28 March 2021: Medical Technology
Biomechanical Behavior of All-on-4 and M-4 Configurations in an Atrophic Maxilla: A 3D Finite Element Method
Delal Bozyel1ABCDEFG, Simge Taşar Faruk1ACE*DOI: 10.12659/MSM.929908
Med Sci Monit 2021; 27:e929908
Abstract
BACKGROUND: In edentulous patients, the concept of 4 implants with early loading has been widely used in clinical settings. In the case of bone atrophy in the anterior maxilla, using short implants or an angulated implant may be a good choice for treatment. The occlusal scheme remains a key aspect of All-on-4. The aim of this study was to use the 3-dimensional (3D) finite element method (FEM) to evaluate how different All-on-4 designs for canine-guided and group function occlusion affected the distribution of stress in the atrophic premaxilla.
MATERIAL AND METHODS: A 3D edentulous maxilla model was created and in 3D FEM, 3 different configurations – M4, All-on-4, and short implant – were modeled by changing the anterior implants and using 2 different occlusal schemes. For each model, the occlusal load was applied to simulate lateral movements. For cortical bone, the maximum and minimum principal stress values were generated, and for ductile materials, von Mises stress values were obtained.
RESULTS: No significant differences were detected among the models; generally, however, the highest stress values were observed in the M-4 model and the models with short implants. Slightly higher stress values were observed in the group function occlusion group than in the canine-guided occlusion group.
CONCLUSIONS: To promote better primary stabilization, M-4 or short implant configurations with canine-guided occlusion appear to be preferable for patients who have severe atrophy in the anterior maxilla.
Keywords: Dental Occlusion, Finite Element Analysis, Prostheses and Implants, Alveolar Bone Loss, Biomechanical Phenomena, Computer Simulation, cortical bone, Dental Implants, Dental Stress Analysis, Dogs, Maxilla, Maxillary Diseases, Stress, Mechanical
Background
Dental implantation is an efficient treatment for rehabilitation of fully and partially edentulous patients [1]. High rates of implant and prosthesis survival and patient satisfaction with aesthetics, phonetics, and functionality have been reported [2,3].
The clinical success and durability of dental implants are largely controlled by mechanical factors [4]. The shape and size of the infrastructure, passive compatibility with the implant platform, number and distribution of implants, provision of aesthetics, and oral hygiene affect the success of hybrid prostheses such as the All-on-4. When selecting the infrastructure, factors that should be considered include resistance to incoming forces, facilitation of oral hygiene, creation of occlusal surfaces, and use acrylic resin to ensure maximum retention of prosthetic teeth and prosthetic edges [5,6]. When choosing the diameter, length, and design of an implant, the amount of existing bone should be considered because it affects the success of the treatment [7]. In fully edentulous patients, the “4 implants with early loading” method (All-on-4) has been widely used in clinical settings. Success with this treatment modality depends on the distal inclination of the posterior implants and the axial positioning of the front 2 implants [8–10]. Those factors not only increase primary stability but also decrease the need for bone augmentation by optimizing use of available bone [11].
In cases of bone atrophy, use of a short implant in the anterior with a zygomatic implant placed in the posterior also is recommended. In an atrophic maxilla, use of short or angled implants is an alternative to grafting. Other posterior implant positions can be achieved by placing the distal implants toward the anterior during All-on-4 treatment [12–14].
Inserting the long implants at an angle and posterior in the maxilla, in the shape of the letter “M,” is another alternative for atrophic bone that provides support from the thick basal bone instead of the thin crestal bone [15]. In an M-shaped configuration (M-4), the anterior implants are angled distally up to 30 degrees in the axial plane and extended into the lateral nasal rim [16]. This placement supports the anterior sinus wall and lateral nasal wall, facilitating maximum anterior or posterior spread. Angled implants can settle in the bone pyramid in front of the maxillary sinus without disturbing vital anatomical structures, such as arteries and nerves [16,17].
Implants and their bony integument need to be planned and placed to support the functional and parafunctional requirement of occlusal loading [18]. This is achieved with correct occlusal planning. The primary goal of occlusal therapy is to maintain and/or improve optimal masticatory function and comfort, including stability of the occlusion [19]. The choice of an occlusal scheme dictates the design of occlusal contacts between opposing teeth during centric relation and how the mandible will function. The number and concentration of these contacts determines the amount and direction of force conducted from the denture down to the bone [20]. Group function occlusion is defined as multiple contact relationships among the maxillary and mandibular teeth during lateral movements on the working side. Canine-guided occlusion is defined as preventing contact of the posterior teeth by vertically and horizontally overlapping the canine teeth when the mandible movements are irregular [21]. Experts also recommend group function or guidance with flat linear pathways and in lateral and protrusive movements with All-on-4 treatments [4].
With All-on-4 treatment, it is important to ensure an occlusal relationship that will result in even distribution of occlusal forces. To achieve that, it is necessary to maximize the bilateral intercuspal contacts, create freedom in the centric position, eliminate premature contacts in the intercuspal position and centric relationships, and free the centric during lateral and protrusive movements of the mandibula [4]. Tallarico et al [22] have suggested use of anterior-guided or balanced occlusion in All-on-4 treatment that abuts natural dentition.
Decreasing the shear (unaligned) forces and targeting the compression (aligned) forces by applying forces in the occlusal direction is recommended. Therefore, occlusion should generate axial forces rather than lateral or horizontal forces. The reason for higher stress and tension around the crestal bone is nonaxial forces [23]. Among the ways to apply force and movement are a concentrated load (at a point or single node), force on a line or edge, a distributed load (force varying as an equation), bending movements, and torque. The finite element method (FEM) allows researchers to predict stress/strain distribution patterns in the peri-implant bone.
With FEM, elasticity modulus and Poisson’s ratio are 2 important distinguishing features in materials with homogeneous, isotropic, and linear elastic properties [24]. FEM has been found to be more effective than other stress analysis methods, such as strain gauge and photoelastic methods. With FEM, it is possible to assign numerical values to displacement of structures, bending, fracture, stress, vibration, elastic deformations of materials, and bond strength [25].
The aim of the present study was to analyze the distribution of stress in group function and canine-guided occlusion for All-on-4 concepts modeled with 3D-FEM using short, standard, and angled standard implants (M-4) placed anteriorly.
Material and Methods
In the present study, 3D FEM (Ay Tasarım, Ankara, Turkey) was used. Models were created geometrically with VRMesh software, version 6.1 (Bellevue, Washington, United States) and then transferred to Algor Fempro software (Algor Inc., Version 2.0, Pittsburgh, Pennsylvania, United States) using a standard tessellation language (STL) format for analysis. The STL format is widely used in 3D modeling programs. With the coordinate information for the nodes in STL format, no information was lost during the transfer between programs. After the transfer to the Algor software, data from the model about the maxilla and the material used for dentition were input. Each of the structures that constituted the models bear had their own material values (modulus of elasticity and Poisson’s ratio), which defined their physical properties. We expressly chose common values to express them [24]. All of the models developed were for linear, homogeneous, and isotropic materials. The homogeneity of a material indicates that the mechanical properties of all its structural elements are similar. Homogeneity indicates that the isotropic material properties of a structural element are the same in all directions.
The implants and prosthetic parts used in the present study were scanned with a 3D scanner (SmartOptics 3D scanner, Germany). The models obtained in STL format were transferred to Rhinoceros software, version 4.0 (Seattle, Washington, United States). With the Rhinoceros software, the transfer of force between the upper and lower parts of the prosthesis and implant screws and bone tissues was assessed.
To model bony tissue in the maxilla (3M Iluma CBCT, IMTEC, United States), a computed tomography (CT) scan from a patient was used. With CT, a 3D geometric model was generated of an edentulous maxilla with extensive crestal bone loss. Spongious bone was obtained from the bone tissue and assessment of the force transfer was achieved by making necessary adjustments. Modeling was performed with the Rhinoceros software by placing the models at the correct coordinates in 3D space. Boundary conditions for the model were defined according to the union of the maxilla to the skull base, by which the movement of the maxilla was restrained. Boundary constraints were applied to the top of the bone. The movements of the nodes in this area were completely constrained.
There were 3 models in the present study:
In all models, standard-length implants (4.3×13 mm) (Nobel Biocare, Zurich, Switzerland) were placed in the second premolar area at a 30-degree angle. In each model in the All-on-4 protocol, the posterior implants were angled in exactly the same position.
To create prosthetic models, abutments and implants were evaluated as a whole unit. The multi-unit abutments were modeled to be 4 mm in diameter and 4 mm in length for the anterior region and 5 mm in diameter and 4 mm in length for the posterior region. The implant infrastructure was titanium. In the present study, the superstructure prosthesis consisted of 12 monolithic lithium disilicate single crowns. The base height was 11 mm and the crown length was 4 mm. Acrylic resin was used for the gingival part.
To create different occlusion designs, stresses were measured at different points and occlusal schemes and cuspal contacts were established in accordance with the standards reported in the literature [22]. Occlusal loads were applied as oblique occlusal loads to assess how the models performed against a lateral force. Forces were defined on contacts formed in the lateral movement position in canine-guided and group function occlusion. A unilateral horizontal static load of 93 N was applied for canine-guided occlusion in the palatal region of the left canine and 200 N was applied for group function occlusion in the palatal region of the left canine molar to observe the stress distribution in the stress analysis phase, as described by Silva et al [26] and Turker et al [27].
A color scale was used to express the concentration of stress. Red indicated regions with higher stress values whereas navy blue indicated areas with lower stress values. These color codes also corresponded to numerical values for von Mises stress and maximum/minimum principal stress. The von Mises stress values represented stress values for elastic material. The maximum and minimum values were for stress on cortical and spongious bone. Maximum and minimum principal stresses (Pmax and Pmin, respectively), allowed for differentiation between tensile and compressive stresses. The maximum and minimum von Mises stresses and Pmax and Pmin values were localized and quantified for comparison. The data are shown as maximum and minimum values and were subject to numerical comparison.
In the present study, it was assumed that the trabecular-cortical bone, bone-implant, implant-multi-unit abutment, multi-unit abutment-framework, and framework-prosthetic restoration interfaces were bonded to each other. Some simplifications were made in the models, which were related to the osseointegration level, bone type, boundary conditions, and the amount and direction of forces. The limitations were similar for all 3 models in the present study. The aim of the research was to biomechanically compare the behavior of several implant configurations and not to determine exact stress values.
Results
STRESS IN ALVEOLAR BONE:
For all 3 models, stress values were higher for group function than for canine-guided occlusion (Figures 2–5). The Pmax stress values on the cortical bone were similar in all 3 models on the working side with group function occlusion. The stress values for the posterior region were 21.83 N/mm2 in Model 1, 22.83 N/mm2 in Model 2, and 21.95 N/mm2 in Model 3, and for the anterior region, they were 7.72 N/mm2 in Model 1, 6.09 N/mm2 in Model 2, and 7.19 N/mm2 in Model 3 on the working side. The highest Pmin stress value was observed on cortical bone in the posterior region; however, the highest von Mises stress value was observed in Model 3 (28.92 N/mm2). In spongious bone, Pmax and Pmin values were detected mostly in the posterior region on the working side. For Pmin, only the posterior implant area was red (indicative of the highest stress area); for Pmax, however, that color was uniformly distributed in the bone.
