15 February 2021: Clinical Research
Comparison of Arthroscopic Surgery Versus Open Surgical Repair of the Anterior Talofibular Ligament: A Retrospective Study of 80 Patients from a Single Center
Bo-Yuan Su1ABG, Shu-Yun Yi2CD, Ting Peng3E, Gang Yi4567F, Lei Zhang4567BCG*DOI: 10.12659/MSM.928526
Med Sci Monit 2021; 27:e928526
Abstract
BACKGROUND: This retrospective study from a single center aimed to compare the safety and clinical outcomes of arthroscopic surgery vs open surgical repair of the anterior talofibular ligament (ATFL).
MATERIAL AND METHODS: We randomly divided 80 patients with ATFL injury divided into 2 groups: an open surgery group and an arthroscopic group. The operation time, intraoperative bleeding volume, and the postoperative recovery time of all patients were analyzed. The anterior displacement and talus tilt angle, the American Orthopedic Foot and Ankle Society Ankle-Hindfoot Score (AOFAS), the Jersey Shore Science Fair (JSSF) ankle-hindfoot scale score, and the Karlsson Ankle Functional Score (KAFS) were compared at 6 months, 1 year, and 2 years after surgery. We collected data on the incidence of postoperative complications during follow-up. All significant results were supported with a P value.
RESULTS: The operation time, intraoperative bleeding volume, and postoperative recovery time in the arthroscopic group were better than in the open group (P<0.05). The AOFAS, JSSF, and KAFS in the arthroscopic group were better than in the open group at 6 months after the operation (P<0.05). The AOFAS, JSSF, and KAFS scale scores were not significantly different between the 2 groups at 1 year and 2 years after the operation (P<0.05).
CONCLUSIONS: The findings from this retrospective study showed that the use of arthroscopic surgical repair of the ATFL is a safe minimally invasive technique with reduced blood loss and surgical duration and good clinical outcomes.
Keywords: Ankle Injuries, Arthroscopy, Lateral Ligament, Ankle, Suture Anchors, Ankle, Ankle Joint, Joint Instability, operative time, Postoperative Complications, Postoperative Period, Talus
Background
Sprained ankle, a common injury that accounts for approximately 9–12% of all orthopedic injuries, has received much attention in recent years. In the United States, there are 2300 sprained ankles reported every day [1,2]. The lateral stability of the ankle joint is maintained by the bone structure, muscle structure, and ligaments, among which the lateral ligaments include the anterior talofibular ligament (ATFL), calcaneofibular ligament and talofibular posterior ligament [3,4]. Due to the characteristics of anatomical structure, the ATFL is the most vulnerable to injury and is affected in different degrees of sprained ankle [5–8]. When the anterior talofibular ligament is injured, most patients receive non-surgical treatment such as rehabilitation functional treatment, while conservative treatment needs more time to restore normal motor function [9–11].
Here, we evaluated the feasibility and safety of arthroscopic technique in repair of the anterior talofibular ligament. Surgical treatment can restore ankle joint stability and function. Some scholars showed that all kinds of open surgical reconstruction of ATFL obtain a satisfactory clinical effect [12,13], but due to the large incision, post-surgical recovery was difficult, especially for the elderly [14,15]. Ankle sprains easily reoccur and cause lateral instability of the ankle [16–18]. Long-term LIA can lead to the traumatic arthritis of the tibiotalar joint and subtalar joint, with pain, swelling, and limited mobility. It not only causes pain and abnormal movement, but also affect the patients’ normal life and imposes an economic burden [19–21]. With the increasing development of arthroscopy technology, some osteologists reported that arthroscopy technique in repair of ATFL had satisfactory clinical effectiveness [22,23]. According to previous studies, arthroscopy technique in repair of ATFL required at least 3 portals, but we treated ATFL arthroscopically with only 2 portals, which had the advantages of convenience, complete exposure, strong stability, and satisfactory recovery after the operation [24].
Therefore, this retrospective study from a single center aimed to compare the safety and clinical outcomes of arthroscopic surgery with open surgical repair of the anterior talofibular ligament (ATL).
Material and Methods
ETHICS STATEMENT:
Ethics approval and the details of patient informed consent were given by the Medical Ethics Committee of Southwest Medical University (reference number KY2019042).
MATERIAL:
We performed retrospective analysis of clinical data of 80 patients in the Affiliated Traditional Chinese Medicine Hospital of Southwest Medical University for ATFL injury from January 2014 to June 2018. The patients were randomly divided into 2 groups with 40 in each group.
Inclusion criteria of patients were: age 18–55 years, recurrent ankle sprain with ineffective conservative treatment, preoperative examination of MRI showed ATFL injury with sufficient residual (Figure 1), ankle arthroscopy confirmed ATFL injury at peroneal end, followed up regularly for more than 2 years.
Exclusion criteria of patients were: tendon reconstruction should be performed because of insufficient stump of ATFL, with other serious ankle diseases or ankle deformity, with fractures around the ankle, revision operation, not suitable for surgery due to infectious disease or chronic wasting disease.
Group A had 23 males and 17 females, age range 18–55 years (mean 38.68±14.23). The ratio of left to right ankle was 22 to 18. The time from injury to surgery ranged from 1 to 5 months, with an average of 3.2 months.
Group B had 18 males and 22 females, age 18–55 years (mean 34.27±15.73). The ratio of left to right ankle was 16 to 24. The time from injury to surgery ranged from 1 to 4 months, with an average of 2.8 months.
SURGICAL TECHNIQUES:
The operations in both groups were performed by the same doctors under general anesthesia or subarachnoid block anesthesia combined with continuous epidural anesthesia. The patients were placed in a supine position with a pneumatic tourniquet attached to the affected thigh.
In Group A, the ankle joint was fastened in the metatarsal flexion neutral position, the anteromedial approach was the visual approach, and the auxiliary anterolateral approach was the operational approach (Figure 2A). The anteromedial approach was located on the lateral edge of the tendon of anterior tibia muscle, and the auxiliary anterior lateral approach was about 1.5 cm in front of the peroneal tip (Figure 2B). The incision length was about 0.5 cm. The injury of intra-articular cartilage and ATFL was explored and evaluated under arthroscopy. In I type articular cartilage injury, there is softening of cartilage surface, but the shape of the surface is relatively intact without cracks. Type II articular cartilage injury usually shows superficial cartilage injury and is not very deep. Type III articular cartilage injury shows deep cartilage injury and cracking, but the injury has not reached subchondral bone. In IV type articular cartilage injury, the whole cartilage layer shows peeling, tearing, and other injuries [25]. We performed osteophyte removal, synovium cleaning, and talus cartilage surface repairing (Figure 3A). Three cases of type I–II cartilage injuries were treated with cartilage repair, and 7 cases of type III–IV cartilage injuries were treated with micro-fracturing. It was confirmed that all the patients had ATFL injury at the lateral fibula and the ATFL had sufficient residual for repair [26,27].
ATFL suturing was divided into 2 steps. In step 1, using an anteromedial approach, a double-sutures absorbable anchor (3.5 mm) with ULTRABRAID No. 2 super sutures (Smith & Nephew, London, U.K.) was implanted at the fibula attachment point of the ATFL through the auxiliary anterior lateral approach. In step 2, 2 sutures were inserted through the ATFL and tied to the fibula. Specific operation steps included the following. A needle was pierced from 1 cm at the front bottom of the auxiliary anterolateral approach, and the needle carried a PDS suture, which could guide the anchor thread to pass through the ATFL (Figure 3B). The needle passed through the skin and subcutaneous tissue and entered the ankle cavity. Orthopedist passed it through the ATFL, and then pulled out the PDS suture after clamping it through the auxiliary anterior lateral approach with a grip forceps. The PDS suture guided a suture through the ATFL and skin. Then, the orthopedist pulled out it through the auxiliary anterolateral approach (Figure 3C, 3D). The above steps were repeated, so that another suture passed through the ATFL and strengthened the inferior extensor retinaculum (IER) (Figure 3E). Finally, the sutures were tied to the fibula attachment point of the ATFL (Figure 3F), and the distance between 2 sutures was appropriate. Doctors sutured the incision after exploration of ankle stability [28,29].
