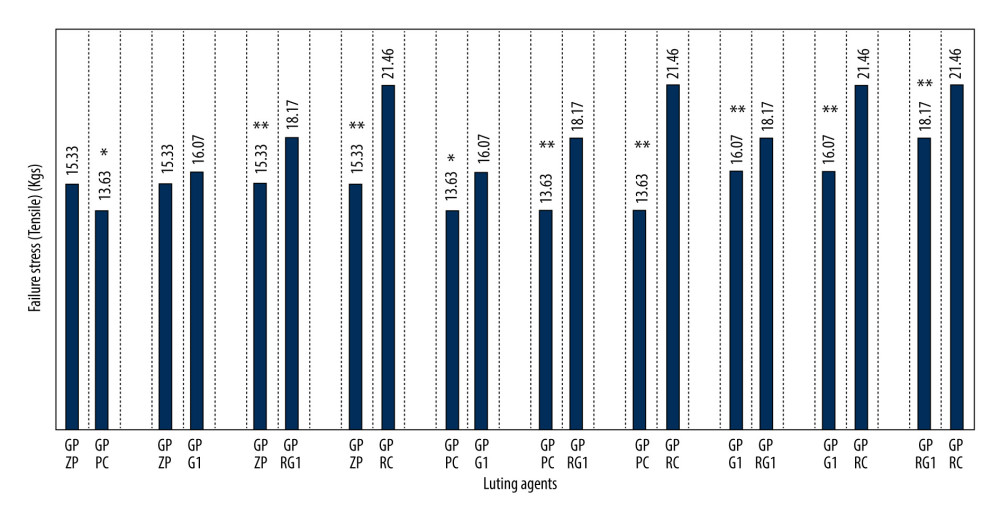 Figure 3. Graphic presentation of comparative differences in mean adhesive failure stresses between cast post and natural root using different luting agents (pairwise comparison). Figure created using MS Excel sheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft corporation).
Figure 3. Graphic presentation of comparative differences in mean adhesive failure stresses between cast post and natural root using different luting agents (pairwise comparison). Figure created using MS Excel sheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft corporation). Tables
Table 1. Comprehensive list of experimental materials.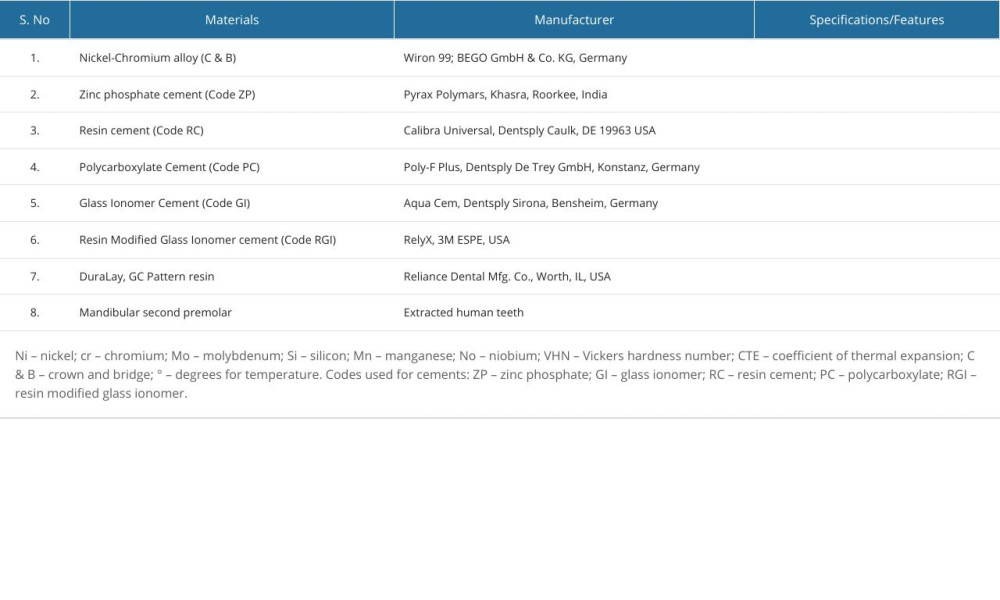 Table 2. Comparative differences in mean values and one-way ANOVA results for adhesive failure stress obtained for different luting agents between cast post and natural tooth.
