17 November 2021: Clinical Research
Percutaneous Kyphoplasty for Osteoporotic Vertebral Compression Fractures Associated with Spinal Canal Encroachment without Neurological Symptoms
Yang Li1AEF, Yi Mao2BCE, Guodong Wang1BF, Jianmin Sun1DF, Zhensong Jiang1D, Zihai Ding3A, Xingang Cui1ADF*DOI: 10.12659/MSM.930848
Med Sci Monit 2021; 27:e930848
Abstract
BACKGROUND: Percutaneous kyphoplasty (PKP) has been widely used for osteoporotic vertebral compression fractures (OVCFs). However, whether this approach is suitable for osteoporotic vertebral fractures with spinal canal encroachment remains controversial.
MATERIAL AND METHODS: Of 526 patients who underwent PKP at our hospital, 40 had conditions associated with spinal canal encroachment, and were enrolled in the study. Detailed physical, neurological, and radiological examinations were performed on each patient before and after surgery and at the followup. A visual analog scale (VAS) and the Oswestry Disability Index (ODI) were used for the clinical assessment. The vertebral body height, the local kyphosis, and the spinal canal width were used for the radiological evaluation.
RESULTS: There were 11 male and 29 female patients, with a mean age of 71±8 years. The VAS score decreased from 6.4±0.7 preoperatively to 1.6±0.7 postoperatively and to 2.3±1.5 at the last followup visit. The ODI score was 78±9.5 before surgery, declined to 24±11.3 after surgery, and was 27.6±12.5 at the last followup visit. The vertebral body height increased from 11.7±4.3 mm to 14.6±4.4 mm. The local kyphosis decreased from 15.0±10.7 degrees preoperatively to 8.5±11.3 degrees postoperatively. The spinal canal width remained stable, at 8.5±2.0 mm before PKP and 8.7±1.9 after PKP.
CONCLUSIONS: PKP effectively relieved back pain in OVCF patients with spinal canal encroachment. Their social function improved as well.
Keywords: Cementoplasty, Osteoporotic Fractures, Spinal Canal, Aged, 80 and over, Female, Fractures, Compression, Humans, kyphoplasty, Male, Spinal Fractures
Background
Percutaneous kyphoplasty (PKP) has been used to treat osteoporotic vertebral compression fractures (OVCFs) since 1998 [1]. Using this technique, the doctors who originated this method restored vertebral body height and created a void that was filled with cement, using the swelling of an inflatable bone tamp. This was initially performed by a modified vertebroplasty technique. Currently, this technique is widely used for OVCF, vertebral myelomas, metastases, hemangiomas, and other conditions [2–5].
For painful fractures, PKP can prevent morbidity and save and prolong the lives of patients, and is more effective than conservative treatment [6,7]. However, due to potential neurological complications, there is still intense debate about the use of PKP for osteoporotic vertebral fractures with spinal canal encroachment [8–12]. Few reports have investigated its safety and efficacy.
The senior author initially used PKP a decade ago to treat OVCFs with spinal canal encroachment and has used the technique over the past decade. The current study retrospectively evaluated a case series to determine the safety and efficacy of PKP for patients with OVCFs with spinal canal encroachment.
Material and Methods
PATIENTS:
Between January 2008 and December 2016, 526 patients with OVCFs were enrolled at our university-affiliated hospital and underwent a percutaneous kyphoplasty. Of these 526 patients, 40 patients had associated spinal canal encroachment. All the surgeries were performed by the same surgeon at the university-affiliated hospital.
The patient demographics, including age, gender, and level of fracture, were recorded.
The inclusion criteria were as follows: 1) diagnosis of osteoporosis with a low bone-mineral density with a T value less than −2.52) severe back pain that was refractory to conservative treatment; 3) sufficient conservative treatment performed; 4) spinal canal encroachment on computed tomography (CT) and magnetic resonance imaging (MRI); and 5) no neurological deficits.
The exclusion criteria were as follows: 1) neurological deficits and symptoms; 2) no diagnosis of osteoporosis; 3) spinal tumors, metastases, or infections; and 4) followup of less than 2 years.
