19 November 2020: Clinical Research
Suture Anchor Versus Allogenic Tendon Suture in Treatment of Haglund Syndrome
Yan Xu1BCE, Deyu Duan1BCE, Lei He1CDF, Liu Ouyang1AEG*DOI: 10.12659/MSM.927501
Med Sci Monit 2020; 26:e927501
Abstract
BACKGROUND: Haglund’s deformity is an abnormal bony enlargement on the back of the heel. It can cause the impact of the posterior calcaneal bursa and Achilles tendon insertion, and finally result in pain. This syndrome is called Haglund syndrome. The purpose of this study was to explore the effect of the suture anchor and allogeneic tendon suture in the treatment of Haglund syndrome.
MATERIAL AND METHODS: We retrospectively studied 20 patients with Haglund syndrome treated from January 2015 to December 2016. The patients were randomly divided into Group 1 (the suture anchor group) and Group 2 (the allogeneic tendon group), with 10 patients in each group and an average follow-up of 32 months after surgery. The AOFAS, VAS, and Arner-Lindholm scales were used to summarize the patient follow-up results and complications.
RESULTS: In the 2 groups of patients, the postoperative AOFAS, VAS scores, and the Arner-Lindholm scale showed good results. However, the postoperative AOFAS score and VAS of the suture anchor group were better than those of the allogeneic tendon group, with shorter operation times. No Achilles tendon rupture or wound infection occurred during the entire postoperative period in either group. These results show the superiority of suture anchors.
CONCLUSIONS: The higher AOFAS and VAS score and shorter operation time in the suture anchor group suggest it is the better alternative for treatment of Haglund syndrome.
Keywords: Achilles Tendon, Ankle Joint, Ligaments, Articular, Calcaneus, Magnetic Resonance Imaging, Postoperative Care, Suture Anchors, Sutures, Syndrome
Background
Haglund syndrome is a pathological disease mainly caused by the impact between the Achilles tendon and the posterior superior tubercle of the calcaneus, causing swelling of the inflamed retrocalcaneal bursa [1], first reported by Patrick Haglund in 1928 [2]. It is reported that the disease has a certain genetic predisposition, and the probability of Haglund syndrome in people with a family history is 5 times higher than in those without. Diabetes, gout, and rheumatoid arthritis can affect the pathology of the Achilles tendon insertion [3,4]. Clinically, it is characterized by abnormal protrusion of the posterior superior tubercle of the calcaneus, accompanied by inflammation around the insertion of the Achilles tendon, resulting in corresponding swelling, pain, lameness, and limited dorsal extension of the foot [5,6]. When a large piece of protruding bone rubs against a harder upper area, the patient will feel discomfort in soft tissue near the heel. Generally speaking, this kind of foot syndrome is more common in middle-aged people, and women are more often affected than men [7]. The specific pathogenesis is not yet known. Clinical experience suggests it may be caused by foot valgus, talipes equinus, wearing tight shoes, calcaneal trauma, or professional athlete injury [8].
During the initial treatment of Haglund syndrome, we recommend conservative treatment first. Eccentric strength exercises, extra-corporeal shock wave therapy (ESWT), and orthopedic insoles are currently the most common treatments [9]. Eccentric strength exercises promote the formation of cross-links of collagen fibers in the tendon, thereby promoting tendon remodeling. Low-energy wave therapy can stimulate soft tissue healing, inhibit pain receptors, and relieve pain. Patients should replace shoes that have rubbing heels with shoes that have exposed heels to reduce heel pressure, and reduce stimulation of the Achilles tendon by using heel elevators or ankle-foot orthoses [14]. However, if such methods do not help, non-steroidal anti-inflammatory drugs are also recommended. Additionally, it is not recommended to inject steroids directly into the tendon, as this can have an adverse effect on the tendon and cause severe Achilles tendon rupture [12]. Although early conservative treatment partially controls the deterioration of bursitis, the bulge of the posterior upper calcaneus cannot be eliminated, and the persistent heel pain caused by this mechanical shock is unbearable. When conservative treatment lasting 3–6 months does not adequately relieve symptoms, surgery is usually required [13,14]. The most commonly used surgical methods are Achilles tendon debridement+resection of the posterior tubercle of the root bone and debridement+Achilles tendon insertion reconstruction [15]. It is necessary to perform removal of the abnormal osseous process of the posterior superior tubercle of the root bone, debridement of the Achilles tendon, and removal of the deformed Achilles tendon and peripheral inflammatory tissue, and the insertion of the Achilles tendon is re-strengthened and fixed.
A variety of reliable suture techniques and materials have been reported clinically. Previously, traditional wire repairing methods were used, which often had disadvantages such as local skin bruises, difficulty in nursing care, and infection. When the internal fixation is removed, it causes pain. For patients with Achilles tendon avulsion, the bone should also be fixed with steel wire through the sole of the foot. This surgical method has been used for many years, but too long a period of plaster fixation is likely to cause gastrocnemius muscle atrophy, ankle capsule contracture, and ankle extension dysfunction. The above problems led to consideration of a novel suture anchor method [16]. In suture anchoring, the anchor is directly fixed on the calcaneal surface, and then the proximal end of the Achilles tendon is fixed by the sliding suture on the anchor so that the contractile force of the gastrocnemius muscle acts directly on the calcaneus, which helps eliminate the tension between the broken ends of the Achilles tendon. At the same time, a thin absorbable suture is used for continuous sutures of the Achilles tendon stump, which can reduce foreign body indwelling and increase the contact area of the stump, thus improving the patient’s prognosis. Kuru et al. reported that use of suture anchors may be a suitable choice for specific patients, and a modified Lindholm procedure may be a safe choice for Achilles tendon rupture [17,18].
As a transplantation material applied after biological treatment, the allogenic tendon performs well in avoiding the adverse effects associated with use of the autologous tendon, which has limited material and large associated trauma. Allogeneic tendon transplantation is equivalent to bridging a tendon at the tendon rupture. By allowing the recipient capillaries and fibroblasts to invade the surface of both ends of the allogeneic tendon, the cells are transformed into tendon cells, gradually repairing the injured tendon area [19]. When transplanting, the allogeneic tendon and the normal tendon morphology should be compared to ensure that the thickness and width of the allogenous tendon to be transplanted conform to the reconstruction range. During suturing, tension, overlap, and other suture techniques should be used flexibly to enhance the suture effect and improve tendon stability after surgery [20]. Allogeneic tendons can come from many sources, and can not only maintain the original biological structural characteristics, but also meet the requirements of physique and quantity, and this makes it a feasible choice for clinical treatment of Haglund syndrome.