For canine-guided occlusion, Model 3 demonstrated the highest Pmax stress value (10.58 N/mm2) on cortical bone. The highest Pmin values were detected mostly in the posterior region of the working side; the Pmin values were similar for all 3 models. Stress values for the posterior region were 8.71 N/mm2 in Model 1, 9.32 N/mm2 in Model 2, and 9.31 N/mm2 in Model 3 on the working side. The highest Pmax stress values were observed in the posterior region and the lowest Pmax stress values were detected in Model 3 on the spongious bone. The highest Pmin stress values were detected in Model 2 for the working side in the posterior region (0.463 N/mm2), whereas the lowest Pmin stress values were observed in Model 3 on the balancing side in the posterior region (0.271 N/mm2).
STRESS IN ABUTMENTS:
The stress values observed in group function occlusion were higher than for canine-guided occlusion in all the models (Figures 6, 7). In group function, the highest stress values were detected on the working side and in the abutments of Model 3 (86.29 N/mm2 and 29 308 N/mm2, respectively). In the anterior region, the stress values on the balancing side were similar in Models 1 and 2 (18.26 and 19.33 N/mm2, respectively); in Model 3, the stress value was lower (17.76 N/mm2).
In canine-guided occlusion, the stress values in posterior abutments on the working side were similar in Models 1 and 2 (26.42 and 27.03 N/mm2, respectively). The lowest stress values were observed in Model 3 (23.78 N/mm2). The stress values in the anterior abutments were similar in all of the models.
STRESS IN IMPLANTS:
For group function occlusion, the von Mises stress values in posterior implants were almost the same for Models 3 and 1 (139.87 N/mm2 and 139.37 N/mm2, respectively), while the lowest stress was in Model 2 (132.25 N/mm2) on the working side (Figure 8). The highest stress values were noted in Model 2 on the working side (48.20 N/mm2) for anterior implants. The lowest stress values were noted in Model 3 on the working and balancing sides of anterior implants (34.62 N/mm2 and 27.58 N/mm2, respectively).
In canine-guided occlusion, the von Mises stress values for the anterior implants on the working side were similar in Models 1 and 2 (23.72 N/mm2 and 23.35 N/mm2, respectively), but on the working side of Model 3, there was lower stress (17.36 N/mm2) (Figure 9). The highest von Mises stress values (39.29 N/mm2) were detected in Model 1 on the working side of posterior implants.
STRESS IN PROSTHESIS:
In the anterior region, Model 2 (0.004506 N/mm2) had the highest stress values for group function occlusion, whereas the highest stress values for canine-guided occlusion were in Model 1 (0.003481 N/mm2). The lowest stress values for group function occlusion were in Model 1 (1.579735 N/mm2), whereas Model 2 had the lowest stress values (0.223784 N/mm2) for canine-guided occlusion in the premolar-molar area.
STRESS IN FRAMEWORK:
For all models of group function occlusion, the posterior region had the highest stress values and the numerical values were very similar to each other. In canine-guided occlusion, on the working side, the posterior side had the highest stress values and the stress values were similar in Models 2 and 3 (27.27 N/mm and 25.56N/mm2, respectively); however, they were lower in Model 1 (16.25 N/mm2).
Because the values obtained from FEM are the result of mathematical calculations without variance, it was impossible to perform a statistical analysis of them. The values obtained in finite element analysis are fixed numerical values and there is no variable value [28]. Therefore, the results of the mathematical solutions were converted into visual results, characterized by degrees of color and graphics. We then compared and interpreted the stress values obtained and their distributions.
Discussion
The clinical success and longevity of dental implants depend upon their ability to withstand functional loading. Implant failures can be explained with incorrect occlusal design, which may concentrate stress in the bone and lead to bone resorption. Occlusion type and occlusal design are the most important factors in the long-term success of an implant-supported prosthesis [29]. The occlusal scheme is also important in the All-on-4 concept, which offers treatment options with few implants. In the present study, stress values for bone, abutments, implants, and prosthetics were examined for dental restoration with group function or canine-guided occlusion using the All-on-4 concept. This comparison was performed using 3D FEM. FEM was chosen because it is composed of elements that are easy to calculate on a computer and it is an appropriate method for comparing various types of occlusions.
Studying a patient’s current oral health, chewing pattern, static occlusion type, craniofacial morphology, and parafunctional habits could provide important and relevant information about which functional occlusion type is suitable for that individual [30]. Occlusal load tends to be predominantly aligned vertically and parallel with the long axis of the teeth; however, with grinding of food, there are shearing forces among the teeth and forces directed laterally and/or anteroposteriorly [31]. Occlusion and attachment, with their proprioceptive feedback mechanism, are lost when natural teeth are missing. The periodontal ligaments in a natural tooth can make a difference in how force is adapted compared with osseointegrated implants because they have shock-absorbing and stress-distributing functions. Furthermore, non-vertical forces on natural teeth during function influence only the teeth involved and are generally tolerated, whereas with implants, the effect involves the crest of the bone, which is usually traumatic to the supporting structures [32]. Therefore, in the present study, it was preferable to simulate lateral stresses to compare the effect of non-vertical forces on All-on-4 treatment concepts. For lateral movement, canine guidance opposing natural dentition, group function opposing a posterior implant-supported prosthesis with flat linear pathways, and minimum vertical superimposition are recommended [4]. The destructive effects of lateral movements have been observed largely with group function and canine-guided occlusion [33]. For this reason, lateral movement stress was examined for canine-guided occlusion and group function occlusion in the present study. Either canine-guided or group function occlusion can be used to guide the laterality of movement of laterality with dental contact [33]. There is general agreement that balancing contact of the side teeth is not desirable in lateral movements [30]. Balancing side interference is a contact on the balancing side that causes disclusion of the working side or that interferes with smooth gliding movements [30]. In the present study, with group function occlusion, stress values were higher on the balancing side than on the working side. A similar finding was made by Miralles [34], showing that stress concentration is mostly seen on the balancing side in group function occlusion. Likewise, in the present study, the balancing side may have had higher stress values than the working side when the incorrect occlusion scheme was restored. In the present study, there were no major differences between stress values on the balancing and working sides. Therefore, canine-guided and group function occlusion may be suitable for All-on-4 and M-4 treatments.
A crucial factor that affects the outcome of implant treatment is the way occlusal forces are transferred to the bone-implant interface via the superstructure and the implant [35]. The Pmax and Pmin stress values for bone were higher for group function than for canine-guided occlusion in the present study. With both occlusion types, higher stress values have been demonstrated in cortical than in spongious bone in the present study, which is in keeping with several previous studies [36,37]. The explanation for this may be the high-elasticity modulus of cortical bone [37]. Generally, cortical bone is prioritized in terms of bone quality because of the role it plays in providing primary stability; its modulus of elasticity also is an element that contributes to the mechanical strength of the bone [38].
One of the important factors that causes implant failure is bone remodeling, which is affected by changes in normal biological stress [38]. Load transfer from implants to surrounding bone depends on the type of loading; the shape, length and diameter of the implants; the bone-implant interface; characteristics of the implant surface, the type of prosthesis; and the quantity and attributes of surrounding bone [24]. Also, a review of stresses on elastic materials during lateral movement has showed that some stress values here higher in group function than in canine-guided occlusion. In the present study, the highest von Mises stress levels, obtained with elastic materials, were calculated for the abutments and implants in group function occlusion. If occlusal stresses are well tolerated by the remaining natural dentition, the lateral disclusion factors should be on the natural teeth. When 2 substances have a differing modulus of elasticity and one is loaded, the stress will be located where the substances meet. There is a greater variance in elasticity between titanium and spongious bone than between titanium and cortical bone [23]. Group function occlusion was found to result in higher stress values on the prosthesis than canine-guided occlusion. Canine-guided occlusion ensures that the force is met in lateral movements without damaging the antagonist’s teeth. Hence, it can be said that canine-guided occlusion is more protective against stress than group function occlusion. This finding has been supported by reports from Karamshahi et al and Sidana et al [21,30].
The critical threshold value is the maximum force level that a material can withstand without deformation. Previous studies have shown that bone can withstand approximately 150 N tensile strength and 250 N compression force. Resorption has been observed in bone in cases in which these stress values were exceeded [39]. However, occlusal loads are continuously formed during the functional movement of jaws. Therefore, resorptive changes in bone could be caused by these changing loads. The risk of resorption of alveolar bone increases with continued formation of significant stress in the same area [27,40]. Also, the direction and magnitude of force during chewing can vary, unlike the lateral force [41]. To reduce the risks associated with different forms of stress, the type of occlusion should be chosen carefully.
Materials with ductility characteristics have a threshold value as does bone. The yield strength of the implants was determined to be 550 MPa, the threshold stress value beyond which the von Mises deforms [42]. In the present study, no stress exceeding that value was detected. Therefore, group function and canine-guided occlusion – but especially the latter – are recommended for long-term success with a prosthesis, based on the results of the present study.
Bone types III and IV, which represent a small amount and low quality of bone, have been considered a prosthetic and surgical challenge for implant rehabilitation in the atrophic maxilla. In the presence of marginal bone loss, the lever arm of force will be greater; therefore, movement at the marginal bone level will result in increased stress levels [43]. With progressive bone loss after tooth extraction in the premaxillary area, the alveolar crest may approach anatomic structures, which complicates implant placement and prosthesis retention [44]. The All-on-4 concept is an option for placing a short or angled implant in the premaxilla region [14,15]. Model 3, the scenario in which angulated implants were used in the anterior region, had the highest Pmin stress values in the posterior and anterior regions on the balancing side with both types of occlusion. The highest stress values on the balancing side can be attributed to a decreased load on the working side, which compensates for the stress on the other side. The highest stress values were obtained in Model 3 for abutments on the working side with group function occlusion. Some researchers have suggested that in the presence of an angled abutment, it is preferable to reduce forces associated with lateral movement [45]. Despite that, the M-4 model is advantageous because it allows insertion of longer implants and angled abutments in situations in which primary stability is a concern [46]. Besides that, among the implant concepts, Model 3 had the lowest and Model 1 the highest von Mises stress values in the posterior region with canine-guided occlusion; in Model 3, the stress values may have been reduced by use of angled implants. The success of angled implants has been demonstrated in various studies [47,48]. Some reports, however, have shown no difference between angled and non-angled implants in terms of biomechanics. Those researchers have stated that the crucial factor was the coronal region [49,50]. In the present study, the red color, which was indicative of the highest stress, was concentrated in the coronal region. From the point of view of biomechanics, the position of the coronal end of the implant is more important than its inclination, whether the implant is tilted or not [49].
Setting the occlusion correctly is important because every 10-degree increase in the implant angle results in a 5% increase in the cortical bone. Likewise, if the loads onto the implants are angulated, peri-implant bone resorption will occur as a consequence of shear forces in the implant-bone surface [37]. In these cases, some searchers have recommended the use of a zygomatic implant [51,52]. Other studies have recommended the All-on-6, a tilted configuration using 6 implants, instead of the All-on-4 to reduce stress [4,12]. The results of the present study, however, showed that M-4 treatment was successful in dissipating incoming forces. Jensen et al [16] reported a superior biomechanical advantage for the M-4 technique in comparison with the standard All-on-4 technique and recommended the M-4 configuration as an option for use by dentists to achieve implant stability. Likewise, in the present study, the stress values for Models 2 and 3 were similar to those for Model 1, which has been presented as the classical All-on-4 treatment. For this reason, the use of short and angled implants may be preferable in patients who have atrophic maxilla.
