09 September 2021: Clinical Research
Efficacy of Low-Temperature Plasma-Assisted Unilateral/Bilateral Tonsillectomy and Adenoidectomy in Children with Obstructive Sleep Apnea Hypopnea Syndrome
Yi Qiao1ABCDEFG, Jie Chen1BCDFG*DOI: 10.12659/MSM.930792
Med Sci Monit 2021; 27:e930792
Abstract
BACKGROUND: The aim of this study was to investigate the efficacy of low-temperature plasma-assisted bilateral or unilateral tonsillectomy (LTPABT or LTPAUT) and adenoidectomy in treatment of children with obstructive sleep apnea hypopnea syndrome (OSAHS).
MATERIAL AND METHODS: The present observational cohort study included a total of 244 children with OSAHS during December 2017 to December 2018. The patients were divided into the LTPABT group, the LTPAUT group, and the control group that received traditional bilateral tonsillectomy and adenoidectomy. The apnea hypopnea index (AHI) and the lowest oxygen saturation (LSaO2) were measured. The patients’ pain condition was determined using the Visual Analog Score (VAS) and intraoperative indices were collected. Patients’ quality of life was assessed by OSA-18 scale and patients’ immune function was determined.
RESULTS: The postoperative VAS scores were remarkably lower in the LTPABT and LTPAUT groups. At 6 months after surgery, the AHI significantly had decreased and LSaO2 levels were significantly enhanced for all groups, and the AHI was significantly lower and LSaO2 was markedly higher in the LTPABT group. The ratio of patients with efficacy of cured and remarkably effective was remarkably higher in the LTPABT group. The rates of postoperative hemorrhage and infection were significantly lower in the LTPABT and LTPAUT groups, and 4 cases showed tonsillar hyperplasia. OSA-18 scores were lowest in the LTPABT group. No significant difference was found in levels of IgM, IgA and IgG, and T lymphocyte subtypes.
CONCLUSIONS: The low-temperature plasma-assisted bilateral tonsillectomy combined with adenoidectomy had the best efficacy. None of the surgery methods influenced the patients’ immune function.
Keywords: Plasma, Sleep Apnea Syndromes, Adenoidectomy, Adolescent, Child, Child, Preschool, Cohort Studies, Cold Temperature, Female, Humans, Immunity, Plasma Gases, Sleep apnea, obstructive, Tonsillectomy
Background
Obstructive sleep apnea hypopnea syndrome (OSAHS), defined as repeated upper respiratory tract obstruction during sleep, can cause a series of syndromes, including snoring, apnea, and hypoventilation, as well as hypoxemia and hypercapnia [1–3]. Delayed treatment of OSAHS can lead to dysfunction of many organs, such as the endocrine system, cardiovascular system, and nervous system. It is reported that the prevalence of OSAHS is 2~4% in adults, and in children the incidence rate is 1~2% [4,5]. Adenotonsillar hypertrophy (ATH) accounts for more than 75% of OSAHS patients [6,7].
The treatment for OSAHS includes surgical and non-surgical methods, in which the non-surgical treatment mainly includes weight loss, exercise, cessation of smoking and alcohol consumption, changing sleep position, continuous positive airway pressure ventilation, oral appliances, electrical stimulation therapy, behavior therapy, and drug therapy [8–11]. Currently, surgery is still the main treatment method for OSAHS [12]. In recent decades, many surgical methods have been developed for treatment of OSAHS, such as uvulopalatopharyngoplasty, Z-shaped palatopharyngoplasty, correction of nasal septum, radiofrequency ablation of the turbinate, removal of nasal polyps, radiofrequency ablation of tongue base, Pillar implantation, repose tongue base traction, hyoid osteotomy, and tracheotomy [13–17]. For children with ATH, tonsillectomy and adenoidectomy are the most common methods for treating OSAHS [18]. It was found that tonsillectomy and adenoidectomy can significantly improve the apnea hypopnea index (AHI) in OSAHS children [19], and the long-term efficacy of tonsillectomy was also sufficient to relieve obstruction while maintaining immunological function [20].
However, up to now, there are limited clinical data on differences between low-temperature plasma-assisted bilateral and unilateral tonsillectomy (LTPABT or LTPAUT) combined with adenoidectomy, and their effects on postoperative immunological function are also unclear. In the present study, we assessed and compared the efficacy of LTPABT, LTPAUT, and traditional method combined with adenoidectomy. This research may provide more clinical evidence for low-temperature plasma-assisted bilateral or unilateral tonsillectomy in OSAHS treatment.
Material and Methods
PATIENTS:
The present observational cohort study included a total of 244 pediatric patients with OSAHS who went to our department from December 2017 to December 2018. All patients were diagnosed with OSAHS according to the draft guidelines for diagnosis and treatment of OSAHS in children by the Chinese Medical Association. The diagnostic criteria included: 1) patients with clinical syndrome of sleep apnea, mouth breathing, snoring, which can be alleviated or not after turning over, and sometimes can be accompanied by daytime sleepiness and inattention; 2) patients with bilateral tonsillar enlargement of II
SURGERY STRATEGY:
All patients were divided into 3 groups according to the surgery strategies: 1) the LTPABT group, which received LTPABT and adenoidectomy; 2) the LTPAUT group, which received LTPAUT and adenoidectomy; and 3) the control group, which received traditional bilateral tonsillectomy and adenoidectomy. The surgery strategies were selected based on the patients’ condition and parents’ willingness. For sample size calculation, the formula
For all groups, patients received routine tests, including whole-blood test, electrocardiogram, liver and kidney function, before surgery. The surgeries were performed under general anesthesia with endotracheal intubation for all groups. For severe OSAHS patients, nasal continuous positive airway pressure ventilation (CPAP) was used for 5~7 days to improve the hypoxia condition of the patients.
For the LTPABT group, after anesthesia, patients were placed in supine position. The operation area was disinfected with 75% alcohol and a normal sterile towel was used to spread the sheet. A Davis mouth-gag was put to the mouth for fixation and bilateral tonsils were exposed. The integrated plasma radiofrequency cutter head (Arthro Care Corporation, USA) was used with foot-controlled electrocoagulation to resect the tonsils from the upper pole to the lower pole along the bilateral tonsillar capsule. The electric switch was adjusted to 7~8 gears and the coagulation mode was adjusted to 3~4 gears. The resection was performed along with hemostasis. The catheter was passed out from the front nostril through the nasopharynx and suspended in the soft palate, and was fixed with hemostatic forceps. Then, the hypertrophic adenoids were ablated by cryoplasma assisted by a 70° nasal endoscopy. After the posterior nostril was entirely exposed, electrocoagulation hemostasis was performed, followed by oral secretions cleaning, bleeding check, and instrument removal. The surgical duration was measured from the start of the mucosal incision to the end of the surgery. For the LTPAUT group, the same procedure was performed but only 1 tonsil on 1 side was resected.
