22 September 2021: Clinical Research
Comparison of Total Laminectomy and Pedicle Screw Internal Fixation with Ultrasonic- and Microscopic-Assisted Laminectomy Replantation for Tumors of the Lumbar Spinal Canal: A Retrospective Study of 60 Cases from a Single Center
YongChi Duan1A, Jun Ma1D, Sheng Miao1E, JinHong Zhang1F, JieLin Deng1B*, Han Wu2CDOI: 10.12659/MSM.931768
Med Sci Monit 2021; 27:e931768
Abstract
BACKGROUND: Total laminectomy with pedicle screw internal fixation is the most common surgical procedure for patients with primary tumors arising in the spinal canal, but the procedure has several limitations. This study aimed to compare total laminectomy and pedicle screw internal fixation with ultrasound- and microscope-assisted laminectomy replantation surgery in patients with tumors of the lumbar spinal canal.
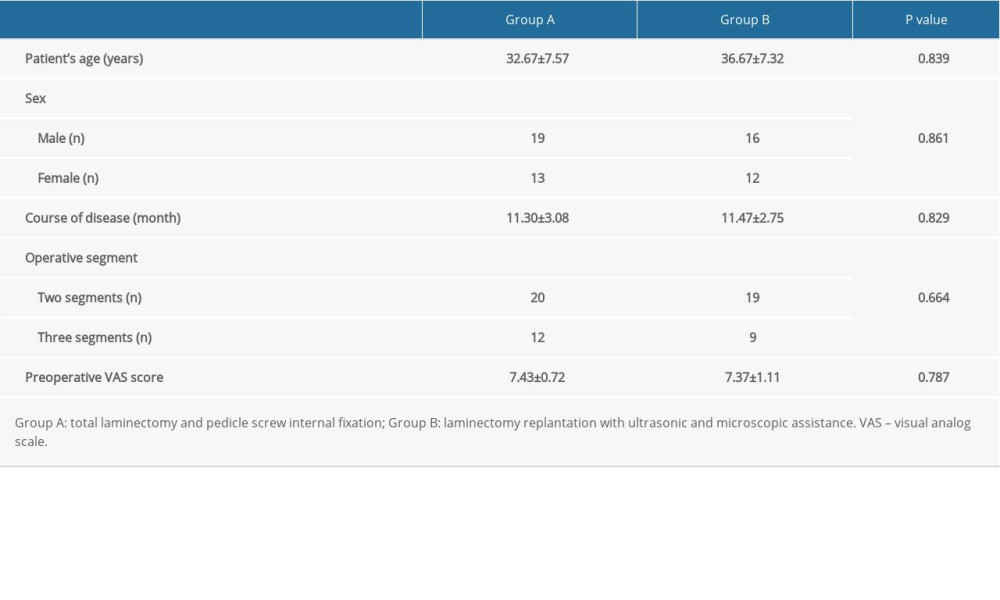
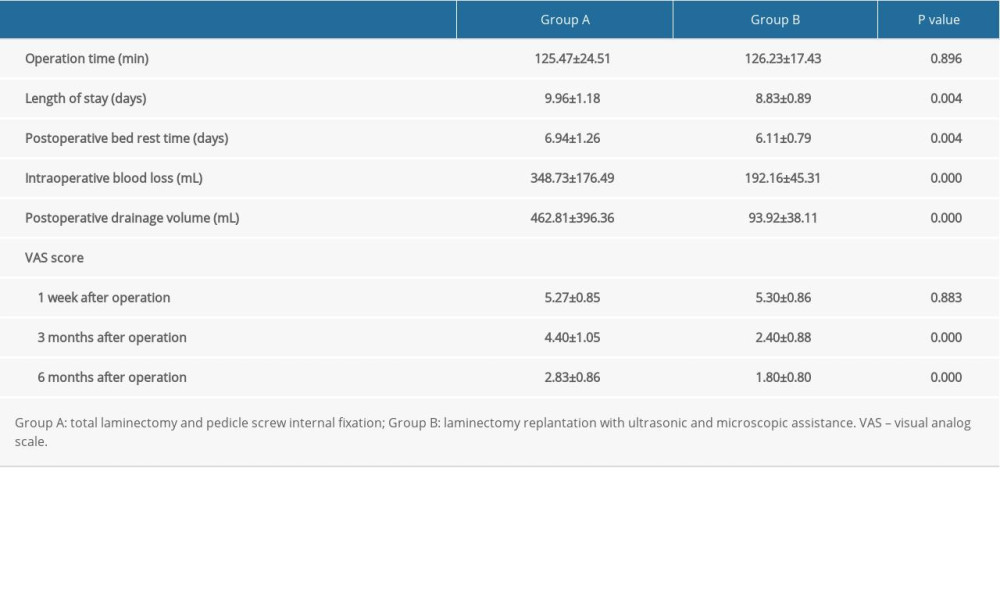
MATERIAL AND METHODS: A retrospective study was conducted. Sixty patients with tumor spinal canal were admitted to our hospital. Patients in group A (n=32) underwent total laminectomy and pedicle screw internal fixation; patients in group B (n=28) underwent laminectomy replantation with ultrasonic and microscopic assistance. Operative time, intraoperative blood loss, operative segment, length of hospital stay, postoperative length of bed rest, and visual analog scale (VAS) score after surgery were analyzed.