Table 2. Comparative differences in mean values and one-way ANOVA results for adhesive failure stress obtained for different luting agents between cast post and natural tooth.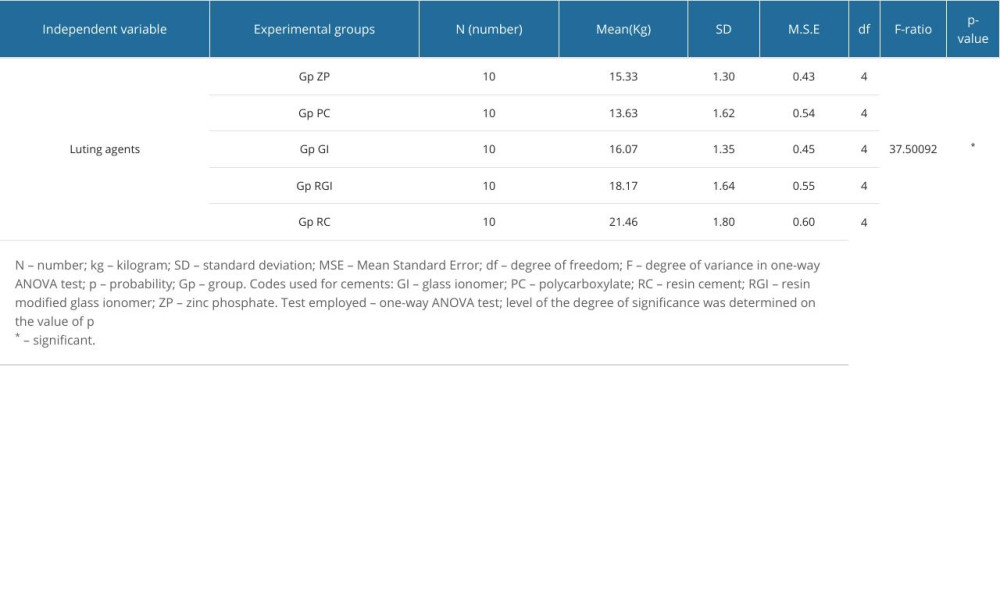 Table 3. Pairwise intergroup comparison (post hoc) of adhesive failure stress between cast post and various luting agents showing differences between various groups.
Table 3. Pairwise intergroup comparison (post hoc) of adhesive failure stress between cast post and various luting agents showing differences between various groups.
References
1. Smith CT, Schuman NJ, Wasson W, Biomechanical criteria for evaluating prefabricated post-and-core systems: A guide for the restorative dentist: Quintessence Int, 1998; 29(5); 305-12
2. Smith CT, Schuman N, Prefabricated post-and-core systems: An overview: Compend Contin Educ Dent, 1998; 19(10); 1013-20
3. Marcos RM, Kinder GR, Alfredo E, Influence of the resin cement thickness on the push-out bond strength of glass fiber posts: Braz Dent J, 2016; 27(5); 592-98
4. Barcelos LM, Bicalho AA, Veríssimo C, Stress distribution, tooth remaining strain, and fracture resistance of endodontically treated molars restored without or with one or two fiberglass posts and direct composite resin: Oper Dent, 2017; 42(6); 646-57
5. Mannocci F, Cowie J, Restoration of endodontically treated teeth: Br Dent J, 2014; 216(6); 341-46
6. Ariki EK, Gonçalves MC, Souza ROA, Influence of different luting protocols on the bond strength of fiber posts to root dentin: Pesq Bras Odontoped Clin Integr, 2013; 13(3); 265-71
7. Alharbi FA, Nathanson D, Morgano S, Baba NZ, Fracture resistance and failure mode of fatigued endodontically treated teeth restored with fiber reinforced resin posts and metallic posts in vitro: Dent Traumatol, 2014; 30(4); 317-25
8. Faria ACL, Rodrigues RCS, Antunes RPA, Endodontically treated teeth: Characteristics and considerations to restore them: J Prosthodont Res, 2011; 55(2); 69-74
9. Cheveux N, Sharrock PJ, Mechanical properties of glass fiber-reinforced endodontic posts: Acta Biomaterials, 2009; 5(8); 3224-30
10. Dietschi D, Duc O, Krejci I, Sadan A, Biomechanical considerations for the restoration of endodontically treated teeth: A systematic review of the literature, Part II (Evaluation of fatigue behavior, interfaces, and in vivo studies): Quint Int, 2008; 39(2); 117-29
11. Rayyan MR, Roa’a AA, Alsadun SF, Hijazy FR, Accuracy of cast posts fabricated by the direct and the indirect techniques: J Prosthet Dent, 2016; 116(3); 411-15
12. Prado M, Kohl J, Nogueira R, Geraldo-Martins V, Post and core systems: A literature review: J Heal Sci, 2014; 16(1); 51-56
13. Maroli A, Hoelcher KAL, Reginato VF, Biomechanical behavior of teeth without remaining coronal structure restored with different post designs and materials: Mater Sci Eng C, 2017; 76; 839-44
14. Tiwari A, Sethuraman R, Patel V, Computer-aided design computer-aided manufacturing fabricated polyetherether ketone post, and core restoration: Int J Oral Care Res, 2018; 5(1); S101-5
15. Sarkis-Onofre R, de Castilho Jacinto R, Cast metal vs. glass fibre posts: A randomized controlled trial with up to 3 years of follow up: J Dent, 2014; 42(5); 582-87
16. Giok KC, Veettil SK, Menon RK, Comparative effectiveness of fiber and metal posts in the restoration of endodontically treated teeth: A systematic review with network meta-analysis: J Prosthet Dent, 2023 [Online ahead of print]
17. Jurema AL, Filgueiras AT, Santos KA, Effect of intraradicular fiber post on the fracture resistance of endodontically treated and restored anterior teeth: A systematic review and meta-analysis: J Prosthet Dent, 2022; 128(1); 13-24