For the control group, the patients were also placed in supine position. The operation area was disinfected with 75% alcohol and a normal sterile towel was used to spread the sheet. After fixation by Davis mouth-gag and exposure of bilateral tonsils, an incision was made at the position of 2 mm along the palatopharyngeal arch with a sickle knife, and the tonsil capsule was separated. The tonsil capsule was stripped down and separated to the root, and was then resected using a snare. The hemostasis was performed by compression hemostasis or electrocoagulation, or suture hemostasis if necessary. Then, the index finger of the left hand was extended to the nasopharynx and the hypertrophic adenoids was scraped using a curette. After hemostasis, oral secretions were cleaned, followed by bleeding check and instrument removement.
To reduce postoperative pain, all patients received a submandibular cold compress using a soft ice bag, as well as nursing treatment including patient education, attention transfer, and eating honey.
DATA MEASUREMENT AND COLLECTION:
All patients received PSG measurement before the surgery as well as 6 months after surgery. The postoperative examination was accomplished by another physician rather than the main surgeon. The PSG measurement was conducted using a Rembrandt Embla-32 instrument (Embla-Rembrandt, Iceland) while sleeping for at least 7 h [21]. The main clinical outcomes were defined as: cured as AHI <5 and LSaO2 >90% with no syndrome, remarkably effective as AHI <20 or the reduction of AHI ≥50% and the syndrome improved, effective as the reduction of AHI ≥25% and the syndrome improved, and not effective as AHI <25% and no obvious change of syndrome.
After surgery, patients’ pain condition was determined using the Visual Analog Score (VAS) at 12 h, 24 h, and 48 h after the operation. For patients age <6 years, the VAS test was accomplished under the help of their parents. During the interview, children ≥6 years were asked if they had any pain, and children age 4~6 years were asked about this with the help of parents [22]. Patients’ intraoperative indices including surgical time and blood loss were recorded. The duration of complete shedding of tonsil leucorrhea was recorded. Patients’ quality of life was assessed by OSA-18 scale before and at 6 months after surgery [23].
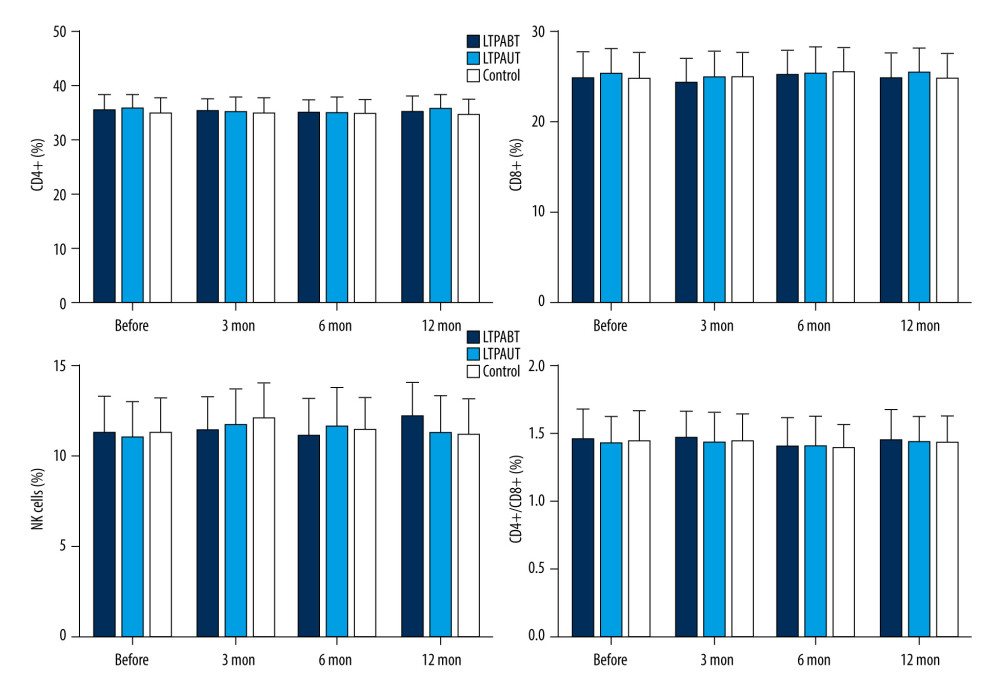
For patients’ immune function, the peripheral blood samples of all patients were collected before the surgery as well as at 3 months, 6 months, and 12 months after surgery. The levels of IgM, IgA, and IgG were measured by immunoturbidimetry using an automatic biochemical analyzer (OlympusAU4500). The T lymphocyte subsets (ratios of CD4+, CD8+, natural killer (NK) cells, and CD4+/CD8+) were measured by flow cytometry using a flow cytometer (BD FACSCanto II) [24].
Patients’ postoperative complications, including hemorrhage, wound infection, and tonsillar hyperplasia, were recorded. All patients were followed up for 12 months.
STATISTICAL ANALYSIS:
The measurement data was expressed by mean±SD. Comparison among 3 groups were performed using one-way analysis of variance (ANOVA) followed by Tukey post hoc test. The rates were compared using the chi-square test.
Results
BASIC CLINICAL CHARACTERISTICS AND INTRAOPERATIVE INDICES:
As shown in Table 1, the present study included 244 OSAHS pediatric patients (age 4~14 years) with 81 cases in the LTPABT group, 75 cases in the LTPAUT group, and 88 cases in the control group. The patients who were lost to follow-up or quit the study were already excluded. No significant difference was found in age, sex, or OSAHS severity among the 3 groups of patients. For patients’ intraoperative indices, it was found the surgical time was significantly shorter, and the blood loss was markedly less in the LTPABT and LTPAUT groups compared with the control group (P<0.05). However, no significant difference was found between the LTPABT and LTPAUT groups.
VAS SCORES AND DURATION OF COMPLETE SHEDDING OF TONSIL LEUCORRHEA:
VAS scores and duration of complete shedding of tonsil leucorrhea were compared among the groups. At 12 h, 24 h, and 48 h after surgery, the VAS scores were remarkably lower in the LTPABT and LTPAUT groups compared with the control group (P<0.05, Table 2). However, the tonsil leucorrhea shedding time showed no significant difference. No significant difference was found between the LTPABT and LTPAUT groups. These results indicated that both LTPABT and LTPAUT could reduce parents’ postoperative pain condition.
