06 July 2020: Clinical Research
Efficacy and Safety of Mechanical Thrombectomy for Acute Mild Ischemic Stroke with Large Vessel Occlusion
Gui-fang Wang12ABCEF, Xue Zhao2ABEF, Shu-ping Liu1AD, Yi-lei Xiao3AF, Zu-neng Lu1ABF*DOI: 10.12659/MSM.926110
Med Sci Monit 2020; 26:e926110
Abstract
BACKGROUND: The suitability of mechanical thrombectomy (MT) for patients with acute mild ischemic stroke (AMIS) caused by large vessel occlusion (LVO) is controversial. This study evaluated MT in patients with AMIS and LVO.
MATERIAL AND METHODS: Forty-seven patients diagnosed as AMIS with LVO received MT or intravenous thrombolysis (IVT). Primary outcomes were National Institute of Health Stroke Scale (NIHSS) and modified Rankin Scale scores. Secondary outcomes were incidence of systemic complications and symptomatic intracranial hemorrhage.
RESULTS: There were no significant differences between IVT and MT groups for gender, age, risk factors of cerebrovascular disease, past history, NIHSS score at admission, blood pressure, and LVO sites. For all patients, the NIHSS scores at discharge were lower than those at admission. Patients with excellent outcomes were 66.6% (16/24) in the IVT group and 60.8% (14/23) in the MT group; favorable outcome rates were 75% (18/24) in the IVT group and 69.6% (16/23) in the MT group, with no significant differences between groups. Twelve patients (52.2%) in the MT group and 5 (20.8%) in the IVT group had systemic complications. Symptomatic intracranial hemorrhage was not detected in the IVT group, but manifested in 2 (8.7%) patients in the MT group. During 90-day follow-up, 1 patient died in each of the IVT and MT groups, with 4.2% and 4.4% mortality rates, respectively.
CONCLUSIONS: The efficacy of MT and IVT was comparable in AMIS patients with LVO. While MT had a higher incidence of systemic complications, its short- and long-term effects were equivalent to IVT.
Keywords: Dental Occlusion, Balanced, Stroke, Thrombolytic Therapy, Administration, Intravenous, Aged, 80 and over, Brain Ischemia, Fibrinolytic Agents, ischemic stroke, Mechanical Thrombolysis, Risk Factors, Thrombectomy, Tissue Plasminogen Activator
Background
The early stages of acute mild ischemic stroke (AMIS) manifest as slight neurologic symptoms, with a National Institute of Health Stroke Scale (NIHSS) score of 5 or lower [1]. However, when AMIS is caused by large vessel occlusion (LVO), patients are at higher risk of early deterioration and poor prognosis [2]. Considering the generally favorable outcomes of AMIS and possible hemorrhage during intravenous thrombolysis (IVT), clinical trials on IVT generally exclude patients with LVO, resulting in disparate findings in published studies [3–7].
In 2015, five international, multi-center studies with randomized and controlled prospective trials were published in the New England Journal of Medicine, demonstrating the superior effect of endovascular therapy (EVT) to standard medical care in improving the prognosis of patients suffering from anterior circulation LVO [8–12]. Subsequently, guidelines identified mechanical thrombectomy (MT) as a Class I recommendation with level of evidence A [13]. However, the benefits of MT in AMIS with LVO remain controversial. For instance, out of the 5 stated studies, only MR CLEAN [8] and EXTEND-IA [11] included some participants with low NIHSS scores. Moreover, clinical trials reached substantially divergent conclusions as to whether the AMIS with LVO patients should receive EVT [14–16]. These conflicting results increase the difficulty in selecting appropriate treatment regimens for this type of case.
Therefore, the current retrospective single-center study was carried out to compare the safety and efficacy of MT and IVT in treating patients with AMIS and LVO. The aim of this study is to provide scientific evidence to instruct this clinical practice.
Material and Methods
SUBJECTS:
Patients diagnosed as AMIS with LVO that received IVT or MT in Liaocheng People’s Hospital from January 1, 2017 to July 30, 2019, were recruited. The inclusion criteria were as follows: NIHSS ≤5, cranio-cervical CT angiography detected intracranial LVO at the M1 or M2 segment of the middle cerebral artery, internal carotid artery, or vertebrobasilar artery. The exclusion criteria were as follows: patients <18 years of age, modified Rankin Scale score (mRS) ≥1, active hemorrhage or apparent hemorrhagic tendency, severe cardiac, renal, or hepatic insufficiency, hematological disease, major operation in the past month, blood glucose < 2.7 mmol/L or >22.2 mmol/L, refractory hypertension, incomplete clinical data, and refusal to participate in follow-up. The study protocol was approved by the Ethics Committee of the Liaocheng People’s Hospital. All procedures involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Declaration of Helsinki and its later amendments, or comparable ethical standards.
DATA COLLECTION:
Demographic and basic clinical information, imaging data, and follow-up details of patients were collected.
THERAPEUTIC PROCEDURES:
Patients were placed in the IVT (24 cases) or MT group (16 cases, MT+IVT; 7 cases, MT alone). In the IVT group, alteplase (rt-PA) was administrated at a dose of 0.9 mg/kg, with a maximum total dose of 90 mg. MT was performed under general anesthesia through right femoral artery puncture. Stent thrombectomy alone or in combination with balloon dilation, stent implantation, or both was selected depending on arterial conditions. The choice of therapeutic approach was based on several criteria. First, the patients or family members were fully informed about the risks and benefits of the treatments so that they could make independent decisions regarding treatment options. Second, for patients with IVT contraindication, MT alone was performed. And third, for cases that became aggravated after IVT, an expert group made individual assessments to decide whether MT should be given as a rescue therapy.
