28 May 2021: Clinical Research
Assessment of Lower Limb Load Distribution in Patients Treated with the Ilizarov Method for Tibial Nonunion
Łukasz Pawik1ABCDEFG, Andżelika Pajchert-Kozłowska2ABCDEF, Łukasz Szelerski3BCDE, Sławomir Żarek3BCDE, Radosław Górski3BCDE, Malwina Pawik4BCDE, Felicja Fink-Lwow4BCDE, Piotr Morasiewicz25ABCDEF*DOI: 10.12659/MSM.930849
Med Sci Monit 2021; 27:e930849
Abstract
BACKGROUND: Successful treatment of tibial nonunion should lead to a complete bone union, lack of pain, and pathological mobility of the lower extremity, as well as to the achievement of satisfactory joint mobility and muscle strength, which in turn improves its biomechanics. The objective of this study was to assess the load placed on the lower limbs in patients subjected to treatment with the Ilizarov method due to aseptic tibial nonunion.
MATERIAL AND METHODS: This research involved 24 participants (average age, 55 years). All were diagnosed with aseptic tibia nonunion and treated with the Ilizarov external fixator between 2000 and 2017. The control group was matched to the treated group in terms of sex and age. This study used pedobarography evaluation to assess lower limb load distribution.
RESULTS: No differences were found in the distribution of the load over the entire foot or of the forefoot and hindfoot of the treated limb in comparison to the non-dominant limb of the controls, or in the healthy limb of the treated group compared to the dominant limb of the control group. Similarly, differences in load distribution between the operated and healthy limbs of the treated group were insignificant.
CONCLUSIONS: Patients subjected to treatment with the Ilizarov external fixator for aseptic tibial nonunion show symmetrical load distribution on both lower limbs following treatment, which does not differentiate them in this respect from healthy individuals. Treated patients presented with a symmetrical distribution of the load on the lower extremities over the entire foot surface, including the forefoot and hindfoot. Finally, the Ilizarov external fixator enables restoration of correct static biomechanics of the treated limbs over the period of aseptic tibial nonunion therapy.
Keywords: Ilizarov Technique, Tibia, Weight-Bearing, Biomechanical Phenomena, External Fixators, Fractures, Ununited, Lower Extremity, muscle strength, Outcome Assessment, Health Care, Postoperative Complications, Radiography, Reproducibility of Results, Tibial Fractures
Background
Problems with bone union or lack of union are common complications following fractures of the tibia [1–7]. One of these complications is tibial nonunion, for which the Ilizarov fixator is a widely accepted treatment method [2–28]. Surgical techniques and clinical and radiological results of this treatment have been described in numerous publications [2–28].
Delayed union or nonunion after a fracture manifests in many adverse symptoms, including pain. Such complications can lead to pathological mobility of the affected limb, limited joint movement, weakness and edema of the muscles, and in turn, worsen its functioning [2–33]. These symptoms impair the biomechanics of the limb in the case of nonunion. A good treatment outcome is characterized by the achievement of the bone union, elimination of pain and pathological limb mobility, improvement in joint mobility, and restoration of muscle strength, which in turn improve the biomechanics of the limbs [33–45].
To our knowledge, no evidence has been published regarding lower limb statics following tibial nonunion treatment using nails, plates or external fixators. Earlier work analyzed pedobarographic foot loading distribution in patients with unilateral ankylosis of the talonavicular joint, after osteotomy and after ankle arthrodesis [33–36,38].
Examinations with a pedobarographic platform deliver reproducible and objective information on the biomechanics of the lower limbs [33–38,45].
We propose 2 hypotheses: (1) patients treated with the Ilizarov method for aseptic tibial nonunion would place equal and symmetric load on both lower limbs, and (2) patients subjected to treatment with the Ilizarov external fixator due to aseptic tibial nonunion would display similar lower limb loading to healthy people.
The aim of this study was to assess the load placed on the lower limbs by patients treated with the Ilizarov method for aseptic tibial nonunion.
Material and Methods
STATISTICAL ANALYSIS:
Data were statistically analyzed using the SigmaPlot v13 (Systat Software Inc., San Jose, CA, USA) statistics package. The Kolmogorov-Smirnov test was used to check for normality of distribution. For comparisons of variables, the unpaired
Results
We did not observe significant differences between the treated group and control group in terms of age, body weight, height, or BMI (Table 1). None of the patients during the follow-up reported knee or ankle stiffness. Five patients developed pin track infection, which resolved after administration of oral antibiotics. In 4 patients, during treatment, limitation of the ankle joint movement appeared, which disappeared after rehabilitation.
Table 2 depicts the measurements of load distribution over the entire foot and of the forefoot and hindfoot of participants from both groups. The load distribution was not significantly different over the entire foot or of the forefoot and hindfoot of the operated limb of the treated group compared to the non-dominant limb of the control group, or in the healthy, not operated, limb of the patient group compared to the dominant limb of the control group (Table 2).
Measurements comparing the load distribution in the operated and healthy limbs of the patients and the load distribution in the non-dominant and dominant limbs of the control group are shown in Table 3 and Figure 5. Results obtained with eyes closed and open for the load distribution over the entire foot and of the forefoot and hindfoot were assessed. There were no significant differences in load distribution between the operated and healthy (not operated) limbs of participants in the treated group (Table 3, Figure 5). In the control group, a significantly different load distribution of the entire foot between the non-dominant and dominant limbs was observed for open and closed eyes (Table 3, Figure 5).
Discussion
Fractures of the tibia often result in complications in the form of bone union disorders and nonunions [1–7]. The Ilizarov method is recognized as one of the best methods for treating joint nonunion [2–28], but it does not guarantee a complete recovery [12,13,16,20,21,24].
Studies from the literature reported various aspects of tibial nonunion treatment using the Ilizarov external fixator, including the surgical techniques, complications, clinical outcomes, and radiological results [2–28]. However, these studies did not focus on a very important outcome of treatment; namely, the biomechanics of the lower limbs. McHale and colleagues evaluated complicated cases, including 10 patients with tibial nonunions with debridement, antibiotic beads, and the Ilizarov method with a circular external fixator used for infected nonunions [43]. The authors tested dynamic parameters and observed impaired lower limb function due to limitations in ankle and knee joint movement and associated reductions in muscular strength in 6 persons. In the present study, we described the static parameters of the lower limb but not the dynamic ones. Our work is a part of the entire cycle of assessing the effectiveness of the Ilizarov method for biomechanics as well as statics and dynamics of patients’ gait. In another paper submitted for review, we evaluated dynamic tests depicting ground reaction forces and gait parameters.
Restoration of correct biomechanical parameters is an important element in the treatment of various limb diseases [33–42,45]. Improvements in muscle strength, proprioception, joint mobility, pain, and swelling translated into an improvement in the limb functioning, enhancing the biomechanics of limbs, and, at the same time, quality of life of individuals subjected to complicated therapy. The effectiveness of the Ilizarov external fixator in treating tibial nonunion has been explored by many authors [33–42,45].
