06 December 2020: Clinical Research
Long-Term Clinical Results of Use of an Anal Fistula Plug for Treatment of Low Trans-Sphincteric Anal Fistulas
Yu Tao1BCDEF, Yi Zheng1BCDEF, Jia Gang Han1ABCDEFG*, Zhen Jun Wang1ACDF, Jin Jie Cui1BF, Bao Cheng Zhao1BF, Xin Qing Yang1ADDOI: 10.12659/MSM.928181
Med Sci Monit 2020; 26:e928181
Abstract
BACKGROUND: An anal fistula plug is a sphincter-sparing procedure that uses biological substances to close an anorectal fistula. This study aimed to evaluate the long-term therapeutic effect of an anal fistula plug procedure in patients with trans-sphincteric fistula-in-ano and to determine the risk factors affecting fistula healing.
MATERIAL AND METHODS: A single-center retrospective study was performed assessing long-term treatment outcomes of patients with low trans-sphincteric anal fistulas who initially underwent anal fistula plug procedures between August 2008 and September 2012. Risk factors affecting fistula healing were identified using univariate and multivariate analyses.
RESULTS: A total of 135 patients who had low trans-sphincteric anal fistulas and underwent anal fistula plug procedures were analysed. The overall healing rate was 56% (75/135) with a median follow-up time of 8 years (range, 72–121 months). The primary reasons for treatment failure were plug extrusion (n=12, 20%) and surgical site infection (n=9, 15%), occurring within 30 days after surgery. Multiple logistic regression analysis showed that the duration of anal fistula ≥6 months was significantly associated with treatment failure using an anal fistula plug (OR=3.187, 95% CI: 1.361–7.466, P=0.008). Of the patients who failed initial treatment with an anal fistula plug, 6 (9%) had anal fistulas that healed spontaneously after 2–3 years without additional treatment.
CONCLUSIONS: As a sphincter-preserving procedure, the anal fistula plug can effectively promote healing of low trans-sphincteric anal fistulas. The long-term efficacy is good and the procedure warrants wider use in clinical practice.
Keywords: Anus Diseases, Fistula, Risk Factors, Adolescent, Anal Canal, Logistic Models, Rectal Fistula, Time Factors, Wound Healing, young adult
Background
An anal fistula is one of the most common diseases of the anus, and although the exact incidence is difficult to ascertain, rates of 2 per 10 000 persons have been reported [1]. Treatment of complex anal fistula remains a challenge. The ideal goal of treatment is to eliminate the anal fistula, while minimizing damage to the anal sphincter and preventing anal incontinence [2]. Surgery has been the mainstay of treatment, and a number of procedures are advocated for the treatment of anal fistulas, with variable healing rates and different treatment effects [3].
Conventional procedures for treating anal fistulas include fistulotomy, fistulectomy, cutting setons, and mucosal advancement flap; the treatment success rate of which has been shown to be up to 90% [4]. However, due to the large trauma of traditional procedures, the anal sphincter is easily injured during surgery, and patients were prone to develop anal dysfunction postoperatively [3,5,6]. To preserve maximum function of the anus and reduce postoperative complications, several sphincter-preserving techniques have been introduced and applied over the past decade [7]. Among these techniques, the anal fistula plug was developed to offer a simple surgical procedure for sphincter-preserving anal fistula treatment, which was first described by Johnson et al. [8] in 2006. Johnson et al. conducted a prospective cohort study to compare treatment effect between the anal fistula plug and fibrin glue, showing that the healing rate of anal fistula plugs was significantly higher than that of fibrin glue (87%
The anal fistula plug is made of biological materials, including acellular dermal, porcine small-intestine submucosa, or new bioabsorbable synthetic materials, which exhibited weak levels of immunogenicity and promoted the formation of new blood vessels and epithelialization, and had some ability to tolerate infection in chronically infected wounds [10–12]. Several studies demonstrated that the anal fistula plug has the characteristic of simple operation, mild pain, preservation of the anal sphincter, and repeatable application [11–13]. In addition, a multicenter randomized controlled trial by Jayne et al. [14] showed that the healing rate and quality of life scores were similar between the anal fistula plugs group and the surgeon’s preference group (including advancement flap, cutting seton, and fistulotomy).
At present, there are many studies involving anal fistula plugs. However, these studies have the limitation of short follow-up time and small sample size, and the long-term success rate of the anal fistula plug procedure remains to be further assessed [15]. Our study aimed to evaluate the long-term therapeutic effect of anal fistula plugs and to determine the risk factors affecting anal fistula healing.
Material and Methods
PATIENTS:
We retrospectively reviewed the clinical data from patients who had a low trans-sphincteric anal fistula and underwent initial anal fistula plug procedures between August 2008 and September 2012. The clinical data were obtained by medical record review.
This study was approved by the Ethics Committee of Beijing Chaoyang Hospital, Capital Medical University, Beijing, China (reference number: 2018-ke-284). All enrolled patients gave informed consent for use of their data in this study.
Patients were eligible for inclusion if they had a trans-sphincteric anal fistula for the first time and were initially treated by anal fistula plugs, had complete case information, and had not received any other treatment previously. The fistulas were classified according to the St James University Hospital (SJUH) [16] and Garg [17] classifications (Table 1). Low trans-sphincteric was defined as a fistula that crosses both sphincters or the external anal sphincter in the lower one-third of the anal canal, and high trans-sphincterics were defined as fistulas that cross both sphincters or the external sphincter in two-thirds of the anal canal [18]. Patients were excluded if they had fistulas related to Crohn’s disease or ulcerative colitis, anorectal tumours, or they had undergone surgical incision and drainage for acute perianal infections within the last 3 months. The physical examination, endoscopy, ultrasonography examination, or magnetic resonance imaging (MRI) were undertaken for all patients to confirm fistula complexity before surgery.
SURGICAL TECHNIQUE:
All patients had digital rectal examinations to ensure the position and direction of the fistula before surgery and were given lactulose oral solution as mechanical bowel preparation on the day before surgery. A single dose of broad-spectrum antibiotic (cefoxitin) was administered to all patients before surgery. All procedures were performed by trained surgeons and were conducted under epidural or lumbar anaesthesia in the left lateral decubitus position.
The anal fistula plugs used consisted of a human acellular dermal matrix and were obtained from Ruinuo (Qingyuanweiye BioTissue Engineering, Ltd., Beijing, China). The technique for insertion of the anal fistula plug was similar to the method described by Song et al. [19]. All surgical procedures were performed independently by the surgeon. The fistula probe or hydrogen peroxide instillation was used to identify fistula tracts and internal and external openings. Gentle mechanical debridement was performed with a blunt curette to remove the necrotic tissue, taking care not to enlarge the track. Hydrogen peroxide and sterile saline were used to repeatedly irrigate the fistula. The anal fistula plug was filled into the fistula and sutured with a figure-eight 2-to-0 Vicryl suture to ensure the plug was fixed in the internal opening of the fistula, avoiding extrusion of the plug. Plugs were trimmed at the external fistula so they were flush with the skin. The external opening was left open to ensure adequate drainage, and the wound was covered with sterile gauzes. All patients were prophylactically given broad-spectrum antibiotic (cefoxitin) and metronidazole for 1 day after surgery, and oral analgesics (e.g., non-steroidal anti-inflammatory drugs) were given as need. Patients were instructed to avoid strenuous activity, sexual activity, exercise, and lifting weights for the first postoperative month.
