24 September 2020: Clinical Research
Correlations Between Hip Extension Range of Motion, Hip Extension Asymmetry, and Compensatory Lumbar Movement in Patients with Nonspecific Chronic Low Back Pain
Won-deuk Kim1ABCDEF, DooChul Shin2ADEG*DOI: 10.12659/MSM.925080
Med Sci Monit 2020; 26:e925080
Abstract
BACKGROUND: This study aimed to confirm the correlations among hip extension range of motion, hip extension asymmetry, pain intensity, disability index, and compensatory lumbar movement in patients with nonspecific chronic low back pain.
MATERIAL AND METHODS: Of 66 patients with nonspecific chronic low back pain and limited hip extension, 59 met the inclusion criteria and were enrolled in the study. Pain intensity, Oswestry Disability Index (ODI), hip range of motion, compensatory lumbar extension, and compensatory lumbar rotation of the subjects were assessed. Pain was measured using a numeric pain rating scale (NPRS), and hip extension range of motion and compensatory lumbar movement were evaluated using a digital dual inclinometer (Dualar IQ, JTech Medical, United States). Correlation analysis was used to analyze the data.
RESULTS: A strong correlation was observed among hip extension asymmetry, pain intensity, and disability index (P<0.05). However, no correlation was observed among compensatory lumbar rotation and extension, pain intensity, and ODI. A strong correlation also was observed between limited hip extension range of motion and compensatory lumbar rotation (P<0.05) but not between limited hip extension range of motion and compensatory lumbar extension (P>0.05).
CONCLUSIONS: The results of this study showed that hip extension asymmetry might be a more critical factor than hip extension range of motion. The strong correlation between limited hip extension and compensatory lumbar rotation suggests a risk of micro-trauma due to compensatory lumbar rotation.
Keywords: Hip Joint, Low Back Pain, Range of Motion, Articular, chronic pain, Lumbar Vertebrae
Background
Nonspecific chronic back pain refers to a condition in which pain arising in the lower back without pathological abnormality continues for more than 90 days [1]. Most people experience nonspecific back pain more than once in their lifetime [2]. A recent systematic review reported an estimated 1-year incidence of back pain ranging from 1.5% to 36% and an estimated initial incidence ranging from 6.3% to 15.3% [3]. Walker et al. reported a 1-year prevalence of back pain of 22–65% and lifetime prevalence of 11–84% [4]. Chronic back pain also increases with age [5]. Approximately 90–95% of cases of low back pain are nonspecific [6].
Nonspecific low back pain can occur without severe medical or psychological symptoms and signs. Mobility impairment of the chest, lumbar spine, and sacroiliac joint; lower-extremity radiating pain, and general pain also can occur [7]. Characteristic symptoms of nonspecific chronic low back pain include enhanced symptoms due to repeated movement or sustained posture, mobility defects in the trunk and lumbopelvic and hip joint, and reduced muscle strength and endurance of the trunk or pelvis. Furthermore, leisure- and job-related activities are also restricted due to impaired motor coordination [8–10]. Fear also plays an important role in persisting pain in individuals with nonspecific chronic low back pain [11]. Psychosocial problems such as distress and depression are also important contributing factors during the transition from acute to chronic pain [12].
Because the hip joint and lumbar spine are adjacent to the pelvis, they exhibit coordinated movement. However, limited hip joint mobility is a risk factor that causes pain by changing mechanical forces and causing excessive stress [2,13]. Studies of low back pain have focused on low back anatomy, biomechanics, and motor control, or dysfunction of the trunk and spine itself, without considering the contributions of adjacent joints to low back pain [14,15].
The hip joint is considered a latent cause of and contributing factor to low back pain; mobility impairment of the hips is related to low back pain [16–19]. Limitation of hip mobility can lead to excessive compensatory movement of the lumbar spine [20]. In addition, people with back pain have more limited range of motion in the hip joint and larger asymmetry than those without low back pain [21,22]. Prior studies, however, only described limitation of hip mobility and consequent pain patterns and movements in individuals with nonspecific chronic low back pain. Knowledge remains limited about the relationship between hip joint characteristics, pain intensity, disability index, and compensatory lumbar movement. In addition, most studies have studied only 1 hip joint range of motion; thus, correlations of degree of pain, disability index, and compensatory lumbar movement with hip joint asymmetry have not yet been elucidated.
Therefore, this study assessed correlations among hip joint mobility, hip extension asymmetry, pain intensity, disability index, compensatory lumbar movement, and hip extension limitation in patients with nonspecific chronic back pain.
Material and Methods
SUBJECTS:
This study included individuals with low back pain who visited the J General Welfare Center Physical Therapy Clinic in Changwon, Kyungnam, Korea.
Inclusion criteria were: 1) diagnosis of nonspecific back pain in patients over 50 and under 70 years of age; 2) experience of at least 6 weeks of back pain in the last 12 weeks; and 3) low back pain and limited hip joint range of motion.
Exclusion criteria were: 1) malignant tumor; 2) spinal infection or fracture; 3) history of waist bone, abdomen, pelvis, and hip joint surgery; 4) cauda equine syndrome; 5) neurological symptoms such as pain radiating from the lower extremities; 6) abdominal and systemic inflammatory diseases; and 7) other serious conditions leading to mobility problems.