In this study, we applied a suture anchor to treat Haglund syndrome and achieved good clinical outcomes. The clinical results, safety, and effectiveness were analyzed to evaluate whether this method provided better long-term results than the allogeneic tendon technique.
Material and Methods
PATIENT DATA:
With the approval of our hospital’s Institutional Review Board, we retrospectively collected data on patients who underwent Haglund syndrome surgery with allogeneic tendons or suture anchors from January 2015 to December 2016 at the Department of Orthopedics, Union Hospital, Tongji Medical College of Huazhong Science and Technology University. Symptoms included persistent swelling and pain at the horizontal and posterior levels of the calcaneus and heel pain during active and passive movements. After 3 to 6 months of conservative treatment, it was not effective, and the calcaneal impact test was positive. X-ray images were taken to assess posterior calcaneal tubercle proliferation, the presence of calcification, and the size of the proximal calcaneal condyle that needed to be removed during surgery. MRI showed bursitis, rupture, local calcification, soft tissue hyperplasia, and edema in Achilles tendon (Figures 1, 2). As a major imaging study, other physical findings were not specifically considered, but patients were excluded if they had experienced a rupture of the Achilles tendon or had undergone any surgery on the same heel, or had undergone Haglund syndrome with complete detachment of the Achilles tendon [21,22]. Patients with other complications, such as diabetes, severe heart disease, morbid obesity, or peripheral vascular disease, are also excluded to avoid serious surgical complications. The medical data of 20 patients were collected and divided into 2 groups: the suture anchor group and the allogeneic tendon group (Table 1). All patients provided signed informed consent.
GROUP 1: The patients were operated on in supine position under continuous epidural anesthesia. The procedure was performed under a tourniquet. Through a lateral incision, the skin and subcutaneous tissue were cut, the broken end of the Achilles tendon was exposed, and the proximal end of the Achilles tendon was exposed about 5.0–6.0 cm (Figure 3). We were careful to protect the aponeurosis while removing blood clots. In particular, the exposure to the central area of the Achilles tendon should be reduced to protect the blood supply around the tendon. The ankle plantar flexion relaxed the Achilles tendon, a retractor was used to detect the degree of Achilles tendon lesion, calcification, or even rupture, and whether there were inflammatory changes in the surface bursa and posterior synovial bursa of the Achilles tendon. At the same time, the synovial bursa was removed around the Achilles tendon, along with the proliferative connective tissue behind the calcaneus. According to the impact test during surgery, the size of the abnormal protrusion of the posterior superior nodule of the calcaneus was determined. A sharp knife was used to sharply separate the Achilles tendon insertion until the level of the osteotomy line, generally peeling off only 50% to 70% of the tendon insertion. Based on the impact test, we assess whether further osteotomy was needed until there was no impact [23]. With the ankle in neutral position, 2 Fastin bone anchors 5.0 (Johnson, USA) were inserted at an angle of 45° to the Achilles tendon, and then 2 super sutures at the tail of the anchor were passed through the distal end to suture with the proximal Achilles tendon by Bunnell or Krackow method. The length of the braided Achilles tendon was about 6.0 cm. The broken end was strengthened with absorbable suture, and the broken end covered with aponeurosis was sutured and bandaged with aseptic dressing (Figure 4).
GROUP 2: The allogeneic tendon (ATorui biomaterials Co., Ltd, Shanxi, China) was preserved at low temperature, opened, and quickly rewarmed in aseptic Ringer solution at 45°C. After rewarming, the tendon was washed 5 to 6 times with aseptic saline, soaked in a saline solution containing gentamicin (320 mg/L) for 30 min, and then rinsed for subsequent use. The operation position and anesthesia method were the same as in the suture anchor group. An incision of about 3 cm was made upward from the insertion point and along the medial side of the Achilles tendon to expose the distal severed end and the normal insertion. Based on the degree of retraction, a 5–8 cm incision was made at the proximal end, and part of the normal tissue of the Achilles tendon was thus exposed, with a long (4 cm) skin bridge in the middle. After the distal and proximal ends were exposed, the scar tissue was removed, and the remaining scar tissue in the skin bridge was separated and removed with long curved forceps along the inner side of the tendon sheath. The length of the Achilles tendon defect was measured, and an appropriate allogeneic tendon was selected and sutured to the distal and proximal end of the Achilles tendon through the skin bridge. The distal allogenous tendon was fixed to the calcaneus with squeeze screws, the incision was sutured and rinsed, and a sterile dressing was applied (Figure 5).
POSTOPERATIVE MANAGEMENT:
After the operation, all the patients were fixed in ankle extension position with a short leg plaster for 4 weeks, and then fixed with lower-limb ankle walking braces to guide functional rehabilitation exercise and lower-limb muscle contraction and rupture to prevent muscle atrophy. After 6 weeks, the patients walked on the floor with crutches and wearing walking braces, and gradually walked without crutches after 3 months.
:
According to the scale used to judge pain in the clinic, the corresponding scores were given according to pain, function, autonomous activity, and maximum walking distance. According to the clinical judgment, 90~100 points indicates “excellent”, 75~89 indicates “good”, 50~74 indicates “fair”, and less than 50 points indicates “poor”.
:
During clinical application, the patients turned their backs to the graduated side and marked the corresponding position on the ruler that represents the degree of pain. The doctor gave a score based on the position marked by the patient. 0~2 means “excellent”, 3~5 is “good”, 6~8 is “fair”, and greater than 8 is “poor”. Before and after clinical treatment, the same method was used to make a more objective score, and the treatment efficacy was objectively evaluated.