The pedobarographic platform used in our study allows for reproducible, objective evaluation of the dynamics and statics of the musculoskeletal system [33–38,45], enabling a comparison of previously published results with the outcomes of the present study.
Lorkowski and colleagues analyzed pedobarographic foot loading distribution in patients with unilateral ankylosis of the talonavicular joint. An improvement in load distribution was observed following orthopedic treatment, along with a reduction in pain [38].
A previous study by Morasiewicz and colleagues assessed the load distribution on the lower extremities in individuals after osteotomy [35,36] and ankle arthrodesis [33,34] using the Ilizarov fixators. In all cases, symmetrical loading of both lower limbs distribution was found following treatment [33–36]. After lower limb osteotomy using the Ilizarov external fixators, patients were found to place a similar load on their lower extremities to healthy people [36].
To date, no studies have assessed the load distribution on the lower limbs following the treatment of aseptic tibial nonunion. Ling and colleagues performed a systematic literature review on the results of ankle arthrodesis treatment [44]. Based on information from 24 manuscripts (18 clinical studies, 5 biomechanical studies, and 1 gait analysis study), the majority of biomechanical studies showed altered biomechanics in the fused ankle. Several studies that assessed biomechanics following ankle arthrodesis found a load distribution disorder, but there is no real consensus in the literature regarding the effect of ankle arthrodesis on biomechanics [44]. For this reason, a symmetric load distribution between the dominant and non-dominant limb can be assumed.
In our study, we performed trials with eyes open and eyes closed. Restricting the use of vision was intended to force patients to additionally activate receptors located in joints and muscles, thus using somatosensory and vestibular senses to balance. When testing with eyes closed, in many cases, we can see significantly better results of loading symmetry due to improvement of postural control elicited by enhancing proprioceptive and vestibular sensations. This is especially observable in people recovering from strokes or returning after prolonged immobilization [46,47]. In the present study, differences between the sample with eyes open and closed were not observed.
In this study, patients showed symmetrical lower limb load distribution on the non-operated and operated limbs following the Ilizarov treatment of aseptic tibial nonunion. These results were better than those observed in the control group, in which we found significant differences in load distribution between the dominant and non-dominant limbs. Moreover, in the treated group, we recorded a symmetrical load distribution of the forefoot and hindfoot in both the healthy and operated limbs.
Comparing the lower limbs load distribution posed on the operated limb in the patient group to the non-dominant limb in the healthy (control) group, no significant differences were observed. Also, the load on the healthy limb in the patients subjected to the surgery and the load on the dominant limb in the healthy controls did not show a significant difference. When the load distributions of the forefoot and hindfoot were assessed, no significant differences were found between the operated limb and the non-dominant limb of the control group. In addition, the load distribution of the forefoot and hindfoot did not differ between the healthy (non-operated) limb of the treated group and the dominant limb of the controls.
This study has some limitations. First, lower limb load was not assessed before surgery due to the small size of the study groups that could be examined before and after the treatment. Second, patients with nonunion had difficulties with the movement of the limb before treatment, which prevented pedobarographic examination. Finally, in this study, only static parameters were assessed, but the inclusion of the dynamic data is essential for evaluating the effectiveness of the applied therapeutic method and would have made the conclusions stronger and more clinically relevant. A strength of our work was the comparative assessment with a healthy group of volunteers matched for sex and age.
Conclusions
In summary, patients treated with the Ilizarov fixators for tibial aseptic nonunion show symmetrical load distribution on both lower limbs following treatment, which does not differentiate them in this respect from healthy individuals. In the patient group, we observed a symmetrical distribution of lower limb load over the entire foot surface, as well as for the forefoot and hindfoot. Finally, in the treatment of tibial nonunion, the Ilizarov method enables the restoration of correct static biomechanics of the lower limbs.
Figures
 Figure 1. Radiological findings of nonunion – hypertrophic (A Patient before treatment, B Patient during the treatment process, C Patient after treatment).
Figure 1. Radiological findings of nonunion – hypertrophic (A Patient before treatment, B Patient during the treatment process, C Patient after treatment). 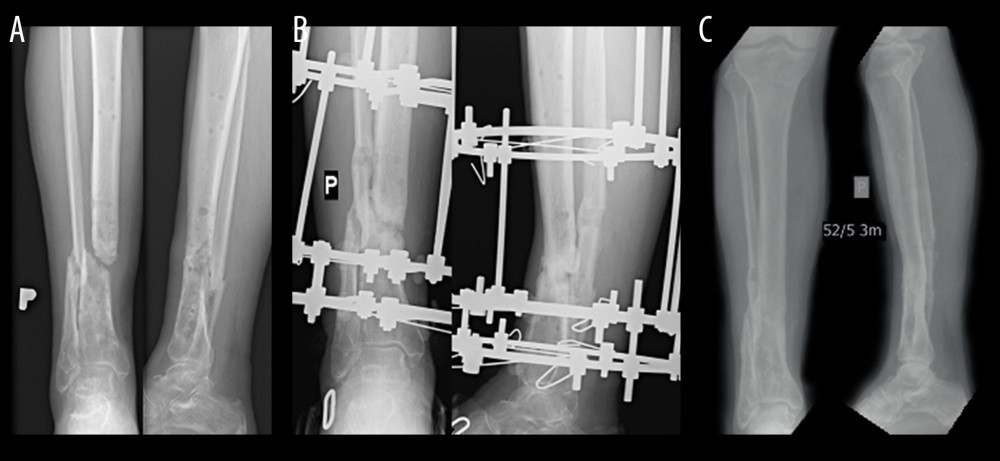 Figure 2. Radiological findings of nonunion – atrophic (A Patient before treatment, B Patient during the treatment process, C Patient after treatment).
Figure 2. Radiological findings of nonunion – atrophic (A Patient before treatment, B Patient during the treatment process, C Patient after treatment).  Figure 3. Subject during measurements on the pedobarographic platform manufactured by Zebris Medical GmbH.
