07 June 2021: Clinical Research
Ultrasound Measurement of the Transverse Abdominis, Internal Oblique, and External Oblique Muscles Associated with Forward Head Posture and Reduced Cranio-Vertebral Angle
Kyung Woo Kang1ADEF, Yong Hyun Kwon1ADF, Sung Min Son2BCE*DOI: 10.12659/MSM.928987
Med Sci Monit 2021; 27:e928987
Abstract
BACKGROUND: Abnormal posture can affect the alignment of the cervical spine, which can lead to various physical problems. There are many ways to solve the problem by limiting the area around the neck to restore abnormal neck condition. However, there is a need to look at these problems from an enlarged perspective through the relationship between the cervical spine and trunk. This study aimed to investigate the significance of the thickness of the transverse abdominis, internal oblique, and external oblique muscles in patients with forward head posture and reduced cranio-vertebral angle.
MATERIAL AND METHODS: We included 24 healthy adult males in their 20s without lower back pain. The cranio-vertebral angle (CVA) in all the subjects was measured with the help of pictures taken in the sagittal plane using a digital camera. The thickness of muscles, including transverse abdominis (TrA), internal oblique (IO), and external oblique (EO), was measured using a diagnostic ultrasound device. Pearson’s correlation analysis was used to identify the correlation between the variables measured.
RESULTS: CVA showed a statistically significant correlation with TrA thickness (r=0.506/p=0.012), and among the abdominal muscles, there was a significant correlation between IO and EO thickness (r=0.663/p=0.000).
CONCLUSIONS: A reduced CVA due to FHP was significantly associated with reduced TrA thickness. Therefore, increasing the bulk of the abdominal muscles with restoration of the abnormal CVA is a potential treatment approach and requires further study.
Keywords: Abdominal Muscles, Posture, Ultrasonography, Abdominal Oblique Muscles, Cervical Vertebrae, Head, Neck, Torso
Background
The constant use of computers in modern society has led to posture-related problems. Various effects of postural change by forward head posture (FHP) has been reported in many studies [1–4]. FHP is described as a posture occurring with an extension in the upper cervical vertebrae accompanying flexion in the lower cervical vertebrae [4]. Such an abnormal posture is increasing worldwide; therefore, there is a need for a fundamental treatment method to correct the abnormal posture. For this, it is important to clearly assess the body changes caused by the abnormal posture [5–7].
Most of the researchers who studied FHP mainly focused on the neck angle, such as the cranio-vertebral angle (CVA), or changes in the length of muscles around the neck [8–11]. Its association with rounded shoulders, an abnormal posture accompanied with FHP, has also been studied [12,13]. Studies on FHP report that it causes various symptoms such as neck pain, headache, jaw pain, and musculoskeletal disorders around the neck, and these studies only mention how to correct the abnormal neck posture [14–17]. However, we must contemplate more essential solutions rather than a direct correction in the area with problems.
Researchers who studied from a clinical point of view tend to look at the problems localized to the neck conditions such as restoration of the neck angle, improvement of neck joint performance, changes in the thickness of the neck muscles, and neck pain [2,8–11]. However, we also need a closer look at the trunk, which can be affected by neck conditions, to correct abnormal postures such as FHP. The vertebral column comprises 26 vertebrae that act as a single unit. Accordingly, abnormal conditions of the neck bones affect the upper and lower spine, consequently affecting the extent of muscle activation of the trunk [18,19]. Therefore, we need to bear in mind that FHP may affect postural changes in the trunk or trunk muscle activation, turning our attention away from the view that it causes changes or problems only around the neck. Further, it is necessary to investigate the relationship between the neck angle and trunk muscle activation for improvement of abnormal posture [18,19].