SURGICAL PROCEDURES:
The whole surgical procedure was performed under fluoroscopy (G-arm, Whale Inc., Beijing, China). The projection of the pedicles was marked on the skin. The needles and tubes (Kyphon, Sunnyvale, CA, USA) were inserted through the pedicle into the vertebral body. Biopsy forceps were placed into the vertebral body through the tube. Bone tissue samples were taken for pathological examination. The balloons (Kyphon, Sunnyvale, CA, USA) were inserted through the tubes and placed inside the anterior of the vertebral body from a lateral view. The balloons were expanded slowly, without overinflation. Then, polymethylmethacrylate (PMMA) acrylic cement (Dragoncrown Inc., Jinan, China) was injected into the vertebral body. The injection process was performed under continuous fluoroscopic monitoring, until the PMMA spread near the posterior wall of the vertebral body. The amount of cement and the operative time were recorded.
CLINICAL ASSESSMENT:
Every patient underwent detailed physical and neurological examinations before surgery. A visual analog scale (VAS) was used to assess each patient’s pain before surgery. The Oswestry Disability Index (ODI) was used to evaluate functional activity. After surgery, all the patients were asked to finish the VAS and ODI questionnaires. These questionnaires were also required at the followup visit.
RADIOLOGICAL EVALUATION:
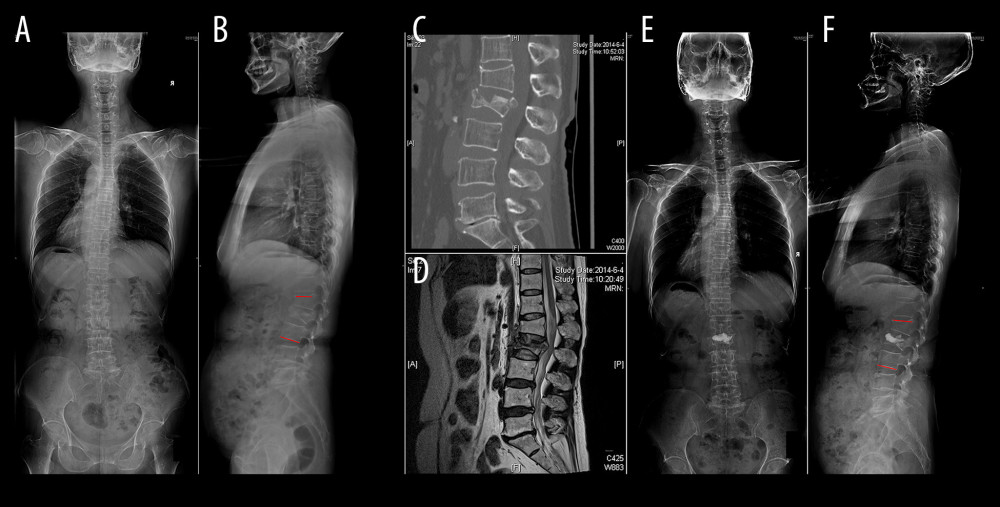
Anterior and lateral radiographs of the entire spine, as well as CT and MRI, were employed to evaluate the radiological measures before and after surgery (Figure 1). Anterior and lateral radiographs of the entire spine were also performed at the followup visit. The radiological parameters included the height of the fractured vertebral body at the anterior margin and at the mid portion, the local kyphotic angle, and the width of the spinal canal. The relative height was calculated as the fractured vertebral height divided by the average height of the cranial and caudal vertebral body. Cobb’s methods were used to measure the local kyphotic angle.
STATISTICAL ANALYSIS:
All data are presented as the mean±standard deviation. The postoperative and followup data were analyzed with the preoperative data using the Wilcoxon matched-pairs signed-ranks test, with a P value of <0.05 considered to be statistically significant. Statistical analysis was performed using SPSS software package version 21 (SPSS Inc, Chicago, IL).