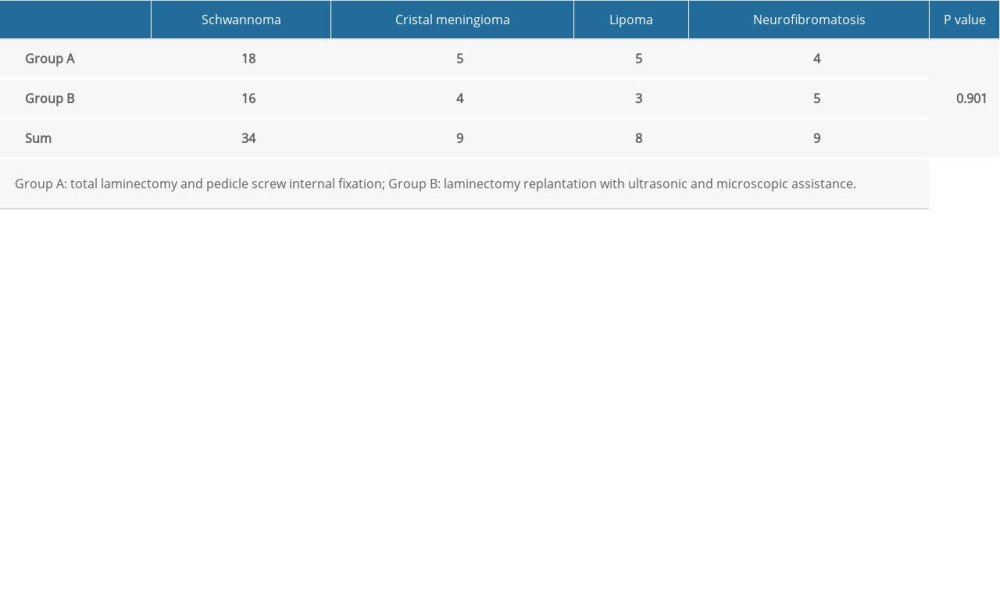
RESULTS: Hospital stay and postoperative bed rest time of patients in group B were shorter than those in group A (P=0.004). Intraoperative blood loss, postoperative drainage volume, and postoperative pain relief of group B were significantly lower than those of group A (P=0.000). There was no significant difference in postoperative pathological results between the 2 groups (P=0.901).
CONCLUSIONS: Ultrasound- and microscope-assisted laminectomy replantation resulted in the reduced intraoperative blood loss, postoperative drainage volume, length of hospital stay, and postoperative VAS pain score, compared with total laminectomy and pedicle screw internal fixation for the surgical removal of tumors of the lumbar spinal canal.
Keywords: Electron Microscope Tomography, Laminectomy, Osteotomy, Spinal Canal, Female, Fracture Fixation, Internal, Humans, Lumbar Vertebrae, Pedicle Screws, Replantation, Spinal Neoplasms, young adult
Background
Lumbar intraspinal tumors are tumors occurring in various tissues of the lumbar spinal canal, of which neurogenic tumors account for about 99% [1]. Lumbar intraspinal tumors are divided into intramedullary tumors and extramedullary tumors, with extramedullary tumors consisting of mainly schwannomas, and intramedullary tumors consisting of mainly astrocytomas [2]. The symptoms of both types are similar to lumbar disc herniation, with low back pain, sensation, and dysfunction of both lower limbs [3]. At present, total laminectomy and pedicle internal screw fixation are widely used in clinical practice. Total laminectomy for the treatment of intraspinal tumors was first carried out by Professor William Gowers in 1888. After more than 100 years of improvement, the internal fixation system was added, forming the present total laminectomy and pedicle screw internal fixation surgery. In total laminectomy and pedicle screw internal fixation surgery, part of the posterior column of the vertebral body is removed and the pedicle screw is used to provide spinal stability and support. According to the 3-column theory proposed by Denis [4], the anterior and middle columns provide support for the spine, while the posterior column protects the spinal cord and nerve roots. From the mechanical point of view, the posterior column bears 24% to 30% of pressure and 21% to 54% of rotation pressure, so the complete posterior column structure can provide the overall stability of the spine [5]. The facet joint is located in the posterior part of the vertebral body and is an important part of the posterior column of the lumbar spine. The facet joint has a special locking function and plays an important role in preventing spondylolisthesis. If the posterior column is damaged, it will lead to excessive flexion or forward sliding of the spine, resulting in lumbar spondylolisthesis and lumbar instability. According to the literature, total laminectomy and pedicle screw internal fixation affect the stability of the spine, especially when there are many surgical segments, and can cause spondylolisthesis [6,7]. During total laminectomy and pedicle screw internal fixation, the muscle attachment point is removed, which further weakens spinal stability. Therefore, the ideal surgical method would not only completely remove the tumor, but also restore the integrity and stability of the spine as much as possible and reduce postoperative complications [8,9].
To avoid these complications, some spinal surgeons began using new equipment and new surgical methods to treat lumbar intraspinal tumors, the most representative of which is laminectomy replantation assisted by a microscope and ultrasonic osteotome. Ultrasound- and microscope-assisted laminectomy replantation is a relatively new surgical method. The surgical method uses an ultrasonic osteotome for laminectomy, tumor resection under the microscope, and then a miniature titanium plate to replant the removed lamina [10]. Therefore, this study aimed to compare total laminectomy and pedicle screw internal fixation with ultrasound- and microscope-assisted laminectomy replantation surgery in 60 patients with tumors of the lumbar spinal canal.
Material and Methods
PATIENTS:
This was a retrospective study. Sixty patients with spinal canal tumors spinal who were admitted to our hospital from September 2016 to January 2019 and met the inclusion criteria were selected. Patients were divided into 2 groups according to different surgical methods. In group A, 32 patients underwent total laminectomy and pedicle screw internal fixation. In group B, 28 patients underwent ultrasound- and microscope-assisted laminectomy replantation. All 60 patients were followed up for 6 months. The study was approved by the Ethics Committee of the First People’s Hospital of Suqian (No. 2020-KYSB-003). The study procedures complied with the Declaration of Helsinki. All participants provided informed consent to participate in the study.
INCLUSION CRITERIA:
The inclusion criteria were as follows: (1) imaging examination showed a space-occupying lesion in the lumbar spinal canal; (2) the space-occupying lesion was confined to the lumbar spinal canal; (3) patient age ranged from 15 to 55 years, and patient was otherwise physically fit and had no other diseases; (4) patient had a normal vertebral sequence and no previous lumbar surgery history; and (5) all surgeries were performed by the same surgeon and surgical team.
EXCLUSION CRITERIA:
The exclusion criteria were as follows: (1) severe clotting dysfunction; (2) malignant tumor; (3) severe spinal deformity; (4) patient with severe mental illness who did not cooperate with the surgery; (5) the existence of other types of underlying diseases; (6) patients with unexplained pain and dysfunction.
IMAGING EXAMINATION:
All patients had a preoperative examination by lumbar X-ray imaging and computed tomography to determine whether the lumbar spine sequence and vertebral body shape were normal (Figure 1). Lumbar magnetic resonance imaging was performed on all patients before surgery to determine the tumor signal, size, and location and to make a preliminary judgment on the nature of the tumor.