Sixty-six subjects were initially selected. Seven of them were excluded based on the criteria previous described; therefore, 59 subjects were enrolled in the study. Three subjects were excluded due to radiating lower-extremity pain, one due to vertebral fracture, and 3 due to a history of hip surgery. All subjects were provided full explanations of the study procedure and purpose and provided written informed consent. All research protocols were approved by the Kyungnam University Research Ethics Committee.
PROCEDURE:
The range of motion in the left and the right hip joints of the enrolled patients were assessed and differences between them in each patient were calculated. Compensatory lumbar extension and compensatory lumbar rotation were measured during hip extension with subjects in the prone position. The pain intensity and disability index of the subjects were assessed using a questionnaire. Hip extension range of motion, compensatory lumbar extension, and compensatory lumbar rotation were measured 3 times and the average value was used (Figure 1).
HIP EXTENSION RANGE OF MOTION:
A modified Thomas test was used to measure the hip extension range of motion using a digital inclinometer (Dualar IQ, JTech Medical, USA). The subjects rested freely on a bed with the lower leg out of the bed and free. The examiner bent the subjects’ knees and hips so that the subjects’ waists were flat on the bed. One leg maintained this position and the pelvis was tilted posteriorly about 10 degrees while keeping the knees and hips bent. The adduction and abduction angles of the hip were maintained at 0 degrees and the legs were slowly dropped to the floor. The angle between the femoral centerline and bed was measured (Figure 2). This study used the average of 3 measurements. The tester reliability (intraclass correlation [ICC]) was 0.70–0.89 [23]), while the test-retest reliability was ICC=0.87–0.91 [24].
HIP EXTENSION ASYMMETRY:
Hip extension asymmetry was evaluated by calculating the difference between the left and right hip ranges of motion.
PAIN INTENSITY:
Pain was evaluated using a numeric pain rating scale (NPRS) ranging from pain-free (0 points) to extreme pain (10 points). The numerical value of the scale indicated the overall pain intensity. The test-retest reliability was ICC=0.61–0.77 and the validity was ICC=0.85 [25].
DISABILITY INDEX:
The disability index was measured using the Oswestry disability index (ODI), a tool commonly used to identify perceived disorders in patients with back pain [26,27]. The ODI evaluates 10 parameters, 8 and 2 of which are related to daily life activities and pain, respectively. Each parameter is graded from 0 to 5, with the total score translated to percentages. The higher the score, the higher the ODI. Of the 10 parameters, questions related to sexual life were considered unsuitable to Korean culture; thus, this study used a revised scale with 9 items. The intra-evaluator reliability of this test was ICC=0.84 and the test-retest reliability was ICC=0.9167 [28].
COMPENSATORY LUMBAR MOVEMENT:
To assess compensatory lumbar movement, compensatory lumbar extension and rotation movements during hip joint extension motion were measured with the subjects in a prone position. Compensatory lumbar extension and rotation were evaluated using a digital dual inclinometer (Dualar IQ, JTech Medical, United States). The degree of lumbar extension and rotation within 10 degrees of hip joint motion were measured with the subjects in the prone position. The position of the hip joint was set using a smartphone goniometer app (G-Pro, 5FUF5 Co., United States). If a subject’s hip joint reached 10 degrees, the evaluator stopped the subject’s hip joint motion by verbal instruction. To measure compensatory lumbar extension and rotation, the subjects were placed in a prone position, at the center of the thoracic spine and posterior superior iliac spine, and allowed 10 degrees of active hip joint extension, and the tilt of the inclinometer was evaluated (Figures 3, 4). The average value after 3 measurements was used.
STATISTICAL ANALYSIS:
SPSS 21.0 was used to perform statistical analyses. All data were tested for normality by Kolmogorov-Smirnov tests. Spearman correlation coefficients were used to analyze correlations among limited hip extension, hip extension asymmetry, pain, ODI, compensatory lumbar extension, and compensatory lumbar rotation. The significance level (α) was set at P≤0.05.
Results
Of 59 recruited subjects, 24 were male (39%) and 36 were female (61%). Mean age, height, and weight were 63.03 years, 161.25 cm, and 67.26 kg, respectively (Table 1).
Normality tests of all measured variables showed non-normal distributions. Therefore, Spearman correlation coefficient nonparametric statistical tests were used.
Patients’ hip extension was limited to 27.93 degrees on the left and 24.10 degrees on the right. The difference between the left and right extension ranges of the hip joint was 5.03 degrees. The pain intensity was 4.54 points and the disability index was 18.75%. Compensatory lumbar extensions were 18.49 and 15.35 degrees on the left and right, respectively. Compensatory lumbar rotations were 5.93 and 3.49 degrees on the left and right, respectively (Table 2).