Results
There were 11 male and 29 female patients. The mean age of the patients was 71±8 years (range, 50 to 84 years). The fractured vertebral body was at T11 in 1 patient, T12 in 5 patients, L1 in 21 patients, L2 in 10 patients, and L3 in 4 patients. Among these, 1 patient had 2 vertebral body fractures. According to the time of fracture, 16 cases were chronic fractures (more than 8 weeks) and 24 cases were acute fractures (less than 8 weeks). Thirteen patients had hypertension, 5 patients had a previous history of coronary heart disease, and 3 patients had a history of cerebral infarction. The mean bone mineral density (T value) was −2.98±0.42 (range, −4.05 to −2.5).
The mean operative time per vertebral body level was 29±12 min (range, 21 to 45 min). The mean amount of bone cement injected was 5.9±1.6 ml (range, 3.0 to 10.5 ml). The mean hospital stay was 2±1 days (range, 1 to 4 days). The mean followup period was 44±12 months (range, 24 to 80 months). No neurological deficits occurred after surgery.
The mean vertebral body height at the anterior margin was 15.1±3.9 mm before surgery and 18.6±3.6 mm after surgery. The mean vertebral body height at the mid portion was 11.7±4.3 mm before surgery and 14.6±4.4 mm after PKP. Compared with the preoperative vertebral body heights, the mean postoperative heights at the anterior margin and the mid portion were significantly increased (Table 1).
The mean preoperative VAS score was 6.4±0.7 (range, 4 to 8). The mean postoperative VAS score was 1.6±0.8 (range, 1 to 3) the day after PKP and was 2.3±1.5 at the last followup visit. Substantial pain relief was achieved. The mean preoperative ODI score was 78±9.5 (range, 65 to 89). The mean postoperative ODI score was 24±11.3 (range, 16 to 40), and it was 27.6±12.5 at the last followup visit. The differences between the preoperative and postoperative VAS scores and ODI assessments were statistically significant. The average VAS and ODI scores changed slightly at the final followup visit. The effect of pain relief was persistent (Table 2).
The local kyphotic angle improved significantly, from 15.0±10.7 degrees preoperatively to 8.5±11.3 degrees postoperatively (P=0.02) and 9.6±12.2 at the 2-year followup (Table 2). The spinal canal width did not change significantly. It was 8.5±2.0 mm before PKP and 8.7±1.9 mm after PKP (P=0.17). Cement leakage into the spinal canal and further dislodging of the posterior vertebral body fragments did not occur.
Discussion
PKP has been proven to be effective for treating painful osteoporotic vertebral compression fractures. However, its use is controversial in OVCF patients with spinal canal encroachment. The main issue is concern about its safety [13–15]. The injection of PMMA cement may lead to deterioration in spinal cord compression. Because of the higher rate of cement leakage in percutaneous vertebroplasty (PVP) compared with PKP, we chose to use PKP in this study. No obvious cement leakage or neurological deterioration occurred.
Through the retrospective review conducted as part of this study, the OVCF cases involving spinal canal encroachment were found to have some common characteristics. First, the vertebral compression rate was above 50%, combined with substantial local kyphosis. Second, nearly half of these cases were old fractures, and some involved Kummell’s disease. Third, the vertebral height at the mid portion was often shorter than that at the anterior margin. Finally, the posterior wall of the vertebral body was usually fractured, which might cause cement leakage into the spinal canal during PKP.
The best surgical approach for vertebral fractures with spinal canal encroachment may be to reduce the stress and then achieve fusion. The first goal is to reduce the stress. However, in OVCF patients, if there are no obvious neurological symptoms, the first goal is to reduce the pain.
Elderly patients often have comorbidities associated with other organs, such as coronary heart disease or cerebral infarction. Their bone mineral density is usually very low, which does not allow good pedicle screw purchase. Thus, PKP may be a more viable option for those patients.
In this study, all the OVCF patients with spinal canal encroachment underwent PKP surgery. All the patients achieved good pain relief and improved social function. The radiological results were quite good. The height of the compressed vertebral body was reconstructed, and the local kyphosis was corrected. The spinal canal width remained stable. There was no PMMA cement leakage into the spinal canal.