NEUROLOGICAL FUNCTION ASSESSMENT: The neurological function deficiency of patients at admission, 24 h after treatment, and on discharge was evaluated using NIHSS. Recovery of neurological function at 90 days after treatment was assessed using mRS [17], in which a score of 0–1 was regarded as an excellent outcome, and 0–2 as favorable. Revascularization was estimated using modified thrombolysis in cerebral infarction (mTICI) classification, with grade 2b-3 indicating successful recanalization [18].
SAFETY ASSESSMENT:
Symptomatic intracranial hemorrhage (sICH) was determined according to the European Cooperative Acute Stroke Study (ECASS-III), which included the hemorrhagic features on imaging and an NIHSS score of higher than 4 or death. Complications included sICH and other disorders, such as mucocutaneous hemorrhage, gastrointestinal hemorrhage, urinary tract infection, pulmonary infection, and deep venous thrombosis. The number of patients that died and causes of death during the 90 days following treatment were recorded by telephone follow-up.
STATISTICAL ANALYSIS:
All statistical analyses were performed with SPSS 22.0 (IBM SPSS, Armonk, NY, USA). Continuous variables were analyzed by Student’s
Results
DEMOGRAPHIC AND BASIC CLINICAL INFORMATION OF PATIENTS:
A total of 47 patients were included in this study, of which 24 received IVT and 23 received MT. There were no significant differences between the 2 groups with respect to sex, age, risk factor of cerebrovascular diseases, past stroke history, NIHSS score on admission, blood pressure, and LVO sites (Table 1).
THERAPEUTIC EFFECT OF IVT AND MT ON AMIS PATIENTS WITH LVO:
For the IVT treatment, the mean time between onset to thrombolysis with rt-PA was 181.25±87.18 min. For the MT group, bridging therapy was performed in 16 out of 23 patients (69.5%), of which 12 received MT and IVT simultaneously, and showed a mean time of 302.00±85.22 min from onset to femoral artery puncture. Four patients manifested with neurological deterioration after IVT (NIHSS score increased by more than 4 as compared to that on admission); thus, MT was conducted as rescue therapy. The mean time from onset to femoral artery puncture was 465.00±165.22 min (Table 2).
Direct endovascular therapy was used in 7 patients, of which 4 had contraindications of IVT, and 3 were treated at the request of family members. For these patients, the mean time from onset to femoral artery puncture was 270.00±87.19 min.
A total of 22 cases were recanalized successfully, of which 11 received just stent thrombectomy, 8 received thrombectomy and stent implantation, 1 received thrombectomy and balloon dilatation, and 2 received a combination of thrombectomy, stent implantation, and balloon dilatation. In each patient, thrombectomy was implemented fewer than 3 times, and it was implemented successfully the first time in 13 patients. The post-operative mTICI was grade 3 for 19 patients and 2b for 3 patients (Table 2).
Offending vessel occlusion was confirmed by digital subtraction angiography, which encompassed the middle cerebral artery in 12 cases (M1 segment in 10 cases and M2 segment in 2 cases), internal carotid artery in 5 cases, and vertebrobasilar artery in 6 cases (Table 2).
TREATING OUTCOMES OF IVT AND MT ON AMIS PATIENTS WITH LVO:
For all patients, NIHSS scores were lower at discharge compared to those at admission. The NIHSS scores 24 h after treatment and at discharge were similar in both groups. At all timepoints, there were no significant differences in the NIHSS scores between the IVT and MT groups. At 90 days after treatment, excellent outcome (mRS 0–1) was obtained in 66.6% (16/24) of patients in the IVT group and 60.8% (14/23) of patients in the MT group. Favorable outcome (mRS 0–2) rating was obtained in 75% (18/24) and 69.6% (16/23) of patients in the IVT and MT groups, respectively. Neither parameter was significantly different between the 2 groups (P=0.671 and P=0.667, respectively, Table 3).
SAFETY OF IVT AND MT IN AMIS PATIENTS WITH LVO:
A total of 12 cases (52.2%) in the MT group and 5 cases (20.8%) in the IVT group developed systemic complications (Tables 3, 4). The difference between the 2 groups was significant (χ2=4.063, P=0.044). Two patients had sICH (8.7%) in the MT group, with none in the IVT group (Table 5). During the 90-day follow-up, there was 1 case of death each in the IVT (4.2%) and MT (4.4%) groups. The mortality rate of the 2 groups was similar. In both cases, the offending vessel was the basilar artery. The causes of death were central circulatory and respiratory failure, as well as severe pulmonary infection (Table 3).
Discussion
The current study revealed lower NIHSS scores at discharge compared to those at admission for all patients, and the scores were similar in both groups 24 h after treatment and at discharge. The favorable and excellent outcomes 90 days after onset were satisfactory. The rates of sICH and mortality in the MT group were comparable to those of the IVT group, despite a higher incidence of systemic complications in the MT group.
In clinical practice, some patients have low NIHSS scores but also have proximal LVO. One-third of such patients are not able to walk without assistance if they do not receive acute recanalization. For these cases, careful assessment and active IVT and MT when necessary are required for vascular recanalization. These practices improve prognosis and reduce the risk of disability and mortality. The current study provides evidence supporting the application of EVT in AMIS, and agrees with cohort studies showing that MT has a similar effect on mild and severe stroke patients [19,20]. Current guidelines state that patients with an NIHSS score of 6 or higher should receive EVT, while patients within 3 h of experiencing mild disabling stroke should receive IVT [21]. Meta-analyses on the therapeutic effect of MT alone or in combination with rt-PA on AMIS patients with an NIHSS score of 5 or lower have demonstrated that both approaches improved the 3-month functional outcomes of AMIS patients with LVO [22,23].