PSG RESULTS AND PROGNOSIS:
As shown in Table 3, no significant difference was found for AHI and LSaO2 levels before surgery. At 6 months after surgery, the AHI significantly decreased and LSaO2 levels significantly increased compared with levels before surgery for all groups (P<0.05). AHI was significantly lower and LSaO2 was markedly higher in the LTPABT group compared with the LTPAUT and control groups at 6 months after surgery (P<0.05). The ratio of patients with efficacy of cured and remarkably effective (50 cases 61.73%) was remarkably higher in the LTPABT group compared with the LTPAUT and control groups (27 cases 36.00% and 37 cases 42.05%) (P<0.05). No significant difference was found for patients for whom treatment was not effective (6 cases 7.41% in the LTPABT group, 7 cases 9.33% in the LTPAUT group, and 6 cases 6.82% in the control group). The rates of postoperative hemorrhage and infection were significantly lower in the LTPABT and LTPAUT groups (P<0.05). All cases of hemorrhage were posthemorrhage, and the symptom disappeared after application of routine hemostasis methods like pressure and ice treatment. All hemorrhages were mild (stage I) according to the classification of hemorrhage following tonsillectomy [25]. In the LTPAUT group, 4 cases showed tonsillar hyperplasia within 12 months after surgery along with hyperplasia of the lateral pharyngeal cord on the surgery side. No other significant difference was found between the LTPAUT and control groups.
The patients’ quality of life by OSA-18 scale showed that 6 months after surgery, all scores, including scores of sleep disorders, body syndrome, emotion, daytime function, effects on guardian, and total scores, were markedly lower compared with the levels before surgery for all groups (all P<0.05, Table 4). However, scores of sleep disorders and body syndrome, as well as total scores were significantly lower in LTPABT patients than in the other groups (P<0.05). All these results show that the LTPABT method had better efficacy and fewer complications in treatment of OSAHS patients.
IMMUNE FUNCTIONS:
Finally, we determined immune functions by measurement of levels of IgM, IgA and IgG, ratios of CD4+, CD8+, NK cells, and CD4+/CD8+ before the surgery as well as at 3 months, 6 months and 12 months after surgery. No significant difference was found in all factors before surgery in all groups. Besides, after 3 months, 6 months and 12 months, all factors also showed no significant difference in all patients (Figure 1). And also, the levels before and after surgery showed no significant difference for all patients, suggesting that the surgical methods did not influence the patients’ immune functions.
Discussion
As a disease first reported in 1976, the definition, diagnosis, and treatment for OSAHS have been gradually improved and developed for no more than 20 years [26]. Currently, surgery is still the main method for treatment of OSAHS [12]. However, clinical evidence for different surgical methods in treatment of OSAHS is still inadequate, especially for application of unilateral tonsillectomy. In the present study, we found that the low-temperature plasma-assisted bilateral tonsillectomy had better efficacy in treatment for OSAHS children than the unilateral tonsillectomy and traditional surgery, with less tonsillar hyperplasia than LTPAUT and better pain management than the control and no obvious effects on immune function.
Several studies have already reported the effects of tonsillectomy (unilateral or bilateral) with or without low-temperature plasma-assist in treatment of OSAHS. Cao et al compared the efficacy between tonsillectomy by low-temperature plasma and tonsil-pecking and found that tonsillectomy by low-temperature plasma was better for growth development and psychological behavior in OSAHS pediatric patients [27]. Dai et al demonstrated that plasma-mediated temperature-controlled radiofrequency ablation of partial tonsillectomy (internal one-third to one-half portion of the bilateral tonsils) and complete tonsillectomy showed no difference in patients’ immune function in children with OSAHS [28]. Wang et al investigated the pulmonary function in pediatric OSAHS patients and found that low-temperature plasma treatment could achieve better efficacy and lower postoperative pain than traditional methods, but did not influence the pulmonary function [29]. Inthe present study, we compared the efficacy of low-temperature plasma-assisted bilateral or unilateral tonsillectomy combined with adenoidectomy, as well as the traditional surgical and found LTPABT had better efficacy than the traditional method and LTPAUT, while all methods showed no obvious effects on children’s immune function. The difference between LTPABT and LTPAUT in AHI and LSaO2 might be due to both the severity difference and postoperative unilateral tonsillectomy. In the LTPABT group, 12.34% of cases were severe, and 20% of cases were severe in the LTPAUT group, and the difference was not significant statistically. However, the disease severity might influence the patients’ recovery. LTPAUT achieved similar efficacy as traditional methods with reduced postoperative pain. Although many parents worry about the immune function after bilateral tonsillectomy, it might not be a problem, but for unilateral tonsillectomy, tonsillar hyperplasia after surgery might be a risk. However, the high risk of tonsillar hyperplasia in unilateral tonsillectomy needs further research.
Adenoidectomy is another widely used method in treatment of OSAHS. Yang et al reported that transoral endoscopic adenoidectomy decreased the mean arterial pressure and increased the duration of nocturnal sleep of OSAHS patients [30]. In another study, Ding et al demonstrated that a combination of adenoidectomy, tonsillectomy, and soft palate-pharyngoplasty was effective to enlarge the anteroposterior diameter and transverse diameter of the isthmus faucium to achieve better efficacy in OSAHS patients [31]. In early research, Feng et al investigated the efficacy of endoscopic adenoidectomy in treatment of OSAHS patients and demonstrated that the intelligence, attention, and quality of life were significantly improved after endoscopic adenoidectomy [32]. In the present research, we used adenoidectomy in all surgical strategies, and syndrome improvement was observed in all groups of patients, showing the efficacy of adenoidectomy was good in OSAHS.
This study has some limitations. First, the study sample was small. Secondly, long-term efficacy for the surgeries is still unclear. Our results need to be confirmed by further research.
Conclusions
In conclusion, we conducted an observational cohort study to investigate effects of low-temperature plasma-assisted unilateral/bilateral tonsillectomy combined with adenoidectomy in pediatric OSAHS patients (age 4~14 years). Results showed that the low-temperature plasma-assisted bilateral tonsillectomy combined with adenoidectomy had the best efficacy. Unilateral tonsillectomy combined with adenoidectomy showed similar efficacy to the traditional method, but tonsillar hyperplasia after surgery might be a risk. None of the surgical methods influenced the patients’ immune function.