In Group B, arthroscopy was used for exploration and osteophyte removal, synovium cleaning, and talus cartilage surface repair. Two cases of type I–II injury underwent cartilage repair and 5 cases of type III–IV injuries were treated with micro-fractures. The posture and operation method of the patients were the same as in the arthroscopy group. Microscopic examination showed that all the patients had ATFL injury at the lateral fibula and the ATFL had sufficient residual for repair. Then, the orthopedist used the classical improved open Broström approach to create a 3–4 cm incision in front of the distal peroneal layer by layer and separated the ATFL and IER. A double-sutures absorbable anchor was implanted at the same position as in the arthroscopic group in the distal fibula (fibula attachment point of ATFL). The ATFL was fastened in the fibula under direct vision, and the IER was strengthened [30].
POSTOPERATIVE TREATMENT:
The incision was changed after being dressed with low-temperature and thickness auxiliary materials, and individualized support was fastened. Non-athletes could wear boots to protect themselves and walk with weight-free plaster or fixed support for 4–6 weeks. After walking with crutches for 2 weeks, the patient could walk normally with plaster or support. After 3 months they could exercise, and at 6 months they could jump, and gradually resumed their pre-injury activities. Athletes could wear walking boots to protect themselves and walk with weight-free plaster or fixed support for 2 weeks. After 2 weeks they could wear walking boots, after 2 months they could run, after 3 months they could jump, and after 6 months they gradually resumed their pre-injury activities.
POSTOPERATIVE ASSESSMENT:
The operation time, intraoperative bleeding volume, postoperative recovery time, and complications during follow-up were recorded in the 2 groups. The anterior displacement and tilt angle of the talus were compared after 6 months, 1 year, and 2 years after the operation. The AOFAS, KAF, and JSSF scores were used to evaluate the function, pain, stability, and mobility limitation of the ankle-foot join. The result at 2 years after the operation were graded according to the scoring system scoring standard.
STATISTICAL ANALYSIS:
All data are presented as mean±standard deviation. Statistical analysis was performed using the SPSS software package (SPSS, Inc., Chicago, IL, USA). The statistical significance of differences between groups was assessed by a paired 2-tailed
Results
The patients in the 2 groups were both followed up for 20–24 months (average 22 months). The operation time, intraoperative bleeding volume, and the postoperative recovery time in Group A were significantly better than in Group B (P<0.05) (Table 1). We found that 2 cases had temporary numbness of ankle and foot back, and 1 case had a thread reaction in Group A. Two cases occurred in each of the above-mentioned complications in Group B. The numbness of ankle and foot back was relieved by themselves, and the thread reaction disappeared after incision debridement and thread removed. Other patients’ incisions in Group A and Group B all healed in stage I, and no early surgical complications. At 6 months after the operation, the AOFAS, KAF, and JSSF scale scores in Group A were significantly better than those in Group B (
Discussion
As a common motor-induced complexity injury, ankle sprain is often associated with ATFL injury, which leads to chronic LIA [31]. At present, there are many surgical methods to treat ATFL injury. The purpose of treatment is to restore ankle joint stability and function. Patients with sufficient residual ATFL are more likely to choose anterior talofibular ligament repair [32,33]. ATFL repair surgery can be divided into open surgery and arthroscopic surgery. Many studies shown that the improved classical open Broström anchor nail anatomical repairing operation was effective for ATFL injury, but due to the large incision, it was difficult for patients to recover after the operation, especially for the elderly [34]. With the development of minimally invasive and arthroscopic surgery, arthroscopy technique in ATFL repair has become clinically satisfactory. Arthroscopy repair of the ATFL has become an important research topic.
In this study, the clinical indexes of patients with arthroscopy technique in repair of ATFL recovered well, and no ankle instability or other complications occurred. The curative effect was satisfactory. The clinical data of 80 patients with ATFL repaired by open and arthroscopic surgery were analyzed retrospectively. We found that AOFAS, KAF, and JSSF scale scores in arthroscopy surgery were significantly better than those in open surgery. It was further confirmed that arthroscopy technique in ATFL repair could achieve better effectiveness in the treatment of ATFL injury. The arthroscopy technique in repair of ATFL had the advantages of less trauma, shorter operation time, and fewer postoperative complications. In this study, the open operation time was 34–41 min (average 41.3±6.7 min); and the intraoperative bleeding volume was 26–40 ml (average 33.2±7.4 ml). In contrast, the arthroscopic operation time was 19–30 min (average 24.9±5.3 min) and the intraoperative bleeding volume was 6–10 ml (average 8.6±1.9 ml), showing a clear advantage. Under arthroscopy, IER could be sutured to strengthen the lateral collateral ligaments and improve the curative effect.
Arthroscopic surgery has many advantages because its small skin incision and minimal subcutaneous anatomy minimize invasiveness in the repair process. According to previous studies, arthroscopy technique in repair of ATFL required at least 3 portals [34], while, our arthroscopy surgery required only 2 portals. To successfully complete the minimally invasive surgery, there was no large debridement around the ATFL, and it was very important to carefully choose the location of the 2 operating entrances. According to the skin incision extension technology and trans-skin technology, we used MM and AAL approaches to complete the arthroscopic repair of ATFL. Because of the low invasiveness, the postoperative pain was reduced and the daily functional activities were restored at an early stage.
Li et al [19] found that arthroscopic technique in repair of ATFL has the advantages of faster recovery and fewer complications. Our study shows that arthroscopic technique in repair of ATFL has lower invasion and better curative effect in patient with sufficient residual ATFL.
Our study has some limitations, including the small sample size, the use of a single center, and the bias that may be introduced when the surgeons performing the procedures conduct the study. In addition, this was a retrospective study, and more prospective studies are still needed to evaluate and compare the long-term effects.
Conclusions
The findings of this retrospective study showed that arthroscopic surgical repair of the ATFL is a safe, minimally invasive technique, with less blood loss, shorter surgical duration, and good clinical outcomes.
Figures
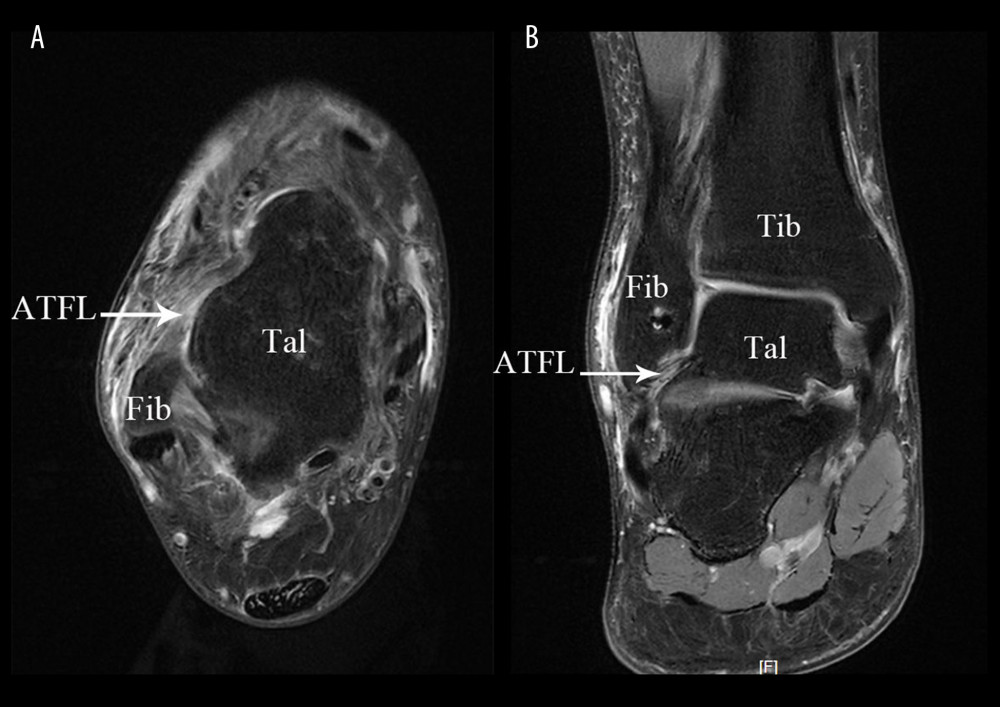 Figure 1. Arthroscopic technique approaches. (A) Physical image of arthroscopic approach; (B) 3D Print Model of Surgical Approach. TA – tibialis anterior; LM – lateral malleolus; Approach MM – medial midline approach; ACAL – accessory anterolateral approach; IER – inferior extensor retinaculum; ATFL – anterior talofibular ligament.