The present study showed that 66.6% and 75% of patients with AMIS and LVO in the IVT group had mRS scores of 0–1 and 0–2, respectively, during the 90-day follow-up. This result was similar to the findings from 2 domestic stroke databases on patients with NIHSS scores of 5 and lower (with 77.6% (0–1) and 85.8% (0–2) mRS scores, respectively); AMIS patients with large artery atherosclerosis benefited from rt-PA in this clinical study [24]. Moreover, the IVT group in the current study had no cases of sICH and 20.8% of cases had systemic complication (5/24 patients), which included 3 cases of gingival bleeding, 1 case of urinary tract infection, and 1 case of severe pneumonia, which led to the only case of death in this group. The functional dependence rate during the 90-day follow-up was high, suggesting a desirable long-term efficacy and a low risk of hemorrhage. The IVT showed apparent advantages, with no increase in the risk of death or hemorrhage of these patients [25]. Therefore, AMIS should not be considered a contraindication of IVT, especially when the imaging tests showed that LVO were the offending vessels.
For patients receiving MT, Pfaff et al. [26] demonstrated 6.1% sICH, 63.6% functional dependence (mRS 0–2), and 9.1% mortality during the 90-day follow-up in patients with LVO and NHISS scores of 8 and lower. The current study recruited AMIS patients with NIHSS scores of 5 or lower, with MT leading to 69.6% functional dependence (mRS 0–2), 8.7% sICH, and 4.4% mortality, which was consistent with the previous study. DaRos et al. [27] evaluated 56 AMIS with LVO patients who had NIHSS scores of 5 or lower and obtained a 100% recanalization rate (mTICI 2b-3) after MT and a 38% recanalization rate after IVT. Although the incidence of sICH was similar between the 2 groups, MT resulted in a higher early discharge rate and better clinical outcomes after 3 months. Despite debate over how mild AIS is defined, these data demonstrate the advantages of MT in improving the clinical outcomes of AMIS patients with LVO.
Sarraj et al. [28] compared the differences in efficacy of EVT and medical treatment in 214 AMIS patients and found similar percentages of favorable (mRS 0–2, 63.3% and 67.8%, respectively) and excellent (mRS 0–1, 55.7% and 54.4%, respectively) outcomes for the 2 approaches. EVT resulted in a higher incidence of sICH compared to that of medical treatment. The current study attained a parallel result, with MT resulting in 60.8% and 69.9% of excellent and favorable outcomes, respectively, while IVT resulted in 66.6% and 75% of excellent and favorable outcomes, respectively. However, no significant difference was detected in the percentage of sICH between the 2 approaches.
Messer et al. [20] conducted a study on 54 AMIS with LVO patients that had NIHSS scores of 5 or lower, of which 8 (14.8%) patients received immediate MT, 6 (11.1%) patients received MT until early neurologic deterioration, and 40 (74.1%) patients received IVT only. Excellent outcomes (mRS 0–1) of 75%, 33.3%, and 55% were obtained in the 3 groups, respectively. None of the cases presented sICH [20]. Patients receiving MT and IVT in the current study showed 60.8% and 66.6% excellent outcomes, respectively (mRS 0–1). Four cases were aggravated after IVT and were transferred to MT. The median NIHSS scores were higher than at the baseline level, which might have reduced the percentage of excellent outcomes.
Regarding systemic complications, the MT group had a higher incidence of pneumonia (5 cases) and lower extremity deep venous thrombosis (2 cases) compared to the IVT group (1 case of pneumonia; no cases of lower extremity deep venous thrombosis). These differences might be explained by the fact that patients receiving MT were under general anesthesia, which involved tracheal intubation and the application of a ventilator. Consequently, there was a greater chance of contracting a pulmonary infection. In addition, delayed expectoration during recovery from anesthesia promoted pulmonary infection. Further, during MT, patients underwent digital subtraction angiography, after which the pressure dressing placed on the femoral artery puncture site impeded venous reflux. Moreover, the straight-leg position of the lower limbs after surgery reduced muscle strength, which hindered blood flow. Lastly, use of non-ionic contrast medium raised blood viscosity. All of these parameters likely contributed to the formation of lower extremity deep venous thrombosis.
Conclusions
The optimal treatment for vascular recanalization of AMIS patients with LVO remains undetermined; therefore, large-scale, multi-center randomized controlled prospective trials are needed to elucidate best treatment practices. The present study provided some evidence for the treatment of AMIS patients at Liaocheng People’s Hospital, which is a comprehensive stroke center and teaching hospital for stroke prevention and treatment, designated by the National Health Commission of the People’s Republic of China. An interventional therapy team is responsible for the continuous quality monitoring and validating the reliability of the hospital’s data. Even for retrospective studies, evaluation of each patient depends on careful examination and analysis.
The limitations of the present study included the use of a single center and retrospective design. Thus, a prospective study at multiple centers with a large patient sample is needed to validate the results of the current study in clinical practice. In addition, EVT was performed by both neurological physicians and neurosurgeons with different qualifications and experiences, which might have influenced therapeutic outcomes. Lastly, a significant number of cases in the MT group received treatment after their clinical situation deteriorated; thus, theoretically, timely MT is required to improve clinical efficacy.
In summary, IVT and MT improved both the short- and long-term prognosis of AMIS patients with LVO and exhibited comparable efficacy. Thus, in clinical practice, the decision to select one or more approaches should depend on the specific condition of the individual patient and should balance risks and benefits.