Figure 3. Subject during measurements on the pedobarographic platform manufactured by Zebris Medical GmbH. 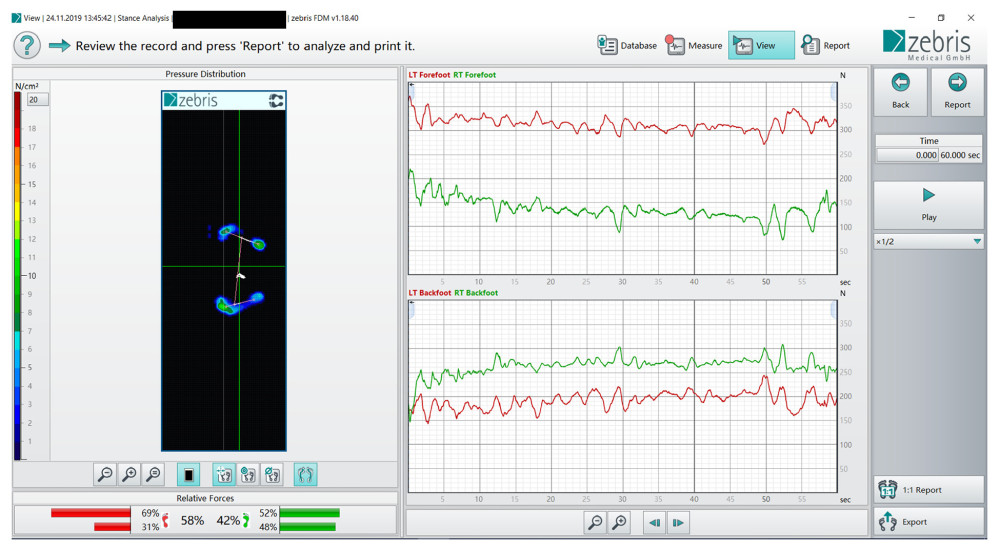 Figure 4. Distribution of load on the operated and healthy limb.
Figure 4. Distribution of load on the operated and healthy limb. 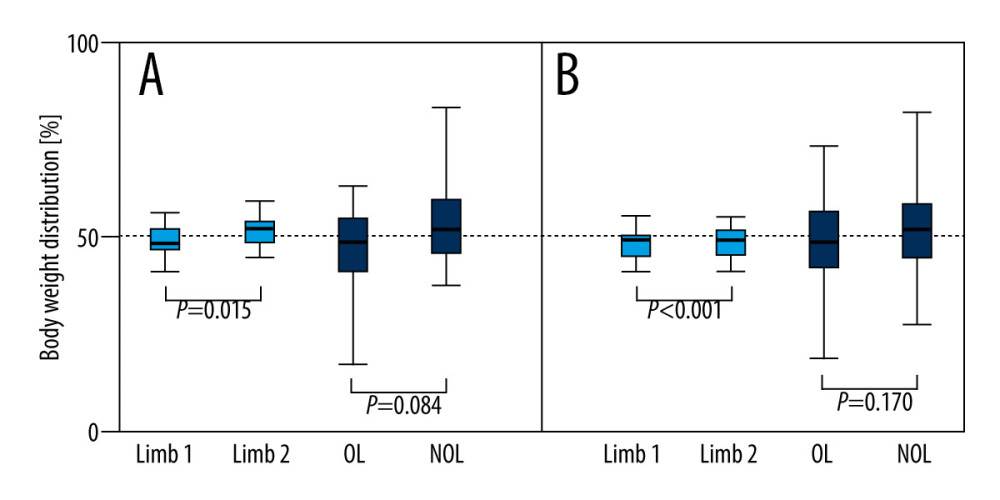 Figure 5. Body weight distribution for patients after treatment with the Ilizarov method between OL and NOL vs healthy people. The test was performed for 60 seconds with participants’ eyes open (A) or closed (B). The boundary of the box closest to zero indicates the 25th percentile, a line within the box marks the median, and the boundary of the box farthest from zero indicates the 75th percentile. Whiskers (error bars) above and below the box indicate the 90th and 10th percentiles. White boxes, healthy people; filled boxes, patients. OL – operated limb; NOL – non-operated limb.
Figure 5. Body weight distribution for patients after treatment with the Ilizarov method between OL and NOL vs healthy people. The test was performed for 60 seconds with participants’ eyes open (A) or closed (B). The boundary of the box closest to zero indicates the 25th percentile, a line within the box marks the median, and the boundary of the box farthest from zero indicates the 75th percentile. Whiskers (error bars) above and below the box indicate the 90th and 10th percentiles. White boxes, healthy people; filled boxes, patients. OL – operated limb; NOL – non-operated limb. Tables
Table 1. Characteristics of the participants.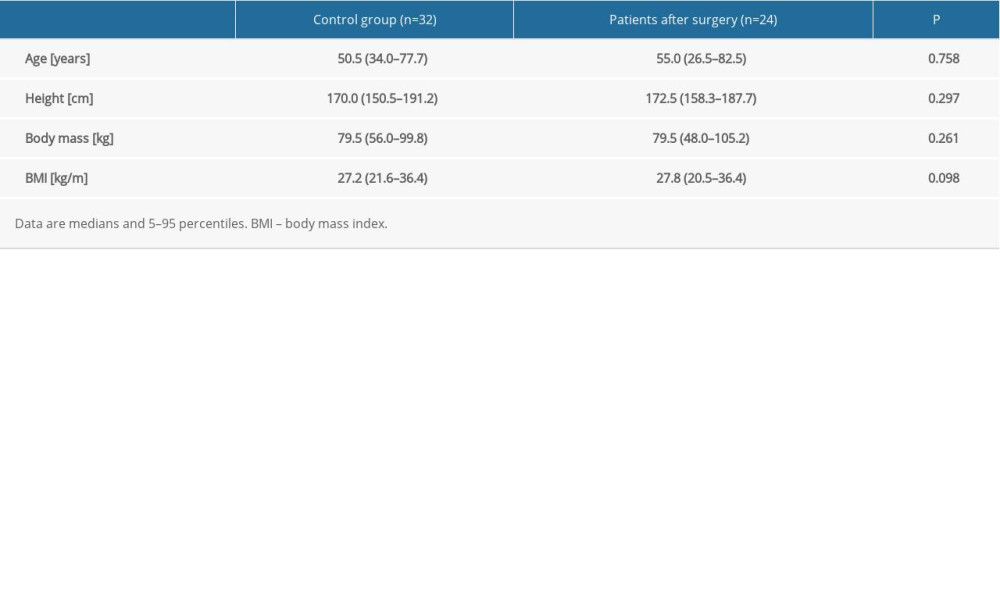 Table 2. Body weight distribution for patients after treatment with the Ilizarov method compared to the control group of healthy people.
Table 2. Body weight distribution for patients after treatment with the Ilizarov method compared to the control group of healthy people.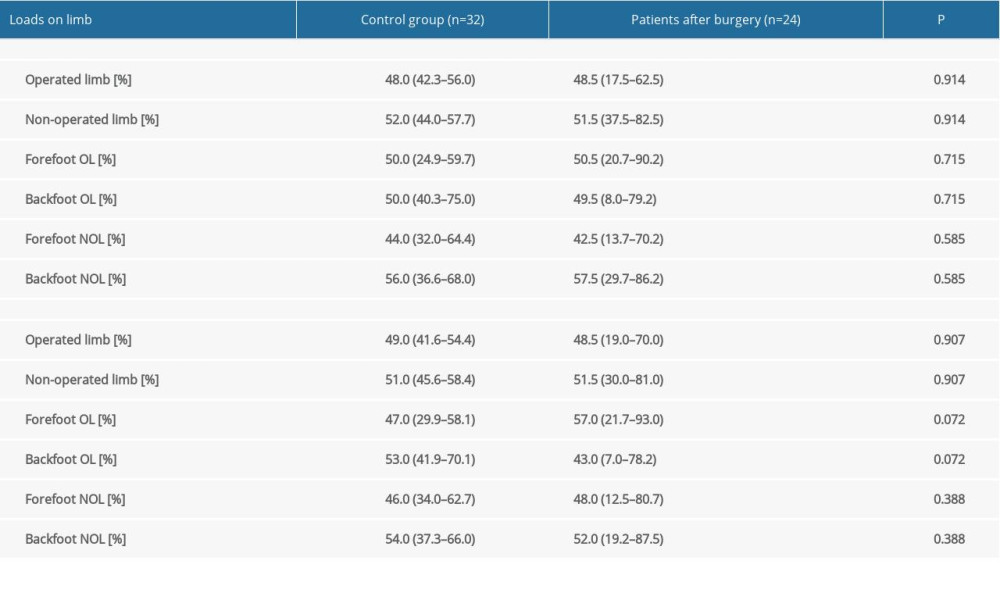 Table 3. Body weight distribution for patients after treatment with the Ilizarov method between OL and NOL vs healthy people.