OUTCOME MEASURES:
All patients were regularly evaluated for healing and recurrence of anal fistula postoperatively by clinical and physical examination and by endoscopy (plus an EAUS if needed) in the outpatient department, according to the following schedule: 1 week, 1–3–6–12 months, and then recommended yearly thereafter. There was no protocol for routine postoperative MRI at our center. Success (fistula healing) was defined as complete resolution of symptoms with no sign of leakage, closure of the internal opening on anoscopy, closure of the external opening on perineal examination, and the absence of infection or abscess formation at a minimum of 6-month follow-up [11]. Treatment failure was defined as anal fistula plug extrusion, persistence of symptoms, or development of an abscess or infection requiring additional surgery [14]. Recurrence was defined as the reappearance of an abscess arising in the area or obvious evidence of fistulation after healing of the anal fistula [11].
STATISTICAL ANALYSIS:
Statistical analysis was performed using SPSS software (version 23.0 for Windows). The
Results
Between August 2008 and September 2012, 135 consecutive patients underwent anal fistula plug procedures for anal fistulas at our institution. The type of anal fistula in all included patients was low trans-sphincteric anal fistula. All anal fistulas were grade I according to Garg classification, and were grade III according to St James’s University Hospital (SJUH) classification.
The median follow-up period was 8 years (range, 72–121 months). The overall healing rate at the time of last follow-up was 56% (75/135), and there were no recurrences in 75 patients with healed anal fistula. Kaplan-Meier survival analysis showed that with the extension of time, the total number of patients who reached the healing standard and were without recurrence gradually increased, and the anal fistula healing rate gradually increased. Finally, the healing rate was stable at about 56% (Figure 1).
The primary reasons for treatment failure using anal fistula plugs were plug extrusion (n=12, 20%) and surgical site infection (n=9, 15%), which occurred within 30 days after surgery. The reasons for treatment failure in other patients were unclear. All 60 patients who failed treatment refused to be treated with an anal fistula plug again: 6 refused further treatment, 33 underwent fistulectomy, 9 underwent the cutting seton procedure, and 12 had no information on further treatment. Of the 33 patients opting for fistulectomy, 32 had fistula healing; all 9 patients who were treated by cutting seton procedure had a successful outcome.
The 135 patients were divided into healed (75 cases) and non-healed groups (60 cases). A comparison of patients in the healed group to the non-healed group showed the following variables to be associated with treatment failure of anal fistula plugs: higher hemoglobin level (
During the follow-up, it was found that the anal fistulas of 6 patients (9%) did not heal after the initial treatment with an anal fistula plug and the anal fistula plugs were extruded, which was considered as treatment failure. However, these 6 patients’ anal fistulas ultimately recovered spontaneously without other treatment, including 3 patients who recovered spontaneously 2 years after surgery and 3 patients who healed spontaneously 3 years after surgery.
From 2008–2012, the annual success rate of anal fistula plugs was 50% (3/3), 62% (24/39), 42% (24/57), 80% (12/15), and 67% (12/18), respectively. With the increase in the number of cases and collective surgical experience, the long-term healing rate of anal fistula plugs shows an increasing trend year-by-year (Figure 2).
Discussion
In our study, 135 patients with trans-sphincteric anal fistulas were treated with anal fistula plugs and had an adequate follow-up, 56% of whom had successful anal fistula closure at the time of the last follow-up evaluation; the median follow-up time was 8 years (range, 72–121 months). The duration of anal fistula ≥6 months was an independent risk factor for treatment failure using the anal fistula plug. Some patients had spontaneous anal fistula healing with initial failure of treatment. This study had the one of the largest sample of patients with low trans-sphincteric anal fistulas had a long follow-up period.
Since the anal fistula plug was initially introduced and recommended for the treatment of anal fistulas, the success rates varied widely in different studies. Han et al. [20] used human acellular dermal matrix plugs to treat complex high trans-sphincteric anal fistulas with a single track, with a median follow-up of 19.5 (range 11–46) months. The results of the study showed that overall success rate was 54.4% (62/114), and no mortalities or major complications were observed. The inexperience of surgeons, smoking, and long distance between external opening and anal verge were possible causes of treatment failure in anal fistula plugs. A multicenter study investigated the long-term efficacy of the Gore Bio-A synthetic plug in the treatment of anal fistulas, and all fistulas were trans-sphincteric and cryptoglandular in origin. After 1 year of follow-up evaluations, the healing rate was 52% (31 of 60 patients) [21]. However, the results of some studies were not encouraging. A multicenter study involving 126 patients reported that the healing rate of anal fistula plug insertion was 24% with a median follow-up time of 13 months [22]. Infection and abscess formation may be significant causes of treatment failure. The randomized clinical trial by Bondi et al. [23] showed that the recurrence rate with the anal fistula plug procedure was significantly higher than with mucosal advancement flap surgery at 12 months after surgery (66%
In our study, the long-term healing rate of anal fistula plugs was 56% with a median follow-up time of 8 years, which is an acceptable result. The anal fistula plug procedure has advantages of simple and repeatable application, minimal discomfort, few complications, and subsequent surgical options if needed [25]. The primary reasons for failure were plug extrusion and infection, which requires us to strengthen the plug fixation during surgery, regularly change dressings postoperatively to ensure unobstructed drainage, and prolong the use of antibiotics if necessary.
A prospective study included 363 patients with a high anal fistula and treated with a cutting seton, and the duration of symptoms varied from 3–21 months. The authors found that there was no significant difference between the duration of anal fistula and the anal fistula healing rate [26]. Another study, by Rosen et al. [27], showed that the median duration of symptoms of the trans-sphincteric fistula-in-ano was 6 (1–84) months, which had no significant correlation with anal fistula healing. In the present study, multivariate analysis showed that the duration of anal fistula ≥ 6 months was an independent risk factor for anal fistula healing, which has not been reported in a previous study. We consider that when anal fistula duration is more than 3 months, and the infection is effectively controlled, treatment with anal fistula plug insertion for patients with anal fistulas should be initiated as early as possible. Because at this point the degree of fibrosis in the lining of the fistula is low, there is less infectious granulation tissue and necrotic substances, and the number of fistula branches is also less. The fistula can be cleaned thoroughly, which is beneficial for healing of the anal fistula. Furthermore, it was recommended in the consensus on the treatment of anal fistula plugs that better control of acute inflammation or infection is more conducive to promoting anal fistula healing [4,9].
In our study, it was worth noting that 6 patients with trans-sphincteric anal fistulas healed spontaneously within 2–3 years after failure of initial treatment, during which time no other treatment was received. Similarly, Stamos et al. [28] reported that the healing time of anal fistulas in some patients after anal fistula plug insertion was significantly prolonged (more than 1 year), and eventually the anal fistula healed without additional treatment. This may be because there is still a small amount of necrotic material or infectious granulation tissue remaining in the fistula postoperatively, which delays healing of the anal fistula. Lenisa et al. [29] noted that persistent discharge of clear fluid can occur for several weeks after plug insertion, which might affect healing of the anal fistula, but does not necessarily indicate that the anal fistula plug treatment has failed. Therefore, we consider that the anal fistula plug may contribute to fistula healing by promoting the reproduction of new vessels and fibroblasts, and resists infection [20]. The reason for spontaneous healing of anal fistulas might be that the effective components, such as growth factors produced by residual biological materials, play a role in promoting the healing of anal fistulas, but the specific mechanism needs to be defined.