Several research studies have found that PKP could achieve significant vertebral height recovery and kyphosis angle reduction, leading to significant pain relief and functional improvement [16–18]. Wang et al [16] treated 35 patients who suffered OVCF with spinal canal compromise by PKP and achieved good clinical results. Dai et al [19] and Zhang et al [20] described improvement of injured vertebral body height and kyphosis in patients who underwent PKP that was significantly better than that in patients who underwent PVP, with no significant loss of height and kyphosis correction at the final followup visit. However, Wang et al [21] followed 203 patients for 12.7 months and found that recollapse following PKP affected 38.9% of the vertebrae, a condition that increases the risk for back pain. Similar results have been reported by Li et al [22]. Thus, the clinical efficacy of PKP is still controversial, and further studies are needed to clarify it.
During hospitalization, there are several points that need to be noted. First, preoperative evaluation of cardiopulmonary function is particularly important. Several days before surgery, we recommend that the patient lie prostrate in the ward to adapt to the long time spent in a prone position during surgery. Second, the patient’s position should be carefully prepared for surgery. A lordotic position can be helpful for reconstructing the vertebral body height and correcting the local kyphosis. Local anesthesia is more appropriate than general anesthesia or epidural anesthesia for OVCF patients with spinal cord compression. It is essential to observe the sensitivity and activity of the lower limbs. For patients who are more sensitive to pain, small doses of analgesia and sedatives can be given, but anesthetics should not be given intravenously. The key to the surgery is the location of the puncture. The puncture needles and tubes should avoid the unstable fracture fragments. The balloons are inserted through the tubes and placed inside the anterior portion of the vertebral body from a lateral view. The balloons should be expanded slowly, without overinflation. A previous study has shown that low-viscosity PKP is better than high-viscosity PVP for restoring the height of the middle vertebrae [23]. Therefore, we use low-viscosity PMMA cement and inject it slowly until it spreads near the posterior wall of the vertebral body. During the injection, continuous fluoroscopy should be used, and attention should be paid to the sensitivity and activity of the patient’s lower limbs. Finally, postoperative anti-osteoporotic treatment is essential for reducing the risk of refracture.