Tables
Table 1. Basic characteristics of all patients before surgery.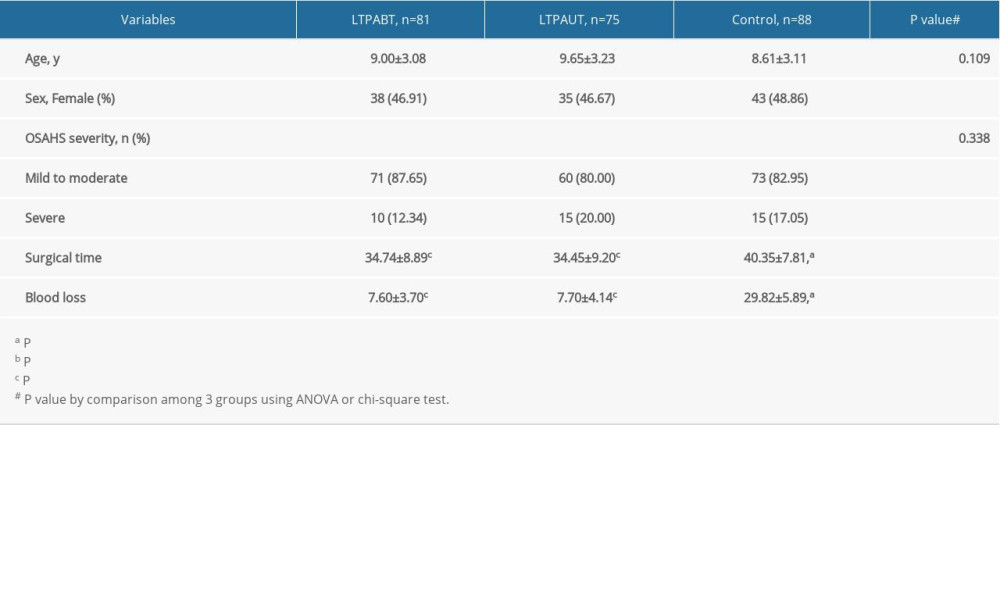 Table 2. VAS scores and duration of complete shedding of tonsil leucorrhea.
Table 2. VAS scores and duration of complete shedding of tonsil leucorrhea.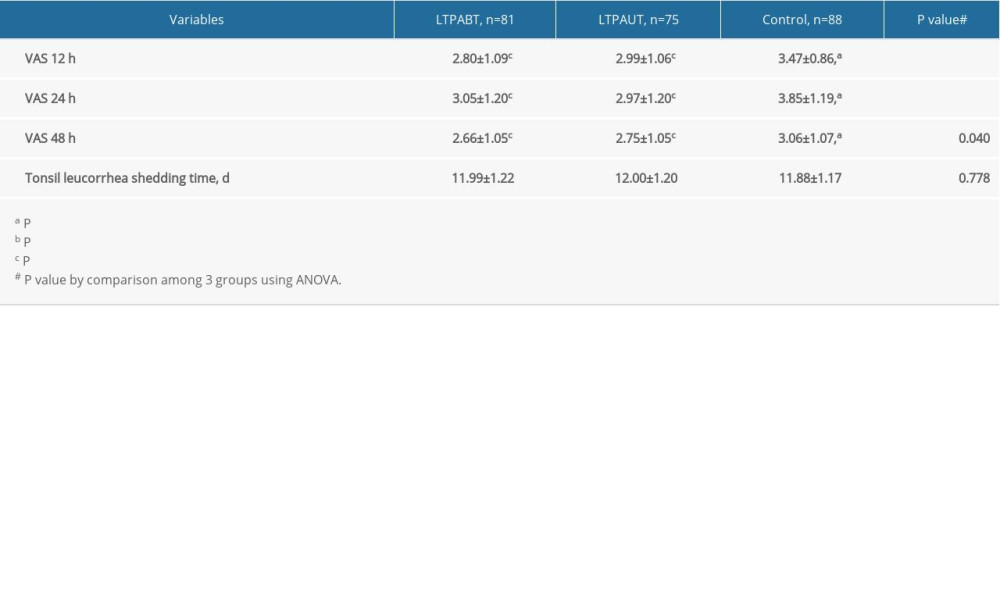 Table 3. AHI and LSaO2 levels before and 6 months after surgery, as well as treatment efficacy and complications.
Table 3. AHI and LSaO2 levels before and 6 months after surgery, as well as treatment efficacy and complications.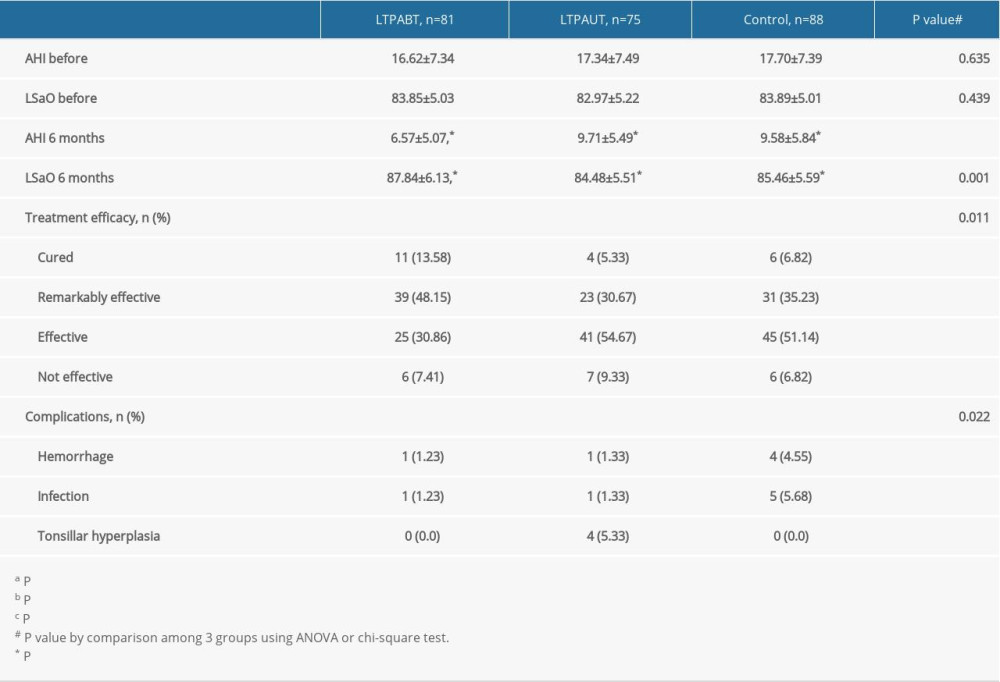 Table 4. Patients’ quality of life by OSA-18 scale before and at 6 months after surgery.