18. Gaeta C, Malvicini G, Mignosa E, Influence of methodological variables on fracture strength test results of intact premolars: An ex-vivo study: Med Res Arch, 2023; 11(9); 146
19. Vogler JA, Lehmann M, Rehmann P, Wöstmann B, Survival time of post and cores: A 16 year retrospective follow-up study: J Dent, 2022; 117; 103923
20. Vogler JA, Stummer AL, Walther KA, Survival of teeth treated with post and core-A retrospective study of more than 1000 cases with observation periods up to 18 years: J Dent, 2023; 138; 104723
21. Sarkis-Onofre R, Amaral Pinheiro H, Poletto-Neto V, Randomized controlled trial comparing glass fiber posts and cast metal posts: J Dent, 2020; 96; 103334
22. Rasimick BJ, Wan J, Musikant BL, Deutsch AS, A review of failure modes in teeth restored with adhesively luted endodontic dowels: J Prosthodont, 2010; 19(8); 639-46
23. Dixon EB, Kaczkowski PJ, Nicholls JI, Harrington GW, Comparison of two ultrasonic instruments for post removal: J Endod, 2002; 28(2); 111-15
24. Cloet E, Debels E, Naert I, Controlled clinical trial on the outcome of glass fiber composite cores versus wrought posts and cast cores for the restoration of endodontically treated teeth: A 5-year follow-up study: Int J Prosthodont, 2017; 30(1); 71-79
25. Goto Y, Nicholls JI, Phillips KM, Junge T, Fatigue resistance of endodontically treated teeth restored with three dowel-and-core systems: J Prosthet Dent, 2005; 93(1); 45-50
26. Rosenstiel SF, Land MF, Walter R: Contemporary fixed prosthodontics-e-book, 2022; 22, Elsevier Health Sciences
27. Schmage P, Özcan M, McMullan-Vogel C, Nergiz I, The fit of tapered posts in root canals luted with zinc phosphate cement: A histological study: Dent Mater, 2005; 21(9); 787-93
28. Thakur A, Ramarao S, A comparative evaluation of fracture resistance of endodontically treated premolar teeth reinforced with different prefabricated and custom-made fiber-reinforced post system with two different post lengths: An in vitro study: J Conserv Dent, 2019; 22(4); 376-82
29. Pranati T, Ranjan M, Sandeep AH, Marginal adaptability of custom made cast post made by different techniques – a literature review: Int J Dentistry Oral Sci, 2021; 8(8); 3954-59
30. dos Reis-Prado AH, Abreu LG, Tavares WL, Comparison between immediate and delayed post space preparations: A systematic review and meta-analysis: Clin Oral Invest, 2021; 25; 417-40
31. Marchiulynaite-Ustiliene R, Trisiniene J, Skucaite N, Microcomputed tomography evaluation of contamination with endodontic obturation material remnants in teeth with different root canal anatomy after post space preparation: J Prosthet Dent, 2021; 125(6); 900-4
32. Fokkinga WA, Kreulen CM, Bronkhorst EM, Creugers NH, Up to 17-year controlled clinical study on post-and-cores and covering crowns: J Dent, 2007; 35(10); 778-86
33. Al-Qarni FD, Customized post and cores fabricated with CAD/CAM technology: A literature review: Int J Gen Med, 2022; 15; 4771-79
34. Lee JH, Fabricating a custom zirconia post-and-core without a post-and-core pattern or a scan post: J Prosthet Dent, 2018; 120(2); 186-89
35. Pang J, Feng C, Zhu X, Fracture behaviors of maxillary central incisors with flared root canals restored with CAD/CAM integrated glass fiber post-and-core: Dent Mater, 2019; 38(1); 114-19
36. Piangsuk T, Dawson DV, El Kerdani T, Lindquist TJ, The accuracy of post and core fabricated with digital technology: J Prosthodont, 2023; 32(3); 221-26
37. Vogler JA, Billen L, Walther KA, Wöstmann B, Conventional cast vs. CAD/CAM post and core in a fully digital chairside workflow – an in vivo comparative study of accuracy of fit and feasibility of impression taking: J Dent, 2023; 136; 104638