:
Excellent: The patient has no discomfort, walks normally, has strong lifting, no significant abnormal muscle strength, the reduction of calf girth is not more than 1 cm, and dorsiflexion or plantar flexion angle is not more than 5°. Good: The patient has mild discomfort, slightly abnormal walking, weak heel lifting, and weaker muscle strength than on the healthy side. The reduction of calf girth is less than 3 cm, dorsal extension angle is decreased by 5°~10°, and metatarsal flexion angle is decreased by 5°~15°. Poor: The patient has obvious discomfort, lameness, inability to lift the heel, and muscle strength decreased significantly, and the reduction of calf girth is more than 3 cm, dorsal extension angle is decreased by more than 10°, and metatarsal flexion angle is decreased by more than 15°.
STATISTICAL ANALYSIS:
SPSS software (version 18.0) was used for statistical analysis. The independent-sample
Results
The average age of the 20 patients was 40 years old (range, 27–57), with an average BMI of 23.1 (range, 19.5–27.5). There were 12 females and 8 males. No complications were identified in this retrospective analysis, including cases of postoperative wound infections and tendon ruptures. Then, we evaluated the situation of these 2 groups of patients from the operation time, VAS, AOFAS ankle-hindfoot score, and Arner-Lindholm standard. The results showed that the average duration of surgery in the suture anchor group was 47.1 min (range, 38–56), which was shorter than that in the allogeneic tendon group (59.5 min) (range, 49–69). The averaged VAS was notably decreased, from 7.6 before the operation to 1.0 at the last visit after the operation, while AOFAS was increased from 47.2 before the operation to 86.3 after the operation. Arner-Lindholm evaluation showed 7 “excellent” and 3 “good” results. In the allogeneic tendon group, the averaged VAS was markedly decreased from 7.7 before surgery to 1.6 after surgery; the averaged AOFAS was increased from 49.4 before surgery to 81.9 after surgery, and the Arner-Lindholm evaluation showed 5 “excellent” and 5 “good”. Thus, the performance of suture anchors is better than that of allogenic tendon suture for Haglund syndrome surgery.
Discussion
Haglund syndrome remains a major challenge for orthopedics [27]. To discover more efficient and practical surgical methods, we designed experiments and explored the clinical application of the technique with suture anchors and allograft tendons. We found that the allogeneic tendon group had worse outcomes than the suture anchor group, and the operation time was generally longer than that of the anchor group, which lowered the overall satisfaction of the patients in this group. In contrast, for the suture anchor, the operation time was shorter and the overall satisfaction of the entire group was significantly better.
Posterior calcaneal decompression and calcaneus osteotomy are the basic methods of surgical treatment of Haglund syndrome. Prior to 2010, the traditional single-row Achilles tendon repair technique was the most commonly used surgical method [16], but the literature reported that this surgical method has some disadvantages, such as high recurrence rates, unstable Achilles tendon, Achilles tendon rupture, and residual heel pain, which limits the use of this technique [28]. It is reported in the literature that at least 2 anchors are used for single-row repair after the Achilles tendon is separated, and the postoperative functional score is significantly better than that with 1 anchor [29]. In the present study, the sutures on each anchor were tied to each other through a double-row suture technique, which provides a larger contact area between the tendon and the bone surface, thereby accelerating the healing process [30,31]. This method does not need a second operation; it is a simple operation and without special instruments, and it is especially suitable for small incisions. No additional incisions are needed, which reduces surgical trauma and avoids the risk of soft-tissue necrosis, infection, and fracture of the lateral wall of the calcaneus. It is worth mentioning that although the postoperative X-ray film showed that the insertion of the anchor was too shallow, there was no re-rupture of the Achilles tendon and no migration or withdrawal of the anchor position after nearly 1 year of follow-up, which fully shows the reliability of the suture anchor.
Previous research showed the clinically excellent and good rate of incision for Haglund syndrome is 69%–76%, and the follow-up time was 2–5 years, but the effect is not ideal, mainly due to incomplete cleaning during the operation and improper selection of the incision [32]. The purpose of this incision is to thoroughly remove the abnormal posterior superior calcaneal process and the posterior inflammatory bursa of the Achilles tendon, and it thus facilitates the removal of calcified tissues [33]. Commonly, surgeons can choose the lateral longitudinal incision, the medial incision, the J-shaped incision, the medial and lateral joint incision, or the central longitudinal incision directly. Clinical experiments have shown that the posterolateral longitudinal incision is more conducive to complete excision of the osteosynthesis, and it is more convenient to treat the degenerated tissue of the Achilles tendon and remove the calcification point [34]. Even so, for patients with poor condition of the lateral wound, a medial incision can be used. However, for patients with poor skin conditions, the choice of open surgery should be carefully considered, as it can easily increase postoperative complications such as skin infection, necrosis, and effusion. Due to the superficial surgical area and large trauma, as well as the inconvenience of measuring the calcaneus posterior angle and the friction of heel shoes during the operation, patients are prone to the typical complications of hindfoot surgery such as poor incision healing, numbness, and rupture of the Achilles tendon [8].
In order to improve this research, there are several problems that need special attention. First, the tendinous tissue to the bone surface insertion is a thin connective tissue structure, the blood transport capacity is poor, and incision skin edge necrosis easily occurs after the operation, and thus does not dissociate widely under the skin during the operation [35]. Moreover, to prevent secondary infection, multiple impact tests are needed to guide the osteotomy range to ensure the anchors completely remove the prominent bone nodules [36]. After the osteotomy surface is flattened during the operation, it is necessary to perform repeated palpations to ensure that all marginal osteophytes are removed. The diseased Achilles tendon and ectopic ossification tissue in the Achilles tendon should be completely removed to decompress the retrocalcaneal space and provide the optimal prognosis.
The present study has certain limitations. Previous research has shown it takes 6 months to 2 years for patients who have undergone an operation to fully recover [16]. To assess the greatest benefit of surgery, longer follow-up may be required. Secondly, the inclusion criteria resulted in a relatively small sample size, which may have been insufficient to accurately assess factors related to the experiment in terms of demography. Finally, this was a retrospective study from a single center, which may have created biases in selection and observation. Subsequent studies with longer follow-up and larger sample sizes are required to evaluate anchor sutures and tendon sutures in the treatment of Haglund syndrome.
Conclusions
We found that the suture anchor is more suitable than allogeneic tendon suture for Haglund surgery.
Figures
 Figure 1. (A, B) Side view of an ankle radiograph of a patient showing Haglund deformity before surgery.