Table 4. Patients’ quality of life by OSA-18 scale before and at 6 months after surgery.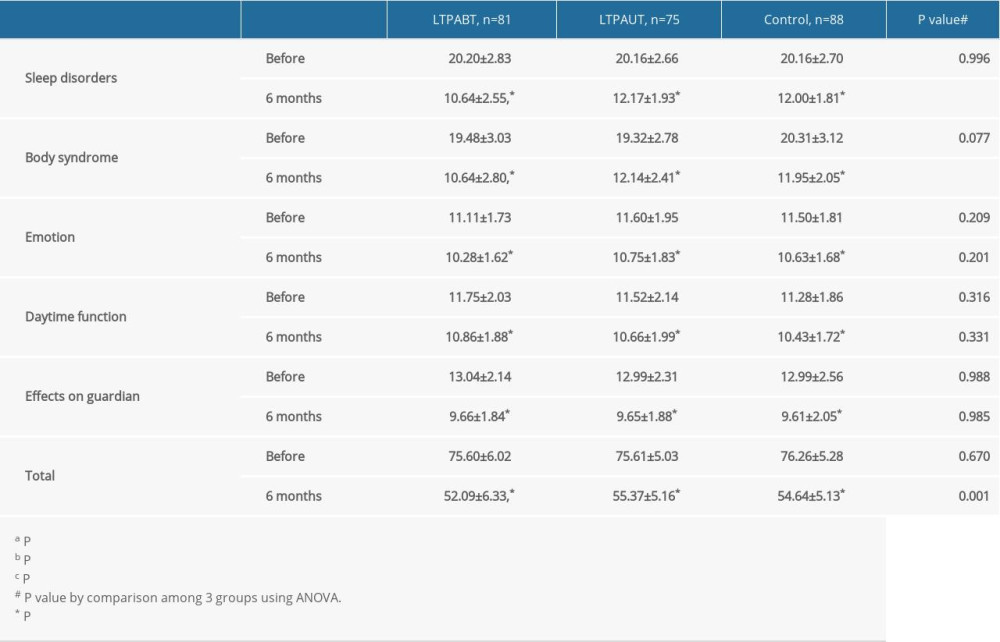
References
1. Lu D, Li N, Yao X, Zhou L, Potential inflammatory markers in obstructive sleep apnea-hypopnea syndrome: Bosn J Basic Med Sci, 2017; 17(1); 47
2. Agha B, Johal A, Facial phenotype in obstructive sleep apnea-hypopnea syndrome: A systematic review and meta-analysis: J Sleep Res, 2017; 26(2); 122-31
3. Lacedonia D, Carpagnano GE, Sabato R, Characterization of obstructive sleep apnea-hypopnea syndrome (OSA) population by means of cluster analysis: J Sleep Res, 2016; 25(6); 724-730
4. Gong X, Huang L, Liu X, Correlation analysis between polysomnography diagnostic indices and heart rate variability parameters among patients with obstructive sleep apnea hypopnea syndrome: PLoS One, 2016; 11(6); e0156628
5. Esteller E, Obstructive sleep apnea-hypopnea syndrome in children: Beyond adenotonsillar hypertrophy: Acta Otorrinolaringol (English Edition), 2015; 66(2); 111-19
6. Pateron B, Marianowski R, Monteyrol PJ, French Society of ENT (SFORL) guidelines (short version) on the roles of the various treatment options in childhood obstructive sleep apnea-hypopnea syndrome: Eur Ann Otorhinolaryngol Head Neck Dis, 2018; 135(4); 265-68
7. Kang K-T, Chou C-H, Weng W-C, Associations between adenotonsillar hypertrophy, age, and obesity in children with obstructive sleep apnea: PLoS One, 2013; 8(10); e78666
8. Abud R, Salgueiro M, Drake L, Efficacy of continuous positive airway pressure (CPAP) preventing type 2 diabetes mellitus in patients with obstructive sleep apnea hypopnea syndrome (OSAHS) and insulin resistance: A systematic review and meta-analysis: Sleep Med, 2019; 62; 14-21
9. Kielb SA, Ancoli-Israel S, Rebok GW, Spira AP, Cognition in obstructive sleep apnea-hypopnea syndrome (OSAS): Current clinical knowledge and the impact of treatment: Neuromolecular Med, 2012; 14(3); 180-93
10. Lloberes P, Durán-Cantolla J, Martínez-García MÁ, Diagnosis and treatment of sleep apnea-hypopnea syndrome: Arch Bronconeumol (English Edition), 2011; 47(3); 143-56
11. Mbata GC, Chukwuka JC, Obstructive sleep apnea hypopnea syndrome: Ann Med Health Sci Res, 2012; 2(1); 74-77
12. Peng B-G, Lai Y-Q, Lei H-J, Strategies in the clinical diagnosis and surgical treatment of OSAHS with multilevel obstruction: J Int Med Res, 2019; 47(4); 1533-43
13. Vicini C, Montevecchi F, Pang K, Combined transoral robotic tongue base surgery and palate surgery in obstructive sleep apnea-hypopnea syndrome: Expansion sphincter pharyngoplasty versus uvulopalatopharyngoplasty: Head Neck, 2014; 36(1); 77-83
14. Zhang X-M, Tham C-J, Yin Y-L, A novel palatal implant surgery combined with uvulopalatopharyngoplasty and inferior turbinate radiofrequency for the treatment of moderate to severe obstructive sleep apnea: A pilot study: Eur Arch Otorhinolaryngol, 2015; 272(5); 1195-202
15. Choi JH, Kim SN, Cho JH, Efficacy of the pillar implant in the treatment of snoring and mild-to-moderate obstructive sleep apnea: A meta-analysis: Laryngoscope, 2013; 123(1); 269-76
16. Yi HL, Sun XQ, Chen B, Z-palatopharyngoplasty plus genioglossus advancement and hyoid suspension for obstructive sleep apnea hypopnea syndrome: Otolaryngol Head Neck Surg, 2011; 144(3); 469-73
17. Lin H-C, Friedman M, Chang H-W, Yalamanchali S, Z-palatopharyngoplasty combined with endoscopic coblator open tongue base resection for severe obstructive sleep apnea/hypopnea syndrome: Otolaryngol Head Neck Surg, 2014; 150(6); 1078-85