Table 3 shows the results of analysis of correlations among the degrees of limited hip extension, asymmetry, pain intensity, ODI, and compensatory lumbar extension and rotation. A strong correlation was observed between the degree of hip extension asymmetry, pain intensity, and disability index (P<0.05). A strong correlation was also observed between the limitation of the left hip joint extension and left compensatory lumbar rotation (P<0.05). The correlation between left hip extension limit and left compensatory movement of lumbar extension was not statistically significant (P>0.05). A strong correlation was also observed between right hip joint extension limitation and right compensatory lumbar rotational movement (P<0.05). No statistically significant correlation was observed between limited right hip joint extension and right compensatory lumbar extension (P>0.05).
Discussion
This study evaluated correlations among the degree of hip extension, degree of hip extension asymmetry, pain intensity, ODI, compensatory lumbar extension, and compensatory lumbar rotation in subjects with nonspecific chronic back pain.
The results of this study revealed a strong correlation between degree of asymmetry of hip extension and pain intensity, and ODI. Furthermore, we also observed a strong correlation between the degree of hip mobility and compensatory lumbar rotational movement, but the correlation between hip extension range of motion and compensatory lumbar extension movement was not statistically significant.
Patients with nonspecific chronic low back pain exhibited less hip extension mobility than that in healthy people. In addition, compensatory rotation of the lumbar spine occurred during hip movement [21,29].
The results of this study showed that the greater the degree of motion in the hip joint extension, the greater the compensatory lumbar spine movement. The hip and lumbar spine exhibit coordinated movement because they both are adjacent to the pelvis. Hence, restricting hip joint mobility could lead to excessive stress in the lumbopelvic region [2,13]. Therefore, these results suggest that restricted motion of hip extension markedly affected compensatory rotational movement of the lumbar spine and could lead to excessive stress in the lumbar region.
Patients with low back pain often exhibit asymmetric hip mobility [30]. Results of this study also show that the greater the asymmetry of the hip extension, the higher the pain intensity and disability index, and the greater the hip extension asymmetry, the greater the compensatory rotational movement of the lumbar spine during activities requiring hip extension. Increased lumbar spine rotation can cause excessive compensatory lumbopelvic region movement and induce increased mechanical stress, leading to back pain [20,31].
The results of this study also demonstrate increased compensatory lumbar rotation with increased limitation of hip joint extension. This finding indicates an association between pain intensity and ODI that affected trunk-pelvic coordination, induced mechanical stress, and overloaded the lumbar spine.
Contrary to our hypothesis, the correlation between the degree of hip extension and the extension of the lumbar spine was not statistically significant. These results showed that patients exhibited reduced flexibility of the muscles around the lumbar spine due to chronic back pain. In addition, with increased hamstring muscle activity, hip joint extension in the prone position was assumed to induce the posterior pelvis tilt, which restricted movement during lumbar extension.
Horment et al. analyzed surface electromyography during hip extension in the prone position in patients with low back pain and reported a significant reduction in erector spine muscle activities on the same and the opposite sides, as well as in the gluteus maximus muscle [32].
Arab et al. reported higher muscle hamstring muscle activity in individuals with back pain compared to those without low back pain during hip joint extension in the prone position [33].
The patients in this study had nonspecific chronic low back pain and limited hip extensor mobility. We observed a strong correlation between limitations in hip extension and compensatory lumbar rotation, as well as among hip extension asymmetry, pain intensity, and disability index. The results may have been a consequence of mechanical stress and micro-trauma to the lumbar region due to compensatory lumbar rotation during activities that required hip extension. Moreover, because patients enrolled in this study had experienced back pain for more than 6 of the past 12 weeks, we assumed a greater degree of hip asymmetry, which led to high pain intensity and ODI scores.
This study has several limitations. First, because the age of the patients was set limited to 50 to 70 years, our data cannot be generalized to all ages. Second, because a digital inclinometer was used as the measuring instrument, it was possible to measure only the angle at which the lumbar spine was tilted; hence, exact movement during hip joint extension could not be determined. Third, because measurements were obtained with subjects in the prone position, the data cannot be generalized to movement-related activities, such as walking and running.
The clinical relevance of this study is that limited hip joint extension strongly affects compensatory lumbar rotation and that the degree of asymmetry affects pain intensity and ODI score. These results can be used to inform more effective management of nonspecific chronic low back pain by improving hip joint extension flexibility and asymmetry amelioration.
Conclusions
This study investigated correlations among the degree of hip extension limitation, degree of hip asymmetry, pain intensity, ODI, compensatory lumbar extension, and compensatory lumbar rotation in patients with nonspecific chronic low back pain.
Strong correlations were observed among the degree of hip extension asymmetry, pain intensity, and ODI as well as between the degree of hip extension and compensatory lumbar rotation movement. The results indicate that improvement in extension flexibility of the hip joint and amelioration of asymmetry can contribute to more efficient management of nonspecific chronic back pain.