As a sphincter-preserving procedure, treatment with anal fistula plug insertion not only promotes anal fistula healing, but also minimizes injury to the anal sphincters and preserves optimal function. Important technical steps in the successful performance of a complex anal fistula plug repair are thorough debridement of the fistula tract, prevention of plug dislodgment, and maintaining drainage [30]. From 2008 to 2012, the healing rate of anal fistula plugs has shown an increasing trend. We consider that with the increase in the number of cases and the proficiency of operative techniques, the healing rate of anal fistula plugs will gradually increase.
This study has some limitations. A major limitation was that this was not a comparative study but rather was a retrospective case series; selection bias was therefore inevitable. Secondly, we used anoscopy and physical examination to confirm the healing, but did not perform MRI. Thirdly, the assessor who evaluated the healing who was clearly non-blinded, so this was necessarily a subjective assessment, which likely added bias. Finally, the lack of data on continence status is a shortcoming.
Conclusions
Among 135 patients with low simple trans-sphincteric anal fistulas treated with anal fistula plugs, the success rate was 56% with a median follow-up of 8 years. The long-term efficacy of the treatment is worthy of recognition. Thus, we suggest that an anal fistula plug is a reasonable option for closure of trans-sphincteric anal fistulas.
Figures
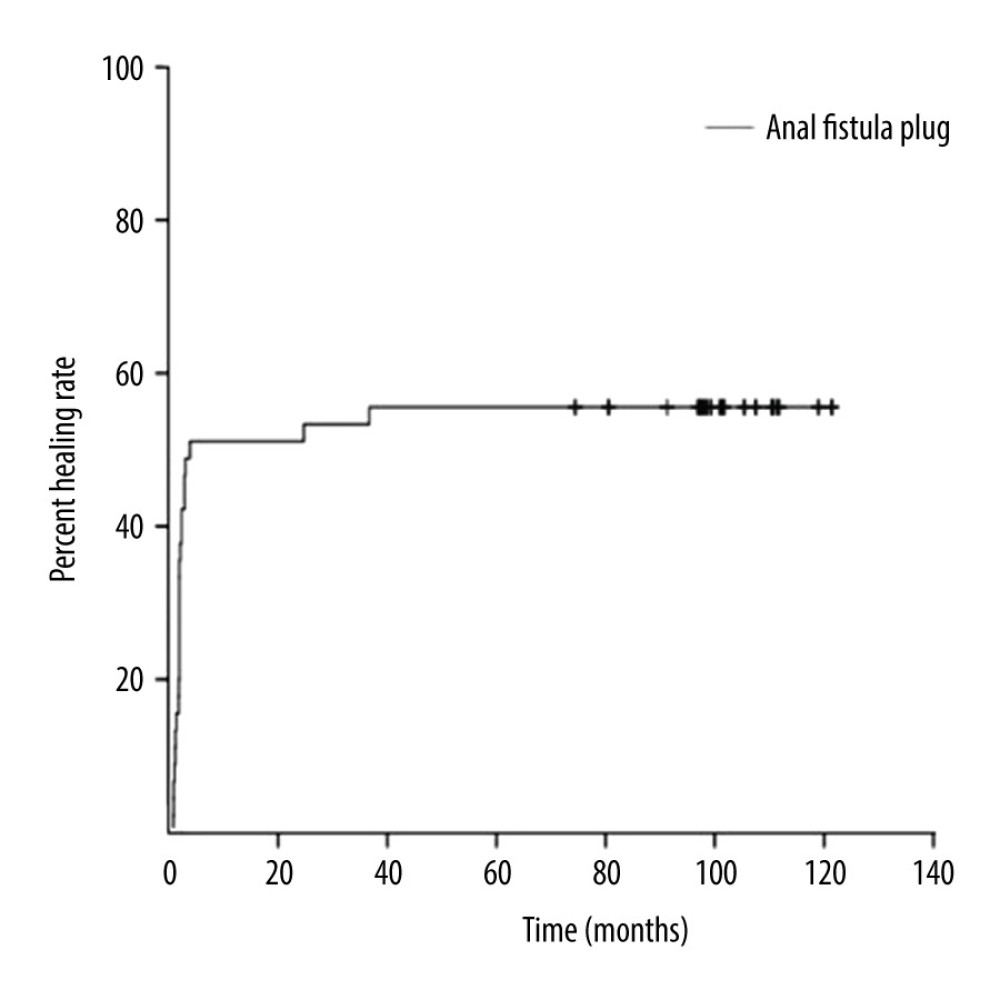 Figure 1. Long-term healing rate of anal fistula plugs for the treatment of trans-sphincteric anal fistulas. Kaplan-Meier survival analysis showed that with the extension of time, the total number of patients reached the healing standard and without recurrence gradually increased, and the anal fistula healing rate gradually increased. Finally, the healing rate was stable at about 56%.
Figure 1. Long-term healing rate of anal fistula plugs for the treatment of trans-sphincteric anal fistulas. Kaplan-Meier survival analysis showed that with the extension of time, the total number of patients reached the healing standard and without recurrence gradually increased, and the anal fistula healing rate gradually increased. Finally, the healing rate was stable at about 56%. 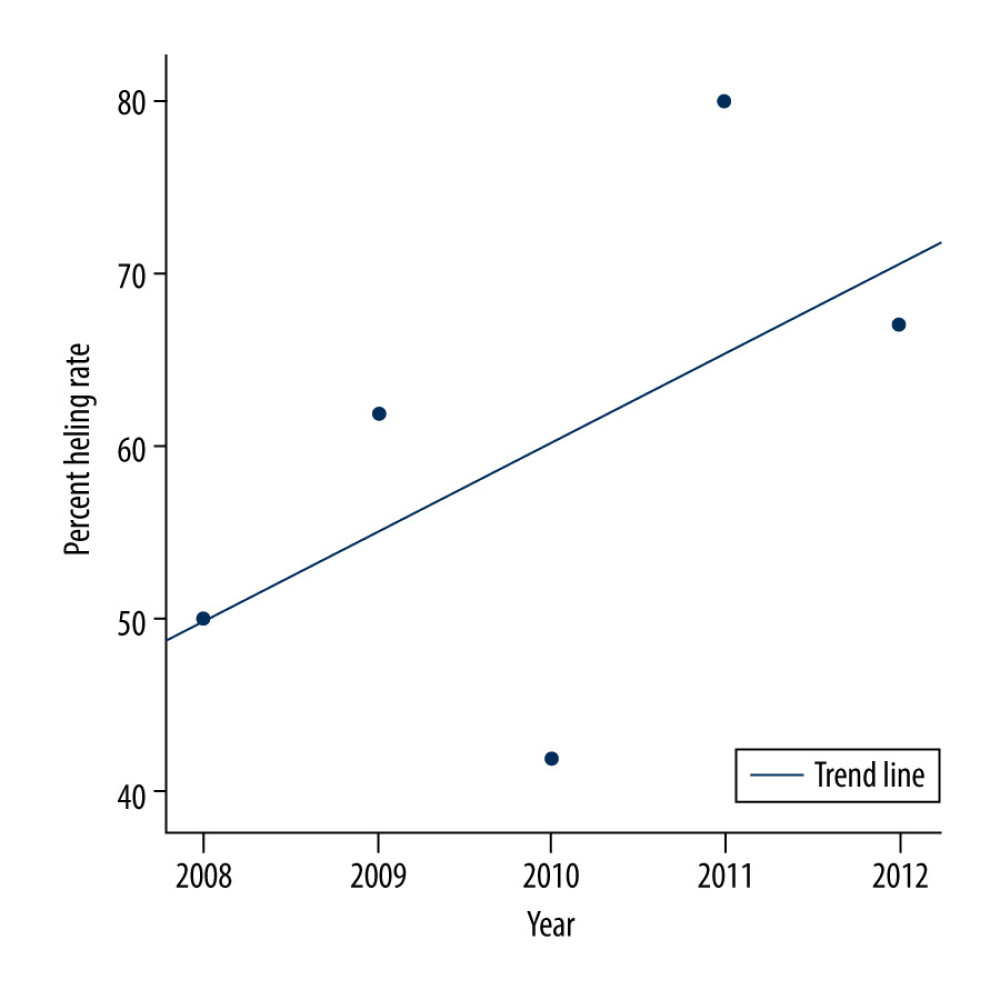 Figure 2. The relationship between the healing rate of an anal fistula plug and year. From 2008–2012, the annual percent healing rate of an anal fistula plug was 50% (3/3), 62% (24/39), 42% (24/57), 80% (12/15), and 67% (12/18), respectively. The long-term healing rate of an anal fistula plug shows an increasing trend year-by-year..