Figure 1. (A, B) Side view of an ankle radiograph of a patient showing Haglund deformity before surgery. 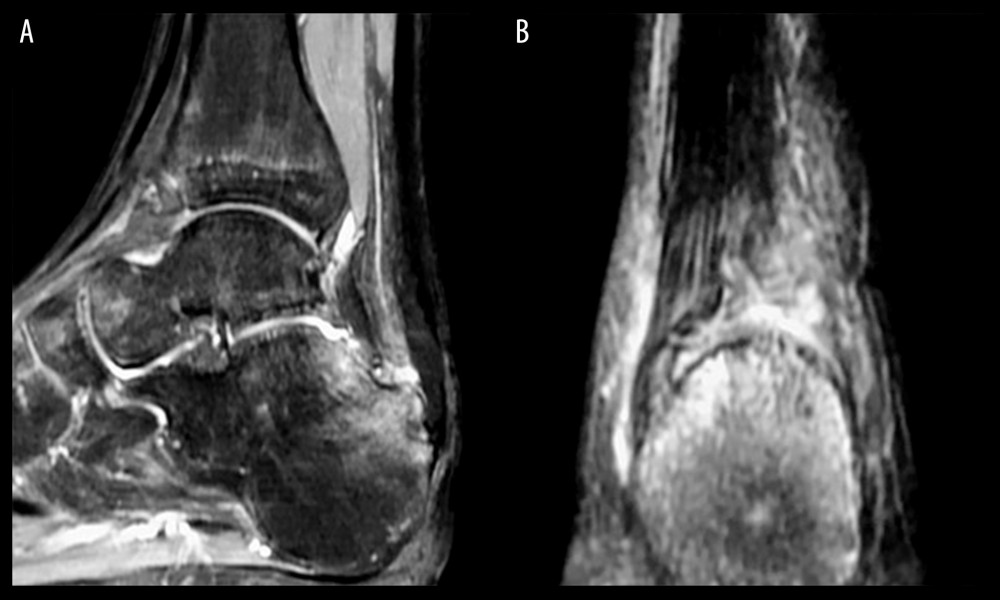 Figure 2. Ankle MRI of a patient with Haglund deformity before surgery. (A) Sagittal image showing the distal side of the Achilles tendon. (B) Coronal image.
Figure 2. Ankle MRI of a patient with Haglund deformity before surgery. (A) Sagittal image showing the distal side of the Achilles tendon. (B) Coronal image. 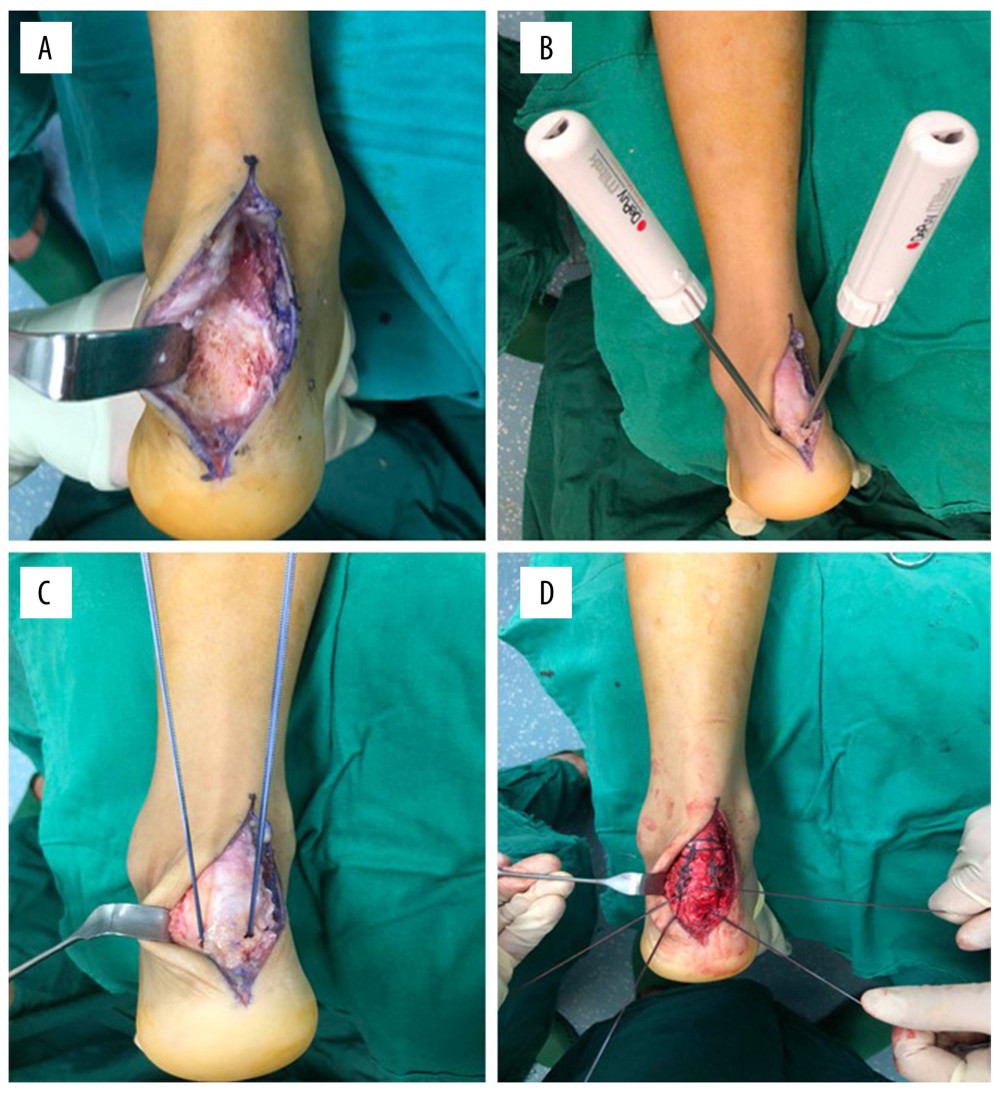 Figure 3. Suture using suture anchor. (A) The Achilles tendon was completely separated, and the calcaneus protrusion was removed. (B) Two suture anchors were inserted. (C) The tendon was repaired with double-row suture. (D) Suturing was complete.