Figures
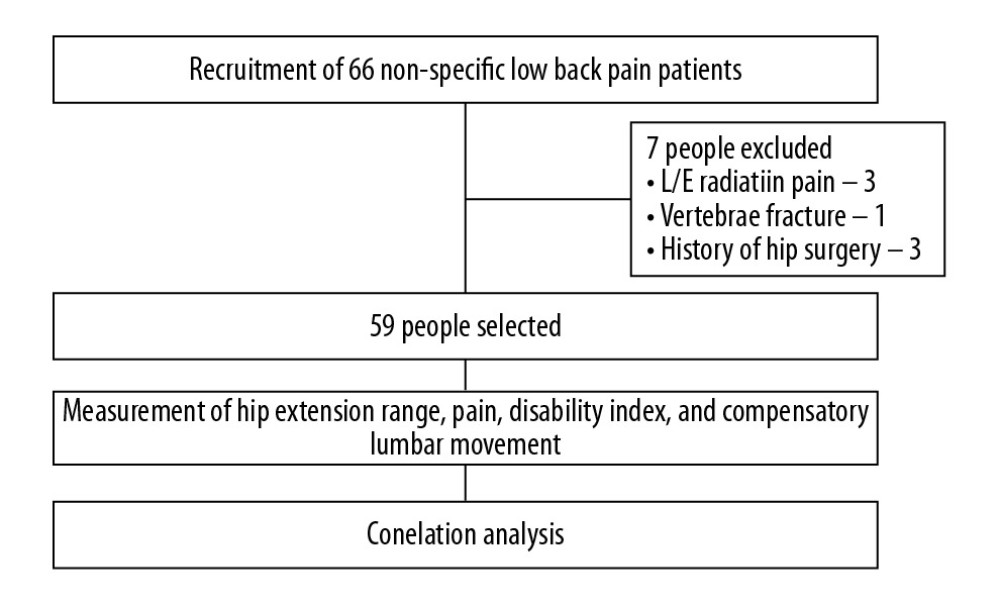 Figure 1. Research procedure.
Figure 1. Research procedure.  Figure 2. Hip joint extension range of motion as measured by digital dual inclinometer.
Figure 2. Hip joint extension range of motion as measured by digital dual inclinometer.  Figure 3. Compensatory lumbar extension as measured by digital dual inclinometer during hip joint extension with participants in the prone position.
Figure 3. Compensatory lumbar extension as measured by digital dual inclinometer during hip joint extension with participants in the prone position.  Figure 4. Compensatory lumbar rotation as measured by digital dual inclinometer during hip joint extension with participants in the prone position.
Figure 4. Compensatory lumbar rotation as measured by digital dual inclinometer during hip joint extension with participants in the prone position. References
1. Koes BW, van Tulder M, Lin CW, An updated overview of clinical guidelines for the management of non-specific low back pain in primary care: Eur Spine J, 2010; 19; 2075-94
2. Harris-Hayes M, Sahrmann SA, Van Dillen LR, Relationship between the hip and low back pain in athletes who participate in rotation-related sports: J Sport Rehabil, 2009; 18; 60-75
3. Hoy D, Brooks P, Blyth F, Buchbinder R, The epidemiology of low back pain: Best Pract Res Clin Rheumatol, 2010; 24; 769-81
4. Walker BF, The prevalence of low back pain: A systematic review of the literature from 1966 to 1998: J Spinal Disord, 2000; 13; 205-17
5. Meucci RD, Fassa AG, Faria NM, Prevalence of chronic low back pain: Systematic review: Rev Saude Publica, 2015; 49
6. Bardin LD, King P, Maher CG, Diagnostic triage for low back pain: A practical approach for primary care: Med J Aust, 2017; 206; 268-73
7. Delitto A, George SZ, Van Dillen L, Whitman JM, Low back pain: Clinical practice guidelines linked to the international classification of functioning, disability, and health from the Orthopaedic Section of the American Physical Therapy Association: J Orthopaedic Sports Physical Therapy, 2012; 42; A1-57
8. Currie SR, Wang J, Chronic back pain and major depression in the general Canadian population: Pain, 2004; 107; 54-60
9. Harris-Hayes M, Van Dillen LR, The inter-tester reliability of physical therapists classifying low back pain problems based on the movement system impairment classification system: PM R, 2009; 1; 117-26
10. Trudelle-Jackson E, Sarvaiya-Shah SA, Wang SS, Interrater reliability of a movement impairment-based classification system for lumbar spine syndromes in patients with chronic low back pain: J Orthop Sports Phys Ther, 2008; 38; 371-76
11. George SZ, Fritz JM, Childs JD, Investigation of elevated fear-avoidance beliefs for patients with low back pain: A secondary analysis involving patients enrolled in physical therapy clinical trials: J Orthop Sports Phys Ther, 2008; 38; 50-58
12. Pincus T, Burton AK, Vogel S, Field AP, A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain: Spine (Phila Pa 1976), 2002; 27; E109-20
13. Jo HJ, Song AY, Lee KJ, A kinematic analysis of relative stability of the lower extremities between subjects with and without chronic low back pain: Eur Spine J, 2011; 20; 1297-303
15. MacDonald D, Moseley GL, Hodges PW, People with recurrent low back pain respond differently to trunk loading despite remission from symptoms: Spine (Phila Pa 1976), 2010; 35; 818-24