Figure 1. Arthroscopic technique approaches. (A) Physical image of arthroscopic approach; (B) 3D Print Model of Surgical Approach. TA – tibialis anterior; LM – lateral malleolus; Approach MM – medial midline approach; ACAL – accessory anterolateral approach; IER – inferior extensor retinaculum; ATFL – anterior talofibular ligament. 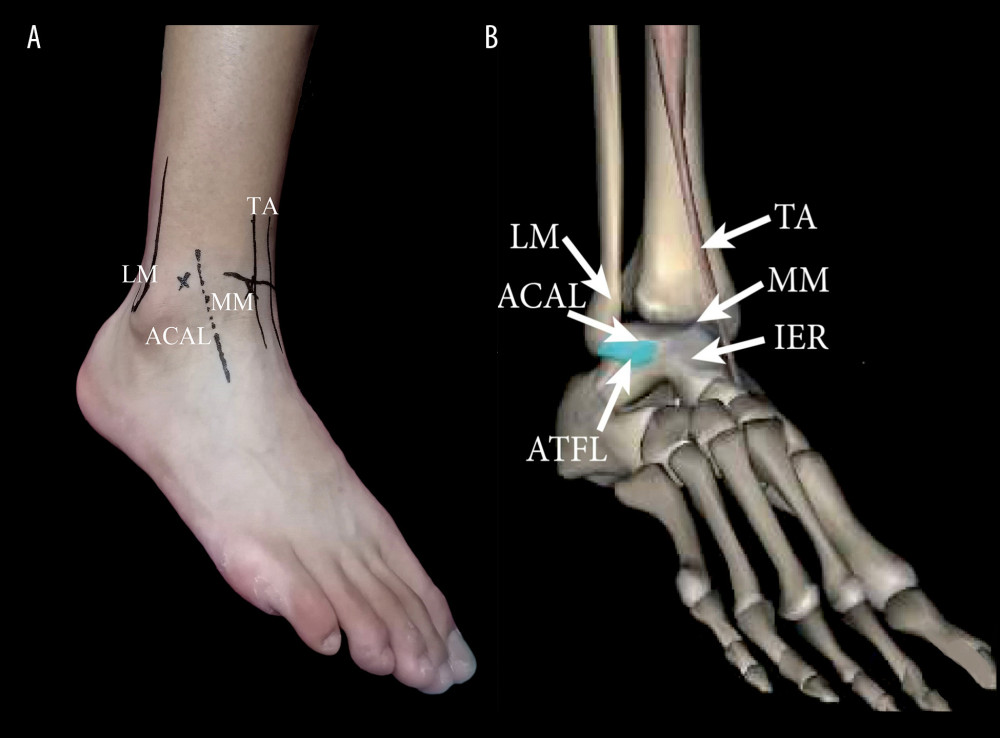 Figure 2. Preoperative examination of MRI showed anterior talofibular ligament injury. (A) In transverse section; (B) In coronal section. Fib – fibulare; Tal – talus; Tib – tibia; ATFL – anterior talofibular ligament.
Figure 2. Preoperative examination of MRI showed anterior talofibular ligament injury. (A) In transverse section; (B) In coronal section. Fib – fibulare; Tal – talus; Tib – tibia; ATFL – anterior talofibular ligament. 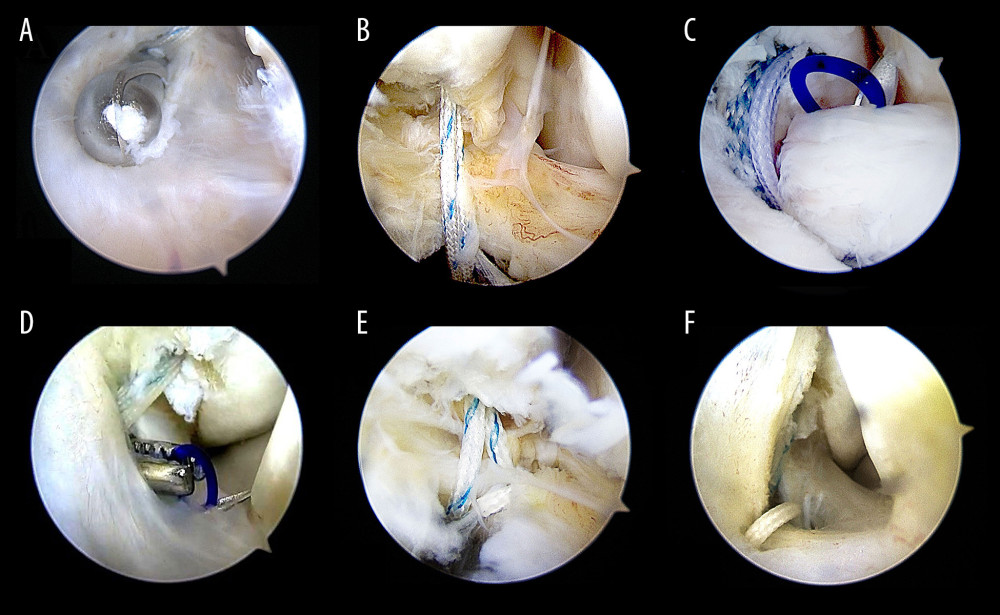 Figure 3. The procedure of all-arthroscopic repair of anterior talofibular ligament (ATFL) with anchors. (A, B) The procedure of arthroscopic repair of ATFL with anchors Arthroscopic placement of suture anchor at the fibular attachment point of ATFL through accessory anterolateral approach; (C) The needle was penetrated the ATFL after entering the articular cavity; (D) The PDS stature was pulled out via accessory anterolateral approach; (E) Repeat the above steps so that the anchor thread is passed through the ATFL and reinforced the IER; (F) Repeat steps to penetrate the other suture was penetrated the ATFL and fixed with top knot.
Figure 3. The procedure of all-arthroscopic repair of anterior talofibular ligament (ATFL) with anchors. (A, B) The procedure of arthroscopic repair of ATFL with anchors Arthroscopic placement of suture anchor at the fibular attachment point of ATFL through accessory anterolateral approach; (C) The needle was penetrated the ATFL after entering the articular cavity; (D) The PDS stature was pulled out via accessory anterolateral approach; (E) Repeat the above steps so that the anchor thread is passed through the ATFL and reinforced the IER; (F) Repeat steps to penetrate the other suture was penetrated the ATFL and fixed with top knot. 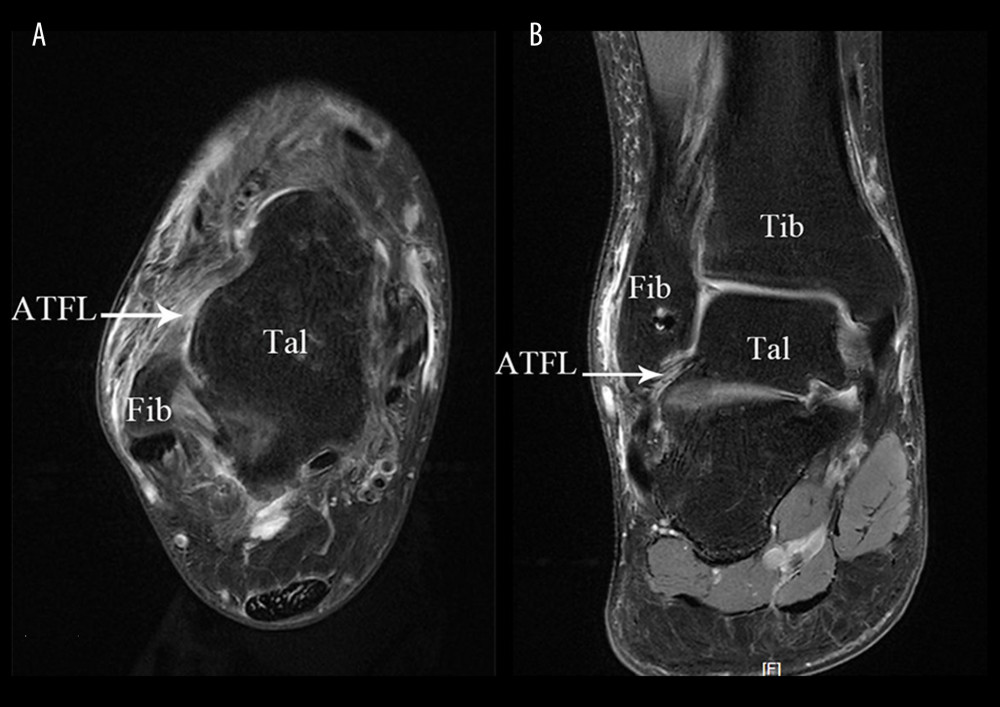 Figure 4. Postoperative MRI of a 32-year-old female patient with right anterior talofibular ligament injury in arthroscopy group. (A) In transverse section; (B) In coronal section. Fib – fibulare; Tal – talus; Tib – tibia; ATFL – anterior talofibular ligament.