Figure 3. Suture using suture anchor. (A) The Achilles tendon was completely separated, and the calcaneus protrusion was removed. (B) Two suture anchors were inserted. (C) The tendon was repaired with double-row suture. (D) Suturing was complete. 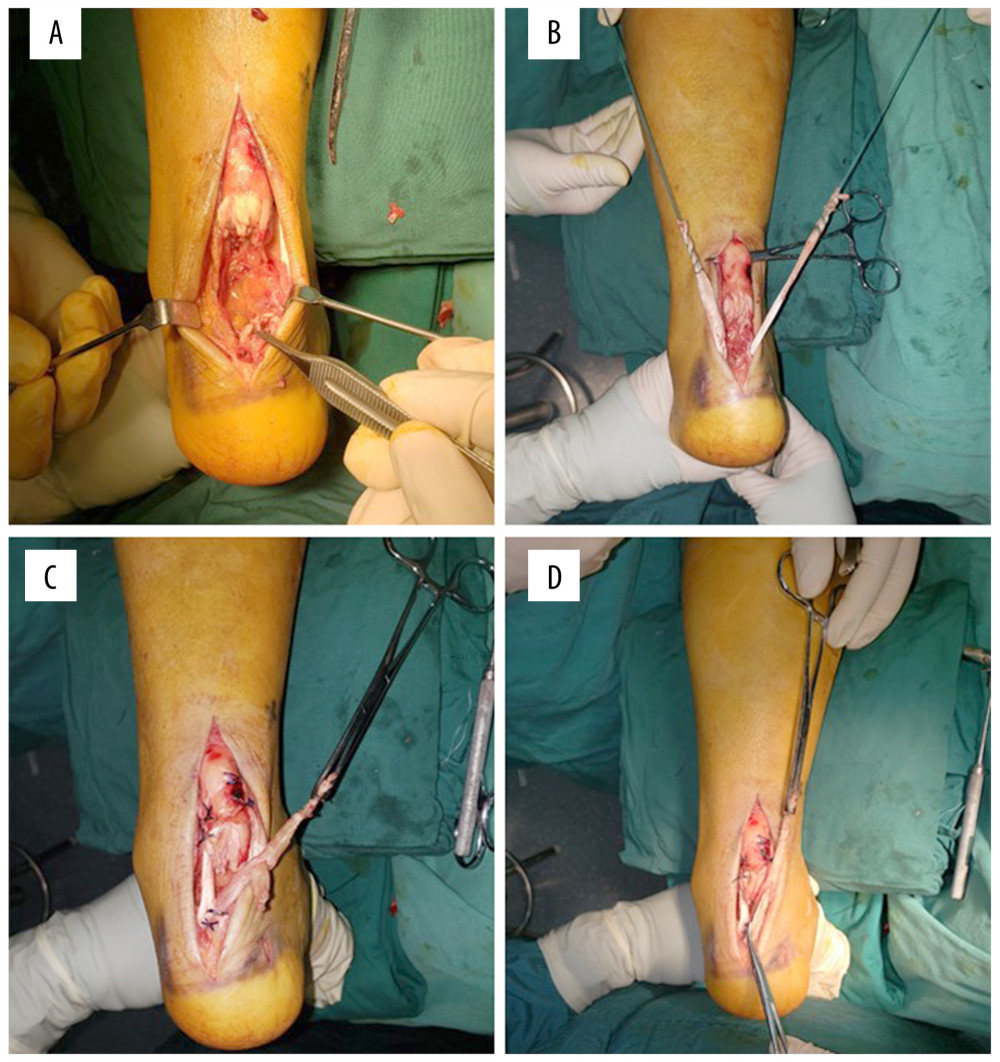 Figure 4. Suturing using allogenic tendon suture. (A) The Achilles tendon was completely separated, and the calcaneus protrusion was removed. (B) Allogeneic tendon was implanted. (C) Suturing was performed. (D) Suturing was complete.
Figure 4. Suturing using allogenic tendon suture. (A) The Achilles tendon was completely separated, and the calcaneus protrusion was removed. (B) Allogeneic tendon was implanted. (C) Suturing was performed. (D) Suturing was complete.  Figure 5. (A, B) Postoperative X-ray of anchor implantation in one patient.
Figure 5. (A, B) Postoperative X-ray of anchor implantation in one patient. Tables
Table 1. Demographic data.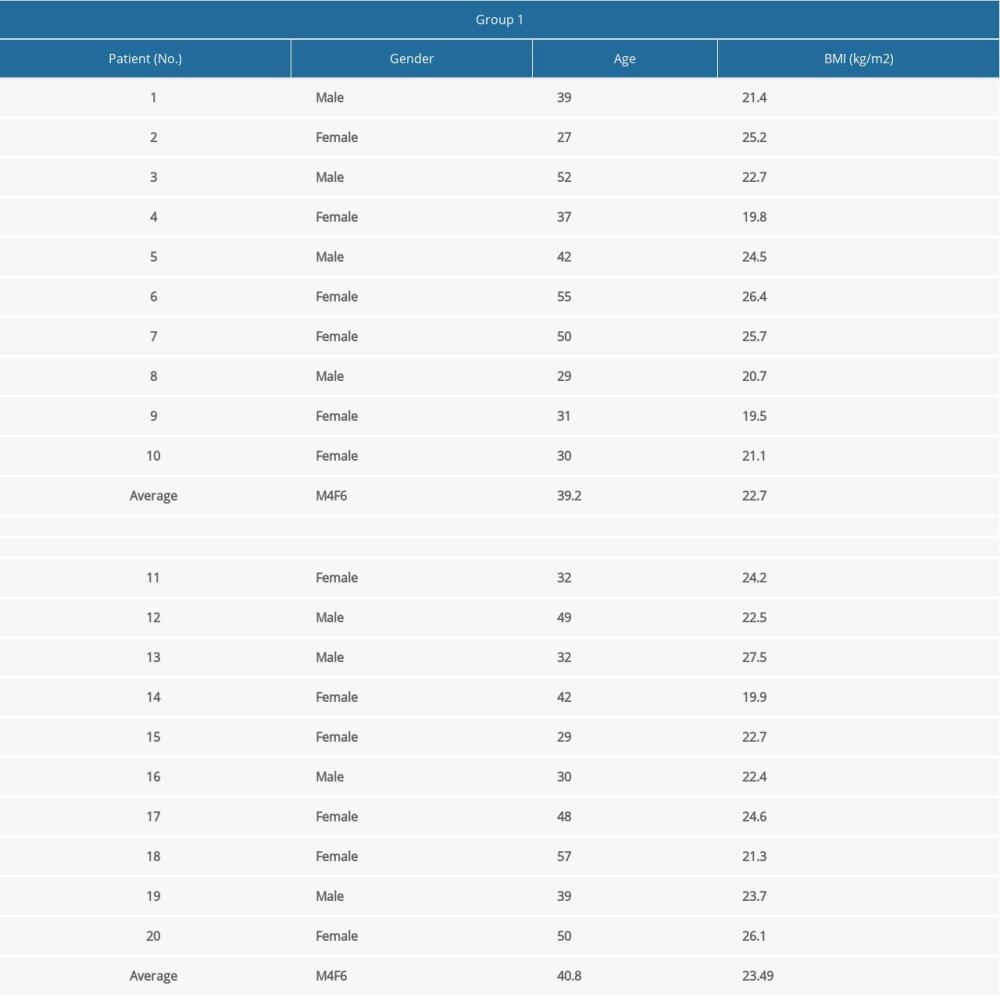
References
1. Vega J, Baduell A, Malagelada F, Endoscopic Achilles Tendon Augmentation With Suture Anchors After Calcaneal Exostectomy in Haglund syndrome: Foot Ankle Int, 2018; 39; 551-59
2. Lawrence DA, Rolen MF, Morshed KA, MRI of heel pain: Am J Roentgenol, 2013; 200(4); 845-55
3. Kraemer R, Wuerfel W, Lorenzen J, Analysis of hereditary and medical risk factors in Achilles tendinopathy and Achilles tendon ruptures: A matched pair analysis: Arch Orthop Trauma Surg, 2012; 132(6); 847-53
4. Irwin TA, Current concepts review: Insertional Achilles tendinopathy: Foot Ankle Int, 2010; 31(10); 933-39
5. Weiss E, Calcaneal spurs: Examining etiology using prehistoric skeletal remains to understand present day heel pain: Foot (Edinb), 2012; 22(3); 125-29
6. Maffulli N, Denaro V, Loppini M, Haglund’s deformity: Foot Ankle Int, 2012; 33(9); 807-8
7. Thomas JL, Christensen JC, Kravitz SR, The diagnosis and treatment of heel pain: A clinical practice guideline-revision 2010: J Foot Ankle Surg, 2010; 49; S1-19