A recent systematic review underscored the importance of improvements in implants and surgical techniques for successful rehabilitation using short implants [14]. With All-on-4 treatment, it may be possible to use short implants before advancing to more difficult and technically demanding rehabilitation protocols. In the present study, the lowest von Mises stress values in the posterior region on the working side in group function and canine-guided occlusion were seen with the implants in Model 2, which were short and in the anterior region; however, the highest stress values were obtained in the anterior region in Model 2 with group function occlusion. In the present study, short and long implants were combined for treatment of completely edentulous maxilla using an All-on-4 design, thus establishing the importance of total control of occlusal design to distribute the occlusal load to the long axis of the implants. Furthermore, the value of short implants was confirmed by the fact that most of the occlusal forces on the bone and/or implant interface are spread across the coronal part of the implant body and close to the alveolar crest, where there is cortical bone at the level of the implant platform [14]. Other studies also have shown that parafunctional activities such as bruxism, which generate overloads, negatively impact short implants [26,53]. Also, in a FEM study, maximum bone stress was determined to be independent of implant length, which is in keeping with the results of the present study [54]. Model 2 showed the highest stress values in the anterior region with group function occlusion in a prosthesis; the presence of antagonistic natural dentition and the type of occlusal scheme may have impacted this result. The occlusal scheme also improves oral hygiene and reduces the risk of porcelain fracture. Dental ceramics are the material most commonly used to fabricate crowns [27,29]. For this reason, they were used in the present study and found to be suitable for the treatment concepts tested. Some studies have shown that ceramic material cannot absorb stress because it is rigid [55]. Reports also suggest that occlusion should be adjusted carefully to prevent fractures and attention should be paid to canine relationships to prevent early contact in the posterior [6]. Likewise, some authors have suggested that group function occlusion is associated with more mechanical complications in the form of ceramic chipping than canine-guided occlusion [56].
A suitable framework design affects the retention and stability of the denture and stress on the abutment and relevant tissues [57]. The highest stress values were seen in Model 2 in the posterior region with group function or canine-guided occlusion on the working and balancing sides of the framework. In contrast, with Model 3, higher stress values were seen in the anterior region with group function and canine-guided occlusion on the working and balancing sides. With canine-guided occlusion, however, these high-stress values were similar for the implant, abutment, and framework. This means that the stress was not concentrated in a single point, but rather, it was distributed among all the prosthetic elements.
The framework for distributing the chewing burden in hybrid dentures is considered another key factor in long-term clinical success [58]. The use of titanium as a framework material has advantages, such as high biocompatibility, high corrosion resistance, low probability of causing allergies, and lower cost. There is also a direct relationship between the amount of strain and the applied load and elastic modulus of titanium [58]. In the present study, approximate numerical values were assigned to levels of stress on the framework. No studies have shown that there is a relationship between use of short implants and framework failure. Thus, the predictability of short implants is related to their design, the insertion protocol and occlusion concept, the residual bone height and volume, and patient hygiene [57]. However, the present study showed that using a short implant with the correct treatment plan is appropriate for treatment of an atrophic maxilla. This may have been a result of increased bone density, decreased stress concentration in bone, and the improved mechanical properties of the implant-bone interface, which facilitated primary stability and early osseointegration and compensated for the reduced implant length. In a previous report, the use of angled implants was considered to be more advantageous than the use of short implants [59], which is consistent with the results of the present study.
Immense functional demands are placed on dental occlusion, from the precise positioning of teeth and light holding forces to the genesis of large bite forces. The maxillary canine determines both the lateral and protrusive movements of the mandible, whereas the mandibular canine is in functional contact with the teeth. If there is no canine-guided occlusion because of canine loss, group function occlusion is indicated; that also has been observed in worn teeth, such as in patients with bruxism [30]. It is important, therefore, to make adjustments based upon the antagonists that are clinically apparent in a patient’s natural dentition. Canine-guided occlusion has various disclusion mechanics. With this type of occlusion, forces are directed axially by limiting the contact of the support cusps of the posterior teeth to their opposing fossae at or near their intercuspal position. All other lateral contacts are prevented by the steeper inclines of the canines [60]. Immediate canine disclusion can cause tooth fracture in the implant prosthesis for the edentulous arch, despite the reduced forces anteriorly. Therefore, it is important that clinicians understand the natural differences among teeth and implants and how force, either normal or excessive, can affect implants under occlusal loading.
The present study simulated clinical circumstances as far as was possible; nonetheless, 3D FEM studies present a limitation in simplification of the analysis. On the other hand, it is difficult to standardize all factors in in vivo studies [26]. The numeric results reported in the present study must be taken as predictions within the limitations of the models presented because FEM models are a simplification of the actual structure. For example, a limitation of the FEM models in the present study related to the mechanical behavior of bone, which was presumed to be linearly elastic, homogeneous, and isotropic. Bone is a complicated living structure without a defined pattern; its characteristics vary between individuals and its actual mechanical properties have not been precisely defined [26]. Nevertheless, FEM is a promising noninvasive methodology that provides consistent results through the measurement of stress, compression, and displacement in implants and structures involved in rehabilitation [58,61].
Other limitations of FEM studies are simplification of the analysis regarding boundary conditions, osseointegration level, and direction of forces [46]. Furthermore, stress distributions around the implant vary according to the loading direction in vivo, whereas the loading direction is kept constant in vitro. This is one of the limitations of FEM studies [62]. Because the goal was not to determine exact stress values but to evaluate the effect of different All-on-4 designs, the limitations were the same for all 3 models in the present study. FEM is useful to provide a general overview of the structural behavior of dental materials. However, it has been demonstrated that some factors can modify the hardness and surface characteristics of restoration materials and the health of peri-implant tissues. One of these factors is cyclic loading [63], which can affect a multi-unit abutment screw and create a weak point that results in prosthetic complications [64]. An acid environment and polishing procedures also can affect surface roughness, microhardness, and flexural strength of ceramics [65–67]. Another factor that should be monitored clinically is smoking, which has been associated with increases in marginal bone loss around implants [68]. There are also various factors that influence occlusal forces, such as age, craniofacial morphology, gender, periodontal support of teeth, signs and symptoms of temporomandibular disorders and pain, tooth loss and type of restoration, malocclusion, total area of teeth in contact, oral motor function, and salivary gland function [69]. More study is required to determine the relevance of these variables in clinical practice. Advanced digital imaging techniques can be used to model the bone geometry more realistically and to more accurately predict stress; the anisotropic and nonhomogeneous character of the material must be considered, and boundary conditions must be attentively treated with the use of computational modeling techniques. Although the findings of the present study may increase understanding of the stress levels and distributions in different implant configurations, in vivo studies would be useful to investigate the influence of different configurations on the long-term viability of prosthetic components and implants.
Conclusions
In the present study, for all the models, the strongest stress was observed on the posterior side with group function occlusion. The stresses in question were not destructive, but continuity of them could be destructive to prostheses. Therefore, correct selection of the occlusion scheme could prevent further biomechanical problems.
In the presence of atrophic premaxilla, placement of a short or angulated implant for All-on-4 treatment is a suitable option.
For all models and for both types of occlusion, more stress was observed in cortical than in spongious bone. The high-elasticity modulus of cortical bone could lead to this result, but the stress values seen did not have destructive effects.
Given the limitations of the present study, the results show that use of short and angled implants in the maxillary edentulous area with the All-on-4 technique can be successful if restoration is performed with an ideal occlusion design because the stress values for all of the models tested were below the threshold for causing damage.
Figures
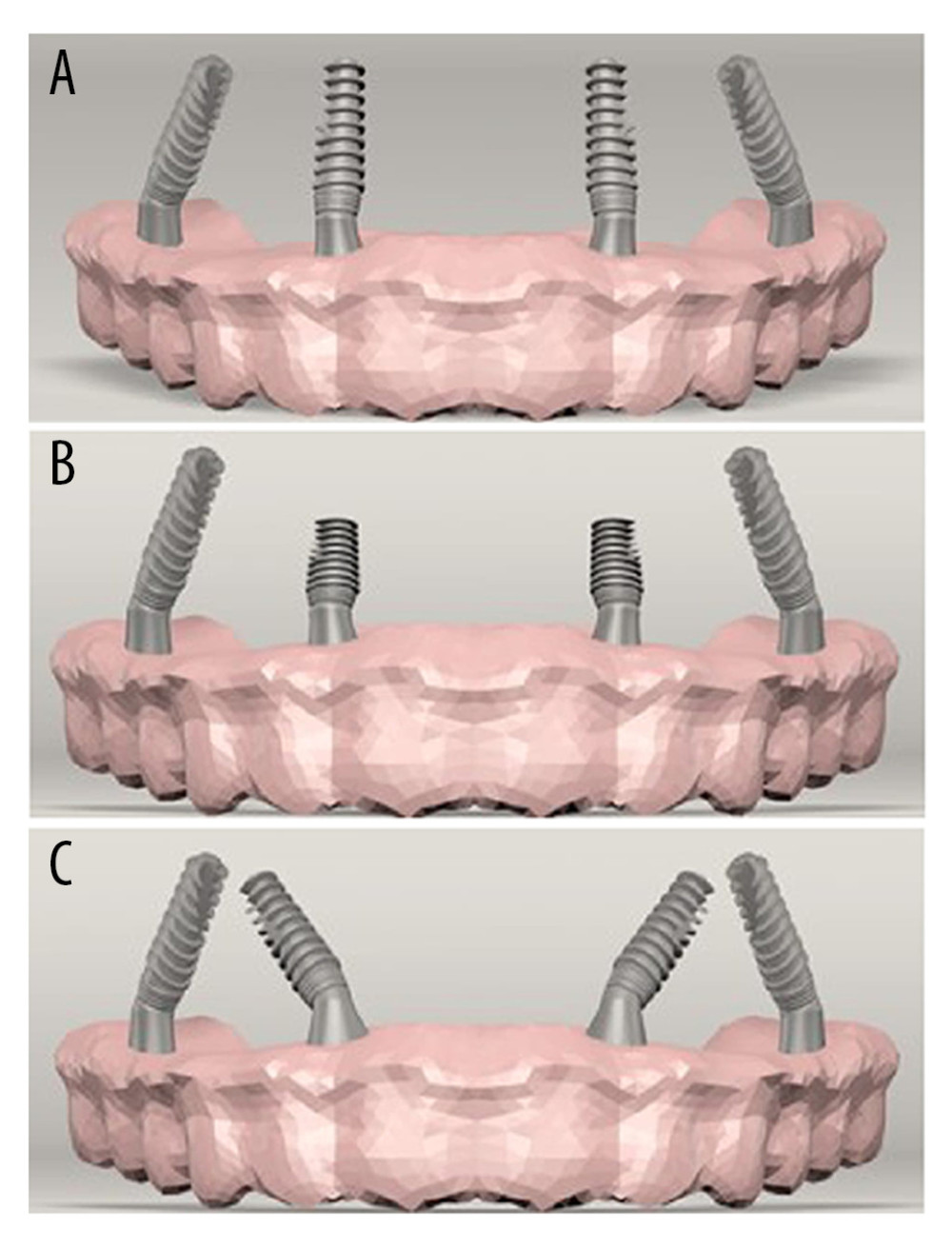 Figure 1. (A) Standard All-on-4 Model (Model 1). (B) All-on-4 Model with short implants (Model 2). (C) M-4 Model (Model 3).