Tables
Table 1. Demographic and basic clinical information of patients receiving IVT or MT.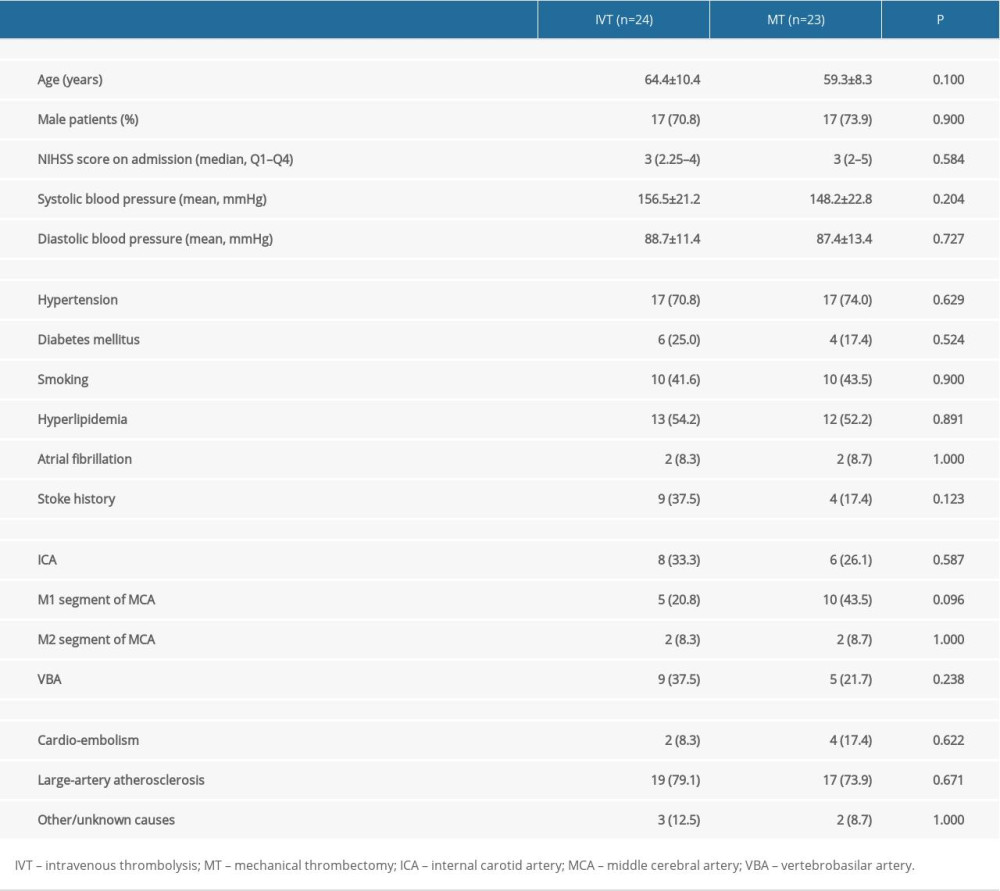 Table 2. Endovascular treatment (EVT) of AMIS patients with LVO (n=23).
Table 2. Endovascular treatment (EVT) of AMIS patients with LVO (n=23).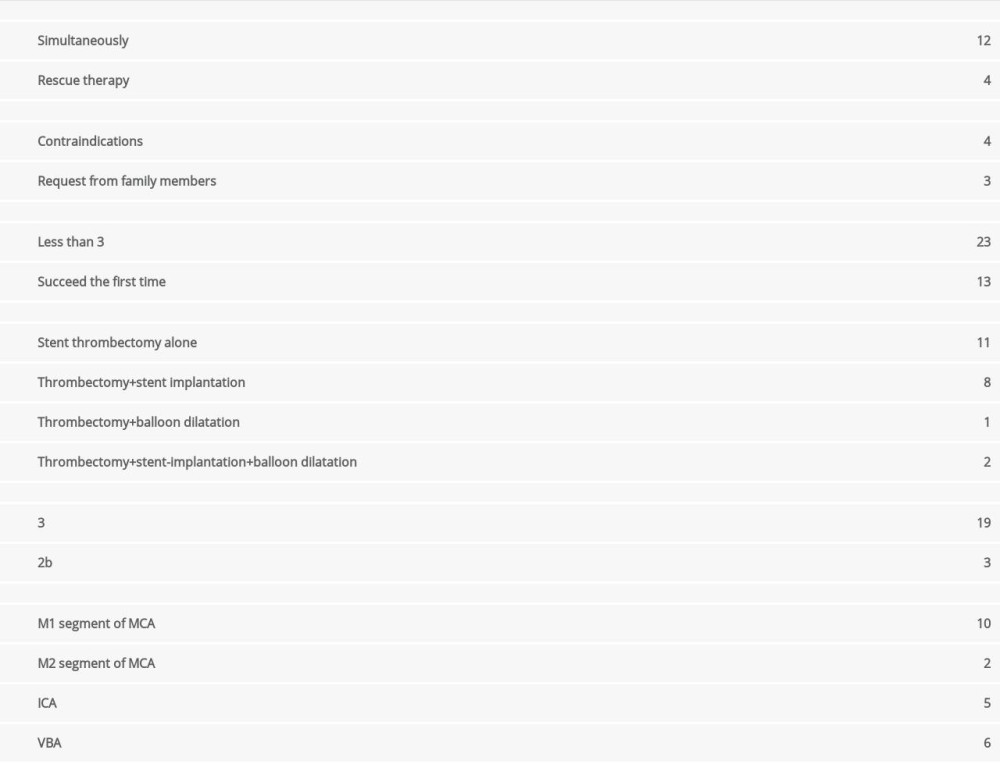 Table 3. Treatment outcomes of IVT and MT on AMIS patients with LVO.