Rapid development in technology has allowed research on the muscle structure in the human body using noninvasive methods such as research using ultrasound imaging [20,21]. The reliability of research on the muscle structure using ultrasound imaging has already been verified via studies on various muscles of the human body [22–24]. Among the studies on the muscle structure using ultrasound, some investigated trunk muscles, including musculus multifidus, transverse abdominis (TrA), external oblique (EO), and internal oblique (IO), to determine the clinical manifestations such as lower back pain [24,25]. Clinical research on muscles is mostly conducted using measurements of muscular power and size. In general, the size of the muscles is measured in the cross-sectional area or thickness, which is associated with the maximum force of muscle contraction [26]. Therefore, changes in the muscle thickness represent muscle conditions that are weakened or strengthened [27]. Ultrasound imaging is a noninvasive diagnostic method that effectively observes changes in muscle conditions by monitoring changes in muscle thickness [28]. Since postural changes caused by CVA can affect the state of the trunk, the abdominal muscle thickness measured by ultrasound image may be able to confirm the correlation with CVA. If their relationship could be confirmed, that information may be used as a basis for the assessment of abnormal posture [18,19,27,28].
The conditions of trunk muscles, commonly known as the core muscles, can be affected by abnormal postural changes such as FHP. However, there are few studies on the correlation between such abnormal neck conditions and trunk muscles. Therefore, this study aimed to investigate the significance of the thickness of the transverse abdominis, internal oblique, and external oblique muscles with FHP and reduced CVA.
Material and Methods
STUDY SUBJECTS:
A total of 24 healthy adult men in their 20s without lower back pain were recruited in Daegu, South Korea. Individuals with the following experiences were excluded from the study: those who had been suffering from lower back pain beginning 6 months before the study or who received treatment for lower back pain, those who underwent abdominal or spinal surgery, those with a neurological or cognitive disorder, those with surgery or trauma in the trunk, or those who received treatment such as lower back stabilization exercises within the last 3 months. All subjects were informed about the study objective, experimental methods, contents, and procedures. Those who agreed to participate were selected. The study was approved by the Bioethics Committee (YNC IRB/201904-01).
MEASUREMENT OF THE CRANIO-VERTEBRAL ANGLE:
A digital camera (Canon 650D, Canon, Japan) was set to a fixed stand for the measurement of CVA, and a photo of the side of the subject was taken from 1 m distance. For the exact measurement of CVA, a plumb line hung from the ceiling descended right next to the subject to draw a horizontal line. The subject was instructed to sit comfortably with both arms relaxed at the sides of the trunk and to maintain the natural head posture. CVA was defined as the angle between the line from the spinous process of the seventh cervical vertebra to the ear tragus and a horizontal line (Figure 1). The smaller the CV angle, the larger the flexion of the lower cervical spine [29].
ULTRASOUND MEASUREMENTS:
Diagnostic ultrasound imaging (MicrUs EXT-1H [TELEMED, Italy]) was used to measure the muscles thickness of TrA, IO, and EO in the brightness mode. All participants were right-handed and all measurements were made on the right abdomen. For imaging, the participant was lying in a comfortable position with knees bent and the hips at 45°. The ultrasound head was moved along the middle line between the sacral crest and the inferior angle of the thoracic cage aligning transversely to the anterolateral abdominal wall to measure abdominal muscle thickness. The ultrasound head was at a right angle to the anterolateral abdominal muscle when the participant was relaxed, and the inner edge of the head was set at almost 2 cm from the inner edge of the TrA on ultrasound images [30]. The measured muscle thickness was divided by the participant’s weight to normalize muscle thickness. Ultrasound images were stored and measured using Echo wave II program and Image J software 1.36b.
STATISTICAL ANALYSIS:
SPSS 22.0 (IBM, Chicago, IL, USA) was used for all statistical analyses. Shapiro-Wilk’s test was used for normality tests of all variables. Pearson’s correlation analysis was used to identify the correlation among the variables. The level of statistical significance was set to 0.05
Results
A total of 24 subjects participated in the study, and the general characteristics such as age, height, and weight of the subjects are shown in Table 1 along with the average and standard deviation for CVA, TrA, IO, and EO. The results from the correlation analyses of these variables are summarized in Table 2. CVA showed a statistically significant correlation with TrA thickness among the abdominal muscles (r=0.506/p=0.012), and thickness IO and EO showed a significant correlation with each other among those muscles (r=0.663/p=0.000; Table 2).
Discussion
We investigated the relationship between the cranio-vertebral angle and trunk muscle thickness using ultrasound imaging. CVA showed a statistically significant correlation with TrA. This means that the larger the CV angle, the larger the TrA muscle thickness. Further, IO and EO thickness showed a significant correlation, indicating that when a muscle is thick between 2 muscles, the other muscle is also thick.