1. TOTAL LAMINECTOMY AND PEDICLE SCREW INTERNAL FIXATION: After general anesthesia was administered, the patient was placed in the prone position. The skin and subcutaneous tissues were incised layer by layer, and the supraspinous ligament, interspinous ligament, and muscle tissue on both sides of the lamina were exposed. An X-ray fluoroscopic machine assisted the appropriate placement of the lumbar pedicle screw. The superior spinous ligament, interspinous ligament, and spinous process were removed with a rongeur. The vertebral lamina and some upper and lower articular processes were removed with a bone chisel and rongeur to expose the dural sac (Figure 2A). The dural sac was incised longitudinally with a scalpel. The tumor and nerve root tissues were carefully separated with tumor forceps (Figure 2B) to explore whether there was residual tumor in the spinal canal. The incision of the dural sac was sutured continuously (Figure 2C), and then the screw connecting rod was connected and locked. The negative-pressure drainage tube was inserted. The skin and subcutaneous tissue were sutured layer by layer. We performed imaging tests on the patients after 3 months (Figure 2D, 2E).
2. ULTRASOUND- AND MICROSCOPE-ASSISTED LAMINECTOMY REPLANTATION: After general anesthesia, the patient was placed in the prone position. The skin and subcutaneous tissues were incised one layer at a time. The muscle tissues on both sides were pulled with a retractor to expose the spinous process, lamina, and upper and lower articular processes. The whole lamina and spinous process were excised with an ultrasonic osteotome (Figure 3A), the spinal canal was opened, and the dura sac was exposed. Under the microscope, a scalpel was used to cut the dural sac longitudinally, and an oval tumor was found in the spinal canal (Figure 3B). Under the microscope, the tumor and nerve root tissues were carefully separated (Figure 3C). No residual tumor was detected in the spinal canal. The incision of the dural sac was sutured continuously. One end of the titanium plate was fixed on the lamina with screws (Figure 3D), and the other end was fixed at the vertebral body to restore the original anatomical position of the lamina (Figure 3E). The lamina and spinous process were fixed stably in a good position. The negative-pressure drainage tube was inserted. The skin and subcutaneous tissue were sutured layer by layer. We performed imaging tests on the patient after 3 months (Figure 3F, 3G).
OBSERVATION ITEMS AND METHODS:
The following variables were collected: (1) operation duration; (2) intraoperative blood loss; (3) length of stay in hospital; (4) postoperative bed rest time; (5) postoperative drainage volume; (6) visual analog scale (VAS) score, which was collected at 1 week, 3 months, and 6 months after surgery.
STATISTICAL ANALYSIS:
Descriptive statistical analysis was performed with SPSS 20.0 statistical software. The results are presented as means with ranges and standard deviations. The chi-squared test was used to analyze patient sex, operative segment, and pathological results. However, because of the small sample, the statistical power of this analysis was limited.
Results
All patients successfully completed the surgery and follow-up. None of the patients had complications, such as infection and loosening of internal fixations. The data showed no significant differences in age or sex between the 2 groups (age range, 21–45 years;
As shown in Table 2, the duration of the 2 surgical methods was almost the same (range 90–178 min;
Discussion
Complete tumor excision and spinal integrity-preserving surgery are the 2 basic principles of surgical treatment [11]. However, total laminectomy and pedicle screw internal fixation require the removal of bilateral lamina with a rongeur, and the posterior column structure of the vertebral body is damaged. Spinal canal dural sac injury and nerve root injury can easily occur when the bone chisel knocks out the lamina because of the operator’s strength in grasping the instrument [12]. Some patients often have cerebrospinal fluid leakage and aggravation of neurological symptoms. Under ultrasound- and microscope-assisted laminectomy replantation procedures, an ultrasonic osteotome was used for lamina cutting because it had an effect on calcified calcium salt, reducing dural sac and nerve root injury [13]. Total laminectomy and pedicle screw internal fixation removed the spinous process and lamina, which made the posterior column structure of the vertebral body incomplete. In addition, the pedicle screw system is used in total laminectomy and pedicle screw internal fixation. Owing to the large screw rod, it is easy to compress the lumbar intermuscular nerve, and patients are prone to lumbar pain after surgery [14]. Under the assistance of a microscope and ultrasonic osteotome, the removed lamina were replanted in the original position, and the anatomical structure of posterior vertebral body was reconstructed in the present study.
From the perspective of lumbar range of motion, the use of the pedicle screw system in total laminectomy and pedicle screw internal fixation impedes the range of motion between vertebrae. Then, the motion and stress compensation increases in the adjacent segments of the vertebral body, causing potential lumbar instability and spondylolisthesis [15]. Papagelopoulos et al demonstrated that 28% of young patients treated with laminectomy exhibited spinal deformity and intervertebral instability [16]. According to the literature, total laminectomy and pedicle screw internal fixation affect the stability of the spine and, if too many surgical segments are involved, can cause kyphosis [17,18]. In the present study, ultrasound- and microscope-assisted laminectomy replantation did not require interbody fixation and fusion, retained the motion function of the surgical segments, and avoided the instability or spondylolisthesis caused by fusion and fixation. At the same time, the spinal canal and the posterior column structure of vertebral body were reconstructed, providing attachment points for muscles on both sides. The biomechanical stability was strong, and the patients could move earlier after surgery [19]. Zhou et al reported that patients who underwent laminectomy replantation had a 36% to 60% increase in longitudinal spinal stress resistance and a 38% to 49% increase in lateral stability, compared with patients who underwent total laminectomy [20]. Moreover, the miniature titanium plate used in replantation is firmly fixed and flexible, has strong plasticity, and is not easy to break [18]. Spinal surgeons can adjust the miniature titanium plate according to the location of the vertebral body. During surgery, the ultrasonic osteotome has the advantages of a low frequency and small amplitude, and, by only cutting bone tissue, it can reduce the damage to capillaries to the maximum extent. In addition, the water spraying equipment of the ultrasonic osteotome has a certain hemostatic function, resulting in less intraoperative bleeding [21,22]. Sanborn et al reported that there is a notable reduction in osseous bleeding in ultrasonic osteotomy [23]. Surgery under a microscope can stop capillary hemorrhage easily and reduce blood loss during surgery [8].