38. Hendi AR, Moharrami M, Siadat H, The effect of conventional, half-digital, and full-digital fabrication techniques on the retention and apical gap of post and core restorations: J Prosthet Dent, 2019; 121(2); 364-e1
39. Khaledi AAR, Sheykhian S, Khodaei S, Evaluation of retention of two different cast post-core systems and fracture resistance of the restored teeth: J Dent (Shiraz), 2015; 16(2); 121-28
40. Duncan JP, Pameijer CH, Retention of parallel sided titanium posts cemented with six luting agents. An in vitro study: J Prosthet Dent, 1998; 80(4); 423-28
41. Gavranovic-Glamoc A, Redzepagic S, Ajanovic M, Comparing the retention of cast posts cemented with three different kinds of cement: Pesquisa Brasileira em Odontopediatria e Clínica Integrada, 2010; 10(1); 41-45
42. Garrido ÂDB, Fonseca TS, Alfredo E, Influence of ultrasound, with and without water spray cooling, on removal of posts cemented with resin or zinc phosphate cements: J Endod, 2004; 30(3); 173-76
43. Pontes EC, Soares DG, Hebling J, Costa CA, Cytotoxicity of resin-based luting cements to pulp cells: Am J Dent, 2014; 27(5); 237-44
44. da Silva DC, Vaz LG, Tavares WL, Cytotoxicity of two self-adhesive resin cements and their interference in the phagocytic activity of murine macrophages: Rest Dent Endodon, 2022; 47(3); 1-9
45. Amelia J, Firman D, Damayanti L, Tensile bond strength of customized cast post and core cemented with two luting agent: SONDE, 2022; 7(2); 1-7
46. Hesarkhani A, Fotovat F, Saneian F, Retention of cast posts cemented with two commonly used conventional and two resin cements and the mode of root fracture following their removal: Front Dent, 2021; 18; 37
47. Al Omari WM, Zagibeh AM, The retention of cast metal dowels fabricated by direct and indirect techniques: J Prosthodont, 2010; 19(1); 58-63
48. Choudhary S, Begum Z, Choudhary P, Tripathi S, Comparative evaluation of retention of prefabricated and conventional cast post: An in vitro study: J Int Soc Prev Community Dent, 2014; 4(2); 87-91
49. Heboyan A, Vardanyan A, Karobari MI, Dental luting cements: An updated comprehensive review: Molecules, 2023; 28(4); 1619
50. , The glossary of prosthodontic terms: J Prosthet Dent, 2005; 94; 10-92
51. Ferro KJ, Morgano SM, Driscoll CF: The glossary of prosthodontic terms, 2017
52. Faggion CM, Guidelines for reporting pre-clinical in vitro studies on dental materials: J Evid Based Dent Pract, 2012; 12(4); 182-89
53. Sandhu SV, Tiwari R, Bhullar RK, Sterilization of extracted human teeth: A comparative analysis: J Oral Biol Craniofac Res, 2012; 2(3); 170-75
54. Vojdani M, Shaghaghian S, Khaledi A, Adibi S, The effect of thermal and mechanical cycling on bond strength of a ceramic to nickel-chromium (Ni-Cr) and cobalt-chromium (Co-Cr) alloys: Ind J Dent Res, 2012; 23(4); 509-13
55. Yadav L, Mattoo KA, Kapoor A, Shuja S, Factors associated with post core correction of malpositioned teeth: Int J Res Med Sci Technol, 2015; 1(2); 5-7
56. Muneera RAG, Mattoo KA, Youseef AM, A novel approach to determine the aesthetic inclination of cast post core-case report: Ann Int Med Dent Res, 2017; 3(6); DE14-17
57. Fakiha Z, Al-Aujan A, Al-Shamrani S, Retention of cast posts cemented with zinc phosphate cement using different cementing techniques: J Prosthodont, 2001; 10; 37-41
58. Radke RA, Barkhordar RA, Podesta RE, Retention of cast endodontic posts: Comparison of cementing agents: J Prosthet Dent, 1988; 59(3); 318-20
59. Sahafi A, Benetti AR, Flury S, Peutzfeldt A, Retention of root canal posts: Effect of cement film thickness, luting cement, and post pretreatment: Oper Dent, 2015; 40(4); E149-57