Table 3. Body weight distribution for patients after treatment with the Ilizarov method between OL and NOL vs healthy people.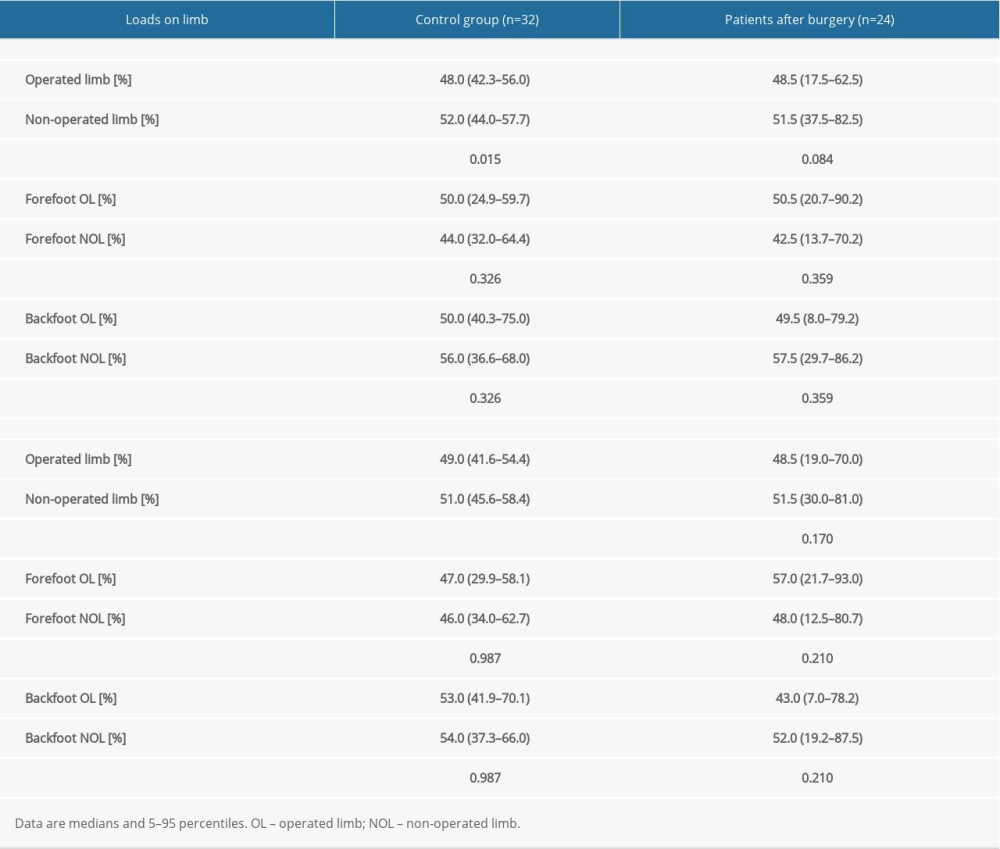
References
1. Zura R, Xiong Z, Einhorn T, Epidemiology of fracture nonunion in 18 human bones: JAMA Surg, 2016; 151; e162775
2. Yin P, Ji Q, Li T, A systematic review and meta-analysis of Ilizarov methods in the treatment of infected nonunion of tibia and femur: PLoS One, 2015; 10; e0141973
3. Peng J, Min L, Xiang Z, Ilizarov bone transport combined with antibiotic cement spacer for infected tibial nonunion: Int J Clin Exp Med, 2015; 8; 10058-65
4. Schoenleber SJ, Hutson JJ, Treatment of hypertrophic distal tibia nonunion and early malunion with callus distraction: Foot Ankle Int, 2015; 36; 400-7
5. Zhang H, Xue F, Jun Xiao H, Ilizarov method in combination with autologous mesenchymal stem cells from iliac crest shows improved outcome in tibial non-union: Saudi J Biol Sci, 2018; 25; 819-25
6. Meleppuram JJ, Ibrahim S, Experience in fixation of infected non-union tibia by Ilizarov technique – a retrospective study of 42 cases: Rev Bras Ortop (English Ed), 2017; 52; 670-75
7. Wani NB, Syed B, Ilizarov ring fixator in the management of infected non-unions of tibia: Sicot-J, 2015; 1; 22
8. Abuomira IEA, Sala F, Elbatrawy Y, Distraction osteogenesis for tibial nonunion with bone loss using combined Ilizarov and Taylor spatial frames versus a conventional circular frame: Strateg Trauma Limb Reconstr, 2016; 11; 153-59
9. Baruah RK, Ilizarov methodology for infected non-union of the Tibia: Classic circular transfixion wire assembly vs. hybrid assembly: Indian J Orthop, 2007; 41; 198-203
10. Eralp IL, Kocaoğlu M, Dikmen G, Treatment of infected nonunion of the juxta-articular region of the distal tibia: Acta Orthop Traumatol Turc, 2016; 50; 139-46
11. Hosny G, Shawky MS, The treatment of infected non-union of the tibia by compression-distraction techniques using the Ilizarov external fixator: Int Orthop, 1998; 22; 298-302
12. Khan MS, Rashid H, Umer M, Salvage of infected non-union of the tibia with an ilizarov ring fixator: J Orthop Surg, 2015; 23; 52-55
13. Madhusudhan TR, Ramesh B, Manjunath K, Outcomes of Ilizarov ring fixation in recalcitrant infected tibial non-unions – a prospective study: J Trauma Manag Outcomes, 2008; 2; 6
14. Magadum MP, Basavaraj Yadav CM, Acute compression and lengthening by the Ilizarov technique for infected nonunion of the tibia with large bone defects: J Orthop Surg (Hong Kong), 2006; 14; 273-79
15. Sahu R, Ranjan R, Treatment of complex nonunion of the shaft of the tibia using Ilizarov technique and its functional outcome: Niger Med J, 2016; 57; 129-33
16. Sanders DW, Galpin RD, Hosseini M, MacLeod MD, Morbidity resulting from the treatment of tibial nonunion with the Ilizarov frame: Can J Surg, 2002; 45; 196-200
17. Shahid M, Hussain A, Bridgeman P, Bose D, Clinical outcomes of the Ilizarov method after an infected tibial non union: Arch Trauma Res, 2013; 2; 71-75
18. Wang H, Wei X, Liu P, Quality of life and complications at the different stages of bone transport for treatment infected nonunion of the tibia: Med (United States), 2017; 96; e8569
19. Yin P, Zhang L, Li T, Infected nonunion of tibia and femur treated by bone transport: J Orthop Surg Res, 2015; 10; 49
20. McNally M, Ferguson J, Kugan R, Stubbs D, Ilizarov treatment protocols in the management of infected nonunion of the tibia: J Orthop Trauma, 2017; 31; 47-54
21. Dróżdż M, Rak S, Bartosz P, Results of the treatment of infected nonunions of the lower limbs using the Ilizarov method: Ortop Traumatol Rehabil, 2017; 19; 111-26
22. Yin P, Zhang Q, Mao Z, Li T, The treatment of infected tibial nonunion by bone transport using the Ilizarov external fixator and a systematic review of infected tibial nonunion treated by Ilizarov methods: Acta Orthop Belg, 2014; 80; 426-35
23. Xu J, Jia YC, Kang QL, Chai YM, Management of hypertrophic nonunion with failure of internal fixation by distraction osteogenesis: Injury, 2015; 46; 2030-35
24. Marsh DR, Shah S, Elliott J, Kurdy N, The Ilizarov method in nonunion, malunion and infection of fractures: J Bone Jt Surg – Ser B, 1997; 79; 273-79