From the perspective of postoperative drainage volume, in the present study, ultrasound- and microscope-assisted laminectomy replantation was used to reconstruct the spinal canal. Because of the natural barrier function of the lamina, cerebrospinal fluid leakage was prevented. In addition, the dural sac sutured under the microscope was relatively dense, which further prevented cerebrospinal fluid leakage. Li et al performed surgery on 38 patients with spinal canal tumors using an ultrasonic osteotome and microscope, and the postoperative drainage volume of the patients was significantly reduced, compared with previous patients [4]. From the perspective of postoperative pain relief, the use of microscopic instruments in laminectomy can accurately separate tumor tissue from nerve tissue, minimize nerve injury, and allow for the quick recovery of nerves after surgery. In Ye et al’s study of 50 patients with spinal canal tumors, patients who underwent lamina replantation had better recovery than those who underwent total laminectomy [24]. Therefore, postoperative pain was significantly reduced. In addition, the microscope can make the surgical field clearly enlarged, improve the safety of surgery, and connect the display screen, which is conducive to teaching. In the present study, under the assistance of a microscope and ultrasonic osteotome, the spinal canal was reconstructed. As reported by Song et al, due to the natural barrier function of the lamina, direct contact between the dural sac and soft tissue is prevented, and the occurrence of scar adhesion and lumbar spinal stenosis is reduced [25]. Asthagiri et al reported that lamina replantation can solve the problems of postoperative scar adhesion and that the surgical design meets anatomical and physiological requirements [26].
This study had some limitations, including a small sample size and single-center design, lack of long-term follow-up results, and the inability to determine the impact of the 2 surgical methods on tumor recurrence rate. Finally, the long-term clinical effects of the 2 surgical methods need further observation.
Conclusions
The findings from this retrospective study from a single center showed that ultrasound- and microscope-assisted laminectomy replantation resulted in reduced intraoperative blood loss, postoperative drainage volume, length of hospital stay, and postoperative VAS pain score, compared with total laminectomy and pedicle screw internal fixation for the surgical removal of tumors of the lumbar spinal canal.
Figures
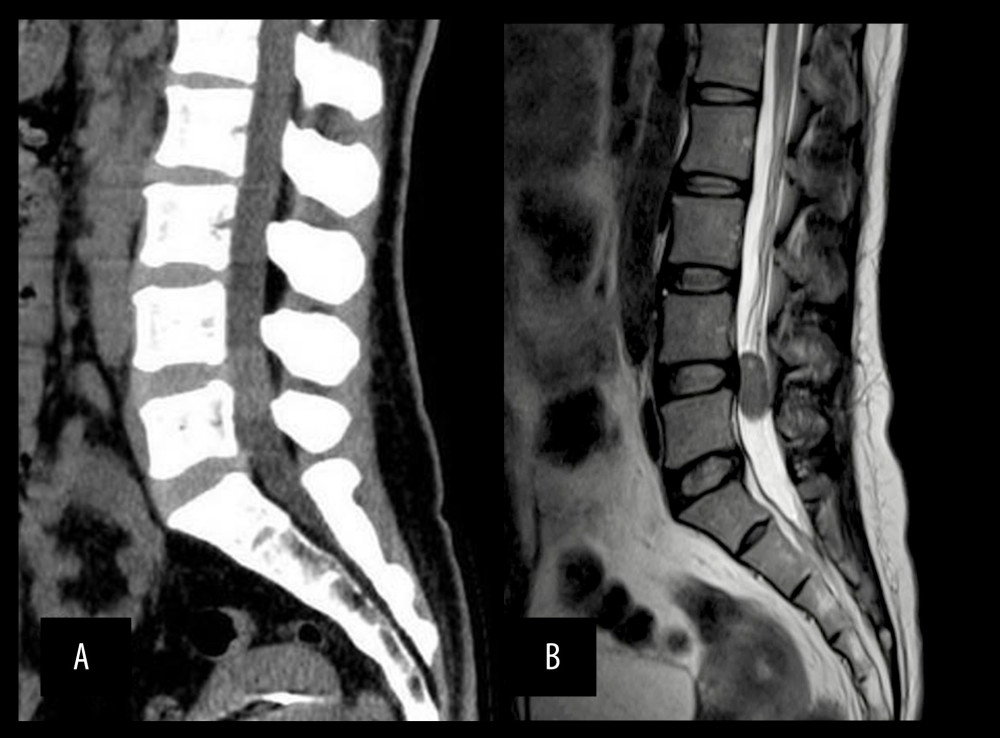 Figure 1. (A) Computed tomography image of the lumbar spine showing a normal vertebral sequence and no calcification in the spinal mass; (B) lumbar magnetic resonance imaging showing an oval mass in the spinal canal.