Figure 1. (A) Standard All-on-4 Model (Model 1). (B) All-on-4 Model with short implants (Model 2). (C) M-4 Model (Model 3). 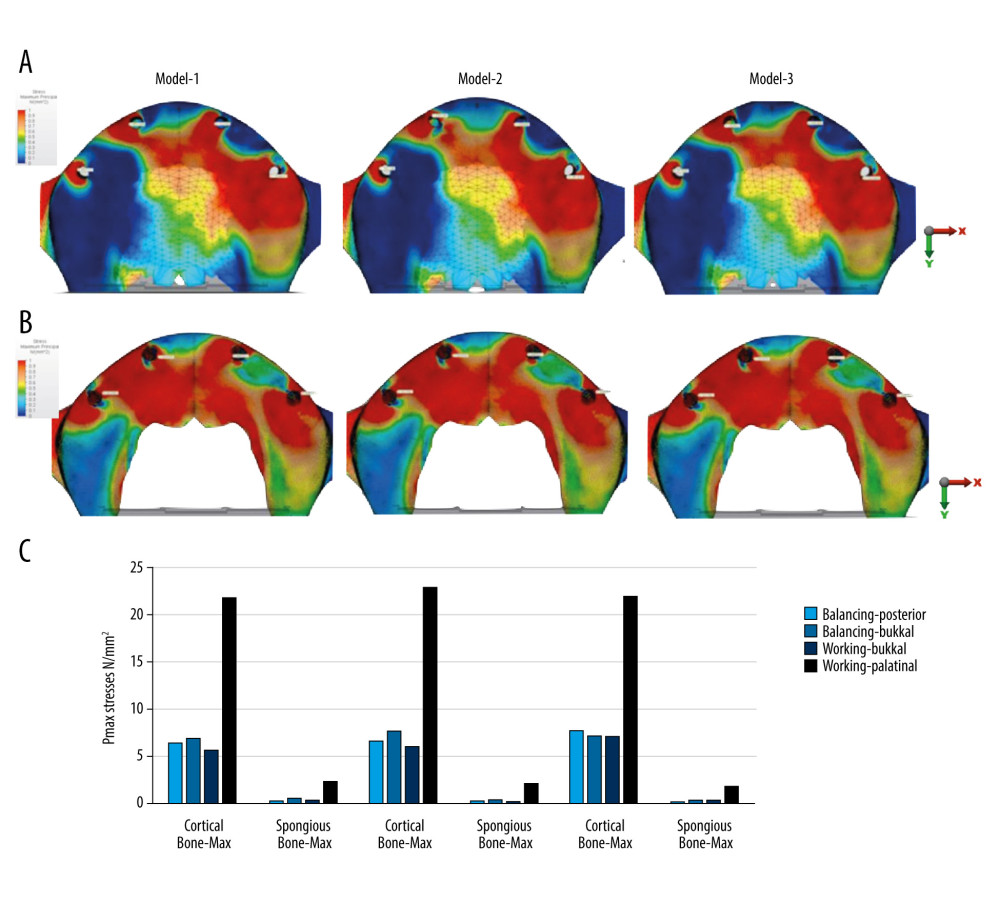 Figure 2. Pmax stresses for group function occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmax stress values (N/mm2) on cortical and spongious bone.
Figure 2. Pmax stresses for group function occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmax stress values (N/mm2) on cortical and spongious bone. 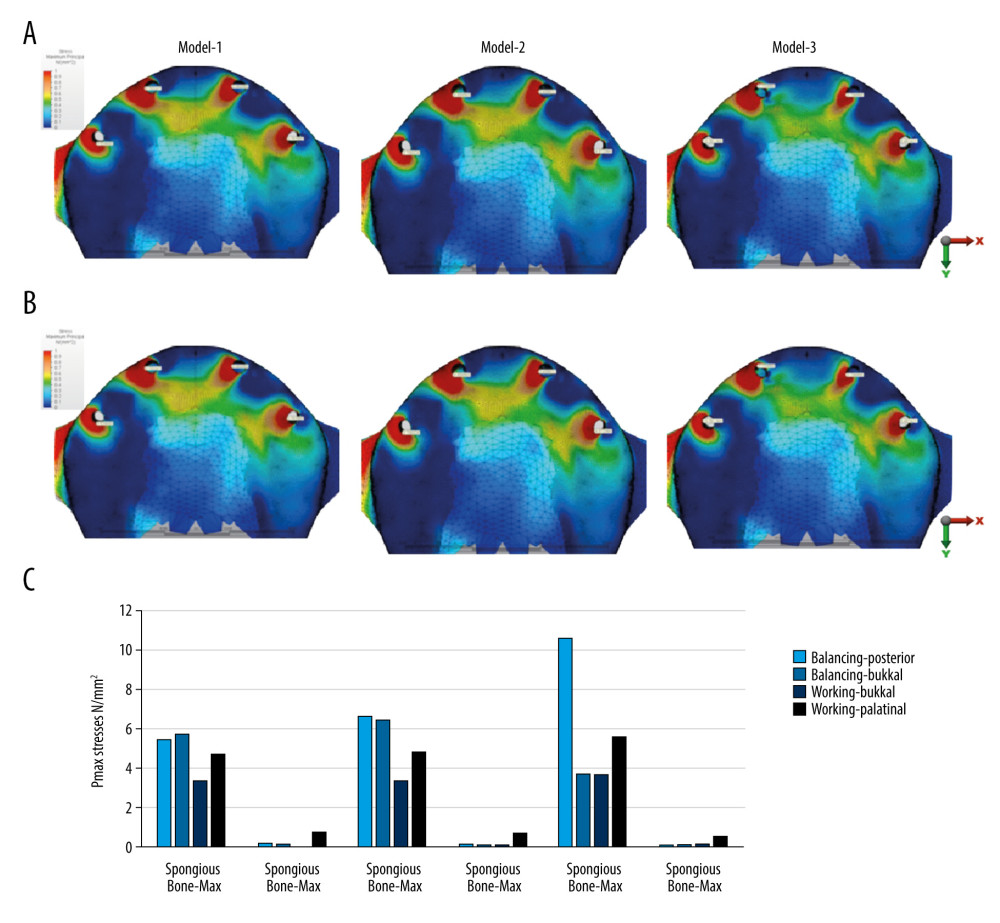 Figure 3. Pmax stresses for canine-guided occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmax stress values (N/mm2) on cortical and spongious bone.
Figure 3. Pmax stresses for canine-guided occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmax stress values (N/mm2) on cortical and spongious bone. 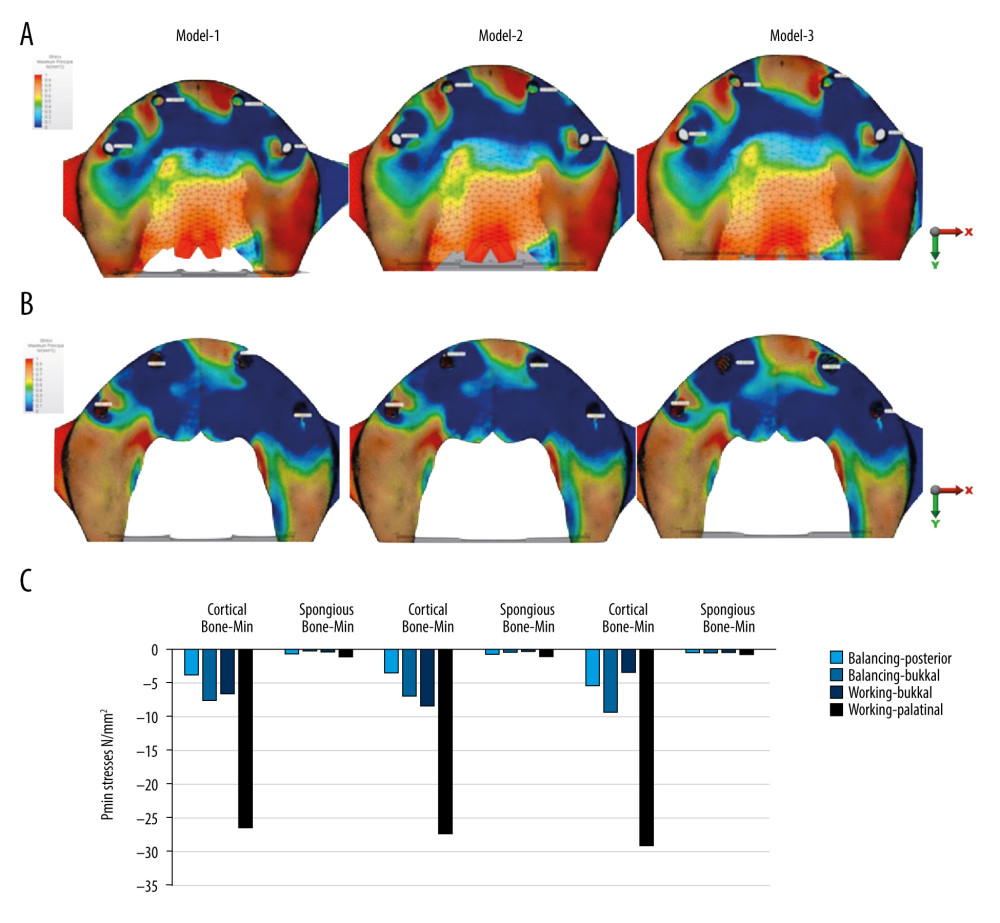 Figure 4. Pmin stresses for group function occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmin stress values (N/mm2) on cortical and spongious bone.