Figure 4. Postoperative MRI of a 32-year-old female patient with right anterior talofibular ligament injury in arthroscopy group. (A) In transverse section; (B) In coronal section. Fib – fibulare; Tal – talus; Tib – tibia; ATFL – anterior talofibular ligament. Tables
Table 1. Comparison of clinical indicators between the 2 groups (χ̆±s). Table 2. Comparison of preoperative and postoperative functional scores between the 2 groups (χ̆±s).
Table 2. Comparison of preoperative and postoperative functional scores between the 2 groups (χ̆±s).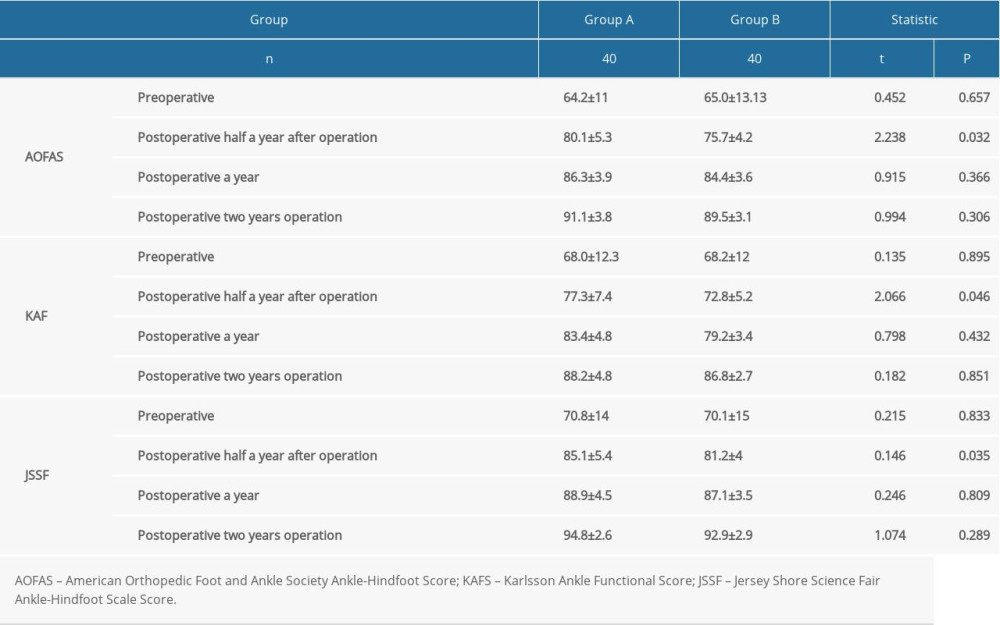 Table 3. Comparison of functional grading at 2 years after operation between the 2 groups (χ̆±s).
Table 3. Comparison of functional grading at 2 years after operation between the 2 groups (χ̆±s).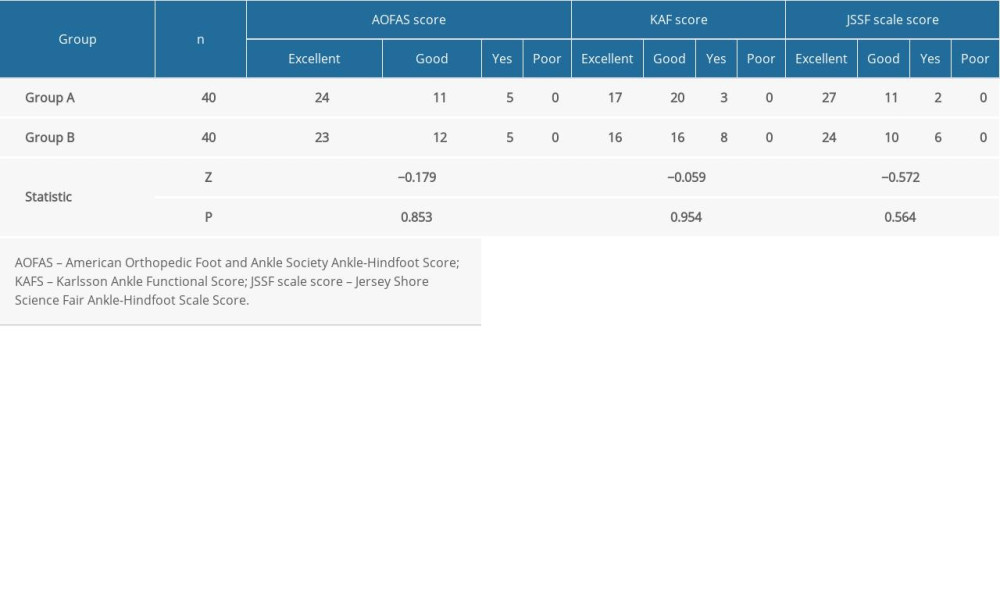 Table 4. Comparison of the anterior displacement and tilt angle of talus preoperative and postoperative between the 2 groups (χ̆±s).