Table 3. Treatment outcomes of IVT and MT on AMIS patients with LVO.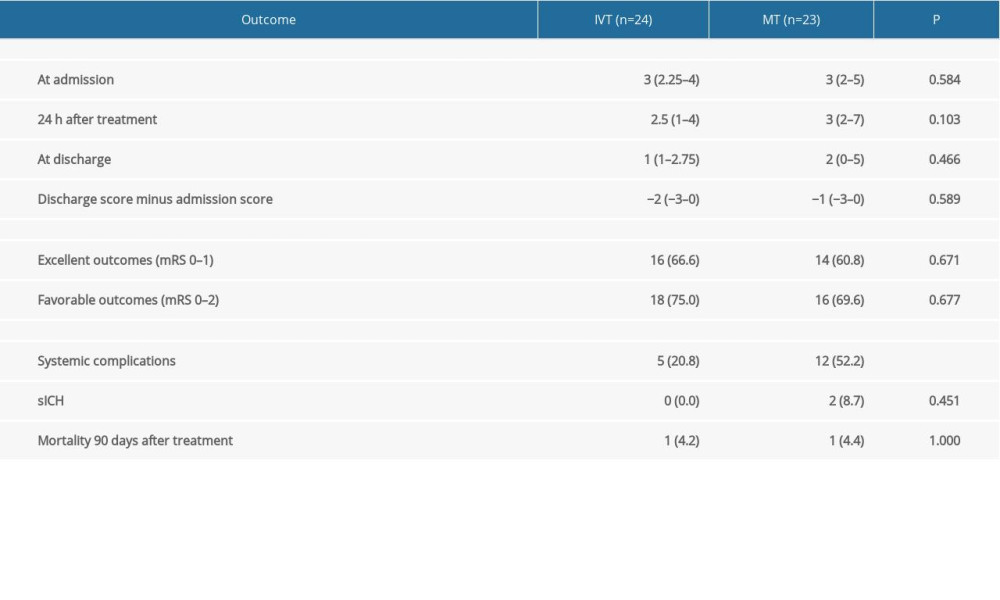 Table 4. Complications of AMIS patients receiving IVT or MT treatment.
Table 4. Complications of AMIS patients receiving IVT or MT treatment.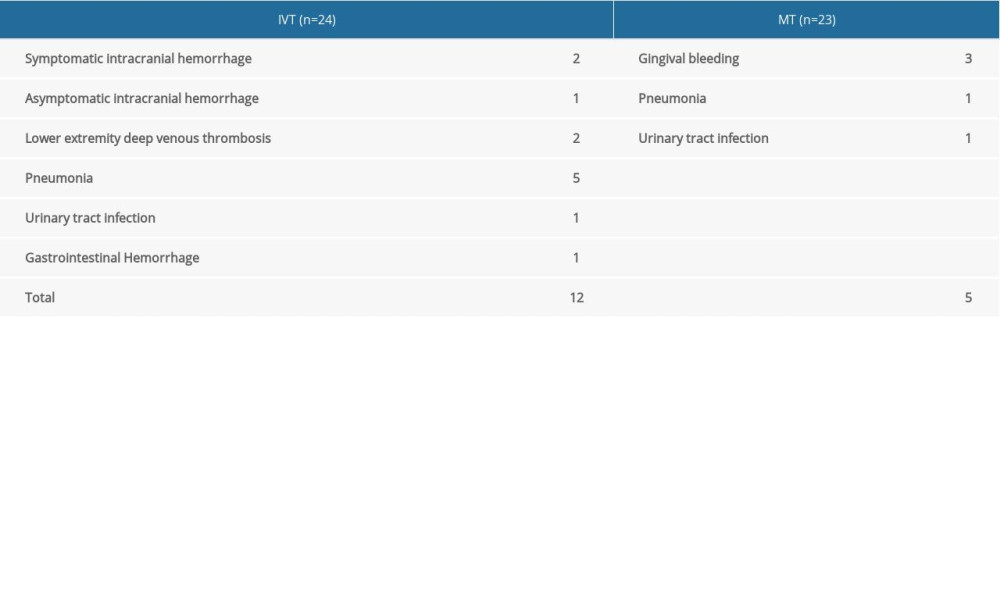 Table 5. Information on the 2 AMIS cases with sICH after MT.
Table 5. Information on the 2 AMIS cases with sICH after MT.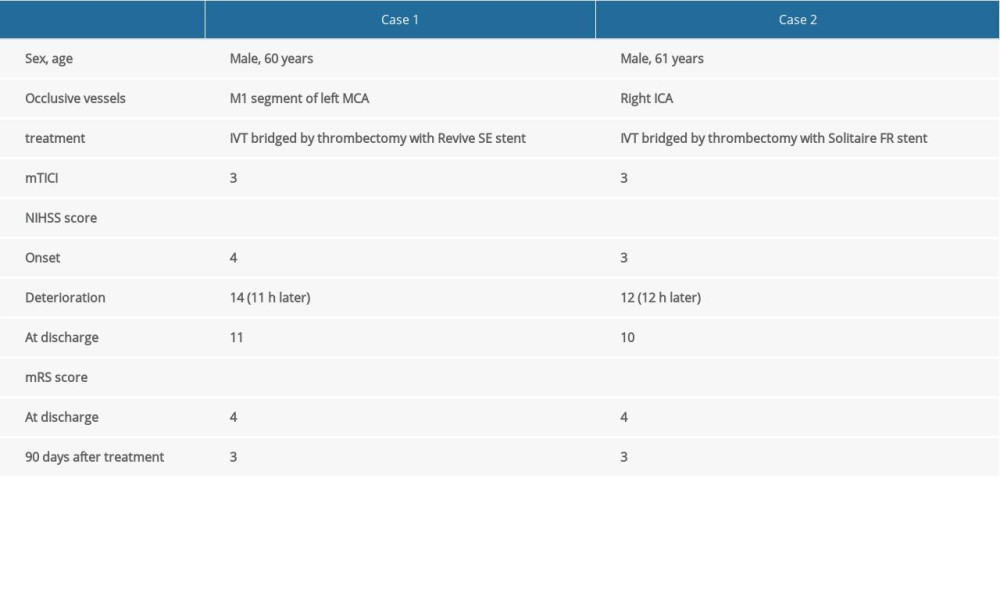
References
1. DeGraba TJ, Hallenbeck JM, Pettigrew KD, Progression in acute stroke: Value of the initial NIH stroke scale score on patient stratification in future trials: Stroke, 1999; 30; 1208-12
2. Cerejo R, Cheng-Ching E, Hui F, Treatment of patients with mild acute ischemic stroke and associated large vessel occlusion: J Clin Neurosci, 2016; 30; 60-64
3. Khatri P, Kleindorfer DO, Devlin T: JAMA, 2018; 320; 156-66
4. Emberson J, Lees KR, Lyden P, Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: A meta-analysis of individual patient data from randomised trials: Lancet, 2014; 384; 1929-35
5. Lees KR, Emberson J, Blackwell L, Effects of alteplase for acute stroke on the distribution of functional outcomes: A pooled analysis of 9 trials: Stroke, 2016; 47; 2373-79
6. Greisenegger S, Seyfang L, Kiechl S, Thrombolysis in patients with mild stroke: Results from the Austrian Stroke Unit Registry: Stroke, 2014; 45; 765-69
7. Laurencin C, Philippeau F, Blanc-Lasserre K, Thrombolysis for acute minor stroke: Outcome and barriers to management. Results from the RESUVAL Stroke Network: Cerebrovasc Dis, 2015; 40; 3-9
8. Berkhemer OA, Fransen PS, Beumer D, A randomized trial of intraarterial treatment for acute ischemic stroke: N Engl J Med, 2015; 372; 11-20
9. Goyal M, Demchuk AM, Menon BK, Randomized assessment of rapid endovascular treatment of ischemic stroke: N Engl J Med, 2015; 372; 1019-30