Figure 2. The relationship between the healing rate of an anal fistula plug and year. From 2008–2012, the annual percent healing rate of an anal fistula plug was 50% (3/3), 62% (24/39), 42% (24/57), 80% (12/15), and 67% (12/18), respectively. The long-term healing rate of an anal fistula plug shows an increasing trend year-by-year.. Tables
Table 1. The classifications of anal fistulas. Anal fistulas were classified according to St James University Hospital (SJUH) and Garg classification criteria.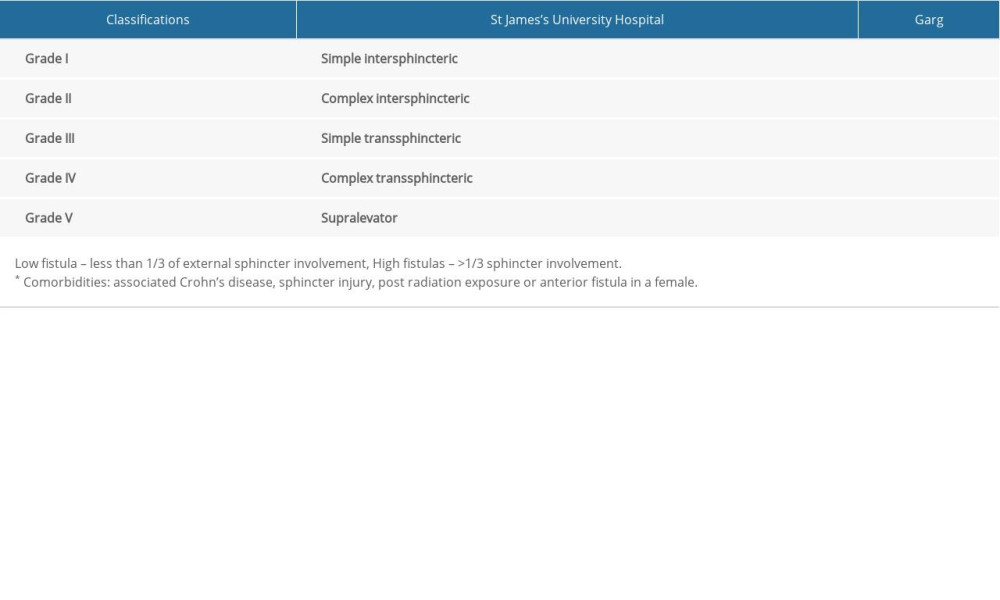 Table 2. Patient characteristics in relation to healed versus non-healed fistulas treated with an anal fistula plug.
Table 2. Patient characteristics in relation to healed versus non-healed fistulas treated with an anal fistula plug.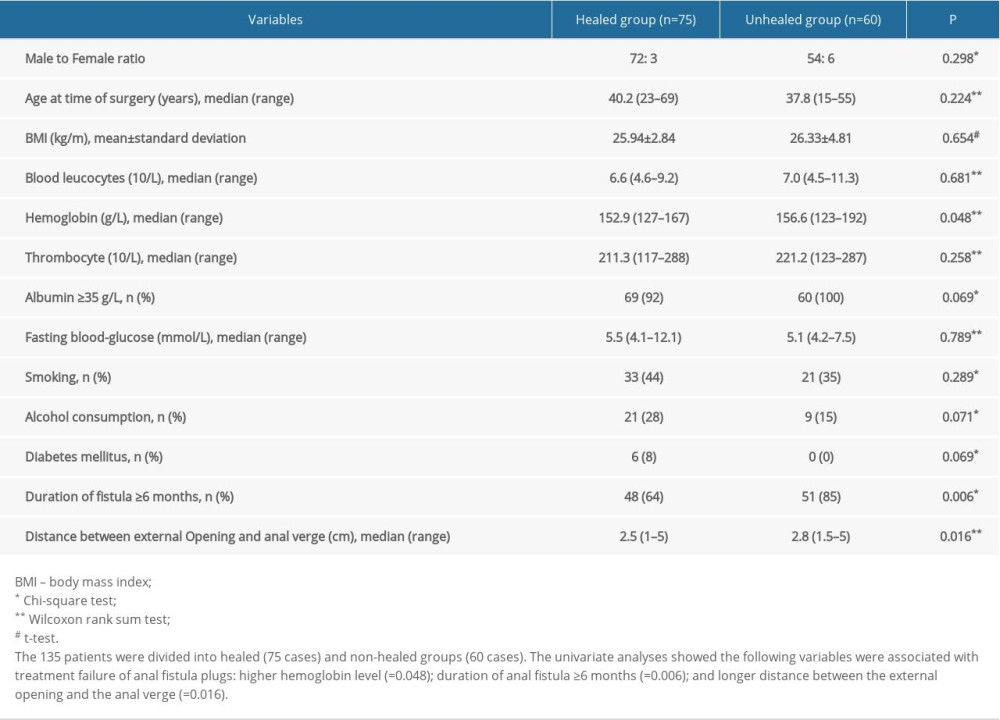 Table 3. Multiple logistic regression analyses of potential predictors of anal fistula plug success.