8. Schneider W, Niehus K, Knahr K, Haglund’s syndrome: Disappointing results following surgery – a clinical and radiographic analysis: Foot Ankle Int, 2000; 21(1); 26-30
9. Longo UG, Ronga M, Maffulli N, Achilles tendinopathy: Sports Med Arthrosc Rev, 2018; 26; 16-30
10. Heckman DS, Gluck GS, Parekh SG, Tendon disorders of the foot and ankle, part 2: Achilles tendon disorders: Am J Sports Med, 2009; 37(6); 1223-34
11. Kennedy JC, Willis RB, The effects of local steroid injections on tendons: A biomechanical and microscopic correlative study: Am J Sports Med, 1976; 4(1); 11-21
12. Knobloch K, Drug-induced tendon disorders: Adv Exp Med Biol, 2016; 920; 229-38
13. Sammarco GJ, Taylor AL, Operative management of Haglund’s deformity in the nonathlete: A retrospective study: Foot Ankle Int, 1998; 19(11); 724-29
14. Watson AD, Anderson RB, Davis WH, Comparison of results of retrocalcaneal decompression for retrocalcaneal bursitis and insertional achilles tendinosis with calcific spur: Foot Ankle Int, 2000; 21; 638-42
15. Ahn JH, Ahn CY, Byun CH, Operative treatment of Haglund syndrome with central Achilles tendon-splitting approach: J Foot Ankle Surg, 2015; 54(6); 1053-56
16. Ballal MS, Walker CR, Molloy AP, The anatomical footprint of the Achilles tendon: A cadaveric study: Bone Joint J, 2014; 96-B(10); 1344-48
17. Kuru T, Mutlu İ, Suture anchor fixation may be an alternative to tension band wiring in olecranon fractures: Finite element analysis: Jt Dis Relat Surg, 2020; 31(2); 238-45
18. Bilge A, Kuru T, Results of surgical management of Achilles tendon rupture using the modified Lindholm procedure: Cureus, 2020; 12; e9159
19. Möller M, Movin T, Granhed H, Acute rupture of tendon Achillis. A prospective randomised study of comparison between surgical and non-surgical treatment: J Bone Joint Surg Br, 2001; 83(6); 843-48
20. Möller M, Movin T, Granhed H, Acute rupture of tendon Achillis. A prospective randomised study of comparison between surgical and non-surgical treatment: J Bone Joint Surg Br, 2001; 83(6); 843-48