Figure 4. Pmin stresses for group function occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmin stress values (N/mm2) on cortical and spongious bone. 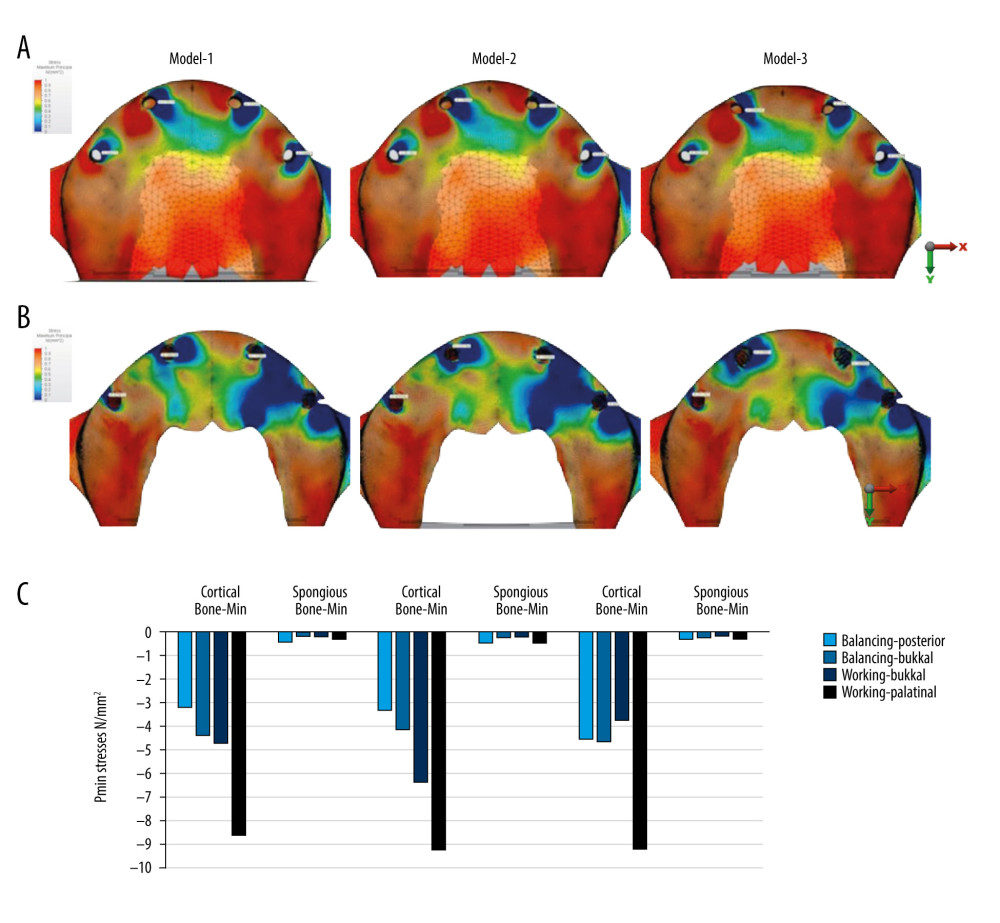 Figure 5. Pmin stresses for canine-guided occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmin stress values (N/mm2) on cortical and spongious bone.
Figure 5. Pmin stresses for canine-guided occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmin stress values (N/mm2) on cortical and spongious bone. 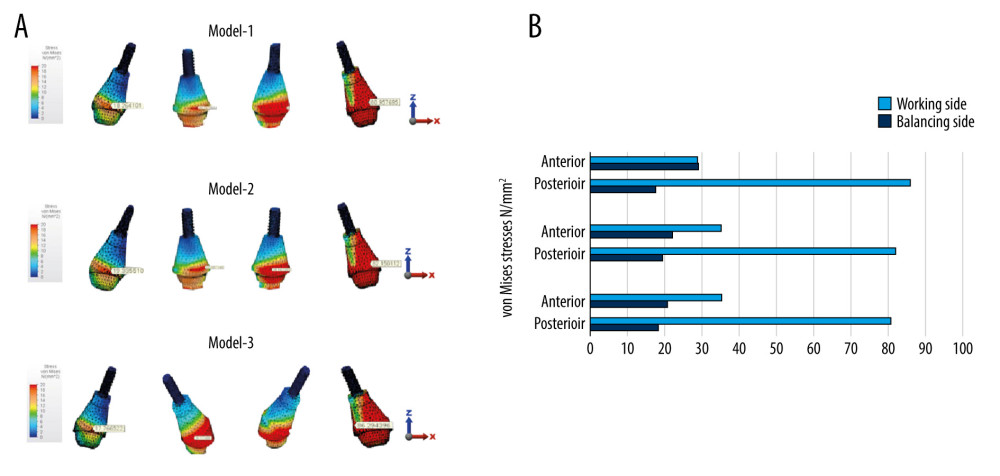 Figure 6. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on abutments for Models 1, 2, and 3 in group function occlusion.
Figure 6. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on abutments for Models 1, 2, and 3 in group function occlusion. 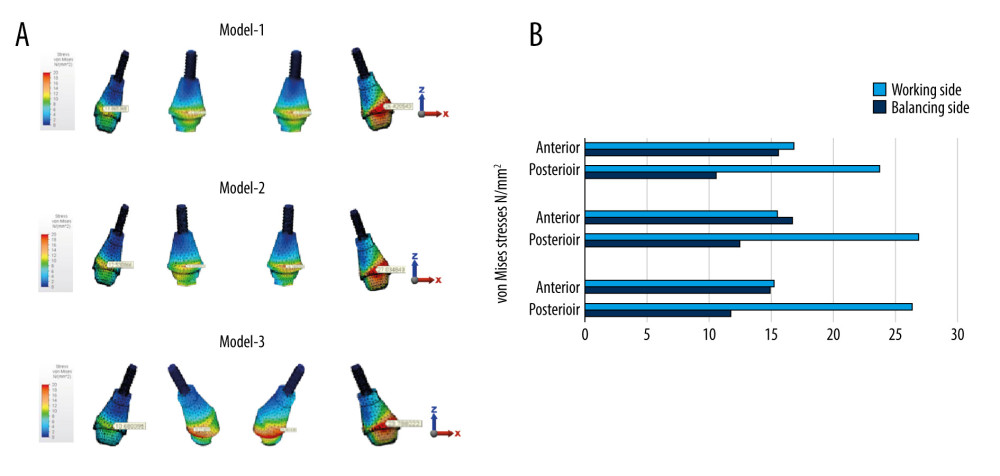 Figure 7. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on abutments for Models 1, 2, and 3 in canine-guided occlusion.
Figure 7. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on abutments for Models 1, 2, and 3 in canine-guided occlusion. 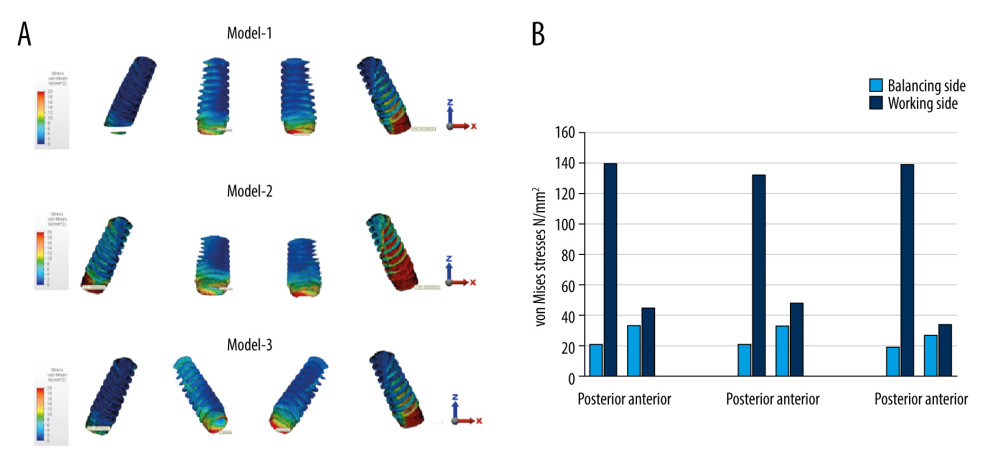 Figure 8. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on implants for Models 1, 2, and 3 in group function occlusion.
Figure 8. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on implants for Models 1, 2, and 3 in group function occlusion. 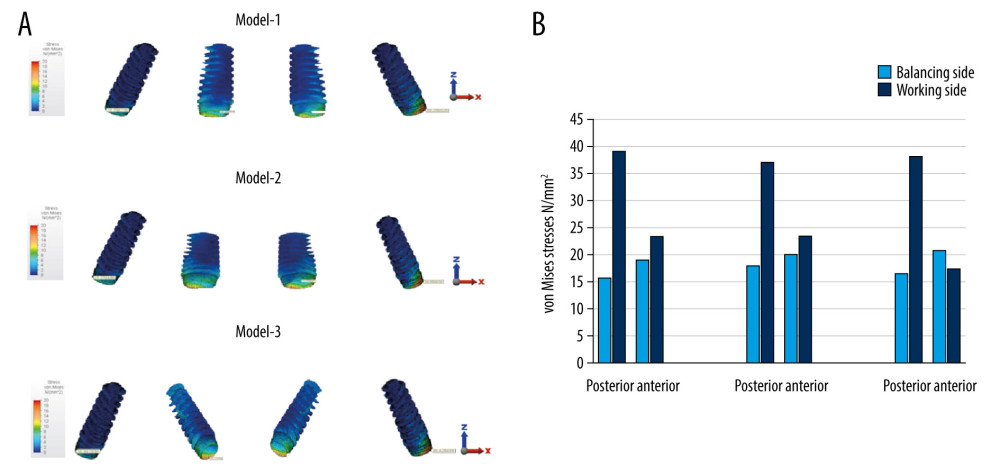 Figure 9. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on implants for Models 1, 2, and 3 in canine-guided occlusion.