Table 3. Multiple logistic regression analyses of potential predictors of anal fistula plug success.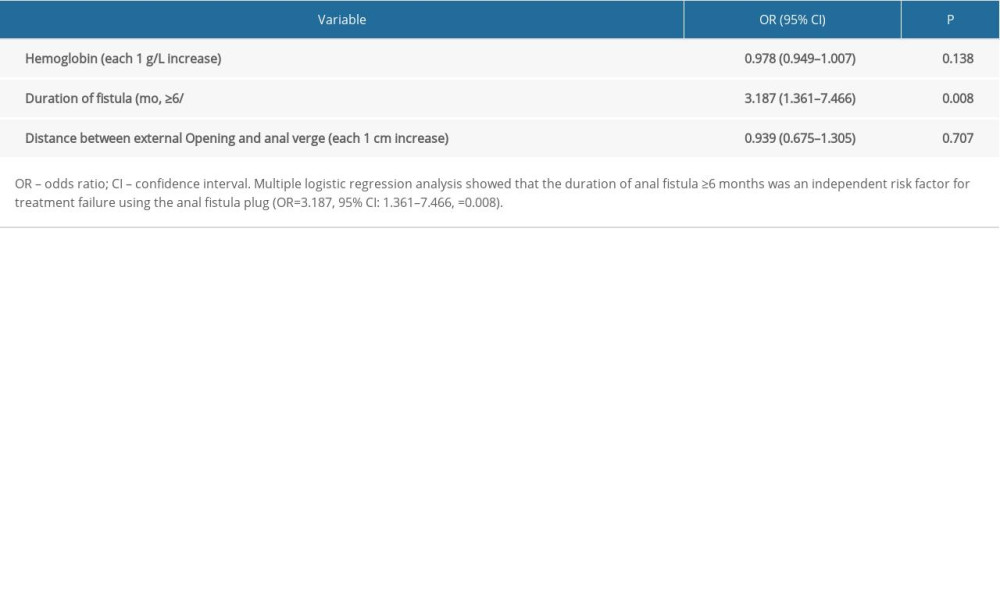
References
1. Sugrue J, Nordenstam J, Abcarian H, Pathogenesis and persistence of cryptoglandular anal fistula: A systematic review: Tech Coloproctol, 2017; 21; 425-32
2. Amato A, Bottini C, De Nardi P, Evaluation and management of perianal abscess and anal fistula: SICCR position statement: Tech Coloproctol, 2020; 24; 127-43
3. Ratto C, Grossi U, Litta F, Contemporary surgical practice in the management of anal fistula: Results from an international survey: Tech Coloproctol, 2019; 23; 729-41
4. Vogel JD, Johnson EK, Morris AM, Clinical practice guideline for the management of anorectal abscess, fistula-in-ano, and rectovaginal fistula: Dis Colon Rectum, 2016; 59; 1117-33
5. Cariati A, Fistulotomy or seton in anal fistula: A decisional algorithm: Updates Surg, 2013; 65; 201-5
6. Litta F, Parello A, De Simone V, Fistulotomy and primary sphincteroplasty for anal fistula: Long-term data on continence and patient satisfaction: Tech Coloproctol, 2019; 23; 993-1001
7. Narang SK, Keogh K, Alam NN, Pathak S, Daniels IR, Smart NJ, A systematic review of new treatments for cryptoglandular fistula in ano: Surgeon, 2017; 15; 30-39
8. Johnson EK, Gaw JU, Armstrong DN: Dis Colon Rectum, 2006; 49; 371-76
9. , The Surgisis AFP anal fistula plug: report of a consensus conference: Colorectal Dis, 2008; 10; 17-20
10. Han JG, Xu HM, Song WL, Histologic analysis of acellular dermal matrix in the treatment of anal fistula in an animal model: J Am Coll Surg, 2009; 208; 1099-106
11. Heydari A, Attina GM, Merolla E, Bioabsorbable synthetic plug in the treatment of anal fistulas: Dis Colon Rectum, 2013; 56; 774-79
12. Cintron JR, Abcarian H, Chaudhry V, Treatment of fistula-in-ano using a porcine small intestinal submucosa anal fistula plug: Tech Coloproctol, 2013; 17; 187-91
13. Xu Y, Tang W, Comparison of an anal fistula plug and mucosa advancement flap for complex anal fistulas: A meta-analysis: ANZ J Surg, 2016; 86; 978-82
14. Jayne DG, Scholefield J, Tolan D, Anal fistula plug versus surgeon’s preference for surgery for trans-sphincteric anal fistula: The FIAT RCT: Health Technol Assess, 2019; 23(21); 1-76
15. Bobkiewicz A, Krokowicz Ł, Borejsza-Wysocki M, Banasiewicz T, A novel model of acellular dermal matrix plug for anal fistula treatment. Report of a case and surgical consideration based on first utility in Poland: Pol Przegl Chir, 2017; 89; 52-55
16. Morris J, Spencer JA, Ambrose NS, MR imaging classification of perianal fistulas and its implications for patient management: Radiographics, 2000; 20; 623-35
17. Garg P, Comparison of preoperative and postoperative MRI after fistula-in-ano surgery: Lessons learnt from an audit of 1323 MRI at a single centre: World J Surg, 2019; 43; 1612-22
18. Malakorn S, Sammour T, Khomvilai S, Ligation of intersphincteric fistula tract for fistula in ano: Lessons learned from a decade of experience: Dis Colon Rectum, 2017; 60; 1065-70