Figure 1. (A) Computed tomography image of the lumbar spine showing a normal vertebral sequence and no calcification in the spinal mass; (B) lumbar magnetic resonance imaging showing an oval mass in the spinal canal. 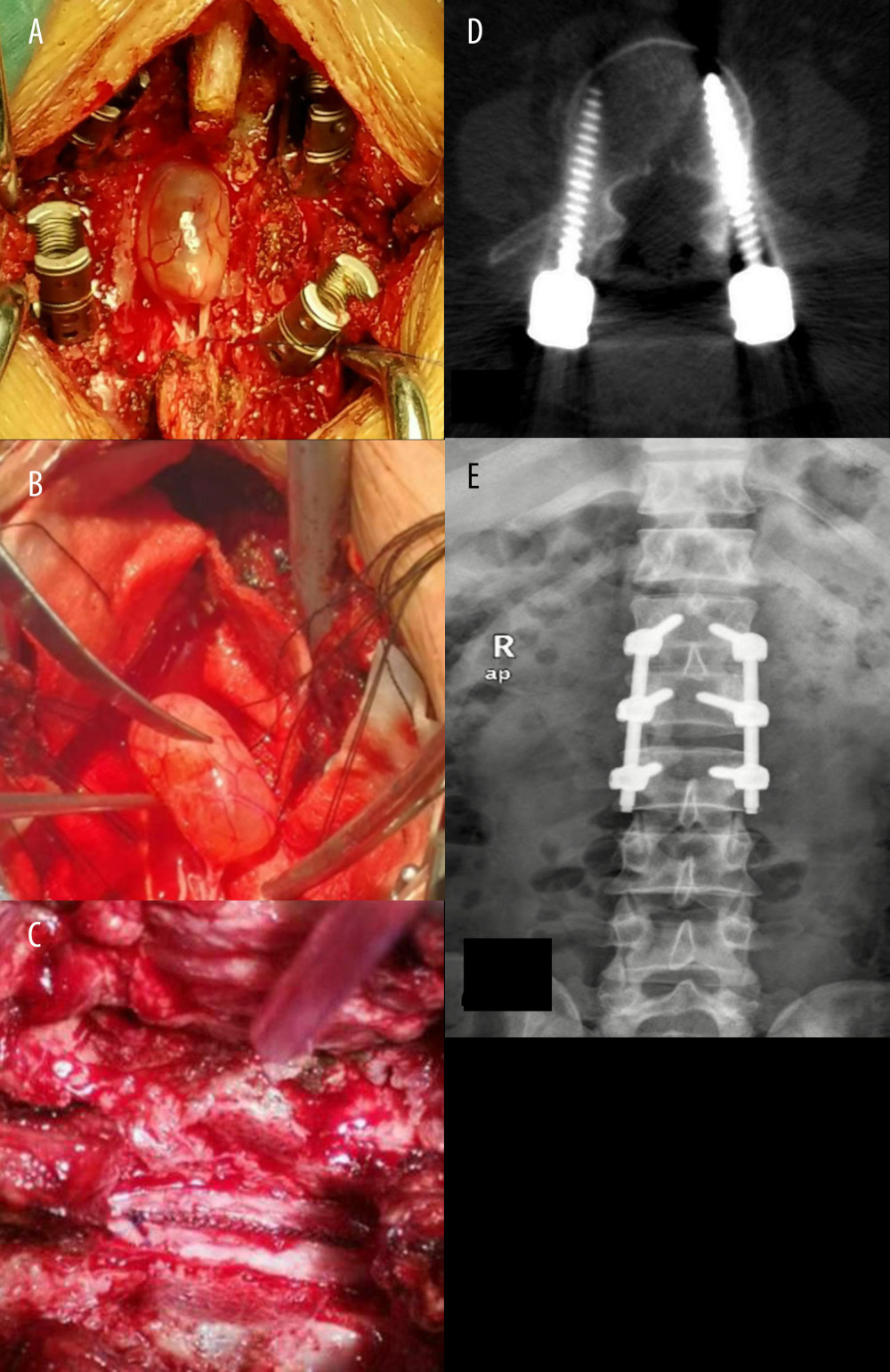 Figure 2. (A) The exposure of the dural sac after total laminectomy; (B) tumor tissue connects with nerve root; (C) the dural sac incision with continuous suture; (D, E) postoperative images of the patient.
Figure 2. (A) The exposure of the dural sac after total laminectomy; (B) tumor tissue connects with nerve root; (C) the dural sac incision with continuous suture; (D, E) postoperative images of the patient. 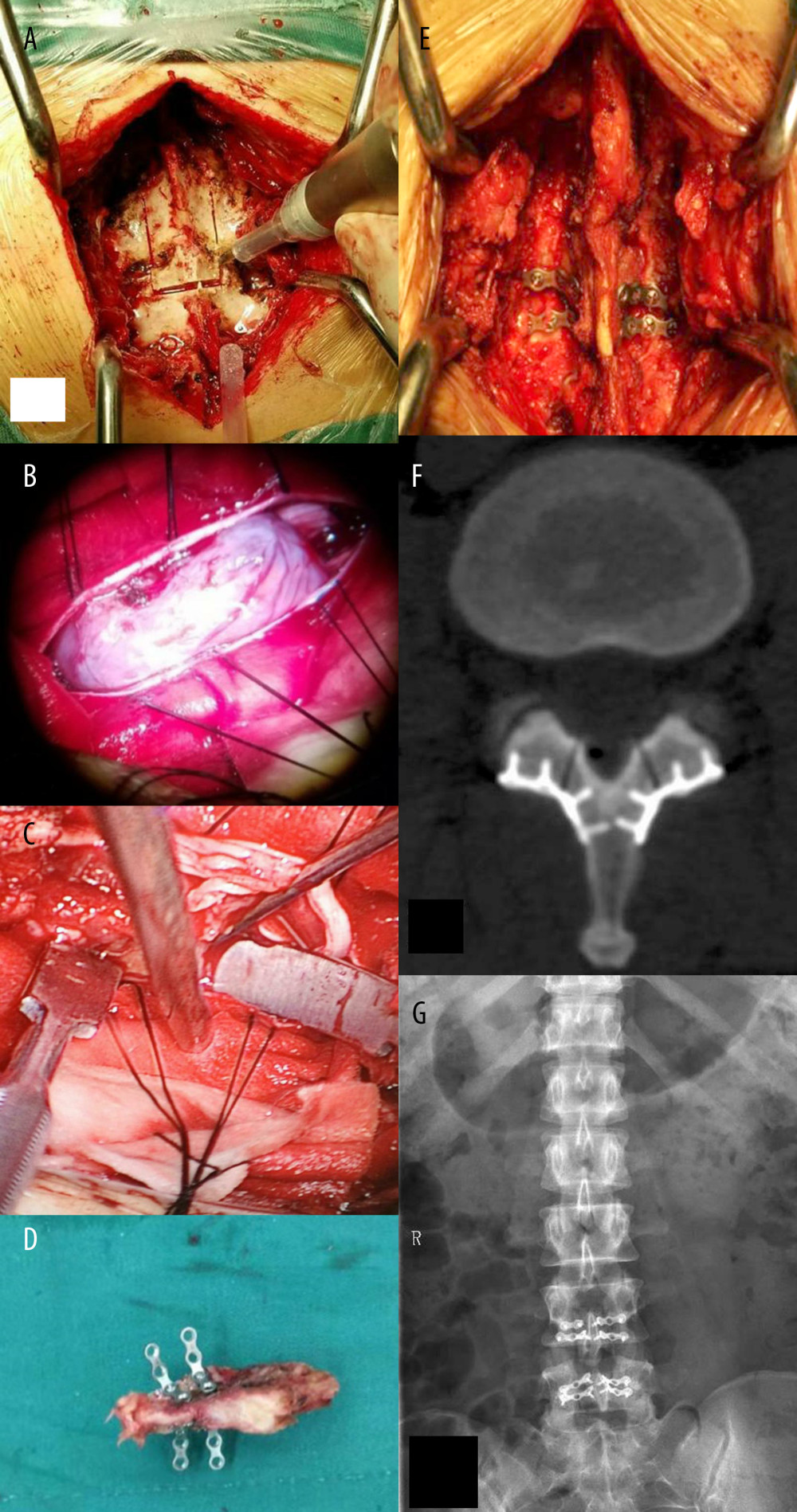 Figure 3. (A) Laminectomy under ultrasonic osteotome; (B) the tumor tissue under a microscope; (C) intraoperative image of the microscope screen; (D) the free lamina with a titanium plate; (E) replantation of lamina and spinous process in the original location; (F, G) postoperative images of the patient.