16. Ben-Galim P, Ben-Galim T, Rand N, Hip-spine syndrome: The effect of total hip replacement surgery on low back pain in severe osteoarthritis of the hip: Spine (Phila Pa 1976), 2007; 32; 2099-102
17. Ellison JB, Rose SJ, Sahrmann SA, Patterns of hip rotation range of motion: A comparison between healthy subjects and patients with low back pain: Phys Ther, 1990; 70; 537-41
18. Reiman MP, Weisbach PC, Glynn PE, The hips influence on low back pain: A distal link to a proximal problem: J Sport Rehabil, 2009; 18; 24-32
19. Wong TK, Lee RY, Effects of low back pain on the relationship between the movements of the lumbar spine and hip: Hum Mov Sci, 2004; 23; 21-34
20. Van Dillen LR, Gombatto SP, Collins DR, Symmetry of timing of hip and lumbopelvic rotation motion in 2 different subgroups of people with low back pain: Arch Phys Med Rehabil, 2007; 88; 351-60
21. Roach SM, San Juan JG, Suprak DN, Passive hip range of motion is reduced in active subjects with chronic low back pain compared to controls: Int J Sports Phys Ther, 2015; 10; 13-20
22. Nagai T, Abt JP, Sell TC, Lumbar spine and hip flexibility and trunk strength in helicopter pilots with and without low back pain history: Work, 2015; 52; 715-22
23. Godges JJ, MacRae PG, Engelke KA, Effects of exercise on hip range of motion, trunk muscle performance, and gait economy: Phys Ther, 1993; 73; 468-77
24. Cejudo A, Sainz de Baranda P, Ayala F, Santonja F, Test-retest reliability of seven common clinical tests for assessing lower extremity muscle flexibility in futsal and handball players: Phys Ther Sport, 2015; 16; 107-13
25. Chiarotto A, Maxwell LJ, Ostelo RW, Measurement properties of visual analogue scale, numeric rating scale, and pain severity subscale of the brief pain inventory in patients with low back pain: A systematic review: J Pain, 2019; 20; 245-63
26. Fritz JM, Irrgang JJ, A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale: Phys Ther, 2001; 81; 776-88
27. Frost H, Lamb SE, Stewart-Brown S, Responsiveness of a patient specific outcome measure compared with the Oswestry Disability Index v2.1 and Roland and Morris Disability Questionnaire for patients with subacute and chronic low back pain: Spine (Phila Pa 1976), 2008; 33; 2450-57 discussion 2458
28. Kim DY, Lee SH, Lee HY, Validation of the Korean version of the oswestry disability index: Spine (Phila Pa 1976), 2005; 30; E123-27
29. Sadeghisani M, Sobhani V, Kouchaki E, Comparison of lumbopelvic and hip movement patterns during passive hip external rotation in two groups of low back pain patients with and without rotational demand activities: Ortop Traumatol Rehabil, 2015; 17; 611-18
30. Sadeghisani M, Manshadi FD, Kalantari KK, Correlation between hip rotation range-of-motion impairment and low back pain. A literature review: Ortop Traumatol Rehabil, 2015; 17; 455-62
31. Scholtes SA, Gombatto SP, Van Dillen LR, Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests: Clin Biomech (Bristol, Avon), 2009; 24; 7-12
32. Horment-Lara G, Cruz-Montecinos C, Nunez-Cortes R, Onset and maximum values of electromyographic amplitude during prone hip extension after neurodynamic technique in patients with lumbosciatic pain: A pilot study: J Bodyw Mov Ther, 2016; 20; 316-23
33. Arab AM, Ghamkhar L, Emami M, Nourbakhsh MR, Altered muscular activation during prone hip extension in women with and without low back pain: Chiropr Man Therap, 2011; 19; 18
Figures
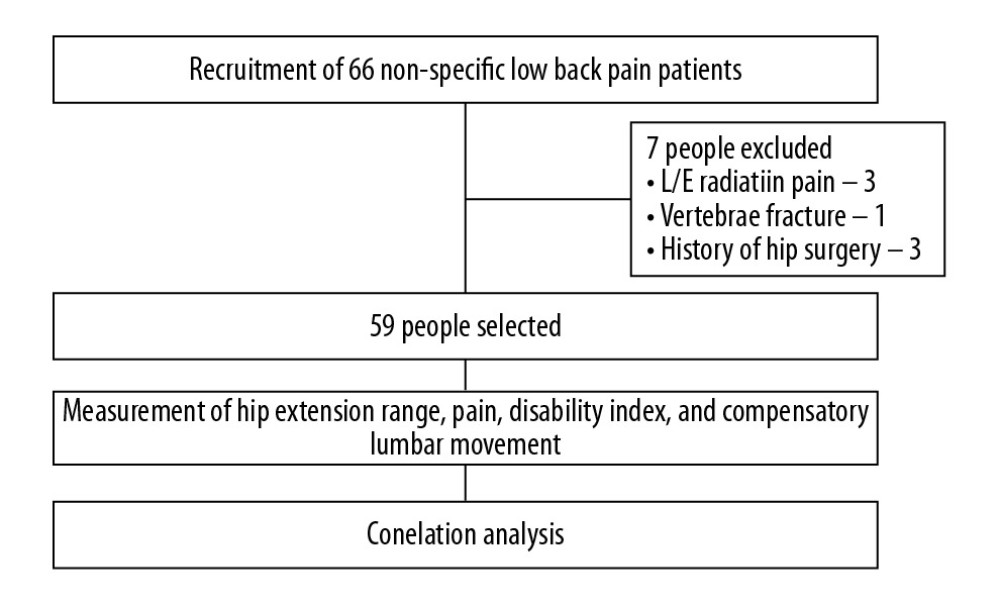 Figure 1. Research procedure.