19. Song WL, Wang ZJ, Zheng Y, An anorectal fistula treatment with acellular extracellular matrix: A new technique: World J Gastroenterol, 2008; 14; 4791-94
20. Han JG, Wang ZJ, Zhao BC, Long-term outcomes of human acellular dermal matrix plug in closure of complex anal fistulas with a single tract: Dis Colon Rectum, 2011; 54; 1412-18
21. Herold A, Ommer A, Fürst A, Results of the Gore Bio-A fistula plug implantation in the treatment of anal fistula: A multicentre study: Tech Coloproctol, 2016; 20; 585-90
22. Blom J, Husberg-Sellberg B, Lindelius A, Results of collagen plug occlusion of anal fistula: A multicentre study of 126 patients: Colorectal Dis, 2014; 16; 626-30
23. Bondi J, Avdagic J, Karlbom U, Randomized clinical trial comparing collagen plug and advancement flap for trans-sphincteric anal fistula: Br J Surg, 2017; 104; 1160-66
24. Narang SK, Jones C, Alam NN: Colorectal Dis, 2016; 18; 37-44
25. Narang SK, Keogh K, Alam NN, A systematic review of new treatments for cryptoglandular fistula in ano: Surgeon, 2017; 15; 30-39
26. Shirah BH, Shirah HA, The impact of the outcome of treating a high anal fistula by using a cutting seton and staged fistulotomy on Saudi Arabian patients: Ann Coloproctol, 2018; 34; 234-40
27. Rosen DR, Kaiser AM, Definitive seton management for transsphincteric fistula-in-ano: Harm or charm?: Colorectal Dis, 2016; 18; 488-95
28. Stamos MJ, Snyder M, Robb BW, Prospective multicenter study of a synthetic bioabsorbable anal fistula plug to treat cryptoglandular transsphincteric anal fistulas: Dis Colon Rectum, 2015; 58; 344-51
29. Lenisa L, Espìn-Basany E, Rusconi A, Anal fistula plug is a valid alternative option for the treatment of complex anal fistula in the long term: Int J Colorectal Dis, 2010; 25; 1487-93
30. Köckerling F, Alam NN, Narang SK, Treatment of fistula-in-ano with fistula plug-a review under special consideration of the technique: Front Surg, 2015; 2; 55
Figures
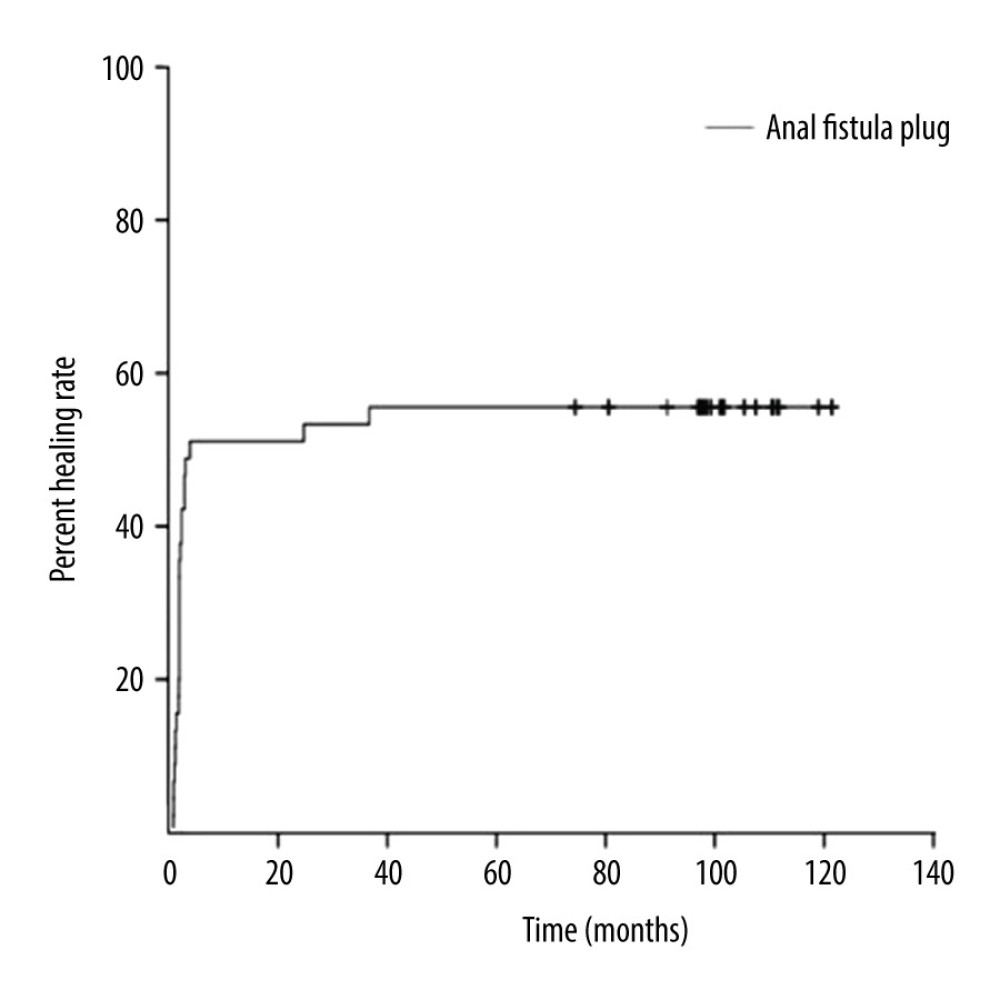 Figure 1. Long-term healing rate of anal fistula plugs for the treatment of trans-sphincteric anal fistulas. Kaplan-Meier survival analysis showed that with the extension of time, the total number of patients reached the healing standard and without recurrence gradually increased, and the anal fistula healing rate gradually increased. Finally, the healing rate was stable at about 56%.
Figure 1. Long-term healing rate of anal fistula plugs for the treatment of trans-sphincteric anal fistulas. Kaplan-Meier survival analysis showed that with the extension of time, the total number of patients reached the healing standard and without recurrence gradually increased, and the anal fistula healing rate gradually increased. Finally, the healing rate was stable at about 56%.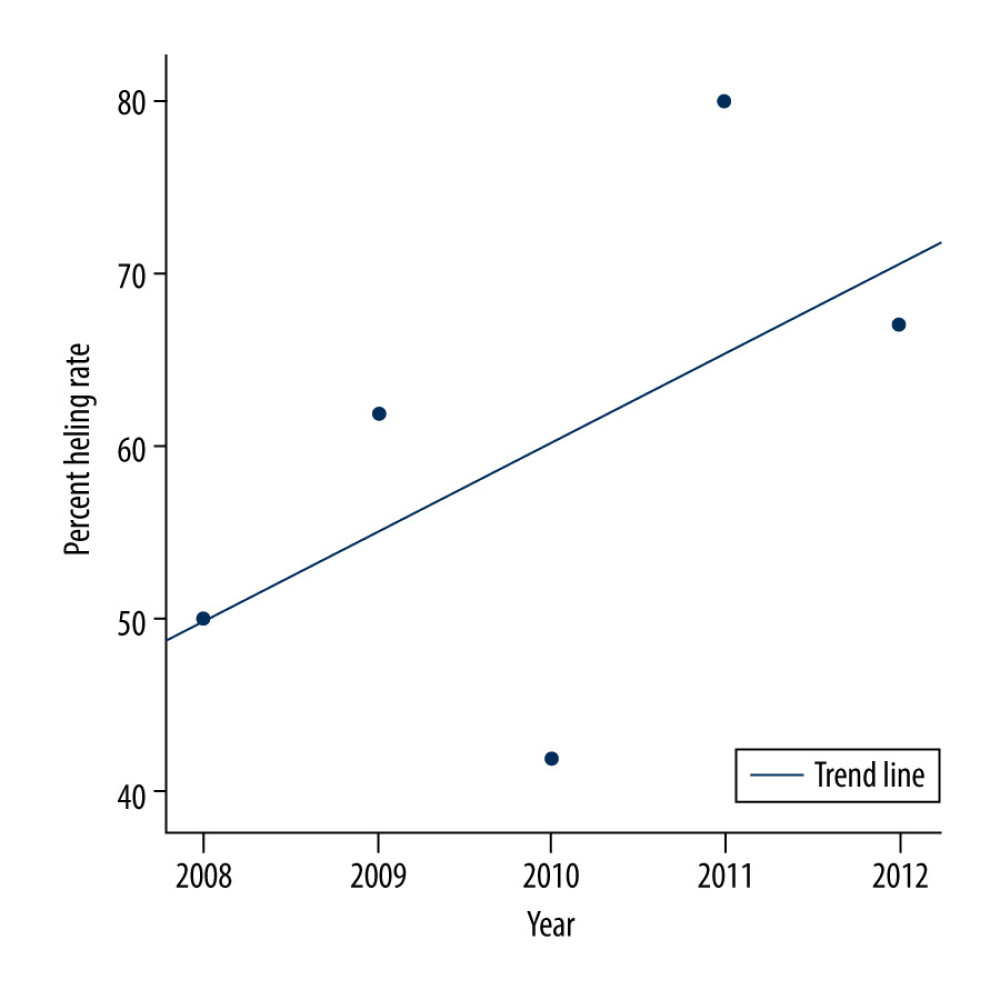 Figure 2. The relationship between the healing rate of an anal fistula plug and year. From 2008–2012, the annual percent healing rate of an anal fistula plug was 50% (3/3), 62% (24/39), 42% (24/57), 80% (12/15), and 67% (12/18), respectively. The long-term healing rate of an anal fistula plug shows an increasing trend year-by-year..