25. Megas P, Saridis A, Kouzelis A, The treatment of infected nonunion of the tibia following intramedullary nailing by the Ilizarov method: Injury, 2010; 41; 294-99
26. Laursen MB, Lass P, Christensen KS, Ilizarov treatment of tibial nonunions results in 16 cases: Acta Orthop Belg, 2000; 66; 279-85
27. Hosny GA, Ahmed ASAA, Hussein MAE, Clinical outcomes with the corticotomy-first technique associated with the Ilizarov method for the management of the septic long bones non-union: Int Orthop, 2018; 42; 2933-39
28. Morandi M, Zembo MM, Ciotti M, Infected tibial pseudarthrosis. A 2-year follow up on patients treated by the Ilizarov technique: Orthopedics, 1989; 12; 497-508
29. Chahal J, Stephen DJG, Bulmer B, Daniels T, Kreder HJ, Factors associated with outcome after subtalar arthrodesis: J Orthop Trauma, 2006; 20; 555-61
30. Dalat F, Trouillet F, Fessy MH, Comparison of quality of life following total ankle arthroplasty and ankle arthrodesis: Retrospective study of 54 cases: Rev Chir Orthop Traumatol, 2014; 100; 542-47
31. Bednarz PA, Beals TC, Manoli A, Subtalar distraction bone block fusion: An assessment of outcome: Foot Ankle Int, 1997; 18; 785-91
32. Martin RRL, Irrgang JJ, Burdett RG, Evidence of validity for the Foot and Ankle Ability Measure (FAAM): Foot Ankle Int, 2005; 26; 968-83
33. Morasiewicz P, Konieczny G, Dejnek M, Assessment of the distribution of load on the lower limbs and balance before and after ankle arthrodesis with the Ilizarov method: Sci Rep, 2018; 8; 15693
34. Morasiewicz P, Konieczny G, Dejnek M, Pedobarographic analysis of body weight distribution on the lower limbs and balance after ankle arthrodesis with Ilizarov fixation and internal fixation: Biomed Eng Online, 2018; 17; 174
35. Morasiewicz P, Urbański W, Kulej M, Balance and lower limb loads distribution after Ilizarov corticotomy: Injury, 2018; 49; 860-65
36. Morasiewicz P, Dragan S, Dragan SŁ, Pedobarographic analysis of body weight distribution on the lower limbs and balance after Ilizarov corticotomies: Clin Biomech, 2016; 31; 2-6
37. Rongies W, Bak A, Lazar A, Dolecki W, A trial of the use of pedobarography in the assessment of the effectiveness of rehabilitation in patients with coxarthrosis: Ortop Traumatol Rehabil, 2009; 11; 242-52
38. Lorkowski J, Trybus M, Hładki W, Brongel L, Underfoot pressure distribution of a patient with unilateral ankylosis of talonavicular joint during rheumatoid arthritis – case report: Przegl Lek, 2008; 65; 54-56
39. Veilleux LN, Robert M, Ballaz L, Gait analysis using a force–measuring gangway: Intrasession repeatability in healthy adults: J Musculoskelet Neuronal Interact, 2011; 11; 27-33
40. Majewski M, Bischoff-Ferrari HA, Grüneberg C, Improvements in balance after total hipreplacement: J Bone Jt Surg – Ser B, 2005; 87; 1337-43
41. Radler C, Kranzl A, Manner HM, Torsional profile versus gait analysis: Consistency between the anatomic torsion and the resulting gait pattern in patients with rotational malalignment of the lower extremity: Gait Posture, 2010; 32; 405-10
42. Bhave A, Paley D, Herzenberg JE, Improvement in gait parameters after lengthening for the treatment of limb-length discrepancy: J Bone Jt Surg – Ser A, 1999; 81; 529-34
43. McHale KA, Ross AE, Treatment of infected tibial nonunions with debridement, antibiotic beads, and the Ilizarov method: Mil Med, 2004; 169; 728-34
44. Ling JS, Smyth NA, Fraser EJ, Investigating the relationship between ankle arthrodesis and adjacent-joint arthritis in the hindfoot a systematic review a systematic review: J Bone Jt Surg – Am Vol, 2015; 97; 513-19
45. Pajchert-Kozłowska A, Pawik Ł, Szelerski Ł, Assessment of body balance of patients treated with the Ilizarov method for tibial nonunion: Acta Bioeng Biomech, 2020; 22; 131-37
46. Kim Y, Moon S, Effects of treadmill training with the eyes closed on gait and balance ability of chronic stroke patients: J Phys Ther Sci, 2015; 27; 2935-38
47. Moon S, Kim Y, Effect of blocked vision treadmill training on knee joint proprioception of patients with chronic stroke: J Phys Ther Sci, 2015; 27; 897-900
Figures
 Figure 1. Radiological findings of nonunion – hypertrophic (A Patient before treatment, B Patient during the treatment process, C Patient after treatment).