Figure 1. Research procedure. Figure 2. Hip joint extension range of motion as measured by digital dual inclinometer.
Figure 2. Hip joint extension range of motion as measured by digital dual inclinometer. Figure 3. Compensatory lumbar extension as measured by digital dual inclinometer during hip joint extension with participants in the prone position.
Figure 3. Compensatory lumbar extension as measured by digital dual inclinometer during hip joint extension with participants in the prone position. Figure 4. Compensatory lumbar rotation as measured by digital dual inclinometer during hip joint extension with participants in the prone position.
Figure 4. Compensatory lumbar rotation as measured by digital dual inclinometer during hip joint extension with participants in the prone position. Tables
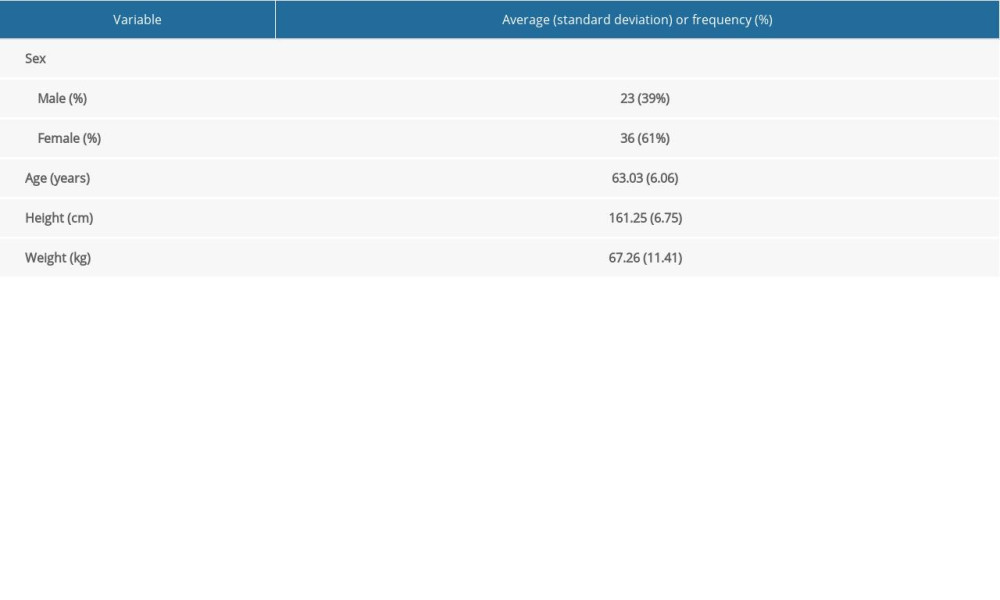 Table 1. General characteristics of study subjects.
Table 1. General characteristics of study subjects.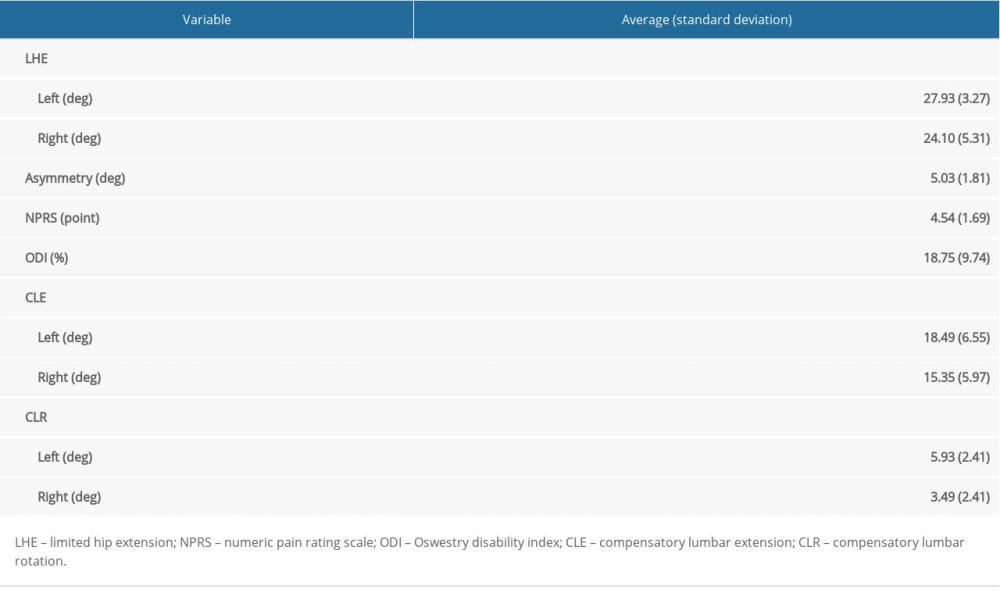 Table 2. Medical characteristics of study subjects.