The mean CVA of the participants was 57.58±5.09°. There are some studies on CVA, but they rarely defined a clear normal range [9,29,31,32]. There were a few studies that indicated the range of the angles according to neck pain or the difference in the severity of FHP [31–33]. Within the range of CVA generally measured, the smaller angle caused deterioration in the condition of FHP or neck pain. Lee et al reported that people with slight FHP had a mean angle of 59.02±3.09° and with moderate-severe FHP the mean angle was 57.51±4.82° [34]. Cheung et al reported that people with pain and without pain had mean CVAs of 43.94±3.61° and 50.58±2.09°, respectively [32]. In contrast, a study of adolescents reported no significant difference between the CVA in those without (48.38±4.79°) and with (48.63±5.5°) pain [33]. People who work in a sitting position for a long time or have a long-term sedentary lifestyle have a small angle of CVA [35–37].
Only TrA showed a statistically significant correlation with CVA among abdominal muscles and a moderate level of correlation (r=0.506). This means that a larger CVA indicates a thicker TrA, and a smaller CVA indicates a thinner TrA. The superficial abdominal muscles such as IO, EO, and rectus abdominis usually create movements such as flexion, lateral flexion, and rotation; TrA contraction increases the tension of the thoracolumbar fascia and intra-abdominal pressure, which can help to reduce the abdominal circumference [38]. Modern people with sedentary work have incorrect posture and have decreased muscular activity of the TrA and multifidus due to low physical activity [39]. Many studies have already shown that prolonged sitting causes postural imbalance such as FHP [35–37]. It can be inferred that people with weakened TrA activity due to prolonged sitting can have a postural imbalance with smaller CVA.
TrA plays an important role in supporting the posture rather than making movements, and the muscle activity increases when adjusting posture after losing balance [40]. In contrast, IO and EO muscles are the prime movers rotating the trunk around the vertical axis. Particularly when the trunk rotates, the movement arises from actions of the contralateral EO and ipsilateral IO. Therefore, these 2 muscles that are activated together on many occasions can be considered to have a close relationship with each other [41]. This supports the results of the present study that showed a significant correlation between IO and EO muscles (r=0.663).
However, IO and EO showed no particular correlation with CVA. Changes in CVA are the postural changes occurring in the sagittal plane, as observed in the measurement methods [32]. This could be one of the reasons why CVA did not show a large correlation with IO and EO muscles, which rotate the trunk in a horizontal plane around the vertical axis. In addition, IO and EO muscles tend to act in “situations when more challenging posture adjustments are needed” such as the presence of illness with difficult anticipatory control or when sitting on unstable surfaces [42,43]. This is in contrast to the result that showed the correlation between CVA and TrA, which plays an important role in “consistent adjustments of posture.” IO and EO muscles tend to mainly act when the movements of the trunk occur, such as rotation and flexion of the trunk. However, TrA acts at all times to maintain compression for viscera and stability of the trunk when movements of the extremities and the trunk occur [40]. There are reports that prolonged sitting posture, which causes a decrease in CVA, can reduce the activity of the TrA or multifidus muscles [35–37]. However, it is difficult to clearly explain the relationship between CVA and IO and EO muscles because insufficient reports, and further research on this topic is warranted.
Our study has a few of limitations. We could not obtain data on thoracic and lumbar angle according to the change of cervical angle, and our sample size was somewhat small, so it is difficult to generalize our results.
Conclusions
The results of this study reveal a significant correlation between a decrease in CVA due to postural imbalance and a decrease in TrA muscle thickness among the abdominal muscles. The study findings showed that a reduced CVA due to FHP was significantly associated with reduced TrA muscle thickness. Therefore, increasing the bulk of the abdominal muscles with correction of the abnormal CVA is a potential treatment approach and requires further study.