Figure 1. Radiological findings of nonunion – hypertrophic (A Patient before treatment, B Patient during the treatment process, C Patient after treatment).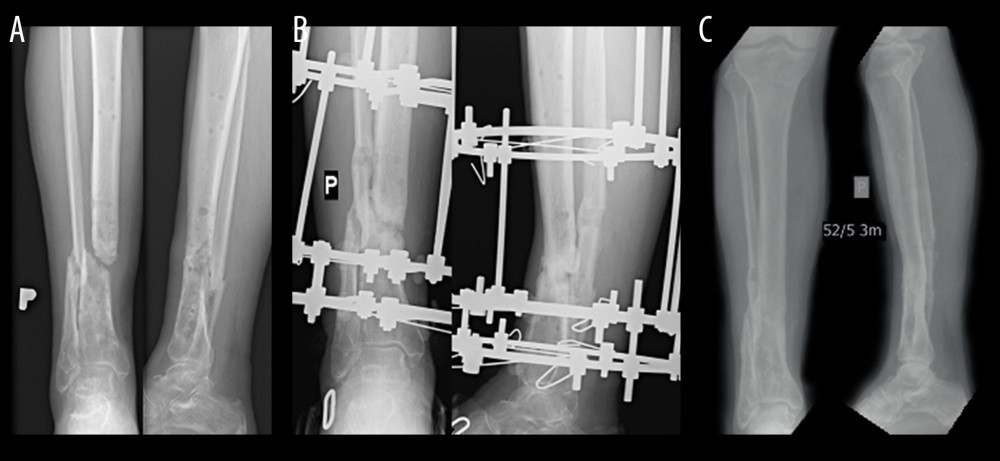 Figure 2. Radiological findings of nonunion – atrophic (A Patient before treatment, B Patient during the treatment process, C Patient after treatment).
Figure 2. Radiological findings of nonunion – atrophic (A Patient before treatment, B Patient during the treatment process, C Patient after treatment). Figure 3. Subject during measurements on the pedobarographic platform manufactured by Zebris Medical GmbH.
Figure 3. Subject during measurements on the pedobarographic platform manufactured by Zebris Medical GmbH.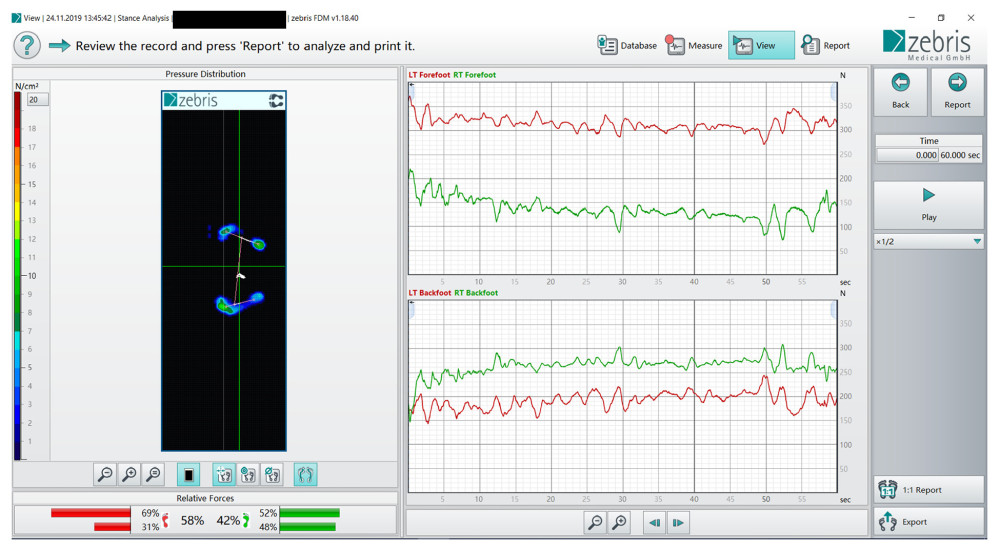 Figure 4. Distribution of load on the operated and healthy limb.
Figure 4. Distribution of load on the operated and healthy limb.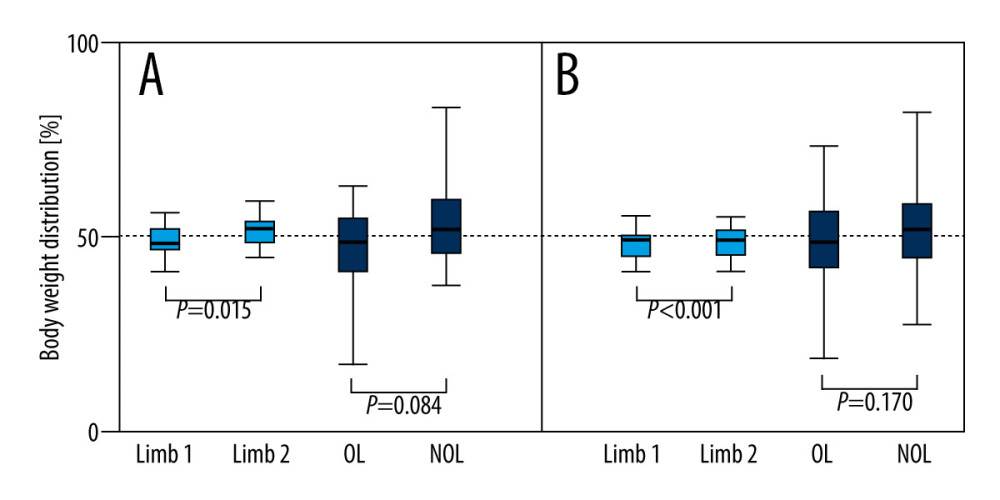 Figure 5. Body weight distribution for patients after treatment with the Ilizarov method between OL and NOL vs healthy people. The test was performed for 60 seconds with participants’ eyes open (A) or closed (B). The boundary of the box closest to zero indicates the 25th percentile, a line within the box marks the median, and the boundary of the box farthest from zero indicates the 75th percentile. Whiskers (error bars) above and below the box indicate the 90th and 10th percentiles. White boxes, healthy people; filled boxes, patients. OL – operated limb; NOL – non-operated limb.