Conclusions
PKP is an effective, minimally invasive procedure for the treatment of osteoporotic vertebral compression fractures associated with spinal canal encroachment without neurological symptoms that leads to significant relief of symptoms and improvement in functional status.
References
1. Garfin SR, Yuan HA, Reiley MA, New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures: Spine (Phila Pa 1976), 2001; 26(14); 1511-15
2. Lieberman IH, Dudeney S, Reinhardt MK, Bell G, Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures: Spine (Phila Pa 1976), 2001; 26(14); 1631-38
3. Wang E, Yi H, Wang M, Huang C, Treatment of osteoporotic vertebral compression fractures with percutaneous kyphoplasty: A report of 196 cases: Eur J Orthop Surg Traumatol, 2013; 23(Suppl 1); S71-75
4. Chen F, Xia YH, Cao WZ, Percutaneous kyphoplasty for the treatment of spinal metastases: Oncol Lett, 2016; 11(3); 1799-806
5. Masala S, Cesaroni A, Sergiacomi G, Percutaneous kyphoplasty: New treatment for painful vertebral body fractures: In Vivo, 2004; 18(2); 149-53
6. Filippiadis DK, Marcia S, Masala S, Percutaneous vertebroplasty and kyphoplasty: Current status, new developments and old controversies: Cardiovasc Intervent Radiol, 2017; 40(12); 1815-23
7. Mao Y, Zheng Y, Li Y, Factors associated with perioperative serum calcium levels in percutaneous kyphoplasty for osteoporotic vertebral compression fracture: A prospective clinical study: Med Sci Monit, 2019; 25; 1800-5
8. Coumans JV, Reinhardt MK, Lieberman IH, Kyphoplasty for vertebral compression fractures: 1-year clinical outcomes from a prospective study: J Neurosurg, 2003; 99(1 Suppl); 44-50
9. Uchida K, Nakajima H, Yayama T, Vertebroplasty-augmented short-segment posterior fixation of osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine: Comparisons with posterior surgery without vertebroplasty and anterior surgery: J Neurosurg Spine, 2010; 13(5); 612-21
10. Ataka H, Tanno T, Yamazaki M, Posterior instrumented fusion without neural decompression for incomplete neurological deficits following vertebral collapse in the osteoporotic thoracolumbar spine: Eur Spine J, 2009; 18(1); 69-76
11. Chen GD, Zhang ZG, Yang HL, Nonunion of osteoporotic vertebral compression fracture with a severe spinal stenosis treated in minimally invasive manner: A case report: Osteoporos Int, 2015; 26(3); 1225-29
12. Chen GD, Lu Q, Wang GL, Percutaneous kyphoplasty for Kümmell disease with severe spinal canal stenosis: Pain Physician, 2015; 18(6); E1021-28