References
1. Koseki T, Kakizaki F, Hayashi S, Effect of forward head posture on thoracic shape and respiratory function: J Phys Ther Sci, 2019; 31(1); 63-68
2. Cheon S, Park S, Changes in neck and upper trunk muscle activities according to the angle of movement of the neck in subjects with forward head posture: J Phys Ther Sci, 2017; 29(2); 191-93
3. Fernandez-de-las-Penas C, Alonso-Blanco C, Cuadrado ML, Neck mobility and forward head posture are not related to headache parameters in chronic tension-type headache: Cephalalgia, 2007; 27(2); 158-64
4. Gonzalez HE, Manns A, Forward head posture: its structural and functional influence on the stomatognathic system, a conceptual study: Cranio, 1996; 14(1); 71-80
5. Lee MY, Lee HY, Yong MS, Characteristics of cervical position sense in subjects with forward head posture: J Phys Ther Sci, 2014; 26(11); 1741-43
6. Nam SH, Son SM, Kwon JW, The Intra- and inter-rater reliabilities of the forward head posture assessment of normal healthy subjects: J Phys Ther Sci, 2013; 25(6); 737-39
7. Garrett TR, Youdas JW, Madson TJ, Reliability of measuring forward head posture in a clinical setting: J Orthop Sports Phys Ther, 1993; 17(3); 155-60
8. Kocur P, Wilski M, Goliwas M, Influence of forward head posture on myotonometric measurements of superficial neck muscle tone, elasticity, and stiffness in asymptomatic individuals with sedentary jobs: J Manipulative Physiol Ther, 2019; 42(3); 195-202
9. Kim DH, Kim CJ, Son SM, Neck pain in adults with forward head posture: effects of craniovertebral angle and cervical range of motion: Osong Public Health Res Perspect, 2018; 9(6); 309-13
10. Ghamkhar L, Kahlaee AH, Is forward head posture relevant to cervical muscles performance and neck pain? A case-control study: Braz J Phys Ther, 2019; 23(4); 346-54
11. Goodarzi F, Rahnama L, Karimi N, The effects of forward head posture on neck extensor muscle thickness: An ultrasonographic study: J Manipulative Physiol Ther, 2018; 41(1); 34-41
12. Lee DY, Nam CW, Sung YB, Changes in rounded shoulder posture and forward head posture according to exercise methods: J Phys Ther Sci, 2017; 29(10); 1824-27
13. Kim EK, Kim JS, Correlation between rounded shoulder posture, neck disability indices, and degree of forward head posture: J Phys Ther Sci, 2016; 28(10); 2929-32
14. Fernandez-de-las-Penas C, Alonso-Blanco C, Cuadrado ML, Forward head posture and neck mobility in chronic tension-type headache: A blinded, controlled study: Cephalalgia, 2006; 26(3); 314-19
15. Szeto GP, Straker L, Raine S, A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers: Appl Ergon, 2002; 33(1); 75-84
16. Lee WY, Okeson JP, Lindroth J, The relationship between forward head posture and temporomandibular disorders: J Orofac Pain, 1995; 9(2); 161-67