Figure 3. (A) Laminectomy under ultrasonic osteotome; (B) the tumor tissue under a microscope; (C) intraoperative image of the microscope screen; (D) the free lamina with a titanium plate; (E) replantation of lamina and spinous process in the original location; (F, G) postoperative images of the patient. References
1. Abul-Kasim K, Thurnher MM, McKeever P, Sundgren PC, Intradural spinal tumors: Current classification and MRI features: Neuroradiology, 2008; 50(4); 301-4
2. Gezen F, Kahraman S, Canakci Z, Beduk A, Review of 36 cases of spinal cord meningioma: Spine, 2000; 25(6); 727-31
3. Wang T, Du C, Zheng X, Surgical strategies for thoracic myelopathy due to ossification of ligamentum flavum: A technical note based on radiological type: Turk Neurosurg, 2008; 28; 616-24
4. Denis F, The three column spine and its significance in the classification of acute thoracolumbar spinal injuries: Spine, 2003; 8; 817-31
5. Nakai O, Ookawa A, Yamaura I, Long-term roentgenographic and functional changes in patients who were treated with wide fenestration for central lumbar stenosis: J Bone Joint Surg, 1991; 73(8); 1184-91
6. McGirt MJ, Giannina L, Parker SL, Short-term progressive spinal deformity following laminoplasty versus laminectomy for resection of intradural spinal tumors: Analysis of 238 patients: Neurosurgery, 2010; 66(55); 1005-12
7. Zhu YJ, Ying GY, Chen AQ, Minimally invasive removal of lumbar intradural extramedullary lesions using the interlaminar approach: Neurosurg Focus, 2015; 39; E10
8. Samartzis D, Gillis CC, Shih P, Intramedullary spinal cord tumors: Part II – management options and outcomes: Global Spine J, 2016; 6(2); 176-85
9. Nong L, Zhou D, Xu NW, Lamina replacement with titanium plate fixation improves spinal stability after total lumbar laminectomy: Comput Methods Biomech Biomed Engin, 2015; 18; 1753-59
10. Lin YP, Li YJ, Chen BL, Lumbar laminotomy and replantation for the treatment of adult spinal epidermoid cyst: A case report: Medicine, 2018; 97; 1-4
11. Millward CP, Bhagawati D, Chan HW, Retrospective observation comparative study of hemilaminectomy versus laminectomy for intraspinal tumour resection; Shorter stays, lower analgesic usage, and less kyphotic deformity: Brit J Neurosurg, 2015; 29(3); 390-95
12. Menku A, Koc RK, Oktem IS, Laminoplasty with miniplates for posterior approach in thoracic and lumbar intraspinal surgery: Turk Neurosurg, 2010; 20(1); 27-32
13. Lee SM, Cho YE, Kwon YM, Neurological outcome after surgical treatment of intramedullary spinal cord tumors: Korean J Spine, 2014; 11(3); 121-26
14. Wiedemayer H, Sandalcioglu IE, Aalders M, Reconstruction of the laminar roof with miniplates for a posterior approach in intraspinal surgery: Technical considerations and critical evaluation of follow-up results: Spine, 2004; 29(16); E333-42
15. Street J, Brain L, DiPaola C, Morbidity and mortality of major adult spinal surgery. A prospective cohort analysis of 942 consecutive patients: Spine J, 2012; 12; 22-34