Table 4. Comparison of the anterior displacement and tilt angle of talus preoperative and postoperative between the 2 groups (χ̆±s).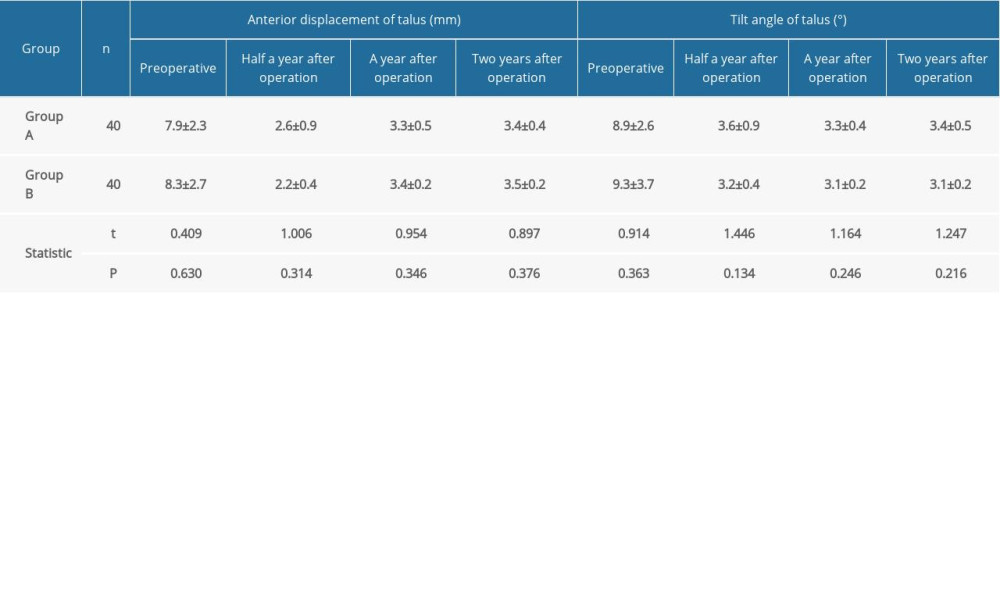
References
1. Guerra-Pinto F, Côrte-Real N, Mota Gomes T, Rotational instability after anterior talofibular and calcaneofibular ligament section: The experimental basis for the ankle Pivot test: J Foot Ankle Surg, 2019; 57(6); 1087-91
2. Dong P, Gu S, Jiang Y, All arthroscopic remnant-preserving reconstruction of the lateral ligaments of the ankle: A biomechanical study and clinical application: Biochem Biophys Res Commun, 2019; 505(4); 985-90
3. Kovaleski JE, Heitman RJ, Gurchiek LR, Joint stability characteristics of the ankle complex after lateral ligamentous injury, part I: A laboratory comparison using arthrometric measurement: Athl Train, 2017; 49(7); 192-97
4. Dalmau-Pastor M, Yasui Y, Calder JD, Anatomy of the inferior extensor retinaculum and its role in lateral ankle ligament reconstruction: A pictorial essay: Knee Surg Sports Traumatol Arthrosc, 2016; 24(4); 957-62
5. Matheny LM, Johnson NS, Liechti DJ, Activity level and function after lateral ankle ligament repair versus reconstruction: Am J Sports Med, 2016; 44(5); 1301-8
6. Aessoe U, Svendsen AW, Christensen MN, Evaluation of functional ankle instability assessed by an instrumented wobble board: Phys Ther Spor, 2019; 35(3); 133-38
7. Vega J, Golanó P, Pellegrino A, All-inside arthroscopic lateral collateral ligament repair for ankle instability with a knotless suture anchor technique: Foot Ankle Int, 2018; 34(6); 1701-9
8. Hassan S, Thurston D, Sian T, Clinical outcomes of the modified Broström technique in the management of chronic ankle instability after early, intermediate, and delayed presentation: J Foot Ankle Surg, 2018; 57(4); 685-88
9. Green T, Willson G, Martin D, Fallon K, What is the quality of clinical practice guidelines for the treatment of acute lateral ankle ligament sprains in adults? A Systematic Review: BMC Musculoskeletal Disord, 2019; 20; 394
10. Batista JP, Del Vecchio JJ, Patthauer L, Arthroscopic lateral ligament repair through two portals in chronic ankle instability: Open Orthop J, 2017; 62(11); 617-32
11. Song B, Li C, Chen N, All arthroscopic anatomical reconstruction of anterior talofibular ligament using semitendinosus autografts: Int Orthop, 2017; 41(5); 975-82
12. Yang Q, Zhou Y, Arthroscopic debridement of anterior ankle impingement in patients with chronic lateral ankle instability: BMC Musculoskelet Disord, 2017; 19(8); 239-45
13. Arroyo-Hernández M, Mellado-Romero M, Páramo-Díaz P, Chronic ankle instability: Arthroscopic anatomical repair: Rev Esp Cir Ortop Traumatol, 2017; 61(2); 104-10
14. Li H, Hua Y, Activity level and function 2 years after anterior talofibular ligament repair: A comparison between arthroscopic repair and open repair procedures: Am J Sports Med, 2017; 45(9); 2044-51
15. De Leeuw PA, Golanó P, Sierevelt IN, The course of the superficial peroneal nerve in relation to the ankle position: Anatomical study with ankle arthroscopic implications: Knee Surg Sports Traumatol Arthrosc, 2019; 18(5); 612-17
16. Song Y, Li H, Sun C, Clinical guidelines for the surgical management of chronic lateral ankle instability: A consensus reached by systematic review of the available data: Orthop J Sports Med, 2019; 7; 2325967119873852
17. Behrens SB, Drakos M, Lee BJ, Biomechanical analysis of Broström versus Broström-Gould lateral ankle instability repairs: Foot Ankle Int, 2015; 34(4); 587-92
18. Maffulli N, Del Buono A, Maffulli GD, Isolated anterior talofibular ligament Broström repair for chronic lateral ankle instability: 9-year follow-up: Am J Sports Med, 2013; 41(4); 858-64
19. Li H, Hua Y, Li H, Activity level and function 2 years after anterior Talofibular ligament repair: A comparison between arthroscopic repair and open repair procedures: Am J Sports Med, 2017; 45; 2044-51
20. Akbari M, Karimi H, Ghabaii M, Balance problems after unilateral lateral ankle sprains: J Rehabil Res Dev, 2016; 43(7); 819-24
21. Higashiyama R, Aikawa J, Iwase D, Anatomical arthroscopic anterior talofibular ligament and calcaneofibular ligament reconstruction using an autogenic hamstring tendon: Safe creation of anatomical fibular tunnel: Arthrosc Tech, 2019; 8(3); e215-22
22. Buerer Y, Winkler M, Burn A, Evaluation of a modified Broström-Gould procedure for treatment of chronic lateral ankle instability: A retrospective study with critical analysis of outcome scoring: Foot Ankle Surg, 2018; 19(1); 36-41
23. Feng SM, Sun QQ, Wang AG, Arthroscopic anatomical repair of anterior talofibular ligament for chronic lateral instability of the ankle: Medium- and long-term functional follow-up: Orthop Surg, 2020; 12(2); 505-14
24. Vega J, Guelfi M, Malagelada F, Arthroscopic all-inside anterior Talofibular ligament repair through a three-portal and no-ankle-distraction technique: JBJS Essent Surg Tech, 2018; 8; e25
25. Wang G, Li Y, Meng X, The study of targeted blocking SDF-1/CXCR4 signaling pathway with three antagonists on MMPs, type II collagen, and aggrecan levels in articular cartilage of guinea pigs: J Orthop Surg Res, 2020; 15(1); 195
26. Vega J, Golanó P, Pellegrino A, All-inside arthroscopic lateral collateral ligament repair for ankle instability with a knotless suture anchor technique: Foot Ankle Int, 2018; 34(6); 1701-9
27. Guillo S, Cordier G, Sonnery-Cottet B, Anatomical reconstruction of the anterior talofibular and calcaneofibular ligaments with an all-arthroscopic surgical technique: Orthop Traumatol Surg Res, 2014; 100(6); S413-17
28. Rasmussen O, Tovborg-Jensen I, Boe S, Distal tibiofibular ligaments. Analysis of function: Acta Orthop Scand, 2017; 53(4); 681-86
29. Coughlin MJ, Schenck RC, Grebing BR, Comprehensive reconstruction of the lateral ankle for chronic instability using a free gracilis graft: Foot Ankle Int, 2015; 25(4); 231-41
30. Guelfi M, Zamperetti M, Pantalone A, Open and arthroscopic lateral ligament repair for treatment of chronic ankle instability: A systematic review: Foot Ankle Surgery, 2018; 24(5); 11-18
31. Vuurberg G, Wink LM, Blankevoort L, A risk assessment model for chronic ankle instability: Indications for early surgical treatment? An observational prospective cohort-study protocol: BMC Musculoskelet Disord, 2018; 19(4); 225-31
32. Lee KT, Park YU, Kim JS, Long-term results after modified Broström procedure without cal caneo-fibular ligament reconstruction: Foot Ankle Int, 2014; 32(8); 153-57
33. Mattacola CG, Dwyer MK, Rehabilitation of the ankle after acute sprain or chronic instability: J Athl Train, 2018; 37(4); 413-29
34. Ucerler H, Aktan Ikiz ’ZA, The variations of the sensory branches of the superficial peroneal nerve course and its clinical importance: Foot Ankle Int, 2015; 26(3); 942-46
Figures
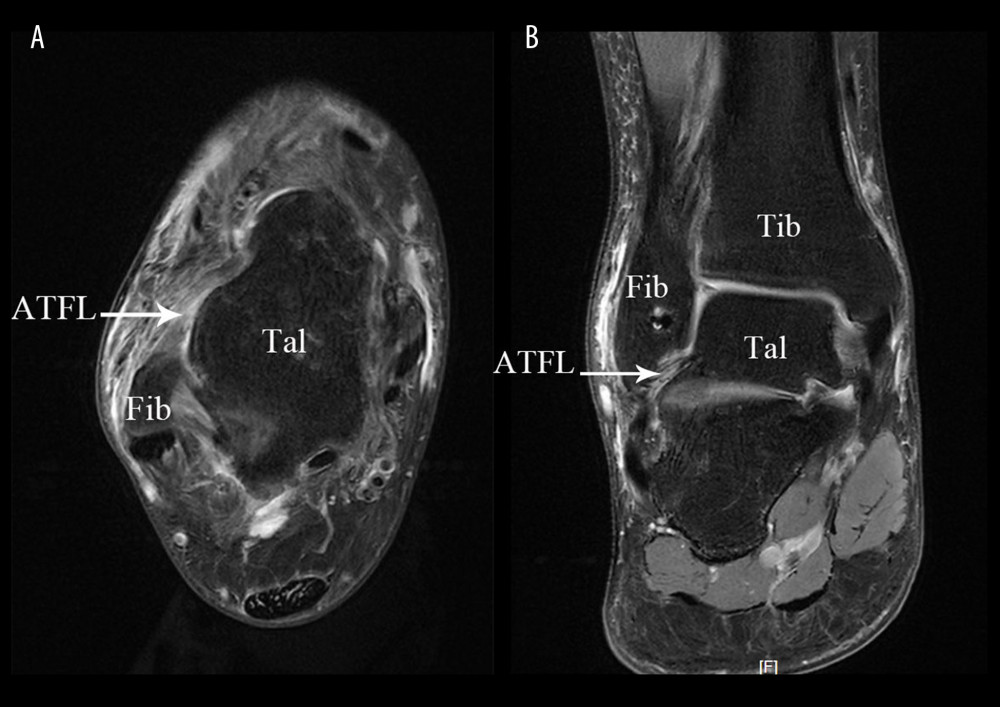 Figure 1. Arthroscopic technique approaches. (A) Physical image of arthroscopic approach; (B) 3D Print Model of Surgical Approach. TA – tibialis anterior; LM – lateral malleolus; Approach MM – medial midline approach; ACAL – accessory anterolateral approach; IER – inferior extensor retinaculum; ATFL – anterior talofibular ligament.