60. Habib B, von Fraunhofer JA, Driscoll CF, Comparison of two luting agents used for the retention of cast dowel and cores: J Prosthodont, 2005; 14(3); 164-69
61. Ertugrul HZ, Ismail YH, An in vitro comparison of cast metal dowel retention using various luting agents and tensile loading: J Prosthet Dent, 2005; 93(5); 446-52
62. Leung GK, Wong AW, Chu CH, Yu OY, Update on dental luting materials: Dent J, 2022; 10(11); 208
63. Burgess JO, Ghuman T, Cakir D, Self adhesive resin cements: J Esthet Restor Dent, 2010; 22(6); 412-19
64. Da Rosa WL, Piva E, da Silva AF, Bond strength of universal adhesives: A systematic review and meta-analysis: J Dent, 2015; 43(7); 765-76
65. Amin F, Fareed MA, Zafar MS, Degradation and stabilization of resin-dentine interfaces in polymeric dental adhesives: An updated review: Coatings, 2022; 12(8); 1094
66. Monticelli F, Ferrari M, Toledano M, Cement system and surface treatment selection for fiber post luting: Med Oral Pathol Oral Cir Bucal, 2008; 13; E214-21
67. Menani LR, Ribeiro RF, Antunes RP, Tensile bond strength of cast commercially pure titanium and cast gold alloy posts and cores cemented with two luting agents: J Prosthet Dent, 2008; 99(2); 141-47
68. Yılmaz CB, Yanıkoğlu N, Farklı post sistemlerinin tutuculuğunda yapıģtırma simanlarının etkisinin ġncelenmesi: Atatürk Üniv DiĢ Hek Fak Derg, 2020; 30(2); 267-73 [in Turkish]
69. Mattoo KA, Kapoor A, Sivach A, Selecting the right cement for cast post core crowns – a dental students quandary: JMSCR, 2014; 2(9); 2323-27
70. Lakshya K, Aditya K, Mattoo KA, Full mouth rehabilitation involving multiple cast post core as foundation restorations – case report: Int J Res Pharm Sci, 2018; 5(7); 11-15
71. Johnson GH, Lepe X, Zhang H, Wataha JC, Retention of metal-ceramic crowns with contemporary dental cements: J Am Dent Assoc, 2009; 140(9); 1125-36
72. Ergin S, Gemalmaz D, Retentive properties of five different luting cements on base and noble metal copings: J Prosthet Dent, 2002; 88(5); 491-97
73. Cheylan JM, Gonthier S, Degrange M, In vitro push-out strength of seven luting agents to dentin: Int J Prosthodont, 2002; 15(4); 365-70
74. Alghamdi NS, Alamoudi RA, Baba SM, A scanning electron microscopy study comparing 3 obturation techniques to seal dentin to root canal bioceramic sealer in 30 freshly extracted mandibular second premolars: Med Sci Monit, 2023; 29; e940599
75. Al Shawkani HA, Mattoo K, Ali FM, Effect of two different experimental mixing ratios on selective physical, antibacterial and tissue compatibility properties of two commonly used endodontic root canal sealers – an in-vitro and in-vivo study: J Biomater Tissue Eng, 2022; 12(10); 2092-99
76. Malhotra S, Bhullar KK, Kaur S, Comparative evaluation of compressive strength and flexural strength of gc gold hybrid, gic conventional and resin-modified glass-ionomer cement: J Pharm Bioallied Sci, 2022; 14(Suppl 1); S214
77. Mickenautsch S, Tyas MJ, Yengopal V, Absence of carious lesions at margins of glass-ionomer cement (GIC) and resin-modified GIC restorations: A systematic review: Eur J Prosthodont Restor Dent, 2010; 18(3); 139-45
Figures
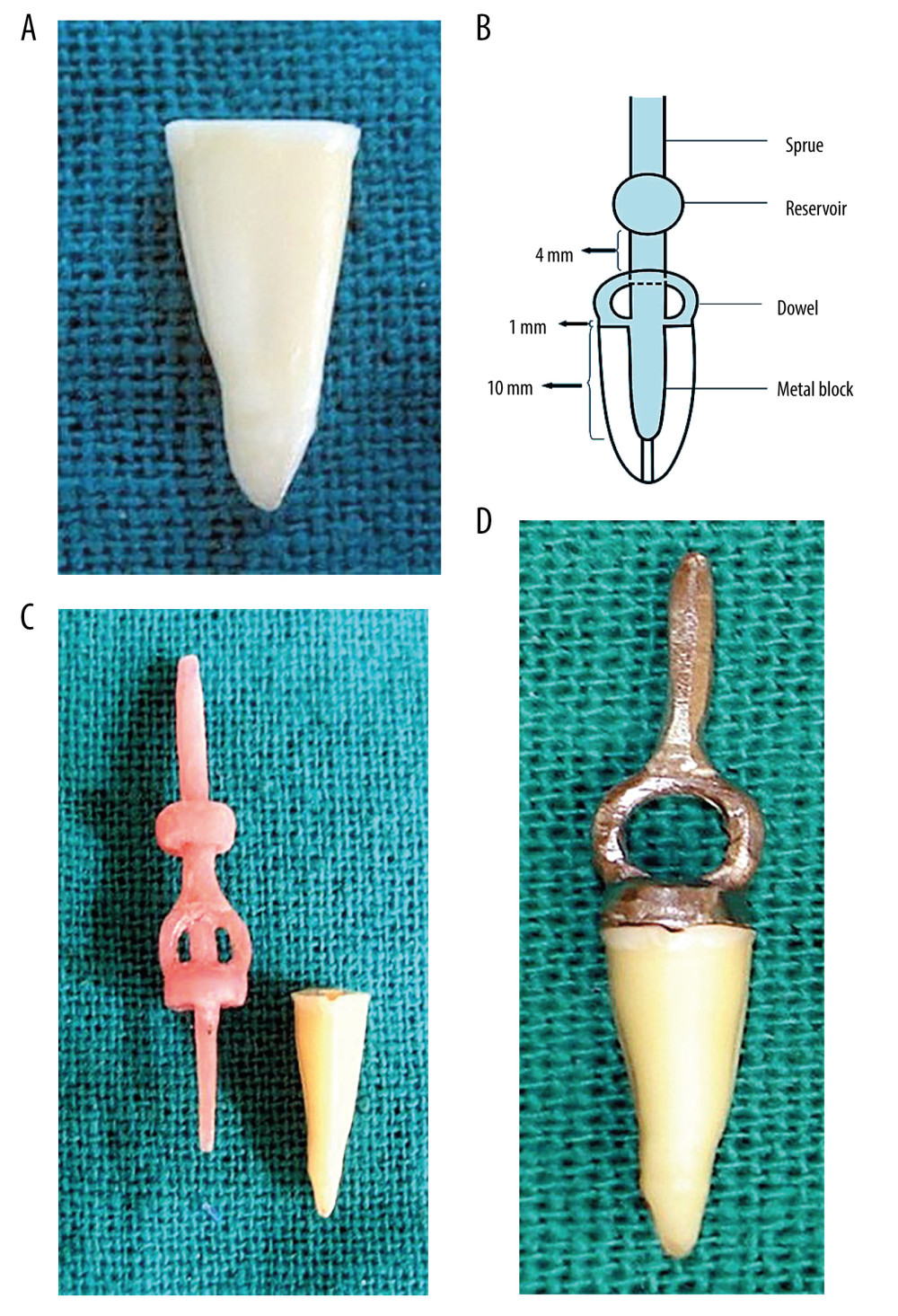 Figure 1. (A) Extracted mandibular second premolar after decoronation. (B) Schematic diagram showing the design of the cast post core and its various dimensions relative to the length of the root. (C) Prepared pattern for cast post core against the back drop of its specimen. (D) Raw cast post core seated on the extracted tooth showing marginal adaptation. Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft corporation).