21. Lu CC, Cheng YM, Fu YC, Angle analysis of Haglund syndrome and its relationship with osseous variations and Achilles tendon calcification: Foot Ankle Int, 2007; 28(2); 181-85
22. Chang CD, Wu JS, MR Imaging findings in heel pain: Magn Reson Imaging Clin N Am, 2017; 25(1); 79-93
23. Sella EJ, Caminear DS, McLarney EA, Haglund’s syndrome: J Foot Ankle Surg, 1998; 37(2); 110-73
24. Pauker M, Katz K, Yosipovitch Z, Calcaneal ostectomy for Haglund disease: J Foot Surg, 1992; 31(6); 588-89
25. Sung YT, Wu JS, The Visual Analogue Scale for Rating, Ranking and Paired-Comparison (VAS-RRP): A new technique for psychological measurement: Behav Res Methods, 2018; 50(4); 1694-715
26. Aktas S, Kocaoglu B, Open versus minimal invasive repair with Achillon device: Foot Ankle Int, 2009; 30(5); 391-97
27. Kang S, Thordarson DB, Charlton TP, Insertional Achilles tendinitis and Haglund’s deformity: Foot Ankle Int, 2012; 33(6); 487-91
28. Jiang Y, Li Y, Tao T, The double-row suture technique: A better option for the treatment of Haglund syndrome: Biomed Res Int, 2016; 2016 1895948
29. Beitzel K, Mazzocca AD, Obopilwe E, Biomechanical properties of double- and single-row suture anchor repair for surgical treatment of insertional Achilles tendinopathy: Am J Sports Med, 2013; 41(7); 1642-48
30. Lo IK, Burkhart SS, Double-row arthroscopic rotator cuff repair: Re-establishing the footprint of the rotator cuff: Arthroscopy, 2003; 19(9); 1035-42
31. Jiang Y, Li Y, Tao T, The Double-Row suture technique: A better option for the treatment of Haglund syndrome: Biomed Res Int, 2016; 2016 1895948
32. Hunt KJ, Anderson RB, Heel pain in the athlete: Sports Health, 2009; 1(5); 427-34
33. Myerson MS, McGarvey W, Disorders of the Achilles tendon insertion and Achilles tendinitis: Instr Course Lect, 1999; 48; 211-18
34. McGarvey WC, Palumbo RC, Baxter DE, Insertional Achilles tendinosis: Surgical treatment through a central tendon splitting approach: Foot Ankle Int, 2002; 23(1); 19-25
35. Xia Z, Yew AKS, Zhang TK, Surgical correction of Haglund’s triad using a central tendon-splitting approach: A retrospective outcomes study: J Foot Ankle Surg, 2017; 56(6); 1132-38