Figure 1. Arthroscopic technique approaches. (A) Physical image of arthroscopic approach; (B) 3D Print Model of Surgical Approach. TA – tibialis anterior; LM – lateral malleolus; Approach MM – medial midline approach; ACAL – accessory anterolateral approach; IER – inferior extensor retinaculum; ATFL – anterior talofibular ligament.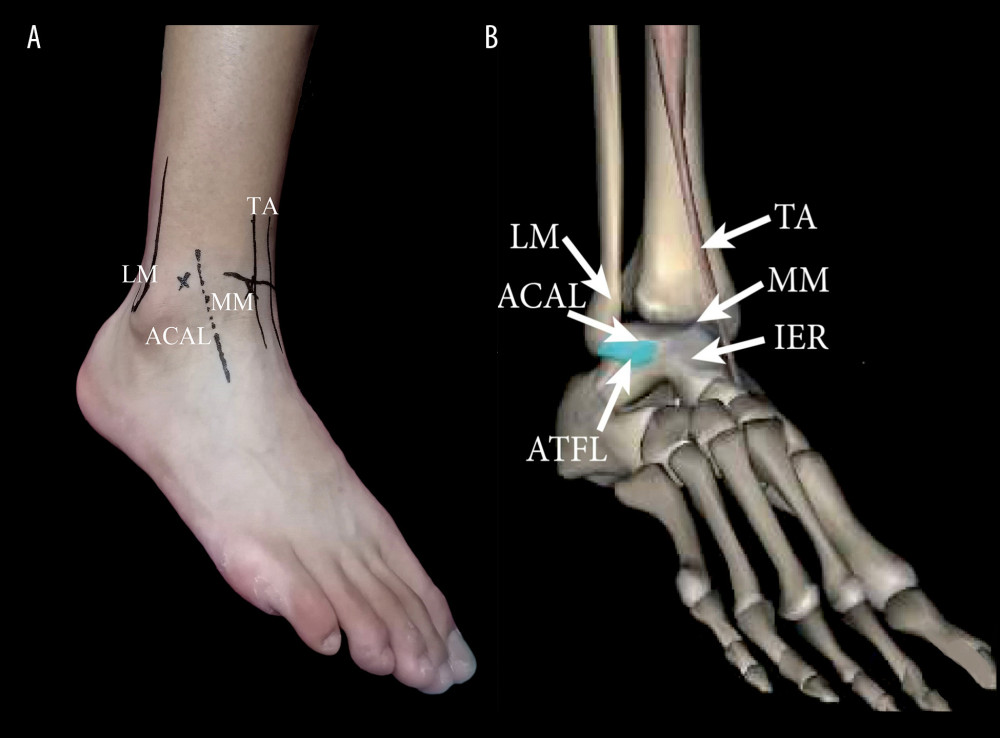 Figure 2. Preoperative examination of MRI showed anterior talofibular ligament injury. (A) In transverse section; (B) In coronal section. Fib – fibulare; Tal – talus; Tib – tibia; ATFL – anterior talofibular ligament.
Figure 2. Preoperative examination of MRI showed anterior talofibular ligament injury. (A) In transverse section; (B) In coronal section. Fib – fibulare; Tal – talus; Tib – tibia; ATFL – anterior talofibular ligament.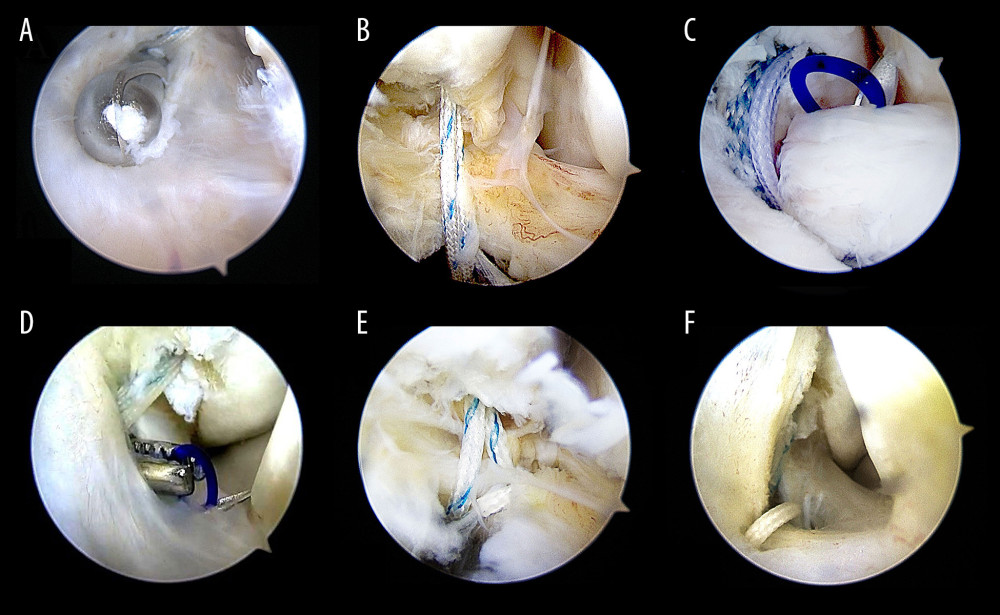 Figure 3. The procedure of all-arthroscopic repair of anterior talofibular ligament (ATFL) with anchors. (A, B) The procedure of arthroscopic repair of ATFL with anchors Arthroscopic placement of suture anchor at the fibular attachment point of ATFL through accessory anterolateral approach; (C) The needle was penetrated the ATFL after entering the articular cavity; (D) The PDS stature was pulled out via accessory anterolateral approach; (E) Repeat the above steps so that the anchor thread is passed through the ATFL and reinforced the IER; (F) Repeat steps to penetrate the other suture was penetrated the ATFL and fixed with top knot.