16. Papagelopoulos PJ, Peterson HA, Ebersold MJ, Spinal column deformity and instability after lumbar or thoracolumbar laminectomy for intraspinal tumors in children and young adults: Spine, 1997; 22; 442-51
17. Morimoto D, Isu T, Kim K, Microsurgical medial fenestration with an ultrasonic bone curette for lumbar foraminal stenosis: J Nippon Med Sch, 2012; 79; 327-34
18. Li K, Wen Z, Li B, Safety and efficacy of cervical laminoplasty using a piezosurgery device compared with a high-speed drill: Medicine, 2016; 95; e4913
19. Sucu HK, Sevin IE, Rezanko T, Prevention of anterior scar formation following discectomy with a Medishield adhesion barrier: Randomized experimental trial: Turk Neurosurg, 2013; 23(3); 317-22
20. Zhou D, Nong LM, Gao GM, Application of lamina replantation with ARCH plate fixation in the thoracic and lumbar intraspinal tumors: Exp Ther Med, 2013; 6; 596-600
21. Shao K, Ji LComparison of the effectiveness of vertebral arch replantation and laminectomy in the treatment of mild to moderate isthmic spondylolisthesis: Zhongguo Xiu Fu Chongjian Wai Ke Za Zhi, 2019; 33(4); 423-29 [in Chinese]
22. Uei H, Tokuhashi Y, Oshima MEfficacy of posterior decompression and fixation based on ossification-kyphosis angle criteria for multilevel ossification of the posterior longitudinal ligament in the thoracic spine: J Neurosurg Spine, 2018; 29(2); 150-56
23. Zhang JT, Lei T, Yang L, Subsection laminectomy with pedicle screw fixation to treat thoracic ossification of ligamentum flavum: A comparative analysis with lamina osteotomy and the replantation technique: Ther Clin Risk Manag, 2020; 16; 311-19
21. Sanborn MR, Balzer J, Gerszten PC, Safety and efficacy of a novel ultrasonic osteotome device in an ovine model: J Clin Neurosci, 2011; 18(11); 1528-33
24. Ye Q, Huang W, He YSApplication of posterior spinal canal reconstruction in surgery of intraspinal tumor: Zhongguo Xiu Fu Chongjian Wai Ke Za Zhi, 2014; 28(8); 965-68 [in Chinese]
25. Song ZJ, Zhang Z, Ye YJ, Efficacy analysis of two surgical treatments for thoracic and lumbar intraspinal tumours: BMC Surgery, 2019; 19; 131-39
26. Asthagiri AR, Mehta GU, Butman JA, Long-term stability after multilevel cervical laminectomy for spinal cord tumor resection in von Hippel-Lindau disease: J Neurosurg Spine, 2011; 14(4); 444-52
Figures
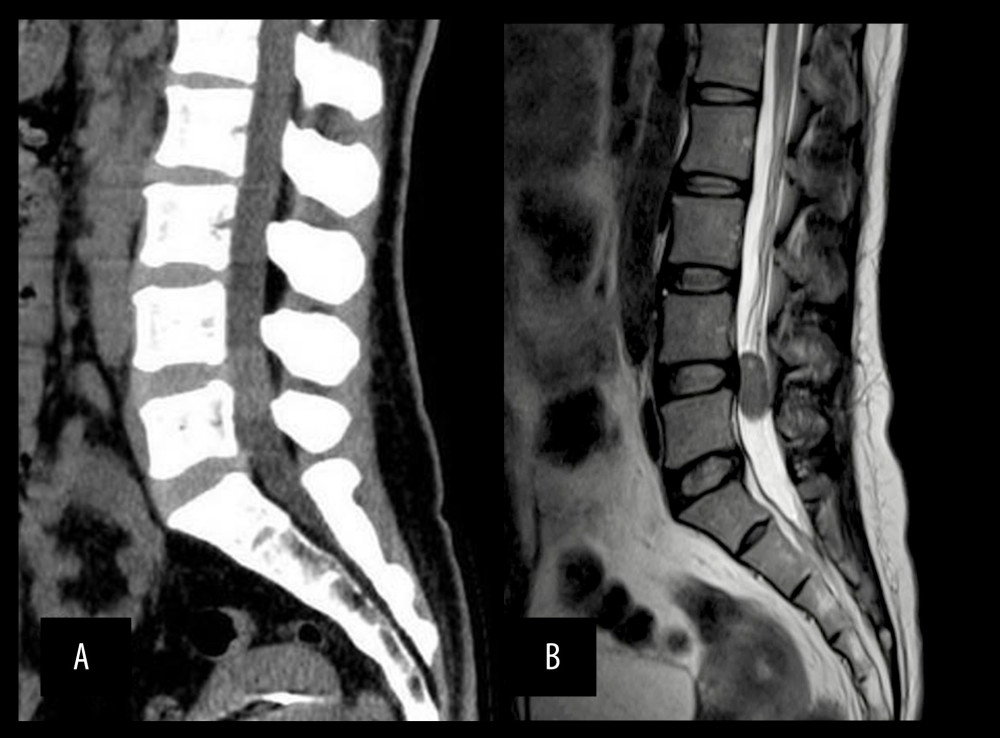 Figure 1. (A) Computed tomography image of the lumbar spine showing a normal vertebral sequence and no calcification in the spinal mass; (B) lumbar magnetic resonance imaging showing an oval mass in the spinal canal.
Figure 1. (A) Computed tomography image of the lumbar spine showing a normal vertebral sequence and no calcification in the spinal mass; (B) lumbar magnetic resonance imaging showing an oval mass in the spinal canal.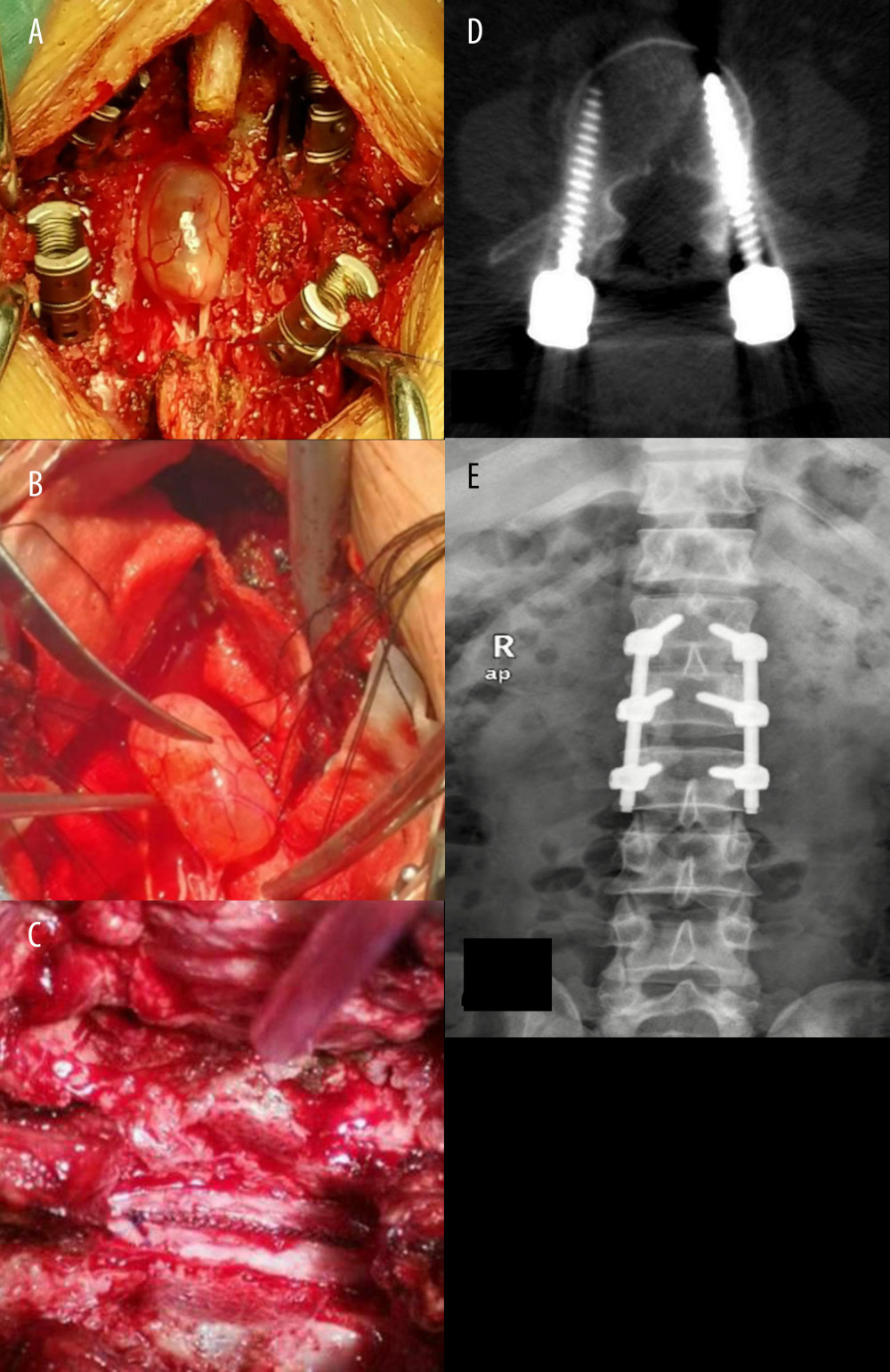 Figure 2. (A) The exposure of the dural sac after total laminectomy; (B) tumor tissue connects with nerve root; (C) the dural sac incision with continuous suture; (D, E) postoperative images of the patient.