13. Garfin SR, Yuan HA, Reiley MA, New technologies in spine: Kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures: Spine (Phila Pa 1976), 2001; 26(14); 1511-15
14. Ren H, Shen Y, Zhang YZ, Correlative factor analysis on the complications resulting from cement leakage after percutaneous kyphoplasty in the treatment of osteoporotic vertebral compression fracture: J Spinal Disord Tech, 2010; 23(7); e9-e15
15. Matsuura M, Fujimoto Y, Yamada K, Nakamae T, Percutaneous vertebroplasty versus balloon kyphoplasty for osteoporotic vertebral fracture with intravertebral cleft: Spine J, 2014; 14(11); S123
16. Wang H, Zhang Z, Liu Y, Jiang W, Percutaneous kyphoplasty for the treatment of very severe osteoporotic vertebral compression fractures with spinal canal compromise: J Orthop Surg Res, 2018; 13(1); 13
17. Wang B, Zhao CP, Song LX, Zhu L, Balloon kyphoplasty versus percutaneous vertebroplasty for osteoporotic vertebral compression fracture: A meta-analysis and systematic review: J Orthop Surg Res, 2018; 13(1); 264
18. Yimin Y, Zhiwei R, Wei M, Jha R, Current status of percutaneous vertebroplasty and percutaneous kyphoplasty – a review: Med Sci Monit, 2013; 19; 826-36
19. Dai SQ, Qin RQ, Shi X, Yang HL, Percutaneous vertebroplasty versus kyphoplasty for the treatment of neurologically intact osteoporotic Kümmell’s disease: BMC Surg, 2021; 21(1); 65
20. Zhang GQ, Gao YZ, Chen SL, Comparison of percutaneous vertebroplasty and percutaneous kyphoplasty for the management of Kümmell’s disease: A retrospective study: Indian J Orthop, 2015; 49(6); 577-82
21. Wang C, Zhang X, Liu J, Percutaneous kyphoplasty: Risk factors for recollapse of cemented vertebrae: World Neurosurg, 2019; 130; e307-15
22. Li YX, Guo DQ, Zhang SC, Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP): Int Orthop, 2018; 42(9); 2131-39
23. Sun K, Liu Y, Peng H, A comparative study of high-viscosity cement percutaneous vertebroplasty vs. low-viscosity cement percutaneous kyphoplasty for treatment of osteoporotic vertebral compression fractures: J Huazhong Univ Sci Technolog Med Sci, 2016; 36(3); 389-94
Tables
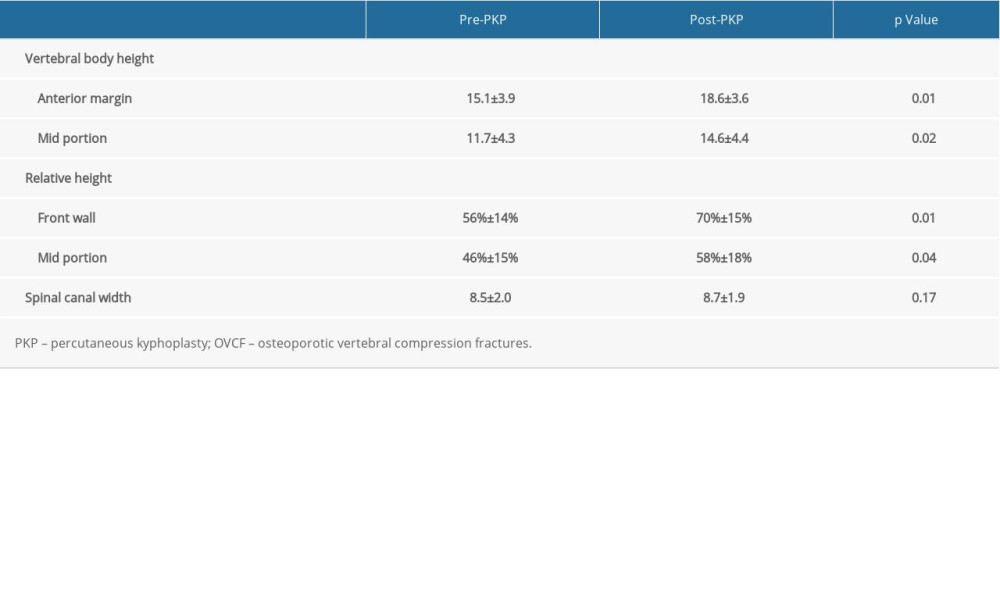 Table 1. Clinical assessment and radiological evaluation before and after the PKP on OVCF patients with spinal encroachment.
Table 1. Clinical assessment and radiological evaluation before and after the PKP on OVCF patients with spinal encroachment.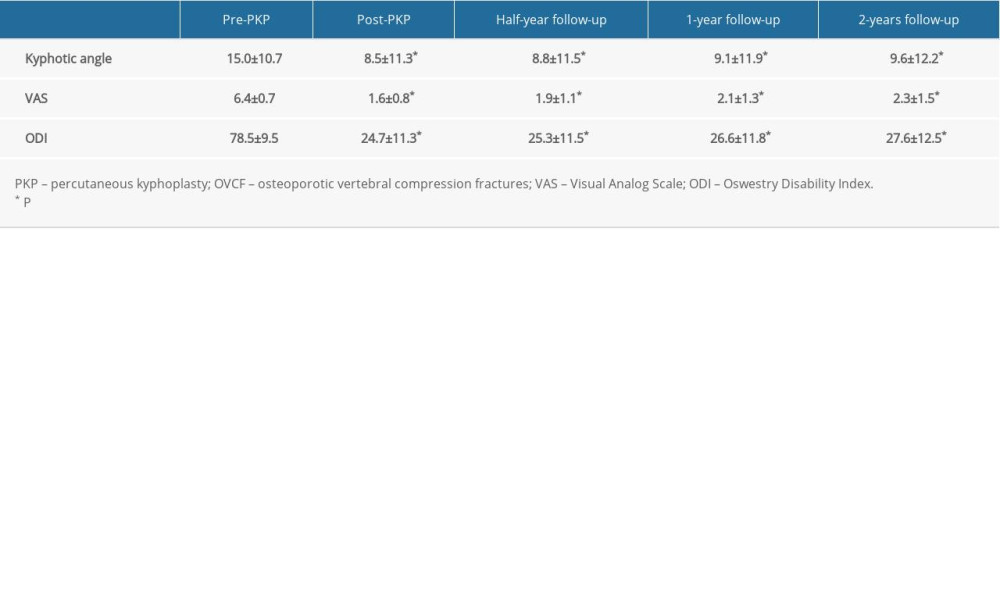 Table 2. Kyphotic angle and clinical assessment before and after the PKP, and the follow-ups on OVCF patients with spinal encroachment.