Figure 1. (A) Extracted mandibular second premolar after decoronation. (B) Schematic diagram showing the design of the cast post core and its various dimensions relative to the length of the root. (C) Prepared pattern for cast post core against the back drop of its specimen. (D) Raw cast post core seated on the extracted tooth showing marginal adaptation. Photographs taken using digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. Figure created using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft corporation).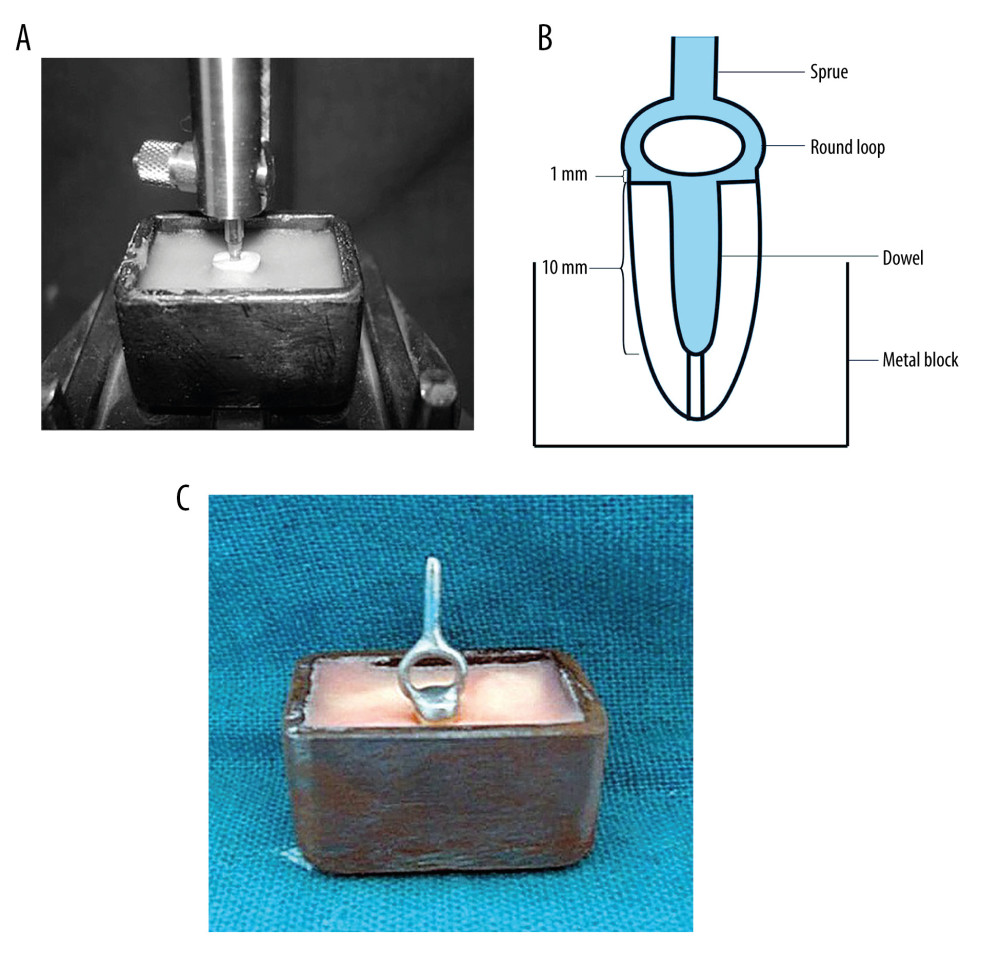 Figure 2. (A) Dental cast surveyor holding the specimen within the customized mold for testing. (B) Schematic diagram showing the design of the customized testing apparatus. (C) Final specimen with cemented cast post core before testing. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100-mm macro lens) with/without ring flash. Figure edited and labelled using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).
Figure 2. (A) Dental cast surveyor holding the specimen within the customized mold for testing. (B) Schematic diagram showing the design of the customized testing apparatus. (C) Final specimen with cemented cast post core before testing. Photographs taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100-mm macro lens) with/without ring flash. Figure edited and labelled using MS PowerPoint, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft Corporation).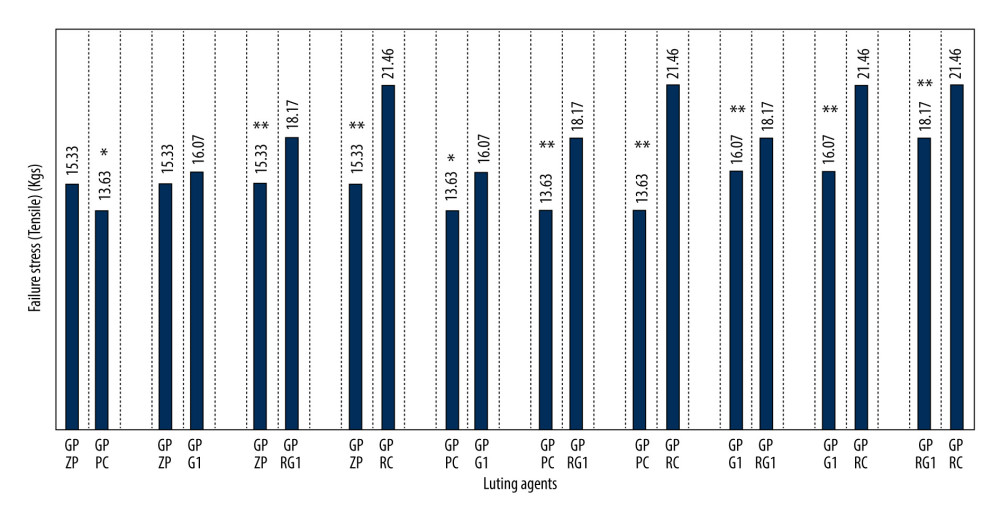 Figure 3. Graphic presentation of comparative differences in mean adhesive failure stresses between cast post and natural root using different luting agents (pairwise comparison). Figure created using MS Excel sheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft corporation).