Table 2. Medical characteristics of study subjects.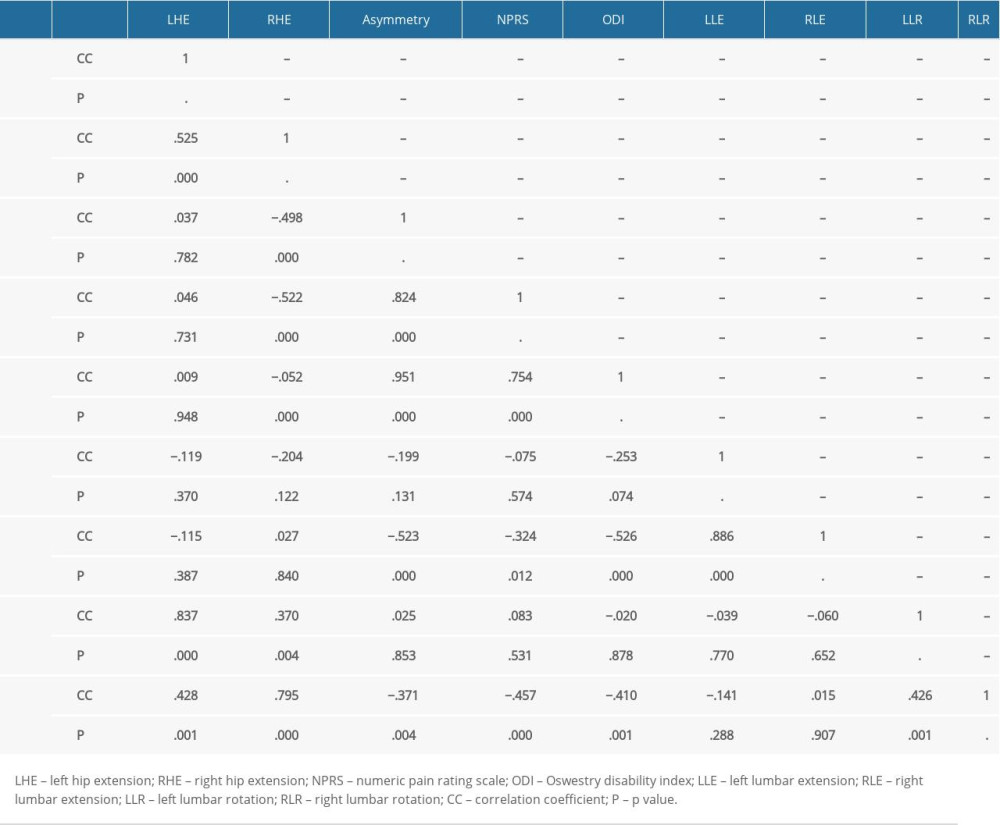 Table 3. Limited hip mobility, compensated lumbar extension, and compensatory lumbar rotation correlation.
Table 3. Limited hip mobility, compensated lumbar extension, and compensatory lumbar rotation correlation.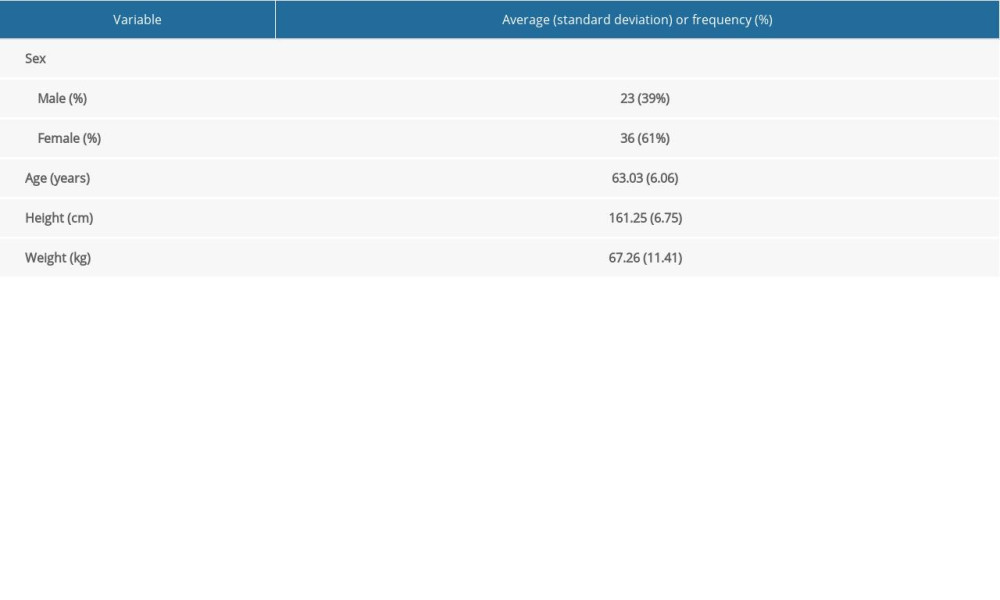 Table 1. General characteristics of study subjects.