Figure 5. Body weight distribution for patients after treatment with the Ilizarov method between OL and NOL vs healthy people. The test was performed for 60 seconds with participants’ eyes open (A) or closed (B). The boundary of the box closest to zero indicates the 25th percentile, a line within the box marks the median, and the boundary of the box farthest from zero indicates the 75th percentile. Whiskers (error bars) above and below the box indicate the 90th and 10th percentiles. White boxes, healthy people; filled boxes, patients. OL – operated limb; NOL – non-operated limb. Tables
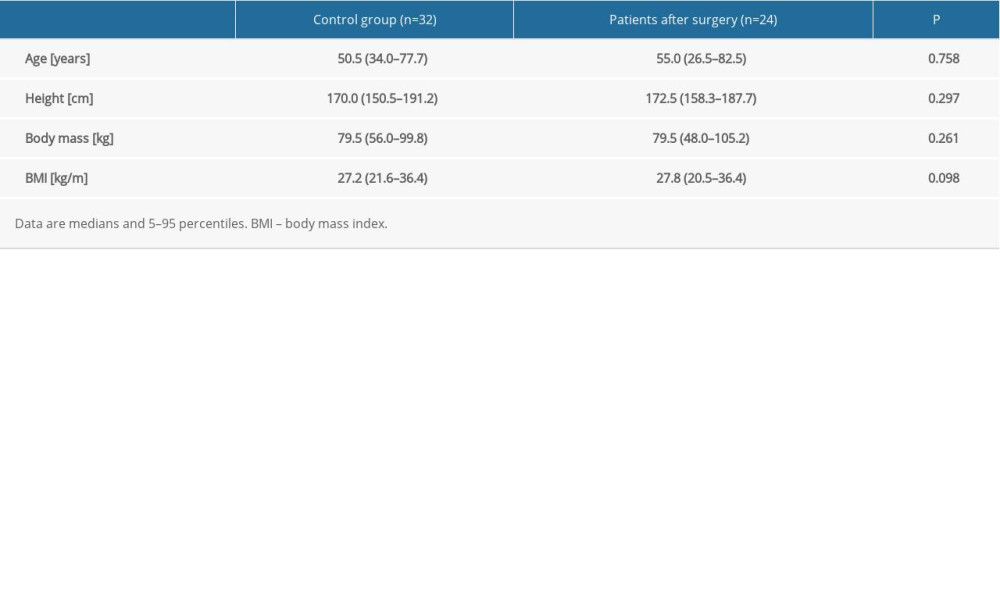 Table 1. Characteristics of the participants.
Table 1. Characteristics of the participants.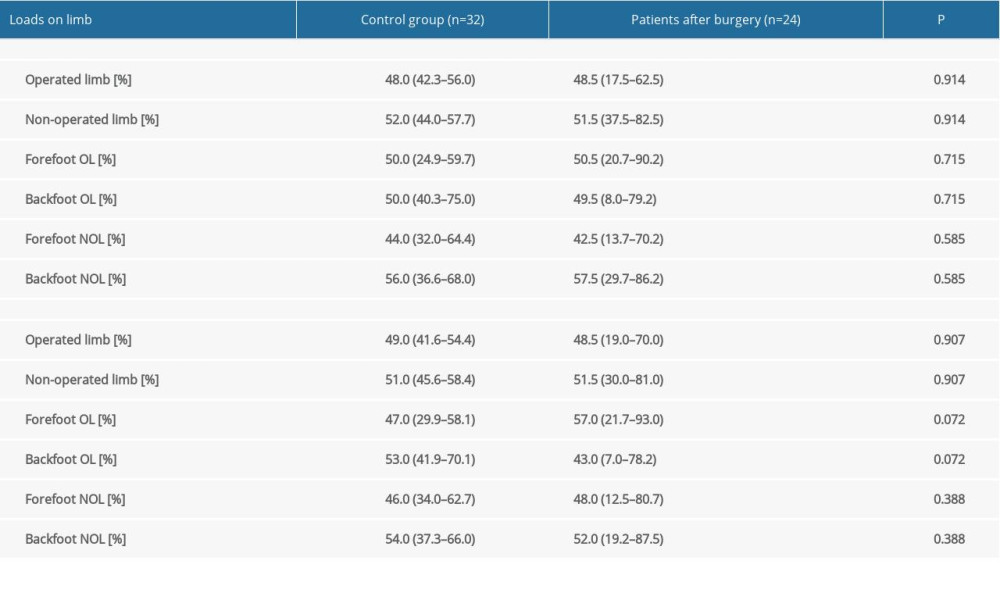 Table 2. Body weight distribution for patients after treatment with the Ilizarov method compared to the control group of healthy people.
Table 2. Body weight distribution for patients after treatment with the Ilizarov method compared to the control group of healthy people.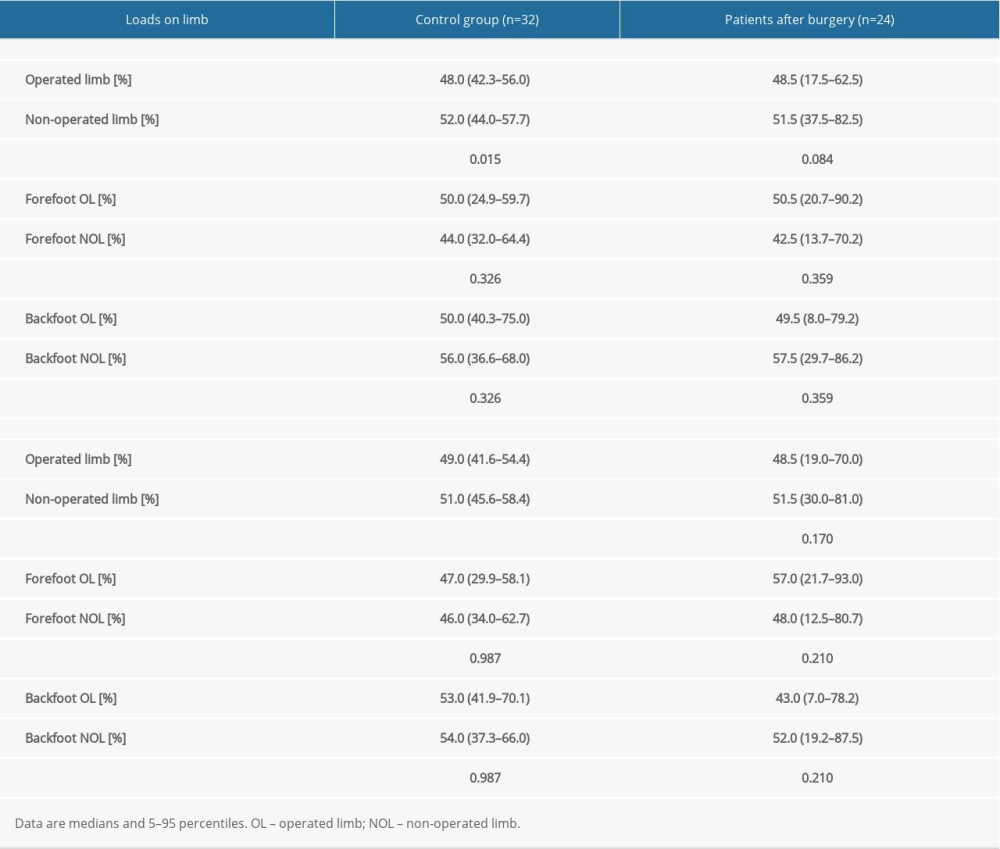 Table 3. Body weight distribution for patients after treatment with the Ilizarov method between OL and NOL vs healthy people.