Figure 2. The relationship between the healing rate of an anal fistula plug and year. From 2008–2012, the annual percent healing rate of an anal fistula plug was 50% (3/3), 62% (24/39), 42% (24/57), 80% (12/15), and 67% (12/18), respectively. The long-term healing rate of an anal fistula plug shows an increasing trend year-by-year.. Tables
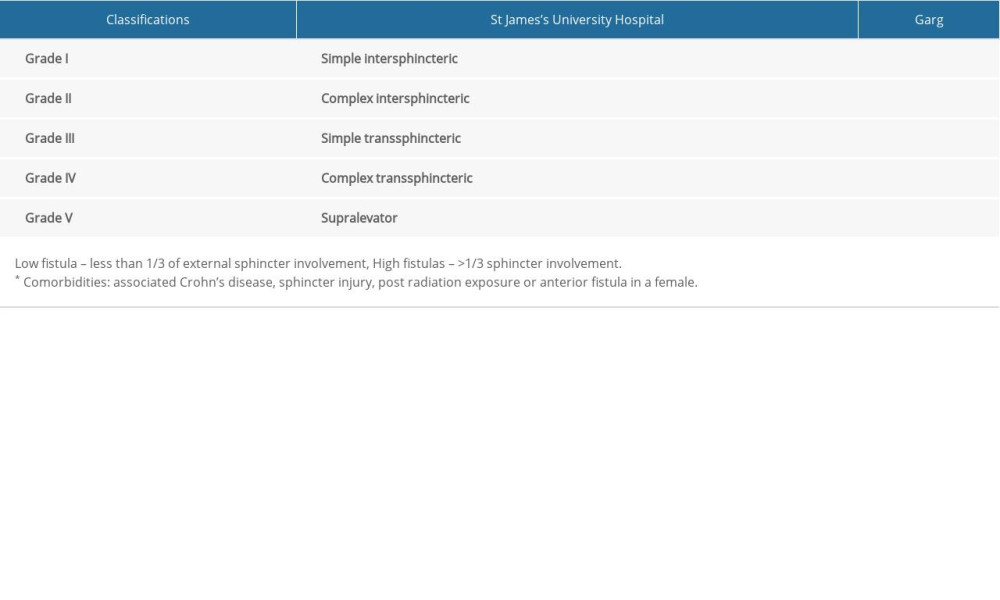 Table 1. The classifications of anal fistulas. Anal fistulas were classified according to St James University Hospital (SJUH) and Garg classification criteria.
Table 1. The classifications of anal fistulas. Anal fistulas were classified according to St James University Hospital (SJUH) and Garg classification criteria.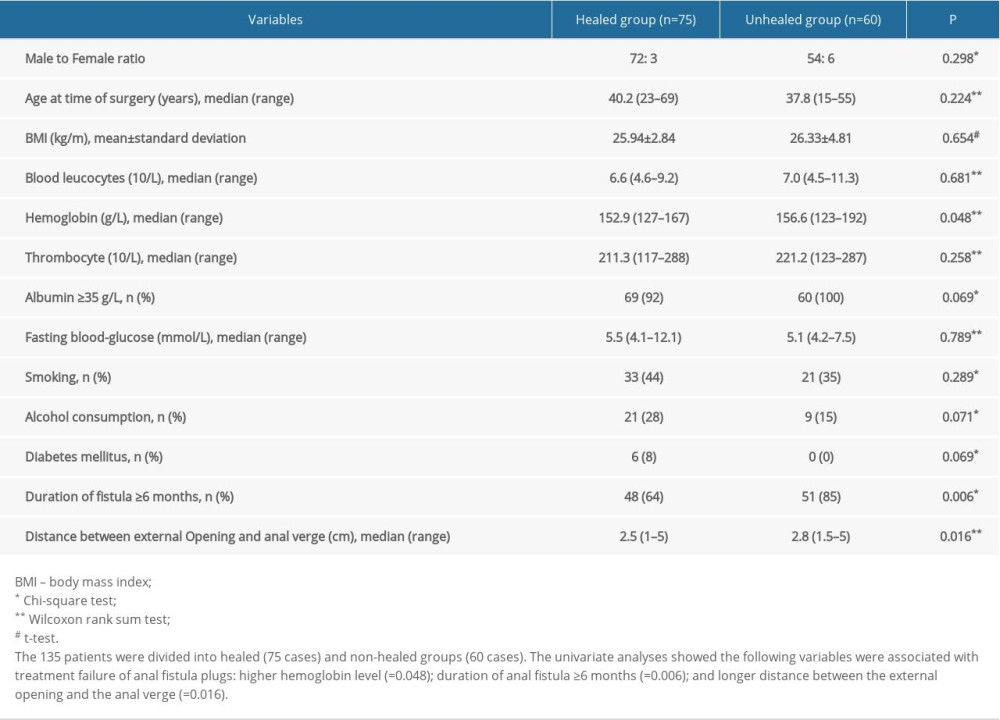 Table 2. Patient characteristics in relation to healed versus non-healed fistulas treated with an anal fistula plug.
Table 2. Patient characteristics in relation to healed versus non-healed fistulas treated with an anal fistula plug.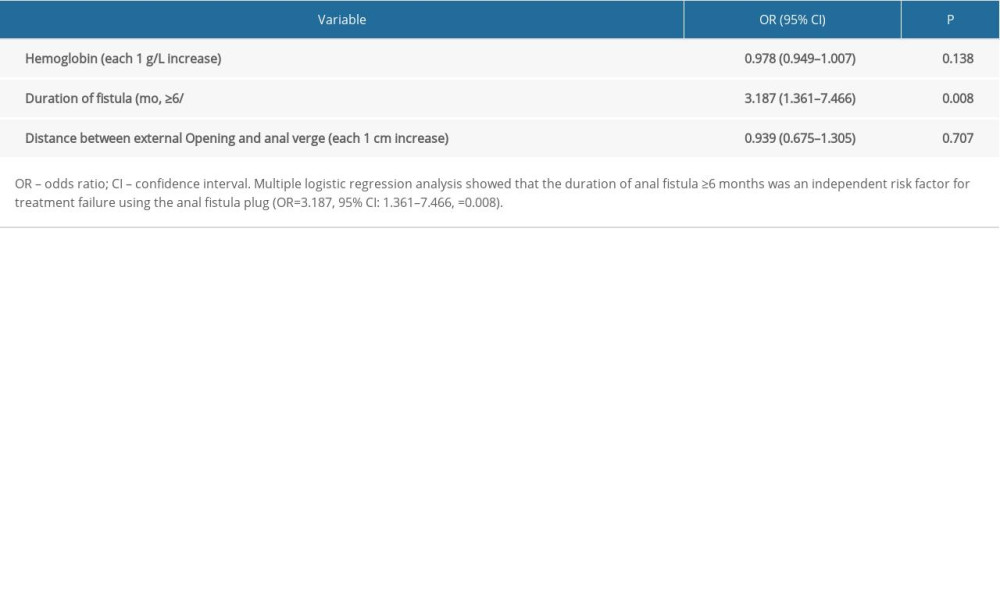 Table 3. Multiple logistic regression analyses of potential predictors of anal fistula plug success.