Figure 2. (A) The exposure of the dural sac after total laminectomy; (B) tumor tissue connects with nerve root; (C) the dural sac incision with continuous suture; (D, E) postoperative images of the patient.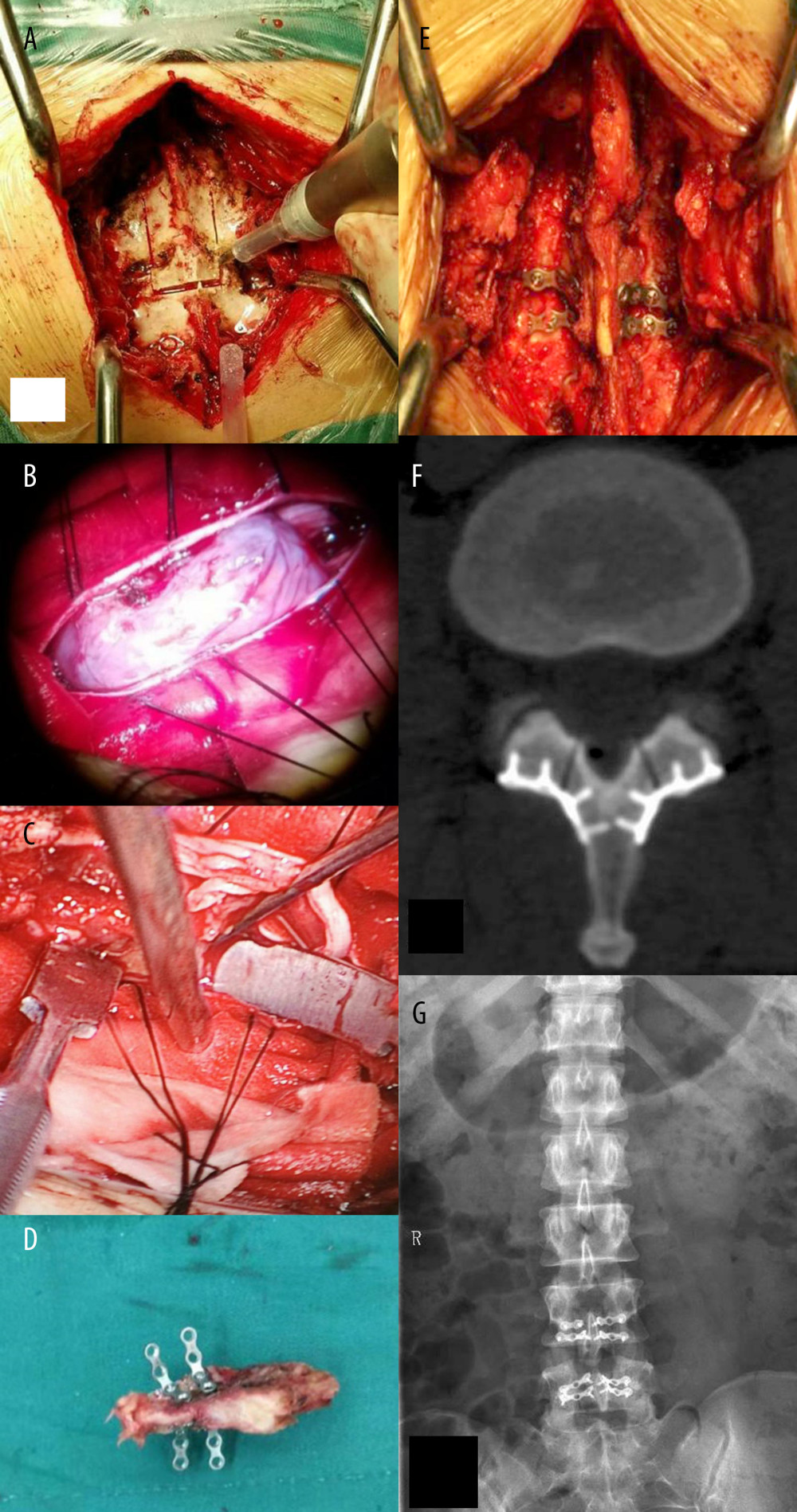 Figure 3. (A) Laminectomy under ultrasonic osteotome; (B) the tumor tissue under a microscope; (C) intraoperative image of the microscope screen; (D) the free lamina with a titanium plate; (E) replantation of lamina and spinous process in the original location; (F, G) postoperative images of the patient.
Figure 3. (A) Laminectomy under ultrasonic osteotome; (B) the tumor tissue under a microscope; (C) intraoperative image of the microscope screen; (D) the free lamina with a titanium plate; (E) replantation of lamina and spinous process in the original location; (F, G) postoperative images of the patient. In Press
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952