Table 3. Body weight distribution for patients after treatment with the Ilizarov method between OL and NOL vs healthy people.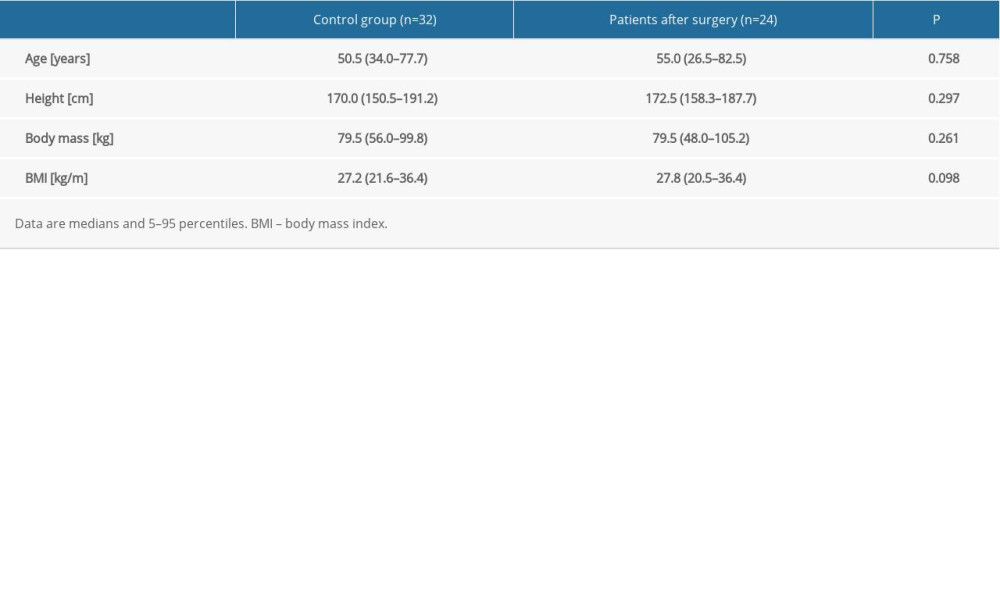 Table 1. Characteristics of the participants.
Table 1. Characteristics of the participants.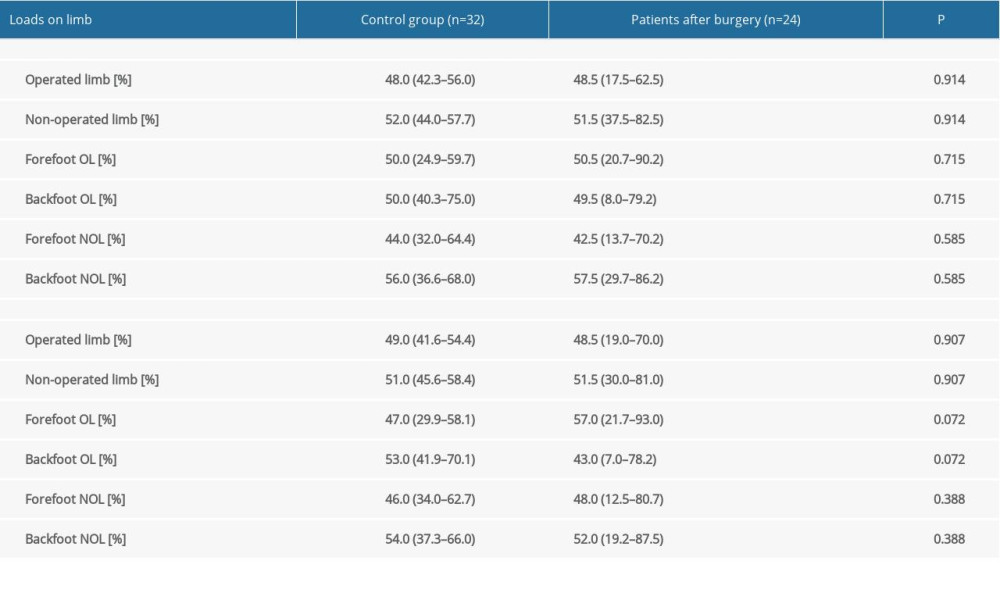 Table 2. Body weight distribution for patients after treatment with the Ilizarov method compared to the control group of healthy people.
Table 2. Body weight distribution for patients after treatment with the Ilizarov method compared to the control group of healthy people.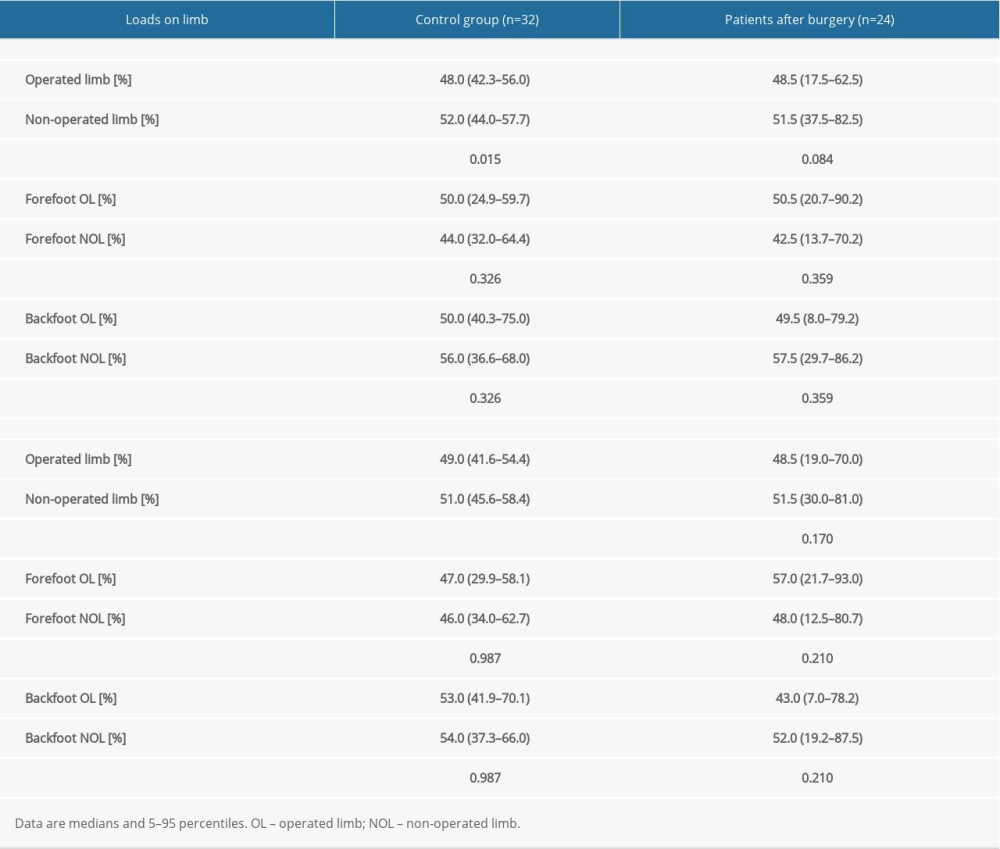 Table 3. Body weight distribution for patients after treatment with the Ilizarov method between OL and NOL vs healthy people.
Table 3. Body weight distribution for patients after treatment with the Ilizarov method between OL and NOL vs healthy people. In Press
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