17. Ciancaglini R, Testa M, Radaelli G, Association of neck pain with symptoms of temporomandibular dysfunction in the general adult population: Scand J Rehabil Med, 1999; 31(1); 17-22
18. Kim SW, Kim TH, Bok DH, Analysis of cervical spine alignment in currently asymptomatic individuals: Prevalence of kyphotic posture and its relationship with other spinopelvic parameters: Spine J, 2018; 18(5); 797-810
19. Xia T, Long CR, Vining RD, Association of lumbar spine stiffness and flexion-relaxation phenomenon with patient-reported outcomes in adults with chronic low back pain – a single-arm clinical trial investigating the effects of thrust spinal manipulation: BMC Complement Altern Med, 2017; 17(1); 303
20. Chow RS, Medri MK, Martin DC, Sonographic studies of human soleus and gastrocnemius muscle architecture: gender variability: Eur J Appl Physiol, 2000; 82(3); 236-44
21. Maganaris CN, Baltzopoulos V, Sargeant AJ, In vivo measurements of the triceps surae complex architecture in man: implications for muscle function: J Physiol, 1998; 512(Pt 2); 603-14
22. Heit M, Intraurethral sonography and the test-retest reliability of urethral sphincter measurements in women: J Clin Ultrasound, 2002; 30(6); 349-55
23. Konig N, Cassel M, Intziegianni K, Inter-rater reliability and measurement error of sonographic muscle architecture assessments: J Ultrasound Med, 2014; 33(5); 769-77
24. Nabavi N, Mosallanezhad Z, Haghighatkhah HR, Reliability of rehabilitative ultrasonography to measure transverse abdominis and multifidus muscle dimensions: Iran J Radiol, 2014; 11(3); e21008
25. Teyhen DS, Miltenberger CE, Deiters HM, The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain: J Orthop Sports Phys Ther, 2005; 35(6); 346-55
26. Arangio GA, Chen C, Kalady M, Thigh muscle size and strength after anterior cruciate ligament reconstruction and rehabilitation: J Orthop Sports Phys Ther, 1997; 26(5); 238-43
27. Calmels P, Berthouze S, Barral FG, A comparative study of the muscle strength and mass of the arm flexors and extensors in paraplegic and in non paraplegic basketball players: Paraplegia, 1992; 30(7); 509-16
28. Dupont AC, Sauerbrei EE, Fenton PV, Real-time sonography to estimate muscle thickness: Comparison with MRI and CT: J Clin Ultrasound, 2001; 29(4); 230-36
29. Lau HM, Chiu TT, Lam TH, Measurement of craniovertebral angle with Electronic Head Posture Instrument: Criterion validity: J Rehabil Res Dev, 2010; 47(9); 911-18
30. Ferreira PH, Ferreira ML, Hodges PW, Changes in recruitment of the abdominal muscles in people with low back pain: Ultrasound measurement of muscle activity: Spine (Phila Pa 1976), 2004; 29(22); 2560-66