10. Saver JL, Goyal M, Bonafe A: N Engl J Med, 2015; 372; 2285-95
11. Campbell BC, Mitchell PJ, Kleinig TJ, Endovascular therapy for ischemic stroke with perfusion-imaging selection: N Engl J Med, 2015; 372; 1009-18
12. Jovin TG, Chamorro A, Cobo E, Thrombectomy within 8 hours after symptom onset in ischemic stroke: N Engl J Med, 2015; 372; 2296-306
13. Powers WJ, Derdeyn CP, Biller J, 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: A guideline for healthcare professionals from the American Heart Association/American Stroke Association: Stroke, 2015; 46; 3020-35
14. Urra X, San Roman L, Gil F, Medical and endovascular treatment of patients with large vessel occlusion presenting with mild symptoms: An observational multicenter study: Cerebrovasc Dis, 2014; 38; 418-24
15. Goyal M, Menon BK, van Zwam WH, Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials: Lancet, 2016; 387; 1723-31
16. Haussen DC, Bouslama M, Grossberg JA, Too good to intervene? Thrombectomy for large vessel occlusion strokes with minimal symptoms: An intention-to-treat analysis: J Neurointerv Surg, 2017; 9; 917-21
17. Wilson JT, Hareendran A, Grant M, Improving the assessment of outcomes in stroke: use of a structured interview to assign grades on the modified Rankin Scale: Stroke, 2002; 33; 2243-46
18. Zaidat OO, Yoo AJ, Khatri P, Recommendations on angiographic revascularization grading standards for acute ischemic stroke: A consensus statement: Stroke, 2013; 44; 2650-63
19. Dargazanli C, Arquizan C, Gory B, Mechanical thrombectomy for minor and mild stroke patients harboring large vessel occlusion in the anterior circulation: A multicenter cohort study: Stroke, 2017; 48; 3274-81
20. Messer MP, Schonenberger S, Mohlenbruch MA, minor stroke syndromes in large-vessel occlusions: Mechanical thrombectomy or thrombolysis only?: Am J Neuroradiol, 2017; 38; 1177-79