Table 2. Kyphotic angle and clinical assessment before and after the PKP, and the follow-ups on OVCF patients with spinal encroachment.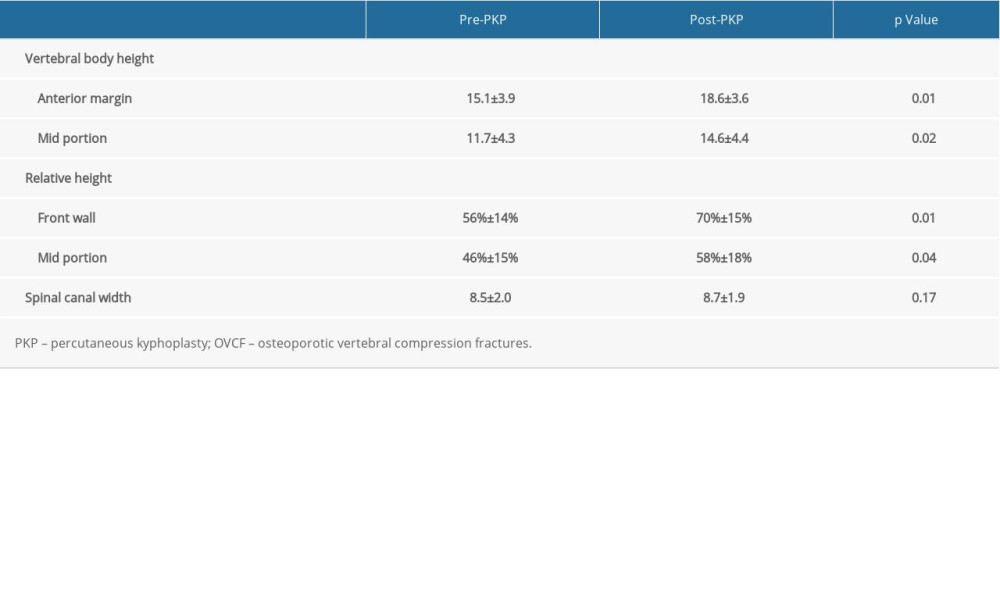 Table 1. Clinical assessment and radiological evaluation before and after the PKP on OVCF patients with spinal encroachment.
Table 1. Clinical assessment and radiological evaluation before and after the PKP on OVCF patients with spinal encroachment.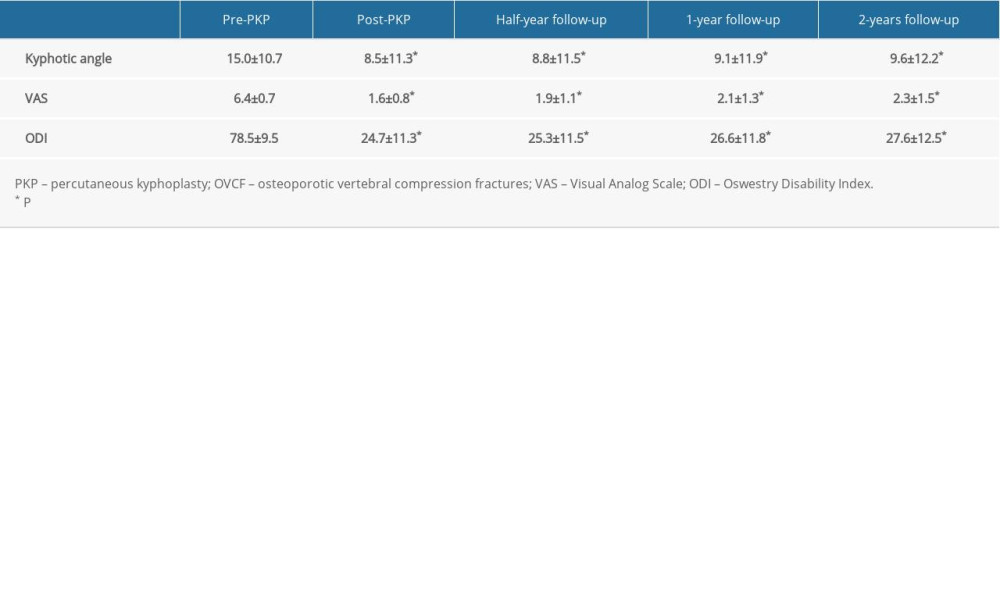 Table 2. Kyphotic angle and clinical assessment before and after the PKP, and the follow-ups on OVCF patients with spinal encroachment.
Table 2. Kyphotic angle and clinical assessment before and after the PKP, and the follow-ups on OVCF patients with spinal encroachment. In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952