Figure 9. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on implants for Models 1, 2, and 3 in canine-guided occlusion. References
1. Chrcanovic BR, Kisch J, Albrektsson T, Survival of dental implants placed in sites of previously failed implants: Clin Oral Implant Res, 2017; 28(11); 1348-53
2. Oh SH, Kim Y, Park JY, Comparison of fixed implant-supported prostheses, removable implant-supported prostheses, and complete dentures: patient satisfaction and oral health-related quality of life: Clin Oral Implant Res, 2016; 27(2); e31-7
3. Chochlidakis K, Einarsdottir E, Tsigarida A, Survival rates and prosthetic complications of implant fixed complete dental prostheses: An up to 5-year retrospective study: J Prosthet Dent, 2020; 124; 539-46
4. Taruna M, Chittaranjan B, Sudheer N: J Clin Diagn Res, 2014; 8(10); ZE16-9
5. Drago C, Howell K, Concepts for designing and fabricating metal implant frameworks for hybrid implant prostheses: J Prosthodont, 2012; 21(5); 413-24
6. Gonzalez J, The evolution of dental materials for hybrid prosthesis: Open Dent J, 2014; 8(Suppl 1); 85
7. Lee JH, Frias V, Lee KW, Effect of implant size and shape on implant success rates: a literature review: J Prosthet Dent, 2005; 94(4); 377-81
8. Maló P, Rangert B, Nobre M: Clin Implant Dentist Relat Res, 2003; 5; 2-9
9. Lopes A, Maló P, de Araújo Nobre M: Clin Implant Dent Relat Res, 2017; 19(2); 233-44
10. Maló P, de Araújo Nobre M, Lopes A, The All-on-4 concept for full-arch rehabilitation of the edentulous maxillae: A longitudinal study with 5–13 years of follow-up: Clin Implant Dent Relat Res, 2019; 21(4); 538-49
11. Hopp M, de Araújo Nobre M, Maló P, Comparison of marginal bone loss and implant success between axial and tilted implants in maxillary All-on-4 treatment concept rehabilitations after 5 years of follow-up: Clin Implant Dent Relat Res, 2017; 19(5); 849-59
12. Almeida EO, Rocha EP, Júnior ACF, Tilted and short implants supporting fixed prosthesis in an atrophic maxilla: A 3D-FEA biomechanical evaluation: Clin Implant Dent Relat Res, 2015; 17; e332-42
13. Verri FR, Santiago JF, Almeida DADF, Three-dimensional finite element analysis of anterior single implant-supported prostheses with different bone anchorages: Sci World J, 2015; 2015 321528
14. Maló P, de Araujo Nobre MA, Lopes AV, Immediate loading short implants inserted on low bone quantity for the rehabilitation of the edentulous maxilla using an All-on-4 design: J Oral Rehab, 2015; 42(8); 615-23
15. Chan MH, Holmes C, Contemporary “All-on-4” concept: Dent Clin, 2015; 59(2); 421-70
16. Jensen OT, Adams MW, Cottam JR, The All-on-4 shelf: Maxilla: J Oral Maxillofac Surg, 2010; 68(10); 2520-27
17. Calandriello R, Tomatis M, Simplified treatment of the atrophic posterior maxilla via immediate/early function and tilted implants: A prospective 1-year clinical study: Clin Implant Dentist Relat Res, 2005; 7; s1-12
18. Gross MD, Occlusion in implant dentistry. A review of the literature of prosthetic determinants and current concepts: Australian Dental J, 2008; 53; S60-68
19. Carlsson GE, Dental occlusion: Modern concepts and their application in implant prosthodontics: Odontol, 2009; 97(1); 8-17
20. Francis T, Ganapathy D, Sivasamy V, Awareness of occlusal scheme for complete dentures among dental students: Drug Invention Today, 2020; 14(4); 536-39
21. Karamshahi M, Ehsanpour MG, Ejlali M, Relationship between occlusion patterns in lateral movement with some periodontal parameters in patients with moderate to severe periodontitis: Ann Dent Spec, 2018; 6(2); 159
22. Tallarico M, Canullo L, Pisano M, An up to 7-year retrospective analysis of biologic and technical complication with the All-on-4 concept: J Oral Implant, 2016; 42(3); 265-71
23. Sheridan RA, Decker AM, Plonka AB, The role of occlusion in implant therapy: A comprehensive updated review: Implant Dent, 2016; 25(6); 829-38
24. Geng JP, Tan KB, Liu GR, Application of finite element analysis in implant dentistry: A review of the literature: J Prosthet Dent, 2001; 85(6); 585-98
25. Mackerle J, Finite element modelling and simulations in dentistry: A bibliography 1990–2003: Comput Methods Biomech Biomed Eng, 2004; 7(5); 277-303
26. Silva GC, Mendonca JA, Lopes LR, Stress patterns on implants in prostheses supported by four or six implants: A three-dimensional finite element analysis: Int J Oral Maxillofac Implant, 2010; 25(2); 239-46
27. Türker N, Büyükkaplan US, Sadowsky SJ, Finite element stress analysis of applied forces to implants and supporting tissues using the “all-on-four” concept with different occlusal schemes: J Prosthodont, 2019; 28(2); 185-94
28. Sannino G, All-on-4 concept: A 3-dimensional finite element analysis: J Oral Implant, 2015; 41(2); 163-71
29. Kim Y, Oh TJ, Misch CE, Occlusal considerations in implant therapy: Clinical guidelines with biomechanical rationale: Clin Oral Implant Res, 2005; 16(1); 26-35
30. Sidana V, Pasricha N, Makkar M, Group function occlusion: Indian J Oral Sci, 2012; 3(3); 124-28
31. Peck CC, Biomechanics of occlusion – implications for oral rehabilitation: J Oral Rehabil, 2016; 43(3); 205-14
32. Chen YY, Kuan CL, Wang YB, Implant occlusion: Biomechanical considerations for implant-supported prostheses: J Dent Sci, 2008; 3(2); 65-74
33. Ifteni G, Apostu A, Tanculescu O, Dental occlusion and the importance of its proper investigation – part II: Roman J Oral Rehabil, 2016; 8(4); 17-22
34. Miralles R, Canine-guide occlusion and group function occlusion are equally acceptable when restoring the dentition: J Evid Based Dent Pract, 2016; 16(1); 41-43
35. Cehreli M, Duyck J, Cooman MD, Implant design and interface force transfer: A photoelastic and strain-gauge analysis: Clin Oral Implant Res, 2004; 15(2); 249-57
36. Eskitascioglu G, Usumez A, Sevimay M, The influence of occlusal loading location on stresses transferred to implant-supported prostheses and supporting bone: A three-dimensional finite element study: J Prosthet Dent, 2004; 91(2); 144-50
37. Saber FS, Ghasemi S, Koodaryan R, The comparison of stress distribution with different implant numbers and inclination angles in all-on-four and conventional methods in maxilla: A finite element analysis: J Dent Res Dent Clin Dent Prospects, 2015; 9(4); 246
38. Van Staden RC, Guan H, Loo YC, Application of the finite element method in dental implant research: Comput Meth Biomech Biomed Eng, 2006; 9(4); 257-70
39. Sugiura T, Horiuchi K, Sugimura M, Evaluation of threshold stress for bone resorption around screws based on in vivo strain measurement of miniplate: J Musculoskelet Neuronal Interact, 2000; 1(2); 165-70
40. Duyck J, Naert I, Rønold HJ, The influence of static and dynamic loading on marginal bone reactions around osseointegrated implants: An animal experimental study: Clin Oral Implant Res, 2001; 12(3); 207-18
41. Morneburg TR, Pröschel PA, Measurement of masticatory forces and implant loads: A methodologic clinical study: Int J Prosthodont, 2002; 15(1); 20-27
42. İplikçioğlu H, Akça K, Comparative evaluation of the effect of diameter, length and number of implants supporting three-unit fixed partial prostheses on stress distribution in the bone: J Dent, 2002; 30(1); 41-46
43. Wallace SS, Froum SJ, Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review: Ann Periodontol, 2003; 8(1); 328-43
44. Mardinger O, Namani-Sadan N, Chaushu G, Morphologic changes of the nasopalatine canal related to dental implantation: A radiologic study in different degrees of absorbed maxillae: J Periodontol, 2008; 79(9); 1659-62
45. Cavallaro J, Greenstein G, Angled implant abutments: A practical application of available knowledge: J Am Dent Assoc, 2011; 142(2); 150-58
46. Ayali A, Altagar M, Ozan O, Biomechanical comparison of the All-on-4, M-4, and V-4 techniques in an atrophic maxilla: A 3D finite element analysis: Comput Biol Med, 2020; 123; 103880
47. Takahashi T, Shimamura I, Sakurai K, Influence of number and inclination angle of implants on stress distribution in mandibular cortical bone with All-on-4 Concept: J Prosthodont Res, 2010; 54(4); 179-84
48. Saab XE, Griggs JA, Powers JM, Effect of abutment angulation on the strain on the bone around an implant in the anterior maxilla: A finite element study: J Prosthet Dent, 2007; 97(2); 85-92
49. Krekmanov L, Kahn M, Rangert B, Tilting of posterior mandibular and maxillary implants for improved prosthesis support: Int J Oral Maxillofac Implant, 2000; 15(3); 405-14
50. Zidani H, Bouslama G, Boukhris H, The all-on-four treatment concept: A case report: IOSR J Dental Med Sci, 2019; 18(1); 2279-861
51. Jensen OT, Cottam J, Ringeman J, Trans-sinus dental implants, bone morphogenetic protein 2, and immediate function for all-on-4 treatment of severe maxillary atrophy: J Oral Maxillofac Surg, 2012; 70(1); 141-48
52. Jensen OT, Complete arch site classification for all-on-4 immediate function: J Prosthet Dent, 2014; 112(4); 741-51
53. Koyano K, Esaki D, Occlusion on oral implants: Current clinical guidelines: J Oral Rehabil, 2015; 42(2); 153-61
54. Pierrisnard L, Renouard F, Renault P, Influence of implant length and bicortical anchorage on implant stress distribution: Clin Implant Dent Relat Res, 2003; 5(4); 254-62
55. Çiftçi Y, Canay Ş, Stress distribution on the metal framework of the implant-supported fixed prosthesis using different veneering materials: Int J Prosthodont, 2001; 14(5); 406-11
56. Abduo J, Tennant M, Impact of lateral occlusion schemes: A systematic review: J Prosthet Dent, 2015; 114(2); 193-204
57. Bhering CLB, Mesquita MF, Kemmoku DT, Comparison between all-on-four and all-on-six treatment concepts and framework material on stress distribution in atrophic maxilla: A prototyping guided 3D-FEA study: Mater Sci Eng C Mater Biol App, 2016; 69; 715-25
58. Tribst JPM, de Morais DC, Alonso AA, Comparative three-dimensional finite element analysis of implant-supported fixed complete arch mandibular prostheses in two materials: J Indian Prosthodont Soc, 2017; 17(3); 255
59. Monje A, Chan HL, Fu JH, Are short dental implants (<10 mm) effective? A meta-analysis on prospective clinical trials: J Periodontol, 2013; 84(7); 895-904
60. Ali SZ, Bhat JT, Canine-guided occlusion simplified: Int J Med Oral Res, 2019; 2; 11-13
61. Greco GD, Jansen WC, Landre J, Biomechanical analysis of the stresses generated by different disocclusion patterns in an implant-supported mandibular complete denture: J Appl Oral Sci, 2009; 17(5); 515-20
62. Deste G, Durkan R, Effects of all-on-four implant designs in mandible on implants and the surrounding bone: A 3-D finite element analysis: Niger J Clin Pract, 2020; 23(4); 456
63. Gaintantzopoulou MD, Farmakis ET, Eliades GC, Effect of load cycling on the fracture strength/mode of teeth restored with FRC posts or a FRC liner and a resin composite: Biomed Res Int, 2018; 2018 9054301
64. Catapano S, Ferrari M, Mobilio N, Comparative analysis of the stability of prosthetic screws under cyclic loading in implant prosthodontics: An in vitro study: Preprints, 2020; 0245.v1
65. Ereifej NS, Oweis YG, Eliades G, The effect of polishing technique on 3-D surface roughness and gloss of dental restorative resin composites: Oper Dent, 2012; 38(1); E9-20
66. Mohammadibassir M, Rezvani MB, Golzari H, Effect of two polishing systems on surface roughness, topography, and flexural strength of a monolithic lithium disilicate ceramic: J Prosthodont, 2019; 28(1); e172-80
67. Colombo M, Poggio C, Lasagna A, Vickers micro-hardness of new restorative CAD/CAM dental materials: Evaluation and comparison after exposure to acidic drink: Materials (Basel), 2019; 12(8); 1246
68. Mumcu E, Dayan SÇ, Effect of smoking and locations of dental implants on peri-implant parameters: 3-year follow-up: Med Sci Monit, 2019; 25; 6104-9
69. Soni R, Yadav H, Pathak A, Comparative evaluation of biting force and chewing efficiency of all-on-four treatment concept with other treatment modalities in completely edentulous individuals: J Indian Prosthodont Soc, 2020; 20(3); 312-20
Figures
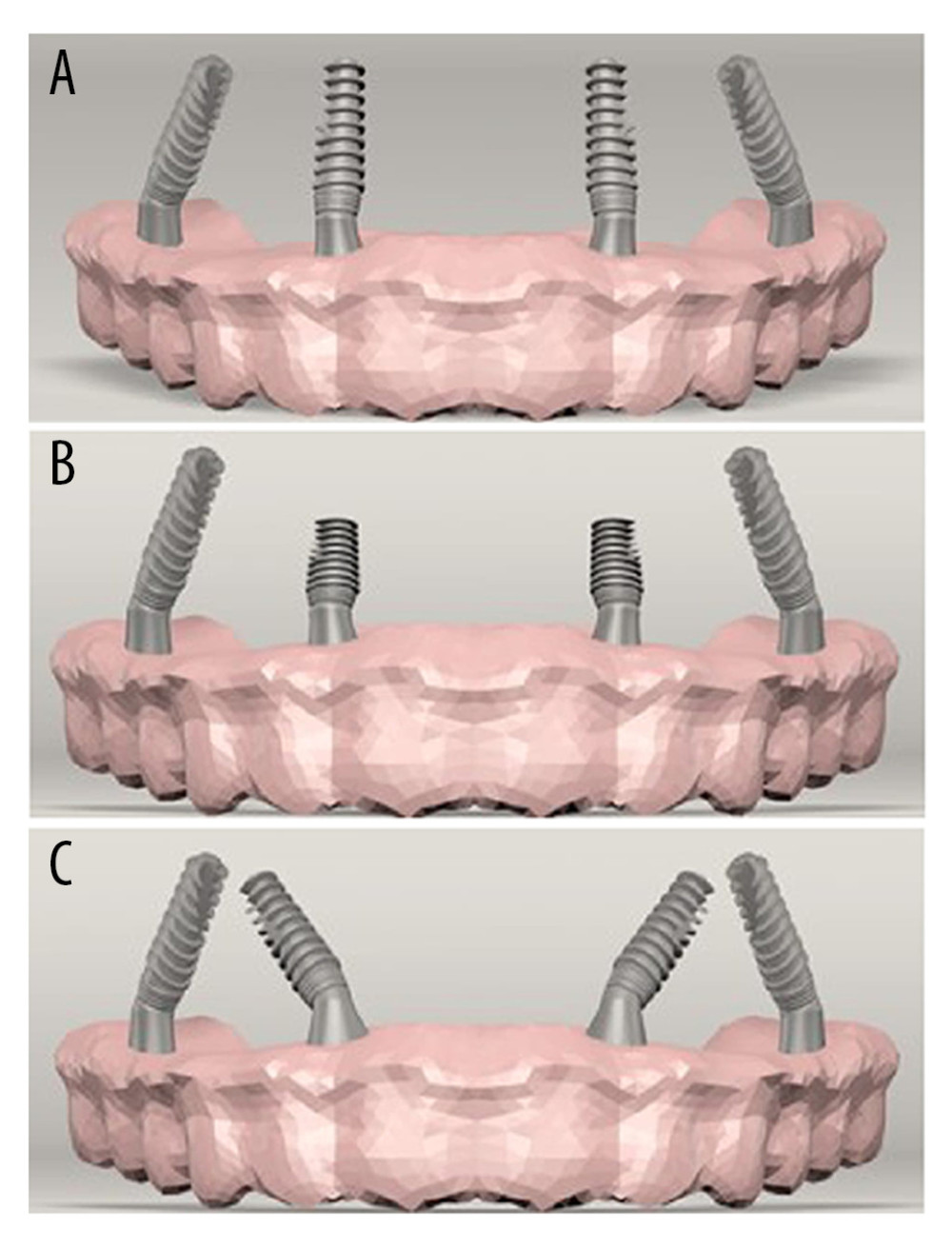 Figure 1. (A) Standard All-on-4 Model (Model 1). (B) All-on-4 Model with short implants (Model 2). (C) M-4 Model (Model 3).