21. Powers WJ, Rabinstein AA, Ackerson T, 2018 Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association: Stroke, 2018; 49; e46-110
22. Griessenauer CJ, Medin C, Maingard J, Endovascular mechanical thrombectomy in large-vessel occlusion ischemic stroke presenting with low national institutes of health stroke scale: Systematic review and meta-analysis: World Neurosurg, 2018; 110; 263-69
23. Xiong YJ, Gong JM, Zhang YC, Endovascular thrombectomy versus medical treatment for large vessel occlusion stroke with mild symptoms: A meta-analysis: PLoS One, 2018; 13; e0203066
24. Chen W, Pan Y, Zhao X, Intravenous thrombolysis in Chinese patients with different subtype of mild stroke: Thrombolysis in patients with mild stroke: Sci Rep, 2017; 7; 2299
25. Yeo LLL, Ho R, Paliwal P, Intravenously administered tissue plasminogen activator useful in milder strokes? A meta-analysis: J Stroke Cerebrovasc Dis, 2014; 23; 2156-62
26. Pfaff J, Herweh C, Pham M, Mechanical thrombectomy in patients with acute ischemic stroke and lower NIHSS scores: Recanalization rates, periprocedural complications, and clinical outcome: Am J Neuroradiol, 2016; 37; 2066-71
27. Da Ros V, Cortese J, Chassin O, Thrombectomy or intravenous thrombolysis in patients with NIHSS of 5 or less?: J Neuroradiol, 2019; 46; 225-30
28. Sarraj A, Hassan A, Savitz SI, Endovascular thrombectomy for mild strokes: How low should we go?: Stroke, 2018; 49; 2398-405
Tables
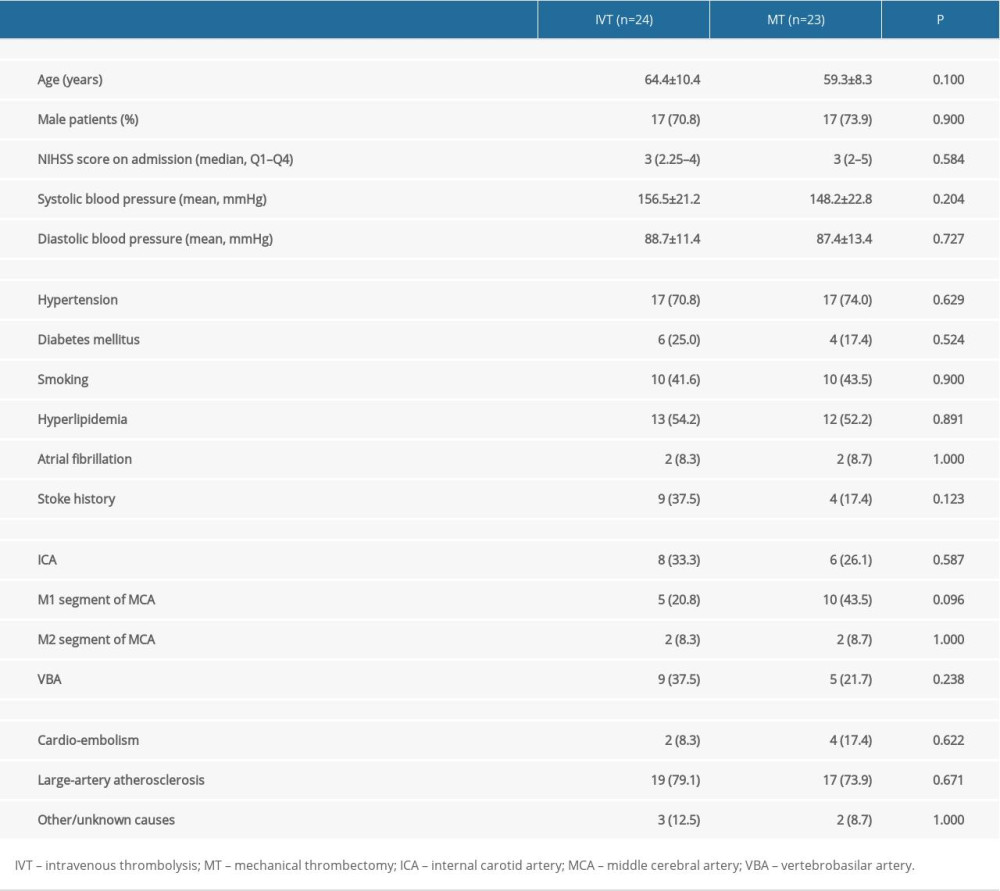 Table 1. Demographic and basic clinical information of patients receiving IVT or MT.
Table 1. Demographic and basic clinical information of patients receiving IVT or MT.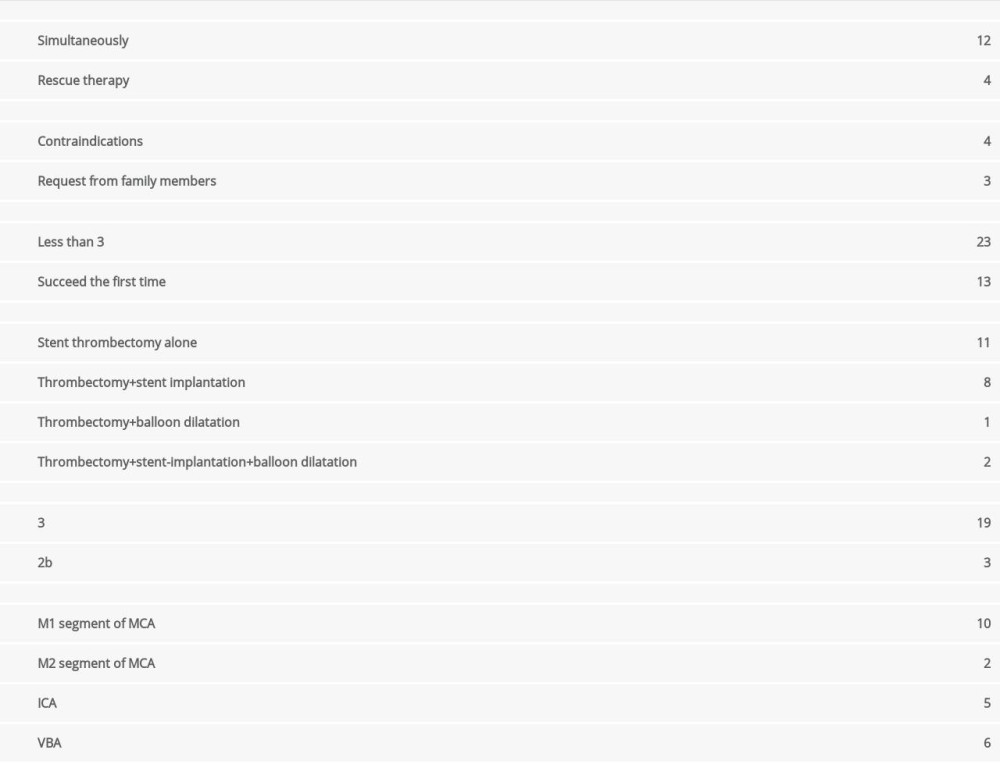 Table 2. Endovascular treatment (EVT) of AMIS patients with LVO (n=23).