Figure 3. The procedure of all-arthroscopic repair of anterior talofibular ligament (ATFL) with anchors. (A, B) The procedure of arthroscopic repair of ATFL with anchors Arthroscopic placement of suture anchor at the fibular attachment point of ATFL through accessory anterolateral approach; (C) The needle was penetrated the ATFL after entering the articular cavity; (D) The PDS stature was pulled out via accessory anterolateral approach; (E) Repeat the above steps so that the anchor thread is passed through the ATFL and reinforced the IER; (F) Repeat steps to penetrate the other suture was penetrated the ATFL and fixed with top knot.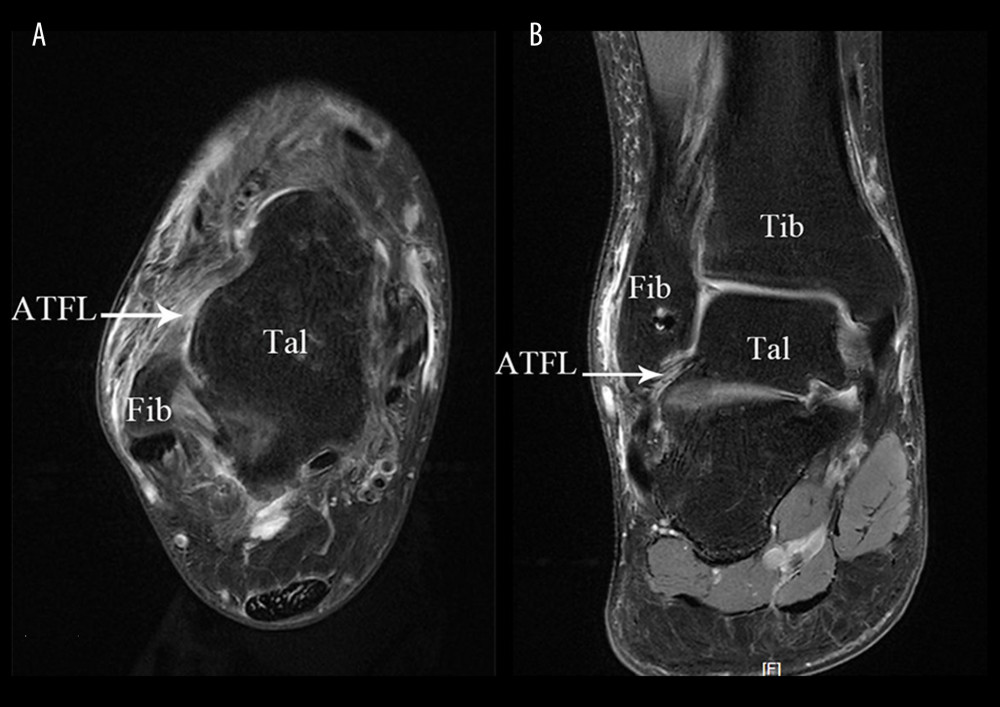 Figure 4. Postoperative MRI of a 32-year-old female patient with right anterior talofibular ligament injury in arthroscopy group. (A) In transverse section; (B) In coronal section. Fib – fibulare; Tal – talus; Tib – tibia; ATFL – anterior talofibular ligament.
Figure 4. Postoperative MRI of a 32-year-old female patient with right anterior talofibular ligament injury in arthroscopy group. (A) In transverse section; (B) In coronal section. Fib – fibulare; Tal – talus; Tib – tibia; ATFL – anterior talofibular ligament. Tables
 Table 1. Comparison of clinical indicators between the 2 groups (χ̆±s).
Table 1. Comparison of clinical indicators between the 2 groups (χ̆±s).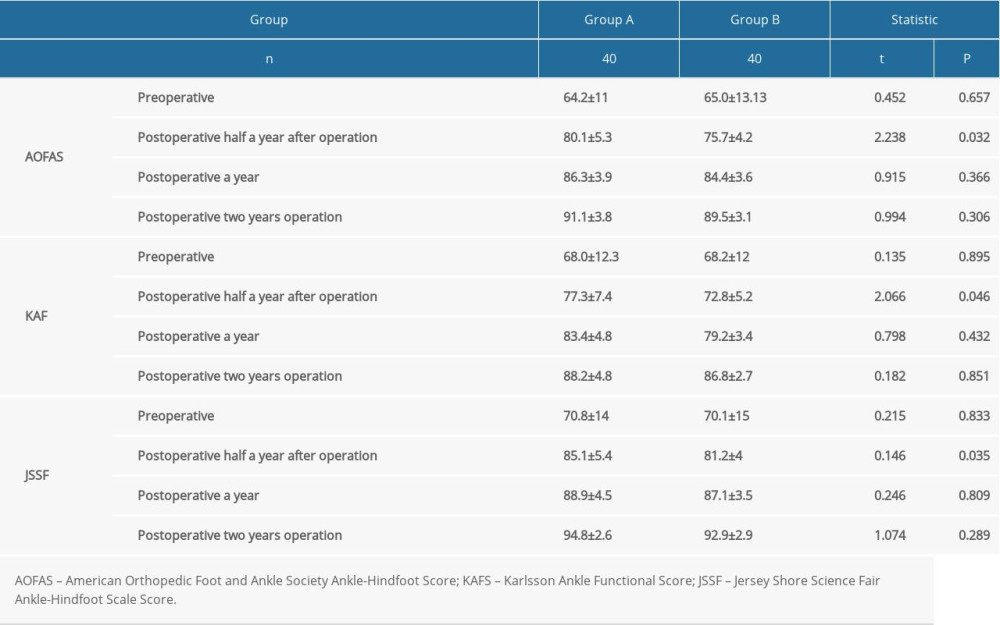 Table 2. Comparison of preoperative and postoperative functional scores between the 2 groups (χ̆±s).
Table 2. Comparison of preoperative and postoperative functional scores between the 2 groups (χ̆±s).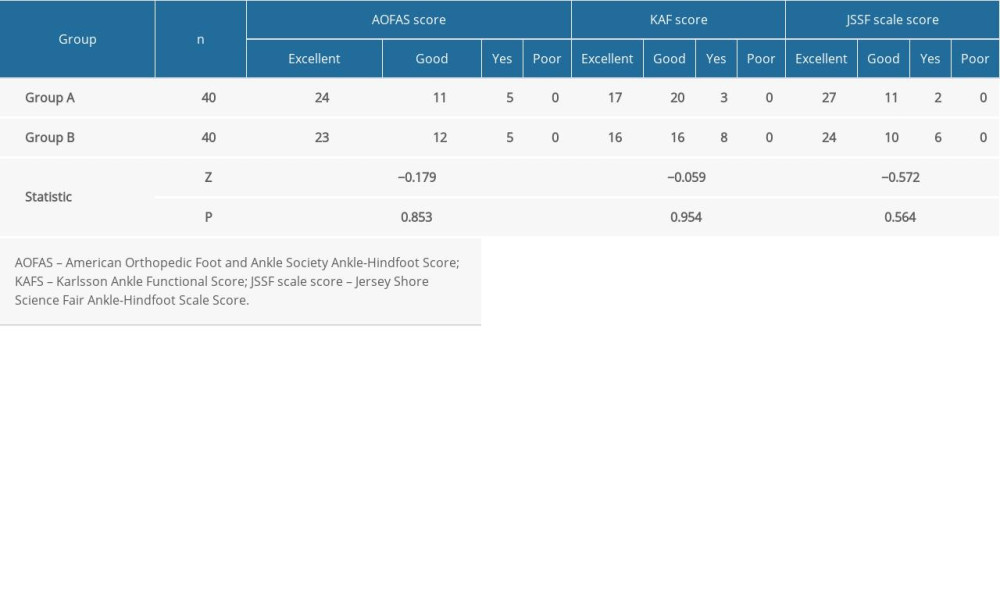 Table 3. Comparison of functional grading at 2 years after operation between the 2 groups (χ̆±s).