Figure 1. (A) Standard All-on-4 Model (Model 1). (B) All-on-4 Model with short implants (Model 2). (C) M-4 Model (Model 3).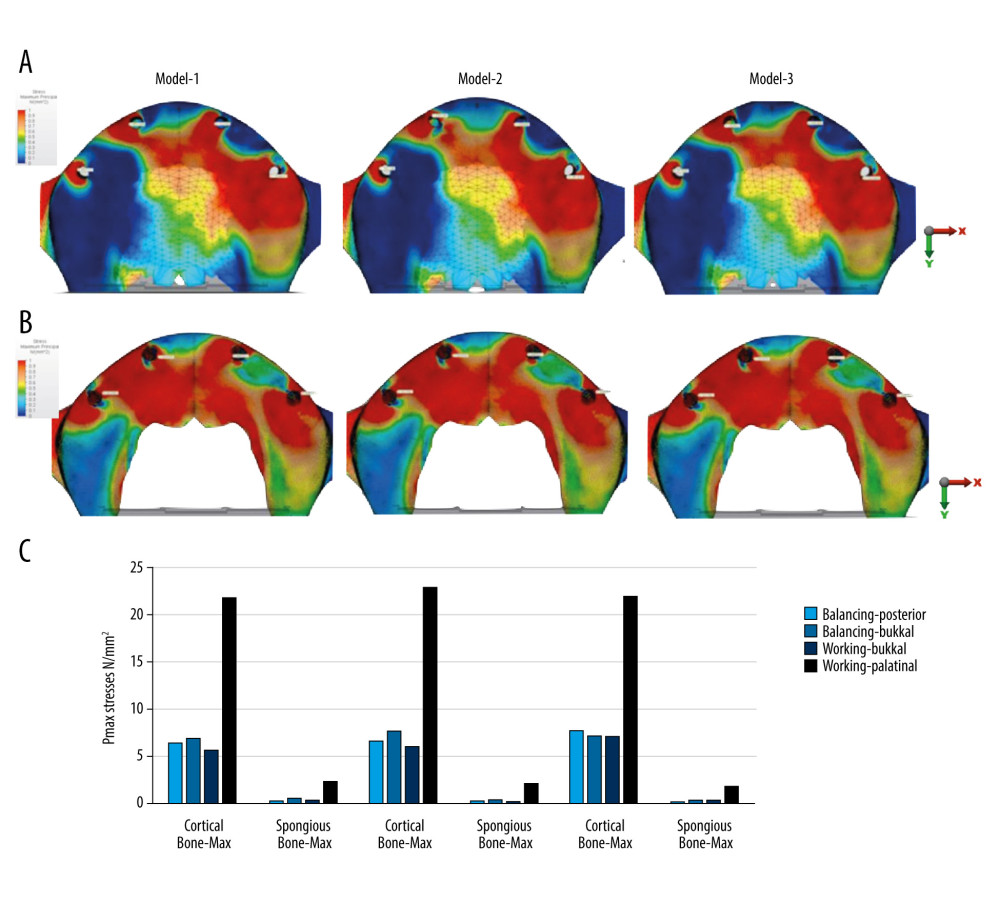 Figure 2. Pmax stresses for group function occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmax stress values (N/mm2) on cortical and spongious bone.
Figure 2. Pmax stresses for group function occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmax stress values (N/mm2) on cortical and spongious bone.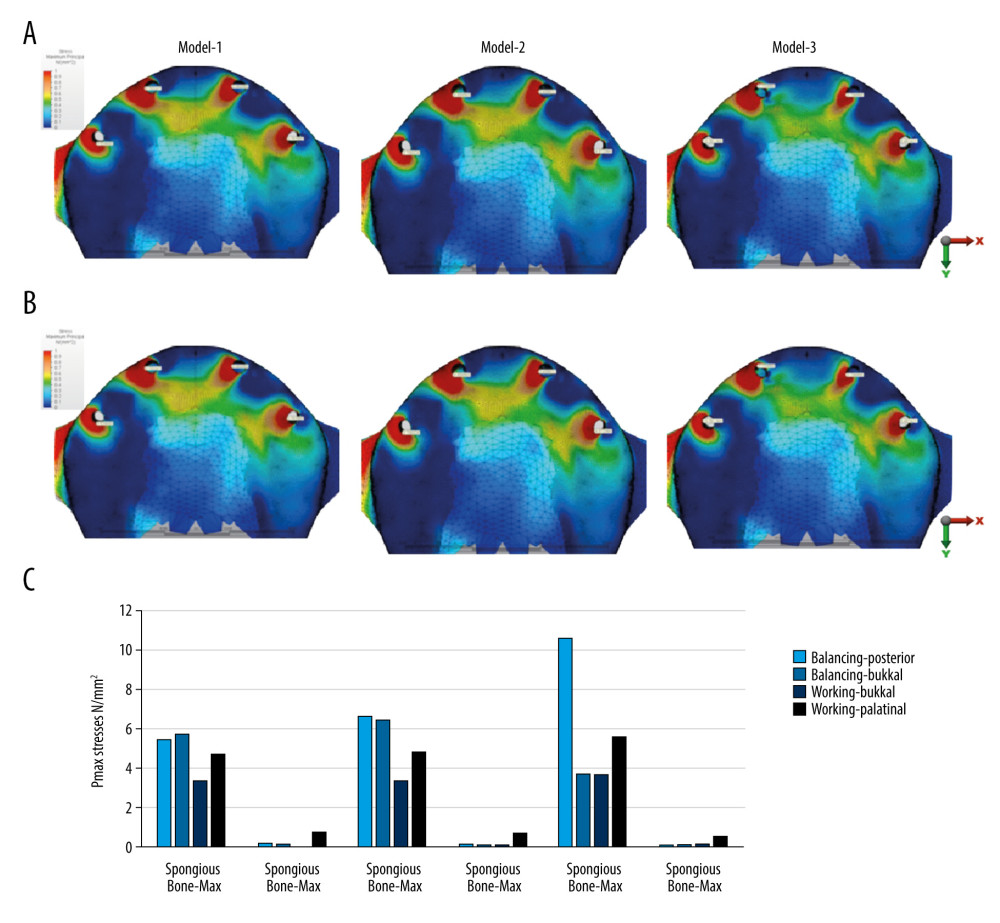 Figure 3. Pmax stresses for canine-guided occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmax stress values (N/mm2) on cortical and spongious bone.
Figure 3. Pmax stresses for canine-guided occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmax stress values (N/mm2) on cortical and spongious bone.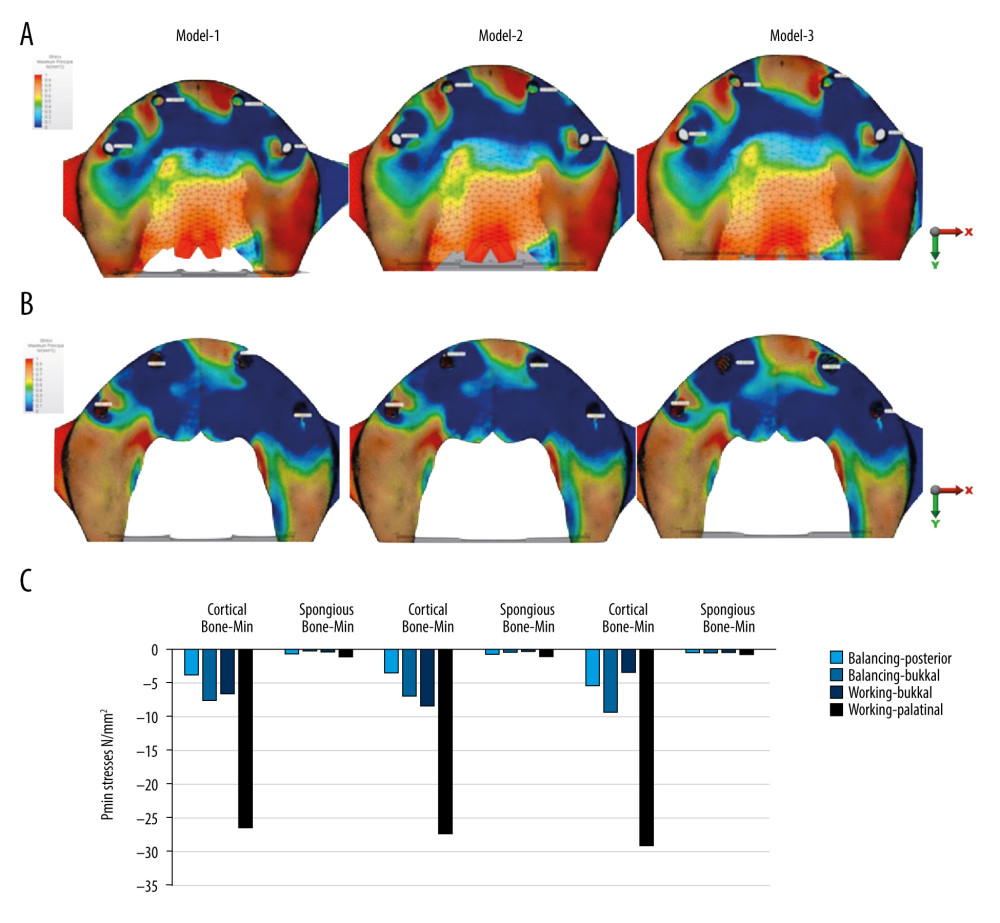 Figure 4. Pmin stresses for group function occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmin stress values (N/mm2) on cortical and spongious bone.