Table 2. Endovascular treatment (EVT) of AMIS patients with LVO (n=23).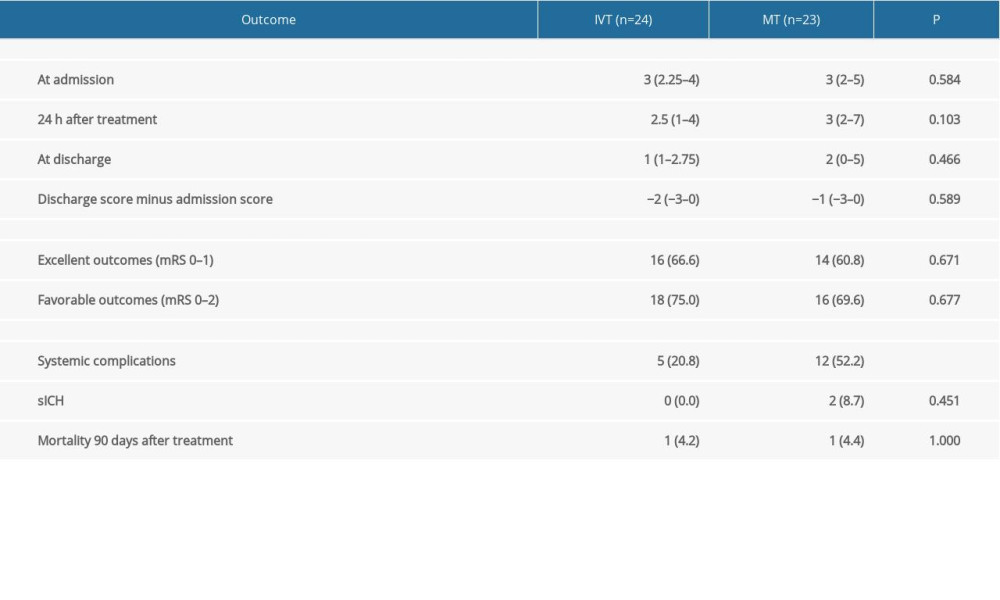 Table 3. Treatment outcomes of IVT and MT on AMIS patients with LVO.
Table 3. Treatment outcomes of IVT and MT on AMIS patients with LVO.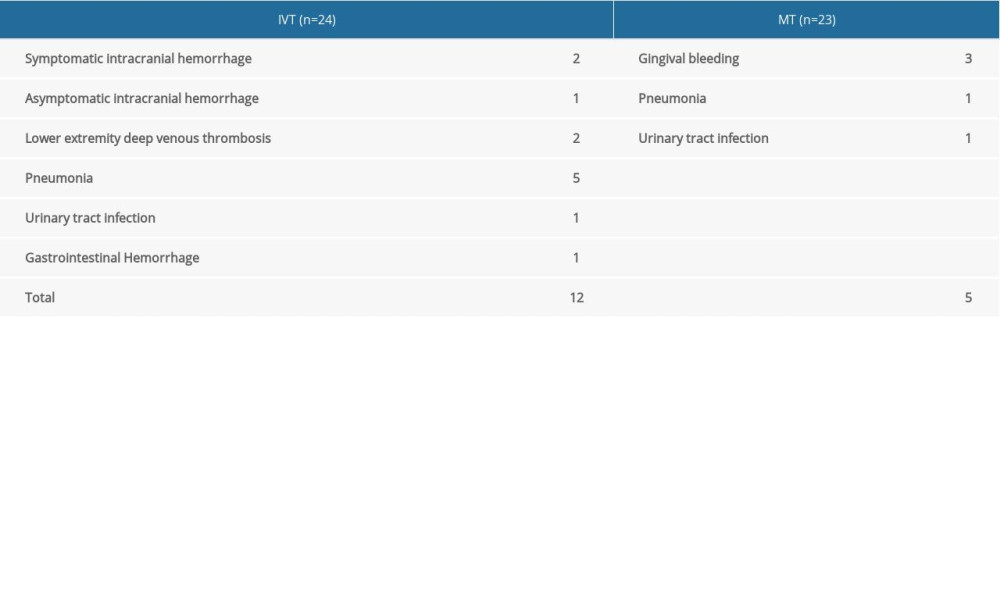 Table 4. Complications of AMIS patients receiving IVT or MT treatment.
Table 4. Complications of AMIS patients receiving IVT or MT treatment.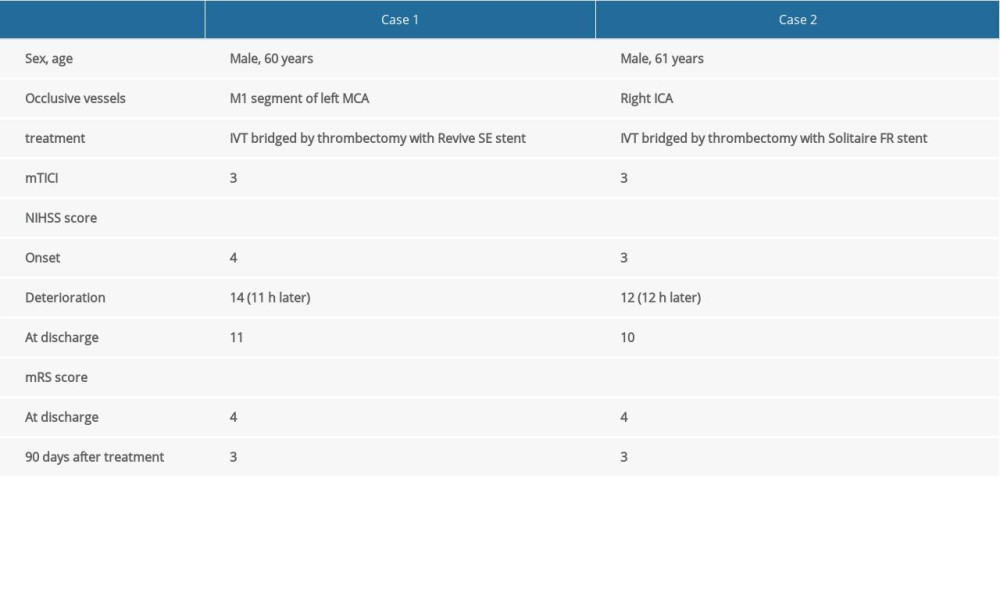 Table 5. Information on the 2 AMIS cases with sICH after MT.
Table 5. Information on the 2 AMIS cases with sICH after MT. In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