Table 3. Comparison of functional grading at 2 years after operation between the 2 groups (χ̆±s).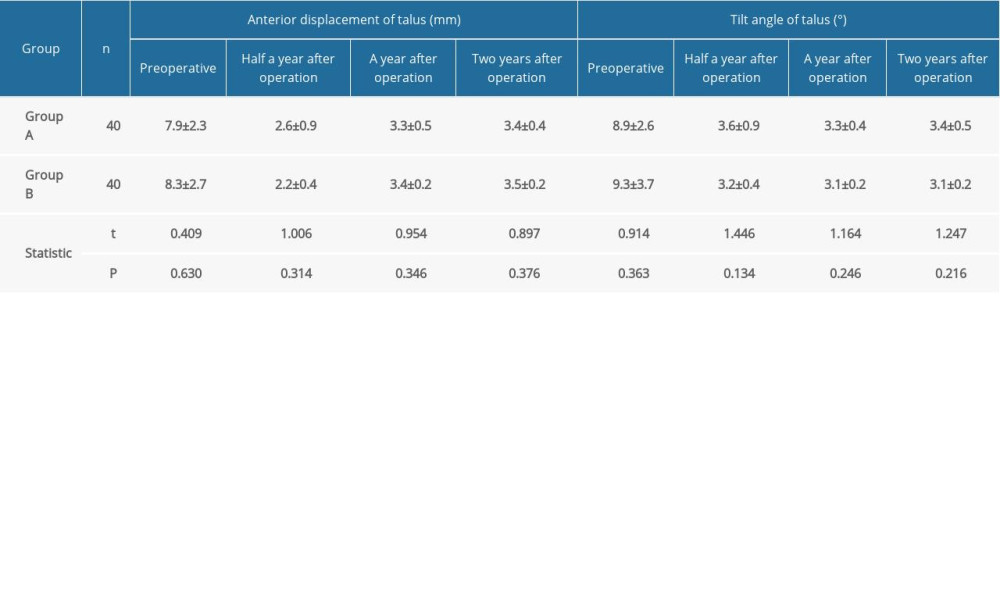 Table 4. Comparison of the anterior displacement and tilt angle of talus preoperative and postoperative between the 2 groups (χ̆±s).
Table 4. Comparison of the anterior displacement and tilt angle of talus preoperative and postoperative between the 2 groups (χ̆±s). Table 1. Comparison of clinical indicators between the 2 groups (χ̆±s).
Table 1. Comparison of clinical indicators between the 2 groups (χ̆±s).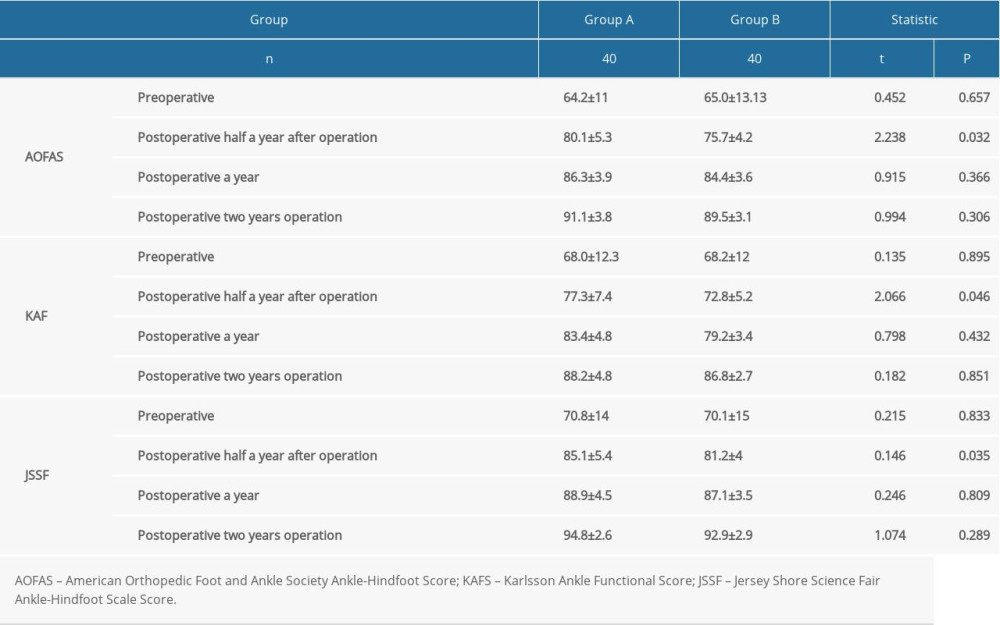 Table 2. Comparison of preoperative and postoperative functional scores between the 2 groups (χ̆±s).
Table 2. Comparison of preoperative and postoperative functional scores between the 2 groups (χ̆±s).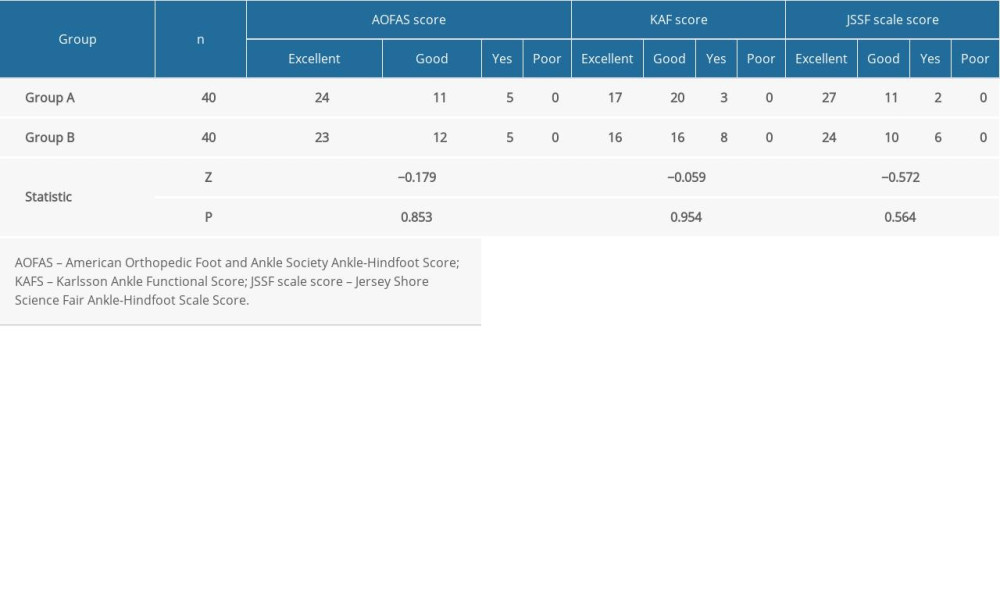 Table 3. Comparison of functional grading at 2 years after operation between the 2 groups (χ̆±s).
Table 3. Comparison of functional grading at 2 years after operation between the 2 groups (χ̆±s).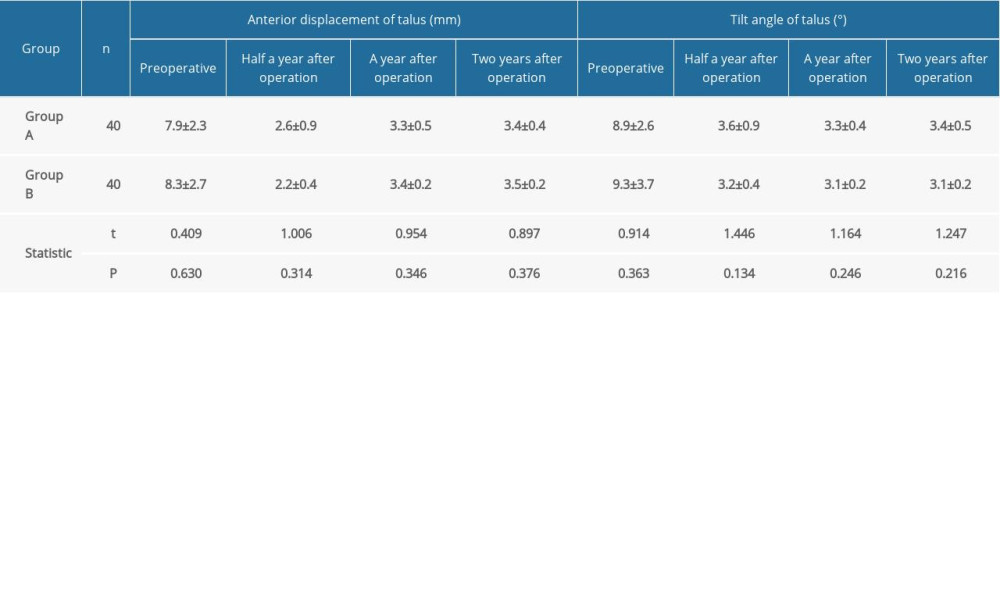 Table 4. Comparison of the anterior displacement and tilt angle of talus preoperative and postoperative between the 2 groups (χ̆±s).
Table 4. Comparison of the anterior displacement and tilt angle of talus preoperative and postoperative between the 2 groups (χ̆±s). In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