31. Cheung CH, Shum ST, Tang SF, The correlation between craniovertebral angle, backpack weights, and disability due to neck pain in adolescents: J Back Musculoskelet Rehabil, 2010; 23(3); 129-36
32. Cheung Lau HM, Wing Chiu TT, Lam TH, Clinical measurement of craniovertebral angle by electronic head posture instrument: A test of reliability and validity: Man Ther, 2009; 14(4); 363-68
33. Ruivo RM, Pezarat-Correia P, Carita AI, Cervical and shoulder postural assessment of adolescents between 15 and 17 years old and association with upper quadrant pain: Braz J Phys Ther, 2014; 18(4); 364-71
34. Lee HS, Chung HK, Park SW, The analysis of severity of forward head posture with observation and photographic method: J Korean Soc Phys Med, 2015; 10(3); 227-35
35. Nejati P, Lotfian S, Moezy A, The study of correlation between forward head posture and neck pain in Iranian office workers: Int J Occup Med Environ Health, 2015; 28(2); 295-303
36. Goda H, Hatta T, Kishigami H, Does a novel-developed product of wheelchair incorporating pelvic support prevent forward head posture during prolonged sitting?: PLoS One, 2015; 10(11); e0142617
37. Kim JB, Yoo JK, Yu S, Neck-tongue syndrome precipitated by prolonged poor sitting posture: Neurol Sci, 2014; 35(1); 121-22
38. Hodges PW, Is there a role for transversus abdominis in lumbo-pelvic stability?: Man Ther, 1999; 4(2); 74-86
39. Aurelijus D, Ieva A, Vytautas G, The effect of prolonged sitting on different unstable chairs on trunk muscles activity and posture for individuals with sedentary work; 1-3
40. Hodges PW, Richardson CA, Delayed postural contraction of transversus abdominis in low back pain associated with movement of the lower limb: J Spinal Disord, 1998; 11(1); 46-56
41. Ng JK, Parnianpour M, Richardson CA, Functional roles of abdominal and back muscles during isometric axial rotation of the trunk: J Orthop Res, 2001; 19(3); 463-71
42. Preuss RA, Grenier SG, McGill SM, Postural control of the lumbar spine in unstable sitting: Arch Phys Med Rehabil, 2005; 86(12); 2309-15
43. Kane K, Barden J, Contributions of trunk muscles to anticipatory postural control in children with and without developmental coordination disorder: Hum Mov Sci, 2012; 31(3); 707-20
Tables
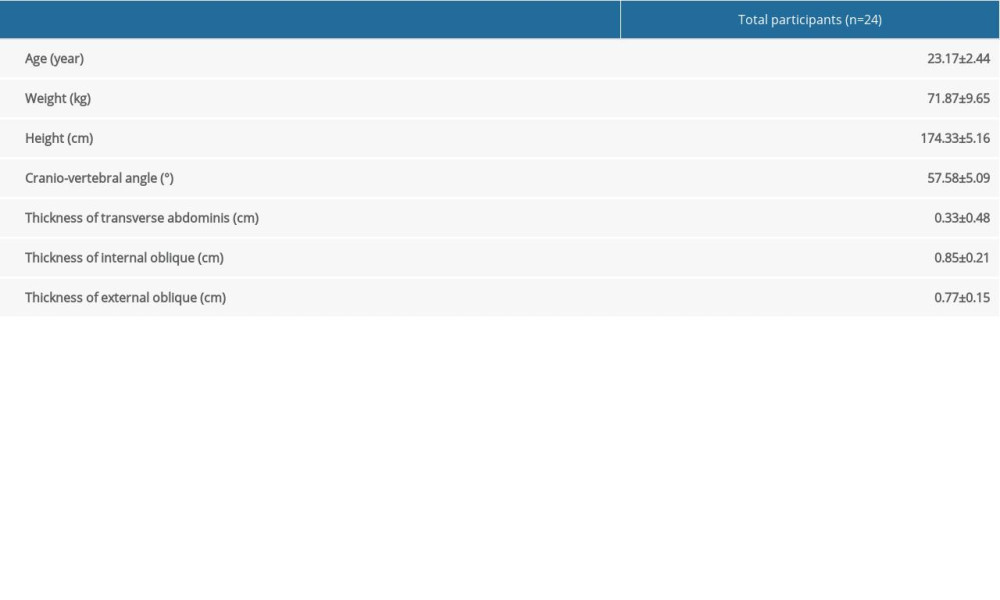 Table 1. Means±SDs of general characteristics and cranio-vertebral angle, transverse abdominis, internal oblique, and external oblique of subjects.
Table 1. Means±SDs of general characteristics and cranio-vertebral angle, transverse abdominis, internal oblique, and external oblique of subjects.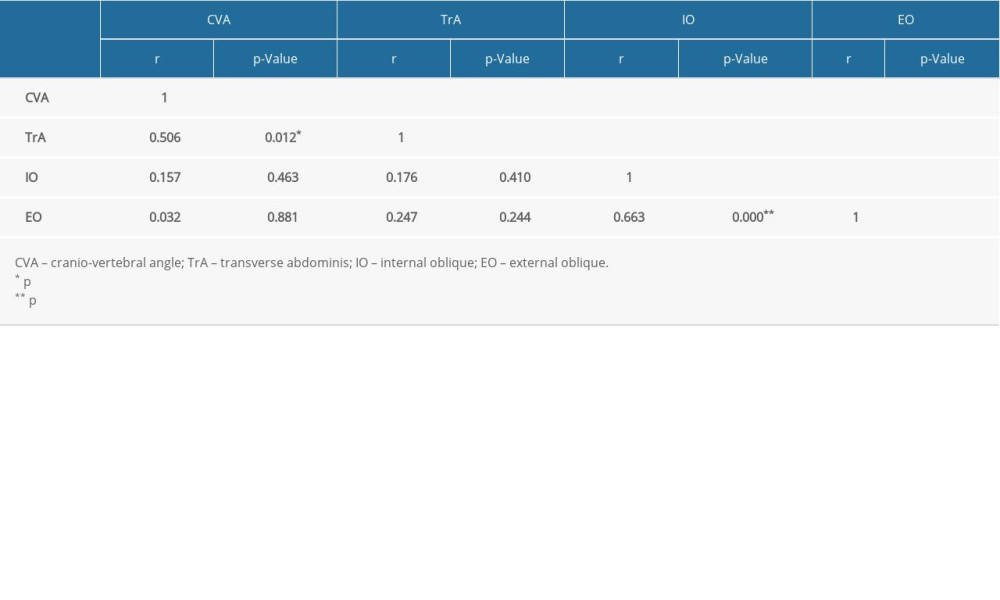 Table 2. Correlation between cranio-vertebral angle, transverse abdominis, internal oblique, external oblique of subjects.