18. Friedman M, Wilson MN, Friedman J, Intracapsular coblation tonsillectomy and adenoidectomy for the treatment of pediatric obstructive sleep apnea/hypopnea syndrome: Otolaryngol Head Neck Surg, 2009; 140(3); 358-62
19. Friedman M, Wilson M, Lin H-C, Chang H-W, Updated systematic review of tonsillectomy and adenoidectomy for treatment of pediatric obstructive sleep apnea/hypopnea syndrome: Otolaryngol Head Neck Surg, 2009; 140(6); 800-8
20. Zhang Q, Li D, Wang H, Long term outcome of tonsillar regrowth after partial tonsillectomy in children with obstructive sleep apnea: Auris Nasus Larynx, 2014; 41(3); 299-302
21. Farney RJ, Walker BS, Farney RM, The STOP-Bang equivalent model and prediction of severity of obstructive sleep apnea: Relation to polysomnographic measurements of the apnea/hypopnea index: J Clin Sleep Med, 2011; 7(5); 459-65B
22. Walther-Larsen S, Pedersen MT, Friis SM, Pain prevalence in hospitalized children: a prospective cross-sectional survey in four Danish university hospitals: Acta Anaesthesiologica Scandinavica, 2017; 61(3); 328-37
23. Wu J, Gu M, Chen S, Factors related to pediatric obstructive sleep apnea-hypopnea syndrome in children with attention deficit hyperactivity disorder in different age groups: Medicine, 2017; 96(42); e8281
24. Gao M, Liu Y, Guo M, Wang Q, Regulatory CD4+ and CD8+ T cells are negatively correlated with CD4+/CD8+ T cell ratios in patients acutely infected with SARS-CoV-2: J Leukoc Biol, 2021; 109(1); 91-97
25. Windfuhr J, Seehafer M, Classification of haemorrhage following tonsillectomy: J Laryngol Otol, 2001; 115(6); 457-61
26. Coccagna G, di Donato G, Verucchi P, Hypersomnia with periodic apneas in acquired micrognathia: A bird-like face syndrome: Arch Neurol, 1976; 33(11); 769-76
27. Cao Y-C, Wang X-Y, Xu W-W, The effects of tonsillectomy by low-temperature plasma on the growth development and psychological behavior in children with obstructive sleep apnea hypopnea syndrome: Medicine, 2018; 97(47); e13205
28. Dai ZY, Huang DY, Zhou CY, Effects of partial tonsillectomy on the immune functions of children with obstructive sleep apnea-hypopnea syndrome at early stage: Genet Mol Res, 2014; 13(2); 3895-902
29. Wang X, Liu Y, Tang G, Effects of low-temperature plasma treatment on pulmonary function in children with obstructive sleep apnea-hypopnea syndrome: Ir J Med Sci, 2020; 189(2); 603-9
30. Yang N, Ji Y, Liu Y, Effect of transoral endoscopic adenoidectomy on peripheral blood T-lymphocyte subsets in children with obstructive sleep apnea-hypopnea syndrome and its treatment strategy: Exp Ther Med, 2017; 14(4); 3022-28
31. Ding X-X, Zhao L-Q, Clinical observation of soft palate-pharyngoplasty in the treatment of obstructive sleep apnea hypopnea syndrome in children: World J Clin Cases, 2020; 8(4); 679-88
32. Feng HW, Jiang T, Zhang HP, Comparisons of thyroid hormone, intelligence, attention, and quality of life in children with obstructive sleep apnea hypopnea syndrome before and after endoscopic adenoidectomy: Biomed Res Int, 2015; 2015; 523716
Tables
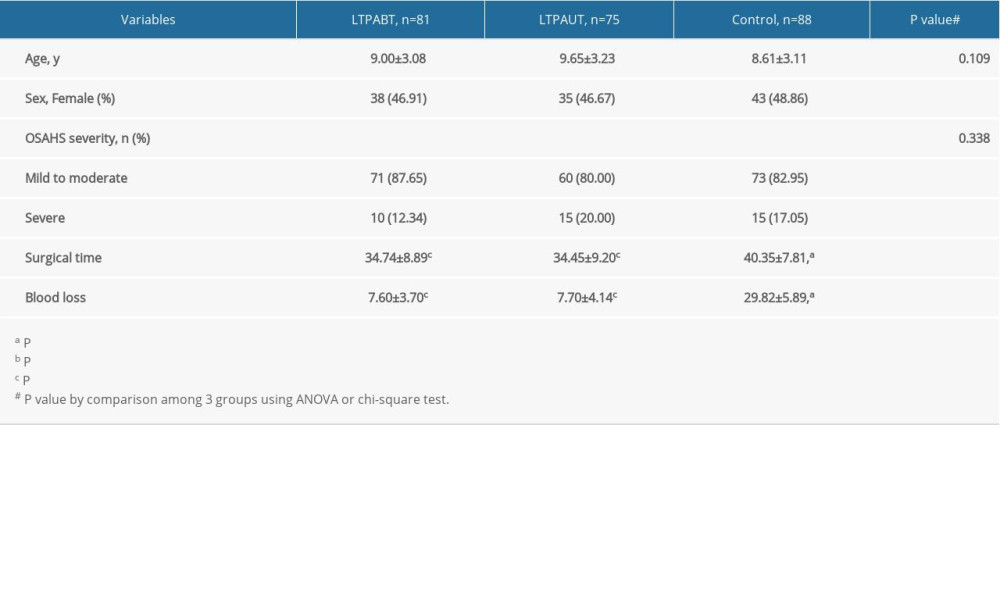 Table 1. Basic characteristics of all patients before surgery.
Table 1. Basic characteristics of all patients before surgery.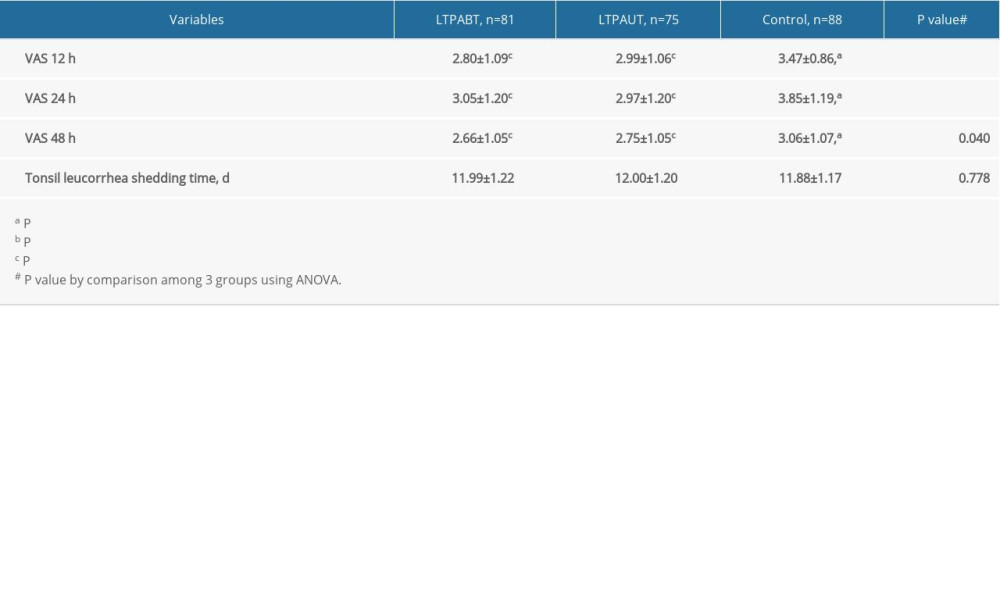 Table 2. VAS scores and duration of complete shedding of tonsil leucorrhea.