Table 3. Multiple logistic regression analyses of potential predictors of anal fistula plug success.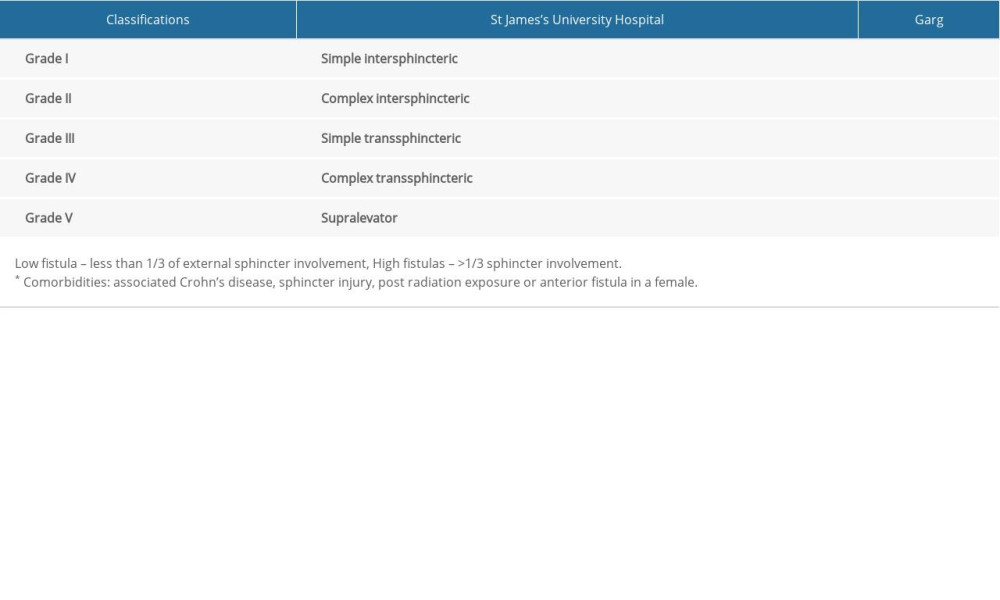 Table 1. The classifications of anal fistulas. Anal fistulas were classified according to St James University Hospital (SJUH) and Garg classification criteria.
Table 1. The classifications of anal fistulas. Anal fistulas were classified according to St James University Hospital (SJUH) and Garg classification criteria.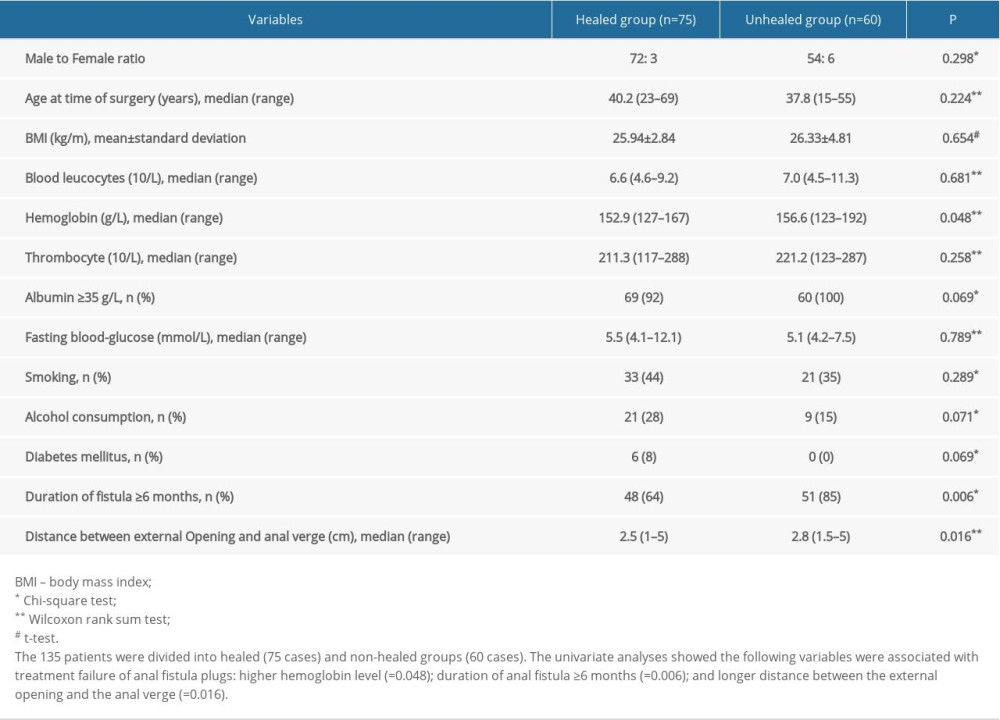 Table 2. Patient characteristics in relation to healed versus non-healed fistulas treated with an anal fistula plug.
Table 2. Patient characteristics in relation to healed versus non-healed fistulas treated with an anal fistula plug.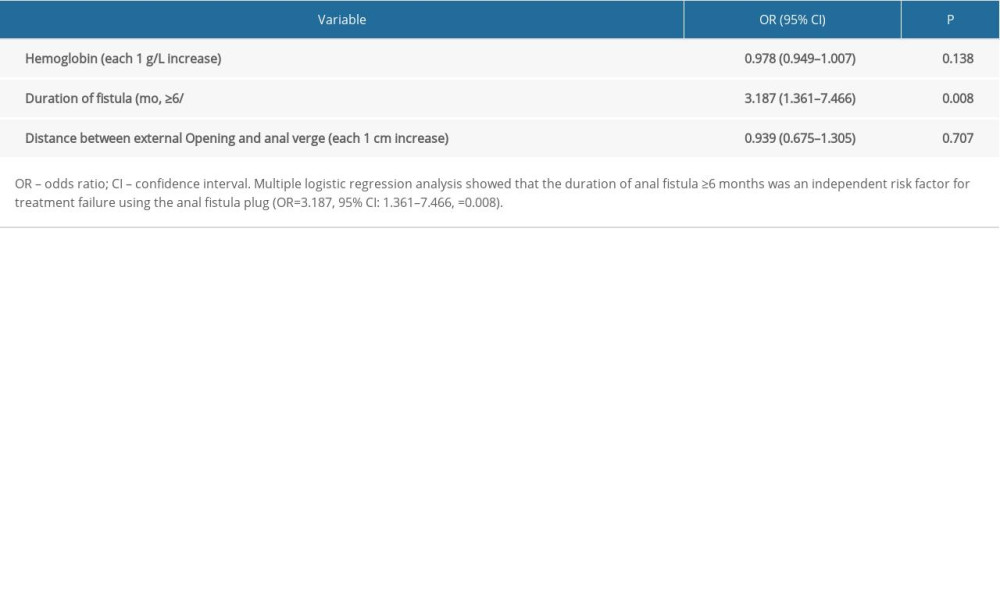 Table 3. Multiple logistic regression analyses of potential predictors of anal fistula plug success.
Table 3. Multiple logistic regression analyses of potential predictors of anal fistula plug success. In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