Figure 3. Graphic presentation of comparative differences in mean adhesive failure stresses between cast post and natural root using different luting agents (pairwise comparison). Figure created using MS Excel sheet, version 20H2 (OS build 19042,1466), Windows 11 Pro, Microsoft corporation). Tables
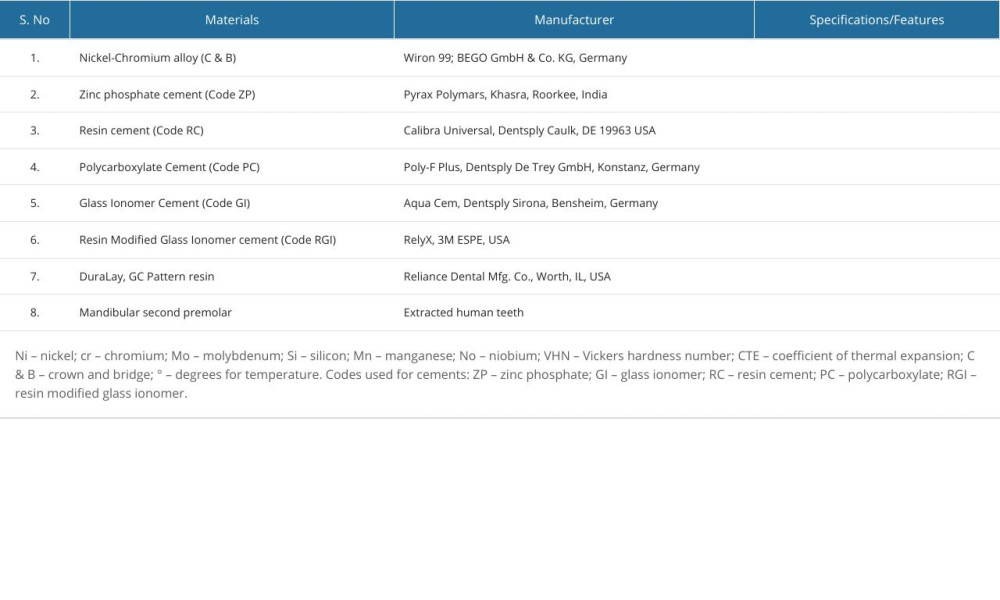 Table 1. Comprehensive list of experimental materials.
Table 1. Comprehensive list of experimental materials.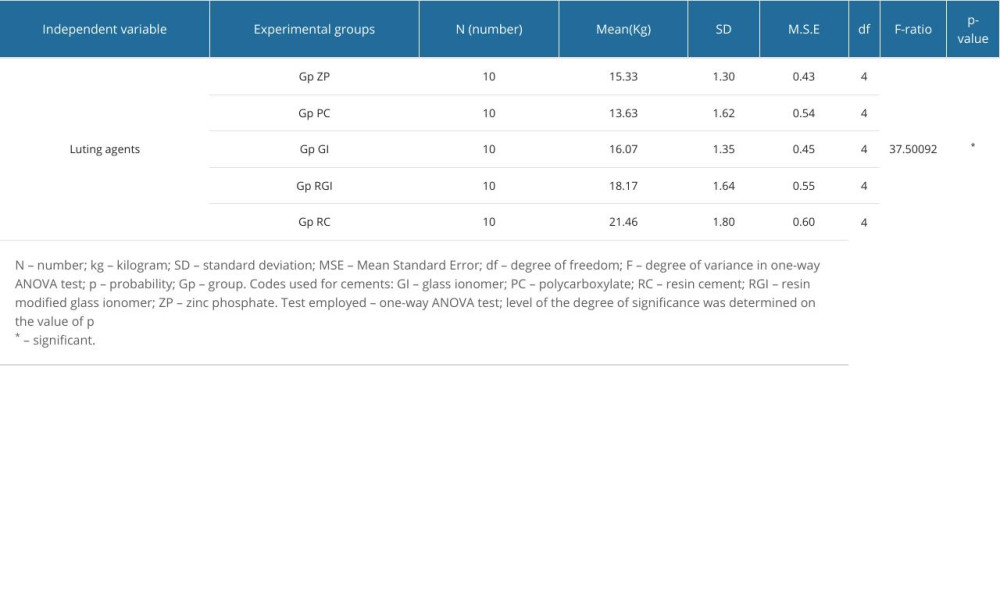 Table 2. Comparative differences in mean values and one-way ANOVA results for adhesive failure stress obtained for different luting agents between cast post and natural tooth.
Table 2. Comparative differences in mean values and one-way ANOVA results for adhesive failure stress obtained for different luting agents between cast post and natural tooth. Table 3. Pairwise intergroup comparison (post hoc) of adhesive failure stress between cast post and various luting agents showing differences between various groups.