Table 2. VAS scores and duration of complete shedding of tonsil leucorrhea.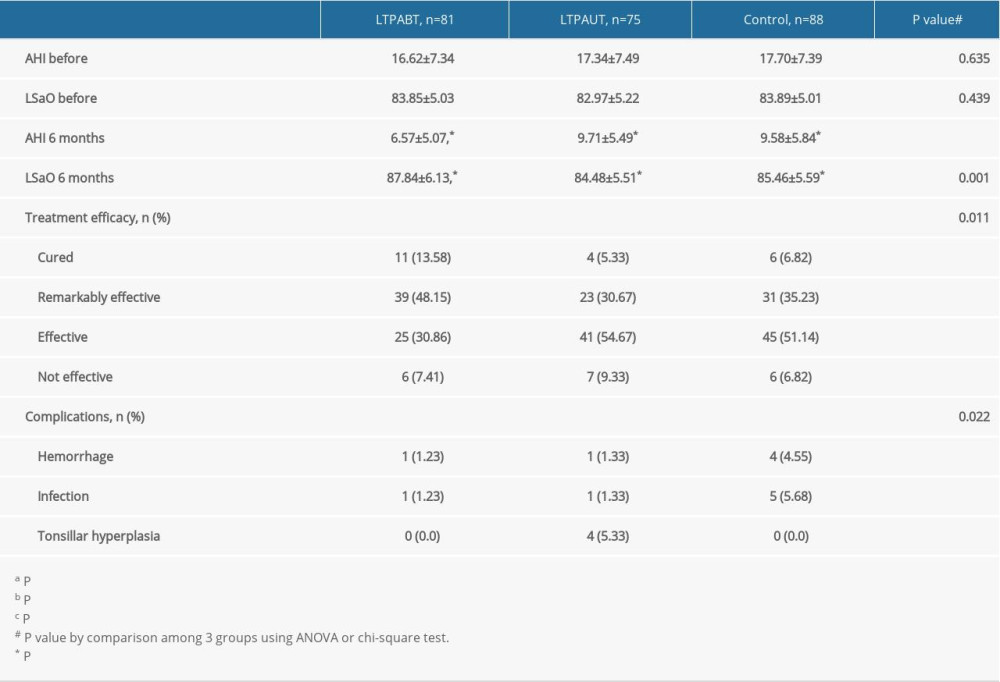 Table 3. AHI and LSaO2 levels before and 6 months after surgery, as well as treatment efficacy and complications.
Table 3. AHI and LSaO2 levels before and 6 months after surgery, as well as treatment efficacy and complications.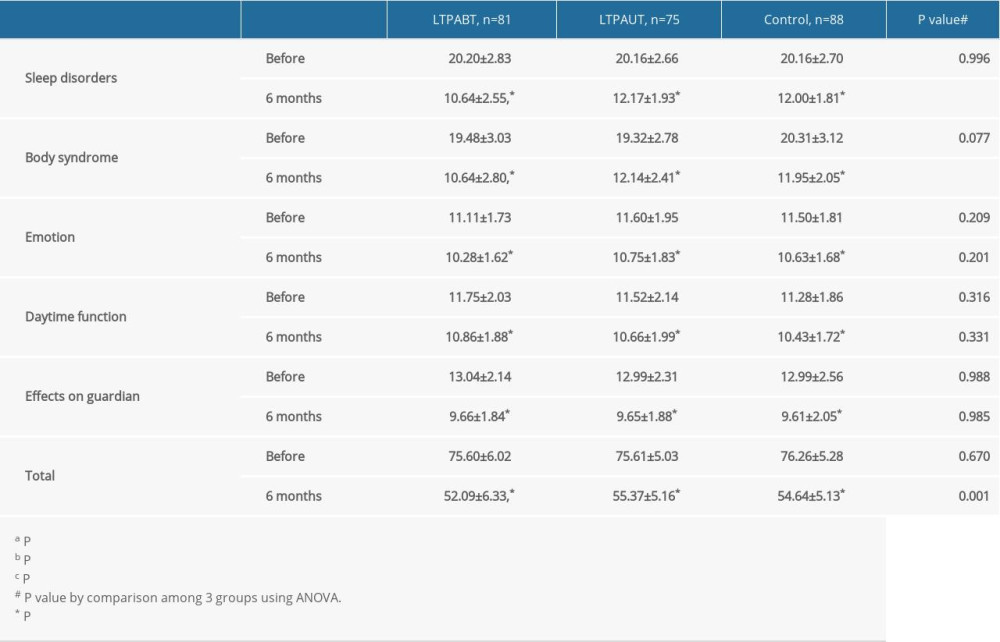 Table 4. Patients’ quality of life by OSA-18 scale before and at 6 months after surgery.
Table 4. Patients’ quality of life by OSA-18 scale before and at 6 months after surgery.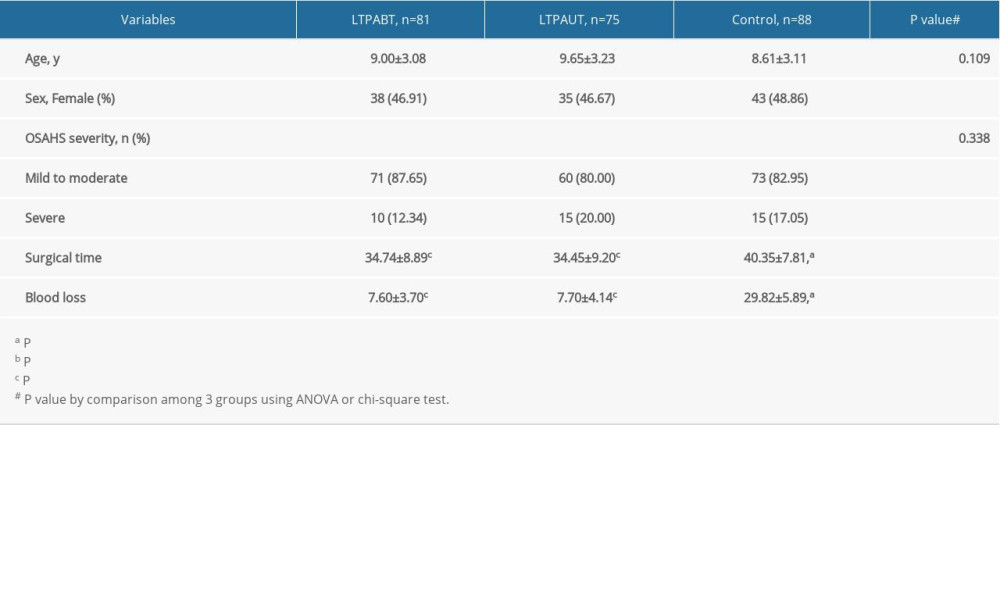 Table 1. Basic characteristics of all patients before surgery.