Table 1. General characteristics of study subjects.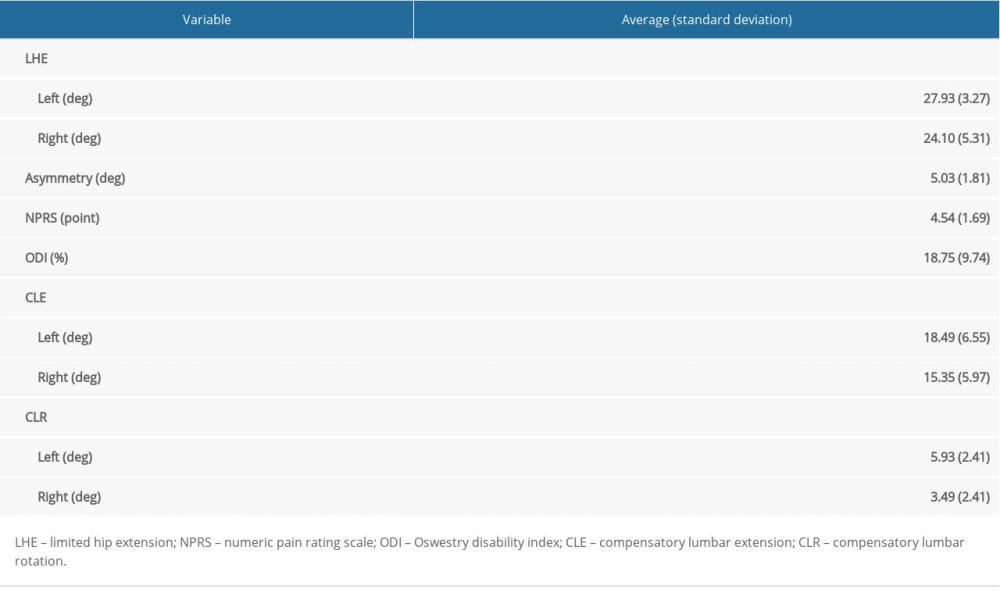 Table 2. Medical characteristics of study subjects.
Table 2. Medical characteristics of study subjects.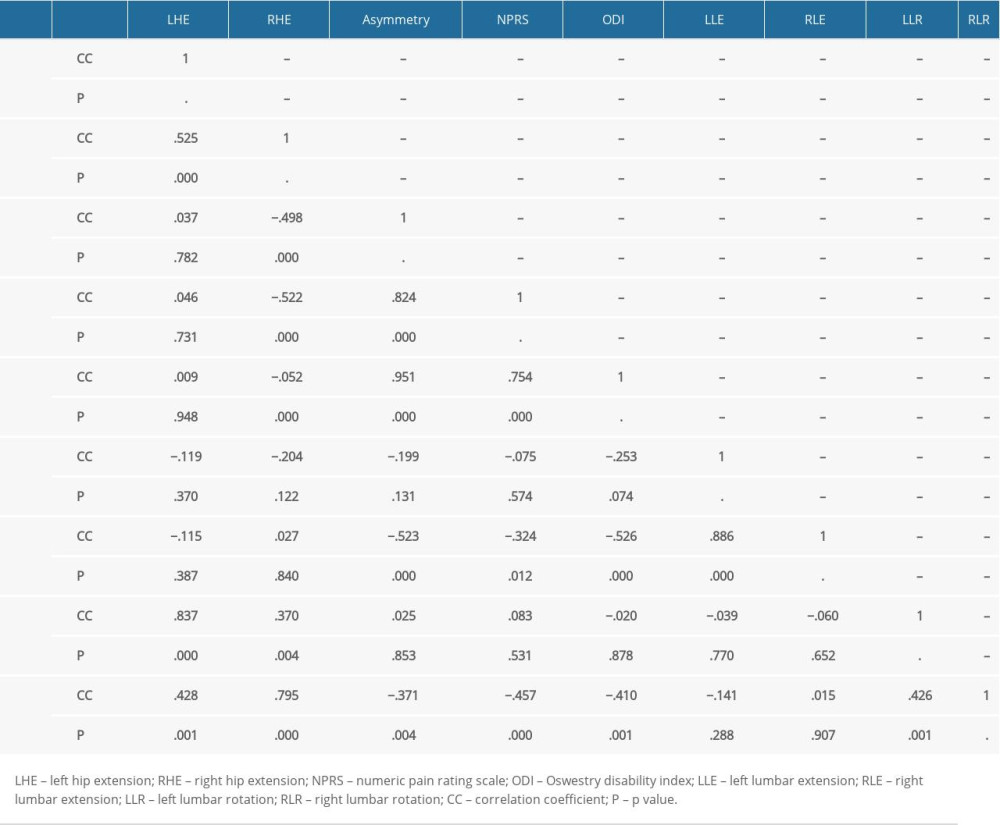 Table 3. Limited hip mobility, compensated lumbar extension, and compensatory lumbar rotation correlation.
Table 3. Limited hip mobility, compensated lumbar extension, and compensatory lumbar rotation correlation. In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