Table 3. Pairwise intergroup comparison (post hoc) of adhesive failure stress between cast post and various luting agents showing differences between various groups.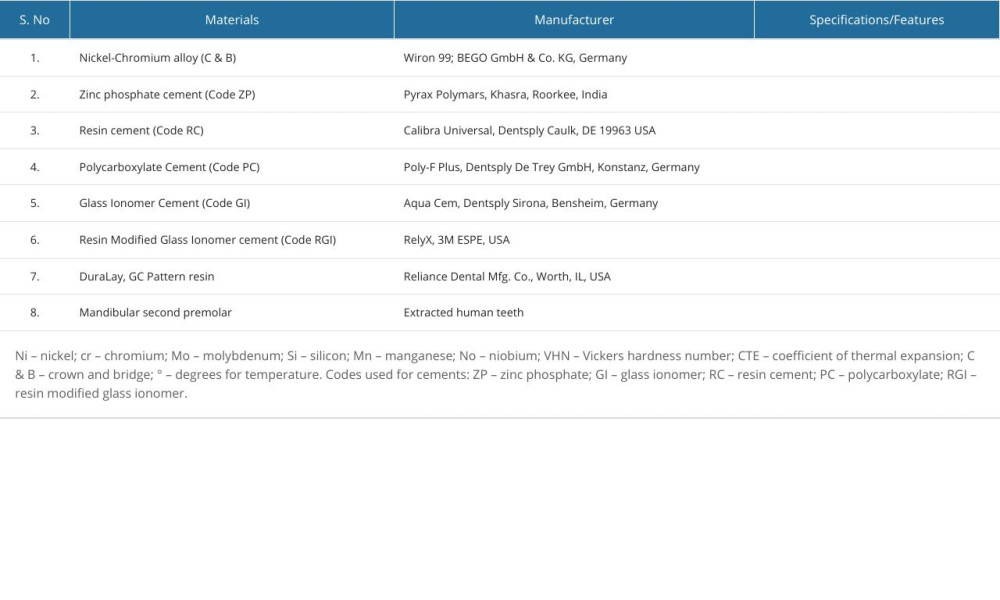 Table 1. Comprehensive list of experimental materials.
Table 1. Comprehensive list of experimental materials.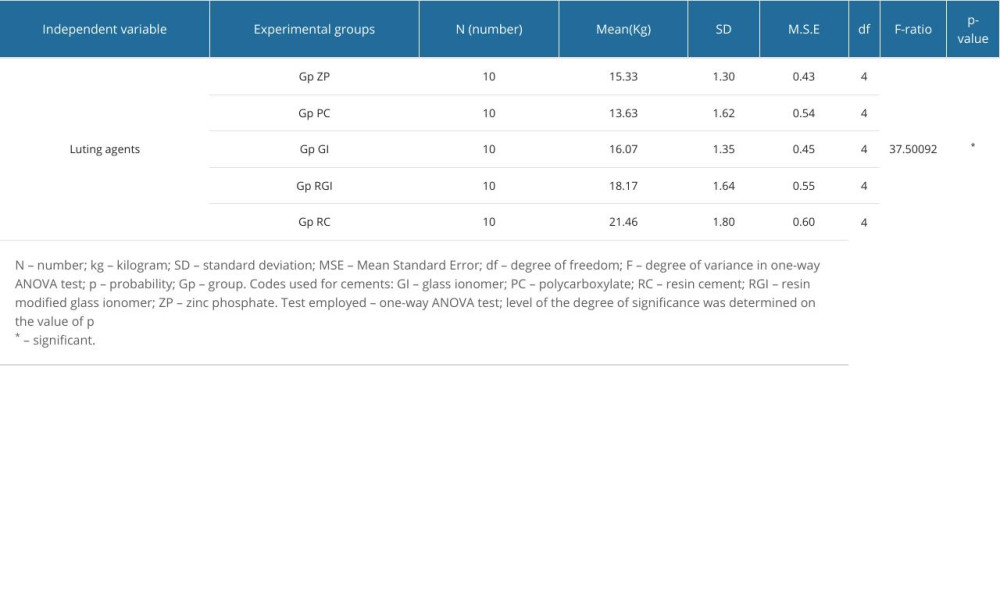 Table 2. Comparative differences in mean values and one-way ANOVA results for adhesive failure stress obtained for different luting agents between cast post and natural tooth.
Table 2. Comparative differences in mean values and one-way ANOVA results for adhesive failure stress obtained for different luting agents between cast post and natural tooth. Table 3. Pairwise intergroup comparison (post hoc) of adhesive failure stress between cast post and various luting agents showing differences between various groups.
Table 3. Pairwise intergroup comparison (post hoc) of adhesive failure stress between cast post and various luting agents showing differences between various groups. In Press
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
12 Mar 2024 : Clinical Research
Metabolomic Alterations in Methotrexate Treatment of Moderate-to-Severe PsoriasisMed Sci Monit In Press; DOI: 10.12659/MSM.943360
14 Mar 2024 : Clinical Research
Renal Dysfunction Increases Risk of Adverse Cardiovascular Events in 5-Year Follow-Up Study of Intermediate...Med Sci Monit In Press; DOI: 10.12659/MSM.943956
15 Mar 2024 : Clinical Research
Impact of One-Lung Ventilation on Oxygenation and Ventilation Time in Thoracoscopic Heart Surgery: A Compar...Med Sci Monit In Press; DOI: 10.12659/MSM.943089
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