Table 1. Basic characteristics of all patients before surgery.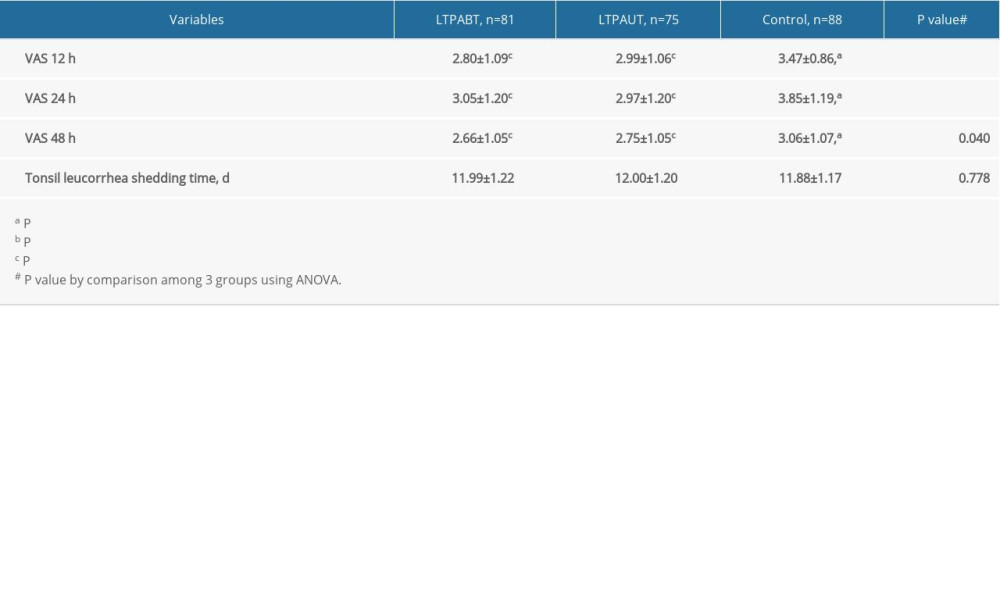 Table 2. VAS scores and duration of complete shedding of tonsil leucorrhea.
Table 2. VAS scores and duration of complete shedding of tonsil leucorrhea.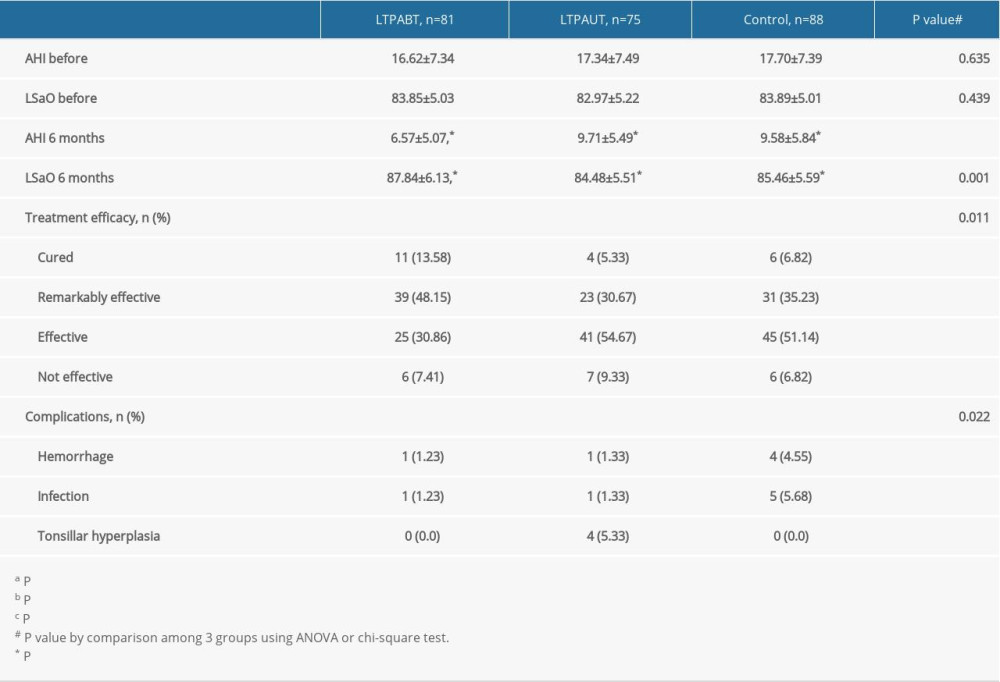 Table 3. AHI and LSaO2 levels before and 6 months after surgery, as well as treatment efficacy and complications.
Table 3. AHI and LSaO2 levels before and 6 months after surgery, as well as treatment efficacy and complications.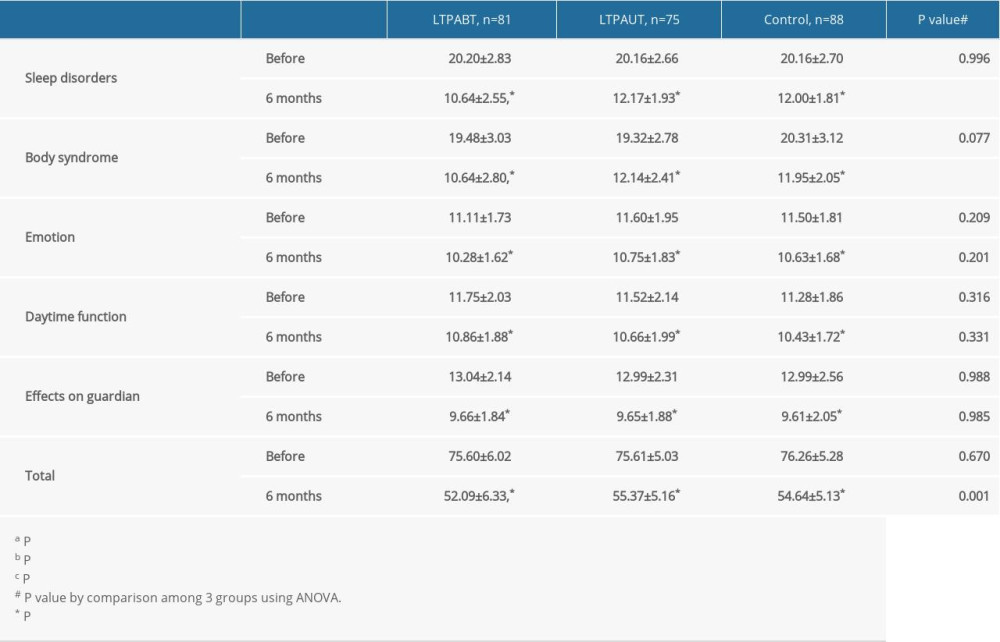 Table 4. Patients’ quality of life by OSA-18 scale before and at 6 months after surgery.
Table 4. Patients’ quality of life by OSA-18 scale before and at 6 months after surgery. In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952