Figure 4. Pmin stresses for group function occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmin stress values (N/mm2) on cortical and spongious bone.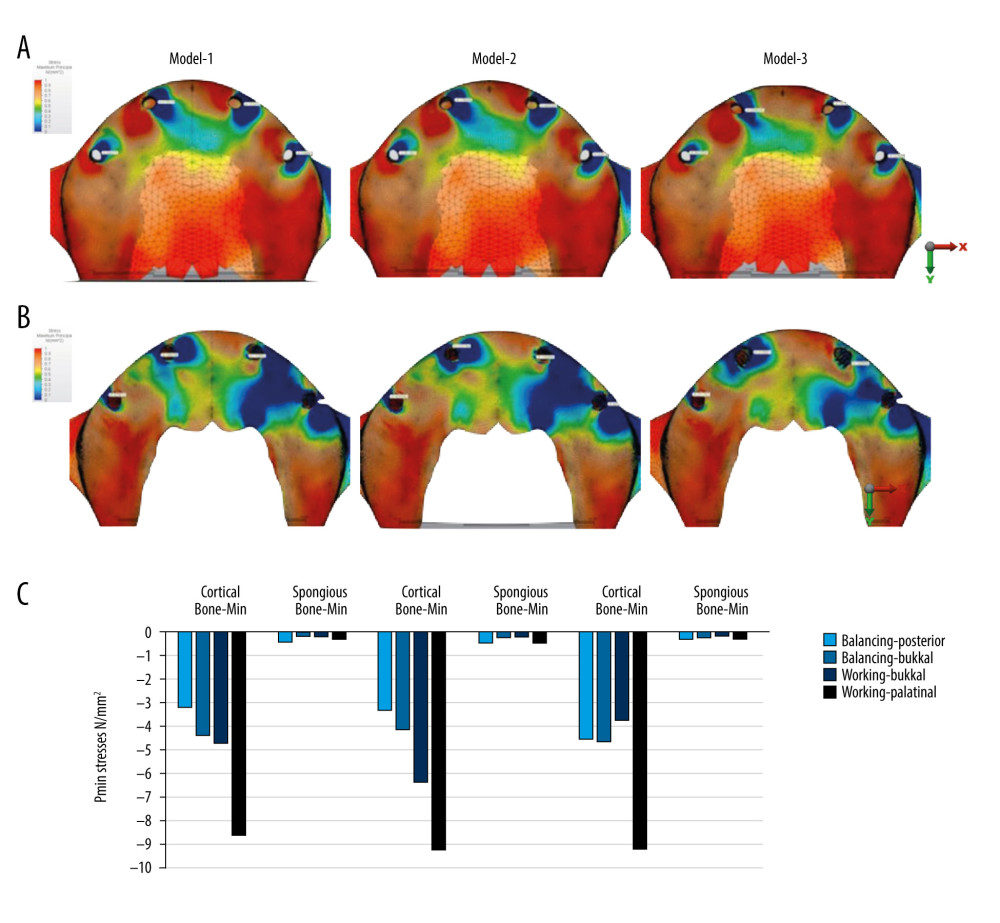 Figure 5. Pmin stresses for canine-guided occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmin stress values (N/mm2) on cortical and spongious bone.
Figure 5. Pmin stresses for canine-guided occlusion. (A) Distribution on cortical bone. (B) Distribution on spongious bone. (C) Pmin stress values (N/mm2) on cortical and spongious bone.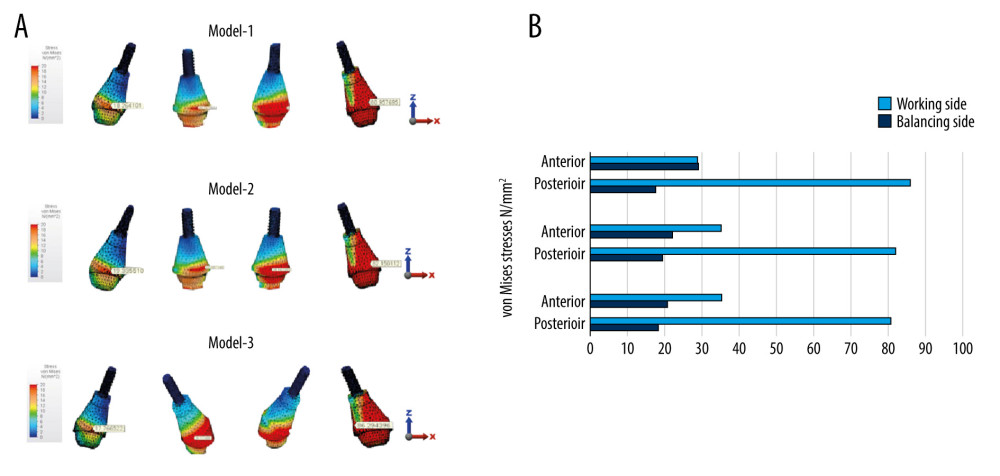 Figure 6. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on abutments for Models 1, 2, and 3 in group function occlusion.
Figure 6. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on abutments for Models 1, 2, and 3 in group function occlusion.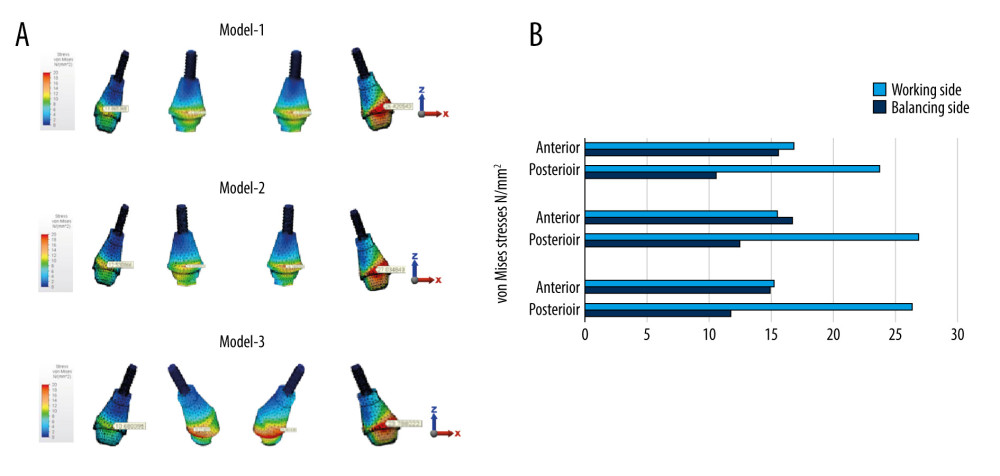 Figure 7. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on abutments for Models 1, 2, and 3 in canine-guided occlusion.
Figure 7. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on abutments for Models 1, 2, and 3 in canine-guided occlusion.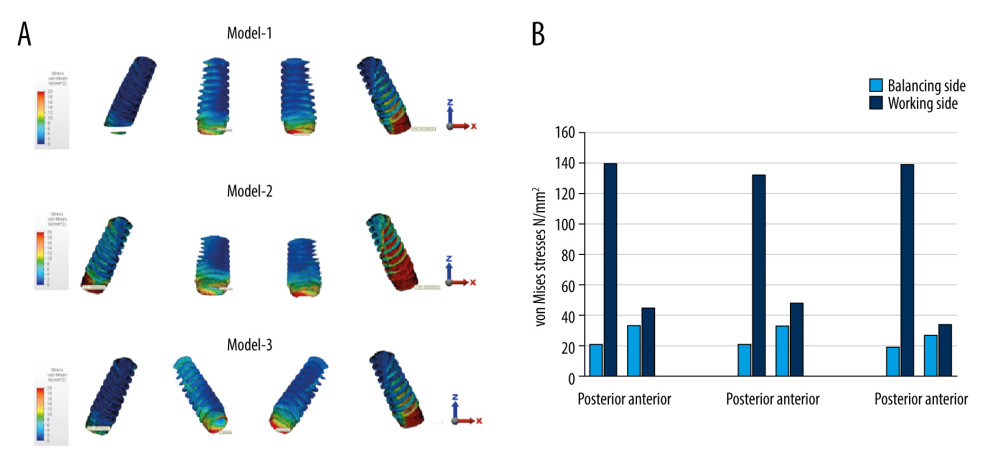 Figure 8. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on implants for Models 1, 2, and 3 in group function occlusion.
Figure 8. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on implants for Models 1, 2, and 3 in group function occlusion.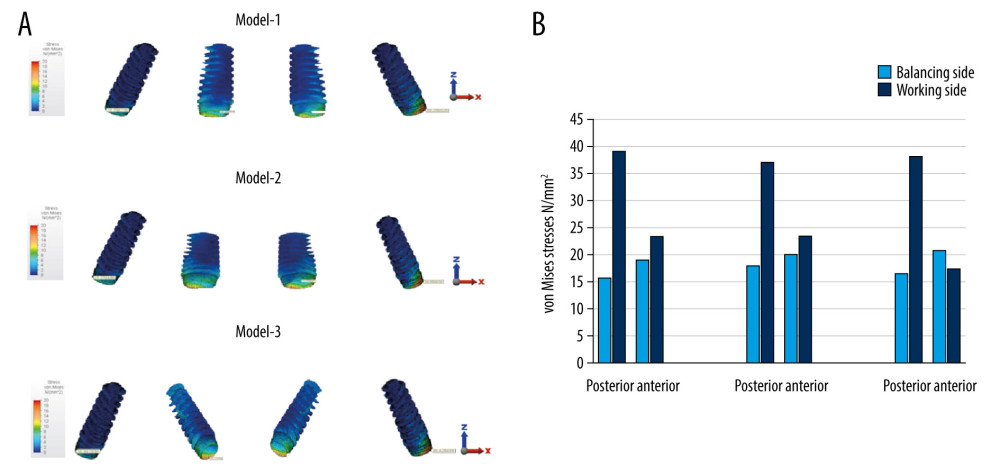 Figure 9. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on implants for Models 1, 2, and 3 in canine-guided occlusion.
Figure 9. (A) von Misses stress distributions and (B) von Mises stress values (N/mm2) on implants for Models 1, 2, and 3 in canine-guided occlusion. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