Table 2. Correlation between cranio-vertebral angle, transverse abdominis, internal oblique, external oblique of subjects.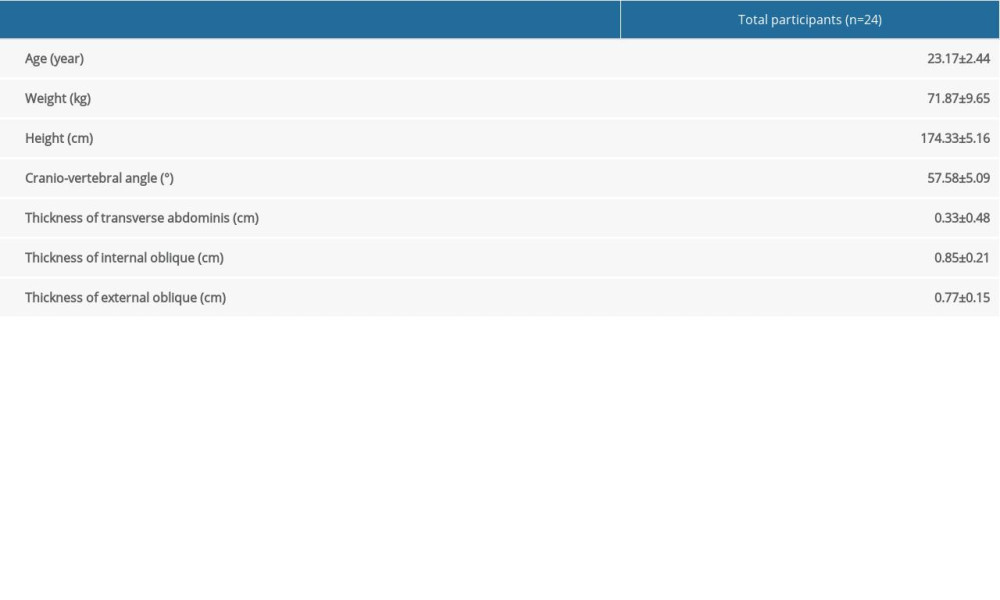 Table 1. Means±SDs of general characteristics and cranio-vertebral angle, transverse abdominis, internal oblique, and external oblique of subjects.
Table 1. Means±SDs of general characteristics and cranio-vertebral angle, transverse abdominis, internal oblique, and external oblique of subjects.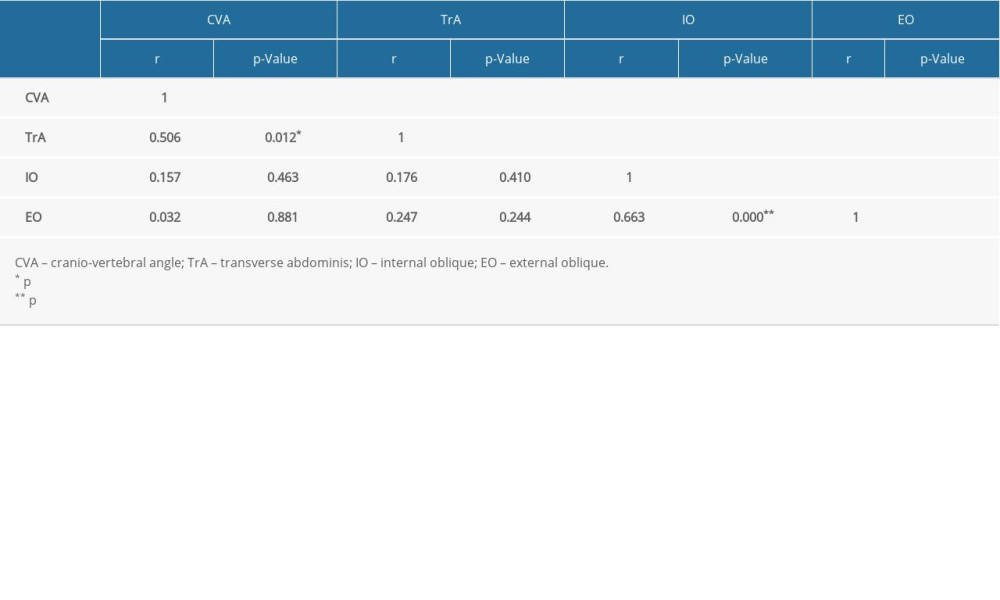 Table 2. Correlation between cranio-vertebral angle, transverse abdominis, internal oblique, external oblique of subjects.
Table 2. Correlation between cranio-vertebral angle, transverse abdominis, internal oblique, external oblique of subjects. In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952