36. Miller AE, Vogel TA, Haglund’s deformity and the Keck and Kelly osteotomy: Aa retrospective analysis: J Foot Surg, 1989; 28(1); 23-29
Figures
 Figure 1. (A, B) Side view of an ankle radiograph of a patient showing Haglund deformity before surgery.
Figure 1. (A, B) Side view of an ankle radiograph of a patient showing Haglund deformity before surgery.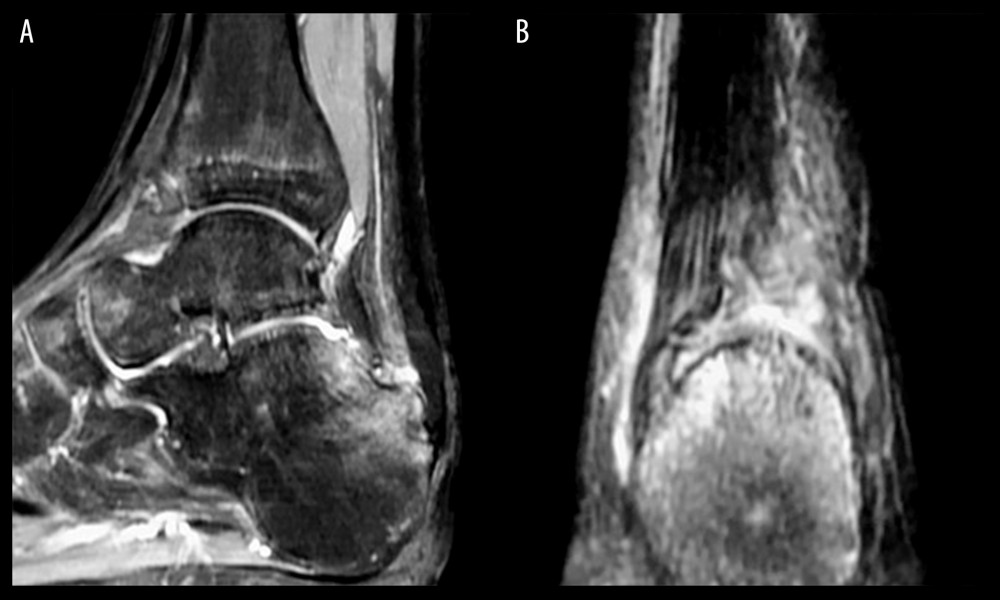 Figure 2. Ankle MRI of a patient with Haglund deformity before surgery. (A) Sagittal image showing the distal side of the Achilles tendon. (B) Coronal image.
Figure 2. Ankle MRI of a patient with Haglund deformity before surgery. (A) Sagittal image showing the distal side of the Achilles tendon. (B) Coronal image.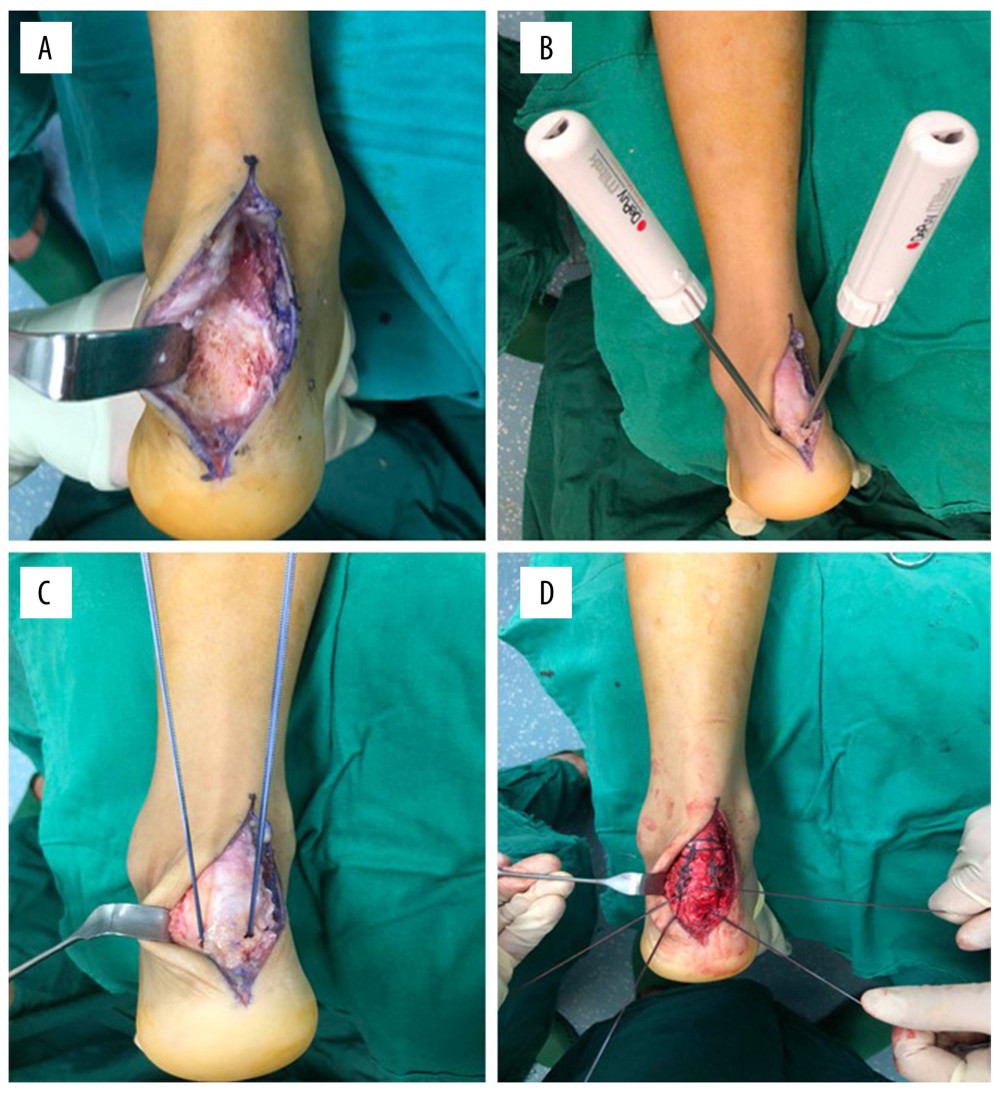 Figure 3. Suture using suture anchor. (A) The Achilles tendon was completely separated, and the calcaneus protrusion was removed. (B) Two suture anchors were inserted. (C) The tendon was repaired with double-row suture. (D) Suturing was complete.
Figure 3. Suture using suture anchor. (A) The Achilles tendon was completely separated, and the calcaneus protrusion was removed. (B) Two suture anchors were inserted. (C) The tendon was repaired with double-row suture. (D) Suturing was complete.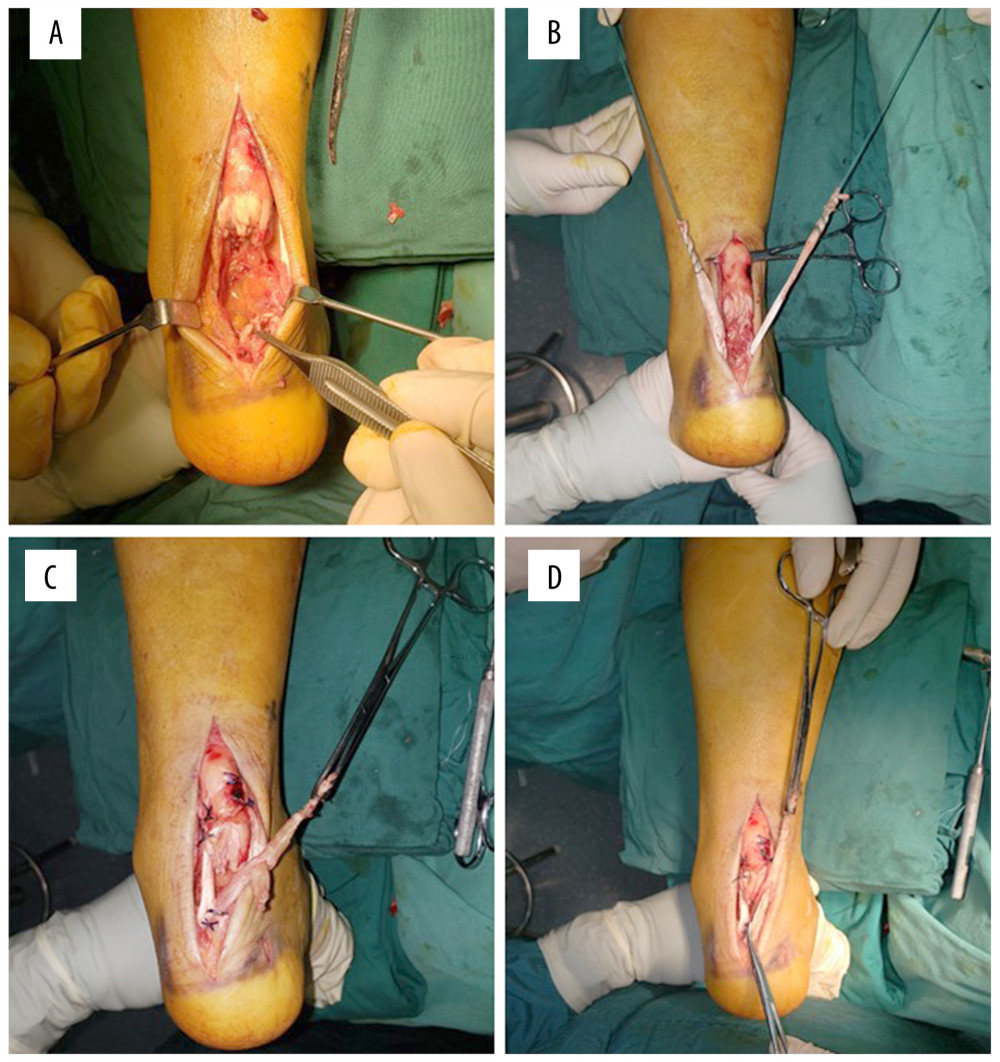 Figure 4. Suturing using allogenic tendon suture. (A) The Achilles tendon was completely separated, and the calcaneus protrusion was removed. (B) Allogeneic tendon was implanted. (C) Suturing was performed. (D) Suturing was complete.
Figure 4. Suturing using allogenic tendon suture. (A) The Achilles tendon was completely separated, and the calcaneus protrusion was removed. (B) Allogeneic tendon was implanted. (C) Suturing was performed. (D) Suturing was complete. Figure 5. (A, B) Postoperative X-ray of anchor implantation in one patient.
Figure 5. (A, B) Postoperative X-ray of anchor implantation in one patient. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








